Abstract
Introduction
Peripheral intravenous catheter (PIVC) insertion is one of the most common invasive procedures performed in a hospital, but most nurses receive little formal training in this area. Blended PIVC insertion training programs that incorporate deliberate simulated practice have the potential to improve clinical practice and patient care.
Methods
The study was a randomized, wait-list control group with crossover using nurses on three medical/surgical units. Baseline PIVC knowledge, confidence, and skills assessments were completed for both groups. The intervention group then received a 2-hour PIVC online course, followed by an 8-hour live training course using a synergistic mix of three simulation tools. Both groups were then reassessed. After crossover, the wait-list group received the same intervention and both groups were reassessed.
Results
At baseline, both groups were similar for knowledge, confidence, and skills. Compared with the wait-list group, the intervention group had significantly higher scores for knowledge, confidence, and skills upon completing the training program. After crossover, the wait-list group had similarly higher scores for knowledge, confidence, and skills than the intervention group. Between the immediate preintervention and postintervention periods, the intervention group improved scores for knowledge by 31%, skills by 24%, and decreased confidence by 0.5%, whereas the wait-list group improved scores for knowledge by 28%, confidence by 16%, and skills by 15%.
Conclusions
Results demonstrate significant improvements in nurses' knowledge, confidence, and skills with the use of a simulation-based blended learning program for PIVC insertion. Transferability of these findings from a simulated environment into clinical practice should be further explored.
Key Words: Nurses, Peripheral intravenous catheter, Skills, Confidence, Knowledge, Simulation, Training program, Blended learning, Education
It is estimated that more than 300 million short (<3 in) peripheral intravenous catheters (PIVCs) are sold annually in the United States with at least 80% of all hospitalized patients receiving some form of infusion therapy.1–3 Even though it is a prevalent, technically difficult, and invasive procedure, most health care practitioners, who have not been trained as vascular access experts, receive little substantive peripheral vascular access education, training, or opportunities to practice skills until competent.1,3–6 A recent analysis revealed overall PIVC catheter failure rates ranging from 35% to 50% leading to premature removal before the catheter's intended dwell time. Health care practitioner PIVC knowledge and skill deficits were identified as one of three primary factors leading to catheter failure and premature removal.7
Research comparing the knowledge, confidence, and skills of staff nurses who receive little PIVC education compared with those who receive more extensive education is limited. There is evidence that PIVC insertion knowledge, confidence, and skills are directly related to first attempt success8,9 and that use of expert nurses to perform PIVC insertion decreases patient complications.10 Numerous practitioner PIVC knowledge and insertion skill deficits have been identified, including patient assessment, insertion site selection, catheter selection and insertion, catheter securement, dwell time, complication identification and treatment, and compliance with best practice guidelines, further punctuating the need for effective education strategies.2,8,10–13 Furthermore, complication rates due to premature removal of PIVCs include phlebitis (15.4%), infiltration (23.9%), catheter occlusion (18.8%), catheter dislodgement (6.9%), and catheter-related infection (0.2%).7
In addition to the need to reduce PIVC patient complications, the need to reduce the financial burden of less than adequate PIVC knowledge and skills is compelling. The average cost of an uncomplicated PIVC insertion is estimated to be US $28 to $35.7 Existing data report first attempt success for staff nurses and more educated and experienced IV nurses, in diverse patient populations, to range from 44% to 76.9% and 91% to 98%, respectively.8–10 Other researchers have reported a range of 2.18 and 2.35 PIVC insertion attempts to establish a patent peripheral IV site.14,15 More broadly, these data align with other investigators who report that approximately 150 million PIVCs (half the number of PIVCs purchased) are successfully inserted.2,16 After a PIVC has been placed, each removal due to complication and subsequent reinsertion progressively increases procedural costs and may lead to the use of more invasive vascular access devices.7 The national financial burden for premature PIVC removal can be conservatively estimated at US $1.5 billion annually, considering the low average PIVC failure rate of 35% multiplied by the estimated 150 million PIVCs placed and by a low average uncomplicated procedure cost of US $28.
Despite the demonstrated need, research related to innovative peripheral vascular access education has been limited. Early investigators searched for a technological solution by trying to identify the most effective simulation tools for PIVC insertion training.17,18 More recently, others have focused on technology versus traditional methods by comparing PIVC insertion simulation-based educational methodology to a “see one, do one” training technique.5,6
One randomized trial of 46 nurses found that participants who received simulation-based training had a significantly lower number of IV insertion attempts per patient compared with those who received traditional training (P = 0.043). In addition, the number of reported patient complications was lower with the simulation-based trained nurses (21% vs. 33%), although the statistical significance of this result was not reported.6 Although these results suggest that the simulation-based training resulted in greater first stick success, there were several limitations in the study including limited dependent variable measurement, narrowly defined insertion success, and reliance on self-report measures.
Other researchers have explored blended learning methodologies that combine didactic, demonstration, and a variety of simulation-based experiential tools to facilitate improved PIVC insertion knowledge, confidence, and skills. Lyons and Kasker5 measured the impact of a 1-day didactic instruction and IV insertion skills/competency validation continuing education program with experienced nurses (n = 40). In this study, the average pretest PIVC insertion knowledge scores were 77.88% versus 96.67% immediate posttest (P < 0.001) and 90.38% 8 to 12 weeks posttest, demonstrating retained new knowledge over time compared with baseline. In addition, of the 14 PIVC insertion core skills measured, there were improvements in 12. The limitations of this study included a self-selected, nonrandomized population.
