Abstract
Aim
Central venous access is frequently provided by way of umbilical venous catheter placement in critically ill newborns. This study compared the methods of Dunn, Shukla-Ferrara, and Revised Shukla-Ferrara in determining the appropriate insertion length of umbilical vein catheters.
Material and Methods
This prospective observational study was carried out in 121 newborns with umbilical venous catheter, group 1 (n=41) used Dunn method, group 2 (n=40) used the Shukla-Ferrara formula, and group 3 used revised Shukla-Ferrara formula (n=40). Catheter tip position was evaluated with an anterior-posterior chest radiograph after insertion of the umbilical venous catheter. The ideal position for the umbilical venous catheter was defined as the catheter tip being visible between the 9th and 10th thoracic vertebrae on an anterior-posterior chest radiograph. The position of the umbilical venous catheter was considered too high if the tip of the catheter was higher than the 9th thoracic vertebra and too low if the tip was below the 10th thoracic vertebra. The following data were collected: appropriate, inappropriate (low, high) placement, and complications of umbilical venous catheterization.
Results
In the Shukla-Ferrara group, 53% (17/32) of umbilical venous catheters were placed directly in the appropriate position, compared with 40% (12/30) in the revised Shukla-Ferrara group and 38% (11/29) in the Dunn method group. Umbilical venous catheter-related complications developed in two patients, thrombus in one, and catheter-related blood stream infection in the other.
Conclusions
This study showed that the Shukla-Ferrara formula is more accurate in predicting the insertion length for umbilical venous catheters, though statistical significance was not found. Further studies with larger samples are needed on this topic.
Keywords: Catheter, umbilical vein, newborn
Introduction
Insertion of umbilical venous catheters in newborns hospitalized in neonatal intensive care units (NICU) who are preterm or have severe morbidity is a commonly used method with different objectives, including maintenenace of fluid support and administration of blood products, parenteral nutrition, administration of intravenous therapies, exchange transfusion and investigations, as well as providing emergency intravenous access (1–3). There is no definite rule related with how far umbilical catheters should be inserted in the umbilical vein; different methods including the Dunn method, Shukla-Ferrara, and modified Shukla-Ferrara formula are used (4–6). Selection of the most correct and feasible among these methods is very important in terms of decreasing the risk and frequency of complications. In the literature, no studies have compared all three methods in determining how far umbilical catheters should be inserted in the umbilical vein (6, 7).
In this prospective study, we aimed to compare the efficiencies of the Dunn method, Shukla-Ferrara, and modified Shukla formulas, which are used to determine how far umbilical catheters should be inserted in the umbilical vein, and to determine the most appropriate method by this way.
Material and Methods
This prospective and observational study was conducted in Karadeniz Technical University, Faculty of Medicine, Department of Pediatrics, Division of Neonatology between January 2015 and December 2015 after ethics committee approval was obtained (File number: 2015/3 24237859, Number: 152). Written informed consent was obtained from the parents of the patients who were included in the study.
Patients who were given intravenous fluid and parenteral nutrition because of unstable condition, received intravenous medications, those who were going to undergo exchange transfusion because of hyperbilirubinemia, and patients who needed to receive blood products were included in the study.
Patients who had abdominal wall defects including omphalitis, omphalocele, gastroschisis, and patent urachus, severe problems including peritonitis, necrotizing enterocolitis, hydrops fetalis, and significant congential anomalies, and those in whom catheters were inadvertently placed in the umbilical artery instead of the umbilical vein were not included in the study.
The patients were assigned to one of the three groups according to the sequence of presentation [(group 1: Dunn method), (group 2: Shukla-Ferrara formula) and (group 3: modified Shukla-Ferrara formula)] and umbilical vein catheters were placed.
In patients for whom a Dunn nomogram was used, the insertion length of catheter inside the umbilical vein was determined by reading the equivalent value obtained by measuring the shoulder-umbilical length on the Dunn normogram (4). In the patients for whom the Shukla-Ferrara formula was used, the insertion length was calculated using the following formula : [(Birth weight x 3 + 9)/2+1] (5). In patients for whom the modified Shukla-Ferrara formula was used, the insertion length of catheter was calculated using the following formula: [(Birth weight x 3 + 9)/2] (6).
The patients were divided into subgroups according to birth weight (2500 g and ≥2500 g), gestational age (≤32 weeks and >32 weeks) and appropriateness of birth weight for gestational age (AGA) or small for gestational age (SGA).
The diagnosis of catheter-related sepsis (CRS) was made according to the diagnostic criteria specified by the Centers for Disease Control (CDC) (8).
