Abstract
Prostate organogenesis is a complex process that is primarily mediated by the presence of androgens and subsequent mesenchyme-epithelial interactions. The investigation of prostate development is partly driven by its potential relevance to prostate cancer, in particular the apparent re-awakening of key developmental programs that occur during tumorigenesis. However, our current knowledge of the mechanisms that drive prostate organogenesis is far from complete. Here, we provide a comprehensive overview of prostate development, focusing on recent findings regarding sexual dimorphism, bud induction, branching morphogenesis and cellular differentiation.
KEY WORDS: Androgen signaling, Development, Differentiation, Induction, Prostate
Summary: This Review article provides a comprehensive overview of prostate development, focusing on recent findings regarding sexual dimorphism, bud induction, branching morphogenesis and cellular differentiation.
Introduction
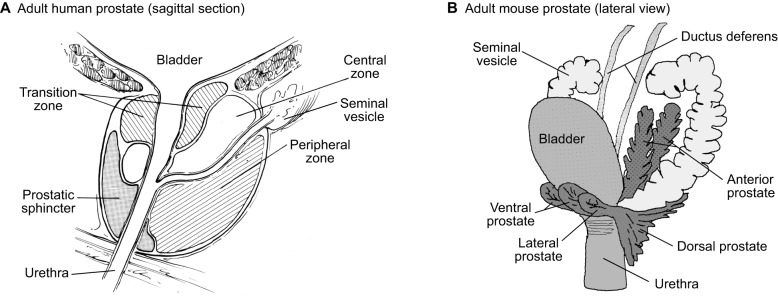
The human prostate is a small walnut-sized organ that is located just below the bladder and surrounds the urethra (Fig. 1). It contains a system of branching ducts comprising pseudo-stratified epithelium surrounded by a fibromuscular stroma. The prostate is a male sex accessory gland that functions by producing and secreting fluids that contribute to the ejaculate, and thereby significantly enhances male fertility. Intriguingly, the prostate is highly susceptible to oncogenic transformation at a frequency significantly greater than that of other male secondary sexual tissues, such as the seminal vesicles. Indeed, approximately one in seven men will be diagnosed with prostate cancer during their lifetime (Siegel et al., 2016). Consequently, this disease has been the focus of intense investigation in order to understand its pathobiology and to provide improved treatment (Attard et al., 2016; Shen and Abate-Shen, 2010). It has long been hypothesized that malignancy, including that of the prostate, occurs due to a re-awakening of the developmental processes that occur during organogenesis. Although this concept that tumors are caricatures of organogenesis has been proposed for some time (Pierce and Speers, 1988), more recent studies have demonstrated key similarities in gene expression programs between prostate organogenesis and cancer (Pritchard et al., 2009; Schaeffer et al., 2008). Thus, there is considerable rationale to gain a comprehensive understanding of the fundamental mechanisms behind prostate development.
Fig. 1.
Overview of prostate anatomy. (A,B) Schematics of the adult human (A) and adult mouse (B) prostate gland. Key structures and regions of the prostate are indicated. Adapted from Cunha et al. (1987) and McNeal (1969) and reproduced from Abate-Shen and Shen (2000).