Although integrating limited simulated practice into existing training paradigms has demonstrated some promising results, truly solving this complex practice issue likely requires a total reinvention of how health care practitioners are educated in peripheral vascular access. The far-reaching clinical and financial implications of effective PIVC insertion necessitate a more robust, evidence-based educational strategy to improve health care practitioners' skills and maximize patient outcomes in this area. However, to date, there have been no formal, randomized studies to evaluate a more robust comprehensive, simulation-based blended educational curriculum on health care practitioner PIVC insertion knowledge, confidence, and skills.
METHODS
Aims
The primary aim of this study was to determine the impact of a blended, comprehensive instructional program, which incorporated self-paced interactive online education and deliberate PIVC procedural practice using a synergistic mix of three different simulation technologies on nurses' PIVC insertion knowledge, confidence, and skills in a simulated environment. Secondary aims included determining the impact of the program on nurses' first attempt success and PIVC insertion procedure time, study units' PIVC inventory, and number of calls to the IV therapy team for support in the clinical environment.
Design and Methodology
The study was conducted using a randomized, wait-list control group, with crossover design.19,20 See Figure 1 for Consolidated Standards of Reporting Trials diagram, outlining participant flow through the study. Baseline measurements, including a demographic survey and PIVC insertion knowledge, confidence, and skills assessments, were completed for both groups during period 1. Two months from baseline measurements and immediately after group A completion of the intervention, both groups were reassessed for knowledge, confidence, and skills during period 2. Group B then crossed over to receive the intervention. Two months from the second assessment and immediately after group B completion of the intervention, both groups were reassessed for knowledge, confidence, and skills during period 3.
FIGURE 1.
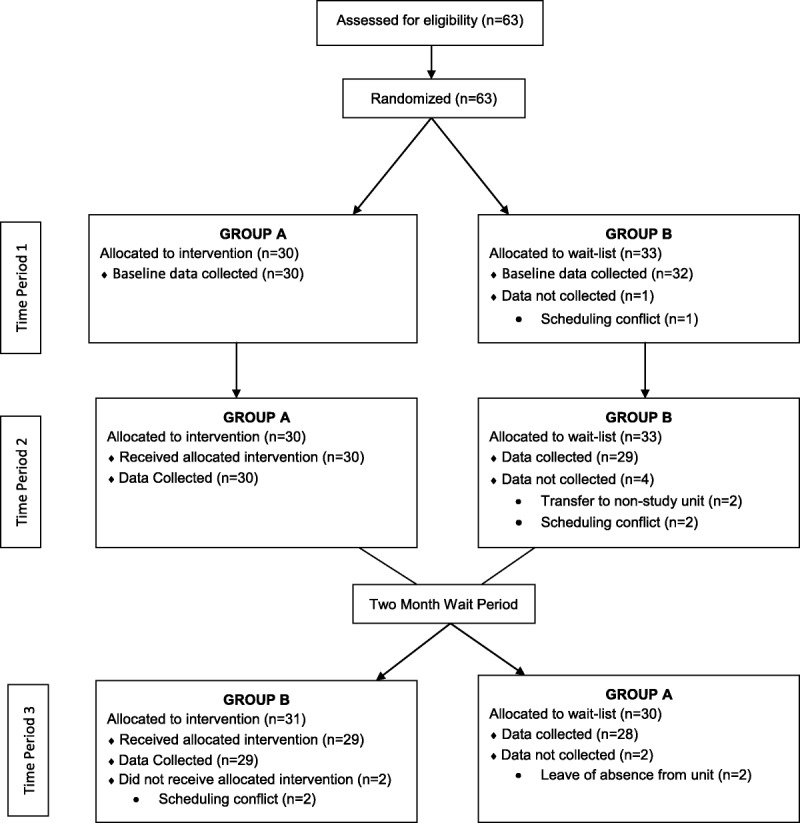
Consolidated Standards of Reporting Trials flow diagram.
Participants
The study was conducted at a 504-bed, nonuniversity-affiliated, teaching hospital in the northeastern United States. Participants were registered nurses on two postsurgical units and one medical/surgical orthopedic unit. All eligible registered nurses who were employed on the study units and worked at least 48 hours each month at the time of randomization were included. Nurses were excluded if they were hired to the units after randomization, were on leave of absence at the time of randomization, or worked on the hospital's IV therapy support team. A computer-generated randomization list was used to assign participants to each of the study groups. An overview of the study design and participant requirements was presented to the staff by the investigators.
Sample Size Estimation
A power analysis was conducted before the start of the study.21 Using a 1-sided test with an α of 0.05, power of 0.80, and expected assessment preintervention means (knowledge = 15, confidence = 5, skills = 20), postintervention increase in mean score (knowledge = 18, confidence = 7, skills = 25), and standard deviation (knowledge = 6, confidence = 4, skills = 10), it was determined that a minimum of 25 participants in each group was required. Values used to estimate the sample size were based on previous experience using variations of the instruments in similar populations.
Intervention
The primary aim of this study is to determine the impact of a blended, comprehensive instructional program, which incorporated self-paced interactive online education and deliberate PIVC procedural practice using a synergistic mix of three different simulation technologies on nurses' PIVC insertion knowledge, confidence, and skills in a simulated environment. Both intervention components were adapted from an established 2-day proprietary training program used by industry to train clinical nurse educators and sales specialists on the PIVC insertion process.22,23 In compliance with the hospital's existing protocol, study participants were given 4 weeks to complete the online learning course before participating in the live simulation-based training course. This approach facilitated evaluating the learning intervention in an authentic, real-world hospital environment, which requires the continuous education of staff while allowing for flexible scheduling and maintaining patient care responsibilities.
