Abstract
Objectives:
In January 2014, 4-methylcyclohexanemethanol spilled into the Elk River near Charleston, West Virginia, contaminating the water supply for about 120 000 households. The West Virginia American Water Company (WVAWC) issued a “do not use” water order for 9 counties. After the order was lifted (10 days after the spill), the communities’ use of public water systems, information sources, alternative sources of water, and perceived impact of the spill on households were unclear to public health officials. To assist in recovery efforts, the West Virginia Bureau for Public Health and the Centers for Disease Control and Prevention conducted a Community Assessment for Public Health Emergency Response (CASPER).
Methods:
We used the CASPER 2-stage cluster sampling design to select a representative sample of households to interview, and we conducted interviews in 171 households in April 2014. We used a weighted cluster analysis to generate population estimates in the sampling frame.
Results:
Before the spill, 74.4% of households did not have a 3-day alternative water supply for each household member and pet. Although 83.6% of households obtained an alternative water source within 1 day of the “do not use” order, 37.4% of households reportedly used WVAWC water for any purpose. Nearly 3 months after the spill, 36.1% of households believed that their WVAWC water was safe, and 33.5% reported using their household water for drinking.
Conclusions:
CASPER results identified the need to focus on basic public health messaging and household preparedness efforts. Recommendations included (1) encouraging households to maintain a 3-day emergency water supply, (2) identifying additional alternative sources of water for future emergencies, and (3) increasing community education to address ongoing concerns about water.
Keywords: water, environmental health, disaster
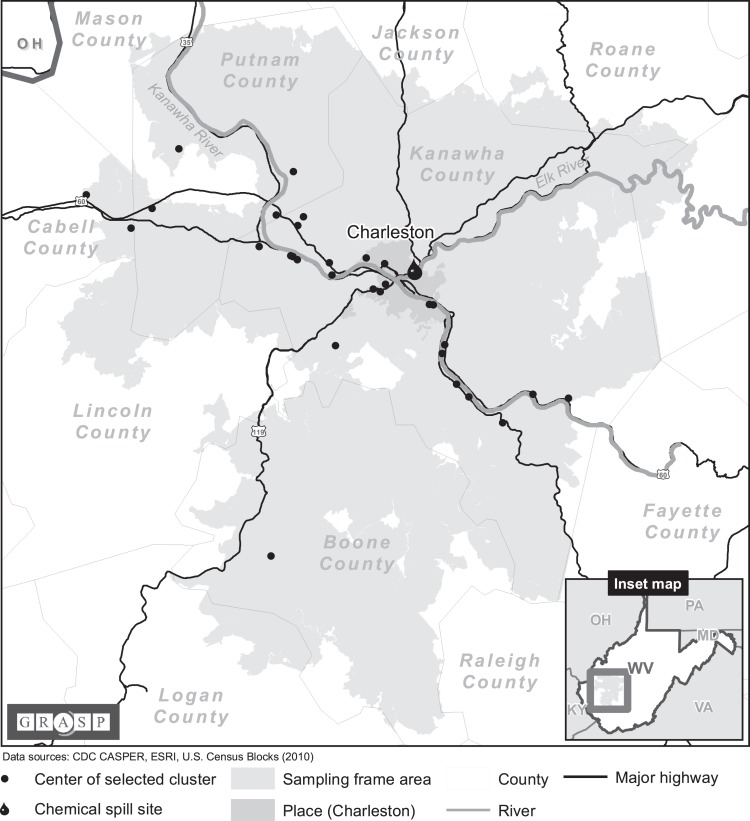
On January 9, 2014, 4-methylcyclohexanemethanol (MCHM) and a mixture of propylene glycol phenyl ethers spilled into the Elk River near Charleston, West Virginia, contaminating the water supply for about 120 000 households in West Virginia (approximately 300 000 people).1 That day, the governor of West Virginia declared a state of emergency, and the West Virginia American Water Company (WVAWC), the primary supplier of public water in the area, issued a “do not use” water order. This order instructed affected residents not to use their municipal water for anything other than flushing toilets or extinguishing fires. The order fully or partially included 9 counties: Boone, Cabell, Clay, Jackson, Kanawha, Lincoln, Logan, Putnam, and Roane (Figure).2 Schools, day care centers, and businesses were forced to close because they could no longer use their public water supply for cooking, cleaning, and drinking.3 A federal emergency was declared on January 10, 2014.4
Figure.
