Abstract
Asymmetric and symmetric dimethylarginine (ADMA and SDMA, respectively) are toxic, non-proteinogenic amino acids formed by post-translational modification and are uremic toxins that inhibit nitric oxide (NO) production and play multifunctional roles in many human diseases. Both ADMA and SDMA have emerged as strong predictors of cardiovascular events and death in a range of illnesses. Major progress has been made in research on ADMA-lowering therapies in animal studies; however, further studies are required to fill the translational gap between animal models and clinical trials in order to treat human diseases related to elevated ADMA/SDMA levels. Here, we review the reported impacts of ADMA and SDMA on human health and disease, focusing on the synthesis and metabolism of ADMA and SDMA; the pathophysiological roles of these dimethylarginines; clinical conditions and animal models associated with elevated ADMA and SDMA levels; and potential therapies against ADMA and SDMA. There is currently no specific pharmacological therapy for lowering the levels and counteracting the deleterious effects of ADMA and SDMA. A better understanding of the mechanisms underlying the impact of ADMA and SDMA on a wide range of human diseases is essential to the development of specific therapies against diseases related to ADMA and SDMA.
Keywords: alanine-glyoxylate aminotransferase-2, asymmetric dimethylarginine, cardiovascular disease, chronic kidney disease, dimethylarginine dimethylaminohydrolase, nitric oxide, non-proteinogenic amino acid, protein arginine methyltransferase, symmetric dimethylarginine, uremic toxins
1. Introduction
The dimethylarginines, asymmetric dimethylarginine (ADMA) and symmetric dimethylarginine (SDMA), were first isolated from human urine in 1970 [1]. Among the guanidine compounds listed as uremic toxins [2], ADMA and SDMA and have been increasingly recognized as putative toxic non-proteinogenic amino acids in a wide range of human diseases over the past decades [3,4,5,6,7,8,9,10,11].
The biological relevance of ADMA as an endogenous inhibitor of nitric oxide synthase (NOS) was first described by Vallance et al. [3]. Although less attention has been paid to SDMA, Bode-Boger et al. were the first to report in vitro inhibitory effects of nitric oxide (NO) production by SDMA [12]. Given that NO has pleiotropic bioactivities, it is not surprising that a variety of important biological functions are regulated by ADMA and SDMA. Emerging clinical and experimental evidence indicates that ADMA and SDMA are involved in the pathophysiology of endothelial dysfunction [13], atherosclerosis [4], oxidative stress [14,15], inflammation [16,17], uremia [8], apoptosis, [18], autophagy [19], and impaired immunological function [20].
This review provides an overview of potential pathophysiological roles for both ADMA and SDMA in human health and disease, with emphasis on the synthesis and metabolism of ADMA and SDMA, the pathophysiology of dimethylarginines, clinical conditions with elevated ADMA and SDMA concentrations, and potential therapies to reduce ADMA and SDMA levels.
2. Synthesis and Metabolism of ADMA and SDMA
2.1. Synthesis of ADMA and SDMA
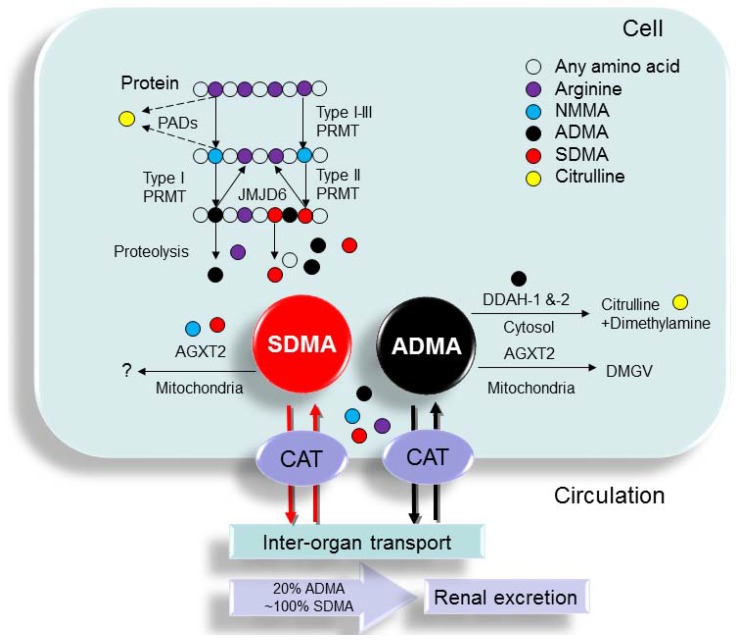
Non-proteinogenic amino acids are those not naturally encoded or found in the genetic code of organisms. Some of them are formed by post-translational modification of the side chains of proteinogenic amino acids present in proteins. Protein-incorporated ADMA is formed by post-translational methylation: two methyl groups are placed on one of the terminal nitrogen atoms of the quanidino group of arginine in proteins by a family of protein arginine methyltransferases (PRMTs) [21]. SDMA, with one methyl group positioned on each of the terminal guanidine nitrogens, is a structural isomer of ADMA. To date, nine human PRMT genes have been cloned and PRMTs are divided into enzymes with type I, type II, or type III activity. Type I PRMTs (PRMT-1, -3, -4, -6, and -8) generate ADMA, whereas type II PRMTs (PRMT-5 and -9) produce SDMA. Although peptidyl arginine deiminases (PADs) can block methylation of arginine residues within proteins by converting them to citrulline [22], PADs are not demethylases. The first arginine demethylase, JMJD6, has been identified [23]; however, a direct role for JMJD6 in the demethylation of protein-incorporated ADMA and SDMA has not been validated [24].
2.2. Metabolism of ADMA and SDMA
Free ADMA and SDMA are released following proteolysis. A healthy adult produces 60 mg (~300 μmol) ADMA per day, of which approximately 20% is excreted in urine via the kidneys [25]. In contrast to ADMA, SDMA is present at only ~50% of the levels of ADMA and the elimination of SDMA is largely dependent on urinary excretion. Free ADMA and SDMA share a common transport process with l-arginine and as such can be moved into or out of cells via the cationic amino acid transporter (CAT) family [26]. Circulating ADMA can hence be transported to major organs such as the kidney, brain, and liver for enzymatic degradation. To date, three enzymes have been reported to metabolize ADMA: dimethylarginine dimethylaminohydrolase-1 (DDAH-1) and -2 (DDAH-2) as well as alanine-glyoxylate aminotransferase 2 (AGXT2), among which DDAHs metabolize ADMA to citrulline and dimethylamine. Similarly, ADMA can also be transaminated by the enzyme AGXT2 to α-keto-δ-(NG,NG-dimethylguanidino) valeric acid (DMGV) [27]. Accordingly, plasma and tissue ADMA levels are highly dependent on factors that affect the expression and activity of DDAHs and AGXT2. Several mechanisms of inhibition of the expression and/or activity of DDAHs have been described [28], including hyperglycemia [29], oxidative stress [30], and angiotensin II administration [31]. Unlike DDAHs, AGXT2, a mitochondrial aminotransferase expressed primarily in the kidney, can metabolize not only ADMA but also SDMA [27]. This AGXT2-mediated pathway of dimethylarginine metabolism has, however, received relatively little attention and the metabolic pathway of this mechanism is still poorly understood. Only one report has shown that D-β-aminoisobutyric acid can inhibit Agxt2-mediated metabolism of ADMA and SDMA [32].
In addition to ADMA and SDMA, a third methylarginine residue—NG monomethyl-l-arginine (NMMA)—is produced in mammals. Since the levels of NMMA are much lower than those of ADMA and SDMA, very little information is available regarding its pathophysiological role in clinical conditions, except that it can function as a NOS inhibitor [28]. The biochemical pathways related to the synthesis and metabolism of SDMA and ADMA are illustrated in Figure 1.
Figure 1.
Schema outlining the synthesis and metabolism of ADMA and SDMA. Protein arginine (purple circle) methylation is performed by a family of enzymes termed protein arginine methyltransferases (PRMTs), which methylate protein-incorporated l-arginine residues to generate protein-incorporated NG monomethyl-l-arginine (NMMA; blue circle). Type I PRMTs generate asymmetric dimethylarginine (ADMA; black circle) and type II PRMTs convert NMMA to symmetric dimethylarginine (SDMA; red circle). Protein-incorporated l-arginine residues can also be converted to citrulline (yellow circle) by peptidylarginine deaminases (PADs), thereby blocking methylation on the arginine residue. Upon proteolytic cleavage of arginine-methylated proteins, free ADMA and SDMA are released into the cytoplasm. ADMA and SDMA can be moved out of the cells via cationic amino acid transporter (CAT) and transported to other organs or excreted in urine. ADMA can be converted to l-citrulline and dimethylamine by dimethylarginine dimethylaminohydrolase-1 (DDAH-1) and -2 (DDAH-2). Alanine-glyoxylate aminotransferase 2 (AGXT2), a mitochondrial aminotransferase expressed primarily in the kidney, can metabolize ADMA as well as SDMA. ADMA can be transaminated by the enzyme AGXT2 to α-keto-δ-(NG,NG-dimethylguanidino) valeric acid (DMGV).
2.3. Quantification of ADMA and SDMA
Since ADMA and SDMA show a very narrow range of normal concentrations, high analytical precision is mandatory to distinguish between normal and slightly elevated concentrations [33]. So far, analytical techniques for the quantification of ADMA and SDMA levels include high-performance liquid chromatography (HPLC) [34], gas chromatography (GC)–mass spectrometry (MS) [35], liquid chromatography with mass spectrometric detection (LC-MS and LC-MS/MS) [36,37], ultrahigh performance liquid chromatography (UPLC)-MS/MS [38], and enzyme-linked immunosorbent assay (ELISA) [39]. Since ADMA and SDMA are structural isomers of each other with an identical molecular weight of 202.1, chromatographic separation using HPLC with ultra violet (UV), radioimmunoassay, and fluorescence (FL) detection was shown to be required. HPLC-based methods are the most widely used techniques for assessing ADMA and SDMA levels in biological fluids such as plasma, urine, and tissue homogenate. These HPLC methods, however, are very time consuming. Although MS-based methods are more sensitive, ADMA and SDMA exhibit different patterns of dissociation between various MS systems. ELISA methods, furthermore, tend to overestimate ADMA concentrations [40,41]; there is only moderate correlation between quantification by ELISA compared with that by UPLC-MS/MS for both ADMA and SDMA [38]. Standardized analytical techniques are required in order for ADMA and SDMA levels to be reliably assessed on a routine basis in clinical practice.
3. Clinical Conditions Associated with Elevated ADMA and SDMA Levels
3.1. ADMA and SDMA: From Uremic Toxins to CVD Risk Factors
Numerous clinical studies have demonstrated elevated ADMA and SDMA levels in a wide spectrum of human diseases [3,4,5,6,7,8,9,10,11]. Since ADMA and SDMA are both uremic toxins [2], the pathophysiological relevance of these two toxic non-proteinogenic amino acids has been extensively investigated in chronic kidney disease (CKD) and end-stage renal disease (ESRD) [42]. Although nearly all studies show that circulating ADMA levels are elevated in patients with CKD, even before a reduction in glomerular filtration rate (GFR), ADMA is not considered a prognosis biomarker in patients with renal disease [42]. A meta-analysis including 2136 patients from 18 studies, however, demonstrated a strong correlation between SDMA and renal function [43]. Zoccali et al. were the first to report the association between circulating ADMA and cardiovascular disease (CVD) and mortality in patients with renal disease [44]. Since then, a number of studies have linked circulating ADMA to CVD risk and mortality in many different study populations. A recent meta-analysis based on 30 studies with 30,624 subjects and 3396 incident CVD events reported that the relative risks for all-cause mortality associated with CVD were 1.52 (1.37–1.68) and 1.33 (1.22–1.45) for high and low ADMA concentrations, respectively [45]. Additionally, high vs. low levels of SDMA were shown to be associated with 31% and 36% increased risk for all-cause mortality and CVD events, respectively [45].