Online Learning Course
The online learning course was designed by three of the investigators for front-line nurses performing PIVC insertion, care, and maintenance to further develop their knowledge and understanding of important topics related to PIVC insertion and how to systematically apply best practices to improve patient care and promote patient safety. Participants were presented with best practice information while being continually engaged and immersed in the learning experience through the use of clinical notes, case studies, simulated practice exercises, and knowledge checks with built-in feedback.
Simulation-Based Live Course
Upon completion of the online course, participants attended an 8-hour live PIVC insertion simulation-based training course developed and facilitated by two of the investigators. Participants practiced PIVC placements in three sequential procedural workshops that included the synergistic use of three simulation tools. During the workshops, participants were randomly paired to promote learning through doing, observing, and coaching. Each workshop provided hands-on simulations with deliberate practice using varied clinical and patient scenarios.
First, PIVC insertions were practiced repeatedly on the Virtual I.V. Simulator (Laerdal Medical, Wappingers Falls, NY), a computer-based, interactive, self-directed PIVC learning system. Three hours were allotted to this first workshop, which focused on the procedure itself and incorporated the use of a simulated catheter and haptic device. A detailed case review followed each simulated procedure providing feedback and individual procedural performance scores. The 3 hours were divided, so that 1.25 hours were provided for orientation and practice on the simulator and 1.75 hours were allotted for completion of competency cases. Participants were required to complete two successful PIVC insertions with 90% competency before proceeding to the second workshop.
The second workshop incorporated the Advanced Venipuncture Training Aid (VATA Inc, Canby, OR), a task trainer that includes four veins of various depths and visibility in a tissue-like material with simulated blood. This simulation tool allowed for the use of most IV supplies used in clinical practice. Instruction was provided for guided practice using the PIVC insertion skills checklist and peer-to-peer coaching. Each participant completed six self-paced simulated PIVC insertion procedures during this 1-hour workshop.
The Advanced Venipuncture Arm (Limbs & Things LTD, Savannah, GA), a realistic adult task training arm with multiple access sites and controllable blood flow, was used during the final 1-hour workshop. Using this higher-fidelity task trainer, participants performed and practiced all steps within the IV insertion process using all necessary IV supplies. Through guided practice, the process of PIVC insertion and use of supplies were brought together completely in simulated insertions. Participants completed six simulated PIVC insertion procedures on the Advanced Venipuncture Arm.
The remaining 3 hours of the course were dedicated to completion of the knowledge, confidence, and skills assessment as well as a group debriefing. Formative debriefs were conducted after each workshop and an informal summative group debrief occurred at the conclusion of the learning intervention. Participants were given the opportunity to discuss the training course and key learnings and applications. The debrief was not structured or timed and continued until conversation ceased.
Data Collection
Unique personal identification numbers were assigned to each participant to be used on all study-related documents. Beginning 2 months before baseline assessment and throughout the study, participants were asked to complete IV start data cards for every patient on which they assessed, attempted, or started a PIVC. Data collection took place from June to December 2014. Excluding the IV start data cards, all data were collected by study investigators and a team of site nurses who had been trained as skills evaluators. The principal investigator entered and managed all data.
Instruments
The knowledge, confidence, and skills assessments were adapted specifically for the current research and underwent content validity review and reliability testing. Content validity was obtained from a panel of three infusion therapy experts for all three assessments.
Demographic Data Form
This form contains the following five questions: sex, age, number of years practicing as a nurse, academic degrees, and certifications.
Peripheral Intravenous Catheter Insertion Knowledge Assessment
The PIVC Insertion Knowledge Assessment is a 14-item, 22-point tool to measure nurses' knowledge of correct PIVC insertion including anatomy, assessment, procedure, complications, and documentation. Question format is varied and includes multiple choice, placing items in sequence, and fill in the blank. A pilot test using 22 practicing nurses was conducted to measure 2-day test/retest reliability (r = 0.81).
Peripheral Intravenous Catheter Insertion Confidence Assessment
The PIVC Insertion Confidence Assessment consists of 10 items each scored on a 5-point Likert scale from “strongly agree” to “strongly disagree.” The items measure nurses' confidence in their personal PIVC insertion skills including site selection/assessment, procedure, dressing, and documentation. A pilot test using 22 practicing nurses was conducted to measure 2-day test/retest reliability (r = 0.96).24
Peripheral Intravenous Catheter Insertion Skills Checklist
The PIVC Insertion Skills Checklist is a 28-item checklist based on the Infusion Nurses Society Standards of Practice.25 It was used to measure PIVC insertion skills in a simulated clinical environment using the Advanced Venipunture Arm. The simulated arm was harnessed to a confederate patient to provide participants with the sense and stress of performing the PIVC insertion on a real patient. Each study participant was expected to complete a routine PIVC insertion, from reading a prescribing provider's order through documentation of the procedure, while being observed by a trained evaluator. Before using the checklist, all evaluators (n = 9) completed a 3-hour classroom training program that included instrument instruction, practice, and debrief. Evaluators were also required to complete online refresher training by observing IV start videos and practicing with the checklist to maintain proficiency within 5 days of scheduled observations. In addition, evaluators were reoriented with the instrument 30 minutes before scheduled observations. During the current study, interrater reliability was determined by comparing at least two evaluator observations during each study period to a study investigator, who was considered the criterion standard. Pearson correlation between evaluator and criterion standard for the total score was r value of 0.98 for 94 observations.
