Abstract
Gastric cancer (GC) is the fifth most common cancer in the world and accounts for 7% of the total cancer incidence. The prognosis of GC is dismal in Western countries due to late diagnosis: approximately 70% of the patients die within 5 years following initial diagnosis. Recently, integrative genomic analyses led to the proposal of a molecular classification of GC into four subtypes, i.e.,microsatellite-instable, Epstein-Barr virus–positive, chromosomal-instable (CIN), and genomically stable GCs. Molecular classification of GC advances our knowledge of the biology of GC and may have implications for diagnostics and patient treatment. Diagnosis of microsatellite-instable GC and Epstein-Barr virus–positive GC is more or less straightforward. Microsatellite instability can be tested by immunohistochemistry (MLH1, PMS2, MSH2, and MSH6) and/or molecular-biological analysis. Epstein-Barr virus–positive GC can be tested by in situ hybridization (Epstein-Barr virus encoded small RNA). However, with regard to CIN, testing may be more complicated and may require a more in-depth knowledge of the underlying mechanism leading to CIN. In addition, CIN GC may not constitute a distinct subgroup but may rather be a compilation of a more heterogeneous group of tumors. In this review, we aim to clarify the definition of CIN and to point out the molecular mechanisms leading to this molecular phenotype and the challenges faced in characterizing this type of cancer.
Introduction
Worldwide, gastric cancer (GC) is the fifth most common cancer and accounts for 7% of the total cancer incidence. The prognosis of GC is dismal in Western countries due to late diagnosis: approximately 70% of the patients die within 5 years following initial diagnosis. GC may occur sporadically, as a familial disease, or as a hereditary disease. The vast majority of GCs occurs sporadically, and only 5% to10% of the cases are truly hereditary GCs caused by germline mutations, such as in APC Promoter 1B, CDH1, or CTNNA1. A model for the carcinogenesis of sporadic GC was described by Correa [1]: the colonization of the stomach mucosa by Helicobacter pylori, a diet rich in salt, and medication lead to chronic atrophic gastritis, intestinal and pseudopyloric metaplasia, dysplasia, and finally the occurrence of GC. The genomic alterations found in GC enclose a wide range of genetic changes including, e.g., point mutations (for instance, base substitutions, base deletions, or nucleotide insertions), changes on the chromosome level [such as chromosome fusions, chromosomal translocations, chromosomal segment duplication, segment insertions, segment deletions, and chromosomal number alterations (aneuploidy)], and gene amplifications [2]. They affect a diverse number of proto-oncogenes and tumor suppressor genes, and GC belongs to the group of cancers with a high frequency of somatic mutations as well as a substantial interindividual variability of mutational load [3]. Recently, an integrative genomic analysis [2] led to the proposal of a molecular classification of GC into four subtypes, i.e., microsatellite-instable (MSI), Epstein–Barr virus (EBV)–positive, chromosomal-instable (CIN), and genomically stable GCs [2], [4].
A molecular classification of GC is urgently needed. It advances our knowledge of the biology of GC and may spur translational research aiming to improve diagnostics and treatment of GC toward precision medicine [5]. A sound categorization of GC based on molecular subtypes has implications for validation studies as well as clinical trials. Diagnosis of MSI-GC and EBV+ GC is more or less straightforward. MSI can be tested by immunohistochemistry (IHC) using antibodies directed against DNA-mismatch repair proteins (MLH1, PMS2 MSH2, MSH6) and/or molecular biological analysis of MSI using mononucleotide markers. EBV+ GC can be tested by Epstein-Barr virus encoded small RNA (EBER) in situ hybridization. However, with regard to chromosomal instability (CIN), testing may be more complicated and may require a more in-depth knowledge of the underlying mechanism leading to CIN. It also raises the question of whether CIN really defines a distinct subgroup or is a compilation of a more heterogeneous group of tumors.
Definition of Chromosomal Instability
Malignant tumors may be characterized by high levels of abnormal genomic alterations referred to as genomic instability [6]. However, genomic alterations are not equal to genomic instability. A tumor cell is classified as genomically instable when the number of genomic alterations accumulates rapidly in a short period of time, i.e., there is a high rate of accumulating mutations [7]. Genomic instability can be categorized into microsatellite instability (MSI) and chromosomal instability (CIN) [8]. Both instabilities indicate a mutator phenotype in cancer [9].
Mutations occurring at a high rate in microsatellite regions of the DNA sequence are the hallmark of MSI, which is caused by genetic and/or epigenetic alterations of genes coding for DNA mismatch repair proteins, such as MSH2, MSH6, PMS2, and MLH1 [10], [11], [12]. If such genomic alterations occur on the chromosomal level, they are referred to as CIN.
Although CIN is a major characteristic in many types of cancers, it remains a dubious phenomenon with an inaccurate definition: some groups refer to it as aneuploidy or polyploidy, whereas others define CIN as multiple structural rearrangements or frequent changes in chromosome numbers [6], [7], [13], [14]. According to Geigel et al., CIN refers to the rate at which whole or large segments of chromosomes are either gained or lost [8]. CIN is not equal to aneuploidy, but it can lead to aneuploidy. A tumor cell can be aneuploid but still have a stable karyotype [8], [15]. Accelerated loss of heterozygosity in tumor suppressor genes or accelerated gain of oncogene copies due to chromosomal duplication is a result of CIN that leads to cancer [16]. Cancers with CIN reveal a very heterogeneous structure (karyotypically, molecularly, and histologically) in different parts of the tumor [17].
Although many studies have been carried out on CIN in cancers, the definite cause of its incidence still remains controversial. Several theories have been postulated with regard to causes of CIN. One theory states that CIN simply results from defects in oncogenes and tumor suppressor genes. Oncogenes like RAS can cause an increase in genomic aberrations [18], [19], and tumor suppressor genes like TP53 (p53) can make the CIN phenotype worse [20]. However, tumors with a stable karyotype may have mutations in the same genes making this theory unattractive. Another theory postulates that aneuploidy occurs when, by chance, an abnormal chromosome is present within cells that can cause abnormal cell division and instability of the cellular segregation machinery, therefore leading to karyotypically abnormal daughter cells. Preceding genetic alterations in, e.g., oncogenes or tumor suppressor genes, are not required to produce CIN in this scenario [21], [22]. Another theory proposes that CIN cancers arise from early mutational events in a gene or genes responsible for the CIN phenotype, a mechanism similar to MSI [13]. To reveal the definite cause of CIN in cancers, the mechanisms and altered pathways causing CIN necessitate further studies.
CIN Mechanisms
The CIN phenotype can be induced by dysfunctions of different cellular processes, which can be categorized into 1) inaccurate chromosome segregation during mitosis, 2) cell cycle checkpoint defects, 3) oncogene induced mitotic stress, and 4) replication stress.
Inaccurate Chromosome Segregation During Mitosis
Sister chromatid segregation in mitosis is a regulated process, and many events can lead to faulty chromosome separation if not precisely controlled, i.e. mitotic checkpoint defects, kinetochore malfunctions, merotellic attachments, faulty sister chromatid cohesion and separation, centrosome amplification, and telomere dysfunction.
