Abstract
Objectives:
On January 9, 2014, approximately 10 000 gallons of a mixture of 4-methylcyclohexanemethanol and propylene glycol phenyl ether spilled into West Virginia’s Elk River, contaminating the potable water supply of about 300 000 West Virginia residents. This study sought to describe acute health effects after the chemical spill.
Methods:
We conducted a descriptive analysis using 3 complementary data sources: (1) medical records of patients who visited an emergency department during January 9-23, 2014, with illness potentially related to the spill; (2) West Virginia Poison Center caller records coded as “contaminated water” during January 9-23, 2014; and (3) answers to household surveys about health effects from a Community Assessment for Public Health Emergency Response (CASPER) questionnaire administered 3 months after the spill.
Results:
In the 2 weeks after the spill, 2000 people called the poison center reporting exposure to contaminated water, and 369 people visited emergency departments in the affected area with reports of exposure and symptoms potentially related to the spill. According to CASPER weighted cluster analyses, an estimated 25 623 households (21.7%; 95% confidence interval [CI], 14.4%-28.9%) had ≥1 person with symptoms who felt that they were related to the spill in the 3 months after it. Reported health effects across all 3 data sources included mild skin, respiratory, and gastrointestinal symptoms that resolved with no or minimal treatment.
Conclusions:
Medical records, poison center data, and CASPER household surveys were inexact but useful data sources to describe overall community health effects after a large-scale chemical spill. Analyzing multiple data sources could inform epidemiologic investigations of similar events.
Keywords: environmental exposures, disasters, water, chemical spill
On January 9, 2014, approximately 10 000 gallons of 4-methylcyclohexanemethanol (MCHM) spilled from an aboveground chemical storage tank into the Elk River in Charleston, West Virginia, contaminating the potable water supply of approximately 300 000 residents. The governor declared a state of emergency and issued a “do not use” water order for 9 counties, and the West Virginia Department of Health and Human Resources Bureau for Public Health (WVBPH) contacted the Centers for Disease Control and Prevention (CDC) / Agency for Toxic Substances and Disease Registry (ATSDR) for assistance. On January 21, the tank owner disclosed that MCHM was not the only contaminant in the water supply. A proprietary mixture of propylene glycol phenyl ether (PPH) represented a relatively small percentage (approximately 7.3% by weight) of the storage tank’s contents that entered the Elk River on January 9.
MCHM is an industrial chemical used in froth flotation, a separation process used to remove impurities from coal. At the time of the spill, toxicologic data on MCHM were limited. A repeated-dose (28-day) oral toxicity study in rats showed effects on the liver, kidney, and red blood cells at the highest dosage; however, human health effects are unknown.1 The predicted health effects of exposure to the lower concentrations of MCHM resulting from the chemical spill were based on the health effects seen in this study in rats and the chemical structure of MCHM (an alicyclic primary alcohol) and included skin, eye, and respiratory tract irritation.1,2 Toxicologic information on PPH was also limited; however, material safety data sheets provided by the manufacturer reported that the toxicity of PPH was likely much lower than that of MCHM. Eye irritation was shown at high-dose repeated exposures.3,4
On January 10, the day after the spill, CDC/ATSDR stated that short-term exposure to levels of MCHM ≤1 ppm was not likely to be associated with any adverse health effects.5 This level was established as a screening level for drinking water below which the “do not use” water order could be lifted. During the first 2 days after the spill, MCHM levels in 44 samples of treated potable water at the West Virginia American Water Company ranged from 0.18 to 3.12 ppm (mean = 0.88, median = 0.76). On January 12, all MCHM levels at the water company were below the recommended drinking water screening level of 1 ppm and were nondetectable thereafter.6 The “do not use” water order began to be lifted on January 13 in areas where sampling showed MCHM levels below the screening level. By January 19, the “do not use” water order was lifted in all counties.
Because MCHM has a high vapor pressure and a noxious licorice-like odor that can be smelled at levels that are one-thousandth the screening level2,7 and although levels of MCHM in this public water system were low, many residents could smell MCHM in their water even after it was declared safe for drinking. CDC/ATSDR recommended a short-term drinking water screening level of 1.2 ppm for PPH5; the highest concentration of PPH detected was 0.01 ppm.8 Given the low levels of PPH detected and the lack of toxicologic information suggesting additional health effects associated with exposure to low levels of PPH, this investigation focused on the acute health effects after exposure to MCHM.