Intravenous Start Cards
Participants were asked to complete an IV start card documenting date/time, number of attempts, success, and total time of procedure each time they attempted an IV start on a patient. A secure slotted box was provided on each unit for depositing the completed cards.
Ethical Considerations
The research protocol was approved with exempt status by the hospital's institutional review board.
Statistical Analysis
Descriptive statistical analyses were performed for the study sample. The two groups were initially compared in terms of baseline demographic factors. Scores reflecting PIVC insertion knowledge, confidence, and skills as well as procedural time and proportion of first attempt success were also evaluated and compared in the two groups for each period in the study. For continuous variables, the t test or Mann-Whitney U test was used as appropriate. Categorical data were analyzed using either the χ2 test or Fisher exact test as appropriate. Pairwise comparisons were also made across periods within each of the two groups using the paired t test or the Wilcoxon signed-ranks test for the analysis of total scores on instruments and the McNemar test for paired proportions for analyzing proportion of first attempt success. Calls to the IV therapy support team and PIVC inventory data were analyzed using the t test. Statistical significance was considered at a P value of less than 0.05. All statistical analyses were performed using SPSS 21.0 (SPSS Inc, Release 21.0).
RESULTS
Sample
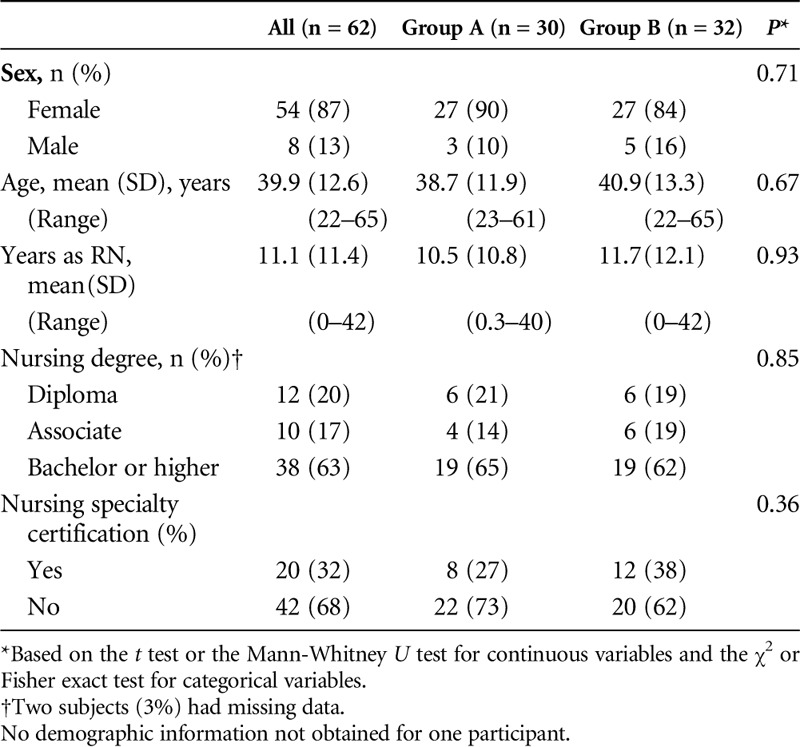
A total of 63 subjects participated in the study with demographic data collected on 62 subjects. Table 1 provides the demographic characteristics of the study participants in each group. The two groups were not statistically different in terms of sex, age, years of nursing experience, education, or certification status.
TABLE 1.
Demographic Characteristics of Study Participants (N = 62)
Primary Aim (Knowledge, Confidence, and Skills Simulation Assessments)
Between Group Differences
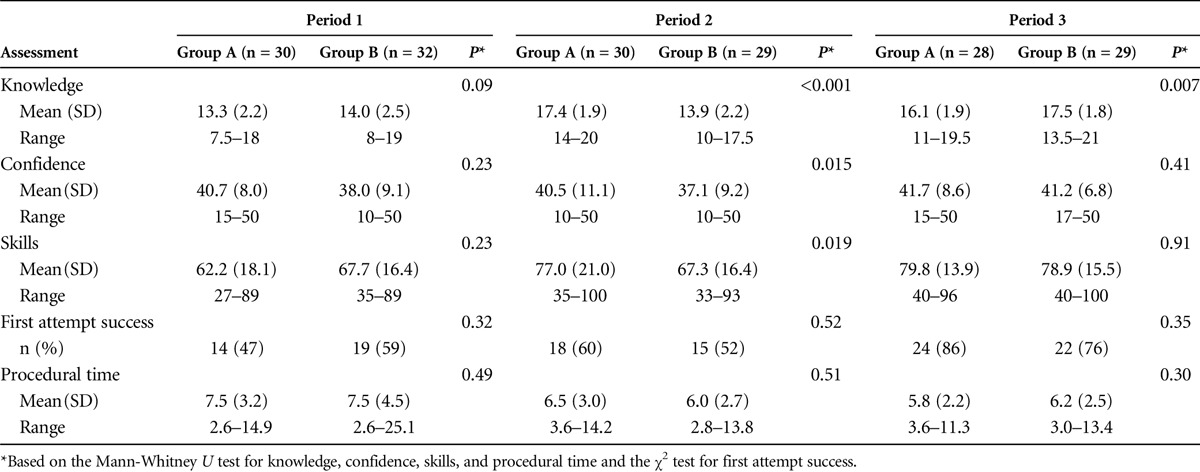
Table 2 describes results for knowledge, confidence, and skills between study groups across periods. At period 1, there were no statistically significant differences between the groups' knowledge (P = 0.09), confidence (P = 0.23), skills (P = 0.23), proportion of first attempt success (P = 0.32), or procedural time (P = 0.49). At period 2, compared with group B, group A had significantly higher scores for knowledge (P < 0.001), confidence (P = 0.015), and skills (P = 0.019) but not proportion of first attempt success (P = 0.52) or procedural time (P = 0.51) upon receiving the intervention. Group B received the intervention at period 3. At this time, results for both groups were similar for confidence (P = 0.41), skills (P = 0.91), proportion of first attempt success (P = 0.35), and procedural time (P = 0.30), whereas group B had significantly higher knowledge scores compared with group A (P = 0.007).
