Abstract
Human subcutaneous (SC) white adipose tissue (WAT) increases the expression of beige adipocyte genes in the winter. Studies in rodents suggest that a number of immune mediators are important in the beiging response. We studied the seasonal beiging response in SC WAT from lean humans. We measured the gene expression of various immune cell markers and performed multivariate analysis of the gene expression data to identify genes that predict UCP1. Interleukin (IL)-4 and, unexpectedly, the mast cell marker CPA3 predicted UCP1 gene expression. Therefore, we investigated the effects of mast cells on UCP1 induction by adipocytes. TIB64 mast cells responded to cold by releasing histamine and IL-4, and this medium stimulated UCP1 expression and lipolysis by 3T3-L1 adipocytes. Pharmacological block of mast cell degranulation potently inhibited histamine release by mast cells and inhibited adipocyte UCP1 mRNA induction by conditioned medium (CM). Consistently, the histamine receptor antagonist chlorpheniramine potently inhibited adipocyte UCP1 mRNA induction by mast cell CM. Together, these data show that mast cells sense colder temperatures, release factors that promote UCP1 expression, and are an important immune cell type in the beiging response of WAT.
Introduction
An important part of mammalian defense against cold involves the generation of heat from brown adipose tissue (BAT) and beige adipose tissue depots. These tissues generate heat through the actions of uncoupling protein 1 (UCP1) (1), which uncouples oxidative respiration in mitochondria to generate heat. In rodents, this function combats obesity by increasing energy expenditure (2,3). BAT is localized to the neck and thorax of humans (4–8), and in a process known as beiging (9), UCP1-positive adipocytes form in subcutaneous (SC) white adipose tissue (WAT) (10). Beige adipocytes have unique developmental origins, gene signatures, and functional properties, including being highly inducible to increase UCP1 in response to catecholamines (9,11–13). Although questions exist about whether beige fat can make a meaningful contribution to energy expenditure in humans (reviewed in Porter et al. [14]), the induction of beige fat in rodent models is associated with increased energy expenditure and improved glucose homeostasis (13).
Activation of the sympathetic nervous system by cold activates BAT and induces beiging (1). In addition, a growing number of factors that induce beiging in mice exist, and some of these factors are produced by the immune system (13). In contrast to BAT, WAT is not highly innervated, and alternatively activated macrophages are postulated to be an important source of catecholamines, which potently induce beiging (15). In this proposed mechanism, alternatively activated macrophages increase in response to cold and synthesize catecholamines, which promote adipocyte beiging (15). Interleukin (IL)-4 promotes this alternative macrophage activation (15) and induces the proliferation and differentiation of beige adipocyte precursor cells (16). Eosinophils are an important source of IL-4 in mouse WAT (17) and are regulated by type 2 innate lymphoid cells (16). Eosinophils were also shown to be the target of meteorin-like (METRNL), a gene expressed in both muscle in response to exercise and adipose tissue in response to cold (18). Consistent with the idea that anti-inflammatory cytokines promote beiging, some inflammatory cytokines inhibit beiging (19,20). WAT beiging thus is regulated by the complex interplay among cells of the immune system.
Although the beiging response is likely more robust in mice than in humans, previous studies by us showed increases in SC WAT UCP1 and peroxisome proliferator–activated receptor γ coactivator α mRNA in response to the winter season and in response to an acute cold stimulus. This increase in UCP1 mRNA was accompanied by an increase in TMEM26 and TBX1 mRNA expression (20), which are specific beige adipocyte markers (9). As with mice, human adipose tissue contains a number of inflammatory cells, including macrophages (21,22) and mast cells (23,24), all of which have the potential to express both pro- and anti-inflammatory cytokines. Therefore, considerable potential exists for the regulation of human WAT beiging by the secretory products of immune cells.
This study investigated the relationship between the immune response and beiging response of the adipose tissue of normal human volunteers in response to changes in seasons. We found evidence linking this response to resident mast cells, and additional studies determined the effects of cold-induced changes in mast cells on the expression of beige adipocyte genes in 3T3-L1 adipocytes in vitro.
Research Design and Methods
Human Subjects
All subjects gave informed consent, and the protocols were approved by the institutional review board at the University of Kentucky (Lexington, KY). Sixteen normal healthy subjects, all aged <30 years (mean 26.6 ± 0.8 years) and with a BMI <30 kg/m2 (mean 26 ± 1 kg/m2), were recruited for SC WAT surgical biopsies, as previously described (20), of the anterior thigh under local anesthesia within 1 h of coming inside. The subjects were 10 males and 6 females, and none indicated that they were taking medications or had medical problems. All were physically active, but none participated in significant outdoor activity. All subjects were weight stable (±3%) for at least 3 months. The biopsy specimens were from seven subjects (three females, four males) in the summer (1 June–15 September) and nine subjects (three females, six males) in the winter (1 December–21 March); four of the subjects from the summer returned for winter biopsies. These procedures and some results from this cohort of subjects have been reported previously (20); there is no overlap in this cohort of 16 subjects with the cohort of lean subjects who had abdominal SC WAT biopsies in that report.
Gene Expression
Real-time RT-PCR was performed as previously described (22) by using 18S RNA to normalize the data. The primers used for each RNA tested are shown in Supplementary Tables 1 and 2. Additional details are available in the Supplementary Data.
Cell Culture
Adult-derived human adipose stem cells (ADHASC) were cultured as previously described (25); TIB64 cells and 3T3-L1 cells were cultured and differentiated as described in the Supplementary Data. The media were analyzed for IL-4 and tumor necrosis factor α (TNFα) by ELISA (AB100710 and MTA00B; R&D Systems, Minneapolis, MN) and for histamine with a histamine kit (589651; Cayman Chemical, Ann Arbor, MI). To determine the effect of pure histamine or IL-4 on 3T3-L1 adipocytes, differentiated 3T3-L1 adipocytes were treated with 10 nmol/L histamine or 1 nmol/L mouse IL-4 (R&D Systems) in DMEM with 2% FBS for 4 h at 37°C. Additional details are available in the Supplementary Data.
Histochemistry
Adipose tissue samples were placed in Bouin fixative, embedded in paraffin, and subsequently cut into 5-μm sections. UCP1 was detected by using an anti-UCP1 antibody (ab10983; Abcam, Cambridge, MA), and TMEM26 was detected with anti-TMEM26 antibody (NBP-27334; Novus Biologicals, Littleton, CO). Immunocytochemistry on differentiated 3T3-L1 cells was performed by using the same UCP1 antibody. More detailed methods are available in the Supplementary Data.
Statistics
Two-sample t tests were performed to compare winter and summer gene expression on log10-transformed data because of a considerable increase in variability in the winter. Multiple linear regression analyses were performed with a random subject effect to account for statistical correlation among repeated measurements from the same subject by using backward elimination at the 5% level to find the best predictors of UCP1. Estimated regression parameter estimates and corresponding 95% CIs and P values are given. Multiple comparisons were made by ANOVA with post hoc tests. Statistical significance for all tests was set at P ≤ 0.05. All analyses were performed with GraphPad Prism version 5 software except for the multivariate analysis, which was done with SAS 9.4 (SAS Institute) software.
