Abstract
Many neurological disorders affect men and women differently regarding prevalence, progression, and severity. It is clear that many of these disorders may originate from defective signaling during fetal or perinatal brain development, which may affect males and females differently. Such sex-specific differences may originate from chromosomal or sex-hormone specific effects. This short review will focus on the estrogen receptor beta (ERβ) signaling during perinatal brain development and put it in the context of sex-specific differences in neurodevelopmental disorders. We will discuss ERβ’s recent discovery in directing DNA de-methylation to specific sites, of which one such site may bear consequences for the susceptibility to the neurological reading disorder dyslexia. We will also discuss how dysregulations in sex-hormone signaling, like those evoked by endocrine disruptive chemicals, may affect this and other neurodevelopmental disorders in a sex-specific manner through ERβ.
Keywords: estrogen, testosterone, dyslexia, aromatase, brain, neurodevelopment, sex-difference, hormone, BPA, epigenetics
1. Introduction
The development of the human brain requires a very fine-tuned orchestration of diverse spatial and temporal cues modulating a regulatory interconnected network. Even a slight miss-regulation may have neurodevelopmental consequences resulting in different outcomes, such as varying degrees of cognitive or psychiatric disorders. Many of these outcomes affect males and females differently, suggesting that chromosomal and sex-hormone effects may play important roles during development [1]. Males are more likely to develop autism spectrum disorders (ASD), attention deficit hyperactivity disorder (ADHD), schizophrenia, and dyslexia, whereas females are more likely to be diagnosed with depression and anxiety [2]. In addition, neurodegenerative diseases such as Parkinson’s disease (PD) and Alzheimer’s disease (AD) affect males and females differently, with differences in susceptibility, progression, and severity [3,4,5,6,7]. Although hereditary components exist, recent studies have pointed out, for example, much lower heritability towards ASD (about 50%) than previously considered [8,9]. This suggests that environmental factors may play a larger role than initially thought [2,10,11]. Sex-specific events, including altered sex-hormone signaling, during early brain development are emerging as key processes that can influence the susceptibility for these disorders. The time window of sex hormone actions is vital in view of the long-term effects on neuronal development. Broadly, two types of hormonal effects, organizational and activational, are believed to contribute to the etiology of neuronal disorders, of which organizational effects presumably ensue during early development. This is at a time when many of the neural structures are orchestrated and establish permanent changes in the brain. Since neurodevelopmental disorders typically persist with an early onset, any hormonal influence on the occurrence of these disorders is expected to be organizational [12]. These effects are paramount during sensitive periods representing the windows of time when a tissue can be formed [13]. Outside this sensitive period, usually postnatally, the effects of hormones are restricted in protecting the animal from disruptive effects. It implicates that even a slight dysregulation of hormone signaling during early development of the brain could manifest long lasting behavioral deficits, whereas such hormonal perturbations in the adult brain is not as devastating.
This short review aims at summarizing and discussing the advances achieved in understanding the signaling of the female sex-hormone estrogen during early brain development. We will focus on the estrogen receptor beta (ERβ) where its recently discovered effects on the epigenome, and sensitivity towards endocrine disruptive chemicals, may bring new concepts behind sex-hormone signaling during neurodevelopment. In particular, such knowledge may be of specific relevance in understanding the etiology of the several neurological disorders. One such is the reading disorder dyslexia, which we will use to illustrate how the recent advances in ERβ research may give clues to how genes, gender, and the environment may affect its susceptibility.
2. Chromosomal Effects: SRY
It is clear that sex hormones such as estrogen and androgens are needed for proper development and maturation of the brain [14,15,16]. In addition, sex chromosomal genes are also of importance. Several studies have shown that both the over- and under-dosage of sex chromosomes (e.g., copy number effects or escape from X-chromosome inactivation) is associated with neurological deficits regardless of gonadal phenotype [2]. This may be linked to over- or under-activation of genes involved in neurodevelopment located either at the X chromosome (e.g., NLGN4X, USP9X, Xlr3b) [17] or Y chromosome (e.g., Dby, Eif2s3y) [18]. In recent years, the Y chromosome-coded SRY gene (sex-determining region on the Y chromosome) has gained attention as a major factor in sex-specific brain development, where its dysegulation has been associated with neurological deficits (see Kopsida E. et al. for review [19]). SRY itself is responsible for the activation of genes important for male gonadal development and therefore for the production of gonadal testosterone, consequently leading to the masculinization of the brain and development of secondary male sex-characteristics [20,21,22,23]. Interestingly, SRY is also found in neurons, where it can directly regulate the transcription of the dopamine biosynthesis machinery (including TH, MAO-A, DBH, DDC, and D2R) and catecholamine-dependent functions in adult male dopaminergic neurons [18,24,25,26]. This may provide a genetic basis for the male preference for “fight-or-flight” sympathetic reactivity over female “tend-or-befriend” in response to stress [27]. In addition, PD and ADHD are more common in males than in females. It is therefore tempting to speculate that the increased prevalence in males could, to some extent, be explained by abnormal regulation or function of SRY on dopaminergic neurons. Since females lack SRY, other factors compensate, and one such factor may be estrogen. Nevertheless, although estrogen has ascribed neuroprotective effects [28], there are conflicting results on the neuroprotective benefit of estrogen administration to postmenopausal women with PD [29,30,31]. In this respect, a different developmental “high-wiring” of the female brain compared to the male brain could account for the lower prevalence of PD in females.
3. Estrogen Signaling during Brain Development
The female sex-hormone 17β-estradiol (E2), commonly referred as estrogen, is primarily produced in the ovaries and is responsible for female sexual development and regulation of the menstrual cycle. The steroidogenic pathway of E2 synthesis involves numerous enzymes to convert cholesterol to testosterone followed by aromatization of testosterone to E2 by the enzyme aromatase (gene name CYP19A1). In rodents, the fetal and perinatal brain is very well protected from circulating E2 (e.g., E2 coming from the mother or the placenta). This protection is achieved by the abundant plasma protein α-fetoprotein (AFP, a fetal analog of serum albumin), which binds and reduces the bioavailability of E2 [32]. In humans, AFP has low affinity for E2 [33] and its developmental function is less clear. Instead, the high-affinity steroid binding protein sex hormone-binding globulin (SHBG) may have a similar function to rodent AFP in humans and primates with the exception that it has higher affinity for androgens than E2, and may thus protect the female brain from masculinization by androgens [34,35]. Interestingly, in females the fetal ovaries do not produce E2 until after birth (in mice at day P7) [36], but they do produce androgens such as dihydrotestosterone (DHT), which is rapidly metabolized to the estrogenic steroid 5α-androstane-3β, 17β-diol (3βAdiol) [37]. In males, 3βAdiol is produced from DHT similarly in the immature testes, but at a later postnatal period (after P20 in rats) [38]. Since SHBG may bind a large portion of circulating androgens, such as escaping DHT, it may be the estrogenic effect of 3βAdiol that is the more relevant in the fetal developing brain, and as mentioned above, 3βAdiol is more abundant in the female perinatal circulation, suggesting sex-dimorphic effects of 3βAdiol during the perinatal period. In addition, the male and female brain is a major site for E2 production [39], and aromatase, a key enzyme in the last step of E2 synthesis, is widely expressed in the neurons of fetal and adult brain [40,41,42,43]. Knockout of aromatase in rodents does not give major neuronal abnormalities; however, these mice show lower sexual motivation, which can be rescued with exogenous E2 administration [44]. In fact, testosterone, and its receptor the androgen receptor, does not appear to be directly responsible for the perinatal masculinization of the brain and for male typical behavior. Instead, it is the local aromatase-dependent conversion of testosterone to E2 in the perinatal brain that accounts for these effects [45]. Local E2 biosynthesis in the fetal brain occurs late in gestation upon expression of brain aromatase [46,47]. Prior to this, 3βAdiol produced by the immature ovaries is the main circulating estrogen. The immature testes also produce 3βAdiol, but only at postnatal time points [38,48]. Female fetuses are therefore exposed to the estrogenic effect of 3βAdiol earlier than male fetuses.