Sampling frame and selected clusters for the Community Assessment for Public Health Emergency Response survey conducted in communities affected by the Elk River chemical spill, West Virginia, April 2014. Abbreviation: CDC, Centers for Disease Control and Prevention.
The main chemical of concern from the spill, MCHM, is an organic compound categorized as a saturated higher alicyclic primary alcohol.5 MCHM is often used as a frothing agent for coal processing.5,6 Because of a dearth of publicly available toxicologic studies of MCHM, the human health effects of MCHM were not well understood at the time of the spill.5,7,8 Additionally, as discovered by research conducted after the spill, MCHM has a licorice-like odor that is detectable by most people at concentrations well below 1 part per million, the concentration established as a screening level for lifting the “do not use” order.3,9
By January 19, 2014, 10 days after the spill occurred, the “do not use” order was lifted for all counties; however, the communities’ use of public water systems, sources of information on the chemical spill, alternative sources of water, and perceived impact of the chemical spill on households were unclear to public health officials. To assist in recovery efforts and improve future responses, the West Virginia Bureau for Public Health (WVBPH) requested assistance in March 2014 from the Centers for Disease Control and Prevention (CDC) to conduct a Community Assessment for Public Health Emergency Response (CASPER) in the communities where the order was issued.
CASPER is a modified version of the World Health Organization’s Rapid Health Assessment. It is an epidemiologic tool designed to provide quick and reliable household-based public health information about communities during any stage of the disaster life cycle: preparedness, response, recovery, and mitigation.10,11 The CASPER sampling methodology is especially useful when a census of the affected population is not possible and when a large number of households needs to be rapidly assessed in a cost- and resource-efficient manner. Information is often collected on demographic characteristics, health status, basic needs, impact of an event, household emergency preparedness (eg, supplies of food and potable water), and public perception. CASPERs provide data that allow public health professionals and emergency managers to accurately prioritize response and recovery interventions and resource distribution.10–12 The goals of this CASPER were to (1) provide WVBPH with information on household water use and practices before, during, and after the “do not use” order; (2) identify sources of information preferred by the public on the chemical spill; and (3) assess the perceived impact of the chemical spill on households to identify effective approaches for current and future events.
Methods
CASPER uses a 2-stage cluster sampling methodology (30 clusters of 7 households each) to collect information at the household level in a way that allows for statistically valid household-level population estimates from the sampling frame.10,12 We selected this CASPER’s sampling frame based on the geographic boundaries of the “do not use” order. The sampling frame contained areas from the 9 affected counties, which included 122 339 housing units based on the 2010 US Census.1
In the first stage of sampling, we selected 30 clusters (census blocks) from the sampling frame based on probability proportional to the number of housing units in the cluster (Figure). Therefore, location of chosen clusters is related to household distribution in the sampling frame. In the second stage, for each cluster, interview teams used systematic random sampling to select 7 households for a targeted goal of 210 interviews.10 Because obtaining sufficient interviews in the short time frame of a CASPER can be difficult, before we began the survey, we decided to continue the systematic random sampling in a cluster until 7 interviews had been obtained, no more households were available in the cluster, or the time allowed for the CASPER had passed. During a 3-day period, teams attempted up to 3 visits to acquire a face-to-face interview at each selected household in a cluster before systematically replacing it with another household in the cluster. If a household refused or was not eligible to participate, that household was also systematically replaced. A selected household was included if a resident of the household aged ≥18 was available during 1 of 3 potential visits and was willing and able to complete a 30-minute interview in English. Households were excluded if a house appeared vacant, the house was inaccessible (eg, “no trespassing” sign, unsafe environment), the resident was not at home during any of the 3 visits, the resident was at home but did not answer, language was a barrier, the only available resident was not eligible to participate (ie, age <18), the resident refused to participate, or the resident declined to finish the interview. This assessment was determined to be exempt from review by the CDC institutional review board.
