Abstract
Gastrointestinal symptoms (GIS) are often among the earliest presenting events in Fabry disease (FD), an X-linked lysosomal disorder caused by the deficiency of α-galactosidase A. Despite recent advances in clinical and molecular characterization of FD, the pathophysiology of the GIS is still poorly understood. To shed light either on differential clinical presentation or on intervariability of GIS in FD, we genotyped 1936 genetic markers across 231 genes that encode for drug-metabolizing enzymes and drug transport proteins in 49 FD patients, using the DMET Plus platform. All nine single nucleotide polymorphisms (SNPs) mapped within four genes showed statistically significant differences in genotype frequencies between FD patients who experienced GIS and patients without GIS: ABCB11 (odd ratio (OR) = 18.07, P = 0,0019; OR = 8.21, P = 0,0083; OR=8.21, P = 0,0083; OR = 8.21, P = 0,0083),SLCO1B1 (OR = 9.23, P = 0,0065; OR = 5.08, P = 0,0289; OR = 8.21, P = 0,0083), NR1I3 (OR = 5.40, P = 0,0191) and ABCC5 (OR = 14.44, P = 0,0060). This is the first study that investigates the relationships between genetic heterogeneity in drug absorption, distribution, metabolism and excretion (ADME) related genes and GIS in FD. Our findings provide a novel genetic variant framework which warrants further investigation for precision medicine in FD.
Keywords: Fabry disease, gastrointestinal symptoms, bile acids, DMET, genetic polymorphisms
INTRODUCTION
Fabry disease (FD [MIM:301500]), or Anderson-Fabry disease, is a rare X-linked lipid storage disorder caused by mutations in the GLA gene (MIM: 300644), encoding the lysosomal enzyme α-galactosidase A (α-Gal A). Deficient activity of α-Gal A leads to a progressive accumulation of neutral glycosphingolipids, predominantly globotriaosylceramide (Gb3), in the vascular endothelium of skin, kidney, nervous system, heart and other tissue with consequent multiorgan dysfunction [1]. In affected males, the clinical presentation of FD varies from a classical phenotype (null or minimal α-Gal A activity), including childhood-onset angiokeratoma, acroparesthesias, gastrointestinal disorders, hypohidrosisand characteristic corneal and lenticular opacities [2, 3] to adult-onset variants (residual α-GalA activity) with only cardiac [4] or renal [5] symptoms. Heterozygous females show a variable phenotype due to random X-inactivation [6]. However, published data showed a high degree of intra-familial phenotypic variability in patients carrying the same mutation [7]. Enzyme replacement therapy (ERT), with agalsidase alfa and agalsidase beta, has been reported to be well tolerated and effective in FD [8–11]. Gastrointestinal symptoms (GIS) are reported in approximately 60% of FD patients and have a profound negative effect on their quality of life. Post-prandial abdominal pain and diarrhea are the most prevalent manifestations, while less common GIS include nausea, vomiting, and early satiety [12]. Despite recent advances in clinical and molecular characterization of FD, the pathophysiology of the GIS is still poorly understood.
Here, we have evaluated the intervariability of GIS recurrence in a cohort of 49 FD patients. In order to determine the involvement of genetic factors unrelated to α-Gal A deficiency in the pathogenesis of GIS, we have performed a profiling of 1936 common and complex functional variants (SNPs, insertions, duplications, deletions) across 231 genes that encode for drug-metabolizing enzymes and drug transport proteins using the DMET Plus platform (Affymetrix, Inc., Santa Clara, CA, US).
RESULTS
Prevalence of gastrointestinal symptoms
The overall prevalence of GIS in the 49 evaluated patients was 24.5% (n = 12). Abdominal pain was present in 12 patients (24.5%) while diarrhea was reported in 11 patients (22.4%). One male patient complained only abdominal pain, all the other patients had more than one GI symptom: ten patients complained abdominal pain and diarrhea, one patient had heartburn, belching and bloating in addition to abdominal pain and diarrhea. The onset of GIS in our patients occurred at a median age of 9.1 years (range: 4–15 years). Ten out of the 12 patients with GIS were under ERT. After a period between 12 and 24 months of ERT, 40% patients (n = 4) reported an improvement in frequency and severity of GIS, while the remaining 60% (n = 6) reported no changes in GI manifestations after starting the treatment. Genotype-phenotype correlation revealed variability in the occurrence of GIS in related individuals carrying the same mutation.
Correlation between genetic polymorphisms and gastrointestinal symptoms
All 49 patients passed QC metrics and produced useable genotypes. The average call rate was more than 95%. One SNP (rs2235033/ABCB1) failed to meet Hardy–Weinberg equilibrium (p < 0.05) and was excluded from further analysis. Of the remaining 1935 SNPs, 1025 SNPs were polymorphic in our population and were used in the association study. Nine SNPs in four genes unrelated to α-Gal A deficiency (NR1I3, ABCC5, ABCB11, SLCO1B1) resulted associated with GIS (Table 1).