The two main receptors for E2 are the nuclear receptors estrogen receptor alpha (ERα) and beta (ERβ). Both receptors appear to be highly expressed throughout the fetal mouse brain [36,49,50] until postnatal day P7, after which their levels sharply drop. This drop coincides with the initiation of E2 production by the ovaries [36,51]. ER localization in the mature brain is restricted to specific brain regions and cells: ERα predominantly localizes to the regions involved in arbitrating sexual behavior such as hypothalamus, whereas ERβ has a broader distribution in neurons of hippocampus, cerebral cortex, dorsal raphe, substantia nigra, and amygdala, as well as in microglia and oligodendrocytes [49,52]. ERα mRNA in the mouse brain is observed form day E16.5 [50] and ERβ mRNA from day E10.5, with a peak in protein levels at day E18.5 [53]. It is likely that varying levels of ERs may be expressed even earlier as embryonic stem cells, embryoid bodies, and neuronal progenitors have been reported to express both ER subtypes [54,55,56]. Knockout of ERα (ERα-/-) or ERβ (ERβ-/-) in mice show different behavioral and brain morphological effects. ERα-/- mice display decreased aggressiveness and aberrant sexual behavior linked to hypothalamic and pituitary defects [57,58], whereas ERβ-/- mice have increased aggressive behavior [59,60]. The ERβ-/- mice display a defective migration and layering of cortical neurons as well as impaired spatial learning [53,61,62] and increased anxiety behavior, which appears to be independent of E2 administration [62,63]. Such behaviors have not been shown for ERα-/- mice, suggesting that ERβ is the main ER isoform in regulating neuronal development associated with cognitive and affective behaviors [49]. In addition, fetal 3βAdiol preferentially binds ERβ over ERα [64], strengthening the importance of ERβ in the developing brain. However, its mechanistic understanding here is far from clear. In adult rodents, it has been shown that ERβ is expressed in serotonergic neurons of the dorsal raphe nucleus, where it mediates E2-dependent tryptophan hydroxylase (TPH) production [65,66], the rate-limiting enzyme for serotonin synthesis, and maintenance of serotonergic neurons [67]. ERβ is also the main ER isoform in dopaminergic (DA) neurons of the substantia nigra [68]. It is well established that E2 promotes neuroprotection of these DA neurons [69,70,71,72]. However, it is not clear if it is a direct effect of E2 on these neurons or if E2 exert its neuroprotective effect through oligodendrocytes, microglia, or astroglia. Interestingly, both oligodendrocytes and microglia express mainly ERβ, while astrocytes express ERα [73,74]. Future studies with cell-specific ER knockout models will bring knowledge to which cell type and which ER subtype is responsible for the neuroprotective effects of E2 in the adult brain, as well as the observed behavioral deficits linked to neurodevelopment.
4. A New Role for ERβ in Epigenetic Remodeling
Epigenetic remodeling events such as DNA methylation and histone modifications are crucial for regulating gene expression during embryonic development [75,76]. It is known that nuclear receptors can attract chromatin-remodeling coactivators with histone acetyltransferase (HAT) activities, promoting gene transcription [77]. DNA de-methylation can be achieved passively by inhibition of the DNA methylation maintaining enzyme DNA methyltransferase (DNMT) during DNA replication [78]. However, it can also be achieved by active DNA de-methylation through oxidation of methylated CpG (cytosine-guanine) marks on the DNA by ten-eleven translocation (TET) proteins and DNA dioxygenases [79]. The oxidized methylated cytosine at the CpG is then recognized by thymine DNA glycosylase (TDG) of the base excision repair system and replaced by an unmethylated cytosine [80,81]. Increased levels of oxidized methylated CpGs (the prerequisite for active DNA de-methylation) have been found in gene regulatory regions of neurons and pluripotent cells [82], coinciding with bivalent histone marks (H3K4m2/3 and H3K27m3) [83]. Active DNA de-methylation pathways have consequently been found to be working during embryonic development and differentiation [84,85]. Studies have shown that transcription factors may direct de novo DNA methylation at proximal regions [86,87,88]. However, the mechanism behind how DNA de-methylation is directed has been elusive. Several studies have shown that nuclear receptors may be involved in regulating DNA methylation [55,89,90,91,92,93,94]. With regard to neurodevelopmental sex-hormone signaling, it is particularly interesting that ERβ may have an important function in DNA de-methylation [55,93]. Recent studies have shown that ERα and ERβ can bind and direct TDG to gene regulatory regions [55,95], where a direct effect on DNA methylation of genes involved in embryonic development was shown for ERβ (not ERα) in mouse embryonic fibroblasts irrespective of ligand treatment [55]. Thus ERβ may function at different levels during the neurodevelopment: by directly promoting transcription of target genes in a ligand-dependent or -independent manner, or by ligand-independently directing DNA de-methylation machineries to different gene regulatory regions during early development. It is not known yet if the latter also takes place during later developmental and mature stages. However, these data put forward ERβ as a very important factor regulating embryonic development. Surprisingly, ERβ-/- mice do survive with relatively mild morphological defects [53,96], suggesting that compensatory mechanisms exist (e.g., through ERα) or that ERβ may exert its effects during short developmental windows. Such windows could be very sensitive to disruptions in endocrine homeostasis.
5. Endocrine Disruptors and Neurodevelopment
Endocrine disruptive chemicals (EDCs) are environmental compounds that have endocrine active properties and can modulate the function of steroid hormone receptors. Such modulations may either be agonistic or antagonistic depending on receptor type and dose. Two types of EDCs are bisphenol A (BPA) and diesters of 1,2-benzenedicarboxylic-acid (phthalates), which have received attention due to their vast use as plasticizers in common plastic products [97,98]. As discussed above, sex-hormone signaling is very important for neuronal development. Therefore, in utero and perinatal exposure to EDCs such as phthalates and BPA may cause imbalanced sex-hormone signaling that may affect neuronal development. Recent biomonitoring data show that exposure to EDCs has increased during the past decades [99]. This coincides with a remarkable increase in children with neurodevelopmental disorders attending child and adolescent psychiatric clinics and increase in ASD prevalence worldwide, even when correcting for new diagnostic practices and increased attention to the hallmarks of ASD [8,100]. BPA interfere with the estrogen signaling [101,102] and phthalates with the androgen and estrogen signaling [103]. Their exposure during development has been associated with neuronal and behavior disorders, as well as affecting the reproductive system [104,105,106,107,108]. Like many other EDCs, BPA has a non-monotonic dose response curve, giving rise to debates regarding the safe dose and its agonistic or antagonistic properties on the estrogen receptors [109]. What is clear so far is that developmental exposure to BPA in various in vivo models results in anxiety, lasting cognitive deficits, and behavioral abnormalities, and that noted findings can be associated with behavioral outcomes in BPA-exposed children (for systematic review see Ejaredar M. et al. [110]). Interestingly, several in vivo models have shown that BPA also has sexually dimorphic effects on brain functions [111,112,113,114,115,116,117] and epidemiological studies have also shown differences between BPA exposed boys and girls regarding neuropsychiatric outcomes [118,119,120]. Recently it was demonstrated that perinatal exposure of male rats to low, physiological levels of BPA altered their stress response through dysregulation of ERβ [121], and that this effect could be linked to ERβ’s role in DNA de-methylation [55,121]. It was shown that BPA was equally potent as the anti-estrogen ICI 182,780 in inhibiting ERβ’s recruitment to the gene regulatory region of Fkbp5, a gene involved in the negative feedback of glucocorticoid signaling and stress response, and that this resulted in increased DNA methylation and decreased Fkbp5 gene expression in an ERβ-dependent and sexually dimorphic manner [121]. In combination with the data discussed above, suggesting that ERβ may affect the epigenetic control of genes involved in embryonic development [55], dysregulation of ERβ by EDCs such as BPA may have neurodevelopmental consequences that deserve deeper investigation.
6. Sex Hormones and Dyslexia Susceptibility
Dyslexia is a neurodevelopmental disorder characterized by difficulties in reading and spelling, despite normal intelligence. Around 5% of children and adolescents suffer from dyslexia and it is more prevalent in boys than girls, especially when in combination with comorbidities such as ADHD [122,123]. This sex bias has been debated and some epidemiological studies have found that males are up to 4 times more likely to be diagnosed with dyslexia compared to females, whereas another study found no sex differences (for review see [124]). Clearly, more studies are warranted to accurately determine the sex difference, taking the environment and co-occurrence of neurodevelopmental and psychiatric disorders into account. Although there is no cure, defining the severity of dyslexia and treatment of possible concurrent mental disorders, and regular individual spelling and reading support in school, has been successful in minimizing the symptoms later in life [123]. Dyslexia has a heritable component associated with several candidate genes restricted to specific risk loci on different chromosomes [125,126]. However, an environmental component appears to exist, which remains virtually uncharacterized [122]. Two proposed candidate genes located on chromosome 15q21 that may bring clues to an environmental link to the susceptibility of dyslexia are CYP19A1 and DYX1C1 [127,128]. CYP19A1, encodes, as mentioned, the aromatase enzyme involved in conversion of testosterone to E2 and in sexual maturation of the brain [44,45]. A dysregulated aromatase gene could result in androgen production without conversion to E2 and thus the possibility for increased androgen exposure of the brain. Interestingly, high testosterone levels during the perinatal period has been proposed as a potential risk factor for learning disabilities and ADHD, and may impact on neuronal development [129,130]. This is consistent with observations that testosterone increases neural lateralization by promoting apoptosis in the right brain hemisphere while slowing development of the left hemisphere [129,131]. Although they are different neurological disorders, an altered hemispheric lateralization has been observed in both ADHD patients [132] and in dyslectic children [133]. It is tempting to speculate that an increased testosterone level in these individuals is a result of dysregulated local E2 production due to aberrant CYP19A1 expression. In this respect, male fetuses would be more affected since females produce the estrogenic 3βAdiol by the fetal ovaries, and would thus be more protected from loss of local E2 production.
