Abstract
Humans commonly exhale aerosols comprised of small droplets of airway-lining fluid during normal breathing. These “exhaled bioaerosols” may carry airborne pathogens and thereby magnify the spread of certain infectious diseases, such as influenza, tuberculosis, and severe acute respiratory syndrome. We hypothesize that, by altering lung airway surface properties through an inhaled nontoxic aerosol, we might substantially diminish the number of exhaled bioaerosol droplets and thereby provide a simple means to potentially mitigate the spread of airborne infectious disease independently of the identity of the airborne pathogen or the nature of any specific therapy. We find that some normal human subjects expire many more bioaerosol particles than other individuals during quiet breathing and therefore bear the burden of production of exhaled bioaerosols. Administering nebulized isotonic saline to these “high-producer” individuals diminishes the number of exhaled bioaerosol particles expired by 72.10 ± 8.19% for up to 6 h. In vitro and in vivo experiments with saline and surfactants suggest that the mechanism of action of the nebulized saline relates to modification of the physical properties of the airway-lining fluid, notably surface tension.
Keywords: drug delivery, lung, infectious disease, influenza
It has long been understood that exhaled bioaerosol particles provide an important vector for the spread of certain infectious diseases (1, 2). Viruses known to spread from humans and/or animals through breathing, sneezing, and coughing include measles, influenza virus (3, 4), adenovirus (5), African swine fever virus (6), foot and mouth disease virus (7), varicella-zoster virus (chicken pox) (8), infectious bronchitis virus (9), and smallpox, among others (10). Airborne bacteria include anthrax, Escherichia coli (11), Klebsiella pneumoniae (12), Francisella tularensis (13), and tuberculosis (14). Normal mouth breathing (more than coughing, nose breathing, or talking) has been observed to produce the largest number of airborne droplets (15, 16). These droplets are primarily <1 μm in size, because larger droplets tend to be filtered out of the expired air by the lungs (16). Given the variable dimensions of common viral and bacterial pathogens (≈25 nm to 5 μm), the ability of exhaled bioaerosol droplets of a given size to carry pathogen obviously varies with pathogen type. Bioaerosols seem to form by the passage of air, during inhalation and exhalation, over the mucus layer lining the lungs (17) or possibly through the reopening of closed small airways, destabilizing the mucus surface through an interplay of surface tension and viscous forces to form small airborne droplets, as has been simulated in vitro via “cough machine” experiments (18). In this study, we aimed to explore the ability to transiently diminish the number of exhaled bioaerosol droplets in normal human subjects by delivery of a simple, safe, liquid aerosol. We also aimed to understand the mechanism of the effect of the inhaled aerosol through in vitro cough machine experiments.
Materials and Methods
Materials. 1,2-Dipalmitoyl-sn-glycero-3-phosphocholine (DPPC) and 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphoglycerol (POPG) were purchased from Genzyme. Aqueous solutions for aerosolization were prepared either as a 0.9% isotonic saline formulation or as a 7:3 wt/wt mixture of DPPC and POPG suspended at 100 mg/ml in 0.9% saline. Mucus mimetics for bioaerosol formation in the simulated cough machine were prepared by adding a small amount of concentrated sodium tetraborate in distilled water solution (Na2B4O7, 50 g/liter; J.T. Baker) to locust bean gum (LBG) in distilled water mixture (2% wt/vol; Fluka) and mixing for 1 min, pipetting onto the trough mimetic and allowing 30 min for proper crosslinking. Two percent LBG and 2 mM Borax were chosen as representative mucus simulants and were in the literature range of 0.4–2% and 1–3 mM (18). Further information related to materials and methods can be found in the Supporting Text, which is published as supporting information on the PNAS web site.
Exhaled Bioaerosol Measurement System. A mouthpiece was connected to a Fleisch pneumotachograph with thermister to prevent condensation (model no. 1, Phipps and Bird, Richmond, VA). A pressure transducer (model no. 239, Setra, Boxborough, MA) measured the pressure drop through the pneumotachograph. The signal from the pressure transducer was amplified and converted to a flow profile (labview software, National Instruments, Austin, TX) for data acquisition and real-time visualization of the patient's flow signal on an external oscilloscope. The outlet of the pneumotachograph was connected to a sampling “T” adapter. One end of the sampling T was connected to a six-channel optical particle counter (OPC; Climet, Ultimate 100, Redlands, CA) to measure expired particle count and size. Each channel on the OPC tabulates particle counts within a size-selective range for a total of six bins: 0.085–0.1, 0.1–0.15, 0.15–0.2, 0.2–0.3, 0.3–0.5, and >0.5 μm. The other end of the sampling T was connected to a Delbag-Luftfilter air filter (COPULAR CKL Macropur-F Acelan, GEA, Berlin), which removed any airborne particulates from the inhaled ambient air stream. A physical representation of the system used to assess in vivo particle exhalation can be seen in Fig. 5, which is published as supporting information on the PNAS web site.
