ABSTRACT
While the immune system is credited with averting tuberculosis in billions of individuals exposed to Mycobacterium tuberculosis, the immune system is also culpable for tempering the ability of antibiotics to deliver swift and durable cure of disease. In individuals afflicted with tuberculosis, host immunity produces diverse microenvironmental niches that support suboptimal growth, or complete growth arrest, of M. tuberculosis. The physiological state of nonreplication in bacteria is associated with phenotypic drug tolerance. Many of these host microenvironments, when modeled in vitro by carbon starvation, complete nutrient starvation, stationary phase, acidic pH, reactive nitrogen intermediates, hypoxia, biofilms, and withholding streptomycin from the streptomycin-addicted strain SS18b, render M. tuberculosis profoundly tolerant to many of the antibiotics that are given to tuberculosis patients in clinical settings. Targeting nonreplicating persisters is anticipated to reduce the duration of antibiotic treatment and rate of posttreatment relapse. Some promising drugs to treat tuberculosis, such as rifampin and bedaquiline, only kill nonreplicating M. tuberculosis in vitro at concentrations far greater than their minimal inhibitory concentrations against replicating bacilli. There is an urgent demand to identify which of the currently used antibiotics, and which of the molecules in academic and corporate screening collections, have potent bactericidal action on nonreplicating M. tuberculosis. With this goal, we review methods of high-throughput screening to target nonreplicating M. tuberculosis and methods to progress candidate molecules. A classification based on structures and putative targets of molecules that have been reported to kill nonreplicating M. tuberculosis revealed a rich diversity in pharmacophores.
INTRODUCTION
Two parallel revolutions were born in the golden era of antibiotics (∼1940 to 1960). One was a revolution in medicine as physicians went to war with microbes. The second was a revolution in biology as microbiologists and geneticists used anti-infectives as tools to reveal how microbes function on a molecular level. Scientists converged on a surprisingly short list of essential biological processes that appeared to make up an Achilles’ heel shared by diverse bacterial pathogens: the biosynthesis of nucleic acids (DNA and RNA), protein, cell walls (peptidoglycan and lipids), and folate. Only later were the far wider dimensions of potential target space appreciated (1). The discovery of targets led to the development of methods to improve existing antibiotics and find new ones.
The success of chemical biology at advancing antibiotic development was spectacular but short-lived. New antibiotics quickly encountered genetically encoded drug resistance (2). The selective pressure imposed by antibiotics presented bacteria with a seemingly impossible task of becoming drug resistant by modifying the antibiotic’s target, modifying the antibiotic’s structure, effluxing the antibiotic, or altering their cell wall’s permeability to the drug without a major fitness cost. Yet bacteria solve this problem routinely in laboratories, the environment, animal models of disease, and patients. Resistant mutants distribute drug resistance by vertical transmission (passing chromosomal DNA to their progeny) and horizontal transmission (via phages and plasmids). Antibiotic research concentrated on understanding the basis of genetically encoded drug resistance, and medical chemistry campaigns focused on bypassing it.
However, genetic drug resistance was not the only hurdle. Pioneering observations published by Hobby, Meyer, and Chaffee in 1942 (3) and by Bigger in 1944 (4) cast an ominous cloud over the remnants of optimism that antibiotics could eradicate diseases of bacterial origin. Hobby and her colleagues observed that about 1 streptococcus of 106 in a replicating culture survived exposure to penicillin, while in a culture whose replication was halted by cold, nearly all the cocci survived (3). Bigger made the same observation with staphylococcus and additionally noted that the cocci became tolerant to penicillin when their replication was halted by acidification or hypotonicity of the medium (4). Microbiologists had long assumed that logarithmically growing bacterial cultures were uniform. Use of penicillin as a tool allowed Hobby, Meyer, Chafee, and Bigger to discover that the assumption of bacterial homogeneity was incorrect. Moreover, they demonstrated that bacteria could resist killing by antibiotics through a nonheritable mechanism. The penicillin-resistant cells were as sensitive to penicillin as the population from which they came when they were expanded in fresh medium and exposed to penicillin a second time. Bigger used the term “persisters” for bacteria that survived antibiotics without heritable resistance. The property allowing persisters to survive was later termed “phenotypic drug resistance” or “phenotypic tolerance.” These historic studies have important implications for anti-infective discovery paradigms today (3, 4).
Two decades later, Hobby and Lenert extended the observation of phenotypic tolerance to a different organism, Mycobacterium tuberculosis, and additional drugs, isoniazid and para-aminosalicylate (5). Isoniazid targets the synthesis of mycolic acids, para-aminosalicylate targets the synthesis of folate, and penicillin targets the synthesis of peptidoglycan. Thus, the phenomenon of phenotypic tolerance was independent of the chemical class of antibiotics and of the pathways they inhibit.
The problem of persisters is central to the chemotherapy of tuberculosis. It is believed to be a major reason why the current WHO-approved treatment regimen for drug-sensitive tuberculosis takes 6 months to achieve cure in ∼95% of participants in formal studies; the cure rate is about 86% in routine practice. Drug-resistant tuberculosis generally requires treatment for over 2 years, and cure is often not achieved (6). In the “Cornell model,” mice with drug-sensitive tuberculosis that are treated with isoniazid and pyrazinamide for 2 months harbor no detectable CFU of M. tuberculosis when their organ homogenates are spread on bacteriologic agar. However, about one-third of the remaining members of the same cohort of mice relapse spontaneously some months later, and nearly all of them relapse if immunosuppressed with corticosteroids, anti-interferon-γ (IFN-γ), anti-tumor necrosis factor, or inhibitors of inducible nitric oxide synthase (7–9). The M. tuberculosis recovered at relapse is as sensitive to isoniazid and pyrazinamide as the population used for inoculation. These observations indicate the presence of drug-tolerant persister populations after antibiotic treatment, even if they are temporarily undetectable by standard microbiologic methods. Likewise, sputa from about 80% of treatment-naive tuberculosis patients contained M. tuberculosis that was not quantifiable by CFU analysis (10, 11).
Experience with metronidazole illustrates the challenge of translating the foregoing knowledge into a faster and more effective treatment of tuberculosis. In some animal models, M. tuberculosis encounters hypoxia in necrotic granulomas (Table 1). In vitro, hypoxia causes mycobacteria to cease replicating and become phenotypically tolerant to most drugs. In contrast, the antibacterial and antiparasitic drug metronidazole kills hypoxic mycobacteria in vitro. Thus, metronidazole seemed well suited to kill nonreplicating M. tuberculosis. However, metronidazole’s activity in animal models of tuberculosis correlated imperfectly with hypoxia in granulomas (Table 1) (12–19). Metronidazole improved the proportion of patients whose sputum became smear- or culture-negative at 1 month of treatment but did not impact treatment outcome at 6 months, other than contributing to peripheral neuropathy (14). In retrospect, the ability of metronidazole to kill hypoxic M. tuberculosis in vitro was studied in the absence of an alternative electron acceptor, putting the organism at a greater disadvantage than it is likely to face in vivo. M. tuberculosis is not restricted to using oxygen as an electron acceptor; it can also use nitrate or fumarate (20–22). Nitrate is a physiologic constituent of human body fluids. Inclusion of nitrate markedly diminished the in vitro efficacy of pyrazinamide (23).
TABLE 1.
Evaluating the relationship between hypoxia and metronidazole activity in vitro and in vivo
| Model | Method to measure or demonstrate hypoxia | Evidence of hypoxia? | Caseating granulomas? | Activity of metronidazole | References |
|---|---|---|---|---|---|
| Wayne in vitro model of dormancy | <0.06% O2, methylene blue decolorization | Yes | No | Active | 19, 95 |
| Mouse: C57Bl/6 | Pimonidazole (immunohistochemistry), EF5/ELK3-51 antibody | No | No | Inactive | 13, 17, 294, 295 |
| Mouse: BALB/c | Copper(II)-diacetyl-bis(N4-methyl-thiosemicarbazone), pimonidazole (immunohistochemistry) | No | No | Inactive | 17, 64, 296, 297 |
| Mouse: C3HeB/FeJ “Kramnik model” | Copper(II)-diacetyl-bis(N4-methyl-thiosemicarbazone), pimonidazole (immunohistochemistry), gene expression of hypoxia-associated genes in M. tuberculosis | Yes | Yes | Inactive | 64, 296, 297 |
| Guinea pig | Pimonidazole (immunohistochemistry) | Yes | Yes | Inactive | 15, 17 |
| Rabbit | Pimonidazole (immunohistochemistry), fiber-optic O2 probe | Yes | Yes | Active | 17 |
| Non-human primates | Pimonidazole (immunohistochemistry) | Yes | Yes | Active | 16, 17 |
| Human | EF5/ELK3-51 antibody, HIF-1α (hypoxia inducible factor) (immunohistochemistry), [18F]-fluoromisonidazole (positron emission tomography imaging) | Yes | Yes | Clinically ineffective | 14, 245, 294, 298 |
The experience with metronidazole suggests that it may not be enough to find antibiotics with the exceptional property of killing bacteria that are phenotypically tolerant to most other antibiotics; it matters how the bacteria are rendered phenotypically tolerant. If phenotypic tolerance is achieved by using conditions that prevent the bacteria from replicating, it matters how they are prevented from replicating. The more the conditions resemble those in the host, the more likely that drugs that work under those conditions may also work in the host.
The foregoing statements are a hypothesis whose testing is just beginning. After Bigger’s report (4), it took another 40 years until Coates proposed large-scale screening to target nonreplicating M. tuberculosis (24). His proposal came at a time when many pharmaceutical companies were scaling back or abandoning anti-infective discovery. Other firms stuck to the industry’s standard practice of seeking broad-spectrum agents that could cure infections prevalent in economically advantaged regions. Only after 1999 did a new funding landscape emerge that supported academic-industrial partnerships for drug discovery for infectious diseases that are prevalent chiefly in economically disadvantaged regions (1, 25–27). Only about 10 years ago did pharmaceutical companies and their academic partners begin large-scale screens for drugs targeting phenotypically tolerant mycobacteria (28, 29).
This chapter describes and categorizes approximately 100 compounds that have been reported to kill mycobacteria rendered nonreplicating in one or another in vitro model. We also offer comments about the biology of drug tolerance, strategies for screening compounds against phenotypically tolerant mycobacteria, progressing the “actives” through secondary assays, and pitfalls in data interpretation.
SUMMARY OF KEY OBSERVATIONS
At least two types of phenotypic tolerance are important to distinguish because different strategies will probably be needed to overcome them (25, 27). Class I phenotypic tolerance is manifest by a small proportion of bacteria in a replicating population. Existing evidence, while incomplete, suggests that different individual bacteria in the population can be phenotypically tolerant to different antibiotics by different mechanisms. To the degree that this is the case, phenotypic tolerance can be overcome by treating the overall population with a combination of drugs. Class II phenotypic tolerance is manifest by almost all the cells in a population whose number is not changing during the period of observation. Almost every cell must be phenotypically tolerant to all the antibiotics to which the population as a whole is tolerant. Overcoming class II phenotypic tolerance will likely require new kinds of drugs that are highly active on nonreplicating bacteria.
While nonreplication imposed by diverse stresses is closely associated with phenotypic tolerance, mycobacteria that become nonreplicating under different conditions may be phenotypically diverse.
While nonreplication is a state associated with phenotypic tolerance, nonreplication is not a mechanistic explanation for phenotypic tolerance. Nonreplication is not equivalent to dormancy and does not connote a lack of dependence on biosynthetic pathways.
Nonreplicating mycobacteria are reportedly killed by a large number of chemically diverse compounds. However, only a few of these compounds have been tested and found to be active against mycobacteria rendered nonreplicating in multiple ways.
Only a few of the compounds reported to kill nonreplicating mycobacteria have been tested under conditions designed to exclude false-positive results that can arise from drug carryover from the nonreplicating phase of the assay to the replicating phase, such as by enumerating viable bacilli on a solid bacteriologic medium containing activated charcoal (30–33).
Some approved drugs for tuberculosis, such as rifampin and moxifloxacin, are genuinely active in vitro against nonreplicating M. tuberculosis, but at far higher concentrations and with far less reduction in bacterial numbers than under replicating conditions. For others, such as bedaquiline, the apparent activity against nonreplicating M. tuberculosis in vitro was largely attributable to carryover in one study (30). Among the approved tuberculosis drugs tested in that study, only PA-824 was genuinely and comparably active against M. tuberculosis under replicating and nonreplicating conditions (30). Encouragingly, ongoing research is identifying more such compounds among anti-infectives approved for other indications (34) or as new members of drug-like chemical classes.
DIVERSITY IN NONREPLICATION
Sensitivity to an antibiotic is conventionally defined under replicating conditions and reported as an MIC, typically meaning a concentration that restricts growth by at least 90% compared to a culture under the same conditions that is exposed to the vehicle alone for the same period of time. Phenotypically tolerant bacteria of class I are those rare cells that survive exposure to the antibiotic at or above its MIC when tested under these standard, replicating conditions. In contrast, phenotypically tolerant bacteria of class II are the majority of a population that survives exposure to the antibiotic at or above its MIC under different conditions, typically those that impose nonreplication. To distinguish the nonreplication imposed by the test conditions from death imposed by the antibiotic usually requires removing the antibiotic by washing or dilution, reversing the conditions that impose nonreplication, and then detecting recovery or the lack of recovery of the surviving bacteria by allowing survivors to replicate. The hallmark of both class I and class II phenotypic tolerance is that the survivors, when tested again under the standard conditions, display the same MIC as the original population (25).
To fully appreciate the diversity exhibited by nonreplicating cells, it will be useful to start by correcting several misconceptions. First, when Hobby et al. (3) and Bigger (4) discovered what we now call class I persistence, they attributed it to nonreplication of about one bacterium in a million in an otherwise replicating population. They had no direct evidence for this. More than half a century later, it became possible to test this notion, and the results have been mixed. In short, class I phenotypic tolerance sometimes is and sometimes is not associated with nonreplication of a minority of cells in a replicating population. By definition, class II persisters are nonreplicating. Therefore, class I and class II persisters should not be grouped together as “nonreplicating cells.” Second, just because a bacterial population has stopped changing in number over a period of time, this does not exclude the occurrence of balanced replication and death. For simplicity, we use the term “nonreplication” to describe a population of static size, but without implying the degree of turnover. Third, just because one population of bacteria has entered a nonreplicating state in response to one condition, this does not mean that it has the same phenotype as another population that has entered a nonreplicating state in response to another condition.
Single-cell analyses of persister populations are now feasible. For example, cell division can be monitored by dilution of a fluorescent signal from a chromosomal copy of mCherry (35, 36) and metabolism monitored using redox sensor green, which generates a fluorescent signal upon reduction by bacterial reductases. The fates of individual cells can be tracked over time by microfluidics and time-lapse microscopy (36–39). Replicating and nonreplicating cells, and metabolically active and metabolically inactive cells, may be sorted using a fluorescence-activated cell sorter. For example, Brynildsen and colleagues found that while nongrowing cells were enriched for class I persisters, 20% of the persisters were replicating, and slow metabolism correlated with, but was not required for, persistence (36).
Persister diversity may result from heterogeneity in such bacterial processes as maintenance of membrane potential, DNA replication, and ribosomal translation (40, 41) or in host environments, where bacteria may be extracellular in connective tissue or caseum or intracellular in phagosomes or cytosol (42). The transcriptome of M. tuberculosis class I persisters enriched by d-cycloserine treatment to kill replicating cells overlapped very little with the transcriptomes of class II phenotypically tolerant cells generated by incubating M. tuberculosis under conditions of hypoxia (43, 44), stationary phase (12, 44, 45), or nutrient starvation (12). Moreover, only five genes were identified as commonly upregulated in the four nonreplicating models (46), and there was little overlap of M. tuberculosis’s differentially regulated genes in the three class II nonreplicating models (43, 44, 46). Another comprehensive comparison found a poor correlation of transcriptomes of M. tuberculosis rendered nonreplicating in multiple models, including removing streptomycin from the streptomycin-addicted strain SS18b; exposing wild-type M. tuberculosis to reactive nitrogen intermediates; depriving it of phosphate, nutrients, or oxygen; or combining a variety of stresses (47). On the other hand, Voskuil et al. found a correlation among the transcriptomes of M. tuberculosis exposed to hypoxia, the nitric oxide donor DETA-NO, and cyanide (48), and the transcriptional changes were similar to those seen during infection by M. tuberculosis of IFN-γ-activated bone marrow-derived macrophages (49). While these transcriptomics experiments were insightful, we do not know the relevance of transcriptional regulation of individual genes to the survival of mycobacteria as class I or class II phenotypically tolerant. Transcriptomics profiles are time-dependent, making it difficult to compare transcriptomes studied at different times. Moreover, many key regulatory steps are posttranslational.
Another indication of the diversity of nonreplicating mycobacteria is that the same compounds are differentially active against M. tuberculosis rendered nonreplicating in different ways, such as nutrient starvation, stationary phase, hypoxia, and a combination of acidic pH and reactive nitrogen intermediates (50–52). In the multistress model (acidic pH, reactive nitrogen intermediates, hypoxia, and a fatty acid carbon source), some compounds specifically required reactive nitrogen intermediates for their activity (28, 53). Grant et al. found that of 52 molecules active against M. tuberculosis in a carbon starvation model, only 33% were also active against bacilli rendered nonreplicating by hypoxia (54). The same study found diversity of the activity profiles of four compounds, from three chemical classes, in a class I persister model and three class II models: hypoxia, starvation, and removal of streptomycin from the addicted strain, SS18b (54, 55).
Very few compounds have been demonstrated to kill M. tuberculosis rendered nonreplicating in more than one way. This may be because such “pan-actives” are rare in chemical space or because investigators do not routinely test “actives” from one model in other models. We describe pan-actives in the section “Proof-of-Concept Molecules.”
CLASS I PERSISTERS: RARE, DRUG-TOLERANT CELLS
Long before the work of Bigger, Hobby, and colleagues was rediscovered (3, 4) and the term “phenotypic tolerance” became widely used (56), researchers had observed evidence of class I persisters in vitro and in vivo. Kill curves, in which the x axis of the graph represents time and the y axis represents the number of viable bacteria recovered on agar plates using a CFU-based assay, often have a biphasic, or “hockey stick,” shape (25). Following a sharp, logarithmic decrease in viable CFUs at early time points, the CFUs plateau or decrease at a reduced rate. Notably, compounds fail to reduce CFUs below the limit of detection at any concentration tested (46, 55). Put differently, the CFU assay reveals a small population of cells that are refractory to killing by the antibiotic. Biphasic kill curves have been observed for M. tuberculosis and other mycobacterial species treated with dapsone, ciprofloxacin, isoniazid, d-cycloserine, rifampin, streptomycin, and various combinations of these antibiotics (30, 46, 54, 55, 57, 58). Class I persisters appear to play a role in phenotypic drug tolerance during human infections caused by Pseudomonas aeruginosa, Escherichia coli, and Candida albicans (57, 59–61). Evidence of class I persisters was observed in murine and guinea pig models of tuberculosis (62–64) and in the human disease (57).
By definition, class I mycobacterial persisters are reversibly tolerant to one or another of the standard antibiotics (46, 55, 65) but not necessarily to their combinations. There is no reason to expect class I phenotypically tolerant bacteria to be more resistant than their siblings to molecules that have multiple targets, such as hydroxyl radicals (55, 66). Unlike in E. coli (67), there is conflicting evidence whether class I mycobacterial persisters are cross-tolerant to other antibiotics. In one study, Mycobacterium smegmatis and M. tuberculosis persisters that survived exposure to a combination of ciprofloxacin and isoniazid were tolerant to a bactericidal concentration of rifampin (55). However, a different study found persister populations of ∼1.7 × 10−5 to isoniazid, ∼7.0 × 10−4 to rifampin, and >10−1 to pyrazinamide (65). The persister population resistant to the combination of isoniazid, rifampin, and pyrazinamide was ∼2.8 × 10−7, indicating that individual persisters were not broadly resistant to other antibiotics (65). While strategies to target class I persisters have been proposed (40, 41, 68), to our knowledge, high-throughput screens targeting class I mycobacterial persisters have not been undertaken. Conversely, most compounds known to have activity against mycobacteria have not been tested for activity against mycobacteria displaying class I phenotypic tolerance to other compounds. Compound 57, identified in a class II phenotypic screen against carbon-starved M. tuberculosis, serves as an illustrative example of a compound whose ability to additionally kill class I phenotypically tolerant M. tuberculosis was discovered postscreening (54). Compound 57 is described in more detail in the section “Carbon Starvation” (54).
In vitro, genetic mutations in hipA and hipB (high persister genes) lead to approximately 10- to 10,000-fold more class I drug-tolerant persisters in E. coli, Salmonella, and other species (57, 69–73). Use of hip mutants permitted the observation of persisters by time-lapse studies in microfluidic devices (39). High-persister mutants that survived treatment with streptomycin and rifampin were recently identified in an ethyl methanesulfonate-mutagenized auxotrophic strain of M. tuberculosis and were characterized by genome resequencing and transcriptomics (57). Genetic control over the size of a class I phenotypically tolerant population should not be confused with heritable resistance. The survivors, when grown without antibiotic and exposed again, have the same MIC as the population from which they were derived. Even a mutant strain of E. coli with a 10,000-fold increase in the wild-type proportion of class I phenotypically tolerant persisters to ampicillin will display a 99% reduction in survival at the same concentration of ampicillin as the wild-type strain if the proportion of class I persisters has increased from 1 × 10−6 to 1 × 10−2.
Numerous mechanisms can impel a cell to display class I phenotypic tolerance (39, 74–79). Mycobacterial asymmetric division results in differential antibiotic sensitivity of daughter cells (80, 81). As in E. coli (82, 83), mycobacteria may depend on toxin-antitoxin genes (46, 65, 84) to induce class I tolerance. Javid and colleagues found that mistranslation of two amino acids, glutamate for glutamine, and aspartate for asparagine, resulted in modified RNA polymerase (RpoB, encoded by rv0667) that was more resistant to rifampin (85). Only a minority of cells in a wild-type population accumulated enough mutant copies of RpoB with Asp in place of Asn at position 434 to survive rifampin at its MIC (85, 86). When these cells were expanded, the MIC remained the same.
Analogous to the situation with hip genes in E. coli, mutation in the GatCAB aminotransferase that normally corrects mistranslation of the Asn codon increased the frequency of these class I phenotypically tolerant mycobacteria, but the MIC was no greater in progeny of these cells than in the population from which they were selected (86). Rendering M. smegmatis nonreplicating by acidic pH or nutrient starvation led to protein mistranslation and phenotypic kanamycin resistance (85). Isoniazid is a prodrug that requires oxidation by a catalase-peroxidase (KatG, encoded by rv1908c) and forms an NAD-isoniazid adduct that targets NADH-dependent enoyl-ACP reductase (InhA, encoded by rv1484). Isoniazid kills multiple log10 CFU of replicating mycobacteria within days; yet isoniazid dosed by itself takes weeks to months to achieve a modest reduction in the M. tuberculosis bacterial burden in mice (87). Stochastic gene expression has been described in eukaryotes and prokaryotes (88, 89) and provides one potential explanation for the appearance of class I phenotypic tolerance in a small subpopulation of bacteria. For example, Wakamoto et al. found that stochastic expression of katG explains some mycobacterial tolerance to isoniazid (90). In E. coli, fluoroquinolones can damage DNA and induce an SOS response protein, TisB, which transforms cells to a persister phenotype by depolarizing the membrane and depleting ATP (91–93).
CLASS II PERSISTERS: A MAJORITY POPULATION OF NONREPLICATING, DRUG-TOLERANT CELLS
Class II persisters are defined as a population of cells displaying phenotypic drug tolerance under externally applied conditions that halt net replication. As noted, nonreplication in this sense is a terminologic simplification that encompasses balanced bacterial growth and death. In some models of nonreplication, there is a slow reduction in viable bacteria over the period of observation that may be difficult to detect by a CFU assay (28, 94). Conditions that arrest growth are associated with resistance to a large number of antibiotics. Some investigators have assumed that failure to grow is synonymous with shutdown of the bacterial machinery that synthesizes macromolecules and that the lack of need for macromolecules explains the lack of sensitivity to drugs that inhibit their synthesis (30, 50–52, 95, 96). However, M. tuberculosis adapts to the stresses that impose nonreplication with a robust transcriptional response (46, 49, 97) and cell wall remodeling (98, 99) and maintains metabolic activity, although with a different profile of metabolites than during replication (K. Rhee, personal communication). Nonreliance on biosynthetic processes is an unsatisfactory explanation for class II phenotypic tolerance.
