Abstract
Objective
Evaluate an Internet-facilitated cognitive-behavioral treatment intervention for depression, tailored to economically disadvantaged mothers of young children.
Method
Economically disadvantaged mothers (N = 266) of pre-school aged children, who reported elevated levels of depressive symptoms, were randomized to either the eight-session, Internet-facilitated intervention (Mom-Net) or to Motivational Interviewing and Referral to Services (MIRS). Outcomes were measured using the Patient Health Questionnaire 9 (PHQ-9; Spitzer et al., 1999), the Structured Clinical Interview for DSM IV-TR Axis I Disorders (SCID; First, Spitzer, Gibbon, & Williams, 2002), and the Hamilton Depression Rating Scale (HDRS; Hamilton, 1960).
Results
Relative to participants in the MIRS condition, participants in Mom-Net demonstrated significantly greater reduction in depression as indexed by self-report questionnaire (primary outcome), interviewer-rated symptoms, and diagnostic outcomes.
Conclusions
Results suggest that the Mom-Net intervention is effective as a remotely delivered intervention for economically disadvantaged mothers.
Keywords: Depression, Mothers, Internet Intervention, Cognitive Behavioral Treatment
Mom-Net: Evaluation of an Internet-Facilitated Cognitive Behavioral Intervention for Low-Income Depressed Mothers
Socioeconomically disadvantaged mothers of young children are at particular risk for unipolar depressive symptoms and disorder (Malik et al., 2007; McLennan, Kotelchuck, & Cho, 2001; Weissman & Jensen, 2002). Though the disability associated with depression is well documented (McQuaid, Stein, Laffaye, & McCahill, 1999; Moussavi et al., 2007), some of the greatest costs of depressive conditions are those borne by the children of depressed mothers. Children of women with depressive syndromes are at increased risk for both internalizing and externalizing difficulties (Goodman, Lamping, & Ploubidis, 2010) as well as for impairments in cognitive and language development (Chapin & Altenhofen, 2010; Cycyk, Bitetti, & Hammer, 2015). The intergenerational transmission of psychopathology appears to be attributable, in part, to environmental influences associated with depressive symptomatology (Hummel & Kiel, 2015; Natsuaki et al., 2014; Radke-Yarrow & Klimes-Dougan, 2002). Depressed women evidence adverse parenting behavior characterized by less positive, less engaged, and more critical/harsh parenting than do nondepressed women (Lovejoy, Graczyk, O’Hare, & Neuman, 2000; Wang & Dix, 2013). Significantly, mounting evidence indicates that improvement in maternal depression is associated with gains in positive parenting behavior, parenting efficacy, parent-child interactions, and child symptoms (Cuijpers, Weitz, Karyotaki, Garber, & Andersson, 2015; Foster, Weissman, & Durlak, 2008; Garber, Ciesla, McCauley, Diamond, & Schloredt, 2011; Goodman, Broth, Hall, & Stowe, 2008; Shaw, Dishion, Connell, Wilson, & Gardner, 2009; Weissman et al., 2006), and thus suggests the potential benefits of intervention for depressed mothers.
A wealth of research supports the effectiveness of cognitive-behavioral therapy (CBT) interventions for depression (Cuijpers, Muñoz, Clarke, & Lewinsohn, 2009; Gloaguen, Cottraux, Cucherat, & Blackburn, 1998; National Institute of Mental Health [NIMH], 2003) in general and maternal depression, in particular (Ammerman et al., 2013; Chronis-Tuscano et al, 2013; Milgrom, Schembri, Ericksen, Ross, & Gemmill, 2011; Milgrom, Negri, Gemmill, McNeil, & Martin, 2005; cf. Verduyn, Barrowclough, Roberts, Tarrier, & Harrington, 2003). In each of these studies of maternal depression, the interventions have been tailored to address issues related to parenting and family relationships.
Despite the availability of efficacious interventions, however, most depressed persons do not access treatment readily (NIMH, 2003; Wang et al., 2005; Weissman & Jensen, 2002), and this treatment gap is exacerbated amongst low-income persons (Wang et al., 2005). Amongst the many potential barriers, several of the most substantial, including lack of mental health coverage, childcare, and transportation, differentially affect women of low socioeconomic status (NIMH, 2003; Weissman & Jensen, 2002). It is thus of critical importance to develop nontraditional service delivery systems to overcome barriers to treatment utilization. One approach to overcome barriers has been to integrate CBT into in-home visitation programs for at-risk mothers (Ammerman et al., 2013). Another approach has been through the use of Internet-delivered CBT. Because online interventions allow greater flexibility to access services at times and places convenient to the user, and reduce costs associated with travel and therapist time, there is potential for them to overcome many of the barriers facing underserved populations. Moreover, because this approach enables remote delivery, it has particular promise for addressing the challenge posed by the scarcity of providers in rural areas (Gale & Deprez, 2003). It is notable in this regard that amongst Americans living in rural areas, as well as those living in poverty, approximately two-thirds report Internet use (Horrigan, 2009).
Internet-based CBT programs for depression have shown significant promise (i.e., Andersson & Cuijpers, 2009; Andrews, Cuijpers, Craske, McEvoy, & Titov, 2010; Hedman, Ljótsson, & Lindefors, 2012), including interventions targeting new mothers (Danaher et al., 2013; Milgrom et al., 2016; O’Mahen et al., 2014). Meta-analytic data indicate that effects obtained by supported-Internet interventions (i.e., those including modest interaction with a coach or therapist) are comparable to those obtained in face-to-face therapy (Cuijpers, Donker, van Straten, Li, & Andersson, 2010). Supported interventions, moreover, evidence both better program adherence (Mohr, Burns, Schueller, Clarke, & Klinkman, 2013) and stronger effects than nonsupported interventions (Andersson, Bergström, Carlbring, & Lindefors, 2005; Andersson & Cuijpers, 2009; Kleiboer et al., 2015; Spek et al., 2007).
Mom-Net
In prior work, we developed and piloted Mom-Net, an Internet-facilitated, cognitive-behavioral treatment for depression, tailored to mothers of young children (Sheeber et al., 2012). The content foundation for the program was the Coping with Depression Course (CWDC; Lewinsohn, Antonuccio, Breckenridge, & Teri, 1984; Lewinsohn, Clarke, Rohde, Hops, & Seeley, 1996). We chose the CWDC because its extensive history of successful adaptation suggested both that it is amenable to diverse delivery modalities and that core content could be tailored to suit disparate populations (Cuijpers et al., 2009), including depressed and at-risk mothers (Chronis, Gamble, Roberts, & Pelham, 2006; Milgrom et al, 2005) and low-income individuals (Miranda et al., 2003). Mom-Net was designed as an integrated program consisting of both coach support and online materials. Core content is presented via online tutorials. Coaches use session-specific phone calls to assist mothers in understanding and applying the CBT strategies as well as to address barriers to implementation and engagement.
Content adaptations were based on research indicating that material perceived to be of high personal relevance is learned more easily (Knowles, 1984) and translated more effectively into behavioral change (Kreuter & Holt, 2001). To this end, the rationale for the intervention was expanded to cover the relations between depressive symptoms and parenting. Moreover, the teaching of each skill included a discussion of its relevance for improving both mood and parenting behavior. These adaptations were informed by the work of Milgrom, Martin, and Negri, (1999), who adapted the CWDC for treatment of postpartum depression. As well, participants were taught to implement the strategies in the context of parent-child interactions. The intervention was shortened to eight from twelve sessions because of the difficulty of maintaining engagement over longer periods (Christensen, Griffiths, & Farrer, 2009).
In our administration of Mom-Net, initiation of the intervention is preceded by a brief motivational interview (MI;Miller & Rollnick, 2002). The MI is intended to address motivational deficits that can be a barrier to participation in depressed populations, resulting in pervasive problems with attendance, homework completion, and ultimately, drop out (Weissman & Jensen, 2002). Brief pre-intervention MI is effective in promoting participation across a range of interventions and populations (e.g., Nock & Kazdin, 2005; Walitzer, Dermen, & Connors, 1999).