Mitotic Checkpoint Defects
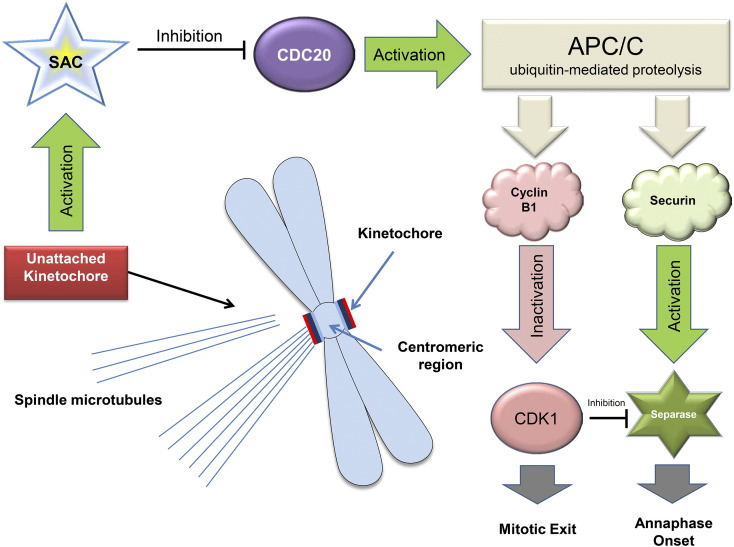
Mitotic checkpoint, also known as the spindle assembly checkpoint (SAC), has many roles in the regulation of the mitosis [23]. Mitotic checkpoint dysfunction, which is due to mutations of the genes involved, can lead to the CIN phenotype [13]. SAC controls proper attachment of chromosomes at the centromeric regions (kinetochores) to microtubules of the mitotic spindles [23]. If the chromosomes are not properly attached to the microtubules, SAC is activated and delays the progress of mitosis [23]. SAC regulates this by a cascade of events even if one kinetochore of a chromosome is not attached [24]. SAC is able to inhibit CDC20 and thereby anaphase-promoting complex/cyclosome (APC/C). APC/C is a large complex of proteins with ubiquitin ligase activity. It triggers the transition from metaphase to anaphase by ubiquitylating cyclins (e.g., cyclin B1) and securin (Figure 1).
Figure 1.
The mitotic checkpoint or SAC. SAC factors are activated when a signal is detected from unattached kinetochores to spindle microtubules. Active SAC inhibits CDC20. CDC20 is an essential regulator of cell division, which binds to and activates the APC/C. APC/C is a large complex of proteins with ubiquitin ligase activity. It triggers the transition from metaphase to anaphase by ubiquitylating cyclins (e.g., cyclin B1) and securin. Securin forms a complex with separase and thereby blocks separase activity. APC/C-mediated proteasomal degradation of securin liberates and activates separase. A second regulatory step of separase activity is its phosphorylation by CDK1. APC/C-mediated proteasomal degradation of cyclin B1 inactivates CDK1. Activated separase cleaves cohesin, resulting in the separation of sister chromatids and triggering the anaphase. Thus, inhibition of CDC20 and APC/C by SAC leads to a temporary pause of mitosis and continuation of the attachment of the sister chromatids (due to inactive separase enzyme) until all kinetochores are joined to the mitotic spindle [24].
SAC components involved in APC/C inhibition are BUB1, BUB3, BUBR1, MAD1, MAD2, CMT2/p31, MPS1, CENP-E, ZW10, ZWILCH, and ROD [23], [25]. Other components also known to be involved in SAC are Aurora B, MAPK, NEK2, PLK1, dynein, dynactin, CLIP170, and LIS1 [25]. If any of the SAC components is deregulated, the inhibition of APC/C will not take place, and cells containing unattached kinetochores will proceed with mitosis, leading to mis-segregation of chromosomes [23]. However, SAC only controls the interaction among the kinetochores and the spindle microtubules, and therefore, kinetochores are also an important determinant of chromosome segregation [25].
Kinetochore Malfunctions
Kinetochores are protein structures located at the centromeric regions of chromosomes. They form an interface between the chromosome and microtubules [26]. The kinetochore structure consists of three sections: the inner section (interacts with chromatin), the outer section (interacts with 15 to 20 of the spindle microtubules), and the central section [27]. The kinetochore functions involve regulation of proper attachment of microtubules to chromosomes, assistance of chromosome movement on spindles, and activation of a signaling pathway to stop cell cycle progression when defects are detected [26]. Determination of the place of kinetochore assembly and the kinetochore assembly itself are important for error-free chromosome segregation [27]. During mitosis, the kinetochore assembles on the surface of the peripheral centromeric regions [24]. The centromeric regions consist of tandemly repeated sequences called α-satellite regions and a CENP-B box, which is bound by the CENP-B protein. The centromere contains CENP-A protein, which is a histone variant (instead of H3 in nucleosomes) and some other additional proteins [24], [28]. The CENP-A levels are important in determination of the centromeric region, where the kinetochore is formed. If there is an overexpression of the CENP-A, it can be incorporated in noncentromeric loci, and the kinetochore will be formed at an inappropriate chromosomal site. If the kinetochores form in other locations rather than on the centromeres or form at multiple regions on the chromosome, the attachment to spindles is inaccurate. This leads to a fragmentation of the chromosome due to spindle forces. If a chromosome does not have a site for kinetochore formation, it will not attach to the spindle and will not be segregated during mitosis [27].
Some evolutionarily conserved proteins, i.e., MIS12, HEC1, and MCM21, are recruited to the outer plate of the kinetochore just before mitosis and form sites for microtubule attachment [24], [27], [28]. CENP-C/H/I/K/F, Ndc80, Zwint, and KNL1 (SPC105) are known to be other proteins important in kinetochore assembly and function. Ndc80 associated with MIS12 and KNL1 is essential for microtubule-kinetochore binding [27]. Dynein and kinesin (CENP-E) are important in kinetochore motility [27]. Six protein kinases regulate kinetochore assembly and ensure the formation of bipolar chromosome attachments to the spindle, i.e., Aurora B, Polo-like kinase-1 (PLK1), cyclin-dependent kinase-1 (CDK1), MPS1, BUB1, and BUBR1 (MAD3) [27]. Defects in any of these proteins can lead to aberrant chromatid segregation, aneuploidy, and hence CIN.
Merotellic Attachments
The attachment of the microtubules to the kinetochores is a stochastic process and error prone. Although the errors are usually detected by SAC proteins, merotellic attachments remain undetected by the checkpoint. Merotellic attachments occur when one or both kinetochores have an attachment to both spindle poles. This causes a hindrance in chromosome segregation due to its lagging and leads to aneuploidy in the daughter cells. This is a hallmark of CIN [26]. Aurora B has been indicated in correcting syntelic and merotelic chromosome attachments, and its inactivation can cause chromatid segregating defects (for a review, see [29]).
Faulty Sister Chromatid Cohesion and Separation
During the S phase of the cell cycle, cohesin, an evolutionarily conserved protein complex, forms between the sister chromatids and holds them together. During the transition of the metaphase into the anaphase, the activation of separase leads to a cleavage of cohesin and the separation of the sister chromatids. Separase cleaves Rad21, Mcd1, and SCC1 cohesins and if uncontrolled leads to premature separation of chromatids, lagging chromosomes, and anaphase bridges. Thus, the expression of separase (encoded by ESPL1) is important for the fate of chromosomes after mitosis [30]. Interestingly, abnormal sister chromatid cohesion due to somatic mutations can also lead to CIN [31]. STAG2 encodes a cohesin complex subunit and is mutated in multiple CIN cancers [32].
Centrosome Amplification
Centrosomes are microtubule organizing centers that form bipolar spindles at the beginning of mitosis to ensure the equal distribution of the chromosomes. Each centrosome or microtubule organizing center contains two centrioles surrounded by the pericentriolar matrix, which is the source of microtubule assembly. During the S phase of the cell cycle, the centrosome is duplicated. Daughter centrosomes split and move to opposite sites of the cell to form the mitotic spindle. After normal mitosis, each daughter cell receives a single centrosome [33].
If centrosome amplification is not regulated, it will lead to multiple centrosomes in the cell and multipolar spindles in mitosis, resulting in chromosome mis-segregation. The cyclin-dependent kinases (CDKs) and the Aurora I1l-like kinases are involved in the regulation of the centrosome duplication process [34], [35]. Some studies provided evidence that TP53 inactivation and STK15/AURKA overexpression lead to centrosome replication in a single cycle due to checkpoint alterations [36], [37], [38]. However, centrosome duplication may also occur in the absence of TP53 mutations [39]. Aurora A and PLK1 are also known to be involved in centrosome duplication [40], [41]. Cytokinesis failure, cell fusions, centrosome fragmentation, and cell cycle arrest in the S phase are additional events that lead to multicentrosome cells [33]. Extra centrosomes are known to promote chromosome mis-segregation and result in high merotelic attachments in CIN cancers [42]. More recent investigations indicated a role for Tpx2 in centrosome duplication regulation [43].
