Abstract
Purpose. The aim of this study was to compare the effects of high-intensity interval training (INTERVAL) and moderate-intensity continuous training (CONTINUOUS) on aerobic capacity in cardiac patients. Methods. A meta-analysis identified by searching the PubMed, Cochrane Library, EMBASE, and Web of Science databases from inception through December 2016 compared the effects of INTERVAL and CONTINUOUS among cardiac patients. Results. Twenty-one studies involving 736 participants with cardiac diseases were included. Compared with CONTINUOUS, INTERVAL was associated with greater improvement in peak VO2 (mean difference 1.76 mL/kg/min, 95% confidence interval 1.06 to 2.46 mL/kg/min, p < 0.001) and VO2 at AT (mean difference 0.90 mL/kg/min, 95% confidence interval 0.0 to 1.72 mL/kg/min, p = 0.03). No significant difference between the INTERVAL and CONTINUOUS groups was observed in terms of peak heart rate, peak minute ventilation, VE/VCO2 slope and respiratory exchange ratio, body mass, systolic or diastolic blood pressure, triglyceride or low- or high-density lipoprotein cholesterol level, flow-mediated dilation, or left ventricular ejection fraction. Conclusions. This study showed that INTERVAL improves aerobic capacity more effectively than does CONTINUOUS in cardiac patients. Further studies with larger samples are needed to confirm our observations.
1. Introduction
Cardiovascular diseases (CVDs) remain the greatest cause of death worldwide. In 2008, more than 17 million people died due to CVDs, of whom 7.3 million died of heart attacks [1]. Interventions are urgently needed to address this worrying trend. CVDs are largely preventable, and cardiac rehabilitation is increasingly recognized as an important component of the continuum of care for patients with coronary artery disease (CAD) and chronic heart failure (CHF). It is included in Class 1 recommendations of the American Heart Association and the American College of Cardiology for the treatment of these patients [2, 3].
According to the World Health Organization, insufficient physical activity is the fourth leading risk factor for mortality, with 6% of deaths worldwide attributed to this factor [1]. Exercise training is essential for cardiac patients. It has an important role in improving endothelial function, which in turn enhances blood flow by causing vasodilatation and improving vasomotor function. Exercise training also contributes to the improvement of many other functions, such as the achievement of good glycemic control and insulin sensitivity, leading to weight loss; the improvement of blood pressure; and the correction of deranged lipid profiles [4, 5]. Proper exercise training is a cost-effective and well-established primary intervention that delays the onset of health burdens associated with various chronic diseases in many cases. The appropriate amount, frequency, and mode of exercise, however, remain unknown. Moreover, the optimum “dose” of exercise to obtain maximum cardiac benefits remains unclear.
Aerobic capacity has been found to be the single best parameter of cardiac function and all-cause death among known cases of CVDs [6]. It is measured directly as peak VO2. The improvement of the peak VO2 can improve aerobic capacity and promote cardiac rehabilitation. Moreover, reduction of the most common traditional risk factors for CVDs (e.g., hypertension, hyperlipidemia, and obesity) can decrease the occurrence of cardiovascular events. Research suggests that CAD and CHF are associated with impaired endothelial dysfunction, which is evaluated by flow-mediated dilation (FMD) and can be improved through physical exercise [7]. Thus, the identification of more effective exercise programs is needed to improve cardiovascular benefits in cardiac patients.
Moderate-intensity continuous training (CONTINUOUS), a traditional exercise prescription, usually involves walking or cycling for 30–60 min [to reach 40–80% peak oxygen uptake (peak VO2)] [8]. However, recent evidence from patients with CHF [9] and CAD [10] suggests that high-intensity interval training (INTERVAL) may be a better modality for the improvement of aerobic capacity. Although INTERVAL has no standard definition, it refers to repeated sessions of brief intermittent exercise, often performed with maximal effort or intensity (i.e., to achieve ≥90% peak VO2) [11]. This intensity can be achieved by a single effort lasting a few seconds to several minutes, or with multiple efforts separated by a few minutes of rest or low-intensity exercise. INTERVAL has been shown to have significant benefits, including improved aerobic capacity, endothelial function, and other cardiac functions, in patients with CAD and CHF [12, 13].
Although several reviews and meta-analyses of INTERVAL for CAD and CHF were published [14–16], no consensus has been reached about whether INTERVAL produces superior physical, clinical, and functional benefits compared to CONTINUOUS. We are also unware of any systematic reviews that have assessed the effect of INTERVAL among cardiac patients.
This systematic review was conducted to assess whether INTERVAL produces larger effect sizes for change in aerobic capacity [peak VO2, oxygen consumption at anaerobic threshold (VO2 at AT), VE/VCO2 slope, respiratory exchange ratio (RER), peak minute ventilation (peak VE), peak heart rate (PHR)], and physiological and clinical parameters compared with CONTINUOUS among patients with known cardiac disease (including CAD and CHF). The hypothesis of our study was that INTERVAL will have a greater effect on aerobic capacity given the superior improvement in mitochondrial function and cardiac contractility.
2. Methods
We conducted this study according to the methods of the Cochrane Handbook for Systematic Reviews of Interventions [17].
2.1. Search Strategy
The PubMed, Cochrane Library, EMBASE, and Web of Science electronic databases were searched to identify relevant clinical trials published between the earliest available date and December 2016 using the keywords “heart failure,” “coronary artery disease,” “high intensity interval training,” “interval exercise,” and “high-intensity interval exercise.” The reference lists of retrieved articles were also searched to identify other appropriate studies.
2.2. Inclusion and Exclusion Criteria
Only full-text English-language reports of clinical trials were considered for inclusion. In addition, we considered only studies that compared outcomes between an intervention group performing INTERVAL and a control group performing CONTINUOUS, with rhythmic aerobic exercise programs lasting at least 4 weeks. Eligible studies also reported on at least one cardiorespiratory exercise training outcome measure in patients with cardiac disease. Reviews, cases reports, editorial comment, communications, and reports without sufficient data were excluded in our meta-analysis.
2.3. Study Selection
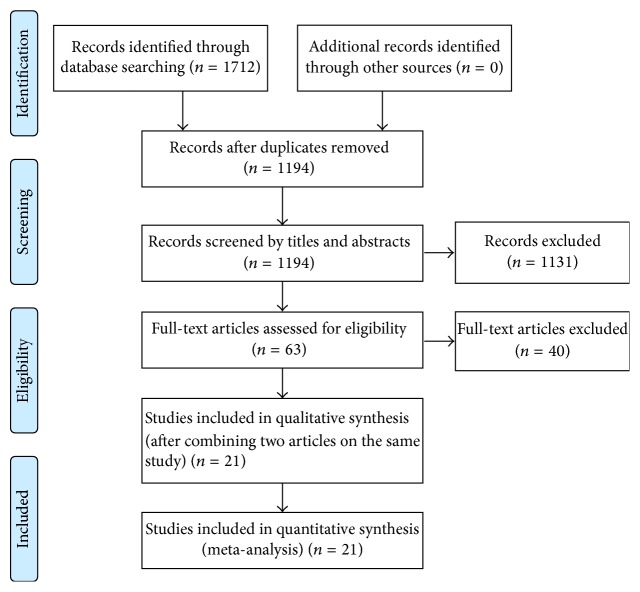
Figure 1 illustrates the flow of study selection. Two reviewers independently screened article titles and abstracts, excluding irrelevant studies. Full texts were then reviewed, and any study not fulfilling the inclusion criteria was excluded. Differences in the assessment of study eligibility were resolved by discussion.