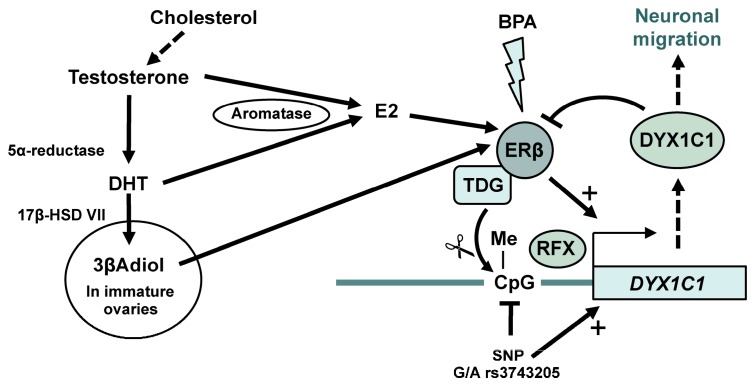
Postmortem human dyslectic brains show morphological brain abnormalities, such as cortical ectopias and heterotopias and that such abnormalities are more common in male dyslexic brains compared to dyslexic female or control brains [124,134,135,136,137]. These abnormalities are very similar to those found in rats with impaired prenatal DYX1C1 expression. However, sex differences were not analyzed in these studies [138,139,140]. Although not entirely characterized, the function of DYX1C1 appears to involve migration of cortical neurons [138,140,141] through modulating the assembly of ciliary structures [142]. Interestingly, E2 may be involved in DYX1C1 expression. As previously mentioned, E2 is produced through aromatization of testosterone by the proposed dyslexia candidate gene aromatase (CYP1A1) [127]. ERβ (not ERα) was found to associate with DYX1C1 cis-regulatory region to promote its transcription in the presence of E2 [143]. DYX1C1 protein itself then associates with ERs to promote their proteasomal degradation [144], implying that DYX1C1 is under a tight feedback regulation. The transcription of DYX1C1 also appears to be under tight epigenetic control, as methylation of a single CpG in its cis-regulatory region drastically reduced the ERβ-mediated transcription [143]. Interestingly, a single nucleotide polymorphism (SNP rs3743205 [G/A]) that was previously shown associated with dyslexia [139] lies within this CpG. Hence, this SNP impacts on the regulatory control of DYX1C1 [143]. As described above, ERβ can direct DNA de-methylation events to specific loci [55,121]. This could also be the case for ERβ’s association at the DYX1C1 regulatory region. Recent data show that ERβ deficiency in mouse embryonic stem cells correlates with decreased DYX1C1 expression as long as the cells remain in their pluripotent stage [55]. More differentiated cells had higher overall DNA methylation and either less DYX1C1 expression irrespective of ERβ status, or increased DYX1C1 expression in the absence of ERβ, depending on cell type. This implies that DYX1C1 expression is under a strict developmental and cell-specific control and can under some developmental windows be regulated by E2 through ERβ, including possibly by ERβ-mediated DNA de-methylation (Figure 1). Interestingly, a functional X-box motif is located at the same regulatory region to which ERβ binds upstream of the DYX1C1 transcription start site [145]. X-box motifs bind regulator function X transcription factors (RFX TFs) that are involved in regulation of, among other, ciliary genes [146] and reading of DNA methylation marks [147,148]. Although an interaction between ERβ and RFX TFs has not yet been shown, differential methylation of RFX1 and RFX2 binding sites was correlated to the absence or presence of ERβ [55], further strengthening the hypothesis that ERβ has an important regulatory role on DYX1C1. Combined, these data suggest that the tight temporal and spatial control of DYX1C1 expression is very sensitive to endocrine imbalances, such as those evoked by aromatase dysregulation and EDCs. As mentioned above, ovarian 3βAdiol may compensate for loss of E2 upon aromatase dysfunction in females, but obviously not in males. However, endocrine imbalances evoked by EDCs such as BPA may disrupt ERβ-mediated DNA de-methylation events [121] in both sexes, and may impact on DYX1C1 expression (Figure 1).
Figure 1.
A model of how 17β-estradiol (E2) and 3βAdiol production may affect ERβ regulation of dyslexia susceptibility 1 candidate gene 1 (DYX1C1) gene expression during neuronal development. E2 is produced locally through the conversion of androgens to E2 by the enzyme aromatase (CYP19A1 gene). In the normal situation, ERβ can promote DYX1C1 expression E2-dependetly, but probably also by recruiting Thymine-DNA Glycosylase (TDG) to the promoter to replace methylated cytosines by unmethylated ones, thereby promoting DYX1C1 transcription (+). A specific single nucleotide polymorphism (SNP rs3743205) may abolish this DNA methylation, loosing one important level of regulation. Indeed, the different levels of regulation of DYX1C1 (including feedback degradation of ERβ) suggest that this gene must be under a very tight regulatory control, which would be disrupted by the SNP. If the second dyslexia candidate gene, CYP19A1, encoding aromatase, is dysregulated, it should result in lower local production of E2, leading to androgen accumulation. The developing female brain may be less affected by the loss of aromatase since the immature ovaries produce the estrogenic 3βAdiol, which can preferentially bind and activate ERβ. Finally, the complex regulation of DYX1C1 may be very sensitive to hormonal imbalances such as those evoked by endocrine disruptive chemicals (EDCs) (e.g., bisphenol A, BPA) that can dysregulate ERβ’s transcriptional activity as well as ERβ-mediated DNA de-methylation events.
Of note, the genomic region 15q in which DYX1C1 and CYP19A1 are located also contains several susceptibility genes for ADHD, a comorbidity of dyslexia [149]. Although no clear support exists for DYX1C1 and CYP19A1 being risk genes for ADHD, abnormal perinatal testosterone levels has been suggested to be a risk factor of ADHD [129,130]. In fact, low CYP19A1 expression and abnormal testosterone levels have been observed in an ADHD rat model [150]. With this in mind, it may be speculated that abnormal perinatal testosterone levels (or defective testosterone aromatization to E2) could dysregulate perinatal DYX1C1 expression and be predisposal to ADHD in addition to dyslexia. Such effects may not necessarily be visible at genomic level. Future studies will give us clues to the regulations and functions of DYX1C1 and CYP19A1 in ADHD patients. Thus, neurodevelopmental effects of sex hormones, ERβ, and EDCs must be considered as important new factors that need to be taken into consideration when studying the etiology of, and sex differences in, dyslexia and its comorbidities.
7. Conclusions
Males and females are affected differently by different neurodevelopmental disorders such as dyslexia, ADHD, and ASD. Clues to understanding these disorders may lie within their observed sexually dimorphic effects. These dimorphic effects may be ascribed to chromosomal differences, such as defective SRY expression, or to differences in sex-hormone signaling. New studies have suggested that ERβ may play a more important role in mediating both E2- (or 3βAdiol) dependent and independent signaling during neuronal development, as well as having new functions in regulating temporal DNA methylation dynamics. Such effects of ERβ may be dysregulated by exposure to EDCs, which are increasingly more present in our environment and correlate with neurological deficits. With this in mind, the neurological reading disorder dyslexia may be a prime example of how genes, gender, and environment may contribute to its susceptibility. A genetic component is established, with candidate genes such as CYP19A1 and DYX1C1 among others; however, environmental and sex-specific factors are likely to be involved too. In particular, imbalanced sex-hormone signaling, for example through aberrant CYP19A1 expression itself or from environmentally present EDCs, could affect ERβ function and its regulation of DYX1C1 expression. The recent discovery that ERβ may modulate DNA de-methylation further strengthens the importance of ERβ and a balanced sex-hormone signaling during development. In addition, males may be more affected by sex-hormone imbalances than females since the circulating estrogenic compound 3βAdiol, produced by the immature ovaries, may likely compensate for perinatal E2 dysregulations and thereby protect the female brain. Thus, understanding the interplay between genes, gender and environment may hold great promises in understanding and developing sex specific treatments or prevention strategies for neurological disorders.
Acknowledgments
This work was supported by Emil and Wera Cornell’s Foundation.