During April 8-10, 2014, teams conducted a 30-minute interview in English with a resident aged ≥18 in each selected household using a 2-page questionnaire created by WVBPH and CDC. We conducted interviews from 2:00 pm to 7:30 pm EST to ensure that working adults had the opportunity to participate.13 The questionnaire included questions on household demographic characteristics, household water use and practices, sources of information on the chemical spill, preparedness (ie, 3-day alternative potable water supply for each household member and pet, as recommended by the Federal Emergency Management Agency [FEMA]),14 alternative sources of water, perceived health effects related to the chemical spill, and other impacts of the spill. During on-the-ground final preparations for the CASPER, we discovered that some households in the sampling frame were not directly affected by the “do not use” order, because their water was not supplied by WVAWC. We included these households in the survey because they were in the sampling frame and were likely to have experienced effects of the chemical spill. However, for these households, interview teams skipped questions on water use and alternative water sources.
Interview teams provided a copy of the participant consent sheet, which contained contact information for WVBPH and, at WVBPH’s request, provided information about the Substance Abuse and Mental Health Services Administration’s Disaster Distress Helpline and local community behavioral health centers to all potential respondents who were approached. Of the 413 households approached, contact was made at 270 households, and interview teams completed 171 interviews, for an overall completion rate of 81.4% (171 of 210 targeted households). The most common reasons for noninterview of a household were either resident not at home during any of 3 visits (n = 81) or resident refused to participate (n = 86). Of those residents who began the interview, only 2 declined to finish.
We used EpiInfo 7.1.3 to conduct a final weighted cluster analysis.15 The weight for each household was the inverse of the probability that the household would be included in the sample, given the sampling design of choosing 30 clusters from the sampling frame based on probability proportional to the number of housing units in the cluster. We conducted a weighted analysis of the 171 household interviews to generate population estimates for the total number and percentage of affected households in the sampling frame, in the form of a weighted frequency and weighted percentage with a 95% CI for each questionnaire response. This method allowed for a descriptive analysis of the data that was representative of the 122 339 households in the sampling frame and accounted for the survey design.10 For all results, frequencies and percentages were weighted unless otherwise stated.
Results
Most interviewees identified all household members’ race/ethnicity as non-Hispanic white. Most households had at least 1 person aged 18-64, and very few had children aged <2 (Table 1). Additionally, 79.7% (95% CI, 69.6%-89.8%) of households were single-family houses, and 80.6% (95% CI, 70.8%-90.4%) of household respondents owned their homes.
Table 1.
Household demographic characteristics for the Community Assessment for Public Health Emergency Response survey conducted in communities affected by the Elk River chemical spill, West Virginia, April 2014
| Characteristics | Household Frequency (n = 171) | Weighted % (95% CI) |
|---|---|---|
| Sexa,b | ||
| Male | 140 | 84.0 (76.5-91.6) |
| Female | 148 | 87.9 (83.0-92.7) |
| Pregnantc | 8 | 5.2 (1.4-9.0) |
| Age,a,d y | ||
| <2 | 6 | 3.2 (0.3-6.0) |
| 2-17 | 42 | 25.3 (17.0-33.7) |
| 18-64 | 130 | 77.4 (69.4-85.3) |
| ≥65 | 61 | 34.4 (26.3-42.6) |
| Ethnicitya | ||
| Hispanic/Latino | 2 | 1.0 (0.0-2.4) |
| Non-Hispanic/Latino | 169 | 99.0 (97.6-100.0) |
| Racea,e | ||
| American Indian/Alaska Native | 3 | 2.3 (0.0-6.0) |
| Asian | 2 | 1.0 (0.0-3.0) |
| Black | 7 | 4.8 (0.3-9.2) |
| White | 161 | 93.6 (87.2-100.0) |
| Native Hawaiian/other Pacific Islander | 1 | 0.5 (0.0 -1.5) |
| Otherf | 3 | 1.9 (0.0-4.0) |
| Yearly total household income, $g | ||
| <15 000 | 8 | 5.0 (0.9-9.2) |
| 15 000-24 999 | 27 | 15.5 (9.5-21.5) |
| 25 000-49 999 | 43 | 25.9 (17.8-34.0) |
| 50 000-99 999 | 44 | 25.4 (18.0-32.9) |
| 100 000-150 000 | 10 | 5.4 (1.8-9.0) |
| >150 000 | 7 | 4.7 (0.0-9.8) |
| Don’t know | 9 | 5.2 (1.4-9.0) |
| Refused | 23 | 12.9 (6.3-19.5) |
Abbreviation: CI, confidence interval.
