Abstract
Little is known about the role of romantic partner symptom accommodation in PTSD symptom maintenance. To explore the bidirectional associations of posttraumatic stress disorder (PTSD) symptoms and romantic partner symptom accommodation over time, military servicemen (n = 64) with symptoms of PTSD and their co-habiting heterosexual civilian romantic partners (n = 64) completed a 2-week daily diary study. Cross-lagged, autoregressive models assessed the stability of men’s PTSD symptoms and partners’ accommodation, as well as the prospective associations of earlier PTSD symptoms with later accommodation and vice versa. Analyses used Bayesian estimation to provide point estimates (b) and Credible Intervals (CIs). In all models, PTSD symptoms (total and individual clusters) were highly stable (b = 0.91; CI: 0.88–0.95), and accommodation was moderately stable (b = 0.48; CI: 0.40–0.54). In all models, earlier PTSD symptoms (total and clusters) were significantly, positively associated with later accommodation (b = 0.04; CI: 0.02–0.07). In contrast, earlier accommodation was significantly associated only with later situational avoidance (b = 0.02; CI: 0.00–0.07). Thus, PTSD symptoms may lead to subsequent accommodating behaviors in romantic partners, but partner accommodation seems to contribute only to survivors’ future situational avoidance symptoms. The findings reinforce the notion that PTSD symptoms have an impact on relationship behaviors, and that accommodation from partners may sustain avoidant behaviors in particular. Clinicians should attend to romantic partners’ accommodating behaviors when working with survivors.
Keywords: PTSD, romantic relationships, accommodation, maintenance
In the aftermath of traumatic events, some individuals develop posttraumatic stress disorder (PTSD). The disorder is characterized by intrusive reminders of trauma (i.e., intrusion), avoidance of trauma-related thoughts and places (i.e., situational avoidance), constricted affect and diminished interest in activities (i.e., emotional numbing), and alterations in arousal and reactivity (i.e., hyperarousal). Although several treatments for PTSD have been shown to be effective (Ponniah & Hollon, 2009), roughly 46% of patients are classified as treatment non-responders (Bradley, Greene, Russ, Dutra, & Westen, 2005). Thus, additional knowledge about the factors that influence the development and maintenance of PTSD is needed.
One such factor may be interpersonal relationships. Relationship problems are associated with more severe and chronic symptoms of PTSD (Evans, Cowlishaw, Forbes, Parslow, & Lewis, 2010; Evans, Cowlishaw, & Hopwood, 2009; Kaniasty & Norris, 2008), with many researchers hypothesizing a bidirectional cycle of individual and interpersonal problems related to PTSD (Campbell & Renshaw, 2016; Monson, Taft, & Fredman, 2009). Studies exploring specific behaviors of romantic partners of trauma survivors have largely focused on explicitly negative behaviors, such as hostility (e.g., Glenn, et al., 2002), but partners’ more seemingly benign or positive behaviors may also be associated with the maintenance of survivors’ PTSD symptoms. One such behavior that has been increasingly discussed in the context of PTSD is accommodation, or partners’ behavioral adjustments in response to symptoms that attempt to minimize relationship conflict and patient distress. Partner accommodation (sometimes called enabling or over-involvement) can entail well-intentioned attempts to help those who are suffering, but it has been associated with fewer treatment gains across a number of disorders, such as OCD, agoraphobia, social anxiety, and eating disorders (Boeding et al., 2013; Craske, Burton, & Barlow, 1989; Rapee, Peters, Carpenter, & Gaston, 2015; Salerno et al., 2016). Additionally, across disorders, partner accommodation is typically positively associated with partner distress and feelings of caregiving burden (e.g., Boeding et al., 2013; Sepulveda, Kyriacou, & Treasure, 2009).
In the context of PTSD, accommodation may include behavioral changes in the partner to accommodate survivors’ symptoms of intrusion (e.g., sleeping in separate beds in case of trauma-related nightmares), situational avoidance (e.g., allowing or encouraging the survivor to avoid going to places or doing things that make him/her uncomfortable), emotional numbing (e.g., avoiding physical contact with the survivor because he/she finds it uncomfortable), and arousal (e.g., “tiptoeing” around the survivor so as not to anger him/her). Partner accommodation of PTSD symptoms has been reported anecdotally in the literature for the last few decades (e.g., Figley, 1989; Maloney, 1988, Verbosky & Ryan, 1988), but only recently has the construct been explored empirically. Fredman, Vorstenbosch, Wagner, Macdonald, and Monson (2014) found that scores on a newly created measure of partner accommodation of PTSD were strongly associated with partners’ perceptions of trauma survivors’ PTSD symptom severity and with additional distress in romantic partners. Moreover, greater accommodation interfered with natural symptom remission in a sample of largely female, civilian trauma survivors (Fredman et al., 2016). However, prior work did not test the direction of effects over time, but rather looked at cross-sectional associations of PTSD and accommodation. Moreover, past research on accommodation of PTSD symptoms (Fredman et al., 2014, 2016) has not addressed the precise associations of accommodation with PTSD symptom clusters, to better understand how accommodation may be implicated in a lack of natural symptom remission.
A greater understanding of how partners’ accommodation is associated with survivors’ PTSD symptoms could influence treatment recommendations and guide clinical practice for trauma survivors. Indeed, accommodation likely follows perceptions of PTSD symptoms, as evidenced by prior research (e.g., Fredman et al., 2014). However, it could also serve to exacerbate or maintain specific PTSD symptoms, though this hypothesis has not yet been tested. For instance, partners may be more likely to accommodate PTSD symptoms of survivors who are extremely anxious when out in public places, or hostile when discussing trauma. On the other hand, when partners accommodate by avoiding certain topics of discussion or facilitating survivors’ situational avoidance, survivors do not benefit from opportunities to practice distress tolerance or opportunities for natural exposure that can help them learn over time that many avoided situations are safe. Similarly, a survivor with angry outbursts may prompt attempts by partners to avoid confrontation, and partners who avoid confrontation may inadvertently reduce the need for survivors to work toward reducing such behaviors. In sum, partners may be more likely to accommodate PTSD symptoms when they are more severe and pronounced, but symptoms may also be more likely to remain severe and pronounced without opportunities to diminish through exposure. Indeed, past research suggests that overuse of avoidant coping strategies (like those encouraged by accommodation) is associated with PTSD symptom maintenance, particularly for those who are high in physiological reactivity to trauma reminders (e.g., Pineles et al., 2011).
The aim of the present study was to explicitly test the direction of associations between romantic partners’ behavioral accommodation and survivors’ PTSD symptoms, using a 2-week, daily diary design. Daily diary studies allow for evaluation of directionality of effects among variables and are particularly useful when examining dynamic constructs, such as behavior or mood (Laurenceau & Bolger, 2005). Although a small number of studies have examined PTSD through diary studies (e.g., Kaysen et al., 2014; Naragon-Gainey, Simpson, Moore, Varra, & Kaysen, 2012; Tarrier, Sommerfield, Reynolds, & Pilgrim, 1999), this study is the first daily diary study of trauma survivors and their partners. Based on prior research linking partner accommodation with psychiatric symptoms, we expected higher PTSD symptoms in current and former service members (SMs) on a given day to predict greater partner accommodation behavior on the next day, and vice versa.
