Abstract
Background
Many children who have overweight or obesity before puberty can develop obesity in early adulthood, which is associated with increased morbidity and mortality. The preschool years (ages 0–5) represents a point of opportunity for children to be active, develop healthy eating habits, and maintain healthy growth. Surveillance of childhood overweight and obesity in this age group can help inform future policies and interventions.
Objective
To review and report available prevalence data in WHO European Region Member States and determine how many countries can accurately report on rates of overweight and obesity in children under 5 years.
Methods
We conducted a rapid review of studies reporting on overweight and obesity prevalence in children ages 0–5 in the WHO European region member states from 1998 to 2015.
Results
Currently, 35 of the 53 member states have data providing prevalence rates for overweight and obesity for children under 5 years. There was little consistency in study methods, impacting comparability across countries. The prevalence of overweight and obesity in children under 5 years ranges from 1 to 28.6% across member states.
Conclusion
Although measuring overweight and obesity in this age group may be challenging, there is an opportunity to leverage existing surveillance resources in the WHO European Region.
Keywords: surveillance, childhood obesity, European region, policy
Background
Childhood growth is an important factor that influences health outcomes across the lifecourse, including obesity (1). Emerging evidence indicates that a large proportion of children who have obesity before puberty can develop obesity in early adulthood, with early-life fat deposition associated with later risk of adult obesity (2–6). Although the relationship between childhood obesity and poor health outcomes is highly complex and there are individual variations influenced by genetic, maturational, and socioeconomic factors, it is a major public health priority. This is in part because physiological and psychological health consequences during childhood can continue into adolescence and adulthood to impact population health in the future (7, 8). Specifically, childhood obesity is associated with an increased risk of premature illness and mortality, although improving Body Mass Index (a tool used to measure obesity at the population level) in adulthood does appear to reduce the later risk of morbidity and mortality (9–13). For example, rapidly increasing weight trajectories across the life course have been shown to be a risk factor for the development of non-communicable diseases (NCDs), notably cardiovascular diseases, cancer, and diabetes, which collectively are estimated to cause 75% of deaths by 2020, and musculoskeletal and orthopedic complications (7, 12). Prevention and management of obesity in childhood is therefore likely to be an effective way to contribute to preventing chronic diseases in adults.
The prevalence of childhood obesity is increasing across European countries. A quarter of children aged 6–9 years in European Union countries who participated in the WHO Europe Childhood Obesity Surveillance Initiative (COSI) were classified as having overweight or obesity in 2008, increasing to a third in 2010, with estimates ranging from 18.4% (Belgian 6-year-old girls) to 49.0% (Italian 8-year-old boys) (14). This report was based on 12 countries; however, COSI has expanded to currently include the following countries: Albania, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Greece, Hungary, Ireland, Italy, Kazakhstan, Latvia, Lithuania, Malta, Norway, Poland, Portugal, Republic of Moldova, Romania, Slovenia, Spain, Sweden, the former Yugoslav of Macedonia, and Turkey. As a result, many governments and international organizations have recommended some form of policy action to prevent obesity, with a great focus on preventing obesity in children (12, 15, 16).
Identifying policy action to prevent childhood obesity requires a better understanding of potential modifiable factors that drive obesity in particular age groups. Some modifiable risk factors for obesity include dietary and physical activity behaviors, which to a large extent, are learned at an early age (17, 18). In this way, preschool years are increasingly part of the health promotion equation in the context of chronic disease prevention and a point of opportunity for children to be physically active, develop healthy eating habits, and maintain healthy growth trajectories (19–24).
However, in order to plan and evaluate policy interventions designed to change modifiable risk factors, such as social and physical environments in which children live and play, policy makers need good surveillance. While recent studies have shown that the development of obesity may well be initiated in infancy and early childhood (4, 5), in many countries, surveillance data on obesity are missing or not routinely collected at these younger ages. In this article, we review and report on the currently available prevalence data in WHO European Region Member States in order to determine how many countries can accurately estimate the prevalence of obesity in children under 5 years.
Methods
We undertook a rapid review to identify and synthesize current evidence regarding the prevalence of obesity in children under 5 years in the WHO European Region and to determine how many countries can accurately estimate on this issue.
Our specific review questions were
What is the current evidence regarding the prevalence of obesity in children under 5 years in the WHO European Region?
Can WHO European Region Member States accurately estimate the prevalence of obesity in children under 5 years?
These guiding questions helped us define the scope of the search strategy, as well as the inclusion and exclusion criteria, construct summary tables presenting key information and findings, and synthesize the evidence from the included studies.
Search Strategy
We reviewed published and open access studies reporting on obesity prevalence in children aged 0–5 years (defined as data reporting body mass index; not including growth curves or aggregate data with children above these ages) in the WHO European Region Member States.
Our search strategy used structured relevant terms as follows:
population: children, infants
outcomes: body weight, growth, growth and development, body mass index, weight gain, prevalence, and incidence combined with overweight and obesity.
We searched four databases: PubMed, SCOPUS, Web of Science, and EMBASE. This search was conducted on November 16–20, 2015, and the searches were modified to suit the style of each database. We conducted a second search of the literature in 2016 and added a few more studies that were published in 2016. We employed keywords that would be aligned with the Medical Subject Headings used in the MEDLINE database. The following keywords were used: child, infant, ideal body weight, growth, growth and development, body mass index, body weight, weight gain, prevalence, and incidence combined with overweight and obesity. We also reviewed the references of electronically selected articles to see if any other relevant papers turned up. All data included are from studies whose participants signed a written informed consent form prior to inclusion and received approval from the appropriate ethics committee. We included articles that used various definitions of childhood obesity. For example, some articles used the WHO criterion (defined as the proportion of children with weight-for-height or BMI-for-age z-score values more than 2 SDs and more than 3 SDs, respectively, from the WHO growth standard median), while some used the International Obesity Task Force criterion. Other studies used country-specific criterion for obesity classification. We also included articles that used self-reported and/or measured data.
The inclusion criteria can be summarized as follows:
population: child, infant
outcomes: prevalence studies reporting obesity in children using various childhood obesity definitions (e.g., WHO and IOTF definitions) and using self-reported and/or measured data.
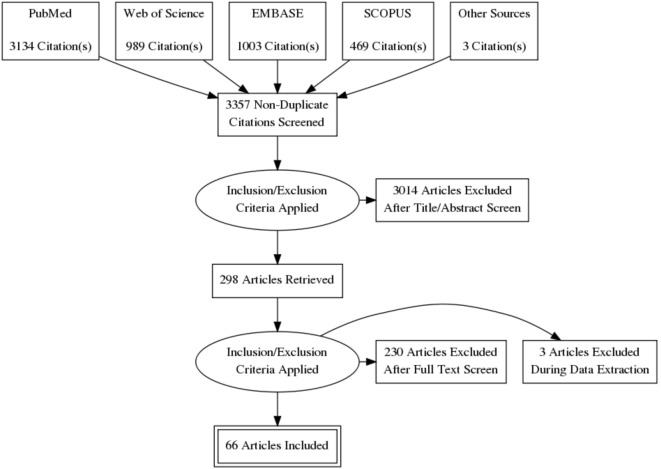
The electronic search yielded 5,595 results, with an additional three articles coming from other sources. We retrieved 3,134 from PubMed, 469 from Scopus, 989 from Web of Science, and 1,003 from EMBASE. We used RefWorks to organize and review all literature. After an initial deletion of exact or close duplicates, we were left with 3,357 articles. We then did two rounds of title screening, which left us with 298 articles for further screening. Our second round of screening involved abstract review for relevance. After full-text review, we were left with 66 records for analysis.