Table 1. Genes and SNPs correlating with GIS in FD patients.
| Gene | SNP | Genotype | P-value |
|---|---|---|---|
| NR1I3 | rs2501870 | AG | 0,0191 |
| ABCC5 | rs7636910 | CT | 0,0060 |
| ABCB11 | rs497692 | CT | 0,0083 |
| rs495714 | CT | 0,0019 | |
| rs496550 | CT | 0,0083 | |
| rs473351 | CT | 0,0083 | |
| SLCO1B1 | rs2291075 | CT | 0,0065 |
| rs11045819 | AC | 0,0289 | |
| rs2306283 | AG | 0,0083 |
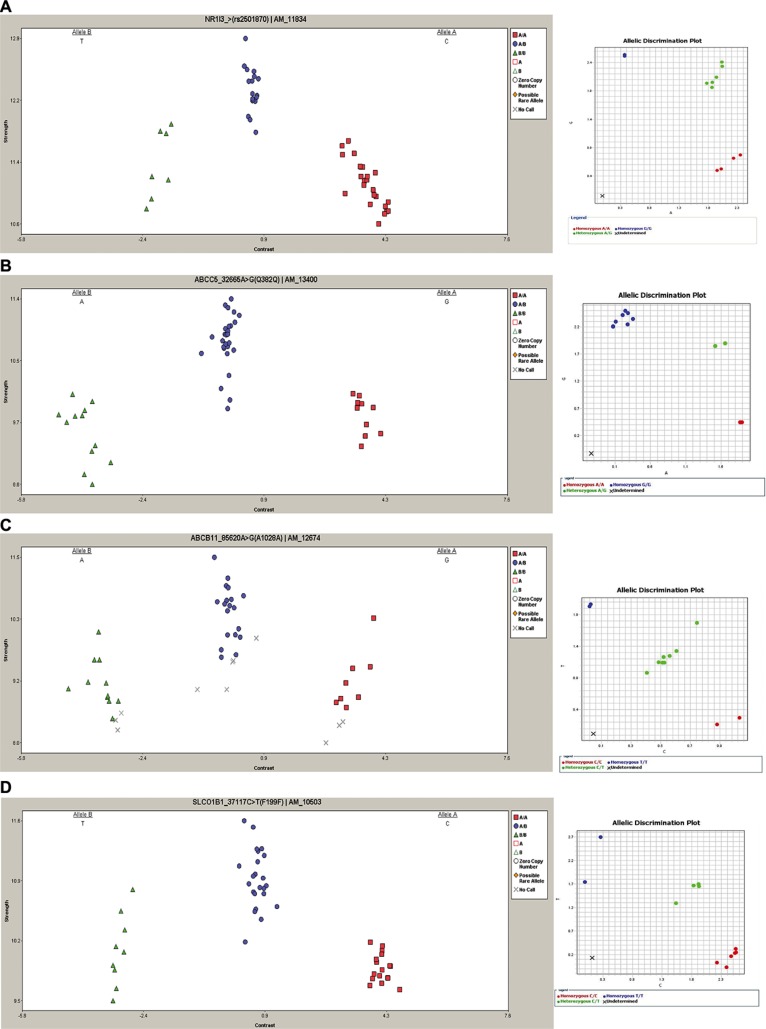
The heterozygous genotype AG (rs2501870) in the NR1I3 gene and the heterozygous genotype CT (rs7636910) in the ABCC5 gene resulted more frequent in patients with GIS compared to patients without GIS (67% versus 27% P = 0.0191, and 92% versus 43% P = 0.0060, respectively) (Table 2). Four ABCB11 polymorphisms (rs497692, rs495714, rs496550, rs473351), in linkage disequilibrium (LD), significantly correlated with GIS, and the frequencies of the heterozygous genotypes CT were significantly higher in FD patients with GIS (CT = 84% versus 38% P = 0.0083, 92% versus 38% P = 0.0019, 84% versus 38% P = 0.0083 and 82% versus 38% P = 0.0083, respectively). In three SLCO1B1 variants (rs2291075, rs11045819, rs2306283) the heterozygous genotypes (CT, AC and AG, respectively) showed statistically differences between the two groups, with higher frequencies in the FD patients with GIS (respectively 84% versus 35% P = 0.0065, 58% versus 22% P = 0.0289 and 84% versus 38% P = 0.0083, respectively), while the homozygous genotypes CC in rs2291075 and rs11045819 were associated with absence of GIS (respectively 43% versus 8% P = 0.0371 and 70% versus 34% P = 0.0392, respectively). These data were completely confirmed by TaqMan SNP Genotyping assays (Figure 1). All genotypes generated are reliable to 100% as we previously demonstrated [13].
Table 2. Polymorphisms associated with GIS in FD patients.
| Genotype number (%) | |||||||
|---|---|---|---|---|---|---|---|
| dsSNP ID* | Gene | Chr | Alleles | Patients with GIS (N=12) | Patients without GIS (N = 37) | P-value | OR (95% C.I.) |
| GG = 4 (33.0) | GG =20 (54.0) | ||||||
| rs2501870 | NR1I3 | 1 | A/G | AG = 8 (67.0) | AG = 10 (27.0) | 0,0191 | 5.4 (1.33 to 21.95) |
| AA = 0 (0.00) | AA = 7 (19.0) | ||||||
| TT = 1 (8.00) | TT=11 (30.0) | ||||||
| rs7636910 | ABCC5 | 3 | C/T | CT =11 (92.0) | CT = 16 (43.0) | 0,0060 | 14.44 (1.69 to 123.69) |
| CC = 0 (0.00) | CC = 10 (27.0) | ||||||
| TT =1 (8.00) | TT = 13 (35.0) | ||||||
| rs497692 | ABCB11 | 2 | C/T | CT = 10 (84.0) | CT = 14 (38.0) | 0,0083 | 8.21 (1.57 to 43.08) |
| CC = 1 (8.00) | CC = 10 (27.0) | ||||||
| TT = 1 (8.00) | TT = 10 (27.0) | ||||||
| rs495714 | ABCB11 | 2 | C/T | CT = 11 (92.0) | CT = 14 (38.0) | 0,0019 | 18.07 (2.10 to 155.49) |
| CC = 0 (0.00) | CC = 13 (35.0) | 0,0215 | 0.073 (0.004 to 1.32) | ||||
| TT = 1 (8.00) | TT = 12 (32.0) | ||||||
| rs496550 | ABCB11 | 2 | C/T | CT =10 (84.0) | CT = 14 (38.0) | 0,0083 | 8.21 (1.57 to 43.08) |
| CC =1 (8.00) | CC = 11 (30.0) | ||||||
| TT = 1 (8.00) | TT = 11 (30.0) | ||||||
| rs473351 | ABCB11 | 2 | C/T | CT =10 (82.0) | CT = 14 (38.0) | 0,0083 | 8.21 (1.57 to 43.08) |
| CC = 1 (8.00) | CC = 12 (32.0) | ||||||
| CC =1(8.00) | CC =16 (43.0) | 0,0371 | 0.12 (0.01 to 1.02) | ||||
| rs2291075 | SLCO1B1 | 12 | C/T | CT = 10 (84.0) | CT = 13 (35.0) | 0,0065 | 9.23 (1.75 to 48.62) |
| TT= 1 (8.00) | TT = 8 (22.0) | ||||||
| CC = 4 (34.0) | CC = 26 (70.0) | 0,0392 | 0.21 (0.05 to 0.85) | ||||
| rs11045819 | SLCO1B1 | 12 | A/C | AC = 7 (58.0) | AC = 8 (22.0) | 0,0289 | 5.08 (1.26 to 20.36) |
| AA = 1 (8.00) | AA = 3 (8.00) | ||||||
| AA = 1 (8.00) | AA = 13 (35.0) | ||||||
| rs2306283 | SLCO1B1 | 12 | A/G | AG = 10 (84.0) | AG = 14 (38.0) | 0,0083 | 8.21 (1.57 to 43.08) |
| GG = 1 (8.00) | GG = 10 (27.0) | ||||||
Figure 1. Representative DMET results and TaqMan SNP validation assay.
