ABSTRACT
Transmissible spongiform encephalopathies (TSEs) are caused by an infectious agent that is thought to consist of only misfolded and aggregated prion protein (PrP). Unlike conventional micro-organisms, the agent spreads and propagates by binding to and converting normal host PrP into the abnormal conformer, increasing the infectious titre. Synthetic prions, composed of refolded fibrillar forms of recombinant PrP (rec-PrP) have been generated to address whether PrP aggregates alone are indeed infectious prions. In several reports, the development of TSE disease has been described following inoculation and passage of rec-PrP fibrils in transgenic mice and hamsters. However in studies described here we show that inoculation of rec-PrP fibrils does not always cause clinical TSE disease or increased infectious titre, but can seed the formation of PrP amyloid plaques in PrP-P101L knock-in transgenic mice (101LL). These data are reminiscent of the “prion-like” spread of misfolded protein in other models of neurodegenerative disease following inoculation of transgenic mice with pre-formed amyloid seeds. Protein misfolding, even when the protein is PrP, does not inevitably lead to the development of an infectious TSE disease. It is possible that most in vivo and in vitro produced misfolded PrP is not infectious and that only a specific subpopulation is associated with infectivity and neurotoxicity.
KEYWORDS: amyloid, prion, prion-like, synthetic prions, TSE
NATURE OF THE TSE INFECTIOUS AGENT
TSEs (or prion diseases) are a unique group of neurodegenerative diseases, including scrapie in sheep, chronic wasting disease in deer, bovine spongiform encephalopathy in cattle and Creutzfeldt Jakob disease in humans. Unlike other neurodegenerative diseases, TSEs are infectious, and can be spread directly between animals in the field, or indirectly by oral, intravenous and peripheral routes of exposure. The infectious agent responsible for TSE is unlike any conventional micro-organism, and has been named a “prion”.1 It is thought to be composed solely of a misfolded and aggregated conformer of the host encoded glycoprotein PrP (prion protein). The Prion Hypothesis predicts that this abnormal conformer (PrPSc) propagates by binding to and converting normal cellular PrP (PrPC) into the abnormal conformer, increasing the infectious titre.2 Deposition of PrPSc in the form of diffuse aggregates or amyloid plaques can be identified in infected tissues by immunohistochemical analyses of infected brain, spinal cord, spleen or lymph node. Following incubation of tissue homogenates with proteinase K (PK), PrPC is totally digested, but PrPSc is only partially digested leaving a PK resistant core of 27–30kDa (PrP 27–30, or PrP-res), and can therefore be identified by immunoblot. PrP-res is thought to be the transmissible agent that causes clinical TSE, however some studies have indicated that there are both PK-resistant and PK-sensitive forms of PrPSc which may be associated with TSE infectivity.3 In this manuscript we use the term “PrPSc” to encompass all abnormal forms of PrP that are associated with TSE disease, and “PrP-res” to specifically refer to PK-resistant PrP. Due to the current use of the term “prion” (discussed later) we also use the term “TSE” to specifically describe cases of infectious transmissible spongiform encephalopathy, and “prion” as a more general term for templated protein misfolding.