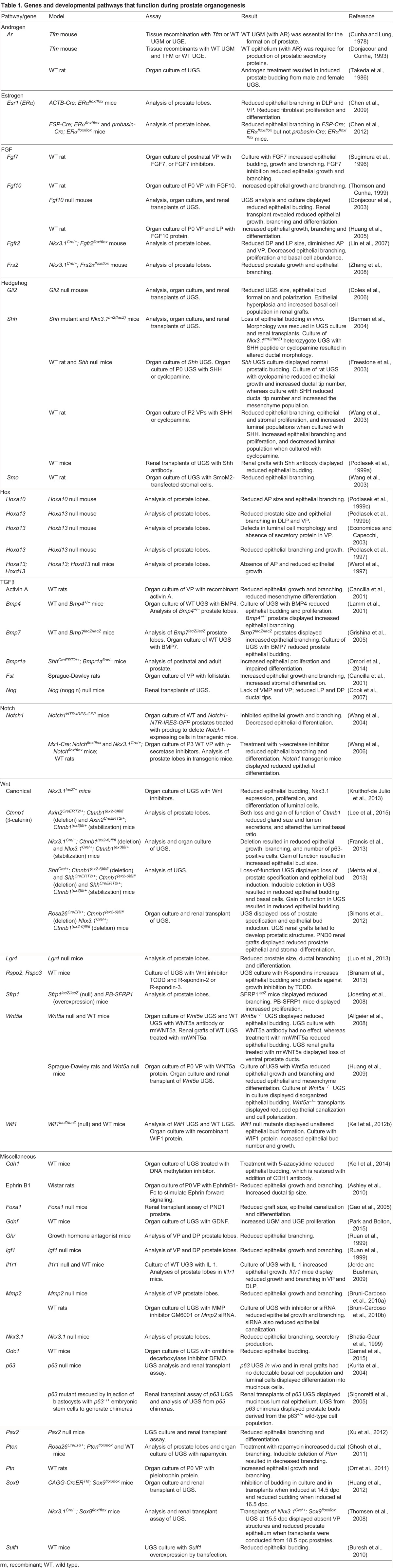
Here, we review what is currently known about the cellular and molecular mechanisms of prostate development, highlighting areas that require further investigation. We describe successive stages of prostate organogenesis, from the specification of prostate identity and epithelial bud induction to cell lineage specification and differentiation. In particular, we focus on the major signaling pathways that mediate androgen function and mesenchymal-epithelial interactions. Although other signaling pathways are also relevant for prostate organogenesis, these will not be described in detail and are instead summarized in Table 1. Finally, it should be noted that a large proportion of our knowledge regarding prostate organogenesis has been elucidated using rat and mouse models, so we also discuss similarities and differences in prostate organogenesis between rodents and humans.
Table 1.
Genes and developmental pathways that function during prostate organogenesis
An overview of prostate development and structure
During embryogenesis, the primitive urogenital sinus – the structure from which the prostate arises – forms as a caudal extension of the hindgut. Indeed, lineage tracing has shown that the entire length of the primitive urogenital sinus, including the distal urethra, has an endodermal origin (Seifert et al., 2008). Both the urogenital sinus and hindgut are initially joined as a single excretory tract at the embryonic cloaca. The subsequent division of the cloaca into separate urogenital and anorectal tracts occurs by 8 weeks of gestation in humans and 13.5 days post coitum (dpc) in the mouse (Hynes and Fraher, 2004); interestingly, this process has long been thought to occur by formation of a urorectal septum, but an alternative model has recently been proposed (Huang et al., 2016). The primitive urogenital sinus is then subdivided into the bladder at its rostral end, the urogenital sinus (UGS) in the middle, and the penile urethra caudally. The prostate forms through epithelial budding from the UGS starting at approximately 10 weeks of gestation in humans (Kellokumpu-Lehtinen et al., 1980), and at 17.5 dpc in the mouse (Bhatia-Gaur et al., 1999; Cunha et al., 1987; Lung and Cunha, 1981). Prostate organogenesis then continues under the influence of circulating androgens through birth and pre-pubertal stages, until the prostate reaches its mature size during puberty. Notably, a detailed description of the anatomy of the developing urogenital system in the mouse has been recently published (Georgas et al., 2015).
