Abstract
Background
Age-related dementia, most commonly caused by Alzheimer disease or cerebrovascular factors (vascular dementia), is a major public health threat. Chronic arterial hypertension is a well-established risk factor for both types of dementia, but the link between hypertension and its treatment and cognition remains poorly understood. In this scientific statement, a multidisciplinary team of experts examines the impact of hypertension on cognition to assess the state of the knowledge, to identify gaps, and to provide future directions.
Methods
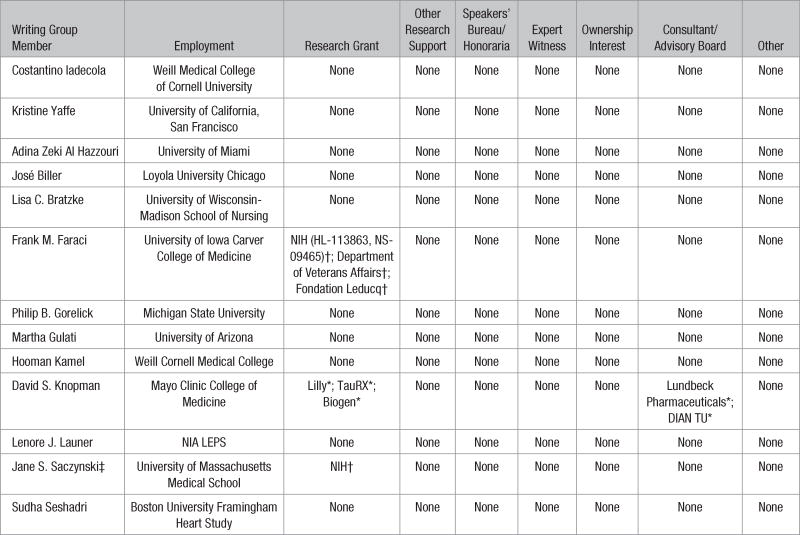
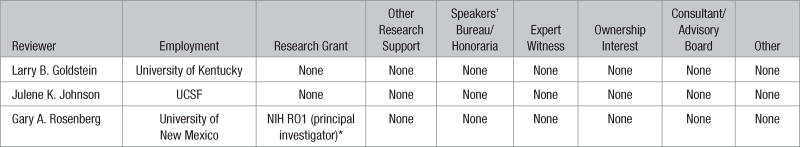
Authors with relevant expertise were selected to contribute to this statement in accordance with the American Heart Association conflict-of-interest management policy. Panel members were assigned topics relevant to their areas of expertise, reviewed the literature, and summarized the available data.
Results
Hypertension disrupts the structure and function of cerebral blood vessels, leads to ischemic damage of white matter regions critical for cognitive function, and may promote Alzheimer pathology. There is strong evidence of a deleterious influence of midlife hypertension on late-life cognitive function, but the cognitive impact of late-life hypertension is less clear. Observational studies demonstrated a cumulative effect of hypertension on cerebrovascular damage, but evidence from clinical trials that antihypertensive treatment improves cognition is not conclusive.
Conclusions
After carefully reviewing the literature, the group concluded that there were insufficient data to make evidence-based recommendations. However, judicious treatment of hypertension, taking into account goals of care and individual characteristics (eg, age and comorbidities), seems justified to safeguard vascular health and, as a consequence, brain health.
Keywords: AHA Scientific Statements, Alzheimer disease, biomarkers, blood pressure, clinical trials, neuroimaging, therapy, vascular cognitive impairment
Dementia is a progressive and typically irreversible deterioration of cognitive function that is most often seen in older adults.1 Dementia is one of the most common neurological disorders, affecting an estimated 30 to 40 million people worldwide. The number of individuals with dementia is anticipated to triple by 2050 as a result of the aging of the population, demographic shifts, and lack of disease-modifying treatments, with an associated cost exceeding $1.1 trillion.2 Alzheimer disease (AD) and cerebrovascular diseases are the 2 leading causes of cognitive impairment, accounting for ≈80% of cases and often having a mixture of both pathologies.3 The term vascular cognitive impairment (VCI) indicates the entire range of cognitive deficits caused by vascular factors, whereas vascular dementia refers to the more severe cases of VCI in which the cognitive decline affects day-to-day functioning negatively.3
Among vascular risk factors, chronic arterial hypertension is a major contributor to cognitive impairment.3 Hypertension, a highly prevalent disease affecting an estimated 80 million people in the United States and 1 billion individuals worldwide,4 is the leading cause of global disease burden and overall health loss.5 The brain is one of the main target organs affected by hypertension. Thus, excluding age, hypertension is the most important risk factor for cerebrovascular pathology leading to stroke and dementia. The harmful effects of hypertension on cognitive function have been recognized at least since the 1960s, when a study on psychomotor speed of air traffic controllers and pilots demonstrated reduced performance in individuals with hypertension.6 Hypertension has been associated with reduced abstract reasoning (executive dysfunction), slowing of mental processing speed, and, less frequently, memory deficits.7
Although dementia caused by AD and vascular dementia have traditionally been considered distinct nosological entities, increasing evidence indicates that these conditions often coexist.8,9 Thus, the neuropathological hallmarks of AD, amyloid plaques and neurofibrillary tangles (NFTs), are frequently associated with microcerebrovascular and macro-cerebrovascular lesions in 40% to 50% of individuals with a clinical diagnosis of AD.10,11 In addition, ischemic lesions markedly enhance the impact of AD pathology on cognitive function.12,13 Furthermore, traditional cardiovascular risk factors have been suggested to play a role in AD,14 and some estimates indicate that risk factor reduction, including treatment of hypertension, could reduce the incidence of clinically diagnosed AD up to 30%.15
Cerebral blood vessels are the main target of the deleterious effects of hypertension on the brain.16 The resulting structural and functional cerebrovascular alterations underlie many of the neuropathological abnormalities responsible for the cognitive deficits, including white matter damage, micro-infarcts, microbleeds, silent brain infarcts, and brain atrophy.17 Hypertension is the most powerful modifiable risk factor for the cerebrovascular damage, and the dramatic reduction in stroke mortality over the past several decades has been attributed to the treatment of hypertension.18,19 Surprisingly, however, the impact of hypertension and its treatment on cognitive impairment has been more difficult to assess, and several key questions remain to be answered.
Considering the growing public health import of dementia,1 a critical appraisal of current knowledge of the cognitive function associated with hypertension is warranted. Although the role of vascular risk factors in cognitive impairment has been addressed in other American Heart Association statements,3 there is a strong rationale for an in-depth evaluation of the specific role of hypertension. First, the effect of hypertension was previously examined in the context of several other risk factors causing vascular dementia, and a detailed analysis of the evidence was not provided.3 Second, new epidemiological data and imaging approaches have provided further insight into the relationship between hypertension and dementia and the cognitive domains that are predominantly affected. Third, the interaction between hypertension and AD pathology, a critical issue for both conditions, was not previously examined in detail. Therefore, an expert assessment is needed to update healthcare professionals on recent advances made in this field, to bring to the forefront outstanding questions, and to chart a path for future research directions.
The present statement seeks to provide an appraisal of the contribution of hypertension to age-related cognitive dysfunction. This statement refers primarily to the effects of chronic arterial hypertension. For simplicity, however, the term hypertension is used throughout the text. We first examine the effects of hypertension on the pathobiology of the cerebral circulation, focusing on the structural and functional changes induced by chronic elevations in blood pressure (BP) on the cerebral vasculature. The cognitive domains most affected by hypertension are then reviewed, highlighting their unique features and their differences from other causes of dementia. The evidence from observational studies of the effect of hypertension on cognition is presented, followed by evidence from randomized, clinical trials of BP treatment and on the cognitive effect of hypertension treatment over the life course. Subsequent sections focus on the interaction of hypertension with other risk factors and the association between hypertension and AD. The final section provides an overall summary of the evidence, identifies knowledge gaps, and provides future directions for advancing the field.
Methods
Authors with expertise in vascular pathophysiology, epidemiology, neuroimaging, neuropathology, and cognitive science pertaining to the effects of hypertension on the brain were selected to contribute to this statement. Selection of the writing group was performed in accordance with the American Heart Association conflict-of-interest management policy. Topics for the statement were identified by the chair and co-chair and revised with input from the writing group. Subgroups of experts for each of the topics were established and charged with writing the section of the statement pertaining to their expertise. Each subgroup performed a search of the relevant English literature considered for inclusion in this statement using an up-to-date search strategy of reference databases and appropriate search terms. In addition to identifying the article reporting the main cognitive outcomes, we also reviewed, if relevant, the report on the primary outcome of the trial and on the trial design. Because of the heterogeneity of the studies spanning several decades, rigid inclusion/exclusion criteria could not generally be applied. We did not use a data abstraction tool. Conflicts were resolved by group consensus. The search also included a review of bibliographies and manual searches of key articles. Drafts of each section were written and sent to the chair and co-chair of the writing group for editing and elimination of redundancy. The edited sections were returned to the group members for clarification and revision and sent back to the chair and co-chair. The sections were then assembled in a single document that was sent back to the members for discussion and comments. On the basis of these discussions and consensus, the sections were then edited accordingly by the primary author and returned to the chair and co-chair for further editing. The final document was circulated among all members of the writing group, and once consensus was reached, the final document was submitted for independent peer review. After peer review, the final document was approved for publication by the American Heart Association Council on Hypertension, Stroke Council, and Science Advisory and Coordinating Committee. After careful review of the available data, the group determined that there were insufficient data to make evidence-based recommendations. Therefore, specific recommendations are not provided.
Effects of Hypertension on Cerebrovascular Structure and Function
The cerebral vasculature is the main target of the deleterious effects of hypertension on the brain. Most of the vascular alterations induced by hypertension contribute to cognitive impairment by leading to hypoperfusion, ischemic and hemorrhagic stroke, and white matter injury. This section outlines the major changes that occur in the cerebral vasculature during hypertension, focusing on the structure and function of large and small cerebral vessels, progression of atherosclerosis, and blood-brain barrier (BBB) integrity.
Vascular Structure
In humans as in animal models, hypertension is associated with changes in structure of the vascular wall of large, medium, and small cerebral vessels (arterioles, capillaries, and venules). At the different levels of the cerebrovascular tree, endothelial and smooth muscle cells are closely associated with brain cells (astrocytes, neurons, microglia) and perivascular cells, constituting the neurovascular unit.20
Atherosclerosis
Hypertension promotes atherosclerosis in both extracranial and intracranial arteries feeding the brain and accelerates the progression of intracranial atherosclerosis.21 Advanced atherosclerotic lesions impair blood flow and are a major site of thrombogenesis.
Vascular Remodeling and Stiffening
Hypertrophic remodeling consists of hypertrophy of smooth muscle cells resulting in an increased cross-sectional area of the arterial or arteriolar wall and a reduction in the vessel lumen.22,23 Inward remodeling is a rearrangement of the vessel wall that results in a reduction in lumen diameter.24 Both forms of remodeling are seen in cerebral arteries and arterioles in experimental models of hypertension, with supporting evidence in human hypertension as well.23–25 Chronic hypertension also induces deposition of collagen and fibronectin and elastin fragmentation of the vessel wall, leading to increased stiffness of large cerebral arteries.26 In smaller arterioles, as a result of disruption of the BBB (see Blood-Brain Barrier below), an inflammatory reaction may ensue that is associated with the production of reactive oxygen species and protease upregulation.27 Clinical measures of aortic and large-artery stiffening are good predictors of cerebrovascular events and VCI.28–30
Small-Vessel Disease
Hypertension causes typical alterations in small arteries and arterioles supplying the subcortical and basal ganglia white matter, resulting in small-vessel disease (SVD), a major cause of lacunar strokes and cerebral hemispheric white matter damage.17 These subcortical vessels might be more vulnerable to the mechanical stresses caused by hypertension because of their short linear path from larger vessels at the base of the brain.16,31 The typical pathological substrate of hypertensive SVD is arteriolosclerosis,17 which is characterized by loss of smooth muscle cells, deposits of fibro-hyaline material, narrowing of the lumen, and thickening of the vessel wall (lipohyalinosis). In more advanced cases, fibrinoid necrosis of the vessel wall results in vessel rupture and hemorrhage (intrace-rebral hemorrhage and microbleeds).
Microvascular Rarefaction
Loss of microvessels occurs in hypertension and during aging.32,33 Such changes, in concert with vascular remodeling and stiffening, are thought to contribute to the progressive reduction in resting cerebral blood flow (CBF) associated with hypertension.34–36 Rarefaction may also reduce the potential for a compensatory collateral circulation in conditions of vascular insufficiency or occlusion.
Mechanisms
The renin-angiotensin-aldosterone system and angiotensin II are key determinants of structural changes during hypertension. The renin-angiotensin-aldosterone system is a major therapeutic target in patients with essential or primary hypertension,37 but the mechanisms of renin-angiotensin-aldosterone system activation remain to be established. Whereas increases in circulating angiotensin II occur in renovascular and obesity-associated hypertension,38 plasma angiotensin II is not elevated in the majority of patients with essential hypertension.39 Rather, local angiotensin II production and signaling in brain, vessels, and other tissues may drive hypertension and the associated vascular changes.37,40
Angiotensin II has also been implicated in plaque composition and instability, which may underlie the effects of hypertension on atherosclerosis progression.41,42 Interestingly, intracranial atherosclerosis has also been linked to AD. It has been postulated that the hypoperfusion caused by arterial stenosis may lead to reduced amyloid-β (Aβ) clearance and increased Aβ production by activating β-secretase, a protease involved in Aβ cleavage from the amyloid precursor protein.43 In turn, Aβ can promote atherosclerosis by inducing inflammation, endothelial dysfunction, and oxidative stress.20,43 Angiotensin II can also promote Aβ cleavage from amyloid precursor protein by activating β- and γ-secretase and aggravate the vascular dysfunction induced by Aβ.44,45
Angiotensin II can induce inward and hypertrophic remodeling and vascular stiffening.22 Remodeling is mediated by free radicals produced by the enzyme NADPH oxidase and hypertrophy by activation of epidermal growth factor receptor probably resulting from mechanical stress and other mechanisms.46,47 Mechanisms of large-artery stiffening may also include mechanical stress leading to activation of p38 mitogen-activated protein kinase and T-cell–mediated interleukin-17 production.48 The factors mediating rarefaction have not been elucidated, but vascular oxidative stress may suppress the production and action of trophic factors, resulting in vascular atrophy.27 In addition, loss of endothelial nitric oxide synthase–derived nitric oxide may also be a factor in micro-vascular rarefaction.32,33 Aging and hypertension may act in an additive fashion because hypertension causes premature rarefaction with aging.32 The mechanisms of hypertension-induced SVD are thought to be diverse and may include endothelial dysfunction, BBB alterations leading to extravasation of plasma proteins, vascular inflammation, and microthrombi (Blood-Brain Barrier section).
Vascular Function
Chronic hypertension exerts profound effects on cerebrovascular function, disrupting major factors regulating the cerebral circulation. These include endothelium-dependent mechanisms, neurovascular coupling, and autoregulation.
Endothelium-Dependent Mechanisms
Endothelial cells are a major determinant of vascular tone. By the release of vasoactive factors such as nitric oxide and prostanoids, along with endothelium-dependent hyperpolarization, these cells influence the contractile state of smooth muscle and regulate CBF in response to neurochemical, metabolic, and mechanical signals (shear stress acting on the vessel lumen).49–51 Therefore, endothelial cells are critical in regulating the distribution of microvascular flow at the local level.22,52 In addition, the endothelium protects vessels against thrombosis, atherogenesis, and formation of vascular Aβ deposits in AD.22,49 Hypertension disrupts endothelial cell function, leading to a reduction of the ability of endothelial cells to regulate microvascular flow and to exert their antithrombotic and antiatherogenic effects.22 Thus, changes in endothelial function may play a role in the effects of hypertension in reducing resting CBF and promoting atherosclerosis and Aβ accumulation and have been associated with stroke, VCI, white matter disease, and AD.53–56
Neurovascular Coupling
Increases in cellular activity in the brain require proportional increases in blood flow, often called neurovascular coupling or functional hyperemia.27,57 Neurovascular coupling ensures adequate delivery of oxygen, glucose, and other nutrients during cellular activation, along with removal of metabolic byproducts. In response to neural activation, neurons and glia produce signals that communicate with vascular cells, resulting in increases in blood flow highly restricted to the activated areas.27,57 In experimental models as in humans, hypertension attenuates the increase in CBF induced by neural activity.16,58 The resulting mismatch between energy demands and blood flow delivery, along with reduced basal CBF, is thought to contribute to the cognitive decline induced by hypertension.16,27
Autoregulation
In humans as in animals, CBF remains relatively constant over a wide range of mean arterial pressures (perfusion pressures; ≈60–150 mm Hg),50,59,60 a property of the cerebral circulation called autoregulation. Cerebral autoregulation depends on the intrinsic ability of vascular muscle to constrict when transmural pressure increases (myogenic tone and reactivity) and to relax when transmural pressure decreases. Hypertension leads to a right shift of the relationship between BP and CBF (autoregulation curve), so that the same level of cerebral perfusion occurs at higher levels of BP.61 This shift protects the cerebral circulation from the damaging effects of high BP but can also cause ischemic brain injury if sudden or large reductions in BP occur. Even in normotensive individuals, sudden large rises in arterial pressure can overwhelm autoregula-tory mechanisms, resulting in massive CBF increases, BBB damage, and cerebral edema, as observed in hypertensive encephalopathy and the posterior reversible encephalopathy syndrome.62–64 In turn, acute hypotension leads to decreases in CBF, causing “watershed” infarcts in border zones between adjacent arterial territories.27,50
Mechanisms
Hypertension-induced vascular oxidative stress has been implicated in the alterations in endothelium-dependent responses and functional hyperemia. In models of angiotensin II–dependent hypertension, NADPH oxidase is a major source of oxidative stress,16 but the cells producing the radicals at the vascular level have not been identified. Evidence of oxidative stress has been reported in the brain of individuals with SVD and white matter damage.65 The mechanisms of the shift of autoregulation may involve hypertension-induced changes in myogenic responses and mechanical consequences of vascular remodeling and stiffening.16 The shift in autoregulation is especially damaging to the periventricular white matter, which is supplied by terminal branches arising from separate arterial territories and thus is most susceptible to hypoperfusion.66,67 Accordingly, the severity of white matter injury correlates with the magnitude of autoregulatory dysfunction.68 In genetic models of hypertension, there is evidence that increased myogenic tone, endothelial dysfunction, and inward remodeling can be prevented with pharmacological targeting of the renin-angiotensin-aldosterone system.69 However, much less is known about the extent to which hypertension-induced vascular changes are reversible. Further work is needed to determine which cerebrovascular end points that are affected by hypertension are also reversible and amenable to treatment.
Blood-Brain Barrier
The structural and molecular features of the BBB are key for normal brain function in that they control the bidirectional movement of ions, molecules, and cells between blood and brain.70,71 The BBB results from the unique properties of cerebral endothelial cells that are adjoined by tight junction, have minimal vesicular transport across their cytoplasm (transcytosis), and are enriched with plasmalemmal influx and efflux transporters regulating the exchange of molecules between blood and brain and vice versa.70,71 However, BBB integrity is also influenced by other cell types, including astrocytes and pericytes (intramural vascular cells present at the level of capillaries), as well as the extracellular matrix.70–72
Hypertension has profound effects on the BBB. Chronic hypertension is associated with BBB disruption in animal models and in humans.73,74 Loss of BBB integrity may be an early event in the pathogenesis of SVD.73,75,76 In genetically hypertensive rats as in models of angiotensin II–dependent hypertension, reductions in CBF, loss of tight junction proteins, loss of BBB integrity, and white matter lesions have all been described.77,78 Loss of BBB integrity has also been described in hypertensive patients79,80 in association with SVD and white matter damage.74,75,79 The mechanisms of the effect have not been fully elucidated, but one hypothesis is that hypoxia, caused by reduced CBF in susceptible white matter regions, leads to activation of hypoxia inducible factor-1α–dependent genes, including metalloproteases, which may promote BBB damage.81 Cellular elements beside endothelial cells are also involved in the BBB dysfunction. Pericytes, which are required for maintenance of the BBB,82 may undergo degeneration during hypertension,83 suggesting that loss or dysfunction of these cells may also contribute to disruption of BBB integrity. Extravasation of plasma proteins leading to vascular and perivascular inflammation and microvascular thrombosis are thought to be key pathogenic consequences of the BBB disruption contributing to white matter damage through inflammatory mediators and reactive oxygen and nitrogen species, but conclusive evidence is lacking, especially in humans.27
Summary of Evidence
Hypertension induces adaptive changes in cerebral blood vessels that reduce stress on the vessel wall and protect downstream arterioles, capillaries, and venules from potentially damaging fluctuations in arterial pressure.23 However, these structural alterations, in concert with the associated impairment of critical vascular regulatory mechanisms, may result in CBF reductions in regions of the subcortical white matter at risk for vascular insufficiency. Angiotensin II–dependent vascular oxidative stress is a critical factor in both the structural and functional cerebrovascular alterations induced by hypertension. In addition, alterations of endothelial cells and the BBB represent a key early event in SVD, but the pathogenic mechanisms remain poorly defined. An unexpected reciprocal interaction between hypertension and AD pathology has emerged whereby the hypertensive vasculopathy exacerbates the accumulation of Aβ in brain and acts in concert with Aβ to suppress vital cerebrovascular regulatory mechanisms. Although it remains to be established whether the deleterious effects of hypertension on cognition are reversible or lessened by treatment, experimental evidence suggests that some vascular changes induced by hypertension may be reversible with appropriate treatments.
Cognitive Domains Targeted by Hypertension
This section describes the specific cognitive domains targeted by hypertension. Although the majority of early studies examining cognitive function in individuals with hypertension such as the MMSE (Mini-Mental Status Examination) have focused on global cognitive outcomes or composite measures of several cognitive tests, there is a growing literature on specific domains of cognitive function and possible differential association with hypertension. Studies focused on identifying specific domains may contribute to identifying the mechanism by which hypertension impairs cognitive function, for example, microvascular effects versus brain atrophy, and informing the development, timing, and evaluation of pharmacological and behavioral interventions, for example, disease self-management and medication adherence. Cognitive function is assessed in studies of hypertension with a number of measures. The most common measures administered in these studies assess the specific domains of memory, executive function, and processing speed.
Memory
Memory function includes tests of short-term memory, verbal learning, and working memory. Common short-term memory tasks include the Digits Forward Test, in which the subject is asked to repeat strings of numbers in same order in which they were read,84 and immediate recall tasks, in which the subject is asked to recite back a list of words immediately after hearing them (eg, first trial of the Rey Auditory Learning Test).85,86 Delayed memory is then assessed, usually after a 30-minute interval, with recall of short verbal stories or lists. Delayed memory can also be evaluated with 5-minute delayed recall, after a brief distraction task, of a list of words that have been used in sentences to promote encoding.84,87 Working memory tasks also tap into executive function. The most common measure is the Digits Backwards Test, in which the subject is asked to repeat a string of words in the reverse order that they were read.84
Executive Function
Executive function involves multiple brain processes and consequently is the cognitive domain that is most difficult to assess and has the most heterogeneity in measurements across studies. Of note, the widely used MMSE does not test domains related to executive function. Executive function is of particular importance for daily life because of the role it plays in decision making and problem solving, critical tasks for self-management of chronic illnesses. The most common tests used were the Controlled Oral Word Association Test (word fluency), category fluency (eg, animal naming), and the Trail Making Test Part B. The word fluency test requires subjects to generate as many words as possible beginning with the same letter of the alphabet (F, A, or S) in 60 seconds.88,89 Category fluency, in which subjects are asked to name as many words as possible in a single category, for example, animals, is also used but is less difficult.90 On average, older adults without cognitive impairment generate 12 to 16 words per minute and 19 to 22 animals per minute.89 The Trail Making Test has 2 parts, A and B.91,92 In part A, the subject is timed while drawing a continuous line to connect consecutive numbers (1–25). Part B times how long a subject takes to draw a continuous line connecting alternating letters (A–L) and numbers (1–13). The total time for Part B or the difference between the 2 parts (time for part B minus time for part A) is used as the outcome, with higher scores reflecting poorer performance. The difference score attempts to remove the speed element from the test evaluation and thus is more commonly used to examine executive function.89
Speed of Processing
Although not a cognitive domain, reduced speed of processing leads to declines in other domains. Many tests of processing speed also tap into attention and may be referenced as attention tasks. The 2 most common speed of processing/attention tasks are the Digit Symbol Substitution Test and the Trail Making Test Part A. The Digit Symbol Substitution Test is a paper and pencil task in which the subject is given 90 seconds to translate numbers into symbols using a key at the top of a page.84 The total number of correct responses is used as the score. The Trail Making Test Part A, described above, uses the time required to draw a continuous line to connect numbers (1–25), with higher scores reflecting poorer (slower) performance.
