Abstract
Cell death is an innate capability of cells to be removed from microenvironment, if and when they are damaged by multiple stresses. Cell death is often regulated by multiple molecular pathways and mechanism, including apoptosis, autophagy, and necroptosis. The molecular network underlying these processes is often intertwined and one pathway can dynamically shift to another one acquiring certain protein components, in particular upon treatment with various drugs. The strategy to treat human cancer ultimately relies on the ability of anticancer therapeutics to induce tumor-specific cell death, while leaving normal adjacent cells undamaged. However, tumor cells often develop the resistance to the drug-induced cell death, thus representing a great challenge for the anticancer approaches. Numerous compounds originated from the natural sources and biopharmaceutical industries are applied today in clinics showing advantageous results. However, some exhibit serious toxic side effects. Thus, novel effective therapeutic approaches in treating cancers are continued to be developed. Natural compounds with anticancer activity have gained a great interest among researchers and clinicians alike since they have shown more favorable safety and efficacy then the synthetic marketed drugs. Numerous studies in vitro and in vivo have found that several natural compounds display promising anticancer potentials. This review underlines certain information regarding the role of natural compounds from plants, microorganisms and sea life forms, which are able to induce non-apoptotic cell death in tumor cells, namely autophagy and necroptosis.
Keywords: Cancer, Autophagy, Necroptosis, Paraptosis, Natural compounds
1. INTRODUCTION
Tumor cells often display the well-known and expanding traits (“hallmarks”) of cancer designated as “sustained proliferative signaling, resistance to cell death, tumor angiogenesis, enabling replicative immortality (self-sufficiency in growth signals), activating invasion and metastasis, evasion of growth suppression (insensitivity to anti-growth signals), metabolic reprogramming and deregulated metabolism, genome instability (mutations and epigenetics), tumor-promoting inflammation, and evasiveness from immune destruction”, as reviewed elsewhere [1, 2]. Accumulating evidence shows that ubiquitous disruptive environmental chemical exposures, especially associated with a late industrial revolution that have been shown to greatly increase the tumor incidence in humans affecting practically each of cancer hallmarks [3]. Moreover, these factors might to disrupt key pathways and mechanisms inducing oncogenic factors and repressing tumor-suppressing regulators, as reviewed elsewhere [4-14].
Programmed cell death is natural way of removing aged or damaged cells from the body, as reviewed elsewhere [4, 15-17]. Most of the anti-cancer therapies trigger various cell death mechanisms and pathways to eliminate tumor cells, while leaving normal cells unscathed as much as possible, as reviewed in [4, 15-17]. However, in cancer, de-regulated apoptotic signaling, particularly the activation of an anti-apoptotic systems, allows tumor cells to escape these treatments leading to uncontrolled proliferation resulting in tumor survival, and chemotherapeutic resistance often displayed by tumors [4, 15-17]. Up to date various pathways underlying the programmed cell death include apoptosis, autophagy, and necroptosis, as reviewed elsewhere [18-23]. While numerous reviews focused on the apoptotic pathways, extrinsic and intrinsic alike, we concentrate our efforts on the latest developments regarding autophagy and necroptosis induced by natural compounds in tumor cells [24-29]. Apoptosis is the most often occurred mechanism of tumor cell death induced upon chemotherapeutic treatment. Apoptosis is characterized by specific morphological and biochemical features distinct from other cell death pathways, including blebbing, cell shrinkage, nuclear fragmentation, and chromatin condensation, as well as activation of caspase cascade and mitochondrial processes, as reviewed in [30-32].
Autophagy is characterized by the formation of specific vesicles “autophagosomes”, which envelope denatured proteins, damaged protein aggregates and disintegrated cellular organelles. The content of autophagosomes is subsequently dumped into lysosomes for subsequent enzymatic degradation, as depicted in (Fig. 1) and reviewed elsewhere [30-33]. Additionally, a necroptotic process, which is characterized by alterations in plasma membranes leading to inflammatory cell functions, was recently found to be under genetically controlled program. Necroptosis can be induced by cytokines, pathogens, ischemia, heat, and irradiation triggering various pathways (e.g. death receptors, kinase cascades, and mitochondrial), as depicted in (Fig. 2) and reviewed in [34-36].
Fig. (1).
Schematic representation of autophagic pathway. Several cytoplasmic proteins interact to upregulate autophagy. mTOR, which inhibit autophagy, is regulated negatively by different steps modulated by MAPKs or p53. Once mTOR is inhibited, the formation of ULK complex, which is composed of FIP200, ULK1/2 and ATG13/101, is stimulated. In turn, ULK complex phosphorylates AMBRA1, leading to the activation of a complex that includes p-AMBRA1, BECN1, and VPS15/34 to the formation of phagophoro in the nucleation step. The elongation step is controlled by LC3B-II, which is conjugated to PE and regulated by ATG5/12/16 complex. The completion step includes the formation of an Autophagosome carrying the proteins or organelles, which fuses to Lysosome in the Maturation step, forming an Autolysosome. The final step consists in the Degradation of the content in the Autolysosome.
Fig. (2).
Schematic representation of autophagic pathway. Several cytoplasmic proteins interact to upregulate autophagy. mTOR, which inhibit autophagy, is regulated negatively by different steps modulated by MAPKs or p53. Once mTOR is inhibited, the formation of ULK complex, which is composed of FIP200, ULK1/2 and ATG13/101, is stimulated. In turn, ULK complex phosphorylates AMBRA1, leading to the activation of a complex that includes p-AMBRA1, BECN1, and VPS15/34 to the formation of phagophoro in the nucleation step. The elongation step is controlled by LC3B-II, which is conjugated to PE and regulated by ATG5/12/16 complex. The completion step includes the formation of an Autophagosome carrying the proteins or organelles, which fuses to Lysosome in the Maturation step, forming an Autolysosome. The final step consists in the Degradation of the content in the Autolysosome.
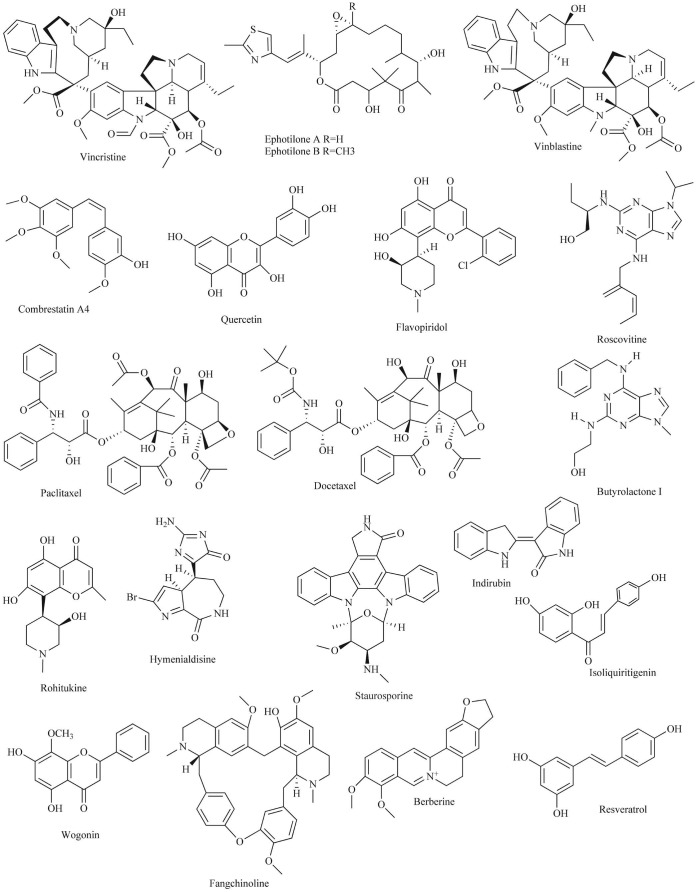
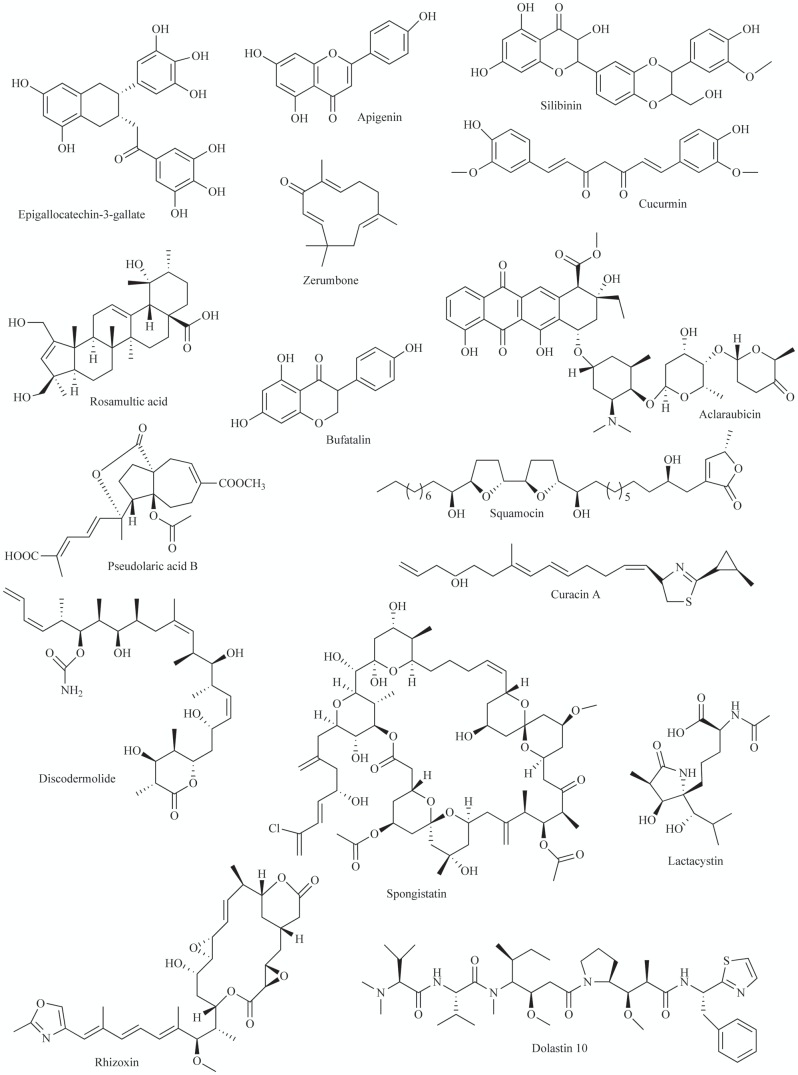
Naturally compounds originated from the diverse plants, microorganisms and marine life forms were widely shown to display anti-carcinogenic, anti-proliferative anti-survival effects inducing tumor cell death via various pathways, including apoptosis, autophagy, necroptosis, paraptosis, parthanatos or mitotic catastrophe, and through multiple molecular mechanisms, such as epigenetic regulation, protein kinase and protease cascades, nuclear and mitochondrial processes leading to cell death, as reviewed in [8, 24-29, 37-44]. Many natural compounds exhibited the ability to inhibit proliferation and cell viability of numerous tumor cells and inhibit tumor growth in animal models, suggesting the potential venue to generate novel anticancer therapeutics, as reviewed in [24-45]. Various compounds were found to induce tumor cell death by deregulating of signaling pathways leading to autophagy [8, 17, 24, 28, 29, 45-49].
2. AUTOPHAGY SIGNALING PATHWAYS
Autophagy is an intrinsic tightly controlled catabolic cellular process in which denatured proteins and damaged organelles are enveloped into autophagic vesicles and subsequently delivered to lysosomes for degradation, as reviewed elsewhere [50]. Autophagy is increased when cell under stress conditions, including metabolic alterations, genome instability, and oxygen deficiency, as well as chemotherapeutic treatments [50]. Notably, an overactive autophagy might cause tumor cell death process [51, 52]. Autophagy processes are designated as macroautophagy, microautophagy and chaperone-mediated autophagy [50-52]. Autophagy can promote a survival to stressful conditions; however, when stress exceeds certain level autophagy could induce a cell death process [50-52].
Autophagy-related genes, Atg (human homologs designated as ATG) were found to regulate autophagy [30, 31]. The autophagic signaling comprises several molecular events: autophagy induction, regulated by the ATG1/unc51-like kinase (ULK) complex; vesicle nucleation involving the BECN1/class III PI3K complex; vesicle elongation controlled by two ubiquitin-like conjugation systems (ATG12 and ATG8/LC3B); retrieval, in which the transmembrane ATG9 and associated proteins provide lipids and recruit other ATG proteins; and fusion between autophagosomes and lysosomes, involving proteins, such as lysosome-associated membrane protein 2 (LAMP2) and RAS-related protein-7 (RAB7A), resulting in vesicle breakdown and degradation by lysosomal hydrolases, as reviewed elsewhere [53-59]. Autophagy is initiated by the ULK1 kinase complex, consisting of ULK1, ATG13, and ATG17 proteins, as described in [53-59]. Meanwhile, vesicle-mediated vacuolar protein sorting (VPS34) protein (possessing the lipid kinase activity) forms a complex with BECN1 proteins after interacting with activating molecule in BECN1-regulated autophagy protein 1 (AMBRA1), SH3-domain GRB2-like endophilin B1 (also known as BIF1), and B-cell lymphoma 2 (BCL-2) proteins, as indicated in [53-59]. BECN1 phosphorylation induced by ULK1 kinase leads to activation of the ATG14L-containing VPS34 complex, which in turn promotes autophagy induction [53-59]. ATG12 and LC3B proteins, which exert the conjugation activities, are critical for transport of matured autophagosome [53-59]. After maturation, autophagosome joins with lysosomes to degrade its content [53-59].
Autophagy pathway involves two ubiquitin-like binding pathways, such as ATG5-ATG12 complex and microtubule-associated protein 1 light chain 3-beta (MAP1LC3B), which is encoded by one of the human homologue of the yeast Atg8, as indicated [60, 61]. Upon induction of autophagy, LC3B protein is cleaved by human ATG4 cysteine protease to produce LC3B-I isoform [60, 61]. As a result of that, LC3B-I is activated by ATG7 protein and is transferred to ATG3, before phosphatidylethanolamine (PE) is conjugated to the carboxyl glycine of LC3B-I to generate a LC3B-II isoform [60, 61]. The synthesis and processing of LC3B is increased during autophagy, making it a key marker of autophagy [30, 31]. The matured autophagosomes integrate with lysosomes, whose enzymes degrade the content of autophagosome generating small molecules, such as amino acids, subsequently used for de novo protein synthesis, thereby supporting cell survival and homeostasis [61].
3. AUTOPHAGIC SIGNALING IN CANCER
In normal cells, autophagy presents a mechanism, which cells develop to fight against malignant transformation, as reviewed elsewhere [62-64]. Various oncoproteins were found to inhibit, whereas and tumor suppressive proteins were shown to activate autophagy, as reviewed elsewhere [64]. However, autophagy contributes to cellular responses associated with extreme stress conditions, thus “favoring tumor progression” [64]. Therefore, autophagy can potentially modulate the pro-survival and pro-death mechanisms in tumor initiation and progression underlying its dual nature, as reviewed in [65]. Defective autophagy might contribute to tumorigenesis via accumulation of damaged organelles and protein aggregates, leading to a production of reactive oxygen species (ROS) and causing genome instability [65]. Altering autophagic signaling in order to induce tumor cell death, inhibit pro-survival of tumor cells and initiate crosstalk of autophagy with tissue-specific apoptosis might provide promising anticancer chemotherapeutic venues [65].
Many reports showed the tumor suppressive function of autophagy, as reviewed in [62, 63]. For example, BECN1 (a human homolog of yeast Atg6) is a key tumor suppressor protein, which acts through a modulating of initiation and regulation of autophagy. Frequent mono-allelic deletions of BECN1 were found in human breast, ovarian and prostate, lung and liver cancers [66, 67]. Autophagy is a central component of the integrated stress response, functioning to suppress apoptosis or just delay apoptotic cell death, as discussed in [50, 68]. Cisplatin-induced autophagy was shown to play a role in tumor cell resistance to platinum-based therapy [69]. Autophagy was found to delay apoptosis in renal tubular epithelial cells, as well as in head/neck and ovarian cancers treated with cisplatin [70-72]. Pharmacologic or genetic inhibition of autophagy often resulted in increased cell death, suggesting that autophagy might increase the cell survival upon genome damage through BECN1 induction, poly (ADP-ribose) polymerase-1 (PARP1) activation or heat shock protein B1 (HMGB1) release [71, 73, 74]. Autophagic flux upon cisplatin treatment was observed during tumor cell chemoresistance, nephrotoxicity and tubular cell injury [70, 72, 75-77].
As known guardians of genome integrity, tumor protein TP53, TP63 and TP73 transcription factors are often involved in autophagic process, as reviewed elsewhere [78]. Accumulating evidence clearly suggests that TP53 family members modulate expression of various genes involved in tumor cell death, and may induce the autophagic cell response [78, 79]. TP53 was found to variably affect the autophagic pathway, depending on its nuclear or cytoplasmic location. When in nucleus, TP53 could activate pro-apoptotic, cell cycle-arresting and pro-autophagic genes, as reviewed in [78-87]. However, cytoplasmic TP53 by triggering a mitochondrial mechanism could induce cell death and reduce autophagy [79, 84]. The critical autophagic modulators, DRAM1 (damage-regulated autophagy modulator) and ATG1/ULK1 (autophagy-initiation kinase) are transcriptionally activated by TP53 and subsequently induce autophagic pathways [78].
TP53 protein activates BCL-2 phosphorylation resulting in the dissociation of the BECN1-BCL-2 complex leading to a liberation of an essential autophagy inducer BECN1, as indicated in [88]. On the other hand, TP53 leads to the DRAM1 upregulation, thereby triggering accumulation of autophagosomes and autophagosome-lysosome fusion [78, 81-83]. TP53-induced autophagy may lead to cell death, which can be blocked by DRAM1 siRNA, as described in [79]. However, TP53-mediated autophagy may also increase tumor cell survival, as blockade of autophagosomal maturation enhances TP53-mediated tumor regression and tumor-cell death [78].
Recently, AEN/ISG20L1 protein was identified as a TP53- dependent, genotoxic stress-induced modulator of autophagy [82]. TP53, TP63 and TP73 proteins were found to transcriptionally regulate AEN expression, while AEN knockdown decreases levels of autophagic vacuoles and LC3B-II protein upon genotoxic stress [82]. Pro-apoptotic genes, such as TP53-upregulated modulator of apoptosis protein (PUMA) and BCL-2-associated X protein (BAX), were shown to act as positive regulators of autophagy (e.g. mitochondrial autophagy), as reviewed elsewhere [76]. Activated TP53 may down regulate the negative regulator of autophagy mTOR through transcriptional regulation of SESN1 and 2 [83]. The key signaling molecules, 5' AMP-activated protein kinase (AMPK, a positive regulator of autophagy), and mTOR (a negative autophagic regulator), which lie upstream of the autophagy core pathway [89]. AMPK may also inhibit mTOR by activating tuberous sclerosis (TSC) 1 and 2 proteins, as indicated in [89].
TP63 and TP73 share similar structure with TP53 and have both unique and coordinate roles during tumorigenesis. The inhibition of mTOR was shown to activate TP73 resulting in TP73-dependent modulation of genes involved in mTOR-induced autophagy, as described in [90]. Endogenous TP73 protein was found to transcriptionally activate specific autophagic genes, such as ATG5, ATG7, while TP73 knockdown increased the UVRAG expression levels [90].
TP53 homolog TP63 is a novel transcription factor implicated in regulation of genes involved in cell death and genome instability in head and neck squamous cell carcinomas (HNSCC) upon cisplatin exposure [76, 91]. Since TP63 gene exhibits two promoters and its transcripts undergo several alternative spliced events, TP63 encodes six protein isotypes with the long transactivation (TA)-domain and with the short TA-domain [76, 91]. The latter is designated as ΔNp63α, which is the longest and the most predominant isotype expressed in HNSCC cells, as indicated in [91]. ΔNp63α was found to induce ATM transcription, thereby contributing to ATM-TSC2-mTOR complex 1-dependent autophagic pathway [76, 89]. Follow-up studies found that the exposure of HNSCC cells to cisplatin treatment led to induced expression of the ATG1/ULK1, ATG3, ATG4A, ATG5, ATG6/BECN1, ATG7, ATG9A and ATG10 genes through ΔNp63α-dependent transcription, as described in [77].
Emerging evidence shows that autophagy is upregulated in tumor cells in response to various stresses, contributing to tumor cell resistance to chemotherapy, as reviewed in [51, 52, 63]. Thus, targeting autophagic signaling pathways may be an innovative strategy in prevention and combinatorial treatments of human cancers, as well battling the tumor-derived chemoresistance, as reviewed in [92, 93].
4. ANTICANCER NATURAL COMPOUNDS AND AUTOPHAGY
Besides chemotherapy, radiation, immune or genetic therapeutic strategies as well as combinatorial strategies, the natural anticancer products with favorable safety and efficacy are setting a center stage for the new venues anticancer therapies, as reviewed in [24-29, 36, 46-49, 94, 95]. Accumulating evidence shows that numerous natural compounds act as positive anticancer regulators through adjusting oxidative stress response, inhibiting cancer cell proliferation and modulating autophagic signaling [24-29, 36, 46-49, 94, 95].
The isoquinoline quaternary alkaloid berberine, isolated from plants of genera Berberis and Hydrasis, or contained in the extract of Rhizoma coptidis, possesses a broad range of therapeutic uses against several diseases, as reviewed elsewhere [96-104]. Berberine was found to inhibit tumor cell proliferation and exhibited cytotoxicity towards tumor cells [96-104]. Berberine was shown inducing autophagic and apoptotic cell death in hepatocellular carcinoma HepG2, MHCC97-1, and SMMC7721 cells, as indicated in [101]. Berberine treatment led to the activation of BECN1 and inhibition of mTOR by modulating the AKT activity and upregulating p38 MAPK signaling [101]. Tumor cell death induced by berberine was diminished with the autophagy inhibitor 3-methyladenine (3-MA), or silencing of the ATG5 expression, as described in [101]. 3-MA and bafilomycin A1, as well as siRNA-mediated silencing of LC3B or BECN1 abrogated berberine-induced cytotoxicity in HepG2 cells, whereas the caspase inhibitor z-VAD-fmk reversed it [100, 101]. Interestingly, the inhibition of AMPK by RNAi abrogated berberine induced caspase-3 (CASP-3) cleavage, apoptosis, and autophagy in HepG2 cells [100]. Berberine was shown to induce autophagic cell death in vitro and in vivo when used in combination with radiotherapy in lung cancer, as indicated in [103]. Berberine enhanced radiosensitivity in nonsmall cell lung cancer (NSCLC) A549 cells through autophagy, as evidenced by increased autophagosome formation, LC3B modification, and mitochondrial disruption, as described in [103]. Berberine derivatives were shown to inhibit the proliferation of human HCT-116 and SW613-B3 colon carcinoma cells and induce autophagy, as described in [96, 97, 99, 102, 104].
Resveratrol (3,5,4'-trihydroxy-trans-stilbene, a polyphenol extracted from red grape skin, peas, nuts, blueberries, mulberries, cranberries, spinaches and lilies) exhibited potent growth-inhibitory effects against various human cancer cells in vitro, and in preclinical cancer models in vivo, as reviewed elsewhere [105-111]. Treatment with resveratrol resulted in the autophagic death of human ovarian cancer A2780 cells through modulating expression of BCL-2 and BCL-xL proteins [112-114]. Resveratrol might triggers cell death via autophagic pathway, however independent from BECN1, in human breast cancer MCF-7 cell line, which is devoid of CASP-3 activity, as described in [115, 116]. Resveratrol was found to induce autophagic cell death in chronic myelogenous leukemia cells via activation of AMPK and JNK-mediated p62/SQSTM1 expression [117]. Downregulation of the TP53-Induced Glycolysis and Apoptosis Regulator (TIGAR) protein by resveratrol reduced glutathione levels resulting in sustained ROS production, subsequently leading to apoptosis and autophagy [118]. Overexpression and silencing of TIGAR were found affecting the ROS-dependent anticancer effects of resveratrol [118].
Resveratrol induced ROS levels in human ovarian cancer cells (OVCAR-3 and Caov-3), which triggers autophagy and subsequent apoptotic tumor cell death, as described elsewhere [119]. Resveratrol induced ATG5 expression and promoted LC3B cleavage [119]. Targeting ATG5 by siRNA also suppressed resveratrol-induced apoptotic cell death [119]. Resveratrol activates autophagic cell death in human prostate cancer PC3 and DU145 cells by downregulation of the stromal interaction molecule 1 (STIM1) expression leading to induction of endoplasmic reticulum stress, thereby, activating AMPK and inhibiting the AKT/mTOR pathway [120]. Resveratrol increased autophagy and autophagy-mediated degradation of p62 in non-small lung adenocarcinoma A549 cells [119]. Protein p62 (SQSTM1) was shown to co-localize with Fas/Cav-1 complexes, known to induce apoptosis [121]. However, silencing of p62 expression enhanced formation of Fas/Cav-1 complexes, suggesting that p62 inhibited Fas/Cav-1 complex formation [121]. Fas/Cav-1 complexes were found to trigger CASP8 activation and cleavage of BECN1, releasing a C-terminal of the latter, which subsequently translocated to the mitochondria leading to initiation of apoptosis. Inhibition of autophagy by siRNA to BECN1 also blocked resveratrol-induced apoptosis, showing a dependence of apoptosis on autophagy [121].