The rate at which M. tuberculosis achieves stasis may impact the bacilli’s biology and sensitivity to certain compounds. For example, some models of nonreplication, such as hypoxia or starvation, require preadaptation periods of 1 to 2 weeks or more (12, 54, 95). In contrast, reactive nitrogen intermediates cause immediate growth arrest (48, 100). In addition, exogenously applied stresses may be perceived at different rates by mycobacteria at different locations within a clump.
Designing High-Throughput Screens To Target Phenotypically Tolerant Mycobacteria
There have been numerous whole-cell screens to identify small molecules in academic and industrial collections that kill nonreplicating mycobacteria (29, 53, 54, 94, 96, 101–105). Compounds arising from whole-cell screening are presumably taken up into the cell to exert bactericidal activity, without any preconceptions about suitable targets. An alternative approach is to postulate which enzymes play a role in nonreplicating persistence based on informatics or biochemical or genetic studies, set up relevant biochemical assays, identify inhibitors, and then assay those inhibitors for whole-cell activity in nonreplicating models (100, 106–115). The limitation of biochemical screening, however, is that the majority of enzyme inhibitors so identified lack activity against intact M. tuberculosis due to poor uptake, the sufficiency of residual enzyme activity for cell survival, intracellular metabolism, or redundant pathways (116). Translating biochemical screening hits to whole-cell activity is hampered by using a binary readout of the life/death of a bacterial cell as a surrogate to monitor target engagement (117).
In screens carried out against nonreplicating bacteria, a failure to increase in optical density over time cannot be used as a measure of antibacterial activity since, by definition, the optical density does not change for the duration of a nonreplicating experiment. There are limited examples of screening by recording fluorescence from nonreplicating mycobacteria (29, 118, 119). While most replicating assays use an inoculum of ∼A580 of 0.01 or lower, use of a fluorescent readout can require a larger inoculum (upwards of ∼50-fold) to achieve a sufficient signal (119). Using a high inoculum of cells may preclude identifying active molecules from compound classes such as beta-lactams, which are highly sensitive to inoculum effects (120). Moreover, nonreplicating screens employing fluorescent readouts often depend on subtle differences in the fluorescence of compound-treated versus vehicle-treated cells (often less than 2-fold), which in turn requires exceptional Z′ scores (29). In some nonreplicating assays, the drug-exposure phase of the assay is coupled to a drug-free secondary phase that permits bacterial growth and allows one to make a semiquantitative estimation of the number of surviving cells (Fig. 1) (53, 54, 96). The two-stage assay, while effective, can take 14 to 17 days (a 7-day drug exposure and a 7- to 10-day outgrowth) and runs a risk of evaporation, edge effects, and contamination with mold (30, 94).
FIGURE 1.

Strategies to evaluate the viability of nonreplicating mycobacteria for high-throughput screening. The arrow color indicates the quality of each readout strategy (considering robustness, ease of use, dynamic range, etc.) as excellent (green arrows), average to poor (black arrows), or infeasible (red line). Compound carryover may result from compound transfer from the nonreplicating assay to replicating assay bacteriologic growth medium or by compound adherence to the bacterial cell wall.
One must carefully weigh the relative importance of potential variables when designing a high-throughput screen against nonreplicating mycobacteria (Fig. 2). Table 2 provides a nonexhaustive list of potential microenvironments encountered by M. tuberculosis during infections that may lead to suboptimal growth or nonreplication. The numerous nonreplicating models and technical variables lead to a staggering number of possible combinations.
FIGURE 2.

Selecting and designing nonreplicating (NR) models. (Left) Nonexhaustive list of models of class I and class II nonreplication. (Right) Variables to consider when designing models. (Center, bottom) Potential activity profiles of nonreplicating actives. The success of compounds targeting nonreplicating mycobacteria is dependent on the interactions among models, variables, and activity profiles. The term “DD Mtb” (differentially detectable M. tuberculosis) is used interchangeably with “viable-but-nonculturable” (VBNC) M. tuberculosis.
TABLE 2.
Conditions encountered by M. tuberculosis that may contribute to suboptimal replication rates or complete growth stasisa
| Condition(s) | Chemical mediator(s), examples | Location or situation, example(s) | Responsible for microenvironmental condition | References |
|---|---|---|---|---|
| Acidic pH | H+ | M. tuberculosis-containing phagosome | Immune-stimulated macrophages | 231, 232 |
| Lactate in extracellular fluid at inflammatory sites | Crowding of stromal and parenchymal cells by macrophages, monocytes, dendritic cells, lymphocytes, neutrophils leading to enhanced reliance on glycolysis | 299 | ||
| Succinate | Secreted by M. tuberculosis under hypoxic conditions | 168, 300 | ||
| Hypoxia | Limiting O2 | Necrotic granulomas | Poor vascularization of necrotic granuloma that has a surrounding rim composed of epithelioid macrophages, T cells, B cells, and neutrophils; phagosomes of human macrophages infected with wild-type M. tuberculosis | 17, 21, 301–303 |
| Reactive nitrogen intermediates | •NO, ONOO–, ONOOH, •NO2, N2O3, N2O5 | Macrophage phagosomes | Human blood, human interstitial fluid, diet, enterosalivary nitrite cycle, inducible and constitutive nitric oxide synthases in macrophages, fibroblasts, vascular smooth muscle, endothelium, and bronchial epithelium, M. tuberculosis under hypoxic conditions or in human macrophages | 27, 232, 304–308 |
| Reactive oxygen intermediates | •O2–, H2O2, ROOH, •OH, 1O2, O3, HOCl, HOBr, HOI | Macrophage phagosomes, antibiotics | Activated macrophages and polymorphonuclear leukocytes, the respiratory chain, catabolism (enzymatic and nonenzymatic), response of M. tuberculosis to antibiotics | 66, 309–312 |
| Metal deficiency | Iron | Animal models, humans | Iron sequestration by host iron-binding proteins such as lactoferrin | 229, 313 |
| Magnesium | Macrophage phagosome, mycobacterial membrane lipids | NRAMP (natural resistance-associated macrophage protein) ion transporter | 243, 314 | |
| Metal intoxication | Cu(I) | Macrophage phagosome, blood, lungs | Copper transporter ATP7A, copper importer CTR1, ceruloplasmin, NO-dependent release of copper from Cu(I)-protein complexes | 140, 230, 315–319 |
| Osmolarity | Chloride ion | Macrophage phagosome, airway surface liquid | Chloride channels, such as chloride channel protein 1 | 320–323 |
| Carbon sources that support slow growth or survival; growth rate less than maximal | Fatty acids (short/long chain; saturated/unsaturated), cholesterol, amino acids, CO2 | Macrophage phagosomes, caseum, granulomas, adipose tissue | Krebs cycle, glycolysis | 233, 236, 237, 324–328 |
| Nutritional starvation | Use of M. tuberculosis metabolic reserves: trehalose, glycogen, fatty acids, glutamate | Unlikely to occur | Krebs cycle, glyoxylate shunt | 12, 216, 329 |
| Amino acid or vitamin deficiency | Methionine, lysine, leucine, panthothenate | Macrophage phagosomes | Limited quantities in vivo, or amino acids and vitamins are not in a form accessible for mycobacterial uptake | 238–240, 330, 331 |
| Nitrogen metabolism | Amino acids, inorganic NH4+, urea, NO3– (nitrate) | Hypoxic lesions and/or hypoxic-acidic phagosomes | M. tuberculosis respiring nitrate as an alternative electron acceptor, acid resistance, nutrient starvation | 21, 332, 333 |
Individual conditions, or combinations of them, that are anticipated to lead to phenotypic tolerance observed in animal models of tuberculosis and in human patients.
The most commonly used models for nonreplicating mycobacteria are hypoxia (the Wayne model) and the low oxygen recovery assay (LORA) (29, 95, 96); carbon starvation (54, 121); nutrient starvation (12, 52); stationary phase (105); maintenance of intrabacterial pH under acidic culture conditions (119, 122–126); biofilms (102, 127–130); depleting strain SS18b of streptomycin (103, 104, 131, 132); and a multistress model that combines acidic pH (pH 5.0), mild hypoxia (1% O2), nitric oxide and other reactive nitrogen intermediates (0.5 mM NaNO2), and a fatty acid carbon source (0.05% butyrate) (28, 53, 94, 100, 133). There are variations of these models, including an acidic Wayne model that combines hypoxia with mild acidity (130) and a nutrient-poor, multistress model in which cells are cultured at low pH (pH 5.0) under mild hypoxia or tissue-level normoxia (5% O2) and supra-physiologic levels of CO2 (10% CO2) (134). Sublethal doses of antibiotics targeting translation can also arrest growth (135). Potassium starvation has been reported to lead to the formation of differentially detectable mycobacteria (also called “viable but not culturable”) (136, 137).
High-throughput screening typically identifies many molecules with properties unsuitable for further progression, including those whose structures contain toxicophores and/or metabolic liabilities (138, 139). Comprehensive postscreening characterization of compounds from primary screens is extremely expensive in terms of time and resources. In Table 3, we summarize postscreening assays that are suitable for molecules with activity against replicating and/or nonreplicating mycobacteria. Table 4 summarizes assays used to characterize the action of compounds on nonreplicating mycobacteria. A hit progression flowchart for a nonreplicating active compound should attempt to include the assays described in both Tables 3 and 4.
TABLE 3.
Postscreening assays for molecules active on replicating and/or nonreplicating M. tuberculosis
| Hit triage assay/study | Description and/or techniques used | Function |
|---|---|---|
| Validate chemical identity and purity | LC-MS, nuclear magnetic resonance | Sometimes overlooked, this is an essential component of high-throughput screening that can prevent heartbreak after years of work. It is imperative to confirm that the proposed structure is the molecule responsible for the observed activity. |
| Confirm activity with resupplied compound; confirm activity with resynthesized compound | Reorder from trusted supplier and conduct de novo chemical synthesis | |
| Medical chemist analysis for structural alerts or toxicophores | Organic, physical, and medical chemistry; cheminformatics; experience | Identification of structural alerts or toxicophores may predict alternative mechanisms of action (often general reactivity) and in vivo liabilities, such as liver toxicity or metabolism. |
| Glutathione reactivity | Mix compound with reduced glutathione and look for possible glutathione-compound adducts | Highly unstable transformation products may be difficult to observe due to their transient nature. Glutathione, with a cysteine nucleophile, reacts avidly with electrophilic molecules and can form stable glutathione-compound adducts. |
| Toxicity to HepG2 and/or Vero cells | EC50 determination by correlating ATP levels with cellular viability | Both the human hepatocellular carcinoma cell lines (HepG2) and monkey kidney epithelial cell lines (Vero) are used to test for cellular toxicity; HepG2 cells also assay for possible bioactivation in the liver. |
| Determine the selectivity index (SI) | EC50 in Vero or HepG2 cells divided by the MIC90 against M. tuberculosis | Helps prioritize compounds that are more potent against M. tuberculosis than against eukaryotic cells. Typically, an SI of >10 is used as a threshold for structure-activity relationship analysis, and an SI of >50 is required to advance to lead candidacy. The duration of compound exposure to M. tuberculosis and HepG2/Vero cells and equivalence of serum proteins in the two assays should be taken into account. |
| Serum shift | Determine MIC90 in screening medium ±10% heat inactivated mouse or human serum | A serum shift may indicate if a compound is highly protein bound and provide a warning that eukaryotic toxicity results, typically performed with 10% serum, may have underestimated toxicity. |
| Inoculum effect | Determine MIC90 at an OD580 of 0.01 and 0.10 | Some compounds such as beta-lactams are well known for inoculum effects, in which their potency decreases as the inoculum increases. |
| Microbiologic spectrum | Test activity against representative Gram-positive and Gram-negative bacteria and fungi | To determine if a compound has broad- or narrow-spectrum activity |
| Frequency of resistance (FOR) | Plate 106 to 109 M. tuberculosis on agar plates containing 1-20× the broth MIC90 of compound | Determine the number of pre-existing mutants in a population that are naturally resistant to a drug or determine if the drug itself is mutagenic. Acceptable FORs are ≤1 × 10−6 (the FOR of isoniazid). |
| Test activity against drug-resistant M. tuberculosis strains | Determine the MIC90 of a drug against M. tuberculosis strains resistant to isoniazid, rifampin, streptomycin, ethionamide, ethambutol, etc. | A new agent should have activity against drug-resistant strains. |
| Test activity against clinical isolates of M. tuberculosis | Determine the MIC90 of a drug against clinical isolates from tuberculosis patients | A new agent should have activity against strains of M. tuberculosis with diverse genotypes. |
| Genotoxicity | Ames and micronucleus | Compound series with genotoxicity may be mutagenic. SAR campaigns may find analogues that are not mutagenic; if not, series should be deprioritized or terminated. |
| Activity against intracellular M. tuberculosis | Examples include M. tuberculosis infecting human blood monocytes, human macrophage cell lines such as THP-1, or murine J774 and RAW macrophage cell lines | This assay usually omits immunological stimulation of the macrophages. Consequently, M. tuberculosis is predominantly replicating. |
| Activity against M. tuberculosis grown with different carbon sources | Test acetate, propionate, dextrose, glutamate, glycerol (without dextrose) | It is essential to confirm that the activity of a molecule is not strictly dependent on the carbon source. |
| CFU assays: time- and dose-dependency | Test for CFU reduction at multiples of MIC90 and at different times of compound exposure | The CFU assay is considered the “gold standard” to enumerate viable bacteria. Molecules that fail to demonstrate dose- and time-dependent kill may have a nonspecific mechanism of action. |
TABLE 4.
Postscreening assays specific for nonreplicating active or candidate dual-active molecules (active on both replicating and nonreplicating bacilli)a
| Assay/method | Function/description | References |
|---|---|---|
| Charcoal agar resazurin assay | (i) To distinguish replicating-, nonreplicating-, and dual-active molecules; (ii) to distinguish replicating bacteriostatic and replicating bactericidal activity; (iii) to serve as a semiquantitative pretest prior to CFU assays; (iv) to permit testing of the impact of a compound over a wide range of concentrations and time points | 30, 145 |
| Cell-free stability assay | To determine if a compound undergoes structural modification in the cell-free medium used for the nonreplicating high-throughput screening model | 28, 53 |
| Pre-nonreplicating assay | To determine if any potential transformation products have activity against replicating M. tuberculosis. Compounds are preincubated for ∼24 hours in cell-free nonreplicating medium and then added to replicating culture of M. tuberculosis to determine if any potential transformation products have bacteriostatic or bactericidal activity. | 28, 53 |
| Membrane depolarization assays: membrane potential (Δψ) and transmembrane proton concentration gradient (ΔpH) | To identify if the mechanism of action is related to inhibition of an enzymatic target or nonspecific depolarization of the bacterial membrane | 157, 258 |
| Intrabacterial pH | To determine if a compound impacts the ability of M. tuberculosis to regulate intrabacterial pH. Compounds active in acidic nonreplicating models often function as protonophores and decrease intrabacterial pH. This assay employs a pH-sensitive green fluorescent protein variant. | 119, 122, 124 |
| Activity against intracellular M. tuberculosis: IFN-γ-activated, bone marrow-derived murine macrophages | To determine if a compound has bactericidal activity against intracellular M. tuberculosis. Immunological stimulation of macrophages adapts the M. tuberculosis-containing phagosome to a microenvironment that is no longer conducive for exponential replication. Such conditions include acidic pH, a shift to using fatty acid carbon sources, mild hypoxia, reactive oxygen and nitrogen intermediates, itaconic acid production, metal starvation, metal intoxication, etc. | 49, 156, 231, 232 |
| CFU-based time-kill curves under both replicating and nonreplicating conditions | To enumerate viable M. tuberculosis after exposure to a test agent. The CFU assay is widely considered the gold standard to experimentally demonstrate a compound’s activity on replicating and nonreplicating bacteria. | 28, 34, 53, 100 |
| Inclusion of 0.4% (wt/vol) activated charcoal or 5% bovine serum albumin (wt/vol) in bacteriologic agar plates used to enumerate CFU assays | To avoid carryover effects when enumerating viable M. tuberculosis by a CFU assay. Dual-active molecules, and potent replicating active molecules, may artifactually display activity due to compound carryover in agar plates. Activated charcoal or bovine serum albumin can sequester carryover compound. Activated charcoal is preferred due to its ability to bind a wider range of compounds. | 30–33 |
| Deconvolution of nonreplicating assay conditions | To determine which stress, or combination of stresses, is required for a compound to kill nonreplicating M. tuberculosis | 28, 53 |
| Test activity in alternative class I and/or class II models | To identify candidate molecules with pan-activity against nonreplicating mycobacteria | 50, 51, 54, 100 |
| Determination of the Wayne Cidal Concentration (WCC90) and Loebel Cidal Concentration (LCC90) | To determine the concentration of compound that leads to killing ≥90% of the starting inoculum under hypoxic (Wayne) or nutrient starvation (Loebel) conditions | 51, 157 |
| Test for activity against nonreplicating Gram-positive and/or Gram-negative bacteria | To determine if a compound kills nonmycobacterial bacterial species under nonreplicating conditions. This is an adaptation of the standard “microbial spectrum” typically run under replicating conditions. | 28 |
| Most probable number assay | To quantitate “viable-but-not-culturable,” otherwise known as “differentially detectable,” M. tuberculosis that fails to grow on standard agar-based bacteriologic media. The ability to kill differentially detectable M. tuberculosis is considered a highly desirable property of compounds targeting nonreplicating persisters. | 10 |
These assays are used in addition to the standard postscreening assays (Table 3).
Potential Compound Transformation during Screening and Secondary Assays
As molecules progress from the initial high-throughput screen to in vivo models, there are mounting risks of wasting progressively larger amounts of time and money. Meticulous analysis of physicochemical and metabolic properties (138) of compounds is the norm in pharmaceutical companies and, unfortunately, is often pursued insufficiently in academia due to lack of experience, personnel, funds, or access to expert chemistry advice, experimental analysis, and synthesis (139).
Chemical structures can be misidentified as a result of inaccurate assembly of the compound library, erroneous dispensing of compounds, incorrect structure assignment, splashing of compounds between microtiter wells, compound degradation, and incomplete removal of reagents or catalysts used to synthesize the original compound, such as organotin, which can have antiseptic properties (140). For these reasons, it is critical to validate a molecule’s structure after cherry-pick confirmation and prior to initiating downstream hit characterization. Validation studies include testing a subset of screening hits for correct molecular mass, structure, and purity by liquid chromatography/mass spectrophotometry and nuclear magnetic resonance. Prioritized molecules should be resynthesized and re-evaluated in the original assay to confirm that they recapitulate the activity of the original hits. A surprisingly large number of screening compounds fail to meet these criteria.
Compound solubility is a problem at the forefront of high-throughput screening. The real and assumed concentrations of drug stocks can differ by several orders of magnitude (141–143). Dimethyl sulfoxide is hygroscopic and can absorb water from room air, leading to precipitation of water-insoluble compounds. Some dimethyl sulfoxide-soluble compounds precipitate immediately or over time when transferred to assay plates containing aqueous media or buffers. Antimycobacterial compounds often have high logP values (144) that favor their precipitation in aqueous solution. Compound precipitation can lead to false-negative activity or to false-positive activity in optical density-based assays.
As scientists explore more diverse bacteriologic media for whole-cell screening to mimic in vivo microenvironments and stresses, another issue arises: the chemical stability of the compounds in the assay conditions. Careful determination of the structure of a molecule under the nonreplicating assay conditions is a critical, and often overlooked, step. As illustrated in Fig. 3a, structures may be transformed by conditions found in nonreplicating assays, including acidic pH, reactive oxygen intermediates, and reactive nitrogen species. If specific transformation products can be identified, they should be tested for activity in the original model of nonreplication and for their potential toxicity to eukaryotic cells. For example, oxyphenbutazone was chemically transformed in cell-free medium used in the multistress assay of nonreplication (Fig. 3b) (53). In acidic medium containing reactive nitrogen species, the carbon on which the butyl chain attaches to the pyrazolidinedione ring was hydroxylated to form 4-hydroxy-oxyphenbutazone. This oxidation was followed by the pyrazolidinedione ring opening and formation of a quinoneimine. 4-Hydroxy-oxyphenbutazone’s quinoneimine, a Michael acceptor, reacted in vitro with glutathione and mycothiol (Fig. 3b). In live M. tuberculosis, intracellular covalent adducts formed between 4-hydroxy-oxyphenbutazone and mycothiol, N-acetyl cysteine, and other uncharacterized metabolites. 4-Hydroxy-oxyphenbutazone killed replicating M. tuberculosis and mediated some of oxyphenbutazone’s activity against nonreplicating mycobacteria. In another example, three cephalosporin analogues (one of which was compound 68) with equipotent activity against M. tuberculosis rendered nonreplicating in the multistress model had different stability profiles: two were stable, and one was unstable (145). These results suggested that their uptake into M. tuberculosis occurred more rapidly than their extracellular transformation. As this example indicates, the relevance of cell-free stability should be evaluated on a case-by-case basis.
FIGURE 3.

Compound transformation during screening assays. (a) Predicted, and experimentally validated, points of compound modification that may occur during phenotypic screening. (b) In cell-free, nonreplicating conditions imposed by the multistress model, oxyphenbutazone (left) rapidly transforms in acidic and nitrosative conditions to the intermediate, 4-hydroxy-oxyphenbutazone (center), which further transforms to 4-hydroxy-oxyphenbutazone quinoneimine (right). The electrophilic quinoneimine (red) can react at carbon atoms (green) with intrabacterial nucleophiles such as N-acetyl cysteine (NAC) and/or mycothiol (MSH).
Evaluating Bactericidal Action against Nonreplicating Mycobacteria
Replicating bacterial cultures fail to increase in biomass when treated with effective concentrations of either bacteriostatic or bactericidal molecules. This makes it relatively straightforward to recognize when compounds are active on replicating mycobacteria. Assays can be short in duration; there are many ways to assess viability; and false-positives are unlikely.
In contrast, determining the impact of compounds on nonreplicating cells is technically challenging. Nonreplicating conditions are themselves bacteriostatic, precluding the detection of viability using methods suitable for replicating cells. By coupling nonreplicating assays to a recovery phase under replicating conditions, one only obtains a rough estimation of a compound’s activity (Fig. 1) (28, 53, 54, 94, 96). In the case of dual-active molecules, one must ensure bona fide activity against the nonreplicating cells or, alternatively, determine if the nonreplicating activity is an artifact of compound carryover from the nonreplicating phase of the assay into the replicating phase of the assay (Fig. 1) (30). Carryover need not be via the fluid phase; compounds can absorb to mycobacterial components and be carried over to the replicating phase of the assay (30). As noted, drug carry-over was shown to be particularly troublesome for the extremely potent and extremely hydrophobic compound TMC207 (30, 32, 146). This is not to deny that TMC207 has utility in animal (146, 147) and human (148) tuberculosis, and in fact, drug adsorption to mycobacteria may be a useful property. For example, compounds that associate with the bacterial cell wall may deliver a potent postantibiotic effect (30) as they are slowly released into the intrabacterial cytosol. In vitro assays have arbitrary time points that are far shorter than clinical regimens and as such may grossly underestimate a drug’s bactericidal potential.
We and others have attempted to minimize carryover effects from enumerating bacilli from in vitro assays or from organs harvested from antibiotic-treated, M. tuberculosis-infected animals (31–33). One solution was to include 0.4% (wt/vol) activated charcoal in bacteriologic agar plates to rapidly and completely bind the majority of first- and second-line antimycobacterial antibiotics (30).
Many compounds with nonreplicating activity were originally identified as highly potent replicating actives. Only a few studies confirmed their nonreplicating activity with a CFU assay, and almost never in the presence of activated charcoal or bovine serum albumin in the agar plates. Given the challenge of testing large numbers of candidate dual-active molecules by the CFU assay, the charcoal agar resazurin assay was developed to rapidly categorize molecules as replicating-bacteriostatic, replicating-bactericidal, nonreplicating-bactericidal, or dual-active (that is, replicating bacteriostatic or bactericidal and nonreplicating bactericidal) (30). The charcoal agar resazurin assay helps indicate which compounds should be explored by CFU assays and at which concentrations.
Killing Class II Persisters
Molecules that reportedly kill class II phenotypically tolerant mycobacteria are structurally diverse. We have grouped approximately 100 such compounds according to core structure, potential targets, and/or method of discovery (Fig. 4, 6 to 11, and 13).
FIGURE 4.