Early studies showed a correlation between the presence of PrPSc and infectivity in hamster brain tissue.4 However, subsequent studies in our laboratory and by others have shown that in several cases of disease there is a dissociation between levels of PrPSc and TSE infectivity,5,6 questioning the true nature of the infectious agent. In our laboratory we have been studying the nature of TSE infections associated with the P102L mutation in human PrP (P101L in mice) which is linked with the development of the human familial TSE, Gerstman-Sträussler-Scheinker disease (GSS). P102L GSS is thought to arise spontaneously in humans due to the presence of the mutation and is not associated with an exogenous infectious agent. The disease in humans also presents with two different phenotypes, both linked with the same P102L mutation and codon 129 genotype (129M).7 Classical P102L GSS displays PrP deposition, spongiform degeneration and PrP-res with all three glycoforms by immunoblotting. Atypical P102L GSS shows more restricted pathology, with no spongiform degeneration, PrP deposition mainly in the form of amyloid plaques, and often following PK digestion, only an 8kDa PrP fragment can be identified by immunoblotting. Tissues from P102L GSS cases have also been difficult to transmit in animal models, questioning whether infectious TSE agents were present. We were interested in why two different disease profiles were linked with a single mutation in PrP, and performed transmission experiments using PrPSc preparations from both human phenotypes into PrP knock-in mice expressing the equivalent mutation in murine PrP (101LL).8 These mice were produced to model P102L GSS, but did not show clinical signs of TSE or develop any abnormal PrP aggregates in the brain during their lifespan.9 Inoculation of classical P102L GSS produced clinical signs (ataxia, hind limb paralysis and kyphosis) and pathological signs (spongiform degeneration, and limited PrP deposition) of TSE in 101LL mice (but not wildtype mice), confirming the presence of an infectious transmissible agent in P102L GSS tissue. Disease could then be transmitted from brain tissue of sick 101LL mice to both 101LL and wildtype mice. However the majority of animals inoculated with atypical P102L GSS (21/22) remained healthy with no clinical signs of TSE and were culled due to old age (up to 814 days post inoculation). No disease was transmitted on subpassage from these mice.8 When brain tissue from both groups of mice was examined we observed little or no PrP deposition by IHC, and very low levels of PrP-res by immunoblot in animals that were inoculated with classical P102L GSS and developed clinical TSE. Conversely, several 101LL mice that received atypical P102L GSS and lived full lifespan showed (by IHC) large PrP amyloid plaques had formed in the corpus callosum and hippocampus.8 In both cases, the presence of PrPSc did not correlate with the infectious status of the tissue (as demonstrated by subpassage). Although atypical P102L GSS did not transmit disease efficiently (1/22) to mice bearing the same mutation in PrP, disease transmission has recently been shown in bank voles.10 Transmission to only one 101LL mouse in our study suggests low titre of infectious agent, or the presence of a transmission barrier. However the bank vole transmission confirms that atypical P102L GSS tissues do harbour TSE infectivity, and can cause disease in an appropriate host where the agent/strain interaction favours propagation of infectivity. Although the reasons for the apparent universal susceptibility of bank voles to all TSE agents are still unclear, these data do suggest that different isoforms or conformers of abnormal PrP present in P102L GSS tissues may be responsible for infectivity (in a susceptible host) and for amyloid plaque seeding. The true nature of the TSE agent is therefore far from certain. If PrPSc and infectivity do not correlate in all cases of TSE, it suggests that “PrPSc” in general is not the infectious agent, and that a specific subpopulation of misfolded PrP may instead be infectious and responsible for TSE disease.
SYNTHETIC PRIONS
Our data in the 101LL mice show that it is possible to misfold PrP and form amyloid plaques in the brain without TSE disease or TSE agent replication. This phenotype was produced following inoculation with atypical P102L GSS8 and also brain homogenate from GSS22 mice overexpressing P101L PrP.11 These mice express 12x the normal level of 101L PrP, and develop a neurological phenotype at 150–300 days of age that is neither consistent between animals nor consistent with clinical signs of TSE disease according to experienced animal scorers.11,12 They do however show abundant PrP amyloid plaques in the brain.13 We therefore hypothesised that the amyloid fibrils present in both inocula were responsible for inducing plaque formation in the recipient 101LL brain. This would indicate that amyloid fibrils were not the TSE infectious agent, but could template misfolding of host PrPC. In order to test this hypothesis, we inoculated 101LL and wildtype mice with a source of pure PrP amyloid fibrils.14 This allowed us to test the ability of amyloid fibrils to induce PrP misfolding in the absence of any other factors present in the material prepared from brain homogenate. Recombinant 101L and wildtype mouse PrP were expressed in E. coli, purified and refolded into α-monomeric, β-oligomeric and amyloid isoforms using techniques which were most appropriate at that time (described in.ref 14) These different PrP isoforms were then inoculated intracerebrally into groups of 101LL and wildtype mice (Fig. 1). Several other research groups have previously described the production and re-folding of recombinant PrP into a fibrillar conformation, which is claimed to create a “synthetic prion”.15-18 Generation of de novo synthetic prions is seen as the absolute proof of the Prion Hypothesis. Such preparations have been inoculated into mice which were shown to develop TSE disease, and replicate TSE infectivity.15-18 Published data are difficult to compare as each laboratory has used different refolding conditions, different PrP sequences and different recipient mice. However in general, no disease is seen following primary inoculation of these synthetic prions, but neurologic disease is often generated on subpassage, suggesting low titre of prions in the initial inoculum, or a selection and amplification of a specific conformer or aggregate from the primary inoculum. In our laboratory, fibrils produced from both 101L and wildtype PrP using our methods also failed to produce neurologic disease on primary inoculation of 101LL and wildtype mice. In contrast to other studies, we failed to produce TSE disease on subpassage of brain tissue from these mice.14 Our data indicated that using these specific refolding conditions, fibrils produced from both 101L and wildtype PrP did not contain TSE infectivity. However, on pathological analysis of all animals following cull, large PrP amyloid plaques were observed in 10/21 101LL mice inoculated with wildtype PrP fibrils, and 14/19 101LL mice inoculated with 101L PrP fibrils (Fig. 1). This phenotype was maintained on subpassage in 101LL mice.14 Importantly, plaques were induced by inoculation of both wildtype and 101L rec-PrP fibrils, indicating that the amyloid structure of the inoculated fibril and not the primary PrP sequence was responsible for plaque formation. No plaques were observed in wildtype 129/Ola mice that received the same inocula, or any animals that received α-monomeric or β-oligomeric PrP isoforms. No spongiform degeneration was observed in any of the inoculated animals. Our data therefore show that in contrast to other reported studies of synthetic prions, inoculation of refolded rec-PrP fibrils does not always lead to TSE disease, and that instead, PrP amyloid plaques can be seeded in brain tissue in what appears to be more akin to a proteinopathy than TSE.