Telomere Dysfunction
Telomeres are structures at the endings of chromosomes, which prevent the formation of DNA rings and chromosome fusions. Each DNA replication round shortens the telomeres, and telomerase maintains a functional length of telomeres. In cells with defective telomerase function, chromosomes finally reach a critical shortening of the telomeres. The exposed chromosome ends activate the DNA damage response which connects the chromosome ends together, and causes flaws in chromosome segregation. A series of breakage fusion bridge cycles occurs in proliferating cells, giving rise to CIN (reviewed in [44]).
Cell Cycle Checkpoint Defects
The three cell cycle checkpoints, i.e., G1-S, S-G2, and G2-M, consist of mechanisms that control the cell cycle and detect errors in DNA repair, DNA synthesis, and chromosome segregation. Signals are then sent to the replication/segregation machinery to repair the damage [45]. Cdks drive cell division and regulate the different phases of the cell cycle. They consist of a catalytic subunit (cdk) and a regulatory subunit (cyclin). The Cdk1 also known as cell division cycle 2 (CDC2) is a mitotic kinase controlling the G2-M checkpoint or the “mitotic checkpoint” [46]. Cdk1along with cyclin A or B controls the start of mitosis and the centrosome cycle. When Cdk1 is activated, it phosphorylates more than 70 substrates to trigger centrosome separation and perform many other tasks [46]. Among other kinases, NEK, Aurora kinase, and Polo-like kinase are known regulators of this phase. Other regulators of this checkpoint, i.e., MPS1, BUB1, and BUBR1, have been described previously. Upregulation of CDK1 and its regulators, i.e., cyclin B1/B2, cyclin A, CDC25, CKS1, and CKS2, has been reported as a signature of CIN in malignant tumors [46]. Cdk2, Cdk4, and Cdk6 are kinases active in the interphase (G1-S checkpoint). Cdk4 and Cdk6 are activated by D-type cyclins, whereas Cdk2 is activated by E-type cyclins [46]. The “DNA damage checkpoint,” which checks the DNA for replication accuracy, ceases G1/S and G2/M transitions in case of DNA damage by repression of CDK activity. Hyperactive CDKs, caused by mutations in genes active in the DNA damage response pathway, lead to the continuation of the cell cycle and proliferation of the cells containing damaged DNA. These series of events lead to an instability of the genome [46]. The G1-S checkpoint induces G1 arrest via a pathway including several molecules. The pathway starts when DNA damage is sensed by ATM/ATR protein. This protein phosphorylates p53 transcription factor and targets MDM2 protein, too. The CHK1/CHK2 also target p53 and MDM2 proteins. P53/MDM2 modifications lead to p53 accumulation and its higher activity. The transcriptional target of p53 is the p21cip1/WAF1, an inhibitor of cyclin-dependent kinases. Activation of this pathway results in cyclin E/CDK2 kinase inhibition and thus G1 arrest [47]. Elimination of the G1-S checkpoint, for instance, by TP53 mutation, results in gene amplifications, deletions, and high genomic rearrangement frequency [45]. Cyclin E upregulation induces CIN in tumors [46], and CDK4 amplification is also said to result in mitosis deregulation and CIN by duplicating centrosomes [48]. Replication fork integrity during S phase (replication phase) is controlled by the S-G2 checkpoint. In this case, stalled replication activates the checkpoint, leading to inhibition of DNA double-strand breaks [47].
The Oncogene-Induced Mitotic Stress Theory
The mechanisms described above all lead to incorrect chromosome segregation during mitosis. However, CIN necessitates additional major cellular changes. Chromosomal alterations are usually negatively selected, cannot be tolerated by cells because they are deleterious, and would induce apoptosis. This can be overcome by genetic alterations that inactivate apoptosis like TP53 mutations [49]. Thus, the chromosomal segregation errors have to be accompanied by defects in tumor suppressor genes and the overexpression of oncogenes that simulate proliferation and inactivate apoptosis.
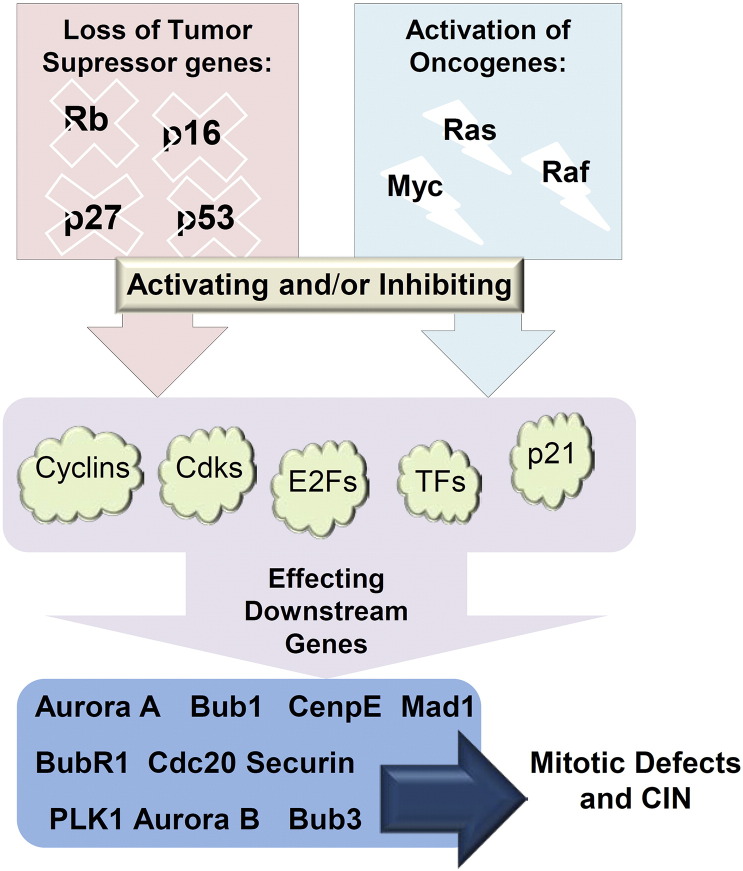
Paradoxically, most cancers with CIN harbor only few or no mutations in chromosome segregating genes [50]. A recent hypothesis, denoted “oncogene induced mitotic stress,” proposed that mitotic processes controlling chromosome segregation are affected indirectly by oncogenes and tumor suppressor genes (Figure 2). An example is the RAS oncogene. Its overexpression induces centrosome overduplication, the production of anaphase bridges, and the formation of multipolar spindles [51].
Figure 2.
The “oncogene-induced mitotic stress” theory. Mutations on genes involved in accurate chromosome segregation are a rare event; nevertheles, CIN is prevalent in cancers. This theory proposes that the key oncogenes and/or tumor suppressor genes (top of diagram) have an indirect effect on mitosis genes (bottom of diagram), controlling chromosome segregation indirectly. Aberration in these main pathways results in mitotic stress and eventually CIN (simplified from [50]).
The overexpression of MET (hepatocyte growth factor receptor) can induce the rise of multiple centrosomes and deregulation of centrosome duplication, which in turn leads to multipolar spindles and aneuploidy. MET is said to impose this affect via the PI3K-AKT pathway. MET expression can induce CIN in TP53-deficient cells, which is important in understanding its function [52]. Among different Raf oncogenes, BRAF mutation was shown to induce aberrant spindles, supernumerary centrosomes, chromosome mis-segregation, and aneuploidy in malignant melanoma [53].
RB and TP53 inactivation in turn may lead to MAD2 (and BubR1) overexpression and hence CIN [54]. Thus, these two genes are other candidates in this regard. However, a number of cancers with mutant TP53 are chromosomal stable and show MSI [55]. The effect of TP53 inactivation depends on the type of TP53 mutation: If it does not affect the function of p21cip1, the tumors are stable. The unstable tumors have a defective p21cip1 function. P21cip1 defective mice overexpress Mad2, and because p21cip1 is a CDK inhibitor, it is important in preventing CIN. P53 represses MAD2 through p21cip1-dependent inhibition of CDKs and activation of Rb. Thus, two major tumor suppressors, i.e.,TP53 and RB, are important in genomic integrity (reviewed in [54]). Teh et al. indicated that the upregulation of FOXM1 in epidermal keratinocytes triggers DNA damage response of TP53 gene without leading to cell cycle arrest or apoptosis. High FOXM1 expression induced copy number variation, loss of heterozygosity (LOH), and whole chromosomal gain, which are characteristics of genomic instability [56].