aFrequency and weighted percentage of households that reported containing at least 1 person with the characteristic.
bOf households reporting sex of household members (n = 167).
cOf households reporting female household members and pregnancy status (n = 144).
dOf households reporting age of household members (n = 170).
eRespondents could choose >1 answer to account for the race of all residents in a household. Multiracial residents were recorded under the option “other.”
fOther races included biracial black/white (n = 1), Filipino (n = 1), and Arabic (n = 1).
gSum of incomes for all residents within a household.
Before the spill, 74.4% (95% CI, 63.9%-84.9%) of households did not have a 3-day alternative potable water supply for each household member and pet. For the remaining households, 14.1% (95% CI, 7.6%-20.6%) had a 3-day alternative potable water supply for only the people in the household; 9.7% (95% CI, 4.0%-15.4%) had a 3-day alternative potable water supply for people and pets; 1.1% (95% CI, 0.0%-2.6%) did not know if they had a 3-day alternative potable water supply; and the remainder did not respond.
The “do not use” order directly affected approximately 75.0% (95% CI, 58.5%-91.5%) of households. The remaining households did not receive their water from WVAWC and therefore were not directly affected.
When asked about communication methods for the chemical spill, more than half of households first learned about the chemical spill and the “do not use” order via television (chemical spill: 54.3%; 95% CI, 46.7%-61.9%; “do not use” order: 52.5%; 95% CI, 44.6%-60.5%). Most households (58.0%; 95% CI, 49.1%-66.9%) considered television the most reliable source of information about the chemical spill.
Almost every household directly affected by the “do not use” order (97.5%; 95% CI, 94.6%-100.0%) reported trying to obtain alternative sources of potable water. Of these households, 83.6% (95% CI, 77.6%-89.6%) obtained an alternative source of potable water the same day (eg, from a store, distribution site, or friend or relative). For households that were unable to obtain an alternative source of potable water within 1 day, the reasons included the following: stores out of water, lack of transportation, inability to leave work, and distribution sites not found or out of water. Approximately 37.4% (95% CI, 26.7%-48.2%) of households directly affected by the “do not use” order reported using WVAWC water despite the order; the most common uses included nonpotable uses, such as showering, washing hands, and cleaning clothes (Table 2).
Table 2.
Reported water use of households during the January 2014 “do not use” water order, CASPER survey after the Elk River chemical spill, West Virginia, April 2014
| Item | Household Frequency (n = 128)a | Weighted % (95% CI) |
|---|---|---|
| WVAWC water used during “do not use” water orderb | ||
| Yes | 47 | 37.4 (26.7-48.2) |
| No | 79 | 61.9 (51.1-72.7) |
| Don’t know | 1 | 0.7 (0.0-2.0) |
| How water was usedc | ||
| Showered/bathed in waterd | 37 | 80.1 (71.4-88.8) |
| Washed handsd | 22 | 45.9 (28.8-63.0) |
| Washed clothesd | 19 | 37.7 (21.7-53.6) |
| Ran dishwasher/handwashed dishesd | 16 | 32.2 (15.5-48.8) |
| Brushed teethd | 16 | 31.8 (18.9-44.6) |
| Ate or drank food prepared with waterd | 13 | 26.9 (14.3-39.4) |
| Drank the waterd | 13 | 26.6 (14.1-39.0) |
| Gave water to petse | 6 | 19.2 (6.4-32.0) |
| Watered plantsd | 4 | 8.4 (0.0-17.3) |
| WVAWC water used at the time of CASPER survey | ||
| Yes | 126 | 98.3 (95.9-100.0) |
| No | 2 | 1.7 (0.0-4.1) |
| How water was usedc | ||
| Showering/bathingf | 123 | 97.2 (94.0-100.0) |
| Washing clothesf | 121 | 95.4 (90.9-99.9) |
| Hand washingf | 119 | 94.2 (90.1-98.3) |
| Dishwashingf | 115 | 90.6 (84.3-96.8) |
| Brushing teethf | 84 | 66.6 (58.7-74.4) |
| Cookingf | 62 | 50.7 (41.0-60.4) |
| Watering plantsf | 53 | 43.2 (31.1-55.3) |
| Giving water to petsg | 42 | 55.0 (42.6-67.4) |
| Drinkinge | 41 | 33.5 (26.6-40.4) |
Abbreviations: CASPER, Community Assessment for Public Health Emergency Response; CI, confidence interval; WVAWC, West Virginia American Water Company.