Figure 1.
Flow chart of the study selection procedure.
2.4. Data Extraction and Management
One reviewer collected the data and the second reviewer rechecked it. Collected data included authors' names, year of publication, country in which the study was conducted, duration of the trial period, participant characteristics, intervention description, and outcomes assessed [peak VO2, VE/VCO2 slope, RER, peak VE, PHR, VO2 at AT, body mass, blood pressure, blood lipid parameters, FMD findings, and left ventricular ejection fraction (LVEF)]. Disagreements regarding the data collected were resolved by consensus.
2.5. Quality Assessment
The Cochrane collaboration's tool for assessing risk of bias was used for assessing the quality of randomized controlled trials (RCTs) and Physiotherapy Evidence Database (PEDro) scale nonrandomized controlled studies, respectively [17, 18].
2.6. Statistical Analysis
The Cochrane Collaboration software (RevMan 5.3; Cochrane Collaboration, Oxford, UK) was used for meta-analyses. We calculated effect sizes by subtracting preintervention from postintervention values. When only baseline and postintervention standard deviations (SDs) were reported, the following formula was used to obtain the missing change value [17]: SDchange = √[(SDpre)2 + (SDpost)2 − 2 × corr(pre, post) × SDpre × SDpost], where corr is the correlation coefficient calculated for each outcome using the formula of Conraads et al. [10]: corr = (SDpre2 + SDpost2 − SDchange2)/(2 × SDpre × SDpost). The heterogeneity of included trials was assessed using the I2 statistic and the chi-squared test for heterogeneity. We used a fixed-effects model for studies showing significant homogeneity (I2 < 50%) and a random-effects model for other studies. Results were considered significant when p < 0.05. To determine the influence of individual studies on the results obtained, we conducted a sensitivity analysis with one-by-one removal of studies. Publication bias was investigated using funnel plots and Egger's regression model.
3. Results
3.1. Characteristics of Identified Studies
The database search yielded 1712 titles. After the removal of duplicate records and the screening of abstracts and titles to assess relevance, 63 studies were selected for full-text review. After the exclusion of 40 articles which did not comply with the inclusion criteria, the final sample consisted of 23 articles [9, 10, 12, 13, 19–37] that reported on 21 studies. The characteristics of included studies are summarized in Table 1. All included studies were the randomized controlled trials. The 21 studies involved a total of 736 patients (81% male, 19% female) with cardiac disease (eleven studies examined patients with CAD and ten studies examined those with CHF). Four studies were conducted in Norway, three were conducted in Brazil, two each were conducted in the United States, Greece, and Canada, and one each was conducted in the Republic of Korea, Belgium, Netherlands, France, Taiwan, Italy, Spain, and United Kingdom. The duration of training programs ranged from 4 to 24 weeks, and the frequency of exercise training ranged from 2 to 5 days/week.
Table 1.
Characteristics of included studies.
| Study | Country | Disease | Patient number | Mean age, year | Mode | Exercise program | Exercise duration (weeks) | |||
|---|---|---|---|---|---|---|---|---|---|---|
| INTERVAL | CONTINUOUS | INTERVAL | CONTINUOUS | INTERVAL | CONTINUOUS | |||||
| Angadi et al., 2015 | US | CHF | 9 | 6 | 69 | 71.5 | TM | 3 d/wk, 4 × 4 mins @ 85%–90% of peak HR, 3 min recovery | 3 d/wk, 30 mins @ 70% of peak HR | 4 |
|
| ||||||||||
| Benda et al., 2015 | Netherlands | CHF | 10 | 10 | 63 | 64 | Cycling | 2 d/wk, 3.5 × 1 min @ 90%, of maximal workload, 10 periods | 2 d/wk, 30 min @ 60%–75% of maximal workload | 12 |
|
| ||||||||||
| Cardozo et al., 2015 | Brazil | CAD | 23 | 24 | 56 | 62 | TM | 3 d/wk, 2 mins @ 90% of peak HR 2 min recovery @ 60% peak HR | 3 d/wk, 30 mins @ 70%–75% of peak HR | 16 |
|
| ||||||||||
| Conraads et al., 2015 | Belgium | CAD | 85 | 89 | 57 | 59.9 | Cycling | 3 d/wk, 4 × 4 mins @ 90–95% of peak HR, 3 min recovery. 38 min total | 3 d/wk, 37 mins @ 70–75% of peak HR. 47 min total | 12 |
|
| ||||||||||
| Currie et al., 2013 | Canada | CAD | 11 | 11 | 62 | 68 | Cycling | 2 d/wk, 10 × 1 min @ 80%–104% PPO, 1 min recovery@10% PPO | 2 d/wk, 30–50 min @ 51%–65% PPO | 12 |
|
| ||||||||||
| Dimopoulos et al., 2006 | Greece | CHF | 10 | 14 | 59.2 | 61.5 | Cycling | 3 d/wk, 30 s@100% of WRp, 30 s rest, 40 min total | 3 d/wk, 40 mins @ 50% of WRp | 12 (36 sessions) |
|
| ||||||||||