FIGURE 1.
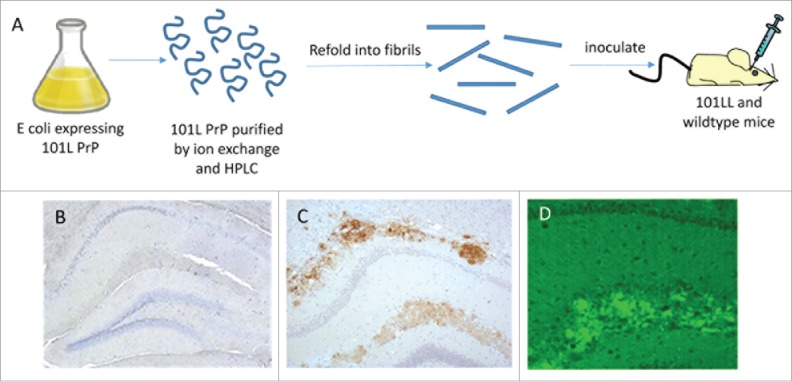
PrP amyloid plaque seeding in 101LL mice. Recombinant PrP was expressed in E coli and purified before refolding into amyloid fibrils. These preparations were inoculated into 101LL and wildtype mice (A). Animals survived for lifespan, and while no PrP aggregation was observed in wildtype mice (B), large thioflavin fluorescent (D) PrP amyloid plaques were detected in several 101LL mice (C).
PRION-LIKE TRANSMISSION IN OTHER ND
Recently it has been shown that several other neurodegenerative diseases associated with protein misfolding may spread within an organism by a “prion-like” mechanism. Inoculation of pre-formed amyloid seeds from patients with Alzheimer's disease (AD), or aged transgenic mice expressing human amyloid precursor protein (APP) was shown to accelerate the formation of Aβ plaques in the brains of APP transgenic mice.19 Similar results have been obtained from models of Parkinson's disease (PD),20 amyotrophic lateral sclerosis (ALS) 21 and Tauopathies.22 The introduction of a misfolded protein seed increased the recruitment and misfolding of normal host protein, leading to the spread of protein aggregation in the tissue. Similarities with the proposed mechanism of agent propagation in TSE (or prion) disease led to the use of the term “prion-like” and even to suggestions that, as these proteins were “prions”, all these diseases were potentially infectious. Recently, studies examining archival material from cases of iatrogenic Creutzfeldt Jakob disease (iCJD) that occurred following the administration of pituitary-derived human growth hormone,23 or dura matter grafts,24 have also shown the probable seeding of Aβ plaques. However despite the formation of Aβ plaques, these individuals did not show any abnormal tau pathology in the brain, or signs of clinical AD. Therefore whilst the materials appeared to be the source of the Aβ seeds, they did not reproduce the full clinicopathological phenotype of AD in the recipients.