In an initial, tightly controlled efficacy trial (Sheeber et al., 2012), 70 women with elevated depressive symptoms were randomized to either the Mom-Net intervention or a delayed intervention/facilitated treatment as usual condition (DI/TAU). Participants in both conditions were provided with a computer, printer, and Internet access. Participants in both conditions participated in a pre-intervention, in-home motivational interview. Sixty-nine of 70 participants completed posttest assessments. Participants assigned to the Mom-Net condition were highly engaged, completing an average of 6.37 out of 8 sessions (SD=2.56, median=8.00) with 63% completing the entire intervention. They participated in an average of 6.70 coach calls (SD=2.11). Self-reported satisfaction with Mom-Net, as assessed with an adaptation of the Therapy Attitude Inventory (Brestan, Jacobs, Rayfield, & Eyberg, 1999) was high, averaging over 4 on each 5-point scale. Results indicated a large and significant effect of the Mom-Net intervention over the control condition on the primary treatment outcome measure of maternal depression as assessed by the BDI (Beck, Steer, & Brown, 1996). Results were maintained at 12 week follow up and replicated when participants in the DI/TAU condition subsequently received the intervention.
The Present Study
Though the efficacy trial demonstrated high levels of engagement, satisfaction, and efficacy, it was conducted with a small sample and under the tightly controlled conditions typical of initial efficacy tests. In particular, to provide equal access to the technology, computers and Internet connections were supplied to all participants, the coaches who provided phone support were research staff, and initial recruitment and MI sessions were conducted via home visits to participants. These conditions likely facilitated recruitment and retention of participants, as well as ease and fidelity of treatment delivery. Additionally, as only one third of the DI/TAU participants accessed services in the community, the control condition was less rigorous than desired. The goal of the current project, therefore, was to evaluate Mom-Net intervention effects within a larger trial under conditions that were more rigorous and closer (though not identical) to those of real-world service providers and recipients. As well, because one of the advantages of Internet delivery is to overcome access barriers, participant recruitment included rural areas. To this end, the current investigation is different in several ways from the initial trial. First, in the initial trial, coach contact was not provided for participants in the DI/TAU condition, and hence, we could not rule out the possibility that greater improvement for those in the Mom-Net condition was due to the effect of supportive attention from research staff. Thus, in the current investigation, participants in the comparison condition received biweekly calls from research staff who used an MI approach to facilitate engagement in services or other behavioral change activities. Second, to approximate real-world conditions, (a) coaching sessions for those in the Mom-Net condition were conducted by therapists employed by a not-for-profit agency providing community mental health services; (b) participants were not provided Internet access or gifted computers, though a small number (n=6) accessed the program through laptops borrowed from the mental health agency; and (c) the MI preceding the intervention for both conditions was conducted by phone rather than in a home visit.
Method
Trial Design
Participants were individually randomized (allocation ratio of 1:1) into two parallel intervention groups: Internet-facilitated CBT intervention (Mom-Net) or Motivational Interview and Referral to Services (MIRS). Research staff were blind to randomization sequence until allocation was revealed during the MI that preceded the intervention. The trial was conducted with approval of an appropriate institutional review board and registered with ClinicalTrials.gov.
Participants and Inclusion Criteria
Participants were 266 low-income mothers (aged 17.7 to 59.8) of pre-school aged children. Inclusion criteria were major or minor depressive disorder as reported on a screening assessment with the Patient Health Questionnaire 8 (PHQ-8; Kroenke & Spitzer, 2002), the ability to comprehend spoken English, and living at or below 185% of the federal poverty level. To be screened in as meeting criteria for major or minor depression, participants had to endorse either the depressed mood or anhedonia symptoms at the level of at least “more than half the days”, report impairment in social functioning, and endorse a total of 5 symptoms (for major depressive disorder) or 2 symptoms (for minor depressive disorder) at the level of at least “more than half the days” on the PHQ-8. Presence of a full scale diagnosed maternal depressive disorder was not a prerequisite for inclusion given evidence that elevated maternal depressive symptoms are associated with parenting difficulties and higher risk for adverse child outcomes regardless of diagnostic status (Lovejoy et al., 2000). Based on subsequent responses to the Structured Clinical Interview for DSM-IV (SCID: First, Spitzer, Gibbon, & Williams, 1997), 59.8 % of the sample met DSM-IV criteria for Major Depressive Disorder, 2.6% for Dysthymia, 2.3% for Minor Depressive Disorder (American Psychiatric Association, 2000) and 5.3% met criteria for Bipolar conditions. Outreach to communities with less access to resources was prioritized such that 37% of residents lived in communities that were micropolitan or more rural as defined by Rural-Urban Commuting Area Codes (RUCA2; Hart, Larson, & Lishner, 2005; http://depts.washington.edu/uwruca/ruca-data.php). Participants were enrolled regardless of whether they were involved in community-based treatments. Demographic data are presented in Table 1.
Table 1.
Baseline Demographics, Outcomes, and Treatment Utilization by Condition
| Demographics | Mom-Net (n = 134 ) |
MIRS (n = 132 ) |
Test Statistic |
|---|---|---|---|
| Latino/Hispanic/Spanish n (%) | |||
| Mother | 17 (12.7) | 14 (10.6) | 0.28 |
| Racial Category n (%) | 2.54a | ||
| White | 106 (79.1) | 105 (79.5) | |
| Non-Caucasian | 4 (3.0) | 9 (6.8) | |
| More than one race | 15 (11.2) | 11 (8.3) | |
| Not reported | 9 (6.7) | 7 (5.3) | |
| Education n (%) | 1.18 | ||
| Less than high school | 21 (15.7) | 19 (14.4) | |
| High school | 24 (17.9) | 28 (21.2) | |
| Vocational | 8 (6.0) | 11 (8.3) | |
| Some college | 68 (50.7) | 62 (47.0) | |
| Bachelor’s Degree or higher | 13 (9.7) | 12 (9.1) | |
| Marital Status n (%) | 11.09 | ||
| Married | 55 (41.0) | 52 (39.4) | |
| Living together | 30 (22.4) | 23 (17.4) | |
| Divorced/separated | 14 (10.4) | 32 (24.2) | |
| Widowed | 0 (0.0) | 1 (0.8) | |
| Single | 35 (26.1) | 24 (18.2) | |
| Mother’s age M (SD) | 31.4 (7.0) | 32.2 (7.5) | −0.90 |
Notes
Due to low frequencies, we tested Caucasian vs. Non-Caucasian; “not reported” cases were excluded from the analysis (n = 16).
All Bonferroni-corrected test statistics were nonsignificant.
Recruitment and Assessment Procedures
Screening
Head Start centers in micropolitan and smaller communities in Oregon were our primary point of contact, but in order to bolster recruitment and increase the diversity of the sample, we also invited women receiving services in two mid-size cities through both Head Start and a local department of human services, and posted ads in a local circular targeted toward families. Potential participants received an invitation letter and the PHQ-8 (Kroenke & Spitzer, 2002). The letter provided the informed consent information for the screening. The questionnaire was printed such that the answers (but not the questions) were recorded on a $20 check.1 This methodology allowed for convenient completion and compensation, and was used in previous research (Feil, et al., 2007; Sheeber et al., 2012). The invitation letter explained that if they completed the questionnaire, provided contact information on the check, and cashed the check, this would indicate consent to the screening and to being contacted by research staff if they were selected for possible further participation.