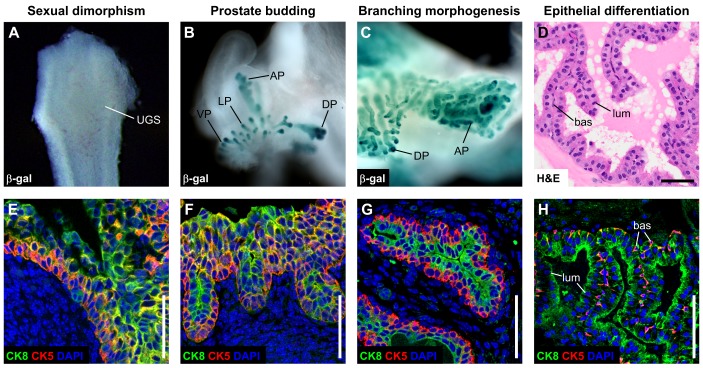
Conceptually, the process of prostate organogenesis can be divided into four stages (Fig. 2). In the first stage, prior to epithelial budding, developmental cues that are directly or indirectly mediated by androgens result in prostate induction in males. In the second stage, after prostatic fate is determined, the urogenital sinus epithelium (UGE) buds into the surrounding urogenital sinus mesenchyme (UGM), initiating tissue outgrowth and branching morphogenesis to form a system of ducts composed of solid epithelial cords. This process involves paracrine signaling to the UGE from the UGM, in which androgen receptor (AR) function is necessary to mediate epithelial outgrowth. In the third stage, ductal outgrowth is associated with a process of branching morphogenesis, which gives rise to the mature ductal network. In the mouse, this process results in the formation of four sets of prostatic lobes (Fig. 1B), each with distinct patterns of ductal branching, whereas in humans this process leads to the formation of different prostatic zones (Fig. 1A) within a uni-lobular organ (Cunha et al., 1987; Timms, 2008). In the final stage, the solid epithelial cords undergo canalization to form the ductal lumen and cytodifferentiation to give rise to functional glandular epithelium with fully differentiated cell types.
Fig. 2.
Stages of prostate organogenesis. Whole-mount images of Nkx3.1lacZ/+ mouse UGS stained for β-galactosidase (β-gal) activity, at 16.5 dpc (A), P2 (B) and P14 (C). (D) Hematoxylin & Eosin (H&E) staining of the adult mouse prostatic duct. (E,F) Immunofluorescence staining for cytokeratin 5 (CK5) and cytokeratin 8 (CK8) in the mouse prostate epithelium, at 16.5 dpc (E), P2 (F), P14 (G) and 8 weeks old (H). These images illustrate four stages of prostate organogenesis: sexual dimorphism, budding, branching morphogenesis and epithelial differentiation. At 16.5 dpc, the male UGS is devoid of epithelial buds (A) and the majority of urethral epithelial progenitors express CK5 and CK8 (E). Epithelial budding is induced shortly afterwards under the influence of androgens, resulting in the main ductal structures of the four prostatic lobes (B), during which CK5 and CK8 co-expression remains abundant (F). Extensive branching morphogenesis continues during postnatal development (C), when basal and luminal populations become segregated (G), although subsets of intermediate cells are still observed. In the adult prostate, the basal and luminal cells express specific cytokeratin profiles (H), and prostatic excretions can be observed in the ductal lumen (D). AP, anterior prostate; bas, basal; DP, dorsal prostate; LP, lateral prostate; lum, luminal; VP, ventral prostate. Scale bars: 50 µm.