Human Study. To test the hypothesis that by transiently perturbing the balance between surface tension and viscous forces acting on or within lung-lining fluid, we might substantially reduce the number of exhaled bioaerosol particles expired during normal mouth breathing, we constructed a device similar to that of Papineni and Rosenthal (16) for monitoring the number and size of particles exhaled by human subjects breathing particle-free air. This device and the clinical trial are further described here. Eleven healthy adult volunteers ages 18–65 with normal lung function [% forced expiratory volume (FEV1) >80%] provided informed written consent and were selected for participation in this crossover placebo-controlled study. Exclusion criteria included history or evidence of significant pulmonary disease (e.g., cystic fibrosis, chronic obstructive pulmonary disease, or severe asthma), history or evidence of cardiovascular disease or acute/chronic infection of the upper or lower respiratory tract, pregnancy, or lactation. Each subject had three clinical visits during the study for measurement of particle exhalation. During their first visit, subjects were randomly assigned to a treatment group and received an aerosol of either a saline formulation (0.9% isotonic saline) or the DPPC/POPG surfactant formulation. After at least a 1-week period, subjects were crossed over for dosing during their second visit. Particle expiration was measured immediately before and 5 min, 30 min, 1 h, 2 h, and 6 h after inhalation. During the third visit, at least 1 month after the last treatment, particle expiration was assessed in the absence of treatment. During dosing, each subject received saline or surfactant aerosol from a PARI LC Plus Jet nebulizer (PARI, Starnberg, Germany) connected to a compressed air source at 18 psi (1 psi = 6.89 kPa) (1.24 bar). Aerosol was administered to the respiratory tract of the subjects with mass median aerodynamic diameter (MMAD) of 3.7 μm and a geometric standard deviation (GSD) of 1.9 μm over a 6-min period. The MMAD was derived from inertial impaction data [as measured by an Andersen Cascade Impactor (Thermo Electron, Beverly, MA)]. The distribution around this median diameter was described by assuming a log-normal dispersion of sizes. The GSD was calculated from the particle size at the 84th percentile (by mass) divided by the MMAD. Based on the MMAD and the nebulized mass of fluid (≈2.5 g), we estimate, based on standard lung deposition models, to have delivered ≈1 g of liquid aerosol to the respiratory tract. This delivered mass falls below or within the range of masses of isotonic saline delivered to human asthmatics during standard therapy with albuterol inhalation solution (Ventolin, GSK, London) (5–15 min of nebulization) and is significantly less than the hypertonic saline delivered by nebulization to achieve sputum expectoration (up to 20 min of nebulization) (19). Patients wore nose clamps and inhaled through mouthpieces at steady-state volume (≈1 liter) while seated for 6 min (≈2.5 ml of aerosol volume). Patients observed their breathing patterns on an oscilloscope (Fig. 6, which is published as supporting information on the PNAS web site) that provided a visual representation of breath volume to aid compliance. At each assessment, patients first breathed through the Delbag-Luftfilter air filter (Fig. 6; Fig. 7, which is published as supporting information on the PNAS web site) for a 2-min washout period to remove ambient particles. After washout, patients breathed through the system for two 1-min sessions and the optical particle counter (Fig. 6; see also Fig. 8, which is published as supporting information on the PNAS web site) tabulated average particle concentration and size in the exhaled air.
Cough Machine Apparatus. An air-tight 6.25-liter Plexiglas volume reservoir (for a diagram of the apparatus, see Fig. 8) with a digital pressure gauge and pressure relief valve was constructed to supply a volume of air representative of average lung capacity. A dry compressed air source was connected to the volume reservoir to provide the appropriate volume and pressurize the tank for cough simulation. At the outlet of the volume reservoir, an electronically controlled solenoid valve (model no. 8210G94, Asco, Florham Park, NJ) was connected to control volume release. The solenoid valve was connected to a Fleisch pneumotachograph (model no. 4, Phipps and Bird) with a differential pressure transducer (model no. DP45-14, Validyne, North Ridge, CA). To assess the flow rate through the system, the signal from the pressure transducer was amplified with a Validyne CD15 sine wave carrier demodulator (Validyne) and converted to a differential pressure over time (insta-cal software, Validyne).