Assessment and Assignment
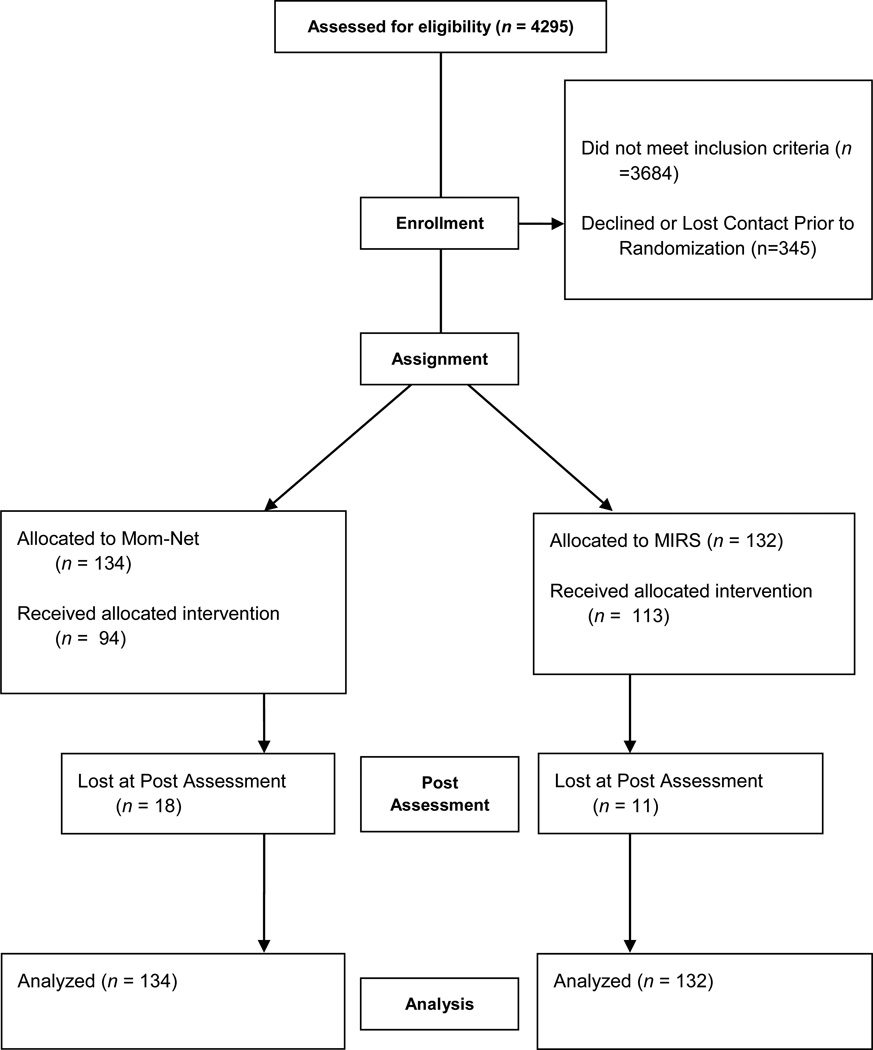
Informed consent information and questionnaires were collected by mail. Diagnostic interviews and motivational interviews were completed by phone by research staff. Randomization was accomplished by placing allocations in sealed envelopes which were shuffled prior to assignment. Research staff were blind to condition during the diagnostic interview and up until the point in the MI in which treatment options were discussed, at which point, staff opened the envelope containing the condition assignment. Post-assessments were conducted after the intervention period (T2; 26.2 weeks after T1); interviewers conducting the diagnostic interviews were blind to condition. Participants were compensated for each assessment. Figure 1 presents the participant flow diagram, utilizing Journal Article Reporting Standards (JARS).
Figure 1.
This flow diagram, utilizing JARS guidelines, depicts the numbers of participants at each assessment, and allocation to study conditions.
Measures
Maternal Depression
The PHQ-8 was administered as a screening instrument to determine study eligibility (Cronbach’s alpha = .89 for current sample). Subsequently the PHQ-9 was administered as an index of depressive symptoms at each full assessment point (Cronbach’s alpha = .85). The reliability and diagnostic accuracy of both versions of the PHQ are well established (Kroenke & Spitzer, 2002; Kroenke, Spitzer, & Williams, 2001; Kroenke et al., 2009; Spitzer, Kroenke, & Williams, 1999). The Structured Clinical Interview for DSM IV-TR Axis I Disorders (SCID; First et al., 2002) was administered by trained interviewers by phone to obtain affective diagnoses; in order to minimize respondent burden, only those modules relevant to diagnosis of depressive disorders were included. Inter-rater reliability on the SCID was excellent (kappa = .89). Finally, the 17-item Hamilton Depression Rating Scale (HDRS; Hamilton, 1960) was collected as part of the diagnostic interview to assess interviewer-rated depression severity (Cronbach’s alpha = .82). Each of these measures has been shown to be sensitive to change (e.g., Danaher et al., 2013; Titov et al., 2011).
Potential Moderators
Several indices were used to assess potential moderators of treatment effects. A demographic form queried marital status and income. Recruitment source was tracked at screening. Economic stress was assessed with Conger and Elder’s (1994) measure of financial strain. Anxiety was measured with the Generalized Anxiety Disorder 7-item scale (Spitzer, Kroenke, Williams, & Lowe, 2006) a widely used index of anxiety symptoms. Substance use was indexed as frequency of use of licit and illicit substances as assessed with the Monitoring the Future Survey (O’Malley, Johnston, Bachman, Schulenberg, & Kumar, 2006). Depression severity, as assessed by the PHQ-9, and presence of Bipolar Disorder, as assessed by the SCID, were also included as potential moderators.
Treatment Process
To assess treatment engagement in the Mom-Net condition we used computer-generated data, captured in real time, with regard to modules and coach calls completed, time spent online on Mom-Net program pages (page timeout was 5 minutes of inactivity), and number of program visits (i.e., number times Mom-Net website was accessed). These variables are well-established as indicants of treatment usage (Christensen et al., 2009; Donkin et al., 2011; Donkin et al., 2013). Number of coach calls was also documented for the MIRS condition. Usability and satisfaction with the Mom-Net intervention was assessed at post-intervention with an adapted version of the System Usability Scale (Sauro, 2011) and a series of 5-point Likert rating scales regarding the helpfulness of Mom-Net content and activities and the acceptability of characteristics of the coach calls. These items were modeled after the Therapy Attitude Inventory (Brestan et al., 1999) and used in our previous trial of the Mom-Net program (Sheeber et al., 2012). Coach fidelity with call scripts was assessed via session specific content adherence during coach calls for participant completed sessions
Community-Service Utilization
Participants’ report of community-based service utilization for behavioral or mental health difficulties was documented at each assessment. With written consent, we contacted providers to obtain verification of service provided.
Interventions
A motivational interview was conducted prior to intervention with participants in both conditions. During the interview, staff provided feedback from the initial depression screener and explored how depressive symptoms impacted the participants’ life, the participants’ desire for change, prior change efforts, and impediments or ambivalence about addressing depressive symptoms. The interviewer then encouraged the participant to make a decision as to whether participating in the project as a way to address depressive symptoms was desirable to them at current time. For participants in the Mom-Net condition, the MI ended with a brief role induction that outlined what to expect from the intervention and the behaviors on the part of the client that were recommended for a successful experience. Role induction has been found to improve participation in treatment (Walitzer et al., 1999). The interview took 60–90 minutes.
Mom-Net Intervention
Mom-Net consists of 8 sessions focused on CBT skills for the treatment of depression. Participants were permitted 4 months to complete the intervention (Md duration 70 days). Session content, outlined in Table 2, includes both core CBT skills (left column), and adaptations relevant to mothers of young children (right column). Relative to the original CWDC, Mom-Net had a greater emphasis on positive affect and behavioral activation (Hopko, Lejuez, Ruggiero, & Eifert, 2003; McMakin, Siegle, & Shirk, 2011), and lesser focus on cognitive restructuring.
Table 2.