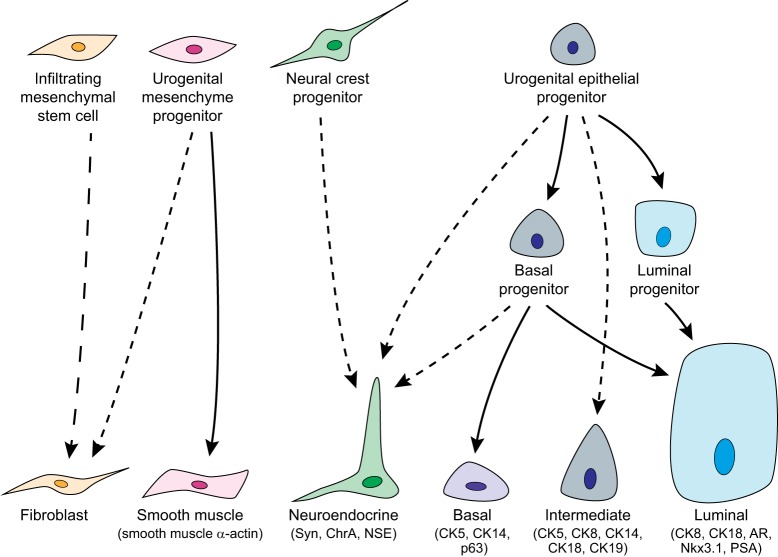
The mature prostate epithelium contains several distinct cell types that differ in their morphology (Figs 2, 3). The luminal cells are tall columnar epithelial cells that express cytokeratins (CK; also known as KRT) 8 and 18 as well as secretory proteins such as prostate specific antigen (PSA; also known as KLK3) (Liu et al., 1997; Verhagen et al., 1988, 1992; Wang et al., 2001). Below the luminal layer are non-secretory basal cells that line the basement membrane and express CK5, CK14 and p63 (Trp63) (Signoretti et al., 2000; Verhagen et al., 1988, 1992; Wang et al., 2001). Notably, mouse and human prostate basal cells express low or undetectable levels of AR compared with luminal cells, nearly all of which express high levels of AR (El-Alfy et al., 1999; Mirosevich et al., 1999). Within the basal layer are occasional intermediate cells that co-express luminal and basal markers as well as additional markers such as CK19 (De Marzo et al., 1998; Wang et al., 2001; Xue et al., 1998); despite considerable speculation, it remains unclear whether intermediate cells represent a functionally distinct cell type. Finally, rare neuroendocrine cells correspond to basally localized cells that express secreted neuropeptides and other hormones, and often display a dendritic-like process that contacts the glandular lumen (Abrahamsson, 1999).
Fig. 3.
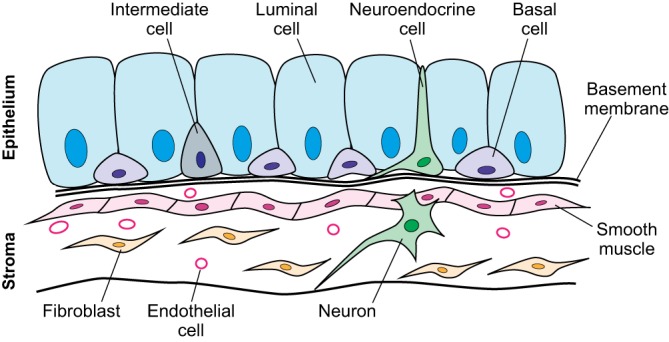
Differentiated cell types in the prostate. Schematic of cell types in the adult prostate. The epithelial compartment is composed of basal cells that line the basement membrane, secretory luminal cells, and rare intermediate and neuroendocrine cell populations. These epithelial ducts are adjacent to a stromal compartment that includes smooth muscle cells, fibroblasts, and vascular and neural components.
The mesenchymal compartment of the prostate also contains a number of differentiated cell types (Fig. 3). For example, cells of the embryonic UGM form a layer of smooth muscle, which lines the epithelium and exhibits contractile activity to aid expulsion of prostatic fluid into the ejaculate (Hayward et al., 1996b). The adult prostate stroma also contains a large population of mature fibroblasts that secrete extracellular matrix, consisting of fibrillar proteins, glycoproteins and proteoglycans that form a structural network and mediate growth factor signaling (Tuxhorn et al., 2001). Finally, other components of the stroma include blood vessels, lymphatics, nerves, and immune cells, which have been implicated in stem cell regulation as well as tumorigenesis within the prostate.
A comparison of rodent and human prostate development, anatomy and histology
Although analyses of archival human tissue samples have provided descriptive insights into prostate development, functional and mechanistic studies of human prostate organogenesis have been limited, and have depended on the use of animal models, particularly genetically engineered mice. Key features of androgen-mediated prostate induction, epithelial budding, branching morphogenesis and differentiation, as well as the pathways that drive these processes, are similar in rodent and human prostate organogenesis. However, there are significant differences between rodents and humans in terms of the temporal and spatial regulation of these processes. In humans, prostate epithelial budding occurs relatively early during embryogenesis, followed by interrupted phases of organogenesis at postnatal and pubertal stages (Cunha et al., 1987). In contrast, prostate epithelial budding initiates at late fetal stages in the mouse and rat, but the remainder of organogenesis occurs continuously during postnatal stages through puberty.