3.2. Clinical Conditions Associated with Elevated ADMA Levels
To date, the list of clinical conditions in which elevated ADMA levels are found continues to grow. Here, we summarize studies previously reviewed [25,42,43,44,45,46] and highlight new data documenting associations between elevated ADMA levels and clinical conditions in specific patient populations. As shown in Table 1, elevated circulating ADMA concentrations have been described in a variety of diseases across different age and sex groups [3,42,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90]. Differences in ADMA concentrations between sexes are small [33], whereas difference between different age groups do exist. In adults, plasma ADMA levels increase with age and the mean plasma concentration of ADMA for a healthy adult is between 0.4 and 0.6 μM [40]. ADMA levels vary by almost two-fold across the geriatric population [91] and in neonates, venous cord blood ADMA levels are markedly elevated (~1.06 μM) and fall significantly close to the normal adult value by the second postnatal day (~0.66 μM) [92]. ADMA levels are higher in children than in adults and levels diminish from birth until around 25 years of age with a mean decrease rate of 15 nM per year [93]. Although ADMA levels are the highest in geriatric and neonatal populations, whether this U-shaped relationship between normal ADMA levels and age relates to renal function remains unclear.
Table 1.
Clinical conditions associated with elevated ADMA levels.
| Patient Population | N | Correlation with Clinical Outcome | Year of First Report | Ref. |
|---|---|---|---|---|
| CKD/ESRD | >1500 | ND | 1992 | [3,46] |
| Schizophrenia | 16 | ND | 1996 | [47] |
| Childhood hypertension | 38 | ND | 1997 | [48] |
| Peripheral arterial occlusive disease (PAOD) | 77 | ND | 1997 | [49] |
| Hypercholesteremia | 49 | ND | 1998 | [50] |
| Congestive heart failure | 84 | ADMA positively correlates with severity of heart failure | 1998 | [51] |
| Preeclampsia | 12 | ND | 1998 | [52] |
| Type 2 diabetes | 50 | ADMA correlates with brachial arterial dilation | 2000 | [53] |
| Congenital heart disease (CHD) | 20 | Elevated ADMA in CHD with pulmonary hypertension | 2001 | [54] |
| Stroke | 52 | ADMA correlates with homocysteine level | 2001 | [55] |
| Hyperthyroidism | 19 | ADMA correlates with free T4 level | 2002 | [56] |
| Critical illness in intensive care unit | 52 | ADMA increases risk for ICU death | 2003 | [57] |
| Liver cirrhosis | 11 | ND | 2004 | [58] |
| Type 1 diabetes | 408 | ADMA correlates with CVD events | 2004 | [59] |
| Obesity | 563 | ND | 2004 | [60] |
| Systemic lupus erythematous | 107 | ADMA correlates with CVD events | 2005 | [61] |
| Idiopathic pulmonary arterial hypertension | 57 | ND | 2005 | [62] |
| Hepatorenal syndrome | 11 | ND | 2006 | [63] |
| Coronary artery disease | 145 | ADMA correlates with homocysteine level; ADMA negatively correlates with GFR | 2006 | [64] |
| Prematurity | 19 | Elevated ADMA in male premature | 2006 | [65] |
| Systemic sclerosis | 21 | Elevated ADMA in diffuse systemic sclerosis | 2006 | [66] |
| Polycystic ovary syndrome (PCOS) | 106 | ND | 2008 | [67] |
| Obstructive sleep apnea-hypopnea syndrome (OSAHS) | 34 | ND | 2008 | [68] |
| Congenital urea cycle enzyme defects | 15 | Elevated ADMA in argininosuccinate synthase (ASS) deficiency and argininosuccinate lyase (ASL) deficiency | 2009 | [69] |
| Rheumatiod arthritis (RA) | 25 | ND | 2009 | [70] |
| Sickle cell disease (SCD) | 177 | ADMA correlates with mortality | 2009 | [71] |
| Congenital portosystemic venous shunt (PSVS) | 14 | ND | 2010 | [72] |
| Primary dysmenorrhea | 33 | ND | 2010 | [73] |
| Inflammatory bowel diseases (IBD) | 63 | ADMA correlates with Crohn’s disease activity | 2010 | [74] |
| Asthma | 17 | ND | 2011 | [75] |
| Nonalcoholic fatty liver disease (NAFLD) | 35 | ND | 2011 | [76] |
| Psoriatic arthritis | 22 | ADMA correlates with coronary flow reserve | 2011 | [77] |
| Fibromyalgia | 27 | ND | 2011 | [78] |
| Childhood acute lymphoblastic leukemia (ALL) | 25 | ND | 2012 | [79] |
| Glaucoma | 210 | Elevated ADMA in advanced glaucoma | 2012 | [80] |
| Pheochromocytoma | 18 | ND | 2013 | [81] |
| Brucellosis | 39 | ND | 2014 | [82] |
| Deep vein thrombosis (DVT) | 34 | ND | 2015 | [83] |
| Short stature | 66 | ND | 2015 | [84] |
| COPD | 58 | ND | 2015 | [85] |
| Nocturia | 262 | ND | 2015 | [86] |
| Neonatal sepsis | 31 | ADMA correlates with disease severity | 2015 | [87] |
| Transient tachypnea of the newborn (TTN) | 36 | ND | 2016 | [88] |
| Arginase 1 deficiency | 19 | ND | 2016 | [89] |
| Idiopathic Parkinson’s disease (PD) | 82 | ND | 2016 | [90] |
Studies tabulated according to year of first report. ND, not determined.
In addition to renal disease [46], increased plasma ADMA levels are associated with clinical conditions mainly associated with endothelial dysfunction such as hypertension [48], peripheral arterial occlusive disease [49], hypercholesterolemia [50], preeclampsia [52], diabetes mellitus [53,59], stroke [55], obesity [60], coronary artery disease [64], polycystic ovary syndrome [67], and sickle cell disease [71]. Many diseases affect both women and men alike; however, some diseases occurring at a higher frequency in women (e.g., systemic lupus erythematous) or affecting only women (e.g., preeclampsia [52], polycystic ovary syndrome [67], and primary dysmenorrhea [73]) have been linked with elevated ADMA concentrations. Additionally, some pediatric diseases such as prematurity [64], congenital urea cycle enzyme defects [69], and transient tachypnea in newborns [88] are associated with elevated plasma ADMA levels. As shown in Table 1, patients with ASL deficiency have been shown to have elevated ADMA levels [69]. It has been noted that hypertension is over-represented in persons with argininosuccinate lyase (ASL) deficiency, a urea cycle disorder [94]. Since ADMA levels are highly correlated with CVD outcome and the occurrence of preclinical CVD during childhood is rare, consideration should be given to elucidating the pathophysiological role of ADMA and to determining the long-term CV outcome in these pediatric diseases. Moreover, it is important to note that diseases reported with elevated ADMA concentrations exhibit remarkable variability across different subspecialties. The extent to which the ADMA affects human health warrants further investigation.
3.3. Clinical Conditions Associated with Elevated SDMA Levels
Despite less attention having been paid to SDMA than to ADMA, there is still a substantial body of research linking elevated SDMA levels to clinical conditions (Table 2) [44,48,56,57,63,64,95,96,97,98,99,100,101,102,103]. As already mentioned, a meta-analysis study showed that SDMA levels correlate well with renal function [44]. SDMA has furthermore been considered a marker of acute kidney injury [104]. As in the case of ADMA, elevated SDMA levels have been reported in clinical conditions related to endothelial dysfunction such as hypertension [56], coronary artery disease [64], diabetes mellitus [96], preeclampsia [99], stroke [100], polycystic ovary syndrome [101], and hyperuricemia [102]. Similar to ADMA, SDMA has been shown to be able to predict all-cause mortality and CVD events, which is independent of renal function [44].
Table 2.
Clinical conditions exhibiting elevated SDMA levels.
| Patient Population | N | Correlation with Clinical Outcome | Year of First Report | Ref. |
|---|---|---|---|---|
| CKD/ESRD | 10 | SDMA correlates with renal function | 1996 | [44,95] |
| Childhood hypertension | 38 | SDMA correlates with GFR | 1997 | [48] |
| Hyperthyroidism | 19 | ND | 2002 | [56] |
| Critical illness in intensive care unit | 52 | SDMA correlates with creatinine level | 2003 | [57] |
| Hepatorenal syndrome | 11 | ND | 2006 | [63] |
| Coronary artery disease | 145 | SDMA negatively correlates with GFR | 2006 | [64] |
| Type 2 diabetes mellitus (DM) | 103 | Elevated SDMA in type 2 DM with albuminuria | 2007 | [96] |
| Alcoholic hepatitis | 52 | ND | 2007 | [97] |
| Heart failure | 132 | ND | 2008 | [98] |
| Preeclampsia | 47 | ND | 2009 | [99] |
| Stroke | 394 | SDMA predicts all-cause mortality | 2010 | [100] |
| Polycystic ovary syndrome (PCOS) | 16 | ND | 2011 | [101] |
| Glaucoma | 210 | Elevated SDMA in advanced glaucoma | 2012 | [80] |
| Hyperuricemia | 58 | SDMA correlates with uric acid level | 2013 | [102] |
| Malaria | 123 | ND | 2014 | [103] |
Studies tabulated according to year of first report. ND, not determined.
3.4. Causal Link between the Plasma Levels of ADMA or SDMA and Clinical Outcome
The list of clinical conditions associated with elevated ADMA and SDMA levels continues to grow; however, these clinical observations only describe relationships and do not allow for interpretation of the causality. A few human studies have demonstrated that the administration of ADMA to healthy volunteers leads to endothelial dysfunction, increased vascular resistance and arterial blood pressure, as well as decreased cardiac output [105,106]. Although dimethylarginine levels have been analyzed in different tissue fluid samples in specific populations [107,108], almost all studies demonstrating an association between ADMA or SDMA and clinical diseases referred to blood plasma levels of ADMA or SDMA and not tissue levels. Although many studies have demonstrated that plasma ADMA or SDMA levels are elevated in patients with a broad range of disorders, intracellular ADMA and SDMA levels in these disorders have not been well studied. Human tissue samples are difficult to attain and thus in vitro studies may be advantageous for studying intracellular dimethylarginine regulation. It furthermore remains to be determined whether reduced levels of ADMA and SDMA result in reduced CVD risk and improved outcome in the above mentioned diseases. It stands to reason that much of our knowledge on potential therapies involving lowering ADMA and SDMA in specific diseases is based on animal research.
4. Pathophysiology of ADMA and SDMA
4.1. ADMA and SDMA: Inhibition of NO Synthesis
The most well-known effect of ADMA and SDMA is the inhibition of NO production. At physiological extracellular l-arginine and ADMA concentrations, intracellular NOS is well saturated with the substrate l-arginine and physiological levels of NO are produced. In the presence of pathological concentrations of ADMA, NOS activity decreases, resulting in a reduction of NO. Cellular ADMA levels can be 5- to 20-fold higher than those in the plasma and can fall in the range known to inhibit NOS [26]. Under such conditions, the addition of exogenous l-arginine shifts intracellular ADMA and restores the physiological l-arginine:ADMA ratio to a level that preserves sufficient NO production. The state of NOS activation or inhibition therefore depends on the local intracellular l-arginine:ADMA ratio. SDMA, on the other hand, does not directly inhibit NOS but is a competitive inhibitor of l-arginine transport [12].
4.2. Tissue ADMA and SDMA Concentrations
Although many human diseases, including CVD, are associated with increased plasma levels of ADMA and SDMA, little is known to date about intracellular levels. Elevated ADMA levels in the kidneys develop early on, even before the onset of hypertension in four-week-old spontaneously hypertensive rats (SHRs) [109]. Moreover, elevated levels of ADMA in the lung were observed in the hypertensive stage in SHRs [110]. A previous report furthermore demonstrated that ADMA concentrations are increased in the aortas of obese diabetic mice [111] and in a streptozotocin (STZ)-induced diabetic mother rat model, offspring developed hypertension and kidney disease, which is associated with elevated renal levels of ADMA [112]. These findings suggest a role for intracellular ADMA in the development of CVD.