PLKs, also known proto-oncogenes, contribute to the maintenance of genomic stability. The overexpression of PLK1 can result in multinucleation and skipping of the G1 arrest checkpoint [57]. PLK4 plays a central role in centrosome duplication and precise reproduction of centromeres [40]. PLK1 also inhibits proapoptotic function of p53 via its phosphorylation [57].
Cyclin D1 is able to induce centrosome amplification and produce chromosomal abnormalities after expression in normal cells. Cyclin D1 is an activator of cdk2 which controls centrosome duplication. p21cip1, which is activated by p53, is an inhibitor of cdk2 and can in turn inhibit centrosome duplication [48].
Replication Stress
Recently, Burrell et al. claimed that CIN occurring in colorectal cancer (CRC) is mostly a result of premitotic errors and damaged replication fork progression causing replication stress, and not the reason of mitotic errors. Thus, replication stress leads to chromosomal mis-segregation. While searching for causative gene mutations leading to this event, only TP53 mutation was detected. Further analyses identified also a loss of 18q, which contained three genes [PIGN (MCD4), MEX3C (RKHD2), and ZNF516 (KIAA0222)].These were considered as new CIN suppressors in CRC [58]. It is important to mention that amounts of segregation errors can vary among different cancer types. Thus, observations made in CRC cannot be generalized to other types of cancers, including GC. Multiple observations suggest both premitotic and mitotic events to be important in CIN occurrence [59].
DNA replication deficiency can result in a collapse of the replication forks. Putative causes are the activation of oncogenes (like CCND1 and KRAS) and the inactivation of tumor suppressor genes (like RB1 and APC). These two events accelerate cell proliferation and lead to a hyperreplicative phase with DNA double-strand breakage and fork collapse. Usually, after replication stress, apoptosis is induced via the p53 pathway. In TP53-deficient cells, this leads to tumorigenesis. Apart from structural chromosomal abnormalities caused by replication stress, it can also lead to chromosome mis-segregation due to loss of CIN suppressors or an instability of centromeres (reviewed in [49]).
CIN Occurrence in Various Cancers
Defects in chromosome segregation are considered as a first step toward CIN, and the assessment of the expression of genes involved in chromosome segregation might give us insights into the biology of CIN cancers.
hBUB1, ATM, ATR, and BRCA1/2 gene mutations have indicated CIN production in experimental models [13], [60], [61]. The APC (adenomatous polyposis coli) is a tumor suppressor gene coding for a regulator of the Wnt pathway and has many tasks like labeling β-catenin for degradation [62]. Loss of the C terminus of APC can induce CIN in CRC, making it a prominent factor involved in chromosomal stability [63]. Dunican et al. reported that PLK, CCNA2, and RanBP2 are overexpressed in CIN-type CRC and claimed them to be a tool for separating CIN-type from MSI-type cancers [64]. Mutations in three gene classes, i.e., MRE11 (double-strand break repair gene); hZw10, hZwilch, and hRod (chromosome segregation gene); and Ding were found in CIN CRC [65].
Yuan et al. analyzed sequences and mRNA expression profiles as well as protein expression patterns of SAC genes [MAD1L1, MAD2L1, MAD2L2, BUB1, BUB1B, BUB3, CDC20, and TTK (MPS1)] in breast cancer and found high expression of the genes in CIN type, especially for BUB1B gene, which could be a CIN breast cancer marker [66].
Carter et al. used gene expression data to infer chromosomal imbalance or functional aneuploidy in cancer. They assessed more than 10,000 gene expression data sets and found 70 genes to be highly associated with CIN in lymphoma, lung adenocarcinoma, glioma, medulloblastoma, mesothelioma, and breast cancers and called it the “CIN70” signature. Among the CIN70 genes, the genes with the highest CIN score were TPX2, PRC1, CDC2, FOXM1, and KIF20A. The top 70 genes included AURKA/B, NEK2, H2AFX, CDC20, Zwint, and CCNB1/B2, which are genes involved in chromosome segregation and cytokinesis [67].
The 12-gene genomic instability signature assessed by Habermann et al. revealed overexpression of CDKN2A, SCY18 and STK15 (AURKA), CCNA2, CCNE1, and BIRC5 genes in genomically instable breast cancers compared with stable cohorts [68].
Beroukhim et al. analyzed a large data set of cancer specimens for somatic copy number aberrations. It was shown that most genes amplified were oncogenes (MYC, CND1, ERBB2, CDK4, NKX2-1, MDM2, EGFR, FGFR1, KRAS), BCL2 family genes (apoptosis regulators), and the NF-kB pathway–related genes [69].
Birkbak et al. applied the CIN70 signature to 2125 breast tumor expression profiles along with 3 ovarian cancers, 2 squamous cell lung cancers, and a GC cohort. The results indicated the highest CIN70 score with estrogen receptor‐negative and basal-like breast cancers. Structural complexity of chromosomes and CIN was also highly correlated with the CIN70 signature [70].
Watanabe et al. divided CRCs into two groups of CIN high and CIN low types based on LOH rates and found a set of differentially expressed genes characterizing the two groups. However, the genes were responsible for cell growth, cell communication, host pathogen interaction, and others, which are not attractive candidates to define CIN [71].
Szász et al. gathered expression profiles for the CIN70 genes in 10 publicly available breast cancer data sets. The highest correlated genes with tumor CIN score (Aurora A, FOXM1, TOP2A, and TPX2) were chosen as CIN4. These four genes indicated to be a good indicator of CIN and ploidy status in breast cancer. Thus, they claimed that the CIN4 expression status may serve as a prognostic marker in breast cancer [72].
Recently, How et al. examined CIN70 in cervical cancer to assess its relevance with clinical outcome prediction, which revealed high correlation [73].
CIN in Gastric Cancer
Many genes until now have been implicated in GC carcinogenesis. These include MET, MYC, HST1/INT2, and ERBB2 amplification, some of which are associated with a poor prognosis [74]. However, genes involved in CIN type have not been precisely defined, and yet there is a need for identification of a marker or a set of markers to define CIN GC.
AURKA (BTAK) is a gene located on 20q13 and encodes a serine threonine kinase, which is regulated via the cell cycle [75]. AURKA plays a role in centrosome integrity and correct cytokinesis [76]. However, its overexpression leads to centrosome duplication and aneuploidy [38]. AURKA is amplified in GC, and its overexpression is possibly the reason for aneuploidy. AURKA can be overexpressed without gene amplification possibly due to accelerated transcriptional activation [77]. This gene interacts with GSK-3b and is important in β-catenin regulation in GC [78]. It is also involved in TP53 regulation [79].
The APC gene regulates β-catenin [78] and chromosome segregation. APC mutations or LOH leads to structural chromosomal changes and aneuploidy. An APC mutation occurs in approximately 10% of GCs [80].
The The Cancer Genome Atlas network reported that the CIN GCs usually show an intestinal phenotype and are TP53 mutated (71% of cases). They are enriched in amplifications of genes encoding receptor tyrosine kinases (EGFR, ERBB2, ERBB3, FGFR2, and MET). Other genes were also amplified in CIN GCs, i.e., MYC, GATA4, GATA6, and ZNF217, VEGFA, KRAS, NRAS, and cell cycle–related genes (CCNE1, CCND1, CDK6)[81].
The expression of EGFR, AKT, and HER2 was assessed in GC, and it was shown that AKT overexpression was related to EGFR and HER2 expression. EGFR/HER2 overexpression was highly correlated with aneuploidy in GC [82].
Table 1 summarizes the most important and frequent factors involved in producing the CIN phenotype in cancers that were mentioned previously.
Table 1.