A cough profile generated through these components in comparison to a graphical representation of a real cough is shown in Fig. 7. A typical cough profile (Fig. 7a) is biphasic; an initial high-velocity phase of ≈12 liter/s with a duration of ≈30–50 ms followed by a second phase of diminishing flow rate lasting ≈200–500 ms. We found the simulated cough (Fig. 7b) to have a similar biphasic profile over ≈0.5 s.
The flow generated through the pneumotachograph traveled through an airtight rectangular acrylic model trachea (30 cm × 1.6 cm × 1.6 cm) lined on the bottom of the trough with a mucus mimetic (Figs. 6 and 8). A rectangular cross section was chosen to enable uniform mucus mimetic height and to avoid problems associated with round tubes and gravity drainage. The cross-sectional area of the model trachea was chosen to simulate the human trachea (20). The distal end of the model trachea remained open to the atmosphere. The LBG and Borax solutions were mixed for 1 min on a rotator, and the resulting mixture was pipetted into the model trachea at a depth of ≈1.5 mm and allowed to crosslink for 30 min, creating the mucus simulant. The viscoelastic 2% LBG and 2 mM sodium tetraborate mucus mimetic enabled examination of multiple successive coughs while keeping most of the 20-cm mucus simulant lining in place after coughs. The viscoelastic fingerprint of this mucus mimetic is shown in Fig. 9, which is published as supporting information on the PNAS web site. Simulated cough experiments for assessment of exhaled bioaerosol particle size were conducted immediately and at 30 and 60 min. The Fleisch pneumotachograph was disconnected from the model trachea system and a PARI LC Jet nebulizer and Proneb Ultra compressor (PARI) were connected for delivery of test formulations. Formulations tested included saline and 100 mg/ml DPPC/POPG (Genzyme). The test formulations were nebulized through the system for 6 min (equivalent to the clinical study) from a PARI LC Plus Jet nebulizer (PARI) connected to a compressed air source at 18 psi (1.24 bar). Immediately after nebulization, the model trachea was reattached to the Fleisch pneumotachograph. Experiments for bioaerosol detection were performed at 0, 30, and 60 min after nebulization of test formulations.
Physical Property Measurement. Static surface tension measurements were performed by using a Wilhelmy Plate Microbalance (WS1; Riegler and Kirstein, Potsdam, Germany). A small (3-mm-wide) filter paper probe (no. 576, Schleicher & Schuell) connected to the electronic balance tensiometer was immersed into the formulations to make the tension measurements. The tensiometer was calibrated by using pure water known to have a surface tension of 72 dyne/cm (1 dyne = 10 μN). Formulation viscosity measurements over a range of shear rates were performed on a TA Instruments AR1000-N Rheolyst Rheometer (New Castle, DE) by using a 60-mm-diameter 1° acrylic cone-and-plate configuration. Experiments were performed on a Peltier plate at 20°C. Over the shear range of 10–10,000 s–1, the surfactant formulation yielded a similar but slightly higher viscosity to water or saline (≈0.03 vs. 0.01 poise; 1 poise = 0.1 Pa·sec). These results can be seen in Fig. 6.