| Freyssin et al., 2012 | France | CHF | 12 | 14 | 54 | 55 | Cycling | 5 d/wk, 12 × 30 s @ 50% (4 wks) + 80% (4 wks) of maximum power, 1 min recovery @ rest | 5 d/wk, 45 mins @ HRVT1 | 8 |
|
| ||||||||||
| Fu et al., 2013 | Taiwan | CHF | 14 | 13 | 67.5 | 66.3 | Cycling | 3 d/wk, 5 × 3 mins @ 80% of peak VO2 3 min recovery @ 40% peak VO2 |
3 d/wk, 60 mins @ 60% of peak VO2 | 12 |
|
| ||||||||||
| Iellamo et al., 2013 | Italy | CHF | 8 | 8 | 62.2 | 62.6 | TM | 2–5 d/wk, 2–4 × 4 mins @ 75%–80% of HHR 3 min recovery @ 45%–50% of HHR |
2–5 d/wk, 30–45 mins @ 45%–60% of HHR | 12 |
|
| ||||||||||
| Jaureguizar et al., 2016 | Spain | CAD | 36 | 36 | 58 | 58 | TM | (15–30) × 40 s @ the first (second) steep ramp test | 15–30 mins @ VT1 | 8 |
|
| ||||||||||
| Keteyian et al., 2014 | US | CAD | 15 | 13 | 60 | 58 | TM | 3 d/wk, 4 × 4 mins @ 80%–90% of HRR, 3 min recovery @ 60%–70% of HRR | 3 d/wk, 30 mins @ 60%–80% of HRR | 10 |
|
| ||||||||||
| Kim et al., 2015 | Republic of Korea | CAD | 14 | 14 | 57 | 60.2 | TM walking |
3 d/wk, 4 × 4 mins @ 85%–95% of HRR, 3 min recovery @ 450%–70% of HRR. 5 min total | 3 d/wk, 25 mins @ 70%–85% of HRR. 45 min total | 6 |
|
| ||||||||||
| Koufaki et al., 2014 | UK | CHF | 9 | 8 | 59.8 | 59.7 | Cycling | 3 d/wk, 2 × 10 min @ 100% of PPO, 5 min recovery @ 20%–30% of PPO | 3 d/wk, 1–4 months: 3 × (7–10) mins; 5-6 months: 40 mins; @ 40%–60% of peak VO2 | 24 |
|
| ||||||||||
| Madssen et al., 2014 | Norway | CAD | 15 | 21 | 55.5 | 60.5 | TM | 3 d/wk, 34 × 4 mins @ 85%–95% of peak HR, 3 min recovery @ 70% of peak HR | 3 d/wk, 46 mins @ 70% of peak HR | 12 |
|
| ||||||||||
| Moholdt et al., 2009 | Norway | CAD | 28 | 31 | 60.2 | 62 | TM | 5 d/wk, 4 × 4 mins @ 90% of peak HR, 3 min recovery @ 70% peak HR, 40 min total | 5 d/wk, 46 mins @ 70% of peak HR | 4 |
|
| ||||||||||
| Rocco et al., 2012∗ Prado et al., 2016∗ | Brazil | CAD | 17 | 20 | 56.5 | 62.5 | TM | 3 d/wk, 7 × 3 mins @ RCP, 7 × 3 min @ VAT. 42 min total | 3 d/wk, 50 mins @ VAT | 12 |
|
| ||||||||||
| Roditis et al., 2007 | Greece | CHF | 11 | 10 | 63 | 61 | Cycling | 3 d/wk, 30 × 30 s @ 100% of WRp, 40 min total | 3 d/wk, 40 mins @ 50% of WRp | 12 (36 sessions) |
|
| ||||||||||
| Rognmo et al., 2004∗ Amundsen et al., 2008∗ | Norway | CAD | 8 | 9 | 62.9 | 61.2 | TM walking |
3 d/wk, 4 × 4 mins @ 85%–95% of peak HR, 3 min recovery. 33 min total | 3 d/wk, 41 mins @ 50%–60% of peak VO2 | 10 |
|
| ||||||||||
| Ulbrich et al., 2016 | Brazil | CHF | 12 | 10 | 53.1 | 54 | TM | 3 d/wk, (4–6) × 3 mins @ 95% of peak HR, 3 min recovery @ 70% peak HR. 60 min total | 3 d/wk, 30 mins @ 75% of peak HR. 60 min total | 12 |
|
| ||||||||||
| Warburton et al., 2005 | Canada | CAD | 7 | 7 | 55 | 57 | TM | 2 d/wk, 2 mins @ 90% of VO2 reserve, 2 min recovery. 30 min total | 2 d/wk, 30 mins @ 65% of VO2 reserve | 16 |
|
| ||||||||||
| Wisløff et al., 2007 | Norway | CHF | 9 | 9 | 76.5 | 74.4 | TM | 3 d/wk, 4 mins @ 90%–95% of peak HR, 3 min recovery @ 50%–70% peak HR. 38 min total | 3 d/wk, 47 mins @ 70%–75% of peak HR | 12 |
INTERVAL, high-intensity interval training; CONTINUOUS, moderate-intensity continuous training; CHF, chronic heart failure; CAD, coronary artery disease; TM, treadmill; HR, heart rate; PPO, peak power output; HRR, heart rate reserve. WRp, 100% peak work rate. VAT, ventilatory anaerobic threshold. VO2, oxygen uptake. ∗means two articles on the same study.
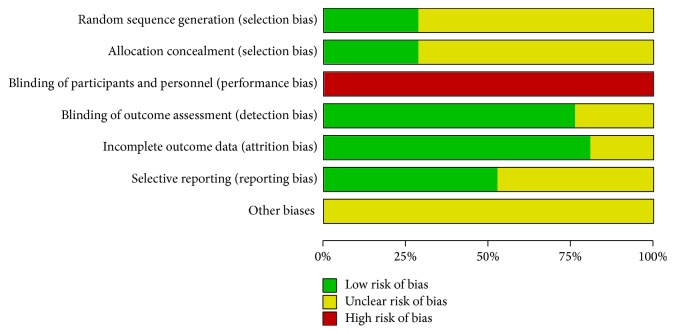
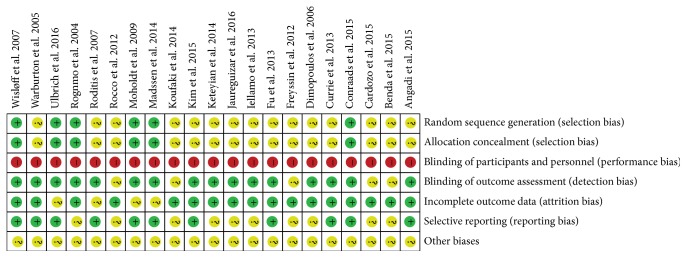
3.2. Risk of Bias
Figure 2 shows the risk of bias of the selected studies. Six (28.5%) studies described the methods used to generate and conceal allocation sequences. Participants were not blinded in any study. Outcome assessors were blinded to treatment allocation in sixteen (76.2%) studies. Seventeen (80.9%) studies had incomplete descriptions of outcomes, and eleven (52.3%) studies had low risks of selective reporting bias.
Figure 2.
Quality assessment of RCTs using Cochrane collaboration's tool for assessing risk of bias.
3.3. Effects of Interventions on the Cardiorespiratory Measurements
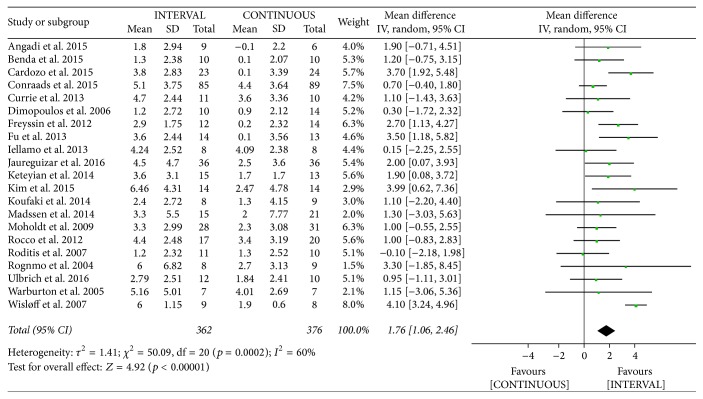
3.3.1. Peak VO2
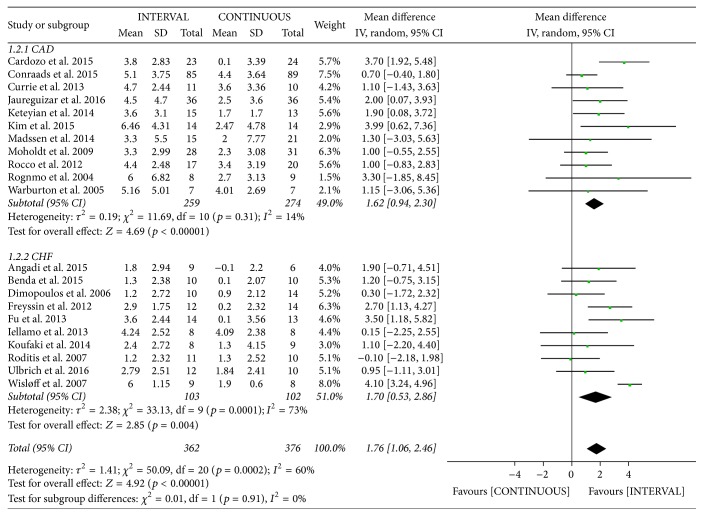
The authors of 21 studies [9, 10, 12, 13, 19–37] involving 738 patients reported on peak oxygen uptake following INTERVAL and CONTINUOUS. Peak VO2 improved by 1.76 mL/kg/min [95% confidence interval (CI) 1.06 to 2.46 mL/kg/min] among patients in the INTERVAL groups, which was greater than observed in the CONTINUOUS groups, based on a random-effects model (overall Z = 4.92, p < 0.001). However, this outcome showed significant heterogeneity (I2 = 60%, p <0.001; Figure 3).