According to the body weights of the patients, a 3.5-F umbilical vein catheter was used in patients who weighed below 1500 g and a 5-F single lumen umbilical vein catheter (Vygon, France) was used in patients who weighed ≥1500 g. The positions of placement of the catheters were specified with an anterior-posterior chest radiograph.
The position of placement of the catheters, which proceeded along the vertebral column and were specified with anterior-posterior chest radiograph, was considered appropriate when it was between the 9th and 10th thoracic vertebrae (T9–10), “too high” when it was above T9 and “too low” when it was below T10 (6, 7). Catheters that directed to the portal or splenic veins were defined as having an abnormal position. All radiographs were assessed by the same radiologist.
In cases where the umiblical venous catheter tip could not be advanced along the thoracic vertebra, a second attempt was made by inserting a second catheter alongside the first catheter. Catheters that had appropritate position were removed immediately if any complication developed, and after 14 days of use if no complication developed. Regular care of the catheters was made throughout the dwell period.
The gestational ages, sex, weight, height and head circumference values, mode of delivery, weight by gestational age, reasons for hospitalization, reasons for placement of umbilical venous catheter, number of successful trials, and the catheter position were recorded. The patients were followed up in terms of complications and the distribution of mortality rates by groups was specified.
Ultrasonography (USG) and Doppler USG were performed weekly during the catheter dwell period, 72 hours after the catheter was removed, and on the 15th day in all patients in order to determine potential complications. In patients in whom thrombus was found at any stage, USG and Doppler USG were performed weekly until the thrombus was dissolved.
Statistical analysis
Analyses of the data were performed using the Statistical Package for the Social Sciences version 23.0 (SPSS IBM, Armonk, NY, USA) program. Continuous variables were expressed as mean ± standard deviaiton and qualitative data were expressed as numbers and percentages. Pearson’s Chi-square test was used to compare the qualitative data of the groups. The one-sample Kolmogorov-Smirnov test was used to measure the compatibility of the continuous data to normal distribution. In the comparison of the measurable data between three independent groups, ANOVA was used when the data were compatible with normal distribution and the Kruskal-Wallis test was used when data were not compatible with normal distribution. P values <0.05 were considered statistically significant.
Results
Umblical venous catheter was placed in a total of 121 patients including 41 patients in group 1 (Dunn method), 40 patients in group 2 (Shukla-Ferrara formula) and 40 patients in group 3 (modified Shukla-Ferrara formula). The birth weight values of the patients ranged between 390 g and 4500 g and the gestational ages ranged between 22 weeks and 41 weeks. Sixty-four percent of these patients (n=77) were preterm babies. No statistically significant difference was found between the groups in terms of demographic characteristicss including sex, mode of delivery, gestational age, birth weight, height, head circumference, and weight by gestational age (p>0.05) (Table 1).
Table 1.
Distribution of the demographic characteristics of the newborns by groups
| Demographic characteristics | Group 1 (n=41) | Group 2 (n=40) | Group 3 (n=40) | p |
|---|---|---|---|---|
| Gender | ||||
| Male [n (%)]a | 22 (53.7) | 17 (42.5) | 19 (47.5) | >0.05 |
| Female [n (%)]a | 19 (46.3) | 23 (57.5) | 21 (52.5) | |
| Mode of delivery | ||||
| C/S [n (%)]a | 8 (19.5) | 9 (22.5) | 7 (17.5) | >0.05 |
| NSVD [n (%)]a | 33 (80.5) | 31 (77.5) | 33 (82.5) | |
| Birth weight (g)b [Mean± SD (min–max)] | 2 239±984 (500–4 070) | 2 003±1 034 (390–3 780) | 2 189±1 123 (580–4 500) | >0.05 |
| ≥2500 g [n (%)] | 19 (46.4) | 15 (37.5) | 16 (40) | |
| 1 500–2499 g [n (%)] | 10 (24.4) | 10 (25) | 10 (25) | |
| 1 000–1499 g [n (%)] | 8 (19.5) | 6 (15) | 5 (12.5) | |
| 750–999 g [n (%)] | 2 (4.9) | 2 (5) | 6 (15) | |
| <750 g [n (%)] | 2 (4.9) | 7 (17.5) | 3 (7.5) | |