To understand which PTSD symptoms are most likely to be associated with partner accommodation, we also evaluated associations of accommodation with each specific PTSD symptom cluster (American Psychiatric Association, 1994). Accommodation should logically occur in response to partners’ perceptions of PTSD symptoms, and thus we expected that accommodation would temporally follow PTSD, but theory also suggests that accommodation may help maintain or even exacerbate PTSD symptoms. Based on prior research suggesting that romantic partners can accommodate each type of PTSD symptom (Fredman et al., 2014), we hypothesized that the severity of each symptom cluster on a given day would be positively associated with levels of partner accommodation on the next day, and vice versa. However, given the conceptual similarities between the situational avoidance cluster of PTSD and the types of avoidance common to other anxiety disorders (e.g. social phobia, panic disorder with agoraphobia), we hypothesized a more robust effect for situational avoidance. As one of the most effective treatments for anxiety disorders is exposure therapy, which reduces conditional fear through repeated presentation of the conditional stimulus in the absence of the unconditional stimulus, any impediment to exposure should interfere with reduction of conditional fear and associated symptoms (Craske, Treanor, Conway, Zbozinek, & Vervliet, 2014). Indeed, there is a particularly strong link between accommodation behaviors, which may include a partner serving as a safety signal or inadvertently preventing opportunities for inhibitory learning, and reduced effectiveness of in vivo exposure in anxiety disorders (e.g., Craske et al., 1989; Rapee et al., 2015). Thus, we hypothesized that the bidirectional association would be strongest between symptoms of situational avoidance and partner accommodation behaviors.
Method
Participants
The sample included 64 couples composed of male SMs and female spouses/partners (partners). SMs had a mean age of 34.94 years (SD = 7.53), and most were white (84.4%), with approximately 58% of the sample having completed at least some college. SMs had an average of 2.3 (SD = 1.18) deployment to Iraq and/or Afghanistan and were mostly members of the Army (81.3%). Active duty SMs comprised 35.9% of the sample, with 17.2% of the sample reporting National Guard/Reserves (NG/R) status, and 46.9% reporting veteran status. Partners had a mean age of 34.14 years (SD = 7.48) and most were white (84.4%), with 42% having completed at least some college. Nearly half (48.4%) of the sample had an annual household income of less than $50,000. Approximately 94% of couples reported that they were married, with a mean relationship length of 9.45 years (SD = 5.86). SMs’ and partners’ scores on a measure of relationship intimacy (Personal Assessment of Intimacy in Relationships; Schaefer & Olson, 1981) were comparable to prior samples of Veterans with PTSD and lower than Veterans without PTSD (e.g., Carroll, Reuger, Foy & Donahoe, 1985). Additionally, SM and partner reports of baseline relationship support and conflict (Quality of Relationships Inventory; Pierce, Sarason, & Sarason, 1991) were comparable to community couples with mild depression (Blais & Renshaw, 2014). SMs and partners did not significantly differ on relationship support or conflict, though partners reported significantly lower intimacy (M = 11.42, SD = 5.78) than SMs (M =13.73, SD =5.67), t(63) = −3.57, p < .01. Of note, approximately 78% of SMs were seeking treatment for any psychological disorder at the time of baseline assessments, with 62.5% receiving medication, and 59.4% receiving therapy. Only 25% of partners reported that they had ever undergone treatment for a psychological disorder. SMs who noted that they were receiving psychological treatment for comorbid disorders listed depression, anxiety, and insomnia, all of which are highly overlapping with symptoms of PTSD.
Procedure
All procedures were approved by the [redacted] Institutional Review Board, as well as the NIH Office of Human Subjects Research Protections. Recruitment occurred primarily via notices in online military community and social media sites, Family Readiness Groups, military psychology listservs, and blog and social media posts by military/veteran research organizations. Recruitment materials directed potential participants to the study website, which described the purpose of the study and provided an overview of the procedures. This basic information was followed by a link to a list of resources and referrals for those needing support for relationship, family, or individual mental health issues (both military and civilian resources), and study staff contact information. All individuals who visited the site received this information, regardless of whether they chose to participate or were eligible.
After participants received the list of resources, they were presented with a series of screening and eligibility questions. To be included in the study, both members of the couple needed to be in a committed romantic relationship for a minimum of 6 months, currently cohabitating, minimum age of 18 years, fluent in English, and able to access the Internet daily. Additional inclusion criteria for SMs were male sex, current or former military status, at least one deployment since 9/11/2001, and a score on the PTSD Checklist (see below) of at least 35, which is above the cut-off scores used to identify SMs with a clinical diagnosis of PTSD in primary care settings (Bliese et al., 2008). Partners were required to be female and to have no current or prior military service. Participants who failed either of two English grammar comprehension questions, or reported other characteristics that did not meet eligibility criteria (e.g., no partner who would be interested in participating) received “not eligible” messages after the screening questions and were prevented from providing consent.
Individuals whose responses to the screening questions indicated that they were potentially eligible were directed to a page with the consent form, which was followed by a series of consent comprehension questions. Any person who indicated that they did not agree to the conditions stipulated in the consent or who failed the consent form comprehension questions was directed to a page that provided them with contact information for the research team for any questions. No identifying information beyond IP addresses was collected to this point, thus preserving anonymity. Respondents who provided consent but had IP addresses from unanticipated locations (e.g., Argentina) received additional email contact from study staff to confirm their permanent location and reason for unanticipated location (n = 6). Additionally, study staff reviewed IP addresses in order to identify any participants who received a message indicating ineligibility but then passed the screen again with altered responses (n = 9).
Upon consenting, SM participants responded to a series of questions about their military service (e.g., permanent duty station, UIC code, military occupation specialty). Responses were subsequently reviewed by study staff (including one active-duty SM and one reserve SM) to verify military status by ensuring that participants’ responses were consistent and logical. After SMs recorded their military information, they completed the PTSD Checklist – Military version (see Measures). After consenting and completing screening measures, participants provided the name and email address of their romantic partner, and indicated whether staff could contact their partner if the partner had not already completed the screener. Names and email addresses were matched within couples, and each member of the couple received an individual and couple ID.
Each member of eligible couples received an email to their personal email address with a unique link to their own baseline questionnaire and unique ID numbers. Couples were compensated $25 for completing baseline questionnaires. After both members of the couple completed baseline questionnaires, each partner then received an email with instructions for beginning the daily diary portion of the study. Participants completed the daily diary measures each evening for 14 consecutive nights, with instructions to complete the survey within the hour before going to bed, to capture as much of the day as possible. Study staff analyzed time stamps each day and communicated with participants following missing days of diary data or inappropriately time-stamped entries, in order to encourage better compliance and answer procedural questions. Couples were paid $70 for completing the diary, and were rewarded with financial bonuses of $15 per participant for completing at least 5 diary days per diary week.