Results
Seasonal Effects on Thigh SC Adipose Gene Expression
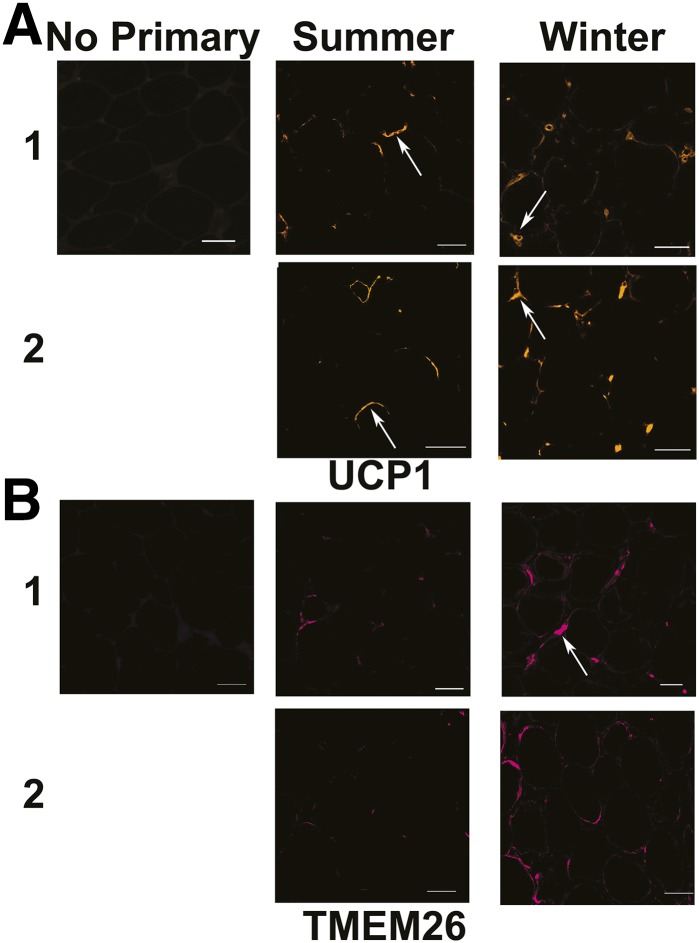
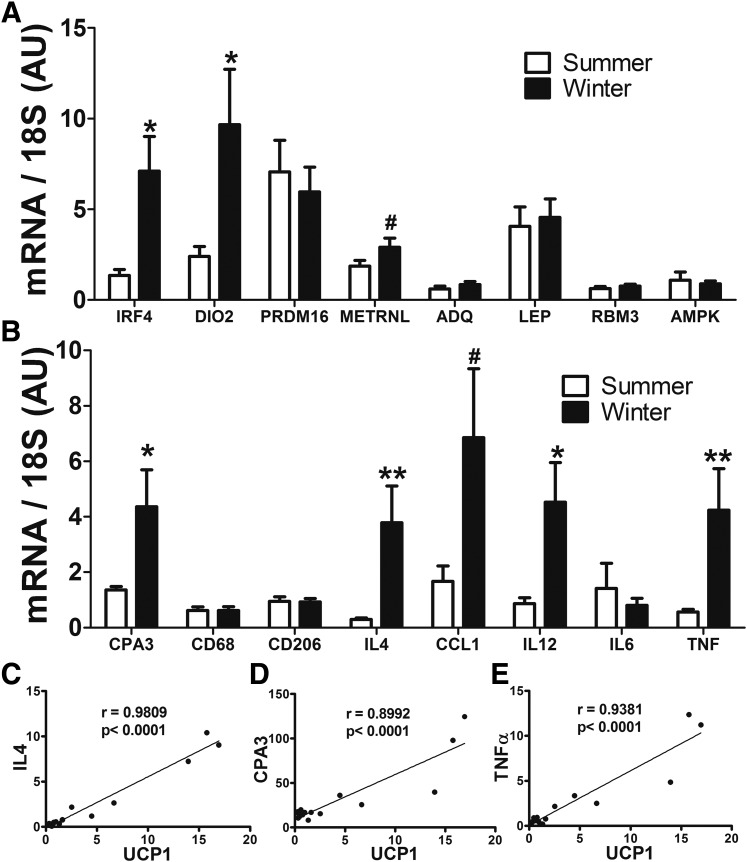
We previously described increases in the gene expression of UCP1 (12-fold), PGC1α (2-fold), and TMEM26 (10-fold) in anterior thigh SC WAT in the winter in a cohort of 16 lean, physically fit subjects (research design and methods and Kern et al. [20]). In the current study, we determined the localization and abundance of UCP1 and TMEM26 protein in thigh SC adipose tissue by immunohistochemistry. Figure 1A shows UCP1 immunohistochemistry in paired biopsy specimens of thigh SC WAT from two lean subjects in the summer and winter. In the summer, UCP1 is associated with unilocular adipocytes, usually in a crescent-shaped pattern surrounding the large lipid droplet; punctate staining also is observed. In the winter, we observe UCP1 staining in cells between adipocytes in addition to the ringing pattern around unilocular adipocytes. A similar induction of TMEM26 occurred in the winter, with expression observed around large unilocular adipocytes and in cells between adipocytes (Fig. 1B). Thus, the seasonal induction of UCP1 mRNA is likely associated with changes in UCP1 and TMEM26 protein in the winter. We further analyzed gene expression in summer and winter biopsy specimens from the cohort of 16 lean subjects and found that IRF4 and DIO2, which are important for beige adipose tissue and BAT thermogenic function, are higher in the winter than in the summer (P < 0.05) (Fig. 2A), but PRDM16 mRNA expression was not changed. The adipokines adiponectin and leptin were not significantly altered and neither were RBM3 or AMPK (Fig. 2A).
Figure 1.
Seasonal changes in UCP1 and TMEM26 immunohistochemistry in thigh SC WAT. A: Histochemical analysis of UCP1 expression in thigh SC WAT of two lean subjects in the summer and winter. The left panel shows no primary antibody control. The arrows in the middle panels point to UCP1 staining in unilocular adipocytes in the summer. The arrows in the right panels point to UCP1 staining in cells between adipocytes in the winter. B: TMEM26 staining in the same subjects. The arrow points to TMEM26 staining in cells between adipocytes in the winter. Scale bars = 50 μm.
Figure 2.
Seasonal changes in gene expression of beige adipocyte markers, immune cell markers, and cytokines. A and B: Gene expression in thigh SC adipose tissue was measured in the summer (n = 7) and winter (n = 9) by real-time RT-PCR, and the relative expression of each gene is represented in arbitrary units (AU). Data are mean ± SEM. *P < 0.05, **P < 0.01; #P = 0.06 (unpaired Student t test). C–E: Gene expression of UCP1 and the indicated genes. Pearson correlation coefficients (r) and two-tailed P values are indicated (n = 16).
