Abstract
Background and Objectives:
Postoperative adhesions occur less often in laparoscopies than in laparotomies, but the incidence can be reduced further. Seprafilm, a sodium hyaluronate/carboxymethylcellulose absorbable barrier, was developed to prevent adhesions after abdominal surgery, and is approved for postoperative adhesion prevention. However, Seprafilm is seldom used in laparoscopic surgery because of its tendency to break apart when it is inserted into the abdominal cavity through a trocar, resulting in a high placement failure rate. We propose a better method for applying the adhesion barrier Seprafilm in single- or multiport gynecologic surgery.
Methods:
This is a retrospective analysis of patients who underwent multi- or single-port gynecologic laparoscopies from December 2014 through January 2016 in Buddhist Tzu Chi General Hospital, Hualien, 46 patients received Seprafilm (Genzyme Corp., Cambridge, MA, USA) via the proposed method. A piece of Seprafilm was cut into quarters. To moisten and soften the Seprafilm, each piece was placed on a wet wrung gauze until it became naturally curled. Two pieces of the film were rolled up with the backing paper that came from the package of Seprafilm. Holding the rolled Seprafilm with a grasper, the surgeon delivered it into the abdomen through a 11-mm trocar.
Results:
The success rates of Seprafilm insertion and correct placement were 100% (46/46) and 95.7%, respectively. In 2 single-port (2/26) laparoscopic surgeries, the placement of the film failed; all placements in the multiport laparoscopic surgeries were successful (20/20). The average time required for placement of pieces of Seprafilm per surgery was 4.0 ± 1.47 minutes among all surgeries; significantly more time was needed in the single-port surgeries (mean, 4.4 ± 1.59 minutes) than in the multiport surgery (mean, 3.4 ± 1.13 minutes) (P < .05).
Conclusions:
This method of Seprafilm placement is a simple technique that does not need special equipment and ensures a high success rate. The placement of the film takes longer in single-port surgeries than in multiport surgeries.
Keywords: Adhesion barrier, Laparoscopy, Seprafilm, Single-port access
INTRODUCTION
Therapeutic or diagnostic laparoscopic procedures cause fewer postoperative adhesions than laparotomies. The application of an adhesion barrier can minimize the adhesions.1 Seprafilm (Genzyme Corp., Cambridge, MA, USA), composed of sodium hyaluronate and carboxymethylcellulose, was approved by the U.S. Food and Drug Administration (FDA) in 1996 and is one of the adhesion barriers widely used in surgery today. This product is indicated for abdominal or pelvic laparotomy surgery to reduce the incidence, extent, and severity of postoperative adhesions.2–5 However, Seprafilm is seldom used in laparoscopic surgery because of its tendency to break apart when it is inserted into the abdominal cavity through a trocar, resulting in a high placement failure rate.6 Several techniques of insertion of Seprafilm have been developed,7–10 but some require special equipment and some are complicated.11 Moreover, Seprafilm placement in single-port surgery is more difficult than in multiport surgery.
This work presents a modified approach to Seprafilm placement, in which the Seprafilm is prepared by softening and rolling before insertion into the abdomen. This proposed method is a better method that combines and simplifies the two previously reported methods.11,12
MATERIALS AND METHODS
Forty-six patients were recruited into this study. They had undergone single-port (n = 26) or multiport (n = 20) laparoscopic gynecology surgery including the insertion of Seprafilm between December 2014 and January 2016.