After the chemical spill, the West Virginia Poison Center received calls about exposure and symptoms that callers attributed to the contaminated water, such as vomiting, nausea, rash, and headache. Emergency departments reported hundreds of visits by people reporting exposure to contaminated water. However, the acute health effects after MCHM exposure among these emergency department patients were not well described. Therefore, state and federal epidemiologists at WVBPH and CDC/ATSDR collaborated on an Assessment of Chemical Exposures investigation, which is a rapid epidemiologic assessment after a chemical incident.9,10
We reviewed medical records of people who visited emergency departments in the affected area with reported exposure to the contaminated water to describe acute health effects after the chemical spill. Because the Assessment of Chemical Exposures investigation provided information only for those who sought medical care at emergency departments, we analyzed 2 additional data sources. First, we reviewed poison center caller records to capture data on acute health effects in people who contacted the poison center but did not visit the emergency department. Second, to identify acute health effects among members of households in the affected communities, we included household questions on health effects in the Community Assessment for Public Health Emergency Response (CASPER) conducted in April, 3 months after the spill. A CASPER is a representative cross-sectional survey that produces household-based population estimates.11 By combining these 3 data sources, we provide a multifaceted picture of acute health effects after the chemical spill.
Methods
Assessment of Chemical Exposures Investigation
Ten hospitals in the affected area were required to report to WVBPH the number of people who visited an emergency department and reported MCHM exposure. All 10 emergency departments used case definitions that included patients reporting MCHM exposure; 4 emergency departments included alternative criteria. Among these 4 emergency departments, 3 case definitions included patients who reported certain symptoms but did not mention MCHM exposure, and 1 case definition included any patient who was in the affected area on the day of the chemical spill. We obtained 584 medical records of patients who went to an emergency department during January 9-23, 2014, with illness potentially related to the chemical spill. After a review by epidemiologists from WVBPH and CDC/ATSDR, 215 records were excluded for the following reasons: the patient left without being seen by a physician (n = 41), no exposure was recorded (n = 110), an alternate diagnosis was more likely to have caused the patient’s symptoms (n = 45), the patient reported no symptoms (n = 3), and the patient was previously seen for this same event (n = 16). A total of 369 records from patients who reported MCHM exposure and symptoms remained for analysis. We abstracted data on demographic and clinical characteristics, exposure, diagnostics, and laboratory results.
We reviewed laboratory results from 369 patient records to assess potential effects on red blood cells (ie, erythropoietic effects) and liver and kidney function. To assess potential erythropoietic effects, we analyzed records with laboratory results for platelets (n = 127), hemoglobin (n = 130), and hematocrit (n = 134). To assess liver and kidney function, we analyzed records with laboratory results for blood levels of alanine aminotransferase (n = 99), aspartate aminotransferase (n = 99), alkaline phosphatase (n = 81), total bilirubin (n = 98), and creatinine (n = 132). Because this investigation was not considered research, it was exempt from review by the institutional review boards at WVBPH and CDC/ATSDR.
West Virginia Poison Center
The poison center is a certified regional poison center that takes calls for information about poisons and poisoning management from members of the public and health care professionals from all 55 counties in West Virginia 24 hours per day, 7 days per week. After the chemical spill, the poison center toll-free number was displayed during press conferences and added to brochures and informational websites. The public was encouraged to call the poison center for exposure concerns and to self-refer to the hospital only if serious symptoms were present. Hospitals were required to report to the poison center any person admitted who reported MCHM exposure. Poison center poison specialists created a record for each call reporting potential MCHM exposure; when a single call represented multiple people or animals, a record for each person or animal was created. We collected information on caller location, route of exposure, time of exposure, reported health effects, duration of health effects, therapy received, and health outcome for each record.12 If it was determined during the call that the person was never in the area where contamination occurred, the call was categorized as an informational call. Follow-up calls were made to hospitalized patients (n = 10) and symptomatic people (n = 63) reporting more than minor symptoms or people who expressed extreme concern or worry to ascertain treatment received and outcome.
During January 9-23, 2014, the poison center documented 2574 records coded as “contaminated water”; the chemical spill was the only contamination event that used this code during that time. After records for animals (n = 113) and callers requesting information only (n = 461) were excluded, 2000 records for people with reported MCHM exposure remained for analysis. All reports of records were run from a de-identified database; therefore, the descriptive analysis was determined to be exempt from review by the Charleston Area Medical Center Institutional Review Board.