Author Contributions
I.N. conceived, planned and performed experiments. I.N. and M.V. wrote the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Gillies G.E., McArthur S. Estrogen actions in the brain and the basis for differential action in men and women: A case for sex-specific medicines. Pharmacol. Rev. 2010;62:155–198. doi: 10.1124/pr.109.002071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loke H., Harley V., Lee J. Biological factors underlying sex differences in neurological disorders. Int. J. Biochem. Cell Biol. 2015;65:139–150. doi: 10.1016/j.biocel.2015.05.024. [DOI] [PubMed] [Google Scholar]
- 3.Andersen K., Launer L.J., Dewey M.E., Letenneur L., Ott A., Copeland J.R., Dartigues J.F., Kragh-Sorensen P., Baldereschi M., Brayne C., et al. Gender differences in the incidence of ad and vascular dementia: The eurodem studies. Eurodem incidence research group. Neurology. 1999;53:1992–1997. doi: 10.1212/WNL.53.9.1992. [DOI] [PubMed] [Google Scholar]
- 4.Baldereschi M., Di Carlo A., Rocca W.A., Vanni P., Maggi S., Perissinotto E., Grigoletto F., Amaducci L., Inzitari D. Parkinson’s disease and parkinsonism in a longitudinal study: Two-fold higher incidence in men. Ilsa working group. Italian longitudinal study on aging. Neurology. 2000;55:1358–1363. doi: 10.1212/WNL.55.9.1358. [DOI] [PubMed] [Google Scholar]
- 5.Rocca W.A., Amaducci L.A., Schoenberg B.S. Epidemiology of clinically diagnosed Alzheimer’s disease. Ann. Neurol. 1986;19:415–424. doi: 10.1002/ana.410190502. [DOI] [PubMed] [Google Scholar]
- 6.Ruitenberg A., Ott A., van Swieten J.C., Hofman A., Breteler M.M. Incidence of dementia: Does gender make a difference? Neurobiol. Aging. 2001;22:575–580. doi: 10.1016/S0197-4580(01)00231-7. [DOI] [PubMed] [Google Scholar]
- 7.Van Den Eeden S.K., Tanner C.M., Bernstein A.L., Fross R.D., Leimpeter A., Bloch D.A., Nelson L.M. Incidence of Parkinson’s disease: Variation by age, gender, and race/ethnicity. Am. J. Epidemiol. 2003;157:1015–1022. doi: 10.1093/aje/kwg068. [DOI] [PubMed] [Google Scholar]
- 8.Hallmayer J., Cleveland S., Torres A., Phillips J., Cohen B., Torigoe T., Miller J., Fedele A., Collins J., Smith K., et al. Genetic heritability and shared environmental factors among twin pairs with autism. Arch. Gen. Psychiatry. 2011;68:1095–1102. doi: 10.1001/archgenpsychiatry.2011.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sandin S., Lichtenstein P., Kuja-Halkola R., Larsson H., Hultman C.M., Reichenberg A. The familial risk of autism. JAMA. 2014;311:1770–1777. doi: 10.1001/jama.2014.4144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li R., Cui J., Shen Y. Brain sex matters: Estrogen in cognition and Alzheimer’s disease. Mol. Cell. Endocrinol. 2014;389:13–21. doi: 10.1016/j.mce.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yu L., Kuo Y., Cherng C.G., Chen H.H., Hsu C.H. Ovarian hormones do not attenuate methamphetamine-induced dopaminergic neurotoxicity in mice gonadectomized at 4 weeks postpartum. Neuroendocrinology. 2002;75:282–287. doi: 10.1159/000057337. [DOI] [PubMed] [Google Scholar]
- 12.Phoenix C.H., Goy R.W., Gerall A.A., Young W.C. Organizing action of prenatally administered testosterone propionate on the tissues mediating mating behavior in the female guinea pig. Endocrinology. 1959;65:369–382. doi: 10.1210/endo-65-3-369. [DOI] [PubMed] [Google Scholar]
- 13.Hines M. Neuroscience and intersex. Psychologist. 2004;17:455–458. [Google Scholar]
- 14.McEwen B. Estrogen actions throughout the brain. Recent Prog. Horm. Res. 2002;57:357–384. doi: 10.1210/rp.57.1.357. [DOI] [PubMed] [Google Scholar]
- 15.McEwen B.S., Alves S.E. Estrogen actions in the central nervous system. Endocr. Rev. 1999;20:279–307. doi: 10.1210/er.20.3.279. [DOI] [PubMed] [Google Scholar]
- 16.Pfaff D. Hormone-driven mechanisms in the central nervous system facilitate the analysis of mammalian behaviours. J. Endocrinol. 2005;184:447–453. doi: 10.1677/joe.1.05897. [DOI] [PubMed] [Google Scholar]
- 17.Schaafsma S.M., Pfaff D.W. Etiologies underlying sex differences in autism spectrum disorders. Front. Neuroendocrinol. 2014;35:255–271. doi: 10.1016/j.yfrne.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 18.Dewing P., Shi T., Horvath S., Vilain E. Sexually dimorphic gene expression in mouse brain precedes gonadal differentiation. Brain Res. Mol. Brain Res. 2003;118:82–90. doi: 10.1016/S0169-328X(03)00339-5. [DOI] [PubMed] [Google Scholar]
- 19.Kopsida E., Stergiakouli E., Lynn P.M., Wilkinson L.S., Davies W. The role of the y chromosome in brain function. Open Neuroendocrinol. J. 2009;2:20–30. doi: 10.2174/1876528900902010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hutchison J.B. Gender-specific steroid metabolism in neural differentiation. Cell. Mol. Neurobiol. 1997;17:603–626. doi: 10.1023/A:1022581902880. [DOI] [PubMed] [Google Scholar]
- 21.Koopman P., Munsterberg A., Capel B., Vivian N., Lovell-Badge R. Expression of a candidate sex-determining gene during mouse testis differentiation. Nature. 1990;348:450–452. doi: 10.1038/348450a0. [DOI] [PubMed] [Google Scholar]
- 22.Sinclair A.H., Berta P., Palmer M.S., Hawkins J.R., Griffiths B.L., Smith M.J., Foster J.W., Frischauf A.M., Lovell-Badge R., Goodfellow P.N. A gene from the human sex-determining region encodes a protein with homology to a conserved DNA-binding motif. Nature. 1990;346:240–244. doi: 10.1038/346240a0. [DOI] [PubMed] [Google Scholar]
- 23.Wilson C.A., Davies D.C. The control of sexual differentiation of the reproductive system and brain. Reproduction. 2007;133:331–359. doi: 10.1530/REP-06-0078. [DOI] [PubMed] [Google Scholar]
- 24.Czech D.P., Lee J., Correia J., Loke H., Moller E.K., Harley V.R. Transient neuroprotection by sry upregulation in dopamine cells following injury in males. Endocrinology. 2014;155:2602–2612. doi: 10.1210/en.2013-2158. [DOI] [PubMed] [Google Scholar]
- 25.Czech D.P., Lee J., Sim H., Parish C.L., Vilain E., Harley V.R. The human testis-determining factor sry localizes in midbrain dopamine neurons and regulates multiple components of catecholamine synthesis and metabolism. J. Neurochem. 2012;122:260–271. doi: 10.1111/j.1471-4159.2012.07782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dewing P., Chiang C.W., Sinchak K., Sim H., Fernagut P.O., Kelly S., Chesselet M.F., Micevych P.E., Albrecht K.H., Harley V.R., et al. Direct regulation of adult brain function by the male-specific factor sry. Curr. Biol. CB. 2006;16:415–420. doi: 10.1016/j.cub.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 27.Lee J., Harley V.R. The male fight-flight response: A result of sry regulation of catecholamines? BioEssays News Rev. Mol. Cell. Dev. Biol. 2012;34:454–457. doi: 10.1002/bies.201100159. [DOI] [PubMed] [Google Scholar]
- 28.Spence R.D., Voskuhl R.R. Neuroprotective effects of estrogens and androgens in cns inflammation and neurodegeneration. Front. Neuroendocrinol. 2012;33:105–115. doi: 10.1016/j.yfrne.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Benedetti M.D., Maraganore D.M., Bower J.H., McDonnell S.K., Peterson B.J., Ahlskog J.E., Schaid D.J., Rocca W.A. Hysterectomy, menopause, and estrogen use preceding Parkinson’s disease: An exploratory case-control study. Mov. Disord. 2001;16:830–837. doi: 10.1002/mds.1170. [DOI] [PubMed] [Google Scholar]
- 30.Currie L.J., Harrison M.B., Trugman J.M., Bennett J.P., Wooten G.F. Postmenopausal estrogen use affects risk for Parkinson disease. Arch. Neurol. 2004;61:886–888. doi: 10.1001/archneur.61.6.886. [DOI] [PubMed] [Google Scholar]
- 31.Tsang K.L., Ho S.L., Lo S.K. Estrogen improves motor disability in parkinsonian postmenopausal women with motor fluctuations. Neurology. 2000;54:2292–2298. doi: 10.1212/WNL.54.12.2292. [DOI] [PubMed] [Google Scholar]
- 32.Vannier B., Raynaud J.P. Effect of estrogen plasma binding on sexual differentiation of the rat fetus. Mol. Cell. Endocrinol. 1975;3:323–337. doi: 10.1016/0303-7207(75)90034-9. [DOI] [PubMed] [Google Scholar]
- 33.Swartz S.K., Soloff M.S. The lack of estrogen binding by human alpha-fetoprotein. J. Clin. Endocrinol. Metab. 1974;39:589–591. doi: 10.1210/jcem-39-3-589. [DOI] [PubMed] [Google Scholar]