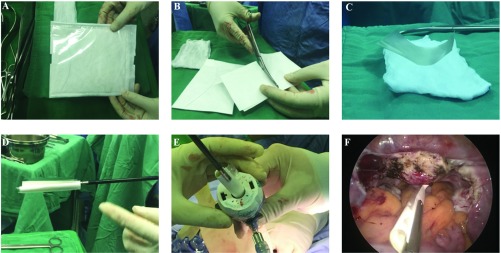
After the major laparoscopic procedures were performed, Seprafilm was prepared and placed as follows. Seprafilm and its paper backing (Figure 1A) were cut together into 4 equal pieces (Figure 1B). Each piece of the film was placed on damp gauze until it naturally curled up (∼6–8 seconds) (Figure 1C). Two pieces of the film were rolled up with the backing (from the Seprafilm package). The roll was gripped with forceps (Figure 1D) and insert into the abdominal cavity through the 11-mm trocar sleeve (Figure 1E, 1F).
Figure 1.
Seprafilm preparation. (A) A sealed Seprafilm package. (B) The film is cut, together with its paper backing sheet, into 4 equal pieces. (C) A piece is placed on moistened gauze to soften it until it naturally curls up. The process is repeated for the second piece. (D) Two pieces are rolled up in 1 backing sheet, and gripped with an intestine-holding forcep. (E, F) The roll is inserted into the abdominal cavity through the 11-mm trocar.
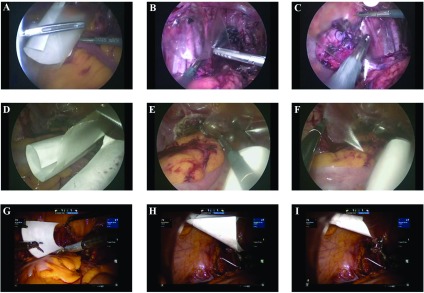
In multiport laparoscopy, after the abdominal cavity was entered, another forceps was used to unroll the Seprafilm (Figure 2A) and move the first piece to the intended site (Figure 2B), followed by the second piece (Figure 2C). The other 2 pieces were placed in the same manner. In the single-port laparoscopy, only 1 forcep was used to unroll the Seprafilm and subsequently move it to the intended site (Figure 2D–F). Some skill was needed to remove the 2 residual paper sheets in the abdomen, grasping one corner of the paper (Fig. 2G), pulling it out gently and rotating it at the same time so that the paper could be rolled and passed through the 11-mm trocar or single port (Figure 2H) without friction (Figure 2I).
Figure 2.
The placement of Seprafilm in multiport (A–C) and single-port (D–F) procedures and removal of the residual paper holders (G–I). (A) The film is unrolled with 2 graspers. Placement of the first (B) and the second (C) layers of film. One corner of the paper backing is grasped (G) and pulled out and rotated (H) via the 11 mm-trocar and completely removed through the trocar (I).
The number of successful insertions and placements of Seprafilm was calculated and the time from the moistening of the film until all pieces were positioned were reviewed in every case.
The definitions of successfully placed Seprafilm were as follows: in myomectomy, the film framed the suture line, 1 cm away the line; in total and subtotal hysterectomy, the film framed the endocervical region and bilateral peritoneum opening; in sacrocolpopexy, the film framed the anterior, posterior, and lateral peritoneal suture lines; in ovarian cystectomy, the film was placed on the lower and upper surface of the ovary; in cancer surgery, the film was placed on the rough surfaces of all surgical sites.
Total time needed for application in the different groups was compared by Student's t test. The application time data are expressed as the mean ± SD. Differences reaching P < .05 were significant.
RESULTS
A total of 184 pieces of Seprafilm were inserted. The success rate of insertion into the abdominal cavity through the trocar was 100%.
Regarding the placement, the success rate of placement at the intended site in all surgeries was 95.7%. In the single-port surgery group, the placement failed in 2 cases (92.3% success rate), whereas in the multiport surgery group, the placement had a 100% success rate.
The mean application time was 4.0 ± 1.47 minutes. The application time was significantly longer in the single-port surgery group than in the multiport group (4.4 ± 1.59 vs 3.4 ± 1.13 minute; P = .013 by Student t test) (Table 1).
Table 1.