A recent report showed strong differences in ADMA and SDMA levels between different tissues from mice [113]: the concentrations of ADMA and SDMA are high in the kidney, liver, pancreas, and spleen; intermediate in the lung and heart; and lowest in the brain. The differences in ADMA abundance across different tissues may be due to differential expression of DDAHs in various tissues. Data from a DDAH-1 and -2 knockdown model showed that ADMA is regulated by DDAH-1, which is expressed at sites of ADMA metabolism in the kidney cortex and liver, whereas NO is regulated primarily by DDAH-2, which is expressed strongly in the blood vessels [114]. Although DDAH-1 is also highly expressed in the kidney and liver [115], both these organs have been reported as major sites for the metabolism of excessive circulating ADMA [116]. Accordingly, ADMA concentrations are high in the liver and kidney. Since DDAH-1 is abundantly expressed in the brain at sites of neuronal NOS expression [98], ADMA may be expeditiously metabolized by DDAH-1 in the brain. Intracellular ADMA can, moreover, be regulated differentially in different tissues in the same disease model. Plasma, hepatic, and renal ADMA levels have been evaluated simultaneously in young rats two weeks after bile-duct ligation (BDL), a commonly used cholestatic liver disease model [117]. The increase in circulating ADMA results primarily from increased synthesis of ADMA (by increased PRMT1 abundance) in the liver. The metabolism of ADMA is unaltered in the damaged liver, indicating unaltered DDAH expression and/or activity in the liver. The decreased renal DDAH activity, however, suggests that the kidney is unable to metabolize excessive ADMA. Unlike liver and kidney ADMA levels, ADMA levels in brain cortex of young BDL rats were not altered [118]. These findings highlight the importance of studying tissue ADMA levels instead of plasma ADMA levels: changes in plasma ADMA do not correlate with intracellular ADMA levels in different tissues. It is therefore important to note that systemic and tissue ADMA levels must be assessed simultaneously to elucidate the relative importance of different mechanisms regulating ADMA homeostasis.
4.3. ADMA: Multifunctional Effects
ADMA can uncouple NOS isoenzymes to produce superoxide, contributing to the burden of oxidative stress [119]. Furthermore, three transcriptomic studies have suggested that ADMA may contribute to a wide range of pathologies [120,121,122]. Using microarray technology, Smith et al. first reported that >50 genes were altered in endothelial cells in response to pathological concentrations of ADMA [120] and BMP signaling and enzymes involved in the arginine methylation pathway were also shown to be significantly regulated by ADMA levels. Next-generation sequencing (NGS) was subsequently used to assess the renal transcriptome response to ADMA in the developing kidney. A total of 1221 differentially expressed genes (DEGs) (735 up- and 486 down-regulated genes in ADMA-treated vs. control samples) were identified. Thirteen significantly related Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways were identified in the developing kidney treated with ADMA, including ribosome, cytokine-cytokine receptor interaction, chemokine signaling pathway, neuroactive ligand-receptor interaction, arachidonic acid metabolism, intestinal immune network for IgA production, systemic lupus erythematosus, toll-like receptor signaling pathway, NOD-like receptor signaling pathway, tyrosine metabolism, and the MAPK signaling pathway [112,122]. A recent report furthermore showed that serum starvation profoundly altered the gene expression of LoVo tumor cells by microarray analysis and that ADMA could restore most of the changes at the transcriptional level [122]. These findings imply that pathophysiological concentrations of ADMA can elicit significant changes at the gene expression level and that these changes may be exerted in a NO pathway-independent manner.
4.4. SDMA: Pro-Inflammatory and Pro-Oxidant Properties
Compared with ADMA, little attention has been paid to the pathophysiological role of SDMA. In addition to inhibiting NO production [12], SDMA may have pro-inflammatory effects [123]. SDMA has been reported to induce the expression of CD11a, CD11b, and CD14 in monocytes as well as CD18 expression in granulocytes to enhance the differentiation and adhesion capacity of leukocytes to the endothelium. Additionally, SDMA may induce reactive oxygen species (ROS) via store-operated calcium influx in monocytes [15] and enhancement of NADPH-oxidase via the activation of endothelial Toll-like receptor-2 [124]. Accordingly, SDMA may be involved directly or indirectly in the pathogenesis of CVD because of its pro-inflammatory and pro-oxidant properties.
5. Potential Therapies for Reducing ADMA and SDMA Levels
To date, there is a lack of potential therapeutic strategies against elevated ADMA and SDMA levels in various diseases. Since both dimethylarginines are water-soluble uremic toxins [2], it would be logical to consider dialysis as a potential means of decreasing of circulating ADMA and SDMA levels. A previous study showed that a single dialysis session reduced ADMA and SDMA plasma levels by 23% and 40%, respectively [125], and the removal of ADMA and SDMA by dialysis seems to be hampered by complex kinetics of these two uremic toxins. Dialysis is furthermore not suitable for non-uremia patients in clinical practice.
Since approximately 80% of ADMA is metabolized in the body, alternative therapeutic approaches have been assessed; however, to date, a specific ADMA-lowering agent is still not available. As previously reviewed by us and others [6,122,126], a few drugs have been reported to lower ADMA levels in clinical studies. These include angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, fenofibrate, oral contraceptives, folic acid, metformin, and α-lipoic acid. Despite a partial reduction of plasma ADMA levels by these therapies, the underlying mechanisms of their ADMA-lowering effects are still unclear. Since PRMTs control ADMA production and as DDAHs and AGXT2 regulate its metabolism, the discovery and application of specific PRMT inhibitors, DDAH activators, or AGXT2 activators may represent potential therapeutic strategies. The development of specific PRMT inhibitors, DDAH activators, and AGXT2 activators for ADMA suppression, however, remains a challenging area of research [7,127,128]. Currently, numerous therapies have been shown to reduce ADMA concentrations in a wide range of animal models (Table 3) [110,112,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168]. Some of the major approaches include the restoration of the imbalance between l-arginine and ADMA, the regulation of DDAH enzymes and/or activity, and the inhibition of PRMT expression.
Table 3.
Animal models showing intervention with ADMA-lowering effects.
| Animal Models | Intervention | Protective Effects | Year of First Report | Ref. |
|---|---|---|---|---|
| LDL injection-induced endothelial dysfunction in rat | Probucol | Preserve endothelial function | 2002 | [129] |
| LDL injection-induced endothelial dysfunction in rat | 17β-estradiol | Preserve endothelial function | 2004 | [130] |
| Spontaneously hypertensive rat (SHR) | Pioglitazone | Increase renal DDAH-2 expression; Prevent hypertension | 2005 | [131] |
| Zucker diabetic fatty rat | Farnesoid X receptor agonist | Increase hepatic DDAH-1 expression; Prevent atherosclerosis | 2006 | [132] |
| LDL injection-induced endothelial dysfunction in rat | Taurine | Preserve endothelial function | 2007 | [133] |
| Stress-induced preeclampsia in pregnant rat | l-arginine | Prevent hypertension and proteinuria | 2008 | [134] |
| SHR | Rosuvastatin | Attenuate hypertension | 2008 | [135] |
| STZ-induced diabetic rat | Telmisartan | Reduce renal PRMT-1 expression; Increase renal DDAH-1 expression | 2008 | [136] |
| Ethanol-induced gastric mucosal injury in rat | Resveratrol analog BTM-0512 | Prevent gastric mucosa injury; Increase DDAH activity | 2010 | [137] |
| Bile duct-ligated cirrhotic rat | Melatonin | Prevent liver damage; Increase DDAH activity | 2010 | [117] |
| SHR | Melatonin | Prevent hypertension; Increase DDAH activity | 2010 | [138] |
| SHR | Aliskiren | Prevent hypertension | 2011 | [139] |
| SHR | Nebivolol | Prevent hypertension | 2011 | [140] |
| Monocrotaline-induced pulmonary hypertension in rat | Rosuvastatin | Prevent pulmonary hypertension | 2011 | [141] |
| Bile duct-ligated cirrhotic rat | Ornithine phenylacetate | Prevent liver damage | 2012 | [142] |
| High-fat diet in rat | Atorvastatin | Improve endothelial function; Increase DDAH activity | 2012 | [143] |
| 5/6 nephrectomized rats | Shichimotsukokato | Prevent hypertension; Increase DDAH-2 level | 2012 | [144] |
| Bile duct-ligated cirrhotic rat | Vitamin E | Improve endothelial function; Increase hepatic DDAH-2 level | 2012 | [145] |
| Coronary artery-ligated rat | Salvianolic acid A | Improve cardiac damage; Increase DDAH activity | 2013 | [146] |
| STZ-induced diabetic pregnant rat | l-citrulline | Prevent offspring hypertension; Increase renal DDAH-2 level | 2013 | [112] |
| STZ-induced diabetic rat | Glucagon-like peptide-1 receptor agonist | Protect diabetic nephropathy; Reduce PRMT-1 expression | 2013 | [147] |
| SHR | N-acetylcysteine | Prevent gastric mucosa injury; Increase DDAH activity | 2013 | [148] |
| Prenatal dexamethasone exposure in rat | l-citrulline | Prevent offspring hypertension | 2014 | [149] |
| SHR | l-citrulline | Prevent hypertension | 2014 | [150] |
| SHR | Sodium nitrate | Prevent hypertension | 2014 | [150] |
| High-fat and high-cholesterol diet in rat | Atorvastatin plus rosiglitazone | Protect endothelial function | 2014 | [151] |
| Isoproterenol-induced heart failure in rat | Oxymatrine | Ameliorate ventricular function and hypertrophy; Increase DDAH-2 expression | 2014 | [152] |
| Angiotensin II-induced hypertension in rat | Serelaxin | Attenuate hypertension and proteinuria | 2014 | [153] |
| Lipopolysaccharide/D-galactosamine-induced liver injury | Metformin | Protect liver injury/Increase DDAH activity | 2014 | [154] |
| SHR | Metformin | Prevent hypertension | 2014 | [110] |
| Maternal caloric restriction.rat | Melatonin | Prevent offspring hypertension | 2014 | [155] |
| Constriction of artery-induced subarachnoid hemorrhage in rat | 18β-glycyrrhetinic acid | Improve neurological outcome | 2015 | [156] |
| Myocardial ischemia/reperfusion injury in rat | Apocynin | Protect myocardial injury | 2015 | [157] |
| Maternal caloric restriction.rat | Aliskiren | Prevent offspring hypertension | 2015 | [158] |
| High-fat and high-cholesterol diet in rat | Atorvastatin | Protective endothelial function | 2015 | [159] |
| 10% furctose administration rat | Fenofibrate | Reduce triglyceride level | 2015 | [160] |
| Cyclosporine-induced nephrotoxicity | Nebivolol | Ameliorate endothelial function | 2016 | [161] |
| l-NAME induced hypertension in rat | Novokinin | Prevent hypertension | 2016 | [162] |
| Bile duct-ligated cirrhotic rat | Etanercept | Prevent brain damage | 2016 | [163] |
| 2016 | [164] | |||
| STZ-induced cognitive impairment in rat | H2S releasing compounds ATB-346 and diallyl trisulfide | Ameliorate behavior performance | 2016 | [165] |
| Aged rat | Epigallocatechin-3-gallate | Ameliorate erectile function; reduce PRMT-1 expression; Increase DDAH activity | 2016 | [166] |
| Prenatal dexamethasone plus postnatal high-fat diet in rat | N-acetylcysteine | Prevent hypertension | 2016 | [167] |
| Isoproterenol-induced heart failure in rat | Rosuvastatin | Ameliorate ventricular function and hypertrophy; Reduce PRMT-1 expression; Increase DDAH-2 expression | 2016 | [168] |
Studies tabulated according to year of first report.
Since l-arginine is the substrate for NOS-mediated production of NO, l-arginine and l-citrulline (the precursor of l-arginine) supplementation have been reported to reduce ADMA and increase NO bioavailability in a variety of models with elevated ADMA levels [112,134,149,150]. A number of animal studies have furthermore indicated that pioglitazone [131], farnesoid X receptor agonist [132], telmisartan [136], resveratrol [137], melatonin [117,138], atorvastatin [143], shichimotsukokato [144], vitamin E [145], salvianolic acid A [146], N-acetylcysteine [148], oxymatrine [152], metformin [154], epigallocatechin-3-gallate [166], and rosuvastatin [168] can increase the activity and/or expression of DDAHs and thereby reduce ADMA levels. On the other hand, telmisartan [136], glucagon-like peptide-1 receptor agonist [147], epigallocatechin-3-gallate [166], and rosuvastatin [168] may reduce ADMA levels via decreased PRMT-1 expression. However, whether these ADMA-lowering therapies not only reduce circulating ADMA levels but also ADMA levels in target organs requires further clarification. Further investigation is also required to determine the mechanisms of other effective ADMA-lowering agents and to clarify whether these agents can be applied to different disease models associated with elevated ADMA levels.