Left column: cluster graphs from DMET Console software displaying the signal data of all 49 samples genotyped for rs2501870, NR1I3 (A), rs7636910, ABCC5 (B), rs497692, ABCB11 (C) and rs2291075, SLCO1B1 (D). In rs2501870, rs497692 and rs7636910 alleles are reported in reverse orientation to genome. Right column: representative allelic discrimination plot (right column) generated from ViiA7 Real-Time PCR System software showing allelic symbols for rs2501870 (A), rs7636910 (B), rs497692 (C), rs2291075 (D) evaluation. In the plot the symbol “X” is referred to the No Template Control.
DISCUSSION
The pathophysiology of GIS in FD remains poorly understood although it is plausible that deposition of Gb3 in endothelial intestinal vasculature might cause enteric neuropathy. Moreover, Gb3 also accumulates in intestinal smooth muscle, and a direct myopathic effect, or combined myopathy and neuropathy, has been also suggested [14]. Enteropathy affecting the sympathetic and parasympathetic divisions of the autonomic nervous system is also possible, being autonomic nerve involvement previously reported in FD [15]. The peripheral neuropathy in FD manifests as neuropathic pain, reduced cold and warm sensation and possibly gastrointestinal disturbances [16].
In the present study, we investigated the relationships between genetic variants in ADME-related genes and GIS in FD, genotyping 49 FD patients with the DMET Plus microarray, that we have previously shown to be a powerful tool for the detection of genetic variants in ADME genes related to interindividual variability to drug response and/or toxicity [13, 17–20]. We identified nine SNPs within four genes (NR1I3, ABCC5, ABCB11, SLCO1B1) potentially associated with GIS.
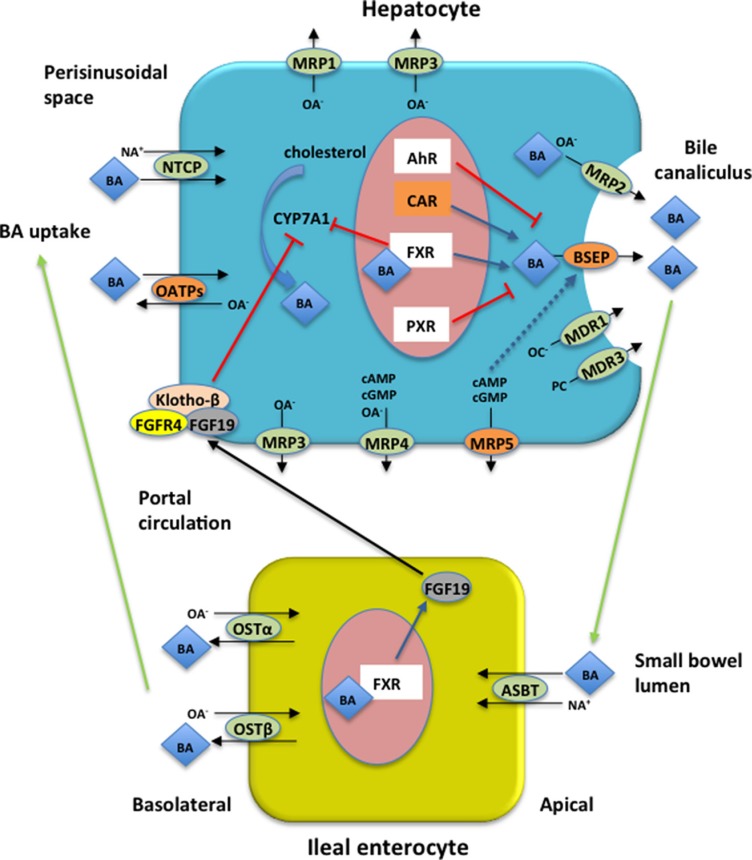
We first found a positive correlation between the heterozygous genotype rs2501870 in the NR1I3 gene and GIS. The NR1I3 gene encodes the constitutive androstane receptor (CAR), which plays an essential and unique role in both controlling the mammalian sulfation pathways and facilitating bile acid (BA) detoxification and transport. The NR1I3 rs2501870 is located in the 5′ region of the gene. Despite the absence of expression and/or function analysis, the presence of this SNP may result in the alteration of mRNA secondary structure, potentially influencing the transcription rate of NR1I3.
