Abstract
Objective
Evaluate if and how neuropsychiatric symptoms of dementia (NPS) influence the management and disposition of older adults who present to emergency care settings.
Methods
This is a retrospective cohort study that involved the medical and psychiatric emergency departments of a tertiary academic medical center. Participants included patients ≥ 65 years of age with dementia who presented between February 1, 2012 and July 16, 2014 (n=347). Subjects with documented NPS (n=78) were compared with a group of subjects without documented NPS (n=78) randomly selected from the overall group with dementia. The groups with and without NPS were compared on demographic, clinical, management, and disposition characteristics.
Results
Patients with NPS were more likely to have additional diagnostic testing performed and receive psychotropic medications including benzodiazepines and antipsychotics. Significantly fewer patients with NPS (59.0%) returned to their original setting from the emergency department than patients without NPS (76.9%). Among patients with NPS, those who had a motor disturbance were more likely to receive psychotropic medications than patients who did not have a motor disturbance. Depression/dysphoria, anxiety, disinhibition, irritability/lability, and motor disturbance were all associated with transfer from medical to psychiatric ED. Patients with depression/dysphoria or anxiety were more likely to be psychiatrically hospitalized.
Conclusions
There are significant differences in the management of dementia with and without NPS in the emergency room setting. Developing and implementing successful methods to manage NPS in the emergency department and outpatient setting could potentially lead to less emergent psychotropic administration and reduce hospitalizations.
Keywords: Dementia, Neuropsychiatric Symptoms, Emergency Department
Introduction
While dementia is a disorder characterized by significant cognitive decline, the associated neuropsychiatric symptoms (NPS) often dominate the clinical presentation (Kales et al., 2015). NPS occur in all types of dementia and include agitation, psychosis, disinhibition, aggression, depression, anxiety, apathy, sleep disturbances, and motor disturbances (Lyketsos et al., 2000, Lyketsos et al., 2011). They are exceptionally common and one or more symptoms will develop in almost all patients with dementia at some point during the disease course. Dementia is also a costly condition relative to other chronic conditions in late life (Kelley et al., 2015), and approximately 1/3 of these costs can be attributed to NPS management (Murman et al., 2002). NPS are a devastating aspect of dementia associated with increased rates of nursing home placement, morbidity, mortality for the patient, along with caregiver stress and depression, reduced caregiver employment income, and additional hours of caregiver support and supervision (Wancata et al., 2003, Van Den Wijngaart et al., 2007, Yaffe et al., 2002, Okura and Langa, 2011, Kales et al., 2005).
The emergency department (ED) is an important site of care for older adults, who have one of the highest visit rates (Gruneir et al., 2010). It often serves as a point-of-entry into the hospital system and provides after-hour care to those unable to access their usual provider (Wofford et al., 1993, Lowthian et al., 2013). However, there are numerous issues facing older adults who present to the ED. As a whole, compared to younger persons, older adults have more urgent emergency visits, longer emergency visits, higher rates of diagnostic test use, higher rates of repeat visits, and higher rates of adverse events following discharge (Samaras et al., 2010, Aminzadeh and Dalziel, 2002). Little is known about how NPS influence presentation to and disposition from emergency medical or psychiatric settings. Caregivers overwhelmed by NPS may take patients to the ED, which may partially account for the increased risk of medical hospitalization among patients with dementia (Bynum et al., 2004, Phelan et al., 2012, Feng et al., 2014).
Once there, management of patients with NPS in the ED may be challenging, as the noisy, chaotic environment may be overwhelming for patients and caregivers. In place of behavioral interventions, patients may receive antipsychotics—with modest efficacy and significantly increased risks for this patient population (Kales et al., 2007, Maust et al., 2015, Gerhard et al., 2013). Benzodiazepines are another alternative used for NPS (Maust et al., 2016), though there are no placebo-controlled trials demonstrating benefit, while there is extensive evidence of harms in older adults (Kales et al., 2015, Tannenbaum et al., 2012, Chang et al., 2008, Berry et al., 2016). Appropriate disposition may also be challenging, as some caregivers may have brought a patient to the ED because they felt they could no longer manage that patient at home. The ED physician may not believe a patient needs to be admitted for medical reasons, yet still recommend admission in the face of an overwhelmed caregiver. Hospitalization, however, has a variety of negative consequences for both patients with dementia and their caregivers, including further cognitive and functional decline and increased distress and healthcare costs (Toot et al., 2013, Krumholz, 2013, Fick et al., 2013, Gillick et al., 1982).
While work has focused on recognition of cognitive impairment in the ED (Wilber et al., 2005, Salen et al., 2009), less has specifically examined the care of patients with dementia in the ED (Parke et al., 2013), and still less is known about how NPS may influence the management of these patients in the emergency setting. The goal of this study was to evaluate the potential role of NPS in the management and disposition of older adults with dementia who presented to the medical emergency department (MED) and psychiatric emergency department (PED) of a large tertiary academic medical center.
Methods
This retrospective cohort study was approved by the University of Michigan Institutional Review Board. Informed consent was waived as there was minimal risk to patients and it was determined that the research could not be practically performed without a waiver.