Resveratrol significantly inhibits the proliferation of human breast cancer stem-like cells isolated from MCF-7 and SUM159 tumors in vitro and in vivo, as described in [122]. Various techniques (e.g. transmission electron microscopy analysis, green fluorescent protein (GFP)-LC3B-II puncta formation assay and immunoblotting analysis of LC3B-II, BECN1 and ATG7 expression) showed that resveratrol induces autophagy in breast cancer stem-like cells [122]. Moreover, resveratrol was found to suppress Wnt/β-catenin signaling pathway in tested cells, while the overexpression of β-catenin markedly reduced resveratrol-induced cytotoxicity and autophagy [122]. Resveratrol inhibited the tumor cell proliferation and induced apoptosis and autophagy in T-acute lymphoblastic leukemia cells, which was accompanied by a decreased expression of antiapoptotic proteins (MCL-1 and BCL-2) and increased expression of proapoptotic proteins (BAX, BIM, and BAD), and induced cleaved-CASP-3, as described in [123]. Significant increase in LC3B-II/LC3B-I ratio and BECN1 expression was also detected upon resveratrol exposure [123]. Furthermore, resveratrol induced significant dephosphorylation of AKT, mTOR, p70 ribosomal protein S6 kinase (p70RS6K), and 4E-BP1, but enhanced specific phosphorylation of p38 MAPK, as indicated in [123]. Resveratrol induced autophagy in human androgen-independent prostate cancer cell lines (C42B, PC3, and DU145) via activation of sirtuin 1 (SIRT1, a mammalian silent mating type information regulation 2 homolog 1), as described elsewhere [124]. Silencing of SIRT1 expression inhibited autophagy by repressing phosphorylation of p70RS6K and 4E-BP1, while the molecular events were reversed in the presence of resveratrol [124].
Resveratrol and pterostilbene (a naturally occurring structural analog of resveratrol) have been reported to exert antiproliferative and proapoptotic effects in various human cancer cells, including human bladder, breast, cervical, colon, non-small lung cancer, and prostate cancer cells, glioma cells, melanoma cells, osteosarcoma U2O cells and leukemia HL-60 cells, as described elsewhere [110, 111, 125-132]. Pterostilbene induced conversion of cytosolic LC3B-I to membrane-bound LC3B-II and accumulation of large LC3B-positive vacuolar structures, as described in [127, 128]. 3,4,4'-trihydroxy-trans-stilbene (3,4,4'-THS), an analogue of resveratrol, increased the formation of acidic compartments, LC3B-II accumulation and GFP-LC3B labeled autophagosomes in human NSCLC A549 cells in vitro [125]. 3,4,4'-THS-induced apoptosis and autophagy in the cells was attenuated by NAC supporting the role for ROS in this process [125]. Pterostilbene induces tumor cell death via a mechanism involving lysosomal membrane permeabilization [128]. Human melanoma A375 cells and A549 lung cancer cells with low levels of heat shock protein (HSP)-70 showed high susceptibility to pterostilbene, whereas HT29 colon and MCF-7 breast cancer cells with higher levels of HSP70 were more resistant [128]. Silencing of HSP70 expression increased susceptibility of human colon cancer HT29 cells and breast cancer MCF-7 cells to pterostilbene [128].
Epigallocatechin-3-gallate (EGCG) is one of the major bioactive components in green tea, as reviewed elsewhere [108, 133-135]. EGCG enhanced the effect of cisplatin and oxaliplatin-induced autophagy in human colorectal cancer DLD-1 and HT-29 cells, as characterized by the accumulation of LC3B-II protein, the increase of acidic vesicular organelles, and the formation of autophagosome, as described in [136]. Exposure of squamous cell carcinoma SSC-4 cells to EGCG induced activation of apoptosis and autophagy, associated with upregulation of BAD, BAK, FAS, IGF1R, WNT11, and ZEB1 protein levels, and downregulation of CASP8, MYC, and TP53 proteins, as indicated in [137]. EGCG increases the formation of autophagosomes, increasing lysosomal acidification, and stimulating autophagic flux in hepatic cells in vitro and in vivo [138]. EGCG also increases phosphorylation of AMPK, as indicated in [138]. However, siRNA knockdown of AMPK inhibited EGCG-induced autophagy [138]. Treatment of human hepatocellular carcinoma Hep3B cells with doxorubicin (DOX) significantly increased a number of autophagic vesicles and levels of autophagic protein markers in tumor cells [139]. This effect resulted in 45% decrease in DOX-induced cell death supporting pro-survival role for autophagy in these experimental conditions [139]. However, EGCG was found to inhibit autophagic signaling, and promoted cellular growth inhibition, as indicated in [139]. The DOX-induced autophagy was blocked by the combination therapy with EGCG [139]. Rapamycin, an autophagic agonist, markedly inhibited the anticancer effect of DOX or its combination with EGCG treatment [139]. Interestingly, siRNAs targeting ATG5 and BECN11 inhibited autophagy pathways, thereby leading to an enhanced cell death in Hep3B cells [139]. On the other hand, EGCG-mediated cell death of human hepatocellular carcinoma HepG2 cells and cervical cancer HeLa cells was found to be caspase-independent and accompanied by cytosolic vacuolization [139]. Interestingly, EGCG was observed to increase non-apoptotic cell death in human hepatocellular carcinoma cells, cervical cancer cells, and mesothelioma cells via ROS-mediated lysosomal membrane permeabilization [140, 141].
Curcumin is the major bioactive component extracted from Curcuma longa L., Curcuma zedoaria (Christm) Rosc., Curcuma amada Roxb., and Curcuma petiolata, as reviewed in [24, 29, 49, 142]. Curcumin has been found to inhibit cell proliferation of chronic granulocytic leukemia, glioblastoma, breast, prostate, lung, skin, colon, and esophageal cancer through inducing autophagy [142-148]. Curcumin can inhibit the growth of leukemia K562 cells accompanied with the upregulation of LC3B-II and BECN1 protein levels, and accumulation of autophagosomes [144]. However, the autophagy inhibitor bafilomycin A1 inhibited the tumor cell death upon curcumin exposure [144]. Curcumin inhibited growth of human lung adenocarcinoma A549 cells by inducing autophagy, evidenced by LC3B immunofluorescence and increased expression of LC3B and SQSTM1, as described in [147]. The autophagy inhibitor 3-MA partly blocked the inhibitory effect of curcumin on the growth of A549 cells [147]. Curcumin was found to induce the AMPK phosphorylation in A549 cells, while the inactivation of the AMPK impaired the autophagy-inducing effect of curcumin [147]. Curcumin induced the expression of BECN1 and TP53, and ROS production, thereby activating autophagic pathway leading to the death in human colon cancer cells [148]. Curcumin markedly induced the LC3B-I to LC3B-II conversion and degradation of SQSTM1, as well as caused GFP-LC3B puncta formation in human colon colorectal carcinoma HCT-116 cells [148]. Antioxidant N-acetyl-l-cysteine (NAC) blocked these curcumin-induced molecular effects, suggesting that curcumin-induced ROS implicated in autophagosome development [148]. NAC also abolished curcumin-induced activation of ERK1/2 and p38MAPK, as indicated in [148].
In human glioblastoma cells (U87-MG and U373-MG) curcumin induced autophagy in vitro and in vivo through inhibiting the AKT/mTOR/p70RS6K pathway and activating the extracellular signal-regulated kinase (ERK)-1/2 pathway, as described elsewhere [143, 149]. Moreover, curcumin treatment resulted in the mitochondrial fission in human hepatocellular carcinoma HepG2 cells, reduced mitochondrial membrane potential and activated the mitochondria-mediated autophagy [150]. Forced overexpression of BCL-2 also blocked curcumin-induced autophagy in human breast cancer MCF-7 cells, through its inhibitory interactions with BECN1, as described in [146]. Pre-treatment of cells with PI3K inhibitor LY294002 enhanced curcumin-induced autophagy via modulating of autophagosome formation in MCF-7 cells [146]. ATG7 silencing further increased apoptotic potential of curcumin in wild type and BCL-2+ MCF-7 cells, as indicated in [146]. Curcumin could induce both apoptosis and autophagy in A431 squamous cell carcinoma cells expressing the p53R273H mutant, as shown in [151]. Rapamycin along with curcumin induced p53 degradation, and increased the autophagosome formation [151]. Silencing of BECN1 or ATG7 blocked the induction of autophagy leading to increasing p53 stability in curcumin-treated cells [151]. Curcumin inhibited the proliferation of human uterine leiomyosarcoma SKN and SK-UT-1 cells [152]. Curcumin induced autophagy and apoptosis in SKN and SK-UT-1 cells [152]. Curcumin increased ERK 1/2 activity in both SKN and SK-UT-1 cells, whereas PD98059, an MEK1 inhibitor, inhibited both the ERK1/2 pathway and curcumin-induced autophagy, as indicated in [152].
Curcumin exhibited anticancer activity against oral squamous cell carcinoma cells via induction of autophagy, marked by autophagic vacuoles formation, and evidenced the LC3B-I to LC3B-II conversion [153]. The curcumin-induced autophagy was shown to be ROS-dependent [153]. Curcumin reduced viability of human malignant pleural mesothelioma ACC-MESO-1 cells [154]. Curcumin increased LC3B-I-to -LC3B-II conversion, and induced the formation of autophagosomes, while silencing of ATG5 attenuated these changes, as described in [154]. Curcumin induced differentiation of glioma-initiating cells that are responsible for the initiation and recurrence of glioblastoma [155]. Curcumin was found to induce autophagy in these cells in vitro and in vivo [155]. Moreover, curcumin also suppressed tumor formation on intracranial implantation of glioma-initiating cells into mice [155]. Tetrahydrocurcumin, a major metabolite of curcumin, has been exhibited the antiproliferative affects on human promyelocytic leukemia HL-60 cells by increasing acidic vascular organelle formation, specific for autophagy [156]. Tetrahydrocurcumin significantly downregulated phosphatidylinositol 3-kinase/protein kinase B and mitogen-activated protein kinase pathways, including decreasing the phosphorylation of mTOR, glycogen synthase kinase 3β and p70RS6K, as indicated in [156].
Some of the Chinese medicinal herbs induce autophagy via downregulation of mTOR and upregulation of BECN1 [24, 43, 45]. Fangchinoline (isolated from Fangji, Stephenia tetrandra S. Moore) triggered autophagy in human hepatocellular carcinoma HepG2 and PLC/PRF/5 cells, as described in [157]. Blocking fangchinoline-induced autophagy process markedly modulated the apoptotic pathway [157]. Ginsenosides, major pharmacological active ingredients in Ginseng, induced cell death of tumor cells, thereby improving sensitivity of tumor cells to chemotherapy [24, 158-162]. Ginsenosides Rg3 and Rh2 can inhibit the tumor cell growth, while Rg3 is instrumental in combating tumor cell resistance to cancer chemotherapy, as reviewed in [24, 163]. Combination of Rg3 with docetaxel, paclitaxel, cisplatin or DOX increased the sensitivity of human colon and prostate cancer cells to chemotherapy [163]. The anticancer function of ginsenosides is associated with its ability to regulate autophagy in various human cancer cells, including hepatocellular carcinoma cells, as reviewed in [24, 164-166]. Rk1 can induce autophagy and increase expression of autophagy marker LC3B-II, as indicated in [165]. Ginsenoside K activated an autophagy pathway evidenced characterized by accumulation of vesicles and LC3B-II, and the increased autophagic flux [166]. Ginsenoside K induced the c-Jun NH2-terminal Kinase (JNK) signaling pathway, as described in [166]. Whereas silencing of JNK attenuated autophagy-mediated cell death in response to ginsenoside K, as indicated in [166]. Notably, ginsenoside K disrupted the interaction between ATG6 and BCL-2 leading to autophagic signaling [166]. Ginsenoside F2 was also found to induce the formation of GFP-LC3B-labeled autophagosomes and upregulate of ATG7 expression in human breast cancer cells [167].
Terpenoids are the largest class of natural compounds exhibited multiple anticancer properties, especially due to their selectivity toward tumor and cancer stem cells (CSC), as reviewed in [29, 168, 169]. Sesquiterpene lactones are 15-C terpenoids, such as parthenolide, artemisinin, and thapsigargin were shown to be beneficial in cancer clinical trials, as reviewed [169-172]. The sesquiterpene lactone parthenolide (4a, 5b-epoxy-germacra-1-(10), 11-(13)-dien-12, 6a-olide from the shoots of feverfew Tanacetum parthenium) was found to be selective against CSCs by targeting specific signaling pathways and epigenetic events [173, 174]. Parthenolide was found to induce autophagy in the triple-negative breast cancer MDA-MB231 cells, as shown by increased expression of BECN1, and the formation of LC3B-II [175]. Parthenolide treatment of human hepatocellular carcinoma HepG2 cells resulted in autophagic cell death, as indicated in [176]. Recently, the translation initiation factor eIF4E binding protein 1 (4E-BP1) was shown to be involved in parthenolide-mediated autophagic cell death in human promyelocytic leukemia HL-60 cells and cervical cancer HeLa cells which was independent of its role in protein translation [177].
Triptolide is a diterpenoid from the roots of Tripterygium wilfordii was found to inhibit the proliferation of 60 US National Cancer Institute cancer cell lines, as reviewed elsewhere [178, 179]. Furthermore, its anticancer activities were confirmed in various animal models grafted with human tumors resulting in the development of several more water-soluble and less toxic derivatives such as PG490-88 or F60008 that entered clinical trials [179]. Triptolide was shown to inhibit the growth of human pancreatic cancer cells in vitro and in vivo, including pancreatic adenocarcinomas [180, 181]. Triptolide may induce caspase-independent autophagic cell death in pancreatic cancer S2-013, S2-VP10, and Hs766T cells [181]. Triptolide treatment was reversed by 3-MA, or silencing of ATG5 and BECN1 [173]. A tripchlorolide was shown to suppress the tumor cell growth and induce autophagic cell death in human lung cancer A549 cells, as well as in human neuroblastoma SH-SY5Y cells with no observed signs of apoptosis [179, 182, 183]. Betulinic acid is a triterpenoid isolated from the bark of the white birch tree, exhibited anticancer properties against several tumor cells in vitro and in vivo [184, 185]. Betulinic acid and its analogues were found to decrease the phosphorylation of AKT and induce autophagic cell death in human glioblastoma cells, as described in [186]. However, in human multiple myeloma KM3 cells, betulinic acid treatment inhibited autophagy and induced apoptosis, associated with decreased BECN1 level, but increased CASP-3 level, as indicated [187]. Betulinic acid was recently found to induce the death in human cervical cancer HeLa cells, while caspase inhibitors and necrostatin-1 (NEC-1) blocked apoptosis and necroptosis, but not cell death in HeLa cells, implicating caspase-independent mechanisms of cell death in these cells [188].
Oridonin, a diterpenoid extracted from Rabdosia rubescens, reduced a proliferation of melanoma cells and cervical cancer cells in vitro and in vivo through regulating apoptosis and autophagy transcription factors [189]. Oridonin promoted autophagy in L929 cells through p38 MAPK and nuclear factor kappa B (NF-κB) pathways [190-193]. Terpinen-4-ol was shown to induce autophagic and apoptotic cell death in human promyelocytic leukemic HL-60 cells through inducing the accumulation of LC3B-I/-II, ATG5 and BECN1 proteins cytochrome C release from mitochondria, and decreasing BCL-xL expression [194]. Celastrol, an active compound extracted from the root bark of Tripterygium wilfordii Hook F., exhibiting a 20S proteasome inhibitor activity, while inducing apoptosis and autophagy in cancer cells [195-201]. Both apoptotic and autophagic pathways were found intertwined upon celastrol treatment, since inhibition of apoptosis enhanced autophagy, while suppression of autophagy diminished apoptosis via the ROS/JNK signaling pathway in human osteosarcoma cells [197]. Celastrol could induce hypoxia-inducible factor (HIF)-1α protein accumulation leading to transcriptional activation of HIF-1 target genes [198, 199]. Moreover, the celastrol-induced accumulation of HIF-1α increased the expression of BCL2/adenovirus E1B 19 kDa protein-interacting protein 3 (BNIP3), which induced autophagy in hepatocellular carcinoma HepG2 cells [198, 199]. Celastrol was found to exhibit potent anti-tumor activity against gliomas in xenografted mouse models.
Celastrol was observed to promote protein instability by accumulation of polyubiquitinated protein aggregates, p62 (SQSTM1), and heat-shock proteins, HSP72 and HSP90, as indicated in [200]. Celastrol induced autophagy in human gastric cancer AGS and YCC-2 cells accompanied with an increase in phosphorylated AMPK, and a decrease in phosphorylated AKT, mTOR and p70RS6K proteins [201]. Moreover, gastric tumor burdens were reduced by celastrol administration in a mouse model with grafted human gastric tumor [201]. Celastrol was found to promote paraptosis-like cytoplasmic vacuolization in human cervix cancer HeLa, lung cancer A549 and prostate cancer PC-3 cells, as indicated in [202].
Sulforaphane (1-isothiocyanato-4- (methylsulfinyl)-butane) is found in cruciferous vegetables, such as broccoli, cabbage, cauliflower and hoary weed, as reviewed elsewhere [203]. Sulforaphane exhibited antiproliferative properties toward various human tumor cells via multiple molecular mechanisms, as reviewed elsewhere [204-209]. Sulforaphane was shown to induce formation of autophagosome-like structures, as well as acidic vesicular organelles in human prostate cancer PC-3 cells, as described in [204]. Sulforaphane increased the LC3B-I protein levels, and promoted a LC3B-I to LC3B-II processing, as indicated in [202]. Upon sulforaphane exposure, tumor cells showed LC3B-II puncta associated with autophagosomes [204]. Sulforaphane was also shown to disrupt the BCL-2/BECN1 interaction leading to autophagic pathway initiated by liberated BECN1 [204]. Sulforaphane decreased the phosphorylated AKT-Ser473 level, and simultaneous treatment of sulforaphane with autophagy inhibitors, 3-MA or chloroquine enhanced drug cytotoxicity and inhibited tumor cell proliferation [204, 209].
Pyrrole colchicine mimetic, JG-03-14, that binds to the tubulin colchicine site was shown to promote cell death through autophagy in human breast cancer MCF-7 cells expressing wild type TP53 and MDA-MB-231 cells expressing mutant TP53 protein and in B16/F10 melanoma and the HCT-116 colon cancer cells, as described elsewhere [210, 211]. A novel derivative of allocolchicine (S)-3,8,9,10-tetramethoxyallocolchicine (also known as Green 1) was observed to promote autophagy and necroptosis in human pancreatic cancer PANC-1 cells and acute T cell leukemia cells (E6-1 or Jurkat), as indicated in [212]. Allicin, an organic sulfide from garlic Allium sativum, was found to exhibit antiproliferative effects on colon cancer, glioma and hepatocellular carcinoma cells, as reviewed in [213, 214]. Allicin can induce death of human hepatocellular carcinoma HepG2 cells through the reduced TP53 expression in the cytoplasm, inhibited PI3K/mTOR signaling pathway, reduced BCL-2 expression and enhanced AMPK/TSC2 and BECN1 pathways, as indicated in [215, 216].
Citreoviridin (CIT), a mycotoxin derived from fungal species (Penicillium citreoviride), was found to expression of LC3B-II protein in human hepatocellular carcinoma HepG2 cells [217, 218]. Inhibition of autophagosome formation with ATG5 siRNA attenuated CIT-induced lysosomal membrane permeabilization and tumor cell death, as indicated in [217]. Decrease in p62 (SQSTM1) levels and increase in LC3B turnover indicated that the accumulation of autophagosomes in the CIT-treated HepG2 cells [217, 218]. 7-hydroxydehydro-nuciferine (7-HDNF) isolated from the leaves of Nelumbo nucifera Gaertn cv. Rosa-plena is an effective inhibitor of melanoma tumor growth in a mouse xenografted model in vivo [219]. 7-HDNF induced an increased autophagic pathway in A375.S2 melanoma cells through the enhanced expression of BECN1 (also known as ATG6), ATG3, ATG12, ATG7, ATG10, ATG16 and ATG5 protein in a dose-dependent manner, as indicated in [219].
Monanchocidin A (MonA) is a novel alkaloid recently isolated from the marine sponge Monanchora pulchra [220]. MonA exhibited cytotoxic activity towards human genitourinary cancer cells, including cisplatin-sensitive and -resistant germ cell tumor cell lines, hormone-sensitive and castration-resistant prostate carcinoma cell lines and different bladder carcinoma cell lines, as described in [220]. In contrast, non-malignant cells were significantly less sensitive [220]. MonA was found to induce autophagy and lysosomal membrane permeabilization in tumor cells, while cytotoxicity and protein degradation could be inhibited by 3-MA, as indicated in [220]. Cryptotanshinone and dihydrotanshinone, two lipophilic tanshinones from a traditional Chinese medicine Salvia miltiorrhiza, were shown to induce autophagic flux and LC3B-II accumulation in multidrug-resistant colon cancer cells SW620 Ad300 cells [221]. Cardamonin (2', 4'-dihydroxy-6'-methoxychalcone) is derived from Alpinia katsumadai Hayata (Zingiberaceae), as described in [221]. Cardamonin inhibited cell proliferation, and enhanced autophagy in human colon colorectal carcinoma HCT-116 cells [222]. Peiminine enhances autophagic flux in HCT-116 cells though repressing the phosphorylation of mTOR, as described in [223]. Silencing ATG5 greatly reduced the peiminine-induced cell death in wild type HCT-116 cells, while treating BAX/BAK-deficient cells with peiminine resulted in significant cell death, as indicated [223].
Cannabinoids promote autophagy-dependent apoptosis in melanoma cells, as reviewed in [224]. Treatment with Δ (9)-Tetrahydrocannabinol (THC) activated autophagy, loss of cell viability, and apoptosis, whereas co-treatment with chloroquine or knockdown of ATG7, but not BECN1 or AMBRA1, prevented THC-induced autophagy and cell death in vitro, as described elsewhere [224]. Similarly, THC inhibited tumor growth of glioma cells in vitro and in animal models in vivo [225]. Moreover, the combined administration of THC and TMZ was more effective for inhibiting glioma growth, than the individual administration of any of these two agents [225]. Natural compounds from the plant Casimiora edulis, Zapotidine (Zap) and Oxo-Zapotidine (Oxo-Zap) alone, or in a combination with THC were found to dramatically reduce in the phosphorylated AKT levels in U87MG glioma cells [225]. Both drugs enhanced autophagic process by increasing LC3B-II/LC3B-I ratio [225].
Glycyrrhetinic acid (GA), one of the main constituents of the Glycyrrhiza uralensis Fisch, exerts potential anticancer effects toward human hepatocellular HepG2 cells [226]. GA reduced the cell viability, and enhanced the expression of LC3B-II in tumor cells, while choloroquine or bafilomycin A1 inhibited these processes [226]. Dihydromyricetin is a natural flavonol, was found to induce the expression of LC3B protein, the degradation of SQSTM1, and the formation of autophagosomes, as described in [227]. An aqueous extract of Hibiscus sabdariffa was shown to increase the expressions of autophagy-related proteins, ATG5, BECN1, and LC3B-I/-II conversion, and induce autophagic cell death in human skin malignant melanoma A375 cells, as indicated in [228]. Sann-Joong-Kuey-Jian-Tang (SJKJT), a Traditional Chinese Medicine, was found to induce autophagy in human BxPC-3 pancreatic adenocarcinoma cells [229]. SJKJT was shown to increase expression of mTOR, LC3B-II, BECN1, ATG3, ATG7 and ATG5, ATG12 proteins in BxPC-3 cells in vitro [229].
Seriniquinone, isolated from a marine bacterium of the genus Serinicoccus, demonstrated potent anti-proliferative activity toward melanoma cell lines by activation of autophagocytosis, while targeting small protein, dermcidin [230]. The cardiotonic steroid UNBS1450 0 from Calotropis procera was shown to autophagy-related cell death, by repressing NF-κB activation, as well as by downregulating c-MYC in cancer cells [231]. Oblongifolin C (OC), a natural small molecule compound extracted from Garcinia yunnanensis Hu, is a potent autophagic flux inhibitor, as described elsewhere [232-234]. Exposure to OC results in an increased number of autophagosomes and impaired degradation of SQSTM1/p62, as described in [233]. Follow-up studies in xenografted mice in vivo showed that OC has anticancer potency as revealed by increased staining of cleaved CASP-3, LC3 puncta, and SQSTM1, as well as reduced expression of lysosomal cathepsins [233]. Furthermore, OC was found to inhibit metastasis in human esophageal squamous carcinoma Eca109 cells and hepatocellular carcinoma HepG2 cells, as indicated in [235].