Domains Affected by Hypertension Versus Clinically Diagnosed AD
There is moderately strong evidence to support the claim that impaired and declining speed of processing and executive function are the most commonly encountered cognitive changes associated with hypertension.93–98 The pattern of cognitive impairment associated with hypertension is often distinguished from the pattern associated with neurodegenerative dementias such as AD by the lack of consistent findings for an impact of hypertension on memory function, a defining characteristic of clinically diagnosed AD. However, the issue is complicated by the fact that hypertension, in addition to acting through cerebrovascular mechanisms, may be a risk factor for AD pathology (Effects of Hypertension on Cerebrovascular Structure and Function section and Hypertension and AD section).
Summary of Evidence and Methodological Considerations
Although the evidence for an effect of late-life hypertension on specific cognitive domains is not conclusive, a few studies suggest that controlling BP from midlife to late life may provide a strategy to decrease the risk of late-life cognitive impairment, particularly in processing speed and executive function.94,96,99,100 There is stronger and more consistent evidence for an association with systolic BP (SBP) than for diastolic BP (DBP), although this comparison has not been made uniformly across studies. This question warrants further examination.
Several methodological issues prevent direct comparison or meta-analysis of studies. Assessment of cognitive function is not standardized across studies, resulting in inconsistency in the domains assessed and even differences in the tests used to assess a single domain, with the most heterogeneity for the executive function. An effort by the National Institute of Neurologic Disorders and Stroke and the Canadian Stroke Network to harmonize assessment batteries for VCI offers standardized batteries of well-validated instruments for various interview lengths (eg, 60, 30, and 5 minutes).101 In addition, there is considerable variability in the potentially confounding factors controlled across studies of hypertension and cognition. Most studies adjust for age, sex, and education. Fewer adjust for additional cardiovascular risk factors such as smoking, comorbid conditions (eg, diabetes mellitus), and body mass index.
Hypertension and Cognition: Observational Studies
The goal of this section is to summarize the evidence from observational studies on the relationship between BP and hypertension and cognitive health. The section is organized into 2 main subsections: evidence from cross-sectional studies and evidence from longitudinal studies. Each section is then further divided into the following categories based on the age at which BP was measured: midlife (age, 40–64 years), late life (age, 65–84 years), and oldest old (age ≥85 years). We report findings on global cognition using measures such as the MMSE or the modified MMSE, and we report findings on specific cognitive domains such as executive function, memory, and processing speed (Cognitive Domains Targeted By Hypertension section).
Cross-Sectional Evidence on the Association Between BP and Cognition
Late-Life BP
Evidence from cross-sectional studies has focused primarily on BP and cognition in late life. The evidence is mixed, with some studies suggesting that exposure to high BP is associated with worse cognitive function but other studies reporting the opposite association, a U-shaped association, or no association.
Several studies that examined the cross-sectional association between BP in late life and cognition suggested that having hypertension or exposure to high BP is associated with worse cognitive function.97,102–105 Examples of such studies include the ARIC study (Atherosclerosis Risk in Communities) and NHANES (the National Health and Nutrition Examination Survey). Early findings from the ARIC study showed that subjects with a diagnosis of hypertension, defined as SBP ≥160 mm Hg or DBP ≥90 mm Hg, had lower scores on tests of processing speed and word fluency compared with those without hypertension.97 More recent findings from NHANES similarly showed that having hypertension or high BP (SBP ≥140 mm Hg or DBP ≥90 mm Hg) at ≥70 years of age was associated with worse performance on a test of global cognition.105 However, other studies reported the opposite; that is, exposure to high BP in late life was associated with better cognitive performance.106,107 For example, in the Honolulu-Asia Aging Study, having an SBP ≥160 mm Hg was associated with 51% lower odds of poor performance on a test of global cognition compared with having an SBP of <100 mm Hg.106 A few other studies reported a U-shaped association.108 For example, in less educated members of the Baltimore Longitudinal Study on Aging, both high and low DBPs were associated with poor performance on a neuropsychological test battery, including tests of executive function and confrontation naming (Boston Naming Test).108 Furthermore, the Framingham Heart Study reported no cross-sectional association between BP in late life and cognitive function.109
Oldest Old BP (≥85 Years of Age)
Findings from a study in centenarians in Australia showed a cross-sectional association between BP and cognition such that higher SBP was correlated with better performance on a test of global cognition.110 More recent findings from the 90+ Study in a retirement community in Southern California showed that the prevalence of hypertension did not differ between those who are cognitively normal and those with mild cognitive impairment (MCI).111 However, the prevalence of hypertension was greatest in those with nonamnestic MCI compared with other MCIs, thus suggesting that hypertension-related cognitive impairment involves skills other than memory.
Longitudinal Evidence on the Association Between BP and Cognition
Longitudinal studies offer a better study design than cross-sectional studies by ensuring a temporal association between a putative exposure and outcome. When repeated assessments of cognitive function are available, a rate of cognitive decline can also be calculated that may provide insight into the cause of cognitive impairment.
BP in Adolescence
A recent study in adolescents of the Seychelles Child Development study failed to find associations between BP measured at 12 to 15 years of age and cognitive function measured at both 17 and 19 years of age.112 It may be that underlying physiological mechanisms linking hypertension and cognition may not be in play at such a young age. It is also possible that the tests used do not capture the variability in cognition that is associated with high BP at a young age.
Midlife BP
Recent findings in subjects of the CARDIA) study (Coronary Artery Risk Development in Young Adults) with mean age of 25 years at baseline showed that higher burden of SBP over 25 years from young adulthood to middle age was associated with worse performance on several cognitive tests in midlife, including verbal memory, processing speed, and executive function, when the cohort was a mean of 50 years of age.93 CARDIA is among the few studies that examined early to midlife BP and cognitive function in midlife. There is more substantial evidence addressing the longitudinal association between midlife BP and cognitive function in late life.98,103,106,113–115 Overall, these studies consistently showed that having high SBP or a hypertension diagnosis in midlife was associated with worse cognitive performance in late life. Examples of such studies include the Framingham study,113 which showed that higher SBP and DBP (increments of 10 mm Hg) in stroke-free individuals in midlife were associated with worse performance on a composite global cognitive score and measures of attention and memory. Similarly, in the Honolulu-Asia Aging Study,106 having a high SBP (≥160 mm Hg) in midlife was associated with a 2-fold increased risk of poor cognitive function on a test of global cognition 25 years later from a fully adjusted model. Findings from the Maine-Syracuse Longitudinal Study showed that higher baseline BP (increments of 10 mm Hg) was associated with worse cognitive performance and a decline in visualization and fluid abilities up to 20 years later.115 Even pre-hypertension, defined as SBP of 120 to 139 mm Hg/DBP of 80 to 89 mm Hg, in middle-aged women of the Women’s Health and Aging Project was associated with reduced cognitive function on processing speed and verbal memory a decade later.116
However, few other studies reported either a U-shaped association or no association between midlife BP and cognition in late life. For example, the SABRE study (Southall and Brent Revisited) showed a U-shaped association between low and high DBP and cognitive impairment, measured as a composite cognitive score, 20 years later.117 In addition, a recent study in members of a French cohort of middle-aged adults showed that elevated BP (SBP/DBP ≥130/85 mm Hg) or treatment in midlife was not associated with cognitive function, measured as a composite score and on subtests, nearly a decade later.118
Evidence on the association between midlife BP exposure and rate of cognitive change is scarce. Findings from the Framingham Offspring Cohort Study suggested that having midlife hypertension or an SBP ≥140 mm Hg was associated with faster annual decline in executive function.99 A recent study in subjects of the Maastricht Aging Study suggested that having midlife hypertension at baseline (ie, prevalent hypertension) was associated with cognitive decline at 6 and 12 years of follow-up on domains of verbal memory, executive function, and processing speed.96 The cognitive decline observed in individuals developing hypertension after baseline (ie, incident hypertension) was more modest compared with the decline in those with prevalent hypertension, potentially suggesting that duration of exposure also may play a role. Another recent study in members of ARIC showed that midlife hypertension was associated with a significantly greater decline in global cognitive function over 20 years. Similar findings were observed with higher SBP in whites but not in blacks.94
Late-Life BP
Several studies have examined the association between late-life BP and cognitive function measured several years after BP was measured. Findings from these studies are inconsistent. Several large-scale studies such as the Chicago Health and Aging Project,119 the Longitudinal Study on Aging,120 the Sacramento Area Latino Study on Aging,121 and WHIMS (Women’s Health Initiative Memory Study)122 failed to find an association. However, other studies reported a U-shaped association107,123 or a linear association.95,124,125 For example, results from the Duke Population Studies of the Elderly found a U-shaped association between SBP and cognitive decline over 3 years, although this association was observed only in white subjects.123 Results from ELSA (English Longitudinal Study on Aging) showed linear associations such that higher SBP and DBP were associated with lower scores on a global cognitive index and a memory index ≈8 years later. Further findings showed that having an SBP ≥160 mm Hg was associated with worse performance on the global and memory cognitive indexes 8 years later compared with having an SBP <140 mm Hg.124 The ARIC study95 showed that having hypertension at baseline, defined as SBP/DBP ≥140/90 mm Hg or taking antihypertensive medications, was associated with a decline in processing speed over a 6-year period. Findings in community-dwelling members without dementia of the Women’s Health and Aging Study II showed that having an SBP ≥160 mm Hg was associated with a greater incidence of cognitive impairment over a 9-year period as measured on executive function.125
Oldest Old BP
There are only a handful of longitudinal studies of BP and cognition in the oldest old. Findings from the Leiden 85-Plus study were inconsistent; although some findings did not show an association between BP and change in global cognitive function over 3 years,126 other analyses of the same study showed that a 10–mm Hg increase in SBP was associated with better cognitive performance on a global test and several domain-specific tests.127 These results were further confirmed in a more recent analysis.128 Furthermore, recent findings in subjects of the Newcastle 85+ study showed that having high BP, defined as SBP/DBP ≥130/85 mm Hg or treatment, was associated with better global cognitive function over 5 years.129
Summary of Evidence
There is consistent evidence that BP in midlife is associated with altered cognitive function in both midlife and late life. The association of BP in late life and oldest old age with cognition is less clear, with evidence of both harmful and beneficial effects of high BP on cognition. Associations were observed mostly with tests of global cognition and executive function, which is not surprising given that vascular risk factors influence executive functioning to a greater extent and are not necessarily related to memory (Cognitive Domains Targeted by Hypertension section). The inconsistency of results across studies, especially in older age, may reflect differences in the cognitive domains assessed, differences in aspects of study design, including length of follow-up and how the rate of cognitive change was modeled, differences in characteristics of the study populations and varying age ranges, and adjustment for shared determinants that may confound the hypertension-cognition association. Reverse causation may also contribute to the observed association between BP and cognition, especially in studies with cross-sectional design. Cognitive impairment is a process that unfolds over decades, thus presenting a challenge to establishing temporality. More research is needed to elucidate the causal link between BP and cognition and to better understand the role of medication in the observed associations. The relationship between BP and cognitive function remains relatively underexplored in minority and racially or ethnically diverse populations. Finally, there remain inadequate examination and reporting of potential sex differences in the effects of BP and hypertension on cognition. Future studies need to closely examine and report sex-specific associations.
Interaction With Other Risk Factors, Including Genetics
This section explores the possible impact of cardiovascular and other risk factors on the cognitive deficit associated with hypertension, focusing on age, sex, race/ethnicity, obesity and central obesity, metabolic syndrome/insulin resistance/diabetes mellitus, inflammatory biomarkers, lipids, smoking, occupation, education, diet, and air pollution. Possible interactions with atrial fibrillation, arterial stiffness, cardiac function, carotid intima-media thickness/stenosis, and stroke were not examined because these intermediate subclinical and clinical disease states could lie along the causal pathway between hypertension and cognitive impairment. However, genetic factors that might underlie both hypertension and cognition were also examined, focusing on genes such as APOE that are known to affect cognition independently, genes thought to be associated with vascular dementia and a vascular pattern of cognitive impairment, and genes affecting the risk of stroke, hypertension, and cognitive impairment.
Interaction With Age, Sex, and Metabolic Traits
Age
An interaction with age has been shown in multiple studies, with higher BP and hypertensive status being associated with worse cognition in younger130 and middle-aged adults (Hypertension Treatment Over the Life Course section). On the other hand, either a J-shaped association of SBP with cognition108 or an association of higher DBP with better cognition and slower rates of decline in cognition was noted in older adults. Thus, a study of centenarians showed a positive association between SBP and cognitive performance.110 This age interaction has been shown both for cognitive function in individuals free of dementia and when the end point of clinical dementia or AD was considered (Hypertension and AD section). Conversely, analysis of 1695 Framingham Study subjects failed to show an interaction with age over the 55- to 88-year range when individuals with concomitant stroke were excluded, and a study of 1130 subjects in the ARIC study also showed no age interaction.100,131
Sex
The interaction of male or female sex with hypertension in affecting cognition has not been investigated in detail, although a single study of 1034 women suggested an interaction of hypertension with menopausal status. Among postmenopausal women, cognitive performance on the Mini-Boston Naming Test was worse in hypertensive women compared with normotensive women, whereas among premenopausal women, no difference was observed between hypertensive and normotensive women.132
Metabolic Traits
An interaction of various metabolic and vascular risk factors such as diabetes mellitus with hypertension has been documented to increase the risk of stroke133 and thus to indirectly increase the risk of dementia. However, studies that have looked for an interaction of diabetes mellitus with hypertension and an adverse impact on cognition have typically found independent, additive effects rather than a synergistic interaction of these 2 risk factors.134 Among the various metabolic dysfunctions noted in diabetes mellitus, insulin resistance appears most likely to interact with hypertension. A measure of central obesity (having a waist-to-hip ratio in the top quartile) was noted to have a synergistic interaction with severity (Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure stage) of hypertension on the impact on visual memory performance in the Framingham Offspring study,135 and a small study has reported an adverse impact of concurrent elevations in BMI, waist-to-hip ratio, and insulin resistance (homeostatic model assessment–insulin resistance) on cognition in hypertensive patients.53 Either no evidence or limited evidence was found for interactions of BP or hypertension with smoking, occupation, education, diet, and air pollution on their impact on cognition, although several of these risk factors are known to have synergistic interactions with hypertension in increasing the risk of cardiovascular events, including clinical stroke.
Interaction With Circulating Biomarkers
In a small study from Maastricht, in hypertensive individuals, higher circulating levels of markers of endothelial activation (eg, vascular cellular adhesion molecules and selections) and of inflammation (eg, C-reactive protein) were found to be associated with worse cognition, and in a Japanese study that has not been replicated, pentraxin-3, another marker of inflammation, was associated with worse cognition in hypertensive individuals. However, these studies included only hypertensive individuals and could not specifically assess possible interactions between BP and inflammation.136 There are only a few reports of interactions between adverse lipid profiles (elevated low-density lipoprotein, lower high-density lipoprotein, and higher triglycerides) and BP in their impact on cognition137; these seem to be in the setting of a metabolic syndrome with concomitant insulin resistance or explained by an APOE ε4 genotype.
Interaction With Genetic Markers
An interaction between the APOE ε4 allele and many cardiovascular risk factors in their impact on cognition has been shown in various studies, and this appears to be true for hypertension in most138,139 but not all of these studies.140 The Honolulu-Asia Aging Study followed up 3065 Japanese American men over 26 years and observed an interaction of the APOE ε4 genotype and an SBP ≥160 mm Hg in their impact on cognition with relative risks of 2.6 and 13, respectively, of impaired cognition when individuals who had hypertension but no APOE ε4 allele and those with both risk factors were compared with a control group with neither.141 An Australian study of 1467 community subjects who were 60 to 64 years of age at baseline and examined for cognitive performance 3 times over 8 years noted that the APOE-hypertension interaction, but not a APOE–mean arterial pressure interaction, was associated with a small but statistically significant increase in the rate of decline of episodic memory, verbal ability, and global cognition.142 A similar interaction was demonstrated in 563 subjects of the Seattle Longitudinal Study in whom cognitive change was assessed over a 21-year period.143 Recently, several genetic variants have been identified to determine cognitive performance in the domains of verbal memory, fluid intelligence (the general intelligence factor), and executive function in older adults. In these older adults, a variant in the KIBRA gene showed an association with worse verbal memory, an effect that was restricted to individuals with hypertension and was larger in hypertensive women compared with men.144
Summary of Evidence
There are limited data on possible interactions between demographic, genetic, and vascular risk factors and hypertension in their impact on age-related cognitive decline and risk of AD. Age is an important factor, with high BPs in midlife and lower BPs in late life increasing the risk of poor cognition. Menopausal status, insulin resistance, inflammation, and the APOE ε4 genotype may each potentiate cognitive decline in hypertensive individuals. The mechanisms underlying these putative interactions remain uncertain, although in the case of APOE, the tau pathway has been implicated in a few studies.
Hypertension and AD
Hypertension is an important vascular risk factor and may influence the risk of MCI or dementia resulting from AD, the neuropathological findings in AD, and the corresponding neuroimaging and cerebrospinal fluid (CSF) biomarkers. The purpose of this section is to explore the relationship between hypertension and the risk for AD and its neuropathological manifestations, as well as neuroimaging and CSF biomarkers.
Hypertension and AD Risk: Epidemiological Studies
Examination of the associations between elevated BP and the risk of clinically diagnosed AD is complicated by several factors, and the associations remain poorly understood. Observational studies suggest that higher BPs before the age of 65 to 70 years increase the risk of AD. In older adults, lower SBP appears to be associated with an increased risk of developing AD, whereas higher DBP may lower risk. Genetic variants associated with higher BP may reduce the risk of developing AD pathology.145 Here, we summarize the epidemiological evidence and then discuss the challenges in interpretation.
Epidemiological Evidence
Cross-sectional analyses in the Hisayama Study,146 in the Canadian Health and Aging Study,147 and in a convenience sample of 1259 Medicare enrollees148 showed an association of high BP with greater overall risk of dementia and with risk of vascular dementia but not with risk of clinically diagnosed AD. The Women’s Health Initiative showed an association of higher BP with greater risks of incident MCI and dementia that disappeared after adjustment for possible confounders.122 The Kungsholmen study found no association of BP with dementia risk over 6 years of follow-up except at the extremes of SBP (>180 mm Hg) and DBP (<65 mm Hg).149 In contrast, other studies in older adults suggest a protective effect of mild hypertension on AD dementia risk.150–154 A U-shaped association with the lowest risk for AD dementia in individuals with a DBP in the 70– to 90–mm Hg range was noted in the Chicago Health and Aging Project.119 Unlike the findings in older adults, recent studies have observed an association of higher midlife BPs or midlife categorical hypertension with increased late-life dementia risk, including studies in Finnish,155,156 Japanese Northern Californian,157 and Hawaiian cohorts.158 However, these studies did not separately examine the risks of developing AD versus vascular dementia.
Challenges
Hypertension, however defined, is associated with an increased risk of stroke in a graded, continuous manner, and stroke, in turn, increases the risk of dementia.12,159 Many epidemiological studies are confident in their clinical diagnosis of dementia but acknowledge uncertainty resulting from limited resources in assigning a subtype of dementia. Thus, if individuals with hypertension were more likely to manifest clinical symptoms of dementia at the same stage of AD pathology, this could lead to a spurious association of hypertension with AD dementia. Conversely, individuals with hypertension are also more likely to be categorized as having vascular or mixed dementia rather than “pure” AD, and this diagnostic bias could result in an apparent protective effect of hypertension on clinically diagnosed AD.
Another reason for the complexity of the association between BP and AD is the many ways in which BP can be assessed (SBP, DBP, pulse pressure,160 mean arterial pressure, and arterial stiffness measured as carotid-femoral pulse wave velocity on tonometry) and the differential impact of each dimension on brain health and AD pathology. SBP in individuals at higher risk of subsequent dementia may rise faster starting in midlife and decline faster at older ages compared with SBP in other individuals.161
There appears to be a progressive decline in BP in the early stages of dementia that may be attributable directly to the neurodegenerative process affecting brainstem and hypothalamic nuclei regulating arterial pressure and systemic metabolism,162,163 may result from the associated systemic changes such as weight loss and increased frailty, or may be secondary to the onset of cardiovascular diseases such as myocardial infarction and congestive heart failure that can reduce the ability of the heart to maintain systemic and cerebral perfusion pressures. Thus, BPs measured 1 to 10 years before the onset of clinical AD may be biased by reverse causality and may not represent the pressures experienced before the onset of the AD pathological process.
In summarizing the literature, 2 recent weighted meta-analyses of cohort studies, including 6 studies of individuals with MCI164 and 28 studies of cognitively normal individuals, that specifically considered the end point of clinically diagnosed AD165 failed to find an association of any BP measure with risk of developing AD, whereas an earlier meta-analysis of 18 cohort and case-control studies had suggested an association of elevated midlife DBP with increased risk of AD and an inverse association of late-life hypertension with lower risk of AD; both effects were small.166 Secular trends in the treatment of hypertension in midlife might be having an impact. The risk for dementia in Japanese American subjects treated with anti-hypertensives for >12 years starting in midlife was lower compared with the risk in hypertensive indiduals not on treatment (for dementia: hazard ratio, 0.40; 95% confidence interval, 0.22–0.75; and for AD: hazard ratio, 0.35; 95% confidence interval, 0.16–0.78) and was similar to the risk in normotensive individuals.167 An added consideration is that antihypertensives may have class-specific effects on AD pathology that are independent of their BP-lowering effect168,169 (Effects of Hypertension on Cerebrovascular Structure and Function section). In this regard, it is of interest that individuals with genetic variants associated with higher BP and use of antihy-pertensive agents have a reduced risk of AD.145
Hypertension and AD Neuropathology
In all of its target organs, hypertension causes dysfunction through alterations in vascular function (Effects of Hypertension on Cerebrovascular Structure and Function section). However, there are some reports that hypertension might have an impact on AD pathology. In Japanese American men (n=243) in the Honolulu-Asia Aging Study, there was an association between midlife BP and burden of NFTs at death, roughly 3 to 4 decades later.170 Elevated SBP at midlife was associated with low brain weight and neocortical and hip-pocampal neuritic plaques, whereas elevated DBP at midlife was associated with increased NFTs in the hippocampus. Another clinical-pathological study from the Bronx, NY,171 that included both men and women (n=291) found that medication-treated hypertensive indivduals had significantly lower levels of neuritic plaques and NFTs compared with nonhypertensive individuals. Untreated hypertensive individuals had more NFTs and neuritic plaques than the treated hypertensive individuals but were not different from the normotensive individuals. The authors emphasized the role of antihypertensive medications over hypertension itself because of the pattern of results in treated versus untreated hypertensive individuals and suggested a protective effect of medications. A clinical-pathological study involving 84 individuals with neuropathological diagnoses of AD with or without cerebrovascular changes from San Diego172 found that antemortem vascular risk factors that included hypertension but also diabetes mellitus, heart failure, atrial fibrillation, peripheral vascular disease, and smoking were associated with lower Braak stage. The study was underpowered to examine hypertension by itself. Because it is difficult to quantify cerebrovascular changes, these results could have been attributable to greater vascular burden. Along those lines, an earlier study from this group found that pulse pressure was associated with cerebrovascular lesions (large-vessel atherosclerosis, infarcts of any size) at autopsy,173 along with no associations with Braak stage or amyloid angiopathy. A study from Seattle Group Health reported an association between systolic hypertension and the presence of >2 microinfarcts in younger subjects (age, 65–80 years), but there were no associations with AD-type lesions (Braak stage or Consortium to Establish a Registry for Alzheimer’s Disease plaque score) or Lewy bodies.174 There were no associations with vascular lesions in older individuals (>80 years old at entry).