6. Conclusions
Since the first isolation of ADMA and SDMA from human urine in 1970, there has been substantial evidence revealing the significance of these two non-proteinogenic amino acids in human health and diseases. ADMA and SDMA are known uremic toxins and the most well-known effect of these two toxic amino acids is the suppression of NO production. High plasma ADMA or SDMA concentrations not only predict all-cause mortality and CVD events, but are also relevant to a broad range of diseases. Although significant progress has been made in research on ADMA and SDMA, there is a need for a simple and sensitive method for measuring ADMA and SDMA levels simultaneously on a routine basis. The development of specific pharmacological therapy for lowering ADMA and SDMA levels in target organs is still a far-off goal and requires a deeper understanding of the multifunctional effects of ADMA and SDMA in target organs that induce a variety of diseases. Accordingly, there is an urgent need for the elucidation of unknown biological functions and for the development of effective strategies for treating diseases associated with high levels of ADMA and SDMA.
Acknowledgments
This work was supported by the Ministry of Science and Technology, Taiwan (MOST 104-2314-B-182-056-MY3) and the Chang Gung Memorial Hospital, Kaohsiung, Taiwan (Grants CMRPG8E0201, CMRPG8E0202, and CMRPG8F0021).
Author Contributions
You-Lin Tain contributed to concept generation, data interpretation, drafting of the manuscript, critical revision of the manuscript, and approval of the article; Chien-Ning Hsu contributed to the concept generation, data interpretation, critical revision of the manuscript, and approval of the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Kakimoto Y., Akazawa S. Isolation and identification of NG,NG- and NG,N'G-dimethyl-arginine, Nε-mono-, di-, and trimethyllysine, and glucosylgalactosyl- and galactosyl-δ-hydroxylysine from human urine. J. Biol. Chem. 1970;245:5751–5758. [PubMed] [Google Scholar]
- 2.Vanholder R., De Smet R., Glorieux G., Argilés A., Baurmeister U., Brunet P., Clark W., Cohen G., De Deyn P.P., Deppisch R., et al. Review on uremic toxins: Classification, concentration, and interindividual variability. Kidney Int. 2003;63:1934–1943. doi: 10.1046/j.1523-1755.2003.00924.x. [DOI] [PubMed] [Google Scholar]
- 3.Vallance P., Leone A., Calver A., Collier J., Moncada S. Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet. 1992;339:572–575. doi: 10.1016/0140-6736(92)90865-z. [DOI] [PubMed] [Google Scholar]
- 4.Vallance P., Leiper J. Cardiovascular biology of the asymmetric dimethylarginine:dimethylarginine dimethylaminohydrolase pathway. Arterioscler. Thromb. Vasc. Biol. 2004;24:1023–1030. doi: 10.1161/01.ATV.0000128897.54893.26. [DOI] [PubMed] [Google Scholar]
- 5.Zakrzewicz D., Eickelberg O. From arginine methylation to ADMA: A novel mechanism with therapeutic potential in chronic lung diseases. BMC Pulm. Med. 2009;9:5. doi: 10.1186/1471-2466-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tain Y.L., Huang L.T. Asymmetric dimethylarginine: Clinical applications in pediatric medicine. J. Formos. Med. Assoc. 2011;110:70–77. doi: 10.1016/S0929-6646(11)60012-0. [DOI] [PubMed] [Google Scholar]
- 7.Leiper J., Nandi M. The therapeutic potential of targeting endogenous inhibitors of nitric oxide synthesis. Nat. Rev. Drug Discov. 2011;10:277–291. doi: 10.1038/nrd3358. [DOI] [PubMed] [Google Scholar]
- 8.Huang L.T., Hsieh C.S., Chang K.A., Tain Y.L. Roles of nitric oxide and asymmetric dimethylarginine in pregnancy and fetal programming. Int. J. Mol. Sci. 2012;13:14606–14622. doi: 10.3390/ijms131114606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schepers E., Speer T., Bode-Böger S.M., Fliser D., Kielstein J.T. Dimethylarginines ADMA and SDMA: The real water-soluble small toxins? Semin. Nephrol. 2014;34:97–105. doi: 10.1016/j.semnephrol.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Brinkmann S.J., de Boer M.C., Buijs N., van Leeuwen P.A. Asymmetric dimethylarginine and critical illness. Curr. Opin. Clin. Nutr. Metab. Care. 2014;17:90–97. doi: 10.1097/MCO.0000000000000020. [DOI] [PubMed] [Google Scholar]
- 11.Kielstein J.T., Fliser D. The past, presence and future of ADMA in nephrology. Nephrol. Ther. 2007;3:47–54. doi: 10.1016/j.nephro.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Bode-Boger S.M., Scalera F., Kielstein J.T., Martens-Lobenhoffer J., Breithardt G., Fobker M., Reinecke H. Symmetrical dimethylarginine: A new combined parameter for renal function and extent of coronary artery disease. J. Am. Soc. Nephrol. 2006;17:1128–1134. doi: 10.1681/ASN.2005101119. [DOI] [PubMed] [Google Scholar]
- 13.Cooke J.P. Does ADMA cause endothelial dysfunction? Arterioscler. Thromb. Vasc. Biol. 2000;20:2032–2037. doi: 10.1161/01.ATV.20.9.2032. [DOI] [PubMed] [Google Scholar]
- 14.Sydow K., Münzel T. ADMA and oxidative stress. Atheroscler. Suppl. 2003;4:41–51. doi: 10.1016/S1567-5688(03)00033-3. [DOI] [PubMed] [Google Scholar]
- 15.Schepers E., Glorieux G., Dhondt A., Leybaert L., Vanholder R. Role of symmetric dimethylarginine in vascular damage by increasing ROS via store-operated calcium influx in monocytes. Nephrol. Dial. Transplant. 2009;24:1429–1435. doi: 10.1093/ndt/gfn670. [DOI] [PubMed] [Google Scholar]
- 16.Zhang L., Wan Y.N., Zhao J.H., Wang Y.J., Wang Y.X., Yan J.W., Huang X.L., Wang J. The association between systemic sclerosis, arginine and asymmetric dimethylarginine. Inflammation. 2015;38:218–223. doi: 10.1007/s10753-014-0025-9. [DOI] [PubMed] [Google Scholar]
- 17.Schepers E., Barreto D.V., Liabeuf S., Glorieux G., Eloot S., Barreto F.C., Massy Z., Vanholder R., European Uremic Toxin Work Group (EUTox) Symmetric dimethylarginine as a proinflammatory agent in chronic kidney disease. Clin. J. Am. Soc. Nephrol. 2011;6:2374–8233. doi: 10.2215/CJN.01720211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park M.J., Oh K.S., Nho J.H., Kim G.Y., Kim D.I. Asymmetric dimethylarginine (ADMA) treatment induces apoptosis in cultured rat mesangial cells via endoplasmic reticulum stress activation. Cell Biol. Int. 2016;40:662–670. doi: 10.1002/cbin.10602. [DOI] [PubMed] [Google Scholar]
- 19.Shirakawa T., Kako K., Shimada T., Nagashima Y., Nakamura A., Ishida J., Fukamizu A. Production of free methylarginines via the proteasome and autophagy pathways in cultured cells. Mol. Med. Rep. 2011;4:615–620. doi: 10.3892/mmr.2011.488. [DOI] [PubMed] [Google Scholar]
- 20.Pekarova M., Kubala L., Martiskova H., Bino L., Twarogova M., Klinke A., Rudolph T.K., Kuchtova Z., Kolarova H., Ambrozova G., et al. Asymmetric dimethylarginine regulates the lipopolysaccharide-induced nitric oxide production in macrophages by suppressing the activation of NF-kappaB and iNOS expression. Eur. J. Pharmacol. 2013;713:68–77. doi: 10.1016/j.ejphar.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 21.Morales Y., Cáceres T., May K., Hevel J.M. Biochemistry and regulation of the protein arginine methyltransferases (PRMTs) Arch. Biochem. Biophys. 2016;590:138–152. doi: 10.1016/j.abb.2015.11.030. [DOI] [PubMed] [Google Scholar]
- 22.Raijmakers R., Zendman A.J., Egberts W.V., Vossenaar E.R., Raats J., Soede-Huijbregts C., Rutjes F.P., van Veelen P.A., Drijfhout J.W., Pruijn G.J. Methylation of arginine residues interferes with citrullination by peptidylarginine deiminases in vitro. J. Mol. Biol. 2007;367:1118–1129. doi: 10.1016/j.jmb.2007.01.054. [DOI] [PubMed] [Google Scholar]
- 23.Chang B., Chen Y., Zhao Y., Bruick R.K. JMJD6 is a histone arginine demethylase. Science. 2007;318:444–447. doi: 10.1126/science.1145801. [DOI] [PubMed] [Google Scholar]
- 24.Böttger A., Islam M.S., Chowdhury R., Schofield C.J., Wolf A. The oxygenase Jmjd6—A case study in conflicting assignments. Biochem. J. 2015;468:191–202. doi: 10.1042/BJ20150278. [DOI] [PubMed] [Google Scholar]
- 25.Bode-Böger S.M., Scalera F., Ignarro L.J. The l-arginine paradox: Importance of the l-arginine/asymmetrical dimethylarginine ratio. Pharmacol. Ther. 2007;114:295–306. doi: 10.1016/j.pharmthera.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 26.Teerlink T., Luo Z., Palm F., Wilcox C.S. Cellular ADMA: Regulation and action. Pharmacol. Res. 2009;60:448–460. doi: 10.1016/j.phrs.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rodionov R.N., Martens-Lobenhoffer J., Brilloff S., Hohenstein B., Jarzebska N., Jabs N., Kittel A., Maas R., Weiss N., Bode-Böger S.M. Role of alanine:glyoxylate aminotransferase 2 in metabolism of asymmetric dimethylarginine in the settings of asymmetric dimethylarginine overload and bilateral nephrectomy. Nephrol. Dial. Transplant. 2014;29:2035–2042. doi: 10.1093/ndt/gfu236. [DOI] [PubMed] [Google Scholar]
- 28.Palm F., Onozato M.L., Luo Z., Wilcox C.S. Dimethylarginine dimethylaminohydrolase (DDAH): Expression, regulation, and function in the cardiovascular and renal systems. Am. J. Physiol. Heart Circ. Physiol. 2007;293:H3227–H3245. doi: 10.1152/ajpheart.00998.2007. [DOI] [PubMed] [Google Scholar]
- 29.Sorrenti V., Mazza F., Campisi A., Vanella L., Li V.G., Di G.C. High glucose-mediated imbalance of nitric oxide synthase and dimethylarginine dimethylaminohydrolase expression in endothelial cells. Curr. Neurovasc. Res. 2006;3:49–54. doi: 10.2174/156720206775541778. [DOI] [PubMed] [Google Scholar]
- 30.Tain Y.L., Kao Y.H., Hsieh C.S., Chen C.C., Sheen J.M., Lin I.C., Huang L.T. Melatonin blocks oxidative stress-induced increased asymmetric dimethylarginine. Free Radic. Biol. Med. 2010;49:1088–1098. doi: 10.1016/j.freeradbiomed.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 31.Brands M.W., Bell T.D., Gibson B. Nitric oxide may prevent hypertension early in diabetes by counteracting renal actions of superoxide. Hypertension. 2004;43:57–63. doi: 10.1161/01.HYP.0000104524.25807.EE. [DOI] [PubMed] [Google Scholar]
- 32.Kittel A., Maas R., König J., Mieth M., Weiss N., Jarzebska N., Hohenstein B., Martens-Lobenhoffer J., Bode-Böger S.M., Rodionov R.N. In vivo evidence that Agxt2 can regulate plasma levels of dimethylarginines in mice. Biochem. Biophys. Res. Commun. 2013;430:84–89. doi: 10.1016/j.bbrc.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 33.Tsikas D. A critical review and discussion of analytical methods in the l-arginine/nitric oxide area of basic and clinical research. Anal. Biochem. 2008;379:139–163. doi: 10.1016/j.ab.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 34.Teerlink T., Nijveldt R.J., de Jong S., van Leeuwen P.A.M. Determination of arginine, asymmetric dimethylarginine, and symmetric dimethylarginine in human plasma and other biological samples by high-performance liquid chromatography. Anal. Biochem. 2002;303:131–137. doi: 10.1006/abio.2001.5575. [DOI] [PubMed] [Google Scholar]