aIncludes only households that were directly affected by the “do not use” water order (n = 128).
bOne answer to this question was missing.
cRespondents could choose >1 answer.
dOf households reporting WVAWC water use during the “do not use” order (n = 47).
eOf households reporting WVAWC water use and any pet ownership during the “do not use” order (n = 31).
fOf households reporting WVAWC water use at the time that the questionnaire was administered (n = 126).
gOf households reporting WVAWC water use and any pet ownership at the time that the questionnaire was administered (n = 77).
When asked about perceived health effects related to the chemical spill, an estimated 21.7% (95% CI, 14.4%-28.9%) of households had at least 1 person with self-reported physical health effects (eg, rash, cough, diarrhea, nausea), and 3.5% (95% CI, 0.7%-6.4%) of respondents self-reported that someone in the household had experienced mental health effects (eg, anxiety, stress).
Problems beyond the use of water in their own homes also affected residents. Among all households, 21.2% (95% CI, 13.2%-29.1%) reported having a child who attended a school or day care center that closed because of the chemical spill; almost one-quarter of those residents reported either taking time off work to care for their children (19.2%; 95% CI, 5.1%-33.4%) or paying someone to supervise their children (4.7%; 95% CI, 0.0%-11.4%). Of the 10.3% (95% CI, 6.0%-14.7%) of households that included a business owner, only 4.8% (95% CI, 0.0%-15.3%) reported that the business was ordered to close because of the chemical spill. Of all households, 18.1% responded that ≥1 family members were told not to go to work because of the chemical spill: 11.3% (95% CI, 6.1%-16.4%) received paid leave, and 6.8% (95% CI, 3.6%-10.1%) received unpaid leave (Table 3).
Table 3.
Additional household impacts beyond the use of water at home for the Community Assessment for Public Health Emergency Response survey conducted in communities affected by the Elk River chemical spill, West Virginia, April 2014
| Impact | Household Frequency (n = 171) | Weighted % (95% CI) |
|---|---|---|
| School (K-12) or daycare closeda-c | ||
| Yes | 35 | 21.2 (13.2-29.1) |
| No | 21 | 11.8 (6.2-17.4) |
| Don’t know | 1 | 0.5 (0.0 -1.5) |
| Do not have children | 95 | 56.4 (46.1-66.7) |
| Children do not go to school/daycare | 16 | 9.4 (4.9-13.9) |
| Had to take time off of work to care for childrena,d | ||
| Yes | 7 | 19.2 (5.1-33.4) |
| No, unpaid friend/relative supervised | 14 | 44.6 (22.8-66.5) |
| No, they did not require supervision | 11 | 29.1 (10.8-47.3) |
| No, someone was paid to supervise them | 2 | 4.7 (0.0-11.4) |
| Othere | 1 | 2.4 (0.0-7.4) |
| Told not to come into work because of chemical spilla-c | ||
| Yes, with paid leave | 19 | 11.3 (6.1-16.4) |
| Yes, with unpaid leave | 12 | 6.8 (3.6-10.1) |
| No | 110 | 65.8 (58.0-73.6) |
| Don’t know | 3 | 1.5 (0.0-3.7) |
| Not applicablef | 22 | 12.9 (6.1-19.8) |
| Otherg | 2 | 1.0 (0.0-2.4) |
| Own a businessa,c,h | ||
| Yes | 18 | 10.3 (6.0-14.7) |
| No | 150 | 88.1 (83.7-92.5) |
| Don’t know | 1 | 0.9 (0.0-2.6) |
| Business ordered to closea,i | ||
| Yes | 1 | 4.8 (0.0-15.3) |
| No | 17 | 95.2 (84.7-100.0) |
Abbreviation: CI, confidence interval.
aFrequency and weighted percentage of households that reported containing at least 1 person who experienced the impact.
bMissing, n = 2.
cOne household respondent refused to answer the question.
dOf households indicating “yes” to school or day care closure (n = 35).
eOther reported was “stay-at-home parent.”
fIncludes households with no residents in the workforce. Residents were either unemployed or retired.
gOther reported was “yes, but unsure about leave” (n = 2).
hMissing, n = 1.
iOf households reporting ownership of a business (n = 18).