Plant lectins have been considered as possible anti-tumor drugs because of their ability to induce autophagic cell death, as reviewed elsewhere [236-243]. Polygonatum odoratum lectin (POL), a mannose-binding GNA-related lectin from traditional Chinese medicine herb, was shown to exhibit anti-proliferative and apoptosis-inducing activities toward a variety of cancer cells, as reviewed in [236]. POL could induce both apoptosis and autophagy in human breast cancer MCF-7 cells and NSCLC A549 cells [236, 237]. POL promoted apoptosis through inhibiting AKT/NF-κB pathway, while induced autophagy via suppressing AKT-mTOR pathway [236, 237]. Polygonatum cyrtonema lectin (PCL), a mannose/sialic acid-binding plant lectin, was shown to induce cancer cell autophagic death via activating mitochondrial ROS-p38-p53 pathway, as well as via blocking RAS-RAF and PI3K-AKT pathways [238-240]. PCL was shown to markedly inhibit the growth of human melanoma A375 cells while normal melanocytes were not affected [238-240]. PCL was found to induce both apoptosis and autophagy in A375 cells [239].
Experimental data confirmed that the ROS-p38MAPK-p53 pathway could be involved in the stimulation of autophagy, suggesting that autophagy may play a death-promoting role via the above-mentioned apoptotic pathway, as indicated in [238, 239]. ArtinM, a D-mannose-binding lectin from Artocarpus heterophyllus, interacts with N-glycosylated receptors on the surface of human myelocytic leukemia NB4 cells [241]. ArtinM was found to suppress tumor growth via induction of ROS generation and autophagy in NB4 cells [241]. Momordica charantia lectin (MCL) induced autophagy, and subsequently apoptosis in HCC cells, as indicated in [242]. Concanavalin-A (ConA) lectin was found to regulate expression of the autophagy biomarker BNIP3 in human U87 glioblastoma cells [243].
Thymoquinone exposure resulted in caspase-independent, autophagic cell death via mitochondrial outer membrane permeabilization and activation of JNK and p38 MAPK in human LoVo colon cancer cells [244]. Honokiol (HNK), purified from the Magnolia officinalis bark, is a promising anticancer agent against prostate cancer cells (PC-3 and LNCaP cells) in vitro and (PC-3 xenografts) in vivo [245]. The PC-3 tumor xenografts from HNK-treated mice contained higher levels of LC3B-II protein compared to control tumors [245]. Both cell viability inhibition and apoptosis induced by HNK was significantly decreased with 3-MA, as well as ATG5 RNAi, as indicated in [245]. Mollugin, a bioactive phytochemical isolated from Rubia cordifolia L., exhibited anticancer activity against various cancer cells [246]. Further experiments demonstrated that PI3K/AKT/mTOR/ p70RS6K and ERK signaling pathways participated in mollugin-induced autophagy and apoptosis [247]. Cyclovirobuxine D (CVB-D) could induce autophagy in the MCF-7 human breast cancer cell line evidenced by accumulation of autophagosomes and elevated LC3B fluorescent puncta, as well as increased LC3B-I-to-LC3B-II conversion, and the expression of ATG5, as described in [247]. CVB-D-induced autophagy and decrease in cell viability could be blocked by 3-MA [247].
Jujuboside B, a saponin from the seeds of Zizyphus jujuba var. spinosa, induced apoptosis and autophagy in human AGS and HCT-116 gastric adenocarcinoma cells in vitro and effectively suppressed tumor growth in a nude mouse xenograft model bearing HCT-116 cells in vivo [248]. Moreover, jujuboside B activated p38/c-Jun N-terminal kinase (JNK), and induced autophagy indicated by the formation of cytoplasmic vacuoles and LC3B-I/II conversion [248]. The autophagy inhibitor bafilomycin A1 decreased jujuboside B-induced cell viability, as indicated [248]. Feroniellin A (FERO), a novel furanocoumarin, was shown to induce autophagy, associated with LC3B-I to LC3B-II conversion, induction of GFP-LC3B puncta, enhanced expression of BECN1 and ATG5, and inactivation of mTOR in etoposide-resistant human lung carcinoma A549RT-eto cells [249]. Silencing of BECN1 by siRNA reduced FERO-induced apoptosis in A549RT-eto cells and activation of autophagy by rapamycin accelerated FERO-induced apoptosis [249].
5. NECROPTOSIS SIGNALING PATHWAYS, CANCER AND NATURAL COMPOUNDS
Necroptosis is classified as a programmed cell death in the absence of morphological traits of apoptosis or autophagy [15, 18, 20, 23, 34-36]. Upon necroptosis induced by the tumor necrosis factor α (TNFα) receptor ligand/TNFα receptor 1 (TNFR1), the latter recruits a receptor-interacting protein kinase (RIPK)-1- and -3, as reviewed elsewhere [35, 250-258]. Similarly, other death domain receptors trigger a non-apoptotic cell death resembling necroptosis, as indicated in [35, 250-258]. Upon death receptor oligomerization, they recruit various proteins, including TNFR-associated death domain (TRADD), cellular inhibitor of apoptosis proteins (cIAP), TNF receptor-associated factor (TRAF)-2, and -5, as well as RIPK-1 and -3 into a multimeric protein complex called TNFR1 complex I, as reviewed in [35, 250-258]. Within this complex, RIPK-1 is polyubiquitinated with lysine-63 (K63)-linked ubiquitin chains by cIAPs leading to the activation of the NF-κB signaling, as reviewed elsewhere [250-258]. After TNFR is rapidly internalized upon ligand binding, RIPK-1 becomes deubiquitinated by the cylindromatotis deubiquitinase (CYLD), as indicated [35, 259-262].
When CASP8 is inhibited or inactivated, RIPK-1 associates with RIPK-3, thereby triggering the necroptotic signaling pathway, as reviewed in [35, 250, 255]. On the other hand, activation of CASP8 leads to RIPK-1 cleavage and inactivation of necroptotic pathway [35, 250, 255]. This RIPK-1/RIPK-3 cytoplasmic protein complex called necrosome constitutes a key molecular platform of necroptosis, which involves the reciprocal phosphorylation of RIPK-1 and RIPK-3, as indicated in [35, 250, 256]. RIPK-3 subsequently phosphorylates the mixed-lineage kinase domain-like (MLKL) protein finalizing the necroptotic choice for cell death, as reviewed in [35, 262-264]. MLKL forms a homotrimer through its amino-terminal coiled-coil domain and is localized in the cell plasma membrane during TNF-induced necroptosis [263, 264]. TRPM7 (transient receptor potential melastatin related 7) was shown to act as MLKL downstream target for the mediation of calcium influx and TNF-induced necroptosis [264]. Notably, the final consequences of necroptotic cell death can be distinguished from apoptotic cell death, as the plasma membrane typically ruptures, resulting in the release of the intracellular content into the microenvironment, known as danger-associated molecular patterns (DAMPs), as reviewed in [265-267].
Emerging evidence shows that necroptosis can be disturbed in human cancers, including cervical and pancreatic cancers, leukemia, glioma, glioblastoma, fibroblastoma, neuroblastoma, as reviewed in [252, 268-282]. For example, RIPK-3 and CYLD were found to be deregulated in chronic lymphocytic leukemia (CLL) cells [273, 275]. Several natural compounds were shown to induce necroptosis in human tumor cells. For example, shikonin, a naphthoquinone derived from Lithospermum erythrorhizon Siebold & Zucc. (Zicao), was found to be the first natural product capable to induce both apoptosis and necroptosis in human several cancer cell lines, including human breast cancer MCF-7 cells, osteosarcoma cells, glioma/glioblastoma cells, multiple myeloma and leukemia cells, as reviewed elsewhere [282-295]. Shikonin-treated cells were showing morphological alterations distinct from those occurring in apoptosis or autophagic cell death [282-295]. The loss of plasma membrane integrity was one of the morphologic characteristics of necrotic cell death, as indicated in [282-295]. Shikonin exerts a dramatic anticancer effect on both primary and metastatic osteosarcoma by inducing RIPK-1 and 3- dependent necroptosis [282, 284]. Induction of cell death pathway by shikonin could be blocked a specific necroptosis inhibitor NEC-1, but not by general caspase inhibitor Z-VAD-fmk could block shikonin-induced of cell death pathway, suggesting the necroptotic pathway rather than apoptotic pathway is a signaling of choice in these experimental conditions [268, 282-295]. The number of K7 osteosarcoma necrotic cells caused by shikonin was decreased after being pretreated with NEC-1, as indicated in [282, 284]. Treatment with shikonin led to an increased expression of RIPK-1 and RIPK-3, while CASP-3, -6 and PARP were not activated in K7 and U2OS cells [282, 284]. Size of primary osteosarcoma tumors and lung metastases were significantly reduced by shikonin treatment accompanied the elevated levels for RIPK-1 and RIPK-3 proteins [282, 284]. Shikonin was observed to induce necroptotic cell death in cancer cells including drug- and apoptosis-resistant cancer cells that overexpress P-glycoprotein, multidrug resistance protein-1 (MRP1), breast cancer resistance protein-1 (BCRP1), BCL-2, or BCL-xL [282]. Shikonin-induced necroptosis can be reverted to apoptosis in the presence of necrostatin-1 (NEC-1), due to the conversion from mitochondrial inner to outer membrane permeability, which was associated with BAX translocation [268].
The combination of erlotinib (Tarceva, known inhibitor of EGFR kinase) and shikonin or its derivatives (e.g. deoxyshikonin, isobutyrylshikonin, acetylshikonin, β, β-dimethylacrylshikonin and acetylalkannin) showed synergistic cytotoxicity toward human glioblastoma U87MGΔEGFR cells (expressing kinase defective mutant of epidermal growth factor receptor, EGFR), as well as in EGFR-expressing cell lines, glioblastoma BS153 cells (wild type EGFR amplified), epidermoid skin cancer A431 cells (wild type EGFR) and glioblastoma DK-MG cells (mutated EGFR), as described elsewhere [285]. Shikonin inhibited EGFR phosphorylation and decreased phosphorylation of EGFR downstream molecules, including AKT, P44/42 MAPK and phospholipase C (PLC)-γ1, but also synergistically (along with erlotinib) inhibited ΔEGFR phosphorylation in U87MGΔEGFR cells [285]. Shikonin exerted potent cytotoxic effects on human multiple myeloma bortezomib-resistant KMS11/BTZ cells, as described in [286]. Shikonin (10-20 µM) induced cell death, which was inhibited by NEC-1, while its activity was unaffected by Z-VAD-fmk, suggesting the necroptotic nature of cell death in these cells [286]. Shikonin induced cell death in rat C6 and human U87 glioma cells, which was inhibited by NEC-1, not by pan-caspase inhibitor z-VAD-fmk [287]. The increased level of reactive oxygen species (ROS) caused by shikonin was attenuated by NEC-1 and blocking ROS by NAC rescued shikonin-induced cell death in both C6 and U87 glioma cells [287]. Moreover, shikonin upregulated the RIPK-1 protein level, but NAC suppressed RIPK-1 expression, suggesting a role for ROS in regulation of RIPK-1 expression [287]. The allosteric inhibitor of RIPK-1, NEC-1, was found to increase nuclear condensation and caspase activation induced by shikonin in human promyelocytic HL60 cells, bone marrow CLL K562 cells and primary leukemia cells [288]. Small interfering RNA (siRNA)-mediated knockdown of RIPK-1 significantly enhanced shikonin-induced cell death in K562 and HL60 cells [288]. Shikonin could circumvent drug resistance, displayed by tumor cells and mediated by P-glycoprotein, BCL-2 and BCL-xL, by induction of necroptosis [289-293]. Naturally-occurring shikonin analogues (deoxyshikonin, acetylshikonin, isobutyrylshikonin, beta, beta-dimethylacrylshikonin, isovalerylshikonin, alpha-methyl-n-butylshikonin) were found to induce necroptosis in resistant tumor cells overexpressing MDR1 and BCRP1, as indicated in [285-292]. Shikonin induced a cell death in human breast cancer MCF-7 cells distinct from apoptosis, and that the cell death was prevented by NEC-1, as described in [292-295].
Staurosporine, an inhibitor of protein kinases, was found to induce necroptosis in leukemia cells, when caspase activation is inhibited [296]. TNF-related apoptosis-inducing ligand (TRAIL) was recently described to induce necroptosis via RIPK-1-/RIPK-3-dependent PARP1 activation, thereby placing PARP1 activation as an effector mechanism downstream of RIPK-1 [297, 298]. Obatoclax (GX15-070), a small-molecule inhibitor of antiapoptotic BCL-2 proteins, was shown to induce autophagy-dependent necroptosis in glucocorticoid-resistant childhood acute lymphoblastic leukemia, as described elsewhere [299-301]. Obatoclax was found to induce assembly of necrosome on autophagosomal membranes [299]. Obatoclax increased the physical association of ATG5 with RIPK-1 and 3, as indicated in [299]. Furthermore, photodynamic therapy using the 5-aminolevulinic acid was found to trigger a RIPK-3-mediated necrosis in glioblastoma cells [302].
Piperlongumine (a natural product constituent of the fruit of the Piper longum), and Taurolidine (derivative of natural product taurine) were found to inhibit tumor cells growth in vitro and in vivo [303]. Piperlongumine may selectively kill some types cancer cells over normal cells [303]. Piperlongumine inhibits the growth of xenografted human malignant breast tumors in vivo [303]. Taurolidine induces cytotoxicity for various tumor cells in vitro and in vivo, including cancer stem cells [303]. The effect of Piperlongumine and Taurolidine is based on the induction of programmed cell death, largely via apoptosis but also necroptosis and autophagy via a redox-directed mechanism, as indicated in [303]. Annonaceous acetogenin mimic AA005 cell death in human colorectal adenocarcinoma SW620 cells, characterized by lack of CASP-3 activation or apoptotic body formation [304]. Decrease in ROS levels markedly reduced the AA005-mediated cell death in SW620 cells [304]. Moreover, repression of RIPK-1 by NEC-1 inhibited translocation of apoptosis-inducing factor and partially suppressed AA005-induced cell death in SW620 cells, suggesting the role for necroptotic pathway [304].
Eupomatenoid-5 (Eup-5), a neolignan isolated from Piper regnellii (Miq.) C. DC. var. regnellii leaves, was found to induce cell death in human breast cancer MCF-7 cells and kidney cancer 786-0 cells, as described in [305]. In MCF-7 cells, Eup-5 led to phosphatidylserine externalization and caspase activation, whereas Eup-5-treated 786-0 cells exhibited characteristics of programmed necroptosis process [305]. Green tea polyphenol was shown to induce BAX and BAK activation, cytochrome c release, caspase activation, and necroptosis of human hepatocellular carcinoma Hep3B cells [304]. Intriguingly, cytochrome c release and necroptosis were diminished in Hep3B cells lacking expression of BAX (BAX -/-), or BAK (BAK -/-), as indicated in [306].
Parthenolide was shown to induce necrosis and apoptosis simultaneously in human acute promyelocytic HL-60 cells and Jurkat T lymphoma cells [307]. The interaction of parthenolide with the plasma membrane led to membrane rupture and resulted in rapid necrotic cell death [308]. Intriguingly, parthenolide-mediated necrosis in human breast cancer MDA-MB231 cells was reduced by NAC and NEC-1, implying the role for activation of ROS and RIPK-1 in these processes [309]. Furthermore, parthenolide was found to inhibit the NF-κB activity associated with necrosis in multiple myeloma via targeting TNF receptor associated factor (TRAF)-6, as indicated in [310].
6. NATURAL COMPOUNDS AND OTHER CELL DEATH PATHWAYS
Under extreme stress conditions, cells undergo cell death, while employing multiple pathways, which are not limited to apoptosis, autophagy or necroptosis, as reviewed elsewhere [311, 312]. Some anticancer chemotherapies trigger multiple oncosuppressive mechanisms, including paraptosis, parthanatos, and mitotic catastrophe [311, 312]. A few natural compounds were shown to affect some of these pathways, as described below.
Paraptosis is morphologically distinct from apoptosis, autophagy and necrosis and characterized by cytoplasmic vacuole formation and late mitochondrial swelling and clumping, which is independent of caspase activation and inhibition, as reviewed in [313, 314]. In contrast to apoptosis, in which HMGB1 is localized to the nucleus, HMGB1 is released from the nucleus during paraptosis [313, 314]. Autophagic cell death inhibitor 3-MA is ineffective at inhibiting paraptosis [313, 314]. Many anticancer drugs, including natural compounds, have been shown to cause paraptosis in various human cancer cells. Paclitaxel (70μM) was found to induce a paraptosis-like cell death, suggesting that this pathway could be beneficial in treating apoptosis-resistant cancers [315]. γ-Tocotrienol, a vitamin E derived from palm oil, induced paraptosis-like cell death, while suppressing the Wnt signaling pathway in colon cancer cells [316]. Protopanaxadiols Rg3 and Rh2 were shown to induce cytosolic vacuolization in human colorectal cancer HCT116 cells [317]. Rh2-induced vacuolization was decreased by a MEK1/2 specific inhibitor U0126, thus supporting the MAPK-dependent mechanism underlying paraptosis [317]. Silencing of p53 reduced the ability of Rh2 to induce vacuole formation characteristic for paraptosis [317]. Honokiol from Magnolia officinalis can induce paraptosis in human leukemia NB4 cells [318]. Hesperidin, a flavanone glycoside found in citrus fruits, induced paraptotic cell death in human hepatocellular carcinoma HepG2 cells [319]. Celastrol, a triterpene extracted from Tripterygium wilfordii, was found to induce paraptosis in several human breast and colon cancer cell lines, which was characterized by extensive vacuolization in the endoplasmic reticulum and mitochondria [202, 320].
Excessive PARP-1 activation triggers a parthanatos, in which poly (ADP)-ribose (PAR) induces the mitochondrial release and nuclear translocation of apoptosis-inducing
factor (AIF) to initiate a chromatin destruction and subsequent cell death, as indicated [284, 321-325]. In contrast to apoptosis, parthanatos does not require activated caspases for its execution [321-325]. AIF binding to PAR is required for parthanatos both in vitro and in vivo, as reviewed in [321-325]. This interaction triggered AIF release from the cytosolic side of the mitochondrial outer membrane [321-325]. Sepantronium bromide (YM155), a survivin suppressant, inhibited growth of esophageal squamous-cell carcinoma xenografts in mice [326]. YM155 decreased survivin levels and caused PARP-1 activation, poly-ADP polymer formation, and AIF translocation from the cytosol to the nucleus [326]. Genetic knockdown of PARP-1 or AIF abrogated YM155-induced parthanatos cell death. PARP-1-stimulated expression of FOS, JUN and c-MYC transcription factors was also increased upon YM155 treatment [326].
Mitotic catastrophe is a cell death resulted from an aberrant chromosomal segregation, or DNA damage, as reviewed elsewhere [327-329]. It can be triggered by instability of microtubule, various anticancer drugs, as well as induced by ionizing radiation [327-329]. Altered cells resisting a mitotic catastrophe are likely to undergo oncogenesis, potentially leading to cancer [327-329]. Mitotic catastrophe is an intrinsic oncosuppressive mechanism that senses mitotic failure and responds by driving a cell to an irreversible antiproliferative death, as reviewed in [330]. Natural compounds were recently found to induce this type of cell death. For example, moscatilin from the orchid Dendrobium loddigesii, was found to exhibit anticancer activity and induce multipolar mitosis and subsequent multinucleation in moscatilin-treated cells, indicating the development of mitotic catastrophe in human SCC cells and adenocarcinoma cells [331]. 2-deprenyl-rheediaxanthone B (XB) isolated from the Metaxya rostrata C. Presl. (Metaxyaceae) induced loss of cell viability in human colorectal cancer cell lines [332]. Tumor cells exposed to the compound XB were incapable of undergoing regular mitosis due to downregulation of FoxM1 transcription factor and absence of chromosome condensation [332]. Intriguingly, the anti-apoptotic proteins BCL-2 and BCL-xL were upregulated; therefore caspase-3 was not activated upon exposure to the compound XB [332]. However, XB triggered Ataxia telangiectasia and Rad3 related (ATR) kinase damage pathway and activated caspase-2 causing tumor cell death by a mitotic catastrophe mechanism, as indicated in [332]. Flavone eupatorin isolated from Orthosiphon stamineus was found to reduce viability of various cancer cells through induction of mitotic catastrophe, accompanied by key molecular events defining apoptosis, as described in [333]. MMH01 from Antrodia cinnamomea was shown to decrease growth of human leukemia U937 and pancreatic cancer BxPC3 cells [334]. MMH01 was found to induce apoptosis and mitotic catastrophe in U937 cells, while trigger apoptosis or necrosis in BxPC3 cells [334]. A homeopathic medicine, Ruta isolated from Ruta graveolens was found to induce telomere erosion and mitotic catastrophe in human brain cancer and HL-60 leukemia cells in vitro and in vivo [335]. Ethanolic extract of Derris scandens Benth is a potent radiosensitizer of human colon cancer HT29 cells, as described in [336]. Treatment of HT29 cells with D. scandens extract in combination with gamma irradiation synergistically sensitizes HT29 cells to mitotic catastrophe by decreasing ERK1/2 activation [336].
CONCLUSION AND FUTURE PERSPECTIVES
Evasion from programmed cell death mechanisms is a hallmark of cancer contributing to tumor initiation, progression and tumor resistance to chemotherapy [1, 2, 4]. Thus, novel anticancer therapeutic solutions to reactivate cell death programs in human malignancies are welcomed. Accumulating evidence shows that natural compounds exert damaging effects on cancer cells with minimal adverse effects on the normal cells, therefore they hold a great promise for the future anticancer therapeutics [29]. More than 3000 plant species have been reported to treat cancer and about thirty plant-derived compounds have been isolated and tested in cancer clinical trials so far, as indicated in [29]. The molecular mechanisms of action for plant-derived anticancer drugs are often associated with cell death pathways, especially with intrinsic or extrinsic caspase-dependent apoptosis [20, 29, 42, 45, 65, 96, 108, 111, 156, 337-343]. A number of natural compounds reviewed in this work have shown to play a significant role in non-apoptotic pathways leading to tumor cell death, namely autophagy, necroptosis, paraptosis, parthanatos, and mitotic catastrophe [20, 29, 42, 45, 65, 96, 108, 111, 158, 284, 311-313, 321, 337-343]. The tumor suppressive action of natural compounds-induced autophagy may provoke apoptosis-independent cell death, and complement apoptotic cell death by robust or target-specific mechanisms [20, 29, 42, 45, 65, 96, 108, 111, 158, 337-343]. (Tables 1 and 2) summarize the ability of natural compounds to induce autophagy and other pathways leading to tumor cell death.
Table 1.