Figure 3.
Meta-analysis of effects of INTERVAL on peak VO2.
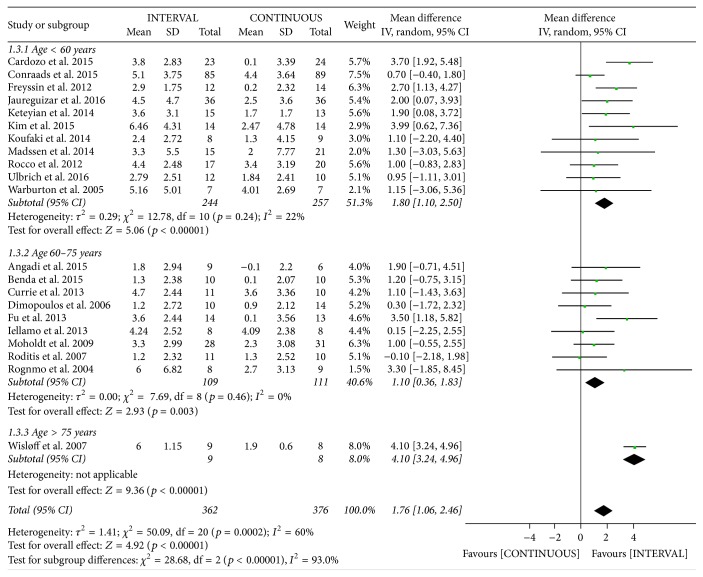
There was significant heterogeneity in the study outcomes. Therefore, subgroup analysis was performed based on the patient's mean age and disease types. INTERVAL led to significantly greater improvements in peak VO2 than did CONTINUOUS in patients aged < 60 years [mean difference (MD) 1.80 mL/kg/min, 95% CI 1.10 to 2.50 mL/kg/min, p < 0.001, I2 = 22%], those aged 61–75 years (MD 1.10 mL/kg/min, 95% CI 0.36 to 1.83 mL/kg/min, p = 0.003, I2 = 0%), and those aged > 75 years (included in only one study [12]; Figure 4). From disease types subgroup analyses, INTERVAL also led to significantly greater improvements in peak VO2 than did CONTINUOUS in patients with CAD (MD 1.62 mL/kg/min, 95% CI 0.94 to 2.30 mL/kg/min, p < 0.001, I2 = 14%) and those with CHF (MD 1.70 mL/kg/min, 95% CI 0.53 to 2.86 mL/kg/min, p = 0.004, I2 = 73%; Figure 5).
Figure 4.
Meta-analysis of the effects of INTERVAL on peak VO2 according to age.
Figure 5.
Meta-analysis of the effects of INTERVAL on peak VO2 according to disease types.
Sensitivity analysis did not change the statistical significance of the overall results. Exclusion of the study conducted by Wisløff et al. [12], which provided inferior evidence for the effect of INTERVAL on peak VO2, significantly improved homogeneity.
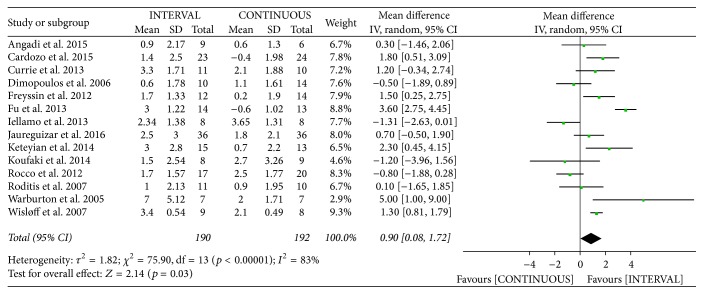
3.3.2. VO2 at AT
The authors of fourteen studies [12, 13, 20, 22–28, 30, 34, 35, 37] involving 382 patients reported on VO2 at AT following INTERVAL and CONTINUOUS. VO2 at AT improved by 0.90 mL/kg/min [95% CI 0.08 to 1.79 mL/kg/min] among patients in the INTERVAL groups, which was greater than observed in the CONTINUOUS groups, based on a random-effects model (overall Z = 2.14, p = 0.03). However, this outcome showed significant heterogeneity (I2 = 83%, p < 0.001; Figure 6).
Figure 6.
Meta-analysis of effects of INTERVAL on VO2 at AT.
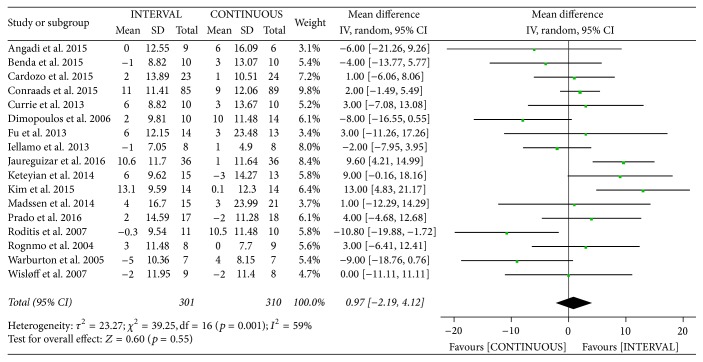
3.3.3. Peak Heart Rate
The authors of seventeen studies [10, 12, 13, 20–23, 25–29, 31, 33, 35–37] involving 611 patients reported on peak heart rate following INTERVAL and CONTINUOUS. A random-effects model revealed no significant difference between groups (MD 0.97 bpm, 95% CI −2.19 to 4.12 bpm, p = 0.55).
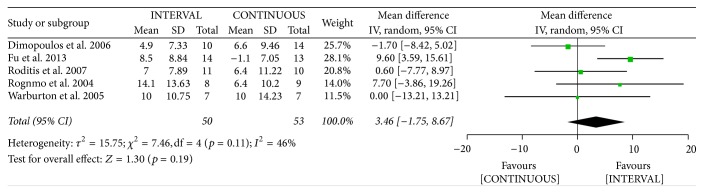
3.3.4. Peak Minute Ventilation
The authors of five studies [23, 25, 35–37] involving 103 patients reported on peak VE following INTERVAL and CONTINUOUS. A random-effects model revealed no significant difference between groups (MD 3.46 l/min, 95% CI −1.75 to 8.67 l/min, p = 0.19).
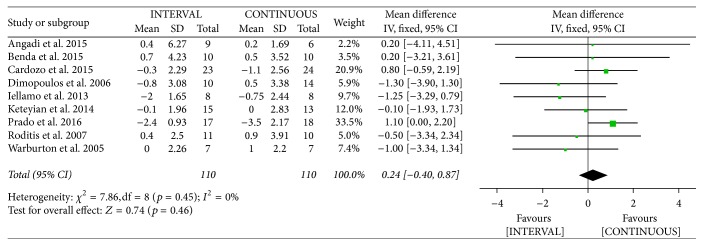
3.3.5. VE/VCO2 Slope
The authors of nine studies [20–23, 26, 28, 34, 35, 37] involving 220 patients reported on VE/VCO2 slope following INTERVAL and CONTINUOUS. A fixed-effects model revealed no significant difference between groups (MD 0.24, 95% CI −0.40 to 0.87, p = 0.46).