| Birth height (cm)b [mean ± SD (min–max)] | 44.6±6.2 (27–51) | 41.5±7.5 (27–51) | 43.3±7.7 (29–52) | >0.05 |
| Head circumference at birth (cm)c [Mean± SD (min–max)] | 32.4±3.4 (23–37) | 30.3±5.2 (20–36) | 31.2±4.5 (22–36) | >0.05 |
| Gestational age (weeks)c [Mean± SD (min–max)] | 34.1±4.7 (24–40) | 32.6±5.0 (23–41) | 33.5±4.8 (22–41) | >0.05 |
| ≥37 weeks [n (%)] | 18 (43.9) | 11 (27.5) | 15 (37.5) | |
| 32–36 weeks [n (%)] | 11 (26.8) | 12 (30) | 13 (32.5) | |
| 28–32 weeks [n (%)] | 7 (17.1) | 10 (25) | 7 (17.5) | |
| <28 weeks [n (%)] | 5 (12.2) | 7 (17.5) | 5 (12.5) | |
| Weight by gestational agea | ||||
| AGA [n (%)] | 1 (2.5) | 1 (2.5) | 2 (5) | |
| SGA [n (%)] | 24 (58.5) | 24 (60) | 23 (57.5) | >0.05 |
| SGA [n (%)] | 16 (39) | 15 (37.5) | 15 (37.5) | |
| Asymmetricala | 9 | 8 | 7 | >0.05 |
| Symmetricala | 7 | 7 | 8 | |
Pearson’s Chi-square;
ANOVA;
Kruskal-Wallis;
AGA: baby with a birth weight by gestational week between the 10th and 90th percentile; C/S: cesarean section; NSVD: normal spontaneous vaginal delivery; SGA: baby with a birth weight by gestational age below the 10th percentile
The reasons for hospitalization in the patients in order of frequency included respiratory tract problems (n=73, 60%), neurologic problems (n=19, 16%), high glucose requirement because of undernutrition and/or hypoglycemia (n=12, 10%), requirement for exchange transfusion or intravenous immunoglobulin because of hyperbilirubinemia (n=10, 8%), congenital heart disease (n=5, 4%), and neonatal sepsis (n=2, 2%).
The umbilical venous catheter tip advanced along the thoracic vertebra at the first attempt in 66% of patients (80/121) and showed abnormal position in the other patients. In these patients, a second trial was attempted by inserting a second catheter next to the first catheter. In this way, advancement of the catheter was enabled along the thoracic vertebra in 11 (27%) of 41 patients in whom abnormal position was observed (two patients in group 1, four patients in group 2, and five patients in group 3). When all patients were evaluated together in terms of catheter tip position, it was found that the umbilical catheter tip advanced along the vertebral column in 91 patients and showed abnormal position in 30 patients (Table 2). When the patients in whom the catheter tip advanced along the vertebral column and patients with abnormal positioning were compared in terms of demographic characteristics, no statistically significant difference was found (p>0.05).
Table 2.
The rates of advancement along the thoracic vertebrae and abnormal positioning of the catheter tips on the first two trials: distribution by groups
| Group 1 (n=41) n % |
Group 2 (n=40) n % |
Group 3 (n=40) n % |
Total (n=121) | p | |
|---|---|---|---|---|---|
| Cases with advancement along the vertebral columna | 29 (71) | 32 (80) | 30 (75) | 91 (75) | 0.474 |
| 1st trial | 27 (93) | 28 (88) | 25 (83) | 80 (88) | |
| 2nd trial | 2 (7) | 4 (12) | 5 (17) | 11 (12) | |
| Abnormal positiona | 12 (29) | 8 (20) | 10 (25) | 30 (25) | |
| Portal vein | 11 (92) | 8 (100) | 10 (100) | 29 (97) | |
| Splenic vein | 1 (8) | 0 | 0 | 1 (3) |
Pearson’s Chi-square test
The catheter tip was placed in an appropriate position in 40 (44%) of 91 patients whose umbilical venous catheter tips advanced along the vertebral column and positioned “too low” or “too high” in 51 (56%) patients. No significant difference was found between the three groups in terms of appropriate and inappropriate positions (p>0.05). The distribution of positions of umbilical venous catheter tips that advanced along the vertebral column by groups is shown in Table 3 and its graphic is shown in Figure 1.
Table 3.
Positions of the umbilical catheter tips that advanced along the vertebral column: distribution by groups
| Catheter position | Group 1 (n=29) n % |
Group 2 (n=32) n % |
Group 3 (n=30) n % |
Total (n=91) | p |
|---|---|---|---|---|---|
| Appropriate positiona | 11 (38) | 17 (53) | 12 (40) | 40 (44) | 0,425 |
| Inappropriate positiona | 18 (62) | 15 (47) | 18 (60) | 51 (56) | |
| Low position [n (%)] | 3 (17) | 1 (7) | 6 (33) | 10 (20) | |
| High position [n (%)] | 15 (83) | 14 (93) | 12 (67) | 41 (80) |
Pearson’s Chi-square test, percentages express column percentages
Figure 1.