To examine the mechanism of induction of these beige/brown fat genes, we examined markers of inflammatory cells, including macrophages, eosinophils, and mast cells, that could influence the expression of beige fat genes (24). As shown in Fig. 2B, we did not observe a change in CD68, a global marker for macrophages (P = 0.92); the mannose receptor (CD206), a marker of alternatively activated macrophages (P = 0.79); or MCP1, a chemokine for macrophages (P = 0.63) (data not shown). The eosinophil marker SIGLEC8 was expressed at a very low level and was not different in winter (data not shown). IL-6, which has been implicated in beiging (26), was also unchanged. However, the mast cell marker CPA3 increased in the winter (P < 0.05) (Fig. 2B). IL-4 is postulated to be important for promoting beige adipogenesis (16,17) and was induced 13-fold in the winter (P < 0.01) (Fig. 2B). Some inflammatory cytokines, including TNFα and IL-12β, were also induced (P < 0.05) (Fig. 2B). METRNL and CCL1 had statistical trends for higher mRNA expression in the winter (P = 0.06) (Fig. 2A and B).
To determine whether the seasonal difference in UCP1 was related to any of these cytokines or cell markers, we performed multiple linear regression analysis on all the genes measured. (Supplementary Table 1 lists all genes analyzed.) As shown in Table 1, IL-4, TMEM26, TNFα, and CPA3 gene expression predicted UCP1 gene expression. The relationship between UCP1 and these genes was further investigated by linear regression analysis and is shown in Fig. 2C–E. Although the model predicts a negative association for TNFα (Table 1), further analysis of the data in Fig. 2E demonstrates that it positively correlates with UCP1. When added to the model, sex was not significant (P = 0.1) and did not notably change parameter estimates. The multivariate model also identified significant relationships among CPA3, TNFα, and IL-12β (Table 1), suggesting that mast cells could be a source of these cytokines in the winter.
Table 1.
Multivariate analysis of gene expression
| Estimate | 95% CI | P value | |
|---|---|---|---|
| Predictor of UCP1 | |||
| IL-4 | 1.72 | 1.18, 2.27 | <0.0001 |
| TMEM26 | 0.29 | 0.11, 0.46 | 0.004 |
| TNFα | −1.67 | −2.65, −0.70 | 0.003 |
| CPA3 | 0.09 | 0.03, 0.15 | 0.01 |
| Predictor of CPA3 | |||
| TNFα | 8.69 | 8.08, 9.30 | 0.004 |
| IL-12β | 0.90 | 0.21, 1.60 | 0.04 |
| IRF4 | −1.12 | −1.57, −0.67 | 0.02 |
Interactions Among Cold, Mast Cells, Cytokines, and Adipocytes In Vitro
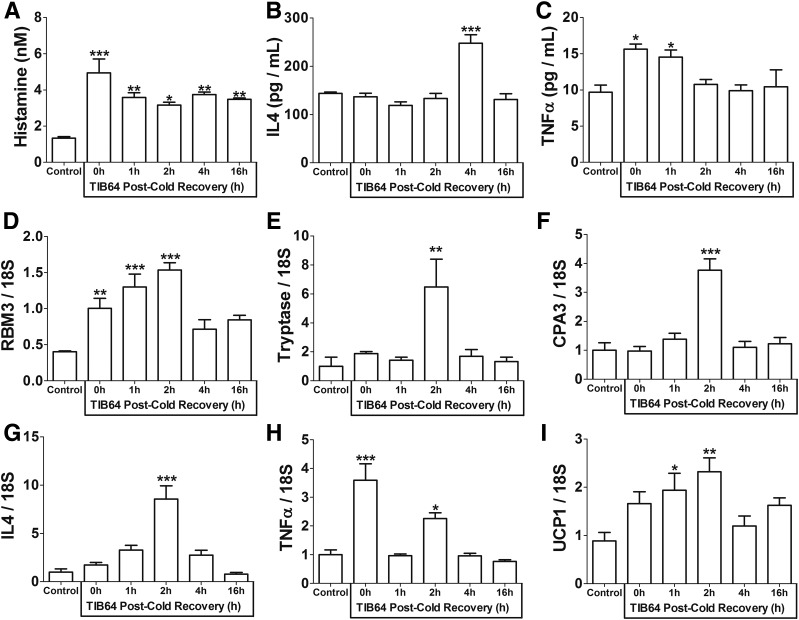
The clinical data above suggest that mast cells and cytokines, such as IL-4, could regulate adipocyte UCP1 expression seasonally; therefore, for a better understanding, we performed in vitro experiments with TIB64 cells, a mouse mast cell line, and 3T3-L1 adipocytes. First, we determined whether mast cells sense the cold. TIB64 cells were cultured at 37°C (control) or for 4 h at 30°C, a temperature that induces cold shock responses in mammalian cells but does not inhibit normal cellular functions (27–31). The cells and media were then harvested at several time points during recovery at 37°C for up to 16 h; media and cells harvested at 0 h after the 30°C incubation had no recovery at 37°C. Cold exposure increased the secretion of histamine from TIB64 mast cells; histamine levels in the media were higher at all time points of 37°C recovery from the 4-h cold shock than histamine levels in the media harvested from mast cells maintained at 37°C (P < 0.05) (Fig. 3A), indicating that cold triggered mast cell histamine release. IL-4 secretion was also induced by the 4-h cold shock, and occurred as a peak at 4 h of recovery at 37°C (P < 0.001) (Fig. 3B). TNFα protein levels were transiently increased at 0 and 1 h of recovery (P < 0.05) (Fig. 3C). We then determined whether cold changed mast cell gene expression. After cold exposure, gene expression of the cold shock protein RBM3 was increased at 0 h (P < 0.01) and remained elevated until 2 h of recovery at 37°C (P < 0.001) (Fig. 3D), indicating that the incubation at 30°C induced a cold shock response. The proteases tryptase and CPA3 were transiently induced by cold at 2 h of recovery at 37°C (tryptase: P < 0.01; CPA3: P < 0.001) (Fig. 3E and F). TIB64 cells increased cytokine expression, with different kinetics observed for TNFα and IL-4. IL-4 gene expression increased 8.6-fold with a peak at 2 h during recovery at 37°C (P < 0.001) (Fig. 3G). TNFα gene expression increased 3.6-fold immediately after the cold exposure (P < 0.001) (Fig. 3H). Finally, UCP1 is induced in mast cells after cold exposure (1 h: P < 0.05; 2 h: P < 0.01) (Fig. 3I). Together, these data suggest that mast cells sense cold and release histamine, IL-4, and TNFα to potentially influence UCP1 gene expression in adipocytes. The induction of TNFα and IL-4 gene expression by mast cells in response to the cold may explain the strong association between these genes and UCP1 in our multivariate analysis. However, this analysis also indicates that the mast cell response to cold is complicated: Both inflammatory and anti-inflammatory cytokines are secreted in a temporal manner.
Figure 3.