Study Population
Patients were included in the study if they were ≥ 65 years old, had a diagnosis of dementia present in the health system clinical data warehouse, and had presented to either the medical center’s MED or PED between February 1, 2012 and July 16, 2014. A total of 1,466 patients with dementia were identified in the health system during the study interval; of these, 347 patients had a MED or PED visit. There were no exclusion criteria.
Medical Record Search
The records of these 347 patients were screened using EMERSE (Electronic Medical Record Search Engine) to identify those patients who possibly had NPS. EMERSE is a Google-like search engine that allows rapid screening of charts for review, saving significant time while preserving clinical accuracy and privacy (Seyfried et al., 2009, Hanauer et al., 2015). Records were screened using search bundles that consisted of key search terms corresponding to each domain on the Neuropsychiatric Inventory, brief questionnaire form (NPI-Q) (Kaufer et al., 2000), and included the entire physician note. Medical records flagged by EMERSE as having a term corresponding to at least one NPI-Q domain were included for further review (n=78 [22.4%]). The applicable PED or MED encounter for each patient was then reviewed in detail by a psychiatrist (RMS) to verify the presence of NPS based on the ED clinician documentation. For comparison, an equivalent number of charts (n=78) were randomly selected from the remaining pool of patients whose records did not include at least one NPS (n=269).
Data collected from the corresponding patient encounter included the following: demographic information, county of current residence, insurance information, visit location (MED or PED), referral source, current living situation, presence of family during visit, prior hospitalization(s), presence of mental health provider during visit, prior use (and types) of psychiatric medications, diagnoses (as recorded in the assessment and plan portion of the physician note), labs and tests ordered (urinalysis, urine drug screen, chest x-ray, CT head or MR brain, or blood alcohol level), NPS present (as categorized by the NPI-Q domains), use of medications, restraint and/or seclusion use, transfer between visit locations, and final disposition. For patients that were transferred between ED settings, we captured data from the PED visit, which we anticipated would have the most accurate documentation of NPS.
Data Analysis
The patients with documented NPS (n=78) and the randomly selected non-NPS patient comparison group (n=78) were included in further analysis. All analyses were performed using t-test for continuous variables and chi-square test for categorical variables. First, within the group with documented NPS, the specific NPS domains present as well as the overall number of domains was calculated for each patient. Then, the groups with and without documented NPS were compared in the following areas: baseline patient characteristics (e.g., demographics, living situation, psychotropic medication use), ED encounter characteristics (e.g., laboratory testing, restraint use), ED clinician diagnosis, and disposition from the ED. Finally, we used unadjusted logistic regression to determine whether specific NPS were associated with the following outcomes: psychotropic administration, transfer from the medical to psychiatric ED, or psychiatric hospitalization. A p-value of < 0.05 was used as the level of statistical significance.
Results
Baseline patient characteristics
Baseline patient characteristics are presented in Table 1. Among patients with any documented NPS, the most common symptom categories present were agitation/aggression (67.9%), motor disturbance (37.2%), and depression/dysphoria (32.1%) (Figure 1). Among patients with dementia who presented to the ED, the groups with and without documented NPS did not significantly differ by: age, sex, race, marital status, county of residence, presence of medical insurance between the two groups, or type of current living situation with most patients residing at home. Overall, 57.5% of patients were taking a psychotropic medication; including including acetylcholinesterase inhibitors and/or memantine, this rose to 72.4%. Antidepressants were the most common (50.0%) followed by acetylcholinesterase inhibitors (37.2%), antipsychotics (24.4%), memantine (21.8%), benzodiazepines (12.2%), mood stabilizers (7.7%), other anxiolytics (1.9%), and hypnotics (1.3%). Patients with documented NPS were more likely to be taking any psychotropic medication than patients without documented NPS (84.6% vs. 60.3%, p=0.003). This difference was driven by higher use of antidepressants (61.5% vs. 38.5%, p=0.004) and antipsychotics (37.2% vs. 11.5%, p<0.001); the groups did not differ otherwise on psychotropic medications upon presentation.
Table 1.