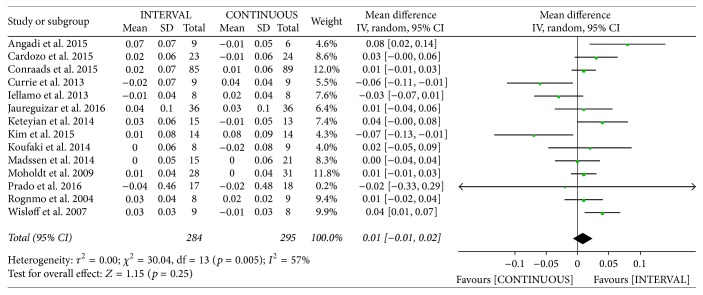
3.3.6. Respiratory Exchange Ratio
The authors of fourteen studies [10, 12, 13, 20, 22, 26–33, 36] involving 579 patients reported on RER following INTERVAL and CONTINUOUS. A random-effects model revealed no significant difference between groups (MD 0.01, 95% CI −0.01 to 0.02, p = 0.25).
3.4. Effects of Interventions on Physiological and Clinical Parameters
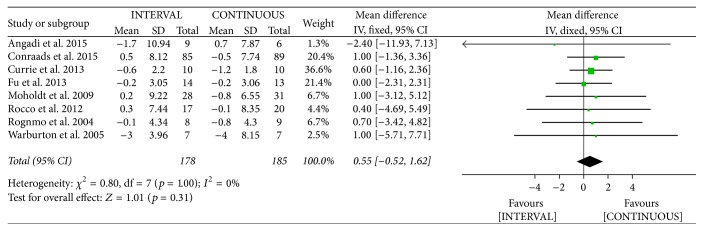
3.4.1. Body Mass
The authors of eight studies [10, 13, 20, 25, 32, 34, 36, 37] involving 363 patients reported decreased body mass following INTERVAL and CONTINUOUS. A fixed-effects model revealed no significant difference between groups (MD 0.55 kg, 95% CI −0.52 to 1.62 kg, p = 0.31).
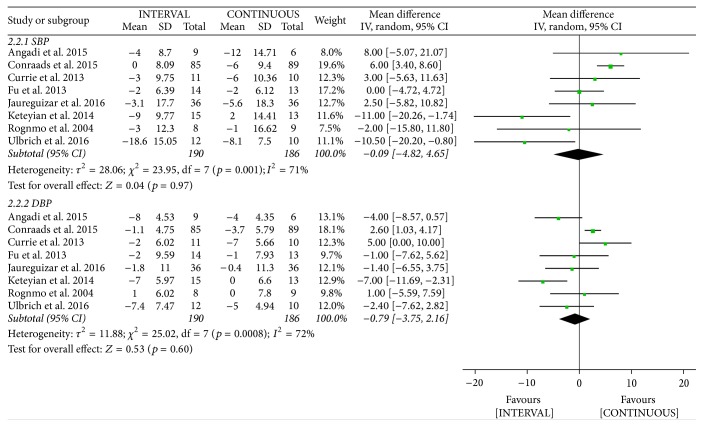
3.4.2. Blood Pressure
The authors of eight studies [9, 10, 13, 20, 25, 27, 28, 36] involving 376 patients reported on systolic blood pressure (SBP) and diastolic blood pressure (DBP) following INTERVAL and CONTINUOUS. A random-effects model revealed no significant difference between groups (SBP: MD −0.09 mmHg, 95% CI −4.82 to 4.65 mmHg, p = 0.97; DBP: MD −0.79 mmHg, 95% CI −3.75 to 2.16 mmHg, p = 0.60).
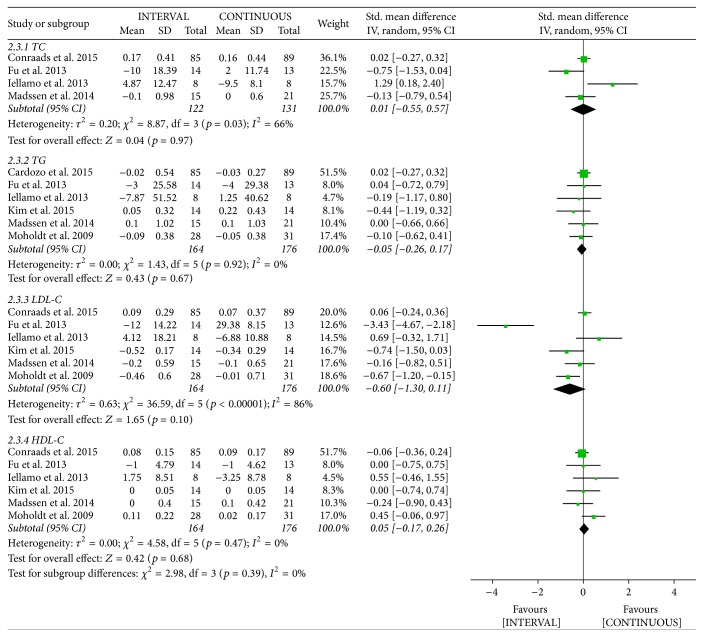
3.4.3. Blood Lipids
Data on high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglyceride (TG) levels following INTERVAL and CONTINUOUS were reported in six studies [22, 25, 26, 29, 31, 32] involving 340 patients. A random-effects model showed no significant difference between groups (TG: standardized mean difference (SMD) −0.05, 95% CI −0.26 to 0.17; LDL-C: SMD −0.6, 95% CI −1.3 to 0.11; HDL-C: SMD 0.05, 95% CI −0.17 to 0.26). The result of cholesterol was assessed in four studies [22, 25, 26, 31] involving 253 patients. A random-effects model revealed no significant difference between groups (SMD 0.01, 95% CI −0.55 to 0.57).
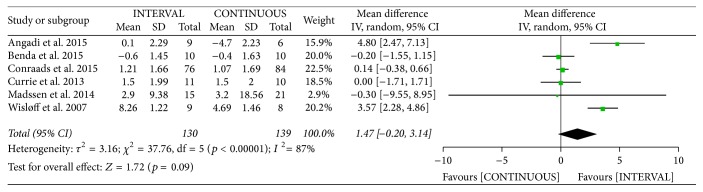
3.4.4. Flow-Mediated Dilation
The authors of six studies [10, 12, 13, 20, 21, 31] involving 269 patients reported on FMD following INTERVAL and CONTINUOUS. A random-effects model showed no significant difference between groups (MD 1.47%, 95% CI −0.20% to 3.14%, p = 0.09).
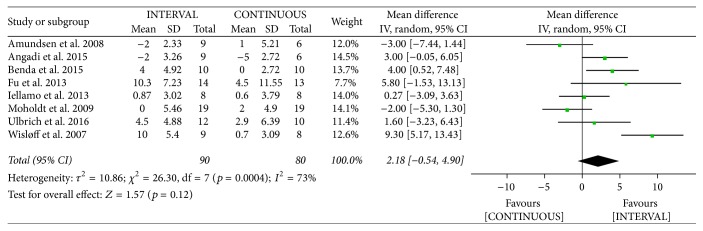
3.4.5. Left Ventricular Ejection Fraction
The authors of eight studies [9, 12, 19–21, 25, 26, 32] involving 170 patients reported increased LVEF following INTERVAL and CONTINUOUS. A random-effects model showed no significant difference between groups (MD 2.18%, 95% CI −0.54% to 4.90%, p = 0.12).
3.5. Publication Bias
Egger's regression analysis excluded relevant publication bias for peak VO2 (p = 0.14), and the funnel plot of these data was symmetrical.