At the time of the survey in April, almost 3 months after the chemical spill and lifting of the “do not use” order, 98.3% (95% CI, 95.9%-100.0%) of directly affected households were using the household’s WVAWC water for at least 1 purpose; however, only 33.5% (95% CI, 26.6%-40.4%) were using the water for drinking (Table 2). Among directly affected households, 85.6% (95% CI, 79.8%-91.3%) of respondents reported that before the chemical spill, they believed that the water supplied by WVAWC was safe. When asked, “Since the ‘do not use’ order was lifted, do you believe that the WVAWC water supply your household receives is safe?” only 36.1% (95% CI, 27.8%-44.4%) replied “yes.”
Discussion
Although the “do not use” order was lifted 10 days after the spill, the results of the CASPER survey indicate that when the questionnaire was administered, 3 months after the chemical spill, only 33.5% of households were using WVAWC water for drinking, but most used it for daily activities (eg, showering/bathing and washing clothes, dishes, and hands). Although the survey did not determine how many households were drinking WVAWC water before the chemical spill, most households reported that they felt that WVAWC water was safe before the chemical spill. The lingering licorice-like odor—detectable at concentrations of MCHM well below the level used to establish lifting the “do not use” order—and the uncertainty of the human health effects of MCHM might have contributed to the persistent decrease in the perceived safety of the WVAWC water supply.16–20 In previous events, negative experiences with drinking water systems have resulted in loss of trust and an increase in perceived risk posed by the system involved.16,18 Using public messaging to address the community’s water quality concerns could help to strengthen its trust in the municipal water supply.18 Households reported television as the most common and most trusted source of information on the chemical spill; this finding is consistent with findings on previous events in the United States that involved areas where communication infrastructure was not affected.21
Before the spill, 74.4% of households did not have a 3-day alternative potable water supply for each household member and pet. FEMA recommends that households maintain a 3-day potable water supply of 1 gallon (3.8 L) per day for each person and a species- and weight-appropriate amount of water for each pet in the household for drinking and sanitation in the event of an emergency.14 These communities might benefit from increased outreach and education on the basics of personal emergency preparedness.
WVBPH provided numerous water distribution sites at fire departments, churches, and schools, and most households (83.6%) obtained an alternative potable water source within 1 day of the “do not use” order. Conversely, 16.4% of households were not able to obtain, or did not know if they had obtained, an alternative water source the first day that they tried to access one. In future emergencies, especially water contamination events, the number of households that are able to obtain water quickly and efficiently could be increased through additional distribution sites, such as community centers, businesses, and volunteer agencies, as well as delivery of water to homes.
More than one-third of directly affected households reported that they used the water while under the “do not use” order and that their most common uses were nonpotable uses (eg, showering and washing clothes). We did not ask why households used water during the “do not use” order, but potential reasons include household members not receiving the information in a timely manner (either they missed the announcement, or the delivery was not timely) or not fully understanding that inhalation and dermal pathways could lead to possible exposures.22,23 More detailed results and discussion of self-reported health effects are described elsewhere.24
During a water contamination event, households are often affected by problems beyond exposure to water at home (eg, closure of schools, day care centers, hospitals, nursing homes, and businesses). The Elk River chemical spill was no exception: 21.2% of households reported that a child’s school or day care center closed because of the chemical spill, and in almost 20% of these households, an adult had to take time off of work to care for a child. To decrease the disruption and financial impact of emergencies on households, it is important that each household have alternate plans for the care of dependent members. FEMA recommends that all households have an emergency plan. Such plans are especially important for families with children, dependent adults, and those with medical issues or disabilities.25 The 2012 FEMA Personal Preparedness in America report found that, nationally, only 43% of people reported that their household had an emergency plan.26 Increased outreach and education on the basics of personal emergency preparedness might help households address this issue.