Results and Discussion
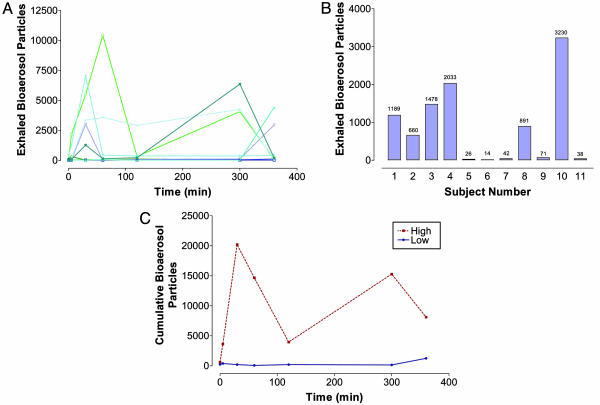
After Institutional Review Board approval of our human study protocol, 12 healthy subjects were enrolled in the study, of which 11 finished the entire trial. Exhaled particle production was measured after a 2-min “wash-out” period on the device. We assessed expired bioaerosol particle number concentration over a 2-min period with the per-minute count derived from the average of the 2 min. We first measured the baseline-exhaled bioaerosol among the 11 human subjects at seven time points over a period of 6 h (Fig. 1A). The number of exhaled particles per liter varied dramatically over time and among subjects, ranging from a low of one particle per liter to a high of >10,000. To better characterize intersubject variability, we examined the average number of particles counted over 6 h per subject. The results, shown in Fig. 1B, reveal the existence of two distinct groups: high-producer human subjects, whom we define as those human subjects expiring on average >500 particles per liter over the 6-h interval, and low-producer human subjects, expiring less than an average of 500 particles per liter over the 6-h period. The high-producer subjects (n = 6) bear the burden of total bioaerosol production (98.16% of all particles counted) within the human subject group; this is shown graphically in Fig. 1C, which compares the cumulative bioaerosol particle numbers at each time point over the 6-h interval for high versus low producers.
Fig. 1.
Exhaled bioaerosol particles during normal breathing of 11 healthy human subjects. (A) Exhaled bioaerosol particles per liter vs. time for 11 healthy human subjects. Particles of >150 nm were counted in these measurements, after a period of 2-min expiration at each represented time point. (B) Average exhaled bioaerosol particles per liter vs. human subject over the 6-h measurement interval. The average exhaled particle per liter number was obtained by summing the measured particle numbers for every time point during the 6-h period and dividing by the number of time points. High producers are defined as those subjects who expire on average >500 particles per liter. (C) Cumulative expired particles per liter vs. time for the high- (n = 6 subjects) and low-producer (n = 5 subjects) groups. Cumulative expired particles were determined by summing up the expired particles per liter for all individuals of a group at each time point.
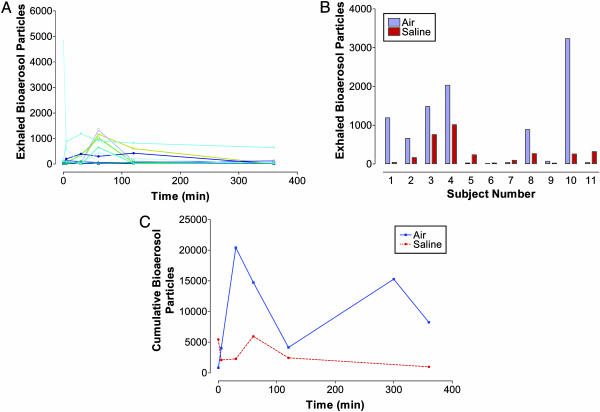
To test our hypothesis that by altering the surface tension properties of the lung-lining fluid we might significantly diminish exhaled bioaerosol in healthy subjects, we next delivered to the same 11 human subjects isotonic saline by nebulization. As with the baseline results of Fig. 1A, we observed considerable inter-subject variability (Fig. 2A). The effect of saline delivery on the average number of expired bioaerosol particles is shown in Fig. 2B on a per-subject basis. High-producer subjects (n = 6) responded to saline delivery with a statistically significant drop in average expired bioaerosol particle number (–72.10 ± 8.19%) relative to baseline. The opposite trend was observed for low-producer subjects (n = 5), who expired more particles on average after saline (340.35 ± –181.88%) relative to baseline. Note that after saline delivery the major change in exhaled particle number was dominated by the high-producer subjects, resulting in a substantial diminishment of cumulative particle count for all 11 subjects combined (Fig. 2C).
Fig. 2.
Exhaled bioaerosol particles after delivery of isotonic saline during normal breathing in 11 healthy human subjects. (A) Exhaled bioaerosol particles per liter vs. time for 11 healthy human subjects after inhalation of isotonic saline at t = 0. Particles of >150 nm were counted in these measurements, after a period of 2-min expiration at each represented time point. (B) Average exhaled bioaerosol particles per liter vs. human subject over the 6-h measurement interval for the cases of baseline and saline delivery. The average exhaled particle per liter number was obtained by summing the measured particle numbers for every time point during the 6-h period and dividing by the number of time points. (C) Cumulative expired particles per liter vs. time for all human subjects after inspiration of saline (n = 11 subjects) and of air (i.e., baseline) (n = 11 subjects). Cumulative expired particles were determined by summing up the expired particles per liter for all individuals of a group at each time point.