Proof-of-concept molecules. Molecules with nonreplicating activity that serve as proof of concept include those that (a) selectively kill nonreplicating mycobacteria; (b) have dual activity, kill mycobacteria in the majority of nonreplicating models, and are effective at treating tuberculosis in animal models; and (c) have selective activity against slowly replicating or nonreplicating mycobacteria and are efficacious in tuberculosis models. n.t., not tested; *, pyrazinamide has activity against slowly replicating mycobacteria; #, experimental data indicate that pyrazinamide is inactive against intracellular mycobacteria in vitro (292, 293). However, pyrazinamide’s dependency on an acidic environment for activity, and potent in vivo activity, suggests that it kills intracellular mycobacteria during animal and human tuberculosis.
FIGURE 6a.

Replicating and nonreplicating mycobacteria may share common targets. Examples of compounds that engage standard antibiotic target pathways under replicating conditions, and also kill nonreplicating mycobacteria, include inhibitors of the biosynthesis of (a) lipids, (b) DNA, (c) RNA, (d) protein, and (e) peptidoglycan.
FIGURE 11.

Nitro-containing compounds.
FIGURE 13.

Salicylanilides are protonophores. (a) The commonly drawn structure of niclosamide (left). Compound S-13, which was used for experimental logP calculations (266), is shown for reference (right). (b) As illustrated by niclosamide, salicylanilides capture protons by forming a stable pseudo-6-membered ring via hydrogen bonding. Once inside the bacterial cell and releasing their proton, they maintain a stable anionic form from electron delocalization. Adapted from Terada (266).
The list of compounds was assembled with the intent of demonstrating both diversity and common themes. However, this is by no means a complete catalog. Additional actives can be found in databases such as SciFinder (https://scifinder.cas.org), PubChem (https://pubchem.ncbi.nlm.nih.gov), and Collaborative Drug Discovery (https://www.collaborativedrug.com) (149). Many other actives found in screening do not have their structures in scientific reports or deposited in public databases.
A relatively small number of compounds described to have bacteriostatic or bactericidal activity against replicating mycobacteria have also been tested for activity against nonreplicating bacteria. At best, most compounds were tested against mycobacteria in a single model of nonreplication. Many studies did not test the activity of the reported compounds with the gold standard CFU-based assay to determine viability.
Highly potent replicating actives may register as false-positives in nonreplicating assays due to compound carryover from the nonreplicating phase to a replicating phase (see the section “Evaluating Bactericidal Action against Nonreplicating Mycobacteria”). TMC207, which is active in multiple nonreplicating models, is an example of a compound that has a high propensity for carryover, clouding interpretation of results (30, 150). Some molecules are listed under more than one classification. For example, TMC207 is in three figures depicting structures: Fig. 4, Fig. 7, and Fig. 12.
FIGURE 7.

Quinolines.
FIGURE 12.

Compounds that depolarize the mycobacterial membrane.
The distinction between bactericidal and bacteriostatic varies significantly in the literature. For this review, we define bacteriostatic as preventing growth and affording <99% bacterial kill (<2 log10 CFU) in ≤15 days (30, 151).
Proof-of-concept molecules
A major hurdle for large-scale commitment of resources toward identifying compounds that target nonreplicating bacteria is the paucity of examples that demonstrate the success of this approach. ADEP4 (compound 48), a synthetic acyldepsipeptide that dysregulates ClpP proteolysis, may serve as a prototype (152). ADEP4 killed both S. aureus class I persisters surviving ciprofloxacin exposure and bacteria in three class II models of nonreplication: stationary phase, chemically defined minimal medium, and biofilms (153). ADEP4, when dosed with rifampin, eradicated S. aureus in a mouse thigh infection. It is unknown to what extent the activity of ADEP4 against the replicating and nonreplicating populations contributes to its in vivo efficacy (153). In the following sections we explore examples of proof-of-concept molecules active on mycobacteria.
Selective nonreplicating activity
There are few examples of molecules that fail to kill replicating mycobacteria and that kill those rendered nonreplicating in one or more in vitro models of nonreplication (Fig. 4a). Although a limited number of molecules with pan-activity against nonreplicating mycobacteria have been identified, it is likely that more would emerge if the appropriate tests were performed. Since there is a paucity of common transcriptional responses among M. tuberculosis populations rendered nonreplicating in different in vitro models, such experiments are critical. The first example of a molecule with pan-activity against nonreplicating mycobacteria was published in 2008 (100). Bryk et al. identified a rhodanine, D157070 (compound 1), from a structure activity relationship campaign to develop a prodrug inhibitor of dihydrolipoamide acyltransferase, DlaT (100, 154, 155). D157070 selectively killed Mycobacterium bovis bacillus Calmette-Guérin (BCG) and M. tuberculosis rendered nonreplicating by acidic pH and reactive nitrogen intermediates (34); hypoxia (95); a multistress model of nonreplication combining acidic pH, reactive nitrogen intermediates, hypoxia, and restriction of the carbon source to a fatty acid (53, 94); human tissue culture medium (Dulbecco’s modified Eagle medium containing 10% fetal bovine serum); and infection of bone marrow-derived macrophages activated with IFN-γ (100, 156).
Dual actives with in vivo efficacy
Dual-active molecules are defined as possessing bacteriostatic or bactericidal activity against replicating bacteria and bactericidal activity against nonreplicating bacteria. Of the dual actives, moxifloxacin (compound 2 [30, 50, 51, 96, 131, 157]), PA-824 (compound 3 [30, 50, 51, 96, 131, 150, 158]), rifampin (compound 4 [30, 50, 51, 95, 96, 131, 150, 157–162]), and TCM207 (compound 5, bedaquiline [30, 50, 51, 131, 148, 150, 157, 163, 164]) are reported to kill mycobacteria rendered nonreplicating in diverse ways, including hypoxia, nutrient starvation, stationary phase, multistress, and deprivation of streptomycin from an addicted strain (Fig. 4b). Moxifloxacin, PA-824, rifampin, and TMC207 target DNA gyrase, lipid/protein biosynthesis, RNA polymerase, and ATP synthase, respectively.
While none of the available in vitro or in vivo assays (including those described in Tables 3 and 4) can predict the efficacy of a compound in human tuberculosis, it is reasonable to prioritize compounds that have dual activity and potency against mycobacteria infecting macrophages and mice. A combination of three compounds in Fig. 4b—PA-824, moxifloxacin, and PZA (PaMZ)—showed promise in the NC001 clinical trial in tuberculosis patients (165). The 14-day NC001 early bactericidal activity study was too brief to evaluate the impact of PaMZ on eradicating persisters and decreasing relapse rates (165). The Nix-TB clinical trial is evaluating the combination of TMC207, PZA, and linezolid on multidrug-resistant and extensively drug-resistant tuberculosis and may shed light on this question by increasing the duration of treatment up to 6 to 9 months (http://www.tballiance.org/portfolio/trials).
Nonreplicating actives with in vivo efficacy
Of the molecules with selective activity against slowly replicating or nonreplicating mycobacteria, only metronidazole (compound 6) (95) and pyrazinamide (compound 7) (166) have been shown to be effective in animal models of tuberculosis (Fig. 4c). As described in the introduction, metronidazole is bactericidal to hypoxic mycobacteria, but this was only demonstrated under conditions in which no alternative electron acceptor was provided; killing was attenuated by inclusion of nitrate, a physiologic electron acceptor used by hypoxic M. tuberculosis and present in body fluids (167, 168). Activity of metronidazole did not correlate with evidence of lesion hypoxia (Table 1). Pyrazinamide is the sole representative of the nonreplicating-active class of compounds that is known to kill M. tuberculosis in humans, but pyrazinamide also kills slowly replicating mycobacteria in vitro. Pyrazinamide’s activity on M. tuberculosis under acidic conditions was enhanced by additionally including hypoxia (23) or a 3- to 10-day period of preadaptation to nutrient starvation in phosphate-buffered saline (169). While its complete set of targets is still under investigation, pyrazinamide inhibits fatty acid biosynthesis by targeting FAS-I (170–172), trans-translation by targeting ribosomal protein S1 (RpsA, encoded by rv1630) (173), and pantothenate and coenzyme A by targeting aspartate decarboxylase (PanD, encoded by rv3601c) (174, 175).
Molecules anticipated to engage canonical antibiotic targets and pathways
The potency of many dual-active molecules in Fig. 4 was lower against nonreplicating bacilli than against mycobacteria replicating in a standard bacteriologic medium. This could be due to less reliance on these processes during nonreplication, decreased uptake of the compounds due to a change in membrane composition and/or permeability (176), compound modification by the assay conditions (Fig. 3) (28, 53), increased or altered intrabacterial metabolism of the compound (116), or sequestration of the compound into lipid bodies that accumulate in mycobacteria in some in vitro models of nonreplication (28, 53, 134). Moreover, dual actives may kill nonreplicating mycobacteria by engaging noncanonical targets, or they may have a nonspecific mechanism of action (Fig. 5).
FIGURE 5.

Canonical and noncanonical targets of dual-active molecules. Dual-active molecules, which have bacteriostatic or bactericidal activity against replicating M. tuberculosis and bactericidal activity against nonreplicating M. tuberculosis, are often presumed to engage the same target under both conditions. Dual-active molecules may exert activity against nonreplicating mycobacteria via novel targets or nonspecific mechanisms. The list of dual-active molecules is not exhaustive.
The canonical targets of many compounds that kill nonreplicating mycobacteria are in pathways for the biosynthesis of the cell wall, lipids, RNA, DNA, protein, or peptidoglycan (Fig. 6). These compounds build a compelling case that nonreplicating mycobacteria engage in turnover of macromolecules. It is particularly encouraging that numerous antibiotic classes, some of whose members are approved for use in humans, including fluoroquinolones, rifamycins, macrolides, tetracyclines, and beta-lactams, have representatives that kill nonreplicating M. tuberculosis. This suggests that the antimycobacterial members of these families may likewise be tailored to display the pharmacokinetic and pharmacodynamic properties and low toxicities that allowed approval of the family members in clinical use (177).
Compounds that generate reactive oxygen species or reactive nitrogen species likely impact the function of numerous targets, including lipids, DNA, and the membrane. For example, PA-824 donates reactive nitrogen species (158). Sublethal nitric oxide induced a specific set of genes in the dos regulon, but higher concentrations of nitric oxide induced the expression of hundreds of other genes and implicated reactive nitrogen species in interfering with numerous processes (48, 178). In addition to engaging high-affinity targets, compounds like PA-824 are probably promiscuous when they achieve higher intrabacterial concentrations.
High-affinity targets may exist that have an essential function unique to mycobacteria in a nonreplicating state. However, to date, we know of no instance in which differential expression or differential essentiality of a target has been shown to explain how a compound selectively kills nonreplicating mycobacteria.
Lipid synthesis
A tetrahydrobenzothienopyrimidine (compound 8) targeting InhA killed M. tuberculosis rendered nonreplicating by hypoxia (179) (Fig. 6a). That InhA might be an essential target during hypoxia is surprising. Isoniazid, which targets InhA, does not kill hypoxic M. tuberculosis or M. tuberculosis rendered nonreplicating in other conditions. Isoniazid is even used experimentally as a control compound to confirm that cells have achieved a state of nonreplication. This raises an important question of why isoniazid fails to kill hypoxic, nonreplicating mycobacteria. The structure of isoniazid (likely the hydrazide moiety) may be unstable in hypoxia and/or other nonreplicating conditions (Fig. 3a). Perhaps KatG fails to activate isoniazid under nonreplicating conditions. To test this hypothesis, InhA inhibitors that do not require KatG activation could be tested against nonreplicating bacilli (180). Another possibility is that compound 8, like isoniazid itself, may have more than one target, but unlike isoniazid, one of the alternate targets of compound 8 may be essential in hypoxia.
PA-824 is an inhibitor of lipid and protein synthesis (181, 182). While it has multiple targets, pyrazinamide is an inhibitor of lipid biosynthesis (170–172). Both PA-824 and pyrazinamide are described in the section “Proof-of-Concept Molecules.”
DNA synthesis
Nonreplicating conditions may lead to oxidative stress, as may antibiotics with diverse primary targets (55, 66). DNA damage may result and survival may require DNA repair. Compounds that target DNA synthesis and kill nonreplicating mycobacteria are shown in Fig. 6b. Inhibitors of topoisomerase I (TopA, encoded by rv3646) (compound 9) (113) and DNA gyrase B (GyrB, encoded by rv0005) (compounds 10 and 11) (108, 112) killed M. tuberculosis rendered nonreplicating by nutrient starvation, redox stress, or hypoxia. Cyclohexyl griselimycin (compound 12), which targets the DnaN (encoded by rv0002) sliding clamp of DNA polymerase, is anticipated to kill nonreplicating M. tuberculosis due to its ability to reduce CFUs during the persistent phase of murine tuberculosis (183–185). To our knowledge, the activity of cyclohexyl griselimycin against M. tuberculosis rendered nonreplicating by in vitro models has not been explored. Multiple fluoroquinolones, whose canonical targets are DNA gyrase and/or topoisomerase IV (186), including ciprofloxacin (compound 13) (51), gatifloxacin (compound 14) (51), levofloxacin (compound 15) (51), moxifloxacin (30, 50, 51, 96, 131, 157), and sparfloxacin (compound 16) (51), killed nonreplicating M. tuberculosis (also described in the section “Quinolones and Their Derivatives”).
RNA synthesis
The transcriptomic adaptations of mycobacteria in nonreplicating conditions imply a requirement for RNA synthesis for their survival. Inhibitors of RNA polymerase (RpoB, encoded by rv0667) (Fig. 6c), including rifampin (described in the section “Proof-of-Concept Molecules”) (30, 50, 51, 95, 96, 131, 150, 157–159), rifabutin (compound 17), and rifapentine (compound 18), killed nutrient-starved and hypoxic M. tuberculosis (51, 96).
Protein synthesis
Mycobacteria are killed by a large number of compounds belonging to different structural classes and targeting diverse steps in protein biosynthesis (Fig. 6d). The newly synthesized proteins may help mycobacteria detoxify or compensate for the stresses imposed by nonreplication. In mycobacteria, protein translation is vastly decreased, but not abrogated, during the first 40 days of nonreplication (187). Numerous compounds targeting the 30S and 50S components of the ribosomal machinery killed M. tuberculosis in multiple models of nonreplication, including deprivation of strain SS18b for streptomycin, hypoxia, and nutrient starvation. The protein synthesis inhibitors included the oxazolidinones linezolid (compound 19) (103) and sutezolid (compound 20) (103); the tetracycline minocycline (compound 21) (96); the aminoglycosides amikacin (compound 22) (51, 96), streptomycin (compound 23) (50, 51, 96), and kanamycin (compound 24) (51); an aminocyclitol antibiotic, the spectinamycin analogue 1599 (compound 25) (188); the cyclic peptide antibiotic capreomycin (compound 26) (50, 51, 96); the quinoline macrolide RU66252 (compound 27) (96); and fusidic acid, which prevents elongation factor G turnover and translocation (compound 28) (96). M. tuberculosis rendered nonreplicating by incubation for 2 months in stationary phase and then acidified to pH 5.5 under mild hypoxia (1% O2) was susceptible to methionine aminopeptidase inhibitors (compounds 29 [114, 115] and 30 [114]). PA-824, previously described as disrupting lipid biosynthesis, was also shown to inhibit protein synthesis (181).
Peptidoglycan synthesis
Until recently, the dogma in the tuberculosis field was that M. tuberculosis was naturally resistant to beta-lactams. The two leading hypotheses were that beta-lactams failed to cross the mycobacterial outer membrane and that beta-lactams were susceptible to beta-lactamase cleavage (189–193). Unexpectedly, there are now multiple examples of beta-lactams and other molecules targeting steps in peptidoglycan biosynthesis that kill nonreplicating mycobacteria (Fig. 6e).
The canonical targets of beta-lactam antibiotics are enzymes catalyzing steps in peptidoglycan biosynthesis. The correlation between the bacterial replication rate and beta-lactam activity fostered the assumption that beta-lactams selectively target replicating bacteria (194). The choice of compounds for these studies led to the belief that activity was restricted to replicating cells, although some beta-lactams were identified that killed both replicating and nonreplicating Streptococcus pneumoniae and E. coli (56). The basis of dual activity remained a mystery for many years. Most bacteria contain murein predominantly composed of 4→3 transpeptides (195, 196). M. tuberculosis in stationary phase, or in hypoxia, had peptidoglycan enriched for 80% and 68% 3→3 cross-links, respectively (98, 99). These studies suggest that the peptidoglycan layer in nonreplicating cells may be different than that of replicating cells, and if so, it offers an underexplored set of target enzymes, such as the l,d-transpeptidases (197). A caveat to this conclusion, however, is that 3→3 cross-links were also enriched in replicating M. tuberculosis (∼62%) and may not be unique to nonreplicating mycobacteria (99).
A landmark paper in 2009 by Hugonnet et al. demonstrated that meropenem (compound 31), when paired with the beta-lactamase inhibitor clavulanic acid (compound 32), killed replicating M. tuberculosis (193). The Hugonnet study made a critical, and unanticipated, discovery—that the combination of meropenem and clavulanate also killed hypoxic, nonreplicating M. tuberculosis (193). A 14-day trial demonstrated that meropenem, amoxicillin, and clavulanate had marked early bactericidal activity in human tuberculosis (198).
A number of other molecules have been reported to target nonreplicating mycobacteria by disrupting steps of peptidoglycan biosynthesis. These include inhibition of the l,d-transpeptidases by faropenem (compound 33) (38, 199), UDP-galactopyranose mutase by compound 34 (200), phospho-N-acetylmuramoyl-pentapeptidetransferase (MurX) by CPZEN-45 (compound 35) (201), and the capuramycin analogue UT-01320 (compound 36) (202). CPZEN-45 may additionally target decaprenyl-phosphate-GlcNAc-1-transferase (WecA, encoded by rv1302), which has a role in synthesizing teichoic acid in Bacillus subtilis and mycoylarabinogalactan in mycobacteria (203). UT-01320 (compound 36) was bactericidal to both hypoxic and nutrient-starved M. tuberculosis (202). The structure of capuramycin (compound 37) illustrates an example in which replacing a hydroxyl group with an O-methyl (UT-01320, yellow highlighted carbon atom in Fig. 6e) confers nonreplicating activity on a molecule whose activity was restricted to replicating mycobacteria. However, UT-01320’s activity profile change was accompanied by the failure to inhibit MurX in vitro and suggests that its ability to kill nonreplicating M. tuberculosis may have been due to engaging a different target (202).
Folate synthesis
We did not find reports of nonreplicating mycobacteria being killed by inhibitors of folate biosynthesis.
Quinolines and Their Derivatives
There are numerous examples of quinolines and their derivatives that kill nonreplicating mycobacteria (Fig. 7).
Quinolines
Maintaining ATP levels is critical for mycobacteria to survive the nonreplicating state (164). TMC207, which has a quinoline core, is bacteriostatic to replicating mycobacteria and has been reported to kill those rendered nonreplicating by hypoxia, nutrient starvation, and streptomycin removal from the addicted strain SS18b (30, 50, 51, 131, 148, 150, 157, 163, 164). Due to its hydrophobic nature (logP of 7.3) and nanomolar potency, TMC207 is subject to carryover artifacts that make it challenging to evaluate its activity in nonreplicating models (30). To our knowledge, TMC207’s activity against mycobacteria in nonreplicating models has not been established by CFU enumeration under conditions that prevent drug carryover, such as the presence of 0.4% (wt/vol) activated charcoal in the bacteriologic agar (described above in “Evaluating Bactericidal Action against Nonreplicating Mycobacteria”). In our own studies, the use of activated charcoal eliminated most of the apparent activity of TMC207 against M. tuberculosis in a multistress model of nonreplication (30).
Another ATP synthase inhibitor, the substituted chloroquinoline compound 38 (159, 204), was reported to be bactericidal to hypoxic M. tuberculosis. The antimalarial drug mefloquine (compound 39) was reported to kill M. tuberculosis rendered nonreplicating by hypoxia and nutrient starvation (51). Mefloquine targets ATP synthase in S. pneumoniae (205, 206), but its target in M. tuberculosis is currently not known.
8-Hydroxyquinolines
8-Hydroxyquinolines have antibacterial activities on M. tuberculosis in vitro and in vivo (207, 208). The unsubstituted 8-hydroxyquinoline (compound 40) killed replicating M. tuberculosis and was bactericidal to M. tuberculosis rendered nonreplicating by mild hypoxia (1% O2), acid (pH 5.5), and nitrosative conditions (pH 5.5 with 0.5 mM NaNO2) (101). Compound 30, a 5-chloro, 7-bromo-substituted 8-hydroxyquinoline inhibitor of methionine aminopeptidase, killed M. tuberculosis that had been in stationary phase for 2 months (114). Some 8-hydroxyquinolines may mediate toxicity by chelating metals essential for mycobacterial survival or by forming metal-quinoline complexes that engage target enzymes (209).
4-Hydroxyquinolines
Phenotypic screening led to the discovery of mefloquine-like molecules with a 4-hydroxyquinoline core (compounds 41 and 42) that killed both replicating and hypoxic, nonreplicating M. tuberculosis (210–213). Nontoxic isoxazolecarboxylic acid ethyl ester analogues of compounds 41 and 42, represented by compound 43, killed replicating and nonreplicating hypoxic M. tuberculosis (213, 214). 2-Substituted 4-hydroxyquinoline (compounds 44 and 45) inhibitors of triacylglycerol lipase LipY (encoded by rv3097c) killed hypoxic M. tuberculosis (215). The activity of compounds 44 and 45 was specific to recovery of dormant M. tuberculosis, in which LipY plays an essential role in triacylglycerol breakdown (216). With our colleagues at Sanofi, the University of North Carolina, Memorial Sloan Kettering, and the Lankenau Institute, we identified and characterized 4-hydroxyquinolines with bactericidal activity against mycobacteria in the multistress model of nonreplication (data not shown).
Fluoroquinolones
Numerous fluoroquinolones kill nonreplicating M. tuberculosis (Fig. 8). As mentioned, moxifloxacin kills mycobacteria in numerous nonreplicating models (30, 50, 51, 96, 131, 157). Similar to moxifloxacin, other fluoroquinolones possess activity against hypoxic, nonreplicating M. tuberculosis, including ciprofloxacin (51), gatifloxacin (51), levofloxacin (51), and sparfloxacin (51).
FIGURE 8.

Quinolones.
The Proteolysis/Proteostasis Pathway
Inhibitors of the mycobacterial proteolysis and proteostasis pathways are selectively active against bacilli that are nonreplicating or have dual activity (Fig. 9). In addition to turnover of undamaged proteins, the proteolysis pathway also degrades damaged or misfolded proteins that result from exposure to stresses such as reactive nitrogen intermediates or oxidative damage (55, 217). The proteostasis pathway helps ensure proper folding of nascent, misfolded, or damaged proteins with the aid of chaperone proteins and refoldases (218). Some stresses that contribute to nonreplicating persistence engage the proteolysis and proteostasis pathways (Table 2) (55, 66, 217). As described previously, the acyldepsipeptide ADEP4 (compound 49) forces a bacterium to eat itself by unregulated digestion of intrabacterial proteins (153). Unlike the PrcBA proteasome (encoded by rv2109c and rv2110c), the ClpP1P2 proteolytic machinery (encoded by rv2461c and rv2460c) is essential for M. tuberculosis to survive under replicating conditions (219). The dual-active molecules cyclomarin A (compound 46) (220), ecumicin (compound 47) (51, 131, 157, 164, 220, 221), and lassomycin (compound 48, [cyclic(GLRRLFAD)]-QLVGRRNI-CO2CH3) (221–223), target the ClpP1P2 pathway by engaging ClpC, and kill M. tuberculosis rendered nonreplicating by hypoxia or stationary phase (220, 221, 223, 224). Ecumicin stimulates ClpC’s ATPase and impairs its activator activity, while sparing ClpP1P2’s proteolytic activity (221, 224). This results in depletion of cellular ATP (see the section “Membrane Depolarizers”). While not essential for logarithmic growth, the M. tuberculosis proteasome is required to survive stationary phase and long-term nutrient starvation (225, 226). Small-molecule inhibitors targeting the proteasome, such as GL-5 (compound 50, an irreversible inhibitor) (106) and DPLG-2 (compound 52, a reversible inhibitor) (227), killed M. tuberculosis rendered nonreplicating with acidified nitrite. Compound 51, an analogue of GL-5, had bactericidal activity against a 2-week nutrient-starved culture of M. tuberculosis (228). These studies suggest that targeting the ClpP1P2 and PrcAB proteolysis pathways may be good strategies to kill nonreplicating persisters.
FIGURE 9.