Effect of natural compounds on the autophagy in tumor cells.
| Compound Name | Compound Source | Tumor Cells | Mode of Action | Refs. | ||||
|---|---|---|---|---|---|---|---|---|
| Berberine | Rhizoma coptidis | nonsmall cell lung cancer A549 cells; hepatocellular carcinoma HepG2, MHCC97-1, and SMMC7721 cells; colon carcinoma HCT116 and SW613-B3 cells |
Activation of autophagic intermediates; BECN1, ATG5, LC3B-I/-II conversion | [94-102] | ||||
| Resveratrol | red grape skin, blueberries, mulberries, cranberries | ovarian cancer A2780 cells; breast cancer MCF-7 cells; ovarian cancer cells (OVCAR-3 and Caov-3); prostate cancer PC3 and DU145 cells; non-small lung adenocarcinoma A549 cells; in T-acute lymphoblastic leukemia cells | Activation of AMPK and JNK-mediated p62/SQSTM1 expression; ROS generation, induction of ATG5; increase in LC3B-I/LC3B-II conversion and BECN1 expression | [110-115, 117-119, 121] | ||||
| Epigallocatechin-3-gallate | Green tea | colorectal cancer DLD-1 and HT-29 cells; hepatocellular carcinoma HepG2 cells; cervical cancer cells, and mesothelioma cells | Inducing accumulation of LC3B-II protein; ROS-mediated lysosomal membrane permeabilization | [134, 137-139] | ||||
| Curcumin | Curcuma longa L., Curcuma zedoaria (Christm) Rosc., Curcuma amada Roxb., and Curcuma petiolata, | leukemia K562 cells; colon cancer cells; glioblastoma cells; colorectal carcinoma HCT116 cells, breast cancer MCF-7 cells; lung adenocarcinoma A549 cells; oral squamous cell carcinoma cells; malignant pleural mesothelioma ACC-MESO-1 cells | Induced the expression of BECN1 and TP53, and ROS production; induced LC3B-I/-II conversion; ATG5 expression; autophagosome formation; activation of AMPK signaling | [142, 144-147, 151, 152] | ||||
| Ginsenosides | Ginkgo biloba | hepatocellular carcinoma cells; breast cancer cells | induced LC3B-I/-II conversion; disrupted the interaction between ATG6 and BCL-2; upregulate of ATG7 expression | [163-165] | ||||
| Parthenolide | Tanacetum parthenium | breast cancer MDA-MB231 cells; hepatocellular carcinoma HepG2 cells; promyelocytic leukemia HL-60 cells and cervical cancer HeLa cells | Increased expression of BECN1, and LC3B-I/II conversion | [173-175] | ||||
| Triptolide | Tripterygium wilfordii | pancreatic cancer S2-013, S2-VP10, and Hs766T cells; lung cancer A549 cells; neuroblastoma SH-SY5Y cells | Activation of BECN1, ATG5, and LC3B-I/-II conversion | [177, 179, 181] | ||||
| Terpinen-4-ol | Tea tree oil | promyelocytic leukemic HL-60 cells | Activation of BECN1, ATG5, and LC3B-I/-II conversion | [192] | ||||
| Celastrol | Tripterygium wilfordii Hook F | hepatocellular carcinoma HepG2 cells; gastric cancer AGS and YCC-2 cells | Increased BNIP3 expression | [196] | ||||
| Sulforaphane | Brassicaceae | prostate cancer PC-3 cells | Increased LC3B-I/-II conversion; disrupts the BCL-2/BECN1 interaction | [197, 201] | ||||
| Allicin | Allium sativum | hepatocellular carcinoma HepG2 cells | Enhanced AMPK/TSC2 and BECN1 pathways | [212, 213] | ||||
| Citreoviridin | Penicillium citreoviride | hepatocellular carcinoma HepG2 cells | Increased LC3B-I/-II conversion; activation of ATG5 | [214, 215] | ||||
| 7-hydroxydehydronuciferine | Nelumbo nucifera Gaertn cv. Rosa-plena | melanoma A375.S2 cells | Enhanced expression of BECN1 (also known as ATG6), ATG3, ATG12, ATG7, ATG10, ATG16 and ATG5 protein | [216] | ||||
| Glycyrrhetinic acid | Glycyrrhiza uralensis Fisch | hepatocellular HepG2 cells | Increased LC3B-I/-II conversion | [223] | ||||
| Honokiol | Magnolia officinalis | prostate cancer PC-3 and LNCaP cells | Increased LC3B-I/-II conversion, ATG5 expression | [242] | ||||
| Jujuboside B | Zizyphus jujuba var. spinosa | gastric adenocarcinoma AGS cells; colon adenocarcinoma HCT116 cells | Increased LC3B-I/-II conversion | [245] | ||||
Table 2.
Effect of natural compounds on the necroptotic, paraptotic, parthanatos, and mitotic catastrophe pathways in tumor cells.
| Compound Name | Compound Source | Tumor Cells | Mode of Action | Refs. |
|---|---|---|---|---|
| Shikonin | Lithospermum erythrorhizon Siebold & Zucc. | breast cancer MCF-7 cells, osteosarcoma cells, glioma cells, multiple myeloma and leukemia cells | Induced RIPK-1 and RIPK-3 | [279, 280, 279, 287-299] |
| Piperlongumine | Piper longum | malignant breast tumors in xenografted mice in vivo | ROS production | [300] |
| Acetogenin mimic AA005 | Annonaceae | colorectal adenocarcinoma SW620 cells | ROS production; induced RIPK-1 | [301] |
| Eupomatenoid-5 | Piper regnellii (Miq.) C. DC. var. regnellii | kidney cancer 786-0 cells | necrosis morphology | [302] |
| Parthenolide | Tanacetum parthenium | acute promyelocytic HL-60 cells; Jurkat T lymphoma cells; breast cancer MDA-MB231 cells | Activation of ROS and RIPK-1 | [304-307] |
| γ-Tocotrienol, | vitamin E derived from palm oil | colon cancer cells | Paraptosis | [314] |
| Ginsenoside Rh2 | Ginseng biloba | colorectal cancer cells | Paraptosis | [315] |
| Honokiol | Magnolia officinalis, | leukemia NB4 cells | Paraptosis | [316] |
| Hesperidin | citrus fruits | hepatocellular carcinoma HepG2 cells | Paraptosis | [317] |
| Celastrol | Tripterygium wilfordii | breast and colon cancer cells | Paraptosis | [200, 318] |
| Moscatilin | Dendrobium loddigesii | squamous cell carcinoma and adenocarcinoma cells | Mitotic catastrophe | [328] |
| 2-deprenyl-rheediaxanthone B | Metaxya rostrata C. Presl | colorectal cancer cells | Mitotic catastrophe | [329] |
| Flavone eupatorin | Orthosiphon stamineus | various cancer cells | Mitotic catastrophe | [330] |
| MMH01 | Antrodia cinnamomea | leukemia U937 cells | Mitotic catastrophe | [331] |
| Ruta | Ruta graveolens | brain cancer and HL-60 leukemia cells | Mitotic catastrophe | [332] |
| Ethanolic extract | Derris scandens Benth | colon cancer HT29 cells | Mitotic catastrophe | [333] |
The understanding of molecular pathways involved in non-apoptotic cell death induced by these natural anticancer drugs would assist in exploiting novel molecular targets of plant-derived compounds necessary to advance more safe and effective anticancer therapeutics allowing to circumvent cancer drug resistance [20, 29, 42, 45, 65, 96, 108, 111, 158, 337-343]. The success with natural product shikonin, which able to induce multiple cell death mechanisms, supports the notion that natural compounds could bypass specific drug resistance developed by tumor cells using simultaneous activation of multiple death pathways (apoptosis, autophagy, necroptosis), as reviewed elsewhere [20, 29, 42, 45, 65, 96, 108, 111, 158, 337-343]. Thus, a rationalized combination of several cell death inducers that complement each other would maximize their efficacy while minimizing their side effects [20, 29, 42, 45, 65, 96, 108, 111, 158, 337-343]. While in vitro studies showed the strong ability of natural compounds to induce non-apoptotic death of tumor cells, more in vivo investigations needed to strengthen this notion before making a leap to clinical application [339-343].
ACKNOWLEDGEMENTS
Authors would like to express their gratitude to the Prometeo Project of the Secretariat for Higher Education, Science, Technology and Innovation (SENESCYT) of the Republic of Ecuador.
LIST OF ABBREVIATIONS
- AMPK
AMP-activated Protein Kinase
- ATG
Autophagy-related Gene
- ATR
Ataxia Telangiectasia and Rad3 Related
- BCL
B-cell Lymphoma
- BAX
BCL-2-associated X Protein
- cIAP
Cellular Inhibitor of Apoptosis Protein
- CIT
Citreoviridin
- CYLD
Cylindromatotis Deubiquitinase
- CSC
Cancer Stem Cells
- DRAM1
Damage-regulated Autophagy Modulator
- DAMP
Danger-associated Molecular Patterns
- DOX
Doxorubicin
- 4E-BP
eIF4E Binding Protein
- EGFR
Epidermal Growth Factor Receptor
- EGCG
Epigallocatechin-3-gallate
- ERK
Extracellular Signal-regulated Kinases
- GA
Glycyrrhetinic Acid
- HSP
Heat Shock Protein
- HDNF
Hydroxydehydronuciferine
- LAMP2
Lysosomal-associated Membrane Protein 2
- mTOR
Mammalian Target of Rapamycin
- 3-MA
Methyladenine
- MAP1LC3B
Microtubule-associated Protein 1 light chain 3-beta
- MLKL
Mixed-lineage Kinase Domain-like
- MonA
Monanchocidin A
- MCL
Momordica Charantia Lectin
- NAC
N-acetyl Cysteine
- NSCLC
Necrostatin, NEC, Nonsmall Cell Lung Cancer
- NF-κB
Nuclear Factor-kappa B
- Oxo-Zap
Oxo-Zapotidine
- PARP
Poly (ADP-ribose) Polymerase
- POL
Polygonatum Odoratum Lectin
- p70RS6K
p70 ribosomal Protein S6 Kinase
- PKB
Protein Kinase B
- PCL
Polygonatum Cyrtonema Lectin
- RIPK
Receptor-interacting Protein Kinase
- ROS
Reactive Oxygen Species
- SJKJT
Sann-Joong-Kuey-Jian-Tang
- SCC
Squamous Cell Carcinoma
- STIM1
Stromal Interaction Molecule 1
- TMZ
Temozolomide
- THC
Δ(9)-tetrahydrocannabinol
- TSC
Tuberous Sclerosis
- TNFα
Tumor Necrosis Factor α
- TRAIL
TNF-related Apoptosis-inducing Ligand
- TP
Tumor Protein
- PUMA
TP53-upregulated Modulator of Apoptosis Protein
- ULK
unc51-like Kinase
- Zap
Zapotidine
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Hanahan D., Weinberg R.A. The hallmarks of cancer. Cell. 2000;100(1):57–70. doi: 10.1016/S0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 2.Hanahan D., Weinberg R.A. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Goodson W.H., III, Lowe L., Carpenter D.O., Gilbertson M., Manaf Ali A., Lopez de Cerain Salsamendi A., Lasfar A., Carnero A., Azqueta A., Amedei A., Charles A.K., Collins A.R., Ward A., Salzberg A.C., Colacci A., Olsen A.K., Berg A., Barclay B.J., Zhou B.P., Blanco-Aparicio C., Baglole C.J., Dong C., Mondello C., Hsu C.W., Naus C.C., Yedjou C., Curran C.S., Laird D.W., Koch D.C., Carlin D.J., Felsher D.W., Roy D., Brown D.G., Ratovitski E., Ryan E.P., Corsini E., Rojas E., Moon E.Y., Laconi E., Marongiu F., Al-Mulla F., Chiaradonna F., Darroudi F., Martin F.L., Van Schooten F.J., Goldberg G.S., Wagemaker G., Nangami G.N., Calaf G.M., Williams G., Wolf G.T., Koppen G., Brunborg G., Lyerly H.K., Krishnan H., Ab Hamid H., Yasaei H., Sone H., Kondoh H., Salem H.K., Hsu H.Y., Park H.H., Koturbash I., Miousse I.R., Scovassi A.I., Klaunig J.E., Vondráček J., Raju J., Roman J., Wise J.P., Sr, Whitfield J.R., Woodrick J., Christopher J.A., Ochieng J., Martinez-Leal J.F., Weisz J., Kravchenko J., Sun J., Prudhomme K.R., Narayanan K.B., Cohen-Solal K.A., Moorwood K., Gonzalez L., Soucek L., Jian L., DAbronzo L.S., Lin L.T., Li L., Gulliver L., McCawley L.J., Memeo L., Vermeulen L., Leyns L., Zhang L., Valverde M., Khatami M., Romano M.F., Chapellier M., Williams M.A., Wade M., Manjili M.H., Lleonart M.E., Xia M., Gonzalez M.J., Karamouzis M.V., Kirsch-Volders M., Vaccari M., Kuemmerle N.B., Singh N., Cruickshanks N., Kleinstreuer N., van Larebeke N., Ahmed N., Ogunkua O., Krishnakumar P.K., Vadgama P., Marignani P.A., Ghosh P.M., Ostrosky-Wegman P., Thompson P.A., Dent P., Heneberg P., Darbre P., Sing Leung P., Nangia-Makker P., Cheng Q.S., Robey R.B., Al-Temaimi R., Roy R., Andrade-Vieira R., Sinha R.K., Mehta R., Vento R., Di Fiore R., Ponce-Cusi R., Dornetshuber-Fleiss R., Nahta R., Castellino R.C., Palorini R., Abd Hamid R., Langie S.A., Eltom S.E., Brooks S.A., Ryeom S., Wise S.S., Bay S.N., Harris S.A., Papagerakis S., Romano S., Pavanello S., Eriksson S., Forte S., Casey S.C., Luanpitpong S., Lee T.J., Otsuki T., Chen T., Massfelder T., Sanderson T., Guarnieri T., Hultman T., Dormoy V., Odero-Marah V., Sabbisetti V., Maguer-Satta V., Rathmell W.K., Engström W., Decker W.K., Bisson W.H., Rojanasakul Y., Luqmani Y., Chen Z., Hu Z. Assessing the carcinogenic potential of low-dose exposures to chemical mixtures in the environment: the challenge ahead. Carcinogenesis. 2015;36(Suppl. 1):S254–S296. doi: 10.1093/carcin/bgv039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Narayanan K.B., Ali M., Barclay B.J., Cheng Q.S., DAbronzo L., Dornetshuber-Fleiss R., Ghosh P.M., Gonzalez Guzman M.J., Lee T.J., Leung P.S., Li L., Luanpitpong S., Ratovitski E., Rojanasakul Y., Romano M.F., Romano S., Sinha R.K., Yedjou C., Al-Mulla F., Al-Temaimi R., Amedei A., Brown D.G., Ryan E.P., Colacci A., Hamid R.A., Mondello C., Raju J., Salem H.K., Woodrick J., Scovassi A.I., Singh N., Vaccari M., Roy R., Forte S., Memeo L., Kim S.Y., Bisson W.H., Lowe L., Park H.H. Disruptive environmental chemicals and cellular mechanisms that confer resistance to cell death. Carcinogenesis. 2015;36(Suppl. 1):S89–S110. doi: 10.1093/carcin/bgv032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu Z., Brooks S.A., Dormoy V., Hsu C.W., Hsu H.Y., Lin L.T., Massfelder T., Rathmell W.K., Xia M., Al-Mulla F., Al-Temaimi R., Amedei A., Brown D.G., Prudhomme K.R., Colacci A., Hamid R.A., Mondello C., Raju J., Ryan E.P., Woodrick J., Scovassi A.I., Singh N., Vaccari M., Roy R., Forte S., Memeo L., Salem H.K., Lowe L., Jensen L., Bisson W.H., Kleinstreuer N. Assessing the carcinogenic potential of low-dose exposures to chemical mixtures in the environment: focus on the cancer hallmark of tumor angiogenesis. Carcinogenesis. 2015;36(Suppl. 1):S184–S202. doi: 10.1093/carcin/bgv036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thompson P.A., Khatami M., Baglole C.J., Sun J., Harris S.A., Moon E.Y., Al-Mulla F., Al-Temaimi R., Brown D.G., Colacci A., Mondello C., Raju J., Ryan E.P., Woodrick J., Scovassi A.I., Singh N., Vaccari M., Roy R., Forte S., Memeo L., Salem H.K., Amedei A., Hamid R.A., Lowe L., Guarnieri T., Bisson W.H. Environmental immune disruptors, inflammation and cancer risk. Carcinogenesis. 2015;36(Suppl. 1):S232–S253. doi: 10.1093/carcin/bgv038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robey R.B., Weisz J., Kuemmerle N.B., Salzberg A.C., Berg A., Brown D.G., Kubik L., Palorini R., Al-Mulla F., Al-Temaimi R., Colacci A., Mondello C., Raju J., Woodrick J., Scovassi A.I., Singh N., Vaccari M., Roy R., Forte S., Memeo L., Salem H.K., Amedei A., Hamid R.A., Williams G.P., Lowe L., Meyer J., Martin F.L., Bisson W.H., Chiaradonna F., Ryan E.P. Metabolic reprogramming and dysregulated metabolism: cause, consequence and/or enabler of environmental carcinogenesis? Carcinogenesis. 2015;36(Suppl. 1):S203–S231. doi: 10.1093/carcin/bgv037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kravchenko J., Corsini E., Williams M.A., Decker W., Manjili M.H., Otsuki T., Singh N., Al-Mulla F., Al-Temaimi R., Amedei A., Colacci A.M., Vaccari M., Mondello C., Scovassi A.I., Raju J., Hamid R.A., Memeo L., Forte S., Roy R., Woodrick J., Salem H.K., Ryan E.P., Brown D.G., Bisson W.H., Lowe L., Lyerly H.K. Chemical compounds from anthropogenic environment and immune evasion mechanisms: potential interactions. Carcinogenesis. 2015;36(Suppl. 1):S111–S127. doi: 10.1093/carcin/bgv033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Langie S.A., Koppen G., Desaulniers D., Al-Mulla F., Al-Temaimi R., Amedei A., Azqueta A., Bisson W.H., Brown D.G., Brunborg G., Charles A.K., Chen T., Colacci A., Darroudi F., Forte S., Gonzalez L., Hamid R.A., Knudsen L.E., Leyns L., Lopez de Cerain Salsamendi A., Memeo L., Mondello C., Mothersill C., Olsen A.K., Pavanello S., Raju J., Rojas E., Roy R., Ryan E.P., Ostrosky-Wegman P., Salem H.K., Scovassi A.I., Singh N., Vaccari M., Van Schooten F.J., Valverde M., Woodrick J., Zhang L., van Larebeke N., Kirsch-Volders M., Collins A.R. Causes of genome instability: the effect of low dose chemical exposures in modern society. Carcinogenesis. 2015;36(Suppl. 1):S61–S88. doi: 10.1093/carcin/bgv031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Engström W., Darbre P., Eriksson S., Gulliver L., Hultman T., Karamouzis M.V., Klaunig J.E., Mehta R., Moorwood K., Sanderson T., Sone H., Vadgama P., Wagemaker G., Ward A., Singh N., Al-Mulla F., Al-Temaimi R., Amedei A., Colacci A.M., Vaccari M., Mondello C., Scovassi A.I., Raju J., Hamid R.A., Memeo L., Forte S., Roy R., Woodrick J., Salem H.K., Ryan E.P., Brown D.G., Bisson W.H. The potential for chemical mixtures from the environment to enable the cancer hallmark of sustained proliferative signalling. Carcinogenesis. 2015;36(Suppl. 1):S38–S60. doi: 10.1093/carcin/bgv030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nahta R., Al-Mulla F., Al-Temaimi R., Amedei A., Andrade-Vieira R., Bay S.N., Brown D.G., Calaf G.M., Castellino R.C., Cohen-Solal K.A., Colacci A., Cruickshanks N., Dent P., Di Fiore R., Forte S., Goldberg G.S., Hamid R.A., Krishnan H., Laird D.W., Lasfar A., Marignani P.A., Memeo L., Mondello C., Naus C.C., Ponce-Cusi R., Raju J., Roy D., Roy R., Ryan E.P., Salem H.K., Scovassi A.I., Singh N., Vaccari M., Vento R., Vondráček J., Wade M., Woodrick J., Bisson W.H. Mechanisms of environmental chemicals that enable the cancer hallmark of evasion of growth suppression. Carcinogenesis. 2015;36(Suppl. 1):S2–S18. doi: 10.1093/carcin/bgv028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carnero A., Blanco-Aparicio C., Kondoh H., Lleonart M.E., Martinez-Leal J.F., Mondello C., Scovassi A.I., Bisson W.H., Amedei A., Roy R., Woodrick J., Colacci A., Vaccari M., Raju J., Al-Mulla F., Al-Temaimi R., Salem H.K., Memeo L., Forte S., Singh N., Hamid R.A., Ryan E.P., Brown D.G., Wise J.P., Sr, Wise S.S., Yasaei H. Disruptive chemicals, senescence and immortality. Carcinogenesis. 2015;36(Suppl. 1):S19–S37. doi: 10.1093/carcin/bgv029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casey S.C., Vaccari M., Al-Mulla F., Al-Temaimi R., Amedei A., Barcellos-Hoff M.H., Brown D.G., Chapellier M., Christopher J., Curran C.S., Forte S., Hamid R.A., Heneberg P., Koch D.C., Krishnakumar P.K., Laconi E., Maguer-Satta V., Marongiu F., Memeo L., Mondello C., Raju J., Roman J., Roy R., Ryan E.P., Ryeom S., Salem H.K., Scovassi A.I., Singh N., Soucek L., Vermeulen L., Whitfield J.R., Woodrick J., Colacci A., Bisson W.H., Felsher D.W. The effect of environmental chemicals on the tumor microenvironment. Carcinogenesis. 2015;36(Suppl. 1):S160–S183. doi: 10.1093/carcin/bgv035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ochieng J., Nangami G.N., Ogunkua O., Miousse I.R., Koturbash I., Odero-Marah V., McCawley L.J., Nangia-Makker P., Ahmed N., Luqmani Y., Chen Z., Papagerakis S., Wolf G.T., Dong C., Zhou B.P., Brown D.G., Colacci A.M., Hamid R.A., Mondello C., Raju J., Ryan E.P., Woodrick J., Scovassi A.I., Singh N., Vaccari M., Roy R., Forte S., Memeo L., Salem H.K., Amedei A., Al-Temaimi R., Al-Mulla F., Bisson W.H., Eltom S.E. The impact of low-dose carcinogens and environmental disruptors on tissue invasion and metastasis. Carcinogenesis. 2015;36(Suppl. 1):S128–S159. doi: 10.1093/carcin/bgv034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu X., Xuan Y. Bypassing cancer drug resistance by activating multiple death pathwaysa proposal from the study of circumventing cancer drug resistance by induction of necroptosis. Cancer Lett. 2008;259(2):127–137. doi: 10.1016/j.canlet.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 16.Fuchs Y., Steller H. Live to die another way: modes of programmed cell death and the signals emanating from dying cells. Nat. Rev. Mol. Cell Biol. 2015;16(6):329–344. doi: 10.1038/nrm3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mohammad R.M., Muqbil I., Lowe L., Yedjou C., Hsu H.Y., Lin L.T., Siegelin M.D., Fimognari C., Kumar N.B., Dou Q.P., Yang H., Samadi A.K., Russo G.L., Spagnuolo C., Ray S.K., Chakrabarti M., Morre J.D., Coley H.M., Honoki K., Fujii H., Georgakilas A.G., Amedei A., Niccolai E., Amin A., Ashraf S.S., Helferich W.G., Yang X., Boosani C.S., Guha G., Bhakta D., Ciriolo M.R., Aquilano K., Chen S., Mohammed S.I., Keith W.N., Bilsland A., Halicka D., Nowsheen S., Azmi A.S. Broad targeting of resistance to apoptosis in cancer. Semin. Cancer Biol. 2015;35(Suppl.):S78–S103. doi: 10.1016/j.semcancer.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Su Z., Yang Z., Xu Y., Chen Y., Yu Q. Apoptosis, autophagy, necroptosis, and cancer metastasis. Mol. Cancer. 2015;14:48. doi: 10.1186/s12943-015-0321-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lalaoui N., Lindqvist L.M., Sandow J.J., Ekert P.G. The molecular relationships between apoptosis, autophagy and necroptosis. Semin. Cell Dev. Biol. 2015;39:63–69. doi: 10.1016/j.semcdb.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Radogna F., Dicato M., Diederich M. Cancer-type-specific crosstalk between autophagy, necroptosis and apoptosis as a pharmacological target. Biochem. Pharmacol. 2015;94(1):1–11. doi: 10.1016/j.bcp.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 21.Tait S.W., Ichim G., Green D.R. Die another waynon-apoptotic mechanisms of cell death. J. Cell Sci. 2014;127(Pt 10):2135–2144. doi: 10.1242/jcs.093575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nikoletopoulou V., Markaki M., Palikaras K., Tavernarakis N. Crosstalk between apoptosis, necrosis and autophagy. Biochim. Biophys. Acta. 2013;1833(12):3448–3459. doi: 10.1016/j.bbamcr.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Long J.S., Ryan K.M. New frontiers in promoting tumour cell death: targeting apoptosis, necroptosis and autophagy. Oncogene. 2012;31(49):5045–5060. doi: 10.1038/onc.2012.7. [DOI] [PubMed] [Google Scholar]
- 24.Zhang S.F., Wang X.L., Yang X.Q., Chen N. Autophagy-associated targeting pathways of natural products during cancer treatment. Asian Pac. J. Cancer Prev. 2014;15(24):10557–10563. doi: 10.7314/APJCP.2014.15.24.10557. [DOI] [PubMed] [Google Scholar]
- 25.Kim J., Park E.J. Cytotoxic anticancer candidates from natural resources. Curr. Med. Chem. Anticancer Agents. 2002;2(4):485–537. doi: 10.2174/1568011023353949. [DOI] [PubMed] [Google Scholar]
- 26.Kinghorn A.D., Chin Y.W., Swanson S.M. Discovery of natural product anticancer agents from biodiverse organisms. Curr. Opin. Drug Discov. Devel. 2009;12(2):189–196. [PMC free article] [PubMed] [Google Scholar]
- 27.Meiyanto E., Hermawan A. Anindyajati. Natural compounds for cancer-targeted therapy: citrus flavonoids as potent chemopreventive agents. Asian Pac. J. Cancer Prev. 2012;13:427–436. doi: 10.7314/APJCP.2012.13.2.427. [DOI] [PubMed] [Google Scholar]
- 28.Wang N., Feng Y. Elaborating the role of natural compounds-induced autophagy in cancer treatment: achievements and artifacts in the state of the art. 2015. [DOI] [PMC free article] [PubMed]
- 29.Gali-Muhtasib H., Hmadi R., Kareh M., Tohme R., Darwiche N. Cell death mechanisms of plant-derived anticancer drugs: beyond apoptosis. Apoptosis. 2015;20(12):1531–1562. doi: 10.1007/s10495-015-1169-2. [DOI] [PubMed] [Google Scholar]