Community Assessment for Public Health Emergency Response
WVBPH and CDC conducted a CASPER during April 8-10, 2014, using a 2-stage cluster sampling methodology (30 clusters of 7 households each) to select a representative sample of households for interview within a geographic sampling frame. The sampling frame was the area within the 9 counties included in the West Virginia American Water Company’s “do not use” water order boundaries, as described by Burrer and colleagues.11,13
The sample of households was selected for interview from the 122 339 housing units in the sampling frame, based on the 2010 US Census. At a visit to each selected household, we asked residents about symptoms that they felt were related to the chemical spill. We asked the respondent, “Since the chemical spill on January 9, did anyone in your household have any health issues they felt were related to the chemical spill?” If the respondent answered yes, we asked the following questions: “How many people in your household feel they had health issues related to the chemical spill?” “What type of health issues did you or your household members have?” “When did the symptom(s) start?” and “Where was medical care sought?” If household members did not seek medical care, we asked the respondent, “What were reason(s) for not doing so?” Finally, we asked, “Since the chemical spill, has anyone in your household experienced any mental health issues they felt were related to the chemical spill?” If the respondent answered yes, we asked, “What kinds of mental health issues?”
After data collection was completed, we conducted a weighted cluster analysis to calculate the projected number and percentage of households with 95% confidence intervals (CIs) for the sampling frame. We calculated the weight for each household as the total number of housing units (n = 122 339) divided by the product of the number of household interviews completed in a cluster (range, 0-7) and the number of clusters selected (n = 30). In this manner, we generated population-based estimates.
We present the CASPER results based on responses to the aforementioned questions about perceived health issues; additional results of the CASPER are reported by Burrer and colleagues in this issue of Public Health Reports.11
Results
Assessment of Chemical Exposures Investigation
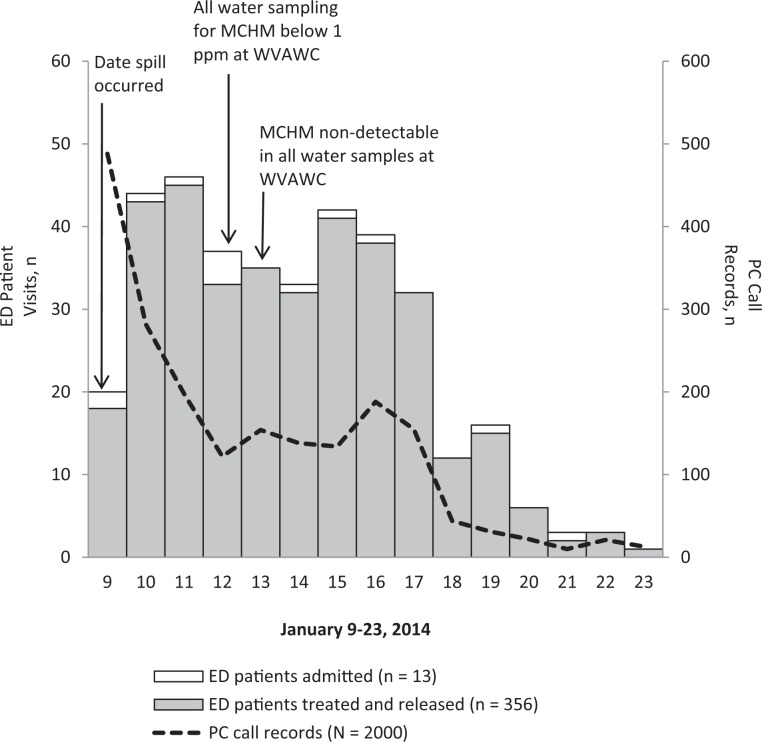
Of 369 patients in the emergency department medical record review, 356 (96%) were treated and released, and 13 (4%) were admitted (Figure). No deaths were reported. The mean patient age was 40 (range, <1-87); 59% (n = 219) were female. Of the 13 admitted patients, 12 had at least 1 underlying chronic condition (range, 1-6); the most frequently reported conditions were diabetes and chronic obstructive pulmonary disease. Reported routes of exposure included direct contact with skin or mucous membranes (53%, n = 194), ingestion (44%, n = 162), and inhalation (15%, n = 54); some patients reported multiple routes of exposure (18%, n = 66). Of the 369 patients in the emergency department medical record review, the most frequently reported symptoms were nausea (n = 140, 38%), rash (n = 105, 28%), vomiting (n = 104, 28%), abdominal pain (n = 90, 24%), and diarrhea (n = 90, 24%; Table 1). For most patients tested, laboratory tests for platelets, hemoglobin, and hematocrit were within the reference range. Laboratory values for liver and kidney function tests were also within reference limits for most patients tested; no new cases of acute kidney or liver injury were diagnosed.