In summary, the evidence linking antemortem hypertension to postmortem neuropathological changes seen in AD is modest and confounded by differential survival, indication bias, and small numbers. Although results from the Honolulu-Asia Aging Study170 support the idea of an overlap between hypertension and AD pathophysiology, other reports do not. With antemortem amyloid and tau positron emission tomography (PET) imaging now available, prospects for determining the true relationship between hypertension and AD pathological changes are much brighter.
Impact of Hypertension on Biomarkers and Association With AD
Hypertension and AD-type pathophysiology appear to share a common pathogenesis in several imaging features: white matter hyperintensities (WMHs), cerebral microbleeds, and brain volume/atrophy.
White Matter Hyperintensities
WMHs, as detected by fluid-attenuated inversion recovery magnetic resonance imaging (MRI), are widely regarded as lesions associated with cerebrovascular disease175–177 (see elsewhere for a discussion of relevant white matter imaging modalities75,178,179). Hypertension is the most important risk factor for the development of WMH.99,180–182 Hypertension in general,180,183–185 high SBP,99,185–190 high DBP,186,189,191–193 low DBP,194 pulse pressure,185 mean arterial pressure,195,196 pulse wave velocity,197 and arterial stiffness198 have all been associated with WMHs, and it is not clear that one measure of BP predominates over the others in magnitude of the association. Treatment adds considerable complexity to the relationship between hypertension and WMH, but a few clinical trials have shown that WMH progression is reduced with antihypertensive treatment.199,200 Diffusion tensor imaging is another imaging technique for examining anatomic integrity in white matter. Changes in fractional anisotropy or mean diffusivity have been associated with some aspect of hypertension,201–206 although not invariably.207 Carriage of the APOE ε4 genotype has been associated with higher levels and faster rates of accumulation of WMH in some studies208,209 but not others.210 Some studies have claimed that the combination of hypertension and carriage of the APOE ε4 genotype was linked to more WMHs.211,212 We found no studies claiming interactions at the mechanistic level between hypertensive pathophysiological process and AD pathophysiological processes on WMH burden. On the other hand, there is evidence that cerebrovascular disease and AD pathophysiology have at least additive effects at the clinical level.213–216 Thus, although cerebrovascular mechanisms do not worsen AD processes, the combination of the two may lead to earlier and greater cognitive decline.
Cortical Microbleeds
Cortical microbleeds, microhemorrhages of 1 to 3 mm in diameter that often are attributable to cerebral amyloid angiopathy,217 are also associated with hypertension.182,218–221 Deep locations, that is, the putamen and thalamus, are much more likely to be associated with hypertension, whereas cortical locations are more likely to be associated with carriage of the APOE ε4 allele209,222,223 or with elevated Aβ levels by PET imaging.224 In patients with AD, hypertension increased the likelihood of cortical microbleeds,225 but that effect could be additive or interactive. We otherwise uncovered no evidence for or against an interaction between hypertension and Aβ burden for cortical microbleeds. Cortical microbleeds are modestly related to cognition197,226 but not to decline in individuals with AD.227
Brain Atrophy
In some reports, loss of brain volume has been associated with hypertension,190,194,228,229 mean arterial pressure,196 or arterial stiffness,198 but other studies failed to demonstrate the association99,195,230,231 (Beauchet et al232 provide further discussion). Treatment effects might confound the interpretation of associations.233 The mechanisms whereby hypertension causes brain volume loss are not clear. To the extent that WMHs are also associated with brain volume,208,234–240 the effects of hypertension on brain volume could be mediated via loss of white matter integrity. Other potential mechanisms could include microinfarction, remote effects of axonal injury in white matter, and an interaction with AD processes such as trafficking of damaged proteins in the perivascular spaces.241 Hypotension and falling BP over time are also associated with loss of brain volume.242 Indeed, the U-shaped relationship between BP and brain integrity is an important feature of the relationship between BP and late-life cognitive impairment (Hypertension and Cognition: Observational Studies section).
Aβ PET Imaging
Only a few studies have examined associations between hypertension and Aβ levels by PET imaging. In a subset of subjects from a ginkgo clinical trial who underwent Pittsburgh compound B PET imaging, there was an association between pulse wave velocity and higher brain amyloid levels243 that was independent of BP and APOE ε4 genotype. In a group of middle-aged volunteers, an association of SBP and pulse pressure with burden of Aβ by PET imaging was seen,244 but in older individuals, concurrent DBP but not SBP was associated with Aβ burden by Pittsburgh compound B PET.245 Another study found an interaction between the APOE ε4 genotype and hypertension and Pittsburgh compound B PET.246 This same group also found a main effect for pulse pressure.
CSF Biomarkers for AD
We found only a few studies that examined associations of BP and CSF markers of AD. In a group of cognitively normal individuals who had CSF examinations, there was an association of pulse pressure with increased phospho-tau and reduced Aβ42,247 a finding that was replicated in an independent cohort.248 Another study of CSF biomarkers showed an interaction between the APOE ε4 allele (especially ε4 homozygosity) and hypertension in elevating CSF tau and phospho-tau levels.249 However, in that study, there was no similar interaction of hypertension and carriage of an ε4 allele on CSF Aβ levels. The relevance of these findings to the progression of AD requires further study.
Summary of Evidence
Several epidemiological and clinical pathological studies have reported a link between hypertension and AD. However, a challenge to the interpretation of the relationship between hypertension and AD is the substantial lag from the onset of the study of hypertension to the time of pathological diagnosis of AD. The growing availability of amyloid PET imaging and structural MRI offers the opportunity to better understand the role of hypertension and brain pathology in vivo. In population-based or special (enriched) cohort studies, large sample sizes would be needed to distinguish separate roles for SBP, DBP, pulse pressure, mean arterial pressure, and carotid-femoral pulse wave velocity on each of the imaging features. Longitudinal studies would be needed to assign priority to assessing hypoperfusion, white matter changes, cortical volumetric changes, microbleeds, and amyloid accumulation to understand their interrelationships. Future imaging techniques that can detect specific target involvement will be needed to understand what cells or cellular elements are the site of the initial pathogenic insult of hypertension. The cell types and end points that are most amenable to therapy are still unclear.
Hypertension and Cognition: Clinical Trials of BP Lowering
This section examines available data from clinical trials on the effect of hypertension treatment on cognitive function. We excluded studies that were not randomized, prospective trials with a primary or secondary outcome relating to cognitive status. Using the search criteria outlined in Methods, we identified 27 trials for consideration. We considered criteria based on sample size and excluded studies with <500 individuals per treatment arm. This is an arbitrary cut point based on a generic power analysis using data reported by Hypertension in the HYVET-COG (Very Elderly Trial Cognitive Function Assessment) for dementia events (36 of 1000 in the control group and 24 of 1000 in the treatment group250) and differences in end-trial MMSE measured in SYST-EUR (Systolic Hypertension in Europe).251 All studies were further assessed for bias according to the Cochrane Collaborations checklist.252
Trial Descriptions
Nine trials met the general inclusion criteria. Most trials testing cognition were based on the total main trial population (SPS3 [Secondary Prevention of Small Subcortical Strokes Trial], PROGRESS [Perindopril Protection Against Recurrent Stroke Study], SCOPE [Study on Cognition and Prognosis in the Elderly], PROFESS [Prevention Regimen for Effectively Avoiding Second Strokes], ONTARGET [Ongoing Telmisartan Alone and in Combination With Ramipril Global Endpoint Trial], TRANSCEND [Telmisartan Randomised Assessment Study in ACE Intolerant Subjects With Cardiovascular Disease], and SHEP [Systolic Hypertension in the Elderly Program]), were ancillary studies embedded in a subsample of the main trial,253 or included selected sites (SYST-EUR251). Sample sizes ranged from 1439 to 25 620, and mean patient age ranged from 62 to 83 years. Follow-up time ranged from ≈2 years (SYST-EUR)251 to ≈5 years (ONTARGET/TRANSCEND254). Two trials were stopped early because they reached their primary end point (SYST-EUR251 and HYVET250). The SPS3 antiplatelet arms were stopped early because of futility and evidence of harm.255
Target populations for the trials differed. The main inclusion of some trials was based on BP levels256 (SHEP257 and HYVET250,251) or resistance to a particular class of antihypertensives (TRANSCEND).254 Other trials included patients with cardiovascular disease or at high risk for cardiovascular events: The ACCORD MIND trial (Action to Control Cardiovascular Risk in Diabetes–Memory in Diabetes) included individuals with long-standing diabetes mellitus at high risk for cardiovascular events253; ONTARGET included patients with subclinical evidence of cardiovascular risk254; and some trials included patients with a recent to more remote history of different stroke subtypes, that is, ischemic and lacunar (PROFESS, SPS3, and PROGRESS).258–261
The mean BP levels at baseline have declined over time, consistent with evolving evidence supporting lower BP treatment goals. Thus, the earlier trials (SHEP,262 SYST-EUR,251 and SCOPE256) included people now classified in the stage 2 hypertension range. More recent trials included patients with qualifying BP levels that fell into the stage 1 hypertension range, so mean baseline BPs were lower.
Treatment protocols have also changed, and designs have become more complex. The range of designs include testing a single drug against placebo (TRANSCEND254; a single drug versus placebo, allowing open-label antihypertensive treatment in the placebo arm if needed in SCOPE256) or a primary drug followed by a standardized step procedure with a protocol-driven sequence for adding additional drugs (HYVET,250 SYST-EUR,251 SHEP,257 and SCOPE256) or without specified BP goals (SPS3,259 PROFESS,258 PROGRESS,260 and ONTARGET/TRANSCEND254) ACCORD MIND253 tested 2 therapeutic strategies with different SBP goals, <120 versus <140 mm Hg. Several trials used a 2-by-2 factorial design that allowed a test of >1 intervention. The 2-by-2 factorial of SPS3 had 2 arms comparing different SBP goal–defined therapeutic strategies and comparing a dual antiplatelet therapy with aspirin plus placebo.259 The PROFESS trial had 4 arms that tested antiplatelets, angiotensin II receptor inhibitors, and placebo258; ONTARGET had 3 arms comparing an angiotensin-converting enzyme inhibitor, angiotensin II receptor inhibitors, and a combination of drugs.254 The achieved reduction in BP (SBP/DBP) ranged from −0.9/0.6 in the telmisartan versus ramipril arm in the ONTARGET trial254 to 15/5.9 in HYVET.250
Cognitive Outcomes
The most widely used test, as a single and primary outcome, has been the MMSE, which is a 30-point test of global cognition. The SPS3 trial259 used the Cognitive Abilities Screening Instrument, another, longer test of global cognitive function. ACCORD MIND253 had as its primary outcome psychomotor speed (Digit Symbol Substitution Test; Cognitive Domains Targeted by Hypertension section). The MMSE score was used in several metrics to define outcome, including the absolute MMSE score, percent scoring <24 (HYVET,250 ONTARGET,254 SCOPE,256 and PROGRESS260), or a drop of 3 points (PROGRESS260). The MMSE was also used as a screening instrument to identify people for additional workup for dementia (HYVET250 and PROGRESS260) or to define dementia (ONTARGET254). The second most frequent outcome was dementia, which was diagnosed by investigator-assessed and specialist-confirmed diagnosis of dementia (ONTARGET254 and PROFESS clinical impression258), a local investigator following international criteria (SCOPE256), and an examination of screen-positive individuals by a local specialist following international guidelines and then central adjudication (PROGRESS260; SCOPE,256 SYSTEUR,250,251 and SHEP257). Trials that aimed to subtype the dementia used the Hachinski ischemic score263 in addition to the MMSE and clinical assessment to assess the likelihood of a cardiovascular contribution and a computed tomography scan to image cerebrovascular lesions.
Other Measures of Brain Function and Structure
Three trials had imaging substudies (MIND,253 PROFESS,264 and PROGRESS199) to test whether the intervention was related to the development or progression of pathology in the brain, as measured by MRI. PROFESS imaged 777 people on average 27 months apart; in that subsample, there were no differences between treatment groups264 in BP levels or in the outcome, progression of WMHs assessed by fluid-attenuated inversion recovery MRI. In the PROGRESS substudy of 192 subjects followed up for 36 months, a significant slowing of WMH progression was detected between treatment groups.199 The 314 MRIs acquired at baseline and 40 months later in ACCORD MIND showed that total brain volume had declined more in the group with intensive versus standard strategy to lower BP.253 Few trials assessed >1 cognitive function in all (SPS3)253,259 or a subsample of subjects (SHEP262 and SCOPE265). A SCOPE substudy (n=257)265 found suggestive evidence of a small effect of treatment on attention and episodic memory tests but not working memory or executive function. Other trials found no treatment differences in test scores.253,259,262
Results of Clinical Trials
Only 1 trial, SYST-EUR, had a marginally significant result suggesting the treatment benefit of reducing dementia (21 versus 11 patients; P=0.05), an effect that persisted during an open follow-up phase.251,266 The PROGRESS trial, using a definition of “dementia (or cognitive decline) after stroke” and “other dementia (cognitive decline),” found a significantly (P=0.03) reduced risk in the patients with treated dementia after stroke compared with control subjects (43 versus 65) and an overall reduction in cognitive decline in the treated group, with the difference attributable mainly to the cognitive decline with stroke group.260 Other trials report no differences on cognitive test performance between intervention and control arms. Post hoc analyses in several trials indicate that within treatment arms, there was a negative association of more cognitive decline in those with a smaller decrease in BP (SYST-EUR and ONTARGET).251,259
Evidence for a Particular Class of Antihypertensive Drug
A meta-analysis in 2011 of 8 trials reviewed here found that overall there was no effect of BP lowering on the risk for dementia.267 However, there was a suggestion that calcium channel blockers may slightly reduce the incidence of dementia, but the authors note that the benefit could be attributable mostly to the amount of BP lowering achieved in those trials. Such comparisons point out the difficulty in identifying any one drug class as being particularly beneficial for cognition: There is a confounding between baseline BP, number of drug classes used to lower BP, and the amount of BP lowering achieved in the trials. The evidence suggests that there is no Class A evidence for treating hypertensive patients (>160/90 mm Hg) with no apparent cardiovascular disease to preserve cognition. At lower levels of BP and in trials based on patients with preexisting cardiovascular disease, the existing trials have been uniformly negative. However, this conclusion should be tempered given several sources of bias in these trials and the strength of the trials to test the hypotheses. These are examined next.
Possible Sources of Bias and Heterogeneity of Results
Five studies reported the power of their analyses to detect treatment differences related to the cognitive outcomes.250,251,253,258,260 There is a possibility that the trials using the MMSE as their primary outcome were underpowered for the small differences that have been reported. In multicenter, multicultural studies, standardized assessment of dementia is important, particularly for mild cases of dementia, for which the cutoff for clinical dementia can vary substantially. Several trials reporting dementia outcomes do not provide sufficient information to determine whether and how assessments of dementia followed standardized protocols to fulfill international guidelines (ONTARGET,254 PROFESS,258 SCOPE,256 PROGRESS260, HYVET,250 SYST-EUR,251 and SHEP262). There is also a lack of documentation about the blinding of the individuals administering tests or rendering a dementia diagnosis.
Separation of BP levels between treatment arms was, in some of the trials testing specific drugs, attenuated because the control group was treated with antihypertensive drugs. This was a particular issue in the early trials when ethics guidelines called for treating very high BP (SCOPE,256 SHEP,262 and SYST-EUR266), although the definition of very high varied.
Finally, negative trial results could be attributable, in some trials, to the loss of data from those who either did not receive the full BP intervention or missed cognitive assessments.
Possibility of Finding Effects and Sources of Heterogeneity
Even in the absence of specific bias in implementation or reporting, it is important to consider the overall question of whether the trials were appropriately designed to test the efficacy of BP lowering to reduce cognitive decline/dementia. One factor to consider is whether the outcome measured was appropriate for the subjects’ age. The MMSE or a similar test of global cognition was used as the only cognitive measure250,254,256,258,259 in subjects from 60 to 65 years of age. Others were investigating dementia in patients of that age. This age range is likely too young to see a detectable change on the MMSE because that test has a low ceiling and a nonlinear pattern of change and is unlikely to provide cases of incident dementia, which begins to increase in incidence after 80 years of age. Furthermore, the MMSE was designed to screen for cognitive deficits caused by AD and may miss some of the major cognitive changes thought to accompany vascular-related cognitive impairment.3
Another issue about the strength of the completed trials investigating BP lowering and cognition is the likelihood of detecting clinically relevant outcomes during the short intervention periods. Several trials included a relatively cognitively healthy group with a mean MMSE score of 29 of 30 points. Post hoc analyses of several studies suggested that those who were more cognitively compromised, but still without dementia, may benefit more from short-term interventions (SCOPE268 and ONTARGET/TRANSCEND254).
Finally, if loss to follow-up or stopping treatment is related to cognitive impairment, then differences between treatment arms may be attenuated, with negative results. A simulation analysis based on SHEP269 suggested that if those with cardiovascular disease who dropped out of the trial were also cognitively impaired and had stayed in the trial, different, positive results of the intervention might have been detected.
Summary of Evidence
Early trials treating patients with very high baseline BP suggested that lowering BP at these levels might be efficacious. However, issues related to the choice of outcomes relative to the age of the trial population, possible bias caused by sample attrition, and questions about quality control protocols raise the question of whether the hypothesis of cognitive benefit from BP lowering has been adequately tested. Furthermore, bringing in new imaging-based outcomes to better understand the response to therapy and its relation to cognitive outcomes would enhance these trials. Trials recently ending should shed more light on this question. One trial, the SPRINT trial (Systolic Blood Pressure Intervention Trial),270 with target treatment goals for elevated BP ended early because of efficacy on the main cardiovascular events271 but has extensive data on brain health. Results from SPRINT-MIND (SPRINT Memory and Cognition in Decreased Hypertension) will be available next year. In the interim, careful control of BP might be a reasonable course of action, taking into account age and comorbidities.
Hypertension Treatment Over the Life Course
Managing BP to maintain cognitive health will likely require taking into account the complex relationship among BP, age, the presence of comorbidities, and antihypertensive therapy. In this section, we review available evidence that sheds light on the expected cognitive benefit of treating hypertension across the life course.
Treatment of Hypertension in Children and Adolescents
Clinically apparent vascular disease rarely occurs in children and adolescents. However, preclinical risk factors for vascular disease such as hypertension appear to have become more prevalent in the past few decades.272–274 The basis for this rise in pediatric hypertension is unclear but may be explained in part by an increase in the rate of obesity.275,276
Given the rarity of pediatric vascular events such as stroke, little evidence directly ties pediatric hypertension to subsequent vascular outcomes during childhood and adolescence. However, 3 factors implicate childhood hypertension in the subsequent development of adverse outcomes in adulthood. First, childhood and adolescent hypertension often continues into adulthood. Moderate correlations have been found between BP during childhood and BP years later,277,278 which suggests that early-life hypertension will often persist into later life stages in which it is a well-established risk factor for vascular events and cognitive impairment. Second, prospective cohort studies have found associations between childhood vascular risk factors such as hypertension and the presence of subclinical atherosclerotic lesions on autopsies of study subjects who died in young adulthood as a result of accidental trauma.279,280 Similarly, hypertension in early life has been linked to in vivo measures of vascular dysfunction such as left ventricular hypertrophy on echocardiogram and carotid intima-media thickness on ultrasound.281 Such findings place childhood hypertension on the pathway to preclinical vascular dysfunction, which in turn has been strongly linked to clinical vascular events such as stroke and heart failure. This parallels the pathway seen with adult-onset hypertension. Finally, the childhood presence of metabolic syndrome, of which hypertension is an integral part, has been directly associated with clinical vascular outcomes in early adulthood.282 Taken together, these findings indicate that hypertension in early life not only serves as a prelude to hypertension in adulthood but also has already begun to have insidious effects on the vascular system that predispose to symptomatic vascular disease early in life. In addition, several small studies have raised the suggestion that elevated BP has immediate adverse implications for cognitive function even in childhood.283–285
No randomized, clinical trial has evaluated the effect of antihypertensive therapy on clinical outcomes or markers of end-organ damage in the pediatric population.286 The considerations above provide a plausible rationale for carefully treating hypertension in children and adolescents in the hope of preventing vascular events and cognitive impairment in adulthood. However, several cautionary points apply. The long-term safety of pharmacological treatment in children’s growth has not been studied.286 This supports a preferential emphasis on lifestyle modification, especially weight loss, before resorting to pharmacological therapy. Furthermore, many children with hypertension no longer manifest elevated BP in adulthood.277,278 This uncertainty about the long-term durability of childhood hypertension calls for continual reassessment of BP and whether pharmacological therapy is needed, especially in patients who have successfully lost weight.276
Treatment of Hypertension in Young Adults
Most cases of hypertension in individuals <40 years of age involve isolated diastolic hypertension.287 This often progresses to also involve systolic hypertension as patients enter middle age.288 Furthermore, even across the fifth decade of life, a strong association remains between increasing DBP and cardiovascular events such as myocardial infarction.289 This natural history argues for attempts to reduce BP even in young adults, especially in patients who manifest any evidence of end-organ injury. Across randomized trials of anti-hypertensive therapy, the relative benefits of treatment and of specific classes of drugs do not appear to vary on the basis of whether patients were >65 or <65 years of age.290 However, randomized, clinical trials have not been performed to specifically assess the benefits of pharmacological treatment of hypertension in young adults. In this context, nonpharmacological measures may be an especially compelling first-line approach. The PREMIER trial enrolled 810 relatively young adults (mean age, 50 years) with stage 1 hypertension (mean BP, ≈135/85 mm Hg) who were not receiving antihypertensive therapy. Subjects were randomly enrolled to a brief session of advice about factors affecting BP or to 1 of 2 intensive behavioral interventions. At 6 months, the intensive interventions led to an ≈4–mm Hg reduction in SBP.291 This suggests that intensive nonpharmacological interventions in young adulthood may prevent the onset of hypertension or at least may delay the need for pharmacological therapy until later in midlife.
Treatment of Hypertension in Midlife
Numerous randomized, clinical trials in middle-aged populations have shown that antihypertensive therapy substantially decreases the risk of adverse cardiovascular events such as stroke.292–295 Some of these trials included measures of cognition. As discussed in the Interaction With Other Risk Factors, Including Genetics section, trial results do not clearly support or refute a beneficial effect of antihypertensive therapy in preserving cognition.296–300
Furthermore, by midlife, hypertension often occurs in the context of other systemic vascular risk factors such as dyslipidemia, diabetes mellitus, obesity, a sedentary lifestyle, and exposure to tobacco and environmental pollutants. Recent evidence from a large, randomized, clinical trial suggests that an overarching strategy for modifying these vascular risk factors helps to preserve cognition in individuals in their 60s and 70s.301
Finally, both clinically overt stroke and silent brain infarcts appear to lie on the causal pathway to cognitive impairment,159,302,303 so widespread adoption of antihypertensive therapy to prevent stroke is likely to also result in improvements in cognition over the long term. A recent comparison of cognitive outcomes between 2 successive cohorts of elderly subjects born about a decade apart demonstrated better cognition in the later-born cohort.304 These findings follow several prior reports to the same effect. An analysis of long-term care surveys from the United States across the 1980s and 1990s first suggested a temporal decline in the prevalence of dementia.305 This pattern was corroborated by a separate US population–based survey that found an ≈5% decrease in the prevalence of cognitive impairment between 1993 and 2002.306 Similar patterns have been found in analyses from Sweden and England.307,308 These secular trends may have been driven by less exposure to adverse environmental influences such as pollution and greater exposure to antihypertensive therapy. However, such ecological conclusions cannot be drawn without more detailed data (Hypertension and Cognition: Clinical Trials of BP Lowering).