Mom-Net Content
| Sessions | Core CBT | Parenting Focus |
|---|---|---|
| 1 | Intervention Rationale | |
|
|
|
| 2–3 | Behavioral Activation | |
|
|
|
| 4–5 | Interpersonal Skills | |
|
|
|
| 6 | Cognitive Skills: Positive Thoughts | |
|
|
|
| 7 | Cognitive Skills: Negative Thoughts | |
|
|
|
| 8 | Planning for the Future | |
|
|
|
We designed the program in accordance with principles of quality instructional design (Kameenui & Carnine, 2001), with a particular focus on design principles relevant to promoting self-regulated learning. Effective instructional design facilitates learning by reducing the cognitive load so as to not tax the learner’s working memory (Kirschner, 2002). This focus is particularly important in an intervention for individuals with depressive symptoms given their difficulties with cognitive processes and vulnerability to depressogenic thoughts under conditions of stress (Wenzlaff & Bates, 1998). Key structural elements, consistent with these principles included: (a) judicious review, wherein earlier concepts are revisited in subsequent sessions, varied examples are used to promote generalization, and homework is used to provide practice; (b) conspicuous and integrated strategies, in which the component steps of each skill are taught to mastery before they are integrated; and (c) mediated scaffolding, such that models and feedback are provided to the learner and faded as mastery is achieved (Kameenui & Carnine, 2001). In Mom-Net, the scaffolding was provided via immediate feedback from the computer program as well as by the coach. Another key structural feature was the use of varied multimedia materials and interactive elements to maintain participant engagement. We developed a competency-based approach in which knowledge acquisition was examined at the completion of each session. The goal was to achieve mastery (i.e., 80% correct responses) before the user proceeded to the next module. The program identifies incorrect responses, reviews related content, and re-tests the material, as needed. Most text elements are accompanied by corresponding audio and the remaining elements have optional narration in order to reduce literacy requirements. Participants were prompted to complete a PHQ-9 biweekly for safety monitoring.
Coaches were staff at the community mental health agency implementing the program. Of 7 coaches, 5 were masters level therapists and 2 were bachelor level paraprofessionals. Prior to initiating the trial, coaches participated in two days of training conducted by one of the intervention developers (ES), who served as one of the clinical supervisors. Training included didactic presentations and practice in MI and CBT skills as well as in protocols for responding to clinical emergencies. During the trial, coaches participated in weekly supervision with the trainer and a clinical supervisor at the agency.
Coaches scheduled phone conferences with participants to correspond with each Mom-Net session. The average duration of calls was 33.5 minutes. Coaches assisted mothers in understanding and applying the CBT strategies. They recognized participants’ accomplishments, reviewed content that the participant had not yet “mastered,” and answered questions. Reluctance or barriers to engaging in the intervention were addressed within the MI framework, with coaches making reflective statements, emphasizing positive statements, helping mothers to identify if goals had changed, and problem-solving ways to meet their goals.
Coaching was facilitated by an online infrastructure that provided coaches and supervisors with tools for monitoring client progress and participation. An administrative webpage, enabled coaches to: (a) monitor participation, understanding, and clinical progress (i.e., program utilization, homework completion, mood/activity ratings, content mastery, and biweekly depression ratings); and (b) tailor content of coach calls based on the information provided. The infrastructure also allowed mothers to connect with coaches in crisis situations via an online crisis link, which alerted coaches and supervisors via an immediate text message.
Motivational Interviewing and Referral to Services
The MIRS condition included several features consistent with patient navigation strategies developed for chronic conditions (Dohan & Schrag, 2005; Freeman & Rodriguez, 2011; Natale-Pereira, Enard, Nevarez, & Jones, 2011) including depression (Diaz-Linhart et al., 2016), such as an MI engagement interview, referral to community services, and ongoing monitoring and support. As noted earlier, participants in the MIRS condition participated in the MI engagement interview at the conclusion of the pre-intervention assessment. Research staff then provided mothers with information about, and referrals to, community providers who serve low-income individuals. Research staff offered to initiate contact with the treatment provider to make an initial appointment. Participants also received biweekly motivational calls from a research staff who served as a coach during the 4-month intervention period these calls lasted an average of 20.4 minutes. Working within an MI framework, the coach: (a) checked in with mothers about the concerns they had raised in the initial motivational interview; (b) queried as to what mothers were doing to seek/engage in mental health services and to otherwise improve their mood; and (c) used reflective statements to emphasize mothers’ change statements. They also administered the PHQ-9 for safety monitoring. Research staff doing the MIRS coaching consisted of two bachelors level and one doctoral level nonclinical staff, trained in the use of MI skills. Training and ongoing supervision was provided by a research supervisor who was a masters level clinician.
Provision of MI calls to mothers was intended to have two effects. First, it was an effort to actively engage mothers in intervention to render the MIRS condition as robust as possible, and akin to a comparative intervention. Secondly, given the strong associations between social support and depression (Santini, Koyanagi, Tyrovolas, Mason, & Haro, 2015) the MI calls were designed to provide some control for the support provided by Mom-Net coaches; that is, to rule out the possibility that Mom-Net benefits accrue primarily as a function of supportive contact.
Sample Size Determination and Statistical Methods
Sample Size
Estimates of effect sizes were based on a meta-analysis of the CWDC (average ES = .65 for controlled trials; Cuijpers, 1998) as well as on a trial of an Internet-based cognitive intervention (ES = .54 for participants with elevated CES-D scores; Clarke et al., 2005). We selected a sample size (n=130/group) that would provide adequate power (estimate = .80) to detect a small-to-medium effect size (Cohen’s d = .38).
Missing data
Rates of missing data for study outcomes was <1% at baseline and 13–18% at posttest. Multiple imputation was used to replace missing values following best-practice recommendations (Graham, 2009). Missing data were imputed using the IVEWare program (Raghunathan, Solenberger, & Van Hoewyk, 2002), which uses all available data to impute missing data via a sequential regression approach. The observed and imputed data were compared to ensure they showed similar distributions (Abayomi, Gelman, & Levy, 2008). Missing data points were replaced with imputed data in 20 data sets, which were analyzed separately. Model parameters and standard errors, which incorporate within and between model parameter variability, were combined following Rubin (1987) as implemented in SAS PROC MIANALYZE (SAS Institute Inc., 2011).
Analytic Models
Group differences in continuous posttest depression scores (PHQ-9 and HDRS) were examined separately with mixed effects regression models estimated with SAS PROC MIXED using restricted maximum likelihood with intercepts allowed to vary randomly. Group differences in the dichotomous posttest depression diagnosis were estimated with SAS PROC LOGISTIC. All models included the pretest score as a covariate and study condition as a two-level predictor with Mom-Net as the reference group. Next, we tested moderation of the main effects of condition, separately for each hypothesized moderator, by adding the moderator and its interaction with condition to the main effects models. Effect sizes were summarized as Cohen’s d-statistic for continuous outcomes (.2 small, .5 medium, and .8 large effect; Cohen, 1988) and odds ratios (OR) for the dichotomous depression diagnosis (1.48 small, 2.48 medium, 4.28 large; Lipsey & Wilson, 2001).
Results
Preliminary analyses
All 266 participants completed the pretest assessment and 89% completed the posttest assessment. Number of completed assessments was not related to study condition (χ2[1,266]=1.78, p=.182) or any pretest measure. Demographic and pre-test variables were examined for baseline equivalence, with a Bonferroni correction applied to multiple tests. No significant differences were found as a function of condition on pre-test values or demographic variables. No between group differences emerged between participants who initiated participation in one of the two conditions and those who did not. Demographic data are presented in Table 1.
Program Utilization, Satisfaction, and Usability
Table 3 presents the descriptive statistics for the measures of program utilization, satisfaction, and usability. Of the 134 Mom-net participants, 67.8% initiated program usage, with 56.7% completing four or more sessions. Participants who initiated the program completed on average 6.6 of the eight modules (70% completed all modules). Amongst participants who initiated use, the website was used extensively as indicated by the mean number of program visits and the average total hours of use. With respect to program satisfaction, the mean ratings were above 4 on a 5-point Likert-type scale for skills and website usability, indicating that the participants were highly satisfied with the Mom-Net intervention. In the MIRS condition, 85% if participants engaged in at least one coach call. Participants in both conditions also rated the coach support highly, with mean ratings above 4.3 on a 5-point Likert-type scale. Across all completed sessions, Mom-Net coaches covered 78.0% of relevant content.