List of the Most Common Gene Modifications Related to CIN
| Chromosome Segregation Genes and Cell Cycle Genes Involved in CIN Cancers | Tumor Suppressor Genes or Oncogenes Involved in CIN Cancers | Gene Changes in CIN GC |
|---|---|---|
| PLK1 overexpression (proto-oncogene) | TP53 mutation (tumor suppressor) | AURKA (BTAK) overexpression (chromosome segregation regulation) |
| AURKA (BTAK) and AURKB overexpression | MET overexpression (proto-oncogene) | APC mutation (tumor suppressor) |
| BUB1/BUB3/BUB1B overexpression | RB1 mutation (tumor suppressor) | EGFR/HER2/ERBB2 overexpression (proto-oncogene) |
| MAD1/MAD2/MAD3 (BUBR1) overexpression | RAS (KRAS) overexpression (proto-oncogene) | RAS (KRAS and NRAS) overexpression (proto-oncogene) |
| ZWINT overexpression | ERBB2(HER2/neu/EGFR) overexpression (proto-oncogene) | MYC overexpression (proto-oncogene) |
| hZw10, hZwilch, and hRod mutations | FOXM1 overexpression (proto-oncogene) | CCNE1, CCND1, CDK6 overexpression (cell cycle–related genes) |
| NEK2 and MPS1 (TTK) overexpression | MYC overexpression (proto-oncogene) | MET overexpression (proto-oncogene) |
| CCNA2 (cyclin A2)/CCNB1 (cyclin-B1)/CCNB2/CCNE1/CCND1 overexpression | MDM2 overexpression (proto-oncogene) | TP53 mutation (tumor suppressor) |
| CDK1(CDC2)/CDK4 overexpression | BIRC5 (survivin) overexpression (proto-oncogene) | FGFR2 overexpression |
| CDC20 overexpression | VEGFA overexpression |
The table includes gene modifications in various cancers and the gene modifications detected in CIN GC up to present.
GC Classification
The World Health Organization published a new classification system for malignant tumors of the gastrointestinal tract in 2010 [83]. GC is now subclassified into tubular, papillary, mucinous, poorly cohesive (including the signet ring cell variant), and mixed type. The carcinoma with lymphoid stroma (medullary carcinoma) and the hepatoid adenocarcinoma were added. However, the histological classification system described by Laurén is still widely used in many clinical trials and GC research publications [84]. Recently, several attempts had been undertaken to also classify GC molecularly. A morphomolecular classification of GC might be more attractive to better understand GC biology and to improve attempts for targeted therapy. It may spur the development of novel prognostic and predictive biomarkers for patient management [85].
Lei et al. [86] were among the first who categorized GC into three subtypes, i.e., the proliferative (with high mutation rates on TP53; high genomic instability; and high activity in E2F, MYC, and RAS oncogenic pathways), the metabolic (with low TP53 mutation rates and high sensitivity to 5-fluorouracil), and the mesenchymal type (with low CDH1 expression, and most sensitive to phosphatidyl inositol 3 kinase–AKT–mTOR inhibitors and expression of stem cell markers).
In 2014, The Cancer Genome Atlas published an integrative genomic analysis of 295 GCs including array-based somatic copy number analysis, whole-exome sequencing, array-based DNA methylation profiling, messenger RNA sequencing, microRNA sequencing, and reverse-phase protein array analysis. Finally, four molecular subtypes were proposed: EBV+ GCs with CDKN2A hypermethylation and frequent PIK3A/PLL1 mutations, MSI-GCs (having hypermethylation and MLH1 silencing), genomic stable GCs (GS; with frequent CDH1/RHOA mutations), and CIN GC (frequently harboring TP53 mutations) [81]. Based on a proposed algorithm, GC can be first recognized by EBV status and subsequent MSI analysis. The remaining cases can be divided into genomically stable or chromosomal-instable tumors [85].
The Asian Cancer Research Group classified GCs based on sequencing and gene expression data into four similar groups, i.e. MSI, MSS/EMT (corresponding to GS), MSS/TP53+ (corresponding to EBV+), and MSS/TP53− (corresponding to CIN). However, they noted the presence of some overlap in different molecular targets among the groups [87].
Recently, Gonzalez et al. classified GCs into four similar subtypes using IHC for p53 and MLH1 detection and fluorescent in situ hybridization for EBER detection in tissue sections. They classified GCs into EBER+ (EBV+), MLH1− (MSI), aberrant p53 (CIN), and the remaining sections into a fourth group (GS). However, they claimed difficulty in the detection of CIN cancers with wild-type TP53. This causes a problem in distinction of the CIN and GS types, and somatic copy number aberrations have to be defined molecularly rather than by IHC [62].
Setia et al. aimed at classifying GCs based on protein and mRNA expression of a set of biomarkers [EBER, p53, mismatch repair proteins (MLH1, PMS2, MSH2, MSH6), E-cadherin (CDH1), PD-L1, MUC2, MUC6, MUC5AC, CDX2, CD10, and HER2]. They classified GCs into five groups, i.e., EBER-positive GC, mismatch repair-deficient GC, E-cadherin aberrant GC, p53 aberrant GC, and GC with normal p53 expression. They further classified the p53 aberrant group into four subtypes (intestinal, gastric, mixed, and null) based on expression of MUC2, MUC6, MUC5AC, and CD10. It was suggested that p53 aberrant GCs incline toward higher HER2/neu expression, and the potential targeting molecules can be HER2, EGFR, VEGFR, MET, FGFR2, and cell cycle mediators (CCNE1, CCND1, and CDK6), which were all overexpressed. Oppositely, the p53 normal group had a high MUC6 expression and had been defined as the subtype with expression of normal gastric mucosa genes [63].
Based on all these findings, three groups can be characterized based on defined molecular markers: EBV+ GC, MSI-GC, and genomically stable GCs (CDH1-mutated and diffuse-type GC). The CIN GC is still vaguely characterized and ultimately may also be a diagnosis of exclusion. CIN GC more commonly shows an intestinal phenotype, is characterized by amplification of genes coding for receptor tyrosine kinases, and shows cell cycle–related gene overexpression. Thus, utilizing inhibitors targeting molecules involved (ERBB2, EGFR, MET, FGFR2, CDK2, KRAS) can be considered as a treatment option [88], but still less attention has been paid to the mechanism causing CIN.
CIN Characterization in GC
Despite the diversity of pathways leading to CIN, various CIN cancers share similar gene modifications, which lead to chromosomal rearrangements, aneuploidy, LOH, and complete disorder of the genome. However, molecularly and histologically, CIN GC still comprises a very heterogeneous group of tumors. A valid and “easy-to-use” CIN marker is still lacking and may be difficult to find. Several methods were utilized for the determination and quantification of CIN, including fluorescent in situ hybridization, LOH analysis, karyotyping, cytometry, single nucleotide polymorphism array, micronuclei counting, and comparative genomic hybridization [8], [89]. None of these methods is optimal as a diagnostic tool in a more clinical setting. For CIN diagnosis in a cancer cohort, not only should the assay measure chromosomal imbalances (as a whole or in part), but it should also measure the rate of the chromosomal modifications by a simple, efficient, and rapid means, Thus, diagnostics of CIN GC have not reached the “bedside” [8], and further “benchwork” is needed to provide more insights into this phenomenon and develop reliable diagnostic tools.
