Psoriasis of palms and soles is an important condition for various reasons. Diagnosis is not always straightforward considering frequent clinical overlap with chronic eczema. To complicate this, there is frequent co-localization of these two conditions. Incidence of development of psoriasis over persistent chronic eczema due to Koebner's phenomena is not uncommon. Treatment of these two conditions will vary. Thus, proper diagnosis is essential for a successful outcome.
Palmoplantar areas may be affected in pustular psoriasis. This may be extensive involving many areas of the body or it may specifically located over the palms and soles. Palmoplantar pustular psoriasis, however, is not discussed here. Only classical plaque-type palmoplantar psoriasis (PPP) is described here.
PPP causes a significant psychological impact on the sufferer and hampers his/her daily activities. Management is difficult and more difficult than plaque psoriasis of nonpalmo-plantar areas.
Discussion on Evidence
There is serious lack of evidence. Continuous activities and trauma might adversely affect this. Thus, protection from trauma and frequent emollient application is generally advocated (LOE 5).
Topical treatment
Topical treatment is always preferred as the first-line therapy, but more than two-third of the patients require systemic therapy.
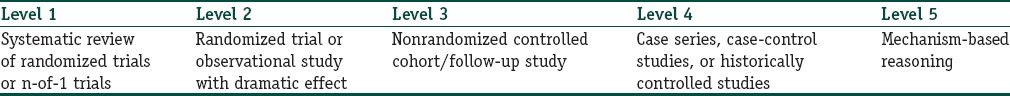
A randomized controlled trial (RCT) evaluated the comparative efficacy of topical 0.1% tazarotene cream and topical clobetasol propionate among 30 patients for 12 weeks. There was a good improvement in both without any significant difference between them. Complete clearance was noted among 52.9% and 61.5% of the patients, respectively, in tazarotene and clobetasol Group[1] (LOE 2).
Studies on other keratolytic agents such as salicylic acid are lacking. However, considering their safety and efficacy, many, including the author of this review, believe that these should be tried alone or in combination with other topicals such as topical corticosteroids (TCS) to reduce scaling (LOE 5).
Efficacy of calcipotriol has been reviewed.[2] One randomized study among 39 patients reported that twice weekly topical calcipotriol under occlusion was as effective twice daily application without occlusion[3] (LOE 2).
One retrospective analysis reported 12 out of 60 patients (20%) to have marked improvement with TCS while a similar extent of response was noticed among 17% (n = 5, total patients: 30) of patients who use only topical calcipotriol[4] (LOE 4).
Coal tar is another inexpensive agent and known to have some efficacy. Increased strength increases efficacy at the cost being increasingly cosmetically unacceptable. In a controlled trial, 6% crude coal tar was found to be better than salicylic acid and petroleum (both overnight, under occlusion). Coal tar resulted in good response among 76.5% of patients which was significantly higher than control group[5] (LOE 3).
One Cochrane review found one RCT that evaluated the comparative efficacy of narrowband ultraviolet B (NB-UVB) and topical psoralen-ultraviolet A (PUVA). There was no significant difference in terms of clearance rate.[6]
Topical PUVA was found to effectively improve in 63% of cases in an uncontrolled study on 48 patients[7] (LOE 3).
Topical PUVAsol (alternate day) was compared with topical clobetasol propionate cream and coal tar daily. In both groups, patients perceived “good improvement.” Improvement or cure was noticed among 90% versus 75% of palmar lesions and 76% versus 79% of plantar lesions, respectively, after TCS/tar and topical PUVAsol therapies.[8]
Broadband UVB (BB UVB) and paint PUVA (pPUVA) have been compared among 248 patients (124 in each arm). pPUVA was found to have relatively higher efficacy. Complete remission was noticed among 36 (30%) and 53 (42%) and no response was found among 57 (47%) and 14 (11%) patients who were treated, respectively, with BB UVB and pPUVA.[9]
PUVA and NB-UVB have some efficacy. Studies are sparse, and psoralens have known adverse effect. Thus, NB-UVB is better in high resource setting, and PUVAsol is better option as it is cheap and easily available everywhere. Topical PUVAsol and pPUVA are advantageous as oral psoralens are not needed. Considering all the available literature, topical PUVAsol or pPUVA appears preferable to PUVA and NB-UVB.
Studies have shown the efficacy of excimer laser (308 nm) in a case series[10] (LOE 4). However, this is expensive and not available widely.
Systemic drugs
A retrospective study evaluated the comparative efficacy of methotrexate (MTX) versus acitretin among 100 patients who had significant PPP. MTX was found to be significantly superior to acitretin after 12 weeks of therapy[11] (LOE 4). However, its extent of response is generally less than in psoriasis vulgaris and often requires higher dose.
In another study, MTX and acitretin were compared head to head. High-dose MTX (28 mg/week) appears to be significantly superior to 35 mg/day of acitretin[12] (LOE 2).
Only one retrospective study on cyclosporine (CyA) was found, in which only two patients were given CyA. There was a marked response in both (100%)[4] (LOE 4).