Overall, although robust evidence is lacking to prove that antihypertensive therapy in middle age provides a cognitive benefit, such a benefit appears likely on the basis of the epidemiological considerations above. Given the expected burden of cognitive impairment and dementia in an aging population, this suggestion of benefit provides a strong rationale for randomized, clinical trials of antihypertensive therapy designed primarily to test the hypothesis that aggressive control of hypertension during middle age can delay cognitive decline in later life. Although antihypertensive therapy in midlife is already supported by evidence of its benefit in reducing clinical events such as stroke, more robust evidence of its role in cognition would have important implications for our understanding of the pathogenesis of dementia. The results of the ongoing SPRINT-MIND trial (Interaction With Other Risk Factors, Including Genetics section) may help shed light on this question.
Treatment of Hypertension in Late Life
Randomized, clinical trials did not shed much light on whether antihypertensive treatment protects cognitive function (Interaction With Other Risk Factors, Including Genetics section), but this uncertainty has been especially important in the very elderly. As discussed above, this population was well represented in HYVET (mean age, ≈84 years),250 but other randomized, clinical trials of antihypertensive therapy have enrolled few patients >80 years of age.292–295 Furthermore, several observational studies have found that low BP, particularly low DBP, is associated with cognitive and physical decline in the elderly107,128,149,154,309–311 (Hypertension and Cognition: Observational Studies section).
It is unclear whether the relationship between low BP and cognitive decline in late life reflects a dysfunctional autonomic nervous system resulting in low BP, low BP leading to progressive hypoperfusion and brain atrophy, or some combination of these and other factors. Clearly, much more research is needed on the complex relationships among BP, antihypertensive treatment, frailty and multimorbidity, and cognitive and functional status in the oldest old. In the meantime, it may be reasonable to consider frailty and multimorbidity as a factor in decisions about antihypertensive therapy in late life. This is especially the case in patients who manifest intolerance of antihypertensive therapy in the form of symptoms such as orthostatic hypotension.312 On the other hand, the results of the recently completed SPRINT trial, which included the oldest old, support the hypothesis that pharmacological treatment of elevated SBP reduces the risk of stroke and could help preserve cognition. The hope is that more detailed subgroup analyses of this age group will shed more light on the risks and benefits of antihypertensive treatment in the oldest old.
It is possible that better treatment of vascular risk factors earlier in life will reduce the prevalence of frailty in late life. Aging is associated with a progressive increase in SBP that occurs in the setting of stiffening of the arterial system313 (Effects of Hypertension on Cerebrovascular Structure and Function section). Indirect evidence suggests that aggressive treatment of early-life and midlife vascular risk factors may retard the progression of these pathological changes. Caloric restriction, low-sodium diet, increased levels of exercise, and low exposure to hypertension have all been associated with less arterial stiffening.314–318 If this is the case, then early treatment of hypertension and other vascular risk factors may both lessen the need for antihypertensive therapy and increase its safety in late life.
Summary of Evidence
Direct evidence from randomized, clinical trials does not allow conclusive recommendations about treating hypertension throughout the life span to protect cognition. Observational studies suggest that hypertension causes an accumulating burden of vascular injury across all stages of life, but paradoxically, the end stages of vascular disease in frail elderly patients may be marked by low BP. Such considerations support the use of antihypertensive therapy throughout middle age and then continued efforts at judicious control of BP in elderly patients who appear likely to tolerate it. Results of randomized, clinical trials are awaited to prove the likely hypothesis that good control of BP and other vascular risk factors across the life span will help to stem the tide of cognitive impairment and dementia that would otherwise be expected with a continually aging population.
Overall Summary and Future Directions
We have provided a broad overview of the cognitive impact of chronic hypertension. Hypertension disrupts the structure of cerebral blood vessels, promotes atherosclerosis, and impairs vital cerebrovascular regulatory mechanisms. These vascular changes increase the susceptibility of the brain to ischemic injury, especially in vulnerable white matter regions critical for cognitive function, and may promote AD pathology. The evidence to date points strongly to a deleterious influence of midlife hypertension on cognitive function in midlife and late life. Executive function and processing speed seem to be the cognitive domains most affected, but memory can also be impaired. Therefore, it can be difficult to differentiate VCI from AD solely on the basis of the neurocognitive deficits. Although the data are not conclusive, there is evidence of an association between higher late-life BP and better cognition, highlighting the complexities of recommending uniform levels of BP across the life course. In addition to aging, menopausal status, APOE ε4 genotype, insulin resistance, systemic inflammation, and other comorbidities may potentiate the cognitive decline in individuals with hypertension.
Less clear are the effects of hypertension treatment on cognitive function. Observational studies have demonstrated a cumulative effect of hypertension on cerebrovascular damage, but evidence from randomized, double-blind, clinical trials that treatment of high BP at any stage over the life course improves cognition is far from conclusive. An intriguing relationship has emerged between hypertension and AD, raising the prospect that a chronic elevation in BP aggravates AD pathology, contributing to dementia. These findings are critically important because they raise the possibility that treatment of hypertension may also contribute to reduce the development or progression AD. Because no evidence-based recommendations can be made at this time, treatment of high BP in midlife and judicious use of antihypertensives in late life, taking into account cerebrovascular status and comorbidities, seem justified.3
Our analysis of the evidence also revealed a number of knowledge gaps that need to be addressed to gain a better understanding of the pathobiology and clinical impact of hypertension and to develop preventive and therapeutic strategies. One of the most promising aspects of an association between hypertension and dementia, including AD, is the prospect of prevention or early treatment as a strategy to reduce downstream cognitive impairment. Indeed, given how prevalent hypertension is and that there are many accessible and effective drugs, treatment of hypertension may prove to be one of the best ways to prevent or delay dementia. However, numerous questions and caveats remain. These are considered next.
How hypertension acts on cerebral arteries, the micro-circulation, and other cellular elements in the neurovascular unit to produce changes in structure and function has not been fully elucidated. As we gain a better understanding of how the cells of the neurovascular unit and elsewhere interact to regulate cerebrovascular homeostasis and BBB permeability in the normal state, studies should also probe how hypertension interferes with the signaling pathways regulating such interactions in different districts of the cerebrovascular tree. The resulting knowledge may provide insight into the regional susceptibility of cerebral vessels to the effects of hypertension, that is, subcortical white matter and basal ganglia. The relative impact of the neurohumoral signals driving the elevation in BP and the mechanical forces acting on the vessel walls to induce changes in vascular cells and the extracellular matrix need to be explored further. While elucidating how hypertension may lead to brain damage, these investigations could point to new therapeutic targets to prevent or ameliorate the deleterious effect of hypertension on the brain and may unveil class-specific effects on pathological processes driving cognitive impairment. Better use of available models and new experimental models that more closely reflect chronic hypertension in humans may be needed to generate translationally relevant results.
A key question concerns how the structural and functional effects of hypertension on the brain lead to cognitive impairment. WMHs and other brain lesions produced by SVD could reduce the connectivity, speed, timing, and spatial precision of the communication among brain regions critical for cognition (eg, the prefrontal cortex, cingulated cortex, and sensory regions), leading to psychomotor slowing and executive dysfunction.27 On the other hand, hypoperfusion and reduced neurovascular coupling could induce brain dysfunction by depriving the energy-demanding regions involved in cognition of oxygen and glucose.319 Hypertension-induced amyloid production and deposition could also play a role by promoting AD pathology. In the long run, whole brain and hippocampal atrophy are also likely to contribute by further reducing the processing power of the brain. Although these mechanisms are all plausible, supporting human data on their relative impact throughout the life course are lacking. Studies using connectomic-based approaches to investigate how hypertension affects brain networks in the presence or absence of structural damage (WMHs, silent strokes, etc) are now feasible and could provide new mechanistic insights. In addition, brain imaging approaches to investigate the relationship among CBF, cerebral energy metabolism, BBB permeability, and amyloid deposition could clarify the interaction among these different pathogenic factors and provide new biomarkers for risk assessment and early disease identification.
Whether treatment as early in the life course as possible, for example, hypertension in adolescence, would offer advantages for dementia prevention or pose too many side effects or other risks that would offset early and aggressive treatment is a critical question. This is particularly a concern at the extremes of the life span. It may be that childhood or early adulthood treatment is not cost-effective or the side effects outweigh the advantages. Similarly, in very late life, aggressive treatment may be more problematic than helpful. Although it is challenging to conduct a trial that covers much of the life span, adding sensitive and state-of-the-art cognitive outcomes to ongoing hypertension studies would be cost-effective and highly informative. Furthermore, advanced statistical methods could be applied to existing data sets to gain additional insight and to help better plan future trials. Trials should also include biomarkers of AD and other dementias because they may be helpful surrogate markers and may suggest new ways to identify hypertensive individuals at increased risk for cognitive impairment.
Related questions pertain to the trajectory of the cognitive decline in the hypertensive population and to the factors determining vulnerability. Although cognitive impairment is well documented in people with hypertension, little is known about the temporal dynamics of cognitive change in this population. Prospective studies documenting the rate and timing of cognitive changes and identifying factors that may predict cognitive decline, for example, adherence to BP medication regimens or BP control and development of other comorbidities, would be highly relevant. Furthermore, in the AD and diabetic populations, brain changes may occur decades before cognitive changes.320,321 It is unknown when the brain is most vulnerable to the deleterious effects of hypertension. Prospective studies that use state-of-the-art neuroimaging techniques and prehypertension samples would provide valuable insight into this brain-behavior relationship.
The effects of other comorbid illnesses, that is, clusters of comorbidities that combined with hypertension may have a greater cognitive impact, remain to be defined. It is well documented that multiple chronic illnesses, for example, diabetes mellitus, renal insufficiency/failure, and heart failure, are associated with cognitive impairment.3 Furthermore, 3 of 4 individuals >65 years of suffer from ≥2 chronic illnesses (ie, multimorbidity).322 No research to date has examined the effect of multimorbidity on cognition; therefore, future studies should be designed around novel analysis techniques (eg, latent class analysis) to explore whether certain clusters of chronic illnesses are more predictive of cognitive impairment.
The cognitive tests that are most sensitive to changes in cognition across the life course also remain to be defined. As documented in this statement, cognitive tests vary dramatically between studies, making comparison of findings across studies difficult. Furthermore, the most commonly used instrument, the MMSE, is a measure of global cognition and is not as sensitive to subtle but clinically significant changes in cognition as domain-specific measures.323 Given the inconsistency in cognitive measures, it is difficult to determine which neuropsychological tests are most sensitive to the cognitive changes that occur within the hypertensive population. Studies to document the psychometric properties of comprehensive neuropsychological batteries are needed to better determine which cognitive measures are most sensitive in hypertension across the life span.
Although some studies provided hints that certain classes of antihypertensive drugs may be more effective at improving cognition or lowering cognitive decline, most of these studies were underpowered or without equivalent cognitive end points. To better guide treatment, much more information will be needed on class of drugs and possibly how the efficacy of drugs may differ by sex and ethnicity. Future trials should ensure a diverse population that is large enough to detect the efficacy of drugs on subpopulations and ensure that more uniform cognitive outcomes are used. The question of the differential effect of treating SBP versus DBP is also understudied and has important clinical implications for risk assessment.
Furthermore, although the preponderance of evidence suggests that hypertension, especially at midlife, is a risk factor for late-life cognitive impairment and dementia, several fundamental issues remain unanswered. Among these is how hypertension interacts with key pathogenic factors involved in neurodegeneration such as tau and Aβ in promoting neurodegenerative disease.44,45 The complicated interplay between cerebrovascular dysfunction and the production and clearance of these proteins through trans-vascular, perivascular, and paravascular pathways324,325 is an important area for further investigation. The role of the dural lymphatics326 in these clearance processes and the impact that hypertension has on lymphatic drainage remain to be assessed. These investigations may help address the role of hypertension in the alterations in amyloid trafficking observed in AD and in the evolution of neurodegeneration. With the advent of new neuroimaging techniques, especially amyloid and tau imaging, and biomarkers that can track preclinical disease, it may be possible to assess these interactions more readily.
In summary, basic, clinical, and neuropathological investigations have made remarkable progress in improving the understanding of the effect of hypertension on the brain vasculature and cognitive health, but much remains to be learned. Although there is substantial evidence that hypertension leads to cognitive impairment, an effect attributed to oxidative stress-driven cerebrovascular dysfunction and damage, the underlying cellular and molecular mechanisms remain incompletely understood. In addition, a critically important question still unanswered is whether treating hypertension prevents or reverses cognitive decline. Whereas difficulties in carrying on longitudinal studies for decades have played a role, the lack of appropriate and uniform cognitive outcomes across studies has also been a complicating factor. A complex relationship of hypertension with ethnicity, age, sex, and cerebrovascular risk factors has emerged, making it difficult to assess treatment effectiveness. The upcoming release of the results of the SPRINT-MIND trial may help fill some of these knowledge gaps. Despite numerous outstanding questions and caveats, personalized treatment of hypertension, taking into account age, sex, APOE genotype, metabolic traits, comorbidities, etc, remains a most promising and eminently feasible approach to safeguard vascular health and, as a consequence, brain heath. Antihypertensive drugs are generally safe and widely available, but there is still much to be learned about how to best use them over the life course in the presence of comorbidities and whether specific classes of drugs may confer cognitive benefits beyond BP lowering. New discoveries in the cellular and molecular pathology of the cerebrovascular tree and associated cells, coupled with the use of new imaging tools, biomarkers, and genomic-proteomic approaches in clinical trials, offer the prospect to address these unanswered questions and to develop new treatments to mitigate the devastating impact of hypertension on cognitive health.
Disclosures
Writing Group Disclosures.
This table represents the relationships of writing group members that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all members of the writing group are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $10 000 or more during any 12-month period, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
*Modest.
†Significant.
‡Dr Saczynski is now at Northeastern University.
Reviewer Disclosures.
This table represents the relationships of reviewers that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all reviewers are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $10 000 or more during any 12-month period, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
*Modest.
Footnotes
The American Heart Association makes every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
This statement was approved by the American Heart Association Science Advisory and Coordinating Committee on June 10, 2016, and the American Heart Association Executive Committee on July 20, 2016. A copy of the document is available at http://professional.heart.org/statements by using either “Search for Guidelines & Statements” or the “Browse by Topic” area. To purchase additional reprints, call 843-216-2533 or ramsay@wolterskluwer.com.
The American Heart Association requests that this document be cited as follows: Iadecola C, Yaffe K, Biller J, Bratzke LC, Faraci FM, Gorelick PB, Gulati M, Kamel H, Knopman DS, Launer LJ, Saczynski JS, Seshadri S, Al Hazzouri AZ; on behalf of the American Heart Association Council on Hypertension; Council on Clinical Cardiology; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; and Stroke Council. Impact of hypertension on cognitive function: a scientific statement from the American Heart Association.
Expert peer review of AHA Scientific Statements is conducted by the AHA Office of Science Operations. For more on AHA statements and guidelines development, visit http://professional.heart.org/statements. Select the “Guidelines & Statements” drop-down menu, then click “Publication Development.”
References
- 1.Dementia: A Public Health Priority. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 2.Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9:63–75.e2. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 3.Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, Launer LJ, Laurent S, Lopez OL, Nyenhuis D, Petersen RC, Schneider JA, Tzourio C, Arnett DK, Bennett DA, Chui HC, Higashida RT, Lindquist R, Nilsson PM, Roman GC, Sellke FW, Seshadri S, on behalf of the American Heart Association Stroke Council, Council on Epidemiology and Prevention, Council on Cardiovascular Nursing, Council on Cardiovascular Radiology and Intervention, and Council on Cardiovascular Surgery and Anesthesia Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2672–2713. doi: 10.1161/STR.0b013e3182299496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB, American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics–2015 update: a report from the American Heart Association [published corrections appear in Circulation. 2015;131:e535 and Circulation. 2016;133:e417] Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 5.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD, 3rd, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Mohd Hanafiah K, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA, 3rd, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJ, Ezzati M, AlMazroa MA, Memish ZA. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010 [published corrections appear in Lancet. 2013;381:628 and Lancet. 2013;381:1276] Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elias MF, Goodell AL, Dore GA. Hypertension and cognitive functioning: a perspective in historical context. Hypertension. 2012;60:260–268. doi: 10.1161/HYPERTENSIONAHA.111.186429. [DOI] [PubMed] [Google Scholar]
- 7.Gąsecki D, Kwarciany M, Nyka W, Narkiewicz K. Hypertension, brain damage and cognitive decline. Curr Hypertens Rep. 2013;15:547–558. doi: 10.1007/s11906-013-0398-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iadecola C, Gorelick PB. Converging pathogenic mechanisms in vascular and neurodegenerative dementia. Stroke. 2003;34:335–337. doi: 10.1161/01.str.0000054050.51530.76. [DOI] [PubMed] [Google Scholar]