References
- 1.Correa P. Human gastric carcinogenesis: a multistep and multifactorial process—first American Cancer Society award lecture on cancer epidemiology and prevention. Cancer Res. 1992;52:6735–6740. [PubMed] [Google Scholar]
- 2.Cancer Genome Atlas Research N Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawrence MS, Stojanov P, Polak P, Kryukov GV, Cibulskis K, Sivachenko A, Carter SL, Stewart C, Mermel CH, Roberts SA. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature. 2013;499:214–218. doi: 10.1038/nature12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang K, Yuen ST, Xu J, Lee SP, Yan HH, Shi ST, Siu HC, Deng S, Chu KM, Law S. Whole-genome sequencing and comprehensive molecular profiling identify new driver mutations in gastric cancer. Nat Genet. 2014;46:573–582. doi: 10.1038/ng.2983. [DOI] [PubMed] [Google Scholar]
- 5.Röcken C. Molecular classification of gastric cancer. Expert Rev Mol Diagn. 2017;17:293–301. doi: 10.1080/14737159.2017.1286985. [DOI] [PubMed] [Google Scholar]
- 6.Lengauer C, Kinzler KW, Vogelstein B. Genetic instability in colorectal cancers. Nature. 1997;386:623–627. doi: 10.1038/386623a0. [DOI] [PubMed] [Google Scholar]
- 7.Lengauer C, Kinzler KW, Vogelstein B. Genetic instabilities in human cancers. Nature. 1998;396:643–649. doi: 10.1038/25292. [DOI] [PubMed] [Google Scholar]
- 8.Geigl JB, Obenauf AC, Schwarzbraun T, Speicher MR. Defining ‘chromosomal instability’. Trends Genet. 2008;24:64–69. doi: 10.1016/j.tig.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Loeb LA. A mutator phenotype in cancer. Cancer Res. 2001;61:3230–3239. [PubMed] [Google Scholar]
- 10.Aaltonen LA, Peltomaki P, Leach FS, Sistonen P, Pylkkanen L, Mecklin JP, Jarvinen H, Powell SM, Jen J. Clues to the pathogenesis of familial colorectal cancer. Science. 1993;260:812–816. doi: 10.1126/science.8484121. [DOI] [PubMed] [Google Scholar]
- 11.Ionov Y, Peinado MA, Malkhosyan S, Shibata D, Perucho M. Ubiquitous somatic mutations in simple repeated sequences reveal a new mechanism for colonic carcinogenesis. Nature. 1993;363:558–561. doi: 10.1038/363558a0. [DOI] [PubMed] [Google Scholar]
- 12.Thibodeau SN, Bren G, Schaid D. Microsatellite instability in cancer of the proximal colon. Science. 1993;260:816–819. doi: 10.1126/science.8484122. [DOI] [PubMed] [Google Scholar]
- 13.Cahill DP, Lengauer C, Yu J, Riggins GJ, Willson JK, Markowitz SD, Kinzler KW, Vogelstein B. Mutations of mitotic checkpoint genes in human cancers. Nature. 1998;392:300–303. doi: 10.1038/32688. [DOI] [PubMed] [Google Scholar]
- 14.Rajagopalan H, Jallepalli PV, Rago C, Velculescu VE, Kinzler KW, Vogelstein B, Lengauer C. Inactivation of hCDC4 can cause chromosomal instability. Nature. 2004;428:77–81. doi: 10.1038/nature02313. [DOI] [PubMed] [Google Scholar]
- 15.Holland AJ, Cleveland DW. Boveri revisited: chromosomal instability, aneuploidy and tumorigenesis. Nat Rev Mol Cell Biol. 2009;10:478–487. doi: 10.1038/nrm2718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rajagopalan H, Lengauer C. Aneuploidy and cancer. Nature. 2004;432:338–341. doi: 10.1038/nature03099. [DOI] [PubMed] [Google Scholar]
- 17.Cahill DP, Kinzler KW, Vogelstein B, Lengauer C. Genetic instability and darwinian selection in tumours. Trends Cell Biol. 1999;9:M57–M60. [PubMed] [Google Scholar]
- 18.Denko NC, Giaccia AJ, Stringer JR, Stambrook PJ. The human Ha-ras oncogene induces genomic instability in murine fibroblasts within one cell cycle. Proc Natl Acad Sci. 1994;91:5124–5128. doi: 10.1073/pnas.91.11.5124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Felsher DW, Bishop JM. Transient excess of MYC activity can elicit genomic instability and tumorigenesis. Proc Natl Acad Sci. 1999;96:3940–3944. doi: 10.1073/pnas.96.7.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Livingstone LR, White A, Sprouse J, Livanos E, Jacks T, Tlsty TD. Altered cell cycle arrest and gene amplification potential accompany loss of wild-type p53. Cell. 1992;70:923–935. doi: 10.1016/0092-8674(92)90243-6. [DOI] [PubMed] [Google Scholar]
- 21.Duesberg P, Rausch C, Rasnick D, Hehlmann R. Genetic instability of cancer cells is proportional to their degree of aneuploidy. Proc Natl Acad Sci. 1998;95:13692–13697. doi: 10.1073/pnas.95.23.13692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rasnick D, Duesberg PH. How aneuploidy affects metabolic control and causes cancer. Biochem J. 1999;340:621–630. [PMC free article] [PubMed] [Google Scholar]
- 23.Kops GJ, Weaver BA, Cleveland DW. On the road to cancer: aneuploidy and the mitotic checkpoint. Nat Rev Cancer. 2005;5:773–785. doi: 10.1038/nrc1714. [DOI] [PubMed] [Google Scholar]
- 24.Cleveland DW, Mao Y, Sullivan KF. Centromeres and kinetochores: from epigenetics to mitotic checkpoint signaling. Cell. 2003;112:407–421. doi: 10.1016/s0092-8674(03)00115-6. [DOI] [PubMed] [Google Scholar]
- 25.Musacchio A, Salmon ED. The spindle-assembly checkpoint in space and time. Nat Rev Mol Cell Biol. 2007;8:379–393. doi: 10.1038/nrm2163. [DOI] [PubMed] [Google Scholar]
- 26.Maiato H, DeLuca J, Salmon ED, Earnshaw WC. The dynamic kinetochore-microtubule interface. J Cell Sci. 2004;117:5461–5477. doi: 10.1242/jcs.01536. [DOI] [PubMed] [Google Scholar]
- 27.Cheeseman IM, Desai A. Molecular architecture of the kinetochore–microtubule interface. Nat Rev Mol Cell Biol. 2008;9:33–46. doi: 10.1038/nrm2310. [DOI] [PubMed] [Google Scholar]
- 28.Meraldi P, McAinsh AD, Rheinbay E, Sorger PK. Phylogenetic and structural analysis of centromeric DNA and kinetochore proteins. Genome Biol. 2006;7:R23. doi: 10.1186/gb-2006-7-3-r23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cimini D, Degrassi F. Aneuploidy: a matter of bad connections. Trends Cell Biol. 2005;15:442–451. doi: 10.1016/j.tcb.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 30.Zhang N, Ge G, Meyer R, Sethi S, Basu D, Pradhan S, Zhao Y-J, Li X-N, Cai W-W, El-Naggar AK. Overexpression of separase induces aneuploidy and mammary tumorigenesis. Proc Natl Acad Sci. 2008;105:13033–13038. doi: 10.1073/pnas.0801610105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barber TD, McManus K, Yuen KW, Reis M, Parmigiani G, Shen D, Barrett I, Nouhi Y, Spencer F, Markowitz S. Chromatid cohesion defects may underlie chromosome instability in human colorectal cancers. Proc Natl Acad Sci. 2008;105:3443–3448. doi: 10.1073/pnas.0712384105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Solomon DA, Kim T, Diaz-Martinez LA, Fair J, Elkahloun AG, Harris BT, Toretsky JA, Rosenberg SA, Shukla N, Ladanyi M. Mutational inactivation of STAG2 causes aneuploidy in human cancer. Science. 2011;333:1039–1043. doi: 10.1126/science.1203619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brinkley BR. Managing the centrosome numbers game: from chaos to stability in cancer cell division. Trends Cell Biol. 2001;11:18–21. doi: 10.1016/s0962-8924(00)01872-9. [DOI] [PubMed] [Google Scholar]