Results of a pooled analysis on apremilast from three large, multicenter, randomized, placebo-controlled studies reported a complete clearance of lesions in 46% of the treated group at 16th week[13] (LOE 1).
Infliximab (5 mg/kg, every 4 weeks) has been tried in a placebo-controlled randomized pilot trial among 24 patients. This pilot study did not reach its primary end point of m-PPPASI 75 at week 14, but improvement was higher than placebo[14] (LOE 2).
One RCT and one open-label study had evaluated the efficacy of adalimumab in PPP. Efficacy was found in both the studies[15,16] (LOE 2).
Ustekinumab was found to be moderately effective in an open-label study[17] (LOE 3).
Unpublished data from one randomized, double-blind, placebo-controlled trial (GESTURE study) evaluated secukinumab among a large number of patients with PPP. One-third of the patients who were on secukinumab 300 mg had clear or almost clear palms and soles at week 16. The result was higher than secukinumab 150 mg and placebo. Overall, palmoplantar disease improved by more than 50% in patients on secukinumab 300 mg at week 16.
However, a pooled analysis of a previously published RCT[18] on secukinumab in plaque-type psoriasis revealed that its efficacy in PPP was efficacious in comparison to placebo[19] (LOE 2).
A single case report showed good response after combination therapy with etanercept and alitretinoin[20] (LOE 4). More studies are necessary.
Suggested Therapeutic Protocol
Emollient is the first-line therapy and should be used as adjunctive to any other therapy. Topical keratolytics may be used as adjunctive therapy
Overall, this is resistant to treatments. Suggestion for a therapeutic ladder is difficult. In addition to efficacy, selection of drugs will depend on safety profile as frequently long-term treatment is necessary
Topical tazarotene, topical calcipotriol, and topical PUVAsol/pPUVA have been compared with potent TCS and were found to have slightly less efficacy (mostly statistically insignificant difference). They all can be considered as the first-line therapy. They are safer than potent TCS and can be used for longer duration
Potent TCS may be preferred as the first-line therapy when faster response is required. However, safety data beyond 12 weeks are unknown and should be avoided
Topical tazarotene, topical calcipotriol, and topical PUVAsol/pPUVA can also be considered as the first-line therapy. They are safer than potent TCS and can be used for longer duration and also be used after TCS as maintenance therapy
Topical calcipotriol can be used under occlusion intermittently for faster response and higher efficacy and for avoiding daily therapy
Topical coal tar is another option possibly of lesser efficacy than the above-mentioned first-line topical drugs. Higher available strength should be used. This can be considered as the second-line topical drug and may be tried before systemic drugs are used
Phototherapy in the form of 308-nm UVB monochromatic excimer light is effective, possibly safe, but expensive. This can be used if facility is available
MTX is the systemic drug of choice and is used when topical and phototherapies fail. However, higher dose is necessary
Acitretin is less effective than MTX. This can be tried in cases that do not respond to MTX
Apremilast and many biologics (many tumor necrosis factor inhibitors [TNFi] other than infliximab), secukinumab, and ustekinumab have shown variable efficacy. They can be used when standard therapies fail.
References
-
1.Mehta BH, Amladi ST. Evaluation of topical 0.1% tazarotene cream in the treatment of palmoplantar psoriasis: An observer-blinded randomized controlled study. Indian J Dermatol. 2011;56:40–3. doi: 10.4103/0019-5154.77550. [DOI] [PMC free article] [PubMed] [Google Scholar]
-
2.Thiers BH. The use of topical calcipotriene/calcipotriol in conditions other than plaque-type psoriasis. J Am Acad Dermatol. 1997;37(3 Pt 2):S69–71. [PubMed] [Google Scholar]
-
3.Duweb GA, Abuzariba O, Rahim M, al-Taweel M, al-Alem S, Abdulla SA. Occlusive versus nonocclusive calcipotriol ointment treatment for palmoplantar psoriasis. Int J Tissue React. 2001;23:59–62. [PubMed] [Google Scholar]
-
4.Adisen E, Tekin O, Gülekon A, Gürer MA. A retrospective analysis of treatment responses of palmoplantar psoriasis in 114 patients. J Eur Acad Dermatol Venereol. 2009;23:814–9. doi: 10.1111/j.1468-3083.2009.03197.x. [DOI] [PubMed] [Google Scholar]
-