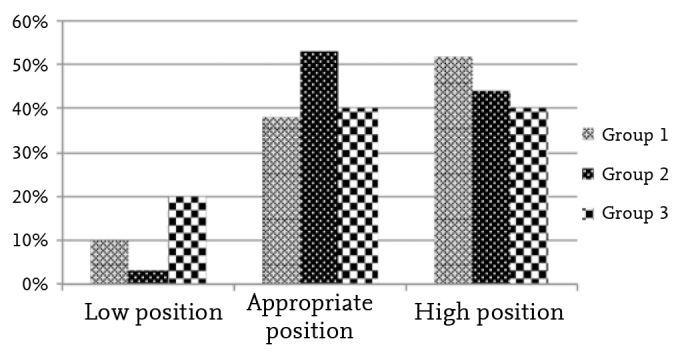
Distribution of the rates of low, appropriate, and high positions of the umblical venous catheters that advanced along the vertebral column
The rates of reaching the T9–10 vertebrae level, which is the ideal position for catheter tip, were as follows: 53% in group 2 (n=17), 40% in group 3 (n=12), and 38% in group 1 (n= 11), respectively. A “too high” position was found most frequently in group 1 (52%) and a “too low” position was found most frequently in group 3 (20%).
In 91 patients in whom the umbilical venous catheter tip advanced along the thoracic vertebra, the catheter tip was positioned between T2 and T12. The median vertebra level at which the umbilical venous cathater tip adavanced along the vertebral column and positioned was T8 (T6–12) in group 1, T9 (T2–11) in group 2, and T9 (T6–12) in group 3; no statistically significant difference was found between the groups (p>0.05). The distribution of throacic vertebra levels of catheter tips that advanced along the thoracic vertebra in anterior-posterior chest ragiographs by groups is shown in Figure 2.
Figure 2.
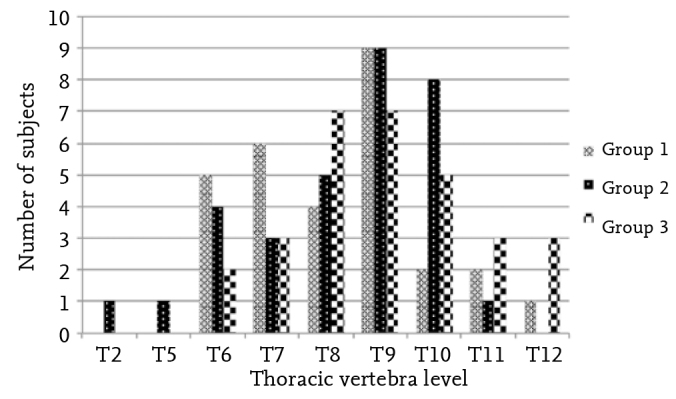
Thoracic vertebra levels of the umbilical venous catheter tips on anterior-posterior radiograph: distribution by groups
When the demographic characteristics of the patients whose umbilical venous catheter tips showed appropriate and inappropirate positions were compared, no statistically significant difference was found (p>0.05).
The mean time of placement of umbilical venous catheters was found as 7.6±4.4 (range,1–14) days; no statistically significant difference was found between the groups (p>0.05).
When the patients were examined in terms of complications, a patient in group 3 developed CRS caused by Staphylococcus epidermidis, and a patient in group 2 developed thrombus in the region where the left hepatic vein drains into vena cava inferior. Low-molecular-weight heparin treatment was administered in the patient in whom thrombus was found and the thrombus disappeared in the weekly USG and Doppler USG follow-up. The catheter of the patient who developed catheter-related sepsis was removed, appropriate antibiotic treatment was arranged, and the patient recovered.
Catheter-related mortality was not observed in any patients in the present study. The mortality rate related with primary morbidity was found as 24% in group 1 (10 patients), 35% in group 2 (14 patients), and 20% in group 3 (8 patients).
Discussion
The umbilical vein is frequently used to provide central venous access in newborns. The most appropriate position for an umbilical venous catheter tip position is considered as the junction of the inferior vena cava and right atrium (6, 7, 9–11). This regions corresponds to the T9–10 range on anterior-posterior chest radiographs. Ideally, umbilical venous catheters are placed under guidance of imaging methods. However, umbilical venous catheters are placed without accompaniment of any imaging method in emergency cases in NICUs. This leads to frequent occurrence of inappropriate positioning. It has been reported that placement of umbilical venous catheter under USG guidance or echocardiography is more sensitive compared with radiography in terms of prevention of complications related with abnormal positioning and reduces exposure to ionizing radiation (11, 12).
