A summer 2015 outbreak of Legionnaires’ disease in New York City called attention to how little is known about this pervasive environmental pathogen, despite an increasing incidence of human disease. Shifting the public health community’s response to Legionnaires’ disease from reactive to proactive will require data, analysis, and action. This commentary uses the occasion of the 2015 New York City outbreak to argue that public health entities need to prioritize research on the ecology of Legionella and its relationship to cooling towers. Our reflection is unrelated to the details of the outbreak investigation, which is reported in this issue of Public Health Reports.1
With 138 cases and 16 deaths, New York City’s cooling tower–related outbreak of Legionnaires’ disease in July 2015 was the largest reported community outbreak in the United States since 1976,1 when Legionnaires’ disease was first recognized in Philadelphia, Pennsylvania.2 In New York City, epidemiologic, environmental, and laboratory investigations implicated a single cooling tower on the roof of a South Bronx hotel as the source. Cooling towers typically provide heat transfer (ie, cooling) to air-conditioning systems and can emit aerosolized water droplets that may contain Legionella and be spread through the air. In response to the outbreak, New York City implemented regulations to reduce and contain Legionnaires’ disease, becoming the first US jurisdiction to adopt such stringent requirements.3
New York City and New York State passed laws almost simultaneously in August 2015 mandating the registration, inspection, and maintenance of cooling towers, among other requirements.3,4 New York City’s law further called for regular water testing, biocide application, and cleaning, among other measures. Both city and state laws required cooling tower owners to develop maintenance and management plans consistent with the recommendations of the American Society of Heating, Refrigerating and Air-Conditioning Engineers standard 188-2015.5 New York City’s law, designed to respond to > 6100 cooling towers, departs from current American Society of Heating, Refrigerating and Air-Conditioning Engineers and Centers for Disease Control and Prevention guidance by requiring, rather than recommending, regular sampling and analysis of cooling tower water, as well as other efforts, in the absence of an outbreak.
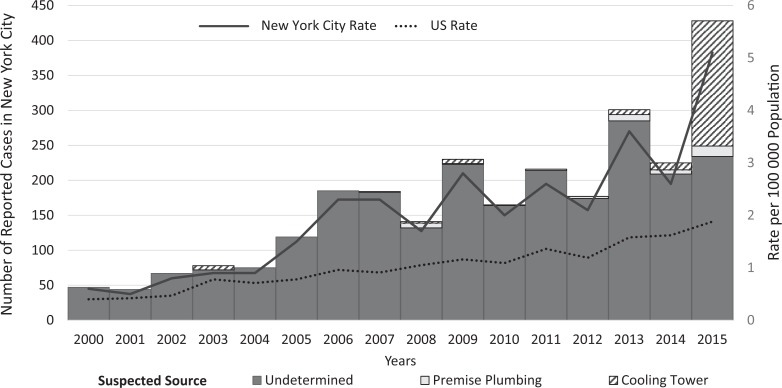
Why were comprehensive regulations needed? Legionnaires’ disease preys on the vulnerable—people who are elderly, who have compromised immune systems, or who have other chronic health conditions. In addition, its incidence is rising dramatically. The number of cases of legionellosis reported to the New York City Department of Health and Mental Hygiene rose from 47 in 2000 to 428 in 2015—a > 9-fold increase6 (Figure).
Figure.
Number and suspected source of reported cases and rates of legionellosis in New York City and the United States, 2000-2015. Data sources: New York City Department of Health and Mental Hygiene6; unpublished data, “Legionellosis 2000-2015,” New York City Bureau of Communicable Disease’s disease surveillance database; and Centers for Disease Control and Prevention.7,8
Regulations similar to those adopted by New York City have been promulgated in Europe since 1992.9 Although the Wisconsin Department of Health Services issued pioneering guidance—but notably not regulations—for treating cooling towers to control Legionella growth in 1987,10 the United States as a whole has been slow to regulate. Instead, the United States has relied on clusters of human illness to trigger cooling tower inspections.
Explosive outbreaks of Legionnaires’ disease attributed to cooling towers have been described in many parts of the world. In Spain, >800 people were sickened in 2001 in the largest documented outbreak presumed related to a cooling tower.11 The source of the initial Philadelphia outbreak was also likely a cooling tower, but it was never identified.2 In the 2015 outbreak of Legionnaires’ disease in New York City, a contaminated cooling tower was the suspected source from the outset. Case patients shared exposure to a common geography but not to a specific building, ornamental fountain, or other environmental source.
Four decades after the first outbreak, the public health community knows surprisingly little about how Legionella infects and kills. Like many illnesses, Legionnaires’ disease follows a socioeconomic gradient, with the highest incidence of disease occurring in neighborhoods of increasing poverty.12 Recognition of an outbreak is often delayed because Legionnaires’ disease has a 2- to 10-day incubation period; historically, outbreaks end before local health departments have sufficient information to intervene. Outbreaks often resolve inexplicably without intervention, as did the original outbreak in Pennsylvania.2 The only approach to improving health is to prevent outbreaks. However, the public health community knows too little about how some cooling towers become contaminated and disperse Legionella in sufficient quantities to cause disease. Legionella can multiply and spread through other water systems (eg, fountains, hot tubs, spas), but most of the largest outbreaks since 1976 have been associated with cooling towers.9,13–16 Factors requiring further exploration include cooling tower design and maintenance, environmental conditions (ie, temperature, humidity), susceptibility of people who live near towers, and virulence of the pathogen.