Exclusion Criteria
We extracted studies that were most relevant for the purpose of our review. We assessed relevance based on a number of factors, which included study type, the country in which the research was undertaken (i.e., WHO European Region), whether the research is single center or multi-center, and whether it included more than one measurement cycle. This process of quality and relevance assessment allowed us to determine the quantities of surveillance studies and their overall quality and direction. The studies included in the review were restricted to quantitative studies to ensure they addressed the key review questions and outcomes of interest (i.e., prevalence and reporting). We only included peer-reviewed studies that have been published and undergone methodological and expert scrutiny.
Flowchart of Study Inclusions
As an additional step and to form a cohesive perspective on the prevalence of overweight and obesity in the Region, we used data from existing nutrition surveillance studies. For example, the Demographic and Health Survey (DHS) and the Multiple Indicator Cluster Survey (MICS) monitor the prevalence of undernutrition in children under 5 in several European countries. We used data from the DHS and MICS surveys to calculate overweight and obesity prevalence in European countries that did not have specific overweight and obesity surveillance studies. Data available for Italy arises from WHO field-test data collected when trialing new WHO growth rate charts.
Results
Sixty-one studies provided overweight and obesity prevalence data for children under 5 years in WHO European Region member states. These studies analyzed overweight and obesity outcomes in different age ranges. For example, 29 studies analyzed overweight and obesity outcomes in children who were between 0 and 4 years old. While other studies, evaluated overweight and obesity outcomes in one particular age group (e.g., 3 years). The majority (N = 38) of the studies used the WHO criteria for overweight obesity, while other studies (N = 20) used the IOTF cutoffs. Three studies used country-specific cutoff (25–27). Furthermore, these studies provided little consistency in terms of time points of measurements and national representativeness, impacting comparability across countries.
Despite these limitations, currently 38 of the 53 member states in the European Region of the WHO have data providing prevalence rates for overweight and obesity in children under 5 years. More data were available in eastern and northern Europe, with data for the eastern region provided primarily via the DHS and MICS.
Table 1 illustrates the variability in prevalence within the region and within countries, based on all resources for all available countries. In regards to DHS and MICS reports, the most recent report for each available country was used. Sixteen of the 53 Member States have available DHS or MICS reports. The proportion of the population classified as having overweight and obesity varied from 1 to 28.6% in these Member States.
Table 1.
Prevalence of overweight and obesity for children under 5 years of age in the WHO European Region by country from published datasets and literature.
| Prevalence of overweight, including obesity (%) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference | Survey year | Country/region | Source | Age (years) | Sample (n) | Cutoffs of BMI (kg/m2) | 0 year | 1 year | 2 years | 3 years | 4 years | Total |
| Albania Demographic and Health Survey 2008–2009, Institute of Statistics, Institute of Public Health, and I. Macro (28) | 2008–2009 | Albania | DHS | 0–4 | 1,575 | WHO | 22.0 | |||||
| Armenia Demographic and Health Survey 2010, National Statistic Service (Armenia), Ministry of Health (Armenia), and I. Macro (29) | 2010 | Armenia | DHS | 0–4 | 1,491 | WHO | 15.0 | |||||
| Serbanescu (30) | 2001 | Azerbaijan | National | 0–4 | 2,426 | WHO | 4.4 | |||||
| Azerbaijan Demographic and Health Survey 2006, State Statistical Committee (Azerbaijan), Macro International (31) | 2006 | Azerbaijan | DHS | 0–4 | 2,242 | WHO | 13.0 | |||||
| UNICEF (32) | 2013 | Azerbaijan | National | 0–4 | 1,569 | WHO | 13.0 | |||||
| Greier and Riechelmann (26) | 2011–2012 | Austria | Subnational | 4–5 | 1,063 | German BMI reference | 13.0 | |||||
| Belarus Multiple Indicator Cluster Survey 2005, Final Report, Ministry of Statistics and Analysis of the Republic of Belarus (33) | 2005 | Belarus | MICS | 0–4 | 3,018 | WHO | 10.0 | |||||
| Bayingana (34) | 2004 | Belgium | National | 1–4 | 218 | IOTF | 7.0 | |||||
| Massa (35) | 1998–1999 | Belgium | Subnational (Limburg) | 0–4 | 970 | IOTF | 7.0 | |||||
| Verbestel et al. (36) | 2008–2009 | Belgium | Subnational | 0–2 | 191 | WHO | 16.9 | |||||
| Multiple Indicator Cluster Survey (MICS) Bosnia and Herzegovina 2011–2012 Final Report, The Agency for Statistics Bosnia and Herzegovina, et al. (37) | 2011–2012 | Bosnia and Herzegovina | MICS | 0–4 | 2,078 | WHO | 17.0 | |||||
| Baykova et al. (38) | 2004 | Bulgaria | National | 1–4 | 315 | WHO | 19.1 | 19.8 | 5.3 | 8.8 | ||
| Savva et al. (39) | 2004 | Cyprus | National | 2–4 | 744 | WHO | 6.4 | 10.8 | 18.0 | |||
| Savva (40) | 2004 | Cyprus | National | 2–4 | 647 | WHO | 5.2 | 5.4 | 5.8 | 10.6 | ||
| Vignerova et al. (41) | 2001 | Czech Republic | National | 0–4 | 16,457 | WHO | 2.1 | 7.9 | 5.5 | 4.8 | 5.4 | |
| Larsen et al. (42) | 2001 | Denmark | National | 0–4 | 5,580 | IOTF | Girls:12.3 boys: 10.8 | Girls: 10.8 boys: 5.2 | ||||
| Mattheissen et al. (43) | 2005–2008 | Denmark | National | 4–5 | - | IOTF | Girls: 21.9 boys: 17.6 | |||||
| Morgen et al. (44) | 1998–2010 | Denmark | Subnational | 0–1 | 155,635 | WHO | 1.2–7.3 | |||||
| Chollet et al. (45) | 2007–2009 | France | Subnational | 3–4 | 9,558 | IOTF | 8.4 | |||||
| Lioret et al. (46) | 1998–1999 | France | National | 3–4 | 170 | IOTF | 16.5 | |||||
| Lioret et al. (47) | 2006–2007 | France | National | 3–4 | 92 | IOTF | 10.1 | |||||
| Unité de surveillance et d’épidémiologie nutritionnelle (48) | 2006–2007 | France | National | 3–4 | 191 | IOTF | 11.4 | 17.9 | ||||
| Report of the Georgia National Nutrition Survey (GNNS) 2009 (49) | 2009 | Georgia | National | 0–4 | – | WHO | 20.0 | |||||