Although the literature contains studies that compared the Dunn method with the Shukla-Ferrara formula, and Shukla-Ferrara formula with modified Shukla-Ferrara formula, no study has compared the three methods together (6, 7). In our study, the three methods were compared together. A Comparison of the positions of the umbilical venous catheter tips advanced along the vertebral column is shown in Table 4.
Table 4.
Comparison of the positions of the umbilical venous catheter tips with the literature
| Shukla-Ferrara | Modified Shukla-Ferrara | Dunn | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| Y n (%) |
U n (%) |
A n (%) |
Y n (%) |
U n (%) |
A n (%) |
Y n (%) |
U n (%) |
A n (%) |
||
| Verheij (2010)(7) | n=153 | 63/84 (75) | 20/84 (24) | 1/84 (1) | 39/69 (56) | 28/69 (41) | 2/69 (3) | |||
| Verheij (2013)(6) | n=185 | 68/93 (73) | 24/93 (26) | 1/93 (1) | 50/92 (54) | 40/92 (44) | 2/92 (2) | |||
| Our study | n=91 | 14/32 (44) | 17/32 (53) | 1/32 (3) | 12/30 (40) | 12/30 (40) | 6/30 (20) | 15/29 (52) | 11/29 (38) | 3/29 (10) |
A: Low position; U: Appropriate position; Y: High position
In the study conducted by Verheij et al. (7) in 2010, the rate of appropriate positioning was found as 41% (28/69) in patients in whom catheter placement was performed using the Dunn formula, and 24% (20/84) in patients in whom catheter placement was performed using the Shukla-Ferrara formula. In another study in which the Shukla-Ferrara formula and the modified Shukla-Ferrara formula were compared, the rate of appropriate positioning was 26% (24/93) in the Shukla-Ferrara group and 43% (40/92) in the modified Shukla-Ferrara formula group (6). In both studies, the appropriate position was considered the T9–10 vertebral range, similar to our study. In our study, the rate of appropriate positioning was 38% (11/29) in the Dunn group, 53% (17/53) in the Shukla-Ferrara group, and 40% (12/30) in the modified Shukla-Ferra group; no statistically significant difference was found between the three groups in terms of appropriate positioning of the catheter tip. In contrast to these two studies, a high rate of appropriate positioning was found in the Shukla-Ferrara group in our study.
In two different studies conducted by Verheij et al. (6, 7) in 2010 and 2013, a “too high” position was found with a higher rate in the Shukla-Ferrara group [75% (63/84), 73% (68/93) respectively]. In our study, the highest rate for a “too high” position was found in the Dunn group [52% (15/29)]. In a study conducted by Verheij et al. (7) in 2010, the rate of a “too low” position was reported at a rate of 3% (2/69) in the Dunn group, and 1% (1/84) in the Shukla-Ferrara group. In another study conducted by the same investigators in 2013, the rate of “too low” positions was reported as 1% (1/93) in the Shukla-Ferrara group and 2% (2/92) in the modified Shukla-Ferrara group (6). In that study, the investigators reported that the modified Shukla-Ferrara formula enabled a higher rate of umbilical venous catheterization with appropriate positioning by reducing the rate of “too high” positions without causing a “too low” position (6). In our study, a higher rate of “too low” positions [20 % (6/30)] was observed in patients in whom umbilical venous catheters were placed using the modified Shukla-Ferrara formula. In our study, no statistically significant difference was found when the catheters placed using the three diffirent methods were compared with each other in terms of appropriate and inappropriate (too high and too low position) positions.
In asymmetric SGA patients in whom umbilical venous catheter has been placed using the modified Shukla-Ferrara formula and Shukla-Ferrara formula, which especially consider birth weight, higher rates of “too low” positions may be expected because the birth weight is in the lower percentiles compared with the height and head circumference values. However, a statistically significant difference was not found between the three groups in this aspect. This may be related with the low numbers of patients. Therefore, studies with larger series are needed.
In a study in which the Shukla-Ferrara formula and modified Shukla-Ferrara Formula were compared, umbilical venous catheter tips were observed between T4 and T11 on anterior-posterior chest radiographs; the median value was found as T7 (T6–T9) in the Shukla-Ferrara group and T8 (T7–T9) in the modified Shukla-Ferrara group (6). In our study, the catheter tips were observed to be between T2 and T12 on anterior-posterior chest radiographs; the median value was found as T8 in the Dunn group and T9 in the Shukla-Ferrara and modified Shukla-Ferrara groups.