- 30.Levine B., Kroemer G. Autophagy in the pathogenesis of disease. Cell. 2008;132(1):27–42. doi: 10.1016/j.cell.2007.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mizushima N. The role of the Atg1/ULK1 complex in autophagy regulation. Curr. Opin. Cell Biol. 2010;22(2):132–139. doi: 10.1016/j.ceb.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 32.Mizushima N., Yoshimori T., Ohsumi Y. The role of Atg proteins in autophagosome formation. Annu. Rev. Cell Dev. Biol. 2011;27:107–132. doi: 10.1146/annurev-cellbio-092910-154005. [DOI] [PubMed] [Google Scholar]
- 33.Yang Z., Klionsky D.J. Eaten alive: a history of macroautophagy. Nat. Cell Biol. 2010;12(9):814–822. doi: 10.1038/ncb0910-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vandenabeele P., Galluzzi L., Vanden Berghe T., Kroemer G. Molecular mechanisms of necroptosis: an ordered cellular explosion. Nat. Rev. Mol. Cell Biol. 2010;11(10):700–714. doi: 10.1038/nrm2970. [DOI] [PubMed] [Google Scholar]
- 35.Galluzzi L., Kepp O., Krautwald S., Kroemer G., Linkermann A. Molecular mechanisms of regulated necrosis. Semin. Cell Dev. Biol. 2014;35:24–32. doi: 10.1016/j.semcdb.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 36.Zhou W., Yuan J. Necroptosis in health and diseases. Semin. Cell Dev. Biol. 2014;35:14–23. doi: 10.1016/j.semcdb.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 37.Luo X., Yu X., Liu S., Deng Q., Liu X., Peng S., Li H., Liu J., Cao Y. The role of targeting kinase activity by natural products in cancer chemoprevention and chemotherapy (Review). Oncol. Rep. 2015;34(2):547–554. doi: 10.3892/or.2015.4029. [DOI] [PubMed] [Google Scholar]
- 38.Barrera L.N., Cassidy A., Johnson I.T., Bao Y., Belshaw N.J. Epigenetic and antioxidant effects of dietary isothiocyanates and selenium: potential implications for cancer chemoprevention. Proc. Nutr. Soc. 2012;71(2):237–245. doi: 10.1017/S002966511200016X. [DOI] [PubMed] [Google Scholar]
- 39.Shen M., Chan T.H., Dou Q.P. Targeting tumor ubiquitin-proteasome pathway with polyphenols for chemosensitization. Anticancer. Agents Med. Chem. 2012;12(8):891–901. doi: 10.2174/187152012802649978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cerella C., Dicato M., Jacob C., Diederich M. Chemical properties and mechanisms determining the anti-cancer action of garlic-derived organic sulfur compounds. Anticancer. Agents Med. Chem. 2011;11(3):267–271. doi: 10.2174/187152011795347522. [DOI] [PubMed] [Google Scholar]
- 41.Huang J., Plass C., Gerhauser C. Cancer chemoprevention by targeting the epigenome. Curr. Drug Targets. 2011;12(13):1925–1956. doi: 10.2174/138945011798184155. [DOI] [PubMed] [Google Scholar]
- 42.Fulda S. Modulation of apoptosis by natural products for cancer therapy. Planta Med. 2010;76(11):1075–1079. doi: 10.1055/s-0030-1249961. [DOI] [PubMed] [Google Scholar]
- 43.Wang S., Penchala S., Prabhu S., Wang J., Huang Y. Molecular basis of traditional Chinese medicine in cancer chemoprevention. Curr. Drug Discov. Technol. 2010;7(1):67–75. doi: 10.2174/157016310791162794. [DOI] [PubMed] [Google Scholar]
- 44.Sarkar F.H., Li Y. Harnessing the fruits of nature for the development of multi-targeted cancer therapeutics. Cancer Treat. Rev. 2009;35(7):597–607. doi: 10.1016/j.ctrv.2009.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang X., Feng Y., Wang N., Cheung F., Tan H.Y., Zhong S., Li C., Kobayashi S. Chinese medicines induce cell death: the molecular and cellular mechanisms for cancer therapy. 2014. [DOI] [PMC free article] [PubMed]
- 46.Zhou M., Wang R. Small-molecule regulators of autophagy and their potential therapeutic applications. ChemMedChem. 2013;8(5):694–707. doi: 10.1002/cmdc.201200560. [DOI] [PubMed] [Google Scholar]
- 47.Sun H., Wang Z., Yakisich J.S. Natural products targeting autophagy via the PI3K/Akt/mTOR pathway as anticancer agents. Anticancer. Agents Med. Chem. 2013;13(7):1048–1056. doi: 10.2174/18715206113139990130. [DOI] [PubMed] [Google Scholar]
- 48.Mukhtar E., Adhami V.M., Khan N., Mukhtar H. Apoptosis and autophagy induction as mechanism of cancer prevention by naturally occurring dietary agents. Curr. Drug Targets. 2012;13(14):1831–1841. doi: 10.2174/138945012804545489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang X., Chen L.X., Ouyang L., Cheng Y., Liu B. Plant natural compounds: targeting pathways of autophagy as anti-cancer therapeutic agents. Cell Prolif. 2012;45(5):466–476. doi: 10.1111/j.1365-2184.2012.00833.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kroemer G., Mariño G., Levine B. Autophagy and the integrated stress response. Mol. Cell. 2010;40(2):280–293. doi: 10.1016/j.molcel.2010.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen N., Karantza-Wadsworth V. Role and regulation of autophagy in cancer. 2009. [DOI] [PMC free article] [PubMed]
- 52.Chen N., Karantza V. Autophagy as a therapeutic target in cancer. Cancer Biol. Ther. 2011;11(2):157–168. doi: 10.4161/cbt.11.2.14622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wesselborg S., Stork B. Autophagy signal transduction by ATG proteins: from hierarchies to networks. Cell. Mol. Life Sci. 2015;72(24):4721–4757. doi: 10.1007/s00018-015-2034-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khalfan W.A., Klionsky D.J. Molecular machinery required for autophagy and the cytoplasm to vacuole targeting (Cvt) pathway in S. cerevisiae. Curr. Opin. Cell Biol. 2002;14(4):468–475. doi: 10.1016/S0955-0674(02)00343-5. [DOI] [PubMed] [Google Scholar]
- 55.Yorimitsu T., Klionsky D.J. Autophagy: molecular machinery for self-eating. Cell Death Differ. 2005;12(Suppl. 2):1542–1552. doi: 10.1038/sj.cdd.4401765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Codogno P., Meijer A.J. Autophagy and signaling: their role in cell survival and cell death. Cell Death Differ. 2005;12(Suppl. 2):1509–1518. doi: 10.1038/sj.cdd.4401751. [DOI] [PubMed] [Google Scholar]
- 57.Xie Z., Klionsky D.J. Autophagosome formation: core machinery and adaptations. Nat. Cell Biol. 2007;9(10):1102–1109. doi: 10.1038/ncb1007-1102. [DOI] [PubMed] [Google Scholar]
- 58.Maiuri M.C., Zalckvar E., Kimchi A., Kroemer G. Self-eating and self-killing: crosstalk between autophagy and apoptosis. Nat. Rev. Mol. Cell Biol. 2007;8(9):741–752. doi: 10.1038/nrm2239. [DOI] [PubMed] [Google Scholar]
- 59.Frankel L.B., Lund A.H. MicroRNA regulation of autophagy. Carcinogenesis. 2012;33(11):2018–2025. doi: 10.1093/carcin/bgs266. [DOI] [PubMed] [Google Scholar]
- 60.Romanov J., Walczak M., Ibiricu I., Schüchner S., Ogris E., Kraft C., Martens S. Mechanism and functions of membrane binding by the Atg5-Atg12/Atg16 complex during autophagosome formation. EMBO J. 2012;31(22):4304–4317. doi: 10.1038/emboj.2012.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Satoo K., Noda N.N., Kumeta H., Fujioka Y., Mizushima N., Ohsumi Y., Inagaki F. The structure of Atg4B-LC3 complex reveals the mechanism of LC3 processing and delipidation during autophagy. EMBO J. 2009;28(9):1341–1350. doi: 10.1038/emboj.2009.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Degenhardt K., Mathew R., Beaudoin B., Bray K., Anderson D., Chen G., Mukherjee C., Shi Y., Gélinas C., Fan Y., Nelson D.A., Jin S., White E. Autophagy promotes tumor cell survival and restricts necrosis, inflammation, and tumorigenesis. Cancer Cell. 2006;10(1):51–64. doi: 10.1016/j.ccr.2006.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mathew R., Karp C.M., Beaudoin B., Vuong N., Chen G., Chen H.Y., Bray K., Reddy A., Bhanot G., Gelinas C., Dipaola R.S., Karantza-Wadsworth V., White E. Autophagy suppresses tumorigenesis through elimination of p62. Cell. 2009;137(6):1062–1075. doi: 10.1016/j.cell.2009.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Galluzzi L., Pietrocola F., Bravo-San Pedro J.M., Amaravadi R.K., Baehrecke E.H., Cecconi F., Codogno P., Debnath J., Gewirtz D.A., Karantza V., Kimmelman A., Kumar S., Levine B., Maiuri M.C., Martin S.J., Penninger J., Piacentini M., Rubinsztein D.C., Simon H.U., Simonsen A., Thorburn A.M., Velasco G., Ryan K.M., Kroemer G. Autophagy in malignant transformation and cancer progression. EMBO J. 2015;34(7):856–880. doi: 10.15252/embj.201490784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Panda P.K., Mukhopadhyay S., Das D.N., Sinha N., Naik P.P., Bhutia S.K. Mechanism of autophagic regulation in carcinogenesis and cancer therapeutics. Semin. Cell Dev. Biol. 2015;39:43–55. doi: 10.1016/j.semcdb.2015.02.013. [DOI] [PubMed] [Google Scholar]
- 66.Qu X., Yu J., Bhagat G., Furuya N., Hibshoosh H., Troxel A., Rosen J., Eskelinen E.L., Mizushima N., Ohsumi Y., Cattoretti G., Levine B. Promotion of tumorigenesis by heterozygous disruption of the beclin 1 autophagy gene. J. Clin. Invest. 2003;112(12):1809–1820. doi: 10.1172/JCI20039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Laddha S.V., Ganesan S., Chan C.S., White E. Mutational landscape of the essential autophagy gene BECN1 in human cancers. Mol. Cancer Res. 2014;12(4):485–490. doi: 10.1158/1541-7786.MCR-13-0614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Guerrero-Preston R., Ratovitski E.A. 2013. [Google Scholar]
- 69.Borst P., Rottenberg S., Jonkers J. How do real tumors become resistant to cisplatin? Cell Cycle. 2008;7(10):1353–1359. doi: 10.4161/cc.7.10.5930. [DOI] [PubMed] [Google Scholar]
- 70.Kaushal G.P., Kaushal V., Herzog C., Yang C. Autophagy delays apoptosis in renal tubular epithelial cells in cisplatin cytotoxicity. Autophagy. 2008;4(5):710–712. doi: 10.4161/auto.6309. [DOI] [PubMed] [Google Scholar]
- 71.ODonovan T.R., OSullivan G.C., McKenna S.L. Induction of autophagy by drug-resistant esophageal cancer cells promotes their survival and recovery following treatment with chemotherapeutics. Autophagy. 2011;7(5):509–524. doi: 10.4161/auto.7.5.15066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang Y., Cheng Y., Ren X., Zhang L., Yap K.L., Wu H., Patel R., Liu D., Qin Z.H., Shih I.M., Yang J.M. NAC1 modulates sensitivity of ovarian cancer cells to cisplatin by altering the HMGB1-mediated autophagic response. Oncogene. 2012;31(8):1055–1064. doi: 10.1038/onc.2011.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Huang J., Liu K., Yu Y., Xie M., Kang R., Vernon P., Cao L., Tang D., Ni J. Targeting HMGB1-mediated autophagy as a novel therapeutic strategy for osteosarcoma. Autophagy. 2012;8(2):275–277. doi: 10.4161/auto.8.2.18940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wyrsch P., Blenn C., Bader J., Althaus F.R. Cell death and autophagy under oxidative stress: roles of poly(ADP-Ribose) polymerases and Ca(2+). Mol. Cell. Biol. 2012;32(17):3541–3553. doi: 10.1128/MCB.00437-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Harhaji-Trajkovic L., Vilimanovich U., Kravic-Stevovic T., Bumbasirevic V., Trajkovic V. AMPK-mediated autophagy inhibits apoptosis in cisplatin-treated tumour cells. J. Cell. Mol. Med. 2009;13(9B):3644–3654. doi: 10.1111/j.1582-4934.2009.00663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Huang Y., Ratovitski E.A. Phospho-ΔNp63α/Rpn13-dependent regulation of LKB1 degradation modulates autophagy in cancer cells. Aging (Albany, N.Y.) 2010;2(12):959–968. doi: 10.18632/aging.100249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Huang Y., Guerrero-Preston R., Ratovitski E.A. Phospho-ΔNp63α-dependent regulation of autophagic signaling through transcription and micro-RNA modulation. Cell Cycle. 2012;11(6):1247–1259. doi: 10.4161/cc.11.6.19670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ryan K.M. p53 and autophagy in cancer: guardian of the genome meets guardian of the proteome. Eur. J. Cancer. 2011;47(1):44–50. doi: 10.1016/j.ejca.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 79.Sui X., Jin L., Huang X., Geng S., He C., Hu X. p53 signaling and autophagy in cancer: a revolutionary strategy could be developed for cancer treatment. Autophagy. 2011;7(6):565–571. doi: 10.4161/auto.7.6.14073. [DOI] [PubMed] [Google Scholar]
- 80.Crighton D., Wilkinson S., OPrey J., Syed N., Smith P., Harrison P.R., Gasco M., Garrone O., Crook T., Ryan K.M. DRAM, a p53-induced modulator of autophagy, is critical for apoptosis. Cell. 2006;126(1):121–134. doi: 10.1016/j.cell.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 81.Crighton D., OPrey J., Bell H.S., Ryan K.M. p73 regulates DRAM-independent autophagy that does not contribute to programmed cell death. Cell Death Differ. 2007;14(6):1071–1079. doi: 10.1038/sj.cdd.4402108. [DOI] [PubMed] [Google Scholar]
- 82.Eby K.G., Rosenbluth J.M., Mays D.J., Marshall C.B., Barton C.E., Sinha S., Johnson K.N., Tang L., Pietenpol J.A. ISG20L1 is a p53 family target gene that modulates genotoxic stress-induced autophagy. Mol. Cancer. 2010;9:95. doi: 10.1186/1476-4598-9-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Maiuri M.C., Malik S.A., Morselli E., Kepp O., Criollo A., Mouchel P.L., Carnuccio R., Kroemer G. Stimulation of autophagy by the p53 target gene Sestrin2. Cell Cycle. 2009;8(10):1571–1576. doi: 10.4161/cc.8.10.8498. [DOI] [PubMed] [Google Scholar]
- 84.Tasdemir E., Maiuri M.C., Galluzzi L., Vitale I., Djavaheri-Mergny M., DAmelio M., Criollo A., Morselli E., Zhu C., Harper F., Nannmark U., Samara C., Pinton P., Vicencio J.M., Carnuccio R., Moll U.M., Madeo F., Paterlini-Brechot P., Rizzuto R., Szabadkai G., Pierron G., Blomgren K., Tavernarakis N., Codogno P., Cecconi F., Kroemer G. Regulation of autophagy by cytoplasmic p53. Nat. Cell Biol. 2008;10(6):676–687. doi: 10.1038/ncb1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kenzelmann Broz D., Attardi L.D. TRP53 activates a global autophagy program to promote tumor suppression. Autophagy. 2013;9(9):1440–1442. doi: 10.4161/auto.25833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kenzelmann Broz D., Spano Mello S., Bieging K.T., Jiang D., Dusek R.L., Brady C.A., Sidow A., Attardi L.D. Global genomic profiling reveals an extensive p53-regulated autophagy program contributing to key p53 responses. Genes Dev. 2013;27(9):1016–1031. doi: 10.1101/gad.212282.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kusama Y., Sato K., Kimura N., Mitamura J., Ohdaira H., Yoshida K. Comprehensive analysis of expression pattern and promoter regulation of human autophagy-related genes. Apoptosis. 2009;14(10):1165–1175. doi: 10.1007/s10495-009-0390-2. [DOI] [PubMed] [Google Scholar]
- 88.Maiuri M.C., Criollo A., Kroemer G. Crosstalk between apoptosis and autophagy within the Beclin 1 interactome. EMBO J. 2010;29(3):515–516. doi: 10.1038/emboj.2009.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Alexander A., Cai S.L., Kim J., Nanez A., Sahin M., MacLean K.H., Inoki K., Guan K.L., Shen J., Person M.D., Kusewitt D., Mills G.B., Kastan M.B., Walker C.L. ATM signals to TSC2 in the cytoplasm to regulate mTORC1 in response to ROS. Proc. Natl. Acad. Sci. USA. 2010;107(9):4153–4158. doi: 10.1073/pnas.0913860107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rosenbluth J.M., Pietenpol J.A. mTOR regulates autophagy-associated genes downstream of p73. Autophagy. 2009;5(1):114–116. doi: 10.4161/auto.5.1.7294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hibi K., Trink B., Patturajan M., Westra W.H., Caballero O.L., Hill D.E., Ratovitski E.A., Jen J., Sidransky D. AIS is an oncogene amplified in squamous cell carcinoma. Proc. Natl. Acad. Sci. USA. 2000;97(10):5462–5467. doi: 10.1073/pnas.97.10.5462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pandey S., Chandravati Autophagy in cervical cancer: an emerging therapeutic target. Asian Pac. J. Cancer Prev. 2012;13(10):4867–4871. doi: 10.7314/APJCP.2012.13.10.4867. [DOI] [PubMed] [Google Scholar]
- 93.Rikiishi H. Autophagic action of new targeting agents in head and neck oncology. Cancer Biol. Ther. 2012;13(11):978–991. doi: 10.4161/cbt.21079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Balunas M.J., Kinghorn A.D. Drug discovery from medicinal plants. Life Sci. 2005;78(5):431–441. doi: 10.1016/j.lfs.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 95.Kinghorn A.D., Carcache de Blanco E.J., Chai H.B., Orjala J., Farnsworth N.R., Soejarto D.D., Oberlies N.H., Wani M.C., Kroll D.J., Pearce C.J., Swanson S.M., Kramer R.A., Rose W.C., Fairchild C.R., Vite G.D., Emanuel S., Jarjoura D., Cope F.O. Discovery of anticancer agents of diverse natural origin. Pure Appl. Chem. 2009;81(6):1051–1063. doi: 10.1351/PAC-CON-08-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ortiz L.M., Lombardi P., Tillhon M., Scovassi A.I. Berberine, an epiphany against cancer. Molecules. 2014;19(8):12349–12367. doi: 10.3390/molecules190812349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Guamán Ortiz L.M., Croce A.L., Aredia F., Sapienza S., Fiorillo G., Syeda T.M., Buzzetti F., Lombardi P., Scovassi A.I. Effect of new berberine derivatives on colon cancer cells. Acta Biochim. Biophys. Sin. (Shanghai) 2015;47(10):824–833. doi: 10.1093/abbs/gmv077. [DOI] [PubMed] [Google Scholar]
- 98.Lee K.H., Lo H.L., Tang W.C., Hsiao H.H., Yang P.M. A gene expression signature-based approach reveals the mechanisms of action of the Chinese herbal medicine berberine. Sci. Rep. 2014;4:6394. doi: 10.1038/srep06394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Guamán-Ortiz L.M., Tillhon M., Parks M., Dutto I., Prosperi E., Savio M., Arcamone A.G., Buzzetti F., Lombardi P., Scovassi A.I. Multiple effects of berberine derivatives on colon cancer cells. 2014. [DOI] [PMC free article] [PubMed]
- 100.Yu R., Zhang Z.Q., Wang B., Jiang H.X., Cheng L., Shen L.M. Berberine-induced apoptotic and autophagic death of HepG2 cells requires AMPK activation. Cancer Cell Int. 2014;14:49. doi: 10.1186/1475-2867-14-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wang N., Feng Y., Zhu M., Tsang C.M., Man K., Tong Y., Tsao S.W. Berberine induces autophagic cell death and mitochondrial apoptosis in liver cancer cells: the cellular mechanism. J. Cell. Biochem. 2010;111(6):1426–1436. doi: 10.1002/jcb.22869. [DOI] [PubMed] [Google Scholar]
- 102.Tillhon M., Guamán Ortiz L.M., Lombardi P., Scovassi A.I. Berberine: new perspectives for old remedies. Biochem. Pharmacol. 2012;84(10):1260–1267. doi: 10.1016/j.bcp.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 103.Peng P.L., Kuo W.H., Tseng H.C., Chou F.P. Synergistic tumor-killing effect of radiation and berberine combined treatment in lung cancer: the contribution of autophagic cell death. Int. J. Radiat. Oncol. Biol. Phys. 2008;70(2):529–542. doi: 10.1016/j.ijrobp.2007.08.034. [DOI] [PubMed] [Google Scholar]
- 104.Aredia F., Guamán Ortiz L.M., Giansanti V., Scovassi A.I. Autophagy and cancer. Cells. 2012;1(3):520–534. doi: 10.3390/cells1030520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tyihák E., Király-Véghely Z., Móricz A.M. Multiple beneficial effects of resveratrol and their chemical-biochemical basis. Nat. Prod. Commun. 2011;6(5):631–638. [PubMed] [Google Scholar]
- 106.Szende B., Tyihák E., Király-Véghely Z. Dose-dependent effect of resveratrol on proliferation and apoptosis in endothelial and tumor cell cultures. Exp. Mol. Med. 2000;32(2):88–92. doi: 10.1038/emm.2000.16. [DOI] [PubMed] [Google Scholar]
- 107.Király-Véghely Z., Tyihák E., Albert L., Németh Z.I., Kátay G. Identification and measurement of resveratrol and formaldehyde in parts of white and blue grape berries. Acta Biol. Hung. 1998;49(2-4):281–289. [PubMed] [Google Scholar]
- 108.Aras A., Khokhar A.R., Qureshi M.Z., Silva M.F., Sobczak-Kupiec A., Pineda E.A., Hechenleitner A.A., Farooqi A.A. Targeting cancer with nano-bullets: curcumin, EGCG, resveratrol and quercetin on flying carpets. Asian Pac. J. Cancer Prev. 2014;15(9):3865–3871. doi: 10.7314/APJCP.2014.15.9.3865. [DOI] [PubMed] [Google Scholar]
- 109.Jang M., Cai L., Udeani G.O., Slowing K.V., Thomas C.F., Beecher C.W., Fong H.H., Farnsworth N.R., Kinghorn A.D., Mehta R.G., Moon R.C., Pezzuto J.M. Cancer chemopreventive activity of resveratrol, a natural product derived from grapes. Science. 1997;275(5297):218–220. doi: 10.1126/science.275.5297.218. [DOI] [PubMed] [Google Scholar]
- 110.Delmas D., Solary E., Latruffe N. Resveratrol, a phytochemical inducer of multiple cell death pathways: apoptosis, autophagy and mitotic catastrophe. Curr. Med. Chem. 2011;18(8):1100–1121. doi: 10.2174/092986711795029708. [DOI] [PubMed] [Google Scholar]
- 111.Hasima N., Ozpolat B. Regulation of autophagy by polyphenolic compounds as a potential therapeutic strategy for cancer. 2014. [DOI] [PMC free article] [PubMed]
- 112.Lao F., Shang Y., Liu D. Autophagy pathway of raji cell death induced by resveratrol. Chinese J. Biologicals. 2009;22:654–658. [Google Scholar]
- 113.Lao C.D., Demierre M.F., Sondak V.K. Targeting events in melanoma carcinogenesis for the prevention of melanoma. Expert Rev. Anticancer Ther. 2006;6(11):1559–1568. doi: 10.1586/14737140.6.11.1559. [DOI] [PubMed] [Google Scholar]
- 114.Opipari A.W., Jr, Tan L., Boitano A.E., Sorenson D.R., Aurora A., Liu J.R. Resveratrol-induced autophagocytosis in ovarian cancer cells. Cancer Res. 2004;64(2):696–703. doi: 10.1158/0008-5472.CAN-03-2404. [DOI] [PubMed] [Google Scholar]
- 115.Scarlatti F., Maffei R., Beau I., Ghidoni R., Codogno P. Non-canonical autophagy: an exception or an underestimated form of autophagy? Autophagy. 2008;4(8):1083–1085. doi: 10.4161/auto.7068. [DOI] [PubMed] [Google Scholar]
- 116.Scarlatti F., Maffei R., Beau I., Codogno P., Ghidoni R. Role of non-canonical Beclin 1-independent autophagy in cell death induced by resveratrol in human breast cancer cells. Cell Death Differ. 2008;15(8):1318–1329. doi: 10.1038/cdd.2008.51. [DOI] [PubMed] [Google Scholar]
- 117.Puissant A., Auberger P. AMPK- and p62/SQSTM1-dependent autophagy mediate resveratrol-induced cell death in chronic myelogenous leukemia. Autophagy. 2010;6(5):655–657. doi: 10.4161/auto.6.5.12126. [DOI] [PubMed] [Google Scholar]