Attrition and Compliance
In total, 670 individuals clicked on the study link. Of those individuals, 226 partners and 156 SMs completed the eligibility and consent screen without being ruled out based on screening eligibility criteria. Twenty-three SMs had appropriate military information but reported PCL-M scores below 35. From the remaining individuals, we matched and identified 96 eligible couples who were invited to participate. Of these matched couples, 78 partners and 72 SMs completed baseline questionnaires, with 70 couples who had baseline questionnaire data from both partners. These 70 couples were subsequently invited into the daily diary portion of the study. Six couples opted to withdraw from the study after failing to complete a sufficient number of entries, leaving a final sample of 64 couples. Participants who completed only baseline questionnaires and those who completed baseline questionnaires and the daily diary did not differ on any demographic variable or variable of interest tested, including age, race, number of deployments, SM PTSD, or partner accommodation (ps >.10).
Of these 64 couples, 88% of SMs and 89% of partners completed at least 10 of 14 entries, with 34% of SMs and 30% of partners completing all 14 diary entries. Based on correspondence with numerous SMs who indicated that their insomnia led them to “go to bed” in the late morning, we classified any diaries completed after noon as the same “psychological day” and any entries completed prior to noon as the previous “psychological day” (Nezlek, 2012). If participants completed multiple entries on the same day, we retained the first entry if all entries were complete; otherwise we retained the most complete entry. In total, the 64 SMs provided 785 days of diary data, while the 64 partners provided 792 days of diary data.
Measures
PTSD Checklist – Military Version (PCL-M; Weathers, Litz, Herman, Huska, & Keane, 1993)
Only SMs completed the PCL-M, which is a 17-item, self-report, Likert-type scale that measures the degree to which participants have been bothered by military-related PTSD symptoms in the past month from 1 (not at all) to 5 (extremely). Each scale item is derived from a criterion symptom of PTSD as defined by the DSM-IV (American Psychiatric Association, 1994). Respondents receive an overall PTSD severity score, which is the sum total of all item responses. Suggested cut-off scores for estimating a clinical diagnosis of PTSD range from 30–34 for SMs seen in primary care settings (Bliese et al., 2008) to 50 for large-scale military prevalence studies (Weathers et al., 1993). Consistent with our inclusion criteria (≥35), our sample’s mean PCL-M total score suggested a highly symptomatic sample (see Table 1 for details). Internal consistency in the present sample was high for the total scale (α = .93).
Table 1.
Means and Standard Deviations of Baseline and Daily PTSD and SORTS Measures
| Baseline | Daily | |
|---|---|---|
|
| ||
| Scale | M (SD) | M (SD) |
| PCL-M (Baseline) | ||
| Total | 63.55 (13.07) | 52.29 (17.36) |
| Intrusion | 17.95 (4.33) | 13.28 (6.01) |
| Situational Avoidance | 7.68 (1.88) | 6.23 (2.81) |
| Emotional Numbing | 17.41 (5.31) | 14.88 (6.05) |
| Hyperarousal | 20.51 (4.01) | 17.84 (5.25) |
| SORTS | ||
| Total | 43.20 (22.43) | N/A |
| Frequency | 21.77 (12.18) | 7.16 (6.54) |
| Intensity | 20.98 (11.43) | N/A |
Note: PCLM = PTSD Checklist – Military Version; SORTS = Significant Others’ Responses to Trauma Scale. The baseline version of the SORTS frequency scale uses 14 items, while the daily version of the SORTS frequency scale uses 8 items.
In addition, respondents can receive individual symptom cluster scores, which are calculated by summing the item responses for each cluster. Based on a 4-cluster emotional numbing model, the intrusion, emotional numbing, and hyperarousal subscales are all 5 items, with total subscale scores ranging from 5 to 25. The situational avoidance subscale is two items, with the subscale score ranging from 2 to 10. Internal consistencies in the present sample were also strong for the individual cluster scales of intrusion (α = .88), situational avoidance (α = .79), emotional numbing (α =.87), and hyperarousal (α = .84).
We assessed daily PTSD symptoms over the previous 24 hours using the PCL-Military version modified for daily use, consistent with Naragon-Gainey et al.’s (2012) use of a daily version of the PCL-Civilian version. The measure retains the items and response scale used in the monthly retrospective PCL, with instructions amended to refer to the current day. Various authors (e.g., Bolger & Laurenceau, 2013; Shrout & Lane, 2012) have recommended reporting both within-person (RC) and between-person (R1F) reliability for intensive longitudinal measures. Consistent with the reliability of the PCL-C in Naragon-Gainey et al.’s (2012) sample, the daily version of the PCL-M in our sample demonstrated acceptable to good RC and very high R1F for the total scale (.88, .98), as well as for the cluster subscales of intrusion (.79, .95), situational avoidance (.61, .91), emotional numbing (.72, .95), and hyperarousal (.74, .94).
Significant Others’ Responses to Trauma Scale (SORTS; Fredman et al., 2014)
Only partners completed the SORTS, which is a 14-item measure of partners’ accommodation of survivors’ PTSD symptoms. Each item consists of two questions. First, respondents indicate how often they have performed a particular behavior over the past month from 0 (Not at all) to 4 (Daily). Second, they indicate how distressed they are by engaging in the behavior from 0 (Not at all) to 4 (Extremely), or how much effort they exerted on the behavior from 0 (None) to 4 (An extreme amount). Items are summed to provide a total score, a frequency score, and an intensity score. The original measure validation study of the SORTS showed the measure to demonstrate strong internal consistency (α = .93 for total, .86, and .87 for frequency and intensity subscales, respectively), test-retest reliability, and construct validity via strong positive correlations with partners’ perceptions of patients’ PTSD symptoms, and strong positive associations with individual and relationship distress (Fredman et al., 2014). Our sample demonstrated levels of accommodation comparable to or higher than those of Fredman et al.’s (2014) normative sample (see Table 1). Internal consistency in the present study was high (α = .95 for total score, .92 for frequency, .90 for intensity). Additionally, discriminant validity of the baseline SORTS was assessed in this sample via bivariate correlations with partners’ reports of willingness to offer support to SMs (r = −.00, p =.99), and SMs’ reports of felt relationship support (r = −.23, p = .07), all of which demonstrated near-zero or negative associations with partner accommodation.
We assessed frequency of daily accommodation in partners with 8 of the 14 items from the SORTS to reduce the burden for partners completing two weeks of daily data. The 8 items selected were those with the highest item-total correlations with the full measure in the development study (personal communication, S. Fredman, February 27, 2014). Using the same 0 to 4 Likert scale as the frequency items of the baseline version, partners were asked how often over the previous 24 hours they felt the need to: 1) Avoid your spouse/partner because of his irritable or angry mood?; 2) “Bite your tongue” or hold back from trying to discuss any relationship issues with your spouse/partner?; 3) Help your spouse/partner with a task because he was having trouble concentrating?; 4) Make excuses to others for your spouse/partner’s behavior or try to manage his relationships with other people?; 5) “Tiptoe” around your spouse/partner so as not to anger him?; 6) Not share your own feelings or concerns with your spouse/partner due to concerns that he would become upset?; 7) Change your routine due to your spouse/partner’s difficulties?; 8) How much have you modified your leisure activities due to your spouse/partner’s difficulties? All daily SORTS items were significantly, positively correlated with all daily PTSD symptom clusters (.08 < all rs < .31), though hyperarousal symptoms were most strongly correlated with SORTS items.