- 34.Petra P.H., Woodcock K.T., Orr W.R., Nguyen D.K., Sui L.M. The sex steroid binding protein (SBP or SHBG) of human plasma: Identification of Tyr-57 and Met-107 in the steroid binding site. J. Steroid Biochem. Mol. Biol. 2000;75:139–145. doi: 10.1016/S0960-0760(00)00169-2. [DOI] [PubMed] [Google Scholar]
- 35.Wallen K. Hormonal influences on sexually differentiated behavior in nonhuman primates. Front. Neuroendocrinol. 2005;26:7–26. doi: 10.1016/j.yfrne.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 36.Sugiyama N., Andersson S., Lathe R., Fan X., Alonso-Magdalena P., Schwend T., Nalvarte I., Warner M., Gustafsson J.A. Spatiotemporal dynamics of the expression of estrogen receptors in the postnatal mouse brain. Mol. Psychiatry. 2009;14:223–232. doi: 10.1038/mp.2008.118. [DOI] [PubMed] [Google Scholar]
- 37.Handa R.J., Pak T.R., Kudwa A.E., Lund T.D., Hinds L. An alternate pathway for androgen regulation of brain function: Activation of estrogen receptor beta by the metabolite of dihydrotestosterone, 5alpha-androstane-3beta,17beta-diol. Horm. Behav. 2008;53:741–752. doi: 10.1016/j.yhbeh.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cochran R.C., Schuetz A.W., Ewing L.L. Age-related changes in conversion of 5 alpha-androstan-17 beta-ol-3-one to 5 alpha-androstane-3 alpha,17 beta-diol and 5 alpha-androstane-3 beta,17 beta-diol by rat testicular cells in vitro. J. Reprod. Fertil. 1979;57:143–147. doi: 10.1530/jrf.0.0570143. [DOI] [PubMed] [Google Scholar]
- 39.Do Rego J.L., Seong J.Y., Burel D., Leprince J., Luu-The V., Tsutsui K., Tonon M.C., Pelletier G., Vaudry H. Neurosteroid biosynthesis: Enzymatic pathways and neuroendocrine regulation by neurotransmitters and neuropeptides. Front. Neuroendocrinol. 2009;30:259–301. doi: 10.1016/j.yfrne.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 40.Abdelgadir S.E., Roselli C.E., Choate J.V., Resko J.A. Distribution of aromatase cytochrome P450 messenger ribonucleic acid in adult rhesus monkey brains. Biol. Reprod. 1997;57:772–777. doi: 10.1095/biolreprod57.4.772. [DOI] [PubMed] [Google Scholar]
- 41.Biegon A., Kim S.W., Alexoff D.L., Jayne M., Carter P., Hubbard B., King P., Logan J., Muench L., Pareto D., et al. Unique distribution of aromatase in the human brain: In vivo studies with pet and [n-methyl-11c]vorozole. Synapse. 2010;64:801–807. doi: 10.1002/syn.20791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boon W.C., Chow J.D., Simpson E.R. The multiple roles of estrogens and the enzyme aromatase. Prog. Brain Res. 2010;181:209–232. doi: 10.1016/S0079-6123(08)81012-6. [DOI] [PubMed] [Google Scholar]
- 43.Hojo Y., Higo S., Kawato S., Hatanaka Y., Ooishi Y., Murakami G., Ishii H., Komatsuzaki Y., Ogiue-Ikeda M., Mukai H., et al. Hippocampal synthesis of sex steroids and corticosteroids: Essential for modulation of synaptic plasticity. Front. Endocrinol. 2011;2:43. doi: 10.3389/fendo.2011.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bakker J., Honda S., Harada N., Balthazart J. The aromatase knock-out mouse provides new evidence that estradiol is required during development in the female for the expression of sociosexual behaviors in adulthood. J. Neurosci. 2002;22:9104–9112. doi: 10.1523/JNEUROSCI.22-20-09104.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu M.V., Manoli D.S., Fraser E.J., Coats J.K., Tollkuhn J., Honda S., Harada N., Shah N.M. Estrogen masculinizes neural pathways and sex-specific behaviors. Cell. 2009;139:61–72. doi: 10.1016/j.cell.2009.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.George F.W., Ojeda S.R. Changes in aromatase activity in the rat brain during embryonic, neonatal, and infantile development. Endocrinology. 1982;111:522–529. doi: 10.1210/endo-111-2-522. [DOI] [PubMed] [Google Scholar]
- 47.George F.W., Tobleman W.T., Milewich L., Wilson J.D. Aromatase activity in the developing rabbit brain. Endocrinology. 1978;102:86–91. doi: 10.1210/endo-102-1-86. [DOI] [PubMed] [Google Scholar]
- 48.Auchus R.J. The backdoor pathway to dihydrotestosterone. Trends Endocrinol. Metab. TEM. 2004;15:432–438. doi: 10.1016/S1043-2760(04)00214-0. [DOI] [PubMed] [Google Scholar]
- 49.Fan X., Xu H., Warner M., Gustafsson J.A. Erbeta in CNS: New roles in development and function. Prog. Brain Res. 2010;181:233–250. doi: 10.1016/S0079-6123(08)81013-8. [DOI] [PubMed] [Google Scholar]
- 50.Lemmen J.G., Broekhof J.L., Kuiper G.G., Gustafsson J.A., van der Saag P.T., van der Burg B. Expression of estrogen receptor alpha and beta during mouse embryogenesis. Mech. Dev. 1999;81:163–167. doi: 10.1016/S0925-4773(98)00223-8. [DOI] [PubMed] [Google Scholar]
- 51.Sugiyama N., Barros R.P., Warner M., Gustafsson J.A. Erbeta: Recent understanding of estrogen signaling. Trends Endocrinol. Metab. TEM. 2010;21:545–552. doi: 10.1016/j.tem.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 52.Walf A.A., Koonce C.J., Frye C.A. Adult female wildtype, but not oestrogen receptor beta knockout, mice have decreased depression-like behaviour during pro-oestrus and following administration of oestradiol or diarylpropionitrile. J. Psychopharmacol. 2009;23:442–450. doi: 10.1177/0269881108089598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang L., Andersson S., Warner M., Gustafsson J.A. Estrogen receptor (er)beta knockout mice reveal a role for erbeta in migration of cortical neurons in the developing brain. Proc. Natl. Acad. Sci. USA. 2003;100:703–708. doi: 10.1073/pnas.242735799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hong S.H., Nah H.Y., Lee Y.J., Lee J.W., Park J.H., Kim S.J., Lee J.B., Yoon H.S., Kim C.H. Expression of estrogen receptor-alpha and -beta, glucocorticoid receptor, and progesterone receptor genes in human embryonic stem cells and embryoid bodies. Mol. Cells. 2004;18:320–325. [PubMed] [Google Scholar]
- 55.Liu Y., Duong W., Krawczyk C., Bretschneider N., Borbely G., Varshney M., Zinser C., Schar P., Ruegg J. Oestrogen receptor beta regulates epigenetic patterns at specific genomic loci through interaction with thymine DNA glycosylase. Epigenet. Chromatin. 2016;9:7. doi: 10.1186/s13072-016-0055-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Martinez-Cerdeno V., Noctor S.C., Kriegstein A.R. Estradiol stimulates progenitor cell division in the ventricular and subventricular zones of the embryonic neocortex. Eur. J. Neurosci. 2006;24:3475–3488. doi: 10.1111/j.1460-9568.2006.05239.x. [DOI] [PubMed] [Google Scholar]
- 57.Ogawa S., Lubahn D.B., Korach K.S., Pfaff D.W. Behavioral effects of estrogen receptor gene disruption in male mice. Proc. Natl. Acad. Sci. USA. 1997;94:1476–1481. doi: 10.1073/pnas.94.4.1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kim H.J., Gieske M.C., Trudgen K.L., Hudgins-Spivey S., Kim B.G., Krust A., Chambon P., Jeong J.W., Blalock E., Ko C. Identification of estradiol/eralpha-regulated genes in the mouse pituitary. J. Endocrinol. 2011;210:309–321. doi: 10.1530/JOE-11-0098. [DOI] [PubMed] [Google Scholar]
- 59.Nomura M., Durbak L., Chan J., Smithies O., Gustafsson J.A., Korach K.S., Pfaff D.W., Ogawa S. Genotype/age interactions on aggressive behavior in gonadally intact estrogen receptor beta knockout (betaerko) male mice. Horm. Behav. 2002;41:288–296. doi: 10.1006/hbeh.2002.1773. [DOI] [PubMed] [Google Scholar]
- 60.Ogawa S., Chan J., Chester A.E., Gustafsson J.A., Korach K.S., Pfaff D.W. Survival of reproductive behaviors in estrogen receptor beta gene-deficient (betaerko) male and female mice. Proc. Natl. Acad. Sci. USA. 1999;96:12887–12892. doi: 10.1073/pnas.96.22.12887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu F., Day M., Muniz L.C., Bitran D., Arias R., Revilla-Sanchez R., Grauer S., Zhang G., Kelley C., Pulito V., et al. Activation of estrogen receptor-beta regulates hippocampal synaptic plasticity and improves memory. Nat. Neurosci. 2008;11:334–343. doi: 10.1038/nn2057. [DOI] [PubMed] [Google Scholar]
