Abstract
The role of different genotypes of apolipoprotein E (apoE) in the etiology of Alzheimer’s disease is widely recognized. It has been shown that altered functioning of apoE may promote 4-hydroxynonenal modification of mitochondrial proteins, which may result in mitochondrial dysfunction, aggravation of oxidative stress, and neurodegeneration. Mitochondrial aldehyde dehydrogenase (ALDH2) is an enzyme considered to perform protective function in mitochondria by the detoxification of the end products of lipid peroxidation, such as 4-hydroxynonenal and other reactive aldehydes. The goal of our study was to apply a differential proteomics approach in concert with molecular and morphological techniques to elucidate the changes in the frontal cortex and hippocampus of apolipoprotein E knockout (apoE−/−) mice upon treatment with Alda-1—a small molecular weight activator of ALDH2. Despite the lack of significant morphological changes in the brain of apoE−/− mice as compared to age-matched wild type animals, the proteomic and molecular approach revealed many changes in the expression of genes and proteins, indicating the impairment of energy metabolism, neuroplasticity, and neurogenesis in brains of apoE−/− mice. Importantly, prolonged treatment of apoE−/− mice with Alda-1 led to the beneficial changes in the expression of genes and proteins related to neuroplasticity and mitochondrial function. The pattern of alterations implies mitoprotective action of Alda-1, however, the accurate functional consequences of the revealed changes require further research.
Keywords: ALDH2, mitochondria, Alzheimer’s disease, apolipoprotein E, brain
1. Introduction
Alzheimer’s disease (AD) is the most widespread neurodegenerative disorder in the elderly, characterized by irreversible loss of cortical neurons associated with the accumulation of β-amyloid deposits and neurofibrillary tangles (NFTs) formed by aggregates of hyperphosphorylated Tau protein [1,2]. It has been recently shown that oxidative stress and multi-faceted dysfunction of mitochondria take part in the pathogenesis of neurodegeneration [3,4]. Indeed, impaired energy metabolism with decreased activity of mitochondrial electron transport chain enzymes (mainly complex I and IV) and citric acid cycle enzymes (pyruvate dehydrogenase complex, α-ketoglutarate dehydrogenase complex) as well as an increased number of mitochondrial DNA mutations, accompanied by augmented mitochondrial reactive oxygen species (ROS) formation have been observed in animal models of neurodegeneration [4] and in AD patients [5,6]. It has been shown that the ROS-dependent lipid peroxidation results in the generation of electrophilic aldehydes such as 4-hydroxy-2-nonenal (4-HNE), malondialdehyde (MDA), and acrolein, which may fervently react with thiols and amino acid residues in proteins. Importantly, it has been observed, that 4-HNE could mediate oxidation of major mitochondrial proteins (e.g., electron transport chain and citric acid enzymes or its cofactors such as lipoic acid) [7]. Moreover, 4-HNE and accumulation of its protein adducts were implicated in mitochondrial dysfunction and have been postulated to play a role in neurodegenerative processes [8,9,10].
Mitochondrial aldehyde dehydrogenase (ALDH2) plays a main role in the degradation of aldehydes to corresponding non-toxic acids [11]. N-(1,3-benzodioxol-5-ylmethyl)-2,6-dichloro -benzamide (Alda-1) is a cell-permeable, small molecular weight activator of ALDH2 [12]. It has been observed that Alda-1 administration shows beneficial action in diseases linked to mitochondrial dysfunction (e.g., acute ischemic injury in the heart [13], atherosclerosis and hepatic steatosis [14], diabetes-induced myocardial dysfunction [15], and parkinsonism [16]). Recently, we have demonstrated attenuation of depressive- and anxiety-like behaviors by Alda-1 in rat model of depression [17]. Interestingly, it has also been reported that pharmacological activation of ALDH2 prevents dysfunction of endothelial cells induced by β-amyloid in vitro [18]. However, there is no information whether prolonged ALDH2 activation by Alda-1 may offer any benefits in animal models of neurodegeneration.
Apolipoprotein E (apoE) is a glycoprotein mainly expressed by brain, liver, spleen, lung, adrenal, ovary, kidney, and muscle. In the brain it is predominantly synthetized by astrocytes and microglia, and involved in cholesterol transport as well as in the development and regeneration of the central nervous system (CNS) [19]. The presence of epsilon4 allele of apoE (apoE4) was found to predispose to the development of AD, possibly by impairing proteolytic break-down of β-amyloid [20]. Interestingly, it has also been shown that apoE4 may augment 4-HNE-dependent modification of mitochondrial proteins and cause mitochondrial dysfunction [21,22]. The apoE knockout mice (apoE−/−) are primarily used in atherosclerosis studies since they spontaneously develop hypercholesterolemia, dyslipidemia, and arterial lesions [23,24]. They are not considered as a model of full-blown Alzheimer’s disease, however, they have been shown to develop several neurodegenerative changes relevant to the early stages of AD, such as low-grade synaptic and dendrite loss as well as behavioral alterations and deficits in long-term potentiation (LTP) [25,26]. Importantly, despite such delicate morphological alterations, some biochemical disturbances—increased ROS formation and lipid peroxidation—have been clearly demonstrated in brains of apoE−/− mice [27].
Proteomics represents a valuable tool for the study of mitochondrial pathobiology and may contribute to the better understanding of mitochondrial mechanisms of neurodegenerative disorders [28]. However, so far the proteomic research has not been used to evaluate the changes in the brain mitochondria in apoE−/− mice. Thus, the goal of our study was to apply a differential proteomics approach in concert with molecular and morphological techniques to elucidate the changes in the mitochondria-enriched fractions isolated from the frontal cortex and hippocampus of apoE−/− mice as compared to age-matched wild type animals and in apoE−/− mice upon treatment with Alda-1.
2. Results
2.1. Biochemistry Results
To assess the Alda-1 action in apoE−/− mice, we measured the changes in 4-HNE levels by an enzyme-linked immunosorbent assay (ELISA). Importantly, Alda-1 treatment resulted in a significant decrease of 4-HNE-protein content in the plasma (0.27 vs. 0.44 pmol; F(2,6) = 97.78; p < 0.05) and FC (11.91 vs. 19.41 pmol/g; F(2,6) = 10.53; p < 0.05) of apoE−/− mice (Figure 1). In addition we observed an increase of 4-HNE-protein content in the plasma (0.44 vs. 0.3 pmol; F(2,6) = 169.81; p < 0.05) of apoE−/− mice as compared to control mice (Figure 1).
Figure 1.
The level of 4-hydroxy-2-nonenal (4-HNE)-protein adducts in the plasma and the frontal cortex of control mice, apolipoprotein E (apoE)−/− mice and Alda-1-treated apoE−/− mice. The data are presented as the mean ± SEM, with n = 3 for each group. * p < 0.05 vs. control group; # p < 0.05 vs. apoE−/− group.
2.2. Histology and Immunohistochemistry Results
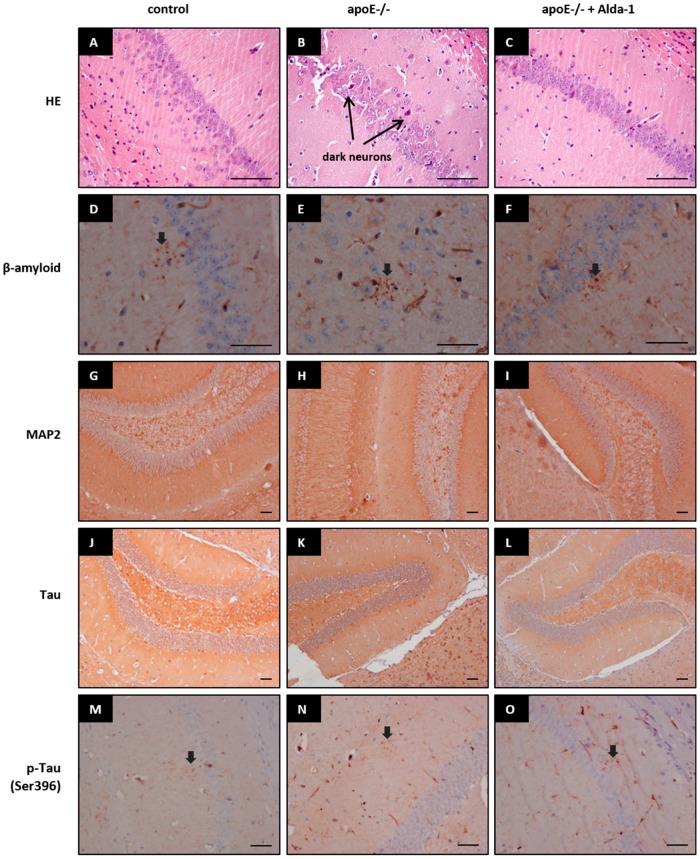
Hematoxylin/eosin (HE) staining did not reveal any major changes in the brain structures in control mice, apoE−/− mice, and Alda-1-treated apoE−/− mice. However, apoE−/− mice as compared to wild type animals exhibited signs of the mild tissue injury: some neurons were shrunken and deeply stained (“dark neurons”). These changes were visually slightly less pronounced in brains of Alda-1-treated apoE−/− mice (Figure 2A–C). Immunohistochemistry staining of β-amyloid, microtubule-associated protein 2 (MAP2) (marker of dendrites), and Tau and phospho-Tau (Ser396) (marker of neurofibrillary tangles) did not show any differences between brain structures of wild type mice, apoE−/− mice, and Alda-1-treated apoE−/− mice (Figure 2D–O).