The gross morphology and histology of the human and rodent prostates (Fig. 1) also display several important differences (Ittmann et al., 2013; Shappell et al., 2004). One of the first studies of human prostate development observed that epithelial buds emerge from the UGE in defined pairs, suggesting that the human gland comprises multiple lobes (Lowsley, 1912). In the adult, however, such lobes are no longer recognizable (Price, 1963). Instead, the human prostate is uni-lobular, containing three zones – the central, transition and peripheral zones – that are believed to originate from five pairs of epithelial buds (McNeal, 1988). The central zone branches anteriorly from the prostatic urethra to surround the ejaculatory duct and constitutes approximately 20% of the prostate. The transition zone encircles the urethra and comprises approximately 10% of the prostate volume; it also represents the site of benign prostatic hyperplasia (BPH), a tissue enlargement that is unrelated to malignancy (McNeal, 1978; Timms and Hofkamp, 2011). Finally, the peripheral zone constitutes approximately 70% of the prostate, and represents the most common site of malignancy (McNeal, 1981). In addition to these epithelial components, the human prostate also has an anterior fibromuscular stroma that covers the glandular tissue, as well as a fibrous capsule that covers the exterior of the organ (McNeal, 1988).
In contrast, the rodent prostate is composed of distinct pairs of lobes (Fig. 1B), termed the anterior prostate (AP), ventral prostate (VP), lateral prostate (LP) and dorsal prostate (DP), which differ significantly in their branching patterns, histology and expression of secretory proteins (McNeal, 1983; Shappell et al., 2004; Thomson and Marker, 2006); the dorsal and lateral lobes are frequently referred to together as the dorsolateral lobes (DLPs). Consistent with the distinct identity of these lobes, several genetically engineered mouse mutants display lobe-specific mutant phenotypes, including null mutants for Nog (noggin), Sox9 and Wnt5a, as well as mutants with conditional deletion of Fgfr2 in the prostate epithelium (Table 1). Interestingly, despite the differences in adult prostate anatomy between mouse and human, their patterns of prostate epithelial budding during early organogenesis have significant similarities (Timms, 2008). However, the relationship of the early budding pattern of the human prostate to the zonal architecture of the adult tissue remains unclear. In this regard, although previous studies have suggested that the mouse DLP most closely resembles the human peripheral zone (Berquin et al., 2005; Price, 1963), the current consensus among veterinary and human pathologists is that there is no clear correspondence between mouse prostate lobes and human prostate zones (Ittmann et al., 2013; Shappell et al., 2004).
There are also differences between the human and rodent prostate in terms of the architecture of their epithelial and stromal compartments. Notably, although luminal, basal, intermediate and neuroendocrine cell populations are present in both the human and rodent prostate epithelium, the basal cell layer appears to be continuous in histological sections of the human prostate, but not the mouse prostate; instead, rodent basal cells may contact each other through long cytoplasmic processes (Hayward et al., 1996c). Thus, there is a 1:1 ratio of basal to luminal cells in the human prostate, whereas the ratio in mouse and rat is approximately 1:7 (El-Alfy et al., 2000). Furthermore, the stromal tissue surrounding the epithelium also differs between the two species. Human prostate ducts are contained within a continuous thick mass of fibromuscular stroma; in contrast, rodent prostate ducts contain epithelium surrounded by a thin smooth muscle layer and are joined by loose connective tissue to neighboring ducts (Ittmann et al., 2013; Shappell et al., 2004), except for the most proximal prostate ducts, which are adjacent to a thicker stromal layer. As a consequence, although the stromal to epithelial ratio varies between the mouse and rat lobes as well as human zones, there is less stromal content in the rodent compared with the human prostate, where stromal and epithelial cells are present in equal numbers (Bartsch and Rohr, 1980).