There is no evidence to show an infectious aetiology for AD, PD, ALS and Tauopathies,25 which separates them from TSEs. While some TSEs are contagious and spread naturally between animals in the field, most TSEs can be transmitted to appropriate susceptible hosts by intracerebral, peripheral, intravenous, intraocular and intranasal routes; although the main route of transmission between ruminants and also zoonotic transmission to man, is by the oral route. Prion-like spread of Aβ has only been shown following direct intracerebral or intraperitoneal inoculation, and not by any other routes.26 We have yet to determine if plaques can be seeded in 101LL mice following oral or peripheral challenge with rec-PrP fibrils, but we suspect such experiments would behave similarly to seeded Aβ proteinopathies.
WHEN IS A PRION NOT A PRION?
The recent description of “prion-like” mechanisms of spread of misfolded protein in other neurodegenerative diseases such as AD, PD, ALS and tauopathy19-22 has increased interest in protein misfolding and prion/TSE disease, but has also introduced confusion and a degree of misunderstanding into the field of neurodegeneration. If the definition of a prion is a misfolded protein seed that can induce the autocatalytic conversion of normal protein into misfolded aggregates, then Aβ, α-synuclein, superoxide dismutase and hyperphosphorylated tau could indeed be considered as prions in addition to PrPSc. The term prion was originally defined as “ …proteinatious infectious particles which are resistant to inactivation by most procedures that modify nucleic acids.” and were the infectious agent responsible for scrapie.1 However prions are now more generally referred to as infectious proteins that cause neurodegenerative disease. In this case, abnormal PrP aggregates seeded in 101LL mice by atypical P102L GSS and rec-PrP fibrils are not prions, as they do not cause TSE disease in recipient animals. Similarly, no reproduction of the specific disease pathology seen in AD, PD, ALS, or tauopathy is seen following inoculation of pre-formed fibril seeds in mice. Even in humans, Aβ plaques may be seeded in the brain following the administration of cadaver-derived growth hormone 23 or dura matter grafting,24 but the individuals do not develop AD. Indeed, there is currently no evidence to support an infectious aetiology for AD, PD, ALS or Tauopathies.25 The use of the term “prion” to describe all these diseases may therefore be inappropriate, as there is a general assumption this refers to an infectious neurodegenerative disease. It has been proposed that the term “propagon” may better describe these pre-formed seeds,24,27 to define the propagation of a misfolded protein in tissue, and avoid confusion with TSE transmissibility and infection. The similarities between seeding of PrP aggregation in our 101LL model and the seeding of Aβ in APP transgenic mouse models is striking. In both cases, protein aggregates are formed following the inoculation of pre-formed seeds, in neither case does the clinicopathological phenotype of the diseases these misfolded proteins are associated with present in the animals, and neither are infectious. So even when the protein is PrP, misfolding and aggregation does not always result in a transmissible neurodegenerative disease.
CONCLUSION: ARE ALL PROTEINOPATHIES INFECTIOUS PRION DISEASES?
We have now shown that seeded protein aggregation does not inevitably produce infectious prions, even when the protein is PrP.14 Data produced using our specific refolding methods do not demonstrate generation of infectious synthetic prions following fibrillisation of recombinant PrP in vitro. Pre-formed fibrils introduced directly into the brain seeded the formation of amyloid plaques in a manner similar to that shown with Aβ, α-synuclein, superoxide dismutase and hyperphosphorylated-tau seeds,19-22 but did not cause infectious TSE disease. However due to the different refolding conditions used by several labs, and recent advances made in methods of refolding and fibrillisation, it is possible that a small population of misfolded PrP conformers produced under specific experimental conditions are infectious. Yet, even in animals which appeared to show signs of TSE on subpassage of synthetic prions, some specific ultrastructural characteristics observed in TSE infection (tubulo-vesicular bodies and lysosomal staining) were absent.28 These characteristics were also absent in 101LL mice inoculated with atypical GSS and rec-PrP fibrils, despite the presence of PrP amyloid plaques.14,29
Synthetic prions (formed from recombinant PrP) and prions generated in vitro by amplification assays such as protein misfolding amplification (PMCA), appear to show a general lack of correlation between the amount of misfolded protein produced and levels of infectivity. Synthetic prions generally do not produce disease on primary inoculation despite the inoculation of large amounts of PrP fibrils (∼5 µg).30 PMCA amplification experiments were shown to generate large amounts of PrP-res, but the ratio of infectivity titre to PrP-res was lower than seen in infected brain samples.31 Both of these data sets indicate that a substantial portion of the misfolded PrP generated in vitro is non-infectious. Such non-infectious forms of misfolded PrP may also be generated in vivo under the correct conditions, and in some cases may form or seed amyloid plaque formation.