- 118.Kumar B., Iqbal M.A., Singh R.K., Bamezai R.N. Resveratrol inhibits TIGAR to promote ROS induced apoptosis and autophagy. Biochimie. 2015;118:26–35. doi: 10.1016/j.biochi.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 119.Lang F., Qin Z., Li F., Zhang H., Fang Z., Hao E. Apoptotic Cell Death Induced by Resveratrol Is Partially Mediated by the Autophagy Pathway in Human Ovarian Cancer Cells. PLoS One. 2015;10(6):e0129196. doi: 10.1371/journal.pone.0129196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Selvaraj S., Sun Y., Sukumaran P., Singh B.B. Resveratrol activates autophagic cell death in prostate cancer cells via downregulation of STIM1 and the mTOR pathway. Mol. Carcinog. 2015 doi: 10.1002/mc.22324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhang J., Ma K., Qi T., Wei X., Zhang Q., Li G., Chiu J.F. P62 regulates resveratrol-mediated Fas/Cav-1 complex formation and transition from autophagy to apoptosis. Oncotarget. 2015;6(2):789–801. doi: 10.18632/oncotarget.2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Fu Y., Chang H., Peng X., Bai Q., Yi L., Zhou Y., Zhu J., Mi M. Resveratrol inhibits breast cancer stem-like cells and induces autophagy via suppressing Wnt/β-catenin signaling pathway. PLoS One. 2014;9(7):e102535. doi: 10.1371/journal.pone.0102535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ge J., Liu Y., Li Q., Guo X., Gu L., Ma Z.G., Zhu Y.P. Resveratrol induces apoptosis and autophagy in T-cell acute lymphoblastic leukemia cells by inhibiting Akt/mTOR and activating p38-MAPK. Biomed. Environ. Sci. 2013;26(11):902–911. doi: 10.3967/bes2013.019. [DOI] [PubMed] [Google Scholar]
- 124.Li G., Rivas P., Bedolla R., Thapa D., Reddick R.L., Ghosh R., Kumar A.P. Dietary resveratrol prevents development of high-grade prostatic intraepithelial neoplastic lesions: involvement of SIRT1/S6K axis. Cancer Prev. Res. (Phila.) 2013;6(1):27–39. doi: 10.1158/1940-6207.CAPR-12-0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhang L., Dai F., Sheng P.L., Chen Z.Q., Xu Q.P., Guo Y.Q. Resveratrol analogue 3,4,4-trihydroxy-trans-stilbene induces apoptosis and autophagy in human non-small-cell lung cancer cells in vitro. Acta Pharmacol. Sin. 2015;36(10):1256–1265. doi: 10.1038/aps.2015.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wang M., Yu T., Zhu C., Sun H., Qiu Y., Zhu X., Li J. Resveratrol triggers protective autophagy through the ceramide/Akt/mTOR pathway in melanoma B16 cells. Nutr. Cancer. 2014;66(3):435–440. doi: 10.1080/01635581.2013.878738. [DOI] [PubMed] [Google Scholar]
- 127.Siedlecka-Kroplewska K., Jozwik A., Boguslawski W., Wozniak M., Zauszkiewicz-Pawlak A., Spodnik J.H., Rychlowski M., Kmiec Z. Pterostilbene induces accumulation of autophagic vacuoles followed by cell death in HL60 human leukemia cells. J. Physiol. Pharmacol. 2013;64(5):545–556. [PubMed] [Google Scholar]
- 128.Mena S., Rodríguez M.L., Ponsoda X., Estrela J.M., Jäättela M., Ortega A.L. Pterostilbene-induced tumor cytotoxicity: a lysosomal membrane permeabilization-dependent mechanism. PLoS One. 2012;7(9):e44524. doi: 10.1371/journal.pone.0044524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Tedesco I., Russo M., Bilotto S., Spagnuolo C., Scognamiglio A., Palumbo R., Nappo A., Iacomino G., Moio L., Russo G.L. Dealcoholated red wine induces autophagic and apoptotic cell death in an osteosarcoma cell line. Food Chem. Toxicol. 2013;60:377–384. doi: 10.1016/j.fct.2013.07.078. [DOI] [PubMed] [Google Scholar]
- 130.García-Zepeda S.P., García-Villa E., Díaz-Chávez J., Hernández-Pando R., Gariglio P. Resveratrol induces cell death in cervical cancer cells through apoptosis and autophagy. Eur. J. Cancer Prev. 2013;22(6):577–584. doi: 10.1097/CEJ.0b013e328360345f. [DOI] [PubMed] [Google Scholar]
- 131.Miki H., Uehara N., Kimura A., Sasaki T., Yuri T., Yoshizawa K., Tsubura A. Resveratrol induces apoptosis via ROS-triggered autophagy in human colon cancer cells. Int. J. Oncol. 2012;40(4):1020–1028. doi: 10.3892/ijo.2012.1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Yamamoto M., Suzuki S.O., Himeno M. Resveratrol-induced autophagy in human U373 glioma cells. Oncol. Lett. 2010;1(3):489–493. doi: 10.3892/ol_00000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Siddiqui I.A., Malik A., Adhami V.M., Asim M., Hafeez B.B., Sarfaraz S., Mukhtar H. Green tea polyphenol EGCG sensitizes human prostate carcinoma LNCaP cells to TRAIL-mediated apoptosis and synergistically inhibits biomarkers associated with angiogenesis and metastasis. Oncogene. 2008;27(14):2055–2063. doi: 10.1038/sj.onc.1210840. [DOI] [PubMed] [Google Scholar]
- 134.Tang S.N., Singh C., Nall D., Meeker D., Shankar S., Srivastava R.K. The dietary bioflavonoid quercetin synergizes with epigallocathechin gallate (EGCG) to inhibit prostate cancer stem cell characteristics, invasion, migration and epithelial-mesenchymal transition. J. Mol. Signal. 2010;5:14. doi: 10.1186/1750-2187-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Shammas M.A., Neri P., Koley H., Batchu R.B., Bertheau R.C., Munshi V., Prabhala R., Fulciniti M., Tai Y.T., Treon S.P., Goyal R.K., Anderson K.C., Munshi N.C. Specific killing of multiple myeloma cells by (-)-epigallocatechin-3-gallate extracted from green tea: biologic activity and therapeutic implications. Blood. 2006;108(8):2804–2810. doi: 10.1182/blood-2006-05-022814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hu F., Wei F., Wang Y., Wu B., Fang Y., Xiong B. EGCG synergizes the therapeutic effect of cisplatin and oxaliplatin through autophagic pathway in human colorectal cancer cells. J. Pharmacol. Sci. 2015;128(1):27–34. doi: 10.1016/j.jphs.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 137.Irimie A.I., Braicu C., Zanoaga O., Pileczki V., Gherman C., Berindan-Neagoe I., Campian R.S. Epigallocatechin-3-gallate suppresses cell proliferation and promotes apoptosis and autophagy in oral cancer SSC-4 cells. Onco Targets Ther. 2015;8:461–470. doi: 10.2147/OTT.S78358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zhou J., Farah B.L., Sinha R.A., Wu Y., Singh B.K., Bay B.H., Yang C.S., Yen P.M. Epigallocatechin-3-gallate (EGCG), a green tea polyphenol, stimulates hepatic autophagy and lipid clearance. PLoS One. 2014;9(1):e87161. doi: 10.1371/journal.pone.0087161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chen L., Ye H.L., Zhang G., Yao W.M., Chen X.Z., Zhang F.C., Liang G. Autophagy inhibition contributes to the synergistic interaction between EGCG and doxorubicin to kill the hepatoma Hep3B cells. PLoS One. 2014;9(1):e85771. doi: 10.1371/journal.pone.0085771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Satoh M., Takemura Y., Hamada H., Sekido Y., Kubota S. EGCG induces human mesothelioma cell death by inducing reactive oxygen species and autophagy. Cancer Cell Int. 2013;13(1):19. doi: 10.1186/1475-2867-13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zhang Y., Yang N.D., Zhou F., Shen T., Duan T., Zhou J., Shi Y., Zhu X.Q., Shen H.M. (-)-Epigallocatechin-3-gallate induces non-apoptotic cell death in human cancer cells via ROS-mediated lysosomal membrane permeabilization. PLoS One. 2012;7(10):e46749. doi: 10.1371/journal.pone.0046749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Boyanapalli S.S., Tony Kong A.N. Curcumin, the King of Spices: Epigenetic Regulatory Mechanisms in the Prevention of Cancer, Neurological, and Inflammatory Diseases. Curr Pharmacol Rep. 2015;1(2):129–139. doi: 10.1007/s40495-015-0018-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Aoki H., Takada Y., Kondo S., Sawaya R., Aggarwal B.B., Kondo Y. Evidence that curcumin suppresses the growth of malignant gliomas in vitro and in vivo through induction of autophagy: role of Akt and extracellular signal-regulated kinase signaling pathways. Mol. Pharmacol. 2007;72(1):29–39. doi: 10.1124/mol.106.033167. [DOI] [PubMed] [Google Scholar]
- 144.Jia Y.L., Li J., Qin Z.H., Liang Z.Q. Autophagic and apoptotic mechanisms of curcumin-induced death in K562 cells. J. Asian Nat. Prod. Res. 2009;11(11):918–928. doi: 10.1080/10286020903264077. [DOI] [PubMed] [Google Scholar]
- 145.Zhou D.Y., Ding N., Du Z.Y., Cui X.X., Wang H., Wei X.C., Conney A.H., Zhang K., Zheng X. Curcumin analogues with high activity for inhibiting human prostate cancer cell growth and androgen receptor activation. Mol. Med. Rep. 2014;10(3):1315–1322. doi: 10.3892/mmr.2014.2380. [DOI] [PubMed] [Google Scholar]
- 146.Akkoç Y., Berrak Ö., Arısan E.D., Obakan P., Çoker-Gürkan A., Palavan-Ünsal N. Inhibition of PI3K signaling triggered apoptotic potential of curcumin which is hindered by Bcl-2 through activation of autophagy in MCF-7 cells. Biomed. Pharmacother. 2015;71:161–171. doi: 10.1016/j.biopha.2015.02.029. [DOI] [PubMed] [Google Scholar]
- 147.Xiao K., Jiang J., Guan C., Dong C., Wang G., Bai L., Sun J., Hu C., Bai C. Curcumin induces autophagy via activating the AMPK signaling pathway in lung adenocarcinoma cells. J. Pharmacol. Sci. 2013;123(2):102–109. doi: 10.1254/jphs.13085FP. [DOI] [PubMed] [Google Scholar]
- 148.Lee Y.J., Kim N.Y., Suh Y.A., Lee C. Involvement of ROS in curcumin-induced autophagic cell death. Korean J. Physiol. Pharmacol. 2011;15(1):1–7. doi: 10.4196/kjpp.2011.15.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Shinojima N., Yokoyama T., Kondo Y., Kondo S. Roles of the Akt/mTOR/p70S6K and ERK1/2 signaling pathways in curcumin-induced autophagy. Autophagy. 2007;3(6):635–637. doi: 10.4161/auto.4916. [DOI] [PubMed] [Google Scholar]
- 150.Qian H., Yang Y., Wang X. Curcumin enhanced adriamycin-induced human liver-derived Hepatoma G2 cell death through activation of mitochondria-mediated apoptosis and autophagy. Eur. J. Pharm. Sci. 2011;43(3):125–131. doi: 10.1016/j.ejps.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 151.Thongrakard V., Titone R., Follo C., Morani F., Suksamrarn A., Tencomnao T., Isidoro C. Turmeric toxicity in A431 epidermoid cancer cells associates with autophagy degradation of anti-apoptotic and anti-autophagic p53 mutant. Phytother. Res. 2014;28(12):1761–1769. doi: 10.1002/ptr.5196. [DOI] [PubMed] [Google Scholar]
- 152.Li B., Takeda T., Tsuiji K., Wong T.F., Tadakawa M., Kondo A., Nagase S., Yaegashi N. Curcumin induces cross-regulation between autophagy and apoptosis in uterine leiomyosarcoma cells. Int. J. Gynecol. Cancer. 2013;23(5):803–808. doi: 10.1097/IGC.0b013e31828c9581. [DOI] [PubMed] [Google Scholar]
- 153.Kim J.Y., Cho T.J., Woo B.H., Choi K.U., Lee C.H., Ryu M.H., Park H.R. Curcumin-induced autophagy contributes to the decreased survival of oral cancer cells. Arch. Oral Biol. 2012;57(8):1018–1025. doi: 10.1016/j.archoralbio.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 154.Yamauchi Y., Izumi Y., Asakura K., Hayashi Y., Nomori H. Curcumin induces autophagy in ACC-MESO-1 cells. Phytother. Res. 2012;26(12):1779–1783. doi: 10.1002/ptr.4645. [DOI] [PubMed] [Google Scholar]
- 155.Zhuang W., Long L., Zheng B., Ji W., Yang N., Zhang Q., Liang Z. Curcumin promotes differentiation of glioma-initiating cells by inducing autophagy. Cancer Sci. 2012;103(4):684–690. doi: 10.1111/j.1349-7006.2011.02198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wu J.C., Lai C.S., Badmaev V., Nagabhushanam K., Ho C.T., Pan M.H. Tetrahydrocurcumin, a major metabolite of curcumin, induced autophagic cell death through coordinative modulation of PI3K/Akt-mTOR and MAPK signaling pathways in human leukemia HL-60 cells. Mol. Nutr. Food Res. 2011;55(11):1646–1654. doi: 10.1002/mnfr.201100454. [DOI] [PubMed] [Google Scholar]
- 157.Wang N., Pan W., Zhu M., Zhang M., Hao X., Liang G., Feng Y. Fangchinoline induces autophagic cell death via p53/sestrin2/AMPK signalling in human hepatocellular carcinoma cells. Br. J. Pharmacol. 2011;164(2b):731–742. doi: 10.1111/j.1476-5381.2011.01349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Wong A.S., Che C.M., Leung K.W. Recent advances in ginseng as cancer therapeutics: a functional and mechanistic overview. Nat. Prod. Rep. 2015;32(2):256–272. doi: 10.1039/C4NP00080C. [DOI] [PubMed] [Google Scholar]
- 159.Choi J.S., Chun K.S., Kundu J., Kundu J.K. Biochemical basis of cancer chemoprevention and/or chemotherapy with ginsenosides (Review). Int. J. Mol. Med. 2013;32(6):1227–1238. doi: 10.3892/ijmm.2013.1519. [DOI] [PubMed] [Google Scholar]
- 160.Nag S.A., Qin J.J., Wang W., Wang M.H., Wang H., Zhang R. Ginsenosides as Anticancer Agents: In vitro and in vivo Activities, Structure-Activity Relationships, and Molecular Mechanisms of Action. Front. Pharmacol. 2012;3:25. doi: 10.3389/fphar.2012.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Chang Y.S., Seo E.K., Gyllenhaal C., Block K.I. Panax ginseng: a role in cancer therapy? Integr. Cancer Ther. 2003;2(1):13–33. doi: 10.1177/1534735403251167. [DOI] [PubMed] [Google Scholar]
- 162.Yun T.K., Lee Y.S., Lee Y.H., Kim S.I., Yun H.Y. Anticarcinogenic effect of Panax ginseng C.A. Meyer and identification of active compounds. J. Korean Med. Sci. 2001;16(Suppl.):S6–S18. doi: 10.3346/jkms.2001.16.S.S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kim S.M., Lee S.Y., Cho J.S., Son S.M., Choi S.S., Yun Y.P., Yoo H.S., Yoon D.Y., Oh K.W., Han S.B., Hong J.T. Combination of ginsenoside Rg3 with docetaxel enhances the susceptibility of prostate cancer cells via inhibition of NF-kappaB. Eur. J. Pharmacol. 2010;631(1-3):1–9. doi: 10.1016/j.ejphar.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 164.Kim D.G., Jung K.H., Lee D.G., Yoon J.H., Choi K.S., Kwon S.W., Shen H.M., Morgan M.J., Hong S.S., Kim Y.S. 20(S)-Ginsenoside Rg3 is a novel inhibitor of autophagy and sensitizes hepatocellular carcinoma to doxorubicin. Oncotarget. 2014;5(12):4438–4451. doi: 10.18632/oncotarget.2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ko H., Kim Y.J., Park J.S., Park J.H., Yang H.O. Autophagy inhibition enhances apoptosis induced by ginsenoside Rk1 in hepatocellular carcinoma cells. Biosci. Biotechnol. Biochem. 2009;73(10):2183–2189. doi: 10.1271/bbb.90250. [DOI] [PubMed] [Google Scholar]
- 166.Kim A.D., Kang K.A., Kim H.S., Kim D.H., Choi Y.H., Lee S.J., Kim H.S., Hyun J.W. A ginseng metabolite, compound K, induces autophagy and apoptosis via generation of reactive oxygen species and activation of JNK in human colon cancer cells. Cell Death Dis. 2013;4:e750. doi: 10.1038/cddis.2013.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Mai T.T., Moon J., Song Y., Viet P.Q., Phuc P.V., Lee J.M., Yi T.H., Cho M., Cho S.K. Ginsenoside F2 induces apoptosis accompanied by protective autophagy in breast cancer stem cells. Cancer Lett. 2012;321(2):144–153. doi: 10.1016/j.canlet.2012.01.045. [DOI] [PubMed] [Google Scholar]
- 168.Huang M., Lu J.J., Huang M.Q., Bao J.L., Chen X.P., Wang Y.T. Terpenoids: natural products for cancer therapy. Expert Opin. Investig. Drugs. 2012;21(12):1801–1818. doi: 10.1517/13543784.2012.727395. [DOI] [PubMed] [Google Scholar]
- 169.Ghantous A., Gali-Muhtasib H., Vuorela H., Saliba N.A., Darwiche N. What made sesquiterpene lactones reach cancer clinical trials? Drug Discov. Today. 2010;15(15-16):668–678. doi: 10.1016/j.drudis.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 170.Yang H., Dou Q.P. Targeting apoptosis pathway with natural terpenoids: implications for treatment of breast and prostate cancer. Curr. Drug Targets. 2010;11(6):733–744. doi: 10.2174/138945010791170842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Merfort I. Perspectives on sesquiterpene lactones in inflammation and cancer. Curr. Drug Targets. 2011;12(11):1560–1573. doi: 10.2174/138945011798109437. [DOI] [PubMed] [Google Scholar]
- 172.Kreuger M.R., Grootjans S., Biavatti M.W., Vandenabeele P., DHerde K. Sesquiterpene lactones as drugs with multiple targets in cancer treatment: focus on parthenolide. Anticancer Drugs. 2012;23(9):883–896. doi: 10.1097/CAD.0b013e328356cad9. [DOI] [PubMed] [Google Scholar]
- 173.Ghantous A., Sinjab A., Herceg Z., Darwiche N. Parthenolide: from plant shoots to cancer roots. Drug Discov. Today. 2013;18(17-18):894–905. doi: 10.1016/j.drudis.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 174.Schneider-Stock R., Ghantous A., Bajbouj K., Saikali M., Darwiche N. Epigenetic mechanisms of plant-derived anticancer drugs. Front. Biosci. (Landmark Ed.) 2012;17:129–173. doi: 10.2741/3919. [DOI] [PubMed] [Google Scholar]
- 175.DAnneo A., Carlisi D., Lauricella M., Puleio R., Martinez R., Di Bella S., Di Marco P., Emanuele S., Di Fiore R., Guercio A., Vento R., Tesoriere G. Parthenolide generates reactive oxygen species and autophagy in MDA-MB231 cells. A soluble parthenolide analogue inhibits tumour growth and metastasis in a xenograft model of breast cancer. Cell Death Dis. 2013;4:e891. doi: 10.1038/cddis.2013.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sun J., Zhang C., Bao Y.L., Wu Y., Chen Z.L., Yu C.L., Huang Y.X., Sun Y., Zheng L.H., Wang X., Li Y.X. Parthenolide-induced apoptosis, autophagy and suppression of proliferation in HepG2 cells. Asian Pac. J. Cancer Prev. 2014;15(12):4897–4902. doi: 10.7314/APJCP.2014.15.12.4897. [DOI] [PubMed] [Google Scholar]
- 177.Lan B., Wan Y.J., Pan S., Wang Y., Yang Y., Leng Q.L., Jia H., Liu Y.H., Zhang C.Z., Cao Y. Parthenolide induces autophagy via the depletion of 4E-BP1. Biochem. Biophys. Res. Commun. 2015;456(1):434–439. doi: 10.1016/j.bbrc.2014.11.102. [DOI] [PubMed] [Google Scholar]
- 178.Li X.J., Jiang Z.Z., Zhang L.Y. Triptolide: progress on research in pharmacodynamics and toxicology. J. Ethnopharmacol. 2014;155(1):67–79. doi: 10.1016/j.jep.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 179.Chen L., Liu Q., Huang Z., Wu F., Li Z., Chen X., Lin T. Tripchlorolide induces cell death in lung cancer cells by autophagy. Int. J. Oncol. 2012;40(4):1066–1070. doi: 10.3892/ijo.2011.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Yang S., Chen J., Guo Z., Xu X.M., Wang L., Pei X.F., Yang J., Underhill C.B., Zhang L. Triptolide inhibits the growth and metastasis of solid tumors. Mol. Cancer Ther. 2003;2(1):65–72. [PubMed] [Google Scholar]
- 181.Mujumdar N., Mackenzie T.N., Dudeja V., Chugh R., Antonoff M.B., Borja-Cacho D., Sangwan V., Dawra R., Vickers S.M., Saluja A.K. Triptolide induces cell death in pancreatic cancer cells by apoptotic and autophagic pathways. Gastroenterology. 2010;139(2):598–608. doi: 10.1053/j.gastro.2010.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Mujumdar N., Banerjee S., Chen Z., Sangwan V., Chugh R., Dudeja V., Yamamoto M., Vickers S.M., Saluja A.K. Triptolide activates unfolded protein response leading to chronic ER stress in pancreatic cancer cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2014;306(11):G1011–G1020. doi: 10.1152/ajpgi.00466.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Krosch T.C., Sangwan V., Banerjee S., Mujumdar N., Dudeja V., Saluja A.K., Vickers S.M. Triptolide-mediated cell death in neuroblastoma occurs by both apoptosis and autophagy pathways and results in inhibition of nuclear factor-kappa B activity. Am. J. Surg. 2013;205(4):387–396. doi: 10.1016/j.amjsurg.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Fulda S. Betulinic Acid for cancer treatment and prevention. Int. J. Mol. Sci. 2008;9(6):1096–1107. doi: 10.3390/ijms9061096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Gheorgheosu D., Duicu O., Dehelean C., Soica C., Muntean D. Betulinic acid as a potent and complex antitumor phytochemical: a minireview. Anticancer. Agents Med. Chem. 2014;14(7):936–945. doi: 10.2174/1871520614666140223192148. [DOI] [PubMed] [Google Scholar]
- 186.Gonzalez P., Mader I., Tchoghandjian A., Enzenmüller S., Cristofanon S., Basit F., Debatin K.M., Fulda S. Impairment of lysosomal integrity by B10, a glycosylated derivative of betulinic acid, leads to lysosomal cell death and converts autophagy into a detrimental process. Cell Death Differ. 2012;19(8):1337–1346. doi: 10.1038/cdd.2012.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Yang L.J., Chen Y., He J., Yi S., Wen L., Zhao J., Zhang B.P., Cui G.H. Betulinic acid inhibits autophagic flux and induces apoptosis in human multiple myeloma cells in vitro. Acta Pharmacol. Sin. 2012;33(12):1542–1548. doi: 10.1038/aps.2012.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Potze L., Mullauer F.B., Colak S., Kessler J.H., Medema J.P. Betulinic acid-induced mitochondria-dependent cell death is counterbalanced by an autophagic salvage response. Cell Death Dis. 2014;5:e1169. doi: 10.1038/cddis.2014.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Cui Q., Tashiro S., Onodera S., Ikejima T. Augmentation of oridonin-induced apoptosis observed with reduced autophagy. J. Pharmacol. Sci. 2006;101(3):230–239. doi: 10.1254/jphs.FPJ06003X. [DOI] [PubMed] [Google Scholar]
- 190.Ye Y.C., Wang H.J., Xu L., Liu W.W., Liu B.B., Tashiro S., Onodera S., Ikejima T. Oridonin induces apoptosis and autophagy in murine fibrosarcoma L929 cells partly via NO-ERK-p53 positive-feedback loop signaling pathway. Acta Pharmacol. Sin. 2012;33(8):1055–1061. doi: 10.1038/aps.2012.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Cheng Y., Qiu F., Ikejima T. Molecular mechanisms of oridonin-induced apoptosis and autophagy in murine fibrosarcoma L929 cells. Autophagy. 2009;5(3):430–431. doi: 10.4161/auto.5.3.7896. [DOI] [PubMed] [Google Scholar]
- 192.Cheng Y., Qiu F., Ye Y.C., Guo Z.M., Tashiro S., Onodera S., Ikejima T. Autophagy inhibits reactive oxygen species-mediated apoptosis via activating p38-nuclear factor-kappa B survival pathways in oridonin-treated murine fibrosarcoma L929 cells. FEBS J. 2009;276(5):1291–1306. doi: 10.1111/j.1742-4658.2008.06864.x. [DOI] [PubMed] [Google Scholar]
- 193.Cheng Y., Qiu F., Huang J., Tashiro S., Onodera S., Ikejima T. Apoptosis-suppressing and autophagy-promoting effects of calpain on oridonin-induced L929 cell death. Arch. Biochem. Biophys. 2008;475(2):148–155. doi: 10.1016/j.abb.2008.04.027. [DOI] [PubMed] [Google Scholar]
- 194.Banjerdpongchai R., Khaw-On P. Terpinen-4-ol induces autophagic and apoptotic cell death in human leukemic HL-60 cells. Asian Pac. J. Cancer Prev. 2013;14(12):7537–7542. doi: 10.7314/APJCP.2013.14.12.7537. [DOI] [PubMed] [Google Scholar]
- 195.Yang H., Chen D., Cui Q.C., Yuan X., Dou Q.P. Celastrol, a triterpene extracted from the Chinese Thunder of God Vine, is a potent proteasome inhibitor and suppresses human prostate cancer growth in nude mice. Cancer Res. 2006;66(9):4758–4765. doi: 10.1158/0008-5472.CAN-05-4529. [DOI] [PubMed] [Google Scholar]
- 196.Guo J., Huang X., Wang H., Yang H. Celastrol Induces Autophagy by Targeting AR/miR-101 in Prostate Cancer Cells. PLoS One. 2015;10(10):e0140745. doi: 10.1371/journal.pone.0140745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Li H.Y., Zhang J., Sun L.L., Li B.H., Gao H.L., Xie T., Zhang N., Ye Z.M. 2015.