We also reported the association of the ABCC5 rs7636910 with GIS. The ABCC5 gene is a member of the ATP-Binding-Cassette family expressed primarily in the colon, liver, kidney and brain, and encodes the MRP5 protein implicated in the transport of cyclic nucleotides, including cAMP and cGMP [21]. The ABCC5 rs7636910 does not change the glutamine at position 324 and so far its role on protein function and expression has not been elucidated. In addition we showed that four variants in ABCB11 gene correlate with GIS. This gene encodes for the bile salt export pump (BSEP), responsible for hepatocyte-canaliculus export of conjugated and unconjugated BAs. Reduced function of BSEP, caused by inherited mutations or acquired factors, may lead to progressive intrahepatic cholestasis and severe liver disease [22]. BSEP expression is regulated by nuclear receptors. The aryl hydrocarbon receptor (AhR) and the pregnance X receptor (PXR) down-regulate BSEP expression while CAR and the farsenoid X receptor (FXR) up-regulate BSEP expression [23]. It also been shown that increased cAMP stimulates BSEP insertion into canalicular membrane [24]. Noteworthy, a previous study showed that ABCB11 overexpression in mice results in BA hypersecretion [25]. The ABCB11 rs497692 results associated with altered transport function, promoting skipping of exon 24 and probably leading to dysfunction of the hepatobiliary bile salt export pump [26]. This SNP was previously associated with primary biliary cirrhosis, intrahepatic cholestasis of pregnancy and benign recurrent intrahepatic cholestasis [27–29]. The other ABCB11 variants (rs495714, rs496550 and rs473351) are located in 3′ region of gene, including exon 28, but no clinical association has been previously reported for these SNPs.
Finally, we found three SNPs (rs2291075, rs2306283, rs11045819) in the SLCO1B1 gene potentially associated with GIS. This gene encodes the organic anion transporting polypeptide1B1 (OATP1B1), a Na+-independent transporter expressed on the basolateral membrane of human hepatocytes that mediates the hepatic uptake of many endogenous compounds and xenobiotics, such as estrogen conjugates, BAs and statins. In vitro studies have shown that the rs2306283 and the rs2291075 are associated with reduced transport activity [30], while the rs11045819 shows unchanged transport function [31]. However, the strong LD between rs2306283 and rs2291075 leads to hypothesize a non-independent effect of the two SNPs. It has been reported that OATP1B1 expression is genotype-dependent and results higher in livers homozygous for rs2306283, rs11045819 and rs2291075. Moreover, livers that are heterozygous for rs11045819 have higher OATP1B1 expression than the wild-type, while the expression of OATP1B1 in livers carrying a single allele of rs2291075 and rs2306283 is not significantly different from the wild-type [32].
Patients with FD quite often report a previous diagnosis of diarrhea-predominant irritable bowel syndrome (IBS), a functional gastrointestinal disorder [33, 34]. In approximately 25% to 50% of the patients with IBS BAs induce diarrhea either through decreased ileal reabsorption or increased hepatic synthesis [35, 36]. The enterohepatic circulation (EC) of BAs is a physiological process mediated by a complex membrane transport system in the liver and intestine, regulated by nuclear receptors [37], as depicted in Figure 2. BAs are synthesized in the liver from cholesterol and are transported into bile ducts in conjugated form. They then accumulate and are stored in the gallbladder where they flow into the duodenum following meal-stimulated gallbladder contraction. After delivery into the intestinal lumen, the vast majority are reabsorbed by the distal ileum into the portal circulation and returned to the liver. A disruption of EC can alter the BA pool with consequent deregulation of the physiological process performed by BAs such as digestion and absorption of nutrient in the gut. The cause of BA diarrhea includes a deficiency in fibroblast growth factor 19 (FGF-19), a hormone produced in enterocytes in response to high intracellular concentration of BAs and that inhibits hepatic BA synthesis through the downregulation of the rate-limiting enzyme cholesterol 7a-hydroxylase (CYP7A1) [38]. However, recent pharmacogenomics evidence suggests that BA transporters are highly polymorphic leading to variable expression and function in humans [39, 40], so other potential causes of BA diarrhea can include genetic variations that affect the proteins involved in BA EC and synthesis. Theoretically, an excessive BA transport through the hepatocyte decreases their intracellular concentration and thus leading to enhanced BA biosynthesis; the increasing BA efflux that exceeds the normal capacity for ileal reabsorption can produce BA diarrhea.
Figure 2. Enterohepatic circulation (EC) of bile acids (BAs) and proteins encoded by the four genes associated with GIS in FD patients.