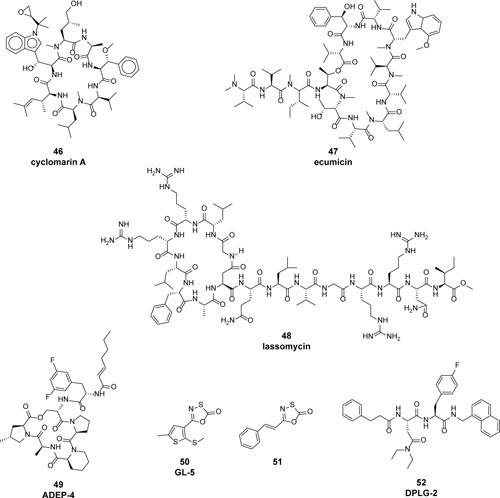
Compounds targeting the proteostasis and proteolysis pathways.
Screening Hits
There have been a limited number of phenotypic high-throughput screens to discover molecules that kill nonreplicating mycobacteria (Fig. 10). The following nonexhaustive set of examples illustrates screening methods and the molecular diversity of the hits.
FIGURE 10.

Representative compounds identified by whole-cell high-throughput screening (HTS) against mycobacteria rendered nonreplicating by (a) carbon starvation (54); (b) hypoxia (29); (c) multiple stresses, including low pH, nitric oxide and reactive nitrogen intermediates, hypoxia, and a fatty acid carbon source (28, 53, 145); (d) acidic pH (119); and (e) culture as a biofilm (102).
Carbon starvation
Grant et al. identified compounds that killed carbon-starved, nonreplicating M. tuberculosis (54) (Fig. 10a). The screen was notable for testing a set of confirmed actives against M. tuberculosis in different class I and class II models of phenotypic tolerance. This strategy revealed that the hits had diverse activities: some molecules were active only in the carbon starvation model used for the screen (compounds 53 and 54); others were active in carbon starvation and hypoxia models (compounds 55, 56, and 57); compound 58 was bactericidal to M. tuberculosis rendered nonreplicating by carbon starvation or hypoxia as well as to M. tuberculosis in a class I persister model.
Hypoxia
As noted, metronidazole kills hypoxic M. tuberculosis in vitro and can reduce CFUs in some animal models of tuberculosis (Table 1). Mak et al. set out to identify more molecules that killed nonreplicating, hypoxic M. bovis BCG (29) (Fig. 10b). The hypoxia screen was performed using a recombinant M. bovis BCG strain expressing the M. tuberculosis narGHJI operon. This strategy artificially increased ATP levels by augmenting BCG’s use of nitrate as an electron acceptor and made it easier to identify active molecules by their ability to decrease cellular ATP content. Active molecules of the benzamidazole, imidazopyridine, and thiophene classes were confirmed by a CFU assay (compounds 59, 60, and 61).
Multiple physiological stresses
One strategy to identify molecules that kill nonreplicating mycobacteria is to combine various stresses encountered by M. tuberculosis during infections of macrophages, animals, and humans (49, 53, 124, 229–245). A combination of stresses is anticipated to capture a greater diversity of screening hits than a single stress. This strategy requires a secondary hit deconvolution to identify which stress(es) are essential for a given compound’s activity. Our laboratory used this strategy to develop a multistress assay of nonreplication, in which replication of M. tuberculosis was halted by mild acidity (pH 5.0), nitric oxide, and other reactive nitrogen intermediates generated by NaNO2 at acidic pH, a fatty acid carbon source (butyrate), and mild hypoxia (1% O2). Examples of molecules active in the multistress model of nonreplication (Fig. 10c) include compounds 62, 63, 64, 65, and 66 (28); oxyphenbutazone (compound 67) (53); nitrofuranylcalanolide (compound 81) (133) (described further in the section “Nitro-Containing Compounds”); and cephalosporins (compounds 68 and 69 [147]). The cephalosporins, compounds 68 and 69, bearing a C-2 alkyl ester or oxadiazole, had clavulanate-independent bactericidal activity against M. tuberculosis in a multistress model of nonreplication (145) and killed M. tuberculosis infecting IFN-γ-activated bone marrow mouse macrophages. The unusual structures and activity profiles of compounds 68 and 69 suggest that they may engage noncanonical targets (246–249).
Acidic pH
The intraphagosomal environment of an M. tuberculosis-infected, IFN-γ-activated mouse macrophage decreases to approximately pH 4.5 (231). Furthermore, M. tuberculosis may create local acidic environments by secreting succinate when cultured under hypoxic conditions (22, 168). Using an intrabacterial pH-sensitive green fluorescent protein, Darby et al. screened for compounds that disrupted the intrabacterial pH of M. tuberculosis during incubation in growth-restricting conditions of phosphate-citrate pH 4.5 buffer (119, 122, 124) (Fig. 10d). Compounds 70, 71, 72, 40, and 73, identified in this screen, had acidic-pH-dependent bactericidal activity. High-throughput antibacterial screens, in which bacteria are incubated in an acidic pH, often identify protonophores as nonspecific disrupters of the membrane proton gradient. Monensin (compound 88 [119]) is one such example and is described in more detail in the section “Membrane Depolarizers.”
Biofilms
Many pathogenic bacteria form biofilms as a survival strategy to evade host immunity and antibiotics (250, 251). Mycobacteria form drug-tolerant biofilms in vitro (128, 252), although the relevance of mycobacterial biofilm formation in human disease is unknown. Wang et al. screened for compounds that killed nonreplicating M. smegmatis that presented as a pellicle at the interface of the bacteriologic medium and air. They identified a replicating-active molecule, TCA1 (compound 74) (Fig. 10e), that potently inhibited biofilm formation by M. smegmatis, M. tuberculosis, and M. bovis BCG and killed M. tuberculosis in a nutrient starvation model (102). TCA1 targets both decaprenyl-phosphoryl-β-d-ribose 2-oxidase (DprE1, encoded by rv3790), which synthesizes decaprenylphosphoryl-β-d-arabinose, and MoeW (encoded by rv2338c), an enzyme involved in the synthesis of a molybdenum-containing prosthetic group, the molybdenum cofactor. Under nutrient starvation conditions, overexpression of MoeW conferred partial resistance to TCA1 (102).
Nitro-Containing Compounds
A number of dual- and nonreplicating-active molecules contain a nitro functional group (Fig. 11). The strongly electronegative nitro moiety has varying degrees of reactivity that depend on its local environment within a molecule. Mycobacterial nitroreductases may catalyze the conversion of the nitro group (–NO2) by first reducing it to a nitroso (–NO), then to a hydroxylamine (–NHOH), and finally to an amine (–NH2) (253, 254). Nitrofurans and nitroimidazoles undergo intrabacterial bioactivation to metabolites that can redox-cycle and cause oxidative damage and/or dismutate to an electrophilic nitroso intermediate that reacts with intracellular thiols (255, 256). Reactive molecules such as nitrofurantoin may have specific, high-affinity targets such as ribosomal proteins yet become promiscuous at higher intrabacterial concentrations (256). The nitroso radical anion causes DNA oxidation and cell death due to DNA strand breaks (255). PA-824 donates a nitric oxide-like species that may have numerous intrabacterial targets (158, 178).
Examples of nitro-containing molecules that kill nonreplicating mycobacteria include metronidazole (19, 157, 159, 257), furaltadone (compound 75) (257), nitrofurantoin (compound 76) (96, 257), nitrofurazone (compound 77) (257), furazolidone (compound 78) (96), nitazoxanide (compound 79) (34, 50, 258), niclosamide (compound 80) (96), compound 9 (113), nitrofuranylcalanolide (compound 81) (133), OPC-67683 (compound 82) (259, 260), PA-824 (50, 51, 96, 131, 150, 158, 261), TBA-354 (compound 83) (260), and compound 84 (262).
While nitroimidazole-containing molecules such as PA-824 and OPC-67683 are in clinical trials, molecules containing the structurally similar nitrofuran moiety are considered hazardous due to the risk of DNA mutagenicity (263). Even if a molecule is nontoxic to eukaryotic cells, nitroimidazoles, nitrofurans, and nitrothiophenes should be assayed for mutagenicity (Table 4). The nitrofuranylcalanolide (compound 81) has potent MIC90 values against replicating and nonreplicating M. tuberculosis and kills M. tuberculosis infecting human macrophages (133). However, the nitrofuranylcalanolide was genotoxic in vitro (133).
Some nitro-containing molecules, such as nitazoxanide and niclosamide, are described in the next section.
Membrane Depolarizers
Nonreplicating mycobacteria maintain an energized membrane (20). During hypoxia, depolarizing the mycobacterial membrane results in the inability to synthesize ATP by disrupting the intracellular to extracellular proton gradient (157, 164). Collapsing the proton motive force, and depleting intrabacterial ATP levels, may be a common feature of molecules that target replicating and nonreplicating mycobacteria (Fig. 12) (264). The structure of a compound may not provide obvious clues that its anti-infective activity results from nonspecific depolarization of the bacterial membrane. For example, some salicylanilides such as niclosamide shuttle protons by forming a stable six-membered ring via hydrogen bonding (Fig. 13) (265–267). The hydrogen-bonded form of salicylanilide has a higher logP than its non-hydrogen-bonded structure, which is predicted to improve penetration across the lipophilic bacterial membrane. After passing into the bacterial cytosol and releasing its proton, the negatively charged salicylanilide anion, which is internally hydrogen bond stabilized, can return across the membrane again to pick up another proton (266).
Compounds that kill nonreplicating mycobacteria by depolarizing the membrane include valinomycin (compound 85) (29, 157), nigericin (compound 86) (29, 131, 157), boromycin (compound 87) (268), nitazoxanide (34, 50, 258), monensin (compound 88) (119), salinomycin (compound 89) (131), niclosamide (96), a derivative of α-mangostin, A-0016 (compound 90) (269), N,N′-dicyclohexylcarbodiimine (compound 91) (157), clofazimine (compound 92) (50, 55, 96, 270), and thioridazine (compound 93) (29, 51, 157, 159). The prodrug clofazimine is reduced by type 2 NADH-quinone oxidoreductase. Clofazimine likely kills by interfering with mycobacterial respiration by generation of hydroxyl radicals (55, 271). The bactericidal action of clofazimine is reversed by addition of menaquinone-4 (271, 272). The phenothioazines thioridazine and trifluoperazine (compound 94) target the electron transport chain, disrupt membrane potential, and ultimately decrease ATP levels (273). Trifluoperazine was bactericidal to M. tuberculosis that was nonreplicating when cultured at acidic pH, in nutrient-starved cultures, or at neutral pH in the presence of the nitric oxide donor DETA-NO (273). As described in the section on quinolines, TMC207 targets ATP synthase (AtpE, encoded by rv1305). Compound 95, which kills hypoxic M. tuberculosis, targets MenA (encoded by rv0534c) (110). Inhibition of MenA, which catalyzes the prenylation of 1,4-dihydroxy-2-naphthoate to demethylmenaquinone, is anticipated to impact membrane potential and decrease ATP levels (110). N-Octanesulfonylacetamide (OSA, compound 96) killed both replicating and hypoxic, nonreplicating M. tuberculosis (274–277). The rapid depletion in ATP levels after treating mycobacteria with compound 97 was consistent with inhibition of the ATP synthase and/or the respiratory chain. The compound n-decanesulfonylacetamide (similar to compound 96) inhibited ATP synthase and lipid biosynthesis (274, 275, 277), killed hypoxic M. bovis BCG, and had bactericidal activity against class I rifampin-tolerant persisters (276). Q203 (compound 97) targets the cytochrome bc1 complex (QcrB, encoded by rv2196), depletes ATP levels, kills replicating and hypoxic M. tuberculosis, and has activity in a mouse model of tuberculosis (278).
Dual-active protonophores boast low frequencies of resistance. Membrane depolarization, and ensuing depletion of ATP, has an amplified downstream impact on the cell that cannot be easily compensated for by mutating a single gene. In the cases of nitazoxanide, boromycin, and AM-0016, the frequencies of resistance were estimated as <1 × 10−12 (34), <1 × 10−9 (268), and <1 × 10−8 (269), respectively. Low frequencies of resistance are consistent with a nonspecific mechanism of action or multiple specific mechanisms of action (279).
ATP depletion can lead to persister formation in S. aureus (280). It will be interesting to determine if clinical use of protonophores and membrane-targeting molecules selects for live, ATP-depleted persister populations that are tolerant to other antibiotics.
More Examples of Molecules Targeting Nonreplicating Mycobacteria
Many compounds that are reported to kill nonreplicating mycobacteria do not fall into the categories described above (Fig. 14). Auranofin (compound 98), a drug used to treat rheumatoid arthritis, was recently described as a potent inhibitor of mycobacterial thioredoxin reductase TrxB2 (encoded by rv3913) and had bactericidal activity against nutrient-starved M. tuberculosis (281). While auranofin probably forms an Au(I) adduct with the cysteine active site of thioredoxin reductase, it has additional thiol targets (274, 281, 282). Compound 99 inhibits CysM (encoded by rv1336), which has a critical role in mycobacterial cysteine biosynthesis, and killed nutrient-starved M. tuberculosis (107). DevR (also called DosR, encoded by rv3133c) controls expression of genes in response to hypoxia (109, 283). A DevR inhibitor, compound 100, killed M. tuberculosis that was cultured under hypoxic conditions but spared the bacilli when they were nonreplicating during nutrient starvation (284). A 2-thiopyridine, compound 101, killed both replicating and nonreplicating hypoxic and nutrient-starved M. tuberculosis (285). The 2-thiopyridines were bactericidal to viable-but-not-culturable M. tuberculosis in a potassium starvation model (285). Compound 102, an inhibitor of pantothenate synthase (PanC, encoded by rv3602c), killed M. tuberculosis in a nutrient starvation model and killed Mycobacterium marinum infecting zebrafish (111). Compound 103 killed hypoxic M. tuberculosis (286). A quinoxaline 1,4-di-N-oxide, compound 104, displayed potent activity against replicating and hypoxic nonreplicating M. tuberculosis and was active in an acute mouse model (287).
FIGURE 14.

Additional compounds that kill nonreplicating mycobacteria.
FUTURE STUDIES AND CONCLUSIONS
Phenotypic tolerance is complex. We must refrain from projecting the biology deciphered in one persistence model to other persistence models, for fear that we oversimplify phenotypic tolerance, much as Jacques Monod oversimplified biochemical unity when he declared, “Anything found to be true of E. coli must also be true of elephants” (288). We need to focus time and resources on developing antibiotics that target mycobacteria in in vitro states that have relevance to persisters found during human tuberculosis—antibiotics whose structures are accurately understood under the conditions of the assays, that exert bona fide bactericidal activity against nonreplicating mycobacteria, and that have a structure-activity relationship which enables at least one of its derivative compounds to make it through the gauntlet of drug development, or at least to become an informative tool for chemical biology to guide our understanding of bacterial persistence (289, 290).
The challenges are formidable. Our confidence in in vitro screens is shaken by the dissociation between the high value of pyrazinamide in the clinic and its lack of activity in vitro at the highest concentrations typically considered appropriate for screening. We know many ways to put M. tuberculosis into a nonreplicating state in vitro but are not confident which states model the class II phenotypic tolerance that is hypothesized to contribute to the inefficiency of conventional drugs against tuberculosis in the human host. We need to validate compounds in animal models but are not sure which animal models (if any) qualitatively and quantitatively mimic which aspects of the human disease (42, 291). It is commonly noted that all current tuberculosis drugs work in mice, but compounds inactive in mouse models of tuberculosis have, to our knowledge, not been tested in primates or humans. A number of compounds active against replicating or nonreplicating M. tuberculosis in vitro and displaying suitable pharmacokinetics for studies in mice have failed to show efficacy in mice, but unless they were toxic, we almost never learn why they failed, or if the question is answered, the answer is almost never published. Such failures fail again when little or no insight is gained from the investment that led to the in vivo tests.
Two recent developments nonetheless justify optimism. First, academic microbiologists, immunologists, biochemists, structural biologists and physicians interested in these challenges are now working alongside professional medical chemists and pharmacologists. Second, these partnerships involve multiple academic institutions and multiple pharmaceutical companies, and the participants share their questions, hypotheses, failures, and successes as they go along.
FIGURE 6b.

Replicating and nonreplicating mycobacteria may share common targets. Examples of compounds that engage standard antibiotic target pathways under replicating conditions, and also kill nonreplicating mycobacteria, include inhibitors of the biosynthesis of (a) lipids, (b) DNA, (c) RNA, (d) protein, and (e) peptidoglycan.
SUMMARY OF KEY RECOMMENDATIONS
Numerous variables need to be considered when designing high-throughput screens against nonreplicating bacteria, including postscreening assays and how to test molecules in animal models of tuberculosis.
When compounds are reported to kill nonreplicating, phenotypically tolerant mycobacteria, the conditions need to be specified and the assumption of generalizability to other conditions avoided. Whether the compounds kill in more than one model of nonreplication needs to be determined. The structure of the compounds under the test conditions needs to be verified. That the killing took place under nonreplicating conditions, rather than upon removal of the cells from those conditions, needs to be validated.
When compounds kill bacteria under both replicating and nonreplicating conditions, it should not be assumed that the targets are the same in both cases. Conversely, it should not be assumed that a lack of killing under nonreplicating conditions means that the target of a compound that is active in replicating conditions has become dispensable when the bacteria are no longer replicating.
The field will experience substantial advances when we can test large numbers of nonreplicating-active molecules in diverse animal models and analyze and publish negative as well as positive results.
ACKNOWLEDGMENTS
We are thankful to Drs. Thulasi Warrier, Selin Somersan, Landys Lopez-Quezada, Kristin Burns-Huang, and Kyu Rhee (Weill Cornell Medicine, New York, NY); Drs. Christine Roubert, Laurent Gouilleux, Laurent Fraisse, Sophie Lagrange, and Cédric Couturier (Sanofi, Lyon, France); and Alfonso Mendoza-Losana, David Barros, and Robert Bates (GlaxoSmithKline, Tres Cantos, Spain) for insightful discussions and ideas. We are grateful to Drs. Steven Brickner (SJ Bricker Consulting, LLC), Jeff Aubé (University of North Carolina), and Ouathek Ouerfelli (Memorial Sloan Kettering, New York, NY) for invaluable discussions, ideas, and chemistry expertise. We thank S.B. for bringing the chemistry of salicylanilides to our attention. We thank T.W., S.S., K.B.H., L.L.Q., K.R., and S.B. for careful editing of the manuscript. We thank our colleagues (C.R., L.G., L.F., and C.C. at Sanofi [Lyon, France], J.A. at the University of North Carolina [Chapel Hill], O.O. and G.Y. at Memorial Sloan Kettering, and Mel Reichman at the Lankenau Institute [Wynnewood, PA]) for sharing preliminary data on 4-hydroxyquinolines. The work fostering these ideas was supported by the TB Drug Accelerator of the Bill & Melinda Gates Foundation, the Abby and Howard P. Milstein Program in Chemical Biology and Translational Medicine, and NIH TB Research Unit grant U19 AI111143. The Department of Microbiology and Immunology is supported by the William Randolph Hearst Foundation.