- 198.Han X., Sun S., Zhao M., Cheng X., Chen G., Lin S., Guan Y., Yu X. Celastrol stimulates hypoxia-inducible factor-1 activity in tumor cells by initiating the ROS/Akt/p70S6K signaling pathway and enhancing hypoxia-inducible factor-1α protein synthesis. PLoS One. 2014;9(11):e112470. doi: 10.1371/journal.pone.0112470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Ma J., Han L.Z., Liang H., Mi C., Shi H., Lee J.J., Jin X. Celastrol inhibits the HIF-1α pathway by inhibition of mTOR/p70S6K/eIF4E and ERK1/2 phosphorylation in human hepatoma cells. Oncol. Rep. 2014;32(1):235–242. doi: 10.3892/or.2014.3211. [DOI] [PubMed] [Google Scholar]
- 200.Boridy S., Le P.U., Petrecca K., Maysinger D. Celastrol targets proteostasis and acts synergistically with a heat-shock protein 90 inhibitor to kill human glioblastoma cells. Cell Death Dis. 2014;5:e1216. doi: 10.1038/cddis.2014.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Lee H.W., Jang K.S., Choi H.J., Jo A., Cheong J.H., Chun K.H. Celastrol inhibits gastric cancer growth by induction of apoptosis and autophagy. BMB Rep. 2014;47(12):697–702. doi: 10.5483/BMBRep.2014.47.12.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Wang W.B., Feng L.X., Yue Q.X., Wu W.Y., Guan S.H., Jiang B.H., Yang M., Liu X., Guo D.A. Paraptosis accompanied by autophagy and apoptosis was induced by celastrol, a natural compound with influence on proteasome, ER stress and Hsp90. J. Cell. Physiol. 2012;227(5):2196–2206. doi: 10.1002/jcp.22956. [DOI] [PubMed] [Google Scholar]
- 203.Fahey J.W., Talalay P. Antioxidant functions of sulforaphane: a potent inducer of Phase II detoxication enzymes. Food Chem. Toxicol. 1999;37(9-10):973–979. doi: 10.1016/S0278-6915(99)00082-4. [DOI] [PubMed] [Google Scholar]
- 204.Herman-Antosiewicz A., Johnson D.E., Singh S.V. Sulforaphane causes autophagy to inhibit release of cytochrome C and apoptosis in human prostate cancer cells. Cancer Res. 2006;66(11):5828–5835. doi: 10.1158/0008-5472.CAN-06-0139. [DOI] [PubMed] [Google Scholar]
- 205.Jackson S.J., Singletary K.W. Sulforaphane inhibits human MCF-7 mammary cancer cell mitotic progression and tubulin polymerization. J. Nutr. 2004;134(9):2229–2236. doi: 10.1093/jn/134.9.2229. [DOI] [PubMed] [Google Scholar]
- 206.Azarenko O., Okouneva T., Singletary K.W., Jordan M.A., Wilson L. Suppression of microtubule dynamic instability and turnover in MCF7 breast cancer cells by sulforaphane. Carcinogenesis. 2008;29(12):2360–2368. doi: 10.1093/carcin/bgn241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Mi L., Xiao Z., Hood B.L., Dakshanamurthy S., Wang X., Govind S., Conrads T.P., Veenstra T.D., Chung F.L. Covalent binding to tubulin by isothiocyanates. A mechanism of cell growth arrest and apoptosis. J. Biol. Chem. 2008;283(32):22136–22146. doi: 10.1074/jbc.M802330200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Parnaud G., Li P., Cassar G., Rouimi P., Tulliez J., Combaret L., Gamet-Payrastre L. Mechanism of sulforaphane-induced cell cycle arrest and apoptosis in human colon cancer cells. Nutr. Cancer. 2004;48(2):198–206. doi: 10.1207/s15327914nc4802_10. [DOI] [PubMed] [Google Scholar]
- 209.Pawlik A., Wiczk A., Kaczyńska A., Antosiewicz J., Herman-Antosiewicz A. Sulforaphane inhibits growth of phenotypically different breast cancer cells. Eur. J. Nutr. 2013;52(8):1949–1958. doi: 10.1007/s00394-013-0499-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Arthur C.R., Gupton J.T., Kellogg G.E., Yeudall W.A., Cabot M.C., Newsham I.F., Gewirtz D.A. Autophagic cell death, polyploidy and senescence induced in breast tumor cells by the substituted pyrrole JG-0314, a novel microtubule poison. Biochem. Pharmacol. 2007;74(7):981–991. doi: 10.1016/j.bcp.2007.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Biggers J.W., Nguyen T., Di X., Gupton J.T., Henderson S.C., Emery S.M., Alotaibi M., White K.L., Jr, Brown R., Almenara J., Gewirtz D.A. Autophagy, cell death and sustained senescence arrest in B16/F10 melanoma cells and HCT-116 colon carcinoma cells in response to the novel microtubule poison, JG-0314. Cancer Chemother. Pharmacol. 2013;71(2):441–455. doi: 10.1007/s00280-012-2024-6. [DOI] [PubMed] [Google Scholar]
- 212.Larocque K., Ovadje P., Djurdjevic S., Mehdi M., Green J., Pandey S. Novel analogue of colchicine induces selective pro-death autophagy and necrosis in human cancer cells. PLoS One. 2014;9(1):e87064. doi: 10.1371/journal.pone.0087064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Amagase H. Clarifying the real bioactive constituents of garlic. J. Nutr. 2006;136(3) Suppl.:716S–725S. doi: 10.1093/jn/136.3.716S. [DOI] [PubMed] [Google Scholar]
- 214.Altonsy M.O., Andrews S.C. Diallyl disulphide, a beneficial component of garlic oil, causes a redistribution of cell-cycle growth phases, induces apoptosis, and enhances butyrate-induced apoptosis in colorectal adenocarcinoma cells (HT-29). Nutr. Cancer. 2011;63(7):1104–1113. doi: 10.1080/01635581.2011.601846. [DOI] [PubMed] [Google Scholar]
- 215.Chu Y.L., Ho C.T., Chung J.G., Rajasekaran R., Sheen L.Y. Allicin induces p53-mediated autophagy in Hep G2 human liver cancer cells. J. Agric. Food Chem. 2012;60(34):8363–8371. doi: 10.1021/jf301298y. [DOI] [PubMed] [Google Scholar]
- 216.Chu Y.L., Ho C.T., Chung J.G., Raghu R., Lo Y.C., Sheen L.Y. Allicin induces anti-human liver cancer cells through the p53 gene modulating apoptosis and autophagy. J. Agric. Food Chem. 2013;61(41):9839–9848. doi: 10.1021/jf403241s. [DOI] [PubMed] [Google Scholar]
- 217.Wang Y., Liu Y., Liu X., Jiang L., Yang G., Sun X., Geng C., Li Q., Yao X., Chen M. Citreoviridin Induces Autophagy-Dependent Apoptosis through Lysosomal-Mitochondrial Axis in Human Liver HepG2 Cells. Toxins (Basel) 2015;7(8):3030–3044. doi: 10.3390/toxins7083030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Liu Y.N., Wang Y.X., Liu X.F., Jiang L.P., Yang G., Sun X.C., Geng C.Y., Li Q.J., Chen M., Yao X.F. Citreoviridin induces ROS-dependent autophagic cell death in human liver HepG2 cells. Toxicon. 2015;95:30–37. doi: 10.1016/j.toxicon.2014.12.014. [DOI] [PubMed] [Google Scholar]
- 219.Wu P.F., Chiu C.C., Chen C.Y., Wang H.M. 7-Hydroxydehydronuciferine induces human melanoma death via triggering autophagy and apoptosis. Exp. Dermatol. 2015;24(12):930–935. doi: 10.1111/exd.12805. [DOI] [PubMed] [Google Scholar]
- 220.Dyshlovoy S.A., Hauschild J., Amann K., Tabakmakher K.M., Venz S., Walther R., Guzii A.G., Makarieva T.N., Shubina L.K., Fedorov S.N., Stonik V.A., Bokemeyer C., Balabanov S., Honecker F., von Amsberg G. Marine alkaloid Monanchocidin a overcomes drug resistance by induction of autophagy and lysosomal membrane permeabilization. Oncotarget. 2015;6(19):17328–17341. doi: 10.18632/oncotarget.4175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Hu T., Wang L., Zhang L., Lu L., Shen J., Chan R.L., Li M., Wu W.K., To K.K., Cho C.H. Sensitivity of apoptosis-resistant colon cancer cells to tanshinones is mediated by autophagic cell death and p53-independent cytotoxicity. Phytomedicine. 2015;22(5):536–544. doi: 10.1016/j.phymed.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 222.Kim Y.J., Kang K.S., Choi K.C., Ko H. Cardamonin induces autophagy and an antiproliferative effect through JNK activation in human colorectal carcinoma HCT116 cells. Bioorg. Med. Chem. Lett. 2015;25(12):2559–2564. doi: 10.1016/j.bmcl.2015.04.054. [DOI] [PubMed] [Google Scholar]
- 223.Lyu Q., Tou F., Su H., Wu X., Chen X., Zheng Z. The natural product peiminine represses colorectal carcinoma tumor growth by inducing autophagic cell death. Biochem. Biophys. Res. Commun. 2015;462(1):38–45. doi: 10.1016/j.bbrc.2015.04.102. [DOI] [PubMed] [Google Scholar]
- 224.Armstrong J.L., Hill D.S., McKee C.S., Hernandez-Tiedra S., Lorente M., Lopez-Valero I., Eleni Anagnostou M., Babatunde F., Corazzari M., Redfern C.P., Velasco G., Lovat P.E. Exploiting cannabinoid-induced cytotoxic autophagy to drive melanoma cell death. J. Invest. Dermatol. 2015;135(6):1629–1637. doi: 10.1038/jid.2015.45. [DOI] [PubMed] [Google Scholar]
- 225.Ramirez-Orellana M.I., Velazquez G., Lorente M., Ratovitski E.A. Cytotoxic evaluation of the action of naturally derived compounds on glioma cells.; Abstracts of the Keystone Symposia of Molecular and Cell Biology; October 28-November 2, 2014; San Paulo, Brazil. p. 86. [Google Scholar]
- 226.Tang Z.H., Li T., Chang L.L., Zhu H., Tong Y.G., Chen X.P., Wang Y.T., Lu J.J. Glycyrrhetinic Acid triggers a protective autophagy by activation of extracellular regulated protein kinases in hepatocellular carcinoma cells. J. Agric. Food Chem. 2014;62(49):11910–11916. doi: 10.1021/jf503968k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Shi L., Zhang T., Zhou Y., Zeng X., Ran L., Zhang Q., Zhu J., Mi M. Dihydromyricetin improves skeletal muscle insulin sensitivity by inducing autophagy via the AMPK-PGC-1α-Sirt3 signaling pathway. Endocrine. 2015;50(2):378–389. doi: 10.1007/s12020-015-0599-5. [DOI] [PubMed] [Google Scholar]
- 228.Chiu C.T., Hsuan S.W., Lin H.H., Hsu C.C., Chou F.P., Chen J.H. Hibiscus sabdariffa leaf polyphenolic extract induces human melanoma cell death, apoptosis, and autophagy. J. Food Sci. 2015;80(3):H649–H658. doi: 10.1111/1750-3841.12790. [DOI] [PubMed] [Google Scholar]
- 229.Su C.C. Sann-Joong-Kuey-Jian-Tang decreases the protein expression of mammalian target of rapamycin but increases microtubule associated protein II light chain 3 expression to inhibit human BxPC‑3 pancreatic carcinoma cells. Mol. Med. Rep. 2015;11(4):3160–3166. doi: 10.3892/mmr.2014.3090. [DOI] [PubMed] [Google Scholar]
- 230.Trzoss L., Fukuda T., Costa-Lotufo L.V., Jimenez P., La Clair J.J., Fenical W. Seriniquinone, a selective anticancer agent, induces cell death by autophagocytosis, targeting the cancer-protective protein dermcidin. Proc. Natl. Acad. Sci. USA. 2014;111(41):14687–14692. doi: 10.1073/pnas.1410932111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Juncker T., Schumacher M., Dicato M., Diederich M. UNBS1450 from Calotropis procera as a regulator of signaling pathways involved in proliferation and cell death. Biochem. Pharmacol. 2009;78(1):1–10. doi: 10.1016/j.bcp.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 232.Xu D., Lao Y., Xu N., Hu H., Fu W., Tan H., Gu Y., Song Z., Cao P., Xu H. Identification and characterization of anticancer compounds targeting apoptosis and autophagy from Chinese native Garcinia species. Planta Med. 2015;81(1):79–89. doi: 10.1055/s-0034-1383356. [DOI] [PubMed] [Google Scholar]
- 233.Feng C., Zhou L.Y., Yu T., Xu G., Tian H.L., Xu J.J., Xu H.X., Luo K.Q. A new anticancer compound, oblongifolin C, inhibits tumor growth and promotes apoptosis in HeLa cells through Bax activation. Int. J. Cancer. 2012;131(6):1445–1454. doi: 10.1002/ijc.27365. [DOI] [PubMed] [Google Scholar]
- 234.Lao Y., Wan G., Liu Z., Wang X., Ruan P., Xu W., Xu D., Xie W., Zhang Y., Xu H., Xu N. The natural compound oblongifolin C inhibits autophagic flux and enhances antitumor efficacy of nutrient deprivation. Autophagy. 2014;10(5):736–749. doi: 10.4161/auto.28034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Wang X., Lao Y., Xu N., Xi Z., Wu M., Wang H., Li X., Tan H., Sun M., Xu H. Oblongifolin C inhibits metastasis by up-regulating keratin 18 and tubulins. Sci. Rep. 2015;5:10293. doi: 10.1038/srep10293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Ouyang L., Chen Y., Wang X.Y., Lu R.F., Zhang S.Y., Tian M., Xie T., Liu B., He G. Polygonatum odoratum lectin induces apoptosis and autophagy via targeting EGFR-mediated Ras-Raf-MEK-ERK pathway in human MCF-7 breast cancer cells. Phytomedicine. 2014;21(12):1658–1665. doi: 10.1016/j.phymed.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 237.Li C., Chen J., Lu B., Shi Z., Wang H., Zhang B., Zhao K., Qi W., Bao J., Wang Y. Molecular switch role of Akt in Polygonatum odoratum lectin-induced apoptosis and autophagy in human non-small cell lung cancer A549 cells. PLoS One. 2014;9(7):e101526. doi: 10.1371/journal.pone.0101526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Wang S.Y., Yu Q.J., Bao J.K., Liu B. Polygonatum cyrtonema lectin, a potential antineoplastic drug targeting programmed cell death pathways. Biochem. Biophys. Res. Commun. 2011;406(4):497–500. doi: 10.1016/j.bbrc.2011.02.049. [DOI] [PubMed] [Google Scholar]
- 239.Liu B., Cheng Y., Bian H.J., Bao J.K. Molecular mechanisms of Polygonatum cyrtonema lectin-induced apoptosis and autophagy in cancer cells. Autophagy. 2009;5(2):253–255. doi: 10.4161/auto.5.2.7561. [DOI] [PubMed] [Google Scholar]
- 240.Liu B., Cheng Y., Zhang B., Bian H.J., Bao J.K. Polygonatum cyrtonema lectin induces apoptosis and autophagy in human melanoma A375 cells through a mitochondria-mediated ROS-p38-p53 pathway. Cancer Lett. 2009;275(1):54–60. doi: 10.1016/j.canlet.2008.09.042. [DOI] [PubMed] [Google Scholar]
- 241.Carvalho F.C., Soares S.G., Tamarozzi M.B., Rego E.M., Roque-Barreira M.C. The recognition of N-glycans by the lectin ArtinM mediates cell death of a human myeloid leukemia cell line. PLoS One. 2011;6(11):e27892. doi: 10.1371/journal.pone.0027892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Zhang C.Z., Fang E.F., Zhang H.T., Liu L.L., Yun J.P. Momordica charantia lectin exhibits antitumor activity towards hepatocellular carcinoma. Invest. New Drugs. 2015;33(1):1–11. doi: 10.1007/s10637-014-0156-8. [DOI] [PubMed] [Google Scholar]
- 243.Pratt J., Annabi B. Induction of autophagy biomarker BNIP3 requires a JAK2/STAT3 and MT1-MMP signaling interplay in Concanavalin-A-activated U87 glioblastoma cells. Cell. Signal. 2014;26(5):917–924. doi: 10.1016/j.cellsig.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 244.Chen M.C., Lee N.H., Hsu H.H., Ho T.J., Tu C.C., Hsieh D.J., Lin Y.M., Chen L.M., Kuo W.W., Huang C.Y. Thymoquinone induces caspase-independent, autophagic cell death in CPT-11-resistant lovo colon cancer via mitochondrial dysfunction and activation of JNK and p38. J. Agric. Food Chem. 2015;63(5):1540–1546. doi: 10.1021/jf5054063. [DOI] [PubMed] [Google Scholar]
- 245.Hahm E.R., Sakao K., Singh S.V. Honokiol activates reactive oxygen species-mediated cytoprotective autophagy in human prostate cancer cells. Prostate. 2014;74(12):1209–1221. doi: 10.1002/pros.22837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Zhang L., Wang H., Zhu J., Xu J., Ding K. Mollugin induces tumor cell apoptosis and autophagy via the PI3K/AKT/mTOR/p70S6K and ERK signaling pathways. Biochem. Biophys. Res. Commun. 2014;450(1):247–254. doi: 10.1016/j.bbrc.2014.05.101. [DOI] [PubMed] [Google Scholar]
- 247.Lu J., Sun D., Gao S., Gao Y., Ye J., Liu P. Cyclovirobuxine D induces autophagy-associated cell death via the Akt/mTOR pathway in MCF-7 human breast cancer cells. J. Pharmacol. Sci. 2014;125(1):74–82. doi: 10.1254/jphs.14013FP. [DOI] [PubMed] [Google Scholar]
- 248.Xu M.Y., Lee S.Y., Kang S.S., Kim Y.S. Antitumor activity of jujuboside B and the underlying mechanism via induction of apoptosis and autophagy. J. Nat. Prod. 2014;77(2):370–376. doi: 10.1021/np401022g. [DOI] [PubMed] [Google Scholar]
- 249.Kaewpiboon C., Surapinit S., Malilas W., Moon J., Phuwapraisirisan P., Tip-Pyang S., Johnston R.N., Koh S.S., Assavalapsakul W., Chung Y.H. Feroniellin A-induced autophagy causes apoptosis in multidrug-resistant human A549 lung cancer cells. Int. J. Oncol. 2014;44(4):1233–1242. doi: 10.3892/ijo.2014.2297. [DOI] [PubMed] [Google Scholar]
- 250.Fulda S. The mechanism of necroptosis in normal and cancer cells. Cancer Biol. Ther. 2013;14(11):999–1004. doi: 10.4161/cbt.26428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Li J., Yin Q., Wu H. Structural basis of signal transduction in the TNF receptor superfamily. Adv. Immunol. 2013;119:135–153. doi: 10.1016/B978-0-12-407707-2.00005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Vanden Berghe T., Linkermann A., Jouan-Lanhouet S., Walczak H., Vandenabeele P. Regulated necrosis: the expanding network of non-apoptotic cell death pathways. Nat. Rev. Mol. Cell Biol. 2014;15(2):135–147. doi: 10.1038/nrm3737. [DOI] [PubMed] [Google Scholar]
- 253.Newton K. RIPK1 and RIPK3: critical regulators of inflammation and cell death. Trends Cell Biol. 2015;25(6):347–353. doi: 10.1016/j.tcb.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 254.Galluzzi L., Kepp O., Krautwald S., Kroemer G., Linkermann A. Molecular mechanisms of regulated necrosis. Semin. Cell Dev. Biol. 2014;35:24–32. doi: 10.1016/j.semcdb.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 255.Wallach D., Kang T.B., Yang S.H., Kovalenko A. The in vivo significance of necroptosis: lessons from exploration of caspase-8 function. Cytokine Growth Factor Rev. 2014;25(2):157–165. doi: 10.1016/j.cytogfr.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 256.Christofferson D.E., Li Y., Yuan J. Control of life-or-death decisions by RIP1 kinase. Annu. Rev. Physiol. 2014;76:129–150. doi: 10.1146/annurev-physiol-021113-170259. [DOI] [PubMed] [Google Scholar]
- 257.Moriwaki K., Chan F.K. RIP3: a molecular switch for necrosis and inflammation. Genes Dev. 2013;27(15):1640–1649. doi: 10.1101/gad.223321.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Nikoletopoulou V., Markaki M., Palikaras K., Tavernarakis N. Crosstalk between apoptosis, necrosis and autophagy. Biochim. Biophys. Acta. 2013;1833(12):3448–3459. doi: 10.1016/j.bbamcr.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 259.Mathis B.J., Lai Y., Qu C., Janicki J.S., Cui T. CYLD-mediated signaling and diseases. Curr. Drug Targets. 2015;16(4):284–294. doi: 10.2174/1389450115666141024152421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Zhou W., Yuan J. Necroptosis in health and diseases. Semin. Cell Dev. Biol. 2014;35:14–23. doi: 10.1016/j.semcdb.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 261.Dannappel M., Vlantis K., Kumari S., Polykratis A., Kim C., Wachsmuth L., Eftychi C., Lin J., Corona T., Hermance N., Zelic M., Kirsch P., Basic M., Bleich A., Kelliher M., Pasparakis M. RIPK1 maintains epithelial homeostasis by inhibiting apoptosis and necroptosis. Nature. 2014;513(7516):90–94. doi: 10.1038/nature13608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Wang H., Sun L., Su L., Rizo J., Liu L., Wang L.F., Wang F.S., Wang X. Mixed lineage kinase domain-like protein MLKL causes necrotic membrane disruption upon phosphorylation by RIP3. Mol. Cell. 2014;54(1):133–146. doi: 10.1016/j.molcel.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 263.Galluzzi L., Kepp O., Kroemer G. MLKL regulates necrotic plasma membrane permeabilization. Cell Res. 2014;24(2):139–140. doi: 10.1038/cr.2014.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Cai Z., Jitkaew S., Zhao J., Chiang H.C., Choksi S., Liu J., Ward Y., Wu L.G., Liu Z.G. Plasma membrane translocation of trimerized MLKL protein is required for TNF-induced necroptosis. Nat. Cell Biol. 2014;16(1):55–65. doi: 10.1038/ncb2883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Kaczmarek A., Vandenabeele P., Krysko D.V. Necroptosis: the release of damage-associated molecular patterns and its physiological relevance. Immunity. 2013;38(2):209–223. doi: 10.1016/j.immuni.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 266.Krysko D.V., Agostinis P., Krysko O., Garg A.D., Bachert C., Lambrecht B.N., Vandenabeele P. Emerging role of damage-associated molecular patterns derived from mitochondria in inflammation. Trends Immunol. 2011;32(4):157–164. doi: 10.1016/j.it.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 267.Lotze M.T., Deisseroth A., Rubartelli A. Damage associated molecular pattern molecules. Clin. Immunol. 2007;124(1):1–4. doi: 10.1016/j.clim.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Han W., Xie J., Li L., Liu Z., Hu X. Necrostatin-1 reverts shikonin-induced necroptosis to apoptosis. Apoptosis. 2009;14(5):674–686. doi: 10.1007/s10495-009-0334-x. [DOI] [PubMed] [Google Scholar]
- 269.Kroemer G., Piacentini M. Dying to survive - apoptosis, necroptosis, autophagy as supreme experiments of nature. Int. J. Dev. Biol. 2015;59(1-3):5–9. doi: 10.1387/ijdb.150167mp. [DOI] [PubMed] [Google Scholar]