Major BA transporters in human hepatocytes and enterocytes are shown. Blue arrows indicate up-regulation, red bars indicate down-regulation, while black arrows indicate transport across the cell. Proteins encoded by the four genes reported in the current study associated with GIS are represented in orange boxes. BAs are synthesized in hepatocytes from cholesterol by CYP7A1 which is thought to be the rate limiting step in BA synthesis. BAs active FXR to inhibit CYP7A1 gene transcription. FXR induces intestinal hormone FGF19 which is released in the portal circulation and in the hepatocytes activates FGFR4/Klotho-β signaling inhibiting CYP7A1 activity. In hepatocytes BSEP excretes monovalent BAs in the bile canaliculus while divalent BAs and anionic conjugates are excreted via MRP2. MDR3 mediates secretion of phopholipids while organic cations are excreted via MDR1. Basolateral bile acid export system (MRP1, MRP3, MRP4, MRP5) excretes accumulated biliary constituents. In the terminal ilieum BAs are reabsorbed by ASBT and effluxed on the basolateral site via OSTα/β. BAs are taken up by the hepatocytes via NTCP and OATPs transport systems. BSEP expression is regulated by nuclear receptors (see text for details) and BSEP insertion into canalicular membrane is stimulated by cAMP (blue dashed arrow). AhR = aryl hydrocarbon receptor; ASBT = apical sodium bile salt transporter; BA = bile acid; BSEP = bile salt expert pump; CAR = constitutive androstane receptor; CYP7A1 = cholesterol 7a-hydroxylase; FGF19 = fibroblast growth factor 19; FGFR4 = FGF receptor 4; FXR = farsenoid X receptor; MRP1= multidrug resistance protein 1; MRP2 = multidrug resistance protein 2; MRP3= multidrug resistance protein 3; MRP4 = multidrug resistance protein 4; MRP5 = multidrug resistance protein 5; NA+ = sodium ion; NTCP = Na+-dependent taurocholate cotransport peptide; OATPs = Na+-independent organic anion transport proteins; OA- = organic anions; OC- = organic cations; OSTα/β = organic solute transporter α/β; PC = phosphatidylcholine; PXR = pregnance X receptor.
In this study, we postulate that polymorphisms in NR1I3, ABCC5, ABCB11 and SLCO1B1 are associated with susceptibility to develop GIS in FD through an hypothetic mechanism that affect EC of BAs. However, further well-designed studies need to better investigate this hypothesis including methods for the diagnosis of BA diarrhea.
To our knowledge, this is the first study that uses a pharmacogenomics approach to explore genetic factors potentially involved in clinical manifestations in FD. Even if the effects associated to the identified variants remain to be investigated, our study is a hypothesis-generating early work. Further investigations will be required to better understand the role of these polymorphic variants in the pathogenesis of FD and a validation study in an independent FD patient group will be planned.
MATERIALS AND METHODS
Patients
49 patients (18 males; median age 40.3 years and 31 females; median age 39.4 years) from 18 families were enrolled in this study between December 2012 to April 2015 from the Department of Medical and Surgical Sciences, Pediatric Unit, Magna Graecia University of Catanzaro and from the Department of Nephrology, University Federico II of Naples. All patients were classically affected by FD and the diagnosis was confirmed by enzyme and/or molecular genetic analyses. Among the 49 FD patients, 12 experienced GIS while 37 did not. The mean age at diagnosis among FD patients with GIS was 31 years (range: 4–53), while among FD patients without GIS was 34,9 years (range: 2–60).
Moreover, 37 patients were under ERT at the time of enrolment in the study: 4 received infusions of agalsidase beta every 2 weeks at a dose of 1 mg/kg, while 33 received infusions of agalsidase alfa 0.2 mg/kg every other week, for an average of 5 years and 2 months (range: 11 months −11 years and 4 months). Baseline features of our FD patients and mutations are reported respectively in Table 3 and Table 4.
Table 3. Baseline details of FD patients.
| Total | Male | Female | |
|---|---|---|---|
| Total patients (no.) | 49 | 18 | 31 |
| Age (y; median SD) | 40.3 ± 14.4 | 40.3 ± 10.1 | 39.4 ± 16.2 |
| Under ERT | 37 | 17 | 20 |
| With Agalsidase alfa | 33 | 16 | 17 |
| With Agalsidase beta | 4 | 0 | 4 |
| Gastrointestinal symptoms (GIS) | 12 | 7 | 6 |
| abdominal pain | 12 | 7 | 5 |
| diarrhea | 11 | 7 | 4 |
| other GIS | 1 | 1 | 0 |
Table 4. Mutations and phenotype of FD patients.
| Family | Mutations | phenotype |
|---|---|---|
| 1 | g.7192-7188delCAGCC(GGCTG) | classic |
| 2 | c.515G > A | classic |
| 3 | c.818T > C | classic |
| 4 | c.846_874delTC | classic |
| 5 | c.901C > G | classic |
| 6 | c.424T > C | classic |
| 7 | IVS2-76_80del5 | classic |
| 8 | c.335G > A | classic |
| 9 | c.1184G > C | classic |
| 10 | IVS4+5G > T | classic |
| 11 | c.485G > A | classic |
| 12 | c.1066 C > T | classic |
| 13 | c.901C > T | classic |
| 14 | c.1066 C > T | classic |
| 15 | c.1133C > T | classic |
| 16 | c.67T >G | classic |
| 17 | c.680G > C | classic |
| 18 | c.1021dupG | classic |
Laboratory and medical evaluations were undertaken at baseline to exclude other possible causes of GI complaints. All patients underwent clinical evaluation, laboratory tests such as full blood cell count, inflammatory markers (ESR and CRP), coeliac screening (antitransglutaminase and antiendomysial antibodies) including immunoglobulin levels, liver and kidney biochemical profiles, stool tests for infection (stool culture, examination for ova and parasites and for viral infection), fecal calprotectin, urinalysis and culture; moreover all patient underwent a trial with a lactose-free diet for 2 weeks or breath hydrogen testing for sugar malabsorption. No other cause of GIS was found in our FD patients. Frequency and consistency of GIS for each patient under ERT were evaluated every 2 weeks (at the time of ERT) by interviews and questionnaires as previously validated from our group [41]. Peripheral blood samples were collected from all participants after appropriate informed consent. The study was approved by the institutional review board in accordance with the Recommendation of the Declaration of Helsinki for biomedical research involving human subjects.