4. Discussion
To our knowledge, most previous systematic reviews on this topic have focused on patients with specific diseases, such as CAD and CHF. One previous review [38] has examined whether INTERVAL is more effective than CONTINUOUS for improving peak VO2 and LVEF in CHF patients. However, this review focused only on CHF and only seven articles were included in the review. This systematic review examined the efficacy of INTERVAL as a part of cardiac rehabilitation in patients with cardiac disease (including CHF and CAD). Twenty-one studies involving 738 cardiac patients were included in the review. The main findings were that INTERVAL appears to be at least as effective as and in some cases more effective than CONTINUOUS, for the improvement of aerobic capacity, although we found evidence of heterogeneity among studies. Heterogeneous results for this outcome in the study conducted by Wisløff et al. [12] were due mainly to the inclusion of elderly patients.
4.1. Rationale and Potential Working Mechanisms of INTERVAL
Due to repeated alternation of high- and low-intensity exercise, INTERVAL's stimulation of the body fluctuates. The rationale is to accumulate more time in high-intensity zones compared to a continuous exercise where exhaustion would occur more prematurely and therefore to produce a stronger stimulus for cardiovascular and muscular adaptations [39, 40]. The mechanisms involved in the superiority of INTERVAL to CONTINUOUS have not been clearly elucidated. The potential mechanisms for the greater improvement in aerobic capacity achieved by INTERVAL include increased activation of peroxisome-proliferator activated receptor γ coactivator (PGC-1α), which improves mitochondrial function [12, 41, 42], and increased maximal rate of Ca2+ reuptake into the sarcoplasmic reticulum, which reduces skeletal muscle fatigue [12, 42]. The increase in PGC-1α to be strongly correlated with the improved VO2 peak (r = 0.72, p < 0.01) was found by Wisløff et al. [12], supporting the influence of mitochondrial function on exercise capacity.
INTERVAL has been demonstrated to activate p38 mitogen-activated protein kinase and 5′-adenosine monophosphate-activated protein kinase. Both of these exercise-responsive signaling kinases are implicated in direct phosphorylation and activation of PGC-1α. Increased nuclear abundance of PGC-1α following INTERVAL may coactivate transcription factors to increase mitochondrial gene transcription, ultimately resulting in accumulation of more mitochondrial proteins to drive mitochondrial biogenesis [43]. Mitochondrial biogenesis is essential to maintain the structural integrity of skeletal muscle. Mitochondrial function is associated with aerobic physical fitness and plays an important pathophysiological role in cardiac patients. Consequently, the major benefits of INTERVAL interventions include enhanced peripheral blood circulation [44], as well as increased skeletal muscle and functional capacity [45–47]. The improvement of peak VO2, a strong, independent predictor of all-cause and cardiovascular-specific mortality [48, 49], through INTERVAL is thus of clinical significance.
The magnitude of difference in the effects of INTERVAL and CONTINUOUS in terms of VE/VCO2 slope, RER, peak VE, PHR, body mass, blood pressure, blood lipids, FMD, and LVEF was small in the present analysis, which may be related to the examination of short-term outcomes in the included studies. Thus, more research is necessary to provide information on the long-term effects of INTERVAL.
A meta-analysis focused mainly on patients with CHF by Haykowsky et al. [38] showed INTERVAL is more effective than CONTINUOUS for improving peak VO2 (MD 2.14 mL/kg/min, 95% CI 0.66 to 3.63 mL/kg/min) but not the LVEF. Another systematic analysis by Smart et al. [50] that analyzed 446 CHF patients revealed that INTERVAL determined a significant increase in peak VO2 (MD 1.04 mL/kg/min, 95% CI 0.42 to 1.66 mL/kg/min) and VE/VCO2 slope (MD −1.35, 95% CI −2.15 to −0.55). A more recent meta-analysis including CAD patients by Pattyn et al. [51] reported higher increase in VO2 peak with INTERVAL (MD 1.6 mL/kg/min, 95% CI 0.8 to 3.02 mL/kg/min) but VE/VCO2 slope, VO2 at AT, and body mass. From our analysis, INTERVAL had similar effect results in improving peak VO2 in above meta-analysis. In addition, our systematic review included more evaluative indicators, such as PHR, peak VE, VE/VCO2 slope, RER, VO2 at AT, blood pressure, blood lipids, FMD, and LVEF, than did the previous meta-analysis.
Pooled estimates showed significant heterogeneity among studies included in this review. Important clinical and methodological differences may have affected the results obtained in the intervention and control groups. Some of these differences were in inclusion criteria and among participants, who were in different countries and of different ages.
4.2. Study Limitations
Our systematic review has some limitations. Few trials included in the study provided clear descriptions of the randomization and allocation of participants to treatments. Many of the studies failed to describe the blinding of assessors to treatment allocation, which raises the possibility of performance bias. In addition, although we examined publication bias because we searched only four electronic databases, we did not search for unpublished trials. Moreover, the review included only RCTs published in English. Consequently, our results may have been affected by publication bias. Several meta-analyses were affected by statistical heterogeneity, possibly due to differences in study methodologies and data collection techniques (e.g., wide ranges of variability in age, sex, and follow-up duration), which may have affected our findings. Finally, most of the studies had small samples, and no large-scale clinical RCT was included, which likely affected the objectivity and reliability of this meta-analysis and systematic review.
4.3. Conclusion
The current analysis indicated that INTERVAL can provide more benefits than CONTINUOUS in terms of improving peak VO2 and VO2 at AT in patients with cardiac disease. INTERVAL programs, which increase exercise capacity compared with traditional exercise, are thus preferable. Differences in the effects of INTERVAL and CONTINUOUS in terms of PHR, peak VE, VE/VCO2 slope, RER, body mass, blood pressure, blood lipids, FMD, and LVEF were small and may not be clinically meaningful. The results of this analysis should be interpreted with caution due to the small sample. Accordingly, more high-quality, large-sample, multicenter, long-term randomized interventional studies are needed to assess the effects of INTERVAL in cardiac patients.
Appendix
Figure 7.
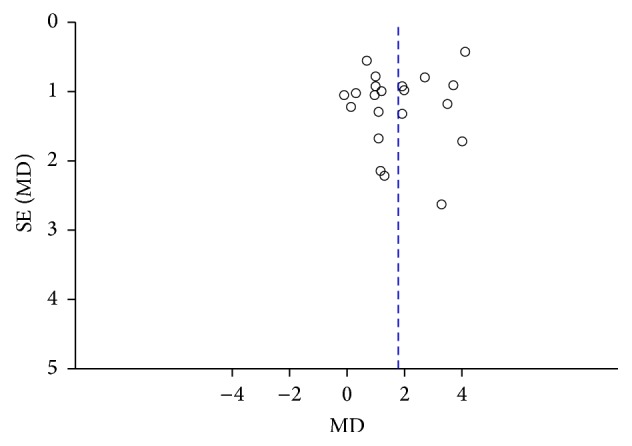
Funnel plot of publication bias.
Figure 8.
Risk of bias summary.
Figure 9.
Meta-analysis of effects of INTERVAL on PHR.
Figure 10.
Meta-analysis of effects of INTERVAL on peak VE.
Figure 11.
Meta-analysis of effects of INTERVAL on VE/VCO2 slope.
Figure 12.
Meta-analysis of effects of INTERVAL on RER.
Figure 13.
Meta-analysis of effects of INTERVAL on body mass.
Figure 14.
Meta-analysis of effects of INTERVAL on blood pressure.
Figure 15.
Meta-analysis of effects of INTERVAL on blood lipid.
Figure 16.
Meta-analysis of effects of INTERVAL on FMD.
Figure 17.
Meta-analysis of effects of INTERVAL on LVEF.