Legionella is widespread, and its importance as a pathogen may be increasing. The rise in cases is attributed to factors such as better diagnosis, an increasing number of cooling towers, poor maintenance practices, and an aging and increasingly vulnerable population. Potentially fatal outbreaks of Legionnaires’ disease will always grab headlines, but sporadic cases (those not associated with outbreaks) and those for which the environmental source is undetermined are with us all the time and increasing. The public health community does not know what proportion of sporadic cases is linked to cooling towers, and we are concerned that many are, if not most. We hope that the new regulations will result in better cooling tower maintenance, fewer cases of sporadic disease, and reduced outbreak frequency and size. Most jurisdictions with enforceable requirements for maintenance and microbiological testing have not eliminated outbreaks. However, most jurisdictions do not make unannounced independent inspections4 that may include analysis by certified third-party laboratories; New York City does.
A reduction in outbreaks of Legionnaires’ disease linked to cooling towers will not eradicate Legionnaires’ disease; however, rigorous oversight of cooling towers should reduce the risk of contamination. Certainly, no outbreak in New York City will begin again as in 2015, with a search for cooling towers in the outbreak-affected area. The massive cooling tower testing effort underway will offer a window into the ecology of Legionella and its relationship to cooling tower types. If New York City is able to demonstrate control of Legionella in cooling towers, it may also be able to illustrate how poorly maintained cooling towers contribute to rates of Legionnaires’ disease by preventing that fraction of disease.
We hope others in the research community will investigate, analyze, and share how environmental factors contribute to the incidence of Legionnaires’ disease. In densely populated US cities—with their many water systems that rely on complex engineering designs and multifaceted equipment to recirculate water—opportunities for Legionella to thrive will continue. Additionally, many cities are home to worryingly susceptible populations.
We will neither eradicate nor eliminate Legionella as a cause of human disease. However, we can reduce its impact. Outbreaks will occur, but we hope to be better placed to prevent or quickly mitigate them. We also hope to stimulate the issuance of federal funding to facilitate rigorous evaluation of environmental sources of Legionnaires’ disease. Better public health protection depends on more knowledge, not just more regulations.
Acknowledgments
We acknowledge James Hadler, MD, MPH, Daniel Kass, MSPH, and Sarah Perl, MPH, for their contributions to this commentary.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Weiss D, Boyd C, Rakeman JL, et al. A large community outbreak of Legionnaires’ disease associated with a cooling tower in New York City, 2015. Public Health Rep. 2017;132(2):241–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fraser DW, Tsai TR, Orenstein W, et al. Legionnaires’ disease: description of an epidemic of pneumonia. N Engl J Med. 1977;297(22):1189–1197. [DOI] [PubMed] [Google Scholar]
- 3. NYC local law 77 of 2015. NYC Adm Code, title 28, article 317.
- 4. NYS Department of Health Emergency Regulation. Protection against Legionella. NYCRR, title 10, part 4.
- 5. American Society of Heating, Refrigerating, and Air-Conditioning Engineers. Legionellosis: Risk Management for Building Water Systems. Atlanta, GA: American Society of Heating, Refrigerating, and Air-Conditioning Engineers; 2015. Standard 188-2015 (ASNA approved). [Google Scholar]
- 6. New York City Department of Health and Mental Hygiene. Legionellosis 2000-2015. https://a816-healthpsi.nyc.gov/epiquery/CDSS/index.html. Accessed December 16, 2016.
- 7. Centers for Disease Control and Prevention. Summary of notifiable infectious diseases: Legionellosis 2000-2014. https://www.cdc.gov/mmwr/mmwr_nd. Accessed November 25, 2016.
- 8. Centers for Disease Control and Prevention. Notice to readers: final 2015 reports of nationally notifiable infectious diseases and conditions. MMWR Morb Mortal Wkly Rep. 2016;65(46):1306–1321. [DOI] [PubMed] [Google Scholar]
- 9. Ricketts KD, Joseph C, Lee J, Wewalka G; European Working Group for Legionella Infections. Survey on legislation regarding wet cooling systems in European countries. Euro Surveill. 2008;13(38):18982. [PubMed] [Google Scholar]
- 10. Wisconsin Division of Health. Control of Legionella in Cooling Towers: Summary Guidelines. Madison, WI: Wisconsin Department of Health and Social Services; 1987. [Google Scholar]
- 11. García-Fulgueiras A, Navarro C, Fenoll D, et al. Legionnaires’ disease outbreak in Murcia, Spain. Emerg Infect Dis. 2003;9(8):915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Farnham A, Alleyne L, Cimini D, Balter S. Legionnaires’ disease incidence and risk factors, New York, New York, USA, 2002-2011. Emerg Infect Dis. 2014;20(11):1795–1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Greig JE, Carnie JA, Tallis GF, et al. An outbreak of Legionnaires’ disease at the Melbourne Aquarium, April 2000: investigation and case-control studies. Med J Aust. 2004;180(11):566–572. [DOI] [PubMed] [Google Scholar]
- 14. Bennett E, Ashton M, Calvert N, et al. Barrow-in-Furness: a large community legionellosis outbreak in the UK. Epidemiol Infect. 2014;142(8):1763–1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Trudel L, Veillette M, Bonifait L, Duchaine C. Management of the 2012 Legionella crisis in Quebec City: need for a better communication between resources and knowledge transfer. Front Microbiol. 2014;5:182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shivaji T, Sousa Pinto C, San-Bento A, et al. A large community outbreak of Legionnaires’ disease in Vila Franca de Xira, Portugal, October to November 2014. Euro Surveill. 2014;19(50):20991. [DOI] [PubMed] [Google Scholar]