5.Kumar B, Kumar R, Kaur I. Coal tar therapy in palmoplantar psoriasis: Old wine in an old bottle? Int J Dermatol. 1997;36:309–12. doi: 10.1046/j.1365-4362.1997.00176.x. [DOI] [PubMed] [Google Scholar]
-
6.Chen X, Yang M, Cheng Y, Liu GJ, Zhang M. Narrow-band ultraviolet B phototherapy versus broad-band ultraviolet B or psoralen-ultraviolet A photochemotherapy for psoriasis. Cochrane Database Syst Rev. 2013;(10) doi: 10.1002/14651858.CD009481.pub2. Art. No.: CD009481. DOI: 10.1002/14651858.CD009481.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
-
7.Carrascosa JM, Plana A, Ferrándiz C. Effectiveness and safety of psoralen-UVA (PUVA) topical therapy in palmoplantar psoriasis: A report on 48 patients. Actas Dermosifiliogr. 2013;104:418–25. doi: 10.1016/j.adengl.2013.04.005. [DOI] [PubMed] [Google Scholar]
-
8.Khandpur S, Sharma VK. Comparison of clobetasol propionate cream plus coal tar vs. topical psoralen and solar ultraviolet A therapy in palmoplantar psoriasis. Clin Exp Dermatol. 2011;36:613–6. doi: 10.1111/j.1365-2230.2011.04061.x. [DOI] [PubMed] [Google Scholar]
-
9.Lozinski A, Barzilai A, Pavlotsky F. Broad-band UVB versus paint PUVA for palmoplantar psoriasis treatment. J Dermatolog Treat. 2016;27:221–3. doi: 10.3109/09546634.2015.1093588. [DOI] [PubMed] [Google Scholar]
-
10.Goldberg DJ, Chwalek J, Hussain M. 308-nm Excimer laser treatment of palmoplantar psoriasis. J Cosmet Laser Ther. 2011;13:47–9. doi: 10.3109/14764172.2011.564769. [DOI] [PubMed] [Google Scholar]
-
11.Spuls PI, Hadi S, Rivera L, Lebwohl M. Retrospective analysis of the treatment of psoriasis of the palms and soles. J Dermatolog Treat. 2003;14(Suppl 2):21–5. doi: 10.1080/jdt.14.s2.21.25. [DOI] [PubMed] [Google Scholar]
-
12.Janagond AB, Kanwar AJ, Handa S. Efficacy and safety of systemic methotrexate vs. acitretin in psoriasis patients with significant palmoplantar involvement: A prospective, randomized study. J Eur Acad Dermatol Venereol. 2013;27:e384–9. doi: 10.1111/jdv.12004. [DOI] [PubMed] [Google Scholar]
-
13.Bissonnette R, Pariser DM, Wasel NR, Goncalves J, Day RM, Chen R, et al. Apremilast, an oral phosphodiesterase-4 inhibitor, in the treatment of palmoplantar psoriasis: Results of a pooled analysis from phase II PSOR-005 and phase III Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis (ESTEEM) clinical trials in patients with moderate to severe psoriasis. J Am Acad Dermatol. 2016;75:99–105. doi: 10.1016/j.jaad.2016.02.1164. [DOI] [PubMed] [Google Scholar]
-
14.Bissonnette R, Poulin Y, Guenther L, Lynde CW, Bolduc C, Nigen S. Treatment of palmoplantar psoriasis with infliximab: A randomized, double-blind placebo-controlled study. J Eur Acad Dermatol Venereol. 2011;25:1402–8. doi: 10.1111/j.1468-3083.2011.03984.x. [DOI] [PubMed] [Google Scholar]
-
15.Poulin Y, Crowley JJ, Langley RG, Unnebrink K, Goldblum OM, Valdecantos WC. Efficacy of adalimumab across subgroups of patients with moderate-to-severe chronic plaque psoriasis of the hands and/or feet: Post hoc analysis of REACH. J Eur Acad Dermatol Venereol. 2014;28:882–90. doi: 10.1111/jdv.12198. [DOI] [PMC free article] [PubMed] [Google Scholar]
-
16.Richetta AG, Mattozzi C, Giancristoforo S, D'Epiro S, Cantisani C, Macaluso L, et al. Safety and efficacy of Adalimumab in the treatment of moderate to severe palmo-plantar psoriasis: An open label study. Clin Ter. 2012;163:e61–6. [PubMed] [Google Scholar]
-
17.Au SC, Goldminz AM, Kim N, Dumont N, Michelon M, Volf E, et al. Investigator-initiated, open-label trial of ustekinumab for the treatment of moderate-to-severe palmoplantar psoriasis. J Dermatolog Treat. 2013;24:179–87. doi: 10.3109/09546634.2012.672710. [DOI] [PubMed] [Google Scholar]
-
18.Rich P, Sigurgeirsson B, Thaci D, Ortonne JP, Paul C, Schopf RE, et al. Secukinumab induction and maintenance therapy in moderate-to-severe plaque psoriasis: A randomized, double-blind, placebo-controlled, phase II regimen-finding study. Br J Dermatol. 2013;168:402–11. doi: 10.1111/bjd.12112. [DOI] [PubMed] [Google Scholar]
-
19.Paul C, Reich K, Gottlieb AB, Mrowietz U, Philipp S, Nakayama J, et al. Secukinumab improves hand, foot and nail lesions in moderate-to-severe plaque psoriasis: Subanalysis of a randomized, double-blind, placebo-controlled, regimen-finding phase 2 trial. J Eur Acad Dermatol Venereol. 2014;28:1670–5. doi: 10.1111/jdv.12359. [DOI] [PubMed] [Google Scholar]
-
20.Meyer V, Goerge T, Luger TA, Beissert S. Successful treatment of palmoplantar hyperkeratotic psoriasis with a combination of etanercept and alitretinoin. J Clin Aesthet Dermatol. 2011;4:45–6. [PMC free article] [PubMed] [Google Scholar]