Baseline Patient Characteristics
| Total (N=156) | NPS (N=78) | No NPS (N=78) | Chi-square/t-value | |
|---|---|---|---|---|
|
| ||||
| Characteristic | N (%) | N (%) | N (%) | |
| Age (years; mean (SD)) | 80 (9.2) | 79.1 (9.4) | 80.9 (9.0) | −1.2500 |
| Sex | ||||
| Female | 93 (59.6) | 49 (62.8) | 44 (56.4) | 0.6656 |
| Race | ||||
| White | 135 (86.5) | 68 (87.2) | 67 (85.9) | 0.0550 |
| Current Living Situation | ||||
| Alzheimer’s care | 5 (3.2) | 3 (3.8) | 2 (2.6) | 10.3546 |
| Assisted living community | 15 (9.6) | 9 (11.5) | 6 (7.7) | |
| Home, alone | 8 (5.1) | 7 (9.0) | 1 (1.3) | |
| Home, with other | 74 (47.4) | 35 (44.9) | 39 (50) | |
| Independent living community | 3 (1.9) | 2 (2.6) | 1 (1.3) | |
| Nursing home | 23 (14.7) | 11 (14.1) | 12 (15.4) | |
| Residential care homes | 2 (1.3) | 2 (2.6) | 0 (0) | |
| Not mentioned/Other | 23 (16.7) | 9 (11.5) | 17 (21.8) | |
| Prior psychiatric hospitalization | ||||
| No | 21 (13.5) | 21 (26.9) | 0 (0) | 37.1429** |
| Yes | 9 (5.8) | 9 (11.5) | 0 (0) | |
| Not mentioned/Unclear | 126 (80.8) | 48 (61.5) | 78 (100) | |
| Use of psychotropics on presentation | ||||
| No | 15 (9.6) | 5 (6.4) | 10 (12.8) | 11.8614** |
| Yes | 113 (72.4) | 66 (84.6) | 47 (60.3) | |
| Not mentioned/Unclear | 28 (17.9) | 7 (9.0) | 21 (26.9) | |
p<0.05
p<0.01
NPS = Neuropsychiatric symptoms
Figure 1.
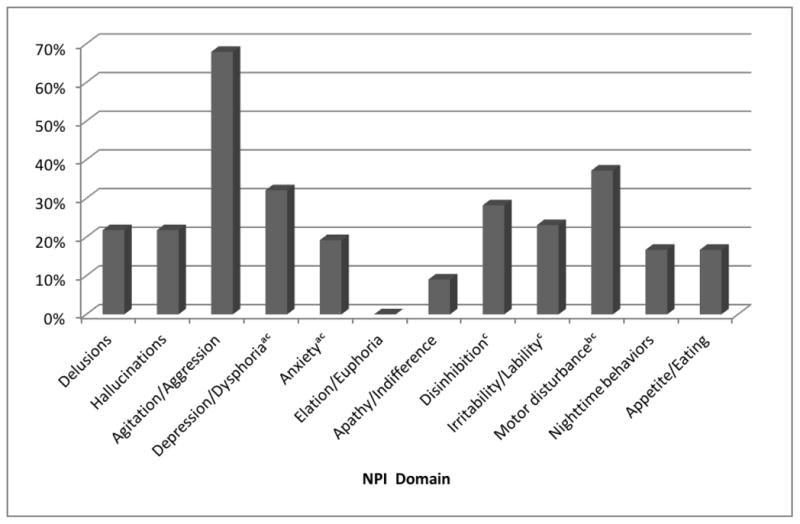
Neuropsychiatric Inventory Categories Present in Patients with Documented Neuropsychiatric Symptoms of Dementia in the Medical Emergency Department (MED) or Psychiatric Emergency Department (PED)
a. Significantly related to psychiatric hospitalization
b. Significantly linked to receiving medications in the medical ED or PED
c. Significantly associated with transfer to PED from the medical ED
Emergency Encounter Characteristics
42.3% of patients with documented NPS presented to the PED, while patients without documented NPS were exclusively seen in the MED (Table 2). A family member was more likely to accompany patients with NPS than those who did not have NPS. In addition, family members accounted for a larger proportion of referrals among those with documented NPS. Patients with documented NPS were also more likely to be seen by a mental health provider in the ED (46.2% vs. 0.0%, p<0.001) and to have a prior psychiatric hospitalization, although any documentation of prior psychiatric hospitalization was rare. Patients with documented NPS were more likely to be administered psychotropic medications while in the emergency setting (19.2% vs. 0.0%, p<0.001) with antipsychotics and benzodiazepines being the most frequently administered medications. Patients who had a motor disturbance were more likely to receive psychotropic medications than patients who did not have a motor disturbance (OR= 4.6, 95% CI: 1.4–15.4, p=0.01).
Table 2.