Figure.
Visits to emergency departments and calls to the West Virginia Poison Center related to the Elk River chemical spill, West Virginia, January 9-23, 2014. Samples of treated potable water or finished water refer to water that has completed all treatment processes at a water treatment plant and is ready to be delivered to consumers. Abbreviations: ED, emergency department; MCHM, 4-methylcyclohexanemethanol; PC, poison center; PPM, parts per million; WVAWC, West Virginia American Water Company.
Table 1.
Most common symptoms potentially related to the January 9, 2014, Elk River chemical spill reported by people visiting an emergency department and by people who called the West Virginia Poison Center about exposure to contaminated water, January 9-23, 2014
| Symptoma | Emergency Department Visits (n = 369), No. (%) | Poison Center Records (n = 2000), No. (%) |
|---|---|---|
| Nausea | 140 (38) | 401 (20) |
| Rash | 105 (28) | 303 (15) |
| Vomiting | 104 (28) | 243 (12) |
| Abdominal pain | 90 (24) | 100 (5) |
| Diarrhea | 90 (24) | 249 (12) |
| Headache | 81 (22) | 344 (17) |
| Itching | 73 (20) | 98 (5) |
| Sore throatb | 55 (15) | 93 (5) |
| Eye painc | 54 (15) | 222 (11) |
| Cough | 47 (13) | 57 (3) |
aPatients could report multiple health effects.
bSore throat includes throat irritation and pain.
cEye pain includes eye irritation and pain.
West Virginia Poison Center
Of the 2000 records of people reporting MCHM exposure through calls to the poison center, 61% (n = 1220) were female, 31% (n = 620) were male, and the sex of 8% (n = 160) was not recorded. Age was recorded for 1449 people, and the mean patient age was 37 (range, <1-98). Caller sites, or the locations from which calls were made, for people who were exposed included private residences (97%), health care facilities (2%), worksites (1%), and schools/public areas/other (<1%).
Of the 2000 callers reporting MCHM exposure, the most commonly reported symptoms were nausea (n = 401, 20%), headache (n = 322, 16%), rash (n = 303, 15%), diarrhea (n = 249, 12%), and vomiting (n = 243, 12%; Table 1). Of 2110 reported symptoms, 993 (47%) were gastrointestinal (eg, nausea, vomiting, abdominal pain, diarrhea), and 401 (19%) were skin related (eg, rash, itching). Of the 73 people who received follow-up calls, symptoms resolved with minimal treatment (eg, nonprescription topical hydrocortisone, nonmedicated lotion, fresh air) and did not require medical referral. Ten people were recorded as being admitted to the hospital for underlying medical conditions not related to their reported exposure. These people were admitted after visiting an emergency department, and their information was also captured in the emergency department medical record review.
Community Assessment for Public Health Emergency Response
The CASPER data included 171 household interviews, a representative sample of the 122 339 housing units located in the sampling frame.
Our analysis indicated that an estimated 25 623 households (21.7%; 95% CI, 14.4%-28.9%) had at least 1 person with symptoms in the 3 months after the spill who thought that the symptoms were related to the chemical spill. Of these households, 89.6% (95% CI, 78.7%-100.0%) had affected household members aged ≥18, and 14.9% (95% CI, 3.4%-26.5%) had affected household members aged <18. Self-reported symptoms included rash (53.2%; 95% CI, 32.9%-73.5%), skin irritation/itching (41.6%; 95% CI, 20.6%-62.6%), respiratory illness/cough (16.1%; 95% CI, 2.6%-29.6%), diarrhea (14.8%; 95% CI, 2.0%-27.5%), and nausea (13.1%; 95% CI, 1.5%-24.6%; Table 2).
Table 2.