Figure 2.
Representative images of hematoxilin and eosin (HE) (A–C), β-amyloid (D–F), microtubule-associated protein 2 (MAP2) (G–I), Tau (J–L), and p-Tau (Ser396) (M–O) staining in brains of control mice, apoE−/− mice, and Alda-1-treated apoE−/− mice. Arrows indicate dark neurons, positive stainings of β-amyloid and p-Tau (Ser396), respectively. Scale bars = 500 µm.
2.3. mRNA Expression of Factors Related to Mitochondrial Biogenesis, Apoptosis, Inflammation, and Neuroplasticity
We measured the mRNA expression of selected, important factors related to mitochondrial biogenesis (PGC1-α, Tfam, Nrf1, CYTB, COX1, COX3, ND1, ND4, ATP6), apoptosis (Bax, Bcl-2, Bcl2l1, Casp8, Casp9, Casp3), inflammation (IL-1β, IL-6, NF-κB), neuroplasticity (Bdnf, Nog, Bmp4), and the pathogenesis of Alzheimer disease (Cdk5, Cdk5r1, Gsk3a, Gsk3b) in the hippocampus and the frontal cortex of C57BL/6J mice, apoE−/− mice, and Alda-1-treated apoE−/− mice. Both in the frontal cortices (FCx) and the hippocampi (Hp) of apoE−/− mice as compared to controls we observed significant decreases in genes expression related to neurogenesis (Bdnf, Nog). In addition, apoE−/− mice exhibited decreased Bcl-2 and Nrf1 mRNA expression in the Hp and the FCx, respectively (Table 1). Alda-1 administration led to a slight increase in gene expression related to neurogenesis (Nog), mitochondrial biogenesis (CYTB, ND1), and apoptosis (Bax, Gsk3b) in the Hp of apoE−/− mice (Table 2). In the FCx of apoE−/− mice, Alda-1 treatment resulted in the reduction of Bmp4 mRNA expression (Table 2).
Table 1.
The statistically significant differences in the relative gene expression between apoE−/− group vs. wild type animals in the hippocampus and the frontal cortex (p < 0.05, n = 3).
| Gene Name | Description | Fold Change | p-Value |
|---|---|---|---|
| The Hippocampus | |||
| Bcl-2 | B-cell lymphoma 2 | −1.30 | 0.0467 |
| Bdnf | Brain-derived neurotrophic factor | −1.27 | 0.0278 |
| Bmp4 | Bone morphogenetic protein 4 | −1.69 | 0.0091 |
| Nog | Noggin | −1.41 | 0.0096 |
| The Frontal Cortex | |||
| Bdnf | Brain-derived neurotrophic factor | −1.29 | 0.0448 |
| Nog | Noggin | −1.39 | 0.0174 |
| Nrf1 | Nuclear respiratory factor 1 | −1.21 | 0.0096 |
Table 2.
The statistically significant differences in the relative gene expression between Alda-1-treated apoE−/− group vs. untreated apoE−/− group in the hippocampus and the frontal cortex (p < 0.05, n = 3).
| Gene Name | Description | Fold Change | p-Value |
|---|---|---|---|
| The Hippocampus | |||
| Bax | Bcl-2-like protein 4 | 1.22 | 0.0303 |
| CYTB | Cytochrom b | 1.33 | 0.0258 |
| Gsk3b | Glycogen synthase kinase 3β | 1.24 | 0.0058 |
| ND1 | Mitochondrially encoded NADH dehydrogenase 1 | 1.35 | 0.0312 |
| Nog | Noggin | 1.20 | 0.0268 |
| The Frontal Cortex | |||
| Bmp4 | Bone morphogenetic protein 4 | −1.28 | 0.0366 |
2.4. Mitochondrial Protein Expression Assessed by iTRAQ Method
We investigated mitochondrial protein expression in the FCx and the Hp of control mice, apoE−/− mice, and Alda-1-treated apoE−/− mice using isobaric tag for relative quantitation (iTRAQ method). Collectively, 20 and 34 differentially expressed proteins in the FCx and Hp of apoE−/− mice, respectively, were detected by iTRAQ/mass spectrometry, as compared to control group (Table 3 and Table 4). Alda-1 administration led to 2 and 10 differentially expressed proteins in the FCx and Hp of apoE−/− mice, respectively (Table 5 and Table 6).
Table 3.
Differentially expressed proteins in the frontal cortex mitochondria of apoE−/− group vs. wild type animals (p < 0.05, n = 3).
| No. | Protein | UniProtKB Accession No. | Unique Peptides | Total Peptides | Fold Change |
|---|---|---|---|---|---|
| 1 | Microtubule-actin cross-linking factor 1 | Q9QXZ0 | 2 | 2 | 1.59 |
| 2 | AP-3 complex subunit δ-1 | O54774 | 2 | 8 | 1.30 |
| 3 | Cytochrome b-c1 complex subunit 7 | Q9D855 | 2 | 3 | 1.28 |
| 4 | Histone H4 | P62806 | 6 | 28 | 1.26 |
| 5 | ATP-dependent 6-phosphofructokinase, muscle type | P47857 | 6 | 15 | 1.24 |
| 6 | Myelin basic protein | P04370 | 10 | 235 | 1.18 |
| 7 | Metabotropic glutamate receptor 3 | Q9QYS2 | 4 | 8 | 1.18 |
| 8 | Tubulin β-3 chain | Q9ERD7 | 12 | 130 | 1.11 |
| 9 | Spectrin α chain, non-erythrocytic 1 | P16546 | 89 | 416 | 1.06 |
| 10 | Tubulin β-4 B chain | P68372 | 11 | 356 | 1.06 |
| 11 | Calcium-binding mitochondrial carrier protein Aralar1 | Q8BH59 | 15 | 73 | −1.13 |
| 12 | NADH dehydrogenase (ubiquinone) flavoprotein 1, mitochondrial | Q91YT0 | 7 | 18 | −1.19 |
| 13 | Pyruvate carboxylase, mitochondrial | Q05920 | 2 | 5 | −1.21 |
| 14 | Solute carrier family 12 member 5 | Q91V14 | 10 | 46 | −1.23 |
| 15 | Dynein light chain 1, cytoplasmic | P63168 | 5 | 17 | −1.23 |
| 16 | Succinyl-CoA ligase (ADP/GDP-forming) subunit α, mitochondrial | Q9WUM5 | 3 | 25 | −1.26 |
| 17 | Ubiquitin-60S ribosomal protein L40 | P62984 | 5 | 57 | −1.26 |
| 18 | Cytochrome c oxidase subunit 7A2, mitochondrial | P48771 | 2 | 7 | −1.33 |
| 19 | Basigin | P18572 | 2 | 4 | −1.41 |
| 20 | Proline-rich transmembrane protein 2 | E9PUL5 | 2 | 5 | −1.72 |
Table 4.