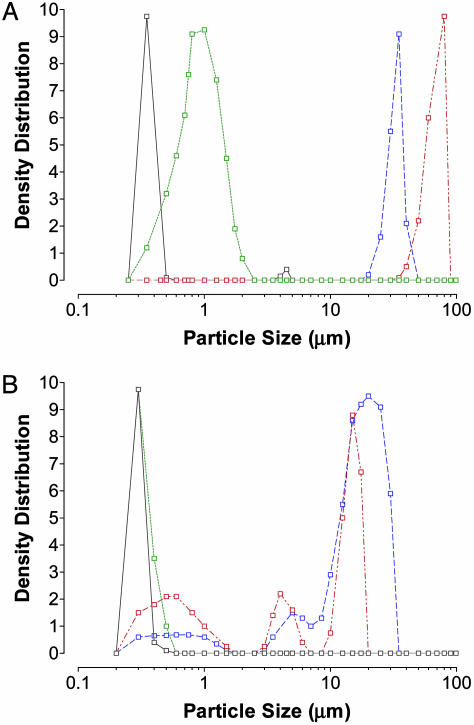
To test our hypothesis that modification of the surface properties of the lung-lining fluid underlies the suppression of exhaled bioaerosol produced in high-producer subjects, we constructed a cough machine apparatus (see Materials and Methods). We delivered a burst of air (12 liters/s for 30–50 ms) over a model mucus layer (formed of 2% LBG crosslinked with sodium tetraborate in distilled water) to simulate a typical cough profile as previously measured by King et al. (18). In the absence of nebulized saline, the burst of air destabilized the mucus/air surface to form submicron droplets with volume-averaged median size of ≈320 nm (Fig. 3A), as measured by a Sympatec (Lawrenceville, NJ) HELOS/KF laser-diffraction particle sizer. After nebulization for 6 min of normal saline through the model trachea/trough of the cough machine, the size distribution of mucus droplets shifted to larger values. Fig. 3A also reveals the mucus droplet size distribution after saline delivery at t = 0, 30, and 60 min, respectively. Median droplet size increased from ≈320 nm in the absence of saline to ≈1 μm with saline at t = 0 min, 65 μm at t = 30 min, and 30 μm at t = 60 min. Given that saline and mucus simulant are relatively immiscible at room temperature, application of saline to mucus simulant produces a thin surface layer of relatively high surface tension [isotonic saline has a surface tension of 72 dyne/cm, which is significantly higher than that reported for mucus and mucus simulant materials (21, 22)]. Isotonic saline also has much lower viscosity in comparison with mucus or mucus simulant. Relatively high surface tension favors the formation of droplets that are relatively large, by equilibrium thermodynamic considerations (23). On the other hand, smaller fluid viscosity tends to favor the creation of smaller droplets (24), suggesting that viscous forces may play a secondary role in the size shift observed in Fig. 3A. Our in vitro results may shed important light on the differences observed in Fig. 1 between high and low producers and in the response of the two groups to saline delivery, as revealed in Fig. 2. Subjects breathing out relatively large numbers of particles may tend to produce more particles in the nanometer range during respiration than subjects breathing out relatively fewer numbers of particles, possibly because of differences in surface tension of the lung-lining fluid. Delivery of saline to high-producer individuals may thus shift droplet sizes on breakup toward droplet sizes of approximately >10 μm, i.e., to droplets that are effectively filtered by gravity sedimentation and inertia in the respiratory tract (25).
Fig. 3.
Aerosol concentration of particles produced in the in vitro cough machine after delivery of isotonic saline or surfactant as a consequence of a burst of air over the simulated mucus. (A) The effect of saline delivery on density distribution of aerosol particles formed after exposure of mucus simulant surface to a burst of air in the in vitro cough machine. Four cases are shown: (i) mucus simulant (solid grey line), (ii) mucus simulant immediately after application of nebulized isotonic saline (dotted green line), (iii) mucus simulant 30 min after application of nebulized isotonic saline (dashed-dotted red line), and (iv) mucus simulant 60 min after application of nebulized isotonic saline (dashed blue line). (B) The effect of surfactant delivery on density distribution of aerosol particles formed after exposure of mucus simulant surface to a burst of air in the in vitro cough machine. Four cases are shown: (i) mucus simulant (solid grey line), (ii) mucus simulant immediately after application of nebulized isotonic saline (dotted green line), (iii) mucus simulant 30 min after application of nebulized isotonic saline (dashed-dotted red line), and (iv) mucus simulant 60 min after application of nebulized isotonic saline (dotted blue line).