Limitations
Our study had several limitations. Considerable publicity surrounded the chemical spill, and the CASPER was conducted 3 months after the spill; these factors might have biased the recall of household experiences. Publicity on the chemical spill could have influenced interviewees’ perception of the spill and events surrounding it, or the 3 months of time between the chemical spill and the interviews could have increased the chance for incorrect recall of events. Additionally, interviews were completed in only 41.4% of all households approached and in 63.3% of approached households where contact was made with an eligible person. Therefore, the representativeness of findings could have been affected if the households that were not available, refused to participate, or were not eligible had substantially different experiences than the households that participated in the CASPER. Also, the replacement of households that were not available, refused to participate, or were not eligible allowed for the potential introduction of selection or self-selection bias, the amount of which is unknown and would require a separate study to be determined. Finally, the precision of estimates was reduced in questions with smaller sample sizes created by stratification, such as estimates of reasons for being without an alternative source of drinking water; only 19 households responded to this question.
Conclusion
CASPERs can provide useful and timely data to help decision makers target resources and messaging throughout the disaster life cycle, including the recovery stage, which was the focus of this assessment.10 CASPERs assess the impact of the emergency, provide information about the impact of public health actions, and identify areas for improvement for future emergencies.10,27,28 This CASPER provided WVBPH with a better understanding of how the Elk River chemical spill affected households and with useful information to improve future responses. Our findings support the following actions: (1) increase outreach and education on personal emergency preparedness to address the low number of households with a 3-day potable water supply for emergency use; (2) create community emergency response plans that designate additional alternative sources of water, such as using community centers, employers, and schools as pickup locations and engaging volunteer agencies for assistance with distribution to increase the number of households that are able to obtain potable water quickly and efficiently; and (3) increase community education via television to alleviate ongoing concerns about the potability of the public water supply.
Acknowledgments
We thank the following people for assistance with the CASPER: students from the West Virginia University School of Public Health and employees from WVBPH who conducted surveys as members of interview teams; Stephanie McLemore, Melissa Scott, and Erica Thomasson (Epidemic Intelligence Service Officer) from WVBPH who assisted with surveys and logistics; the sheriff of Kanawha County, who conducted the safety briefing; Amy Schnall from CDC, who assisted with logistics; Nicole Nakata from CDC, who conducted surveys and assisted with data analysis; Reba Griffith, Kathy Harben, and Caroline Lagoy from CDC, who assisted with communications; and Dana Flanders and David Olson from CDC, who assisted with statistical analysis and interpretation of data.
Authors’ Note: The findings and conclusions in this article are those of the authors and do not necessarily represent the views of CDC.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. US Census Bureau. West Virginia QuickFacts. http://quickfacts.census.gov/qfd/maps/west_virginia_map.html. Accessed October 16, 2015.
- 2. Office of the Governor. Governor Tomblin declares state of emergency in 9 counties. http://www.governor.wv.gov/Pages/State-of-Emergency.aspx. Published January 9, 2014. Accessed October 16, 2015.
- 3. Gallagher DL, Phetxumphou K, Smiley E, Dietrich AM. Tale of two isomers: complexities of human odor perception for cis- and trans-4-methylcyclohexane methanol from the chemical spill in West Virginia. Environ Sci Technol. 2015;49(3):1319–1327. [DOI] [PubMed] [Google Scholar]
- 4. Federal Emergency Management Agency. West Virginia chemical spill (EM-3366). https://www.fema.gov/disaster/3366. Published January 10, 2014. Accessed October 16, 2015.
- 5. Christie RD, Fortin RJ, Gross AE. Process for Coal Flotation Using 4-Methyl Cyclohexane Methanol Frothers. Washington, DC: US Patent and Trademark Office; 1990. [Google Scholar]
- 6. Lan J, Hu M, Gao C, Alshawabkeh A, Gu AZ. Toxicity assessment of 4-methyl-1-cyclohexanemethanol and its metabolites in response to a recent chemical spill in West Virginia, USA. Environ Sci Technol. 2015;49(10):6284–6293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Eastman Chemical Company. Questions and answers regarding Eastman’s assistance in the emergency response to the spill of crude MCHM in Charleston, West Virginia. http://www.eastman.com/literature_center/misc/Q_and_A_West_Virginia_Spill.pdf. Published February 27, 2014. Accessed July 25, 2016.