DMET genotyping analysis
Genomic DNA was isolated from peripheral blood collected in EDTA tubes, using Perfect Pure DNA Blood kit (5 Prime) accordingly to the manufacturer’s recommendations and quantitated with Quanti-iTTM PicoGreen® dsDNA Assay kit (Invitrogen). All sample concentrations were normalized to 60 ng/μl and 1 μl of each DNA samples was analyzed using DMET plus arrays (Affymetrix Inc., Santa Clara, CA, US) according to the manufacturers’ indication as previously described by Di Martino et al. [17]. Briefly, the DMET Plus assay (Affymetrix Inc., Santa Clara, CA, US) uses Molecular Inversion Probe (MIP) technology to amplify the sequence-specific targets for each 1936 marker. The resulting target DNA were then enzymatic fragmented, labeled and hybridized to the arrays containing allele-specific oligonucleotides. Finally the DMET Plus arrays were scanned with the GeneChip Scanner 3000 (Affymetrix Inc., Santa Clara, CA, US) to obtain the intensity data by CEL files. Genotypes were calculated by DMET Console software version 1.1 using the Dynamic Genotype Boundaries algorithm (Affymetrix Inc., Santa Clara, CA, US). Patients with a call rate less than 95% were excluded from further analysis.
TaqMan® genotyping assay
DMET results were validated using pre-designed TaqMan® Genotyping Assays (Thermo Fisher Scientific) provided in custom fast 96-well plates, according to manufacturer’s instructions. For each patient, we genotyped the following SNPs: rs2501870, rs7636910, rs2291075 and rs497692 (assay ID: C_16033318_20; C_25474215_30; C_1901690_1 and C_8813572_30, respectively). Reactions were performed in duplicate using an endpoint plate read on ViiA7 Real Time PCR System (Applied Biosystem). Thermal Cycling conditions included an initial step of denaturation at 95°C for 10 min followed by 40 cycles at 95°C for 15 sec and 60°C for 1 min. Allelic discrimination was made using the SDS software (Applied Biosystem) that plots Rn values (fluorescence of the reporter dye divided by the fluorescence of a passive reference dye) based on the fluorescence signals from each well.
Statistical analysis
Genotypes for all SNPs were tested for deviation from Hardy-Weinberg equilibrium using a χ2 test and SNPs that were not in equilibrium (P < 0.05) were excluded. By DMET-Analyzer Tool software [42] were analyzed the genotype frequencies by two-tailed Fisher exact test in two groups: FD patients with GIS versus patients without GIS. Results of potential interest were limited to those in which the p-value was ≤ 0.05. Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) were calculated for 2 × 2 table using Med Calc v12.3.0. No correction for multiple comparisons was performed.
Footnotes
CONFLICTS OF INTEREST
The authors declare no conflicts of interest
REFERENCES
- 1.Tuttolomondo A, Pecoraro R, Simonetta I, Miceli S, Pinto A, Licata G. Anderson-Fabry disease: a multiorgan disease. Curr Pharm Des. 2013;19:5974–5996. doi: 10.2174/13816128113199990352. [DOI] [PubMed] [Google Scholar]
- 2.Desnick RG JY, Eng CM. α-Galactosidase A deficiency: Fabry disease. In: Graw-Hill M, editor. The Metabolic and Molecular Bases of Inherited Disease. New York: 2001. pp. 3733–3774. [Google Scholar]
- 3.Sestito S, Ceravolo F, Concolino D. Anderson-Fabry disease in children. Pharm Des. 2013;19:6037–6045. doi: 10.2174/13816128113199990345. [DOI] [PubMed] [Google Scholar]
- 4.Nakao S, Takenaka T, Maeda M, Kodama C, Tanaka A, Tahara M, Yoshida A, Kuriyama M, Hayashibe H, Sakuraba H, et al. An atypical variant of Fabry’s disease in men with left ventricular hypertrophy. N Engl J Med. 1995;333:288–293. doi: 10.1056/NEJM199508033330504. [DOI] [PubMed] [Google Scholar]
- 5.Nakao S, Kodama C, Takenaka T, Tanaka A, Yasumoto Y, Yoshida A, Kanzaki T, Enriquez AL, Eng CM, Tanaka H, Tei C, Desnick RJ. Fabry disease: detection of undiagnosed hemodialysis patients and identification of a “renal variant” phenotype. Kidney Int. 2003;64:801–807. doi: 10.1046/j.1523-1755.2003.00160.x. [DOI] [PubMed] [Google Scholar]
- 6.MacDermot KD, Holmes A, Miners AH. Anderson-Fabry disease: clinical manifestations and impact of disease in a cohort of 60 obligate carrier females. J Med Genet. 2001;38:769–775. doi: 10.1136/jmg.38.11.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rigoldi M, Concolino D, Morrone A, Pieruzzi F, Ravaglia R, Furlan F, Santus F, Strisciuglio P, Torti G, Parini R. Intrafamilial phenotypic variability in four families with Anderson-Fabry disease. Clin Genet. 2014;86:258–263. doi: 10.1111/cge.12261. [DOI] [PubMed] [Google Scholar]
- 8.Pisani A, Visciano B, Roux GD, Sabbatini M, Porto C, Parenti G, Imbriaco M. Enzyme replacement therapy in patients with Fabry disease: state of the art and review of the literature. Mol Genet Metab. 2012;107:267–275. doi: 10.1016/j.ymgme.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Schiffmann R, Kopp JB, Austin HA, Sabnis S, 3rd, Moore DF, Weibel T, Balow JE, Brady RO. Enzyme replacement therapy in Fabry disease: a randomized controlled trial. JAMA. 2001;285:2743–2749. doi: 10.1001/jama.285.21.2743. [DOI] [PubMed] [Google Scholar]