- 9.Attems J, Jellinger KA. The overlap between vascular disease and Alzheimer’s disease: lessons from pathology. BMC Med. 2014;12:206. doi: 10.1186/s12916-014-0206-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Toledo JB, Arnold SE, Raible K, Brettschneider J, Xie SX, Grossman M, Monsell SE, Kukull WA, Trojanowski JQ. Contribution of cerebrovascular disease in autopsy confirmed neurodegenerative disease cases in the National Alzheimer’s Coordinating Centre. Brain. 2013;136(pt 9):2697–2706. doi: 10.1093/brain/awt188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schneider JA, Arvanitakis Z, Leurgans SE, Bennett DA. The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann Neurol. 2009;66:200–208. doi: 10.1002/ana.21706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snowdon DA, Greiner LH, Mortimer JA, Riley KP, Greiner PA, Markesbery WR. Brain infarction and the clinical expression of Alzheimer disease: the Nun Study. JAMA. 1997;277:813–817. [PubMed] [Google Scholar]
- 13.Chui HC, Zarow C, Mack WJ, Ellis WG, Zheng L, Jagust WJ, Mungas D, Reed BR, Kramer JH, Decarli CC, Weiner MW, Vinters HV. Cognitive impact of subcortical vascular and Alzheimer’s disease pathology. Ann Neurol. 2006;60:677–687. doi: 10.1002/ana.21009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chui HC, Ramirez-Gomez L. Clinical and imaging features of mixed Alzheimer and vascular pathologies. Alzheimers Res Ther. 2015;7:21. doi: 10.1186/s13195-015-0104-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention of Alzheimer’s disease: an analysis of population-based data [published correction appears in Lancet Neurol. 2014;13:1020] Lancet Neurol. 2014;13:788–794. doi: 10.1016/S1474-4422(14)70136-X. [DOI] [PubMed] [Google Scholar]
- 16.Faraco G, Iadecola C. Hypertension: a harbinger of stroke and dementia. Hypertension. 2013;62:810–817. doi: 10.1161/HYPERTENSIONAHA.113.01063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9:689–701. doi: 10.1016/S1474-4422(10)70104-6. [DOI] [PubMed] [Google Scholar]
- 18.Moser M, Roccella EJ. The treatment of hypertension: a remarkable success story. J Clin Hypertens (Greenwich) 2013;15:88–91. doi: 10.1111/jch.12033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, Kissela BM, Kittner SJ, Lichtman JH, Lisabeth LD, Schwamm LH, Smith EE, Towfighi A, on behalf of the American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; Council on Functional Genomics and Translational Biology Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014;45:315–353. doi: 10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iadecola C. Neurovascular regulation in the normal brain and in Alzheimer’s disease. Nat Rev Neurosci. 2004;5:347–360. doi: 10.1038/nrn1387. [DOI] [PubMed] [Google Scholar]
- 21.Ritz K, Denswil NP, Stam OC, van Lieshout JJ, Daemen MJ. Cause and mechanisms of intracranial atherosclerosis. Circulation. 2014;130:1407–1414. doi: 10.1161/CIRCULATIONAHA.114.011147. [DOI] [PubMed] [Google Scholar]
- 22.Faraci FM. Protecting against vascular disease in brain. Am J Physiol Heart Circ Physiol. 2011;300:H1566–H1582. doi: 10.1152/ajpheart.01310.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Laurent S, Boutouyrie P. The structural factor of hypertension: large and small artery alterations. Circ Res. 2015;116:1007–1021. doi: 10.1161/CIRCRESAHA.116.303596. [DOI] [PubMed] [Google Scholar]
- 24.Baumbach GL, Heistad DD. Remodeling of cerebral arterioles in chronic hypertension. Hypertension. 1989;13(pt 2):968–972. doi: 10.1161/01.hyp.13.6.968. [DOI] [PubMed] [Google Scholar]
- 25.Rizzoni D, De Ciuceis C, Porteri E, Paiardi S, Boari GE, Mortini P, Cornali C, Cenzato M, Rodella LF, Borsani E, Rizzardi N, Platto C, Rezzani R, Rosei EA. Altered structure of small cerebral arteries in patients with essential hypertension. J Hypertens. 2009;27:838–845. doi: 10.1097/HJH.0b013e32832401ea. [DOI] [PubMed] [Google Scholar]
- 26.Faconti L, Bruno RM, Ghiadoni L, Taddei S, Virdis A. Ventricular and vascular stiffening in aging and hypertension. Curr Hypertens Rev. 2015;11:100–109. doi: 10.2174/1573402111666150529131208. [DOI] [PubMed] [Google Scholar]
- 27.Iadecola C. The pathobiology of vascular dementia. Neuron. 2013;80:844–866. doi: 10.1016/j.neuron.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Henskens LH, Kroon AA, van Oostenbrugge RJ, Gronenschild EH, Fuss-Lejeune MM, Hofman PA, Lodder J, de Leeuw PW. Increased aortic pulse wave velocity is associated with silent cerebral small-vessel disease in hypertensive patients. Hypertension. 2008;52:1120–1126. doi: 10.1161/HYPERTENSIONAHA.108.119024. [DOI] [PubMed] [Google Scholar]
- 29.Yang EY, Chambless L, Sharrett AR, Virani SS, Liu X, Tang Z, Boerwinkle E, Ballantyne CM, Nambi V. Carotid arterial wall characteristics are associated with incident ischemic stroke but not coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2012;43:103–108. doi: 10.1161/STROKEAHA.111.626200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zeki Al Hazzouri A, Newman AB, Simonsick E, Sink KM, Sutton Tyrrell K, Watson N, Satterfield S, Harris T, Yaffe K, Health ABCS. Pulse wave velocity and cognitive decline in elders: the Health, Aging, and Body Composition Study. Stroke. 2013;44:388–393. doi: 10.1161/STROKEAHA.112.673533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mitchell GF. Cerebral small vessel disease: role of aortic stiffness and pulsatile hemodynamics. J Hypertens. 2015;33:2025–2028. doi: 10.1097/HJH.0000000000000717. [DOI] [PubMed] [Google Scholar]
- 32.Moore SM, Zhang H, Maeda N, Doerschuk CM, Faber JE. Cardiovascular risk factors cause premature rarefaction of the collateral circulation and greater ischemic tissue injury. Angiogenesis. 2015;18:265–281. doi: 10.1007/s10456-015-9465-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Faber JE, Zhang H, Lassance-Soares RM, Prabhakar P, Najafi AH, Burnett MS, Epstein SE. Aging causes collateral rarefaction and increased severity of ischemic injury in multiple tissues. Arterioscler Thromb Vasc Biol. 2011;31:1748–1756. doi: 10.1161/ATVBAHA.111.227314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Y, Shen Q, Huang S, Li W, Muir ER, Long JA, Duong TQ. Cerebral angiography, blood flow and vascular reactivity in progressive hypertension. Neuroimage. 2015;111:329–337. doi: 10.1016/j.neuroimage.2015.02.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Muller M, van der Graaf Y, Visseren FL, Mali WP, Geerlings MI, SMART Study Group Hypertension and longitudinal changes in cerebral blood flow: the SMART-MR study. Ann Neurol. 2012;71:825–833. doi: 10.1002/ana.23554. [DOI] [PubMed] [Google Scholar]
- 36.De Ciuceis C, Cornali C, Porteri E, Mardighian D, Pinardi C, Fontanella MM, Rodella LF, Rezzani R, Rizzoni D, Boari GE, Rosei EA, Gasparotti R. Cerebral small-resistance artery structure and cerebral blood flow in normotensive subjects and hypertensive patients. Neuroradiology. 2014;56:1103–1111. doi: 10.1007/s00234-014-1423-2. [DOI] [PubMed] [Google Scholar]
- 37.Te Riet L, van Esch JH, Roks AJ, van den Meiracker AH, Danser AH. Hypertension: renin-angiotensin-aldosterone system alterations. Circ Res. 2015;116:960–975. doi: 10.1161/CIRCRESAHA.116.303587. [DOI] [PubMed] [Google Scholar]
- 38.Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116:991–1006. doi: 10.1161/CIRCRESAHA.116.305697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Romero JC, Reckelhoff JF. State-of-the-art lecture: role of angiotensin and oxidative stress in essential hypertension. Hypertension. 1999;34(pt 2):943–949. doi: 10.1161/01.hyp.34.4.943. [DOI] [PubMed] [Google Scholar]
- 40.Young CN, Davisson RL. Angiotensin-II, the brain, and hypertension: an update. Hypertension. 2015;66:920–926. doi: 10.1161/HYPERTENSIONAHA.115.03624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Daugherty A, Rateri DL, Lu H, Inagami T, Cassis LA. Hypercholesterolemia stimulates angiotensin peptide synthesis and contributes to atherosclerosis through the AT1A receptor. Circulation. 2004;110:3849–3857. doi: 10.1161/01.CIR.0000150540.54220.C4. [DOI] [PubMed] [Google Scholar]
- 42.Aono J, Suzuki J, Iwai M, Horiuchi M, Nagai T, Nishimura K, Inoue K, Ogimoto A, Okayama H, Higaki J. Deletion of the angiotensin II type 1a receptor prevents atherosclerotic plaque rupture in apolipoprotein E-/-mice [published correction appears in Arterioscler Thromb Vasc Biol. 2014;34:e18] Arterioscler Thromb Vasc Biol. 2012;32:1453–1459. doi: 10.1161/ATVBAHA.112.249516. [DOI] [PubMed] [Google Scholar]
- 43.Gupta A, Iadecola C. Impaired Aβ clearance: a potential link between atherosclerosis and Alzheimer’s disease. Front Aging Neurosci. 2015;7:115. doi: 10.3389/fnagi.2015.00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu J, Liu S, Matsumoto Y, Murakami S, Sugakawa Y, Kami A, Tanabe C, Maeda T, Michikawa M, Komano H, Zou K. Angiotensin type 1a receptor deficiency decreases amyloid β-protein generation and ameliorates brain amyloid pathology. Sci Rep. 2015;5:12059. doi: 10.1038/srep12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Faraco G, Park L, Zhou P, Luo W, Paul SM, Anrather J, Iadecola C. Hypertension enhances Aβ-induced neurovascular dysfunction, promotes β-secretase activity, and leads to amyloidogenic processing of APP. J Cereb Blood Flow Metab. 2016;36:241–252. doi: 10.1038/jcbfm.2015.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chan SL, Baumbach GL. Deficiency of Nox2 prevents angiotensin II-induced inward remodeling in cerebral arterioles. Front Physiol. 2013;4:133. doi: 10.3389/fphys.2013.00133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chan SL, Umesalma S, Baumbach GL. Epidermal growth factor receptor is critical for angiotensin II-mediated hypertrophy in cerebral arterioles. Hypertension. 2015;65:806–812. doi: 10.1161/HYPERTENSIONAHA.114.04794. [DOI] [PubMed] [Google Scholar]
- 48.Wu J, Thabet SR, Kirabo A, Trott DW, Saleh MA, Xiao L, Madhur MS, Chen W, Harrison DG. Inflammation and mechanical stretch promote aortic stiffening in hypertension through activation of p38 mitogen-activated protein kinase. Circ Res. 2014;114:616–625. doi: 10.1161/CIRCRESAHA.114.302157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Katusic ZS, Austin SA. Endothelial nitric oxide: protector of a healthy mind. Eur Heart J. 2014;35:888–894. doi: 10.1093/eurheartj/eht544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cipolla MJ. The Cerebral Circulation. San Rafael, CA: Morgan & Claypool Life Sciences; 2009. pp. 1–59. [PubMed] [Google Scholar]
- 51.Andresen J, Shafi NI, Bryan RM., Jr Endothelial influences on cerebro-vascular tone. J Appl Physiol (1985) 2006;100:318–327. doi: 10.1152/japplphysiol.00937.2005. [DOI] [PubMed] [Google Scholar]
- 52.Chen BR, Kozberg MG, Bouchard MB, Shaik MA, Hillman EM. A critical role for the vascular endothelium in functional neurovascular coupling in the brain. J Am Heart Assoc. 2014;3:e000787. doi: 10.1161/JAHA.114.000787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Di Marco LY, Venneri A, Farkas E, Evans PC, Marzo A, Frangi AF. Vascular dysfunction in the pathogenesis of Alzheimer’s disease: a review of endothelium-mediated mechanisms and ensuing vicious circles. Neurobiol Dis. 2015;82:593–606. doi: 10.1016/j.nbd.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 54.Madden JA. Role of the vascular endothelium and plaque in acute ischemic stroke. Neurology. 2012;79(suppl 1):S58–S62. doi: 10.1212/WNL.0b013e3182695836. [DOI] [PubMed] [Google Scholar]
- 55.Poggesi A, Pasi M, Pescini F, Pantoni L, Inzitari D. Circulating biologic markers of endothelial dysfunction in cerebral small vessel disease: a review. J Cereb Blood Flow Metab. 2016;36:72–94. doi: 10.1038/jcbfm.2015.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hoth KF, Tate DF, Poppas A, Forman DE, Gunstad J, Moser DJ, Paul RH, Jefferson AL, Haley AP, Cohen RA. Endothelial function and white matter hyperintensities in older adults with cardiovascular disease. Stroke. 2007;38:308–312. doi: 10.1161/01.STR.0000254517.04275.3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hillman EM. Coupling mechanism and significance of the BOLD signal: a status report. Annu Rev Neurosci. 2014;37:161–181. doi: 10.1146/annurev-neuro-071013-014111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jennings JR, Muldoon MF, Ryan C, Price JC, Greer P, Sutton-Tyrrell K, van der Veen FM, Meltzer CC. Reduced cerebral blood flow response and compensation among patients with untreated hypertension. Neurology. 2005;64:1358–1365. doi: 10.1212/01.WNL.0000158283.28251.3C. [DOI] [PubMed] [Google Scholar]
- 59.van Beek AH, Claassen JA, Rikkert MG, Jansen RW. Cerebral autoregulation: an overview of current concepts and methodology with special focus on the elderly. J Cereb Blood Flow Metab. 2008;28:1071–1085. doi: 10.1038/jcbfm.2008.13. [DOI] [PubMed] [Google Scholar]
- 60.Jordan JD, Powers WJ. Cerebral autoregulation and acute ischemic stroke. Am J Hypertens. 2012;25:946–950. doi: 10.1038/ajh.2012.53. [DOI] [PubMed] [Google Scholar]
- 61.Traon AP, Costes-Salon MC, Galinier M, Fourcade J, Larrue V. Dynamics of cerebral blood flow autoregulation in hypertensive patients [published correction appears in J Neurol Sci. 2002;201:91] J Neurol Sci. 2002;195:139–144. doi: 10.1016/s0022-510x(02)00010-2. [DOI] [PubMed] [Google Scholar]
- 62.Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions [published correction appears in Lancet Neurol. 2014;14:874] Lancet Neurol. 2015;14:914–925. doi: 10.1016/S1474-4422(15)00111-8. [DOI] [PubMed] [Google Scholar]
- 63.Price RS, Kasner SE. Hypertension and hypertensive encephalopathy. Handb Clin Neurol. 2014;119:161–167. doi: 10.1016/B978-0-7020-4086-3.00012-6. [DOI] [PubMed] [Google Scholar]
- 64.Varon J, Marik PE. Clinical review: the management of hypertensive crises. Crit Care. 2003;7:374–384. doi: 10.1186/cc2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Back SA, Kroenke CD, Sherman LS, Lawrence G, Gong X, Taber EN, Sonnen JA, Larson EB, Montine TJ. White matter lesions defined by diffusion tensor imaging in older adults. Ann Neurol. 2011;70:465–476. doi: 10.1002/ana.22484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Feekes JA, Cassell MD. The vascular supply of the functional compartments of the human striatum. Brain. 2006;129(pt 8):2189–2201. doi: 10.1093/brain/awl158. [DOI] [PubMed] [Google Scholar]
- 67.Feekes JA, Hsu SW, Chaloupka JC, Cassell MD. Tertiary microvascular territories define lacunar infarcts in the basal ganglia. Ann Neurol. 2005;58:18–30. doi: 10.1002/ana.20505. [DOI] [PubMed] [Google Scholar]
- 68.Purkayastha S, Fadar O, Mehregan A, Salat DH, Moscufo N, Meier DS, Guttmann CR, Fisher ND, Lipsitz LA, Sorond FA. Impaired cere-brovascular hemodynamics are associated with cerebral white matter damage. J Cereb Blood Flow Metab. 2014;34:228–234. doi: 10.1038/jcbfm.2013.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pires PW, Dams Ramos CM, Matin N, Dorrance AM. The effects of hypertension on the cerebral circulation. Am J Physiol Heart Circ Physiol. 2013;304:H1598–H1614. doi: 10.1152/ajpheart.00490.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tietz S, Engelhardt B. Brain barriers: crosstalk between complex tight junctions and adherens junctions. J Cell Biol. 2015;209:493–506. doi: 10.1083/jcb.201412147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhao Z, Nelson AR, Betsholtz C, Zlokovic BV. Establishment and dysfunction of the blood-brain barrier. Cell. 2015;163:1064–1078. doi: 10.1016/j.cell.2015.10.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Winkler EA, Sagare AP, Zlokovic BV. The pericyte: a forgotten cell type with important implications for Alzheimer’s disease? Brain Pathol. 2014;24:371–386. doi: 10.1111/bpa.12152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rosenberg GA. Neurological diseases in relation to the blood-brain barrier. J Cereb Blood Flow Metab. 2012;32:1139–1151. doi: 10.1038/jcbfm.2011.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Huisa BN, Caprihan A, Thompson J, Prestopnik J, Qualls CR, Rosenberg GA. Long-term blood-brain barrier permeability changes in Binswanger disease. Stroke. 2015;46:2413–2418. doi: 10.1161/STROKEAHA.115.009589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wardlaw JM, Smith C, Dichgans M. Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging [published correction appears in Lancet. 2013;12:532] Lancet Neurol. 2013;12:483–497. doi: 10.1016/S1474-4422(13)70060-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Joutel A, Faraci FM. Cerebral small vessel disease: insights and opportunities from mouse models of collagen IV-related small vessel disease and cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Stroke. 2014;45:1215–1221. doi: 10.1161/STROKEAHA.113.002878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nakagawa T, Hasegawa Y, Uekawa K, Ma M, Katayama T, Sueta D, Toyama K, Kataoka K, Koibuchi N, Maeda M, Kuratsu J, Kim-Mitsuyama S. Renal denervation prevents stroke and brain injury via attenuation of oxidative stress in hypertensive rats. J Am Heart Assoc. 2013;2:e000375. doi: 10.1161/JAHA.113.000375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Toth P, Tucsek Z, Sosnowska D, Gautam T, Mitschelen M, Tarantini S, Deak F, Koller A, Sonntag WE, Csiszar A, Ungvari Z. Age-related autoregulatory dysfunction and cerebromicrovascular injury in mice with angiotensin II-induced hypertension. J Cereb Blood Flow Metab. 2013;33:1732–1742. doi: 10.1038/jcbfm.2013.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Akiguchi I, Tomimoto H, Suenaga T, Wakita H, Budka H. Blood-brain barrier dysfunction in Binswanger’s disease; an immunohistochemical study. Acta Neuropathol. 1998;95:78–84. doi: 10.1007/s004010050768. [DOI] [PubMed] [Google Scholar]
- 80.Dankbaar JW, Hom J, Schneider T, Cheng SC, Lau BC, van der Schaaf I, Virmani S, Pohlman S, Wintermark M. Age- and anatomy-related values of blood-brain barrier permeability measured by perfusion-CT in non-stroke patients. J Neuroradiol. 2009;36:219–227. doi: 10.1016/j.neurad.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 81.Rosenberg GA, Wallin A, Wardlaw JM, Markus HS, Montaner J, Wolfson L, Iadecola C, Zlokovic BV, Joutel A, Dichgans M, Duering M, Schmidt R, Korczyn AD, Grinberg LT, Chui HC, Hachinski V. Consensus statement for diagnosis of subcortical small vessel disease. J Cereb Blood Flow Metab. 2016;36:6–25. doi: 10.1038/jcbfm.2015.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Armulik A, Genové G, Betsholtz C. Pericytes: developmental, physiological, and pathological perspectives, problems, and promises. Dev Cell. 2011;21:193–215. doi: 10.1016/j.devcel.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 83.Suzuki K, Masawa N, Sakata N, Takatama M. Pathologic evidence of microvascular rarefaction in the brain of renal hypertensive rats. J Stroke Cerebrovasc Dis. 2003;12:8–16. doi: 10.1053/jscd.2003.1. [DOI] [PubMed] [Google Scholar]
- 84.Wechsler D. Wechsler Adult Intelligence Scale-Revised. New York, NY: Psychological Corp; 1981. [Google Scholar]
- 85.Schmidt M. Rey Auditory Verbal Learning Test: A Handbook. Los Angeles, CA: Western Psychological Services; 1996. [Google Scholar]
- 86.Rosenberg SJ, Ryan JJ, Prifitera A. Rey Auditory-Verbal Learning Test performance of patients with and without memory impairment. J Clin Psychol. 1984;40:785–787. doi: 10.1002/1097-4679(198405)40:3<785::aid-jclp2270400325>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 87.Knopman DS, Ryberg S. A verbal memory test with high predictive accuracy for dementia of the Alzheimer type. Arch Neurol. 1989;46:141–145. doi: 10.1001/archneur.1989.00520380041011. [DOI] [PubMed] [Google Scholar]
- 88.Benton AL, Hamsher JDS, Sivan AB. Multilingual Aphasia Examination. Iowa City, IA: AJA Associates; 1989. [Google Scholar]
- 89.Lezak M. Neuropsychological Assessment. New York, NY: Oxford University Press; 2004. [Google Scholar]
- 90.Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, Mellits ED, Clark C. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD), part I: clinical and neuropsychological assessment of Alzheimer’s disease. Neurology. 1989;39:1159–1165. doi: 10.1212/wnl.39.9.1159. [DOI] [PubMed] [Google Scholar]
- 91.Army Individual Test Battery: Manual of Directions and Scoring. Washington, DC: War Department, Adjutant General’s Office; 1944. [Google Scholar]
- 92.Reitan R. Validity of the Trail Making Test as an indicator of organic brain damage. Perceptual and Motor Skills. 1958;18:271–276. [Google Scholar]
- 93.Yaffe K, Vittinghoff E, Pletcher MJ, Hoang TD, Launer LJ, Whitmer R, Coker LH, Sidney S. Early adult to midlife cardiovascular risk factors and cognitive function. Circulation. 2014;129:1560–1567. doi: 10.1161/CIRCULATIONAHA.113.004798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gottesman RF, Schneider AL, Albert M, Alonso A, Bandeen-Roche K, Coker L, Coresh J, Knopman D, Power MC, Rawlings A, Sharrett AR, Wruck LM, Mosley TH. Midlife hypertension and 20-year cognitive change: the Atherosclerosis Risk in Communities neurocognitive study. JAMA Neurol. 2014;71:1218–1227. doi: 10.1001/jamaneurol.2014.1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Knopman D, Boland LL, Mosley T, Howard G, Liao D, Szklo M, McGovern P, Folsom AR, Atherosclerosis Risk in Communities (ARIC) Study Investigators Cardiovascular risk factors and cognitive decline in middle-aged adults. Neurology. 2001;56:42–48. doi: 10.1212/wnl.56.1.42. [DOI] [PubMed] [Google Scholar]
- 96.Köhler S, Baars MA, Spauwen P, Schievink S, Verhey FR, van Boxtel MJ. Temporal evolution of cognitive changes in incident hypertension: prospective cohort study across the adult age span. Hypertension. 2014;63:245–251. doi: 10.1161/HYPERTENSIONAHA.113.02096. [DOI] [PubMed] [Google Scholar]
- 97.Cerhan JR, Folsom AR, Mortimer JA, Shahar E, Knopman DS, McGovern PG, Hays MA, Crum LD, Heiss G. Correlates of cognitive function in middle-aged adults: Atherosclerosis Risk in Communities (ARIC) Study Investigators. Gerontology. 1998;44:95–105. doi: 10.1159/000021991. [DOI] [PubMed] [Google Scholar]
- 98.Swan GE, Carmelli D, Larue A. Systolic blood pressure tracking over 25 to 30 years and cognitive performance in older adults. Stroke. 1998;29:2334–2340. doi: 10.1161/01.str.29.11.2334. [DOI] [PubMed] [Google Scholar]
- 99.Debette S, Seshadri S, Beiser A, Au R, Himali JJ, Palumbo C, Wolf PA, DeCarli C. Midlife vascular risk factor exposure accelerates structural brain aging and cognitive decline. Neurology. 2011;77:461–468. doi: 10.1212/WNL.0b013e318227b227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Knopman DS, Mosley TH, Catellier DJ, Coker LH, Fourteen-year longitudinal study of vascular risk factors, APOE genotype, and cognition: the ARIC MRI Study longitudinal study of vascular risk factors, APOE genotype, and cognition: the ARIC MRI Study. Alzheimers Dement. 2009;5:207–214. doi: 10.1016/j.jalz.2009.01.027. [DOI] [PubMed] [Google Scholar]