- 35.Tsikas D., Beckmann B., Gutzki F.M., Jordan J. Simultaneous gas chromatography-tandem mass spectrometry quantification of symmetric and asymmetric dimethylarginine in human urine. Anal. Biochem. 2011;413:60–66. doi: 10.1016/j.ab.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 36.Hui Y., Wong M., Kim J.-O., Love J., Ansley D.M., Chen D.D.Y. A new derivatization method coupled with LC-MS/MS to enable baseline separation and quantification of dimethylarginines in human plasma from patients to receive on-pump CABG surgery. Electrophoresis. 2012;33:1911–1920. doi: 10.1002/elps.201100536. [DOI] [PubMed] [Google Scholar]
- 37.Martens-Lobenhoffer J., Krug O., Bode-Boger S.M. Determination of arginine and asymmetric dimethylarginine (ADMA) in human plasma by liquid chromatography/mass spectrometry with the isotope dilution technique. J. Mass Spectrom. 2004;39:1287–1294. doi: 10.1002/jms.684. [DOI] [PubMed] [Google Scholar]
- 38.Boelaert J., Schepers E., Glorieux G., Eloot S., Vanholder R., Lynen F. Determination of Asymmetric and Symmetric Dimethylarginine in Serum from Patients with Chronic Kidney Disease: UPLC-MS/MS versus ELISA. Toxins (Basel) 2016;8:E149. doi: 10.3390/toxins8050149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schulze F., Wesemann R., Schwedhelm E., Sydow K., Albsmeier J., Cooke J.P., Böger R.H. Determination of asymmetric dimethylarginine (ADMA) using a novel ELISA assay. Clin. Chem. Lab. Med. 2004;42:1377–1383. doi: 10.1515/CCLM.2004.257. [DOI] [PubMed] [Google Scholar]
- 40.Horowitz J.D., Heresztyn T. An overview of plasma concentrations of asymmetric dimethylarginine (ADMA) in health and disease and in clinical studies: Methodological considerations. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2007;851:42–50. doi: 10.1016/j.jchromb.2006.09.023. [DOI] [PubMed] [Google Scholar]
- 41.Martens-Lobenhoffer J., Westphal S., Awiszus F., Bode-Boger S.M., Luley C. Determination of asymmetric dimethylarginine: Liquid chromatography-mass spectrometry or ELISA? Clin. Chem. 2005;51:2188–2189. doi: 10.1373/clinchem.2005.056788. [DOI] [PubMed] [Google Scholar]
- 42.Leiper J., Vallance P. Biological significance of endogenous methylarginines that inhibit nitric oxide synthases. Cardiovasc. Res. 1999;43:542–548. doi: 10.1016/S0008-6363(99)00162-5. [DOI] [PubMed] [Google Scholar]
- 43.Jacobi J., Tsao P.S. Asymmetrical dimethylarginine in renal disease: Limits of variation or variation limits? A systematic review. Am. J. Nephrol. 2008;28:224–237. doi: 10.1159/000110092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kielstein J.T., Salpeter S.R., Bode-Boeger S.M., Cooke J.P., Fliser D. Symmetric dimethylarginine (SDMA) as endogenous marker of renal function—A meta-analysis. Nephrol. Dial. Transplant. 2006;21:2446–2451. doi: 10.1093/ndt/gfl292. [DOI] [PubMed] [Google Scholar]
- 45.Zoccali C., Bode-Böger S., Mallamaci F., Benedetto F., Tripepi G., Malatino L., Cataliotti A., Bellanuova I., Fermo I., Frölich J., et al. Plasma concentration of asymmetrical dimethylarginine and mortality in patients with end-stage renal disease: A prospective study. Lancet. 2001;358:2113–2117. doi: 10.1016/S0140-6736(01)07217-8. [DOI] [PubMed] [Google Scholar]
- 46.Schlesinger S., Sonntag S.R., Lieb W., Maas R. Asymmetric and symmetric dimethylarginine as risk markers for total mortality and cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. PLoS ONE. 2016;11:e0165811. doi: 10.1371/journal.pone.0165811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Das I., Khan N.S., Puri B.K., Hirsch S.R. Elevated endogenous nitric oxide synthase inhibitor in schizophrenic plasma may reflect abnormalities in brain nitric oxide production. Neurosci. Lett. 1996;215:209–211. doi: 10.1016/0304-3940(96)12972-4. [DOI] [PubMed] [Google Scholar]
- 48.Goonasekera C.D., Rees D.D., Woolard P., Frend A., Shah V., Dillon M.J. Nitric oxide synthase inhibitors and hypertension in children and adolescents. J. Hypertens. 1997;15:901–909. doi: 10.1097/00004872-199715080-00015. [DOI] [PubMed] [Google Scholar]
- 49.Böger R.H., Bode-Böger S.M., Thiele W., Junker W., Alexander K., Frölich J.C. Biochemical evidence for impaired nitric oxide synthesis in patients with peripheral arterial occlusive disease. Circulation. 1997;95:2068–2074. doi: 10.1161/01.CIR.95.8.2068. [DOI] [PubMed] [Google Scholar]
- 50.Böger R.H., Bode-Böger S.M., Szuba A., Tsao P.S., Chan J.R., Tangphao O., Blaschke T.F., Cooke J.P. Asymmetric dimethylarginine (ADMA): A novel risk factor for endothelial dysfunction: Its role in hypercholesterolemia. Circulation. 1998;98:1842–1847. doi: 10.1161/01.CIR.98.18.1842. [DOI] [PubMed] [Google Scholar]
- 51.Usui M., Matsuoka H., Miyazaki H., Ueda S., Okuda S., Imaizumi T. Increased endogenous nitric oxide synthase inhibitor in patients with congestive heart failure. Life Sci. 1998;62:2425–2430. doi: 10.1016/S0024-3205(98)00225-2. [DOI] [PubMed] [Google Scholar]
- 52.Pettersson A., Hedner T., Milsom I. Increased circulating concentrations of asymmetric dimethyl arginine (ADMA), an endogenous inhibitor of nitric oxide synthesis, in preeclampsia. Acta Obstet. Gynecol. Scand. 1998;77:808–813. doi: 10.1080/j.1600-0412.1998.770805.x. [DOI] [PubMed] [Google Scholar]
- 53.Fard A., Tuck C.H., Donis J.A., Sciacca R., Di Tullio M.R., Wu H.D., Bryant T.A., Chen N.T., Torres-Tamayo M., Ramasamy R., et al. Acute elevations of plasma asymmetric dimethylarginine and impaired endothelial function in response to a high-fat meal in patients with type 2 diabetes. Arterioscler. Thromb. Vasc. Biol. 2000;20:2039–2044. doi: 10.1161/01.ATV.20.9.2039. [DOI] [PubMed] [Google Scholar]
- 54.Gorenflo M., Zheng C., Werle E., Fiehn W., Ulmer H.E. Plasma levels of asymmetrical dimethyl-l-arginine in patients with congenital heart disease and pulmonary hypertension. J. Cardiovasc. Pharmacol. 2001;37:489–492. doi: 10.1097/00005344-200104000-00016. [DOI] [PubMed] [Google Scholar]
- 55.Yoo J.H., Lee S.C. Elevated levels of plasma homocyst(e)ine and asymmetric dimethylarginine in elderly patients with stroke. Atherosclerosis. 2001;158:425–430. doi: 10.1016/S0021-9150(01)00444-0. [DOI] [PubMed] [Google Scholar]
- 56.Hermenegildo C., Medina P., Peiró M., Segarra G., Vila J.M., Ortega J., Lluch S. Plasma concentration of asymmetric dimethylarginine, an endogenous inhibitor of nitric oxide synthase, is elevated in hyperthyroid patients. J. Clin. Endocrinol. Metab. 2002;87:5636–5640. doi: 10.1210/jc.2002-020905. [DOI] [PubMed] [Google Scholar]
- 57.Nijveldt R.J., Teerlink T., Van Der Hoven B., Siroen M.P., Kuik D.J., Rauwerda J.A., van Leeuwen P.A. Asymmetrical dimethylarginine (ADMA) in critically ill patients: High plasma ADMA concentration is an independent risk factor of ICU mortality. Clin. Nutr. 2003;22:23–30. doi: 10.1054/clnu.2002.0613. [DOI] [PubMed] [Google Scholar]
- 58.Lluch P., Torondel B., Medina P., Segarra G., Del Olmo J.A., Serra M.A., Rodrigo J.M. Plasma concentrations of nitric oxide and asymmetric dimethylarginine in human alcoholic cirrhosis. J. Hepatol. 2004;41:55–59. doi: 10.1016/j.jhep.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 59.Tarnow L., Hovind P., Teerlink T., Stehouwer C.D., Parving H.H. Elevated plasma asymmetric dimethylarginine as a marker of cardiovascular morbidity in early diabetic nephropathy in type 1 diabetes. Diabetes Care. 2004;27:765–769. doi: 10.2337/diacare.27.3.765. [DOI] [PubMed] [Google Scholar]
- 60.Eid H.M., Arnesen H., Hjerkinn E.M., Lyberg T., Seljeflot I. Relationship between obesity, smoking, and the endogenous nitric oxide synthase inhibitor, asymmetric dimethylarginine. Metabolism. 2004;53:1574–1579. doi: 10.1016/j.metabol.2004.06.026. [DOI] [PubMed] [Google Scholar]
- 61.Bultink I.E., Teerlink T., Heijst J.A., Dijkmans B.A., Voskuyl A.E. Raised plasma levels of asymmetric dimethylarginine are associated with cardiovascular events, disease activity, and organ damage in patients with systemic lupus erythematosus. Ann. Rheum. Dis. 2005;64:1362–1365. doi: 10.1136/ard.2005.036137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kielstein J.T., Bode-Böger S.M., Hesse G., Martens-Lobenhoffer J., Takacs A., Fliser D., Hoeper M.M. Asymmetrical dimethylarginine in idiopathic pulmonary arterial hypertension. Arterioscler. Thromb. Vasc. Biol. 2005;25:1414–1418. doi: 10.1161/01.ATV.0000168414.06853.f0. [DOI] [PubMed] [Google Scholar]
- 63.Lluch P., Mauricio M.D., Vila J.M., Segarra G., Medina P., Del Olmo J.A., Rodrigo J.M., Serra M.A. Accumulation of symmetric dimethylarginine in hepatorenal syndrome. Exp. Biol. Med. (Maywood) 2006;231:70–75. doi: 10.1177/153537020623100108. [DOI] [PubMed] [Google Scholar]
- 64.Wang J., Sim A.S., Wang X.L., Salonikas C., Naidoo D., Wilcken D.E. Relations between plasma asymmetric dimethylarginine (ADMA) and risk factors for coronary disease. Atherosclerosis. 2006;184:383–388. doi: 10.1016/j.atherosclerosis.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 65.Mittermayer F., Prusa A.R., Pollak A., Wolzt M. Umbilical vein plasma concentrations of asymmetrical dimethylarginine are increased in male but not female neonates delivered preterm: A pilot study. Early Hum. Dev. 2006;82:421–424. doi: 10.1016/j.earlhumdev.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 66.Dooley A., Gao B., Bradley N., Abraham D.J., Black C.M., Jacobs M., Bruckdorfer K.R. Abnormal nitric oxide metabolism in systemic sclerosis: Increased levels of nitrated proteins and asymmetric dimethylarginine. Rheumatology (Oxford) 2006;45:676–684. doi: 10.1093/rheumatology/kei276. [DOI] [PubMed] [Google Scholar]