- 10.Eng CM, Guffon N, Wilcox WR, Germain DP, Lee P, Waldek S, Caplan L, Linthorst GE, Desnick RJ. Safety and efficacy of recombinant human alpha-galactosidase A—replacement therapy in Fabry’s disease. International Collaborative Fabry Disease Study G. N Engl J Med. 2001;345:9–16. doi: 10.1056/NEJM200107053450102. [DOI] [PubMed] [Google Scholar]
- 11.Parini R, Rigoldi M, Santus F, Furlan F, De_Lorenzo P, Valsecchi G, Concolino D, Strisciuglio P, Feriozzi S, Di_Vito R, Ravaglia R, Ricci R, Morrone A. Enzyme replacement therapy with agalsidase alfa in a cohort of Italian patients with Anderson-Fabry disease: testing the effects with the Mainz Severity Score Index. Clin Genet. 2008;74:260–266. doi: 10.1111/j.1399-0004.2008.01012.x. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann B, Schwarz M, Mehta A, Keshav S. Fabry Outcome Survey European I. Gastrointestinal symptoms in 342 patients with Fabry disease: prevalence and response to enzyme replacement therapy. Clin Gastroenterol Hepatol. 2007;5:1447–1453. doi: 10.1016/j.cgh.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 13.Di_Martino MT, Arbitrio M, Guzzi PH, Leone E, Baudi F, Piro E, Prantera T, Cucinotto I, Calimeri T, Rossi M, Veltri P, Cannataro M, Tagliaferri P, et al. A peroxisome proliferator-activated receptor gamma (PPARG) polymorphism is associated with zoledronic acid-related osteonecrosis of the jaw in multiple myeloma patients: analysis by DMET microarray profiling. Br J Haematol. 2011;154:529–533. doi: 10.1111/j.1365-2141.2011.08622.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jack CI, Morris AI, Nasmyth DG, Carroll N. Colonic involvement in Fabry’s disease. Postgrad Med J. 1991;67:584–585. doi: 10.1136/pgmj.67.788.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dutsch M, Marthol H, Stemper B, Brys M, Haendl T, Hilz MJ. Small fiber dysfunction predominates in Fabry neuropathy. J Clin Neurophysiol. 2002;19:575–586. doi: 10.1097/00004691-200212000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Tuttolomondo A, Pecoraro R, Simonetta I, Miceli S, Arnao V, Licata G, Pinto A. Neurological complications of Anderson-Fabry disease. Curr Pharm Des. 2013;19:6014–6030. doi: 10.2174/13816128113199990387. [DOI] [PubMed] [Google Scholar]
- 17.Di_Martino MT, Arbitrio M, Leone E, Guzzi PH, Rotundo MS, Ciliberto D, Tomaino V, Fabiani F, Talarico D, Sperlongano P, Doldo P, Cannataro M, Caraglia M, et al. Single nucleotide polymorphisms of ABCC5 and ABCG1 transporter genes correlate to irinotecan-associated gastrointestinal toxicity in colorectal cancer patients: a DMET microarray profiling study. Biol Ther. 2011;12:780–787. doi: 10.4161/cbt.12.9.17781. [DOI] [PubMed] [Google Scholar]
- 18.Arbitrio M, Di_Martino MT, Barbieri V, Agapito G, Guzzi PH, Botta C, Iuliano E, Scionti F, Altomare E, Codispoti S, Conforti S, Cannataro M, Tassone P, et al. Identification of polymorphic variants associated with erlotinib-related skin toxicity in advanced non-small cell lung cancer patients by DMET microarray analysis. Cancer Chemother Pharmacol. 2015 doi: 10.1007/s00280-015-2916-3. [DOI] [PubMed] [Google Scholar]
- 19.Arbitrio M, Di_Martino MT, Scionti F, Agapito G, Guzzi PH, Cannataro M, Tassone P, Tagliaferri P. DMETTM (Drug Metabolism Enzymes and Transporters): a Pharmacogenomic platform for precision medicine. Oncotarget. 2016;7:54028–54050. doi: 10.18632/oncotarget.9927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agapito G, Botta C, Guzzi PH, Arbitrio M, Di_Martino MT, Tassone P, Tagliaferri P, Cannataro M. OSAnalyzer: A Bioinformatics Tool for the Analysis of Gene Polymorphisms Enriched with Clinical Outcomes. Microarrays. 2016:5. doi: 10.3390/microarrays5040024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jedlitschky G, Burchell B, Keppler D. The multidrug resistance protein 5 functions as an ATP-dependent export pump for cyclic nucleotides. J Biol Chem. 2000;275:30069–30074. doi: 10.1074/jbc.M005463200. [DOI] [PubMed] [Google Scholar]
- 22.Strautnieks SS, Bull LN, Knisely AS, Kocoshis SA, Dahl N, Arnell H, Sokal E, Dahan K, Childs S, Ling V, Tanner MS, Kagalwalla AF, Nemeth A, et al. A gene encoding a liver-specific ABC transporter is mutated in progressive familial intrahepatic cholestasis. Nat Genet. 1998;20:233–238. doi: 10.1038/3034. [DOI] [PubMed] [Google Scholar]
- 23.Claudel T, Zollner G, Wagner M, Trauner M. Role of nuclear receptors for bile acid metabolism, bile secretion, cholestasis, and gallstone disease. Biochim Biophys Acta. 2011;1812:867–878. doi: 10.1016/j.bbadis.2010.12.021. [DOI] [PubMed] [Google Scholar]
- 24.Suchy FJ, Ananthanarayanan M. Bile salt excretory pump: biology and pathobiology. J Pediatr Gastroenterol Nutr. 2006;43:S10–16. doi: 10.1097/01.mpg.0000226385.71859.5f. [DOI] [PubMed] [Google Scholar]