| Multiple Indicator Cluster Survey: Georgia Final Report 2005, State Department of Statistics of Georgia (50) | 2005 | Georgia | MICS | 0–4 | 1,812 | WHO | Girls: 16.2 boys: 14.3 | |||||
| Kurth and Schaffrath (51) | 2003–2006 | Germany | National | 0–4 | 4,667 | WHO | 3.5 | |||||
| Manios et al. (52) | 2003–2004 | Greece | Subnational | 1–4 | 2,348 | WHO | 12.7 | 13.5 | 13.6 | 15.7 | ||
| McCarthy et al. (53) | 2010–2012 | Ireland | Subnational | 2 | 1,189 | IOTF | 14.0 | |||||
| Whelton et al. (54) | 2001–2002 | Ireland | National | 4–5 | 2,109 | IOTF | Girls: 29.0 boys: 26.0 | |||||
| Whelton (40) | 2007 | Ireland | National | 4–5 | 1,352 | IOTF | 27.5 | |||||
| Onyango et al. (55) | 2005–2008 | Italy | Subnational | 0–4 | 2,977 | WHO | 2.8 | 7.3 | 5.7 | 10.9 | 10.2 | |
| The Statistics Committee of the Ministry Economy of the Republic of Kazakhstan (56) | 2015 | Kazakhstan | MICS | 0–4 | 5,510 | WHO | 9.3 | |||||
| 2012 Kyrgyz Demographic and Health Survey: Key Findings, National Statistical Committee (Kyrgyz Republic) and Macro International (57) | 2012 | Kyrgystan | DHS | 0–4 | 4,337 | WHO | 7.0 | |||||
| Zaborskis et al. (58) | 1999–2000 | Lithuania | Subnational | 3–4 | 451 | WHO | 5.1 | 2.0 | ||||
| Statistical Office of Montenegro (MONSTAT) and Strategic Marketing Research Agency (SMMRI) (59) | 2013 | Montenegro | MICS | 0–4 | 1,420 | WHO | 22.3 | |||||
| Van den Hurk et al. (60) | 2002–2004 | Netherlands | National | 4–5 | 1,781 | IOTF | Girls: 16.2 boys: 12.3 | |||||
| Küpers et al. (27) | 2006 | Netherlands | National | 2, 5 | Dutch reference growth curves | 8.4 | 13.2 | |||||
| Schönbeck et al. (61) | 2009 | Netherlands | National | 2–4 | 4,382 | IOTF | Girls: 9.0 boys: 8.7 | Girls: 14.4 boys: 8.6 | Girls: 18.9 boys: 10.2 | |||
| Frenken (40) | 2007–2009 | Netherlands | National | 2 | 1,878 | WHO | 9.0 | |||||
| Juliusson (62) | 2003–2006 | Norway | Subnational | 2–4 | 2,231 | IOTF | 16.0 | 11.0 | 11.5 | |||
| Szponar et al. (63) | 2000 | Poland | National | 1–4 | 175 | WHO | 28.6 | 14.3 | 12.2 | 8.7 | ||
| Rito (64) | 2001 | Portugal | Subnational | 3–4 | 1,546 | WHO | 10.8 | 10.5 | ||||
| Bingham (65) | 2009 | Portugal | Subnational | 3–4 | 3,406 | IOTF | 17.4 | 22.9 | ||||
| National Scientific and Applied Center for Preventive Medicine (NCPM) [Moldova] and ORC Macro (66) | 2012 | Republic of Moldova | MICS | 0–4 | 1,724 | WHO | 4.9 | |||||
| Nanu (67) | 2004 | Romania | National | 0–4 | 3,971 | WHO/UNICEF/ICCIDD | 8.0 | |||||
| Nanu (40) | 2004 | Romania | National | 0–4 | 3,971 | WHO | 3.3 | 8.4 | 8.3 | 8.0 | 5.5 | |
| Nazarova and Kuzmichev (68) | 2012–2013 | Russia | Subnational | 3–4 | 1,242 | WHO | Girls: 18.5 boys: 17.7 | |||||
| MICS (69) | 2014 | Serbia | MICS | 0–4 | 2,270 | WHO | 13.9 | |||||
| Encuesta Nacional de Salud 2006 (70) | 2006 | Spain | National | 0–4 | 2,701 | WHO | 16.8 | 12.8 | 18.4 | 17.1 | 17.2 | |
| Serra-Majem et al. (71) | 1998–2000 | Spain | National | 2–4 | 268 | WHO | 10.2 | 15.6 | 12.9 | |||
| Huus et al. (72) | 1997–2002 | Sweden | Subnational | 0.5–4 | 4,242 | IOTF | 15.4 | |||||
| Huss (40) | 1997–2002 | Sweden | Subnational | 0–4 | 10,438 | WHO | 4.8 | 6.6 | 8.0 | 7.6 | 4.7 | |
| Holmbäck et al. (73) | 2002 | Sweden | Subnational | 4 | 90 | IOTF | 18.0 | |||||
| Holmbäck (40) | 2002 | Sweden | Subnational | 4 | 183 | IOTF | 21.0 | |||||
| Enghardt et al. (74) | 2003 | Sweden | National | 4 | 590 | IOTF | 18.7 | |||||
| TLSS (75) | 2012 | Tajikistan | DHS | 0–4 | 5,478 | WHO | 6.0 | |||||
| Hacettepe University Institute of Population Studies (76) | 2013 | Turkey | DHS | 0–4 | 2,519 | WHO | 10.9 | |||||
| The State Committee of Statistics of Turkmenistan and UNICEF (77) | 2015–2016 | Turkmenistan | MCIS | 0–4 | 3,785 | WHO | 5.9 | |||||
| Multiple Indicator Cluster Survey (MICS) Former Yugoslav Republic of Macedonia Final Report 2011, IPSOS Strategic Puls, et al. (78) | 2011 | the former Yugoslav of Macedonia | MICS | 0–4 | 3,949 | WHO | 12.0 | |||||
| Stamatakis (79) | 2002–2004 | United Kingdom | Subnational | 2–4 | 1,903 | WHO | 11.7 | 11.1 | 10.3 | |||
| Whelton et al. (54) | 2003 | United Kingdom | Subnational | 4 | 104 | IOTF | 21.0 | |||||
| Pearce et al. (80) | 2000–2002 | United Kingdom | National | 3–4 | 12,354 | IOTF | 23.1 | |||||
| Hirani and Stamatakis (25) | 2003 | United Kingdom | Subnational | 2–4 | 4,986 | UK BMI | Girls: 26.0 boys: 24.0 | |||||
| UNICEF and State Statistical Committee of the Republic of Uzbekistan (81) | 2006 | Uzbekistan | MICS | 0–4 | 5,165 | WHO | 12.8 | |||||
Reference 39 is work from other authors which was reanalyzed by Cattaneo et al. (40).
The lack of consistency in methods makes it difficult to assess overweight and obesity trends (both between and within countries at a given point and over time) in children under 5 years. DHS and MICS data also show that there is a large degree of variability in the prevalence of overweight between and even within countries across data collection time points (see Figure 1).
Figure 1.
Prevalence of overweight (including obesity) in children under age 5 in countries with DHS and/or MICS reports over time (93–105).
Discussion
Currently, 35 of the 53 member states from the WHO European Region have prevalence data for overweight and obesity for children under the age of 5 years old. However, the current state of surveillance and monitoring in the European Region for children under the age of 5 years is discouraging with pervasive issues of inconsistency in both method of, and occurrence of, collection. For example, one MICS (which uses measured anthropometrics as opposed to self-reported data) for a Central Asian country from 2006 estimates prevalence of overweight and obesity to be 11.3% for children ages 0–4 using WHO cutoffs (82). The next MICS for the same country in 2010–2011 confusingly reports a prevalence of 0.6%, with the same age range and same cutoffs (83, 84). The next MICS for the same country in 2015 estimates prevalence to be 9.3% (56). This phenomenon holds true for multiple countries (29, 37, 85–88). Bosnia & Herzegovina and Armenia show a similar but less dramatic trend in vast differences between survey waves. Though difficult to provide a concrete explanation for these inconsistencies, it does perhaps highlight a general need for better training of interviewers in anthropometric measurements and/or careful attention to sampling techniques across survey years.