Emergency Encounter Characteristics
| Total (N=156) | NPS (N=78) | No NPS (N=78) | Chi-square | |
|---|---|---|---|---|
|
| ||||
| Characteristic | N (%) | N (%) | N (%) | |
| Referral Source | ||||
| Family member | 67 (42.9) | 39 (50.0) | 28 (35.9) | 11.3828** |
| Medical provider | 49 (31.4) | 28 (35.9) | 21 (26.9) | |
| Self | 29 (18.6) | 7 (9.0) | 22 (28.2) | |
| Unclear/Other | 11 (7.1) | 4 (5.1) | 7 (9.0) | |
| Family member present | ||||
| No | 20 (12.8) | 11 (14.1) | 9 (11.5) | 15.3803** |
| Yes | 122 (78.2) | 67 (85.9) | 55 (70.5) | |
| Not mentioned/Unclear | 14 (9.0) | 0 (0) | 14 (17.9) | |
| Location | ||||
| MED | 123 (78.8) | 45 (57.7) | 78 (100.0) | 41.8537** |
| PED | 33 (21.2) | 33 (42.3) | 0 (0) | |
| Test/Lab performed | ||||
| Urinalyisis | 82 (52.6) | 49 (62.8) | 33 (42.3) | 6.5814* |
| Urine drug screen | 14 (9.0) | 13 (16.7) | 1 (1.3) | 11.2998** |
| Chest X-ray | 57 (36.5) | 31 (39.7) | 26 (33.3) | 0.6911 |
| CT head or MR brain | 50 (32.1) | 30 (38.5) | 20 (25.6) | 2.9434 |
| Blood alcohol level | 3 (1.9) | 3 (3.8) | 0 (0) | 3.0588 |
| Diagnosis of delirium | ||||
| Yes | 7 (4.5) | 7 (9.0) | 0 (0) | 7.3289** |
| Restraint or seclusion in MED/PED | ||||
| None | 153 (98.1) | 75 (96.2) | 78 (100) | 3.0588 |
| Transfer to other location (MED or PED) | ||||
| Transfer to other location | 11 (7.5) | 11(14.1) | 0 (0) | 11.8345** |
p<0.05
p<0.01
NPS = Neuropsychiatric symptoms
MED = Medical emergency department
PED = Psychiatric emergency department
Patients who had documented NPS were more likely to have a urine drug screen and urinalysis performed than patients without documented NPS. There was no significant difference in the frequency of other included diagnostic tests between the two groups. Use of restraints or seclusion was uncommon (n=3, 1.9%) and there was no difference in their use between the two groups. Transfer between the MED and the PED was relatively uncommon, but more likely to occur in patients who had NPS. Depression/dysphoria (OR= 6.5, 95% CI: 1.5–27.3, p=.01), anxiety (OR= 9.8, 95% CI: 2.3–41.8, p=0.002), disinhibition (OR= 4.9, 95% CI: 1.2–19.5, p=0.03), irritability/lability (OR=7.0, 95% CI: 1.7– 28.7, p=0.007), and motor disturbance (OR=4.9, 95% CI: 1.2–20.7, p=0.03) were all associated with transfer from medical to psychiatric ED.
ED clinician diagnosis
Diagnostic data were comprised of the listed diagnoses from the physician’s assessment. The most common encounter diagnoses listed were dementia (32.7%), fall/injury (23.1%), infection (11.5%), altered mental status (10.3%), mood disorder (8.3%), delirium (4.5%), psychosis (3.2%), anxiety disorder (2.6%), agitation (2.6%), and substance use disorders (1.3%). The diagnosis of delirium was more common in patients with documented NPS as well as agitation, psychosis, mood disorders, and anxiety disorders. There was no significant difference between the two groups in the diagnosis of altered mental status.
Encounter disposition
The discharge locations of patients with and without documented NPS are presented in Figure 2. Overall, most patients were discharged to their pre-ED setting; however, a substantial amount were hospitalized either medically (16.7%) or psychiatrically (5.2%). Patients with documented NPS seen in the PED were more likely to be psychiatrically hospitalized than patients with documented NPS seen in the MED (24.2% vs 0.0%, p=0.001). Patients with depression/dysphoria (OR= 20.2, 95% CI: 2.3–175.8, p=0.006) or anxiety (OR= 10.0, 95% CI: 2.1–48.5, p=0.004 were more likely to be psychiatrically hospitalized. The presence of agitation/aggression alone was not significantly related to hospitalization, medication administration, or transfer. Patients with documented NPS were significantly less likely to be discharged to their original setting compared to those without documented NPS (OR= 0.4, 95% CI: 0.2–0.9, p=0.02). Neither restraint/seclusion use, prior psychiatric hospitalization, nor living situation was associated with hospitalization. Amongst patients without documented NPS, a diagnosis of altered mental status was significantly associated with an increased likelihood of medical hospitalization (OR= 14.0, 95% CI: 2.2–87.7, p=0.005).
Figure 2.
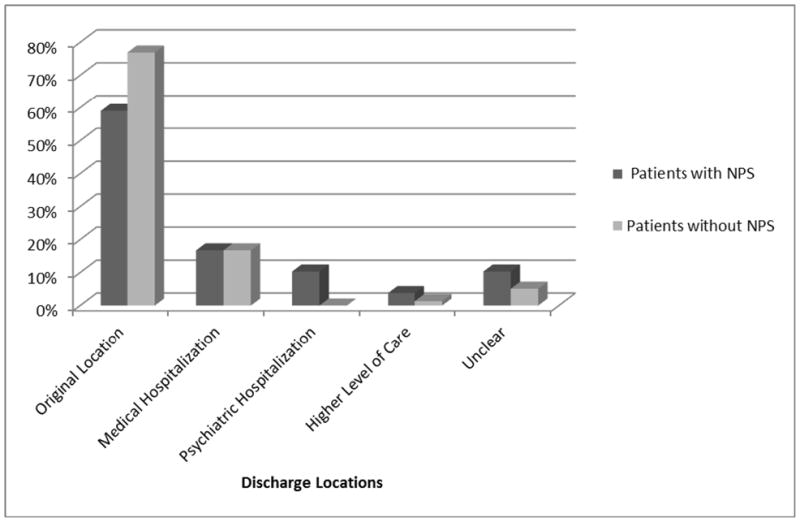
Disposition of Patients with and without Documented Neuropsychiatric Symptoms of Dementia from the Emergency Setting
Discussion
The presentation of patients with dementia to emergency services was a fairly common occurrence, as 24% of patients seen in the health system with a dementia diagnosis recorded had at least one ED visit during the two-year study period. To our knowledge, these are the first analyses exploring NPS among patients with dementia who present to emergency medical or psychiatric services. Of the patients with dementia that presented to the ED, nearly one quarter had at least one NPS present. This prevalence is lower than research-based estimates in community settings (Lyketsos et al., 2002, Okura et al., 2010), which is unsurprising as ED clinicians are not trained to assess NPS and, at an ED visit, there may be more pressing medical issues that require attention. A large retrospective cross-sectional study on older adults in the ED found a much lower prevalence of mental and behavioral symptoms (2.0%), though the authors were not specifically evaluating patients with dementia and this finding was based on diagnosis codes rather than chart review (Latham and Ackroyd-Stolarz, 2014).