- 34.Goepfert T, Brinkley B. vol. 49. 2000. The Centrosome-Associated Aurora/Ipl-like Kinase Family. The Centrosome in Cell Replication and Early Development; p. 331. [DOI] [PubMed] [Google Scholar]
- 35.Mussman JG, Horn HF, Carroll PE, Okuda M, Tarapore P, Donehower LA, Fukasawa K. Synergistic induction of centrosome hyperamplification by loss of p53 and cyclin E overexpression. Oncogene. 2000;19:1635–1646. doi: 10.1038/sj.onc.1203460. [DOI] [PubMed] [Google Scholar]
- 36.Fukasawa K, Choi T, Kuriyama R, Rulong S, Woude GFV. Abnormal centrosome amplification in the absence of p53. Science. 1996;271:1744–1747. doi: 10.1126/science.271.5256.1744. [DOI] [PubMed] [Google Scholar]
- 37.Wang X-J, Greenhalgh DA, Jiang A, He D, Zhong L, Medina D, Brinkley BR, Roop DR. Expression of a p53 mutant in the epidermis of transgenic mice accelerates chemical carcinogenesis. Oncogene. 1998;17:35–45. doi: 10.1038/sj.onc.1201890. [DOI] [PubMed] [Google Scholar]
- 38.Zhou H, Kuang J, Zhong L, Kuo W-L, Gray J, Sahin A, Brinkley B, Sen S. Tumour amplified kinase STK15/BTAK induces centrosome amplification, aneuploidy and transformation. Nat Genet. 1998;20:189–193. doi: 10.1038/2496. [DOI] [PubMed] [Google Scholar]
- 39.Lingle WL, Barrett SL, Negron VC, D'Assoro AB, Boeneman K, Liu W, Whitehead CM, Reynolds C, Salisbury JL. Centrosome amplification drives chromosomal instability in breast tumor development. Proc Natl Acad Sci. 2002;99:1978–1983. doi: 10.1073/pnas.032479999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Habedanck R, Stierhof Y-D, Wilkinson CJ, Nigg EA. The Polo kinase Plk4 functions in centriole duplication. Nat Cell Biol. 2005;7:1140–1146. doi: 10.1038/ncb1320. [DOI] [PubMed] [Google Scholar]
- 41.Meraldi P, Honda R, Nigg EA. Aurora-A overexpression reveals tetraploidization as a major route to centrosome amplification in p53−/− cells. EMBO J. 2002;21:483–492. doi: 10.1093/emboj/21.4.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ganem NJ, Godinho SA, Pellman D. A mechanism linking extra centrosomes to chromosomal instability. Nature. 2009;460:278–282. doi: 10.1038/nature08136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aguirre-Portolés C, Bird AW, Hyman A, Cañamero M, de Castro IP, Malumbres M. Tpx2 controls spindle integrity, genome stability, and tumor development. Cancer Res. 2012;72:1518–1528. doi: 10.1158/0008-5472.CAN-11-1971. [DOI] [PubMed] [Google Scholar]
- 44.Tusell L, Pampalona J, Soler D, Frías C, Genescà A. Different outcomes of telomere-dependent anaphase bridges. Biochem Soc Trans. 2010;38:1698–1703. doi: 10.1042/BST0381698. [DOI] [PubMed] [Google Scholar]
- 45.Hartwell L. Defects in a cell cycle checkpoint may be responsible for the genomic instability of cancer cells. Cell. 1992;71:543–546. doi: 10.1016/0092-8674(92)90586-2. [DOI] [PubMed] [Google Scholar]
- 46.Malumbres M, Barbacid M. Cell cycle, CDKs and cancer: a changing paradigm. Nat Rev Cancer. 2009;9:153–166. doi: 10.1038/nrc2602. [DOI] [PubMed] [Google Scholar]
- 47.Kastan MB, Bartek J. Cell-cycle checkpoints and cancer. Nature. 2004;432:316–323. doi: 10.1038/nature03097. [DOI] [PubMed] [Google Scholar]
- 48.Nelsen CJ, Kuriyama R, Hirsch B, Negron VC, Lingle WL, Goggin MM, Stanley MW, Albrecht JH. Short term cyclin D1 overexpression induces centrosome amplification, mitotic spindle abnormalities, and aneuploidy. J Biol Chem. 2005;280:768–776. doi: 10.1074/jbc.M407105200. [DOI] [PubMed] [Google Scholar]
- 49.Lee J-K, Choi Y-L, Kwon M, Park PJ. Mechanisms and consequences of cancer genome instability: lessons from genome sequencing studies. Annu Rev Pathol. 2016;11:283–312. doi: 10.1146/annurev-pathol-012615-044446. [DOI] [PubMed] [Google Scholar]
- 50.Duijf P, Benezra R. The cancer biology of whole-chromosome instability. Oncogene. 2013;32:4727–4736. doi: 10.1038/onc.2012.616. [DOI] [PubMed] [Google Scholar]
- 51.Saavedra HI, Fukasawa K, Conn CW, Stambrook PJ. MAPK mediates RAS-induced chromosome instability. J Biol Chem. 1999;274:38083–38090. doi: 10.1074/jbc.274.53.38083. [DOI] [PubMed] [Google Scholar]
- 52.Nam H-J, Chae S, Jang S-H, Cho H, Lee J-H. The PI3K-Akt mediates oncogenic Met-induced centrosome amplification and chromosome instability. Carcinogenesis. 2010;31:1531–1540. doi: 10.1093/carcin/bgq133. [DOI] [PubMed] [Google Scholar]
- 53.Cui Y, Borysova MK, Johnson JO, Guadagno TM. Oncogenic B-RafV600E induces spindle abnormalities, supernumerary centrosomes, and aneuploidy in human melanocytic cells. Cancer Res. 2010;70:675–684. doi: 10.1158/0008-5472.CAN-09-1491. [DOI] [PubMed] [Google Scholar]
- 54.Malumbres M. Oncogene-induced mitotic stress: p53 and pRb get mad too. Cancer Cell. 2011;19:691–692. doi: 10.1016/j.ccr.2011.05.023. [DOI] [PubMed] [Google Scholar]
- 55.Eshleman JR, Casey G, Kochera ME, Sedwick WD, Swinler SE, Veigl ML, Willson JK, Schwartz S, Markowitz SD. Chromosome number and structure both are markedly stable in RER colorectal cancers and are not destabilized by mutation of p53. Oncogene. 1998;17:719–725. doi: 10.1038/sj.onc.1201986. [DOI] [PubMed] [Google Scholar]
- 56.Teh M-T, Gemenetzidis E, Chaplin T, Young BD, Philpott MP. Upregulation of FOXM1 induces genomic instability in human epidermal keratinocytes. Mol Cancer. 2010;9:45. doi: 10.1186/1476-4598-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Strebhardt K, Ullrich A. Targeting polo-like kinase 1 for cancer therapy. Nat Rev Cancer. 2006;6:321–330. doi: 10.1038/nrc1841. [DOI] [PubMed] [Google Scholar]
- 58.Burrell RA, McClelland SE, Endesfelder D, Groth P, Weller M-C, Shaikh N, Domingo E, Kanu N, Dewhurst SM, Gronroos E. Replication stress links structural and numerical cancer chromosomal instability. Nature. 2013;494:492–496. doi: 10.1038/nature11935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Burrell RA, McClelland SE, Bartek J, Swanton C. Response to Bakhoum et al. Curr Biol. 2014;24:R150. doi: 10.1016/j.cub.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 60.Smith L, Liu SJ, Goodrich L, Jacobson D, Degnin C, Bentley N, Carr A, Flaggs G, Keegan K, Hoekstra M. Duplication of ATR inhibits MyoD, induces aneuploidy and eliminates radiation-induced G1 arrest. Nat Genet. 1998;19:39–46. doi: 10.1038/ng0598-39. [DOI] [PubMed] [Google Scholar]
- 61.Zhang H, Tombline G, Weber BL. BRCA1, BRCA2, and DNA damage response: collision or collusion? Cell. 1998;92:433–436. doi: 10.1016/s0092-8674(00)80936-8. [DOI] [PubMed] [Google Scholar]
- 62.Gonzalez RS, Messing S, Tu X, McMahon LA, Whitney-Miller CL. Immunohistochemistry as a surrogate for molecular subtyping of gastric adenocarcinoma. Hum Pathol. 2016;56:16–21. doi: 10.1016/j.humpath.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 63.Setia N, Agoston AT, Han HS, Mullen JT, Duda DG, Clark JW, Deshpande V, Mino-Kenudson M, Srivastava A, Lennerz JK. A protein and mRNA expression-based classification of gastric cancer. Mod Pathol. 2016;29:772–784. doi: 10.1038/modpathol.2016.55. [DOI] [PubMed] [Google Scholar]