Furthermore, many of the estimates presented in this paper are outdated with some prevalence estimates reaching as far back as the early 1990s. Current data suggest that overweight and obesity may be increasing in the Central Asian part of the region whereas trends in other parts of the region are not immediately clear (89). Additional and more recent data points are needed to identify current trends and confirm current prevalence rates.
The variability in type of cutoffs used in these studies also reduces the Region’s capability of comparing between and within countries. In 2006, the WHO released growth standards based on the finding that well-nourished children of all populations follow similar growth patterns before puberty (82, 90). These can provide the basis and standardized cutoffs for countries to plot child growth and identify overweight and obesity.
Beyond measurement issues affecting the quality of data, there is a lack of data in general. Only 66% of Member States had published literature on prevalence of overweight and obesity in children under 5 years. Of those countries with data, 34% were from DHS or MICS surveys, which primarily focus on the prevalence of undernutrition in children under 5 years.
Considering that preventing childhood obesity and supporting health across the lifespan is an important priority for WHO European Member States, our review indicates that there is an opportunity to strengthen existing surveillance for children under the age of 5 years in order to provide timely, regular and quality data that can inform policy action. The development of surveillance systems is also vital for the successful monitoring and evaluation of population level interventions and policies and can help strengthening advocacy efforts for government action (12).
The European region has been a forerunner in regards to surveillance in other age groups, particularly with the implementation of COSI in nearly 30 countries. COSI routinely measures the prevalence of overweight and obesity in primary school-aged children (6–9 years) to monitor change in prevalence in this population group as well as to permit inter-country comparisons (91, 92). Furthermore, almost all European countries participate in the Health Behaviors in School-Aged Children survey (HBSC), which provides (self-reported) data on overweight and obesity in children and adolescents aged 11, 13, and 15 (91, 92). Both initiatives have been invaluable to countries in monitoring trends, documenting the prevalence of childhood obesity and helping to prioritize policy responses. Similar monitoring exercises for children under the age of 5 years could be used to detect relevant changes within and between countries over time and to support policy action in early-life years.
Increasing surveillance in this age group may have its challenges. Previous work in the region for older children [COSI (6–9 years) and HBSC (11–15 years)] has effectively used schools as the location for sampling (11, 91). For children under the age of 5 years old, new sampling approaches would be needed. For example, pediatric offices are potential sampling frames to consider, with many young children having repeat check-ups with health-care professionals. Surveillance among this age group may also bring up new challenges concerning measurement (including ensuring standardized approaches). Nevertheless, clear guidance exists for measuring young children’s growth for stunting/wasting, including checklists and step-by-step procedures, and there is no reason that these could not be adapted as a protocol for measurement of overweight/obesity (55).
Conclusion
The need to shift the focus to early-life obesity prevention was underscored by the 2016 “Ending Childhood Obesity Report” and Institute of Medicine’s report “Early Childhood Obesity Prevention Policies.” These called for further research into effective policy interventions to prevent obesity in early childhood (12, 18).
While it is generally recognized that childhood growth surveillance is crucial, despite many countries recommending growth monitoring in health care, routine and representative assessment of the prevalence of overweight and obesity are not common in the majority of the WHO European Member States. In order achieve the best outcomes from any future investment in obesity prevention in early life years, concerted efforts should be made to implement interventions and policies, which are specific and relevant to the target group and sub-groups. To best achieve this aim, there is a need for increased range of coverage and quality of data in surveillance on overweight and obesity in this age group that can be disaggregated according to socioeconomic variables.
More widespread and systematic direct measurement of childhood growth and weight trajectories at younger ages can also provide an improved understanding of how obesity develops in young children. At the European level, the Vienna Declaration committed countries in the European Region to addressing the root causes of obesity and diet-related NCDs and calls on WHO to support Member States monitor population trends. It is fully expected that surveillance programs focusing on younger age groups will complement the good existing work for school-aged children.
Consent for Publication
Not applicable. This was a review solely of previously published data, where the previous researchers had done all consenting and ethical proceedings in line with institutional review boards.
Data Availability
Data used in this paper is all currently publicly available online in journal articles and/or published results from surveys, and full references are provided.
Author Contributions
RJ, together with JB, conceived the idea for this paper, conducted, supported, and interpreted results of literature reviews, and wrote original drafts of most of the text, including creating text. RS assisted in the literature reviews and wrote text. JJ and XRS assisted in the conception of the paper, assisted with the interpretation of the results, contributed to the discussion and all other aspects of the paper, and assisted with editing the paper. JB and JJ are staff members of the World Health Organization Regional Office for Europe. XRS is a technical consultant with the Department of Nutrition, Physical Activity, and Obesity, European Region of World Health Organization, Copenhagen, Denmark. The authors are responsible for the views expressed in this publication and they do not necessarily represent the decisions or stated policy of WHO.
Conflict of Interest Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The handling Editor declared a shared affiliation, though no other collaboration, with several of the authors (RS and JB), and the handling Editor states that the process met the standards of a fair and objective review.
Acknowledgments
The authors would also like to acknowledge the support of the European Commission in facilitating this work.
Abbreviations
NCDs, non-communicable diseases; WHO, World Health Organization; EU, European Union; COSI, WHO Europe Childhood Obesity Surveillance Initiative; DHS, Demographic and Health Survey; MICS, Multiple Indicator Cluster Survey; HBSC, Health Behaviors in School-Aged Children survey.