Mast cells respond to cold. TIB64 mast cells were incubated at 37°C (control) or at 30°C for 4 h and allowed to recover at 37°C for the indicated time. A: Histamine levels were measured in the media. B: IL-4 protein levels were measured in the media. C: TNFα protein levels were measured in the media. D–I: RBM3, tryptase, CPA3, IL-4, TNFα, and UCP1 mRNA expression was measured in the mast cells. Data are mean ± SEM (n = 3). *P < 0.05, **P < 0.01, ***P < 0.001 (ANOVA with Tukey post hoc test).
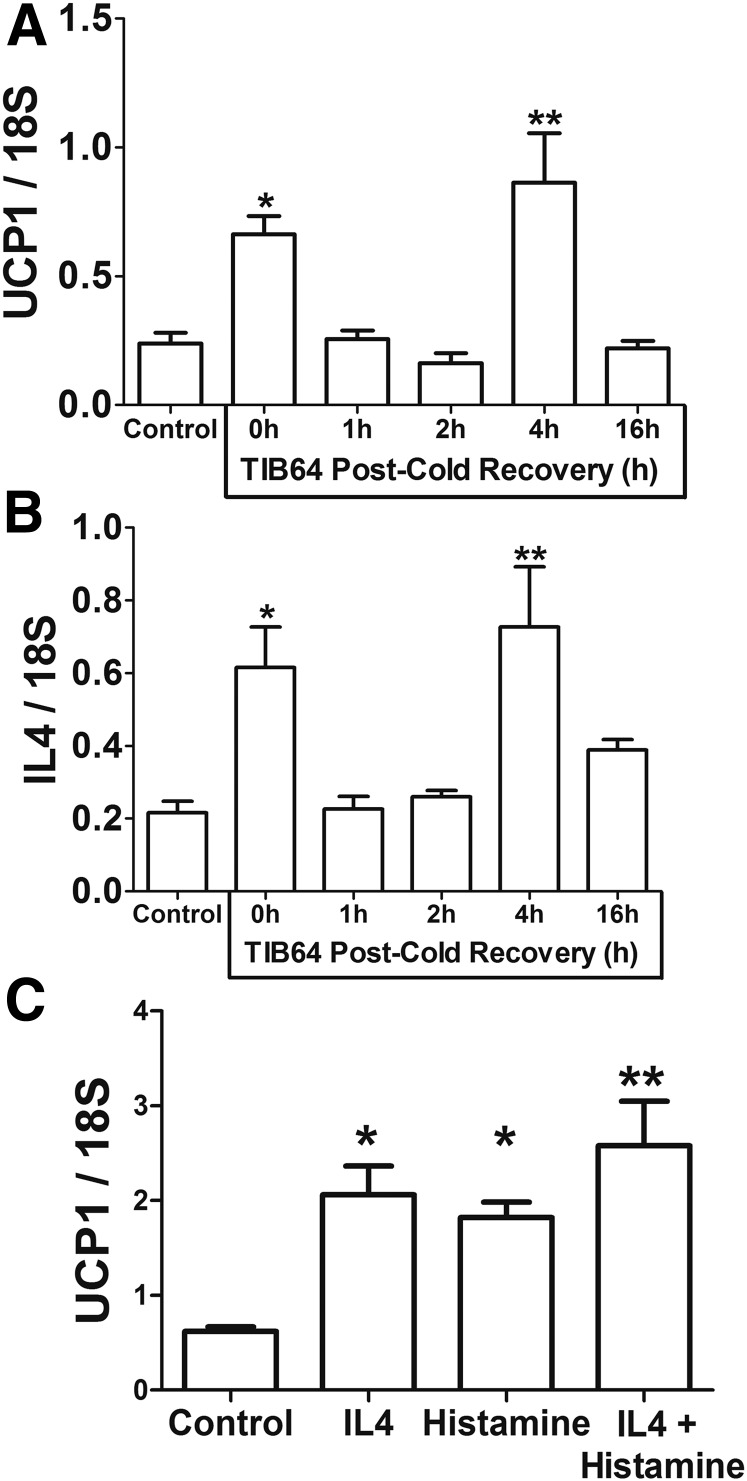
To determine whether the conditioned media (CM) from the cold-shocked mast cells induces UCP1 expression in adipocytes, we added CM from the control and cold-exposed TIB64 cells from Fig. 3 to cultures of differentiated 3T3-L1 adipocytes for 4 h at 37°C. CM at 0 and 4 h of recovery increased UCP1 gene expression in adipocytes (0 h: P < 0.05; 4 h: P < 0.01) (Fig. 4A). IL-4 mRNA was significantly increased in adipocytes treated with medium from the 0-h (P < 0.05) and 4-h recovery (P < 0.01) (Fig. 4B). The results from Fig. 3 indicate that both IL-4 and histamine could be responsible for increasing UCP1. To further explore the factors that induce UCP1, we treated 3T3-L1 adipocytes with recombinant mouse IL-4 or histamine and measured UCP1 gene expression. The response to IL-4 and histamine was time dependent as expected (data not shown). As shown in Fig. 4C, treatment with either IL-4 (P < 0.05), histamine (P < 0.05), or a combination of both (P < 0.01) induced UCP1 gene expression. The results from Fig. 3C demonstrate that TNFα protein levels, which inhibit UCP1 expression (19,20), are increased in the mast cell CM at 0 h of recovery, but nonetheless, UCP1 is induced with 0-h CM (Fig. 4A). Thus, histamine, IL-4, or other factors present in mast cell CM must be able to overcome the inhibitory effects of TNFα on UCP1 expression.
Figure 4.
Mast cell CM from cold-shocked mast cells induces UCP1 expression in adipocytes. Mast cell CM from Fig. 3 was applied to differentiated 3T3-L1 adipocytes for 4 h at 37°C. A and B: Adipocyte gene expression was measured for UCP1 and IL-4. C: Differentiated 3T3-L1 adipocytes were treated with recombinant mouse IL-4 (1 nmol/L), histamine (10 nmol/L), or a combination of both for 3 h. Data are mean ± SEM (n = 3). *P < 0.05, **P < 0.01 (ANOVA with Dunnett post hoc test).