- 101.Hachinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, Powers WJ, DeCarli C, Merino JG, Kalaria RN, Vinters HV, Holtzman DM, Rosenberg GA, Wallin A, Dichgans M, Marler JR, Leblanc GG. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards [published correction appears in Stroke. 2007;38:1118] Stroke. 2006;37:2220–2241. doi: 10.1161/01.STR.0000237236.88823.47. [DOI] [PubMed] [Google Scholar]
- 102.Starr JM, Whalley LJ, Inch S, Shering PA. Blood pressure and cognitive function in healthy old people. J Am Geriatr Soc. 1993;41:753–756. doi: 10.1111/j.1532-5415.1993.tb07466.x. [DOI] [PubMed] [Google Scholar]
- 103.Kilander L, Nyman H, Boberg M, Hansson L, Lithell H. Hypertension is related to cognitive impairment: a 20-year follow-up of 999 men. Hypertension. 1998;31:780–786. doi: 10.1161/01.hyp.31.3.780. [DOI] [PubMed] [Google Scholar]
- 104.Kuo HK, Sorond F, Iloputaife I, Gagnon M, Milberg W, Lipsitz LA. Effect of blood pressure on cognitive functions in elderly persons. J Gerontol A Biol Sci Med Sci. 2004;59:1191–1194. doi: 10.1093/gerona/59.11.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Obisesan TO, Obisesan OA, Martins S, Alamgir L, Bond V, Maxwell C, Gillum RF. High blood pressure, hypertension, and high pulse pressure are associated with poorer cognitive function in persons aged 60 and older: the Third National Health and Nutrition Examination Survey. J Am Geriatr Soc. 2008;56:501–509. doi: 10.1111/j.1532-5415.2007.01592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Launer LJ, Masaki K, Petrovitch H, Foley D, Havlik RJ. The association between midlife blood pressure levels and late-life cognitive function: the Honolulu-Asia Aging Study. JAMA. 1995;274:1846–1851. [PubMed] [Google Scholar]
- 107.Guo Z, Fratiglioni L, Winblad B, Viitanen M. Blood pressure and performance on the Mini-Mental State Examination in the very old: cross-sectional and longitudinal data from the Kungsholmen Project. Am J Epidemiol. 1997;145:1106–1113. doi: 10.1093/oxfordjournals.aje.a009073. [DOI] [PubMed] [Google Scholar]
- 108.Waldstein SR, Giggey PP, Thayer JF, Zonderman AB. Nonlinear relations of blood pressure to cognitive function: the Baltimore Longitudinal Study of Aging. Hypertension. 2005;45:374–379. doi: 10.1161/01.HYP.0000156744.44218.74. [DOI] [PubMed] [Google Scholar]
- 109.Farmer ME, White LR, Abbott RD, Kittner SJ, Kaplan E, Wolz MM, Brody JA, Wolf PA. Blood pressure and cognitive performance: the Framingham Study. Am J Epidemiol. 1987;126:1103–1114. doi: 10.1093/oxfordjournals.aje.a114749. [DOI] [PubMed] [Google Scholar]
- 110.Richmond R, Law J, Kay-Lambkin F. Higher blood pressure associated with higher cognition and functionality among centenarians in Australia. Am J Hypertens. 2011;24:299–303. doi: 10.1038/ajh.2010.236. [DOI] [PubMed] [Google Scholar]
- 111.Peltz CB, Corrada MM, Berlau DJ, Kawas CH. Cognitive impairment in nondemented oldest-old: prevalence and relationship to cardiovascular risk factors. Alzheimers Dement. 2012;8:87–94. doi: 10.1016/j.jalz.2011.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lyngdoh T, Viswanathan B, Kobrosly R, van Wijngaarden E, Huber B, Davidson PW, Cory-Slechta DA, Strain JJ, Myers GJ, Bovet P. Blood pressure and cognitive function: a prospective analysis among adolescents in Seychelles [published correction appears in J Hypertens. 2013;31:2105] J Hypertens. 2013;31:1175–1182. doi: 10.1097/HJH.0b013e3283604176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Elias MF, Wolf PA, D’Agostino RB, Cobb J, White LR. Untreated blood pressure level is inversely related to cognitive functioning: the Framingham Study. Am J Epidemiol. 1993;138:353–364. doi: 10.1093/oxfordjournals.aje.a116868. [DOI] [PubMed] [Google Scholar]
- 114.Kilander L, Nyman H, Boberg M, Lithell H. The association between low diastolic blood pressure in middle age and cognitive function in old age: a population-based study. Age Ageing. 2000;29:243–248. doi: 10.1093/ageing/29.3.243. [DOI] [PubMed] [Google Scholar]
- 115.Elias PK, Elias MF, Robbins MA, Budge MM. Blood pressure-related cognitive decline: does age make a difference? Hypertension. 2004;44:631–636. doi: 10.1161/01.HYP.0000145858.07252.99. [DOI] [PubMed] [Google Scholar]
- 116.Chen KH, Henderson VW, Stolwyk RJ, Dennerstein L, Szoeke C. Prehypertension in midlife is associated with worse cognition a decade later in middle-aged and older women. Age Ageing. 2015;44:439–445. doi: 10.1093/ageing/afv026. [DOI] [PubMed] [Google Scholar]
- 117.Taylor C, Tillin T, Chaturvedi N, Dewey M, Ferri CP, Hughes A, Prince M, Richards M, Shah A, Stewart R. Midlife hypertensive status and cognitive function 20 years later: the Southall and Brent revisited study. J Am Geriatr Soc. 2013;61:1489–1498. doi: 10.1111/jgs.12416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kesse-Guyot E, Julia C, Andreeva V, Fezeu L, Hercberg S, Galan P. Evidence of a cumulative effect of cardiometabolic disorders at midlife and subsequent cognitive function. Age Ageing. 2015;44:648–654. doi: 10.1093/ageing/afv053. [DOI] [PubMed] [Google Scholar]
- 119.Hebert LE, Scherr PA, Bennett DA, Bienias JL, Wilson RS, Morris MC, Evans DA. Blood pressure and late-life cognitive function change: a biracial longitudinal population study. Neurology. 2004;62:2021–2024. doi: 10.1212/01.wnl.0000129258.93137.4b. [DOI] [PubMed] [Google Scholar]
- 120.Solfrizzi V, Panza F, Colacicco AM, D’Introno A, Capurso C, Torres F, Grigoletto F, Maggi S, Del Parigi A, Reiman EM, Caselli RJ, Scafato E, Farchi G, Capurso A, Italian Longitudinal Study on Aging Working Group Vascular risk factors, incidence of MCI, and rates of progression to dementia. Neurology. 2004;63:1882–1891. doi: 10.1212/01.wnl.0000144281.38555.e3. [DOI] [PubMed] [Google Scholar]
- 121.Yaffe K, Haan M, Blackwell T, Cherkasova E, Whitmer RA, West N. Metabolic syndrome and cognitive decline in elderly Latinos: findings from the Sacramento Area Latino Study of Aging study. J Am Geriatr Soc. 2007;55:758–762. doi: 10.1111/j.1532-5415.2007.01139.x. [DOI] [PubMed] [Google Scholar]
- 122.Johnson KC, Margolis KL, Espeland MA, Colenda CC, Fillit H, Manson JE, Masaki KH, Mouton CP, Prineas R, Robinson JG, Wassertheil-Smoller S, Women’s Health Initiative Memory Study and Women’s Health Initiative Investigators A prospective study of the effect of hypertension and baseline blood pressure on cognitive decline and dementia in postmenopausal women: the Women’s Health Initiative Memory Study. J Am Geriatr Soc. 2008;56:1449–1458. doi: 10.1111/j.1532-5415.2008.01806.x. [DOI] [PubMed] [Google Scholar]
- 123.Bohannon AD, Fillenbaum GG, Pieper CF, Hanlon JT, Blazer DG. Relationship of race/ethnicity and blood pressure to change in cognitive function. J Am Geriatr Soc. 2002;50:424–429. doi: 10.1046/j.1532-5415.2002.50104.x. [DOI] [PubMed] [Google Scholar]
- 124.Dregan A, Stewart R, Gulliford MC. Cardiovascular risk factors and cognitive decline in adults aged 50 and over: a population-based cohort study. Age Ageing. 2013;42:338–345. doi: 10.1093/ageing/afs166. [DOI] [PubMed] [Google Scholar]
- 125.Yasar S, Ko JY, Nothelle S, Mielke MM, Carlson MC. Evaluation of the effect of systolic blood pressure and pulse pressure on cognitive function: the Women’s Health and Aging Study II. PLoS One. 2011;6:e27976. doi: 10.1371/journal.pone.0027976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.van Vliet P, Westendorp RG, van Heemst D, de Craen AJ, Oleksik AM. Cognitive decline precedes late-life longitudinal changes in vascular risk factors. J Neurol Neurosurg Psychiatry. 2010;81:1028–1032. doi: 10.1136/jnnp.2009.182519. [DOI] [PubMed] [Google Scholar]
- 127.Euser SM, van Bemmel T, Schram MT, Gussekloo J, Hofman A, Westendorp RG, Breteler MM. The effect of age on the association between blood pressure and cognitive function later in life. J Am Geriatr Soc. 2009;57:1232–1237. doi: 10.1111/j.1532-5415.2009.02264.x. [DOI] [PubMed] [Google Scholar]
- 128.Sabayan B, Oleksik AM, Maier AB, van Buchem MA, Poortvliet RK, de Ruijter W, Gussekloo J, de Craen AJ, Westendorp RG. High blood pressure and resilience to physical and cognitive decline in the oldest old: the Leiden 85-plus Study. J Am Geriatr Soc. 2012;60:2014–2019. doi: 10.1111/j.1532-5415.2012.04203.x. [DOI] [PubMed] [Google Scholar]
- 129.Harrison SL, Stephan BC, Siervo M, Granic A, Davies K, Wesnes KA, Kirkwood TB, Robinson L, Jagger C. Is there an association between metabolic syndrome and cognitive function in very old adults? The Newcastle 85+ Study. J Am Geriatr Soc. 2015;63:667–675. doi: 10.1111/jgs.13358. [DOI] [PubMed] [Google Scholar]
- 130.Suhr JA, Stewart JC, France CR. The relationship between blood pressure and cognitive performance in the Third National Health and Nutrition Examination Survey (NHANES III) Psychosom Med. 2004;66:291–297. doi: 10.1097/01.psy.0000127870.64234.9f. [DOI] [PubMed] [Google Scholar]
- 131.Elias MF, D’Agostino RB, Elias PK, Wolf PA. Neuropsychological test performance, cognitive functioning, blood pressure, and age: the Framingham Heart Study. Exp Aging Res. 1995;21:369–391. doi: 10.1080/03610739508253991. [DOI] [PubMed] [Google Scholar]
- 132.Zilberman JM, Cerezo GH, Del Sueldo M, Fernandez-Pérez C, Martell-Claros N, Vicario A. Association between hypertension, menopause, and cognition in women. J Clin Hypertens (Greenwich) 2015;17:970–976. doi: 10.1111/jch.12643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22:312–318. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 134.Elias PK, Elias MF, D’Agostino RB, Cupples LA, Wilson PW, Silbershatz H, Wolf PA. NIDDM and blood pressure as risk factors for poor cognitive performance: the Framingham Study. Diabetes Care. 1997;20:1388–1395. doi: 10.2337/diacare.20.9.1388. [DOI] [PubMed] [Google Scholar]
- 135.Wolf PA, Beiser A, Elias MF, Au R, Vasan RS, Seshadri S. Relation of obesity to cognitive function: importance of central obesity and synergistic influence of concomitant hypertension: the Framingham Heart Study. Curr Alzheimer Res. 2007;4:111–116. doi: 10.2174/156720507780362263. [DOI] [PubMed] [Google Scholar]
- 136.Uiterwijk R, Huijts M, Staals J, Rouhl RP, De Leeuw PW, Kroon AA, Van Oostenbrugge RJ. Endothelial activation is associated with cognitive performance in patients with hypertension. Am J Hypertens. 2016;29:464–469. doi: 10.1093/ajh/hpv122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kovács KR, Bajkó Z, Szekeres CC, Csapó K, Oláh L, Magyar MT, Molnár S, Czuriga D, Kardos L, Burainé AB, Bereczki D, Soltész P, Csiba L. Elevated LDL-C combined with hypertension worsens subclinical vascular impairment and cognitive function. J Am Soc Hypertens. 2014;8:550–560. doi: 10.1016/j.jash.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 138.Bangen KJ, Beiser A, Delano-Wood L, Nation DA, Lamar M, Libon DJ, Bondi MW, Seshadri S, Wolf PA, Au R. APOE genotype modifies the relationship between midlife vascular risk factors and later cognitive decline. J Stroke Cerebrovasc Dis. 2013;22:1361–1369. doi: 10.1016/j.jstrokecerebrovasdis.2013.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Haan MN, Shemanski L, Jagust WJ, Manolio TA, Kuller L. The role of APOE epsilon4 in modulating effects of other risk factors for cognitive decline in elderly persons. JAMA. 1999;282:40–46. doi: 10.1001/jama.282.1.40. [DOI] [PubMed] [Google Scholar]
- 140.Carmelli D, Swan GE, Reed T, Miller B, Wolf PA, Jarvik GP, Schellenberg GD. Midlife cardiovascular risk factors, ApoE, and cognitive decline in elderly male twins. Neurology. 1998;50:1580–1585. doi: 10.1212/wnl.50.6.1580. [DOI] [PubMed] [Google Scholar]
- 141.Peila R, White LR, Petrovich H, Masaki K, Ross GW, Havlik RJ, Launer LJ. Joint effect of the APOE gene and midlife systolic blood pressure on late-life cognitive impairment: the Honolulu-Asia Aging Study. Stroke. 2001;32:2882–2889. doi: 10.1161/hs1201.100392. [DOI] [PubMed] [Google Scholar]
- 142.Andrews S, Das D, Anstey KJ, Easteal S. Interactive effect of APOE genotype and blood pressure on cognitive decline: the PATH through life study. J Alzheimers Dis. 2015;44:1087–1098. doi: 10.3233/JAD-140630. [DOI] [PubMed] [Google Scholar]
- 143.de Frias CM, Schaie KW, Willis SL. Hypertension moderates the effect of APOE on 21-year cognitive trajectories. Psychol Aging. 2014;29:431–439. doi: 10.1037/a0036828. [DOI] [PubMed] [Google Scholar]
- 144.Wersching H, Guske K, Hasenkamp S, Hagedorn C, Schiwek S, Jansen S, Witte V, Wellmann J, Lohmann H, Duning K, Kremerskothen J, Knecht S, Brand E, Floel A. Impact of common KIBRA allele on human cognitive functions. Neuropsychopharmacology. 2011;36:1296–1304. doi: 10.1038/npp.2011.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Østergaard SD, Mukherjee S, Sharp SJ, Proitsi P, Lotta LA, Day F, Perry JR, Boehme KL, Walter S, Kauwe JS, Gibbons LE, Alzheimer’s Disease Genetics Consortium; GERAD1 Consortium; EPIC-InterAct Consortium. Larson EB, Powell JF, Langenberg C, Crane PK, Wareham NJ, Scott RA. Associations between potentially modifiable risk factors and Alzheimer disease: a mendelian randomization study. PLoS Med. 2015;12:e1001841. doi: 10.1371/journal.pmed.1001841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Yoshitake T, Kiyohara Y, Kato I, Ohmura T, Iwamoto H, Nakayama K, Ohmori S, Nomiyama K, Kawano H, Ueda K, Sueishi K, Tsuneyoshi M, Fujishima M. Incidence and risk factors of vascular dementia and Alzheimer’s disease in a defined elderly Japanese population: the Hisayama Study. Neurology. 1995;45:1161–1168. doi: 10.1212/wnl.45.6.1161. [DOI] [PubMed] [Google Scholar]
- 147.Oveisgharan S, Hachinski V. Hypertension, executive dysfunction, and progression to dementia: the Canadian Study of Health and Aging. Arch Neurol. 2010;67:187–192. doi: 10.1001/archneurol.2009.312. [DOI] [PubMed] [Google Scholar]
- 148.Posner HB, Tang MX, Luchsinger J, Lantigua R, Stern Y, Mayeux R. The relationship of hypertension in the elderly to AD, vascular dementia, and cognitive function. Neurology. 2002;58:1175–1181. doi: 10.1212/wnl.58.8.1175. [DOI] [PubMed] [Google Scholar]
- 149.Qiu C, von Strauss E, Fastbom J, Winblad B, Fratiglioni L. Low blood pressure and risk of dementia in the Kungsholmen project: a 6-year follow-up study. Arch Neurol. 2003;60:223–228. doi: 10.1001/archneur.60.2.223. [DOI] [PubMed] [Google Scholar]
- 150.Skoog I, Lernfelt B, Landahl S, Palmertz B, Andreasson LA, Nilsson L, Persson G, Odén A, Svanborg A. 15-Year longitudinal study of blood pressure and dementia. Lancet. 1996;347:1141–1145. doi: 10.1016/s0140-6736(96)90608-x. [DOI] [PubMed] [Google Scholar]
- 151.Ruitenberg A, Skoog I, Ott A, Aevarsson O, Witteman JC, Lernfelt B, van Harskamp F, Hofman A, Breteler MM. Blood pressure and risk of dementia: results from the Rotterdam study and the Gothenburg H-70 Study. Dement Geriatr Cogn Disord. 2001;12:33–39. doi: 10.1159/000051233. doi: 51233. [DOI] [PubMed] [Google Scholar]
- 152.Qiu C, von Strauss E, Winblad B, Fratiglioni L. Decline in blood pressure over time and risk of dementia: a longitudinal study from the Kungsholmen project. Stroke. 2004;35:1810–1815. doi: 10.1161/01.STR.0000133128.42462.ef. [DOI] [PubMed] [Google Scholar]
- 153.Kokmen E, Beard CM, Chandra V, Offord KP, Schoenberg BS, Ballard DJ. Clinical risk factors for Alzheimer’s disease: a population-based case-control study. Neurology. 1991;41:1393–1397. doi: 10.1212/wnl.41.9.1393. [DOI] [PubMed] [Google Scholar]
- 154.Verghese J, Lipton RB, Hall CB, Kuslansky G, Katz MJ. Low blood pressure and the risk of dementia in very old individuals. Neurology. 2003;61:1667–1672. doi: 10.1212/01.wnl.0000098934.18300.be. [DOI] [PubMed] [Google Scholar]
- 155.Kivipelto M, Helkala EL, Hänninen T, Laakso MP, Hallikainen M, Alhainen K, Soininen H, Tuomilehto J, Nissinen A. Midlife vascular risk factors and late-life mild cognitive impairment: a population-based study. Neurology. 2001;56:1683–1689. doi: 10.1212/wnl.56.12.1683. [DOI] [PubMed] [Google Scholar]
- 156.Kivipelto M, Helkala EL, Laakso MP, Hänninen T, Hallikainen M, Alhainen K, Soininen H, Tuomilehto J, Nissinen A. Midlife vascular risk factors and Alzheimer’s disease in later life: longitudinal, population based study. BMJ. 2001;322:1447–1451. doi: 10.1136/bmj.322.7300.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Whitmer RA, Sidney S, Selby J, Johnston SC, Yaffe K. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology. 2005;64:277–281. doi: 10.1212/01.WNL.0000149519.47454.F2. [DOI] [PubMed] [Google Scholar]
- 158.Launer LJ, Ross GW, Petrovitch H, Masaki K, Foley D, White LR, Havlik RJ. Midlife blood pressure and dementia: the Honolulu-Asia Aging Study. Neurobiol Aging. 2000;21:49–55. doi: 10.1016/s0197-4580(00)00096-8. [DOI] [PubMed] [Google Scholar]
- 159.Ivan CS, Seshadri S, Beiser A, Au R, Kase CS, Kelly-Hayes M, Wolf PA. Dementia after stroke: the Framingham Study. Stroke. 2004;35:1264–1268. doi: 10.1161/01.STR.0000127810.92616.78. [DOI] [PubMed] [Google Scholar]
- 160.Waldstein SR, Rice SC, Thayer JF, Najjar SS, Scuteri A, Zonderman AB. Pulse pressure and pulse wave velocity are related to cognitive decline in the Baltimore Longitudinal Study of Aging. Hypertension. 2008;51:99–104. doi: 10.1161/HYPERTENSIONAHA.107.093674. [DOI] [PubMed] [Google Scholar]
- 161.Stewart R, Xue QL, Masaki K, Petrovitch H, Ross GW, White LR, Launer LJ. Change in blood pressure and incident dementia: a 32-year prospective study. Hypertension. 2009;54:233–240. doi: 10.1161/HYPERTENSIONAHA.109.128744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ishii M, Iadecola C. Metabolic and non-cognitive manifestations of Alzheimer’s disease: the hypothalamus as both culprit and target of pathology. Cell Metab. 2015;22:761–776. doi: 10.1016/j.cmet.2015.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Iadecola C, Davisson RL. Hypertension and cerebrovascular dysfunction. Cell Metab. 2008;7:476–484. doi: 10.1016/j.cmet.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Li JQ, Tan L, Wang HF, Tan MS, Tan L, Xu W, Zhao QF, Wang J, Jiang T, Yu JT. Risk factors for predicting progression from mild cognitive impairment to Alzheimer’s disease: a systematic review and meta-analysis of cohort studies. J Neurol Neurosurg Psychiatry. 2016;87:476–484. doi: 10.1136/jnnp-2014-310095. [DOI] [PubMed] [Google Scholar]
- 165.Xu W, Tan L, Wang HF, Jiang T, Tan MS, Tan L, Zhao QF, Li JQ, Wang J, Yu JT. Meta-analysis of modifiable risk factors for Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2015;86:1299–1306. doi: 10.1136/jnnp-2015-310548. [DOI] [PubMed] [Google Scholar]
- 166.Power MC, Weuve J, Gagne JJ, McQueen MB, Viswanathan A, Blacker D. The association between blood pressure and incident Alzheimer disease: a systematic review and meta-analysis. Epidemiology. 2011;22:646–659. doi: 10.1097/EDE.0b013e31822708b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Peila R, White LR, Masaki K, Petrovitch H, Launer LJ. Reducing the risk of dementia: efficacy of long-term treatment of hypertension. Stroke. 2006;37:1165–1170. doi: 10.1161/01.STR.0000217653.01615.93. [DOI] [PubMed] [Google Scholar]
- 168.Khachaturian AS, Zandi PP, Lyketsos CG, Hayden KM, Skoog I, Norton MC, Tschanz JT, Mayer LS, Welsh-Bohmer KA, Breitner JC. Antihypertensive medication use and incident Alzheimer disease: the Cache County Study. Arch Neurol. 2006;63:686–692. doi: 10.1001/archneur.63.5.noc60013. [DOI] [PubMed] [Google Scholar]
- 169.Seshadri S. Delaying dementia: can antihypertensives prevent Alzheimer dementia? Neurology. 2013;81:860–862. doi: 10.1212/WNL.0b013e3182a35296. [DOI] [PubMed] [Google Scholar]
- 170.Petrovitch H, White LR, Izmirilian G, Ross GW, Havlik RJ, Markesbery W, Nelson J, Davis DG, Hardman J, Foley DJ, Launer LJ. Midlife blood pressure and neuritic plaques, neurofibrillary tangles, and brain weight at death: the HAAS: Honolulu-Asia Aging Study. Neurobiol Aging. 2000;21:57–62. doi: 10.1016/s0197-4580(00)00106-8. [DOI] [PubMed] [Google Scholar]
- 171.Hoffman LB, Schmeidler J, Lesser GT, Beeri MS, Purohit DP, Grossman HT, Haroutunian V. Less Alzheimer disease neuropathology in medicated hypertensive than nonhypertensive persons. Neurology. 2009;72:1720–1726. doi: 10.1212/01.wnl.0000345881.82856.d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Bangen KJ, Nation DA, Delano-Wood L, Weissberger GH, Hansen LA, Galasko DR, Salmon DP, Bondi MW. Aggregate effects of vascular risk factors on cerebrovascular changes in autopsy-confirmed Alzheimer’s disease. Alzheimers Dement. 2015;11:394–403.e1. doi: 10.1016/j.jalz.2013.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Nation DA, Delano-Wood L, Bangen KJ, Wierenga CE, Jak AJ, Hansen LA, Galasko DR, Salmon DP, Bondi MW. Antemortem pulse pressure elevation predicts cerebrovascular disease in autopsy-confirmed Alzheimer’s disease. J Alzheimers Dis. 2012;30:595–603. doi: 10.3233/JAD-2012-111697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wang LY, Larson EB, Sonnen JA, Shofer JB, McCormick W, Bowen JD, Montine TJ, Li G. Blood pressure and brain injury in older adults: findings from a community-based autopsy study. J Am Geriatr Soc. 2009;57:1975–1981. doi: 10.1111/j.1532-5415.2009.02493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Young VG, Halliday GM, Kril JJ. Neuropathologic correlates of white matter hyperintensities. Neurology. 2008;71:804–811. doi: 10.1212/01.wnl.0000319691.50117.54. [DOI] [PubMed] [Google Scholar]
- 176.Fernando MS, Simpson JE, Matthews F, Brayne C, Lewis CE, Barber R, Kalaria RN, Forster G, Esteves F, Wharton SB, Shaw PJ, O’Brien JT, Ince PG, MRC Cognitive Function and Ageing Neuropathology Study Group White matter lesions in an unselected cohort of the elderly: molecular pathology suggests origin from chronic hypoperfusion injury. Stroke. 2006;37:1391–1398. doi: 10.1161/01.STR.0000221308.94473.14. [DOI] [PubMed] [Google Scholar]
- 177.Erten-Lyons D, Woltjer R, Kaye J, Mattek N, Dodge HH, Green S, Tran H, Howieson DB, Wild K, Silbert LC. Neuropathologic basis of white matter hyperintensity accumulation with advanced age. Neurology. 2013;81:977–983. doi: 10.1212/WNL.0b013e3182a43e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.He J, Wong VS, Fletcher E, Maillard P, Lee DY, Iosif AM, Singh B, Martinez O, Roach AE, Lockhart SN, Beckett L, Mungas D, Farias ST, Carmichael O, DeCarli C. The contributions of MRI-based measures of gray matter, white matter hyperintensity, and white matter integrity to late-life cognition. AJNR Am J Neuroradiol. 2012;33:1797–1803. doi: 10.3174/ajnr.A3048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Gouw AA, Seewann A, van der Flier WM, Barkhof F, Rozemuller AM, Scheltens P, Geurts JJ. Heterogeneity of small vessel disease: a systematic review of MRI and histopathology correlations. J Neurol Neurosurg Psychiatry. 2011;82:126–135. doi: 10.1136/jnnp.2009.204685. [DOI] [PubMed] [Google Scholar]