It is therefore possible that a spectrum of disorders can be associated with protein misfolding and aggregation in the brain. In the most extreme case, specific conformers of misfolded PrP cause TSE disease and replication of the infectious TSE agent, which can then be transmitted to other individuals. In other cases the build-up and spread of protein aggregates causes neurotoxicity and neurodegeneration in the brain, but are not infectious. Finally, cases exist where protein aggregates form and spread, but are neither neurotoxic nor infectious and can be tolerated by the animal. These latter two cases would be termed proteinopathies, caused by propagons, and are therefore distinct from infectious TSE disease. Although mechanisms of protein:protein interaction, misfolding and spread may be similar between TSE, AD, PD, ALS and Tauopathies, better definition between TSEs and proteinopathies (or propagons) is needed to examine aetiology, spread and treatment for each disease
ETHICAL STATEMENT
All animal experiments were approved by the local Ethical Review Committee and performed under Licence with the UK Home Office in accordance with the Animals (Scientific Procedures) Act 1986.
DISCLOSURE OF POTENTIAL CONFLICTS OF INTEREST
No potential conflicts of interest were disclosed by the authors.
ACKNOWLEDGEMENTS
I would like to thank Prof Pedro Piccardo and Declan King for comments on the manuscript, and Prof Jean Manson and Prof Glenn Telling for use of the 101LL and GSS22 transgenic mouse lines.
FUNDING
This work was funded by the Biotechnology and Biological Sciences Research Council (BBSRC) UK, under grant numbers BB/E002900 and BB/J004332/1
REFERENCES
- [1].Prusiner S. Novel proteinaceous infectious particles cause scrapie. Science 1982; 216(4542):136-144; PMID:6801762; http://dx.doi.org/ 10.1126/science.6801762 [DOI] [PubMed] [Google Scholar]
- [2].Bolton DC, McKinley MP, Prusiner SB. Identification of a protein that purifies with the scrapie prion. Science 1982; 218(4579):1309-11; PMID:6815801; http://dx.doi.org/ 10.1126/science.6815801 [DOI] [PubMed] [Google Scholar]
- [3].Safar J, Wille H, Itrri V, Groth D, Serban H, Torchia M, Cohen F.E, Prusiner SB. Eight prion strains have PrPSc molecules with different conformations. Nat Med 1998; 4(10):1157-65; PMID:9771749; http://dx.doi.org/ 10.1038/2654 [DOI] [PubMed] [Google Scholar]
- [4].McKinley MP, Bolton DC, Prusiner S.B. A protease-resistant protein is a structural component of the scrapie prion. Cell 1983; 35(1):57-62; PMID:6414721; http://dx.doi.org/ 10.1016/0092-8674(83)90207-6 [DOI] [PubMed] [Google Scholar]
- [5].Barron RM, Campbell SL, King D, Bellon A, Chapman KE, Williamson RA, Manson JC. High titres of TSE infectivity associated with extremely low levels of PrPSc in vivo. J Biol Chem 2007; 282:35878-886; PMID:17923484; http://dx.doi.org/ 10.1074/jbc.M704329200 [DOI] [PubMed] [Google Scholar]
- [6].Lasmezas CI, Deslys J, Robain O, Jaegly A, Beringue V, Peyrin J, Fournier J, Hauw J, Rossier J, Dormont D. Transmission of the BSE agent to mice in the absence of detectable abnormal prion protein. Science 1997; 275(5298):402-5; PMID:8994041; http://dx.doi.org/ 10.1126/science.275.5298.402 [DOI] [PubMed] [Google Scholar]
- [7].Piccardo P, Dlouhy SR, Lievens PMJ, Young K, Thomas DP, Nochlin D, Dickson DW, Vinters HV, Zimmerman TR, Mackenzie IRA, et al.. Phenotypic variability of Gerstmann-Straussler-Scheinker disease is associated with prion protein heterogeneity. J Neuropathol Exp Neurol 1998; 57(10):979-988; PMID:9786248; http://dx.doi.org/ 10.1097/00005072-199810000-00010 [DOI] [PubMed] [Google Scholar]