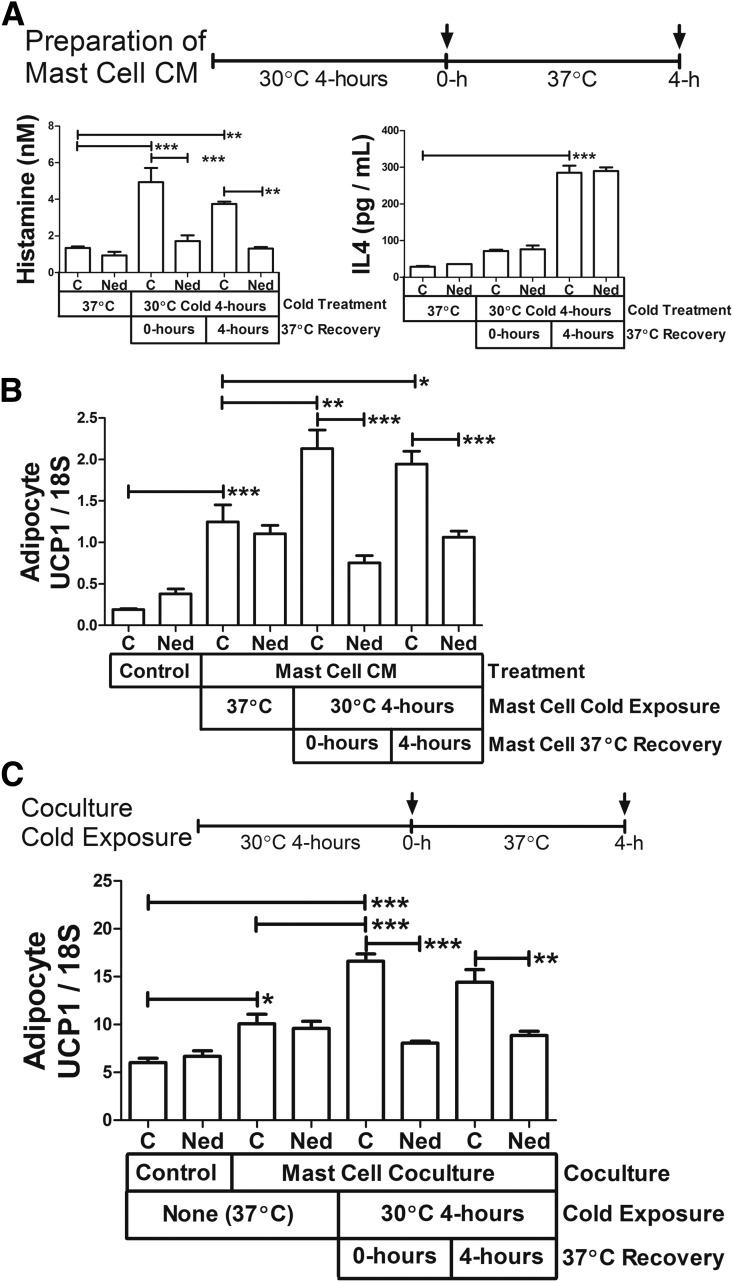
To determine further the contribution of IL-4 and histamine to UCP1 induction by the mast cell CM, we prepared CM from mast cells treated with vehicle or the degranulation inhibitor nedocromil, which blocks histamine release. Histamine and IL-4 were then measured in the 37°C control media and in media from cells incubated at 30°C for 4 h with no recovery at 37°C (0 h) or from cells allowed to recover at 37°C for 4 h. As expected, cold exposure caused histamine and IL-4 to increase in the medium, and nedocromil inhibited histamine secretion (P < 0.001) but not IL-4 secretion (Fig. 5A). Consistent with Fig. 3A, histamine was detected at 0 and 4 h of recovery, suggesting that the mast cells degranulated during the 4-h incubation at 30°C. IL-4 was detected only after 4 h of recovery at 37°C, 2 h after the peak of IL-4 mRNA expression (Fig. 3G). When we treated differentiated 3T3-L1 adipocytes with this mast cell CM at 37°C, UCP1 induction was completely inhibited when nedocromil was used to inhibit mast cell degranulation by 30°C cold treatment (0- or 4-h recovery at 37°C: P < 0.001) (Fig. 5B). This experiment also showed that CM from mast cells cultured at 37°C induced UCP1 (P < 0.001), but this induction was not inhibited by nedocromil.
Figure 5.
Identification of factors in mast cell CM that induce adipocyte UCP1 expression. A: TIB64 mast cells were incubated at 37°C (control) or 30°C (cold) for 4 h in the absence (control) or presence of nedocromil, and the media were harvested (0 h). Another set of 30°C-incubated mast cells was allowed to recover at 37°C for 4 h, and the media were harvested (time course shown above the graph). Shown are the histamine and IL-4 protein levels measured in the media. B: Mast cell CM from A was warmed to 37°C and applied to differentiated 3T3-L1 adipocytes for 4 h at 37°C, and UCP1 mRNA was measured. C: Differentiated 3T3-L1 adipocytes in six-well dishes were cocultured with mast cells in inserts as indicated or were cultured alone (control). Nedocromil was added as indicated. The coculture system was incubated at 30°C or 37°C, and the adipocytes were harvested after 4 h of coculture at 37°C or 0 or 4 h after incubating the coculture at 30°C for 4 h (time course shown above the graph). UCP1 mRNA expression was measured in the adipocytes. Data are mean ± SEM (n = 3). *P < 0.05, **P < 0.01, ***P < 0.001 (ANOVA with a Tukey post hoc test). C, control; Ned, nedocromil.
We also examined adipocyte-mast cell crosstalk with a coculture system in which mast cells in inserts were cocultured with adipocytes; nedocromil was used as a degranulation inhibitor. As shown in Fig. 5C, coculture of mast cells with adipocytes at 37°C increased adipocyte UCP1 expression (P < 0.05). Cold shocking the coculture system further induced UCP1 expression, and this cold shock effect could be inhibited with nedocromil (0-h recovery at 37°C: P < 0.001; 4-h recovery at 37°C: P < 0.01) (Fig. 5C). These results are consistent with the CM experiments, demonstrating an important role for mast cell degranulation in increasing adipocyte UCP1 in response to cold treatment of mast cells. The experiments in Fig. 5B and C also demonstrate that the CM from mast cells that are not cold shocked or mast cell coculture at 37°C increases UCP1 expression in adipocytes, and this mechanism does not rely on degranulation. The identification of the substances secreted by mast cells at 37°C that induce adipocyte UCP1 mRNA will be a goal of future experiments, and we will consider IL-4 because it is secreted and not inhibited by nedocromil (Fig. 5A).