About half of patients with dementia presenting to emergency services were living at home. Although there were no differences in the current living situation between patients with and without documented NPS, patients with documented NPS were more likely to be referred to emergency services by a family member. This might be because patients with documented NPS had more severe dementia, and therefore receiving ED care was through the action of a family member, though we were unable to measure this with the data we had. Alternatively, referral to emergency services by a family member might also suggest an overwhelmed caregiver, which is a known risk factor for hospitalization (Balardy et al., 2004). Our finding that patients with documented NPS were less likely to be discharged to their original setting also suggests this later interpretation, as an ED clinician may be uncomfortable discharging a patient home to an overwhelmed caregiver. The ED setting may be a step in the pathway to institutionalization and, therefore, a point of potential intervention.
We found significant differences in the evaluation and management of patients with and without documented NPS. Patients with documented NPS required greater resource utilization: they were more likely to have diagnostic testing performed, receive psychotropic medications, and be transferred from the medical to the psychiatric emergency department for additional evaluation and management. The reasons for more comprehensive evaluation may be multiple. First, differentiation of NPS from delirium in an emergent setting may be difficult, which might also explain the need for further evaluation. Given that NPS occur in increased frequency and severity in the setting of an underlying medical precipitant (Kales et al., 2015, Hodgson et al., 2011), they may function to providers as a non-specific sign of underlying medical problems. The increased use of psychotropic medications among patients with documented NPS is a cause for concern, given the mixed evidence-base for their efficacy and the risks associated with their use, including increased mortality (Kales et al., 2015). While use of antipsychotics may be appropriate in emergency settings for psychosis, agitation, and aggression that are potentially dangerous, use of other psychotropic medications (e,g., benzodiazepines) with even less evidence for benefit is concerning. To our surprise, however, the only NPS specifically associated with medication administration was motor disturbance, which may suggest that type of NPS that is most disruptive in the ED physical setting. Finally, it may be possible that the differences we found were a function of where the patients were seen—in the medical versus the psychiatric ED—rather than because of NPS.
The primary limitation of this study is its retrospective design, with dementia case identification based on clinician identification and documentation of the symptoms of interest. Certain symptoms may be more readily detected and more likely to be documented by a clinician, especially in an emergency setting. As such, relatively mild dementia or other subtle NPS may be missing from the sample, reflected by the relatively low documented prevalence. This may also help explain why the pool of patients was dementia was smaller than expected, reflecting clinician under-recognition. Another limitation was the inability to determine whether NPS determined by chart review was actually delirium. Patients with a diagnosis of “altered mental status” may have had delirium, dementia, or both, but there was no reliable method to exclude these patients from our investigation. Another limitation is the relatively small sample size drawn from a single medical center, which limits the power of our findings as well as the generalizability. Finally, because of the number of comparisons performed, some statistically significant results would be expected from chance alone. However, given the dearth of information in this area, we think our findings are informative and can inform future avenues of research.
Given the outsize role of NPS in caregiver burden and the potentially difficult nature of some of the symptoms, it is almost impossible that NPS would not influence care in the clinical setting. These preliminary findings suggest several future avenues of work. First, the findings that patients with documented NPS were both more likely to be brought to ED attention by family members and less likely to return to their original setting suggest that the impact of NPS may be through caregiver distress. Prior work has demonstrated that the risk of ED visits and hospitalization for potentially preventable reasons is higher among patients with dementia than other older adults (Phelan et al., 2012, Bynum et al., 2004, Feng et al., 2014) though thus far interventions to reduce hospitalization among patients with dementia have had minimal impact (Phelan et al., 2015). Along with the recent publication of Russ et al. (Russ et al., 2015), our analysis is among the few to consider the potential influence of caregivers on medical utilization among patients with dementia, which has not been addressed in prior work addressing direct medical care among this population (Murman et al., 2002, Herrmann et al., 2006). In addition, it will be important to explore differences in the management of patients with dementia in the medical versus psychiatric ED. The care patients with dementia receive, with or without NPS, should be determined by their history and symptoms rather than by which ED door they walk through.