- [8].Piccardo P, Manson JC, King D, Ghetti B, Barron RM. Accumulation of prion protein in the brain that is not associated with transmissible disease. Proc Natl Acad Sci U S A 2007; 104(11):4712-17; PMID:17360589; http://dx.doi.org/ 10.1073/pnas.0609241104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Manson JC, Jamieson E, Baybutt H, Tuzi NL, Barron R, McConnell I, Somerville R, Ironside J, Will R, Sy MS, et al.. A single amino acid alteration (101L) introduced into murine PrP dramatically alters incubation time of transmissible spongiform encephalopathy. EMBO J 1999; 18(23):6855-64; PMID:10581259; http://dx.doi.org/ 10.1093/emboj/18.23.6855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Pirisinu L, Di Bari MA, D'Agostino C, Marcon S, Riccardi G, Poleggi A, Cohen ML, Appleby BS, Gambetti P, Ghetti B, et al.. Gerstmann-straussler-scheinker disease subtypes efficiently transmit in bank voles as genuine prion diseases. Scientific Reports 2016; 6:9; PMID:27920429; http://dx.doi.org/ 10.1038/srep20443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Piccardo P, King D, Telling G, Manson JC, Barron RM. Dissociation of prion protein amyloid seeding from transmission of a spongiform encephalopathy. J Virol 2013; 87(22):12349-356; PMID:24027305; http://dx.doi.org/ 10.1128/JVI.00673-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Fraser H, Dickinson AG. Distribution of experimentally induced scrapie lesions in the brain. Nature 1967; 216:1310-11; PMID:5625087; http://dx.doi.org/ 10.1038/2161310a0 [DOI] [PubMed] [Google Scholar]
- [13].Nazor KE, Kuhn F, Seward T, Green M, Zwald D, Pürro M, Schmid J, Biffiger K, Power AM, Oesch B. et al.. Immunodetection of disease-associated mutant PrP, which accelerates disease in GSS transgenic mice. EMBO J 2005; 24(13):2472-80; PMID:15962001; http://dx.doi.org/ 10.1038/sj.emboj.7600717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Barron RM, King D, Jeffrey M, McGovern G, Agarwal S, Gill AC, Piccardo P. PrP aggregation can be seeded by pre-formed recombinant PrP amyloid fibrils without the replication of infectious prions. Acta Neuropathol (Berl) 2016; 132(4):1-14; http://dx.doi.org/ 10.1007/s00401-016-1594-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Makarava N, Savtchenko R, Alexeeva I, Rohwer RG, Baskakov IV. New molecular insight into mechanism of evolution of mammalian synthetic prions. Am J Pathol 2016; 186(4):1006-14; PMID:26873446; http://dx.doi.org/ 10.1016/j.ajpath.2015.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Raymond GJ, Race B, Hollister JR, Offerdahl DK, Moore RA, Kodali R, Raymond LD, Hughson AG, Rosenke R, Long D, et al.. Isolation of novel synthetic prion strains by amplification in transgenic mice coexpressing wild-type and anchorless prion proteins. J Virol 2012; 86(21):11763-78; PMID:22915801; http://dx.doi.org/ 10.1128/JVI.01353-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Colby DW, Wain R, Baskakov IV, Legname G, Palmer CG, Nguyen HOB, Lemus A, Cohen FE, DeArmond SJ, Prusiner SB. Protease-sensitive synthetic prions. Plos Pathog 2010; 6(1):e1000736; PMID:20107515; http://dx.doi.org/ 10.1371/journal.ppat.1000736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Legname G, Baskakov I, Nguyen H, Riesner D, Cohen F, DeArmond S, Prusiner S. Synthetic mammalian prions. Science 2004; 305(5684):673-6; PMID:15286374; http://dx.doi.org/ 10.1126/science.1100195 [DOI] [PubMed] [Google Scholar]
- [19].Meyer-Luehmann M, Coomaraswamy J, Bolmont T, Kaeser S, Schaefer C, Kilger E, Neuenschwander A, Abramowski D, Frey P, Jaton AL, et al.. Exogenous induction of cerebral {beta}-Amyloidogenesis is governed by agent and host. Science 2006; 313(5794):1781-84; PMID:16990547; http://dx.doi.org/ 10.1126/science.1131864 [DOI] [PubMed] [Google Scholar]