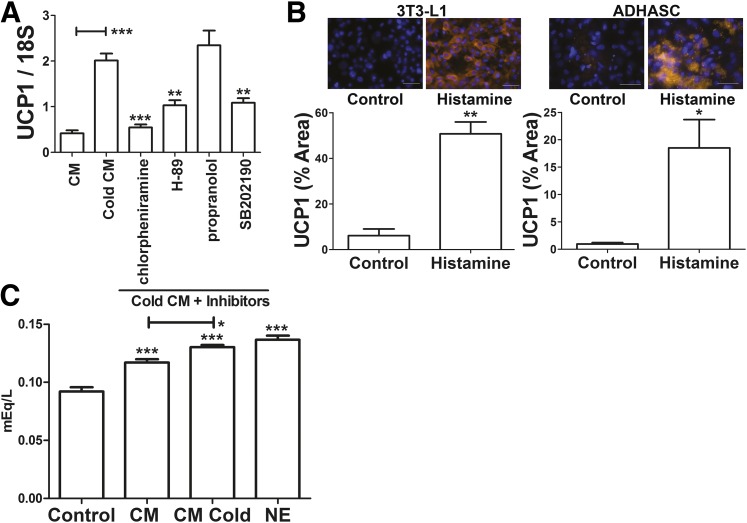
We further evaluated the mechanism of UCP1 induction by testing the effects pharmacological inhibitors of the histamine receptor and of known signaling pathways that regulate UCP1. We treated 3T3-L1 adipocytes with CM from mast cells that were cold shocked and allowed to recover for 4 h at 37°C (Fig. 5A) and the indicated inhibitor. As shown in Fig. 6A, propranolol did not inhibit UCP1 induction by mast cell CM, suggesting that catecholamines are not involved. However, chlorpheniramine, a histamine receptor antagonist, potently inhibited UCP1 mRNA induction (92% inhibition) by mast cell CM (P < 0.001) (Fig. 6A), which is consistent with the potent inhibition of histamine secretion and UCP1 induction by nedocromil treatment. The cAMP-dependent protein kinase (PKA) inhibitor H89 and the p38 inhibitor SB202190 also inhibited UCP1 induction. Together, these data suggest that histamine release by cold exposure of mast cells induces UCP1 mRNA expression by a PKA-dependent pathway consistent with the ability of histamine receptors to induce cAMP signaling pathways (32). We next treated differentiated 3T3-L1 adipocytes and human ADHASC cells with 10 nmol/L histamine for 4 h and measured UCP1 protein expression by immunohistochemistry. As shown in Fig. 6B, histamine potently induced UCP1 protein expression in mouse and human adipocytes (P < 0.01). We then determined whether mast cell CM induces lipolysis. We treated 3T3-L1 adipocytes with media alone as a control, mast cell CM from mast cells at 37°C, and mast cell CM from mast cells cold shocked for 4 h and then allowed to recover for 4 h by using norepinephrine as a positive control. As shown in Fig. 6C, mast cell CM treatment caused free fatty acid levels in the media to increase (P < 0.001), and media from cold-shocked mast cells further stimulated this increase (P < 0.05).
Figure 6.
Histamine in mast cell CM from cold-treated mast cells induces UCP1 expression in adipocytes through a PKA-dependent mechanism. A: Differentiated 3T3-L1 adipocytes were treated with vehicle (control), 5 μmol/L chlorpheniramine, 50 μmol/L H89, 10 μmol/L propranolol, or 100 nmol/L SB202190 in adipocyte differentiation media for 30 min as indicated. The adipocytes were then incubated with 50% mast cell CM (from cold-treated mast cells allowed to recover for 4 h at 37°C [cold CM]) and 50% adipocyte differentiation media containing the same final concentration of inhibitors or vehicle control for 4 h. The cells were harvested, and UCP1 mRNA expression was measured. Data are mean ± SEM (n = 3). **P < 0.01, ***P < 0.001 compared with cold CM treatment (ANOVA with Dunnett post hoc test). B: Differentiated 3T3-L1 or ADHASC adipocytes were treated with vehicle (control) or histamine (10 nmol/L) for 4 h as indicated, and UCP1 immunohistochemistry was performed as described in research design and methods. Representative images of UCP1 staining (orange) and DAPI (blue) identify nuclei. Scale bar = 50 μm. Quantification of UCP1 staining are shown below the images. Data are mean ± SEM (n = 3). *P < 0.05, **P < 0.01 (unpaired Student t test). C: Differentiated 3T3-L1 adipocytes were incubated for 4 h at 37°C with media (control) or CM from mast cells incubated for 8 h at 37°C (CM) or 4 h at 30°C and then 4 h at 37°C (CM cold); 5 μmol/L norepinephrine (NE) was used as a positive control. The media were then replaced with potassium ringers containing 2% fatty acid–free BSA, and the cells were incubated overnight at 37°C. These media were harvested, and free fatty acid concentrations were determined. Data are mean ± SEM (n = 5; NE: n = 3). *P < 0.05, ***P < 0.001 (ANOVA with a Tukey post hoc test).
Finally, we examined histamine receptor expression and regulation in adipose tissue and 3T3-L1 cells. As shown in Supplementary Fig. 1, histamine receptors H1, H2, and H3 are expressed in abdominal fat, and H1 and H3 receptor gene expression is significantly upregulated in the winter (P < 0.05) (Supplementary Fig. 1A and C). To identify the mechanisms, we evaluated the effect of cold, IL-4, and histamine on histamine receptor expression in differentiated 3T3-L1 adipocytes. We measured UCP1 expression as a control and found that UCP1 was induced by cold, IL-4, and histamine as expected (Supplementary Fig. 1D). As shown in Supplementary Fig. 1E–G, histamine receptor expression was induced by IL-4 and histamine but not by cold.
In summary, the analysis of the beiging response of SC WAT of lean human subjects led us to investigate the role of mast cells in the regulation of UCP1 in adipocytes in vitro. Mast cells sense the cold and increase UCP1 expression by multiple mechanisms: IL-4 secretion, histamine release, and stimulation of lipolysis.
Discussion
Adult humans have BAT, which diminishes with age and obesity (5,6,8), and questions exist about whether BAT is present in sufficient quantities to be a therapeutic target to promote weight loss or affect glucose homeostasis. Thus, of interest is the ability of WAT depots to beige. Although activation of the sympathetic nervous system induces beiging, WAT is not nearly as well innervated as BAT, and a number of studies implicate immune cells from the stromal vascular fraction and type 2 cytokines in the beiging of WAT (15–18) in addition to adipocyte autonomous mechanisms (20,33). We previously noted a significant upregulation of UCP1 mRNA expression in SC WAT in the winter and in response to an acute cold stimulus (20). We extend these studies to identify potential mechanisms that increase UCP1 in the winter. These studies implicate mast cells, histamine, histamine receptors, and IL-4 in the seasonal induction of UCP1 in the SC fat of lean humans. In vitro, mast cell degranulation and histamine release increased adipocyte UCP1 and stimulated lipolysis, and pure histamine potently induced UCP1 mRNA and protein expression in adipocytes, which along with the induction of histamine receptors, likely made strong contributions to the seasonal induction of UCP1. A limitation to this study is the small sample size; therefore, future studies are needed to understand the effects of sex, allergies or allergy medications, and exercise duration and intensity.
Human BAT is more metabolically active in the winter (8,34–36), but the impact of increased SC WAT beiging on energy expenditure, glucose and lipid homeostasis, and adipose tissue function in humans remains to be determined. To date, the most potent induction of beiging in humans is burn trauma (37), and beiged SC WAT is estimated to contribute 7% to the increased resting energy expenditure of these subjects (14). The induction of UCP1 mRNA in the cohort of lean subjects of our previous study (20) is lower than the induction in late burn subjects (37), suggesting a much lower contribution to resting energy expediture. However, beige adipose tissue is postulated to have additional effects on WAT function, including functioning as a metabolic sink for glucose and lipids, inducing adipose remodeling, and secreting batokines (13). Determining whether the seasonal increase in beige adipose tissue is functionally important with regard to these effects will be essential.