References
- 1.Monteiro POA, Victora CG. Rapid growth in infancy and childhood and obesity in later life – a systematic review. Obes Rev (2005) 6(2):143–54. 10.1111/j.1467-789X.2005.00183.x [DOI] [PubMed] [Google Scholar]
- 2.Sun SS, Liang R, Huang TT, Daniels SR, Arslanian S, Liu K, et al. Childhood obesity predicts adult metabolic syndrome: the Fels longitudinal study. J Pediatr (2008) 152(2):191–200. 10.1016/j.jpeds.2007.07.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cunningham SA, Kramer MR, Narayan KMV. Incidence of childhood obesity in the United States. N Engl J Med (2014) 370(5):403. 10.1056/NEJMoa1309753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eid EE. Follow-up study of physical growth of children who had excessive weight gain in first six months of life. Br Med J (1970) 2(5701):74. 10.1136/bmj.2.5701.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stettler N, Kumanyika SK, Katz SH, Zemel BS, Stallings VA. Rapid weight gain during infancy and obesity in young adulthood in a cohort of African Americans. Am J Clin Nutr (2003) 77(6):1374–8. [DOI] [PubMed] [Google Scholar]
- 6.Lloyd LJ, Langley-Evans S, McMullen S. Childhood obesity and risk of the adult metabolic syndrome: a systematic review. Int J Obes (2012) 36(1):1–11. 10.1038/ijo.2011.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics (1998) 101(3):518. [PubMed] [Google Scholar]
- 8.World Health Organization. Global Status Report on Non-Communicable Diseases. Geneva: World Health Orgaization; (2014). Available from: http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf [Google Scholar]
- 9.O’Malley G, Santoro N, Northrup V, D’Adamo E, Shaw M, Eldrich S, et al. High normal fasting glucose level in obese youth: a marker for insulin resistance and beta cell dysregulation. Diabetologia (2010) 56(6):1199–209. 10.1007/s00125-010-1693-0 [DOI] [PubMed] [Google Scholar]
- 10.de Onis M, Blössner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr (2010) 92(5):1257–64. 10.3945/ajcn.2010.29786 [DOI] [PubMed] [Google Scholar]
- 11.Wjnhoven TM, van Raaij JM, Sjöberg A, Eldin A, Yngve A, Kunešová M, et al. WHO European Childhood Obesity Surveillance Initiative: school nutrition environment and body mass index in primary schools. Int J Env Res Public Health (1956) 2014:11261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Report of the Commission on Ending Childhood Obesity. (2016). Available from: http://apps.who.int/iris/bitstream/10665/204176/1/9789241510066_eng.pdf
- 13.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Series: maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet (2013) 382:427–51. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- 14.Wijnhoven TM, van Raaij JM, Spinelli A, Rito AI, Hovengen R, Kunesova M, et al. WHO European Childhood Obesity Surveillance Initiative 2008: weight, height and body mass index in 6-9-year-old children. Int J Pediatr Obes (2013) 8(2):79–97. 10.1111/j.2047-6310.2012.00090.x [DOI] [PubMed] [Google Scholar]
- 15.Akdag R, Danzon M. WHO European Ministerial Conference on Countering Obesity: Diet and Physical Activity for Health. Copenhagen: WHO Regional Office for Europe; (2006). Available from: http://www.euro.who.int/__data/assets/pdf_file/0006/96459/E90143.pdf [Google Scholar]
- 16.World Health Organization Regional Office of Europe. Vienna Declaration on Nutrition and Non-Communicable Diseases in the Context of Health 2020. Copenhagen: WHO Regional Office for Europe; (2013). Available from: http://www.euro.who.int/__data/assets/pdf_file/0005/193253/CONSENSUS-Vienna-Declaration-5-July-2013.pdf [Google Scholar]
- 17.Benton D. Role of parents in the determination of the food preferences of children and the development of obesity. Int J Obes Relat Metab Dis (2004) 28(7):858–69. 10.1038/sj.ijo.0802532 [DOI] [PubMed] [Google Scholar]
- 18.McGuire S. Institute of medicine (IOM) early childhood obesity prevention policies. washington, DC: The national academies press; 2011. Adv Nutr (2012) 3(1):56–7. 10.3945/an.111.001347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cole TJ. Children grow and horses race: is the adiposity rebound a critical period for later obesity? BMC Pediatr (2004) 4:6–6. 10.1186/1471-2431-4-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ventura AK, Mennella JA, Ventura AK, Mennella JA. Innate and learned preferences for sweet taste during childhood. Curr Opi Clin Nutr Metab Care (2011) 14(4):379–84. 10.1097/MCO.0b013e328346df65 [DOI] [PubMed] [Google Scholar]
- 21.Wardle J, Cooke L. Genetic and environmental determinants of children’s food preferences. Br J Nutr (2008) 99(Suppl 1):S15–21. 10.1017/S000711450889246X [DOI] [PubMed] [Google Scholar]
- 22.Birch LL. Development of food acceptance patterns in the first years of life. Proc Nutr Soc (1998) 57(4):617–24. 10.1079/PNS19980090 [DOI] [PubMed] [Google Scholar]
- 23.Harris G. Development of taste and food preferences in children. Curr Opi Clin Nutr Metab Care (2008) 11(3):315–9. 10.1097/MCO.0b013e3282f9e228 [DOI] [PubMed] [Google Scholar]
- 24.Mennella JA, Jagnow CP, Beauchamp GK. Prenatal and postnatal flavor learning by human infants. Pediatrics (2001) 107(6):E88–88. 10.1542/peds.107.6.e88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hirani V, Stamatakis E. Chapter 1: Cardiovascular disease and associated risk factors. In: Bromley C, Sproston K, Shelton M, editors. The Scottish Health Survey 2003. Edinburgh, Scotland: Scottish Executive; (2005). Available from: http://www.gov.scot/resource/doc/76169/0019727.pdf [Google Scholar]
- 26.Greier K, Riechelmann H. Effects of migration background on weight status and motor performance of preschool children. Wien Klin Wochenschr (2014) 26(3–4):95–100. 10.1007/s00508-013-0474-4 [DOI] [PubMed] [Google Scholar]
- 27.Küpers LK, de Pijper JJ, Sauer PJJ, Stolk RP, Corpelejn E. Skipping breakfast and overweight in 2-and 5-year-old Dutch children – the GECKO Drenthe cohort. Int J Obes (2014) 38(4):569–71. 10.1038/ijo.2013.194 [DOI] [PubMed] [Google Scholar]
- 28.Albania Demographic and Health Survey 2008–2009, Institute of Statistics, Institute of Public Health, and I. Macro , editors. Tirana, Albania: (2010). Available from: https://dhsprogram.com/pubs/pdf/FR230/FR230.pdf [Google Scholar]
- 29.Armenia Demographic and Health Survey 2010, National Statistic Service (Armenia), Ministry of Health (Armenia), and I. Macro , editors. Calverton, MD: (2012). Available from: https://dhsprogram.com/pubs/pdf/FR252/FR252.pdf [Google Scholar]
- 30.Serbanescu F, Morris L, Rahimova S, Stupp P, editors. Adventists Development and Relief Agency, Azerbaijan Ministry of Health, State Committee of Statistics, Mercy Crops [Baku, Azerbaijan], DRH/CDC, USAID. UNFPA, UNHCR Reproductive health survey Azerbaijan 2001: Final Report. Atlanta, GA: US Department of Health and Human Services, CDC; (2003). [Google Scholar]
- 31.Azerbaijan Demographic and Health Survey 2006, State Statistical Committee (Azerbaijan), Macro International. Calverton, MD: (2008). Available from: https://dhsprogram.com/pubs/pdf/FR195/FR195.pdf [Google Scholar]
- 32.Ministry of Health of the Republic of Azerbaijan, the State Statistical Committee of Azerbaijan, and the Azerbaijan office of the United Nations Children’s Fund (UNICEF) Azerbaijan Nutrition Survey Report. Baku, Republic of Azerbaijan: (2014). [Google Scholar]