Reliabilities for this adapted measure were excellent (RC = .90; R1F = .88). We also tested the convergent validity of the amended daily SORTS measure with the full baseline SORTS by conducting a two-level multilevel model, in which partners’ trait-level accommodation was a Level-2 predictor of their daily accommodation. Results indicated that the daily version of the SORTS was strongly associated with the full version (converted r = .57). Of note, the baseline SORTS frequency score is based on 14 items, while the daily SORTS frequency score is based on 8 items. Thus, the maximum possible baseline SORTS frequency is 56, while the maximum possible daily SORTS frequency is 32.
Analytic Plan
We first calculated descriptive statistics to characterize our sample. Subsequently, we explored the associations of SM PTSD symptoms with partner accommodating behaviors using path analysis in Amos 19.0 (Arbuckle, 2010). To explore the temporal precedence of SM PTSD symptoms and partner accommodation, we used a cross-lagged autoregressive model, which allows for explicit tests of hypothesized reciprocal associations (Selig & Little, 2012). Cross-lagged autoregressive models include three major components: stability paths, covariances, and cross-lagged paths. Stability paths allow each variable to be predicted by the same variable at the prior time point (e.g., SMs’ PTSD symptoms on Day 2 predicted by SMs’ PTSD on the Day 1, etc.). Stability paths for PTSD were constrained to be equal across all time intervals. Stability paths also were estimated for partners’ accommodation and constrained to be equal across intervals. Covariances were modeled between PTSD symptoms and accommodation within each time point to account for same-day associations between those variables. As Day 1 variables are exogenous, the covariance between Day 1 PTSD and Day 1 accommodation was not constrained to be equal to subsequent covariances, but all subsequent covariances between the error terms of PTSD and accommodation were constrained to be equal across time points.
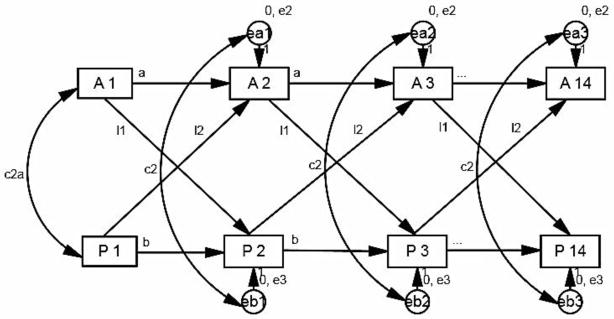
Finally, our primary hypotheses were addressed by evaluating models with cross-lagged paths between PTSD and accommodation. For a given day, PTSD was predicted by accommodation on the previous day, and accommodation was predicted by previous day PTSD (see Figure 1). All cross-lagged paths from PTSD to accommodation were constrained to be equal to one another, and all cross-lagged paths from accommodation to PTSD were also constrained to be equal to one another. We first conducted a model with total PTSD symptoms leading to later accommodation and vice versa. We then conducted a series of four additional models, which substituted each individual PTSD cluster (intrusion, situational avoidance, emotional numbing, hyperarousal) for the total PTSD score in our baseline model.
Figure 1. Base cross-lagged autoregressive model without path estimates.
Note: c2a= 1st day covariance; c2 = remaining day covariances; l1= path from earlier accommodation to later posttraumatic stress disorder (PTSD); l2= path from earlier posttraumatic stress disorder to later accommodation; A1–14 = accommodation on days 1–14; P1–14 = PTSD on days 1–14; ea = error variance of accommodation; eb = error variance of PTSD.
We used Bayesian estimation to obtain point estimates and credible intervals (CIs) for our parameter estimates. Of note, a 95% CI in Bayesian estimation connotes a 95% probability that the population value falls within the limits of the credible interval. We treated paths in which the 95% CI did not contain 0 as significant. Bayesian estimation is advantageous for non-normal data and small sample sizes (Ozechowski, 2014; Price, 2012, Van de Schoot, Broere, Perryck, Zondervan-Zwijnenburg, & van Loey). We used uninformed priors with flat distributions. Finally, we used the posterior predictive p as an indicator of model fit, with values close to .50 representing good-fitting models (Ozechowski, 2014). Regarding missing data, participants completed all questions on a particular day if they selected to complete the diary that day. Thus, missed days are not treated as missing data, but rather treated as fewer observations per subject (Nezlek, 2011). Nonetheless, Bayesian estimation is similar to stochastic regression imputation of data, though it assumes that parameters are estimated rather than known.
To conservatively test our results, we re-analyzed each model while controlling for duty status (with separate models for active duty, veteran, or NG/R status), military branch, number of deployments, SM race, partner race, relationship length, and income (each variable was controlled in a different model, to allow for model convergence). In most cases, the patterns of significance for the cross-lag paths did not change, and path estimates in these models were largely identical to the base model. When CIs for the estimates did change, they were typically wider, suggesting that the increased complexity of the models added greater instability to our confidence in the estimate.1 For reasons of parsimony, we are presenting results of models without covariates.
Results
Table 1 provides means and standard deviations of all baseline and daily measures. Notably, baseline levels of SMs’ PTSD symptoms and partners’ accommodation were somewhat higher than their respective daily levels (even after accounting for differences in the number of items on baseline and daily SORTS). This pattern is consistent with prior studies assessing daily PTSD (e.g., Naragon-Gainey et al., 2012). Also, accommodation frequency may be higher in retrospective than daily reports due to the nature of reporting on specific behaviors, which are more accurately captured on a daily level (cf. Gilmore, Leigh, Hoppe, & Morrison, 2010; Margraf, Taylor, Ehlers, Roth, & Agras, 1987; McAuliffe, DiFranceisco, & Reed, 2007), or the possibility of a ceiling effect regarding behaviors that can/should be exhibited in one day. Of note, SMs’ PTSD and partners’ accommodation were correlated on both the baseline (r = .60, p < .00) and daily (e.g., r = .39, p < .01 for first day) measures. The intraclass correlation for daily PTSD was .87, whereas the intraclass correlation for daily partner accommodation was .86, indicating that 87% of the variability in PTSD and 86% of the variability in accommodation was due to between-couple differences rather than within person variability over time.
Cross-lagged autoregressive models
The overarching model is shown in Figure 1. Posterior predictive p was .50 for all models reported below, indicating excellent fit. Table 2 contains all point estimates, standard deviations, and 95% CIs for all base models. Amos software provides only unstandardized estimates for Bayesian estimation. Thus, point estimates in Table 2 are unstandardized.
Table 2.