- 62.Rissman E.F., Heck A.L., Leonard J.E., Shupnik M.A., Gustafsson J.A. Disruption of estrogen receptor beta gene impairs spatial learning in female mice. Proc. Natl. Acad. Sci. USA. 2002;99:3996–4001. doi: 10.1073/pnas.012032699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Imwalle D.B., Gustafsson J.A., Rissman E.F. Lack of functional estrogen receptor beta influences anxiety behavior and serotonin content in female mice. Physiol. Behav. 2005;84:157–163. doi: 10.1016/j.physbeh.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 64.Kuiper G.G., Lemmen J.G., Carlsson B., Corton J.C., Safe S.H., van der Saag P.T., van der Burg B., Gustafsson J.A. Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor beta. Endocrinology. 1998;139:4252–4263. doi: 10.1210/endo.139.10.6216. [DOI] [PubMed] [Google Scholar]
- 65.Donner N., Handa R.J. Estrogen receptor beta regulates the expression of tryptophan-hydroxylase 2 mrna within serotonergic neurons of the rat dorsal raphe nuclei. Neuroscience. 2009;163:705–718. doi: 10.1016/j.neuroscience.2009.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gundlah C., Alves S.E., Clark J.A., Pai L.Y., Schaeffer J.M., Rohrer S.P. Estrogen receptor-beta regulates tryptophan hydroxylase-1 expression in the murine midbrain raphe. Biol. Psychiatry. 2005;57:938–942. doi: 10.1016/j.biopsych.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 67.Suzuki H., Barros R.P., Sugiyama N., Krishnan V., Yaden B.C., Kim H.J., Warner M., Gustafsson J.A. Involvement of estrogen receptor beta in maintenance of serotonergic neurons of the dorsal raphe. Mol. Psychiatry. 2013;18:674–680. doi: 10.1038/mp.2012.62. [DOI] [PubMed] [Google Scholar]
- 68.Shughrue P.J., Merchenthaler I. Distribution of estrogen receptor beta immunoreactivity in the rat central nervous system. J. Comp. Neurol. 2001;436:64–81. doi: 10.1002/cne.1054. [DOI] [PubMed] [Google Scholar]
- 69.Dluzen D., Horstink M. Estrogen as neuroprotectant of nigrostriatal dopaminergic system: Laboratory and clinical studies. Endocrine. 2003;21:67–75. doi: 10.1385/ENDO:21:1:67. [DOI] [PubMed] [Google Scholar]
- 70.Jourdain S., Morissette M., Morin N., Di Paolo T. Oestrogens prevent loss of dopamine transporter (DAT) and vesicular monoamine transporter (VMAT2) in substantia nigra of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mice. J. Neuroendocrinol. 2005;17:509–517. doi: 10.1111/j.1365-2826.2005.01337.x. [DOI] [PubMed] [Google Scholar]
- 71.Sawada H., Ibi M., Kihara T., Honda K., Nakamizo T., Kanki R., Nakanishi M., Sakka N., Akaike A., Shimohama S. Estradiol protects dopaminergic neurons in a MPP+Parkinson’s disease model. Neuropharmacology. 2002;42:1056–1064. doi: 10.1016/S0028-3908(02)00049-7. [DOI] [PubMed] [Google Scholar]
- 72.Shughrue P.J. Estrogen attenuates the MPTP-induced loss of dopamine neurons from the mouse snc despite a lack of estrogen receptors (eralpha and erbeta) Exp. Neurol. 2004;190:468–477. doi: 10.1016/j.expneurol.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 73.Kruijver F.P., Balesar R., Espila A.M., Unmehopa U.A., Swaab D.F. Estrogen receptor-alpha distribution in the human hypothalamus in relation to sex and endocrine status. J. Comp. Neurol. 2002;454:115–139. doi: 10.1002/cne.10416. [DOI] [PubMed] [Google Scholar]
- 74.Wu W.F., Tan X.J., Dai Y.B., Krishnan V., Warner M., Gustafsson J.A. Targeting estrogen receptor beta in microglia and T cells to treat experimental autoimmune encephalomyelitis. Proc. Natl. Acad. Sci. USA. 2013;110:3543–3548. doi: 10.1073/pnas.1300313110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bird A. DNA methylation patterns and epigenetic memory. Genes Dev. 2002;16:6–21. doi: 10.1101/gad.947102. [DOI] [PubMed] [Google Scholar]
- 76.Chen T., Dent S.Y. Chromatin modifiers and remodellers: Regulators of cellular differentiation. Nat. Rev. Genet. 2014;15:93–106. doi: 10.1038/nrg3607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Martens J.H., Rao N.A., Stunnenberg H.G. Genome-wide interplay of nuclear receptors with the epigenome. Biochim. Biophys. Acta. 2011;1812:818–823. doi: 10.1016/j.bbadis.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 78.Patra S.K., Patra A., Rizzi F., Ghosh T.C., Bettuzzi S. Demethylation of (cytosine-5-c-methyl) DNA and regulation of transcription in the epigenetic pathways of cancer development. Cancer Metastasis Rev. 2008;27:315–334. doi: 10.1007/s10555-008-9118-y. [DOI] [PubMed] [Google Scholar]
- 79.Guo J.U., Su Y., Zhong C., Ming G.L., Song H. Emerging roles of tet proteins and 5-hydroxymethylcytosines in active DNA demethylation and beyond. Cell Cycle. 2011;10:2662–2668. doi: 10.4161/cc.10.16.17093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jacobs A.L., Schar P. DNA glycosylases: In DNA repair and beyond. Chromosoma. 2012;121:1–20. doi: 10.1007/s00412-011-0347-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Maiti A., Drohat A.C. Thymine DNA glycosylase can rapidly excise 5-formylcytosine and 5-carboxylcytosine: Potential implications for active demethylation of cpg sites. J. Biol. Chem. 2011;286:35334–35338. doi: 10.1074/jbc.C111.284620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shen L., Zhang Y. 5-hydroxymethylcytosine: Generation, fate, and genomic distribution. Curr. Opin. Cell Biol. 2013;25:289–296. doi: 10.1016/j.ceb.2013.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gao F., Xia Y., Wang J., Luo H., Gao Z., Han X., Zhang J., Huang X., Yao Y., Lu H., et al. Integrated detection of both 5-mC and 5-hmC by high-throughput tag sequencing technology highlights methylation reprogramming of bivalent genes during cellular differentiation. Epigenetics Off. J. DNA Methylation Soc. 2013;8:421–430. doi: 10.4161/epi.24280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Coskun V., Tsoa R., Sun Y.E. Epigenetic regulation of stem cells differentiating along the neural lineage. Curr. Opin. Neurobiol. 2012;22:762–767. doi: 10.1016/j.conb.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Saitou M., Kagiwada S., Kurimoto K. Epigenetic reprogramming in mouse pre-implantation development and primordial germ cells. Development. 2012;139:15–31. doi: 10.1242/dev.050849. [DOI] [PubMed] [Google Scholar]
- 86.Feldmann A., Ivanek R., Murr R., Gaidatzis D., Burger L., Schubeler D. Transcription factor occupancy can mediate active turnover of DNA methylation at regulatory regions. PLoS Genet. 2013;9:e1003994. doi: 10.1371/journal.pgen.1003994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lienert F., Wirbelauer C., Som I., Dean A., Mohn F., Schubeler D. Identification of genetic elements that autonomously determine DNA methylation states. Nat. Genet. 2011;43:1091–1097. doi: 10.1038/ng.946. [DOI] [PubMed] [Google Scholar]
- 88.Stadler M.B., Murr R., Burger L., Ivanek R., Lienert F., Scholer A., van Nimwegen E., Wirbelauer C., Oakeley E.J., Gaidatzis D., et al. DNA-binding factors shape the mouse methylome at distal regulatory regions. Nature. 2011;480:490–495. doi: 10.1038/nature10716. [DOI] [PubMed] [Google Scholar]
- 89.Kangaspeska S., Stride B., Metivier R., Polycarpou-Schwarz M., Ibberson D., Carmouche R.P., Benes V., Gannon F., Reid G. Transient cyclical methylation of promoter DNA. Nature. 2008;452:112–115. doi: 10.1038/nature06640. [DOI] [PubMed] [Google Scholar]
- 90.Kim M.S., Kondo T., Takada I., Youn M.Y., Yamamoto Y., Takahashi S., Matsumoto T., Fujiyama S., Shirode Y., Yamaoka I., et al. DNA demethylation in hormone-induced transcriptional derepression. Nature. 2009;461:1007–1012. doi: 10.1038/nature08456. [DOI] [PubMed] [Google Scholar]
- 91.Marques M., Laflamme L., Gaudreau L. Estrogen receptor alpha can selectively repress dioxin receptor-mediated gene expression by targeting DNA methylation. Nucleic Acids Res. 2013;41:8094–8106. doi: 10.1093/nar/gkt595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Metivier R., Gallais R., Tiffoche C., Le Peron C., Jurkowska R.Z., Carmouche R.P., Ibberson D., Barath P., Demay F., Reid G., et al. Cyclical DNA methylation of a transcriptionally active promoter. Nature. 2008;452:45–50. doi: 10.1038/nature06544. [DOI] [PubMed] [Google Scholar]