- 33.Belarus Multiple Indicator Cluster Survey 2005, Final Report, Ministry of Statistics and Analysis of the Republic of Belarus. Minsk, Republic of Belarus: (2007). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS3/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Belarus/2005/Final/Belarus%202005%20MICS_English.pdf [Google Scholar]
- 34.Bayingana K, Demarest S, Gisle L, Hesse E, Miermans P, Tafforeau J. Gezondheisenquete door middle van interview Belgie 2004 [Health Interview Survey Belgium 2004]. Brussels: Scientific Institute of Public Health; (2006). [Google Scholar]
- 35.Massa G. Body mass index measurements and prevalence of overweight and obesity in school-children living in the province of Belgian Limburg. Eur J Pediatr (2002) 161(6):343–6. 10.1007/s00431-002-0932-x [DOI] [PubMed] [Google Scholar]
- 36.Verbestel V, De Coen V, Van Winckel M, Huybrechts I, Maes L, De Bourdeaudhuij I. Prevention of overweight in children younger than 2 years old: a pilot cluster-randomized controlled trial. Public Health Nutr (2014) 17(06):1384–92. 10.1017/S1368980013001353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Multiple Indicator Cluster Survey (MICS) Bosnia and Herzegovina 2011–2012 Final Report, The Agency for Statistics Bosnia and Herzegovina et al. Sarajevo: (2013). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS4/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Bosnia%20and%20Herzegovina/2011-2012/Final/Bosnia%20and%20Herzegovina%202011-12%20MICS_English.pdf [Google Scholar]
- 38.Baykova D, Duleva V, Petrova S, Angelova K, Jordanov B, Vatralova K, et al. National Monitoring of Dietary Intake and Nutritional Status of Bulgarian Population 2004. Sofia: Department of Nutrition and Public Health; (2008). [Google Scholar]
- 39.Savva SC, Tornaritis M, Chadjigeorgiou C, Kourides YA, Savva ME, Panagi A, et al. Prevalence and socio-demographic associations of undernutrition and obesity among preschool children in Cyprus. Eur J Clin Nutr (2005) 59(11):1259–65. 10.1038/sj.ejcn.1602237 [DOI] [PubMed] [Google Scholar]
- 40.Cattaneo A, Monasta L, Stamatakis E, Lioret S, Castetbon K, Frenken F, et al. Overweight and obesity in infants and pre-school children in the European Union: a review of existing data. Obes Rev (2010) 11(5):389–98. 10.1111/j.1467-789X.2009.00639.x [DOI] [PubMed] [Google Scholar]
- 41.Vignerová J, Humeníkova L, Brabec M, Riedová J, Bláha P. Long-term changes in body weight, BMI, and adiposity rebound among children and adolescents in Czech Republic. Econ Hum Biol (2007) 5(3):409–25. 10.1016/j.ehb.2007.07.003 [DOI] [PubMed] [Google Scholar]
- 42.Larsen LM, Hertel NT, Mølgaard C, Christensen Rd, Husby S, Jarbøl DE. Prevalence of overweight and obesity in Danish preschool children over a 10-year period: a study of two birth cohorts in general practice. Acta Paediatr (2012) 101:201–7. 10.1111/j.1651-2227.2011.02551.x [DOI] [PubMed] [Google Scholar]
- 43.Matthiessen J, Stockmarr A, Biltoft-Jensen A, Fagt S, Zhang H, Groth M. Trends in overweight and obesity in Danish children and adolescents: 2000-2008: exploring changes according to parental education. Scand J Public Health (2014) 42(4):385–92. 10.1177/1403494813520356 [DOI] [PubMed] [Google Scholar]
- 44.Morgen CS, Rokholm B, Brixval CS, Andersen CS, Andersen LG, Rasmussen M, et al. Trends in prevalence of overweight and obesity in Danish infants, children and adolescents are we still on a plateau. PLoS One (2013) 8(7):e69860. 10.1371/journal.pone.0069860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chollet C, Ehlinger V, Dupuy M, Guitard C, Leautier D, Jouret B, et al. [Prevalence of overweight preschool-aged children: medical examination data of schoolchildren in southwestern France]. Arch Pediatr (2013) 20(11):1187–92. 10.1016/j.arcped.2013.08.010 [DOI] [PubMed] [Google Scholar]
- 46.Lioret S, Mariet B, Volatier JL, Charles MA. Child overweight in France and its relationship with physical activity, sedentary behavior and socioeconomic status. Eur J Clin Nutr (2007) 61:509–16. 10.1038/sj.ejcn.1602538 [DOI] [PubMed] [Google Scholar]
- 47.Lioret S, Touvier M, Dubuisson C. Trends in overweight rates and energy intake in France from 1999 to 2007: relationships with socioeconomic status. Obesity (2009) 17:1092–100. 10.1038/oby.2008.619 [DOI] [PubMed] [Google Scholar]
- 48.Unité de surveillance et d’épidémiologie nutritionnelle. Etude nationale nutrition santé (ENNS, 2006). Situation nutritionnelle en France en 2006 selon les indicateurs d’objectif et les repères du Programme National Nutrition Santé (PNNS). St Maurice: Institut de veille sanitaire Université de Paris 13, Conservatoire national des arts et métiers; (2007). [Google Scholar]
- 49.Report of the Georgia National Nutrition Survey (GNNS) 2009. Tbilisi, Georgia: NCDC&PH and UNICEF; (2010). Available from: http://unicef.ge/uploads/Report_of_the_Georgia_National_Nutrition_Survey_2009_-_eng.pdf [Google Scholar]
- 50.Multiple Indicator Cluster Survey: Georgia Final Report 2005, State Department of Statistics of Georgia. (2008). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS3/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Georgia/2005/Final/Georgia%202005%20MICS_English.pdf
- 51.Kurth BM, Schaffrath RA. Die Verbreitung von Übergewicht und Adipositas bei Kindern und Jugendlichen in Deutschland. Ergebnisse des bundesweiten Kinder- und Jugendgesundheitssurveys (KiGGS). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz (2010) 50:736–43. 10.1007/s00103-007-0235-5 [DOI] [PubMed] [Google Scholar]
- 52.Manios Y, Costarelli V, Kolotourou M, Kondakis K, Tzavara C, Moschonis G. Prevalence of obesity in preschool Greek children, in relation to parental characteristics and region of residence. BMC Public Health (2007) 7:178. 10.1186/1471-2458-7-178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McCarthy EK, ní Chaoimh C, Murray DM, Hourihane JB, Kenny LC, Kiely M. Eating behaviour and weight status at 2 years of age: data from the Cork BASELINE Birth Cohort Study. Eur J Clin Nutr (2015) 69:1356–9. 10.1038/ejcn.2015.130 [DOI] [PubMed] [Google Scholar]
- 54.Whelton H, Harrington J, Crowley E, Kelleher V, Cronin M, Perry IJ. Prevalence of overweight and obesity on the island of Ireland results from the North South Survey of children’s height, weight and body mass index. 2002. BMC Public Health (2007) 7:187. 10.1186/1471-2458-7-187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Onyango AW, de Onis M, Caroli M, Shah U, Sguassero Y, Redondo N, et al. Field-testing the WHO child growth standards in four countries. J Nutr (2007) 137(1):149–52. [DOI] [PubMed] [Google Scholar]
- 56.The Statistics Committee of the Ministry Economy of the Republic of Kazakhstan. 2015 Kazakhstan Multiple Indicator Cluster Survey, Key Findings. Astana, Kazakhstan: The Statistics Committee of the Ministry of National Economy of the Republic of Kazakhstan; (2016). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS5/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Kazakhstan/2015/Key%20findings/Kazakhstan%202015%20MICS%20KFR_English.pdf [Google Scholar]
- 57.Kyrgyz Demographic and Health Survey: Key Findings, National Statistical Committee (Kyrgyz Republic) and Macro International. Bishek, Kyrgyz Republic; Calverton, MD: (2013). Available from: https://dhsprogram.com/pubs/pdf/FR283/FR283.pdf [Google Scholar]