Unstandardized Point Estimates and CIs for Autoregressive Cross-lagged Models
| Parameters | Model 1: Total PTSD | Model 2: Intrusion | Model 3: Situational Avoidance* | Model 4: Emotional Numbing | Model 5: Hyperarousal | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Estimate (SD) | 95% CI | Estimate (SD) | 95% CI | Estimate (SD) | 95% CI | Estimate (SD) | 95% CI | Estimate (SD) | 95% CI | |
| Accommodation Stability | 0.48 (0.03) | 0.40 – 0.54 | 0.48 (0.04) | 0.41 – 0.54 | 0.49 (0.03) | 0.42 – 0.55 | 0.48 (0.03) | 0.42 – 0.54 | 0.47 (0.03) | 0.41 – 0.53 |
| PTSD stability | 0.91 (0.02) | 0.88 – 0.95 | 0.91 (0.02) | 0.88 – 0.94 | 0.85 (0.02) | 0.81 – 0.88 | 0.91 (0.02) | 0.88 – 0.94 | 0.84 (0.02) | 0.80 – 0.88 |
| Accom→PTSD | −0.02 (0.05) | −0.11 – 0.07 | −0.02 (0.05) | −0.11 – 0.06 | 0.02 (0.01) | 0.00 – 0.04 | 0.00 (0.02) | −0.03 – 0.03 | −0.01 (0.02) | −0.04 – 0.03 |
| PTSD→Accom | 0.04 (0.01) | 0.02 – 0.07 | 0.04 (0.01) | 0.02 – 0.06 | 0.24 (0.08) | 0.09 – 0.38 | 0.11 (0.03) | 0.05–0.17 | 0.12 (0.04) | 0.05 – 0.19 |
Note: CIs = Bayesian credible intervals; PTSD = Posttraumatic stress disorder; Accom = partner accommodation.
Estimate for Accom → PTSD path for situational avoidance contains 0 as a result of rounding.
Total PTSD
Consistent with the high ICCs, stability paths for both accommodation and PTSD were highly significant. The cross-lagged path from earlier total PTSD to later accommodation was positive and significant, while the cross-lagged path from earlier accommodation to later total PTSD was non-significant.
Intrusion
Stability paths for both accommodation and intrusion were highly significant. As with total PTSD, the cross-lagged path from earlier intrusion to later accommodation was positive and significant, while the cross-lagged path from earlier accommodation to later intrusion was non-significant.
Situational Avoidance
The cross-lagged model linking earlier situational avoidance to later accommodation and vice versa demonstrated a different pattern of results from previous models. Similar to earlier models, stability paths for accommodation and situational avoidance were highly significant, and the cross-lagged path from earlier situational avoidance to later accommodation was positive and significant. Of note, the coefficient for this path was much stronger. Moreover, the path from earlier accommodation to later situational avoidance was also positive and significant.
Emotional Numbing
In the model isolating emotional numbing, stability paths for both accommodation and emotional numbing were highly significant. The cross-lagged path from earlier numbing to later accommodation was positive and significant, while the cross-lagged path from earlier accommodation to later numbing was non-significant.
Hyperarousal
Finally, in the model isolating hyperarousal symptoms, stability paths for both accommodation and hyperarousal were highly significant. As with intrusion, the cross-lagged path from earlier hyperarousal to later accommodation was positive and significant, while the cross-lagged path from earlier accommodation to later hyperarousal was non-significant.
Discussion
The current study is the first to assess the associations of PTSD symptoms and partner behaviors on a daily level in a sample of military couples. Specifically, we analyzed associations of SMs’ daily PTSD symptoms and partners’ daily levels of accommodation across a 14-day period. For total PTSD symptoms and three of four specific symptom clusters (intrusion, emotional numbing, hyperarousal), SMs’ symptoms predicted subsequent (next-day) levels of accommodation in partners, but partners’ accommodation did not predict future (next-day) levels of PTSD in SMs. In contrast, for situational avoidance, not only did SMs’ symptoms predict subsequent levels of accommodation in partners, but partners’ accommodation was also associated with modest increases in SMs’ subsequent avoidance.
When interpreting these results, one must first consider that PTSD symptoms were highly stable across time. This indicates the possibility that certain aspects of self-reported PTSD become almost trait-like for some survivors, with little day-to-day variability. In the only other study to explore daily PTSD symptom stability to date (Naragon-Gainey et al., 2012), daily symptom stability was fairly low across a 30-day period. Notably, the sample consisted of subclinical civilian female sexual assault survivors (only 20% of the sample met criteria for current PTSD), which may differ in meaningful ways from our male SM sample (all of whom met minimum criteria for PTSD diagnosis based on primary care cutoffs recommended by Bliese et al., 2008). For SMs and veterans, cultural factors may encourage consistent identification with or presentation of a PTSD diagnosis or significant symptomatology (see Frueh et al., 2005; Yehuda, Morris, Labinsky, Zemelman, & Schmeidler, 2007). For example, a minority of veterans in our sample may have required a PTSD diagnosis for service connection compensation, while other SMs may have participated immediately after completing time in a Warrior Transition Battalion. Both subgroups in our sample may have strongly identified with the “PTSD” label as part of their identity, which could have enhanced the stability of their reported symptoms. Further research is needed, however, to determine whether such factors play a role in stability of reported symptoms.
In contrast, although partners’ accommodation behaviors were moderately stable across time, they were more variable than PTSD symptoms. Thus, consistent with predictions, partners’ accommodating behaviors are likely highly dependent on partners’ perceptions of PTSD symptoms, which may vary day-to-day. Notably, all symptom clusters were independently associated with partners’ later accommodating behaviors. This finding lends validity to the baseline measure of accommodation (Fredman et al., 2014), which attempted to capture potential accommodation of all symptoms of PTSD. It also indicates that partners may respond to perceptions of any PTSD symptoms with accommodating behaviors, suggesting the behavior is somewhat pervasive.
If accommodating behaviors functioned purely as responsive support to perceptions of PTSD symptoms, these findings would paint a picture of adaptively functioning interactions between partners in couples where one member survived trauma. However, partner accommodation is linked with greater distress in both trauma survivors and partners (e.g., Fredman et al., 2014; Fredman et al., 2016), which also predicts worse outcomes for those with PTSD (e.g., Evans et al., 2009). Thus, individual and conjoint treatments for PTSD should clearly lay out a treatment rationale for both members of the couple and provide partners with psychoeducation about PTSD symptoms to stem potentially distressing, burdensome, or unhelpful accommodating behaviors. Additionally, and equally as important, PTSD treatments should provide partners with alternative ways of supporting survivors (instead of symptom accommodation). Finally, treatments should further emphasize traditional conflict-management strategies (e.g., communication training, active listening, relaxation strategies). These treatment components may prove helpful in curtailing accommodating behaviors, which may arise as a result of incomplete or faulty beliefs about treatment or accommodation, or in an effort to avoid PTSD-related conflict.
In spite of the overall stability of PTSD symptoms, we did find that greater accommodation by partners predicted modest increases in SMs’ later situational avoidance. These findings, though preliminary, suggest that accommodating behaviors may be implicated in the perpetuation of avoidance, in particular. This possibility is consistent with prior research on accommodation in a number of anxiety disorders that are characterized in large part by direct avoidance of feared stimuli (e.g., Boeding et al., 2013; Craske et al., 1989; Rapee et al., 2015). The foundation of many empirically supported treatments for anxiety disorders is exposure to feared stimuli (e.g., Deacon & Abramowitz, 2004), and most of the primary empirically supported treatments for PTSD incorporate significant elements of exposure, as well (e.g., Foa, Hembree, & Rothbaum, 2007; Resick & Schnicke, 1993). By allowing or even encouraging SMs to avoid situations that are anticipated to cause distress, romantic partners may inadvertently interfere with the natural learning that occurs when feared stimuli are confronted, thus perpetuating avoidance.