Prostate induction: sexual dimorphism in the urogenital sinus
Sexual dimorphism of the UGS is reflected in its ability to form the prostate in males versus a portion of the vagina in females. Formation of the prostate is initiated by the circulating androgen testosterone, which is synthesized at significantly higher levels in male embryos than in female embryos (Pointis et al., 1979, 1980). Testosterone is produced by Leydig cells of the testis, starting at approximately 9 weeks of gestation in humans (Siiteri and Wilson, 1974), and at 13-14 dpc in mice (Pointis et al., 1979, 1980). Once testosterone reaches the UGS, it is converted into its more potent metabolite dihydrotestosterone (DHT) by 5α-reductase (Berman et al., 1995; Ekman, 2000; Ferraldeschi et al., 2013). DHT then binds to AR, a steroid hormone receptor that localizes to the nucleus upon ligand binding and acts as a transcription factor.
Owing to the essential role of androgens, sexual dimorphism of the UGS can be generated independently of genetic sex. For example, XY embryos that lack functional AR develop female external genitalia and fail to form a prostate gland (Brown et al., 1988; Lubahn et al., 1989; Lyon and Hawkes, 1970). Conversely, the UGS of XX mouse embryos or XY embryos that are defective in testis development can develop prostatic structures if administered sufficient levels of androgens in utero or in organ culture ex vivo, or if grafted into male hosts (Berman et al., 2004; Cunha, 1975; Lasnitzki and Mizuno, 1977; Takeda et al., 1986). Importantly, the ability of androgens to induce prostate budding is temporally restricted, as the UGS of XX mice rapidly loses androgen responsiveness during postnatal day (P) 0 to P5, both in grafts and in organ culture (Cunha, 1975; Thomson et al., 2002).
Classical tissue recombination assays have demonstrated that prostate formation requires paracrine interactions between the UGM and UGE (Cunha et al., 1987). In such tissue recombination assays, isolated epithelial and mesenchymal components from the same or different tissues and/or donors are combined and implanted under the renal capsule of immunodeficient hosts (Hayward, 2002). By themselves, UGM or UGE are unable to grow or differentiate in renal grafts, but recombination of UGE with heterologous UGM results in prostate tissue. Importantly, it was shown that prostate specification is largely conferred by the UGM, as recombination of bladder epithelium with UGM also generates prostate tissue (Donjacour and Cunha, 1993). Indeed, epithelial cells of several other endodermal and ectodermal tissue types, including vaginal, mammary gland and skin epithelial tissues, can also be induced by the UGM to form prostate tissue in tissue recombinants (Cunha, 1975; Taylor et al., 2009). These findings suggest that prostate formation occurs as a result of an instructive induction, in which the UGM specifies prostate identity in the adjoining UGE. However, contrary to this, it has been shown that seminal vesicle mesenchyme can induce bladder epithelium to form prostate in tissue recombination assays (Donjacour and Cunha, 1995). This finding that two heterologous tissues can be combined to form prostate suggests that the mesenchymal signal(s) from the urogenital and seminal vesicle mesenchyme is similar, whereas the specificity of the response is at least partially conferred by the epithelium. Additional complexity in mesenchymal signaling has been suggested by a recent study indicating a potential role for the caudal Müllerian duct mesenchyme (CMDM) acting together with the UGM to induce prostate formation and, in particular, to specify prostate versus urethral glands (Brechka et al., 2016).