- 58.Zaborskis A, Petrauskiene A, Gradeckiene S, Vaitkaitiene E, Bartasiūte V. Overweight and increased blood pressure in preschool-aged children. Medicina (Kaunas) (2003) 39(12):1200–7. [PubMed] [Google Scholar]
- 59.Statistical Office of Montenegro (MONSTAT) and Strategic Marketing Research Agency (SMMRI). Montenegro Multiple Indicator Cluster Survey 2005, Final Report. Podgorica: (2006). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS3/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Montenegro/2005-2006/Final/Montenegro%202005-06%20MICS_English.pdf [Google Scholar]
- 60.van den Hurk K, van Dommelen P, van Buuren S, Verkerk PH, Hirasing RA. Prevalence of overweight and obesity in the Netherlands in 2003 compared to 1980 and 1997. Arch Dis Child (2007) 92(11):992–5. 10.1136/adc.2006.115402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schönbeck Y, Talma H, van Dommelen P, Bakker B, Buitendijk SE, Hirasing RA, et al. Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PLoS One (2011) 6(11):e27608. 10.1371/journal.pone.0027608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Juliusson PB. Overweight and Obesity in Norwegian Children: Trends, Current Prevalence, Effect of Socio-Demographic Factors and Parental Perception. Bergen: University of Bergen; (2010). 100 p. 1333–7. [Google Scholar]
- 63.Szponar L, Sekula W, Nelson M, Weisell RC. The household food consumption and anthropometric survey in Poland. Public Health Nutr (2001) 4(5B):1183–6. [PubMed] [Google Scholar]
- 64.Rito AI. Estado nutricional de criancas e oferta alimentar do pre-escolar do municipio de Coimbra, Portugal, 2001. Rio de Janeiro: Escola Nacional De Saude Publica Sergio Arouca De Funcao Oswaldo Cruz and Saude; (2004). [Google Scholar]
- 65.Bingham DD, Varela-Silva MI, Ferrão MM, Augusta G, Mourão MI, Nogueira H, et al. Socio-demographic and behavioral risk factors associated with the high prevalence of overweight and obesity in Portuguese Children. Am J Hum Biol (2013) 25:733–42. 10.1002/ajhb.22440 [DOI] [PubMed] [Google Scholar]
- 66.National Scientific and Applied Center for Preventive Medicine (NCPM) [Moldova] and ORC Macro. Moldova Demographic and Health Survey 2005. Calverton, MD: National Scientific and Applied Center for Preventive Medicine of the Ministry of Health and Social Protection and ORC Macro; (2006). Available from: https://dhsprogram.com/pubs/pdf/FR178/FR178.pdf [Google Scholar]
- 67.Nanu M. Nutritional Status of Children under 5 Years Old. National Nutritional Surveillance Programm 1993-2002. Bucharest: Alfred Rusescu Institue for Mother and Child Care; (2003). [Google Scholar]
- 68.Nazarova E, Kuzmichev Y. The height-, weight- and BMI-for-age of preschool children from Nzihny Novgorod city, Russia, relative to the international growth references. BMC Public Health (2016) 16:274. 10.1186/s12889-016-2946-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Statistical Office of the Republic of Serbia and UNICEF 2014 Serbia Multiple Indicator Cluster Survey and 2014 Serbia Roma Settlements Multiple Indicator Cluster Survey (MICS). Key Findings. Belgrade, Serbia: Statistical Office of the Republic of Serbia and UNICEF; (2014). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS5/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Serbia/2014/Final/Serbia%20%28National%20and%20Roma%20Settlements%29%202014%20MICS_English.pdf [Google Scholar]
- 70.Encuesta Nacional de Salud 2006. Estilos de vida y practicas preventivas. Madrid: Institute Nacional de Estadistica and Consumo; (2008). [Google Scholar]
- 71.Serra-Majem L, Aramcet-Batrina J, Perez-Rodrigo C, Ribas-Barba L, Delgado-Rubio A. Prevalence and determinants of obesity in Spanish children and young people. Br J Nutr (2006) 96(Suppl 1):S67–72. 10.1079/BJN20061703 [DOI] [PubMed] [Google Scholar]
- 72.Huus K, Kudvigsson JF, Enskär K, Ludvigsson J. Risk factors in childhood obesity-findings from the All Babies in Southwest Sweden (ABIS) cohort. Acta Paediatr (2007) 96(9):1321–5. 10.1111/j.1651-2227.2007.00408.x [DOI] [PubMed] [Google Scholar]
- 73.Holmbäck U, Fridman J, Gustafsson J, Proos L, Sundelin C, Forslund A. Overweight more prevalent among children than among adolescents. Acta Paediatr (2007) 96(4):577–81. 10.1111/j.1651-2227.2006.00189.x [DOI] [PubMed] [Google Scholar]
- 74.Enghardt BH, Pearson M, Becker W. Dietary Habits and Nutrient Intake in Swedish Children 4 Year Old and School Children in Grade 2 and 5 (Riksmaten-Barn 2003), Uppsala. Uppsala, Sweden: National Food Administration (Livsmedelsverket) (2006). [Google Scholar]
- 75.State Committee on Statistics [Republic of Tajikistan] and UNICEF Tajikistan Living Standards Measurement Survey (TLSS): Indicators at a Glance. (2007). Available from: http://www.stat.tj/en/img/e4f46968ef1143d0ddb14e16b8d9d6d9_1280833182.pdf
- 76.Hacettepe University Institute of Population Studies. Turkey Demographic and Health Survey. Ankara, Turkey: Hacettepe University; (2013). Available from: https://dhsprogram.com/pubs/pdf/FR160/FR160.pdf [Google Scholar]
- 77.The State Committee of Statistics of Turkmenistan and UNICEF. 2015-2016 Turkmenistan Multiple Indicator Cluster Survey, Key Findings. Ashgabat, Turkmenistan: The State Committee of Statistics of Turkmenistan and UNICEF; (2016). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS5/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Turkmenistan/2015-2016/Key%20findings/Turkmenistan%202015-16%20MICS%20KFR_English.pdf [Google Scholar]
- 78.Multiple Indicator Cluster Survey (MICS) Former Yugoslav Republic of Macedonia Final Report 2011, IPSOS Strategic Puls et al. Former Yugoslav Republic of Macedonia. (2012). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS4/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Macedonia%2C%20The%20Former%20Yugoslav%20Republic%20of/2011/Final/Macedonia%20%28National%20and%20Roma%20Settlements%29%202011%20MICS_English.pdf
- 79.Stamatakis E. Anthropometric measurements, overweight and obesity. In: Sproston K, Primatesta P, editors. The Health for Children and Young People Health Survey for England 2002. London: Department of Health; (2003). [Google Scholar]
- 80.Pearce A, Li L, Abbas J, Ferguson B, Graham H, Law C, et al. Is childcare associated with the risk of overweight and obesity in the early years? Findings from the UK Millennium Cohort Study. Int J Obes (2010) 34(7):1160–8. 10.1038/ijo.2010.15 [DOI] [PubMed] [Google Scholar]
- 81.UNICEF and State Statistical Committee of the Republic of Uzbekistan. Uzbekistan Multiple Indicator Cluster Survey 2006, Final Report. Tashkent, Uzbekistan: UNICEF; (2007). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS3/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Uzbekistan/2006/Final/Uzbekistan%202006%20MICS_English.pdf [Google Scholar]
- 82.WHO Multicentre Growth Reference Study Group. WHO Child Growth. Standards based on length/height, weight and age. Acta Paediatr (2006) 45(Suppl):76–85. [DOI] [PubMed] [Google Scholar]
- 83.The Agency of Statistics (RK) and R.S.E.I.C. Centers. Multiple Indicator Cluster Survey (MICS) in the Republic of Kazakhstan, 2010-2011, Final Report. Astana, Kazakhstan: (2012). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS4/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Kazakhstan/2010-2011/Final/Kazakhstan%202010-11%20MICS_English.pdf [Google Scholar]