Ideally, caregivers and their outpatient providers would have the tools to manage NPS such that their presence alone would not increase the risk of an ED visit. If the behavior has been so severe as to trigger an ED visit, it is unlikely that this caregiver would be comfortable taking the patient home. And even with the best-equipped caregiver, however, patients with dementia will require emergency medical care. Ideally, ED providers would be prepared to recognize and evaluate NPS as any other symptom as part of an evaluation to rule out underlying medical problems. In addition, given the aging of the ED population and limited medication options to deal with challenging behavior, it may be helpful if part of the ED clinical or social work staff were trained in a method such as the DICE approach to help address behaviors in the ED setting (Kales et al., 2014).
Conclusion
Patients with dementia who presented to emergency services with NPS were more likely to receive additional consultation, diagnostic testing, and psychotropic medications and were less likely to return to their original living situation on discharge than those without NPS. Specific NPS domains were associated with medication administration in the emergency department, interdepartmental transfer, and hospitalization. Developing and implementing successful methods to manage NPS in outpatient settings would potentially lead to less presentation to the emergency department, as well as less use of emergent psychotropic administration once patients are there. Given hospitalization-associated cognitive and functional decline for patients and the associated caregiver distress and economic burden, further examination of the interplay of NPS and emergency care is critical.
Acknowledgments
Support: University of Michigan Program for Positive Aging. DTM is supported by the Beeson Career Development Award Program (NIA K08AG048321, the American Federation for Aging Research, The John A. Hartford Foundation, and The Atlantic Philanthropies).
Footnotes
Previous Presentation: “Outcomes for older adults with dementia who present to emergency services with neuropsychiatric symptoms.” Poster presented at: American Association for Geriatric Psychiatry Annual Meeting, New Orleans LA, March 2015.
Conflicts of Interest and Source of Funding: None declared
References
- AMINZADEH F, DALZIEL WB. Older adults in the emergency department: A systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Annals of emergency medicine. 2002;39:238–247. doi: 10.1067/mem.2002.121523. [DOI] [PubMed] [Google Scholar]
- BALARDY L, VOISIN T, CANTET C, VELLAS B. Predictive factors of emergency hospitalisation in Alzheimer’s patients: results of one-year follow-up in the REAL. FR Cohort. The journal of nutrition, health & aging. 2004;9:112–116. [PubMed] [Google Scholar]
- BERRY SD, PLACIDE SG, MOSTOFSKY E, ZHANG Y, LIPSITZ LA, MITTLEMAN MA, KIEL DP. Antipsychotic and Benzodiazepine Drug Changes Affect Acute Falls Risk Differently in the Nursing Home. The journals of gerontology. Series A, Biological sciences and medical sciences. 2016 doi: 10.1093/gerona/glv091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BYNUM JP, RABINS PV, WELLER W, NIEFELD M, ANDERSON GF, WU AW. The relationship between a dementia diagnosis, chronic illness, medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52:187–194. doi: 10.1111/j.1532-5415.2004.52054.x. [DOI] [PubMed] [Google Scholar]
- CHANG CM, WU EC, CHANG IS, LIN KM. Benzodiazepine and risk of hip fractures in older people: a nested case-control study in Taiwan. Am J Geriatr Psychiatry. 2008 doi: 10.1097/JGP.0b013e31817c6a99. [DOI] [PubMed] [Google Scholar]
- FENG Z, COOTS LA, KAGANOVA Y, WIENER JM. Hospital And ED Use Among Medicare Beneficiaries With Dementia Varies By Setting And Proximity To Death. Health affairs. 2014;33:683–690. doi: 10.1377/hlthaff.2013.1179. [DOI] [PubMed] [Google Scholar]
- FICK DM, STEIS MR, WALLER JL, INOUYE SK. Delirium superimposed on dementia is associated with prolonged length of stay and poor outcomes in hospitalized older adults. Journal of hospital medicine: an official publication of the Society of Hospital Medicine. 2013 doi: 10.1002/jhm.2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GERHARD T, HUYBRECHTS K, OLFSON M, SCHNEEWEISS S, BOBO WV, DORAISWAMY PM, DEVANAND DP, LUCAS JA, HUANG C, MALKA ES, LEVIN R, CRYSTAL S. Comparative mortality risks of antipsychotic medications in community-dwelling older adults. The British journal of psychiatry: the journal of mental science. 2013 doi: 10.1192/bjp.bp.112.122499. [DOI] [PubMed] [Google Scholar]