- 67.Charitidou C., Farmakiotis D., Zournatzi V., Pidonia I., Pegiou T., Karamanis N., Hatzistilianou M., Katsikis I., Panidis D. The administration of estrogens, combined with anti-androgens, has beneficial effects on the hormonal features and asymmetric dimethyl-arginine levels, in women with the polycystic ovary syndrome. Atherosclerosis. 2008;196:958–965. doi: 10.1016/j.atherosclerosis.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 68.Ozkan Y., Firat H., Simşek B., Torun M., Yardim-Akaydin S. Circulating nitric oxide (NO), asymmetric dimethylarginine (ADMA), homocysteine, and oxidative status in obstructive sleep apnea-hypopnea syndrome (OSAHS) Sleep Breath. 2008;12:149–154. doi: 10.1007/s11325-007-0148-4. [DOI] [PubMed] [Google Scholar]
- 69.Nagasaka H., Tsukahara H., Yorifuji T., Miida T., Murayama K., Tsuruoka T., Takatani T., Kanazawa M., Kobayashi K., Okano Y., et al. Evaluation of endogenous nitric oxide synthesis in congenital urea cycle enzyme defects. Metabolism. 2009;58:278–282. doi: 10.1016/j.metabol.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 70.Turiel M., Atzeni F., Tomasoni L., de Portu S., Delfino L., Bodini B.D., Longhi M., Sitia S., Bianchi M., Ferrario P., et al. Non-invasive assessment of coronary flow reserve and ADMA levels: A case-control study of early rheumatoid arthritis patients. Rheumatology (Oxford) 2009;48:834–839. doi: 10.1093/rheumatology/kep082. [DOI] [PubMed] [Google Scholar]
- 71.Kato G.J., Wang Z., Machado R.F., Blackwelder W.C., Taylor J.G., 6th, Hazen S.L. Endogenous nitric oxide synthase inhibitors in sickle cell disease: Abnormal levels and correlations with pulmonary hypertension, desaturation, haemolysis, organ dysfunction and death. Br. J. Haematol. 2009;145:506–513. doi: 10.1111/j.1365-2141.2009.07658.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nagasaka H., Okano Y., Aizawa M., Miida T., Yorifuji T., Tajima G., Sakura N., Takatani T., Sanayama Y., Sugamoto K., et al. Altered metabolisms of mediators controlling vascular function and enhanced oxidative stress in asymptomatic children with congenital portosystemic venous shunt. Metabolism. 2010;59:107–113. doi: 10.1016/j.metabol.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 73.Akdemir N., Cinemre H., Bilir C., Akin O., Akdemir R. Increased serum asymmetric dimethylarginine levels in primary dysmenorrhea. Gynecol. Obstet. Investig. 2010;69:153–156. doi: 10.1159/000264671. [DOI] [PubMed] [Google Scholar]
- 74.Owczarek D., Cibor D., Mach T. Asymmetric dimethylarginine (ADMA), symmetric dimethylarginine (SDMA), arginine, and 8-iso-prostaglandin F2α (8-iso-PGF2α) level in patients with inflammatory bowel diseases. Inflamm. Bowel Dis. 2010;16:52–57. doi: 10.1002/ibd.20994. [DOI] [PubMed] [Google Scholar]
- 75.Scott J.A., North M.L., Rafii M., Huang H., Pencharz P., Subbarao P., Belik J., Grasemann H. Asymmetric dimethylarginine is increased in asthma. Am. J. Respir. Crit. Care Med. 2011;184:779–785. doi: 10.1164/rccm.201011-1810OC. [DOI] [PubMed] [Google Scholar]
- 76.Kasumov T., Edmison J.M., Dasarathy S., Bennett C., Lopez R., Kalhan S.C. Plasma levels of asymmetric dimethylarginine in patients with biopsy-proven nonalcoholic fatty liver disease. Metabolism. 2011;60:776–781. doi: 10.1016/j.metabol.2010.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Atzeni F., Sarzi-Puttini P., Sitia S., Tomasoni L., Gianturco L., Battellino M., Boccassini L., De Gennaro Colonna V., Marchesoni A., Turiel M. Coronary flow reserve and asymmetric dimethylarginine levels: New measurements for identifying subclinical atherosclerosis in patients with psoriatic arthritis. J. Rheumatol. 2011;38:1661–1664. doi: 10.3899/jrheum.100893. [DOI] [PubMed] [Google Scholar]
- 78.Topal G., Donmez A., Doğan B.S., Kucur M., Cengiz D.T., Berkoz F.B., Erdogan N. Asymmetric dimethylarginine (ADMA) levels are increased in patients with fibromyalgia: Correlation with tumor necrosis factor-α (TNF-α) and 8-iso-prostaglandin F2α (8-iso-PGF2α) Clin. Biochem. 2011;44:364–367. doi: 10.1016/j.clinbiochem.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 79.Sulicka J., Surdacki A., Strach M., Kwater A., Gryglewska B., Ćwiklińska M., Balwierz W., Grodzicki T.K. Elevated asymmetric dimethylarginine in young adult survivors of childhood acute lymphoblastic leukemia: A preliminary report. Dis. Markers. 2012;33:69–76. doi: 10.1155/2012/250286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Javadiyan S., Burdon K.P., Whiting M.J., Abhary S., Straga T., Hewitt A.W., Mills R.A., Craig J.E. Elevation of serum asymmetrical and symmetrical dimethylarginine in patients with advanced glaucoma. Investig. Ophthalmol. Vis. Sci. 2012;53:1923–1927. doi: 10.1167/iovs.11-8420. [DOI] [PubMed] [Google Scholar]
- 81.Vasilev V., Matrozova J., Elenkova A., Vandeva S., Kirilov G., Zacharieva S. Asymmetric dimethylarginine (ADMA) and soluble vascular cell adhesion molecule 1(sVCAM-1) as circulating markers for endothelial dysfunction in patients with pheochromocytoma. Exp. Clin. Endocrinol. Diabetes. 2013;121:551–555. doi: 10.1055/s-0033-1353183. [DOI] [PubMed] [Google Scholar]
- 82.Mengeloglu Z., Sünnetcioglu M., Tosun M., Kücükbayrak A., Ceylan M.R., Baran A.I., Karahocagil M., Akdeniz H. High asymmetric dimethylarginine (ADMA) levels in patients with brucellosis. Inflammation. 2014;37:127–131. doi: 10.1007/s10753-013-9720-1. [DOI] [PubMed] [Google Scholar]
- 83.Senol S., Tekumit H., Akar I., Ince I. The role of asymmetric and symmetric dimethylarginine in acute deep vein thrombosis. Ann. Vasc. Surg. 2015;29:1003–1006. doi: 10.1016/j.avsg.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 84.Langen J., Kayacelebi A.A., Beckmann B., Weigt-Usinger K., Carmann C., Hörster I., Lilienthal E., Richter-Unruh A., Tsikas D., Lücke T. Homoarginine (hArg) and asymmetric dimethylarginine (ADMA) in short stature children without and with growth hormone deficiency: hArg and ADMA are involved differently in growth in the childhood. Amino Acids. 2015;47:1875–1883. doi: 10.1007/s00726-015-2028-8. [DOI] [PubMed] [Google Scholar]
- 85.Aydin M., Altintas N., Cem Mutlu L., Bilir B., Oran M., Tülübaş F., Topçu B., Tayfur İ., Küçükyalçin V., Kaplan G., et al. Asymmetric dimethylarginine contributes to airway nitric oxide deficiency in patients with COPD. Clin. Respir. J. 2015 doi: 10.1111/crj.12337. [DOI] [PubMed] [Google Scholar]
- 86.Obayashi K., Saeki K., Kurumatani N. Relationship between asymmetric dimethylarginine and nocturia in the general elderly population: The HEIJO-KYO cohort. Neurourol. Urodyn. 2015;34:769–773. doi: 10.1002/nau.22647. [DOI] [PubMed] [Google Scholar]
- 87.Aydemir O., Ozcan B., Yucel H., Bas A.Y., Demirel N. Asymmetric dimethylarginine and l-arginine levels in neonatal sepsis and septic shock. J. Matern. Fetal Neonatal. Med. 2015;28:977–982. doi: 10.3109/14767058.2014.939950. [DOI] [PubMed] [Google Scholar]
- 88.Isik D.U., Bas A.Y., Demirel N., Kavurt S., Aydemir O., Kavurt A.V., Cetin I. Increased asymmetric dimethylarginine levels in severe transient tachypnea of the newborn. J. Perinatol. 2016;36:459–462. doi: 10.1038/jp.2016.9. [DOI] [PubMed] [Google Scholar]
- 89.Huemer M., Carvalho D.R., Brum J.M., Ünal Ö., Coskun T., Weisfeld-Adams J.D., Schrager N.L., Scholl-Bürgi S., Schlune A., Donner M.G., et al. Clinical phenotype, biochemical profile, and treatment in 19 patients with arginase 1 deficiency. J. Inherit. Metab. Dis. 2016;39:331–340. doi: 10.1007/s10545-016-9928-y. [DOI] [PubMed] [Google Scholar]
- 90.Kirbas S., Kirbas A., Tufekci A., Cumhur Cure M., Cakmak S., Yazici T., Cure E. Serum levels of homocysteine, asymmetric dimethylarginine and nitric oxide in patients with Parkinson’s disease. Acta Clin. Belg. 2016;71:71–75. doi: 10.1080/17843286.2016.1138592. [DOI] [PubMed] [Google Scholar]
- 91.Sydow K., Fortmann S.P., Fair J.M., Varady A., Hlatky M.A., Go A.S., Iribarren C., Tsao P.S., ADVANCE Investigators Distribution of asymmetric dimethylarginine among 980 healthy, older adults of different ethnicities. Clin. Chem. 2010;56:111–120. doi: 10.1373/clinchem.2009.136200. [DOI] [PubMed] [Google Scholar]
- 92.Vida G., Sulyok E., Ertl T., Martens-Lobenhoffer J., Bode-Boger S.M. Plasma asymmetric dimethylarginine concentration during the perinatal period. Neonatology. 2007;92:8–13. doi: 10.1159/000098411. [DOI] [PubMed] [Google Scholar]
- 93.Lücke T., Kanzelmeyer N., Kemper M.J., Tsikas D., Das A.M. Developmental changes in the l-arginine/nitric oxide pathway from infancy to adulthood: Plasma asymmetric dimethylarginine levels decrease with age. Clin. Chem. Lab. Med. 2007;45:1525–1530. doi: 10.1515/CCLM.2007.300. [DOI] [PubMed] [Google Scholar]
- 94.Brunetti-Pierri N., Erez A., Shchelochkov O., Craigen W., Lee B. Systemic hypertension in two patients with ASL deficiency: A result of nitric oxide deficiency? Mol. Genet. Metab. 2009;98:195–197. doi: 10.1016/j.ymgme.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.MacAllister R.J., Rambausek M.H., Vallance P., Williams D., Hoffmann K.H., Ritz E. Concentration of dimethyl-l-arginine in the plasma of patients with end-stage renal failure. Nephrol. Dial. Transplant. 1996;11:2449–2452. doi: 10.1093/oxfordjournals.ndt.a027213. [DOI] [PubMed] [Google Scholar]
- 96.Krzyzanowska K., Mittermayer F., Shnawa N., Hofer M., Schnabler J., Etmüller Y., Kapiotis S., Wolzt M., Schernthaner G. Asymmetrical dimethylarginine is related to renal function, chronic inflammation and macroangiopathy in patients with Type 2 diabetes and albuminuria. Diabet. Med. 2007;24:81–86. doi: 10.1111/j.1464-5491.2007.02018.x. [DOI] [PubMed] [Google Scholar]
- 97.Mookerjee R.P., Malaki M., Davies N.A., Hodges S.J., Dalton R.N., Turner C., Sen S., Williams R., Leiper J., Vallance P., et al. Increasing dimethylarginine levels are associated with adverse clinical outcome in severe alcoholic hepatitis. Hepatology. 2007;45:62–71. doi: 10.1002/hep.21491. [DOI] [PubMed] [Google Scholar]
- 98.Tang W.H., Tong W., Shrestha K., Wang Z., Levison B.S., Delfraino B., Hu B., Troughton R.W., Klein A.L., Hazen S.L. Differential effects of arginine methylation on diastolic dysfunction and disease progression in patients with chronic systolic heart failure. Eur. Heart J. 2008;29:2506–2513. doi: 10.1093/eurheartj/ehn360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schulze F., Carter A.M., Schwedhelm E., Ajjan R., Maas R., von Holten R.A., Atzler D., Grant P.J., Böger R.H. Symmetric dimethylarginine predicts all-cause mortality following ischemic stroke. Atherosclerosis. 2010;208:518–523. doi: 10.1016/j.atherosclerosis.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 100.Lakhani K., Kay A.R., Leiper J., Barry J.A., Hardiman P.J. Symmetric dimethylarginine (SDMA) is raised in women with polycystic ovary syndrome: A pilot study. J. Obstet. Gynaecol. 2011;31:417–419. doi: 10.3109/01443615.2011.569779. [DOI] [PubMed] [Google Scholar]