- 270.Dashzeveg N., Yoshida K. Cell death decision by p53 via control of the mitochondrial membrane. Cancer Lett. 2015;367(2):108–112. doi: 10.1016/j.canlet.2015.07.019. [DOI] [PubMed] [Google Scholar]
- 271.Jia L.T., Zhang R., Shen L., Yang A.G. Regulators of carcinogenesis: emerging roles beyond their primary functions. Cancer Lett. 2015;357(1):75–82. doi: 10.1016/j.canlet.2014.11.048. [DOI] [PubMed] [Google Scholar]
- 272.Zamaraev A.V., Kopeina G.S., Zhivotovsky B., Lavrik I.N. Cell death controlling complexes and their potential therapeutic role. Cell. Mol. Life Sci. 2015;72(3):505–517. doi: 10.1007/s00018-014-1757-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Huang Y., Wu J.Z., Li J.Y., Xu W. Know the enemy as well as the weapons in hand: the aberrant death pathways and therapeutic agents in chronic lymphocytic leukemia. Am. J. Cancer Res. 2015;5(8):2361–2375. [PMC free article] [PubMed] [Google Scholar]
- 274.Liu P., Xu B., Shen W., Zhu H., Wu W., Fu Y., Chen H., Dong H., Zhu Y., Miao K., Xu W., Li J. Dysregulation of TNFα-induced necroptotic signaling in chronic lymphocytic leukemia: suppression of CYLD gene by LEF1. Leukemia. 2012;26(6):1293–1300. doi: 10.1038/leu.2011.357. [DOI] [PubMed] [Google Scholar]
- 275.Zhang M., Harashima N., Moritani T., Huang W., Harada M. The Roles of ROS and Caspases in TRAIL-Induced Apoptosis and Necroptosis in Human Pancreatic Cancer Cells. PLoS One. 2015;10(5):e0127386. doi: 10.1371/journal.pone.0127386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Schmidt S.V., Seibert S., Walch-Rückheim B., Vicinus B., Kamionka E.M., Pahne-Zeppenfeld J., Solomayer E.F., Kim Y.J., Bohle R.M., Smola S. RIPK3 expression in cervical cancer cells is required for PolyIC-induced necroptosis, IL-1α release, and efficient paracrine dendritic cell activation. Oncotarget. 2015;6(11):8635–8647. doi: 10.18632/oncotarget.3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Melo-Lima S., Lopes M.C., Mollinedo F. ERK1/2 acts as a switch between necrotic and apoptotic cell death in ether phospholipid edelfosine-treated glioblastoma cells. Pharmacol. Res. 2015;95-96:2–11. doi: 10.1016/j.phrs.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 278.Melo-Lima S., Celeste Lopes M., Mollinedo F. Necroptosis is associated with low procaspase-8 and active RIPK1 and -3 in human glioma cells. Oncoscience. 2014;1(10):649–664. doi: 10.18632/oncoscience.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Chen G., Cheng X., Zhao M., Lin S., Lu J., Kang J., Yu X. RIP1-dependent Bid cleavage mediates TNFα-induced but Caspase-3-independent cell death in L929 fibroblastoma cells. Apoptosis. 2015;20(1):92–109. doi: 10.1007/s10495-014-1058-0. [DOI] [PubMed] [Google Scholar]
- 280.Nugues A.L., El Bouazzati H., Hétuin D., Berthon C., Loyens A., Bertrand E., Jouy N., Idziorek T., Quesnel B. RIP3 is downregulated in human myeloid leukemia cells and modulates apoptosis and caspase-mediated p65/RelA cleavage. Cell Death Dis. 2014;5:e1384. doi: 10.1038/cddis.2014.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Nomura M., Ueno A., Saga K., Fukuzawa M., Kaneda Y. Accumulation of cytosolic calcium induces necroptotic cell death in human neuroblastoma. Cancer Res. 2014;74(4):1056–1066. doi: 10.1158/0008-5472.CAN-13-1283. [DOI] [PubMed] [Google Scholar]
- 282.Fu Z., Deng B., Liao Y., Shan L., Yin F., Wang Z., Zeng H., Zuo D., Hua Y., Cai Z. The anti-tumor effect of shikonin on osteosarcoma by inducing RIP1 and RIP3 dependent necroptosis. BMC Cancer. 2013;13:580. doi: 10.1186/1471-2407-13-580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Piao J.L., Cui Z.G., Furusawa Y., Ahmed K., Rehman M.U., Tabuchi Y., Kadowaki M., Kondo T. The molecular mechanisms and gene expression profiling for shikonin-induced apoptotic and necroptotic cell death in U937 cells. Chem. Biol. Interact. 2013;205(2):119–127. doi: 10.1016/j.cbi.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 284.Deng B., Qiu B. Shikonin inhibits invasiveness of osteosarcoma through MMP13 suppression. Tumour Biol. 2015;36(12):9311–9317. doi: 10.1007/s13277-015-3662-1. [DOI] [PubMed] [Google Scholar]
- 285.Zhao Q., Kretschmer N., Bauer R., Efferth T. Shikonin and its derivatives inhibit the epidermal growth factor receptor signaling and synergistically kill glioblastoma cells in combination with erlotinib. Int. J. Cancer. 2015;137(6):1446–1456. doi: 10.1002/ijc.29483. [DOI] [PubMed] [Google Scholar]
- 286.Wada N., Kawano Y., Fujiwara S., Kikukawa Y., Okuno Y., Tasaki M., Ueda M., Ando Y., Yoshinaga K., Ri M., Iida S., Nakashima T., Shiotsu Y., Mitsuya H., Hata H. Shikonin, dually functions as a proteasome inhibitor and a necroptosis inducer in multiple myeloma cells. Int. J. Oncol. 2015;46(3):963–972. doi: 10.3892/ijo.2014.2804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Huang C., Luo Y., Zhao J., Yang F., Zhao H., Fan W., Ge P. Shikonin kills glioma cells through necroptosis mediated by RIP-1. PLoS One. 2013;8(6):e66326. doi: 10.1371/journal.pone.0066326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Han W., Xie J., Fang Y., Wang Z., Pan H. Nec-1 enhances shikonin-induced apoptosis in leukemia cells by inhibition of RIP-1 and ERK1/2. Int. J. Mol. Sci. 2012;13(6):7212–7225. doi: 10.3390/ijms13067212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Xuan Y., Hu X. Naturally-occurring shikonin analoguesa class of necroptotic inducers that circumvent cancer drug resistance. Cancer Lett. 2009;274(2):233–242. doi: 10.1016/j.canlet.2008.09.029. [DOI] [PubMed] [Google Scholar]
- 290.Hu X., Han W., Li L. Targeting the weak point of cancer by induction of necroptosis. Autophagy. 2007;3(5):490–492. doi: 10.4161/auto.4592. [DOI] [PubMed] [Google Scholar]
- 291.Han W., Li L., Qiu S., Lu Q., Pan Q., Gu Y., Luo J., Hu X. Shikonin circumvents cancer drug resistance by induction of a necroptotic death. Mol. Cancer Ther. 2007;6(5):1641–1649. doi: 10.1158/1535-7163.MCT-06-0511. [DOI] [PubMed] [Google Scholar]
- 292.Jang S.Y., Lee J.K., Jang E.H., Jeong S.Y., Kim J.H. Shikonin blocks migration and invasion of human breast cancer cells through inhibition of matrix metalloproteinase-9 activation. Oncol. Rep. 2014;31(6):2827–2833. doi: 10.3892/or.2014.3159. [DOI] [PubMed] [Google Scholar]
- 293.Li W., Liu J., Jackson K., Shi R., Zhao Y. Sensitizing the therapeutic efficacy of taxol with shikonin in human breast cancer cells. PLoS One. 2014;9(4):e94079. doi: 10.1371/journal.pone.0094079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Yao Y., Zhou Q. A novel antiestrogen agent Shikonin inhibits estrogen-dependent gene transcription in human breast cancer cells. Breast Cancer Res. Treat. 2010;121(1):233–240. doi: 10.1007/s10549-009-0547-2. [DOI] [PubMed] [Google Scholar]
- 295.Hou Y., Guo T., Wu C., He X., Zhao M. Effect of shikonin on human breast cancer cells proliferation and apoptosis in vitro. Yakugaku Zasshi. 2006;126(12):1383–1386. doi: 10.1248/yakushi.126.1383. [DOI] [PubMed] [Google Scholar]
- 296.Dunai Z.A., Imre G., Barna G., Korcsmaros T., Petak I., Bauer P.I., Mihalik R. Staurosporine induces necroptotic cell death under caspase-compromised conditions in U937 cells. PLoS One. 2012;7(7):e41945. doi: 10.1371/journal.pone.0041945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Aredia F., Scovassi A.I. Poly(ADP-ribose): a signaling molecule in different paradigms of cell death. Biochem. Pharmacol. 2014;92(1):157–163. doi: 10.1016/j.bcp.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 298.Sosna J., Voigt S., Mathieu S., Lange A., Thon L., Davarnia P., Herdegen T., Linkermann A., Rittger A., Chan F.K., Kabelitz D., Schütze S., Adam D. TNF-induced necroptosis and PARP-1-mediated necrosis represent distinct routes to programmed necrotic cell death. Cell. Mol. Life Sci. 2014;71(2):331–348. doi: 10.1007/s00018-013-1381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Basit F., Cristofanon S., Fulda S. Obatoclax (GX15070) triggers necroptosis by promoting the assembly of the necrosome on autophagosomal membranes. Cell Death Differ. 2013;20(9):1161–1173. doi: 10.1038/cdd.2013.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Urtishak K.A., Edwards A.Y., Wang L.S., Hudome A., Robinson B.W., Barrett J.S., Cao K., Cory L., Moore J.S., Bantly A.D., Yu Q.C., Chen I.M., Atlas S.R., Willman C.L., Kundu M., Carroll A.J., Heerema N.A., Devidas M., Hilden J.M., Dreyer Z.E., Hunger S.P., Reaman G.H., Felix C.A. Potent obatoclax cytotoxicity and activation of triple death mode killing across infant acute lymphoblastic leukemia. Blood. 2013;121(14):2689–2703. doi: 10.1182/blood-2012-04-425033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Bonapace L., Bornhauser B.C., Schmitz M., Cario G., Ziegler U., Niggli F.K., Schäfer B.W., Schrappe M., Stanulla M., Bourquin J.P. Induction of autophagy-dependent necroptosis is required for childhood acute lymphoblastic leukemia cells to overcome glucocorticoid resistance. J. Clin. Invest. 2010;120(4):1310–1323. doi: 10.1172/JCI39987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Coupienne I., Bontems S., Dewaele M., Rubio N., Habraken Y., Fulda S., Agostinis P., Piette J. NF-kappaB inhibition improves the sensitivity of human glioblastoma cells to 5-aminolevulinic acid-based photodynamic therapy. Biochem. Pharmacol. 2011;81(5):606–616. doi: 10.1016/j.bcp.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 303.Möhler H., Pfirrmann R.W., Frei K. Redox-directed cancer therapeutics: Taurolidine and Piperlongumine as broadly effective antineoplastic agents (review). Int. J. Oncol. 2014;45(4):1329–1336. doi: 10.3892/ijo.2014.2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Han B., Wang T.D., Shen S.M., Yu Y., Mao C., Yao Z.J., Wang L.S. Annonaceous acetogenin mimic AA005 induces cancer cell death via apoptosis inducing factor through a caspase-3-independent mechanism. BMC Cancer. 2015;15:139. doi: 10.1186/s12885-015-1133-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Longato G.B., Fiorito G.F., Vendramini-Costa D.B., de Oliveira Sousa I.M., Tinti S.V., Ruiz A.L., de Almeida S.M., Padilha R.J., Foglio M.A., de Carvalho J.E. Different cell death responses induced by eupomatenoid-5 in MCF-7 and 7860 tumor cell lines. Toxicol. In Vitro. 2015;29(5):1026–1033. doi: 10.1016/j.tiv.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 306.Lin W., Tongyi S. Role of Bax/Bcl-2 family members in green tea polyphenol induced necroptosis of p53-deficient Hep3B cells. Tumour Biol. 2014;35(8):8065–8075. doi: 10.1007/s13277-014-2064-0. [DOI] [PubMed] [Google Scholar]
- 307.Pozarowski P., Halicka D.H., Darzynkiewicz Z. Cell cycle effects and caspase-dependent and independent death of HL-60 and Jurkat cells treated with the inhibitor of NF-kappaB parthenolide. Cell Cycle. 2003;2(4):377–383. doi: 10.4161/cc.2.4.420. [DOI] [PubMed] [Google Scholar]
- 308.Pozarowski P., Halicka D.H., Darzynkiewicz Z. NF-kappaB inhibitor sesquiterpene parthenolide induces concurrently atypical apoptosis and cell necrosis: difficulties in identification of dead cells in such cultures. Cytometry A. 2003;54(2):118–124. doi: 10.1002/cyto.a.10057. [DOI] [PubMed] [Google Scholar]
- 309.Lu C., Zhou L.Y., Xu H.J., Chen X.Y., Tong Z.S., Liu X.D., Jia Y.S., Chen Y. RIP3 overexpression sensitizes human breast cancer cells to parthenolide in vitro via intracellular ROS accumulation. Acta Pharmacol. Sin. 2014;35(7):929–936. doi: 10.1038/aps.2014.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Kong F.C., Zhang J.Q., Zeng C., Chen W.L., Ren W.X., Yan G.X., Wang H.X., Li Q.B., Chen Z.C. Inhibitory effects of parthenolide on the activity of NF-κB in multiple myeloma via targeting TRAF6. J. Huazhong Univ. Sci. Technolog. Med. Sci. 2015;35(3):343–349. doi: 10.1007/s11596-015-1435-0. [DOI] [PubMed] [Google Scholar]
- 311.Delmas D., Solary E., Latruffe N. Resveratrol, a phytochemical inducer of multiple cell death pathways: apoptosis, autophagy and mitotic catastrophe. Curr. Med. Chem. 2011;18(8):1100–1121. doi: 10.2174/092986711795029708. [DOI] [PubMed] [Google Scholar]
- 312.Galluzzi L., Vitale I., Vacchelli E., Kroemer G. Cell death signaling and anticancer therapy. Front. Oncol. 2011;1:5. doi: 10.3389/fonc.2011.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Sperandio S., de Belle I., Bredesen D.E. An alternative, nonapoptotic form of programmed cell death. Proc. Natl. Acad. Sci. USA. 2000;97(26):14376–14381. doi: 10.1073/pnas.97.26.14376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Sperandio S., Poksay K.S., Schilling B., Crippen D., Gibson B.W., Bredesen D.E. Identification of new modulators and protein alterations in non-apoptotic programmed cell death. J. Cell. Biochem. 2010;111(6):1401–1412. doi: 10.1002/jcb.22870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Guo W.J., Chen T.S., Wang X.P., Chen R. Taxol induces concentration-dependent apoptotic and paraptosis-like cell death in human lung adenocarcinoma (ASTC-a-1) cells. J. XRay Sci. Technol. 2010;18(3):293–308. doi: 10.3233/XST-2010-0261. [DOI] [PubMed] [Google Scholar]
- 316.Zhang J.S., Li D.M., Ma Y., He N., Gu Q., Wang F.S., Jiang S.Q., Chen B.Q., Liu J.R. γ-Tocotrienol induces paraptosis-like cell death in human colon carcinoma SW620 cells. PLoS One. 2013;8(2):e57779. doi: 10.1371/journal.pone.0057779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Li B., Zhao J., Wang C.Z., Searle J., He T.C., Yuan C.S., Du W. Ginsenoside Rh2 induces apoptosis and paraptosis-like cell death in colorectal cancer cells through activation of p53. Cancer Lett. 2011;301(2):185–192. doi: 10.1016/j.canlet.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Wang Y., Zhu X., Yang Z., Zhao X. Honokiol induces caspase-independent paraptosis via reactive oxygen species production that is accompanied by apoptosis in leukemia cells. Biochem. Biophys. Res. Commun. 2013;430(3):876–882. doi: 10.1016/j.bbrc.2012.12.063. [DOI] [PubMed] [Google Scholar]
- 319.Yumnam S., Hong G.E., Raha S., Venkatarame Gowda Saralamma V., Lee H.J., Lee W.S., Kim E.H., Kim G.S. Mitochondrial Dysfunction and Ca(2+) Overload Contributes to Hesperidin Induced Paraptosis in Hepatoblastoma Cells, HepG2. J. Cell. Physiol. 2015 doi: 10.1002/jcp.25222. [DOI] [PubMed] [Google Scholar]
- 320.Yoon M.J., Lee A.R., Jeong S.A., Kim Y.S., Kim J.Y., Kwon Y.J., Choi K.S. Release of Ca2+ from the endoplasmic reticulum and its subsequent influx into mitochondria trigger celastrol-induced paraptosis in cancer cells. Oncotarget. 2014;5(16):6816–6831. doi: 10.18632/oncotarget.2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Wang Y., Kim N.S., Haince J.F., Kang H.C., David K.K., Andrabi S.A., Poirier G.G., Dawson V.L., Dawson T.M. Poly(ADP-ribose) (PAR) binding to apoptosis-inducing factor is critical for PAR polymerase-1-dependent cell death (parthanatos). Sci. Signal. 2011;4(167):ra20. doi: 10.1126/scisignal.2000902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Fatokun A.A., Dawson V.L., Dawson T.M. Parthanatos: mitochondrial-linked mechanisms and therapeutic opportunities. Br. J. Pharmacol. 2014;171(8):2000–2016. doi: 10.1111/bph.12416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Aredia F., Scovassi A.I. Involvement of PARPs in cell death. Front. Biosci. (Elite Ed.) 2014;6:308–317. doi: 10.2741/707. [Elite Education]. [DOI] [PubMed] [Google Scholar]
- 324.Basello D.A., Scovassi A.I. Poly(ADP-ribosylation) and neurodegenerative disorders. Mitochondrion. 2015;24:56–63. doi: 10.1016/j.mito.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 325.Andrabi S.A., Umanah G.K., Chang C., Stevens D.A., Karuppagounder S.S., Gagné J.P., Poirier G.G., Dawson V.L., Dawson T.M. Poly(ADP-ribose) polymerase-dependent energy depletion occurs through inhibition of glycolysis. Proc. Natl. Acad. Sci. USA. 2014;111(28):10209–10214. doi: 10.1073/pnas.1405158111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Zhao N., Mao Y., Han G., Ju Q., Zhou L., Liu F., Xu Y., Zhao X. YM155, a survivin suppressant, triggers PARP-dependent cell death (parthanatos) and inhibits esophageal squamous-cell carcinoma xenografts in mice. Oncotarget. 2015;6(21):18445–18459. doi: 10.18632/oncotarget.4315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Castedo M., Perfettini J.L., Roumier T., Andreau K., Medema R., Kroemer G. Cell death by mitotic catastrophe: a molecular definition. Oncogene. 2004;23(16):2825–2837. doi: 10.1038/sj.onc.1207528. [DOI] [PubMed] [Google Scholar]
- 328.Chow J.P., Poon R.Y. Mitotic catastrophe. In: Enders G., editor. Cell Cycle Deregulation in Cancer. New York: Springer; 2010. pp. 79–96. [DOI] [Google Scholar]
- 329.Vakifahmetoglu H., Olsson M., Zhivotovsky B. Death through a tragedy: mitotic catastrophe. Cell Death Differ. 2008;15(7):1153–1162. doi: 10.1038/cdd.2008.47. [DOI] [PubMed] [Google Scholar]
- 330.Mc Gee M.M. 2015.
- 331.Chen C.A., Chen C.C., Shen C.C., Chang H.H., Chen Y.J. Moscatilin induces apoptosis and mitotic catastrophe in human esophageal cancer cells. J. Med. Food. 2013;16(10):869–877. doi: 10.1089/jmf.2012.2617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Kainz K.P., Krenn L., Erdem Z., Kaehlig H., Zehl M., Bursch W., Berger W., Marian B. 2-deprenyl-rheediaxanthone B isolated from Metaxya rostrata induces active cell death in colorectal tumor cells. PLoS One. 2013;8(6):e65745. doi: 10.1371/journal.pone.0065745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Dolečková I., Rárová L., Grúz J., Vondrusová M., Strnad M., Kryštof V. Antiproliferative and antiangiogenic effects of flavone eupatorin, an active constituent of chloroform extract of Orthosiphon stamineus leaves. Fitoterapia. 2012;83(6):1000–1007. doi: 10.1016/j.fitote.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 334.Chen Y.J., Chou C.J., Chang T.T. Compound MMH01 possesses toxicity against human leukemia and pancreatic cancer cells. Toxicol. In Vitro. 2009;23(3):418–424. doi: 10.1016/j.tiv.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 335.Pathak S., Multani A.S., Banerji P., Banerji P. Ruta 6 selectively induces cell death in brain cancer cells but proliferation in normal peripheral blood lymphocytes: A novel treatment for human brain cancer. Int. J. Oncol. 2003;23(4):975–982. [PubMed] [Google Scholar]
- 336.Hematulin A., Ingkaninan K., Limpeanchob N., Sagan D. Ethanolic extract from Derris scandens Benth mediates radiosensitzation via two distinct modes of cell death in human colon cancer HT-29 cells. Asian Pac. J. Cancer Prev. 2014;15(4):1871–1877. doi: 10.7314/APJCP.2014.15.4.1871. [DOI] [PubMed] [Google Scholar]
- 337.Reyjal J., Cormier K., Turcotte S. Autophagy and cell death to target cancer cells: exploiting synthetic lethality as cancer therapies. Adv. Exp. Med. Biol. 2014;772:167–188. doi: 10.1007/978-1-4614-5915-6_8. [DOI] [PubMed] [Google Scholar]
- 338.Fulda S. Therapeutic exploitation of necroptosis for cancer therapy. Semin. Cell Dev. Biol. 2014;35:51–56. doi: 10.1016/j.semcdb.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 339.Cho Y.S., Park S.Y. Harnessing of Programmed Necrosis for Fighting against Cancers. Biomol. Ther. (Seoul) 2014;22(3):167–175. doi: 10.4062/biomolther.2014.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Belaid A., Ndiaye P.D., Filippakis H., Roux J., Röttinger É., Graba Y., Brest P., Hofman P., Mograbi B. Autophagy : Moving Benchside Promises to Patient Bedsides. Curr. Cancer Drug Targets. 2015;15(8):684–702. doi: 10.2174/156800961508151001102452. [DOI] [PubMed] [Google Scholar]
- 341.Zhang D., Tang B., Xie X., Xiao Y.F., Yang S.M., Zhang J.W. The interplay between DNA repair and autophagy in cancer therapy. Cancer Biol. Ther. 2015;16(7):1005–1013. doi: 10.1080/15384047.2015.1046022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Tang J., Di J., Cao H., Bai J., Zheng J. p53-mediated autophagic regulation: A prospective strategy for cancer therapy. Cancer Lett. 2015;363(2):101–107. doi: 10.1016/j.canlet.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 343.Li S., Wang L., Hu Y., Sheng R. Autophagy regulators as potential cancer therapeutic agents: a review. Curr. Top. Med. Chem. 2015;15(8):720–744. doi: 10.2174/1568026615666150302105343. [DOI] [PubMed] [Google Scholar]