- [20].Oueslati A, Ximerakis M, Vekrellis K. Protein transmission, seeding and degradation: Key steps for α-synuclein prion-like propagation. Exp Neurobiol 2014; 23(4):324-336; PMID:25548532; http://dx.doi.org/ 10.5607/en.2014.23.4.324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ayers JI, Diamond J, Sari A, Fromholt S, Galaleldeen A, Ostrow LW, Glass JD, Hart PJ, Borchelt DR. Distinct conformers of transmissible misfolded SOD1 distinguish human SOD1-FALS from other forms of familial and sporadic ALS. Acta Neuropathol 2016; 132(6):827-840; PMID:27704280; http://dx.doi.org/ 10.1007/s00401-016-1623-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Clavaguera F, Hench J, Goedert M, Tolnay M. Invited review: Prion-like transmission and spreading of tau pathology. Neuropathol Appl Neurobiol 2015; 41(1):47-58; PMID:25399729; http://dx.doi.org/ 10.1111/nan.12197 [DOI] [PubMed] [Google Scholar]
- [23].Jaunmuktane Z, Mead S, Ellis M, Wadsworth JDF, Nicoll AJ, Kenny J, Launchbury F, Linehan J, Richard-Loendt A, Walker AS, et al.. Evidence for human transmission of amyloid-[bgr] pathology and cerebral amyloid angiopathy. Nature 2015; 525(7568):247-250; PMID:26354483; http://dx.doi.org/ 10.1038/nature15369 [DOI] [PubMed] [Google Scholar]
- [24].Kovacs GG, Lutz MI, Ricken G, Ströbel T, Höftberger R, Preusser M, Regelsberger G, Hönigschnabl S, Reiner A, Fischer P, et al.. Dura mater is a potential source of Aβ seeds. Acta Neuropathol 2016; 131(6):1-13; PMID:26715564; http://dx.doi.org/ 10.1007/s00401-016-1565-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Irwin DJ, Abrams JY, Schonberger LB, Leschek EW, Mills JL, Lee VMY, Trojanowski JQ. Evaluation of potential infectivity of alzheimer and parkinson disease proteins in recipients of cadaver-derived human growth hormone. Jama Neurol 2013; 70(4):462-8; PMID:23380910; http://dx.doi.org/ 10.1001/jamaneurol.2013.1933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Eisele YS, Bolmont T, Heikenwalder M, Langer F, Jacobson LH, Yan ZX, Roth K, Aguzzi A, Staufenbiel M, Walker LC, et al.. Induction of cerebral beta-amyloidosis: Intracerebral versus systemic A beta inoculation. Proc Natl Acad Sci U S A 2009; 106(31):12926-931; PMID:19622727; http://dx.doi.org/ 10.1073/pnas.0903200106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Eisele YS, Duyckaerts C. Propagation of Aß pathology: Hypotheses, discoveries, and yet unresolved questions from experimental and human brain studies. Acta Neuropathol 2016; 131(1):5-25; PMID:26715565; http://dx.doi.org/ 10.1007/s00401-015-1516-y [DOI] [PubMed] [Google Scholar]
- [28].Jeffrey M, McGovern G, Makarava N, González L, Kim YS, Rohwer RG, Baskakov IV. Pathology of SSLOW, a transmissible and fatal synthetic prion protein disorder, and comparison with naturally occurring classical transmissible spongiform encephalopathies. Neuropathol Appl Neurobiol 2014; 40(3):296-310; PMID:23578208; http://dx.doi.org/ 10.1111/nan.12053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Jeffrey M, McGovern G, Chambers EV, King D, Gonzalez L, Manson JC, Ghetti B, Piccardo P, Barron RM. Mechanism of PrP-amyloid formation in mice without transmissible spongiform encephalopathy. Brain Pathol 2012; 22(1):58-66; PMID:21645162; http://dx.doi.org/ 10.1111/j.1750-3639.2011.00508.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Makarava N, Kovacs GG, Bocharova O, Savtchenko R, Alexeeva I, Budka H, Rohwer RG, Baskakov IV. Recombinant prion protein induces a new transmissible prion disease in wild-type animals. Acta Neuropathol 2010; 119(2):177-187; PMID:20052481; http://dx.doi.org/ 10.1007/s00401-009-0633-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Klingeborn M, Race B, Meade-White KD, Chesebro B. Lower specific infectivity of protease-resistant prion protein generated in cell-free reactions. Proc Natl Acad Sci U S A 2011; 108(48):E1244-253; PMID:22065744; http://dx.doi.org/ 10.1073/pnas.1111255108 [DOI] [PMC free article] [PubMed] [Google Scholar]