- 101.Braekke K., Ueland P.M., Harsem N.K., Staff A.C. Asymmetric dimethylarginine in the maternal and fetal circulation in preeclampsia. Pediatr. Res. 2009;66:411–415. doi: 10.1203/PDR.0b013e3181b33392. [DOI] [PubMed] [Google Scholar]
- 102.Tenderenda-Banasiuk E., Wasilewska A., Taranta-Janusz K., Korzeniecka-Kozerska A. Asymmetric and symmetric dimethylarginine in adolescents with hyperuricemia. Dis. Mark. 2013;35:407–412. doi: 10.1155/2013/267697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Weinberg J.B., Yeo T.W., Mukemba J.P., Florence S.M., Volkheimer A.D., Wang H., Chen Y., Rubach M., Granger D.L., Mwaikambo E.D., et al. Dimethylarginines: Endogenous inhibitors of nitric oxide synthesis in children with falciparum malaria. J. Infect. Dis. 2014;210:913–922. doi: 10.1093/infdis/jiu156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kielstein J.T., Veldink H., Martens-Lobenhoffer J., Haller H., Burg M., Lorenzen J.M., Lichtinghagen R., Bode-Böger S.M., Kliem V. SDMA is an early marker of change in GFR after living-related kidney donation. Nephrol. Dial. Transplant. 2011;26:324–338. doi: 10.1093/ndt/gfq395. [DOI] [PubMed] [Google Scholar]
- 105.Calver A., Collier J., Leone A., Moncada S., Vallance P. Effect of local intra-arterial asymmetric dimethylarginine (ADMA) on the forearm arteriolar bed of healthy volunteers. J. Hum. Hypertens. 1993;7:193–194. [PubMed] [Google Scholar]
- 106.Achan V., Broadhead M., Malaki M., Whitley G., Leiper J., MacAllister R., Vallance P. Asymmetric dimethylarginine causes hypertension and cardiac dysfunction in humans and is actively metabolized by dimethylarginine dimethylaminohydrolase. Arterioscler. Thromb. Vasc. Biol. 2003;23:1455–1459. doi: 10.1161/01.ATV.0000081742.92006.59. [DOI] [PubMed] [Google Scholar]
- 107.Brouns R., Marescau B., Possemiers I., Sheorajpanday R., De Deyn P.P. Dimethylarginine levels in cerebrospinal fluid of hyperacute ischemic stroke patients are associated with stroke severity. Neurochem. Res. 2009;34:1642–1649. doi: 10.1007/s11064-009-9954-3. [DOI] [PubMed] [Google Scholar]
- 108.Kuo H.C., Hsu C.N., Huang C.F., Lo M.H., Chien S.J., Tain Y.L. Urinary arginine methylation index associated with ambulatory blood pressure abnormalities in children with chronic kidney disease. J. Am. Soc. Hypertens. 2012;6:385–392. doi: 10.1016/j.jash.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 109.Hsu C.N., Huang L.T., Lau Y.T., Lin C.Y., Tain Y.L. The combined ratios of l-arginine and asymmetric and symmetric dimethylarginine as biomarkers in spontaneously hypertensive rats. Transl. Res. 2012;159:90–98. doi: 10.1016/j.trsl.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 110.Tsai C.M., Kuo H.C., Hsu C.N., Huang L.T., Tain Y.L. Metformin reduces asymmetric dimethylarginine and prevents hypertension in spontaneously hypertensive rats. Transl. Res. 2014;164:452–459. doi: 10.1016/j.trsl.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 111.Li Volti G., Salomone S., Sorrenti V., Mangiameli A., Urso V., Siarkos I., Galvano F., Salamone F. Effect of silibinin on endothelial dysfunction and ADMA levels in obese diabetic mice. Cardiovasc. Diabetol. 2011;10:62. doi: 10.1186/1475-2840-10-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Tain Y.L., Lee W.C., Hsu C.N., Lee W.C., Huang L.T., Lee C.T., Lin C.Y. Asymmetric dimethylarginine is associated with developmental programming of adult kidney disease and hypertension in offspring of streptozotocin-treated mothers. PLoS ONE. 2013;8:e55420. doi: 10.1371/journal.pone.0055420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Saigusa D., Takahashi M., Kanemitsu Y., Ishida A., Abe T., Yamakuni T., Suzuki N., Tomioka Y. Determination of Asymmetric Dimethylarginine and Symmetric Dimethylarginine in Biological Samples of Mice Using LC/MS/MS. Am. J. Anal. Chem. 2011;2:303–313. doi: 10.4236/ajac.2011.23038. [DOI] [Google Scholar]
- 114.Wang D., Gill P.S., Chabrashvili T., Onozato M.L., Raggio J., Mendonca M., Dennehy K., Li M., Modlinger P., Leiper J., et al. Isoform-specific regulation by NG,NG-dimethylarginine dimethylaminohydrolase of rat serum asymmetric dimethylarginine and vascular endothelium-derived relaxing factor/NO. Circ. Res. 2007;101:627–635. doi: 10.1161/CIRCRESAHA.107.158915. [DOI] [PubMed] [Google Scholar]
- 115.Tran C.T., Fox M.F., Vallance P., Leiper J.M. Chromosomal localization, gene structure, and expression pattern of DDAH1: Comparison with DDAH2 and implications for evolutionary origins. Genomics. 2000;68:101–105. doi: 10.1006/geno.2000.6262. [DOI] [PubMed] [Google Scholar]
- 116.Wilcken D.E., Sim A.S., Wang J., Wang X.L. Asymmetric dimethylarginine (ADMA) in vascular, renal and hepatic disease and the regulatory role of l-arginine on its metabolism. Mol. Genet. Metab. 2007;91:309–317. doi: 10.1016/j.ymgme.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 117.Tain Y.L., Hsieh C.S., Chen C.C., Sheen J.M., Lee C.T., Huang L.T. Melatonin prevents increased asymmetric dimethylarginine in young rats with bile duct ligation. J. Pineal Res. 2010;48:212–221. doi: 10.1111/j.1600-079X.2010.00745.x. [DOI] [PubMed] [Google Scholar]
- 118.Sheen J.M., Huang L.T., Hsieh C.S., Chen C.C., Wang J.Y., Tain Y.L. Bile duct ligation in developing rats: Temporal progression of liver, kidney, and brain damage. J. Pediatr. Surg. 2010;45:1650–1658. doi: 10.1016/j.jpedsurg.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 119.Cardounel A.J., Cui H., Samouilov A., Johnson W., Kearns P., Tsai A.L., Berka V., Zweier J.L. Evidence for the pathophysiological role of endogenous methylarginines in regulation of endothelial NO production and vascular function. J. Biol. Chem. 2007;282:879–887. doi: 10.1074/jbc.M603606200. [DOI] [PubMed] [Google Scholar]
- 120.Smith C.L., Anthony S., Hubank M., Leiper J.M., Vallance P. Effects of ADMA upon gene expression: An insight into the pathophysiological significance of raised plasma ADMA. PLoS Med. 2005;2:e264. doi: 10.1371/journal.pmed.0020264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zheng N., Wang K., He J., Qiu Y., Xie G., Su M., Jia W., Li H. Effects of ADMA on gene expression and metabolism in serum-starved LoVo cells. Sci. Rep. 2016;6:25892. doi: 10.1038/srep25892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Tain Y.L., Hsu C.N. Targeting on Asymmetric dimethylarginine-related nitric oxide-reactive oxygen species imbalance to reprogram the development of hypertension. Int. J. Mol. Sci. 2016;17:E2020. doi: 10.3390/ijms17122020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Schepers E., Glorieux G., Dou L., Cerini C., Gayrard N., Louvet L., Preus P., Rodriguez-Ortiz M., Argiles A., Brunet P., et al. Guanidino compounds as cause of cardiovascular damage in chronic kidney disease: An in vitro evaluation. Blood Purif. 2010;30:277–287. doi: 10.1159/000320765. [DOI] [PubMed] [Google Scholar]
- 124.Speer T., Rohrer L., Blyszczuk P., Shroff R., Kuschnerus K., Kränkel N., Kania G., Zewinger S., Akhmedov A., Shi Y., et al. Abnormal high-density lipoprotein induces endothelial dysfunction via activation of Toll-like receptor-2. Immunity. 2013;38:754–768. doi: 10.1016/j.immuni.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 125.Anderstam B., Katzarski K., Bergstrom J. Serum levels of NG, NG-dimethyl-l-arginine, a potential endogenous nitric oxide inhibitor in dialysis patients. J. Am. Soc. Nephrol. 1997;8:1437–1442. doi: 10.1681/ASN.V891437. [DOI] [PubMed] [Google Scholar]
- 126.Bełtowski J., Kedra A. Asymmetric dimethylarginine (ADMA) as a target for pharmacotherapy. Pharmacol. Rep. 2006;58:159–178. [PubMed] [Google Scholar]
- 127.Hu H., Qian K., Ho M.C., Zheng Y.G. Small molecule inhibitors of protein arginine methyltransferases. Expert Opin. Investig. Drugs. 2016;25:335–358. doi: 10.1517/13543784.2016.1144747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Rodionov R.N., Jarzebska N., Weiss N., Lentz S.R. AGXT2: A promiscuous aminotransferase. Trends Pharmacol. Sci. 2014;35:575–582. doi: 10.1016/j.tips.2014.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Jiang J.L., Li N.S., Li Y.J., Deng H.W. Probucol preserves endothelial function by reduction of the endogenous nitric oxide synthase inhibitor level. Br. J. Pharmacol. 2002;135:1175–1182. doi: 10.1038/sj.bjp.0704563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Dai Z., Zhu H.Q., Jiang D.J., Jiang J.L., Deng H.W., Li Y.J. 17β-estradiol preserves endothelial function by reduction of the endogenous nitric oxide synthase inhibitor level. Int. J. Cardiol. 2004;96:223–227. doi: 10.1016/j.ijcard.2003.07.012. [DOI] [PubMed] [Google Scholar]
- 131.Wakino S., Hayashi K., Tatematsu S., Hasegawa K., Takamatsu I., Kanda T., Homma K., Yoshioka K., Sugano N., Saruta T. Pioglitazone lowers systemic asymmetric dimethylarginine by inducing dimethylarginine dimethylaminohydrolase in rats. Hypertens. Res. 2005;28:255–262. doi: 10.1291/hypres.28.255. [DOI] [PubMed] [Google Scholar]
- 132.Hu T., Chouinard M., Cox A.L., Sipes P., Marcelo M., Ficorilli J., Li S., Gao H., Ryan T.P., Michael M.D., et al. Farnesoid X receptor agonist reduces serum asymmetric dimethylarginine levels through hepatic dimethylarginine dimethylaminohydrolase-1 gene regulation. J. Biol. Chem. 2006;281:39831–39838. doi: 10.1074/jbc.M606779200. [DOI] [PubMed] [Google Scholar]
- 133.Tan B., Jiang D.J., Huang H., Jia S.J., Jiang J.L., Hu C.P., Li Y.J. Taurine protects against low-density lipoprotein-induced endothelial dysfunction by the DDAH/ADMA pathway. Vascul. Pharmacol. 2007;46:338–345. doi: 10.1016/j.vph.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 134.Altun Z.S., Uysal S., Guner G., Yilmaz O., Posaci C. Effects of oral l-arginine supplementation on blood pressure and asymmetric dimethylarginine in stress-induced preeclamptic rats. Cell Biochem. Funct. 2008;26:648–653. doi: 10.1002/cbf.1491. [DOI] [PubMed] [Google Scholar]
- 135.Sicard P., Delemasure S., Korandji C., Segueira-Le Grand A., Lauzier B., Guilland J.C., Duvillard L., Zeller M., Cottin Y., Vergely C., et al. Anti-hypertensive effects of Rosuvastatin are associated with decreased inflammation and oxidative stress markers in hypertensive rats. Free Radic. Res. 2008;42:226–236. doi: 10.1080/10715760701885380. [DOI] [PubMed] [Google Scholar]