- 64.Dunican DS, McWilliam P, Tighe O, Parle-McDermott A, Croke DT. Gene expression differences between the microsatellite instability (MIN) and chromosomal instability (CIN) phenotypes in colorectal cancer revealed by high-density cDNA array hybridization. Oncogene. 2002;21:3253–3257. doi: 10.1038/sj.onc.1205431. [DOI] [PubMed] [Google Scholar]
- 65.Wang Z, Cummins JM, Shen D, Cahill DP, Jallepalli PV, Wang T-L, Parsons DW, Traverso G, Awad M, Silliman N. Three classes of genes mutated in colorectal cancers with chromosomal instability. Cancer Res. 2004;64:2998–3001. doi: 10.1158/0008-5472.can-04-0587. [DOI] [PubMed] [Google Scholar]
- 66.Yuan B, Xu Y, Woo J-H, Wang Y, Bae YK, Yoon D-S, Wersto RP, Tully E, Wilsbach K, Gabrielson E. Increased expression of mitotic checkpoint genes in breast cancer cells with chromosomal instability. Clin Cancer Res. 2006;12:405–410. doi: 10.1158/1078-0432.CCR-05-0903. [DOI] [PubMed] [Google Scholar]
- 67.Carter SL, Eklund AC, Kohane IS, Harris LN, Szallasi Z. A signature of chromosomal instability inferred from gene expression profiles predicts clinical outcome in multiple human cancers. Nat Genet. 2006;38:1043–1048. doi: 10.1038/ng1861. [DOI] [PubMed] [Google Scholar]
- 68.Habermann JK, Doering J, Hautaniemi S, Roblick UJ, Bündgen NK, Nicorici D, Kronenwett U, Rathnagiriswaran S, Mettu RK, Ma Y. The gene expression signature of genomic instability in breast cancer is an independent predictor of clinical outcome. Int J Cancer. 2009;124:1552–1564. doi: 10.1002/ijc.24017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Beroukhim R, Mermel CH, Porter D, Wei G, Raychaudhuri S, Donovan J, Barretina J, Boehm JS, Dobson J, Urashima M. The landscape of somatic copy-number alteration across human cancers. Nature. 2010;463:899–905. doi: 10.1038/nature08822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Birkbak NJ, Eklund AC, Li Q, McClelland SE, Endesfelder D, Tan P, Tan IB, Richardson AL, Szallasi Z, Swanton C. Paradoxical relationship between chromosomal instability and survival outcome in cancer. Cancer Res. 2011;71:3447–3452. doi: 10.1158/0008-5472.CAN-10-3667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Watanabe T, Kobunai T, Yamamoto Y, Matsuda K, Ishihara S, Nozawa K, Yamada H, Hayama T, Inoue E, Tamura J. Chromosomal instability (CIN) phenotype, CIN high or CIN low, predicts survival for colorectal cancer. J Clin Oncol. 2012;2011:2038–6490. doi: 10.1200/JCO.2011.38.6490. [DOI] [PubMed] [Google Scholar]
- 72.Szász AM, Li Q, Eklund AC, Sztupinszki Z, Rowan A, Tőkés A-M, Székely B, Kiss A, Szendrői M, Győrffy B. The CIN4 chromosomal instability qPCR classifier defines tumor aneuploidy and stratifies outcome in grade 2 breast cancer. PLoS One. 2013;8:e56707. doi: 10.1371/journal.pone.0056707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.How C, Bruce J, So J, Pintilie M, Haibe-Kains B, Hui A, Clarke BA, Hedley DW, Hill RP, Milosevic M. Chromosomal instability as a prognostic marker in cervical cancer. BMC Cancer. 2015;15:361. doi: 10.1186/s12885-015-1372-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tahara E. Molecular biology of gastric cancer. World J Surg. 1995;19:484–488. doi: 10.1007/BF00294705. [DOI] [PubMed] [Google Scholar]
- 75.Giet R, Prigent C. Aurora/Ipl1p-related kinases, a new oncogenic family of mitotic serine-threonine kinases. J Cell Sci. 1999;112:3591–3601. doi: 10.1242/jcs.112.21.3591. [DOI] [PubMed] [Google Scholar]
- 76.Bischoff JR, Plowman GD. The Aurora/Ipl1p kinase family: regulators of chromosome segregation and cytokinesis. Trends Cell Biol. 1999;9:454–459. doi: 10.1016/s0962-8924(99)01658-x. [DOI] [PubMed] [Google Scholar]
- 77.Sakakura C, Hagiwara A, Yasuoka R, Fujita Y, Nakanishi M, Masuda K, Shimomura K, Nakamura Y, Inazawa J, Abe T. Tumour-amplified kinase BTAK is amplified and overexpressed in gastric cancers with possible involvement in aneuploid formation. Br J Cancer. 2001;84:824–831. doi: 10.1054/bjoc.2000.1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dar AA, Belkhiri A, El-Rifai W. The aurora kinase A regulates GSK-3β in gastric cancer cells. Oncogene. 2009;28:866–875. doi: 10.1038/onc.2008.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Katayama H, Sasai K, Kawai H, Yuan Z-M, Bondaruk J, Suzuki F, Fujii S, Arlinghaus RB, Czerniak BA, Sen S. Phosphorylation by aurora kinase A induces Mdm2-mediated destabilization and inhibition of p53. Nat Genet. 2004;36:55–62. doi: 10.1038/ng1279. [DOI] [PubMed] [Google Scholar]
- 80.Ottini L, Falchetti M, Lupi R, Rizzolo P, Agnese V, Colucci G, Bazan V, Russo A. Patterns of genomic instability in gastric cancer: clinical implications and perspectives. Ann Oncol. 2006;17:vii97–vii102. doi: 10.1093/annonc/mdl960. [DOI] [PubMed] [Google Scholar]
- 81.(TCGA) CGARN Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hisamatsu Y, Oki E, Otsu H, Ando K, Saeki H, Tokunaga E, Aishima S, Morita M, Oda Y, Maehara Y. Effect of EGFR and p-AKT overexpression on chromosomal instability in gastric cancer. Ann Surg Oncol. 2016;23:1986–1992. doi: 10.1245/s10434-016-5097-3. [DOI] [PubMed] [Google Scholar]
- 83.Bosman FT, Carneiro F, Hruban RH, Theise ND. World Health Organization; 2010. WHO Classification of Tumours of the Digestive System. [Google Scholar]
- 84.Lauren P. The two histological main types of gastric carcinoma, an attempt at a histoclinical classification. Acta Pathol Microbiol Scand. 1965;64:31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 85.Kouros-Mehr H, Whittington CF. Molecular classification of gastric cancer. Transl Gastrointest Cancer. 2014;4:112–114. [Google Scholar]
- 86.Lei Z, Tan IB, Das K, Deng N, Zouridis H, Pattison S, Chua C, Feng Z, Guan YK, Ooi CH. Identification of molecular subtypes of gastric cancer with different responses to PI3-kinase inhibitors and 5-fluorouracil. Gastroenterology. 2013;145:554–565. doi: 10.1053/j.gastro.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 87.Cristescu R, Lee J, Nebozhyn M, Kim K-M, Ting JC, Wong SS, Liu J, Yue YG, Wang J, Yu K. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat Med. 2015;21:449–456. doi: 10.1038/nm.3850. [DOI] [PubMed] [Google Scholar]
- 88.Wong SS, Kim K-M, Ting JC, Yu K, Fu J, Liu S, Cristescu R, Nebozhyn M, Gong L, Yue YG. Genomic landscape and genetic heterogeneity in gastric adenocarcinoma revealed by whole-genome sequencing. Nat Commun. 2014;5:5477. doi: 10.1038/ncomms6477. [DOI] [PubMed] [Google Scholar]
- 89.Pino MS, Chung DC. The chromosomal instability pathway in colon cancer. Gastroenterology. 2010;138:2059–2072. doi: 10.1053/j.gastro.2009.12.065. [DOI] [PMC free article] [PubMed] [Google Scholar]