Differentially expressed proteins in the hippocampus mitochondria of apoE−/− group vs. wild type animals (p < 0.05, n = 3).
| No. | Protein | UniProtKB Accession No. | Unique Peptides | Total Peptides | Fold Change |
|---|---|---|---|---|---|
| 1 | Coronin-2B | Q8BH44 | 2 | 3 | 1.73 |
| 2 | Protein deglycase DJ-1 | Q99LX0 | 5 | 20 | 1.32 |
| 3 | Synaptoporin | Q8BGN8 | 4 | 8 | 1.23 |
| 4 | ATP synthase subunit δ, mitochondrial | Q9D3D9 | 3 | 18 | 1.23 |
| 5 | Spectrin β chain, erythrocytic | P15508 | 3 | 9 | 1.23 |
| 6 | MICOS complex subunit Mic25 | Q91VN4 | 2 | 3 | 1.21 |
| 7 | Ubiquitin-60S ribosomal protein L40 | P62984 | 4 | 51 | 1.21 |
| 8 | Tubulin α-1 chain | A2AQ07 | 7 | 33 | 1.17 |
| 9 | Tropomyosin α-3 chain | P21107 | 3 | 16 | 1.17 |
| 10 | Paralemmin-1 | Q9Z0P4 | 7 | 33 | 1.16 |
| 11 | Disks large homolog 4 | Q62108 | 5 | 19 | 1.14 |
| 12 | Pyruvate dehydrogenase E1 component subunit β, mitochondrial | Q9D051 | 16 | 86 | 1.14 |
| 13 | Creatine kinase B-type | Q04447 | 19 | 306 | 1.11 |
| 14 | Calcium/calmodulin-dependent protein kinase type II subunit α | P11798 | 25 | 329 | 1.10 |
| 15 | Tubulin β-4 B chain | P68372 | 11 | 249 | 1.09 |
| 16 | Heat shock cognate 71 kDa protein | P63017 | 37 | 351 | 1.08 |
| 17 | Hexokinase-1 | P17710 | 33 | 246 | 1.07 |
| 18 | Spectrin β chain, non-erythrocytic 1 | Q62261 | 72 | 351 | 1.07 |
| 19 | ADP/ATP translocase 1 | P48962 | 22 | 217 | −1.11 |
| 20 | Guanine nucleotide-binding protein G(I)/G(S)/G(T) subunit β-1 | P62874 | 12 | 134 | −1.11 |
| 21 | Calcium-dependent secretion activator 1 | Q80TJ1 | 16 | 56 | −1.14 |
| 22 | Fumarate hydratase, mitochondrial | P97807 | 10 | 38 | −1.15 |
| 23 | Glutathione S-transferase Mu 1 | P10649 | 15 | 76 | −1.15 |
| 24 | Dihydropyrimidinase-related protein 1 | P97427 | 8 | 32 | −1.15 |
| 25 | Thioredoxin | P10639 | 3 | 11 | −1.18 |
| 26 | Ras-related protein Rab-1A | P62821 | 6 | 46 | −1.20 |
| 27 | Actin-related protein 2 | P61161 | 6 | 13 | −1.24 |
| 28 | Mitochondrial 2-oxoglutarate/malate carrier protein | Q9CR62 | 6 | 16 | −1.26 |
| 29 | Heterogeneous nuclear ribonucleoprotein K | P61979 | 3 | 13 | −1.28 |
| 30 | α-endosulfine | P60840 | 2 | 3 | −1.30 |
| 31 | Calcium/calmodulin-dependent protein kinase type IV | P08414 | 2 | 4 | −1.34 |
| 32 | Guanine nucleotide-binding protein G(i) subunit α-2 | P08752 | 4 | 13 | −1.37 |
| 33 | Myelin basic protein | P04370 | 11 | 138 | −1.43 |
| 34 | 2′,3′-cyclic-nucleotide 3′-phosphodiesterase | P16330 | 32 | 210 | −1.47 |
Table 5.
Differentially expressed proteins in the frontal cortex mitochondria of Alda-1-treated apoE−/− group vs. untreated apoE−/− group (p < 0.05, n = 3).
Table 6.
Differentially expressed proteins in the hippocampus mitochondria of Alda-1-treated apoE−/− group vs. untreated apoE−/− group (p < 0.05, n = 3).
| No. | Protein | UniProtKB Accession No. | Unique Peptides | Total Peptides | Fold Change |
|---|---|---|---|---|---|
| 1 | Myelin basic protein | P04370 | 11 | 123 | 1.37 |
| 2 | Carbonic anhydrase 2 | P00920 | 4 | 24 | 1.27 |
| 3 | Myelin proteolipid protein | P60202 | 4 | 48 | 1.25 |
| 4 | 2′,3′-cyclic-nucleotide 3′-phosphodiesterase | P16330 | 22 | 141 | 1.25 |
| 5 | Sodium/potassium-transporting ATPase subunit α-2 | Q6PIE5 | 22 | 180 | 1.11 |
| 6 | Excitatory amino acid transporter 2 | P43006 | 15 | 183 | 1.09 |
| 7 | Spectrin β chain, non-erythrocytic 1 | Q62261 | 64 | 303 | −1.06 |
| 8 | Spectrin α chain, non-erythrocytic 1 | P16546 | 98 | 606 | −1.06 |
| 9 | Actin, aortic smooth muscle | P62737 | 24 | 182 | −1.09 |
| 10 | OCIA domain-containing protein 2 | Q9D8W7 | 2 | 7 | −1.40 |
3. Discussion
Several lines of evidence suggest that altered functioning of apoE may aggravate aldehyde modification of mitochondrial proteins, which may result in mitochondrial dysfunction and neurodegeneration [5,6,21]. In the present work, we focused on the effect of Alda-1 activation of ALDH2—an enzyme responsible for the detoxification of toxic aldehydes—on the protein content of mitochondria-enriched fractions isolated from the frontal cortex and hippocampus of apolipoprotein E knockout mice (apoE−/−). Moreover, the proteomic approach was supported by molecular and morphological techniques. This is the first report about the molecular and proteomic effects of pharmacological activation of ALDH2 in CNS structures in apoE−/− mice. The main finding of our study is that Alda-1 administration led to the beneficial changes in the expression of genes and proteins related to neuroplasticity and mitochondrial function.
Although the most recognized function of mitochondrial ALDH2 is the degradation of acetaldehyde in the metabolism of ethanol, it can also efficiently oxidize other reactive aldehydes, especially 4-HNE, to non-toxic acids. Indeed, in our hands, Alda-1 caused a significant decrease in 4-HNE-protein content in the plasma and the frontal cortex of apoE−/− mice, which might depend on ALDH2 activation. However, the exact confirmation of Alda-1 influence on ALDH2 activity regarding the metabolism of 4-HNE to related acids does require further investigations including direct measurements of ALDH2 activity and tissue levels of corresponding acids.
In line with some previous reports [25,26], we observed delicate signs of the nonspecific mild tissue injury in brains of apoE−/− mice. The number of shrunken and deeply stained neurons (“dark neurons”) was higher in brains apoE−/− mice. It should be noted however, that the presence of such changes may depend on the lot of animals, as they were absent in apoE−/− mice studied by Anderson et al. [29]. Moreover, according to some reports, the dark neurons may rather reflect histological artifacts than trustworthy markers of tissue injury [30]. In keeping with the majority of reports [25,26], we did not reveal any changes in tissue contents of β-amyloid, Tau, p-Tau (Ser396), and microtubule-associated protein 2 (MAP2). In our study, we focused on the changes on the levels of the gene/protein expression occurring in the absence of morphologically overt tissue injury.
A growing amount of evidence points to the impairment of neuroplasticity in the pathogenesis of Alzheimer's disease [31,32,33]. Importantly, mitochondria perform a key role in the regulation of neuroplasticity and maintenance of cellular calcium homeostasis [34]. Brain-derived neurotrophic factor (BDNF) is a main regulator of synaptic plasticity, long-term memory, as well as neuronal survival and differentiation [35,36]. Moreover, BDNF is able to streamline mitochondrial respiratory coupling and increase ATP synthesis [37]. Interestingly, it has been observed that lower levels of BDNF in the plasma and the cerebrospinal fluid were presented in the early stages of AD and mild cognitive impairment (MCI) [38]. In keeping with these reports, we showed diminished Bdnf mRNA expression in the FCx and Hp of apoE−/− mice, as compared to wild type animals. In turn, noggin (NOG) and bone morphogenetic protein 4 (BMP4) have been recognized as potent regulators of neurogenesis. It is known that BMP4 is related to decreased neurogenesis and increased gliogenesis, while expression of BMP4 inhibitor, NOG, is linked to increased neurogenesis [39] and therefore plays a significant role in the process of learning and memory [40]. Disturbances in hippocampal neurogenesis have been connected to memory deficits and cognitive impairment in the early stages of AD [41]. In this study, Nog mRNA expression was decreased both in the FCx and Hp of apoE−/− mice. Importantly, Alda-1 administration led to the increase in Nog mRNA expression in the Hp and the decrease in Bmp4 mRNA expression in the FCx.