Competing Interests
The authors declare that there are no competing interests regarding the publication of this paper.
References
- 1.Mendis S., Puska P., Norrving B., editors. Global Atlas on Cardiovascular Disease Prevention and Control. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 2.Antman E. M., Anbe D. T., Armstrong P. W., et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction) Journal of the American College of Cardiology. 2004;44(3):671–719. doi: 10.1016/j.jacc.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Hunt S. A., Abraham W. T., Chin M. H., et al. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112(12):e154–e235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 4.Kelley G. A., Kelley K. S., Vu Tran Z. Aerobic exercise, lipids and lipoproteins in overweight and obese adults: a meta-analysis of randomized controlled trials. International Journal of Obesity. 2005;29(8):881–893. doi: 10.1038/sj.ijo.0802959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornelissen V. A., Fagard R. H. Effect of resistance training on resting blood pressure: a meta-analysis of randomized controlled trials. Journal of Hypertension. 2005;23(2):251–259. doi: 10.1097/00004872-200502000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Keteyian S. J., Brawner C. A., Savage P. D., et al. Peak aerobic capacity predicts prognosis in patients with coronary heart disease. American Heart Journal. 2008;156(2):292–300. doi: 10.1016/j.ahj.2008.03.017. [DOI] [PubMed] [Google Scholar]
- 7.Brunner H., Cockcroft J. R., Deanfield J., et al. Endothelial function and dysfunction. Part II: association with cardiovascular risk factors and diseases. A statement by the Working Group on Endothelins and Endothelial Factors of the European Society of Hypertension. Journal of Hypertension. 2005;23(2):233–246. doi: 10.1097/00004872-200502000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Fletcher G. F., Ades P. A., Kligfield P., et al. Exercise standards for testing and training: a scientific statement from the American heart association. Circulation. 2013;128(8):873–934. doi: 10.1161/cir.0b013e31829b5b44. [DOI] [PubMed] [Google Scholar]
- 9.Ulbrich A. Z., Angarten V. G., Schmitt Netto A., et al. Comparative effects of high intensity interval training versus moderate intensity continuous training on quality of life in patients with heart failure: study protocol for a randomized controlled trial. Clinical Trials and Regulatory Science in Cardiology. 2016;13:21–28. doi: 10.1016/j.ctrsc.2015.11.005. [DOI] [Google Scholar]
- 10.Conraads V. M., Pattyn N., De Maeyer C., et al. Aerobic interval training and continuous training equally improve aerobic exercise capacity in patients with coronary artery disease: the SAINTEX-CAD study. International Journal of Cardiology. 2015;179:203–210. doi: 10.1016/j.ijcard.2014.10.155. [DOI] [PubMed] [Google Scholar]
- 11.Gibala M. J., McGee S. L. Metabolic adaptations to short-term high-intensity interval training: a little pain for a lot of gain? Exercise and Sport Sciences Reviews. 2008;36(2):58–63. doi: 10.1097/jes.0b013e318168ec1f. [DOI] [PubMed] [Google Scholar]
- 12.Wisløff U., Støylen A., Loennechen J. P., et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115(24):3086–3094. doi: 10.1161/circulationaha.106.675041. [DOI] [PubMed] [Google Scholar]
- 13.Currie K. D., Dubberley J. B., McKelvie R. S., Macdonald M. J. Low-volume, high-intensity interval training in patients with CAD. Medicine and Science in Sports and Exercise. 2013;45(8):1436–1442. doi: 10.1249/MSS.0b013e31828bbbd4. [DOI] [PubMed] [Google Scholar]
- 14.Ito S., Mizoguchi T., Saeki T. Review of high-intensity interval training in cardiac rehabilitation. Internal Medicine. 2016;55(17):2329–2336. doi: 10.2169/internalmedicine.55.6068. [DOI] [PubMed] [Google Scholar]
- 15.Giallauria F., Smart N. A., Cittadini A., Vigorito C. Exercise training modalities in chronic heart failure: does high intensity aerobic interval training make the difference? Monaldi Archives for Chest Disease. 2016;86(1-2) doi: 10.4081/monaldi.2016.754. [DOI] [PubMed] [Google Scholar]
- 16.Elliott A. D., Rajopadhyaya K., Bentley D. J., Beltrame J. F., Aromataris E. C. Interval training versus continuous exercise in patients with coronary artery disease: a meta-analysis. Heart Lung and Circulation. 2015;24(2):149–157. doi: 10.1016/j.hlc.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 17.Higgins J. P. T., Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. http://handbook.cochrane.org/ [Google Scholar]
- 18.The George Institute for Global Health and the University of Sydney. Physiotherapy Evidence Database. 2012, http://www.pedro.org.au/english/downloads/pedro-scale/
- 19.Amundsen B. H., Rognmo Ø., Hatlen-Rebhan G., Slørdahl S. A. High-intensity aerobic exercise improves diastolic function in coronary artery disease. Scandinavian Cardiovascular Journal. 2008;42(2):110–117. doi: 10.1080/14017430701744477. [DOI] [PubMed] [Google Scholar]
- 20.Angadi S. S., Mookadam F., Lee C. D., Tucker W. J., Haykowsky M. J., Gaesser G. A. High-intensity interval training vs. moderate-intensity continuous exercise training in heart failure with preserved ejection fraction: a pilot study. Journal of Applied Physiology. 2015;119(6):753–758. doi: 10.1152/japplphysiol.00518.2014. [DOI] [PubMed] [Google Scholar]
- 21.Benda N. M., Seeger J. P., Stevens G. G., et al. Effects of high-intensity interval training versus continuous training on physical fitness, cardiovascular function and quality of life in heart failure patients. PLOS ONE. 2015;10(10) doi: 10.1371/journal.pone.0141256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cardozo G. G., Oliveira R. B., Farinatti P. T. V. Effects of high intensity interval versus moderate continuous training on markers of ventilatory and cardiac efficiency in coronary heart disease patients. The Scientific World Journal. 2015;2015:8. doi: 10.1155/2015/192479.192479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dimopoulos S., Anastasiou-Nana M., Sakellariou D., et al. Effects of exercise rehabilitation program on heart rate recovery in patients with chronic heart failure. European Journal of Cardiovascular Prevention & Rehabilitation. 2006;13(1):67–73. doi: 10.1097/00149831-200602000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Freyssin C., Verkindt C., Prieur F., Benaich P., Maunier S., Blanc P. Cardiac rehabilitation in chronic heart failure: effect of an 8-week, high-intensity interval training versus continuous training. Archives of Physical Medicine and Rehabilitation. 2012;93(8):1359–1364. doi: 10.1016/j.apmr.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Fu T.-C., Wang C.-H., Lin P.-S., et al. Aerobic interval training improves oxygen uptake efficiency by enhancing cerebral and muscular hemodynamics in patients with heart failure. International Journal of Cardiology. 2013;167(1):41–50. doi: 10.1016/j.ijcard.2011.11.086. [DOI] [PubMed] [Google Scholar]
- 26.Iellamo F., Manzi V., Caminiti G., et al. Matched dose interval and continuous exercise training induce similar cardiorespiratory and metabolic adaptations in patients with heart failure. International Journal of Cardiology. 2013;167(6):2561–2565. doi: 10.1016/j.ijcard.2012.06.057. [DOI] [PubMed] [Google Scholar]