- 8. Eastman Chemical Company. Material Safety Data Sheet for Crude MCHM, Version 3.1 [revision date, September 15, 2016]. Kingsport, TN: Eastman Chemical Company; 2015. [Google Scholar]
- 9. Centers for Disease Control and Prevention. Summary Report of Short-Term Screening Level Calculation and Analysis of Available Animal Studies for MCHM. Atlanta, GA: Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 10. Centers for Disease Control and Prevention. Community Assessment for Public Health Emergency Response (CASPER). https://www.cdc.gov/nceh/hsb/disaster/casper. Accessed September 16, 2016.
- 11. World Health Organization. Rapid Health Assessment Protocols for Emergencies. Geneva, Switzerland: World Health Organization; 1999. [Google Scholar]
- 12. Malilay J, Flanders WD, Brogan D. A modified cluster-sampling method for post-disaster rapid assessment of needs. Bull World Health Organ. 1996;74(4):399–405. [PMC free article] [PubMed] [Google Scholar]
- 13. Nyaku MK, Wolkin AF, McFadden J, et al. Assessing radiation emergency preparedness planning by using Community Assessment for Public Health Emergency Response (CASPER) methodology. Prehosp Disaster Med. 2014;29(3):262–269. [DOI] [PubMed] [Google Scholar]
- 14. Federal Emergency Management Agency. Water [FEMA mobile app]. http://www.ready.gov/water. Accessed May 8, 2014.
- 15. Centers for Disease Control and Prevention. EpiInfo: Version 7.1.3. Atlanta, GA: Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 16. Ailes E, Budge P, Shankar M, et al. Economic and health impacts associated with a Salmonella typhimurium drinking water outbreak—Alamosa, CO, 2008. PLoS One. 2013;8(3):e57439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dietrich AM. Aesthetic issues for drinking water. J Water Health. 2006;4(suppl 1):11–16. [PubMed] [Google Scholar]
- 18. de Franca Doria M. Factors influencing public perception of drinking water quality. Water Policy. 2010;12(1):1–19. [Google Scholar]
- 19. Jardine CG, Gibson N, Hrudey SE. Detection of odour and health risk perception of drinking water. Water Sci Technol. 1999;40(6):91–98. [Google Scholar]
- 20. Stoto MA, Piltch-Loeb R, Savoia E. The Public Health System Response to the 2014 West Virginia Water Crisis. Boston, MA: Harvard School of Public Health; 2015. [Google Scholar]
- 21. Burger J, Gochfeld M, Jeitner C, Pittfield T, Donio M. Trusted information sources used during and after Superstorm Sandy: TV and radio were used more often than social media. J Toxicol Environ Health A. 2013;76(20):1138–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Beko G, Weschler CJ, Langer S, Callesen M, Toftum J, Clausen G. Children’s phthalate intakes and resultant cumulative exposures estimated from urine compared with estimates from dust ingestion, inhalation and dermal absorption in their homes and daycare centers. PLoS One. 2013;8(4):e62442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Weschler CJ, Beko G, Koch HM, et al. Transdermal uptake of diethyl phthalate and di(n-butyl) phthalate directly from air: experimental verification. Environ Health Perspect. 2015;123(10):928–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Thomasson E, Scharman E, Fechter-Leggett E, et al. Acute health effects after the Elk River chemical spill, West Virginia, January 2014. Public Health Rep. 2017;132(2):196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Federal Emergency Management Agency. Make a plan: emergency communication plan [FEMA mobile app]. http://www.ready.gov/make-a-plan. Accessed May 8, 2014.
- 26. Federal Emergency Management Agency. Personal Preparedness in America: Findings From the 2012 FEMA National Survey. Washington, DC: Federal Emergency Management Agency; 2013. [Google Scholar]
- 27. Choudhary E, Chen TH, Martin C, et al. Public health needs assessments of Tutuila Island, American Samoa, after the 2009 tsunami. Disaster Med Public Health Prep. 2012;6(3):209–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zane DF, Bayleyegn TM, Haywood TL, et al. Community assessment for public health emergency response following Hurricane Ike—Texas, 25-30 September 2008. Prehosp Disaster Med. 2010;25(6):503–510. [DOI] [PubMed] [Google Scholar]