- 25.Figge A, Lammert F, Paigen B, Henkel A, Matern S, Korstanje R, Shneider BL, Chen F, Stoltenberg E, Spatz K, Hoda F, Cohen DE, Green RM. Hepatic overexpression of murine Abcb11 increases hepatobiliary lipid secretion and reduces hepatic steatosis. J Biol Chem. 2004;279:2790–2799. doi: 10.1074/jbc.M307363200. [DOI] [PubMed] [Google Scholar]
- 26.Byrne JA, Strautnieks SS, Ihrke G, Pagani F, Knisely AS, Linton KJ, Mieli-Vergani G, Thompson RJ. Missense mutations and single nucleotide polymorphisms in ABCB11 impair bile salt export pump processing and function or disrupt pre-messenger RNA splicing. Hepatology. 2009;49:553–567. doi: 10.1002/hep.22683. [DOI] [PubMed] [Google Scholar]
- 27.Keitel V, Vogt C, Haussinger D, Kubitz R. Combined mutations of canalicular transporter proteins cause severe intrahepatic cholestasis of pregnancy. Gastroenterology. 2006;131:624–629. doi: 10.1053/j.gastro.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 28.Kubitz R, Keitel V, Scheuring S, Kohrer K, Haussinger D. Benign recurrent intrahepatic cholestasis associated with mutations of the bile salt export pump. J Clin Gastroenterol. 2006;40:171–175. doi: 10.1097/01.mcg.0000196406.15110.60. [DOI] [PubMed] [Google Scholar]
- 29.Lang C, Meier Y, Stieger B, Beuers U, Lang T, Kerb R, Kullak-Ublick GA, Meier PJ, Pauli-Magnus C. Mutations and polymorphisms in the bile salt export pump and the multidrug resistance protein 3 associated with drug-induced liver injury. Pharmacogenet Genomics. 2007;17:47–60. doi: 10.1097/01.fpc.0000230418.28091.76. [DOI] [PubMed] [Google Scholar]
- 30.Pasanen MK, Miettinen TA, Gylling H, Neuvonen PJ, Niemi M. Polymorphism of the hepatic influx transporter organic anion transporting polypeptide 1B1 is associated with increased cholesterol synthesis rate. Pharmacogenet Genomics. 2008;18:921–926. doi: 10.1097/FPC.0b013e32830c1b5f. [DOI] [PubMed] [Google Scholar]
- 31.Tirona RG, Leake BF, Merino G, Kim RB. Polymorphisms in OATP-C: identification of multiple allelic variants associated with altered transport activity among European- and African-Americans. J Biol Chem. 2001;276:35669–35675. doi: 10.1074/jbc.M103792200. [DOI] [PubMed] [Google Scholar]
- 32.Prasad B, Evers R, Gupta A, Hop CE, Salphati L, Shukla S, Ambudkar SV, Unadkat JD. Interindividual variability in hepatic organic anion-transporting polypeptides and P-glycoprotein (ABCB1) protein expression: quantification by liquid chromatography tandem mass spectroscopy and influence of genotype, age, and sex. Drug Metab Dispos. 2014;42:78–88. doi: 10.1124/dmd.113.053819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Giannetti E, de’Angelis G, Turco R, Campanozzi A, Pensabene L, Salvatore S, de_Seta F, Staiano A. Subtypes of irritable bowel syndrome in children: prevalence at diagnosis and at follow-up. J Pediatr. 2014;164:1099–1103. doi: 10.1016/j.jpeds.2013.12.043. e1091. [DOI] [PubMed] [Google Scholar]
- 34.Boccia G, Manguso F, Coccorullo P, Masi P, Pensabene L, Staiano A. Functional defecation disorders in children: PACCT criteria versus Rome II criteria. J Pediatr. 2007;151:394–398. doi: 10.1016/j.jpeds.2007.04.011. 398 e391. [DOI] [PubMed] [Google Scholar]
- 35.Wong BS, Camilleri M, Carlson P, McKinzie S, Busciglio I, Bondar O, Dyer RB, Lamsam J, Zinsmeister AR. Increased bile acid biosynthesis is associated with irritable bowel syndrome with diarrhea. Clinical gastroenterology and hepatology Clin Gastroenterol Hepatol. 2012;10:1009–1015. doi: 10.1016/j.cgh.2012.05.006. e1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Camilleri M. Bile Acid diarrhea: prevalence, pathogenesis, and therapy. Gut Liver. 2015;9:332–339. doi: 10.5009/gnl14397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dawson PA, Lan T, Rao A. Bile acid transporters. J Lipid Res. 2009;50:2340–2357. doi: 10.1194/jlr.R900012-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Camilleri M. Dissecting Molecular Mechanisms in Bile Acid Diarrhea. Am J Gastroenterol. 2016;111:433–435. doi: 10.1038/ajg.2016.23. [DOI] [PubMed] [Google Scholar]
- 39.Urquhart BL, Tirona RG, Kim RB. Nuclear receptors and the regulation of drug-metabolizing enzymes and drug transporters: implications for interindividual variability in response to drugs. J Clin Pharmacol. 2007;47:566–578. doi: 10.1177/0091270007299930. [DOI] [PubMed] [Google Scholar]
- 40.Kosters A, Karpen SJ. Bile acid transporters in health and disease. Xenobiotica. 2008;38:1043–1071. doi: 10.1080/00498250802040584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pensabene L. SS, Nicoletti A. Gastrointestinal symptoms of patients with Fabry disease. Gastroenterol Res Pract. 2015 doi: 10.1155/2016/9712831. Article ID 125957, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guzzi PH, Agapito G, Di_Martino MT, Arbitrio M, Tassone P, Tagliaferri P, Cannataro M. DMET-analyzer: automatic analysis of Affymetrix DMET data. BMC bioinformatics. 2012;13:258. doi: 10.1186/1471-2105-13-258. [DOI] [PMC free article] [PubMed] [Google Scholar]