Table 3.
Program Utilization, Satisfaction, and Usability by Condition
| Measure | Mom-Net M (SD) |
MIRS M (SD) |
|---|---|---|
| Computer-generated indices | ||
| Number of modules completed | 6.6 (2.4) | N/A |
| Number of program visits | 19.6 (15.7) | N/A |
| Hours on program | 5.5 (3.2) | N/A |
| Participant-rated satisfaction (5 point scale) | ||
| Skills and materials | 4.2 (0.8) | N/A |
| Website | 4.2 (0.7) | N/A |
| Coach Assistance | 4.3 (0.7) | 4.4 (0.8) |
| Coach Calls | ||
| Number of coach calls | 6.9 (4.8) | 5.2 (2.0)* |
| Duration of calls in minutes | 33.50 (20.21) | 20.36 (5.53)** |
Note. This data reflects indices for participants who initiated the program.
t(245) = 3.527, p<.001
t(245) = 6.677, p<.0001
With regard to community service utilization, 37% of participants in the MIRS condition and 31% of participants in the Mom-Net condition received mental health services during the interval between pretest and posttest, χ2(232)=0.93, p=.41. In the MIRS condition, 30.3% received pharmacotherapy intervention and 21% received counseling, while in the Mom-Net condition 26.5% received pharmacotherapy and 14.2% participated in counseling, χ2(232)=0.39, p=56 and χ2(232)=1.87, p=23, respectively.
Between-Group Intervention Effects
Descriptive statistics for the study outcomes at pre-and posttest are shown in Table 4. Mixed effects regression models showed the Mom-Net group had significantly lower posttest adjusted PHQ-9 (estimate = −1.51, t = −2.44, p = .015, d = .27) and HDRS (estimate = −1.85, t = −2.35, p = .019, d = .24) scores compared to MIRS participants (Bonferroni-corrected p = .05/2 = .025). Within group effects in the Mom-Net condition (Cohen’s d = 1.31) were consistent with effects obtained in an earlier small-scale trial (Cohen’s d = 1.11; Sheeber et al., 2012). Effects for the MIRS condition were Cohen’s d = 1.08.
Table 4.
Descriptive Statistics for Study Outcomes
| Mom-Net | MIRS | |||
|---|---|---|---|---|
| Pretest | Posttest | Pretest | Posttest | |
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | |
| PHQ-9 | 14.03 (4.98) | 6.27 (5.00) | 14.43 (5.95) | 7.90 (5.37) |
| Hamilton | 13.31 (7.60) | 7.48 (5.89) | 13.71 (7.95) | 9.41 (6.58) |
| Current depressiona | 68.6% (4.84) | 47.9 % (6.23) | 64.4 % (5.19) | 59.5% (5.54) |
The average percentage and standard error of participants with a current depression diagnosis. Means and standard deviations averaged across 20 imputed data sets.
Logistic regression analysis showed that the Mom-Net group had significantly lower odds of meeting DSM-IV criteria for a depression diagnosis at posttest compared to MIRS participants (adjusted OR = 0.53, 95% CI = 0.29 – 0.98). Remission rates, as defined by DSM IV criteria, were 39.7% in the Mom-Net condition and 28.18% in the MIRS condition. Stated differently, by taking the reciprocal of the adjusted OR (1/0.53 = 1.89) the MIRS participants had approximately 89% greater odds of meeting criteria for a current diagnosis of depression at posttest compared to Mom-Net participants.
Moderation of Condition Effects
Several moderators were evaluated, including recruitment source, depression severity, self-reported anxiety level, substance use, marital status, family income and economic stress, as well as presence of bipolar disorder. Bonferroni corrections were applied to the evaluation of significance, to maintain familywise alpha=.05. None of the condition X moderator effects were statistically significant for PHQ-9, HDRS, and current depression diagnosis at posttest.
Discussion
Mom-Net is coach-facilitated, Internet-delivered CBT intervention comprised of both online tutorials and coach phone calls corresponding to each session. It was developed for and targeted to low-income mothers of young children, as a population at greatly increased vulnerability to depressive conditions. In this RCT, the Mom-Net intervention was administered in a community mental health center by community-based bachelor- and masters-level clinicians. Because motivational deficits can be a barrier to participation in depressed populations, participation in both conditions was preceded by a brief motivational interview aimed at promoting community-based resources as well as engagement and active participation in the Mom-Net intervention. It was compared to an alternative intervention condition that received facilitated referrals to community treatment providers as well as biweekly phone contact with a coach. As discussed, phone calls in the control conditions used an MI framework and were intended to facilitate engagement in community mental health services and provide social support as a control for that provided by the Mom-Net coaches.
With regard to engagement and participation, it is important to note that 30% of participants never initiated program use. It is possible that as the sample was recruited, which is to say, not treatment seeking, that motivation to participate in research may have exceeded motivation for treatment engagement. It is also likely that there are barriers to engagement that were not sufficiently addressed by either our initial motivational interview or ongoing coach support. Nonetheless, these rates are similar to others reported in the literature for both on-line and in person interventions (Kaltenthaler et al., 2008). Identifying factors associated with nonengagement is an important focus of ongoing research.
Notably, however, amongst participants who initiated use, participation in the program was high. On average, participants who initiated the program (70% of Mom-Net participants) completed 80% of sessions, with more that 70% completing all sessions. Additionally, they completed more than 85% of expected coach calls. As well, participants reported high levels of satisfaction with the program, indicating that they found the intervention helpful, the website easy to use, and the coaches to be supportive. Overall these indices of engagement and satisfaction are comparable with that of other Internet interventions (Christensen et. al, 2009; Kaltenthaler et al., 2008; Waller & Gilbody, 2009). By means of comparison, Waller and Gilbody (2009) have reported in a systematic review of computerized CBT that on average 56% of participants complete the full course of intervention.
Turning to effectiveness, the results were very promising. Participants in the Mom-Net condition demonstrated significantly greater reduction in depression as indexed by self-report questionnaire (primary outcome), interviewer-rated symptoms, and diagnostic outcomes. The effect sizes obtained in the current study are comparable to the overall effect size of d = .28 for the 18 CWDC treatment studies included in the meta-analytic review conducted by Cuijpers and colleagues (2009). Moreover, the within group effects for the Mom-Net condition were large, mirroring those obtained in our earlier tightly controlled pilot trial (Sheeber et al., 2012). These effects are notable for a number of reasons. As described, economically disadvantaged mothers of young children experience depressive conditions at high rates (Malik et al., 2007; McLennan et al., 2001; Weissman & Jensen, 2002), resulting in suffering and impairment for themselves and their children. Moreover, evidence suggests that they are unlikely to access traditionally offered services (Wang et al., 2005; Weissman & Jensen, 2002). The current project is important in that it speaks to the feasibility of remotely delivered interventions, which have the potential to overcome barriers to access for this at-risk population. In particular, it speaks to the plausibility of using Internet technology in low income and rural households. The replication of our earlier findings is also significant. This study improved on the initial pilot work (Sheeber et al., 2012) by providing a more robust control condition, eliminating research-specific supports (e.g., provision of computer and internet), and shifting the coaching to community-based therapists, rather than research staff. The significant effects, in this context, suggest the potential disseminability of the intervention for community-based delivery. This will be an important direction for future research.