Proteomic analysis using iTRAQ and mass spectrometry methods also revealed changes in protein expression related to the impairment of neuroplasticity in the Hp of apoE−/− mice: we observed decreased expression of collapsin response mediator protein 1 (CRMP1), heterogeneous nuclear ribonucleoprotein K (hnRNP K), calcium-dependent secretion activator 1 (CAPS-1), and 2′,3′-cyclic-nucleotide 3′-phosphodiesterase (CNP). CRMP1 is involved in axonal growth and long-term potentiation (LTP) [42], whereas hnRNP K regulates neurite outgrowth, dendritic spine density, and synaptic plasticity in hippocampal neurons [43,44]. In turn, CAPS-1 is a calcium-binding protein engaged in exocytosis of neurotransmitters and neuropeptides, while CNP is required for proper axoglial interactions [45]. Decreased CNP expression, observed in entorhinal and auditory cortex of AD patients, might suggest the impairment in myelination with subsequent synaptic and cognition loss [46]. It is worth highlighting that in our study CNP was a common protein differentially expressed in the Hp of control mice, apoE−/− mice, and apoE−/− mice treated with Alda-1. Importantly, Alda-1 administration up-regulated CNP expression, which may denote its beneficial action in the early stages of AD.
It is well known that a major hallmark of Alzheimer’s disease is the loss of short and long-term memory [13]. Interestingly, we noted down-regulation of calcium/calmodulin-dependent protein kinase type IV (CaMK IV) and basigin (CD147) in the Hp and FCx of apoE−/− mice, respectively. CaMK IV has been demonstrated to participate in the activation of CREB transcription factor, thereby regulating genes responsible for memory and neuronal survival [47]. It can also perform a protective role against neuronal injury [48,49]. In turn, glycoprotein CD147 may regulate the activity of β-amyloid processing enzyme, γ-secretase. It was shown that mice deficient in CD147 showed deficits in memory and spatial learning [50]. It might well be that the decreased expression of the aforementioned proteins could be linked to learning and memory impairment observed in apoE−/− mice in the Morris water maze test [51]. In our case, treatment with Alda-1 resulted in the increase in carbonic anhydrase 2 (CA2) expression in the Hp of apoE−/− mice. Interestingly, CA2 has been postulated to modulate hippocampal CA1 neuronal network activity and its downregulation may result in impaired cognition. Moreover, use of CA2 activators has been shown to improve learning and memory [52]. In this regard, Alda-1 activity toward increase of CA2 might represent promising area of research.
A growing amount of evidence points to the presence of mitochondrial dysfunction manifested by energy metabolism impairment and decreased activity of oxidative phosphorylation (OXPHOS) and Krebs cycle enzymes both in animal models of AD and in patients [5,6,53]. Similarly, mostly in the FCx of apoE−/− mice, we have observed diminished expression of OXPHOS proteins (NADH dehydrogenase flavoprotein 1, cytochrome C oxidase subunit 7A2), proteins supporting OXPHOS (mitochondrial aspartate glutamate carrier 1), and proteins involved in Krebs cycle (succinyl-CoA synthetase subunit α, fumarate hydratase). On the other hand, proteins participating in glycolysis (6-phosphofructokinase type A, hexokinase-1) have been upregulated in the Hp and FCx of apoE−/− mice. However, we have also revealed changes, which may be considered as contradictory: increased expression of ATP synthase subunit δ and cytochrome b-c1 complex subunit 7 in the Hp and FCx of apoE−/− mice, respectively. Clearly, further investigations are required to clarify an interpretation of above effects.
Interestingly, in the FCx of apoE−/− mice we have found decreased mRNA expression of nuclear respiratory factor 1 (Nrf1), which is a transcription factor responsible for the activation of expression of many factors involved in energy metabolism, cellular respiration, and replication and transcription of mitochondrial DNA [54]. Diminished expression of peroxisome proliferator-activated receptor gamma coactivator 1-α (PGC-1α) and downregulation of Nrf1 mRNA have been attributed to the impairment of mitochondrial biogenesis in transgenic mouse model of AD [53]. In our case, Alda-1 administration led to the increased expression of proteins that participated in OXPHOS at gene (mitochondrially encoded NADH dehydrogenase 1 (ND1), cytochrom b (CYTB)), and protein level (NADH dehydrogenase 1α subcomplex subunit 10) in the FCx of apoE−/− mice, which may suggest the stimulation of mitochondrial biogenesis.
Recent reports emphasize the role of glutamate-mediated excitotoxicity in the pathogenesis of neurodegenerative diseases, such as Alzheimer’s disease, Huntington disease, and amyotrophic lateral sclerosis (ALS). Our results indicate that proline-rich transmembrane protein 2 (PRRT2) was down-regulated in the FCx of apoE−/− mice. PRRT2 is a transmembrane protein found in glutamatergic neurons, where it interacts with synaptosomal-associated protein 25 (SNAP25), which inhibits glutamate release and neuronal hyperexcitability. Thus, diminished expression of PRRT2 may lead to decreased interactions with SNAP25, which could potentially result in the increased release of glutamate [55]. Importantly, Alda-1 administration led to the upregulation of excitatory amino acid transporter 2 (EAAT2) both in the Hp and FCx of apoE−/− mice. EAAT2 is crucial for tuning of the glutamate neurotransmission by its rapid removal from the synaptic cleft, thus maintaining the levels of glutamate within safe range [56]. Moreover, it has been shown that reduced EAAT2 function observed in AD is associated with cognitive decline and increased amyloid β production, thus restoring EAAT2 protein function could represent a potential therapeutic approach in AD [57]. It is tempting to speculate that upregulation of EAAT2 by Alda-1 may denote its beneficial action in the early stages of AD.
It is well recognized that oxidative stress plays a crucial role in the etiology and progression of AD [58]. We have observed diminished expression of antioxidant proteins, such as glutathione S-transferase Mu 1 (GST 1-1) and thioredoxin (TRX) in the Hp of apoE−/− mice. GST 1-1 is best known for its ability to detoxify xenobiotics, including 4-HNE, by their conjugation with the reduced form of glutathione (GSH). In turn, TRX acts as an antioxidant by maintaining the reduced form of cellular thiols. Our results are in keeping with previous reports: it has been observed that the lack of TRX2 impairs mitochondrial redox homeostasis and leads to early-onset neurodegeneration [59]; the decreased activity of GST 1-1 has been detected in the Hp of AD patients [60].
Interestingly, some changes observed in apoE−/− mice may represent compensatory mechanisms, for example, Parkinson disease protein 7 homolog (PARK7) was upregulated in the Hp of apoE−/− mice. PARK7 plays multiple cellular roles as a modulator of gene transcription, an antioxidant protein, and a regulator of mitochondrial functions. It can also regulate the activity of complex I in mitochondria and exert a mitoprotective effect [61,62]. Mutations in PARK7 gene are associated with hereditary Parkinson’s disease (PD) [63]. In addition, the increased level of oxidized (inactive) form of PARK7 has been detected in the brain of AD and PD patients [64]. The upregulation of PARK7 in the Hp of apoE−/− mice might be interpreted as a compensatory mechanism, to counteract accelerated oxidative stress and mitochondrial dysfunction presented in the early stages of AD. Similarly, the increase in protein required for synaptic plasticity associated with NMDA receptor signaling-postsynaptic density protein 95 (PSD-95) might represent a compensatory mechanism, supporting synaptic plasticity in the Hp of apoE−/− mice [65].
It should also be noted that not all actions of Alda-1 could be interpreted unambiguously in terms of stimulation of neurogenesis, neuroplasticity, and mitogenesis—for example, in our case, Alda-1 upregulated glycogen synthase kinase 3β (Gsk3b) and proapoptotic factor Bax mRNA expression in the Hp of apoE−/− mice. It has been shown that increased expression of the active GSK3B form was associated with the formation of senile plaques and neurofibrillary tangles in AD patients [66]. Clearly, further research is needed to clarify the physiological meaning of Alda-1 effects on mRNA and protein of Gsk3b and Bax in the brain of apoE−/− mice. The main aim of our study was to elucidate the proteomic and molecular changes in the FCx and Hp of apoE−/− mice upon treatment with Alda-1. However, our findings cannot determine whether the changes in gene or protein expression are due to direct or indirect effects of Alda-1 administration in apoE−/− mice. Moreover, the obvious limitation of our study is a lack of corresponding behavioral data, which would significantly increase the impact of the biochemical/molecular and proteomic findings. Clearly, correlation between molecular/proteomic and functional data requires further research.