- 27.Jaureguizar K. V., Vicente-Campos D., Bautista L. R., et al. Effect of high-intensity interval versus continuous exercise training on functional capacity and quality of life in patients with coronary artery disease: a randomized clinical trial. Journal of Cardiopulmonary Rehabilitation and Prevention. 2016;36(2):96–105. doi: 10.1097/hcr.0000000000000156. [DOI] [PubMed] [Google Scholar]
- 28.Keteyian S. J., Hibner B. A., Bronsteen K., et al. Greater improvement in cardiorespiratory fitness using higher-intensity interval training in the standard cardiac rehabilitation setting. Journal of Cardiopulmonary Rehabilitation and Prevention. 2014;34(2):98–105. doi: 10.1097/HCR.0000000000000049. [DOI] [PubMed] [Google Scholar]
- 29.Kim C., Choi H. E., Lim M. H. Effect of high interval training in acute myocardial infarction patients with drug-eluting stent. American Journal of Physical Medicine and Rehabilitation. 2015;94(10):879–886. doi: 10.1097/PHM.0000000000000290. [DOI] [PubMed] [Google Scholar]
- 30.Koufaki P., Mercer T. H., George K. P., Nolan J. Low-volume high-intensity interval training vs continuous aerobic cycling in patients with chronic heart failure: a pragmatic randomised clinical trial of feasibility and effectiveness. Journal of Rehabilitation Medicine. 2014;46(4):348–356. doi: 10.2340/16501977-1278. [DOI] [PubMed] [Google Scholar]
- 31.Madssen E., Moholdt T., Videm V., Wisløff U., Hegbom K., Wiseth R. Coronary atheroma regression and plaque characteristics assessed by grayscale and radiofrequency intravascular ultrasound after aerobic exercise. American Journal of Cardiology. 2014;114(10):1504–1511. doi: 10.1016/j.amjcard.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 32.Moholdt T. T., Amundsen B. H., Rustad L. A., et al. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: a randomized study of cardiovascular effects and quality of life. American Heart Journal. 2009;158(6):1031–1037. doi: 10.1016/j.ahj.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 33.Prado D., Rocco E., Silva A., et al. Effects of continuous vs interval exercise training on oxygen uptake efficiency slope in patients with coronary artery disease. Brazilian Journal of Medical and Biological Research. 2016;49(2) doi: 10.1590/1414-431x20154890.e4890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rocco E. A., Prado D. M. L., Silva A. G., et al. Effect of continuous and interval exercise training on the PETCO2 response during a graded exercise test in patients with coronary artery disease. Clinics. 2012;67(6):623–627. doi: 10.6061/clinics/2012(06)13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roditis P., Dimopoulos S., Sakellariou D., et al. The effects of exercise training on the kinetics of oxygen uptake in patients with chronic heart failure. European Journal of Cardiovascular Prevention & Rehabilitation. 2007;14(2):304–311. doi: 10.1097/hjr.0b013e32808621a3. [DOI] [PubMed] [Google Scholar]
- 36.Rognmo Ø., Hetland E., Helgerud J., Hoff J., Slørdahl S. A. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. European Journal of Cardiovascular Prevention and Rehabilitation. 2004;11(3):216–222. doi: 10.1097/01.hjr.0000131677.96762.0c. [DOI] [PubMed] [Google Scholar]
- 37.Warburton D. E. R., McKenzie D. C., Haykowsky M. J., et al. Effectiveness of high-intensity interval training for the rehabilitation of patients with coronary artery disease. American Journal of Cardiology. 2005;95(9):1080–1084. doi: 10.1016/j.amjcard.2004.12.063. [DOI] [PubMed] [Google Scholar]
- 38.Haykowsky M. J., Timmons M. P., Kruger C., McNeely M., Taylor D. A., Clark A. M. Meta-analysis of aerobic interval training on exercise capacity and systolic function in patients with heart failure and reduced ejection fractions. American Journal of Cardiology. 2013;111(10):1466–1469. doi: 10.1016/j.amjcard.2013.01.303. [DOI] [PubMed] [Google Scholar]
- 39.Wenger H. A., Bell G. J. The interactions of intensity, frequency and duration of exercise training in altering cardiorespiratory fitness. Sports Medicine. 1986;3(5):346–356. doi: 10.2165/00007256-198603050-00004. [DOI] [PubMed] [Google Scholar]
- 40.Wisløff U., Ellingsen Ø., Kemi O. J. High-intensity interval training to maximize cardiac benefits of exercise training? Exercise and Sport Sciences Reviews. 2009;37(3):139–146. doi: 10.1097/JES.0b013e3181aa65fc. [DOI] [PubMed] [Google Scholar]
- 41.Hoshino D., Yoshida Y., Kitaoka Y., Hatta H., Bonen A. High-intensity interval training increases intrinsic rates of mitochondrial fatty acid oxidation in rat red and white skeletal muscle. Applied Physiology, Nutrition, and Metabolism. 2013;38(3):326–333. doi: 10.1139/apnm-2012-0257. [DOI] [PubMed] [Google Scholar]
- 42.Tjønna A. E., Lee S. J., Rognmo Ø., et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: A Pilot Study. Circulation. 2008;118(4):346–354. doi: 10.1161/circulationaha.108.772822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gibala M. J., Little J. P., Macdonald M. J., Hawley J. A. Physiological adaptations to low-volume, high-intensity interval training in health and disease. Journal of Physiology. 2012;590(5):1077–1084. doi: 10.1113/jphysiol.2011.224725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leon A. S., Franklin B. A., Costa F., et al. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005;111(3):369–376. doi: 10.1161/01.cir.0000151788.08740.5c. [DOI] [PubMed] [Google Scholar]
- 45.Ades P. A., Green N. M., Coello C. E. Effects of exercise and cardiac rehabilitation on cardiovascular outcomes. Cardiology Clinics. 2003;21(3):435–448. doi: 10.1016/S0733-8651(03)00056-0. [DOI] [PubMed] [Google Scholar]
- 46.Lavie C. J., Thomas R. J., Squires R. W., Allison T. G., Milani R. V. Exercise training and cardiac rehabilitation in primary and secondary prevention of coronary heart disease. Mayo Clinic Proceedings. 2009;84(4):373–383. doi: 10.4065/84.4.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roveda F., Middlekauff H. R., Rondon M. U. P. B., et al. The effects of exercise training on sympathetic neural activation in advanced heart failure: a randomized controlled trial. Journal of the American College of Cardiology. 2003;42(5):854–860. doi: 10.1016/s0735-1097(03)00831-3. [DOI] [PubMed] [Google Scholar]
- 48.Guiraud T., Nigam A., Gremeaux V., Meyer P., Juneau M., Bosquet L. High-intensity interval training in cardiac rehabilitation. Sports Medicine. 2012;42(7):587–605. doi: 10.2165/11631910-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 49.Oldridge N. Exercise-based cardiac rehabilitation in patients with coronary heart disease: meta-analysis outcomes revisited. Future Cardiology. 2012;8(5):729–751. doi: 10.2217/fca.12.34. [DOI] [PubMed] [Google Scholar]
- 50.Smart N. A., Dieberg G., Giallauria F. Intermittent versus continuous exercise training in chronic heart failure: a meta-analysis. International Journal of Cardiology. 2013;166(2):352–358. doi: 10.1016/j.ijcard.2011.10.075. [DOI] [PubMed] [Google Scholar]
- 51.Pattyn N., Coeckelberghs E., Buys R., Cornelissen V. A., Vanhees L. Aerobic interval training vs. moderate continuous training in coronary artery disease patients: a systematic review and meta-analysis. Sports Medicine. 2014;44(5):687–700. doi: 10.1007/s40279-014-0158-x. [DOI] [PubMed] [Google Scholar]