- 180.van Dijk EJ, Prins ND, Vrooman HA, Hofman A, Koudstaal PJ, Breteler MM. Progression of cerebral small vessel disease in relation to risk factors and cognitive consequences: Rotterdam Scan study. Stroke. 2008;39:2712–2719. doi: 10.1161/STROKEAHA.107.513176. [DOI] [PubMed] [Google Scholar]
- 181.Gouw AA, van der Flier WM, Fazekas F, van Straaten EC, Pantoni L, Poggesi A, Inzitari D, Erkinjuntti T, Wahlund LO, Waldemar G, Schmidt R, Scheltens P, Barkhof F, LADIS Study Group Progression of white matter hyperintensities and incidence of new lacunes over a 3-year period: the Leukoaraiosis and Disability Study. Stroke. 2008;39:1414–1420. doi: 10.1161/STROKEAHA.107.498535. [DOI] [PubMed] [Google Scholar]
- 182.Muller M, Sigurdsson S, Kjartansson O, Aspelund T, Lopez OL, Jonnson PV, Harris TB, van Buchem M, Gudnason V, Launer LJ, Age, Gene/Environment Susceptibility-Reykjavik Study Investigators Joint effect of mid- and late-life blood pressure on the brain: the AGES-Reykjavik study [published correction appears in Neurology. 2014;83:867] Neurology. 2014;82:2187–2195. doi: 10.1212/WNL.0000000000000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Dufouil C, de Kersaint-Gilly A, Besançon V, Levy C, Auffray E, Brunnereau L, Alpérovitch A, Tzourio C. Longitudinal study of blood pressure and white matter hyperintensities: the EVA MRI Cohort. Neurology. 2001;56:921–926. doi: 10.1212/wnl.56.7.921. [DOI] [PubMed] [Google Scholar]
- 184.Henskens LH, Kroon AA, van Oostenbrugge RJ, Gronenschild EH, Hofman PA, Lodder J, de Leeuw PW. Associations of ambulatory blood pressure levels with white matter hyperintensity volumes in hypertensive patients. J Hypertens. 2009;27:1446–1452. doi: 10.1097/HJH.0b013e32832b5204. [DOI] [PubMed] [Google Scholar]
- 185.Liao D, Cooper L, Cai J, Toole J, Bryan N, Burke G, Shahar E, Nieto J, Mosley T, Heiss G. The prevalence and severity of white matter lesions, their relationship with age, ethnicity, gender, and cardiovascular disease risk factors: the ARIC Study. Neuroepidemiology. 1997;16:149–162. doi: 10.1159/000368814. [DOI] [PubMed] [Google Scholar]
- 186.de Leeuw FE, de Groot JC, Oudkerk M, Witteman JC, Hofman A, van Gijn J, Breteler MM. A follow-up study of blood pressure and cerebral white matter lesions. Ann Neurol. 1999;46:827–833. doi: 10.1002/1531-8249(199912)46:6<827::aid-ana4>3.3.co;2-8. [DOI] [PubMed] [Google Scholar]
- 187.Gottesman RF, Coresh J, Catellier DJ, Sharrett AR, Rose KM, Coker LH, Shibata DK, Knopman DS, Jack CR, Mosley TH., Jr Blood pressure and white-matter disease progression in a biethnic cohort: Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2010;41:3–8. doi: 10.1161/STROKEAHA.109.566992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Swan GE, DeCarli C, Miller BL, Reed T, Wolf PA, Jack LM, Carmelli D. Association of midlife blood pressure to late-life cognitive decline and brain morphology. Neurology. 1998;51:986–993. doi: 10.1212/wnl.51.4.986. [DOI] [PubMed] [Google Scholar]
- 189.van Dijk EJ, Breteler MM, Schmidt R, Berger K, Nilsson LG, Oudkerk M, Pajak A, Sans S, de Ridder M, Dufouil C, Fuhrer R, Giampaoli S, Launer LJ, Hofman A, CASCADE Consortium The association between blood pressure, hypertension, and cerebral white matter lesions: Cardiovascular Determinants of Dementia Study. Hypertension. 2004;44:625–630. doi: 10.1161/01.HYP.0000145857.98904.20. [DOI] [PubMed] [Google Scholar]
- 190.Havlik RJ, Foley DJ, Sayer B, Masaki K, White L, Launer LJ. Variability in midlife systolic blood pressure is related to late-life brain white matter lesions: the Honolulu-Asia Aging Study. Stroke. 2002;33:26–30. doi: 10.1161/hs0102.101890. [DOI] [PubMed] [Google Scholar]
- 191.Longstreth WT, Jr, Arnold AM, Beauchamp NJ, Jr, Manolio TA, Lefkowitz D, Jungreis C, Hirsch CH, O’Leary DH, Furberg CD. Incidence, manifestations, and predictors of worsening white matter on serial cranial magnetic resonance imaging in the elderly: the Cardiovascular Health Study. Stroke. 2005;36:56–61. doi: 10.1161/01.STR.0000149625.99732.69. [DOI] [PubMed] [Google Scholar]
- 192.Marcus J, Gardener H, Rundek T, Elkind MS, Sacco RL, Decarli C, Wright CB. Baseline and longitudinal increases in diastolic blood pressure are associated with greater white matter hyperintensity volume: the Northern Manhattan Study. Stroke. 2011;42:2639–2641. doi: 10.1161/STROKEAHA.111.617571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Veldink JH, Scheltens P, Jonker C, Launer LJ. Progression of cerebral white matter hyperintensities on MRI is related to diastolic blood pressure. Neurology. 1998;51:319–320. doi: 10.1212/wnl.51.1.319. [DOI] [PubMed] [Google Scholar]
- 194.den Heijer T, Launer LJ, Prins ND, van Dijk EJ, Vermeer SE, Hofman A, Koudstaal PJ, Breteler MM. Association between blood pressure, white matter lesions, and atrophy of the medial temporal lobe. Neurology. 2005;64:263–267. doi: 10.1212/01.WNL.0000149641.55751.2E. [DOI] [PubMed] [Google Scholar]
- 195.Allan CL, Zsoldos E, Filippini N, Sexton CE, Topiwala A, Valkanova V, Singh-Manoux A, Tabák AG, Shipley MJ, Mackay C, Ebmeier KP, Kivimäki M. Lifetime hypertension as a predictor of brain structure in older adults: cohort study with a 28-year follow-up. Br J Psychiatry. 2015;206:308–315. doi: 10.1192/bjp.bp.114.153536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Tsao CW, Seshadri S, Beiser AS, Westwood AJ, Decarli C, Au R, Himali JJ, Hamburg NM, Vita JA, Levy D, Larson MG, Benjamin EJ, Wolf PA, Vasan RS, Mitchell GF. Relations of arterial stiffness and endothelial function to brain aging in the community. Neurology. 2013;81:984–991. doi: 10.1212/WNL.0b013e3182a43e1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Poels MM, Ikram MA, van der Lugt A, Hofman A, Niessen WJ, Krestin GP, Breteler MM, Vernooij MW. Cerebral microbleeds are associated with worse cognitive function: the Rotterdam Scan Study. Neurology. 2012;78:326–333. doi: 10.1212/WNL.0b013e3182452928. [DOI] [PubMed] [Google Scholar]
- 198.Jochemsen HM, Muller M, Bots ML, Scheltens P, Vincken KL, Mali WP, van der Graaf Y, Geerlings MI, SMART Study Group Arterial stiffness and progression of structural brain changes: the SMART-MR study. Neurology. 2015;84:448–455. doi: 10.1212/WNL.0000000000001201. [DOI] [PubMed] [Google Scholar]
- 199.Dufouil C, Chalmers J, Coskun O, Besançon V, Bousser MG, Guillon P, MacMahon S, Mazoyer B, Neal B, Woodward M, Tzourio-Mazoyer N, Tzourio C, PROGRESS MRI Substudy Investigators Effects of blood pressure lowering on cerebral white matter hyperintensities in patients with stroke: the PROGRESS (Perindopril Protection Against Recurrent Stroke Study) Magnetic Resonance Imaging Substudy. Circulation. 2005;112:1644–1650. doi: 10.1161/CIRCULATIONAHA.104.501163. [DOI] [PubMed] [Google Scholar]
- 200.Firbank MJ, Wiseman RM, Burton EJ, Saxby BK, O’Brien JT, Ford GA. Brain atrophy and white matter hyperintensity change in older adults and relationship to blood pressure: brain atrophy, WMH change and blood pressure. J Neurol. 2007;254:713–721. doi: 10.1007/s00415-006-0238-4. [DOI] [PubMed] [Google Scholar]
- 201.Wang R, Fratiglioni L, Laukka EJ, Lövdén M, Kalpouzos G, Keller L, Graff C, Salami A, Bäckman L, Qiu C. Effects of vascular risk factors and APOE ε4 on white matter integrity and cognitive decline. Neurology. 2015;84:1128–1135. doi: 10.1212/WNL.0000000000001379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Gons RA, de Laat KF, van Norden AG, van Oudheusden LJ, van Uden IW, Norris DG, Zwiers MP, de Leeuw FE. Hypertension and cerebral diffusion tensor imaging in small vessel disease. Stroke. 2010;41:2801–2806. doi: 10.1161/STROKEAHA.110.597237. [DOI] [PubMed] [Google Scholar]
- 203.Kennedy KM, Raz N. Pattern of normal age-related regional differences in white matter microstructure is modified by vascular risk. Brain Res. 2009;1297:41–56. doi: 10.1016/j.brainres.2009.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Leritz EC, Salat DH, Milberg WP, Williams VJ, Chapman CE, Grande LJ, Rudolph JL, Schnyer DM, Barber CE, Lipsitz LA, McGlinchey RE. Variation in blood pressure is associated with white matter microstructure but not cognition in African Americans. Neuropsychology. 2010;24:199–208. doi: 10.1037/a0018108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Maclullich AM, Ferguson KJ, Reid LM, Deary IJ, Starr JM, Seckl JR, Bastin ME, Wardlaw JM. Higher systolic blood pressure is associated with increased water diffusivity in normal-appearing white matter. Stroke. 2009;40:3869–3871. doi: 10.1161/STROKEAHA.109.547877. [DOI] [PubMed] [Google Scholar]
- 206.Maillard P, Seshadri S, Beiser A, Himali JJ, Au R, Fletcher E, Carmichael O, Wolf PA, DeCarli C. Effects of systolic blood pressure on white-matter integrity in young adults in the Framingham Heart Study: a cross-sectional study. Lancet Neurol. 2012;11:1039–1047. doi: 10.1016/S1474-4422(12)70241-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Maillard P, Carmichael OT, Reed B, Mungas D, DeCarli C. Cooccurrence of vascular risk factors and late-life white-matter integrity changes. Neurobiol Aging. 2015;36:1670–1677. doi: 10.1016/j.neurobiolaging.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Godin O, Maillard P, Crivello F, Alpérovitch A, Mazoyer B, Tzourio C, Dufouil C. Association of white-matter lesions with brain atrophy markers: the three-city Dijon MRI study. Cerebrovasc Dis. 2009;28:177–184. doi: 10.1159/000226117. [DOI] [PubMed] [Google Scholar]
- 209.Schilling S, DeStefano AL, Sachdev PS, Choi SH, Mather KA, DeCarli CD, Wen W, Høgh P, Raz N, Au R, Beiser A, Wolf PA, Romero JR, Zhu YC, Lunetta KL, Farrer L, Dufouil C, Kuller LH, Mazoyer B, Seshadri S, Tzourio C, Debette S. APOE genotype and MRI markers of cere-brovascular disease: systematic review and meta-analysis. Neurology. 2013;81:292–300. doi: 10.1212/WNL.0b013e31829bfda4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Grimmer T, Faust M, Auer F, Alexopoulos P, Förstl H, Henriksen G, Perneczky R, Sorg C, Yousefi BH, Drzezga A, Kurz A. White matter hyper-intensities predict amyloid increase in Alzheimer’s disease. Neurobiol Aging. 2012;33:2766–2773. doi: 10.1016/j.neurobiolaging.2012.01.016. [DOI] [PubMed] [Google Scholar]
- 211.de Leeuw FE, Richard F, de Groot JC, van Duijn CM, Hofman A, Van Gijn J, Breteler MM. Interaction between hypertension, apoE, and cerebral white matter lesions. Stroke. 2004;35:1057–1060. doi: 10.1161/01.STR.0000125859.71051.83. [DOI] [PubMed] [Google Scholar]
- 212.Høgh P, Garde E, Mortensen EL, Jørgensen OS, Krabbe K, Waldemar G. The apolipoprotein E epsilon4-allele and antihypertensive treatment are associated with increased risk of cerebral MRI white matter hyperintensities. Acta Neurol Scand. 2007;115:248–253. doi: 10.1111/j.1600-0404.2006.00779.x. [DOI] [PubMed] [Google Scholar]
- 213.Schneider JA, Boyle PA, Arvanitakis Z, Bienias JL, Bennett DA. Subcortical infarcts, Alzheimer’s disease pathology, and memory function in older persons. Ann Neurol. 2007;62:59–66. doi: 10.1002/ana.21142. [DOI] [PubMed] [Google Scholar]
- 214.Arvanitakis Z, Leurgans SE, Barnes LL, Bennett DA, Schneider JA. Microinfarct pathology, dementia, and cognitive systems. Stroke. 2011;42:722–727. doi: 10.1161/STROKEAHA.110.595082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.White L. Brain lesions at autopsy in older Japanese-American men as related to cognitive impairment and dementia in the final years of life: a summary report from the Honolulu-Asia Aging Study. J Alzheimers Dis. 2009;18:713–725. doi: 10.3233/JAD-2009-1178. [DOI] [PubMed] [Google Scholar]
- 216.Sonnen JA, Santa Cruz K, Hemmy LS, Woltjer R, Leverenz JB, Montine KS, Jack CR, Kaye J, Lim K, Larson EB, White L, Montine TJ. Ecology of the aging human brain. Arch Neurol. 2011;68:1049–1056. doi: 10.1001/archneurol.2011.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.De Reuck JL. Histopathological stainings and definitions of vascular disruptions in the elderly brain. Exp Gerontol. 2012;47:834–837. doi: 10.1016/j.exger.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 218.Gao Z, Wang W, Wang Z, Zhao X, Shang Y, Guo Y, Gong M, Yang L, Shi X, Xu X, An N, Wu W. Cerebral microbleeds are associated with deep white matter hyperintensities, but only in hypertensive patients. PLoS One. 2014;9:e91637. doi: 10.1371/journal.pone.0091637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Henskens LH, van Oostenbrugge RJ, Kroon AA, de Leeuw PW, Lodder J. Brain microbleeds are associated with ambulatory blood pressure levels in a hypertensive population. Hypertension. 2008;51:62–68. doi: 10.1161/HYPERTENSIONAHA.107.100610. [DOI] [PubMed] [Google Scholar]
- 220.Goos JD, Henneman WJ, Sluimer JD, Vrenken H, Sluimer IC, Barkhof F, Blankenstein MA, Scheltens PH, van der Flier WM. Incidence of cerebral microbleeds: a longitudinal study in a memory clinic population. Neurology. 2010;74:1954–1960. doi: 10.1212/WNL.0b013e3181e396ea. [DOI] [PubMed] [Google Scholar]
- 221.Hara M, Yakushiji Y, Nannri H, Sasaki S, Noguchi T, Nishiyama M, Hirotsu T, Nakajima J, Hara H. Joint effect of hypertension and lifestyle-related risk factors on the risk of brain microbleeds in healthy individuals. Hypertens Res. 2013;36:789–794. doi: 10.1038/hr.2013.26. [DOI] [PubMed] [Google Scholar]
- 222.Poels MM, Vernooij MW, Ikram MA, Hofman A, Krestin GP, van der Lugt A, Breteler MM. Prevalence and risk factors of cerebral microbleeds: an update of the Rotterdam scan study. Stroke. 2010;41(suppl):S103–S106. doi: 10.1161/STROKEAHA.110.595181. [DOI] [PubMed] [Google Scholar]
- 223.Romero JR, Preis SR, Beiser A, DeCarli C, Viswanathan A, Martinez-Ramirez S, Kase CS, Wolf PA, Seshadri S. Risk factors, stroke prevention treatments, and prevalence of cerebral microbleeds in the Framingham Heart Study. Stroke. 2014;45:1492–1494. doi: 10.1161/STROKEAHA.114.004130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Park JH, Seo SW, Kim C, Kim GH, Noh HJ, Kim ST, Kwak KC, Yoon U, Lee JM, Lee JW, Shin JS, Kim CH, Noh Y, Cho H, Kim HJ, Yoon CW, Oh SJ, Kim JS, Choe YS, Lee KH, Lee JH, Ewers M, Weiner MW, Werring DJ, Na DL. Pathogenesis of cerebral microbleeds: in vivo imaging of amyloid and subcortical ischemic small vessel disease in 226 individuals with cognitive impairment. Ann Neurol. 2013;73:584–593. doi: 10.1002/ana.23845. [DOI] [PubMed] [Google Scholar]
- 225.Shams S, Martola J, Granberg T, Li X, Shams M, Fereshtehnejad SM, Cavallin L, Aspelin P, Kristoffersen-Wiberg M, Wahlund LO. Cerebral microbleeds: different prevalence, topography, and risk factors depending on dementia diagnosis: the Karolinska Imaging Dementia Study. AJNR Am J Neuroradiol. 2015;36:661–666. doi: 10.3174/ajnr.A4176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Qiu C, Cotch MF, Sigurdsson S, Jonsson PV, Jonsdottir MK, Sveinbjrnsdottir S, Eiriksdottir G, Klein R, Harris TB, van Buchem MA, Gudnason V, Launer LJ. Cerebral microbleeds, retinopathy, and dementia: the AGES-Reykjavik Study. Neurology. 2010;75:2221–2228. doi: 10.1212/WNL.0b013e3182020349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.van der Vlies AE, Goos JD, Barkhof F, Scheltens P, van der Flier WM. Microbleeds do not affect rate of cognitive decline in Alzheimer disease. Neurology. 2012;79:763–769. doi: 10.1212/WNL.0b013e3182661f91. [DOI] [PubMed] [Google Scholar]
- 228.de Jong LW, Forsberg LE, Vidal JS, Sigurdsson S, Zijdenbos AP, Garcia M, Eiriksdottir G, Gudnason V, van Buchem MA, Launer LJ. Different susceptibility of medial temporal lobe and basal ganglia atrophy rates to vascular risk factors. Neurobiol Aging. 2014;35:72–78. doi: 10.1016/j.neurobiolaging.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Jennings JR, Mendelson DN, Muldoon MF, Ryan CM, Gianaros PJ, Raz N, Aizenstein H. Regional grey matter shrinks in hypertensive individuals despite successful lowering of blood pressure. J Hum Hypertens. 2012;26:295–305. doi: 10.1038/jhh.2011.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Knopman DS, Penman AD, Catellier DJ, Coker LH, Shibata DK, Sharrett AR, Mosley TH., Jr Vascular risk factors and longitudinal changes on brain MRI: the ARIC Study. Neurology. 2011;76:1879–1885. doi: 10.1212/WNL.0b013e31821d753f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Vlek AL, Visseren FL, Kappelle LJ, Geerlings MI, Vincken KL, Mali WP, van der Graaf Y, SMART Study Group Blood pressure and progression of cerebral atrophy in patients with vascular disease. Am J Hypertens. 2009;22:1183–1189. doi: 10.1038/ajh.2009.166. [DOI] [PubMed] [Google Scholar]
- 232.Beauchet O, Celle S, Roche F, Bartha R, Montero-Odasso M, Allali G, Annweiler C. Blood pressure levels and brain volume reduction: a systematic review and meta-analysis [published correction appears in J Hypertens. 2013;31:2106] J Hypertens. 2013;31:1502–1516. doi: 10.1097/HJH.0b013e32836184b5. [DOI] [PubMed] [Google Scholar]
- 233.Korf ES, White LR, Scheltens P, Launer LJ. Midlife blood pressure and the risk of hippocampal atrophy: the Honolulu Asia Aging Study. Hypertension. 2004;44:29–34. doi: 10.1161/01.HYP.0000132475.32317.bb. [DOI] [PubMed] [Google Scholar]
- 234.Korf ES, Scheltens P, Barkhof F, de Leeuw FE. Blood pressure, white matter lesions and medial temporal lobe atrophy: closing the gap between vascular pathology and Alzheimer’s disease? Dement Geriatr Cogn Disord. 2005;20:331–337. doi: 10.1159/000088464. [DOI] [PubMed] [Google Scholar]
- 235.Guzman VA, Carmichael OT, Schwarz C, Tosto G, Zimmerman ME, Brickman AM, Alzheimer’s Disease Neuroimaging Initiative White matter hyperintensities and amyloid are independently associated with entorhinal cortex volume among individuals with mild cognitive impairment. Alzheimers Dement. 2013;9(suppl):S124–S131. doi: 10.1016/j.jalz.2012.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.de Leeuw FE, Barkhof F, Scheltens P. White matter lesions and hippo-campal atrophy in Alzheimer’s disease. Neurology. 2004;62:310–312. doi: 10.1212/01.wnl.0000103289.03648.ad. [DOI] [PubMed] [Google Scholar]
- 237.Raji CA, Lopez OL, Kuller LH, Carmichael OT, Longstreth WT, Jr, Gach HM, Boardman J, Bernick CB, Thompson PM, Becker JT. White matter lesions and brain gray matter volume in cognitively normal elders. Neurobiol Aging. 2012;33:834.e7–847.e16. doi: 10.1016/j.neurobiolaging.2011.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Nitkunan A, Lanfranconi S, Charlton RA, Barrick TR, Markus HS. Brain atrophy and cerebral small vessel disease: a prospective followup study. Stroke. 2011;42:133–138. doi: 10.1161/STROKEAHA.110.594267. [DOI] [PubMed] [Google Scholar]
- 239.Tuladhar AM, Reid AT, Shumskaya E, de Laat KF, van Norden AG, van Dijk EJ, Norris DG, de Leeuw FE. Relationship between white matter hyperintensities, cortical thickness, and cognition. Stroke. 2015;46:425–432. doi: 10.1161/STROKEAHA.114.007146. [DOI] [PubMed] [Google Scholar]
- 240.Kloppenborg RP, Nederkoorn PJ, Grool AM, Vincken KL, Mali WP, Vermeulen M, van der Graaf Y, Geerlings MI, SMART Study Group Cerebral small-vessel disease and progression of brain atrophy: the SMART-MR study. Neurology. 2012;79:2029–2036. doi: 10.1212/WNL.0b013e3182749f02. [DOI] [PubMed] [Google Scholar]
- 241.Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, Benveniste H, Vates GE, Deane R, Goldman SA, Nagelhus EA, Nedergaard M. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4:147ra111. doi: 10.1126/scitranslmed.3003748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Jochemsen HM, Muller M, Visseren FL, Scheltens P, Vincken KL, Mali WP, van der Graaf Y, Geerlings MI, SMART Study Group Blood pressure and progression of brain atrophy: the SMART-MR Study. JAMA Neurol. 2013;70:1046–1053. doi: 10.1001/jamaneurol.2013.217. [DOI] [PubMed] [Google Scholar]
- 243.Hughes TM, Kuller LH, Barinas-Mitchell EJ, Mackey RH, McDade EM, Klunk WE, Aizenstein HJ, Cohen AD, Snitz BE, Mathis CA, Dekosky ST, Lopez OL. Pulse wave velocity is associated with β-amyloid deposition in the brains of very elderly adults. Neurology. 2013;81:1711–1718. doi: 10.1212/01.wnl.0000435301.64776.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Langbaum JB, Chen K, Launer LJ, Fleisher AS, Lee W, Liu X, Protas HD, Reeder SA, Bandy D, Yu M, Caselli RJ, Reiman EM. Blood pressure is associated with higher brain amyloid burden and lower glucose metabolism in healthy late middle-age persons. Neurobiol Aging. 2012;33:827.e11–827.e19. doi: 10.1016/j.neurobiolaging.2011.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Toledo JB, Toledo E, Weiner MW, Jack CR, Jr, Jagust W, Lee VM, Shaw LM, Trojanowski JQ, Alzheimer’s Disease Neuroimaging Initiative Cardiovascular risk factors, cortisol, and amyloid-β deposition in Alzheimer’s Disease Neuroimaging Initiative. Alzheimers Dement. 2012;8:483–489. doi: 10.1016/j.jalz.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Rodrigue KM, Rieck JR, Kennedy KM, Devous MD, Sr, Diaz-Arrastia R, Park DC. Risk factors for β-amyloid deposition in healthy aging: vascular and genetic effects. JAMA Neurol. 2013;70:600–606. doi: 10.1001/jamaneurol.2013.1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Nation DA, Edland SD, Bondi MW, Salmon DP, Delano-Wood L, Peskind ER, Quinn JF, Galasko DR. Pulse pressure is associated with Alzheimer biomarkers in cognitively normal older adults. Neurology. 2013;81:2024–2027. doi: 10.1212/01.wnl.0000436935.47657.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Nation DA, Edmonds EC, Bangen KJ, Delano-Wood L, Scanlon BK, Han SD, Edland SD, Salmon DP, Galasko DR, Bondi MW, Alzheimer’s Disease Neuroimaging Initiative Investigators Pulse pressure in relation to tau-mediated neurodegeneration, cerebral amyloidosis, and progression to dementia in very old adults. JAMA Neurol. 2015;72:546–553. doi: 10.1001/jamaneurol.2014.4477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Kester MI, van der Flier WM, Mandic G, Blankenstein MA, Scheltens P, Muller M. Joint effect of hypertension and APOE genotype on CSF bio-markers for Alzheimer’s disease. J Alzheimers Dis. 2010;20:1083–1090. doi: 10.3233/JAD-2010-091198. [DOI] [PubMed] [Google Scholar]