- 84.Multiple Indicator Cluster Survey 2006, Kazakhstan, United Nations Children’s Fund (UNICEF). Bishkek, Kyrgyz Republic: (2007). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS3/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Kazakhstan/2006/Final/Kazakhstan%202006%20MICS_English.pdf [Google Scholar]
- 85.National Statistical Service [Armenia], Ministry of Health [Armenia], and ORC Macro. Armenia Demographic and Health Survey 2000. Calverton, MD: National Statistical Service, Ministry of Health and ORC Macro; (2001). Available from: https://dhsprogram.com/pubs/pdf/FR126/FR126.pdf [Google Scholar]
- 86.National Statistical Service [Armenia], Ministry of Health [Armenia], and ORC Macro. Armenia Demographic and Health Survey 2005. Calverton, MD: National Statistical Service, Ministry of Health, and ORC Macro; (2006). Available from: https://dhsprogram.com/pubs/pdf/FR184/FR184.pdf [Google Scholar]
- 87.Directorate for Economic Planning, Ministry of Health and Social Welfare, Ministry of Health of the Federation of Bosnia and Herzegovina. Bosnia and Herzegovina Multiple Indicator Cluster Survey 2006, Final Report. Sarajevo, Bosnia and Herzegovina: (2008). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS3/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Bosnia%20and%20Herzegovina/2006/Final/Bosnia%20and%20Herzegovina%202006%20MICS_English.pdf [Google Scholar]
- 88.Bosnia and Herzegovina Agency for Statistics. Bosnia and Herzegovina Multiple Indicator Cluster Survey 2000, Final Report. Sarajevo, Bosnia and Herzegovina: (2002). Available from: http://mics.unicef.org/surveys [Google Scholar]
- 89.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (2014) 384(9945):766–81. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Frenken F. Statistics Netherlands. Health Interview Survey 1981–2006. Herleen, the Netherlands: (2007). [Google Scholar]
- 91.Wijnhoven TM, van Raaij JM, Spinelli A, Starc G, Hassapidou M, Spiroski I, et al. WHO European Childhood Obesity Surveillance Initiative: body mass index and level of overweight among 6-9-year-old children from school year 2007/2008 to school year 2009/2010. BMC Public Health (2014) 14:806. 10.1186/1471-2458-14-806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Roberts C, Freeman J, Samdal O, Schnohr CW, de Looze ME, Nic Gabhainn S, et al. The health behaviour in school-aged children (HBSC) study: methodological developments and current tensions. Int J Public Health (2009) 54(2):140. 10.1007/s00038-009-5405-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nutrionnelle udsede. Etude national nutrition santé (ENNS, 2006). St. Maurice: Institute de veille sanitaire, Universite de Paris 13, and métiers; (2007). [Google Scholar]
- 94.Statistical Agency under the President of the Republic of Tajikistan (SA), Ministry of Health [Tajikistan], and ICF International. Tajikistan Demographic and Health Survey 2012. Dushanbe, Tajikistan, and Calverton, MD, USA: SA, MOH, and ICF International; (2013). Available from: https://dhsprogram.com/pubs/pdf/FR279/FR279.pdf [Google Scholar]
- 95.National Centre of Public Health of the Ministry of Health of the Republic of Moldova, United Nations Children’s Fund (UNICEf). Republic of Moldova Multiple Indicator Cluster Survey 2012: Final Report (MICS4). Chisinau, Republic of Moldova: (2014). Available from: https://www.unicef.org/moldova/2012_Moldova_MICS_FINAL_EN.1(1).pdf [Google Scholar]
- 96.Analytical and Information Center, Ministry of Health of the Republic of Uzbekistan, State Department of Statistics, Ministry of Macroeconomics and Statistics [Uzbekistan], and ORC Macro. Uzbekistan Health Examination Survey 2002. Demographic and Health Surveys. Calverton, MD, USA: Analytical and Information Center, State Department of Statistics, and ORC Macro; (2004). Available from: https://dhsprogram.com/pubs/pdf/FR143/FR143.pdf [Google Scholar]
- 97.Albanian National Institute of Statistics. Albania Multiple Indicator Cluster Survey 2005, Final Report. Tirana, Albania: Albanian National Institute of Statistics; (2007). Available from: http://mics.unicef.org/surveys [Google Scholar]
- 98.Albanian National Institute of Statistics. Albania Multiple Indicator Cluster Survey 2000, Final Report. Tirana, Albania: Albanian National Institute of Statistics; (2002). Available from: http://mics.unicef.org/surveys [Google Scholar]
- 99.United Nations Children’s Fund (UNICEF). Azerbaijan Multiple Indicator Cluster Survey 2000 Final Report. Baku, Azerbaijan: UNICEF; (2002). Available from: http://mics.unicef.org/surveys [Google Scholar]
- 100.Multiple Indicator Cluster Survey 2006, Kyrgyz Republic. Final Report. National Statistical Committee of the Kyrgyz Republic. United Nations Children’s Fund. (2007). Kyrgyzstan, Bishkek: Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS3/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Kyrgyzstan/2005-2006/Final/Kyrgyzstan%202005-06%20MICS_English.pdf [Google Scholar]
- 101.Statistical Office of Montenegro (MONSTAT) and UNICEF. 2013 Montenegro Multiple Indicator Cluster Survey and 2013 Montenegro Roma Settlements Multiple Indicator Cluster Survey, Final Report. Podgorica, Montenegro: Statistical Office of Montenegro (MONSTAT) and UNICEF; (2014). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS5/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Montenegro/2013/Final/Montenegro%20%28National%20and%20Roma%20Settlements%29%202013%20MICS_English.pdf [Google Scholar]
- 102.Statistical Office of the Republic of Serbia and Strategic Marketing Research Agency. Republic of Serbia Multiple Indicator Cluster Survey 2005, Final Report. Belgrade, Republic of Serbia: Statistical Office of the Republic of Serbia; (2006). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS3/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Serbia/2005-2006/Final/Serbia%202005-06%20MICS_English.pdf [Google Scholar]
- 103.Hacettepe University Institute of Population Studies, Turkey Demographic and Health Survey. Hacettepe University Institute of Population Studies, Ministry of Health General Directorate of Mother and Child Health and Family Planning, State Planning Organization and European Union. Ankara, Turkey: (2003). Available from: https://dhsprogram.com/pubs/pdf/FR160/FR160.pdf [Google Scholar]
- 104.Statistical Office of the Republic of Macedonia. Republic of Macedonia Multiple Indicator Cluster Survey 2005-2006, Final Report. Skopje, Republic of Macedonia: Statistical Office of the Republic of Macedonia; (2006). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS3/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Macedonia%2C%20The%20Former%20Yugoslav%20Republic%20of/2005-2006/Final/Macedonia%202005%20MICS_English.pdf [Google Scholar]
- 105.Statistical Office of the Republic of Serbia. Serbia Multiple Indicator Cluster Survey 2010. Belgrade, Republic of Serbia: Statistical Office of the Republic of Serbia; (2011). Available from: https://mics-surveys-prod.s3.amazonaws.com/MICS4/Central%20and%20Eastern%20Europe%20and%20the%20Commonwealth%20of%20Independent%20States/Serbia/2010/Final/Serbia%202010%20MICS_English.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data used in this paper is all currently publicly available online in journal articles and/or published results from surveys, and full references are provided.