REFERENCES
- 1.Nathan C. 2011. Making space for anti-infective drug discovery. Cell Host Microbe 9:343–348. 10.1016/j.chom.2011.04.013 [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Davies J, Davies D. 2010. Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev 74:417–433. 10.1128/MMBR.00016-10 [PubMed][CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hobby GL, Meyer K, Chaffee E. 1942. Observations on the mechanism of action of penicillin. Exp Biol Med 50:281–285. 10.3181/00379727-50-13773 [DOI] [Google Scholar]
- 4.Bigger J. 1944. Treatment of staphylococcal infections with penicillin by intermittent sterilisation. Lancet 244:497–500. 10.1016/S0140-6736(00)74210-3 [DOI] [Google Scholar]
- 5.Hobby GL, Lenert TF. 1957. The in vitro action of antituberculous agents against multiplying and non-multiplying microbial cells. Am Rev Tuberc 76:1031–1048. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Koul A, Arnoult E, Lounis N, Guillemont J, Andries K. 2011. The challenge of new drug discovery for tuberculosis. Nature 469:483–490. 10.1038/nature09657 [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.McCune RM, Feldmann FM, Lambert HP, McDermott W. 1966. Microbial persistence. I. The capacity of tubercle bacilli to survive sterilization in mouse tissues. J Exp Med 123:445–468. 10.1084/jem.123.3.445 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scanga CA, Mohan VP, Joseph H, Yu K, Chan J, Flynn JL. 1999. Reactivation of latent tuberculosis: variations on the Cornell murine model. Infect Immun 67:4531–4538. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pai SR, Actor JK, Sepulveda E, Hunter RL Jr, Jagannath C. 2000. Identification of viable and non-viable Mycobacterium tuberculosis in mouse organs by directed RT-PCR for antigen 85B mRNA. Microb Pathog 28:335–342. 10.1006/mpat.2000.0353 [DOI] [PubMed] [Google Scholar]
- 10.Mukamolova GV, Turapov O, Malkin J, Woltmann G, Barer MR. 2010. Resuscitation-promoting factors reveal an occult population of tubercle bacilli in sputum. Am J Respir Crit Care Med 181:174–180. 10.1164/rccm.200905-0661OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chengalroyen MD, Beukes GM, Gordhan BG, Streicher EM, Churchyard G, Hafner R, Warren R, Otwombe K, Martinson N, Kana BD. 2016. Detection and quantification of differentially culturable tubercle bacteria in sputum from tuberculosis patients. Am J Respir Crit Care Med [Epub ahead of print]. 10.1164/rccm.201604-0769OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Betts JC, Lukey PT, Robb LC, McAdam RA, Duncan K. 2002. Evaluation of a nutrient starvation model of Mycobacterium tuberculosis persistence by gene and protein expression profiling. Mol Microbiol 43:717–731. 10.1046/j.1365-2958.2002.02779.x [DOI] [PubMed] [Google Scholar]
- 13.Brooks JV, Furney SK, Orme IM. 1999. Metronidazole therapy in mice infected with tuberculosis. Antimicrob Agents Chemother 43:1285–1288. PMCID: PMC89261 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carroll MW, Jeon D, Mountz JM, Lee JD, Jeong YJ, Zia N, Lee M, Lee J, Via LE, Lee S, Eum SY, Lee SJ, Goldfeder LC, Cai Y, Jin B, Kim Y, Oh T, Chen RY, Dodd LE, Gu W, Dartois V, Park SK, Kim CT, Barry CE III, Cho SN. 2013. Efficacy and safety of metronidazole for pulmonary multidrug-resistant tuberculosis. Antimicrob Agents Chemother 57:3903–3909. 10.1128/AAC.00753-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoff DR, Caraway ML, Brooks EJ, Driver ER, Ryan GJ, Peloquin CA, Orme IM, Basaraba RJ, Lenaerts AJ. 2008. Metronidazole lacks antibacterial activity in guinea pigs infected with Mycobacterium tuberculosis. Antimicrob Agents Chemother 52:4137–4140. 10.1128/AAC.00196-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin PL, Dartois V, Johnston PJ, Janssen C, Via L, Goodwin MB, Klein E, Barry CE III, Flynn JL. 2012. Metronidazole prevents reactivation of latent Mycobacterium tuberculosis infection in macaques. Proc Natl Acad Sci USA 109:14188–14193. 10.1073/pnas.1121497109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Via LE, Lin PL, Ray SM, Carrillo J, Allen SS, Eum SY, Taylor K, Klein E, Manjunatha U, Gonzales J, Lee EG, Park SK, Raleigh JA, Cho SN, McMurray DN, Flynn JL, Barry CE III. 2008. Tuberculous granulomas are hypoxic in guinea pigs, rabbits, and nonhuman primates. Infect Immun 76:2333–2340. 10.1128/IAI.01515-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wayne LG. 1994. Dormancy of Mycobacterium tuberculosis and latency of disease. Eur J Clin Microbiol Infect Dis 13:908–914. 10.1007/BF02111491 [PubMed] [DOI] [PubMed] [Google Scholar]
- 19.Wayne LG, Sramek HA. 1994. Metronidazole is bactericidal to dormant cells of Mycobacterium tuberculosis. Antimicrob Agents Chemother 38:2054–2058. 10.1128/AAC.38.9.2054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boshoff HI, Barry CE III. 2005. Tuberculosis: metabolism and respiration in the absence of growth. Nat Rev Microbiol 3:70–80. 10.1038/nrmicro1065 [PubMed] [DOI] [PubMed] [Google Scholar]
- 21.Cunningham-Bussel A, Zhang T, Nathan CF. 2013. Nitrite produced by Mycobacterium tuberculosis in human macrophages in physiologic oxygen impacts bacterial ATP consumption and gene expression. Proc Natl Acad Sci USA 110:E4256–E4265. 10.1073/pnas.1316894110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watanabe S, Zimmermann M, Goodwin MB, Sauer U, Barry CE III, Boshoff HI. 2011. Fumarate reductase activity maintains an energized membrane in anaerobic Mycobacterium tuberculosis. PLoS Pathog 7:e1002287. 10.1371/journal.ppat.1002287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wade MM, Zhang Y. 2004. Anaerobic incubation conditions enhance pyrazinamide activity against Mycobacterium tuberculosis. J Med Microbiol 53:769–773. 10.1099/jmm.0.45639-0 [DOI] [PubMed] [Google Scholar]
- 24.Coates A, Hu Y, Bax R, Page C. 2002. The future challenges facing the development of new antimicrobial drugs. Nat Rev Drug Discov 1:895–910. 10.1038/nrd940 [PubMed] [DOI] [PubMed] [Google Scholar]
- 25.Nathan C. 2012. Fresh approaches to anti-infective therapies. Sci Transl Med 4:140sr2. 10.1126/scitranslmed.3003081 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nathan C. 2015. Cooperative development of antimicrobials: looking back to look ahead. Nat Rev Microbiol 13:651–657. 10.1038/nrmicro3523 [PubMed] [DOI] [PubMed] [Google Scholar]
- 27.Nathan C, Barry CE III. 2015. TB drug development: immunology at the table. Immunol Rev 264:308–318. 10.1111/imr.12275 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Warrier T, et al. 2015. Identification of novel anti-mycobacterial compounds by screening a pharmaceutical small-molecule library against nonreplicating Mycobacterium tuberculosis. ACS Infect Dis 1:580–585. 10.1021/acsinfecdis.5b00025 [PubMed] [DOI] [PubMed] [Google Scholar]
- 29.Mak PA, Rao SP, Ping Tan M, Lin X, Chyba J, Tay J, Ng SH, Tan BH, Cherian J, Duraiswamy J, Bifani P, Lim V, Lee BH, Ling Ma N, Beer D, Thayalan P, Kuhen K, Chatterjee A, Supek F, Glynne R, Zheng J, Boshoff HI, Barry CE III, Dick T, Pethe K, Camacho LR. 2012. A high-throughput screen to identify inhibitors of ATP homeostasis in non-replicating Mycobacterium tuberculosis. ACS Chem Biol 7:1190–1197. 10.1021/cb2004884 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gold B, Roberts J, Ling Y, Quezada LL, Glasheen J, Ballinger E, Somersan-Karakaya S, Warrier T, Warren JD, Nathan C. 2015. Rapid, semi-quantitative assay to discriminate among compounds with activity against replicating or non-replicating Mycobacterium tuberculosis. Antimicrob Agents Chemother 59:6521–6538. 10.1128/AAC.00803-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grosset JH, Tyagi S, Almeida DV, Converse PJ, Li SY, Ammerman NC, Bishai WR, Enarson D, Trébucq A. 2013. Assessment of clofazimine activity in a second-line regimen for tuberculosis in mice. Am J Respir Crit Care Med 188:608–612. 10.1164/rccm.201304-0753OC [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lounis N, Gevers T, Van Den Berg J, Verhaeghe T, van Heeswijk R, Andries K. 2008. Prevention of drug carryover effects in studies assessing antimycobacterial efficacy of TMC207. J Clin Microbiol 46:2212–2215. 10.1128/JCM.00177-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tasneen R, Williams K, Amoabeng O, Minkowski A, Mdluli KE, Upton AM, Nuermberger EL. 2015. Contribution of the nitroimidazoles PA-824 and TBA-354 to the activity of novel regimens in murine models of tuberculosis. Antimicrob Agents Chemother 59:129–135. 10.1128/AAC.03822-14 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Carvalho LP, Lin G, Jiang X, Nathan C. 2009. Nitazoxanide kills replicating and nonreplicating Mycobacterium tuberculosis and evades resistance. J Med Chem 52:5789–5792. 10.1021/jm9010719 [DOI] [PubMed] [Google Scholar]
- 35.Roostalu J, Jõers A, Luidalepp H, Kaldalu N, Tenson T. 2008. Cell division in Escherichia coli cultures monitored at single cell resolution. BMC Microbiol 8:68. 10.1186/1471-2180-8-68 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Orman MA, Brynildsen MP. 2013. Dormancy is not necessary or sufficient for bacterial persistence. Antimicrob Agents Chemother 57:3230–3239. 10.1128/AAC.00243-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vega NM, Allison KR, Khalil AS, Collins JJ. 2012. Signaling-mediated bacterial persister formation. Nat Chem Biol 8:431–433. 10.1038/nchembio.915 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dhar N, Dubée V, Ballell L, Cuinet G, Hugonnet JE, Signorino-Gelo F, Barros D, Arthur M, McKinney JD. 2015. Rapid cytolysis of Mycobacterium tuberculosis by faropenem, an orally bioavailable β-lactam antibiotic. Antimicrob Agents Chemother 59:1308–1319. 10.1128/AAC.03461-14 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Balaban NQ, Merrin J, Chait R, Kowalik L, Leibler S. 2004. Bacterial persistence as a phenotypic switch. Science 305:1622–1625. 10.1126/science.1099390 [PubMed] [DOI] [PubMed] [Google Scholar]
- 40.Allison KR, Brynildsen MP, Collins JJ. 2011. Metabolite-enabled eradication of bacterial persisters by aminoglycosides. Nature 473:216–220. 10.1038/nature10069 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allison KR, Brynildsen MP, Collins JJ. 2011. Heterogeneous bacterial persisters and engineering approaches to eliminate them. Curr Opin Microbiol 14:593–598. 10.1016/j.mib.2011.09.002 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Prideaux B, Via LE, Zimmerman MD, Eum S, Sarathy J, O’Brien P, Chen C, Kaya F, Weiner DM, Chen PY, Song T, Lee M, Shim TS, Cho JS, Kim W, Cho SN, Olivier KN, Barry CE III, Dartois V. 2015. The association between sterilizing activity and drug distribution into tuberculosis lesions. Nat Med 21:1223–1227. 10.1038/nm.3937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Muttucumaru DG, Roberts G, Hinds J, Stabler RA, Parish T. 2004. Gene expression profile of Mycobacterium tuberculosis in a non-replicating state. Tuberculosis (Edinb) 84:239–246. 10.1016/j.tube.2003.12.006 [PubMed] [DOI] [PubMed] [Google Scholar]
- 44.Voskuil MI, Visconti KC, Schoolnik GK. 2004. Mycobacterium tuberculosis gene expression during adaptation to stationary phase and low-oxygen dormancy. Tuberculosis (Edinb) 84:218–227. 10.1016/j.tube.2004.02.003 [PubMed] [DOI] [PubMed] [Google Scholar]
- 45.Talaat AM, Howard ST, Hale W IV, Lyons R, Garner H, Johnston SA. 2002. Genomic DNA standards for gene expression profiling in Mycobacterium tuberculosis. Nucleic Acids Res 30:e104. 10.1093/nar/gnf103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Keren I, Minami S, Rubin E, Lewis K. 2011. Characterization and transcriptome analysis of Mycobacterium tuberculosis persisters. MBio 2:e00100–e00111. 10.1128/mBio.00100-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Benjak A, Uplekar S, Zhang M, Piton J, Cole ST, Sala C. 2016. Genomic and transcriptomic analysis of the streptomycin-dependent Mycobacterium tuberculosis strain 18b. BMC Genomics 17:190. 10.1186/s12864-016-2528-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Voskuil MI, Schnappinger D, Visconti KC, Harrell MI, Dolganov GM, Sherman DR, Schoolnik GK. 2003. Inhibition of respiration by nitric oxide induces a Mycobacterium tuberculosis dormancy program. J Exp Med 198:705–713. 10.1084/jem.20030205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schnappinger D, Ehrt S, Voskuil MI, Liu Y, Mangan JA, Monahan IM, Dolganov G, Efron B, Butcher PD, Nathan C, Schoolnik GK. 2003. Transcriptional adaptation of Mycobacterium tuberculosis within macrophages: insights into the phagosomal environment. J Exp Med 198:693–704. 10.1084/jem.20030846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Franzblau SG, DeGroote MA, Cho SH, Andries K, Nuermberger E, Orme IM, Mdluli K, Angulo-Barturen I, Dick T, Dartois V, Lenaerts AJ. 2012. Comprehensive analysis of methods used for the evaluation of compounds against Mycobacterium tuberculosis. Tuberculosis (Edinb) 92:453–488. 10.1016/j.tube.2012.07.003 [DOI] [PubMed] [Google Scholar]
- 51.Lakshminarayana SB, Huat TB, Ho PC, Manjunatha UH, Dartois V, Dick T, Rao SP. 2015. Comprehensive physicochemical, pharmacokinetic and activity profiling of anti-TB agents. J Antimicrob Chemother 70:857–867. 10.1093/jac/dku457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Xie Z, Siddiqi N, Rubin EJ. 2005. Differential antibiotic susceptibilities of starved Mycobacterium tuberculosis isolates. Antimicrob Agents Chemother 49:4778–4780. 10.1128/AAC.49.11.4778-4780.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gold B, Pingle M, Brickner SJ, Shah N, Roberts J, Rundell M, Bracken WC, Warrier T, Somersan S, Venugopal A, Darby C, Jiang X, Warren JD, Fernandez J, Ouerfelli O, Nuermberger EL, Cunningham-Bussel A, Rath P, Chidawanyika T, Deng H, Realubit R, Glickman JF, Nathan CF. 2012. Nonsteroidal anti-inflammatory drug sensitizes Mycobacterium tuberculosis to endogenous and exogenous antimicrobials. Proc Natl Acad Sci USA 109:16004–16011. 10.1073/pnas.1214188109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grant SS, Kawate T, Nag PP, Silvis MR, Gordon K, Stanley SA, Kazyanskaya E, Nietupski R, Golas A, Fitzgerald M, Cho S, Franzblau SG, Hung DT. 2013. Identification of novel inhibitors of nonreplicating Mycobacterium tuberculosis using a carbon starvation model. ACS Chem Biol 8:2224–2234. 10.1021/cb4004817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grant SS, Kaufmann BB, Chand NS, Haseley N, Hung DT. 2012. Eradication of bacterial persisters with antibiotic-generated hydroxyl radicals. Proc Natl Acad Sci USA 109:12147–12152. 10.1073/pnas.1203735109 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tuomanen E. 1986. Phenotypic tolerance: the search for beta-lactam antibiotics that kill nongrowing bacteria. Rev Infect Dis 8(Suppl 3):S279–S291. 10.1093/clinids/8.Supplement_3.S279 [PubMed] [DOI] [PubMed] [Google Scholar]
- 57.Torrey HL, Keren I, Via LE, Lee JS, Lewis K. 2016. High persister mutants in Mycobacterium tuberculosis. PLoS One 11:e0155127. 10.1371/journal.pone.0155127 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pattyn SR, Dockx P, Rollier MT, Rollier R, Saerens EJ. 1976. Mycobacterium leprae persisters after treatment with dapsone and rifampicin. Int J Lepr Other Mycobact Dis 44:154–158. [PubMed] [PubMed] [Google Scholar]
- 59.Mulcahy LR, Burns JL, Lory S, Lewis K. 2010. Emergence of Pseudomonas aeruginosa strains producing high levels of persister cells in patients with cystic fibrosis. J Bacteriol 192:6191–6199. 10.1128/JB.01651-09 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lafleur MD, Qi Q, Lewis K. 2010. Patients with long-term oral carriage harbor high-persister mutants of Candida albicans. Antimicrob Agents Chemother 54:39–44. 10.1128/AAC.00860-09 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schumacher MA, Balani P, Min J, Chinnam NB, Hansen S, Vulić M, Lewis K, Brennan RG. 2015. HipBA-promoter structures reveal the basis of heritable multidrug tolerance. Nature 524:59–64. 10.1038/nature14662 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ahmad Z, Klinkenberg LG, Pinn ML, Fraig MM, Peloquin CA, Bishai WR, Nuermberger EL, Grosset JH, Karakousis PC. 2009. Biphasic kill curve of isoniazid reveals the presence of drug-tolerant, not drug-resistant, Mycobacterium tuberculosis in the guinea pig. J Infect Dis 200:1136–1143. 10.1086/605605 [DOI] [PubMed] [Google Scholar]
- 63.Ahmad Z, Pinn ML, Nuermberger EL, Peloquin CA, Grosset JH, Karakousis PC. 2010. The potent bactericidal activity of streptomycin in the guinea pig model of tuberculosis ceases due to the presence of persisters. J Antimicrob Chemother 65:2172–2175. 10.1093/jac/dkq277 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Driver ER, Ryan GJ, Hoff DR, Irwin SM, Basaraba RJ, Kramnik I, Lenaerts AJ. 2012. Evaluation of a mouse model of necrotic granuloma formation using C3HeB/FeJ mice for testing of drugs against Mycobacterium tuberculosis. Antimicrob Agents Chemother 56:3181–3195. 10.1128/AAC.00217-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Singh R, Barry CE III, Boshoff HI. 2010. The three RelE homologs of Mycobacterium tuberculosis have individual, drug-specific effects on bacterial antibiotic tolerance. J Bacteriol 192:1279–1291. 10.1128/JB.01285-09 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nandakumar M, Nathan C, Rhee KY. 2014. Isocitrate lyase mediates broad antibiotic tolerance in Mycobacterium tuberculosis. Nat Commun 5:4306. 10.1038/ncomms5306 [PubMed] [DOI] [PubMed] [Google Scholar]
- 67.Wiuff C, Zappala RM, Regoes RR, Garner KN, Baquero F, Levin BR. 2005. Phenotypic tolerance: antibiotic enrichment of noninherited resistance in bacterial populations. Antimicrob Agents Chemother 49:1483–1494. 10.1128/AAC.49.4.1483-1494.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kim JS, Heo P, Yang TJ, Lee KS, Cho DH, Kim BT, Suh JH, Lim HJ, Shin D, Kim SK, Kweon DH. 2011. Selective killing of bacterial persisters by a single chemical compound without affecting normal antibiotic-sensitive cells. Antimicrob Agents Chemother 55:5380–5383. 10.1128/AAC.00708-11 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Black DS, Irwin B, Moyed HS. 1994. Autoregulation of hip, an operon that affects lethality due to inhibition of peptidoglycan or DNA synthesis. J Bacteriol 176:4081–4091. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Black DS, Kelly AJ, Mardis MJ, Moyed HS. 1991. Structure and organization of hip, an operon that affects lethality due to inhibition of peptidoglycan or DNA synthesis. J Bacteriol 173:5732–5739. 10.1128/jb.173.18.5732-5739.1991 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Moyed HS, Bertrand KP. 1983. hipA, a newly recognized gene of Escherichia coli K-12 that affects frequency of persistence after inhibition of murein synthesis. J Bacteriol 155:768–775. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moyed HS, Broderick SH. 1986. Molecular cloning and expression of hipA, a gene of Escherichia coli K-12 that affects frequency of persistence after inhibition of murein synthesis. J Bacteriol 166:399–403. 10.1128/jb.166.2.399-403.1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Slattery A, Victorsen AH, Brown A, Hillman K, Phillips GJ. 2013. Isolation of highly persistent mutants of Salmonella enterica serovar typhimurium reveals a new toxin-antitoxin module. J Bacteriol 195:647–657. 10.1128/JB.01397-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Maisonneuve E, Gerdes K. 2014. Molecular mechanisms underlying bacterial persisters. Cell 157:539–548. 10.1016/j.cell.2014.02.050 [PubMed][CrossRef] [DOI] [PubMed] [Google Scholar]
- 75.Lewis K. 2012. Persister cells: molecular mechanisms related to antibiotic tolerance. Handbook Exp Pharmacol 211:121–133. 10.1007/978-3-642-28951-4_8 [PubMed] [DOI] [PubMed] [Google Scholar]
- 76.Lewis K. 2010. Persister cells. Annu Rev Microbiol 64:357–372. 10.1146/annurev.micro.112408.134306 [DOI] [PubMed] [Google Scholar]
- 77.Lewis K. 2008. Multidrug tolerance of biofilms and persister cells. Curr Top Microbiol Immunol 322:107–131. 10.1007/978-3-540-75418-3_6 [DOI] [PubMed] [Google Scholar]
- 78.Lewis K. 2007. Persister cells, dormancy and infectious disease. Nat Rev Microbiol 5:48–56. 10.1038/nrmicro1557 [PubMed] [DOI] [PubMed] [Google Scholar]
- 79.Conlon BP, Rowe SE, Lewis K. 2015. Persister cells in biofilm associated infections. Adv Exp Med Biol 831:1–9. 10.1007/978-3-319-09782-4_1 [PubMed] [DOI] [PubMed] [Google Scholar]
- 80.Aldridge BB, Fernandez-Suarez M, Heller D, Ambravaneswaran V, Irimia D, Toner M, Fortune SM. 2012. Asymmetry and aging of mycobacterial cells lead to variable growth and antibiotic susceptibility. Science 335:100–104. 10.1126/science.1216166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Vaubourgeix J, Lin G, Dhar N, Chenouard N, Jiang X, Botella H, Lupoli T, Mariani O, Yang G, Ouerfelli O, Unser M, Schnappinger D, McKinney J, Nathan C. 2015. Stressed mycobacteria use the chaperone ClpB to sequester irreversibly oxidized proteins asymmetrically within and between cells. Cell Host Microbe 17:178–190. 10.1016/j.chom.2014.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Keren I, Shah D, Spoering A, Kaldalu N, Lewis K. 2004. Specialized persister cells and the mechanism of multidrug tolerance in Escherichia coli. J Bacteriol 186:8172–8180. 10.1128/JB.186.24.8172-8180.2004 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Maisonneuve E, Shakespeare LJ, Jørgensen MG, Gerdes K. 2011. Bacterial persistence by RNA endonucleases. Proc Natl Acad Sci USA 108:13206–13211. 10.1073/pnas.1100186108 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 84.Sala A, Bordes P, Genevaux P. 2014. Multiple toxin-antitoxin systems in Mycobacterium tuberculosis. Toxins (Basel) 6:1002–1020. 10.3390/toxins6031002 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Javid B, Sorrentino F, Toosky M, Zheng W, Pinkham JT, Jain N, Pan M, Deighan P, Rubin EJ. 2014. Mycobacterial mistranslation is necessary and sufficient for rifampicin phenotypic resistance. Proc Natl Acad Sci USA 111:1132–1137. 10.1073/pnas.1317580111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Su HW, Zhu JH, Li H, Cai RJ, Ealand C, Wang X, et al. 2016. The essential mycobacterial amidotransferase GatCAB is a modulator of specific translational fidelity. Nat Microbiol 1:16147. 10.1038/nmicrobiol.2016.147. PMID: 27564922. [PubMed] [DOI] [PubMed] [Google Scholar]
- 87.Dhar N, McKinney JD. 2010. Mycobacterium tuberculosis persistence mutants identified by screening in isoniazid-treated mice. Proc Natl Acad Sci USA 107:12275–12280. 10.1073/pnas.1003219107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Raj A, Peskin CS, Tranchina D, Vargas DY, Tyagi S. 2006. Stochastic mRNA synthesis in mammalian cells. PLoS Biol 4:e309. 10.1371/journal.pbio.0040309 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Maamar H, Raj A, Dubnau D. 2007. Noise in gene expression determines cell fate in Bacillus subtilis. Science 317:526–529. 10.1126/science.1140818 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wakamoto Y, Dhar N, Chait R, Schneider K, Signorino-Gelo F, Leibler S, McKinney JD. 2013. Dynamic persistence of antibiotic-stressed mycobacteria. Science 339:91–95. 10.1126/science.1229858 [PubMed] [DOI] [PubMed] [Google Scholar]