- 250.Peters R, Beckett N, Forette F, Tuomilehto J, Clarke R, Ritchie C, Waldman A, Walton I, Poulter R, Ma S, Comsa M, Burch L, Fletcher A, Bulpitt C, HYVET Investigators Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial Cognitive Function Assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol. 2008;7:683–689. doi: 10.1016/S1474-4422(08)70143-1. [DOI] [PubMed] [Google Scholar]
- 251.Forette F, Seux ML, Staessen JA, Thijs L, Birkenhäger WH, Babarskiene MR, Babeanu S, Bossini A, Gil-Extremera B, Girerd X, Laks T, Lilov E, Moisseyev V, Tuomilehto J, Vanhanen H, Webster J, Yodfat Y, Fagard R. Prevention of dementia in randomised double-blind placebo-controlled Systolic Hypertension in Europe (Syst-Eur) trial. Lancet. 1998;352:1347–1351. doi: 10.1016/s0140-6736(98)03086-4. [DOI] [PubMed] [Google Scholar]
- 252.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group; Cochrane Statistical Methods Group The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Williamson JD, Launer LJ, Bryan RN, Coker LH, Lazar RM, Gerstein HC, Murray AM, Sullivan MD, Horowitz KR, Ding J, Marcovina S, Lovato L, Lovato J, Margolis KL, Davatzikos C, Barzilay J, Ginsberg HN, Linz PE, Miller ME, Action to Control Cardiovascular Risk in Diabetes Memory in Diabetes Investigators Cognitive function and brain structure in persons with type 2 diabetes mellitus after intensive lowering of blood pressure and lipid levels: a randomized clinical trial. JAMA Intern Med. 2014;174:324–333. doi: 10.1001/jamainternmed.2013.13656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Anderson C, Teo K, Gao P, Arima H, Dans A, Unger T, Commerford P, Dyal L, Schumacher H, Pogue J, Paolasso E, Holwerda N, Chazova I, Binbrek A, Young J, Yusuf S, ONTARGET and TRANSCEND Investigators Renin-angiotensin system blockade and cognitive function in patients at high risk of cardiovascular disease: analysis of data from the ONTARGET and TRANSCEND studies. Lancet Neurol. 2011;10:43–53. doi: 10.1016/S1474-4422(10)70250-7. [DOI] [PubMed] [Google Scholar]
- 255.SPS3 Investigators. Benavente OR, Hart RG, McClure LA, Szychowski JM, Coffey CS, Pearce LA. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. N Engl J Med. 2012;367:817–825. doi: 10.1056/NEJMoa1204133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Lithell H, Hansson L, Skoog I, Elmfeldt D, Hofman A, Olofsson B, Trenkwalder P, Zanchetti A, SCOPE Study Group The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens. 2003;21:875–886. doi: 10.1097/01.hjh.0000059028.82022.89. [DOI] [PubMed] [Google Scholar]
- 257.Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP): SHEP Cooperative Research Group. JAMA. 1991;265:3255–3264. doi: 10.1001/jama.1991.03460240051027. [DOI] [PubMed] [Google Scholar]
- 258.Diener HC, Sacco RL, Yusuf S, Cotton D, Ounpuu S, Lawton WA, Palesch Y, Martin RH, Albers GW, Bath P, Bornstein N, Chan BP, Chen ST, Cunha L, Dahlöf B, De Keyser J, Donnan GA, Estol C, Gorelick P, Gu V, Hermansson K, Hilbrich L, Kaste M, Lu C, Machnig T, Pais P, Roberts R, Skvortsova V, Teal P, Toni D, VanderMaelen C, Voigt T, Weber M, Yoon BW, Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) Study Group Effects of aspirin plus extended-release dipyridamole versus clopidogrel and telmisartan on disability and cognitive function after recurrent stroke in patients with ischaemic stroke in the Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) trial: a double-blind, active and placebo-controlled study [published correction appears in Lancet Neurol. 2008;7:985] Lancet Neurol. 2008;7:875–884. doi: 10.1016/S1474-4422(08)70198-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Pearce LA, McClure LA, Anderson DC, Jacova C, Sharma M, Hart RG, Benavente OR, SPS3 Investigators Effects of long-term blood pressure lowering and dual antiplatelet treatment on cognitive function in patients with recent lacunar stroke: a secondary analysis from the SPS3 randomised trial. Lancet Neurol. 2014;13:1177–1185. doi: 10.1016/S1474-4422(14)70224-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Tzourio C, Anderson C, Chapman N, Woodward M, Neal B, MacMahon S, Chalmers J, PROGRESS Collaborative Group Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease. Arch Intern Med. 2003;163:1069–1075. doi: 10.1001/archinte.163.9.1069. [DOI] [PubMed] [Google Scholar]
- 261.Hornslien AG, Sandset EC, Bath PM, Wyller TB, Berge E, Scandinavian Candesartan Acute Stroke Trial Study Group Effects of candesartan in acute stroke on cognitive function and quality of life: results from the Scandinavian Candesartan Acute Stroke Trial. Stroke. 2013;44:2022–2024. doi: 10.1161/STROKEAHA.113.001022. [DOI] [PubMed] [Google Scholar]
- 262.Applegate WB, Pressel S, Wittes J, Luhr J, Shekelle RB, Camel GH, Greenlick MR, Hadley E, Moye L, Perry HM, Jr, Schron E, Wegener V. Impact of the treatment of isolated systolic hypertension on behavioral variables: results from the Systolic Hypertension in the Elderly Program. Arch Intern Med. 1994;154:2154–2160. [PubMed] [Google Scholar]
- 263.Hachinski VC, Iliff LD, Zilhka E, Du Boulay GH, McAllister VL, Marshall J, Russell RW, Symon L. Cerebral blood flow in dementia. Arch Neurol. 1975;32:632–637. doi: 10.1001/archneur.1975.00490510088009. [DOI] [PubMed] [Google Scholar]
- 264.Weber R, Weimar C, Blatchford J, Hermansson K, Wanke I, Möller-Hartmann C, Gizewski ER, Forsting M, Demchuk AM, Sacco RL, Saver JL, Warach S, Diener HC, Diehl A, PRoFESS Imaging Substudy Group Telmisartan on top of antihypertensive treatment does not prevent progression of cerebral white matter lesions in the Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) MRI substudy. Stroke. 2012;43:2336–2342. doi: 10.1161/STROKEAHA.111.648576. [DOI] [PubMed] [Google Scholar]
- 265.Saxby BK, Harrington F, Wesnes KA, McKeith IG, Ford GA. Candesartan and cognitive decline in older patients with hypertension: a substudy of the SCOPE trial. Neurology. 2008;70(pt 2):1858–1866. doi: 10.1212/01.wnl.0000311447.85948.78. [DOI] [PubMed] [Google Scholar]
- 266.Forette F, Seux ML, Staessen JA, Thijs L, Babarskiene MR, Babeanu S, Bossini A, Fagard R, Gil-Extremera B, Laks T, Kobalava Z, Sarti C, Tuomilehto J, Vanhanen H, Webster J, Yodfat Y, Birkenhäger WH, Systolic Hypertension in Europe Investigators The prevention of dementia with antihypertensive treatment: new evidence from the Systolic Hypertension in Europe (Syst-Eur) study [published correction appears in Arch Intern Med. 2003;163:241] Arch Intern Med. 2002;162:2046–2052. doi: 10.1001/archinte.162.18.2046. [DOI] [PubMed] [Google Scholar]
- 267.Staessen JA, Thijs L, Richart T, Odili AN, Birkenhäger WH. Placebo-controlled trials of blood pressure-lowering therapies for primary prevention of dementia. Hypertension. 2011;57:e6–e7. doi: 10.1161/HYPERTENSIONAHA.110.165142. [DOI] [PubMed] [Google Scholar]
- 268.Skoog I, Lithell H, Hansson L, Elmfeldt D, Hofman A, Olofsson B, Trenkwalder P, Zanchetti A, SCOPE Study Group Effect of baseline cognitive function and antihypertensive treatment on cognitive and cardiovascular outcomes: Study on COgnition and Prognosis in the Elderly (SCOPE) Am J Hypertens. 2005;18:1052–1059. doi: 10.1016/j.amjhyper.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 269.Di Bari M, Pahor M, Franse LV, Shorr RI, Wan JY, Ferrucci L, Somes GW, Applegate WB. Dementia and disability outcomes in large hypertension trials: lessons learned from the Systolic Hypertension in the Elderly Program (SHEP) trial. Am J Epidemiol. 2001;153:72–78. doi: 10.1093/aje/153.1.72. [DOI] [PubMed] [Google Scholar]
- 270.Ambrosius WT, Sink KM, Foy CG, Berlowitz DR, Cheung AK, Cushman WC, Fine LJ, Goff DC, Jr, Johnson KC, Killeen AA, Lewis CE, Oparil S, Reboussin DM, Rocco MV, Snyder JK, Williamson JD, Wright JT, Jr, Whelton PK, SPRINT Study Research Group The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT) Clin Trials. 2014;11:532–546. doi: 10.1177/1740774514537404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.SPRINT Research Group. Wright JT, Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC, Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488–1496. doi: 10.1161/CIRCULATIONAHA.106.683243. [DOI] [PubMed] [Google Scholar]
- 273.Riley M, Bluhm B. High blood pressure in children and adolescents. Am Fam Physician. 2012;85:693–700. [PubMed] [Google Scholar]
- 274.Flynn JT, Daniels SR, Hayman LL, Maahs DM, McCrindle BW, Mitsnefes M, Zachariah JP, Urbina EM, on behalf of the American Heart Association Atherosclerosis, Hypertension and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension. 2014;63:1116–1135. doi: 10.1161/HYP.0000000000000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 276.Chen W, Bao W, Begum S, Elkasabany A, Srinivasan SR, Berenson GS. Age-related patterns of the clustering of cardiovascular risk variables of syndrome X from childhood to young adulthood in a population made up of black and white subjects: the Bogalusa Heart Study. Diabetes. 2000;49:1042–1048. doi: 10.2337/diabetes.49.6.1042. [DOI] [PubMed] [Google Scholar]
- 277.Shear CL, Burke GL, Freedman DS, Berenson GS. Value of childhood blood pressure measurements and family history in predicting future blood pressure status: results from 8 years of follow-up in the Bogalusa Heart Study. Pediatrics. 1986;77:862–869. [PubMed] [Google Scholar]
- 278.Klumbiene J, Sileikiene L, Milasauskiene Z, Zaborskis A, Shatchkute A. The relationship of childhood to adult blood pressure: longitudinal study of juvenile hypertension in Lithuania. J Hypertens. 2000;18:531–538. doi: 10.1097/00004872-200018050-00004. [DOI] [PubMed] [Google Scholar]
- 279.Strong JP, Malcom GT, McMahan CA, Tracy RE, Newman WP, 3rd, Herderick EE, Cornhill JF. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the Pathobiological Determinants of Atherosclerosis in Youth Study. JAMA. 1999;281:727–735. doi: 10.1001/jama.281.8.727. [DOI] [PubMed] [Google Scholar]
- 280.Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults: the Bogalusa Heart Study. N Engl J Med. 1998;338:1650–1656. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 281.Kollias A, Dafni M, Poulidakis E, Ntineri A, Stergiou GS. Out-of-office blood pressure and target organ damage in children and adolescents: a systematic review and meta-analysis. J Hypertens. 2014;32:2315–2331. doi: 10.1097/HJH.0000000000000384. [DOI] [PubMed] [Google Scholar]
- 282.Morrison JA, Friedman LA, Gray-McGuire C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: the Princeton Lipid Research Clinics Follow-up Study. Pediatrics. 2007;120:340–345. doi: 10.1542/peds.2006-1699. [DOI] [PubMed] [Google Scholar]
- 283.Lande MB, Kaczorowski JM, Auinger P, Schwartz GJ, Weitzman M. Elevated blood pressure and decreased cognitive function among school-age children and adolescents in the United States. J Pediatr. 2003;143:720–724. doi: 10.1067/S0022-3476(03)00412-8. [DOI] [PubMed] [Google Scholar]
- 284.Adams HR, Szilagyi PG, Gebhardt L, Lande MB. Learning and attention problems among children with pediatric primary hypertension. Pediatrics. 2010;126:e1425–e1429. doi: 10.1542/peds.2010-1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Krause I, Cleper R, Kovalski Y, Sinai L, Davidovits M. Changes in behavior as an early symptom of renovascular hypertension in children. Pediatr Nephrol. 2009;24:2271–2274. doi: 10.1007/s00467-009-1205-y. [DOI] [PubMed] [Google Scholar]
- 286.Chaturvedi S, Lipszyc DH, Licht C, Craig JC, Parekh R. Pharmacological interventions for hypertension in children. Cochrane Database Syst Rev. 2014:CD008117. doi: 10.1002/14651858.CD008117.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Franklin SS, Jacobs MJ, Wong ND, L’Italien GJ, Lapuerta P. Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension. 2001;37:869–874. doi: 10.1161/01.hyp.37.3.869. [DOI] [PubMed] [Google Scholar]
- 288.Franklin SS, Pio JR, Wong ND, Larson MG, Leip EP, Vasan RS, Levy D. Predictors of new-onset diastolic and systolic hypertension: the Framingham Heart Study. Circulation. 2005;111:1121–1127. doi: 10.1161/01.CIR.0000157159.39889.EC. [DOI] [PubMed] [Google Scholar]
- 289.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies [published correction appears in Lancet. 2003;361:1060] Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 290.Blood Pressure Lowering Treatment Trialists’ Collaboration. Turnbull F, Neal B, Ninomiya T, Algert C, Arima H, Barzi F, Bulpitt C, Chalmers J, Fagard R, Gleason A, Heritier S, Li N, Perkovic V, Woodward M, MacMahon S. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ. 2008;336:1121–1123. doi: 10.1136/bmj.39548.738368.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR, Writing Group of the PREMIER Collaborative Research Group Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289:2083–2093. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 292.Musini VM, Tejani AM, Bassett K, Wright JM. Pharmacotherapy for hypertension in the elderly. Cochrane Database Syst Rev. 2009:CD000028. doi: 10.1002/14651858.CD000028.pub2. [DOI] [PubMed] [Google Scholar]
- 293.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet. 2010;375:906–915. doi: 10.1016/S0140-6736(10)60235-8. [DOI] [PubMed] [Google Scholar]
- 295.Sundström J, Arima H, Jackson R, Turnbull F, Rahimi K, Chalmers J, Woodward M, Neal B, Blood Pressure Lowering Treatment Trialists’ Collaboration Effects of blood pressure reduction in mild hypertension: a systematic review and meta-analysis. Ann Intern Med. 2015;162:184–191. doi: 10.7326/M14-0773. [DOI] [PubMed] [Google Scholar]
- 296.Birns J, Morris R, Donaldson N, Kalra L. The effects of blood pressure reduction on cognitive function: a review of effects based on pooled data from clinical trials. J Hypertens. 2006;24:1907–1914. doi: 10.1097/01.hjh.0000244934.81180.16. [DOI] [PubMed] [Google Scholar]
- 297.Feigin V, Ratnasabapathy Y, Anderson C. Does blood pressure lowering treatment prevents dementia or cognitive decline in patients with cardiovascular and cerebrovascular disease? J Neurol Sci. 2005;229–230:151–155. doi: 10.1016/j.jns.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 298.McGuinness B, Todd S, Passmore AP, Bullock R. Systematic review: blood pressure lowering in patients without prior cerebrovascular disease for prevention of cognitive impairment and dementia. J Neurol Neurosurg Psychiatry. 2008;79:4–5. doi: 10.1136/jnnp.2007.118505. [DOI] [PubMed] [Google Scholar]
- 299.McGuinness B, Todd S, Passmore P, Bullock R. Blood pressure lowering in patients without prior cerebrovascular disease for prevention of cognitive impairment and dementia. Cochrane Database Syst Rev. 2009:CD004034. doi: 10.1002/14651858.CD004034.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Gifford KA, Badaracco M, Liu D, Tripodis Y, Gentile A, Lu Z, Palmisano J, Jefferson AL. Blood pressure and cognition among older adults: a meta-analysis. Arch Clin Neuropsychol. 2013;28:649–664. doi: 10.1093/arclin/act046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Ngandu T, Lehtisalo J, Solomon A, Levälahti E, Ahtiluoto S, Antikainen R, Bäckman L, Hänninen T, Jula A, Laatikainen T, Lindström J, Mangialasche F, Paajanen T, Pajala S, Peltonen M, Rauramaa R, Stigsdotter-Neely A, Strandberg T, Tuomilehto J, Soininen H, Kivipelto M. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385:2255–2263. doi: 10.1016/S0140-6736(15)60461-5. [DOI] [PubMed] [Google Scholar]
- 302.Makin SD, Turpin S, Dennis MS, Wardlaw JM. Cognitive impairment after lacunar stroke: systematic review and meta-analysis of incidence, prevalence and comparison with other stroke subtypes. J Neurol Neurosurg Psychiatry. 2013;84:893–900. doi: 10.1136/jnnp-2012-303645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Vermeer SE, Prins ND, den Heijer T, Hofman A, Koudstaal PJ, Breteler MM. Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med. 2003;348:1215–1222. doi: 10.1056/NEJMoa022066. [DOI] [PubMed] [Google Scholar]
- 304.Christensen K, Thinggaard M, Oksuzyan A, Steenstrup T, Andersen-Ranberg K, Jeune B, McGue M, Vaupel JW. Physical and cognitive functioning of people older than 90 years: a comparison of two Danish cohorts born 10 years apart. Lancet. 2013;382:1507–1513. doi: 10.1016/S0140-6736(13)60777-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Manton KC, Gu XL, Ukraintseva SV. Declining prevalence of dementia in the U.S. elderly population. Adv Gerontol. 2005;16:30–37. [PubMed] [Google Scholar]
- 306.Langa KM, Larson EB, Karlawish JH, Cutler DM, Kabeto MU, Kim SY, Rosen AB. Trends in the prevalence and mortality of cognitive impairment in the United States: is there evidence of a compression of cognitive morbidity? Alzheimers Dement. 2008;4:134–144. doi: 10.1016/j.jalz.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Qiu C, von Strauss E, Bäckman L, Winblad B, Fratiglioni L. Twenty-year changes in dementia occurrence suggest decreasing incidence in central Stockholm, Sweden. Neurology. 2013;80:1888–1894. doi: 10.1212/WNL.0b013e318292a2f9. [DOI] [PubMed] [Google Scholar]
- 308.Matthews FE, Arthur A, Barnes LE, Bond J, Jagger C, Robinson L, Brayne C, Medical Research Council Cognitive Function and Ageing Collaboration A two-decade comparison of prevalence of dementia in individuals aged 65 years and older from three geographical areas of England: results of the Cognitive Function and Ageing Study I and II. Lancet. 2013;382:1405–1412. doi: 10.1016/S0140-6736(13)61570-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Qiu C, Winblad B, Fratiglioni L. Low diastolic pressure and risk of dementia in very old people: a longitudinal study. Dement Geriatr Cogn Disord. 2009;28:213–219. doi: 10.1159/000236913. [DOI] [PubMed] [Google Scholar]
- 310.Glynn RJ, Beckett LA, Hebert LE, Morris MC, Scherr PA, Evans DA. Current and remote blood pressure and cognitive decline. JAMA. 1999;281:438–445. doi: 10.1001/jama.281.5.438. [DOI] [PubMed] [Google Scholar]
- 311.Morris MC, Scherr PA, Hebert LE, Glynn RJ, Bennett DA, Evans DA. Association of incident Alzheimer disease and blood pressure measured from 13 years before to 2 years after diagnosis in a large community study. Arch Neurol. 2001;58:1640–1646. doi: 10.1001/archneur.58.10.1640. [DOI] [PubMed] [Google Scholar]
- 312.Luukinen H, Koski K, Laippala P, Kivelä SL. Prognosis of diastolic and systolic orthostatic hypotension in older persons. Arch Intern Med. 1999;159:273–280. doi: 10.1001/archinte.159.3.273. [DOI] [PubMed] [Google Scholar]
- 313.Mitchell GF, Parise H, Benjamin EJ, Larson MG, Keyes MJ, Vita JA, Vasan RS, Levy D. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham Heart Study. Hypertension. 2004;43:1239–1245. doi: 10.1161/01.HYP.0000128420.01881.aa. [DOI] [PubMed] [Google Scholar]
- 314.Avolio AP, Deng FQ, Li WQ, Luo YF, Huang ZD, Xing LF, O’Rourke MF. Effects of aging on arterial distensibility in populations with high and low prevalence of hypertension: comparison between urban and rural communities in China. Circulation. 1985;71:202–210. doi: 10.1161/01.cir.71.2.202. [DOI] [PubMed] [Google Scholar]
- 315.Fontana L, Meyer TE, Klein S, Holloszy JO. Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc Natl Acad Sci U S A. 2004;101:6659–6663. doi: 10.1073/pnas.0308291101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Meyer TE, Kovács SJ, Ehsani AA, Klein S, Holloszy JO, Fontana L. Long-term caloric restriction ameliorates the decline in diastolic function in humans. J Am Coll Cardiol. 2006;47:398–402. doi: 10.1016/j.jacc.2005.08.069. [DOI] [PubMed] [Google Scholar]
- 317.García-Ortiz L, Recio-Rodríguez JI, Schmidt-Trucksäss A, Puigdomenech-Puig E, Martínez-Vizcaíno V, Fernández-Alonso C, Rubio-Galan J, Agudo- Conde C, Patino-Alonso MC, Rodríguez-Sánchez E, Gómez-Marcos MA, EVIDENT Group Relationship between objectively measured physical activity and cardiovascular aging in the general population: the EVIDENT trial. Atherosclerosis. 2014;233:434–440. doi: 10.1016/j.atherosclerosis.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 318.Seals DR, Tanaka H, Clevenger CM, Monahan KD, Reiling MJ, Hiatt WR, Davy KP, DeSouza CA. Blood pressure reductions with exercise and sodium restriction in postmenopausal women with elevated systolic pressure: role of arterial stiffness. J Am Coll Cardiol. 2001;38:506–513. doi: 10.1016/s0735-1097(01)01348-1. [DOI] [PubMed] [Google Scholar]
- 319.Beason-Held LL, Moghekar A, Zonderman AB, Kraut MA, Resnick SM. Longitudinal changes in cerebral blood flow in the older hypertensive brain. Stroke. 2007;38:1766–1773. doi: 10.1161/STROKEAHA.106.477109. [DOI] [PubMed] [Google Scholar]
- 320.Willette AA, Xu G, Johnson SC, Birdsill AC, Jonaitis EM, Sager MA, Hermann BP, La Rue A, Asthana S, Bendlin BB. Insulin resistance, brain atrophy, and cognitive performance in late middle-aged adults. Diabetes Care. 2013;36:443–449. doi: 10.2337/dc12-0922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Jack CR, Jr, Knopman DS, Jagust WJ, Petersen RC, Weiner MW, Aisen PS, Shaw LM, Vemuri P, Wiste HJ, Weigand SD, Lesnick TG, Pankratz VS, Donohue MC, Trojanowski JQ. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207–216. doi: 10.1016/S1474-4422(12)70291-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Anderson G. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Woods Johnson Foundation; 2010. [Google Scholar]
- 323.Bauer L, Pozehl B, Hertzog M, Johnson J, Zimmerman L, Filipi M. A brief neuropsychological battery for use in the chronic heart failure population. Eur J Cardiovasc Nurs. 2012;11:223–230. doi: 10.1016/j.ejcnurse.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Tarasoff-Conway JM, Carare RO, Osorio RS, Glodzik L, Butler T, Fieremans E, Axel L, Rusinek H, Nicholson C, Zlokovic BV, Frangione B, Blennow K, Ménard J, Zetterberg H, Wisniewski T, de Leon MJ. Clearance systems in the brain-implications for Alzheimer disease [published correction appears in Nat Rev Neurol. 2016;12:248] Nat Rev Neurol. 2015;11:457–470. doi: 10.1038/nrneurol.2015.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Roberts KF, Elbert DL, Kasten TP, Patterson BW, Sigurdson WC, Connors RE, Ovod V, Munsell LY, Mawuenyega KG, Miller-Thomas MM, Moran CJ, Cross DT, 3rd, Derdeyn CP, Bateman RJ. Amyloid-β efflux from the central nervous system into the plasma. Ann Neurol. 2014;76:837–844. doi: 10.1002/ana.24270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Louveau A, Smirnov I, Keyes TJ, Eccles JD, Rouhani SJ, Peske JD, Derecki NC, Castle D, Mandell JW, Lee KS, Harris TH, Kipnis J. Structural and functional features of central nervous system lymphatic vessels [published correction appears in Nature. 2016;533:278] Nature. 2015;523:337–341. doi: 10.1038/nature14432. [DOI] [PMC free article] [PubMed] [Google Scholar]