Type 2 immunity plays an important role in WAT beiging in rodents. Although eosinophils were shown to be important for beige adipocyte induction in mice (16–18), we were unable to detect SIGLEC8, an eosinophil marker, in human thigh fat. However, UCP1 mRNA expression correlated very strongly (P < 0.0001) with IL-4 and CPA3, a protease that is specifically expressed by mast cells. IL-4 mRNA expression also correlated with CPA3, suggesting that mast cells could be an important source of IL-4. Thus, a number of factors that promote UCP1 mRNA expression are upregulated in the winter, and both mast cells and IL-4 could be involved in humans. The identification of TNFα as a predictor of UCP1 expression (Table 1 and Fig. 2E) is surprising because TNFα and other proinflammatory cytokines inhibit UCP1 expression. This association in vivo could be explained in part by mast cells, which increase TNFα gene expression in response to cold in vitro (Fig. 3H) in addition to IL-4 and histamine, which promote UCP1 expression. Thus, the inhibitory effects TNFα are likely countered by histamine and IL-4.
The mast cell response to cold is thus complicated: Mast cells secrete factors that promote or inhibit UCP1 expression in a temporal fashion after cold exposure, which likely contributed to the complicated pattern of UCP1 induction in adipocytes in response to mast cell CM collected at different time points during cold recovery (Fig. 4A). Despite histamine being consistently elevated in the medium during post–cold recovery, UCP1 was not induced at 1, 2, and 16 h postrecovery. A possible explanation is that an inflammatory cytokine is transiently secreted and inhibits UCP1. For instance, TNFα protein levels were transiently induced at 0 and 1 h postrecovery but not at 2 h (Fig. 3C). Thus, other mast cell–secreted factors likely suppress UCP1 mRNA expression at 1, 2, and 16 h postrecovery.
The in vitro studies demonstrate that mast cells degranulate and induce gene expression of a number of genes in response to cold, suggesting that they function as temperature sensors. The cell-autonomous induction of CPA3, IL-4, and TNFα by mast cells in response to the cold that we observed in vitro may explain the induction of these genes in the winter that we observed in human SC WAT. Mast cells have long been known to sense and respond to cold because of their role in cold urticaria (38). The regulation of immune cells in human SC WAT by cold and seasons is largely unexplored, and this study suggests that mast cells are involved in a mechanism where cold is sensed, causing the release of IL-4, TNFα, and histamine.
This study in lean humans suggests that mast cells have beneficial effects on adipocytes. In contrast, in rodent studies that used diet-induced obesity, mast cells contributed to adipose inflammation and reduced UCP1 expression in BAT (23). Thus, in the context of obesity, mast cells are capable of producing factors that promote adipose inflammation and inhibit UCP1 expression. The balance of these factors may be modulated in different settings. Indeed, we found that mast cells produce TNFα in addition to IL-4 and histamine. Thus, mast cell gene expression is likely influenced by obesity, which could alter the balance of factors that inhibit UCP1, such as TNFα, to those that induce UCP1, such as IL-4.
By using degranulation inhibitors and pharmacological inhibition, we identified histamine as the main factor released by mast cells in response to the cold that induces UCP1 expression in adipocytes through a PKA-dependent pathway. The histamine receptor has long been known to increase cAMP and stimulate lipolysis in adipocytes (39), which provides a mechanism for the increase in UCP1 mRNA and protein expression. However, histamine likely has additional effects in vivo. Histamine receptors are expressed on sympathetic nerves in adipose tissue and stimulate sympathetic nerve activity (40). In addition, mast cells are present in BAT, and histamine has been demonstrated to increase blood flow to promote thermogenic responses (41,42).
Although histamine was clearly the main component in mast cell CM on UCP1 induction in vitro, IL-4 released from mast cells could be important in vivo by influencing beige adipogenesis or by influencing other cell types, such as macrophages. Indeed, the correlation between IL-4 and UCP1 in thigh SC WAT was remarkably high, and we found that recombinant IL-4 induced UCP1 expression in adipocytes, which likely involves a different mechanism than UCP1 induction by histamine because of the different nature of the receptors for the molecules. One study suggested that IL-4 stimulates lipolysis through PKA (32), which could be an important part of the mechanism and could allow IL-4 to augment PKA signaling by histamine.
In summary, this study suggests an important role for mast cells in the seasonal induction of UCP1 in SC WAT of lean subjects. Mast cells sense the cold in a cell-autonomous fashion and release histamine and cytokines, including IL-4. The mechanism of UCP1 induction involves direct effects of histamine and/or IL-4 on adipocytes but likely also involves more-complicated interactions with cells of the immune system and perhaps nerves and the vasculature of SC WAT in vivo.
Supplementary Material
Article Information
Acknowledgments. The authors thank Stacy BeBout and Doug Long at the University of Kentucky for assistance with subject recruitment.
Funding. This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R01-DK-107646), National Center for Advancing Translational Sciences (UL1-TR-001998), National Institute of General Medical Sciences (P20-GM-103527-06), and National Center for Research Resources (P20-RR-021954).
Duality of Interest. No conflicts of interest relevant to this article were reported.
Author Contributions. B.S.F., E.E.D.-V., and P.A.K. designed the experiments, analyzed the data, and wrote the manuscript. B.Z. and A.L.C. performed the experiments. P.M.W. and B.D.H. analyzed data. P.A.K. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db16-1057/-/DC1.