To test our hypothesis that surface tension plays a key role in the diminution of expired bioaerosol via saline delivery to the lungs, we formed a suspension of isotonic saline and lung surfactant phospholipid surfactants DPPC and POPG. The mixture consisted of 7% (wt/wt) DPPC and 3% (wt/wt) POPG in isotonic saline. This mixture exhibited an equilibrium surface tension of 42 ± 2 dyne/cm versus a surface tension of 72 dyne/cm for pure isotonic saline, as measured by a Wilhelmy Microbalance (see Materials and Methods). The apparent viscosity of the mixture, as measured by a rotating disk viscometer, was found to be somewhat greater than that of isotonic saline (≈0.03 vs. 0.01 poise). We hypothesized that delivery of this surfactant mixture would produce in our in vitro and in vivo studies surface tensions less than those observed upon delivery of saline alone and therefore have less impact on bioaerosol diminution in high-producer individuals relative to baseline. We based this hypothesis in part on published results (22) that show surfactant delivery to the trachea of horses produces tracheal surface tension significantly below (24.5 ± 0.51 dyne/cm) that achieved by delivery of saline alone (31.9 ± 0.54 dyne/cm). We first nebulized the surfactant mixture into the cough machine apparatus to produce the aerosol profile shown in Fig. 3B. We find that the median droplet size is consistently smaller in the case of surfactant relative to saline delivery, in line with the smaller surface tension of the mixture in comparison with pure saline. This also supported the secondary role of viscosity in the droplet creation process, in that the surfactant mixture displayed a (modestly) greater viscosity than the pure saline.
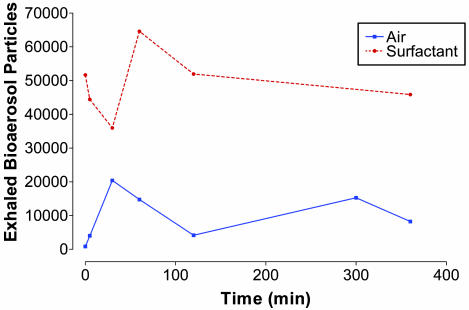
To test our hypothesis in humans, we next delivered to 11 human subjects the mixture of isotonic saline and LS phospholipid surfactants DPPC and POPG. Fig. 4 compares the total number of expired particles for the entire group with baseline particles for the 11 human subjects, revealing that surfactant delivery substantially amplifies exhaled bioaerosol. We observe this amplification in both high and low producers. Thus, surfactant delivery dramatically amplifies bioaerosol particle production among high producers by 325.79 ± 172.92% and among low producers by 5,954.82 ± 5,447.44%.
Fig. 4.
Cumulative expired particles per liter vs. time for all human subjects after inspiration of saline (n = 11 subjects) and of surfactant (n = 11 subjects). Cumulative expired particles were determined by summing up the expired particles per liter for all individuals of a group at each time point.
The saline versus surfactant results of our human studies combined with our in vitro data raise the question of the effect of administered aerosol on the size (and thereby mass) distribution of exhaled bioaerosol. We did not, however, observe any statistical tendency for saline or surfactant to increase the size or mass of exhaled aerosol, possibly because of the filtration capacity of the human lungs, which tend to remove by deposition particles in the inertial size range. These observations must nonetheless be considered within the constraints of our particle-sizing apparatus. As pointed out in Materials and Methods, the Climet particle sizer accurately measures particle size in the 150- to 500-nm range by classifying particles in the following (unequal) size ranges: 150–199, 200–299, and 300–499 nm. We observed that for all human subjects after administration of air only, saline, and surfactant, the distribution of particle sizes within these three particle size ranges showed no statistical variance with time after administration of air, saline, or surfactant. Dividing the three size bins into eight bins of equal size ranges (i.e., spanning 50 nm) and assuming homogeneous particle distribution in the ranges 200–299 and 300–499 nm, the predominant size of exhaled aerosol particles for all subjects was 150–199 nm. This did not change after saline or surfactant administration.