Awareness of these associations is important for clinicians conducting both individual and couple therapy for PTSD. Indeed, assessment of romantic partners’ responses to PTSD symptoms may aid in facilitating in vivo exposures. For instance, if partners express doubt in the effectiveness or safety of exposure therapies, or even encourage survivors to avoid upcoming exposure assignments, survivors are less likely to engage in treatment. Moreover, even if survivors do engage in exposure-based treatment for PTSD, partners who are not aware of the adverse effects of accommodation may be likely to continue to accommodate avoidance to simplify their daily lives, potentially interfering with the full effects of treatment. In recent years, conjoint therapies for PTSD, such as cognitive behavioral conjoint therapy for PTSD (Monson & Fredman, 2012) and structured approach therapy (Sautter, Glynn, Arseneau, Cretu, & Yufik, 2014), have emerged. These therapies do much to intervene in this process by incorporating partners directly into treatment. Partners who are trained to serve as “coaches” in exposures may be more likely to aid survivors in completing exposure assignments and treatment in general. Thus, an understanding the reciprocal associations of situational avoidance and partner accommodation is useful in explaining the treatment rationale to partners and enhancing the effectiveness of empirically-supported treatments for PTSD.
Though situational avoidance appears to be at least partially responsive to partner accommodation, our findings suggest that other symptom clusters were not. Existing research on the mechanisms posited to maintain symptoms of intrusion, numbing, and hyperarousal does tend to implicate intraindividual, rather than interpersonal, processes. Studies have suggested that survivors’ dysfunctional interpretations, rumination, distraction, and thought suppression may be involved in the maintenance of intrusion symptoms (Ehlers & Steil, 1995; Steil & Ehlers, 2000). Other research indicates that numbing symptoms are maintained as a consequence of excess arousal (Tull & Roemer, 2003), or in tandem with the maintenance of situational avoidance, as overlearned escape responses (Keane, Fairbank, Caddell, Zimering, & Bender, 1985). Furthermore, primarily physiological mechanisms have been implicated in the maintenance of hyperarousal symptoms (O’Donnell, Hegadoren, & Coupland, 2004; Yehuda et al., 2007). At the same time, it is plausible that other interpersonal mechanisms may still play a role in the maintenance of these symptoms. For instance, romantic partners who feel overburdened in caring for survivors may be more likely to initiate conflict, which may sustain survivors’ irritability and anger symptoms. Similarly, survivors’ dysfunctional cognitions about interpersonal relationships may prompt alienation from significant others, thereby maintaining estrangement and emotional numbing. However, results from this study suggest that partners’ accommodation may not be as relevant to the maintenance of these specific symptoms, though future research is warranted.
Limitations, Strengths, and Future Directions
This study has important limitations. First, though all SMs had a score of at least 35 on the PCL-M, we did not use the Clinician Administered PTSD Scale (Blake et al., 1995) or another interview-based measure. Though prior research has demonstrated moderate concordance between clinician-rated diagnoses and the PCL-M (e.g., Macdonald, Greene, Torres, Frueh, & Morland, 2013), clinician-rated PTSD diagnoses would provide enhanced confidence in symptom levels.
Second, the sample was largely White and consisted solely of heterosexual, male SM/female partner couples. It is critical to extend this type of research to other racial/ethnic groups, female survivor/male partner couples (both civilian and military), and same-sex couples, to determine whether or not these findings can be generalized. Based on caregiving and social support literature, it is easy to imagine that accommodation would be more frequently enacted by women in relationships with more stereotypical gender roles (e.g., Freedman, 1993; Taylor et al., 2000). In addition, accommodation by partners of survivors of other types of trauma may take different forms. For instance, accommodation of sexual assault survivors’ symptoms may be more focused on facilitating avoidance of sexual activity, which may have additional impacts on relationship intimacy and the frequency of accommodative behaviors.
Our study was also limited by a lack of reports of all constructs by both partners (e.g., partners did not report on SMs’ PTSD symptoms, and SMs did not report on partner accommodation). Such reports would have allowed analysis of the degree to which survivors found the behaviors to be helpful versus intrusive or undermining. We were also unable to assess the degree to which accommodating behaviors were enacted in response to direct requests from SMs. It is possible that some level of accommodating behaviors may be perceived as supportive and responsive or even necessary, due to SMs’ functional impairment. Moreover, partners may continue to accommodate symptoms both in response to perceptions of symptoms as well as in response to direct requests. Along these lines, we were also unable to determine the degree to which partners’ accommodation of SMs’ PTSD symptoms actually resulted in (or was prompted by) functional impairment for SMs. Future research that obtains objective measures of functional impairment will be important for quantifying the level of PTSD interference in survivors’ and partners’ lives (as symptoms are related to but distinct from impairment; McKnight & Kashdan, 2009). Furthermore, although our daily measure of accommodation demonstrated good concordance with the full measure, both measures may be limited in their ability to capture the heterogeneity of symptom accommodation. The daily version in particular may not have been as sensitive to emotional numbing or intrusion symptoms, which may demonstrate changes in response to accommodation over longer periods of time. Indeed, as accommodation maintains daily situational avoidance, there may be residual increases in emotional numbing, irritability, or sleep difficulties over a period of weeks or months. Such effects would not be noticeable over the time frame selected for this study, and should be investigated in future research.
Finally, although we obtained a large number of within-person data points in people’s naturalistic environment, the sample size was relatively small. The use of Bayesian estimation helps address some of the problems with a small sample size, but a larger sample of couples would be preferable to have greater confidence in the results.
These limitations notwithstanding, the current study is the first to gather data at several time points from both members of military couples and to explore hypothesized directional associations of PTSD symptoms with relational processes. This design capitalized on the perspective of each member in the couple to more fully capture dyad-level processes. Moreover, by using a daily diary format, we minimized retrospective bias and captured a more accurate estimate of phenomena, while also allowing for tests of directionality. By using Bayesian estimation of our models, we were able to avoid problems with potentially reduced power in spite of our small sample (Price, 2012). Our results suggest that PTSD symptoms are likely to prompt romantic partners’ accommodation behaviors over time, with some suggestion that such accommodation may be one potential mechanism of the maintenance of trauma survivors’ situational avoidance symptoms over time.
Highlights.
We collected 14 nightly reports of PTSD and accommodation from military couples.
PTSD symptoms are associated with later romantic partner symptom accommodation.
Partners’ earlier accommodation may contribute to avoidance symptom maintenance.
Daily interpersonal processes in military couples may influence PTSD over time.
Acknowledgments
This research was supported in part by grants from the National Institute of Mental Health under Ruth L. Kirschstein National Research Service Award number 1F31MH098581-01A1, the International Society of Traumatic Stress Studies, and the American Psychological Foundation awarded to Sarah B. Campbell, M.A.