References
- 1.Cannon B, Nedergaard J. Brown adipose tissue: function and physiological significance. Physiol Rev 2004;84:277–359 [DOI] [PubMed] [Google Scholar]
- 2.Rothwell NJ, Stock MJ. A role for brown adipose tissue in diet-induced thermogenesis. Nature 1979;281:31–35 [DOI] [PubMed] [Google Scholar]
- 3.Lowell BB, S-Susulic V, Hamann A, et al. . Development of obesity in transgenic mice after genetic ablation of brown adipose tissue. Nature 1993;366:740–742 [DOI] [PubMed] [Google Scholar]
- 4.Virtanen KA, Lidell ME, Orava J, et al. . Functional brown adipose tissue in healthy adults. N Engl J Med 2009;360:1518–1525 [DOI] [PubMed] [Google Scholar]
- 5.Cypess AM, Lehman S, Williams G, et al. . Identification and importance of brown adipose tissue in adult humans. N Engl J Med 2009;360:1509–1517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Marken Lichtenbelt WD, Vanhommerig JW, Smulders NM, et al. . Cold-activated brown adipose tissue in healthy men. N Engl J Med 2009;360:1500–1508 [DOI] [PubMed] [Google Scholar]
- 7.Zingaretti MC, Crosta F, Vitali A, et al. . The presence of UCP1 demonstrates that metabolically active adipose tissue in the neck of adult humans truly represents brown adipose tissue. FASEB J 2009;23:3113–3120 [DOI] [PubMed] [Google Scholar]
- 8.Saito M, Okamatsu-Ogura Y, Matsushita M, et al. . High incidence of metabolically active brown adipose tissue in healthy adult humans: effects of cold exposure and adiposity. Diabetes 2009;58:1526–1531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu J, Boström P, Sparks LM, et al. . Beige adipocytes are a distinct type of thermogenic fat cell in mouse and human. Cell 2012;150:366–376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frontini A, Cinti S. Distribution and development of brown adipocytes in the murine and human adipose organ. Cell Metab 2010;11:253–256 [DOI] [PubMed] [Google Scholar]
- 11.Wu J, Cohen P, Spiegelman BM. Adaptive thermogenesis in adipocytes: is beige the new brown? Genes Dev 2013;27:234–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang QA, Tao C, Gupta RK, Scherer PE. Tracking adipogenesis during white adipose tissue development, expansion and regeneration. Nat Med 2013;19:1338–1344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kajimura S, Spiegelman BM, Seale P. Brown and beige fat: physiological roles beyond heat generation. Cell Metab 2015;22:546–559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Porter C, Chondronikola M, Sidossis LS. The therapeutic potential of brown adipocytes in humans. Front Endocrinol (Lausanne) 2015;6:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyen KD, Qiu Y, Cui X, et al. . Alternatively activated macrophages produce catecholamines to sustain adaptive thermogenesis. Nature 2011;480:104–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee MW, Odegaard JI, Mukundan L, et al. . Activated type 2 innate lymphoid cells regulate beige fat biogenesis. Cell 2015;160:74–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiu Y, Nguyen KD, Odegaard JI, et al. . Eosinophils and type 2 cytokine signaling in macrophages orchestrate development of functional beige fat. Cell 2014;157:1292–1308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rao RR, Long JZ, White JP, et al. . Meteorin-like is a hormone that regulates immune-adipose interactions to increase beige fat thermogenesis. Cell 2014;157:1279–1291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sakamoto T, Takahashi N, Sawaragi Y, et al. . Inflammation induced by RAW macrophages suppresses UCP1 mRNA induction via ERK activation in 10T1/2 adipocytes. Am J Physiol Cell Physiol 2013;304:C729–C738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kern PA, Finlin BS, Zhu B, et al. . The effects of temperature and seasons on subcutaneous white adipose tissue in humans: evidence for thermogenic gene induction. J Clin Endocrinol Metab 2014;99:E2772–E2779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 2003;112:1796–1808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Di Gregorio GB, Yao-Borengasser A, Rasouli N, et al. . Expression of CD68 and macrophage chemoattractant protein-1 genes in human adipose and muscle tissues: association with cytokine expression, insulin resistance, and reduction by pioglitazone. Diabetes 2005;54:2305–2313 [DOI] [PubMed] [Google Scholar]
- 23.Liu J, Divoux A, Sun J, et al. . Genetic deficiency and pharmacological stabilization of mast cells reduce diet-induced obesity and diabetes in mice. Nat Med 2009;15:940–945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spencer M, Yang L, Adu A, et al. . Pioglitazone treatment reduces adipose tissue inflammation through reduction of mast cell and macrophage number and by improving vascularity. PLoS One 2014;9:e102190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spencer M, Yao-Borengasser A, Unal R, et al. . Adipose tissue macrophages in insulin-resistant subjects are associated with collagen VI and fibrosis and demonstrate alternative activation. Am J Physiol Endocrinol Metab 2010;299:E1016–E1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petruzzelli M, Schweiger M, Schreiber R, et al. . A switch from white to brown fat increases energy expenditure in cancer-associated cachexia. Cell Metab 2014;20:433–447 [DOI] [PubMed] [Google Scholar]
- 27.Sonna LA, Fujita J, Gaffin SL, Lilly CM. Invited review: effects of heat and cold stress on mammalian gene expression. J Appl Physiol (1985) 2002;92:1725–1742 [DOI] [PubMed] [Google Scholar]
- 28.Fujita J. Cold shock response in mammalian cells. J Mol Microbiol Biotechnol 1999;1:243–255 [PubMed] [Google Scholar]
- 29.Al-Fageeh MB, Smales CM. Control and regulation of the cellular responses to cold shock: the responses in yeast and mammalian systems. Biochem J 2006;397:247–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shann F. Hypothermia for traumatic brain injury: how soon, how cold, and how long? Lancet 2003;362:1950–1951 [DOI] [PubMed] [Google Scholar]
- 31.Lampe JW, Becker LB. State of the art in therapeutic hypothermia. Annu Rev Med 2011;62:79–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tsao CH, Shiau MY, Chuang PH, Chang YH, Hwang J. Interleukin-4 regulates lipid metabolism by inhibiting adipogenesis and promoting lipolysis. J Lipid Res 2014;55:385–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ye L, Wu J, Cohen P, et al. . Fat cells directly sense temperature to activate thermogenesis. Proc Natl Acad Sci U S A 2013;110:12480–12485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoneshiro T, Matsushita M, Nakae S, et al. Brown adipose tissue is involved in the seasonal variation of cold-induced thermogenesis in humans. Am J Physiol Regul Integr Comp Physiol. 30 March 2016 [Epub ahead of print]. DOI: 10.1152/ajpregu.00057.2015 [DOI] [PubMed]
- 35.Au-Yong IT, Thorn N, Ganatra R, Perkins AC, Symonds ME. Brown adipose tissue and seasonal variation in humans. Diabetes 2009;58:2583–2587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ouellet V, Routhier-Labadie A, Bellemare W, et al. . Outdoor temperature, age, sex, body mass index, and diabetic status determine the prevalence, mass, and glucose-uptake activity of 18F-FDG-detected BAT in humans. J Clin Endocrinol Metab 2011;96:192–199 [DOI] [PubMed] [Google Scholar]
- 37.Sidossis LS, Porter C, Saraf MK, et al. . Browning of subcutaneous white adipose tissue in humans after severe adrenergic stress. Cell Metab 2015;22:219–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kaplan AP, Garofalo J, Sigler R, Hauber T. Idiopathic cold urticaria: in vitro demonstration of histamine release upon challenge of skin biopsies. N Engl J Med 1981;305:1074–1077 [DOI] [PubMed] [Google Scholar]
- 39.Grund VR, Goldberg ND, Hunninghake DB. Histamine receptors in adipose tissue: involvement of cyclic adenosine monophosphate and the H2-receptor in the lipolytic response to histamine in isolated canine fat cells. J Pharmacol Exp Ther 1975;195:176–184 [PubMed] [Google Scholar]
- 40.Shen J, Yao JF, Tanida M, Nagai K. Regulation of sympathetic nerve activity by l-carnosine in mammalian white adipose tissue. Neurosci Lett 2008;441:100–104 [DOI] [PubMed] [Google Scholar]
- 41.Desautels M, Wollin A, Halvorson I, Muralidhara DV, Thornhill J. Role of mast cell histamine in brown adipose tissue thermogenic response to VMH stimulation. Am J Physiol 1994;266:R831–R837 [DOI] [PubMed] [Google Scholar]
- 42.Rothwell NJ, Stock MJ, Wyllie MG. Effects of histamine antagonists on noradrenaline-stimulated blood flow and oxygen consumption of brown adipose tissue in the rat. Pflugers Arch 1984;402:325–329 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.