TABLE 2.
Knowledge, Confidence, and Skills Simulation Assessments Between Study Groups Across Periods
Within Group Differences
Table 3 describes results for knowledge, confidence, and skills within study groups across periods. For group A, there were significantly higher scores for knowledge and skills at period 2 compared with period 1 (P < 0.001, P = 0.008, respectively), whereas no significant improvement was observed in confidence, proportion of first attempt success, or procedural time. For group B, there were no significant differences in scores for knowledge, confidence, total skills, proportion of first attempt success, or procedural time between periods 1 and 2.
TABLE 3.
Knowledge, Confidence, and Skills Simulation Assessments Within Study Groups Across Periods
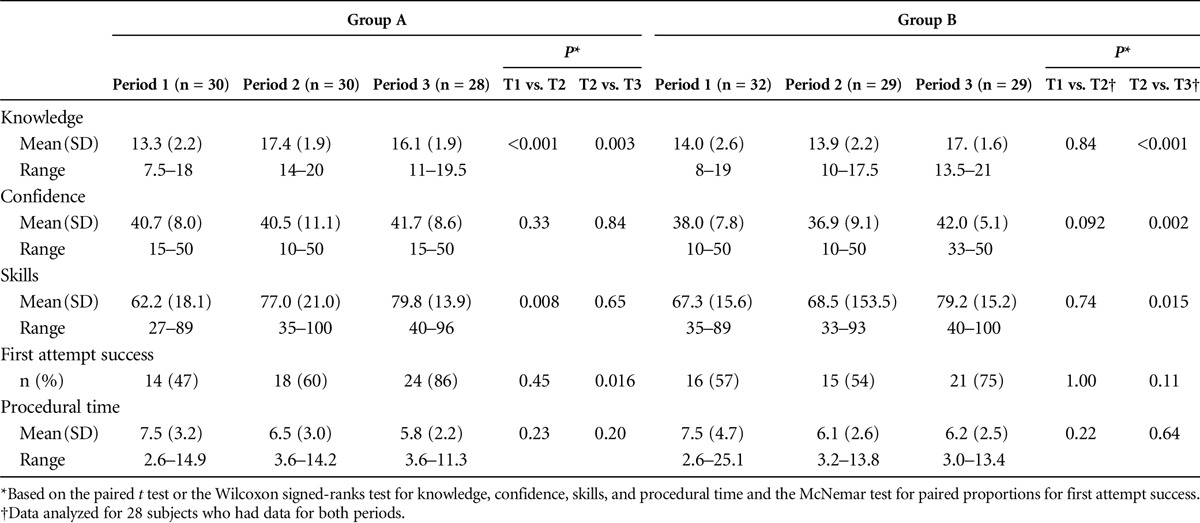
At period 3, group B had significant improvement in knowledge (P < 0.001), confidence (P = 0.002), and skills (P = 0.015) compared with period 2. Group A demonstrated significantly lower knowledge scores in period 3 compared with period 2 (P = 0.003), whereas no significant differences were observed in confidence or skills between the same periods. Proportion of first attempt success was, however, significantly higher during period 3 compared with period 2 for group A (86% vs. 61%, P = 0.016), whereas procedural time remained stable.
Immediate Postintervention Response
Group A scores for knowledge, confidence, skills, and proportion of first attempt success were not statistically different than those for group B immediately after the intervention for each group. Between the immediate preintervention and postintervention periods, group A improved scores for knowledge by 31% and skills by 24% but decreased confidence by 0.5%, whereas group B improved scores for knowledge by 28%, confidence by 16%, and skills by 15%.
Secondary Aims (Clinical Skills, IV Therapy Team Calls, and PIVC Inventory)
Intravenous Start Cards
For the total sample, the average procedural time (in minutes) for inserting a PIVC in the clinical setting was 9.2 for period 1, 10.2 for period 2, and 12.0 for period 3. Proportion of first attempt success ranged from 60% during period 1 to 70% during period 2 to 68% during period 3. No statistically significant differences between the study groups during any of the study periods were observed (P > 0.05).
Intravenous Therapy Support Team Calls
The average number of calls per month to the IV therapy support team during the intervention period and 2 months after (September 2014-February 2015) was compared to the number of calls during the same months in the previous year (September 2013-February 2014). During the study period, there were fewer calls to the IV team compared with those in the previous year (103 vs. 112), although this difference was not statistically significant (P = 0.54).
Peripheral Intravenous Catheter Inventory
No statistically significant difference was observed in the average number of PIVCs ordered on all study units each month for September 2013 to February 2014 ( = 1725) compared with September 2014 to February 2015 (
= 1725) compared with September 2014 to February 2015 ( = 1908, P = 0.546).
= 1908, P = 0.546).
DISCUSSION
Peripheral intravenous catheter insertion remains a fundamental nursing skill that is largely learned during the posteducational period in the clinical setting.3 Rigorous training and reinforcement mechanisms must be instituted in health care organizations to ensure continuous clinical proficiency with this skill.