4. Materials and Methods
4.1. Animal Experiments
All animal procedures were performed in accordance to the guidelines from Directive 2010/63/EU of the European Parliament on the protection of animals used for scientific purposes and approved by the Jagiellonian University Ethical Committee on Animal Experiments (no. 73/2011, 8 June 2011). Animal experiments were carried out as previously described [14]. Briefly, three groups of animals were studied: control group (C57BL/6J mice, without treatment, on chow diet, n = 10), apoE−/− mice from Taconic (Ejby, Denmark) (without treatment, on chow diet, n = 10), and apoE−/− mice treated with Alda-1 (Tocris Bioscience, Bristol, UK, n = 10) at the age of eight weeks and administered to mice for four months at a dose of 5 mg per kg of body weight per day and mixed without heating with chow diet. At the age of six months mice were euthanized 5 min after injection of fraxiparine (1000 UI; Sanofi-Synthelabo, Paris, France), and the blood from the right ventricle was collected and entire brains or hippocampi (Hp) and frontal cortices (FCx) were dissected on ice-cold glass plates.
4.2. Histology and Immunohistochemistry of the Brain
The brain tissue samples were formalin fixed, embedded in paraffin, and 2 µm paraffin sections were stained with the hematoxilin-eosin method or used for immunohistochemistry, as previously described [14]. The following antibodies were used: 1:100 ANTI-MAP2 (sc-20172, Santa Cruz, Dallas, TX, USA), 1:100 ANTI-β-amyloid (A5213, Sigma, Darmstadt, Germany), 1:100 ANTI-Tau (A0024, Dako, Denmark), and 1:100 ANTI-phospho-Tau (Ser396) (SAB4504557, Sigma, Darmstadt, Germany).
4.3. Biochemical Methods
The blood was centrifugated at 1000 g-force at 4 °C for 10 min and the plasma was stored in −80 °C until assayed. The FCx were submerged in a PBS buffer (137 mmol/L NaCl, 2.7 mmol/L KCl, 10 mmol/L Na2HPO4, 1.8 mmol/L KH2PO4) and homogenized using high-speed shaking (120 s) in plastic tubes with stainless steel beads in TissueLyser II apparatus (Qiagen, Hilden, Germany). The action of Alda-1 was assessed indirectly by the evaluation of the changes in tissue 4-HNE levels measured by an enzyme-linked immunosorbent assay (ELISA) using commercially available kits (MBS027502, MyBioSource, San Diego, CA, USA). The equality of variance and the normality of the data were checked and then one-way analysis of variance (ANOVA) with the Tukey’s post-hoc test implemented in Statistica 10.0 software (StatSoft@Polska, Krakow, Poland) was used for statistical analysis of the data. p < 0.05 was considered as statistically significant.
4.4. Real Time (RT)-PCR
Real time (RT)-PCR experiments were performed as previously described [14]. Briefly, total RNA was isolated from the homogenized mouse FCx and Hp using RNeasy Fibrous Tissue Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. Relative gene expression analysis in the FCx and Hp was carried out using 7900HT fast real-time PCR System (Applied Biosystems, Foster City, CA, USA) in triplicate with GAPDH, 18S, ACTB, B2M, and GUSB as internal reference genes. The commercially available TaqMan® Gene Expression Assays (Applied Biosystems) were used as follows: Bax (Mm00432051_m1), Bcl-2 (Mm00477631_m1), Bcl2l1 (Mm00437783_m1), Bdnf (Mm04230607_s1), Bmp4 (Mm00432087_m1), Neurog2 (Mm00437603_g1), Nog (Mm01297833_s1), Casp3 (Mm01195085_m1), Casp8 (Mm00802247_m1), Casp9 (Mm00516563_m1), Cdk5 (Mm00432447_g1), Cdk5r1 (Mm00438148_s1), Gsk3a (Mm01719731_g1), Gsk3b (Mm00444911_m1), IL-1β (Mm00434228_m1), IL-6 (Mm00446190_m1), IL-10 (Rn00563409_m1), NFkB (Mm00476361_m1), Ppargc1a (Mm01208835_m1), Pparg (Mm01184322_m1), CYTB (Mm04225271_g1), ND1 (Mm04225274_s1), ND4L (Mm04225294_s1), COX1 (Mm04225243_g1), COX3 (Mm04225261_g1), ATP6 (Gm10925-Mm03649417_g1), Nrf1 (Mm01135606_m1), and Tfam (Mm00447485_m1). Reactions were performed using TaqMan® Gene Expression Master Mix (Applied Biosystems), according to the manufacturer’s instructions. A threshold value (Ct) for each sample was set in the exponential phase of PCR, and the ΔΔCt method [67] was used for statistical data analysis carried out by Data Assist v3.01 software (Applied Biosystems).
4.5. iTRAQ Method
4.5.1. Sample Preparation
The isolation of mitochondria-enriched fraction (mitochondria with synaptosomes) from the freshly-harvested Hp and FCx was performed at 4 °C, as previously described [14]. Mitochondria-enriched pellets were resuspended in 0.5 mL of lysis buffer (7 M urea, 2 M thiourea, 4% 3-(3-Cholamidopropyl)dimethylammonio-1-propanesulfonate hydrate (CHAPS), 1% dithiothreitol (DTT), the mix of protease inhibitors (Sigma)), vortexed, incubated at 25 °C for 30 min and then centrifuged at 12,000× g-force for 15 min. The protein concentration was determined in the harvested supernatant using the Bradford method [68]. One hundred micrograms of calculated protein content of each sample was precipitated overnight with ice-cold acetone (Sigma) (1:6 v:v). Samples were centrifuged at 12,000× g-force for 10 min at 4 °C. Acetone was carefully removed and precipitates were air-dried for 10 min. Subsequently, samples were dissolved, reduced, and alkylated, as recommended by iTRAQ protocol (ABSciex, Framingham, MA, USA). Proteins were digested with Trypsin (Promega, Mannheim, Germany) overnight, with 1:50 (w:w) ratio at 37 °C. Samples were labeled with iTRAQ reagents as recommended by producer and ordered as follows: control: 113, 114, 115 and apoE−/−: 116, 117, 118 or apoE−/−: 113, 114, 117 and Alda-1-treated: 118, 119, 121. Labeled samples were combined and dried in vacuum concentrator (Eppendorf, Hamburg, Germany). Next, trypsin-digested peptides were dissolved in 5% acetonitrile (ACN), 0.1% trifluoroacetic acid (TFA) and purified with C18 MacroSpin Columns (Harvard Apparatus, Holliston, MA, USA). Eluate was dried in a vacuum concentrator, reconstituted in 5% ACN, 0.1% formic acid (FA), and subjected to strong cation exchange (SCX) fractionation. Samples were loaded onto previously conditioned SCX Macrospin columns (Harvard Apparatus), after which flow-through fraction and 11 consecutive injections of the eluent buffer, which consisted of 5, 10, 20, 40, 60, 80, 100, 150, 200, 300, 500 mM ammonium acetate in 5% ACN, 0.1% FA, respectively, were collected by centrifugation (1 min, 2000 g-force). Thus, the labeled peptides from each sample were distributed across 12 SCX fractions.