Symptoms reported by households and attributed to the January 9, 2014, Elk River chemical spill, Community Assessment for Public Health Emergency Response survey, West Virginia, April 8-10, 2014
| Variable | Frequency (n = 171) | Weighted %a (95% CI) |
|---|---|---|
| Respondent reported household members with health issuesb | ||
| Yes | 39 | 21.7 (14.4-28.9) |
| No | 126 | 75.0 (67.5-82.6) |
| Don’t know | 5 | 2.6 (0.0-5.3) |
| Refused | 1 | 0.7 (0.0-2.1) |
| Age of affected household members, yc,d | ||
| <18 | 6 | 14.9 (3.4-26.5) |
| ≥18 | 35 | 89.6 (78.7-100.0) |
| Health issues reportedc,e | ||
| Rash | 21 | 53.2 (32.9-73.5) |
| Skin irritation/itching | 17 | 41.6 (20.6-62.6) |
| Respiratory illness/cough | 6 | 16.1 (2.6-29.6) |
| Diarrhea | 5 | 14.8 (2.0-27.5) |
| Nausea | 5 | 13.1 (1.5-24.6) |
| Sore throat | 4 | 11.2 (0.4-22.0) |
| Headache | 4 | 10.8 (0.6-21.0) |
| Vomiting | 2 | 6.6 (0.0-16.3) |
| Abdominal pain | 2 | 4.9 (0.0-12.2) |
| Eye irritation/pain | 2 | 4.6 (0.0-10.9) |
| Otherf | 9 | 24.3 (11.2-37.3) |
Abbreviation: CI, confidence interval. aA weighted cluster analysis was used to calculate the projected percentage. The weight for each household was calculated as follows: the number of households in the sampling frame (n = 122 339) / (number of household interviews completed in the cluster [range, 0-7] × number of clusters selected [n = 30]).
bSurvey question: “Since the chemical spill on January 9, did anyone in your household have any health problem they felt was related to the chemical spill?” Time frame: date of chemical spill (January 9, 2014) through day of interview (April 8-10, 2014).
cOf 39 households reporting household members with health issues.
dEach household could have ≥1 member in each age group; therefore, there can be more members than households reporting members with health issues (n = 39).
eRespondents could choose >1 answer.
fOther symptoms reported included dizziness (n = 3), dry skin (n = 2), cellulitis (n = 1), “chest on fire” (n = 1), rapid heartbeat (n = 1), and unspecified (n = 1).
When asked where they sought medical care, most respondents indicated that they did not seek it (54.2%; 95% CI, 39.8%-68.6%), with the most common reason being that the health issues were not serious enough (66.8%; 95% CI, 42.2%-91.4%). An estimated 4175 households (3.5%; 95% CI, 0.7%-6.4%) had someone who experienced mental health issues thought to be related to the chemical spill; of those, 83.7% (95% CI, 41.3%-100.0%) mentioned anxiety or stress.
Discussion
At the time of the Elk River chemical spill, toxicologic data on MCHM and PPH were limited, and human health effects were unknown.1 Since then, multiple studies have reported experimental or modeling data on the potential health effects of MCHM or PPH14–16; a few analyses of human data have also been published.17,18 Notably, a yearlong research program conducted by the US National Toxicology Program identified health effects associated with very high levels of MCHM exposure (eg, skin irritation among mice exposed to MCHM doses >100 000 times the screening level for drinking water established by CDC/ATSDR).5,14 Also, because experiments showed reductions in fetal rat weight when pregnant rats were fed high levels of MCHM,14 WVBPH analyzed birth records to evaluate human birth weights in the affected area of the state and did not find evidence for this effect in humans.17
Our study’s examination of varied health outcomes based on 3 data sources involving people from multiple affected counties adds to the existing literature. Similar to previous reports, our investigation found mild health effects reported after low levels of exposure to MCHM and PPH. Beyond advancing an understanding of the human health effects of MCHM and PPH, the Elk River chemical spill led to the 2014 passage of West Virginia’s Aboveground Storage Tank Act and Public Water Supply Protection Act, which were designed to lessen the likelihood of water contamination by chemicals.19,20
Strengths
This study had several strengths. Analyzing data from 3 sources enabled us to more thoroughly describe reported acute symptoms after the chemical spill and provide a more complete representation of the exposed population. The Assessment of Chemical Exposures investigation included medical records from all 10 emergency departments in the counties affected by the “do not use” water order, and the CASPER sampling frame was based on the geographic boundaries of the “do not use” water order, which included areas from all affected counties. Additionally, the poison center captured data on people living in the affected area, as well as those who lived outside the affected area but were present in the affected area at the time of the spill.