It is worth noting, as well, that the effect size for between-group comparisons was modest, reflecting the beneficial impact of the alternative intervention comparison condition, which also demonstrated a large within-group effect. The large effect may be attributable, in part, to the fact that a sizable percentage of participants accessed services in the community. It may also reveal the beneficial impact of the support provided by the coaches. These effects are notable as the intervention was less intensive than the Mom-Net condition, including fewer and shorter coach calls and no structured intervention. As noted earlier, the MIRS condition shared features consistent with emerging patient navigation strategies for chronic conditions, whose goals are to reduce health disparities experienced by vulnerable populations (Natale-Pereira et al., 2011). The combination of MI, referrals, and ongoing monitoring and support, appears to have been highly beneficial to participants.
A question could be raised regarding the extent to which coach support is necessary for treatment effects. As described earlier, existing research suggests that treatment effects are typically stronger for Internet interventions supplemented by human support. Supported interventions, moreover, evidence both better program adherence (Mohr et al., 2013) and stronger effects than non-supported interventions (Andersson et al., 2005; Andersson & Cuijpers, 2009; Cuijpers et al., 2010; Kleiboer et al., 2015; Spek et al., 2007). Nonetheless, one limitation of our design is that because the two components of the intervention were highly integrated (e.g., “Try this strategy and then discuss how it went with your coach”; “Make a plan and send it to your coach for review”), with both aspects designed to facilitate engagement and skill acquisition, the unique effects of each component cannot be determined. The extent of the integration reflects our conceptualization of the intervention as facilitating remote delivery of services rather than as a stand-alone intervention. That said, revising the tutorials so as to enable self-administration without coach support may be a useful direction for future research. Though effect sizes would likely be significantly lower (Andersson & Cuijpers, 2009), the public health benefit could be large given the potentially greater reach (Glasgow, 2007), if attention to instructional design is successful in overcoming barriers to engagement and retention evident in unsupported programs (Christensen et al., 2009).
There are, of course, limitations to discuss. First, these effects reflect the initial pre-post outcomes, and don’t speak to the extent to which effects are maintained over time. Subsequent analyses will address maintenance of treatment effects as the long-term follow-up data become available. As well, we will examine the effects to which results are mediated by hypothesized changes in cognitive-behavioral mechanisms. Second, because the sample was relatively homogeneous with regard to demographic characteristics and included a large percentage who had attended some college, we do not know how the intervention would have fared in a more diverse sample, though meta-analyses on the CWDC indicate that its effectiveness is robust across diverse populations (Cuijpers et al., 2009). Third, in order to minimize participant burden, we limited the number of outcomes and did not assess comorbid psychopathology. Hence, the effect of comorbid psychopathology on the effectiveness of the Mom-Net intervention awaits future research. As well, our focus hear was on diagnostic outcomes, and we did not include broader indices of well-being such as quality of life measures. Fourth, mothers were included based on the PHQ-9 screener and approximately one-third of the sample did not meet DSM-IV criteria for a depressive diagnosis at pretest based on the SCID interview. However, the CWDC has been shown to be effective for preventing escalation to full syndrome among individuals with subthreshold depression (Cuijpers et al., 2009).
Additional directions for future work are also worth noting. At this stage in the program of research, it makes sense to turn our attention to questions of implementation and sustainability (Curran, Bauer, Mittman, Pyne, & Stetler, C., 2012). Reach is also important: are there nonclinical community sites serving low income families, such as Head Start programs who would be natural partners for the delivery of the Mom-Net intervention? Moreover, given that younger and lower income persons differentially access the Internet through mobile devices, it will be critical to adapt the intervention for these delivery systems (Pew Research Center, 2015).
In closing, the Mom-Net intervention appears to be feasible and effective, as a remotely delivered treatment for economically disadvantaged mothers. Relative to coach-supported, facilitated usual care, it demonstrated significant effects on multiple indices of depressive outcomes.
Public Health Significance Statement.
This study suggests that cognitive behavioral therapy delivered remotely over the Internet will help mothers suffering from depression.
Acknowledgments
This research was supported by a grant from the National Institute for Mental Health.
Footnotes
Questions were not printed on the check so that responses were not interpretable by bank staff.
Contributor Information
Lisa B. Sheeber, Oregon Research Institute, Eugene, Oregon
Edward G. Feil, Oregon Research Institute, Eugene, Oregon
John R. Seeley, Oregon Research Institute, Eugene, Oregon
Craig Leve, Oregon Research Institute, Eugene, Oregon.
Jeff M. Gau, Oregon Research Institute, Eugene, Oregon
Betsy Davis, Oregon Research Institute, Eugene, Oregon.
Erik Sorensen, Eugene, Oregon.
Steve Allan, Options Counseling, Eugene, Oregon.
References
- Abayomi K, Gelman A, Levy M. Diagnostics for multivariate imputations. Journal of the Royal Statistical Society: Series C (Applied Statistics) 2008;57:273–291. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: American Psychiatric Association; 2000. text revision. [Google Scholar]
- Ammerman RT, Putnam FW, Altaye M, Stevens J, Teeters AR, Van Ginkel JB. A clinical trial of in-home CBT for depressed mothers in home visitation. Behavior Therapy. 2013;44(3):359–372. doi: 10.1016/j.beth.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G, Bergström J, Carlbring P, Lindefors N. The use of the Internet in the treatment of anxiety disorders. Current Opinion in Psychiatry. 2005;18(1):73–77. [PubMed] [Google Scholar]
- Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: A meta-analysis. Cognitive Behaviour Therapy. 2009;38(4):196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: A meta-analysis. PloS One. 2010;5(10):e13196. doi: 10.1371/journal.pone.0013196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the beck depression inventory. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Brestan EV, Jacobs JR, Rayfield AD, Eyberg SM. A consumer satisfaction measure for parent-child treatments and its relation to measures of child behavior change. Behavior Therapy. 1999;30(1):17–30. [Google Scholar]
- Chapin LA, Altenhofen S. Neurocognitive perspectives in language outcomes of Early Head Start: Language and cognitive stimulation and maternal depression. Infant Mental Health Journal. 2010;31(5):486–498. doi: 10.1002/imhj.20268. [DOI] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Farrer L. Adherence in Internet interventions for anxiety and depression. Journal of Medical Internet Research. 2009;11(2):e13. doi: 10.2196/jmir.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis AM, Gamble SA, Roberts JE, Pelham WE. Cognitive-behavioral depression treatment for mothers of children with attention-deficit/hyperactivity disorder. Behavior Therapy. 2006;37(2):143–158. doi: 10.1016/j.beth.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Clarke TL, O’Brien KA, Raggi VL, Diaz Y, Mintz AD, Seeley J. Development and preliminary evaluation of an integrated treatment targeting parenting and depressive symptoms in mothers of children with attention-deficit/hyperactivity disorder. Journal of Consulting and Clinical Psychology. 2013;81(5):918. doi: 10.1037/a0032112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke G, Eubanks D, Kelleher C, O’Connor E, DeBar LL, Lynch F, Gullion C. Overcoming Depression on the Internet (ODIN) 2: A randomized trial of a self-help depression skills program with reminders. Journal of Medical Internet Research. 2005;7(2):e16. doi: 10.2196/jmir.7.2.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Conger RD, Elder GH. Families in troubled times: The Iowa youth and families project. In: Conger RD, Elder GH, Lorenz FO, Simons RL, Whitbeck LB, editors. Families in troubled times: Adapting to change in rural America. New York: Aldine de Gruyter; 1994. pp. 3–19. [Google Scholar]