In a study in which the Dunn method and Shukla-Ferrara formula were compared, the catheter could be advanced along the vertebral column with a rate of 32% (6/19) in the Dunn group and 16% (4/25) in the Shukla-Ferrara formula group in second trials when a second catheter was inserted next to the first catheter when the first catheter could not be advanced along the thoracic vertebra and showed an abnormal position (7). In our study, the umbilical venous catheter could be advanced along the vertebral column in the second trial in 2 (14%) of 14 patients in the Dunn group, 4 (33%) of 12 patients in the Shukla-Ferrara formula group, and 5 (33%) of 15 patients in the modified Shukla-Ferrara formula group.
The demographic characteristics of the patients were also evaluated because the formulas that have been developed to enable appropriate positioning of umbilical venous catheters are generally based on birth weight. However, no statistically significant difference was found in terms of demographic characteristics in our study, similar to other studies in the literature (6, 7).
In a study in which the Shukla Ferrara fromula and modified Shukla Ferrara formula were compared, a “too high” position was observed with a rate of 68% (25/37) in patients with a gestational age below 28 weeks, whereas this rate was 63% (93/128) in patients with a gestational age of 28 weeks and over among patients whose umbilical venous catheters could be advanced along the vertebral column, but showed inappropriate position (too low or too high) (6). When our study was evaluated in this aspect, a “too high” positon was found with a rate of 89% (8/9) in patients with a gestational age below 28 weeks and at 79% (33/42) in patients with a gestational age of 28 weeks and over. When the studies included in the literature were evaluated together with our study, it was concluded that the rate of a “too high” positions increased as the gestational age decreased. This may be related with accidental advancement of the catheter 0.5–1 cm further during application.
In addition to the benefits of umbilical venous catheters, there are also life-threatening complications including inappropriate positioning of catheter, CRS, portal vein thrombosis, vascular injury, hepatic injury and necrosis, subcapsular hematoma or abscess in the liver, hemorrhagic infarction in the lung, arrythmia, thrombotic endocarditis, myocardial perforation, pleural and pericardial effusion, and cardiac tamponade (3, 9, 13, 14). Most cardiac complications were reported with catheters positioned “too high,” and most hepatic complications were reported with catheters positioned “too low” (14). The complications of abnormal positioning, thrombus, and CRS were found in our study.
Abnormal positioning of umbilical venous catheter is one of the common complications. Mutlu et al. (14) reported the rate of abnormal positioning of umbilical venous catheters as 14% (27/189). In our study, this rate was 25% (30/121). A higher rate of abnormal positioning was found in the Dunn method group compared with the other two groups.
No cardiac complications were observed in our study. It was thought that the most important factor here was the fact that the position was checked with anterior-posteiror chest radiography immediately after the catheter was placed, and intervention to the catheter was performed in cases where inappropriate positioning was found. In our study, catheters that were positioned “too low” were replaced and the ones that were positioned “too high” were attempted to be repositioned appropriately by pulling the catheter back considering the extra distance specified on the radiograph.
The frequency of thrombosis related with central venous catheter has been reported as 9.2% (15). Thrombi generally occur in the hepatic system, ductus venosus, inside the right atrium, and inside the superior or inferior vena cava (15–19). In our study, thrombus was found in the region where the left hepatic vein drains into the vena cava inferior in only one patient. In many previous studies, it was reported that clinical findings were absent in patients with thrombus. This may be related with the fact that presence of thrombus was found on USGs performed with the objective of monitoring before symptoms occured (15). It is recommended that patients with persistent thrombocytopenia and impaired distal circulation should be evaluated in terms of thrombus (15). In our study, thrombus was observed in one patient on USG, which was performed with the objective of screening. It has been reported that the risk of thrombus increases in cases where the catheter stays in its place for more than six days, in cases where blood products are administered by way of the catheter, and in cases where catheters have been positioned inappropriately (18, 19). In our patient, the catheter stayed in place for eight days and blood product was given once during this time peirod. Low-molecular-weight heparin treatment was given to our patient. The thrombus disappeared at the end of the first month in weekly Doppler USG follow-up.
Catheter-related sepsis is one of the most common complications observed with a frequency ranging between 0% and 29% (20, 21). The most common organisms that lead to infection include coagulase-negative staphylococci (especially Staphylococcus epidermidis), Staphylococcus aureus, Enterococcus spp., Escherichia coli, Klebsiella spp., other enteric Gram (-) bacteriae and Candida spp. (22). In our study, CRS was found in only one (3%) patient. In addition to the clincial findings of sepsis, Staphylococcus epidermidis was grown in cultures obtained simultaneously from the peripheral blood and catheter. The patient recovered with removal of the catheter and appropriate antibiotic treatment.