The current randomized control trial was conducted to evaluate the impact of a simulation-based blended learning program on nurses' PIVC insertion knowledge, confidence, and skills. The blended learning strategy was deliberately selected to meet the needs of various nurses, from new graduates to seasoned nurses, with diverse learning styles. In addition, the use of well-trained skill evaluators promoted the accurate and consistent capture of reliable data for analysis. The intervention was effective and resulted in several statistically significant improvements in knowledge, confidence, and skills both within and between study groups over time. These findings reinforce results of previous studies aimed at evaluating the effectiveness of simulation-based instruction in improving PIVC proficiency, while simultaneously beginning to address some of the methodological limitations of these studies.5,6
Simulation-based learning is used widely to augment clinical rotations for nursing students26 and may also prove beneficial for PIVC insertion. Indeed, some studies have shown lower number of IV insertion attempts per patient and lower patient complication rates as a result of blended learning strategies that incorporate didactic and simulation tools.5,6 However, these studies included limitations that may temper interpretation of findings.
The study population by Lyons and Kasker5 was limited to nurses from one facility who volunteered for the course and were not randomized. In addition, improvements were only observed in the infection prevention and adherence to policy components of the skills checklist used for the study. The only outcome variable measured by Wilfong et al6 was the number of PIVC insertion attempts by study participants in their first patient procedure after training. Insertion success was narrowly defined as “catheter placed properly in vein with a flashback of blood,” and the data collection tool used to report insertion success relied solely on study participants' self-report, as opposed to a more objective data collection process. Moreover, with the exception of Lyons and Kasker5 reporting the interrater reliability of their skills checklist, no validity or reliability of the instruments used in either study was reported. A goal of the present investigation was to improve these promising studies with regard to sampling, instrumentation, and data collection methods and reporting in the simulation-based setting.
Primary Aims
Knowledge
Knowledge of anatomical and physiological aspects of peripheral vascular access is requisite to successful PIVC insertion.2 Retention, retrieval from long-term memory, and application of new knowledge and skills are a complex cognitive process. Therefore, some knowledge decay commonly occurs over time after education.27 Participants in this study showed significant increases in knowledge immediately after completion of the training program. However, knowledge scores significantly decreased upon follow-up in the first group exposed to the intervention between periods 2 and 3, although scores remained higher than at baseline. A similar finding was reported by Lyons and Kasker5 who studied the effect of a blended learning continuing education course on nurses' knowledge, confidence, and skills. This partial decay in knowledge between exposure to the intervention and follow-up could be explained in three ways. First, some of the new knowledge taught might never have been fully encoded or learned after the education. Second, some of the new knowledge might have been learned but could not be easily retrieved. The third and the most likely reason may be interference. Because our study population were experienced practicing nurses, previous PIVC stored knowledge or newly acquired conflicting knowledge between periods 2 and 3 might have interfered with the effective retrieval of the taught PIVC course knowledge by period 3.27 Future research in this emerging area must employ strategies to counteract knowledge decay and ensure that information is retained and translated into clinical practice.
Confidence
Confidence has been identified as an important factor that allows nurses to make appropriate decisions in patient care.28,29 We hypothesized that the study intervention would positively impact participants' confidence. However, we did not observe significant increases in confidence in group A as knowledge and skills improved, whereas the expected improvement in confidence was observed in group B. It may be that a simulated environment can begin to build a nurse's PIVC confidence, but to maximize this confidence, the nurse needs to perform insertions on real patients. Although our unexpected group A finding may be spurious, literature related to nurses' confidence in PIVC insertion remains limited and is an area for continued exploration to determine its relation to actual procedural proficiency.
Skills
The literature is replete with research supporting positive clinical outcomes and decreased complications in patients who have PIVCs placed by expert nurses.8,10,16 Participants in our study showed marked improvements in overall skills upon completing the training program with group A increasing scores by 24% and group B increasing scores by 15%. Moreover, there was a statistically significant improvement in skills in group A upon receiving the training during period 2 compared with group B who had not yet received the training.
Surprisingly, our study found no significant changes in PIVC insertion procedural time or proportion of first attempt success during the simulation. These results are in contrast to Wilfong et al6 who found a statistically significant decrease in number of attempts per patient for nurses who participated in simulation training compared with those who did not but aligned with those of Lyons and Kasker5 who found a nonsignificant improvement in first attempt success in their sample. These conflicting results are likely due to variations in sampling and data collection.
Nevertheless, a notable observation was the fact that proportion of first attempt success remained stable for group A from baseline to period 2, although overall skills scores increased significantly. This finding suggests that total procedural improvement observed in skills in this group was primarily due to improvements in individual procedural steps, such as properly identifying the most suitable vein for access and adequately cleansing the insertion site, but was not reflected in first attempt success. Many of these individual factors hold significant patient safety implications that, if improved, would positively impact common PIVC complications, such as phlebitis or infiltration.30,31 Item level analyses of the skills checklist and longer follow-up times in future studies will need to be performed to confirm this assumption.
It is also important to note that first attempt success was significantly improved between the intervention and follow-up in group A from period 2 to 3 as noted in Table 3. It may be that the simulation experience alone is inadequate to improve skills and that continued practice is necessary to refine and solidify the skill. Similarly, the delay to improved first attempt success might also be explained by interference caused by the pre-existing automatic PIVC procedural habits of the learner. Driscoll27 uses the example of an experienced tennis player learning racquetball to describe the effects of proactive interference. They are both racquet sports, and knowing tennis should help facilitate learning racquetball. However, the automaticity of swinging the tennis racquet with the entire arm will interfere with or delay the new skill of swinging with the wrist. The delay of first attempt success until period 3 for group A might be attributed to this proactive interference.