4.5.2. LC-MS Analysis
Samples were concentrated on a trap column (Acclaim PepMap100 RP C18 75 µm i.d. ×2 cm column (Thermo Scientific, Waltham, MA, USA). Each fraction was then injected on-line on PepMap100 RP C18 75 µm i.d. ×15 cm column (Thermo Scientific Dionex) and peptides were separated in 90 min 7%–55% B phase linear gradient (A phase − 2% ACN and 0.1% FA; B phase − 80% ACN and 0.1% FA) with a flow rate of 300 nL/min by UltiMate 3000 HPLC system (Thermo Scientific Dionex) and applied on-line to a Velos Pro (Thermo Scientific) dual-pressure ion-trap mass spectrometer. The main working nanoelectrospray ion source (Nanospray Flex, Thermo Scientific) parameters were as follows: ion spray voltage 1.7 kV and capillary temperature 250 °C. Spectra were collected in full scan mode (400–1500 Da, 50 ms AT), followed by five Higher energy Collisional Dissociation (HCD) (20 ms AT), MS/MS scans (each consists of two microscans, 100 ms AT) of the five most intense ions from the preceding survey full scan under dynamic exclusion criteria. Collected data were analyzed by the X!Tandem (The GPM Organization) and Comet search algorithms and validated with PeptideProphet and iProphet under Trans-Proteomic Pipeline (TPP) suite of software (Institute for Systems Biology, Seattle, WA, USA). Search parameters were set as follows: taxonomy: mouse (UniProtKB/Swiss-Prot), enzyme: trypsin, missed cleavage sites allowed: 2, fixed modification: Methylthio(C), variable modifications: Methionine oxidation(M), iTRAQ8plex(K), iTRAQ8plex(N-term), iTRAQ8plex(Y); parent mass error −1.5 to +3.0 Da and peptide fragment mass tolerance: 0.7 Da. Quantitative information of the peptides data was extracted from the HCD MS2 data by Libra software under Trans-Proteomic Pipeline (TPP). Peptide False Discovery Rate (FDR) was estimated by Mayu (TPP) and peptide identifications with FDR below 2% were considered as correct matches. DanteR software [69] was used for statistical analysis of iTRAQ-labeled peptides. In brief, replicate peptides were aggregated to unique peptides while the corresponding reporter ion intensities were summed up. The dataset was normalized using linear regression and ANOVA was performed at the peptide level using a robust linear model with minimum 2 and maximum 500 peptides. Finally, the Benjamini and Hochberg False Discovery Rate (FDR) correction was used to adjust p-values. The mass spectrometry proteomics data have been deposited to the ProteomeXchange Consortium via the PRIDE [70] partner repository with the dataset identifier PXD004022.
5. Conclusions
In conclusion, despite the lack of significant morphological changes, differential proteomic approach revealed many changes in mitochondrial protein expression, indicating the impairment of energy metabolism, neuroplasticity, and neurogenesis in the brains of apoE−/− mice. The treatment of apoE−/− mice with ALDH2 activator, Alda-1, led to the beneficial changes in the expression of genes and proteins related to neuroplasticity and mitochondrial function. The accurate functional consequences of the revealed alterations as well as the detailed mechanism of direct and indirect Alda-1 actions require further research.
Acknowledgments
This study was supported by the grants from Jagiellonian University Medical College. (K/ZDS/003802) and National Science Centre (NCN): 2011/01/N/NZ4/01145, 2011/01/N/NZ4/01142, and 2011/01/N/NZ2/00089. Aneta Stachowicz and Katarzyna Głombik acknowledge the financial support from the project Interdisciplinary PhD Studies “Molecular sciences for medicine” (co-financed by the European Social Fund within the Human Capital Operational Programme) and the Foundation for Polish Science (FNP).
Abbreviations
| 4-HNE | 4-hydroxy-2-nonenal |
| ACN | acetonitrile |
| AD | Alzheimer’s disease |
| ALDH2 | mitochondrial aldehyde dehydrogenase |
| apoE | apolipoprotein E |
| BDNF | brain-derived neurotrophic factor |
| BMP4 | bone morphogenetic protein 4 |
| CA2 | carbonic anhydrase 2 |
| CaMK IV | calcium/calmodulin-dependent protein kinase type IV |
| CAPS-1 | calcium-dependent secretion activator 1 |
| CD147 | basigin |
| CHAPS | 3-(3-Cholamidopropyl)dimethylammonio-1-propanesulfonate hydrate |
| CNP | 2′,3′-cyclic-nucleotide 3′-phosphodiesterase |
| CRMP1 | collapsin response mediator protein 1 |
| DTT | dithiothreitol |
| EAAT2 | excitatory amino acid transporter 2 |
| FA | formic acid |
| FCx | frontal cortices |
| GSK3B | glycogen synthase kinase 3β |
| GST 1-1 | glutathione S-transferase Mu 1 |
| hnRNP K | heterogeneous nuclear ribonucleoprotein K |
| Hp | hippocampi |
| LTP | long-term potentiation |
| NOG | noggin |
| NRF1 | nuclear respiratory factor 1 |
| OXPHOS | oxidative phosphorylation |
| PARK7 | Parkinson disease protein 7 homolog |
| PD | Parkinson’s disease |
| SCX | strong cation exchange |
| TFA | trifluoroacetic acid |
| TRX | thioredoxin |
Author Contributions
Rafał Olszanecki and Ryszard Korbut were responsible for the conception and design of the study. Aneta Stachowicz, Maciej Suski, and Katarzyna Głombik were responsible for analyses of the samples. Aneta Stachowicz, Maciej Suski, Agnieszka Basta-Kaim, Dariusz Adamek, and Rafał Olszanecki were responsible for the interpretation of the data. Aneta Stachowicz drafted the article. All authors revised the paper critically for important intellectual content and gave final approval of the version to be published.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Brookmeyer R., Johnson E., Ziegler-Graham K., Arrighi H.M. Forecasting the global burden of Alzheimer’s disease. Alzheimers Dement. J. Alzheimers Assoc. 2007;3:186–191. doi: 10.1016/j.jalz.2007.04.381. [DOI] [PubMed] [Google Scholar]
- 2.Smith M.A. Alzheimer’s disease. Int. Rev. Neurobiol. 1998;42:1–54. doi: 10.1002/smi.2460010406. [DOI] [PubMed] [Google Scholar]
- 3.Beal M.F. Mitochondrial dysfunction in neurodegenerative diseases. Biochim. Biophys. Acta. 1998;1366:211–223. doi: 10.1016/S0005-2728(98)00114-5. [DOI] [PubMed] [Google Scholar]
- 4.Chaturvedi R.K., Flint B.M. Mitochondrial diseases of the brain. Free Radic. Biol. Med. 2013;63:1–29. doi: 10.1016/j.freeradbiomed.2013.03.018. [DOI] [PubMed] [Google Scholar]
- 5.Orsucci D., Mancuso M., Ienco E.C., Simoncini C., Siciliano G., Bonuccelli U. Vascular factors and mitochondrial dysfunction: A central role in the pathogenesis of Alzheimer’s disease. Curr. Neurovasc. Res. 2013;10:76–80. doi: 10.2174/156720213804805972. [DOI] [PubMed] [Google Scholar]
- 6.Wang X., Wang W., Li L., Perry G., Lee H., Zhu X. Oxidative stress and mitochondrial dysfunction in Alzheimer’s disease. Biochim. Biophys. Acta. 2014;1842:1240–1247. doi: 10.1016/j.bbadis.2013.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hardas S.S., Sultana R., Clark A.M., Beckett T.L., Szweda L.I., Murphy M.P. Oxidative modification of lipoic acid by HNE in Alzheimer disease brain. Redox Biol. 2013;1:80–85. doi: 10.1016/j.redox.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Markesbery W.R., Lovell M.A. Four-hydroxynonenal, a product of lipid peroxidation, is increased in the brain in Alzheimer’s disease. Neurobiol. Aging. 1998;19:33–36. doi: 10.1016/S0197-4580(98)00009-8. [DOI] [PubMed] [Google Scholar]
- 9.Ohta S., Ohsawa I., Kamino K., Ando F., Shimokata H. Mitochondrial ALDH2 deficiency as an oxidative stress. Ann. N. Y. Acad. Sci. 2004;1011:36–44. doi: 10.1196/annals.1293.004. [DOI] [PubMed] [Google Scholar]
- 10.Zarkovic K. 4-Hydroxynonenal and neurodegenerative diseases. Mol. Aspects Med. 2003;24:293–303. doi: 10.1016/S0098-2997(03)00024-4. [DOI] [PubMed] [Google Scholar]