- 136.Onozato M.L., Tojo A., Leiper J., Fujita T., Palm F., Wilcox C.S. Expression of NG,NG-dimethylarginine dimethylaminohydrolase and protein arginine N-methyltransferase isoforms in diabetic rat kidney: Effects of angiotensin II receptor blockers. Diabetes. 2008;57:172–180. doi: 10.2337/db06-1772. [DOI] [PubMed] [Google Scholar]
- 137.Li L., Luo X.J., Liu Y.Z., Zhang Y.S., Yuan Q., Tan N., Xiang D.X., Peng J. The role of the DDAH-ADMA pathway in the protective effect of resveratrol analog BTM-0512 on gastric mucosal injury. Can. J. Physiol. Pharmacol. 2010;88:562–567. doi: 10.1139/Y10-027. [DOI] [PubMed] [Google Scholar]
- 138.Tain Y.L., Huang L.T., Lin I.C., Lau Y.T., Lin C.Y. Melatonin prevents hypertension and increased asymmetric dimethylarginine in young spontaneous hypertensive rats. J. Pineal Res. 2010;49:390–398. doi: 10.1111/j.1600-079X.2010.00806.x. [DOI] [PubMed] [Google Scholar]
- 139.Tain Y.L., Hsu C.N., Lin C.Y., Huang L.T., Lau Y.T. Aliskiren prevents hypertension and reduces asymmetric dimethylarginine in young spontaneously hypertensive rats. Eur. J. Pharmacol. 2011;670:561–565. doi: 10.1016/j.ejphar.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 140.Wang Y., Zhang M., Liu Y., Liu Y., Chen M. The effect of nebivolol on asymmetric dimethylarginine system in spontaneously hypertension rats. Vascul. Pharmacol. 2011;54:36–43. doi: 10.1016/j.vph.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 141.Pei Y., Ma P., Wang X., Zhang W., Zhang X., Zheng P., Yan L., Xu Q., Dai G. Rosuvastatin attenuates monocrotaline-induced pulmonary hypertension via regulation of Akt/eNOS signaling and asymmetric dimethylarginine metabolism. Eur. J. Pharmacol. 2011;666:165–172. doi: 10.1016/j.ejphar.2011.05.035. [DOI] [PubMed] [Google Scholar]
- 142.Balasubramaniyan V., Wright G., Sharma V., Davies N.A., Sharifi Y., Habtesion A., Mookerjee R.P., Jalan R. Ammonia reduction with ornithine phenylacetate restores brain eNOS activity via the DDAH-ADMA pathway in bile duct-ligated cirrhotic rats. Am. J. Physiol. Gastrointest. Liver Physiol. 2012;302:G145–G152. doi: 10.1152/ajpgi.00097.2011. [DOI] [PubMed] [Google Scholar]
- 143.Chen P., Xia K., Zhao Z., Deng X., Yang T. Atorvastatin modulates the DDAH1/ADMA system in high-fat diet-induced insulin-resistant rats with endothelial dysfunction. Vasc. Med. 2012;17:416–423. doi: 10.1177/1358863X12467492. [DOI] [PubMed] [Google Scholar]
- 144.Bai F., Makino T., Ono T., Mizukami H. Anti-hypertensive effects of shichimotsukokato in 5/6 nephrectomized Wistar rats mediated by the DDAH-ADMA-NO pathway. J. Nat. Med. 2012;66:583–590. doi: 10.1007/s11418-011-0625-8. [DOI] [PubMed] [Google Scholar]
- 145.Yang Y.Y., Lee T.Y., Huang Y.T., Chan C.C., Yeh Y.C., Lee F.Y., Lee S.D., Lin H.C. Asymmetric dimethylarginine (ADMA) determines the improvement of hepatic endothelial dysfunction by vitamin E in cirrhotic rats. Liver Int. 2012;32:48–57. doi: 10.1111/j.1478-3231.2011.02651.x. [DOI] [PubMed] [Google Scholar]
- 146.He H., Li X., Wang H., Zhang W., Jiang H., Wang S., Yuan L., Liu Y., Liu X. Effects of salvianolic acid A on plasma and tissue dimethylarginine levels in a rat model of myocardial infarction. J. Cardiovasc. Pharmacol. 2013;61:482–488. doi: 10.1097/FJC.0b013e3182893fd5. [DOI] [PubMed] [Google Scholar]
- 147.Ojima A., Ishibashi Y., Matsui T., Maeda S., Nishino Y., Takeuchi M., Fukami K., Yamagishi S. Glucagon-like peptide-1 receptor agonist inhibits asymmetric dimethylarginine generation in the kidney of streptozotocin-induced diabetic rats by blocking advanced glycation end product-induced protein arginine methyltranferase-1 expression. Am. J. Pathol. 2013;182:132–141. doi: 10.1016/j.ajpath.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 148.Fan N.C., Tsai C.M., Hsu C.N., Huang L.T., Tain Y.L. N-acetylcysteine prevents hypertension via regulation of the ADMA-DDAH pathway in young spontaneously hypertensive rats. Biomed. Res. Int. 2013;2013:696317. doi: 10.1155/2013/696317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tain Y.L., Sheen J.M., Chen C.C., Yu H.R., Tiao M.M., Kuo H.C., Huang L.T. Maternal citrulline supplementation prevents prenatal dexamethasone-induced programmed hypertension. Free Radic. Res. 2014;48:580–586. doi: 10.3109/10715762.2014.895341. [DOI] [PubMed] [Google Scholar]
- 150.Chien S.J., Lin K.M., Kuo H.C., Huang C.F., Lin Y.J., Huang L.T., Tain Y.L. Two different approaches to restore renal nitric oxide and prevent hypertension in young spontaneously hypertensive rats: l-citrulline and nitrate. Transl. Res. 2014;163:43–52. doi: 10.1016/j.trsl.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 151.Zhang W.L., Yan W.J., Sun B., Zou Z.P. Synergistic effects of atorvastatin and rosiglitazone on endothelium protection in rats with dyslipidemia. Lipids Health Dis. 2014;13:168. doi: 10.1186/1476-511X-13-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhang W., Zhang J., Liu Y.K., Liu J., Wang X., Xu Q., Wang Y., Xu X., Dai G. Cardioprotective effects of oxymatrine on isoproterenol-induced heart failure via regulation of DDAH/ADMA metabolism pathway in rats. Eur. J. Pharmacol. 2014;745:29–35. doi: 10.1016/j.ejphar.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 153.Sasser J.M., Cunningham M.W., Jr., Baylis C. Serelaxin reduces oxidative stress and asymmetric dimethylarginine in angiotensin II-induced hypertension. Am. J. Physiol. Renal Physiol. 2014;307:F1355–F1362. doi: 10.1152/ajprenal.00407.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Bal F., Bekpinar S., Unlucerci Y., Kusku-Kiraz Z., Önder S., Uysal M., Gurdol F. Antidiabetic drug metformin is effective on the metabolism of asymmetric dimethylarginine in experimental liver injury. Diabetes Res. Clin. Pract. 2014;106:295–302. doi: 10.1016/j.diabres.2014.08.028. [DOI] [PubMed] [Google Scholar]
- 155.Tain Y.L., Huang L.T., Hsu C.N., Lee C.T. Melatonin therapy prevents programmed hypertension and nitric oxide deficiency in offspring exposed to maternal caloric restriction. Oxid. Med. Cell Longev. 2014;2014:283180. doi: 10.1155/2014/283180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zhao D., Liu Q., Ji Y., Wang G., He X., Tian W., Xu H., Lei T., Wang Y. Effect of 18β-glycyrrhetinic acid on cerebral vasospasm caused by asymmetric dimethylarginine after experimental subarachnoid hemorrhage in rats. Neurol. Res. 2015;37:476–483. doi: 10.1179/1743132814Y.0000000462. [DOI] [PubMed] [Google Scholar]
- 157.Uysal A., Sahna E., Ozguler I.M., Burma O., Ilhan N. Effects of apocynin, an NADPH oxidase inhibitor, on levels of ADMA, MPO, iNOS and TLR4 induced by myocardial ischemia reperfusion. Perfusion. 2015;30:472–477. doi: 10.1177/0267659114559260. [DOI] [PubMed] [Google Scholar]
- 158.Hsu C.N., Lee C.T., Huang L.T., Tain Y.L. Aliskiren in early postnatal life prevents hypertension and reduces asymmetric dimethylarginine in offspring exposed to maternal caloric restriction. J. Renin Angiotensin Aldosterone Syst. 2015;16:506–513. doi: 10.1177/1470320313514123. [DOI] [PubMed] [Google Scholar]
- 159.Zheng D., Liang Q., Zeng F., Mai Z., Cai A., Qiu R., Xu R., Li D., Mai W. Atorvastatin protects endothelium by decreasing asymmetric dimethylarginine in dyslipidemia rats. Lipids Health Dis. 2015;14:41. doi: 10.1186/s12944-015-0041-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sun B., Xie Y., Jiang J., Wang Y., Xu X., Zhao C., Huang F. Pleiotropic effects of fenofibrate therapy on rats with hypertriglycemia. Lipids Health Dis. 2015;14:27. doi: 10.1186/s12944-015-0032-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hewedy W.A., Mostafa D.K. Nebivolol suppresses asymmetric dimethylarginine and attenuates cyclosporine-induced nephrotoxicity and endothelial dysfunction in rats. Pharmacol. Rep. 2016;68:1319–1325. doi: 10.1016/j.pharep.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 162.Mutlu E., İlhan S., Onat E., Kara M., Şahna E. The effects of novokinin, an AT2 agonist, on blood pressure, vascular responses, and levels of ADMA, NADPH oxidase, and Rho kinase in hypertension induced by NOS inhibition and salt. Turk. J. Med. Sci. 2016;46:1249–1257. doi: 10.3906/sag-1502-18. [DOI] [PubMed] [Google Scholar]
- 163.Sheen J.M., Chen Y.C., Hsu M.H., Tain Y.L., Yu H.R., Huang L.T. Combined intraperitoneal and intrathecal etanercept reduce increased brain tumor necrosis factor-alpha and asymmetric dimethylarginine levels and rescues spatial deficits in young rats after bile duct ligation. Front. Cell Neurosci. 2016;10:167. doi: 10.3389/fncel.2016.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Quintana-Villamandos B., Arnalich-Montiel A., Arribas S., Lüneburg N., Böger R.H., Delgado-Martos M.J., Fernández-Criado C., Delgado-Baeza E., González M.C. Early regression of coronary artery remodeling with esmolol and DDAH/ADMA pathway in hypertensive rats. Hypertens. Res. 2016;39:692–700. doi: 10.1038/hr.2016.57. [DOI] [PubMed] [Google Scholar]
- 165.Mostafa D.K., El Azhary N.M., Nasra R.A. The hydrogen sulfide releasing compounds ATB-346 and diallyl trisulfide attenuate streptozotocin-induced cognitive impairment, neuroinflammation, and oxidative stress in rats: Involvement of asymmetric dimethylarginine. Can. J. Physiol. Pharmacol. 2016;94:699–708. doi: 10.1139/cjpp-2015-0316. [DOI] [PubMed] [Google Scholar]
- 166.Chen D., Zhang K.Q., Li B., Sun D.Q., Zhang H., Fu Q. Epigallocatechin-3-gallate ameliorates erectile function in aged rats via regulation of PRMT1/DDAH/ADMA/NOS metabolism pathway. Asian J. Androl. 2016 doi: 10.4103/1008-682X.178486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Tai I.H., Sheen J.M., Lin Y.J., Yu H.R., Tiao M.M., Chen C.C., Huang L.T., Tain Y.L. Maternal N-acetylcysteine therapy regulates hydrogen sulfide-generating pathway and prevents programmed hypertension in male offspring exposed to prenatal dexamethasone and postnatal high-fat diet. Nitric Oxide. 2016;53:6–12. doi: 10.1016/j.niox.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 168.Zhou R., Ma P., Xiong A., Xu Y., Wang Y., Xu Q. Protective effects of low dose rosuvastatin on isoproterenol-induced chronic heart failure in rats by regulation of DDAH-ADMA-NO pathway. Cardiovasc. Ther. 2016 doi: 10.1111/1755-5922.12241. [DOI] [PubMed] [Google Scholar]