Limitations
This study had several limitations. A crucial question centered on the extent to which the reported symptoms were caused by exposure to the spill. All 3 analyses were descriptive and did not quantify exposure; therefore, causation cannot be determined. Because noxious odors can result in physiologic and psychological responses independent of toxicity,21,22 some symptoms reported after the spill might have been related to MCHM’s strong odor. No biological marker or standard clinical case definition for MCHM-related toxicity exists, which made it difficult to distinguish between health effects attributable to MCHM and those attributable to another cause.
Analyses such as those described in this article are meant to give a general idea of the medical effects of events such as this chemical spill, but they are hampered by limitations of the 3 data sources. In our assessment of these data sources, the use of various case definitions complicated the interpretation of cases of MCHM exposure recorded in hospital emergency department medical records. Self-reporting of exposures and symptoms to the poison center and during the CASPER could have been subject to recall bias. Furthermore, weeks of extensive news coverage of possible health effects might have influenced individual reporting of symptoms. The CASPER results represented perceived health effects of households at any time during the 3 months after the spill. These health effects were not assessed by a health care professional, and additional information about the temporal relationship between the spill and perceived health effects reported by households was not collected. Because the CASPER mental health question did not include a list of possible responses (ie, types of mental health issues) for interviewees to choose from, respondents who did not consider stress, difficulty concentrating, or trouble sleeping to be mental health issues might have underreported mental health effects in their household.
Conclusion
The Elk River chemical spill contaminated the public water supply of approximately 300 000 people. Water use was not restored to the entire affected community for 8 days, and the state of emergency lasted 50 days. This incident underscores the importance of protecting public drinking water to preserve human health. When a public water system is compromised, rapid assessments by public health agencies to assess health effects—although inexact and unable to ascertain causality—can be useful for assessing exposure, formulating risk communications, and improving understanding of urgent public health needs.
Acknowledgments
We thank the following people for assistance with this article: Leena Anil, Brett Armstrong, Steve Blankenship, Eric Dotseth, J. D. Douglas, Sarah File, Alana Hudson, Walter Ivey, Miguella Mark-Carew, Shannon McBee, Stephanie McLemore, Anil Nair, Maria del Rosario, Kim Shamblin, Lisa Stamm, Carrie Thomas, Stacy Tressler, and Lori Tyson—West Virginia Bureau for Public Health, West Virginia Department of Health and Human Resources; Tesfaye Bayleyegn, Dana Flanders, Reba Griffith, Caroline Lagoy, Royal Law, Nicole Nakata, Rebecca Noe, David Olson, and Amy Schnall—Division of Environmental Hazards and Health Effects, National Center for Environmental Health, Centers for Disease Control and Prevention; Maureen Miller—Epidemiology Elective Program, Office of Public and Scientific Services, Centers for Disease Control and Prevention; and Kathryn Harben and Christian Scheel—Office of Noncommunicable Diseases, Injury, and Environmental Health, National Center for Environmental Health.
Authors’ Note: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, Agency for Toxic Substances and Disease Registry, or the US Department of Health and Human Services.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. TOXNET Toxicology Data Network. HSDB: 4-methylcyclohexanemethanol. http://toxnet.nlm.nih.gov/cgi-bin/sis/search/r?dbs+hsdb:@term+@DOCNO+8182. Accessed March 3, 2014.
- 2. Eastman Chemical Company. Eastman crude MCHM studies. http://www.eastman.com/Pages/Eastman-Crude-MCHM-Studies.aspx. Accessed August 9, 2014.
- 3. Dow Chemical Company. Material safety data sheet: Dowanol PPH glycol ether. http://blogs.edf.org/health/files/2014/01/Glycol-Ether-2-PPH.pdf. Accessed September 22, 2015.
- 4. Dow Chemical Company. Material safety data sheet: Dowanol DiPPH glycol ether. http://blogs.edf.org/health/files/2014/01/Glycol-Ether-1-DiPPH.pdf. Accessed September 22, 2015.