Success Rate and Placement Time for Seprafilm
| Single Port (n = 26) | Multiport (n = 20) | Total (n = 46) | P | |
|---|---|---|---|---|
| Insertion success rate (%) | 100 | 100 | 100 | |
| Placement success rate (%) | 92.3 | 100 | 95.7 | |
| Total placement time (min) | 4.4 ± 1.59 | 3.4 ± 1.13 | 4.0 ± 1.47 | 0.013* |
Data are the mean ± SD.
Single-port vs multiport by Student's t test.
DISCUSSION
We report the development of a simple technique for Seprafilm application in laparoscopic surgery. The overall success rate of this modified method, was 95.7% (44/46). In single-port access laparoscopy surgery, the success rate was 92.3%. The application time in single-port surgery was significantly longer than in the multiport setting (4.4 ± 1.59 vs 3.4 ± 1.13 min, P = 0.013).
The flexibility of Seprafilm depends on the humidity of the environment. If the package of Seprafilm is opened too early, the sheet becomes too soft and sticky to handle. Conversely, if the package is opened just before use, the sheet is stiff and breaks easily, ultimately causing a failed placement. Therefore, the ideal timing for opening the package of Seprafilm is often difficult to discern. The uncertainty discourages surgeons from adopting Seprafilm, especially in laparoscopic surgeries, even though it can decrease the formation of adhesions.
Two procedures have been adopted for the application of Seprafilm in laparoscopic surgery. First, cut the film in pieces and roll together with a soft plastic holder. Then insert the roll into the abdomen via a 10–12 mm trocar, place the film pieces at the intended sites, and remove the soft plastic holder sheets.7–10 The major disadvantage of this method is that the soft plastic holder reflects light that makes the film difficult to differentiate from the plastic holder. In addition, the holder is not hard enough to protect the Seprafilm during insertion. The second method involves cutting and rolling the Seprafilm, and inserting it into an inducer via a trocar for placement.10 The disadvantage of this method is the need for special equipment and the success rate is low, only 31.5% in one report.10
Two of the latest methods reported in 2014 have been proposed to eliminate the disadvantages mentioned above. Chuang et al12 proposed the use of 2 layers of Seprafilm so that it does not stick to the plastic covering, facilitating the removal of the second layer of film from the placement site. Kusuki et al11 suggested moistening the Seprafilm before introducing it into the abdomen cavity by opening the valves of a 12-mm trocar and using no holder. However, these 2 methods still do not fully eliminate the drawbacks mentioned above.
Our proposed method combines and modifies the methods of Chuang and Kusuki, and allows the simple and successful application of Seprafilm. First, the backing paper is sturdy enough and makes insertion through the 11-mm trocar easier than the plastic sheet. Second, the surgeon can easily differentiate the Seprafilm from the paper backing. Third, after placing the first piece of Seprafilm, the surgeon can move the second layer to cover additional areas. Our application successful rate of Seprafilm is 95.7% versus the 80% reported in Kusuki et al.11
Seprafilm is seldom used in single-port access laparoscopic surgery because of the difficulty in applying it to the desired place. Using our modified technique, there were only 2 cases of failure in placing the film in single-port access laparoscopy. In our opinion, these failures may have been caused by the prolonged manipulation of the Seprafilm, making it too sticky to apply. More simulation training may conquer this problem. Use of only 1 forcep to manipulate the film also increased the difficulty of application. According to the result in our study, the placement time was also longer in the single-port than in the multiport setting, probably owing to the limited space and the limited range of motion of the forcep. Possible solutions to this problem are using a flexible grasper for manipulation and regular practice with a training box.
The average time of placing Seprafilm in this study was below 5 minutes, less time than reported in the 2 recent studies mentioned earlier (8 minutes12 and 10 minutes11). The time reduction is probably due to easier entry and ease of distinguishing the Seprafilm from the backing paper. In addition, inserting 2 layers of film at the same time definitely takes less time than inserting 1 sheet at a time.