In our studies, performed over the course of 3 months (February through April) in the spring of 2004, high-producer subjects tended to remain high producers, as defined here. Thus, the six subjects defined as high producers on the basis of our baseline measurements (Fig. 1) accounted for 98.16% of all expired particles for baseline, 78.15% of all particles in the case of saline delivery, and 62.43% of total expired aerosol in the case of surfactant delivery. Whether high-producer individuals are more prone, barring mitigation of bioaerosol expiration, to spread inhaled infectious diseases such as influenza, tuberculosis, and severe acute respiratory syndrome needs to be clarified by further studies.
Conclusion
We have found that, among a group of 11 healthy human subjects, two distinct groups of individuals can be identified, the one expiring on average many more bioaerosol droplets than the other. Delivery of isotonic saline can markedly diminish the number of expired bioaerosol particles among the high-producer subjects for up to 6 h after inhalation. In vitro experiments suggest that the mechanism of action of the saline suppression of exhaled bioaerosol relates to alteration of the surface properties of the airway-lining fluid, notably surface tension. Thus, delivery of a surfactant solution to the lungs actually magnified exhaled bioaerosol expiration, consistent with in vitro experiments that show its effect on droplet formation is unlike that of isotonic saline. Many questions must be resolved by future studies, including those related to the roles of other physical properties of lung mucus, like surface elasticity and surface viscosity, the role of physiological and/or environmental conditions on expired bioaerosol number, and those touching on dose and duration of effect. Recent studies on the characteristics of atmospheric aerosols or those created by nebulizers and inhalation devices have suggested a primary role for surface tension and viscosity in the formation and size distribution of droplets (26–30). Additionally, further investigations into the role of nanoparticles in airborne transmission are warranted. Clearly, the effect of normal saline solution, as well as other inhaled agents that alter surface properties of the lung-lining fluid, on transmission of airborne pathogens needs to be explored further.
Supplementary Material
Acknowledgments
We thank Thomas Meyer, Michael Lipp, Gareth McKinley, Mark Gabrielson, Robert Langer, Alexander Klibanov, David Weitz, Steve Calderwood, and John Treanor for helpful insight and technical assis-tance. We also acknowledge the work of Sascha Roeder, Bernhard Müllinger, Sabine Haeussermann, Christiane Herpich, Martina Schulte and Joseph Gebhart. Funding for the simulated cough experiments was provided by the Technical Support Working Group of the U.S. Government. We also thank Pulmatrix Incorporated, for financial support, formulation preparation, and data analysis.
Author contributions: D.A.E., J.C.M., P.B., J.P.K., H.A.S., and G.S. designed research; D.A.E., J.C.M., P.B., J.P.K., K.S., H.A.S., E.N., and G.S. analyzed data; D.A.E., J.C.M., J.P.K., and E.N. wrote the paper; and P.B., J.P.K., K.S., and G.S. performed research.
Abbreviations: DPPC, 1,2-dipalmitoyl-sn-glycero-3-phosphocholine; POPG, 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphoglycerol; LBG, locust bean gum.
References
- 1.Roy, C. J. & Milton, D. K. (2004) N. Engl. J. Med. 350, 1710–1712. [DOI] [PubMed] [Google Scholar]
- 2.Sattar, S. A. & Ijaz, M. K. (1987) in CRC Critical Reviews in Environmental Control, ed. Logan, T. (CRC, Philadelphia), pp. 89–131.
- 3.Riley, E. C., Murphy, G. & Riley, R. L. (1978) Am. J. Epidemiol. 107, 421–432. [DOI] [PubMed] [Google Scholar]
- 4.Frankova, V. (1975) Acta Virol. 19, 35–40. [PubMed] [Google Scholar]
- 5.Harmory, B. H., Couch, R. B., Douglas, R. G. J., Black, S. H. & Knight, V. (1972) Proc. Soc. Exp. Biol. Med. 139, 890–893. [DOI] [PubMed] [Google Scholar]
- 6.Wilkinson, P. J. & Donaldson, A. I. (1977) J. Comp. Pathol. 87, 497–501. [DOI] [PubMed] [Google Scholar]
- 7.Hyslop, N. S. (1965) J. Comp. Pathol. 79, 119–126. [DOI] [PubMed] [Google Scholar]
- 8.Leclair, J. M., Zair, J. A., Lenin, M. J., Congdon, R. G. & Goldman, D. A. (1980) N. Engl. J. Med. 302, 450–453. [DOI] [PubMed] [Google Scholar]
- 9.Ratanasethakl, C. & Cumming, R. B. (1983) Aust. Vet. J. 60, 209–213. [DOI] [PubMed] [Google Scholar]
- 10.Sattar, S. A. & Ijazm, M. K. (2002) in Manual of Environmental Microbiology, eds. Hurst, C. J. & Knudson, G. R. (Blackwell, Oxford), 2nd Ed., pp. 871–883.