Secondary Aims
As secondary aims, we attempted to examine the potential impact of the training program on clinical level factors beyond the simulated environment. Similar to the simulation results, there was no significant impact on first attempt success or procedural time in the clinical setting. However, the clinical setting data were self-reported, and although all study participants were instructed to complete IV start cards with each new order, the authors were unable to verify that this information was consistently reported. Because both procedural time and first attempt success are important clinical and patient outcome measures, further investigation of strategies to more rigorously collect and evaluate these outcomes is warranted. In addition, Although there was an overall decrease in the number of calls to the IV therapy support team during the study period, this result failed to reach statistical significance. This finding should also be interpreted with caution as other variables, such as the hiring of new nurses on the units during the study period who did not participate in the study, could have influenced the results.
Limitations
Although this study was designed to build upon previous literature, there were still several limitations present. The study was conducted in a single hospital, which limits generalizability. Although all instruments underwent preliminary validity and reliability testing for this study, additional evaluation in more diverse settings/populations is necessary to further refine them for more general applicability. In addition, although we believe the 4-week window for completion of the online course was an authentic test of the learning intervention in a real-world environment, it could also be viewed as a methodological limitation. A postintervention review of the hospital's Learning Management System course data showed that participants took an average of 14.5 days from the initial assignment launch to successful completion of the course, much less than the 4 weeks allotted. Learning Management System course data also showed that participants, on average, accessed and progressed through the course within four sittings. Although these findings support a blended curricular design that provides busy adult learners with the flexibility required for knowledge acquisition,32,33 knowledge assessment results could have been influenced by the variability in when participants completed the online course, for example, closer to or further from the time of assessment. However, the actual impact of this variability is unknown. In addition, the use of administrative and self-report data for clinical secondary outcomes proved to be unreliable. For example, the PIVC inventory data were not solely reflective of the unit use because it is a common practice for other departments, particularly the IV therapy support team, to disproportionately use supplies on one unit for patients on other units. In addition, audits of IV start cards revealed that most cards were regularly completed by the same individuals, which could bias results and not accurately reveal the effect of the intervention. It is critically important that future research identify more reliable means for collecting clinical level data to substantiate the true impact of educational programs in the clinical setting.
CONCLUSIONS
A blended learning program, which included a combination of online and simulation-based instruction, significantly improved nurses' knowledge, confidence, and skills in the PIVC insertion process in a simulated environment. The results of this study are encouraging and support additional research of this innovative program and its impact on direct patient care at the bedside and, ultimately, PIVC complications.
In this study, the transfer of improved knowledge, confidence, and skills from the simulated to the clinical environment was difficult to measure. An attempt to use proxies such as PIVC performance time, IV team consults, and first attempt success yielded unreliable data and is a limitation of this study that should be addressed in subsequent research.
More proficient PIVC insertion skills have been shown to result in fewer complications and improved patient outcomes.10 This research was a first step in evaluating a comprehensive, simulation-based blended education program to address the significant clinical and financial burdens resulting from less than adequate PIVC knowledge, confidence, and skills of staff nurses. Although the results of this learning intervention are promising, a focus of future studies should be to evaluate whether investment in such training to potentially improve patient outcomes is possible, sustainable, and financially viable for health care organizations.
Footnotes
The authors declare no conflict of interest.
All authors certify that they have no affiliations with or involvement in any organizations or entities with a financial interest beyond their full-time employment at either Overlook Medical Center or B. Braun Medical Inc. Overlook Medical Center fully funded the principal investigator and three coinvestigators who participated in this research. B. Braun Medical Inc fully funded five coinvestigators who participated in this research. Other costs incurred by study sponsor (B. Braun Medical Inc) included institutional review board and administration fees, biostatistical support fees, and partial hourly compensation for the staff nurse participants who completed the study intervention and assessments. B. Braun Medical Inc also supplied the simulation equipment and peripheral intravenous access supplies used throughout the study.