- GILLICK MR, SERRELL NA, GILLICK LS. Adverse consequences of hospitalization in the elderly. Social Science & Medicine. 1982 doi: 10.1016/0277-9536(82)90175-7. [DOI] [PubMed] [Google Scholar]
- GRUNEIR A, SILVER MJ, ROCHON PA. Emergency Department Use by Older Adults: A Literature Review on Trends, Appropriateness, and Consequences of Unmet Health Care Needs. Medical Care Research and Review. 2010;68:131–155. doi: 10.1177/1077558710379422. [DOI] [PubMed] [Google Scholar]
- HANAUER DA, MEI Q, LAW J, KHANNA R, ZHENG K. Supporting information retrieval from electronic health records: A report of University of Michigan's nine-year experience in developing and using the Electronic Medical Record Search Engine (EMERSE) J Biomed Inform. 2015 doi: 10.1016/j.jbi.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HERRMANN N, LANCTOT KL, SAMBROOK R, LESNIKOVA N, HEBERT R, MCCRACKEN P, ROBILLARD A, NGUYEN E. The contribution of neuropsychiatric symptoms to the cost of dementia care. Int J Geriatr Psychiatry. 2006;21:972–6. doi: 10.1002/gps.1594. [DOI] [PubMed] [Google Scholar]
- HODGSON NA, GITLIN LN, WINTER L, CZEKANSKI K. Undiagnosed illness and neuropsychiatric behaviors in community residing older adults with dementia. Alzheimer disease and associated disorders. 2011 doi: 10.1097/WAD.0b013e3181f8520a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KALES HC, CHEN P, BLOW FC, WELSH DE, MELLOW AM. Rates of clinical depression diagnosis, functional impairment, and nursing home placement in coexisting dementia and depression. Am J Geriatr Psychiatry. 2005;13:441–9. doi: 10.1176/appi.ajgp.13.6.441. [DOI] [PubMed] [Google Scholar]
- KALES HC, GITLIN LN, LYKETSOS CG. Assessment and management of behavioral and psychological symptoms of dementia. Bmj. 2015;350:h369–h369. doi: 10.1136/bmj.h369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KALES HC, GITLIN LN, LYKETSOS CG DETROIT EXPERT PANEL ON A, MANAGEMENT OF NEUROPSYCHIATRIC SYMPTOMS OF D. Management of neuropsychiatric symptoms of dementia in clinical settings: recommendations from a multidisciplinary expert panel. J Am Geriatr Soc. 2014;62:762–9. doi: 10.1111/jgs.12730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KALES HC, VALENSTEIN M, KIM HM, MCCARTHY JF, GANOCZY D, CUNNINGHAM F, BLOW FC. The American journal of psychiatry. 2007. Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. 2007/09/28 ed. [DOI] [PubMed] [Google Scholar]
- KAUFER DI, CUMMINGS JL, KETCHEL P, SMITH V, MACMILLAN A, SHELLEY T, LOPEZ OL, DEKOSKY ST. Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory. J Neuropsychiatry Clin Neurosci. 2000;12:233–9. doi: 10.1176/jnp.12.2.233. [DOI] [PubMed] [Google Scholar]
- KELLEY AS, MCGARRY K, GORGES R, SKINNER JS. The Burden of Health Care Costs for Patients With Dementia in the Last 5 Years of Life. Annals of internal medicine. 2015;163:729–736. doi: 10.7326/M15-0381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KRUMHOLZ HM. Post-hospital syndrome—an acquired, transient condition of generalized risk. The New England journal of medicine. 2013 doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LATHAM LP, ACKROYD-STOLARZ S. Emergency department utilization by older adults: a descriptive study. Can Geriatr J. 2014;17:118–25. doi: 10.5770/cgj.17.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LOWTHIAN JA, SMITH C, STOELWINDER JU, SMIT DV, MCNEIL JJ, CAMERON PA. Why older patients of lower clinical urgency choose to attend the emergency department. Intern Med J. 2013;43:59–65. doi: 10.1111/j.1445-5994.2012.02842.x. [DOI] [PubMed] [Google Scholar]
- LYKETSOS CG, CARRILLO MC, RYAN JM, KHACHATURIAN AS, TRZEPACZ P, AMATNIEK J, CEDARBAUM J, BRASHEAR R, MILLER DS. Neuropsychiatric symptoms in Alzheimer’s disease. Alzheimers Dement. 2011;7:532–9. doi: 10.1016/j.jalz.2011.05.2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LYKETSOS CG, LOPEZ O, JONES B, FITZPATRICK AL, BREITNER J, DEKOSKY S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA. 2002;288:1475–83. doi: 10.1001/jama.288.12.1475. [DOI] [PubMed] [Google Scholar]
- LYKETSOS CG, STEINBERG M, TSCHANZ JT, NORTON MC, STEFFENS DC, BREITNER JC. Mental and behavioral disturbances in dementia: findings from the Cache County Study on Memory in Aging. Am J Psychiatry. 2000;157:708–14. doi: 10.1176/appi.ajp.157.5.708. [DOI] [PubMed] [Google Scholar]
- MAUST DT, KIM HM, SEYFRIED LS, CHIANG C, KAVANAGH J, SCHNEIDER LS, KALES HC. Antipsychotics, other psychotropics, and the risk of death in patients with dementia: number needed to harm. JAMA Psychiatry. 2015;72:438–45. doi: 10.1001/jamapsychiatry.2014.3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAUST DT, LANGA KM, BLOW FC, KALES HC. Psychotropic use and associated neuropsychiatric symptoms among patients with dementia in the USA. Int J Geriatr Psychiatry. 2016 doi: 10.1002/gps.4452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MURMAN DL, CHEN Q, POWELL MC, KUO SB, BRADLEY CJ, COLENDA CC. The incremental direct costs associated with behavioral symptoms in AD. Neurology. 2002;59:1721–9. doi: 10.1212/01.wnl.0000036904.73393.e4. [DOI] [PubMed] [Google Scholar]