It has been reported that removal of central venous catheters inserted in peripheral veins or umbilical venous catheters after a period of 14 days does not lead to an increased risk of complications (23). In our study, catheters were kept in place for 14 days at the most.
The limitation of our study was the fact that the numbers of patients assigned to the groups was insufficient because the number of patients included in the study was low.
In conclusion, there is no consensus in the literature about the most efficient method to be used for appropriate positioning of umbilical venous catheters in patients who are hospitalized in the NICU. We found that the Shukla-Ferrara formula gave more accurate results, albeit statistically insignificant. It was concluded that studies with higher numbers of patients are needed to make a definite judgement on this subject. It is important to confirm the catheter position and avoid a dwell period longer than 14 days to prevent umbilical venous catheter-related complications.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from Karadeniz Technical University School of Medicine.
Informed Consent: Written informed consent was obtained from patient parents who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - M.M., Y.A.; Design - M.M., Y.A., B.P.K., İ.E., Ş.K., F.A.A.; Supervision - M.M., Y.A.; Funding - M.M., Y.A., B.P.K., İ.E., Ş.K., F.A.A.; Materials - M.M., Y.A.; Data Collection and/or Processing - M.M., Y.A., B.P.K., İ.E., Ş.K., F.A.A.; Analysis and/or Interpretation - M.M., Y.A., İ.E.; Literature Review - M.M., Y.A., B.P.K.; Writing - M.M., Y.A., B.P.K.; Critical Review - Y.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
Kaynaklar
- 1.Gupta AO, Peesay MR, Ramasethu J. Simple measurements to place umbilical catheters using surface anatomy. J Perinatol. 2015;35:476–80. doi: 10.1038/jp.2014.239. https://doi.org/10.1038/jp.2014.239. [DOI] [PubMed] [Google Scholar]
- 2.Tiffany KF, Burke BL, Collins-Odoms C, Oelberg DG. Current practice regarding the enteral feeding of high-risk newborns with umbilical catheters in situ. Pediatrics. 2003;112:20–3. doi: 10.1542/peds.112.1.20. https://doi.org/10.1542/peds.112.1.20. [DOI] [PubMed] [Google Scholar]
- 3.Nash P. Umbilical catheters, placement, and complication management. J Infus Nurs. 2006;29:346–52. doi: 10.1097/00129804-200611000-00005. https://doi.org/10.1097/00129804-200611000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Dunn PM. Localization of the umbilical catheter by postmortem measurement. Arch Dis Child. 1966;41:69–7. doi: 10.1136/adc.41.215.69. https://doi.org/10.1136/adc.41.215.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shukla H, Ferrara A. Rapid estimation of insertional length of umbilical catheters in newborns. Am J Dis Child. 1986;140:786–8. doi: 10.1001/archpedi.1986.02140220068034. https://doi.org/10.1001/archpedi.1986.02140220068034. [DOI] [PubMed] [Google Scholar]
- 6.Verheij GH, te Pas AB, Smits-Wintjens VE, Šràmek A, Walther FJ, Lopriore E. Revised formula to determine the insertion length of umbilical vein catheters. Eur J Pediatr. 2013;172:1011–5. doi: 10.1007/s00431-013-1981-z. https://doi.org/10.1007/s00431-013-1981-z. [DOI] [PubMed] [Google Scholar]
- 7.Verheij GH, Te Pas AB, Witlox RS, Smits-Wintjens VE, Walther FJ, Lopriore E. Poor accuracy of methods currently used to determine umbilical catheter insertion length. Int J Pediatr. 2010;2010:873167. doi: 10.1155/2010/873167. https://doi.org/10.1155/2010/873167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CDC. Guidelines for the prevention of intravascular catheter-related infections. 2011. [Internet]. Available from: URL: https://www.cdc.gov/hicpac/BSI/04-bsibackground-info-2011.html. [DOI] [PMC free article] [PubMed]