- Cuijpers P. A psychoeducational approach to the treatment of depression: A meta-analysis of Lewinsohn’s “Coping With Depression” course. Behavior Therapy. 1998;29:521–533. [Google Scholar]
- Cuijpers P, Muñoz RF, Clarke GN, Lewinsohn PM. Psychoeducational treatment and prevention of depression: The “Coping with Depression” course thirty years later. Clinical Psychology Review. 2009;29(5):449–458. doi: 10.1016/j.cpr.2009.04.005. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Donker T, van Straten A, Li J, Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychological Medicine. 2010;40(12):1943–1957. doi: 10.1017/S0033291710000772. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Weitz E, Karyotaki E, Garber J, Andersson G. The effects of psychological treatment of maternal depression on children and parental functioning: A meta-analysis. European Child & Adolescent Psychiatry. 2015;24(2):237–245. doi: 10.1007/s00787-014-0660-6. [DOI] [PubMed] [Google Scholar]
- Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care. 2012;50(3):217. doi: 10.1097/MLR.0b013e3182408812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cycyk LM, Bitetti D, Hammer CS. Maternal depressive symptomatology, social support, and language development of bilingual preschoolers from low-income households. American Journal of Speech-Language Pathology. 2015;24(3):411–425. doi: 10.1044/2015_AJSLP-14-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danaher BG, Milgrom J, Seeley JR, Stuart S, Schembri C, Tyler MS, Lewinsohn P. MomMoodBooster web-based intervention for postpartum depression: feasibility trial results. Journal of Medical Internet Research. 2013;15(11):e242. doi: 10.2196/jmir.2876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz-Linhart Y, Silverstein M, Grote N, Cadena L, Feinberg E, Ruth BJ, Cabral H. Patient navigation for mothers with depression who have children in Head Start: A pilot study. Social Work in Public Health, May. 2016;19:1–7. doi: 10.1080/19371918.2016.1160341. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohan D, Schrag D. Using navigators to improve care of underserved patients. Cancer. 2005;104(4):848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- Donkin L, Christensen H, Naismith SL, Neal B, Hickie IB, Glozier N. A systematic review of the impact of adherence on the effectiveness of e-therapies. Journal of Medical Internet Research. 2011;13(3):e52. doi: 10.2196/jmir.1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donkin L, Hickie IB, Christensen H, Naismith SL, Neal B, Cockayne NL, Glozier N. Rethinking the dose-response relationship between usage and outcome in an online intervention for depression: Randomized Controlled Trial. Journal of Medical Internet Research. 2013;15(10):e231. doi: 10.2196/jmir.2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feil EG, Severson H, Taylor T, Boles SM, Albert DA, Blair J. An innovative, effective and cost effective survey method using a survey-check response format. Prevention Science. 2007;8(2):133–40. doi: 10.1007/s11121-006-0060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. User’s guide for the Structured clinical interview for DSM-IV axis I disorders SCID-I: Clinician version. Arlington, VA: American Psychiatric Association Publishing; 1997. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Foster CJE, Weissman MM, Durlak JA. Current and past maternal depression, maternal interaction behaviors, and children’s externalizing and internalizing symptoms. Journal of Abnormal Child Psychology. 2008;36:527–537. doi: 10.1007/s10802-007-9197-1. [DOI] [PubMed] [Google Scholar]
- Freeman HP, Rodriguez RL. History and principles of patient navigation. Cancer. 2011;117(S15):3537–3540. doi: 10.1002/cncr.26262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Ciesla JA, McCauley E, Diamond G, Schloredt KA. Remission of depression in parents: Links to healthy functioning in their children. Child Development. 2011;82(1):226–243. doi: 10.1111/j.1467-8624.2010.01552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale JA, Deprez RD. A public health approach to the challenges of rural mental health service integration. In: Stamm HB, editor. Rural behavioral health care: An interdisciplinary guide. Washington, DC: American Psychological Association; 2003. pp. 95–108. [Google Scholar]
- Glasgow RE. eHealth evaluation and dissemination research. American Journal of Preventative Medicine, 32. 2007;(Suppl. 5):S119–S126. doi: 10.1016/j.amepre.2007.01.023. [DOI] [PubMed] [Google Scholar]
- Gloaguen V, Cottraux J, Cucherat M, Blackburn I. A meta-analysis of the effects of cognitive therapy in depressed patients. Journal of Affective Disorders. 1998;49:59–72. doi: 10.1016/s0165-0327(97)00199-7. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Broth MR, Hall CM, Stowe ZN. Treatment of postpartum depression in mothers: Secondary benefits to the infants. Infant Mental Health Journal. 2008;29(5):492–513. doi: 10.1002/imhj.20188. [DOI] [PubMed] [Google Scholar]
- Goodman A, Lamping DL, Ploubidis GB. When to use broader internalising and externalising subscales instead of the hypothesised five subscales on the Strengths and Difficulties Questionnaire (SDQ): Data from British parents, teachers and children. Journal of Abnormal Child Psychology. 2010;38(8):1179–1191. doi: 10.1007/s10802-010-9434-x. [DOI] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. American Journal of Public Health. 2005;95(7):1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedman E, Ljótsson B, Lindefors N. Cognitive behavior therapy via the Internet: A systematic review of applications, clinical efficacy and cost-effectiveness. Expert Review of Pharmacoeconomics & Outcomes Research. 2012;12(6):745–64. doi: 10.1586/erp.12.67. [DOI] [PubMed] [Google Scholar]
- Horrigan J. Pew Internet & American Life Project. Washington, DC: 2009. Home broadband adoption 2009. [Google Scholar]
- Hopko DR, Lejuez C, Ruggiero KJ, Eifert GH. Contemporary behavioral activation treatments for depression: Procedures, principles, and progress. Clinical Psychology Review. 2003;23(5):699–717. doi: 10.1016/s0272-7358(03)00070-9. [DOI] [PubMed] [Google Scholar]
- Hummel AC, Kiel EJ. Maternal depressive symptoms, maternal behavior, and toddler internalizing outcomes: A moderated mediation model. Child Psychiatry & Human Development. 2015;46(1):21–33. doi: 10.1007/s10578-014-0448-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaltenthaler E, Sutcliffe P, Parry G, Beverley C, Rees A, Ferriter M. The acceptability to patients of computerized cognitive behaviour therapy for depression: A systematic review. Psychological Medicine. 2008;38(11):1521–1530. doi: 10.1017/S0033291707002607. [DOI] [PubMed] [Google Scholar]
- Kameenui EJ, Carnine DW. Effective teaching strategies that accommodate diverse learners. Paramus, NJ: Prentice Hall Inc; 2001. [Google Scholar]
- Kirschner PA. Cognitive load theory: Implications of cognitive load theory on the design of learning. Learning and Instruction. 2002;12(1):1–10. [Google Scholar]
- Kleiboer A, Donker T, Seekles W, van Straten A, Riper H, Cuijpers P. A randomized controlled trial on the role of support in internet-based problem solving therapy for depression and anxiety. Behaviour Research and Therapy. 2015;72:63–71. doi: 10.1016/j.brat.2015.06.013. [DOI] [PubMed] [Google Scholar]
- Knowles MS, Associates . Andragogy in action. San Francisco, CA: Jossey Bass; 1984. [Google Scholar]
- Kreuter MW, Holt CL. How do people process health information? Applications in an age of individualized communication. Current Directions in Psychological Science. 2001;10(6):206–209. [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32(9):1–7. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of general internal medicine official journal of the Society for Research and Education in Primary Care Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders. 2009;114(1):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Antonuccio DO, Breckenridge JS, Teri L. The Coping with Depression Course: A psychoeducational intervention for unipolar depression. Eugene, OR: Castalia Publishing Co; 1984. [Google Scholar]
- Lewinsohn PM, Clarke GN, Rhode P, Hops H, Seeley JR. A course in coping: A cognitive-behavioral approach to the treatment of adolescent depression. In: Hibbs ED, Jensen PS, editors. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. Washington DC: American Psychological Association; 1996. pp. 109–135. [Google Scholar]