Footnotes
Results of these additional models controlling for covariates are available from the first author upon request.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Arbuckle JL. IBM SPSS® AmosTM 19 user’s guide. Crawfordville, FL: Amos Development Corporation; 2010. [Google Scholar]
- Blais RK, Renshaw KD. Perceptions of partners’ attributions for depression in relation to perceptions of support and conflict in romantic relationships. Journal of Marital & Family Therapy. 2014;40:498–508. doi: 10.1111/jmft.12055. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the Primary Care Posttraumatic Stress Disorder Screen and the Posttraumatic Stress Disorder Checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology. 2008;76:272–281. doi: 10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- Boeding SE, Paprocki CM, Baucom DH, Abramowitz JS, Wheaton MG, Fabricant LE, Fischer MS. Let me check that for you: Symptom accommodation in romantic partners of adults with Obsessive–Compulsive Disorder. Behaviour Research and Therapy. 2013;51:316–322. doi: 10.1016/j.brat.2013.03.002. [DOI] [PubMed] [Google Scholar]
- Bolger N, Laurenceau J-P. Intensive longitudinal methods: An introduction to diary and experience sampling research. New York, NY: Guilford Press; 2013. [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Renshaw KD. Combat veterans with PTSD and their partners: Interpersonally based behaviors and cognitions as mechanisms of distress. In: MacDermid Wadsworth S, Riggs D, editors. War and Family Life. New York, NY: Springer; 2016. pp. 55–75. [Google Scholar]
- Carroll EM, Rueger DB, Foy DW, Donahoe CP. Vietnam combat veterans with Posttraumatic Stress Disorder: Analysis of marital and cohabitating adjustment. Journal of Abnormal Psychology. 1985;94(3):329–337. doi: 10.1037/0021-843X.94.3.329. [DOI] [PubMed] [Google Scholar]
- Craske MG, Burton T, Barlow DH. Relationships among measures of communication, marital satisfaction and exposure during couples treatment of agoraphobia. Behaviour Research and Therapy. 1989;27:131–140. doi: 10.1016/0005-7967(89)90071-5. [DOI] [PubMed] [Google Scholar]
- Craske MG, Treanor M, Conway C, Zbozinek T, Vervliet B. Maximizing exposure therapy: an inhibitory learning approach. Behaviour Research and Therapy. 2014;58:10–23. doi: 10.1016/j.brat.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deacon BJ, Abramowitz JS. Cognitive and behavioral treatments for anxiety disorders: A review of meta-analytic findings. Journal of Clinical Psychology. 2004;60:429–441. doi: 10.1002/jclp.10255. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Steil R. Maintenance of intrusive memories in posttraumatic stress disorder: A cognitive approach. Behavioural and Cognitive Psychotherapy. 1995;23:217–249. doi: 10.1017/S135246580001585X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans L, Cowlishaw S, Forbes D, Parslow R, Lewis V. Longitudinal analyses of family functioning in veterans and their partners across treatment. Journal of Consulting and Clinical Psychology. 2010;78:611–622. doi: 10.1037/a0020457. [DOI] [PubMed] [Google Scholar]
- Evans L, Cowlishaw S, Hopwood M. Family functioning predicts outcomes for veterans in treatment for chronic posttraumatic stress disorder. Journal of Family Psychology. 2009;23:531–539. doi: 10.1037/a0015877. [DOI] [PubMed] [Google Scholar]
- Figley CR. Helping traumatized families. San Francisco, CA: Jossey-Bass; 1989. [Google Scholar]
- Foa E, Hembree E, Rothbaum BO. Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences therapist guide. New York, NY: Oxford University Press; 2007. [Google Scholar]
- Fredman SJ, Pukay-Martin ND, Macdonald A, Wagner AC, Vorstenbosch V, Monson CM. Partner accommodation moderates treatment outcomes for couple therapy for Posttraumatic Stress Disorder. Journal of Consulting and Clinical Psychology. 2016;84:79–87. doi: 10.1037/ccp0000061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman SJ, Vorstenbosch V, Wagner AC, Macdonald A, Monson CM. Partner accommodation in posttraumatic stress disorder: Initial testing of the Significant Others’ Responses to Trauma Scale (SORTS) Journal of Anxiety Disorders. 2014;28:372–381. doi: 10.1016/j.janxdis.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA. Kin and nursing home lengths of stay: A backward recurrence time approach. Journal of Health and Social Behavior. 1993;34:138–152. doi: 10.2307/2137240. [DOI] [PubMed] [Google Scholar]
- Frueh BC, Elhai JD, Grubaugh AL, Monnier J, Kashdan TB, Sauvageot JA, … Arana GW. Documented combat exposure of US veterans seeking treatment for combat-related post-traumatic stress disorder. The British Journal of Psychiatry. 2005;186:467–472. doi: 10.1192/bjp.186.6.467. [DOI] [PubMed] [Google Scholar]
- Gilmore MR, Leigh BC, Hoppe MJ, Morrison DM. Comparison of daily and retrospective reports of vaginal sex in heterosexual men and women. Journal of Sex Research. 2010;47:279–284. doi: 10.1080/00224490903050584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn DM, Beckham JC, Feldman ME, Kirby AC, Hertzberg MA, Moore SD. Violence and hostility among families of Vietnam veterans with combat-related posttraumatic stress disorder. Violence and Victims. 2002;17:473–489. doi: 10.1891/vivi.17.4.473.33685. [DOI] [PubMed] [Google Scholar]
- Kaniasty K, Norris FH. Longitudinal linkages between perceived social support and posttraumatic stress symptoms: Sequential roles of social causation and social selection. Journal of Traumatic Stress. 2008;21:274–281. doi: 10.1002/jts.20334. [DOI] [PubMed] [Google Scholar]
- Kaysen D, Atkins DC, Simpson TL, Stappenbeck CA, Blayney JA, Lee CM, Larimer ME. Proximal relationships between PTSD symptoms and drinking among female college students: Results from a daily monitoring study. Psychology of Addictive Behaviors. 2014;28:62–73. doi: 10.1037/a0033588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Bender ME. A behavioral approach to assessing and treating post-traumatic stress disorder in Vietnam veterans. In: Figley CR, editor. Trauma and Its Wake. New York: Brunner/Mazel; 1985. pp. 257–294. [Google Scholar]
- Laurenceau JP, Bolger N. Using diary methods to study marital and family processes. Journal of Family Psychology. 2005;19:86–97. doi: 10.1037/0893-3200.19.1.86. [DOI] [PubMed] [Google Scholar]
- Macdonald A, Greene CJ, Torres JG, Frueh CB, Morland LA. Concordance between clinician-assessed and self-reported symptoms of posttraumatic stress disorder across three ethnoracial groups. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:201–208. doi: 10.1037/a0031879. [DOI] [Google Scholar]
- Maloney LJ. Post traumatic stresses on women partners of Vietnam veterans. Smith College Studies in Social Work. 1988;58:122–143. doi: 10.1080/00377318809516639. [DOI] [Google Scholar]