- 11.Chen C.-H., Sun L., Mochly-Rosen D. Mitochondrial aldehyde dehydrogenase and cardiac diseases. Cardiovasc. Res. 2010;88:51–57. doi: 10.1093/cvr/cvq192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perez-Miller S., Younus H., Vanam R., Chen C.H., Mochly-Rosen D., Hurley T.D. Alda-1 is an agonist and chemical chaperone for the common human aldehyde dehydrogenase 2 variant. Nat. Struct. Mol. Biol. 2010;17:159–164. doi: 10.1038/nsmb.1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen C.-H., Budas G.R., Churchill E.N., Disatnik M.-H., Hurley T.D., Mochly-Rosen D. Activation of aldehyde dehydrogenase-2 reduces ischemic damage to the heart. Science. 2008;321:1493–1495. doi: 10.1126/science.1158554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stachowicz A., Olszanecki R., Suski M., Wiśniewska A., Totoń-Żurańska J., Madej J. Mitochondrial aldehyde dehydrogenase activation by Alda-1 inhibits atherosclerosis and attenuates hepatic steatosis in apolipoprotein E-knockout mice. J. Am. Heart Assoc. 2014;3:e001329. doi: 10.1161/JAHA.114.001329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo Y., Yu W., Sun D., Wang J., Li C., Zhang R. A novel protective mechanism for mitochondrial aldehyde dehydrogenase (ALDH2) in type I diabetes-induced cardiac dysfunction: Role of AMPK-regulated autophagy. Biochim. Biophys. Acta. 2014;1852:319–331. doi: 10.1016/j.bbadis.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 16.Chiu C.C., Yeh T.H., Lai S.C., Wu-Chou Y.H., Chen C.H., Mochly-Rosen D. Neuroprotective effects of aldehyde dehydrogenase 2 activation in rotenone-induced cellular and animal models of parkinsonism. Exp. Neurol. 2015;263:244–253. doi: 10.1016/j.expneurol.2014.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stachowicz A., Głombik K., Olszanecki R., Basta-Kaim A., Suski M., Lasoń W. The impact of mitochondrial aldehyde dehydrogenase (ALDH2) activation by Alda-1 on the behavioral and biochemical disturbances in animal model of depression. Brain Behav. Immun. 2015 doi: 10.1016/j.bbi.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 18.Solito R., Corti F., Chen C.-H., Mochly-Rosen D., Giachetti A., Ziche M. Mitochondrial aldehyde dehydrogenase-2 activation prevents β-amyloid-induced endothelial cell dysfunction and restores angiogenesis. J. Cell Sci. 2013;126:1952–1961. doi: 10.1242/jcs.117184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holtzman D.M., Herz J., Bu G. Apolipoprotein E and apolipoprotein E receptors: Normal biology and roles in Alzheimer disease. Cold Spring Harb. Perspect. Med. 2012;2:a006312. doi: 10.1101/cshperspect.a006312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jiang Q., Lee C.Y.D., Mandrekar S., Wilkinson B., Cramer P., Zelcer N. ApoE promotes the proteolytic degradation of Abeta. Neuron. 2008;58:681–693. doi: 10.1016/j.neuron.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kristal B.S., Park B.K., Yu B.P. 4-Hydroxyhexenal is a potent inducer of the mitochondrial permeability transition. J. Biol. Chem. 1996;271:6033–6038. doi: 10.1074/jbc.271.11.6033. [DOI] [PubMed] [Google Scholar]
- 22.Montine K.S., Reich E., Neely M.D., Sidell K.R., Olson S.J., Markesbery W.R. Distribution of reducible 4-hydroxynonenal adduct immunoreactivity in Alzheimer disease is associated with APOE genotype. J. Neuropathol. Exp. Neurol. 1998;57:415–425. doi: 10.1097/00005072-199805000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Imaizumi K. Diet and atherosclerosis in apolipoprotein E-deficient mice. Biosci. Biotechnol. Biochem. 2011;75:1023–1035. doi: 10.1271/bbb.110059. [DOI] [PubMed] [Google Scholar]
- 24.Jawien J. The role of an experimental model of atherosclerosis: ApoE-knockout mice in developing new drugs against atherogenesis. Curr. Pharm Biotechnol. 2012;13:2435–2439. doi: 10.2174/1389201011208062435. [DOI] [PubMed] [Google Scholar]
- 25.Masliah E., Mallory M., Ge N., Alford M., Veinbergs I., Roses A.D. Neurodegeneration in the central nervous system of apoE-deficient mice. Exp. Neurol. 1995;136:107–122. doi: 10.1006/exnr.1995.1088. [DOI] [PubMed] [Google Scholar]
- 26.Masliah E., Samuel W., Veinbergs I., Mallory M., Mante M., Saitoh T. Neurodegeneration and cognitive impairment in apoE-deficient mice is ameliorated by infusion of recombinant apoE. Brain Res. 1997;751:307–314. doi: 10.1016/S0006-8993(96)01420-5. [DOI] [PubMed] [Google Scholar]
- 27.Bradley-Whitman M.A., Lovell M.A. Biomarkers of lipid peroxidation in Alzheimer disease (AD): An update. Arch. Toxicol. 2015;89:1035–1044. doi: 10.1007/s00204-015-1517-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Plum S., Steinbach S., Abel L., Marcus K., Helling S., May C. Proteomics in neurodegenerative diseases: Methods for obtaining a closer look at the neuronal proteome. Proteomics Clin. Appl. 2015;9:848–871. doi: 10.1002/prca.201400030. [DOI] [PubMed] [Google Scholar]
- 29.Anderson R., Barnes J.C., Bliss T.V., Cain D.P., Cambon K., Davies H.A. Behavioural, physiological and morphological analysis of a line of apolipoprotein E knockout mouse. Neuroscience. 1998;85:93–110. doi: 10.1016/S0306-4522(97)00598-8. [DOI] [PubMed] [Google Scholar]
- 30.Jortner B.S. The return of the dark neuron. A histological artifact complicating contemporary neurotoxicologic evaluation. Neurotoxicology. 2006;27:628–634. doi: 10.1016/j.neuro.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 31.Arendt T. Disturbance of neuronal plasticity is a critical pathogenetic event in Alzheimer’s disease. Int. J. Dev. Neurosci. 2001;19:231–245. doi: 10.1016/S0736-5748(01)00007-7. [DOI] [PubMed] [Google Scholar]
- 32.Klyubin I., Cullen W.K., Hu N.-W., Rowan M.J. Alzheimer’s disease Aβ assemblies mediating rapid disruption of synaptic plasticity and memory. Mol. Brain. 2012;5:25. doi: 10.1186/1756-6606-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marcello E., Epis R., Saraceno C., di Luca M. Synaptic dysfunction in Alzheimer’s disease. Adv. Exp. Med. Biol. 2012;970:573–601. doi: 10.1007/978-3-7091-0932-8_25. [DOI] [PubMed] [Google Scholar]
- 34.Cheng A., Hou Y., Mattson M.P. Mitochondria and neuroplasticity. ASN Neuro. 2010;2:e00045. doi: 10.1042/AN20100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aisen P.S. Serum brain-derived neurotrophic factor and the risk for dementia. JAMA. 2014;311:1684–1685. doi: 10.1001/jama.2014.3120. [DOI] [PubMed] [Google Scholar]
- 36.Diniz B.S., Teixeira A.L. Brain-derived neurotrophic factor and Alzheimer’s disease: Physiopathology and beyond. Neuromolecular. Med. 2011;13:217–222. doi: 10.1007/s12017-011-8154-x. [DOI] [PubMed] [Google Scholar]
- 37.Markham A., Bains R., Franklin P., Spedding M. Changes in mitochondrial function are pivotal in neurodegenerative and psychiatric disorders: How important is BDNF? Br. J. Pharmacol. 2014;171:2206–2229. doi: 10.1111/bph.12531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Forlenza O.V., Teixeira A.L., Miranda A.S., Barbosa I.G., Talib L.L., Diniz B.S. Decreased neurotrophic support is associated with cognitive decline in non-demented subjects. J. Alzheimers Dis. 2015;46:423–429. doi: 10.3233/JAD-150172. [DOI] [PubMed] [Google Scholar]
- 39.Xu H., Huang W., Wang Y., Sun W., Tang J., Li D. The function of BMP4 during neurogenesis in the adult hippocampus in Alzheimer’s disease. Ageing Res. Rev. 2013;12:157–164. doi: 10.1016/j.arr.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 40.Fan X.T., Cai W.Q., Yang Z., Xu H.W., Zhang J.-H. Effect of antisense oligonucleotide of noggin on spatial learning and memory of rats. Acta Pharmacol. Sin. 2003;24:394–397. [PubMed] [Google Scholar]