REFERENCES
- 1.Alexandrou E, Ramjan L, Murphy J, Hunt L, Betihavas V, Frost S. Training of undergraduate clinicians in vascular access: an integrative review. Assoc Vasc Assess 2012;17(3):146–160. [Google Scholar]
- 2.Hadaway L. Short peripheral intravenous catheters and infections. J Infus Nurs 2012;35:230–240. [DOI] [PubMed] [Google Scholar]
- 3.Vizcarra C, Cassutt C, Corbitt N, Richardson D, Runde D, Stafford K. Recommendations for improving safety practices with short peripheral catheters. J Infus Nurs 2014;37:121–124. [DOI] [PubMed] [Google Scholar]
- 4.Jensen R. Teaching students about intravenous therapy: increased competence and confidence. JAVA 2009;14:21–26. [Google Scholar]
- 5.Lyons MG, Kasker J. Outcomes of a continuing education course on intravenous catheter insertion for experienced registered nurses. J Contin Educ Nurs 2012;43:177–181. [DOI] [PubMed] [Google Scholar]
- 6.Wilfong DN, Falsetti DJ, McKinnon JL, Daniel LH, Wan QC. The effects of virtual intravenous and patient simulator training compared to the traditional approach of teaching nurses: a research project on peripheral I.V. catheter insertion. J Infus Nurs 2011;34:55–62. [DOI] [PubMed] [Google Scholar]
- 7.Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs 2015;38:189–203. [DOI] [PubMed] [Google Scholar]
- 8.Frey AM. Success rates for peripheral I.V. insertion in a children's hospital. Financial implications. J Intraven Nurs 1998;21:160–165. [PubMed] [Google Scholar]
- 9.Jacobson AF, Winslow EH. Variables influencing intravenous catheter insertion difficulty and failure: an analysis of 339 intravenous catheter insertions. Heart Lung 2005;34:345–359. [DOI] [PubMed] [Google Scholar]
- 10.Palefski SS, Stoddard GJ. The infusion nurse and patient complication rates of peripheral-short catheters. A prospective evaluation. J Intraven Nurs 2001;24:113–123. [PubMed] [Google Scholar]
- 11.Abbas SZ, de Vries TK, Shaw S, Abbas SQ. Use and complications of peripheral vascular catheters: a prospective study. Br J Nurs 2007;16:648 650, 652. [DOI] [PubMed] [Google Scholar]
- 12.Cicolini G, Manzoli L, Simonetti V, et al. Phlebitis risk varies by peripheral venous catheter site and increases after 96 hours: a large multi-centre prospective study. J Adv Nurs 2014;70:2539–2549. [DOI] [PubMed] [Google Scholar]
- 13.Cicolini G, Bonghi AP, Di LL, Di MR. Position of peripheral venous cannulae and the incidence of thrombophlebitis: an observational study. J Adv Nurs 2009;65:1268–1273. [DOI] [PubMed] [Google Scholar]
- 14.Barton AJ, Danek G, Johns P, Coons M. Improving patient outcomes through CQI: vascular access planning. J Nurs Care Qual 1998;13:77–85. [DOI] [PubMed] [Google Scholar]
- 15.Lininger RA. Pediatric peripheral I.V. insertion success rates. Pediatr Nurs 2003;29:351–354. [PubMed] [Google Scholar]
- 16.Gallant P, Schultz AA. Evaluation of a visual infusion phlebitis scale for determining appropriate discontinuation of peripheral intravenous catheters. J Infus Nurs 2006;29:338–345. [DOI] [PubMed] [Google Scholar]
- 17.Scerbo MW, Bliss JP, Schmidt EA, Thompson SN. The efficacy of a medical virtual reality simulator for training phlebotomy. Hum Factors 2006;48:72–84. [DOI] [PubMed] [Google Scholar]
- 18.Reznek MA, Rawn CL, Krummel TM. Evaluation of the educational effectiveness of a virtual reality intravenous insertion simulator. Acad Emerg Med 2002;9:1319–1325. [DOI] [PubMed] [Google Scholar]
- 19.Shadish W, Cook T, Campbell D. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Wadsworth Cengage Learning: Belmont, CA; 2002. [Google Scholar]
- 20.Wayne DB, Butter J, Siddall VJ, et al. Simulation-based training of internal medicine residents in advanced cardiac life support protocols: a randomized trial. Teach Learn Med 2005;17:210–216. [DOI] [PubMed] [Google Scholar]
- 21.Statistical Solutions, LLC. Power Calculator. Available at: http://www.statisticalsolutions.net/pss_calc.php. Accessed September 14, 2013.
- 22.Glover KR, Murray C. Learning by doing in medical device training: the deliberate difficult practice methodology. FOCUS Magazine 2011;21:36–39. [Google Scholar]
- 23.Glover KR. Medical simulation. In: Kapp K, Blair L, Mesch R, eds. The Gamification of Learning and Instruction Field Book: Theory Into Practice. San Francisco, CA: John Wiley and Sons; 2014;371–390. [Google Scholar]
- 24.Schuster C, Stahl B, Murray C, Glover KR. Development and testing of an instrument to measure short peripheral catheter insertion confidence. J Infus Nurs 2016;39:159–165. [DOI] [PubMed] [Google Scholar]
- 25.Infusion Nurses Society. Infusion Nursing Standards of Practice. Available at: http://www.ins1.org/files/public/11_30_11_Standards_of_Practice_2011_Cover_TOC.pdf. Accessed May 18, 2013.
- 26.Hayden JK, Smiley RA, Alexander M, Kardong-Edgren S, Jeffries PR. The NCSBN National Simulation Study: a longitudinal, randomized, controlled study replacing clinical hours with simulation in prelicensure nursing educaiton. J Nurs Regul 2014;5(Suppl 2):S1–S39. [Google Scholar]
- 27.Driscoll MP. Cognitive information processing. In: Psychology of Learning for Instruction. 3rd ed Boston: Pearson Education, Inc.; 2005:71–110. [Google Scholar]
- 28.Sabri A, Szalas J, Holmes KS, Labib L, Mussivand T. Failed attempts and improvement strategies in peripheral intravenous catheterization. Biomed Mater Eng 2013;23:93–108. [DOI] [PubMed] [Google Scholar]
- 29.Hagbaghery MA, Salsali M, Ahmadi F. The factors facilitating and inhibiting effective clinical decision-making in nursing: a qualitative study. BMC Nurs 2004;3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O'Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis 2011;52:e162–e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dychter SS, Gold DA, Carson D, Haller M. Intravenous therapy: a review of complications and economic considerations of peripheral access. J Infus Nurs 2012;35:84–91. [DOI] [PubMed] [Google Scholar]
- 32.Decker S, Sportsman S, Puetz L, Billings L. The evolution of simulation and its contribution to competency. J Contin Educ Nurs 2008;39:74–80. [DOI] [PubMed] [Google Scholar]
- 33.Jeffries PR. Simulation in Nursing Education: From Conceptualization to Evaluation. National League for Nursing: New York, NY; 2007. [Google Scholar]