- OKURA T, LANGA KM. Caregiver burden and neuropsychiatric symptoms in older adults with cognitive impairment: the Aging, Demographics, and Memory Study (ADAMS) Alzheimer Dis Assoc Disord. 2011;25:116–21. doi: 10.1097/WAD.0b013e318203f208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OKURA T, PLASSMAN BL, STEFFENS DC, LLEWELLYN DJ, POTTER GG, LANGA KM. Prevalence of Neuropsychiatric Symptoms and Their Association with Functional Limitations in Older Adults in the United States: The Aging, Demographics, and Memory Study. J Am Geriatr Soc. 2010;58:330–337. doi: 10.1111/j.1532-5415.2009.02680.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PARKE B, HUNTER KF, STRAIN LA, MARCK PB, WAUGH EH, MCCLELLAND AJ. Facilitators and barriers to safe emergency department transitions for community dwelling older people with dementia and their caregivers: a social ecological study. International journal of nursing studies. 2013;50:1206–1218. doi: 10.1016/j.ijnurstu.2012.11.005. [DOI] [PubMed] [Google Scholar]
- PHELAN EA, BORSON S, GROTHAUS L, BALCH S, LARSON EB. Association of incident dementia with hospitalizations. JAMA. 2012;307:165–72. doi: 10.1001/jama.2011.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PHELAN EA, DEBNAM KJ, ANDERSON LA, OWENS SB. A systematic review of intervention studies to prevent hospitalizations of community-dwelling older adults with dementia. Med Care. 2015;53:207–13. doi: 10.1097/MLR.0000000000000294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RUSS TC, PARRA MA, LIM AE, LAW E, CONNELLY PJ, STARR JM. Prediction of general hospital admission in people with dementia: cohort study. Br J Psychiatry. 2015;206:153–9. doi: 10.1192/bjp.bp.113.137166. [DOI] [PubMed] [Google Scholar]
- SALEN P, HELLER M, OLLER C, REED J. The impact of routine cognitive screening by using the clock drawing task in the evaluation of elderly patients in the emergency department. The Journal of emergency medicine. 2009;37:8–12. doi: 10.1016/j.jemermed.2007.06.031. [DOI] [PubMed] [Google Scholar]
- SAMARAS N, CHEVALLEY T, SAMARAS D, GOLD G. Older patients in the emergency department: a review. Ann Emerg Med. 2010;56:261–9. doi: 10.1016/j.annemergmed.2010.04.015. [DOI] [PubMed] [Google Scholar]
- SEYFRIED L, HANAUER DA, NEASE D, ALBEIRUTI R, KAVANAGH J, KALES HC. Enhanced identification of eligibility for depression research using an electronic medical record search engine. International journal of medical informatics. 2009 doi: 10.1016/j.ijmedinf.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TANNENBAUM C, PAQUETTE A, HILMER S, HOLROYD-LEDUC J, CARNAHAN R. A systematic review of amnestic and non-amnestic mild cognitive impairment induced by anticholinergic, antihistamine, GABAergic and opioid drugs. Drugs & aging. 2012;29:639–658. doi: 10.1007/BF03262280. [DOI] [PubMed] [Google Scholar]
- TOOT S, DEVINE M, AKPOROBARO A, ORRELL M. Journal of the American Medical Directors Association. Elsevier Ltd; 2013. Causes of Hospital Admission for People With Dementia: A Systematic Review and Meta-Analysis. [DOI] [PubMed] [Google Scholar]
- VAN DEN WIJNGAART MAG, VERNOOIJ-DASSEN MJFJ, FELLING AJA. The influence of stressors, appraisal and personal conditions on the burden of spousal caregivers of persons with dementia. Aging Ment Health. 2007;11:626–636. doi: 10.1080/13607860701368463. [DOI] [PubMed] [Google Scholar]
- WANCATA J, WINDHABER J, KRAUTGARTNER M, ALEXANDROWICZ R. The Consequences of Non-Cognitive Symptoms of Dementia in Medical Hospital Departments. The International Journal of Psychiatry in Medicine. 2003;33:257–271. doi: 10.2190/ABXK-FMWG-98YP-D1CU. [DOI] [PubMed] [Google Scholar]
- WILBER ST, LOFGREN SD, MAGER TG, BLANDA M, GERSON LW. Academic Emergency Medicine. Blackwell Publishing Ltd; 2005. An Evaluation of Two Screening Tools for Cognitive Impairment in Older Emergency Department Patients. [DOI] [PubMed] [Google Scholar]
- WOFFORD JL, SCHWARTZ E, BYRUM JE. The role of emergency services in health care for the elderly: a review. J Emerg Med. 1993;11:317–26. doi: 10.1016/0736-4679(93)90053-a. [DOI] [PubMed] [Google Scholar]
- YAFFE K, FOX P, NEWCOMER R, SANDS L, LINDQUIST K, DANE K, COVINSKY KE. Patient and caregiver characteristics and nursing home placement in patients with dementia. JAMA. 2002;287:2090–7. doi: 10.1001/jama.287.16.2090. [DOI] [PubMed] [Google Scholar]