- 93.Ruegg J., Cai W., Karimi M., Kiss N.B., Swedenborg E., Larsson C., Ekstrom T.J., Pongratz I. Epigenetic regulation of glucose transporter 4 by estrogen receptor beta. Mol. Endocrinol. 2011;25:2017–2028. doi: 10.1210/me.2011-1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Thomassin H., Flavin M., Espinas M.L., Grange T. Glucocorticoid-induced DNA demethylation and gene memory during development. EMBO J. 2001;20:1974–1983. doi: 10.1093/emboj/20.8.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chen D., Lucey M.J., Phoenix F., Lopez-Garcia J., Hart S.M., Losson R., Buluwela L., Coombes R.C., Chambon P., Schar P., et al. T:G mismatch-specific thymine-DNA glycosylase potentiates transcription of estrogen-regulated genes through direct interaction with estrogen receptor alpha. J. Biol. Chem. 2003;278:38586–38592. doi: 10.1074/jbc.M304286200. [DOI] [PubMed] [Google Scholar]
- 96.Dey P., Barros R.P., Warner M., Strom A., Gustafsson J.A. Insight into the mechanisms of action of estrogen receptor beta in the breast, prostate, colon, and CNS. J. Mol. Endocrinol. 2013;51:T61–T74. doi: 10.1530/JME-13-0150. [DOI] [PubMed] [Google Scholar]
- 97.Calafat A.M., Ye X., Wong L.Y., Reidy J.A., Needham L.L. Exposure of the U.S. Population to bisphenol a and 4-tertiary-octylphenol: 2003–2004. Environ. Health Perspect. 2008;116:39–44. doi: 10.1289/ehp.10753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dodson R.E., Nishioka M., Standley L.J., Perovich L.J., Brody J.G., Rudel R.A. Endocrine disruptors and asthma-associated chemicals in consumer products. Environ. Health Perspect. 2012;120:935–943. doi: 10.1289/ehp.1104052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bergman A., Heindel J.J., Kasten T., Kidd K.A., Jobling S., Neira M., Zoeller R.T., Becher G., Bjerregaard P., Bornman R., et al. The impact of endocrine disruption: A consensus statement on the state of the science. Environ. Health Perspect. 2013;121:A104–A106. doi: 10.1289/ehp.1205448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rossignol D.A., Genuis S.J., Frye R.E. Environmental toxicants and autism spectrum disorders: A systematic review. Transl. Psychiatry. 2014;4:e360. doi: 10.1038/tp.2014.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chevrier J., Gunier R.B., Bradman A., Holland N.T., Calafat A.M., Eskenazi B., Harley K.G. Maternal urinary bisphenol a during pregnancy and maternal and neonatal thyroid function in the chamacos study. Environ. Health Perspect. 2013;121:138–144. doi: 10.1289/ehp.1205092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Xu X.B., He Y., Song C., Ke X., Fan S.J., Peng W.J., Tan R., Kawata M., Matsuda K., Pan B.X., et al. Bisphenol a regulates the estrogen receptor alpha signaling in developing hippocampus of male rats through estrogen receptor. Hippocampus. 2014;24:1570–1580. doi: 10.1002/hipo.22336. [DOI] [PubMed] [Google Scholar]
- 103.Furr J.R., Lambright C.S., Wilson V.S., Foster P.M., Gray L.E., Jr. A short-term in vivo screen using fetal testosterone production, a key event in the phthalate adverse outcome pathway, to predict disruption of sexual differentiation. Toxicol. Sci. Off. J. Soc. Toxicol. 2014;140:403–424. doi: 10.1093/toxsci/kfu081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Betz A., Jayatilaka S., Joshi J., Ramanan S., Debartolo D., Pylypiw H., Franke E. Chronic exposure to benzyl butyl phthalate (BBP) alters social interaction and fear conditioning in male adult rats: Alterations in amygdalar MeCP2, ERK1/2 and eralpha. Neuro Endocrinol. Lett. 2013;34:347–358. [PubMed] [Google Scholar]
- 105.Ji K., Hong S., Kho Y., Choi K. Effects of bisphenol s exposure on endocrine functions and reproduction of zebrafish. Environ. Sci. Technol. 2013;47:8793–8800. doi: 10.1021/es400329t. [DOI] [PubMed] [Google Scholar]
- 106.Li X.J., Jiang L., Chen L., Chen H.S., Li X. Neurotoxicity of dibutyl phthalate in brain development following perinatal exposure: A study in rats. Environ. Toxicol. Pharmacol. 2013;36:392–402. doi: 10.1016/j.etap.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 107.Masutomi N., Shibutani M., Takagi H., Uneyama C., Takahashi N., Hirose M. Impact of dietary exposure to methoxychlor, genistein, or diisononyl phthalate during the perinatal period on the development of the rat endocrine/reproductive systems in later life. Toxicology. 2003;192:149–170. doi: 10.1016/S0300-483X(03)00269-5. [DOI] [PubMed] [Google Scholar]
- 108.Patisaul H.B., Polston E.K. Influence of endocrine active compounds on the developing rodent brain. Brain Res. Rev. 2008;57:352–362. doi: 10.1016/j.brainresrev.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 109.Vandenberg L.N., Colborn T., Hayes T.B., Heindel J.J., Jacobs D.R., Jr., Lee D.H., Shioda T., Soto A.M., vom Saal F.S., Welshons W.V., et al. Hormones and endocrine-disrupting chemicals: Low-dose effects and nonmonotonic dose responses. Endocr. Rev. 2012;33:378–455. doi: 10.1210/er.2011-1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ejaredar M., Lee Y., Roberts D.J., Sauve R., Dewey D. Bisphenol a exposure and children’s behavior: A systematic review. J. Expo. Sci. Environ. Epidemiol. 2017;27:175–183. doi: 10.1038/jes.2016.8. [DOI] [PubMed] [Google Scholar]
- 111.Cao J., Joyner L., Mickens J.A., Leyrer S.M., Patisaul H.B. Sex-specific ESR2 mRNA expression in the rat hypothalamus and amygdala is altered by neonatal bisphenol a exposure. Reproduction. 2014;147:537–554. doi: 10.1530/REP-13-0501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cao J., Rebuli M.E., Rogers J., Todd K.L., Leyrer S.M., Ferguson S.A., Patisaul H.B. Prenatal bisphenol a exposure alters sex-specific estrogen receptor expression in the neonatal rat hypothalamus and amygdala. Toxicol. Sci. Off. J. Soc. Toxicol. 2013;133:157–173. doi: 10.1093/toxsci/kft035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chen F., Zhou L., Bai Y., Zhou R., Chen L. Sex differences in the adult HPA axis and affective behaviors are altered by perinatal exposure to a low dose of bisphenol A. Brain Res. 2014;1571:12–24. doi: 10.1016/j.brainres.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 114.Gioiosa L., Parmigiani S., Vom Saal F.S., Palanza P. The effects of bisphenol a on emotional behavior depend upon the timing of exposure, age and gender in mice. Horm. Behav. 2013;63:598–605. doi: 10.1016/j.yhbeh.2013.02.016. [DOI] [PubMed] [Google Scholar]
- 115.Jasarevic E., Williams S.A., Vandas G.M., Ellersieck M.R., Liao C., Kannan K., Roberts R.M., Geary D.C., Rosenfeld C.S. Sex and dose-dependent effects of developmental exposure to bisphenol a on anxiety and spatial learning in deer mice (peromyscus maniculatus bairdii) offspring. Horm. Behav. 2013;63:180–189. doi: 10.1016/j.yhbeh.2012.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wolstenholme J.T., Rissman E.F., Connelly J.J. The role of bisphenol a in shaping the brain, epigenome and behavior. Horm. Behav. 2011;59:296–305. doi: 10.1016/j.yhbeh.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Xu X., Dong F., Yang Y., Wang Y., Wang R., Shen X. Sex-specific effects of long-term exposure to bisphenol-A on anxiety- and depression-like behaviors in adult mice. Chemosphere. 2015;120:258–266. doi: 10.1016/j.chemosphere.2014.07.021. [DOI] [PubMed] [Google Scholar]
- 118.Braun J.M., Kalkbrenner A.E., Calafat A.M., Yolton K., Ye X., Dietrich K.N., Lanphear B.P. Impact of early-life bisphenol a exposure on behavior and executive function in children. Pediatrics. 2011;128:873–882. doi: 10.1542/peds.2011-1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Evans S.F., Kobrosly R.W., Barrett E.S., Thurston S.W., Calafat A.M., Weiss B., Stahlhut R., Yolton K., Swan S.H. Prenatal bisphenol a exposure and maternally reported behavior in boys and girls. Neurotoxicology. 2014;45:91–99. doi: 10.1016/j.neuro.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Harley K.G., Gunier R.B., Kogut K., Johnson C., Bradman A., Calafat A.M., Eskenazi B. Prenatal and early childhood bisphenol a concentrations and behavior in school-aged children. Environ. Res. 2013;126:43–50. doi: 10.1016/j.envres.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kitraki E., Nalvarte I., Alavian-Ghavanini A., Ruegg J. Developmental exposure to bisphenol A alters expression and DNA methylation of Fkbp5, an important regulator of the stress response. Mol. Cell. Endocrinol. 2015;417:191–199. doi: 10.1016/j.mce.2015.09.028. [DOI] [PubMed] [Google Scholar]