- 9.Hermansen MC, Hermansen MG. Intravascular catheter complications in the neonatal intensive care unit. Clin Perinatol. 2005;32:141–56. doi: 10.1016/j.clp.2004.11.005. https://doi.org/10.1016/j.clp.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Hogan MJ. Neonatal vascular catheters and their complications. Radiol Clin North Am. 1999;37:1109–25. doi: 10.1016/s0033-8389(05)70252-9. https://doi.org/10.1016/S0033-8389(05)70252-9. [DOI] [PubMed] [Google Scholar]
- 11.Greenberg M, Movahed H, Peterson B, Bejar R. Placement of umbilical venous catheters with use of bedside real-time ultrasonography. J Pediatr. 1995;126:633–5. doi: 10.1016/s0022-3476(95)70366-7. https://doi.org/10.1016/S0022-3476(95)70366-7. [DOI] [PubMed] [Google Scholar]
- 12.Ades A, Sable C, Cummings S, Cross R, Markle B, Martin G. Echocardiographic evaluation of umbilical venous catheter placement. J Perinatol. 2003;23:24–8. doi: 10.1038/sj.jp.7210851. https://doi.org/10.1038/sj.jp.7210851. [DOI] [PubMed] [Google Scholar]
- 13.Moens E, Dooy JD, Jansens H, Lammens C, Op de Beeck B, Mahieu L. Hepatic abscesses associated with umbilical catheterisation in two neonates. Eur J Pediatr. 2003;162:406–9. doi: 10.1007/s00431-003-1178-y. [DOI] [PubMed] [Google Scholar]
- 14.Mutlu M, Aslan Y, Kul S, Yılmaz G. Umbilical venous catheter complications in newborns: a 6-year single-center experience. J Matern Fetal Neonatal Med. 2016;29:2817–22. doi: 10.3109/14767058.2015.1105952. [DOI] [PubMed] [Google Scholar]
- 15.Park CK, Paes BA, Nagel K, Chan AK, Murthy P. Neonatal central venous catheter thrombosis: diagnosis, management and outcome. Blood Coagul Fibrinolysis. 2014;25:97–106. doi: 10.1097/MBC.0b013e328364f9b0. https://doi.org/10.1097/MBC.0b013e328364f9b0. [DOI] [PubMed] [Google Scholar]
- 16.Butler-O’Hara M, Buzzard CJ, Reubens L, McDermott MP, DiGrazio W, D’Angio CT. A randomized trial comparing long-term and short-term use of umbilical venous catheters in premature infants with birth weights of less than 1251 grams. Pediatrics. 2006;118:25–35. doi: 10.1542/peds.2005-1880. https://doi.org/10.1542/peds.2005-1880. [DOI] [PubMed] [Google Scholar]
- 17.Roy M, Turner-Gomes S, Gill G, Way C, Mernagh J, Schmidt B. Accuracy of doppler echocardiography for the diagnosis of thrombosis associated with umbilical venous catheters. J Pediatr. 2002;140:131–4. doi: 10.1067/mpd.2002.119591. https://doi.org/10.1067/mpd.2002.119591. [DOI] [PubMed] [Google Scholar]
- 18.Kim JH, Lee YS, Kim SH, Lee SK, Lim MK, Kim HS. Does umbilical vein catheterization lead to portal venous thrombosis? Prospective US evaluation in 100 neonates. Radiology. 2001;219:645–50. doi: 10.1148/radiology.219.3.r01jn17645. https://doi.org/10.1148/radiology.219.3.r01jn17645. [DOI] [PubMed] [Google Scholar]
- 19.Raval NC, Gonzalez E, Bhat AM, Pearlman SA, Stefano JL. Umbilical venous catheters: evaluation of radiographs to determine position and associated complications of malpositioned umbilical venous catheters. Am J Perinatol. 1995;12:201–4. doi: 10.1055/s-2007-994452. https://doi.org/10.1055/s-2007-994452. [DOI] [PubMed] [Google Scholar]
- 20.Ramasethu J. Complications of vascular catheters in the neonatal intensive care unit. Clin Perinatol. 2008;35:199–222. doi: 10.1016/j.clp.2007.11.007. https://doi.org/10.1016/j.clp.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Ilıkkan B, Vural M, Arapoğlu M, Özbek S, Perk Y, İlter Ö. Yenidoğan yoğun bakım ünitesinde umbilikal kateter kullanımına bağlı sepsis sıklığı. Turk Pediatri Ars. 1997;32:34–8. [Google Scholar]
- 22.Wolf J, Curtis N, Worth LJ, Flynn PM. Central line-associated blood stream infection in children: an update on treatment. Pediatr Infect Dis J. 2013;32:905–10. doi: 10.1097/INF.0b013e3182996b6e. https://doi.org/10.1097/INF.0b013e3182996b6e. [DOI] [PubMed] [Google Scholar]
- 23.Arnts IJ, Bullens LM, Groenewoud JM, Liem KD. Comparison of complication rates between umbilical and peripherally inserted central venous catheters in newborns. J Obstet Gynecol Neonatal Nurs. 2014;43:205–15. doi: 10.1111/1552-6909.12278. https://doi.org/10.1111/1552-6909.12278. [DOI] [PubMed] [Google Scholar]