- Lipsey MW, Wilson DB. Practical Meta-Analysis. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20(5):561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Malik NM, Boris NW, Heller SS, Harden BJ, Squires J, Chazan-Cohen R, Kaczynski KJ. Risk for maternal depression and child aggression in Early Head Start families: A test of ecological models. Infant Mental Health Journal. 2007;28(2):171–191. doi: 10.1002/imhj.20128. [DOI] [PubMed] [Google Scholar]
- McLennan JD, Kotelchuck M, Cho H. Prevalence, persistence and correlates of depressive symptoms in a national sample of mothers of toddlers. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(11):1316–1323. doi: 10.1097/00004583-200111000-00012. [DOI] [PubMed] [Google Scholar]
- McMakin DL, Siegle GJ, Shirk SR. Positive Affect Stimulation and Sustainment (PASS) module for depressed mood: A preliminary investigation of treatment-related effects. Cognitive Therapy and Research. 2011;35(3):217–226. doi: 10.1007/s10608-010-9311-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuaid JR, Stein MB, Laffaye C, McCahill ME. Depression in a primary care clinic: The prevalence and impact of an unrecognized disorder. Journal of Affective Disorders. 1999;55:1–10. doi: 10.1016/s0165-0327(98)00191-8. [DOI] [PubMed] [Google Scholar]
- Milgrom J, Martin PR, Negri L. Treating postnatal depression. A psychological approach for health care practitioners. Chichester: Wiley; 1999. [Google Scholar]
- Milgrom J, Negri LM, Gemmill AW, McNeil M, Martin PR. A randomized controlled trial of psychological interventions for postnatal depression. British Journal of Clinical Psychology. 2005;44(4):529–542. doi: 10.1348/014466505X34200. [DOI] [PubMed] [Google Scholar]
- Milgrom J, Schembri C, Ericksen J, Ross J, Gemmill AW. Towards parenthood: An antenatal intervention to reduce depression, anxiety and parenting difficulties. Journal of Affective Disorders. 2011;130(3):385–394. doi: 10.1016/j.jad.2010.10.045. [DOI] [PubMed] [Google Scholar]
- Milgrom J, Danaher BG, Gemmill AW, Holt CJ, Seeley JR, Tyler MS, Ericksen J. Internet cognitive behavioral therapy for women with postnatal depression: A randomized controlled trial of MumMoodBooster. Journal of Medical Internet Research. 2016;18(3):e54. doi: 10.2196/jmir.4993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change. 2nd. New York: Guilford Press; 2002. [Google Scholar]
- Miranda J, Chung JY, Green BL, Krupnick J, Siddique J, Revicki DA, Belin T. Treating depression in predominantly low-income young minority women: A randomized controlled trial. JAMA: Journal of the American Medical Association. 2003;290(1):57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Burns MN, Schueller SM, Clarke G, Klinkman M. Behavioral intervention technologies: Evidence review and recommendations for future research in mental health. General Hospital Psychiatry. 2013;35(4):332–338. doi: 10.1016/j.genhosppsych.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. The Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- Natale-Pereira A, Enard KR, Nevarez L, Jones LA. The role of patient navigators in eliminating health disparities. Cancer. 2011;117(S15):3541–3550. doi: 10.1002/cncr.26264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natsuaki MN, Shaw DS, Neiderhiser JM, Ganiban JM, Harold GT, Reiss D, Leve LD. Raised by depressed parents: Is it an environmental risk? Clinical Child and Family Psychology Review. 2014;17(4):357–367. doi: 10.1007/s10567-014-0169-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health. Breaking Ground, Breaking Through: The Strategic Plan for Mood Disorders. (NIH Publication No 03–5121) Washington, DC: Government Printing Office; 2003. [Google Scholar]
- Nock MK, Kazdin AE. Randomized Controlled Trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology. 2005;73(5):872–879. doi: 10.1037/0022-006X.73.5.872. [DOI] [PubMed] [Google Scholar]
- O’Mahen HA, Richards DA, Woodford J, Wilkinson E, McGinley J, Taylor RS, Warren FC. Netmums: A phase II randomized controlled trial of a guided Internet behavioural activation treatment for postpartum depression. Psychological Medicine. 2014;44(08):1675–1689. doi: 10.1017/S0033291713002092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley PM, Johnston LD, Bachman JG, Schulenberg JE, Kumar R. How substance use differs among American secondary schools. Prevention Science. 2006;7(4):409–420. doi: 10.1007/s11121-006-0050-5. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. The smartphone difference. 2015 Apr; http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/
- Radke-Yarrow M, Kilmes-Dougan B. Parental depression and offspring disorders: A developmental perspective. In: Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington DC: American Psychological Association; 2002. pp. 155–173. [Google Scholar]
- Raghunathan TE, Solenberger PW, Van Hoewyk J. IVEware: imputation and variance estimation software. Ann Arbor, MI: Institute for Social Research. University of Michigan; 2002. [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons, Inc; 1987. [Google Scholar]
- Santini ZI, Koyanagi A, Tyrovolas S, Mason C, Haro JM. The association between social relationships and depression: A systematic review. Journal of Affective Disorders. 2015;175:53–65. doi: 10.1016/j.jad.2014.12.049. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT® 9.3 Procedures Guide. Cary, NC: SAS Institute Inc; 2011. [Google Scholar]
- Sauro J. A practical guide to the System Usability Scale: Background, benchmarks & best practices. Denver, CO: Measuring Usability LLC; 2011. [Google Scholar]
- Shaw DS, Dishion TJ, Connell A, Wilson MN, Gardner F. Maternal depression as a mediator of intervention in reducing early child problem behavior. Development and Psychopathology. 2009;21:417–439. doi: 10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeber LB, Seeley JR, Feil EG, Davis B, Sorensen E, Kosty DB, Lewinsohn PM. Development and pilot evaluation of an Internet-facilitated cognitive-behavioral intervention for maternal depression. Journal of Consulting and Clinical Psychology. 2012;80(5):739–749. doi: 10.1037/a0028820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spek V, Cuijpers PIM, Nyklícek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: A meta-analysis. Psychological Medicine. 2007;37(03):319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: The PHQ Primary Care Study. JAMA: Journal of the American Medical Association. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Titov N, Dear BF, McMillan D, Anderson T, Zou J, Sunderland M. Psychometric comparison of the PHQ-9 and BDI-II for measuring response during treatment of depression. Cognitive Behaviour Therapy. 2011;40(2):126–136. doi: 10.1080/16506073.2010.550059. [DOI] [PubMed] [Google Scholar]
- Verduyn C, Barrowclough C, Roberts J, Tarrier N, Harrington R. Maternal depression and child behaviour problems randomised placebo-controlled trial of a cognitive- behavioural group intervention. The British Journal of Psychiatry. 2003;183(4):342–348. doi: 10.1192/bjp.183.4.342. [DOI] [PubMed] [Google Scholar]
- Walitzer KS, Dermen KH, Connors GJ. Strategies for preparing clients for treatment A review. Behavior Modification. 1999;23(1):129–151. doi: 10.1177/0145445599231006. [DOI] [PubMed] [Google Scholar]
- Waller R, Gilbody S. Barriers to the uptake of computerized cognitive behavioural therapy: A systematic review of the quantitative and qualitative evidence. Psychological Medicine. 2009;39(05):705–712. doi: 10.1017/S0033291708004224. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- Wang Y, Dix T. Patterns of depressive parenting: Why they occur and their role in early developmental risk. Journal of Family Psychology. 2013;27(6):884. doi: 10.1037/a0034829. [DOI] [PubMed] [Google Scholar]
- Weissman M, Jensen P. What research suggests for depressed women with children. Journal of Clinical Psychiatry. 2002;63(7):641–647. doi: 10.4088/jcp.v63n0717. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, Cerda G. Remissions in maternal depression and child psychopathology: A STAR* D-child report. JAMA: Journal of the American Medical Association. 2006;295(12):1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- Wenzlaff RM, Bates DE. Unmasking a cognitive vulnerability to depression: How lapses in mental control reveal depressive thinking. Journal of Personality and Social Psychology. 1998;75:1559–1571. doi: 10.1037//0022-3514.75.6.1559. [DOI] [PubMed] [Google Scholar]