- 41.Chuang T.T. Neurogenesis in mouse models of Alzheimer’s disease. Biochim. Biophys. Acta. 2010;1802:872–880. doi: 10.1016/j.bbadis.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 42.Su K.-Y., Chien W.-L., Fu W.-M., Yu I.-S., Huang H.-P., Huang P.-H. Mice deficient in collapsin response mediator protein-1 exhibit impaired long-term potentiation and impaired spatial learning and memory. J. Neurosci. 2007;27:2513–2524. doi: 10.1523/JNEUROSCI.4497-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Folci A., Mapelli L., Sassone J., Prestori F., D’Angelo E., Bassani S. Loss of hnRNP K impairs synaptic plasticity in hippocampal neurons. J. Neurosci. 2014;34:9088–9095. doi: 10.1523/JNEUROSCI.0303-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hutchins E.J., Szaro B.G. c-Jun N-terminal kinase phosphorylation of heterogeneous nuclear ribonucleoprotein K regulates vertebrate axon outgrowth via a posttranscriptional mechanism. J. Neurosci. 2013;33:14666–14680. doi: 10.1523/JNEUROSCI.4821-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rasband M.N., Tayler J., Kaga Y., Yang Y., Lappe-Siefke C., Nave K.-A. CNP is required for maintenance of axon-glia interactions at nodes of Ranvier in the CNS. Glia. 2005;50:86–90. doi: 10.1002/glia.20165. [DOI] [PubMed] [Google Scholar]
- 46.Silva P.N., Furuya T.K., Sampaio Braga I., Rasmussen L.T., de Labio R.W., Bertolucci P.H. CNP and DPYSL2 mRNA expression and promoter methylation levels in brain of Alzheimer’s disease patients. J. Alzheimers Dis. 2013;33:349–355. doi: 10.3233/JAD-2012-121192. [DOI] [PubMed] [Google Scholar]
- 47.Arrázola M.S., Varela-Nallar L., Colombres M., Toledo E.M., Cruzat F., Pavez L. Calcium/calmodulin-dependent protein kinase type IV is a target gene of the Wnt/β-catenin signaling pathway. J. Cell Physiol. 2009;221:658–667. doi: 10.1002/jcp.21902. [DOI] [PubMed] [Google Scholar]
- 48.Chen S.-D., Lin T.-K., Lin J.-W., Yang D.-I., Lee S.-Y., Shaw F.-Z. Activation of calcium/calmodulin-dependent protein kinase IV and peroxisome proliferator-activated receptor γ coactivator-1α signaling pathway protects against neuronal injury and promotes mitochondrial biogenesis in the hippocampal CA1 subfield after transient global ischemia. J. Neurosci. Res. 2010;88:3144–3154. doi: 10.1002/jnr.22469. [DOI] [PubMed] [Google Scholar]
- 49.Mbebi C., Sée V., Mercken L., Pradier L., Müller U., Loeffler J.-P. Amyloid precursor protein family-induced neuronal death is mediated by impairment of the neuroprotective calcium/calmodulin protein kinase IV-dependent signaling pathway. J. Biol. Chem. 2002;277:20979–20990. doi: 10.1074/jbc.M107948200. [DOI] [PubMed] [Google Scholar]
- 50.Iacono K.T., Brown A.L., Greene M.I., Saouaf S.J. CD147 immunoglobulin superfamily receptor function and role in pathology. Exp. Mol. Pathol. 2007;83:283–295. doi: 10.1016/j.yexmp.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Veinbergs I., Masliah E. Synaptic alterations in apolipoprotein E knockout mice. Neuroscience. 1999;91:401–403. doi: 10.1016/S0306-4522(98)00602-2. [DOI] [PubMed] [Google Scholar]
- 52.Sun M.-K., Alkon D.L. Carbonic anhydrase gating of attention: Memory therapy and enhancement. Trends Pharmacol. Sci. 2002;23:83–89. doi: 10.1016/S0165-6147(02)01899-0. [DOI] [PubMed] [Google Scholar]
- 53.Pedrós I., Petrov D., Allgaier M., Sureda F., Barroso E., Beas-Zarate C. Early alterations in energy metabolism in the hippocampus of APPswe/PS1dE9 mouse model of Alzheimer’s disease. Biochim. Biophys. Acta. 2014;1842:1556–1566. doi: 10.1016/j.bbadis.2014.05.025. [DOI] [PubMed] [Google Scholar]
- 54.Biswas M., Chan J.Y. Role of Nrf1 in antioxidant response element-mediated gene expression and beyond. Toxicol. Appl. Pharmacol. 2010;244:16–20. doi: 10.1016/j.taap.2009.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li M., Niu F., Zhu X., Wu X., Shen N., Peng X. PRRT2 mutant leads to dysfunction of glutamate signaling. Int. J. Mol. Sci. 2015;16:9134–9151. doi: 10.3390/ijms16059134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim K., Lee S.-G., Kegelman T.P., Su Z.-Z., Das S.K., Dash R. Role of excitatory amino acid transporter-2 (EAAT2) and glutamate in neurodegeneration: Opportunities for developing novel therapeutics. J. Cell Physiol. 2011;226:2484–2493. doi: 10.1002/jcp.22609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Takahashi K., Kong Q., Lin Y., Stouffer N., Schulte D.A., Lai L. Restored glial glutamate transporter EAAT2 function as a potential therapeutic approach for Alzheimer’s disease. J. Exp. Med. 2015;212:319–332. doi: 10.1084/jem.20140413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wirz K.T.S., Keitel S., Swaab D.F., Verhaagen J., Bossers K. Early molecular changes in Alzheimer disease: Can we catch the disease in its presymptomatic phase? J. Alzheimers Dis. 2014;38:719–740. doi: 10.3233/JAD-130920. [DOI] [PubMed] [Google Scholar]
- 59.Holzerova E., Danhauser K., Haack T.B., Kremer L.S., Melcher M., Ingold I. Human thioredoxin 2 deficiency impairs mitochondrial redox homeostasis and causes early-onset neurodegeneration. Brain J. Neurol. 2016;139:346–354. doi: 10.1093/brain/awv350. [DOI] [PubMed] [Google Scholar]
- 60.Lovell M.A., Xie C., Markesbery W.R. Decreased glutathione transferase activity in brain and ventricular fluid in Alzheimer’s disease. Neurology. 1998;51:1562–1566. doi: 10.1212/WNL.51.6.1562. [DOI] [PubMed] [Google Scholar]
- 61.Ariga H., Takahashi-Niki K., Kato I., Maita H., Niki T., Iguchi-Ariga S.M.M. Neuroprotective function of DJ-1 in Parkinson’s disease. Oxid. Med. Cell Longev. 2013;2013:683920. doi: 10.1155/2013/683920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang Y., Gong X.-G., Wang Z.-Z., Sun H.-M., Guo Z.-Y., Hu J.-H. Overexpression of DJ-1/PARK7, Parkinson’s disease-related protein, improves mitochondrial function via Akt phosphorylation on threonine 308 in dopaminergic neuron-like cells. Eur. J. Neurosci. 2016 doi: 10.1111/ejn.13216. [DOI] [PubMed] [Google Scholar]
- 63.Sai Y., Zou Z., Peng K., Dong Z. The Parkinson’s disease-related genes act in mitochondrial homeostasis. Neurosci. Biobehav. Rev. 2012;36:2034–2043. doi: 10.1016/j.neubiorev.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 64.Choi J., Sullards M.C., Olzmann J.A., Rees H.D., Weintraub S.T., Bostwick D.E. Oxidative damage of DJ-1 is linked to sporadic Parkinson and Alzheimer diseases. J. Biol. Chem. 2006;281:10816–10824. doi: 10.1074/jbc.M509079200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Savioz A., Leuba G., Vallet P.G. A framework to understand the variations of PSD-95 expression in brain aging and in Alzheimer’s disease. Ageing Res. Rev. 2014;18:86–94. doi: 10.1016/j.arr.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 66.Mendes C.T., Mury F.B., de Sá Moreira E., Alberto F.L., Forlenza O.V., Dias-Neto E. Lithium reduces Gsk3b mRNA levels: Implications for Alzheimer’s disease. Eur. Arch. Psychiatry Clin. Neurosci. 2009;259:16–22. doi: 10.1007/s00406-008-0828-5. [DOI] [PubMed] [Google Scholar]
- 67.Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCt Method. Methods San Diego Calif. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 68.Bradford M.M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 69.Taverner T., Karpievitch Y.V., Polpitiya A.D., Brown J.N., Dabney A.R., Anderson G.A. DanteR: An extensible R-based tool for quantitative analysis of −omics data. Bioinform. Oxf. Engl. 2012;28:2404–2406. doi: 10.1093/bioinformatics/bts449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vizcaíno J.A., Csordas A., del-Toro N., Dianes J.A., Griss J., Lavidas I. 2016 Update of the PRIDE database and its related tools. Nucleic Acids Res. 2016;44:447–456. doi: 10.1093/nar/gkv1145. [DOI] [PMC free article] [PubMed] [Google Scholar]