- 91.Debbia EA, Roveta S, Schito AM, Gualco L, Marchese A. 2001. Antibiotic persistence: the role of spontaneous DNA repair response. Microb Drug Res 7:335–342. 10.1089/10766290152773347. PMID: 11822773. [PubMed] [DOI] [PubMed] [Google Scholar]
- 92.Theodore A, Lewis K, Vulic M. 2013. Tolerance of Escherichia coli to fluoroquinolone antibiotics depends on specific components of the SOS response pathway. Genetics 195:1265–1276. 10.1534/genetics.113.152306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dörr T, Lewis K, Vulić M. 2009. SOS response induces persistence to fluoroquinolones in Escherichia coli. PLoS Genet 5:e1000760. 10.1371/journal.pgen.1000760 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gold B, Warrier T, Nathan C. 2015. A multi-stress model for high throughput screening against non-replicating Mycobacterium tuberculosis. In Parish T, Roberts D (ed), Mycobacteria Protocols. Methods Mol Biol 1285:293–315. 10.1007/978-1-4939-2450-9_18 [DOI] [PubMed] [Google Scholar]
- 95.Wayne LG, Hayes LG. 1996. An in vitro model for sequential study of shiftdown of Mycobacterium tuberculosis through two stages of nonreplicating persistence. Infect Immun 64:2062–2069. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cho SH, Warit S, Wan B, Hwang CH, Pauli GF, Franzblau SG. 2007. Low-oxygen-recovery assay for high-throughput screening of compounds against nonreplicating Mycobacterium tuberculosis. Antimicrob Agents Chemother 51:1380–1385. 10.1128/AAC.00055-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Schnappinger D, Schoolnik GK, Ehrt S. 2006. Expression profiling of host pathogen interactions: how Mycobacterium tuberculosis and the macrophage adapt to one another. Microbes Infect 8:1132–1140. https://www.ncbi.nlm.nih.gov/pubmed/16517202 [PubMed] [DOI] [PubMed] [Google Scholar]
- 98.Lavollay M, Arthur M, Fourgeaud M, Dubost L, Marie A, Veziris N, Blanot D, Gutmann L, Mainardi JL. 2008. The peptidoglycan of stationary-phase Mycobacterium tuberculosis predominantly contains cross-links generated by L,D-transpeptidation. J Bacteriol 190:4360–4366. 10.1128/JB.00239-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kumar P, Arora K, Lloyd JR, Lee IY, Nair V, Fischer E, Boshoff HI, Barry CE III. 2012. Meropenem inhibits D,D-carboxypeptidase activity in Mycobacterium tuberculosis. Mol Microbiol 86:367–381. 10.1111/j.1365-2958.2012.08199.x [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bryk R, Gold B, Venugopal A, Singh J, Samy R, Pupek K, Cao H, Popescu C, Gurney M, Hotha S, Cherian J, Rhee K, Ly L, Converse PJ, Ehrt S, Vandal O, Jiang X, Schneider J, Lin G, Nathan C. 2008. Selective killing of nonreplicating mycobacteria. Cell Host Microbe 3:137–145. 10.1016/j.chom.2008.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Darby CM, Nathan CF. 2010. Killing of non-replicating Mycobacterium tuberculosis by 8-hydroxyquinoline. J Antimicrob Chemother 65:1424–1427. 10.1093/jac/dkq145 [PubMed] [DOI] [PubMed] [Google Scholar]
- 102.Wang F, Sambandan D, Halder R, Wang J, Batt SM, Weinrick B, Ahmad I, Yang P, Zhang Y, Kim J, Hassani M, Huszar S, Trefzer C, Ma Z, Kaneko T, Mdluli KE, Franzblau S, Chatterjee AK, Johnsson K, Mikusova K, Besra GS, Fütterer K, Robbins SH, Barnes SW, Walker JR, Jacobs WR Jr, Schultz PG. 2013. Identification of a small molecule with activity against drug-resistant and persistent tuberculosis. Proc Natl Acad Sci USA 110:E2510–E2517. 10.1073/pnas.1309171110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhang M, Sala C, Dhar N, Vocat A, Sambandamurthy VK, Sharma S, Marriner G, Balasubramanian V, Cole ST. 2014. In vitro and in vivo activities of three oxazolidinones against nonreplicating Mycobacterium tuberculosis. Antimicrob Agents Chemother 58:3217–3223. 10.1128/AAC.02410-14 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhang M, Sala C, Hartkoorn RC, Dhar N, Mendoza-Losana A, Cole ST. 2012. Streptomycin-starved Mycobacterium tuberculosis 18b, a drug discovery tool for latent tuberculosis. Antimicrob Agents Chemother 56:5782–5789. 10.1128/AAC.01125-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bassett IM, Lun S, Bishai WR, Guo H, Kirman JR, Altaf M, O’Toole RF. 2013. Detection of inhibitors of phenotypically drug-tolerant Mycobacterium tuberculosis using an in vitro bactericidal screen. J Microbiol 51:651–658. 10.1007/s12275-013-3099-4 [DOI] [PubMed] [Google Scholar]
- 106.Lin G, Li D, de Carvalho LP, Deng H, Tao H, Vogt G, et al. 2009. Inhibitors selective for mycobacterial versus human proteasomes. Nature 461(7264):621–626. 10.1038/nature08357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Brunner K, Maric S, Reshma RS, Almqvist H, Seashore-Ludlow B, Gustavsson AL, Poyraz Ö, Yogeeswari P, Lundbäck T, Vallin M, Sriram D, Schnell R, Schneider G. 2016. Inhibitors of the cysteine synthase CysM with antibacterial potency against dormant Mycobacterium tuberculosis. J Med Chem 59:6848–6859. 10.1021/acs.jmedchem.6b00674 [DOI] [PubMed] [Google Scholar]
- 108.Chopra S, Matsuyama K, Tran T, Malerich JP, Wan B, Franzblau SG, Lun S, Guo H, Maiga MC, Bishai WR, Madrid PB. 2012. Evaluation of gyrase B as a drug target in Mycobacterium tuberculosis. J Antimicrob Chemother 67:415–421. 10.1093/jac/dkr449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Dasgupta N, Kapur V, Singh KK, Das TK, Sachdeva S, Jyothisri K, Tyagi JS. 2000. Characterization of a two-component system, devR-devS, of Mycobacterium tuberculosis. Tuber Lung Dis 80:141–159. 10.1054/tuld.2000.0240 [PubMed] [DOI] [PubMed] [Google Scholar]
- 110.Debnath J, Siricilla S, Wan B, Crick DC, Lenaerts AJ, Franzblau SG, Kurosu M. 2012. Discovery of selective menaquinone biosynthesis inhibitors against Mycobacterium tuberculosis. J Med Chem 55:3739–3755. 10.1021/jm201608g [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Samala G, Devi PB, Saxena S, Meda N, Yogeeswari P, Sriram D. 2016. Design, synthesis and biological evaluation of imidazo[2,1-b]thiazole and benzo[d]imidazo[2,1-b]thiazole derivatives as Mycobacterium tuberculosis pantothenate synthetase inhibitors. Bioorg Med Chem 24:1298–1307. 10.1016/j.bmc.2016.01.059 [DOI] [PubMed] [Google Scholar]
- 112.Shirude PS, Madhavapeddi P, Tucker JA, Murugan K, Patil V, Basavarajappa H, Raichurkar AV, Humnabadkar V, Hussein S, Sharma S, Ramya VK, Narayan CB, Balganesh TS, Sambandamurthy VK. 2013. Aminopyrazinamides: novel and specific GyrB inhibitors that kill replicating and nonreplicating Mycobacterium tuberculosis. ACS Chem Biol 8:519–523. 10.1021/cb300510w [DOI] [PubMed] [Google Scholar]
- 113.Sridevi JP, Suryadevara P, Janupally R, Sridhar J, Soni V, Anantaraju HS, et al. 2015. Identification of potential Mycobacterium tuberculosis topoisomerase I inhibitors: a study against active, dormant and resistant tuberculosis. Eur J Pharm Sci 72:81–92. 10.1016/j.ejps.2015.02.017. PMID: 25769524. [PubMed] [DOI] [PubMed] [Google Scholar]
- 114.Olaleye O, Raghunand TR, Bhat S, Chong C, Gu P, Zhou J, Zhang Y, Bishai WR, Liu JO. 2011. Characterization of clioquinol and analogues as novel inhibitors of methionine aminopeptidases from Mycobacterium tuberculosis. Tuberculosis (Edinb) 91(Suppl 1):S61–S65. 10.1016/j.tube.2011.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Olaleye O, Raghunand TR, Bhat S, He J, Tyagi S, Lamichhane G, Gu P, Zhou J, Zhang Y, Grosset J, Bishai WR, Liu JO. 2010. Methionine aminopeptidases from Mycobacterium tuberculosis as novel antimycobacterial targets. Chem Biol 17:86–97. 10.1016/j.chembiol.2009.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chakraborty S, Gruber T, Barry CE III, Boshoff HI, Rhee KY. 2013. Para-aminosalicylic acid acts as an alternative substrate of folate metabolism in Mycobacterium tuberculosis. Science 339:88–91. 10.1126/science.1228980 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Chakraborty S, Rhee KY. 2015. Tuberculosis drug development: history and evolution of the mechanism-based paradigm. Cold Spring Harb Perspect Med 5:a021147. 10.1101/cshperspect.a021147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Vocat A, Hartkoorn RC, Lechartier B, Zhang M, Dhar N, Cole ST, Sala C. 2015. Bioluminescence for assessing drug potency against nonreplicating Mycobacterium tuberculosis. Antimicrob Agents Chemother 59:4012–4019. 10.1128/AAC.00528-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Darby CM, Ingólfsson HI, Jiang X, Shen C, Sun M, Zhao N, Burns K, Liu G, Ehrt S, Warren JD, Andersen OS, Brickner SJ, Nathan C. 2013. Whole cell screen for inhibitors of pH homeostasis in Mycobacterium tuberculosis. PLoS One 8:e68942. 10.1371/journal.pone.0068942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Brook I. 1989. Inoculum effect. Rev Infect Dis 11:361–368. 10.1093/clinids/11.3.361 [PubMed] [DOI] [PubMed] [Google Scholar]
- 121.Dahl JL, Kraus CN, Boshoff HI, Doan B, Foley K, Avarbock D, Kaplan G, Mizrahi V, Rubin H, Barry CE III. 2003. The role of RelMtb-mediated adaptation to stationary phase in long-term persistence of Mycobacterium tuberculosis in mice. Proc Natl Acad Sci USA 100:10026–10031. 10.1073/pnas.1631248100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhao N, Darby CM, Small J, Bachovchin DA, Jiang X, Burns-Huang KE, Botella H, Ehrt S, Boger DL, Anderson ED, Cravatt BF, Speers AE, Fernandez-Vega V, Hodder PS, Eberhart C, Rosen H, Spicer TP, Nathan CF. 2015. Target-based screen against a periplasmic serine protease that regulates intrabacterial pH homeostasis in Mycobacterium tuberculosis. ACS Chem Biol 10:364–371. 10.1021/cb500746z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Vandal OH, Nathan CF, Ehrt S. 2009. Acid resistance in Mycobacterium tuberculosis. J Bacteriol 191:4714–4721. doi:JB.00305-09. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Vandal OH, Pierini LM, Schnappinger D, Nathan CF, Ehrt S. 2008. A membrane protein preserves intrabacterial pH in intraphagosomal Mycobacterium tuberculosis. Nat Med 14:849–854. doi:nm.1795 [pii] 10.1038/nm.1795. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Vandal OH, Roberts JA, Odaira T, Schnappinger D, Nathan CF, Ehrt S. 2009. Acid-susceptible mutants of Mycobacterium tuberculosis share hypersusceptibility to cell wall and oxidative stress and to the host environment. J Bacteriol 191:625–631. 10.1128/JB.00932-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Miesenböck G, De Angelis DA, Rothman JE. 1998. Visualizing secretion and synaptic transmission with pH-sensitive green fluorescent proteins. Nature 394:192–195. 10.1038/28190 [DOI] [PubMed] [Google Scholar]
- 127.Ackart DF, Hascall-Dove L, Caceres SM, Kirk NM, Podell BK, Melander C, Orme IM, Leid JG, Nick JA, Basaraba RJ. 2014. Expression of antimicrobial drug tolerance by attached communities of Mycobacterium tuberculosis. Pathog Dis 70:359–369. 10.1111/2049-632X.12144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Recht J, Kolter R. 2001. Glycopeptidolipid acetylation affects sliding motility and biofilm formation in Mycobacterium smegmatis. J Bacteriol 183:57185724. 10.1128/JB.183.19.5718-5724.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Recht J, Martínez A, Torello S, Kolter R. 2000. Genetic analysis of sliding motility in Mycobacterium smegmatis. J Bacteriol 182:4348–4351. 10.1128/JB.182.15.4348-4351.2000 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Piccaro G, Giannoni F, Filippini P, Mustazzolu A, Fattorini L. 2013. Activities of drug combinations against Mycobacterium tuberculosis grown in aerobic and hypoxic acidic conditions. Antimicrob Agents Chemother 57:1428–1433. 10.1128/AAC.02154-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sala C, Dhar N, Hartkoorn RC, Zhang M, Ha YH, Schneider P, Cole ST. 2010. Simple model for testing drugs against nonreplicating Mycobacterium tuberculosis. Antimicrob Agents Chemother 54:4150–4158. 10.1128/AAC.00821-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Hartkoorn RC, Ryabova OB, Chiarelli LR, Riccardi G, Makarov V, Cole ST. 2014. Mechanism of action of 5-nitrothiophenes against Mycobacterium tuberculosis. Antimicrob Agents Chemother 58:2944–2947. 10.1128/AAC.02693-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zheng P, Somersan-Karakaya S, Lu S, Roberts J, Pingle M, Warrier T, Little D, Guo X, Brickner SJ, Nathan CF, Gold B, Liu G. 2014. Synthetic calanolides with bactericidal activity against replicating and nonreplicating Mycobacterium tuberculosis. J Med Chem 57:3755–3772. 10.1021/jm4019228 [DOI] [PubMed] [Google Scholar]
- 134.Deb C, Lee CM, Dubey VS, Daniel J, Abomoelak B, Sirakova TD, Pawar S, Rogers L, Kolattukudy PE. 2009. A novel in vitro multiple-stress dormancy model for Mycobacterium tuberculosis generates a lipid-loaded, drug-tolerant, dormant pathogen. PLoS One 4:e6077. 10.1371/journal.pone.0006077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Deris JB, Kim M, Zhang Z, Okano H, Hermsen R, Groisman A, Hwa T. 2013. The innate growth bistability and fitness landscapes of antibiotic-resistant bacteria. Science 342:1237435. 10.1126/science.1237435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Salina EG, Waddell SJ, Hoffmann N, Rosenkrands I, Butcher PD, Kaprelyants AS. 2014. Potassium availability triggers Mycobacterium tuberculosis transition to, and resuscitation from, non-culturable (dormant) states. Open Biol 4:140106. 10.1098/rsob.140106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ignatov DV, Salina EG, Fursov MV, Skvortsov TA, Azhikina TL, Kaprelyants AS. 2015. Dormant non-culturable Mycobacterium tuberculosis retains stable low-abundant mRNA. BMC Genomics 16:954. 10.1186/s12864-015-2197-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kazius J, McGuire R, Bursi R. 2005. Derivation and validation of toxicophores for mutagenicity prediction. J Med Chem 48:312–320. 10.1021/jm040835a [DOI] [PubMed] [Google Scholar]
- 139.Baell JB. 2010. Observations on screening-based research and some concerning trends in the literature. Future Med Chem 2:1529–1546. 10.4155/fmc.10.237 [DOI] [PubMed] [Google Scholar]
- 140.Gold B, Deng H, Bryk R, Vargas D, Eliezer D, Roberts J, et al. 2008. Identification of a copper-binding metallothionein in pathogenic mycobacteria. Nat Chem Biol 4:609–616. doi:nchembio.109 [pii] 10.1038/nchembio.109. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kozikowski BA, Burt TM, Tirey DA, Williams LE, Kuzmak BR, Stanton DT, Morand KL, Nelson SL. 2003. The effect of freeze/thaw cycles on the stability of compounds in DMSO. J Biomol Screen 8:210–215. 10.1177/1087057103252618 [PubMed] [DOI] [PubMed] [Google Scholar]
- 142.Baillargeon P, Scampavia L, Einsteder R, Hodder P. 2011. Monitoring of HTS compound library quality via a high-resolution image acquisition and processing instrument. J Lab Autom 16:197–203. 10.1016/j.jala.2011.02.004 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Di L, Kerns EH. 2006. Biological assay challenges from compound solubility: strategies for bioassay optimization. Drug Discov Today 11:446–451. 10.1016/j.drudis.2006.03.004 [DOI] [PubMed] [Google Scholar]
- 144.Ekins S, Kaneko T, Lipinski CA, Bradford J, Dole K, Spektor A, Gregory K, Blondeau D, Ernst S, Yang J, Goncharoff N, Hohman MM, Bunin BA. 2010. Analysis and hit filtering of a very large library of compounds screened against Mycobacterium tuberculosis. Mol Biosyst 6:2316–2324. 10.1039/c0mb00104j [DOI] [PubMed] [Google Scholar]
- 145.Gold B, Smith R, Nguyen Q, Roberts J, Ling Y, Lopez Quezada L, Somersan S, Warrier T, Little D, Pingle M, Zhang D, Ballinger E, Zimmerman M, Dartois V, Hanson P, Mitscher LA, Porubsky P, Rogers S, Schoenen FJ, Nathan C, Aubé J. 2016. Novel cephalosporins selectively active on non-replicating Mycobacterium tuberculosis. J Med Chem 59:6027–6044. 10.1021/acs.jmedchem.5b01833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Williams K, Minkowski A, Amoabeng O, Peloquin CA, Taylor D, Andries K, Wallis RS, Mdluli KE, Nuermberger EL. 2012. Sterilizing activities of novel combinations lacking first- and second-line drugs in a murine model of tuberculosis. Antimicrob Agents Chemother 56:3114–3120. 10.1128/AAC.00384-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ibrahim M, Truffot-Pernot C, Andries K, Jarlier V, Veziris N. 2009. Sterilizing activity of R207910 (TMC207)-containing regimens in the murine model of tuberculosis. Am J Respir Crit Care Med 180:553–557. 10.1164/rccm.200807-1152OC [DOI] [PubMed] [Google Scholar]
- 148.Diacon AH, Pym A, Grobusch M, Patientia R, Rustomjee R, Page-Shipp L, Pistorius C, Krause R, Bogoshi M, Churchyard G, Venter A, Allen J, Palomino JC, De Marez T, van Heeswijk RP, Lounis N, Meyvisch P, Verbeeck J, Parys W, de Beule K, Andries K, Mc Neeley DF. 2009. The diarylquinoline TMC207 for multidrug-resistant tuberculosis. N Engl J Med 360:2397–2405. 10.1056/NEJMoa0808427 [DOI] [PubMed] [Google Scholar]
- 149.Hohman M, Gregory K, Chibale K, Smith PJ, Ekins S, Bunin B. 2009. Novel web-based tools combining chemistry informatics, biology and social networks for drug discovery. Drug Discov Today 14:261–270. 10.1016/j.drudis.2008.11.015 [DOI] [PubMed] [Google Scholar]
- 150.Koul A, Vranckx L, Dendouga N, Balemans W, Van den Wyngaert I, Vergauwen K, Göhlmann HW, Willebrords R, Poncelet A, Guillemont J, Bald D, Andries K. 2008. Diarylquinolines are bactericidal for dormant mycobacteria as a result of disturbed ATP homeostasis. J Biol Chem 283:25273–25280. 10.1074/jbc.M803899200 [PubMed] [DOI] [PubMed] [Google Scholar]
- 151.Heifets LB, Cynamon MH. 1991. Drug Susceptibility in the Chemotherapy of Mycobacterial Infections. CRC Press, Boca Raton, FL. [Google Scholar]
- 152.Brötz-Oesterhelt H, Beyer D, Kroll HP, Endermann R, Ladel C, Schroeder W, Hinzen B, Raddatz S, Paulsen H, Henninger K, Bandow JE, Sahl HG, Labischinski H. 2005. Dysregulation of bacterial proteolytic machinery by a new class of antibiotics. Nat Med 11:1082–1087. 10.1038/nm1306 [PubMed] [DOI] [PubMed] [Google Scholar]
- 153.Conlon BP, Nakayasu ES, Fleck LE, LaFleur MD, Isabella VM, Coleman K, Leonard SN, Smith RD, Adkins JN, Lewis K. 2013. Activated ClpP kills persisters and eradicates a chronic biofilm infection. Nature 503:365–370. 10.1038/nature12790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Tian J, Bryk R, Shi S, Erdjument-Bromage H, Tempst P, Nathan C. 2005. Mycobacterium tuberculosis appears to lack alpha-ketoglutarate dehydrogenase and encodes pyruvate dehydrogenase in widely separated genes. Mol Microbiol 57:859–868. 10.1111/j.1365-2958.2005.04741.x [DOI] [PubMed] [Google Scholar]
- 155.Bryk R, Lima CD, Erdjument-Bromage H, Tempst P, Nathan C. 2002. Metabolic enzymes of mycobacteria linked to antioxidant defense by a thioredoxin-like protein. Science 295:1073–1077. 10.1126/science.1067798 [DOI] [PubMed] [Google Scholar]
- 156.Ehrt S, Schnappinger D, Bekiranov S, Drenkow J, Shi S, Gingeras TR, Gaasterland T, Schoolnik G, Nathan C. 2001. Reprogramming of the macrophage transcriptome in response to interferon-gamma and Mycobacterium tuberculosis: signaling roles of nitric oxide synthase-2 and phagocyte oxidase. J Exp Med 194:1123–1140. 10.1084/jem.194.8.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Rao SP, Alonso S, Rand L, Dick T, Pethe K. 2008. The protonmotive force is required for maintaining ATP homeostasis and viability of hypoxic, nonreplicating Mycobacterium tuberculosis. Proc Natl Acad Sci USA 105:11945–11950. 10.1073/pnas.0711697105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Singh R, Manjunatha U, Boshoff HI, Ha YH, Niyomrattanakit P, Ledwidge R, Dowd CS, Lee IY, Kim P, Zhang L, Kang S, Keller TH, Jiricek J, Barry CE III. 2008. PA-824 kills nonreplicating Mycobacterium tuberculosis by intracellular NO release. Science 322:1392–1395. 10.1126/science.1164571 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Khan SR, Singh S, Roy KK, Akhtar MS, Saxena AK, Krishnan MY. 2013. Biological evaluation of novel substituted chloroquinolines targeting mycobacterial ATP synthase. Int J Antimicrob Agents 41:41–46. 10.1016/j.ijantimicag.2012.09.012 [DOI] [PubMed] [Google Scholar]
- 160.Herbert D, Paramasivan CN, Venkatesan P, Kubendiran G, Prabhakar R, Mitchison DA. 1996. Bactericidal action of ofloxacin, sulbactam-ampicillin, rifampin, and isoniazid on logarithmic- and stationary-phase cultures of Mycobacterium tuberculosis. Antimicrob Agents Chemother 40:2296–2299. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hu Y, Coates AR, Mitchison DA. 2003. Sterilizing activities of fluoroquinolones against rifampin-tolerant populations of Mycobacterium tuberculosis. Antimicrob Agents Chemother 47:653–657. 10.1128/AAC.47.2.653-657.2003 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hu Y, Coates A. 2012. Nonmultiplying bacteria are profoundly tolerant to antibiotics. Handbook Exp Pharmacol 211:99–119. 10.1007/978-3-642-28951-4_7 [PubMed] [DOI] [PubMed] [Google Scholar]
- 163.Andries K, Verhasselt P, Guillemont J, Göhlmann HW, Neefs JM, Winkler H, Van Gestel J, Timmerman P, Zhu M, Lee E, Williams P, de Chaffoy D, Huitric E, Hoffner S, Cambau E, Truffot-Pernot C, Lounis N, Jarlier V. 2005. A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science 307:223–227. 10.1126/science.1106753 [PubMed] [DOI] [PubMed] [Google Scholar]
- 164.Gengenbacher M, Rao SP, Pethe K, Dick T. 2010. Nutrient-starved, non-replicating Mycobacterium tuberculosis requires respiration, ATP synthase and isocitrate lyase for maintenance of ATP homeostasis and viability. Microbiology 156:81–87. 10.1099/mic.0.033084-0 [DOI] [PubMed] [Google Scholar]
- 165.Diacon AH, Dawson R, von Groote-Bidlingmaier F, Symons G, Venter A, Donald PR, van Niekerk C, Everitt D, Winter H, Becker P, Mendel CM, Spigelman MK. 2012. 14-day bactericidal activity of PA-824, bedaquiline, pyrazinamide, and moxifloxacin combinations: a randomised trial. Lancet 380:986–993. 10.1016/S0140-6736(12)61080-0 [DOI] [PubMed] [Google Scholar]
- 166.Zhang Y. 2005. The magic bullets and tuberculosis drug targets. Annu Rev Pharmacol Toxicol 45:529–564. 10.1146/annurev.pharmtox.45.120403.100120 [PubMed] [DOI] [PubMed] [Google Scholar]
- 167.Tan MP, Sequeira P, Lin WW, Phong WY, Cliff P, Ng SH, Lee BH, Camacho L, Schnappinger D, Ehrt S, Dick T, Pethe K, Alonso S. 2010. Nitrate respiration protects hypoxic Mycobacterium tuberculosis against acid- and reactive nitrogen species stresses. PLoS One 5:e13356. 10.1371/journal.pone.0013356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Eoh H, Rhee KY. 2013. Multifunctional essentiality of succinate metabolism in adaptation to hypoxia in Mycobacterium tuberculosis. Proc Natl Acad Sci USA 110:6554–6559. 10.1073/pnas.1219375110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Huang Q, Chen ZF, Li YY, Zhang Y, Ren Y, Fu Z, Xu SQ. 2007. Nutrient-starved incubation conditions enhance pyrazinamide activity against Mycobacterium tuberculosis. Chemotherapy 53:338–343. 10.1159/000107723 [PubMed] [DOI] [PubMed] [Google Scholar]