- 11.Varma, J. K, Greene, K. D., Reller, M. E., Delong, S. M., Trottier, J., Nowicki, S. F., DiOrio, M., Koch, E. M., Bannerman, T. L., York, S. T., et al. (2003) J. Am. Med. Assoc. 260, 2709–2712. [DOI] [PubMed] [Google Scholar]
- 12.Bolister, N. J., Johnson, H. E. & Wathes, C. M. (1992) Epidemiol. Infect. 109, 121–131. [PMC free article] [PubMed] [Google Scholar]
- 13.Dennis, D. T., Inglesby, T. V., Henderson, D. A., Bartlett, J. G., Ascher, M. S., Eitzen, E., Fine, A. D., Friedlander, A. M., Hauer, J., Layton, M., et al. (2001) J. Am. Med. Assoc. 285, 2763–2773. [DOI] [PubMed] [Google Scholar]
- 14.Fennelly, K. P., Martyny, J. W., Fulton, K. E., Orme, I. M., Cave, D. M. & Heifets, L. B. (2004) Am. J. Respir. Crit. Care Med. 169, 604–609. [DOI] [PubMed] [Google Scholar]
- 15.Fairchild, C. I. & Stampfer, J. F. (1987) Am. Ind. Hyg. Assoc. J. 48, 948–949. [DOI] [PubMed] [Google Scholar]
- 16.Papineni, R. S. & Rosenthal, F. S. (1997) J. Aerosol Med. 10, 105–116. [DOI] [PubMed] [Google Scholar]
- 17.Moriarty, J. A. & Grotberg, J. B. (1999) J. Fluid Mech. 397, 1–22. [Google Scholar]
- 18.King, M., Brock, G. & Lundell, C. (1985) J. Appl. Physiol. 58, 1776–1782. [DOI] [PubMed] [Google Scholar]
- 19.Cataldo, D., Cataldo, D., Foidart, J. M., Lau, L., Bartsch, P., Djukanovic, R. & Louis, R. (2001) Chest 120, 1815–1821. [DOI] [PubMed] [Google Scholar]
- 20.Weibel, E. R. (1979) Bull. Eur. Physiopathol. Respir. 15, 999–1013. [PubMed] [Google Scholar]
- 21.Schurch, S., Gehr, P., Im Hof, V., Geiser, M. & Green, F. (1990) Respir. Physiol. 80, 17–32. [DOI] [PubMed] [Google Scholar]
- 22.Im Hof, V., Gehr, P., Gerber, V., Lee, M. M. & Schurch, S. (1997) Respir. Physiol. 109, 81–93. [DOI] [PubMed] [Google Scholar]
- 23.Edwards, D. A., Brenner, H. & Wasan, D. T. (1991) in Processes and Rheology (Butterworth–Heinemann, Boston), pp. 161–190.
- 24.Burkdolder, H. C. & Berg, J. C. (1974) AIChE J. 20, 872–880. [Google Scholar]
- 25.Cox, C. S. (1995) in Bioaerosols Handbook, eds. Cox, C. S. & Wathes, C. M. (Lewis, Boca Raton, FL), pp. 15–26.
- 26.Steckel, H. & Eskandar, F. (2003) Eur. J. Pharmacol. Sci. 19, 443–455. [DOI] [PubMed] [Google Scholar]
- 27.Dayal, P., Shaik, M. S. & Singh, M. (2004) Pharmacol. Sci. 93, 1725–1742. [DOI] [PubMed] [Google Scholar]
- 28.Sukhapan, J. & Brimblecombe, P. (2002) Sci. World J. 27, 1138–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spanoghe, P., Steurbaut, W., Van Eeckhout, H. & Van der Meeren, P. (2002) Meded. Rijksuniv. Gent. Fak. Landbouwkd. Toegep. Biol. Wet. 67, 129–132. [PubMed] [Google Scholar]
- 30.McCallion, O. N., Taylor, K. M., Thomas, M. & Taylor, A. J. (1995) Pharmacol. Res. 12, 1682–1688. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.