CONCLUSION
We have demonstrated that when Seprafilm is prepared by moistening and rolling with the backing paper, it is simple to apply in both single and multi-port surgeries. This modified method can extend the use of adhesion barriers in laparoscopic surgeries.
Contributor Information
Mun-Kun Hong, Department of Obstetrics and Gynecology, Buddhist Tzu Chi General Hospital, Tzu Chi University, and Institute of Medical Sciences, Tzu Chi University, Hualien, Taiwan..
Dah-Ching Ding, Department of Obstetrics and Gynecology, Buddhist Tzu Chi General Hospital, Tzu Chi University, and Institute of Medical Sciences, Tzu Chi University, Hualien, Taiwan..
References:
- 1. Bolnick A, Bolnick J, Diamond MP. Postoperative adhesions as a consequence of pelvic surgery. J Minim Invasive Gynecol. 2015;22:549–563. [DOI] [PubMed] [Google Scholar]
- 2. Beck DE, Cohen Z, Fleshman JW, et al. A prospective, randomized, multicenter, controlled study of the safety of Seprafilm adhesion barrier in abdominopelvic surgery of the intestine. Dis Colon Rectum. 2003;46:1310–1319. [DOI] [PubMed] [Google Scholar]
- 3. Becker JM, Dayton MT, Fazio VW, et al. Prevention of postoperative abdominal adhesions by a sodium hyaluronate-based bioresorbable membrane: a prospective, randomized, double-blind multicenter study. J Am Coll Surg. 1996;183:297–306. [PubMed] [Google Scholar]
- 4. Diamond MP. Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL-F): a blinded, prospective, randomized, multicenter clinical study. Seprafilm Adhesion Study Group. Fertil Steril. 1996;66:904–910. [PubMed] [Google Scholar]
- 5. Inoue M, Uchida K, Miki C, et al. Efficacy of Seprafilm for reducing reoperative risk in pediatric surgical patients undergoing abdominal surgery. J Pediatr Surg. 2005;40:1301–1306. [DOI] [PubMed] [Google Scholar]
- 6. Gonzalez-Quintero VH, Cruz-Pachano FE. Preventing adhesions in obstetric and gynecologic surgical procedures. Rev Obstet Gynecol. 2009;2:38–45. [PMC free article] [PubMed] [Google Scholar]
- 7. Khaitan E, Scholz S, Richards WO. Laparoscopic adhesiolysis and placement of Seprafilm: a new technique and novel approach to patients with intractable abdominal pain. J Laparoendosc Adv Surg Tech A. 2002;12:241–247. [DOI] [PubMed] [Google Scholar]
- 8. Chuang YC, Fan CN, Cho FN, et al. A novel technique to apply a Seprafilm (hyaluronate-carboxymethylcellulose) barrier following laparoscopic surgeries. Fertil Steril. 2008;90:1959–1963. [DOI] [PubMed] [Google Scholar]
- 9. Shinohara T, Kashiwagi H, Yanagisawa S, et al. A simple and novel technique for the placement of antiadhesive membrane in laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2008;18:188–191. [DOI] [PubMed] [Google Scholar]
- 10. Takeuchi H, Kitade M, Kikuchi I, et al. A novel instrument and technique for using Seprafilm hyaluronic acid/carboxymethylcellulose membrane during laparoscopic myomectomy. J Laparoendosc Adv Surg Tech A. 2006;16:497–502. [DOI] [PubMed] [Google Scholar]
- 11. Kusuki I, Suganuma I, Ito F, et al. Usefulness of moistening Seprafilm before use in laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2014;24:e13–15. [DOI] [PubMed] [Google Scholar]
- 12. Chuang YC, Lu HF, Peng FS, et al. Modified novel technique for improving the success rate of applying Seprafilm by using laparoscopy. J Minim Invasive Gynecol. 2014;21:787–790. [DOI] [PubMed] [Google Scholar]