- 5. Centers for Disease Control and Prevention. Summary report of short-term screening level calculation and analysis of available animal studies for MCHM. https://emergency.cdc.gov/chemical/MCHM/westvirginia2014/pdf/MCHM-Summary-Report.pdf. Published 2014. Accessed August 17, 2014.
- 6. West Virginia Division of Homeland Security and Emergency Management. WVAW operation log as of 18 Jan at 1800. http://www.dhsem.wv.gov/Documents/Sampling%20Results/Operation%20LOG%2018JAN1800%20water.pdf. Published 2014. Accessed July 23, 2014.
- 7. McGuire MJ, Suffet IH, Rosen J. Consumer panel estimates of odor thresholds for crude 4-methylcyclohexanemethanol. J Am Water Works. 2014;106(10):E445–E458. [Google Scholar]
- 8. West Virginia Division of Homeland Security and Emergency Management. PPh/DiPPH operational sampling results. http://www.dhsem.wv.gov/Documents/Sampling%20Results/Copy%20of%20Master%20PPH%20LOG_PUBLIC%207%20February%201030.pdf. Published 2014. Accessed September 12, 2014.
- 9. Agency for Toxic Substances and Disease Registry. Assessment of Chemical Exposures (ACE) program. http://www.atsdr.cdc.gov/ntsip/ace.html. Accessed August 28, 2014.
- 10. Duncan MA. Assessment of chemical exposures: epidemiologic investigations after large-scale chemical releases. J Environ Health. 2014;77(2):36–38. [PubMed] [Google Scholar]
- 11. Burrer SL, Fechter-Leggett E, Bayleyegn T, et al. Assessment of impact and recovery needs in communities affected by the Elk River chemical spill, West Virginia, April 2014. Public Health Rep. 2017;132(2):188–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mowry JB, Spyker DA, Cantilena LR, Jr, Bailey JE, Ford M. 2012 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th annual report. Clin Toxicol (Phila). 2013;51(10):949–1229. [DOI] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention. Community Assessment for Public Health Emergency Response (CASPER) Toolkit. 2nd ed Atlanta, GA: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 14. US National Toxicology Program. NTP research program on chemicals spilled into the Elk River in West Virginia—final update. http://ntp.niehs.nih.gov/ntp/research/areas/wvspill/wv_finalupdate_july2016_508.pdf. Published 2016. Accessed December 19, 2016.
- 15. Paustenbach DJ, Winans B, Novick RM, Green SM. The toxicity of crude 4-methylcyclohexanemethanol (MCHM): review of experimental data and results of predictive models for its constituents and a putative metabolite. Crit Rev Toxicol. 2015;45(suppl 2):1–55. [DOI] [PubMed] [Google Scholar]
- 16. Lan J, Hu M, Gao C, Alshawabkeh A, Gu AZ. Toxicity assessment of 4-methyl-1-cyclohexanemethanol and its metabolites in response to a recent chemical spill in West Virginia, USA. Environ Sci Technol. 2015;49(10):6284–6293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. West Virginia Department of Health and Human Resources Bureau for Public Health. Analysis of birthweight after the January 9, 2014, chemical spill in Charleston, West Virginia. https://wvdhhr.org/mcfh/files/birthweightanalysis.pdf. Published 2016. Accessed December 19, 2016.
- 18. Schade CP, Wright N, Gupta R, Latif DA, Jha A, Robinson J. Self-reported household impacts of large-scale chemical contamination of the public water supply, Charleston, West Virginia, USA. PLoS One. 2015;10(5):e0126744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. West Virginia Legislature. Senate bill no. 373. http://www.legis.state.wv.us/Bill_Status/bills_text.cfm?billdoc=SB373SUB2ENR.htm&yr=2014&sesstype=RS&i=373. Published 2014. Accessed December 19, 2016.
- 20. West Virginia Department of Environmental Protection. Aboveground storage tanks (ASTs). http://www.dep.wv.gov/WWE/abovegroundstoragetanks/Pages/default.aspx. Accessed December 19, 2016.
- 21. Page LA, Keshishian C, Leonardi G, Murray V, Rubin GJ, Wessely S. Frequency and predictors of mass psychogenic illness. Epidemiology. 2010;21(5):744–747. [DOI] [PubMed] [Google Scholar]
- 22. Dalton P. Cognitive influences on health symptoms from acute chemical exposure. Health Psychol. 1999;18(6):579–590. [DOI] [PubMed] [Google Scholar]