- 170.Zimhony O, Vilchèze C, Arai M, Welch JT, Jacobs WR Jr. 2007. Pyrazinoic acid and its n-propyl ester inhibit fatty acid synthase type I in replicating tubercle bacilli. Antimicrob Agents Chemother 51:752–754. 10.1128/AAC.01369-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Zimhony O, Cox JS, Welch JT, Vilchèze C, Jacobs WR Jr. 2000. Pyrazinamide inhibits the eukaryotic-like fatty acid synthetase I (FASI) of Mycobacterium tuberculosis. Nat Med 6:1043–1047. 10.1038/79558 [PubMed] [DOI] [PubMed] [Google Scholar]
- 172.Boshoff HI, Mizrahi V, Barry CE III. 2002. Effects of pyrazinamide on fatty acid synthesis by whole mycobacterial cells and purified fatty acid synthase I. J Bacteriol 184:2167–2172. 10.1128/JB.184.8.2167-2172.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Shi W, Zhang X, Jiang X, Yuan H, Lee JS, Barry CE III, Wang H, Zhang W, Zhang Y. 2011. Pyrazinamide inhibits trans-translation in Mycobacterium tuberculosis. Science 333:1630–1632. 10.1126/science.1208813 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Shi W, Chen J, Feng J, Cui P, Zhang S, Weng X, Zhang W, Zhang Y. 2014. Aspartate decarboxylase (PanD) as a new target of pyrazinamide in Mycobacterium tuberculosis. Emerg Microbes Infect 3:e58. 10.1038/emi.2014.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Dillon NA, Peterson ND, Rosen BC, Baughn AD. 2014. Pantothenate and pantetheine antagonize the antitubercular activity of pyrazinamide. Antimicrob Agents Chemother 58:7258–7263. 10.1128/AAC.04028-14 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sarathy J, Dartois V, Dick T, Gengenbacher M. 2013. Reduced drug uptake in phenotypically resistant nutrient-starved nonreplicating Mycobacterium tuberculosis. Antimicrob Agents Chemother 57:1648–1653. 10.1128/AAC.02202-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Payne DJ, Gwynn MN, Holmes DJ, Pompliano DL. 2007. Drugs for bad bugs: confronting the challenges of antibacterial discovery. Nat Rev Drug Discov 6:29–40. 10.1038/nrd2201 [DOI] [PubMed] [Google Scholar]
- 178.Rhee KY, Erdjument-Bromage H, Tempst P, Nathan CF. 2005. S-nitroso proteome of Mycobacterium tuberculosis: enzymes of intermediary metabolism and antioxidant defense. Proc Natl Acad Sci USA 102:467–472. 10.1073/pnas.0406133102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Vilchèze C, Baughn AD, Tufariello J, Leung LW, Kuo M, Basler CF, Alland D, Sacchettini JC, Freundlich JS, Jacobs WR Jr. 2011. Novel inhibitors of InhA efficiently kill Mycobacterium tuberculosis under aerobic and anaerobic conditions. Antimicrob Agents Chemother 55:3889–3898. 10.1128/AAC.00266-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Martínez-Hoyos M, Perez-Herran E, Gulten G, Encinas L, Álvarez-Gómez D, Alvarez E, Ferrer-Bazaga S, García-Pérez A, Ortega F, Angulo-Barturen I, Rullas-Trincado J, Blanco Ruano D, Torres P, Castañeda P, Huss S, Fernández Menéndez R, González Del Valle S, Ballell L, Barros D, Modha S, Dhar N, Signorino-Gelo F, McKinney JD, García-Bustos JF, Lavandera JL, Sacchettini JC, Jimenez MS, Martín-Casabona N, Castro-Pichel J, Mendoza-Losana A. 2016. Antitubercular drugs for an old target: GSK693 as a promising InhA direct inhibitor. EBioMedicine 8:291–301. 10.1016/j.ebiom.2016.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Stover CK, Warrener P, VanDevanter DR, Sherman DR, Arain TM, Langhorne MH, Anderson SW, Towell JA, Yuan Y, McMurray DN, Kreiswirth BN, Barry CE, Baker WR. 2000. A small-molecule nitroimidazopyran drug candidate for the treatment of tuberculosis. Nature 405:962–966. 10.1038/35016103 [DOI] [PubMed] [Google Scholar]
- 182.Manjunatha U, Boshoff HI, Barry CE. 2009. The mechanism of action of PA-824: novel insights from transcriptional profiling. Commun Integr Biol 2:215–218. 10.4161/cib.2.3.7926 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Machaba KE, Cele FN, Mhlongo NN, Soliman ME. 2016. Sliding clamp of DNA polymerase III as a drug target for TB therapy: comprehensive conformational and binding analysis from molecular dynamic simulations. Cell Biochem Biophys [Epub ahead of print]. 10.1007/s12013-016-0764-3 [DOI] [PubMed] [Google Scholar]
- 184.Kling A, Lukat P, Almeida DV, Bauer A, Fontaine E, Sordello S, Zaburannyi N, Herrmann J, Wenzel SC, König C, Ammerman NC, Barrio MB, Borchers K, Bordon-Pallier F, Brönstrup M, Courtemanche G, Gerlitz M, Geslin M, Hammann P, Heinz DW, Hoffmann H, Klieber S, Kohlmann M, Kurz M, Lair C, Matter H, Nuermberger E, Tyagi S, Fraisse L, Grosset JH, Lagrange S, Müller R. 2015. Antibiotics. Targeting DnaN for tuberculosis therapy using novel griselimycins. Science 348:1106–1112. 10.1126/science.aaa4690 [DOI] [PubMed] [Google Scholar]
- 185.Herrmann J, Lukežič T, Kling A, Baumann S, Hüttel S, Petković H, Müller R. 2016. Strategies for the discovery and development of new antibiotics from natural products: three case studies. Curr Top Microbiol Immunol [Epub ahead of print] 10.1007/82_2016_498 [DOI] [PubMed] [Google Scholar]
- 186.Higgins PG, Fluit AC, Schmitz FJ. 2003. Fluoroquinolones: structure and target sites. Curr Drug Targets 4:181–190. 10.2174/1389450033346920 [DOI] [PubMed] [Google Scholar]
- 187.Hu YM, Butcher PD, Sole K, Mitchison DA, Coates AR. 1998. Protein synthesis is shutdown in dormant Mycobacterium tuberculosis and is reversed by oxygen or heat shock. FEMS Microbiol Lett 158:139–145. 10.1111/j.1574-6968.1998.tb12813.x [PubMed] [DOI] [PubMed] [Google Scholar]
- 188.Lee RE, Hurdle JG, Liu J, Bruhn DF, Matt T, Scherman MS, Vaddady PK, Zheng Z, Qi J, Akbergenov R, Das S, Madhura DB, Rathi C, Trivedi A, Villellas C, Lee RB, Rakesh, Waidyarachchi SL, Sun D, McNeil MR, Ainsa JA, Boshoff HI, Gonzalez-Juarrero M, Meibohm B, Böttger EC, Lenaerts AJ. 2014. Spectinamides: a new class of semisynthetic antituberculosis agents that overcome native drug efflux. Nat Med 20:152–158. 10.1038/nm.3458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Jarlier V, Nikaido H. 1990. Permeability barrier to hydrophilic solutes in Mycobacterium chelonei. J Bacteriol 172:1418–1423. 10.1128/jb.172.3.1418-1423.1990 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kasik JE. 1965. The nature of mycobacterial penicillinase. Am Rev Respir Dis 91:117–119. 10.1164/arrd.1965.91.1.117 [DOI] [PubMed] [Google Scholar]
- 191.Jarlier V, Gutmann L, Nikaido H. 1991. Interplay of cell wall barrier and beta-lactamase activity determines high resistance to beta-lactam antibiotics in Mycobacterium chelonae. Antimicrob Agents Chemother 35:1937–1939. 10.1128/AAC.35.9.1937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Finch R. 1986. Beta-lactam antibiotics and mycobacteria. J Antimicrob Chemother 18:6–8. 10.1093/jac/18.1.6 [DOI] [PubMed] [Google Scholar]
- 193.Hugonnet JE, Tremblay LW, Boshoff HI, Barry CE III, Blanchard JS. 2009. Meropenem-clavulanate is effective against extensively drug-resistant Mycobacterium tuberculosis. Science 323:1215–1218. 10.1126/science.1167498 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Tuomanen E, Cozens R, Tosch W, Zak O, Tomasz A. 1986. The rate of killing of Escherichia coli by beta-lactam antibiotics is strictly proportional to the rate of bacterial growth. J Gen Microbiol 132:1297–1304 10.1099/00221287-132-5-1297. [PubMed] [DOI] [PubMed] [Google Scholar]
- 195.Schoonmaker MK, Bishai WR, Lamichhane G. 2014. Nonclassical transpeptidases of Mycobacterium tuberculosis alter cell size, morphology, the cytosolic matrix, protein localization, virulence, and resistance to β-lactams. J Bacteriol 196:1394–1402. 10.1128/JB.01396-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Vollmer W, Höltje JV. 2004. The architecture of the murein (peptidoglycan) in gram-negative bacteria: vertical scaffold or horizontal layer(s)? J Bacteriol 186:5978–5987. 10.1128/JB.186.18.5978-5987.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Gupta R, Lavollay M, Mainardi JL, Arthur M, Bishai WR, Lamichhane G. 2010. The Mycobacterium tuberculosis protein LdtMt2 is a nonclassical transpeptidase required for virulence and resistance to amoxicillin. Nat Med 16:466–469. 10.1038/nm.2120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Diacon AH, van der Merwe L, Barnard M, von Groote-Bidlingmaier F, Lange C, García-Basteiro AL, Sevene E, Ballell L, Barros-Aguirre D. 2016. β-Lactams against tuberculosis—new trick for an old dog? N Engl J Med 375:393–394. 10.1056/NEJMc1513236. [DOI] [PubMed] [Google Scholar]
- 199.Solapure S, Dinesh N, Shandil R, Ramachandran V, Sharma S, Bhattacharjee D, Ganguly S, Reddy J, Ahuja V, Panduga V, Parab M, Vishwas KG, Kumar N, Balganesh M, Balasubramanian V. 2013. In vitro and in vivo efficacy of β-lactams against replicating and slowly growing/nonreplicating Mycobacterium tuberculosis. Antimicrob Agents Chemother 57:2506–2510. 10.1128/AAC.00023-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Borrelli S, Zandberg WF, Mohan S, Ko M, Martinez-Gutierrez F, Partha SK, Sanders DA, Av-Gay Y, Pinto BM. 2010. Antimycobacterial activity of UDP-galactopyranose mutase inhibitors. Int J Antimicrob Agents 36:364–368. 10.1016/j.ijantimicag.2010.06.030 [DOI] [PubMed] [Google Scholar]
- 201.Engohang-Ndong J. 2012. Antimycobacterial drugs currently in Phase II clinical trials and preclinical phase for tuberculosis treatment. Expert Opin Investig Drugs 21:1789–1800. 10.1517/13543784.2012.724397 [DOI] [PubMed] [Google Scholar]
- 202.Siricilla S, Mitachi K, Wan B, Franzblau SG, Kurosu M. 2015. Discovery of a capuramycin analog that kills nonreplicating Mycobacterium tuberculosis and its synergistic effects with translocase I inhibitors. J Antibiot (Tokyo) 68:271–278. 10.1038/ja.2014.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Ishizaki Y, Hayashi C, Inoue K, Igarashi M, Takahashi Y, Pujari V, Crick DC, Brennan PJ, Nomoto A. 2013. Inhibition of the first step in synthesis of the mycobacterial cell wall core, catalyzed by the GlcNAc-1-phosphate transferase WecA, by the novel caprazamycin derivative CPZEN-45. J Biol Chem 288:30309–30319. 10.1074/jbc.M113.492173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Singh S, Roy KK, Khan SR, Kashyap VK, Sharma A, Jaiswal S, Sharma SK, Krishnan MY, Chaturvedi V, Lal J, Sinha S, Dasgupta A, Srivastava R, Saxena AK. 2015. Novel, potent, orally bioavailable and selective mycobacterial ATP synthase inhibitors that demonstrated activity against both replicating and non-replicating M. tuberculosis. Bioorg Med Chem 23:742–752. 10.1016/j.bmc.2014.12.060 [DOI] [PubMed] [Google Scholar]
- 205.Danelishvili L, Wu M, Young LS, Bermudez LE. 2005. Genomic approach to identifying the putative target of and mechanisms of resistance to mefloquine in mycobacteria. Antimicrob Agents Chemother 49:3707–3714. 10.1128/AAC.49.9.3707-3714.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Martín-Galiano AJ, Gorgojo B, Kunin CM, de la Campa AG. 2002. Mefloquine and new related compounds target the F(0) complex of the F(0)F(1) H(+)-ATPase of Streptococcus pneumoniae. Antimicrob Agents Chemother 46:1680–1687. 10.1128/AAC.46.6.1680-1687.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Hongmanee P, Rukseree K, Buabut B, Somsri B, Palittapongarnpim P. 2007. In vitro activities of cloxyquin (5-chloroquinolin-8-ol) against Mycobacterium tuberculosis. Antimicrob Agents Chemother 51:1105–1106. 10.1128/AAC.01310-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Tison F. 1952. [The remarkable effect of a combination of iodochloroxyquinoline with a subactive dose of streptomycin on experimental tuberculosis in guinea pigs]. Ann Inst Pasteur (Paris) 83:275–276. [PubMed] [Google Scholar]
- 209.Shah S, Dalecki AG, Malalasekera AP, Crawford CL, Michalek SM, Kutsch O, Sun J, Bossmann SH, Wolschendorf F. 2016. 8-Hydroxyquinolines are boosting-agents of copper related toxicity in Mycobacterium tuberculosis. Antimicrob Agents Chemother 60:5765–5776. 10.1128/AAC.00325-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Mao J, Wang Y, Wan B, Kozikowski AP, Franzblau SG. 2007. Design, synthesis, and pharmacological evaluation of mefloquine-based ligands as novel antituberculosis agents. ChemMedChem 2:1624–1630. 10.1002/cmdc.200700112 [DOI] [PubMed] [Google Scholar]
- 211.Mao J, Yuan H, Wang Y, Wan B, Pieroni M, Huang Q, van Breemen RB, Kozikowski AP, Franzblau SG. 2009. From serendipity to rational antituberculosis drug discovery of mefloquine-isoxazole carboxylic acid esters. J Med Chem 52:6966–6978. 10.1021/jm900340a [DOI] [PubMed] [Google Scholar]
- 212.Jayaprakash S, Iso Y, Wan B, Franzblau SG, Kozikowski AP. 2006. Design, synthesis, and SAR studies of mefloquine-based ligands as potential antituberculosis agents. ChemMedChem 1:593–597. 10.1002/cmdc.200600010 [PubMed] [DOI] [PubMed] [Google Scholar]
- 213.Lilienkampf A, Mao J, Wan B, Wang Y, Franzblau SG, Kozikowski AP. 2009. Structure-activity relationships for a series of quinoline-based compounds active against replicating and nonreplicating Mycobacterium tuberculosis. J Med Chem 52:2109–2118. 10.1021/jm900003c [DOI] [PubMed] [Google Scholar]
- 214.Lilienkampf A, Pieroni M, Wan B, Wang Y, Franzblau SG, Kozikowski AP. 2010. Rational design of 5-phenyl-3-isoxazolecarboxylic acid ethyl esters as growth inhibitors of Mycobacterium tuberculosis. a potent and selective series for further drug development. J Med Chem 53:678–688. 10.1021/jm901273n [DOI] [PubMed] [Google Scholar]
- 215.Saxena AK, Roy KK, Singh S, Vishnoi SP, Kumar A, Kashyap VK, Kremer L, Srivastava R, Srivastava BS. 2013. Identification and characterisation of small-molecule inhibitors of Rv3097c-encoded lipase (LipY) of Mycobacterium tuberculosis that selectively inhibit growth of bacilli in hypoxia. Int J Antimicrob Agents 42:27–35. 10.1016/j.ijantimicag.2013.03.007 [PubMed] [DOI] [PubMed] [Google Scholar]
- 216.Low KL, Rao PS, Shui G, Bendt AK, Pethe K, Dick T, Wenk MR. 2009. Triacylglycerol utilization is required for regrowth of in vitro hypoxic nonreplicating Mycobacterium bovis bacillus Calmette-Guerin. J Bacteriol 191:5037–5043. 10.1128/JB.00530-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Darwin KH, Ehrt S, Gutierrez-Ramos JC, Weich N, Nathan CF. 2003. The proteasome of Mycobacterium tuberculosis is required for resistance to nitric oxide. Science 302:1963–1966. 10.1126/science.1091176 [PubMed] [DOI] [PubMed] [Google Scholar]
- 218.Fay A, Glickman MS. 2014. An essential nonredundant role for mycobacterial DnaK in native protein folding. PLoS Genet 10:e1004516. 10.1371/journal.pgen.1004516 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Raju RM, Unnikrishnan M, Rubin DH, Krishnamoorthy V, Kandror O, Akopian TN, Goldberg AL, Rubin EJ. 2012. Mycobacterium tuberculosis ClpP1 and ClpP2 function together in protein degradation and are required for viability in vitro and during infection. PLoS Pathog 8:e1002511. 10.1371/journal.ppat.1002511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Schmitt EK, Riwanto M, Sambandamurthy V, Roggo S, Miault C, Zwingelstein C, Krastel P, Noble C, Beer D, Rao SP, Au M, Niyomrattanakit P, Lim V, Zheng J, Jeffery D, Pethe K, Camacho LR. 2011. The natural product cyclomarin kills Mycobacterium tuberculosis by targeting the ClpC1 subunit of the caseinolytic protease. Angew Chem Int Ed Engl 50:5889–5891. 10.1002/anie.201101740 [DOI] [PubMed] [Google Scholar]
- 221.Lee H, Suh JW. 2016. Anti-tuberculosis lead molecules from natural products targeting Mycobacterium tuberculosis ClpC1. J Ind Microbiol Biotechnol 43:205–212. 10.1007/s10295-015-1709-3 [DOI] [PubMed] [Google Scholar]
- 222.Lear S, Munshi T, Hudson AS, Hatton C, Clardy J, Mosely JA, Bull TJ, Sit CS, Cobb SL. 2016. Total chemical synthesis of lassomycin and lassomycin-amide. Org Biomol Chem 14:4534–4541. 10.1039/C6OB00631K [PubMed] [DOI] [PubMed] [Google Scholar]
- 223.Gavrish E, Sit CS, Cao S, Kandror O, Spoering A, Peoples A, Ling L, Fetterman A, Hughes D, Bissell A, Torrey H, Akopian T, Mueller A, Epstein S, Goldberg A, Clardy J, Lewis K. 2014. Lassomycin, a ribosomally synthesized cyclic peptide, kills mycobacterium tuberculosis by targeting the ATP-dependent protease ClpC1P1P2. Chem Biol 21:509–518. 10.1016/j.chembiol.2014.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Gao W, Kim JY, Anderson JR, Akopian T, Hong S, Jin YY, Kandror O, Kim JW, Lee IA, Lee SY, McAlpine JB, Mulugeta S, Sunoqrot S, Wang Y, Yang SH, Yoon TM, Goldberg AL, Pauli GF, Suh JW, Franzblau SG, Cho S. 2015. The cyclic peptide ecumicin targeting ClpC1 is active against Mycobacterium tuberculosis in vivo. Antimicrob Agents Chemother 59:880–889. 10.1128/AAC.04054-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Gandotra S, Schnappinger D, Monteleone M, Hillen W, Ehrt S. 2007. In vivo gene silencing identifies the Mycobacterium tuberculosis proteasome as essential for the bacteria to persist in mice. Nat Med 13:1515–1520. doi:nm1683 [pii] 10.1038/nm1683. PMID: 18059281. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Gandotra S, Lebron MB, Ehrt S. 2010. The Mycobacterium tuberculosis proteasome active site threonine is essential for persistence yet dispensable for replication and resistance to nitric oxide. PLoS Pathog 6:e1001040. 10.1371/journal.ppat.1001040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Lin G, Chidawanyika T, Tsu C, Warrier T, Vaubourgeix J, Blackburn C, Gigstad K, Sintchak M, Dick L, Nathan C. 2013. N,C-Capped dipeptides with selectivity for mycobacterial proteasome over human proteasomes: role of S3 and S1 binding pockets. J Am Chem Soc 135:9968–9971. 10.1021/ja400021x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Russo F, Gising J, Åkerbladh L, Roos AK, Naworyta A, Mowbray SL, Sokolowski A, Henderson I, Alling T, Bailey MA, Files M, Parish T, Karlén A, Larhed M. 2015. Optimization and evaluation of 5-styryl-oxathiazol-2-one Mycobacterium tuberculosis proteasome inhibitors as potential antitubercular agents. ChemistryOpen 4:342–362. 10.1002/open.201500001 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Timm J, Post FA, Bekker LG, Walther GB, Wainwright HC, Manganelli R, Chan WT, Tsenova L, Gold B, Smith I, Kaplan G, McKinney JD. 2003. Differential expression of iron-, carbon-, and oxygen-responsive mycobacterial genes in the lungs of chronically infected mice and tuberculosis patients. Proc Natl Acad Sci USA 100:14321–14326. 10.1073/pnas.2436197100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Wolschendorf F, Ackart D, Shrestha TB, Hascall-Dove L, Nolan S, Lamichhane G, Wang Y, Bossmann SH, Basaraba RJ, Niederweis M. 2011. Copper resistance is essential for virulence of Mycobacterium tuberculosis. Proc Natl Acad Sci USA 108:1621–1626. 10.1073/pnas.1009261108 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.MacMicking JD, Taylor GA, McKinney JD. 2003. Immune control of tuberculosis by IFN-gamma-inducible LRG-47. Science 302:654–659. 10.1126/science.1088063 [PubMed] [DOI] [PubMed] [Google Scholar]
- 232.MacMicking JD, North RJ, LaCourse R, Mudgett JS, Shah SK, Nathan CF. 1997. Identification of nitric oxide synthase as a protective locus against tuberculosis. Proc Natl Acad Sci USA 94:5243–5248. 10.1073/pnas.94.10.5243 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Marrero J, Rhee KY, Schnappinger D, Pethe K, Ehrt S. 2010. Gluconeogenic carbon flow of tricarboxylic acid cycle intermediates is critical for Mycobacterium tuberculosis to establish and maintain infection. Proc Natl Acad Sci USA 107:9819–9824. 10.1073/pnas.1000715107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Gomez JE, McKinney JD. 2004. M. tuberculosis persistence, latency, and drug tolerance. Tuberculosis (Edinb) 84(1-2):29–44. doi:S1472979203000866 [pii]. PMID: 14670344. [PubMed] [DOI] [PubMed] [Google Scholar]
- 235.Manina G, Dhar N, McKinney JD. 2015. Stress and host immunity amplify Mycobacterium tuberculosis phenotypic heterogeneity and induce nongrowing metabolically active forms. Cell Host Microbe 17:32–46. 10.1016/j.chom.2014.11.016 [DOI] [PubMed] [Google Scholar]
- 236.Munoz-Elias EJ, McKinney JD. 2005. Mycobacterium tuberculosis isocitrate lyases 1 and 2 are jointly required for in vivo growth and virulence. Nat Med 11:638–644. doi:nm1252 [pii] 10.1038/nm1252. PMID: 15895072. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Munoz-Elias EJ, McKinney JD. 2006. Carbon metabolism of intracellular bacteria. Cell Microbiol 8:10–22. doi:CMI648 [pii] 10.1111/j.1462-5822.2005.00648.x. PMID: 16367862. [PubMed] [DOI] [PubMed] [Google Scholar]
- 238.Berney M, Berney-Meyer L, Wong KW, Chen B, Chen M, Kim J, Wang J, Harris D, Parkhill J, Chan J, Wang F, Jacobs WR Jr. 2015. Essential roles of methionine and S-adenosylmethionine in the autarkic lifestyle of Mycobacterium tuberculosis. Proc Natl Acad Sci USA 112:10008–10013. 10.1073/pnas.1513033112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Hondalus MK, Bardarov S, Russell R, Chan J, Jacobs WR Jr, Bloom BR. 2000. Attenuation of and protection induced by a leucine auxotroph of Mycobacterium tuberculosis. Infect Immun 68:2888–2898. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC97501/ [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Sambandamurthy VK, Wang X, Chen B, Russell RG, Derrick S, Collins FM, Morris SL, Jacobs WR Jr. 2002. A pantothenate auxotroph of Mycobacterium tuberculosis is highly attenuated and protects mice against tuberculosis. Nat Med 8:1171–1174. 10.1038/nm765 [DOI] [PubMed] [Google Scholar]
- 241.Rodriguez GM, Smith I. 2003. Mechanisms of iron regulation in mycobacteria: role in physiology and virulence. Mol Microbiol 47:1485–1494. 10.1046/j.1365-2958.2003.03384.x [DOI] [PubMed] [Google Scholar]
- 242.Gould TA, van de Langemheen H, Munoz-Elias EJ, McKinney JD, Sacchettini JC. 2006. Dual role of isocitrate lyase 1 in the glyoxylate and methylcitrate cycles in Mycobacterium tuberculosis. Mol Microbiol 61:940–947. doi:MMI5297 [pii] 10.1111/j.1365-2958.2006.05297.x. PMID: 16879647. [PubMed] [DOI] [PubMed] [Google Scholar]
- 243.Walters SB, Dubnau E, Kolesnikova I, Laval F, Daffe M, Smith I. 2006. The Mycobacterium tuberculosis PhoPR two-component system regulates genes essential for virulence and complex lipid biosynthesis. Mol Microbiol 60:312–330. doi:MMI5102 [pii] 10.1111/j.1365-2958.2006.05102.x. PMID: 16573683. [PubMed] [DOI] [PubMed] [Google Scholar]
- 244.Miner MD, Chang JC, Pandey AK, Sassetti CM, Sherman DR. 2009. Role of cholesterol in Mycobacterium tuberculosis infection. Indian J Exp Biol 47:407–411. [PubMed] [PubMed] [Google Scholar]
- 245.Belton M, Brilha S, Manavaki R, Mauri F, Nijran K, Hong YT, Patel NH, Dembek M, Tezera L, Green J, Moores R, Aigbirhio F, Al-Nahhas A, Fryer TD, Elkington PT, Friedland JS. 2016. Hypoxia and tissue destruction in pulmonary TB. Thorax [Epub ahead of print] thoraxjnl-2015-207402. 10.1136/thoraxjnl-2015-207402 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Sperka T, Pitlik J, Bagossi P, Tözsér J. 2005. Beta-lactam compounds as apparently uncompetitive inhibitors of HIV-1 protease. Bioorg Med Chem Lett 15:3086–3090. 10.1016/j.bmcl.2005.04.020 [DOI] [PubMed] [Google Scholar]
- 247.Powers JC, Asgian JL, Ekici OD, James KE. 2002. Irreversible inhibitors of serine, cysteine, and threonine proteases. Chem Rev 102:4639–4750. 10.1021/cr010182v [DOI] [PubMed] [Google Scholar]