- Margraf J, Taylor CB, Ehlers A, Roth W, Agras WS. Panic attacks in the natural environment. Journal of Nervous and Mental Disease. 1987;175:558–565. doi: 10.1097/00005053-198709000-00008. [DOI] [PubMed] [Google Scholar]
- McAuliffe TL, DiFranceisco W, Reed BR. Effects of question format and collection mode on the accuracy of retrospective surveys of health risk behavior: A comparison with daily sexual activity diaries. Health Psychology. 2007;26:60–67. doi: 10.1037/0278-6133.26.1.60. [DOI] [PubMed] [Google Scholar]
- McKnight PE, Kashdan TB. The importance of functional impairment to mental health outcomes: A case for reassessing our goals in depression treatment research. Clinical Psychology Review. 2009;29:243–259. doi: 10.1016/j.cpr.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson CM, Fredman SJ. Cognitive-behavioral conjoint therapy for PTSD: Harnessing the healing power of relationships. New York, NY: Guilford Press; 2012. [Google Scholar]
- Monson CM, Taft CT, Fredman SJ. Military-related PTSD and intimate relationships: From description to theory-driven research and intervention development. Clinical Psychology Review. 2009;29:707–714. doi: 10.1016/j.cpr.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naragon-Gainey K, Simpson TL, Moore SA, Varra AA, Kaysen DL. The correspondence of daily and retrospective PTSD reports among female victims of sexual assault. Psychological Assessment. 2012;24:1041–1047. doi: 10.1037/a0028518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nezlek JB. Multilevel Modeling for Social and Personality Psychology. New York, NY: SAGE Publications; 2011. [Google Scholar]
- Nezlek JB. Diary Methods. New York, NY: SAGE Publications; 2012. [Google Scholar]
- Ozechowski TJ. Empirical Bayes MCMC estimation for modeling treatment processes, mechanisms of change, and clinical outcomes in small samples. Journal of Consulting and Clinical Psychology. 2014;82:854–867. doi: 10.1037/a0035889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce GR, Sarason IG, Sarason BR. General and relationship-based perceptions of social support: Are two constructs better than one? Journal of Personality and Social Psychology. 1991;61(6):1028–1039. doi: 10.1037/0022-3514.61.6.1028. [DOI] [PubMed] [Google Scholar]
- Pineles SL, Mostoufi SM, Ready CB, Street AE, Griffin MG, Resick PA. Trauma reactivity, avoidant coping, and PTSD symptoms: A moderating relationship? Journal of Abnormal Psychology. 2011;120:240–246. doi: 10.1037/a0022123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponniah K, Hollon SD. Empirically supported psychological treatments for adult acute stress disorder and posttraumatic stress disorder: A review. Depression and Anxiety. 2009;26:1086–1109. doi: 10.1002/da.20635. [DOI] [PubMed] [Google Scholar]
- Price LR. Small sample properties of Bayesian multivariate autoregressive time series models. Structural Equation Modeling: A Multidisciplinary Journal. 2012;19:51–64. doi: 10.1080/10705511.2012.634712. [DOI] [Google Scholar]
- Rapee RM, Peters L, Carpenter L, Gaston JE. The Yin and Yang of support from significant others: Influence of general social support and partner support of avoidance in the context of treatment for social anxiety disorder. Behaviour Research and Therapy. 2015;69:40–47. doi: 10.1016/j.brat.2015.03.012. [DOI] [PubMed] [Google Scholar]
- Resick PA, Schnicke M. Cognitive processing therapy for rape victims: A treatment manual. Newbury Park, CA: SAGE Publications; 1993. [Google Scholar]
- Salerno L, Rhind C, Hibbs R, Micali N, Schmidt U, Gowers S, … Treasure J. An examination of the impact of care giving styles (accommodation and skillful communication and support) on the one year outcome of adolescent anorexia nervosa: Testing the assumptions of the cognitive interpersonal model in anorexia nervosa. Journal of Affective Disorders. 2016;191:230–236. doi: 10.1016/j.jad.2015.11.016. [DOI] [PubMed] [Google Scholar]
- Sautter FJ, Glynn SM, Arseneau JR, Cretu JB, Yufik T. Structured approach therapy for PTSD in returning veterans and their partners: Pilot findings. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6(Suppl 1):S66–S72. doi: 10.1037/a0036762. [DOI] [Google Scholar]
- Schaefer MT, Olson DH. Assessing intimacy: The PAIR Inventory. Journal of Marital and Family Therapy. 1981;7(1):47–60. doi: 10.1111/j.1752-0606.1981.tb01351.x. [DOI] [Google Scholar]
- Sepulveda AR, Kyriacou O, Treasure J. Development and validation of the Accommodation and Enabling Scale for Eating Disorders (AESED) for caregivers in eating disorders. BMC Health Services Research. 2009;9:171. doi: 10.1186/1472-6963-9-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selig JP, Little TD. Autoregressive and cross-lagged panel analysis for longitudinal data. In: Laursen B, Little TD, Card NA, editors. Handbook of Developmental Research Methods. New York, NY: Guilford Press; 2012. pp. 265–278. [Google Scholar]
- Shrout PE, Lane SP. Psychometrics. In: Mehl MR, Conner TS, editors. Handbook of research methods for studying daily life. New York, NY: Guilford Press; 2012. pp. 302–320. [Google Scholar]
- Steil R, Ehlers A. Dysfunctional meaning of posttraumatic intrusions in chronic PTSD. Behaviour Research and Therapy. 2000;38:537–558. doi: 10.1016/S0005-7967(99)00069-8. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Sommerfield C, Reynolds M, Pilgrim H. Symptom self-monitoring in the treatment of posttraumatic stress disorder. Behavior Therapy. 1999;30:597–605. doi: 10.1016/S0005-7894(99)80027-6. [DOI] [Google Scholar]
- Taylor SE, Klein LC, Lewis BP, Gruenewald TL, Gurung RAR, Updegraff JA. Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review. 2000;107:411–429. doi: 10.1037/0033-295X.107.3.411. [DOI] [PubMed] [Google Scholar]
- Tull MT, Roemer L. Alternative explanations of emotional numbing of posttraumatic stress disorder: An examination of hyperarousal and experiential avoidance. Journal of Psychopathology and Behavioral Assessment. 2003;25:147–154. doi: 10.1023/A:1023568822462. [DOI] [Google Scholar]
- Van de Schoot R, Broere JJ, Perryck KH, Zondervan-Zwijnenburg M, van Loey NE. Analyzing small data sets using Bayesian estimation: The case of posttraumatic stress symptoms following mechanical ventilation in burn survivors. European Journal of Psychotraumatology. 2015;6:25216. doi: 10.3402/ejpt.v6.25216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbosky SJ, Ryan DA. Female partners of Vietnam veterans: Stress by proximity. Issues in Mental Health Nursing. 1988;9:95–104. doi: 10.3109/01612848809140912. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the annual meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- Yehuda R, Morris A, Labinsky E, Zemelman S, Schmeidler J. Ten-year follow-up study of cortisol levels in aging holocaust survivors with and without PTSD. Journal of Traumatic Stress. 2007;20:757–761. doi: 10.1002/jts.20228. [DOI] [PubMed] [Google Scholar]