- 122.Peterson R.L., Pennington B.F. Developmental dyslexia. Lancet. 2012;379:1997–2007. doi: 10.1016/S0140-6736(12)60198-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Schulte-Korne G. The prevention, diagnosis, and treatment of dyslexia. Deutsch. Arzteblatt Int. 2010;107:718–726. doi: 10.3238/arztebl.2010.0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lambe E.K. Dyslexia, gender, and brain imaging. Neuropsychologia. 1999;37:521–536. doi: 10.1016/S0028-3932(98)00146-8. [DOI] [PubMed] [Google Scholar]
- 125.Fisher S.E., DeFries J.C. Developmental dyslexia: Genetic dissection of a complex cognitive trait. Nat. Rev. Neurosci. 2002;3:767–780. doi: 10.1038/nrn936. [DOI] [PubMed] [Google Scholar]
- 126.McGrath L.M., Smith S.D., Pennington B.F. Breakthroughs in the search for dyslexia candidate genes. Trends Mol. Med. 2006;12:333–341. doi: 10.1016/j.molmed.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 127.Anthoni H., Sucheston L.E., Lewis B.A., Tapia-Paez I., Fan X., Zucchelli M., Taipale M., Stein C.M., Hokkanen M.E., Castren E., et al. The aromatase gene CYP19A1: Several genetic and functional lines of evidence supporting a role in reading, speech and language. Behav. Genet. 2012;42:509–527. doi: 10.1007/s10519-012-9532-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ylisaukko-Oja T., Peyrard-Janvid M., Lindgren C.M., Rehnstrom K., Vanhala R., Peltonen L., Jarvela I., Kere J. Family-based association study of DYX1C1 variants in autism. Eur. J. Hum. Genet. EJHG. 2005;13:127–130. doi: 10.1038/sj.ejhg.5201272. [DOI] [PubMed] [Google Scholar]
- 129.Geschwind N., Galaburda A.M. Cerebral lateralization. Biological mechanisms, associations, and pathology: I. A hypothesis and a program for research. Arch. Neurol. 1985;42:428–459. doi: 10.1001/archneur.1985.04060050026008. [DOI] [PubMed] [Google Scholar]
- 130.Morris J.A., Jordan C.L., Breedlove S.M. Sexual differentiation of the vertebrate nervous system. Nat. Neurosci. 2004;7:1034–1039. doi: 10.1038/nn1325. [DOI] [PubMed] [Google Scholar]
- 131.Waddell J., McCarthy M.M. Sexual differentiation of the brain and ADHD: What is a sex difference in prevalence telling us? Curr. Top. Behav. Neurosci. 2012;9:341–360. doi: 10.1007/7854_2010_114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Seidman L.J., Valera E.M., Makris N. Structural brain imaging of attention-deficit/hyperactivity disorder. Biol. Psychiatry. 2005;57:1263–1272. doi: 10.1016/j.biopsych.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 133.Zhao J., Thiebaut de Schotten M., Altarelli I., Dubois J., Ramus F. Altered hemispheric lateralization of white matter pathways in developmental dyslexia: Evidence from spherical deconvolution tractography. Cortex J. Devoted Study Nerv. Syst. Behav. 2016;76:51–62. doi: 10.1016/j.cortex.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 134.Chang B.S., Katzir T., Liu T., Corriveau K., Barzillai M., Apse K.A., Bodell A., Hackney D., Alsop D., Wong S.T., et al. A structural basis for reading fluency: White matter defects in a genetic brain malformation. Neurology. 2007;69:2146–2154. doi: 10.1212/01.wnl.0000286365.41070.54. [DOI] [PubMed] [Google Scholar]
- 135.Chang B.S., Ly J., Appignani B., Bodell A., Apse K.A., Ravenscroft R.S., Sheen V.L., Doherty M.J., Hackney D.B., O’Connor M., et al. Reading impairment in the neuronal migration disorder of periventricular nodular heterotopia. Neurology. 2005;64:799–803. doi: 10.1212/01.WNL.0000152874.57180.AF. [DOI] [PubMed] [Google Scholar]
- 136.Galaburda A.M., Sherman G.F., Rosen G.D., Aboitiz F., Geschwind N. Developmental dyslexia: Four consecutive patients with cortical anomalies. Ann. Neurol. 1985;18:222–233. doi: 10.1002/ana.410180210. [DOI] [PubMed] [Google Scholar]
- 137.Humphreys P., Kaufmann W.E., Galaburda A.M. Developmental dyslexia in women: Neuropathological findings in three patients. Ann. Neurol. 1990;28:727–738. doi: 10.1002/ana.410280602. [DOI] [PubMed] [Google Scholar]
- 138.Wang Y., Paramasivam M., Thomas A., Bai J., Kaminen-Ahola N., Kere J., Voskuil J., Rosen G.D., Galaburda A.M., Loturco J.J. Dyx1c1 functions in neuronal migration in developing neocortex. Neuroscience. 2006;143:515–522. doi: 10.1016/j.neuroscience.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 139.Tapia-Paez I., Tammimies K., Massinen S., Roy A.L., Kere J. The complex of TFII-I, PARP1, and SFPQ proteins regulates the DYX1C1 gene implicated in neuronal migration and dyslexia. FASEB J. 2008;22:3001–3009. doi: 10.1096/fj.07-104455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rosen G.D., Bai J., Wang Y., Fiondella C.G., Threlkeld S.W., LoTurco J.J., Galaburda A.M. Disruption of neuronal migration by rnai of DYX1C1 results in neocortical and hippocampal malformations. Cereb. Cortex. 2007;17:2562–2572. doi: 10.1093/cercor/bhl162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Threlkeld S.W., McClure M.M., Bai J., Wang Y., LoTurco J.J., Rosen G.D., Fitch R.H. Developmental disruptions and behavioral impairments in rats following in utero rnai of DYX1C1. Brain Res. Bull. 2007;71:508–514. doi: 10.1016/j.brainresbull.2006.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Tarkar A., Loges N.T., Slagle C.E., Francis R., Dougherty G.W., Tamayo J.V., Shook B., Cantino M., Schwartz D., Jahnke C., et al. DYX1C1 is required for axonemal dynein assembly and ciliary motility. Nat. Genet. 2013;45:995–1003. doi: 10.1038/ng.2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Tammimies K., Tapia-Paez I., Ruegg J., Rosin G., Kere J., Gustafsson J.A., Nalvarte I. The rs3743205 snp is important for the regulation of the dyslexia candidate gene DYX1C1 by estrogen receptor beta and DNA methylation. Mol. Endocrinol. 2012;26:619–629. doi: 10.1210/me.2011-1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Massinen S., Tammimies K., Tapia-Paez I., Matsson H., Hokkanen M.E., Soderberg O., Landegren U., Castren E., Gustafsson J.A., Treuter E., et al. Functional interaction of DYX1C1 with estrogen receptors suggests involvement of hormonal pathways in dyslexia. Hum. Mol. Genet. 2009;18:2802–2812. doi: 10.1093/hmg/ddp215. [DOI] [PubMed] [Google Scholar]
- 145.Tammimies K., Bieder A., Lauter G., Sugiaman-Trapman D., Torchet R., Hokkanen M.E., Burghoorn J., Castren E., Kere J., Tapia-Paez I., et al. Ciliary dyslexia candidate genes DYX1C1 and DCDC2 are regulated by regulatory factor (RFX) transcription factors through x-box promoter motifs. FASEB J. 2016;30:3578–3587. doi: 10.1096/fj.201500124RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Choksi S.P., Lauter G., Swoboda P., Roy S. Switching on cilia: Transcriptional networks regulating ciliogenesis. Development. 2014;141:1427–1441. doi: 10.1242/dev.074666. [DOI] [PubMed] [Google Scholar]
- 147.Spruijt C.G., Gnerlich F., Smits A.H., Pfaffeneder T., Jansen P.W., Bauer C., Munzel M., Wagner M., Muller M., Khan F., et al. Dynamic readers for 5-(hydroxy)methylcytosine and its oxidized derivatives. Cell. 2013;152:1146–1159. doi: 10.1016/j.cell.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 148.Zhao M., Sun Y., Gao F., Wu X., Tang J., Yin H., Luo Y., Richardson B., Lu Q. Epigenetics and sle: Rfx1 downregulation causes cd11a and cd70 overexpression by altering epigenetic modifications in lupus CD4+ T cells. J. Autoimmun. 2010;35:58–69. doi: 10.1016/j.jaut.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 149.Bakker S.C., van der Meulen E.M., Buitelaar J.K., Sandkuijl L.A., Pauls D.L., Monsuur A.J., van ‘t Slot R., Minderaa R.B., Gunning W.B., Pearson P.L., et al. A whole-genome scan in 164 dutch sib pairs with attention-deficit/hyperactivity disorder: Suggestive evidence for linkage on chromosomes 7p and 15q. Am. J. Hum. Genet. 2003;72:1251–1260. doi: 10.1086/375143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Jesmin S., Togashi H., Sakuma I., Mowa C.N., Ueno K., Yamaguchi T., Yoshioka M., Kitabatake A. Gonadal hormones and frontocortical expression of vascular endothelial growth factor in male stroke-prone, spontaneously hypertensive rats, a model for attention-deficit/hyperactivity disorder. Endocrinology. 2004;145:4330–4343. doi: 10.1210/en.2004-0487. [DOI] [PubMed] [Google Scholar]