- 248.Paetzel M, Dalbey RE, Strynadka NC. 1998. Crystal structure of a bacterial signal peptidase in complex with a beta-lactam inhibitor. Nature 396:186–190. 10.1038/25403 [DOI] [PubMed] [Google Scholar]
- 249.Baranowski C, Rubin EJ. 2016. Could killing bacterial subpopulations hit tuberculosis out of the park? J Med Chem 59:6025–6026. 10.1021/acs.jmedchem.6b00875 [PubMed] [DOI] [PubMed] [Google Scholar]
- 250.Costerton JW, Stewart PS, Greenberg EP. 1999. Bacterial biofilms: a common cause of persistent infections. Science 284:1318–1322. 10.1126/science.284.5418.1318 [PubMed] [DOI] [PubMed] [Google Scholar]
- 251.Hall-Stoodley L, Costerton JW, Stoodley P. 2004. Bacterial biofilms: from the natural environment to infectious diseases. Nat Rev Microbiol 2:95–108. 10.1038/nrmicro821 [DOI] [PubMed] [Google Scholar]
- 252.Ojha AK, Baughn AD, Sambandan D, Hsu T, Trivelli X, Guerardel Y, Alahari A, Kremer L, Jacobs WR Jr, Hatfull GF. 2008. Growth of Mycobacterium tuberculosis biofilms containing free mycolic acids and harbouring drug-tolerant bacteria. Mol Microbiol 69:164–174. 10.1111/j.1365-2958.2008.06274.x [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Purkayastha A, McCue LA, McDonough KA. 2002. Identification of a Mycobacterium tuberculosis putative classical nitroreductase gene whose expression is coregulated with that of the acr aene within macrophages, in standing versus shaking cultures, and under low oxygen conditions. Infect Immun 70:1518–1529. 10.1128/IAI.70.3.1518-1529.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Williams EM, Little RF, Mowday AM, Rich MH, Chan-Hyams JV, Copp JN, Smaill JB, Patterson AV, Ackerley DF. 2015. Nitroreductase gene-directed enzyme prodrug therapy: insights and advances toward clinical utility. Biochem J 471:131–153. 10.1042/BJ20150650 [DOI] [PubMed] [Google Scholar]
- 255.Viodé C, Bettache N, Cenas N, Krauth-Siegel RL, Chauvière G, Bakalara N, Périé J. 1999. Enzymatic reduction studies of nitroheterocycles. Biochem Pharmacol 57:549–557. 10.1016/S0006-2952(98)00324-4 [DOI] [PubMed] [Google Scholar]
- 256.McOsker CC, Fitzpatrick PM. 1994. Nitrofurantoin: mechanism of action and implications for resistance development in common uropathogens. J Antimicrob Chemother. 33(Suppl A):23–30. PMID: 7928834. [PubMed] [DOI] [PubMed] [Google Scholar]
- 257.Murugasu-Oei B, Dick T. 2000. Bactericidal activity of nitrofurans against growing and dormant Mycobacterium bovis BCG. J Antimicrob Chemother 46:917–919. 10.1093/jac/46.6.917 [DOI] [PubMed] [Google Scholar]
- 258.de Carvalho LP, Darby CM, Rhee KY, Nathan C. 2011. Nitazoxanide disrupts membrane potential and intrabacterial pH homeostasis of Mycobacterium tuberculosis. ACS Med Chem Lett 2:849–854. 10.1021/ml200157f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Matsumoto M, Hashizume H, Tomishige T, Kawasaki M, Tsubouchi H, Sasaki H, Shimokawa Y, Komatsu M. 2006. OPC-67683, a nitro-dihydro-imidazooxazole derivative with promising action against tuberculosis in vitro and in mice. PLoS Med 3:e466. 10.1371/journal.pmed.0030466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Upton AM, Cho S, Yang TJ, Kim Y, Wang Y, Lu Y, Wang B, Xu J, Mdluli K, Ma Z, Franzblau SG. 2015. In vitro and in vivo activities of the nitroimidazole TBA-354 against Mycobacterium tuberculosis. Antimicrob Agents Chemother 59:136–144. 10.1128/AAC.03823-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Upton AM, McKinney JD. 2007. Role of the methylcitrate cycle in propionate metabolism and detoxification in Mycobacterium smegmatis. Microbiology 153(Pt 12):3973–3982. doi:153/12/3973 [pii] 10.1099/mic.0.2007/011726-0. PMID: 18048912. [PubMed] [DOI] [PubMed] [Google Scholar]
- 262.Rakesh, Bruhn DF, Scherman MS, Woolhiser LK, Madhura DB, Maddox MM, et al. 2014. Pentacyclic nitrofurans with in vivo efficacy and activity against nonreplicating Mycobacterium tuberculosis. PLoS One 9(2):e87909. 10.1371/journal.pone.0087909. PMID: 24505329; Central PMCID: PMC3914891. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Debnath AK, Lopez de Compadre RL, Debnath G, Shusterman AJ, Hansch C. 1991. Structure-activity relationship of mutagenic aromatic and heteroaromatic nitro compounds. Correlation with molecular orbital energies and hydrophobicity. J Med Chem 34:786–797. 10.1021/jm00106a046 [DOI] [PubMed] [Google Scholar]
- 264.Feng X, Zhu W, Schurig-Briccio LA, Lindert S, Shoen C, Hitchings R, Li J, Wang Y, Baig N, Zhou T, Kim BK, Crick DC, Cynamon M, McCammon JA, Gennis RB, Oldfield E. 2015. Antiinfectives targeting enzymes and the proton motive force. Proc Natl Acad Sci USA 112:E7073–E7082 10.1073/pnas.1521988112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Lee IY, Gruber TD, Samuels A, Yun M, Nam B, Kang M, Crowley K, Winterroth B, Boshoff HI, Barry CE III. 2013. Structure-activity relationships of antitubercular salicylanilides consistent with disruption of the proton gradient via proton shuttling. Bioorg Med Chem 21:114–126. 10.1016/j.bmc.2012.10.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Terada H. 1990. Uncouplers of oxidative phosphorylation. Environ Health Perspect 87:213–218. 10.1289/ehp.9087213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Williamson RL, Metcalf RL. 1967. Salicylanilides: a new group of active uncouplers of oxidative phosphorylation. Science 158:1694–1695. 10.1126/science.158.3809.1694 [DOI] [PubMed] [Google Scholar]
- 268.Moreira W, Aziz DB, Dick T. 2016. Boromycin kills mycobacterial persisters without detectable resistance. Front Microbiol 7:199. 10.3389/fmicb.2016.00199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Mukherjee D, Zou H, Liu S, Beuerman R, Dick T. 2016. Membrane-targeting AM-0016 kills mycobacterial persisters and shows low propensity for resistance development. Future Microbiol 11:643–650. 10.2217/fmb-2015-0015 [PubMed] [DOI] [PubMed] [Google Scholar]
- 270.Tyagi S, Ammerman NC, Li SY, Adamson J, Converse PJ, Swanson RV, Almeida DV, Grosset JH. 2015. Clofazimine shortens the duration of the first-line treatment regimen for experimental chemotherapy of tuberculosis. Proc Natl Acad Sci USA 112:869–874. 10.1073/pnas.1416951112 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Yano T, Kassovska-Bratinova S, Teh JS, Winkler J, Sullivan K, Isaacs A, Schechter NM, Rubin H. 2011. Reduction of clofazimine by mycobacterial type 2 NADH:quinone oxidoreductase: a pathway for the generation of bactericidal levels of reactive oxygen species. J Biol Chem 286:10276–10287. 10.1074/jbc.M110.200501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Lechartier B, Cole ST. 2015. Mode of action of clofazimine and combination therapy with benzothiazinones against Mycobacterium tuberculosis. Antimicrob Agents Chemother 59:4457–4463. 10.1128/AAC.00395-15 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Advani MJ, Siddiqui I, Sharma P, Reddy H. 2012. Activity of trifluoperazine against replicating, non-replicating and drug resistant M. tuberculosis. PLoS One 7:e44245. 10.1371/journal.pone.0044245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Jones PB, Parrish NM, Houston TA, Stapon A, Bansal NP, Dick JD, Townsend CA. 2000. A new class of antituberculosis agents. J Med Chem 43:3304–3314. 10.1021/jm000149l [DOI] [PubMed] [Google Scholar]
- 275.Parrish NM, Houston T, Jones PB, Townsend C, Dick JD. 2001. In vitro activity of a novel antimycobacterial compound, N-octanesulfonylacetamide, and its effects on lipid and mycolic acid synthesis. Antimicrob Agents Chemother 45:1143–1150. 10.1128/AAC.45.4.1143-1150.2001. PMID: 11257028; Central PMCID: PMC90437. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Parrish NM, Ko CG, Dick JD. 2009. Activity of DSA against anaerobically adapted Mycobacterium bovis BCG in vitro. Tuberculosis (Edinb) 89:325–327. 10.1016/j.tube.2009.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Parrish NM, Ko CG, Hughes MA, Townsend CA, Dick JD. 2004. Effect of n-octanesulphonylacetamide (OSA) on ATP and protein expression in Mycobacterium bovis BCG. J Antimicrob Chemother 54:722–729. 10.1093/jac/dkh408 [DOI] [PubMed] [Google Scholar]
- 278.Pethe K, et al. 2013. Discovery of Q203, a potent clinical candidate for the treatment of tuberculosis. Nat Med 19:1157–1160. 10.1038/nm.3262 [PubMed] [DOI] [PubMed] [Google Scholar]
- 279.Wallace KB, Starkov AA. 2000. Mitochondrial targets of drug toxicity. Annu Rev Pharmacol Toxicol 40:353–388. 10.1146/annurev.pharmtox.40.1.353 [PubMed] [DOI] [PubMed] [Google Scholar]
- 280.Conlon BP, Rowe SE, Gandt AB, Nuxoll AS, Donegan NP, Zalis EA, et al. 2016. Persister formation in Staphylococcus aureus is associated with ATP depletion. Nat Microbiol 1. 10.1038/nmicrobiol.2016.51. PMID: 27398229; Central PMCID: PMC4932909. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Harbut MB, Vilchèze C, Luo X, Hensler ME, Guo H, Yang B, Chatterjee AK, Nizet V, Jacobs WR Jr, Schultz PG, Wang F. 2015. Auranofin exerts broad-spectrum bactericidal activities by targeting thiol-redox homeostasis. Proc Natl Acad Sci USA 112:4453–4458. 10.1073/pnas.1504022112 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Lin K, O’Brien KM, Trujillo C, Wang R, Wallach JB, Schnappinger D, Ehrt S. 2016. Mycobacterium tuberculosis thioredoxin reductase is essential for thiol redox homeostasis but plays a minor role in antioxidant defense. PLoS Pathog 12:e1005675. 10.1371/journal.ppat.1005675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Malhotra V, Sharma D, Ramanathan VD, Shakila H, Saini DK, Chakravorty S, Das TK, Li Q, Silver RF, Narayanan PR, Tyagi JS. 2004. Disruption of response regulator gene, devR, leads to attenuation in virulence of Mycobacterium tuberculosis. FEMS Microbiol Lett 231:237–245. 10.1016/S0378-1097(04)00002-3 [DOI] [PubMed] [Google Scholar]
- 284.Gupta RK, Thakur TS, Desiraju GR, Tyagi JS. 2009. Structure-based design of DevR inhibitor active against nonreplicating Mycobacterium tuberculosis. J Med Chem 52:6324–6334. 10.1021/jm900358q [PubMed] [DOI] [PubMed] [Google Scholar]
- 285.Salina E, Ryabova O, Kaprelyants A, Makarov V. 2014. New 2-thiopyridines as potential candidates for killing both actively growing and dormant Mycobacterium tuberculosis cells. Antimicrob Agents Chemother 58:55–60. 10.1128/AAC.01308-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Moraski GC, Chang M, Villegas-Estrada A, Franzblau SG, Möllmann U, Miller MJ. 2010. Structure-activity relationship of new anti-tuberculosis agents derived from oxazoline and oxazole benzyl esters. Eur J Med Chem 45:1703–1716. 10.1016/j.ejmech.2009.12.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Villar R, Vicente E, Solano B, Pérez-Silanes S, Aldana I, Maddry JA, Lenaerts AJ, Franzblau SG, Cho SH, Monge A, Goldman RC. 2008. In vitro and in vivo antimycobacterial activities of ketone and amide derivatives of quinoxaline 1,4-di-N-oxide. J Antimicrob Chemother 62:547–554. 10.1093/jac/dkn214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Friedmann HC. 2004. From “butyribacterium” to “E. coli”: an essay on unity in biochemistry. Perspect Biol Med 47:47–66. 10.1353/pbm.2004.0007 [DOI] [PubMed] [Google Scholar]
- 289.Schnappinger D. 2015. Genetic approaches to facilitate antibacterial drug development. Cold Spring Harb Perspect Med 5:a021139. 10.1101/cshperspect.a021139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Kim JH, O’Brien KM, Sharma R, Boshoff HI, Rehren G, Chakraborty S, Wallach JB, Monteleone M, Wilson DJ, Aldrich CC, Barry CE III, Rhee KY, Ehrt S, Schnappinger D. 2013. A genetic strategy to identify targets for the development of drugs that prevent bacterial persistence. Proc Natl Acad Sci USA 110:19095–19100. 10.1073/pnas.1315860110 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Russell DG, Barry CE III, Flynn JL. 2010. Tuberculosis: what we don’t know can, and does, hurt us. Science 328:852–856. 10.1126/science.1184784 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Heifets L, Higgins M, Simon B. 2000. Pyrazinamide is not active against Mycobacterium tuberculosis residing in cultured human monocyte-derived macrophages. Int J Tuberc Lung Dis 4:491–495. [PubMed] [Google Scholar]
- 293.Rastogi N, Potar MC, David HL. 1988. Pyrazinamide is not effective against intracellularly growing Mycobacterium tuberculosis. Antimicrob Agents Chemother 32:287. 10.1128/AAC.32.2.287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Tsai MC, Chakravarty S, Zhu G, Xu J, Tanaka K, Koch C, Tufariello J, Flynn J, Chan J. 2006. Characterization of the tuberculous granuloma in murine and human lungs: cellular composition and relative tissue oxygen tension. Cell Microbiol 8:218–232. 10.1111/j.1462-5822.2005.00612.x [DOI] [PubMed] [Google Scholar]
- 295.Dhillon J, Allen BW, Hu YM, Coates AR, Mitchison DA. 1998. Metronidazole has no antibacterial effect in Cornell model murine tuberculosis. Int J Tuberc Lung Dis 2:736–742. [PubMed] [PubMed] [Google Scholar]
- 296.Lanoix JP, Lenaerts AJ, Nuermberger EL. 2015. Heterogeneous disease progression and treatment response in a C3HeB/FeJ mouse model of tuberculosis. Dis Model Mech 8:603–610. 10.1242/dmm.019513 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Harper J, Skerry C, Davis SL, Tasneen R, Weir M, Kramnik I, Bishai WR, Pomper MG, Nuermberger EL, Jain SK. 2012. Mouse model of necrotic tuberculosis granulomas develops hypoxic lesions. J Infect Dis 205:595–602. 10.1093/infdis/jir786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Desai CR, Heera S, Patel A, Babrekar AB, Mahashur AA, Kamat SR. 1989. Role of metronidazole in improving response and specific drug sensitivity in advanced pulmonary tuberculosis. J Assoc Physicians India 37:694–697. [PubMed] [PubMed] [Google Scholar]
- 299.Lardner A. 2001. The effects of extracellular pH on immune function. J Leukoc Biol 69:522–530. [PubMed] [PubMed] [Google Scholar]
- 300.Eoh H, Rhee KY. 2014. Methylcitrate cycle defines the bactericidal essentiality of isocitrate lyase for survival of Mycobacterium tuberculosis on fatty acids. Proc Natl Acad Sci USA 111:4976–4981. 10.1073/pnas.1400390111 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Dartois V, Barry CE III. 2013. A medicinal chemists’ guide to the unique difficulties of lead optimization for tuberculosis. Bioorg Med Chem Lett 23:4741–4750. 10.1016/j.bmcl.2013.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Dannenberg AM Jr. 1993. Immunopathogenesis of pulmonary tuberculosis. Hosp Pract (Off Ed) 28:51–58. 10.1080/21548331.1993.11442738 [DOI] [PubMed] [Google Scholar]
- 303.Aly S, Wagner K, Keller C, Malm S, Malzan A, Brandau S, Bange FC, Ehlers S. 2006. Oxygen status of lung granulomas in Mycobacterium tuberculosis-infected mice. J Pathol 210:298–305. 10.1002/path.2055 [PubMed] [DOI] [PubMed] [Google Scholar]
- 304.Schön T, Elmberger G, Negesse Y, Pando RH, Sundqvist T, Britton S. 2004. Local production of nitric oxide in patients with tuberculosis. Int J Tuberc Lung Dis 8:1134–1137. [PubMed] [PubMed] [Google Scholar]
- 305.Nicholson S, Bonecini-Almeida MG, Lapa e Silva JR, Nathan C, Xie QW, Mumford R, Weidner JR, Calaycay J, Geng J, Boechat N, Linhares C, Rom W, Ho JL. 1996. Inducible nitric oxide synthase in pulmonary alveolar macrophages from patients with tuberculosis. J Exp Med 183:2293–2302. 10.1084/jem.183.5.2293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Facchetti F, Vermi W, Fiorentini S, Chilosi M, Caruso A, Duse M, Notarangelo LD, Badolato R. 1999. Expression of inducible nitric oxide synthase in human granulomas and histiocytic reactions. Am J Pathol 154:145–152. 10.1016/S0002-9440(10)65261-3 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Choi HS, Rai PR, Chu HW, Cool C, Chan ED. 2002. Analysis of nitric oxide synthase and nitrotyrosine expression in human pulmonary tuberculosis. Am J Respir Crit Care Med 166:178–186. 10.1164/rccm.2201023 [PubMed] [DOI] [PubMed] [Google Scholar]
- 308.Nathan C. 2002. Inducible nitric oxide synthase in the tuberculous human lung. Am J Respir Crit Care Med 166:130–131. 10.1164/rccm.2205016 [PubMed] [DOI] [PubMed] [Google Scholar]
- 309.Nathan C, Cunningham-Bussel A. 2013. Beyond oxidative stress: an immunologist’s guide to reactive oxygen species. Nat Rev Immunol 13:349–361. 10.1038/nri3423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Nathan C, Shiloh MU. 2000. Reactive oxygen and nitrogen intermediates in the relationship between mammalian hosts and microbial pathogens. Proc Natl Acad Sci USA 97:8841–8848. PMID: 10922044; Central PMCID: PMC34021. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Kohanski MA, Dwyer DJ, Hayete B, Lawrence CA, Collins JJ. 2007. A common mechanism of cellular death induced by bactericidal antibiotics. Cell 130:797–810. 10.1016/j.cell.2007.06.049 [PubMed] [DOI] [PubMed] [Google Scholar]
- 312.Ng VH, Cox JS, Sousa AO, MacMicking JD, McKinney JD. 2004. Role of KatG catalase-peroxidase in mycobacterial pathogenesis: countering the phagocyte oxidative burst. Mol Microbiol 52:1291–1302. 10.1111/j.1365-2958.2004.04078.x 10.1111/j.1365-2958.2004.04078.x [DOI] [PubMed] [Google Scholar]
- 313.Skaar EP. 2010. The battle for iron between bacterial pathogens and their vertebrate hosts. PLoS Pathog 6:e1000949. 10.1371/journal.ppat.1000949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Goodsmith N, Guo XV, Vandal OH, Vaubourgeix J, Wang R, Botella H, Song S, Bhatt K, Liba A, Salgame P, Schnappinger D, Ehrt S. 2015. Disruption of an M. tuberculosis membrane protein causes a magnesium-dependent cell division defect and failure to persist in mice. PLoS Pathog 11:e1004645. 10.1371/journal.ppat.1004645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Wolschendorf F, Ackart D, Shrestha TB, Hascall-Dove L, Nolan S, Lamichhane G, Wang Y, Bossmann SH, Basaraba RJ, Niederweis M. 2010. Copper resistance is essential for virulence of Mycobacterium tuberculosis. Proc Natl Acad Sci USA 108:1621–1626. doi:1009261108 [pii] 10.1073/pnas.1009261108. PMID: 21205886. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Rowland JL, Niederweis M. 2013. A multicopper oxidase is required for copper resistance in Mycobacterium tuberculosis. J Bacteriol 195:3724–3733. 10.1128/JB.00546-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Rowland JL, Niederweis M. 2012. Resistance mechanisms of Mycobacterium tuberculosis against phagosomal copper overload. Tuberculosis (Edinb) 92:202–210. 10.1016/j.tube.2011.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Darwin KH. 2015. Mycobacterium tuberculosis and copper: a newly appreciated defense against an old foe? J Biol Chem 290:18962–18966. 10.1074/jbc.R115.640193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.White C, Lee J, Kambe T, Fritsche K, Petris MJ. 2009. A role for the ATP7A copper-transporting ATPase in macrophage bactericidal activity. J Biol Chem 284:33949–33956. 10.1074/jbc.M109.070201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Tan S, Sukumar N, Abramovitch RB, Parish T, Russell DG. 2013. Mycobacterium tuberculosis responds to chloride and pH as synergistic cues to the immune status of its host cell. PLoS Pathog 9:e1003282. 10.1371/journal.ppat.1003282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Larrouy-Maumus G, Marino LB, Madduri AV, Ragan TJ, Hunt DM, Bassano L, Gutierrez MG, Moody DB, Pavan FR, de Carvalho LP. 2016. Cell-envelope remodeling as a determinant of phenotypic antibacterial tolerance in Mycobacterium tuberculosis. ACS Infect Dis 2:352–360. 10.1021/acsinfecdis.5b00148 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Scott CC, Gruenberg J. 2011. Ion flux and the function of endosomes and lysosomes: pH is just the start: the flux of ions across endosomal membranes influences endosome function not only through regulation of the luminal pH. BioEssays 33:103–110. 10.1002/bies.201000108 [DOI] [PubMed] [Google Scholar]
- 323.Jiang L, Salao K, Li H, Rybicka JM, Yates RM, Luo XW, Shi XX, Kuffner T, Tsai VW, Husaini Y, Wu L, Brown DA, Grewal T, Brown LJ, Curmi PM, Breit SN. 2012. Intracellular chloride channel protein CLIC1 regulates macrophage function through modulation of phagosomal acidification.J Cell Sci 125:5479–5488. 10.1242/jcs.110072 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.McKinney JD, Höner zu Bentrup K, Muñoz-Elías EJ, Miczak A, Chen B, Chan WT, Swenson D, Sacchettini JC, Jacobs WR Jr, Russell DG. 2000. Persistence of Mycobacterium tuberculosis in macrophages and mice requires the glyoxylate shunt enzyme isocitrate lyase. Nature 406:735–738. 10.1038/35021074 [DOI] [PubMed] [Google Scholar]
- 325.Munoz-Elias EJ, Upton AM, Cherian J, McKinney JD. 2006. Role of the methylcitrate cycle in Mycobacterium tuberculosis metabolism, intracellular growth, and virulence. Mol Microbiol 60:1109–1122. doi:MMI5155 [pii] 10.1111/j.1365-2958.2006.05155.x. PMID: 16689789. [PubMed] [DOI] [PubMed] [Google Scholar]
- 326.Beste DJ, Nöh K, Niedenführ S, Mendum TA, Hawkins ND, Ward JL, Beale MH, Wiechert W, McFadden J. 2013. 13C-flux spectral analysis of host-pathogen metabolism reveals a mixed diet for intracellular Mycobacterium tuberculosis. Chem Biol 20:1012–1021. 10.1016/j.chembiol.2013.06.012 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Pandey AK, Sassetti CM. 2008. Mycobacterial persistence requires the utilization of host cholesterol. Proc Natl Acad Sci USA 105:4376–4380. 10.1073/pnas.0711159105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Baek SH, Li AH, Sassetti CM. 2011. Metabolic regulation of mycobacterial growth and antibiotic sensitivity. PLoS Biol 9:e1001065. 10.1371/journal.pbio.1001065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Shi L, Sohaskey CD, Pheiffer C, Datta P, Parks M, McFadden J, North RJ, Gennaro ML. 2010. Carbon flux rerouting during Mycobacterium tuberculosis growth arrest. Mol Microbiol 78:1199–1215. 10.1111/j.1365-2958.2010.07399.x 10.1111/j.1365-2958.2010.07399.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Larsen MH, Biermann K, Chen B, Hsu T, Sambandamurthy VK, Lackner AA, Aye PP, Didier P, Huang D, Shao L, Wei H, Letvin NL, Frothingham R, Haynes BF, Chen ZW, Jacobs WR Jr. 2009. Efficacy and safety of live attenuated persistent and rapidly cleared Mycobacterium tuberculosis vaccine candidates in non-human primates. Vaccine 27:4709–4717. 10.1016/j.vaccine.2009.05.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Sambandamurthy VK, Derrick SC, Jalapathy KV, Chen B, Russell RG, Morris SL, Jacobs WR Jr. 2005. Long-term protection against tuberculosis following vaccination with a severely attenuated double lysine and pantothenate auxotroph of Mycobacterium tuberculosis. Infect Immun 73:1196–1203. 10.1128/IAI.73.2.1196-1203.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Gouzy A, Poquet Y, Neyrolles O. 2014. Nitrogen metabolism in Mycobacterium tuberculosis physiology and virulence. Nat Rev Microbiol 12:729–737. 10.1038/nrmicro3349 [PubMed] [DOI] [PubMed] [Google Scholar]
- 333.Cunningham-Bussel A, Bange FC, Nathan CF. 2013. Nitrite impacts the survival of Mycobacterium tuberculosis in response to isoniazid and hydrogen peroxide. MicrobiologyOpen 2:901–911. 10.1002/mbo3.126 [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]