The specific roles of AR in the UGM and UGE have also been investigated. Tissue recombination studies using Tfm (Testicular-feminization) mice, which are AR null mutants, have shown that AR is necessary in the UGM for prostate induction; wild-type UGE does not form prostate buds if combined with Tfm UGM (Cunha and Lung, 1978; Donjacour and Cunha, 1993). Subsequently, AR is required in the epithelium for the expression of prostatic secretory proteins by the epithelium, and for promoting differentiation of the surrounding mesenchyme into smooth muscle (Cunha et al., 1992; Cunha and Young, 1991; Donjacour and Cunha, 1993; Hayward et al., 1998). Thus, prostate induction requires functional AR expressed by the mesenchyme, but differentiation of both epithelial and mesenchymal compartments requires functional AR in the epithelium. This model is further supported by more recent studies using conditional gene targeting of AR in vivo. In particular, deletion of AR in the majority of stromal fibroblasts and smooth muscle cells leads to the formation of prostate ducts with reduced size and defective branching morphogenesis (Lai et al., 2012), consistent with partial loss of stromal AR function.
Interestingly, small paraurethral glands (sometimes termed Skene's glands) that resemble a rudimentary prostate are present in female rats and humans, but not mice (Mahoney, 1940; Zaviacic and Ablin, 1998). Furthermore, these glands express PSA and prostatic acid phosphatase (PAP; also known as ACPP) (Dietrich et al., 2011; Zaviacic and Ablin, 2000), suggesting that at least some aspects of prostate development also occur in females. Although some reports suggest that Skene's glands might not be paralogous to the male prostate, as they are located caudally along the UGS, other studies have identified prostate-like epithelial buds in females that do emerge in regions analogous to prostatic buds in males (Huffman, 1948; Thomson et al., 2002; Timms et al., 1999). It is possible that low levels of androgens in conjunction with AR expression in the XX mesenchyme could be sufficient for induction of prostate-like buds in females (Thomson, 2008). However, studies in rats have suggested that the presence of prostate-like buds in female embryos is more common when embryos are in proximity to other female embryos within the maternal uterus, raising the possibility that residual estrogens play a role in their induction (Timms et al., 1999).
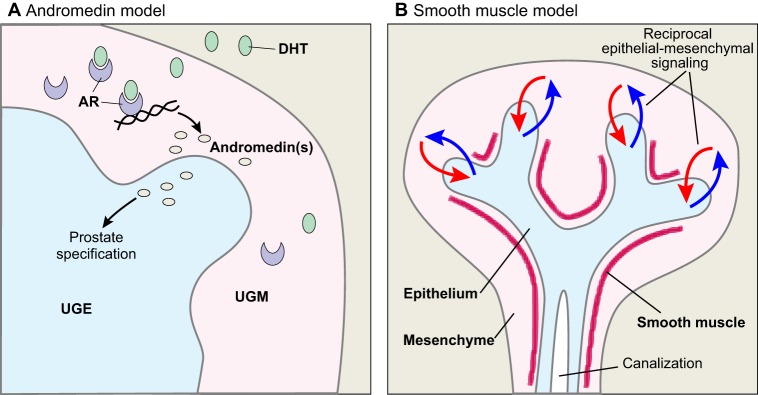
Epithelial budding and specification
Under the influence of androgens, the UGE buds into the surrounding UGM and initiates prostate tissue outgrowth. However, although the activation of AR expressed in the UGM is believed to drive UGE specification and differentiation, the molecular mechanisms mediating this inductive process are poorly defined. In particular, the identity of the intermediary signal(s) from the UGM to the UGE is unclear, and the mechanism of its regulation by AR signaling is unknown. At present, there are two major hypotheses for how androgens mediate prostate epithelial induction and budding: the andromedin model and the smooth muscle model (Fig. 4).
Fig. 4.
Models of prostate bud induction. (A) In the andromedin model, androgen signaling through androgen receptor (AR) expressed in the urogenital mesenchyme (UGM) results in the production of one or more signaling factors (andromedins) that directly induce prostate budding in the adjacent urogenital epithelium (UGE). (B) In the smooth muscle model, signals that promote epithelial budding occur constitutively, and androgen signaling within the mesenchyme indirectly controls this process. In this model, androgen signaling is proposed to regulate the differentiation of smooth muscle around the emerging prostate ducts, thereby inhibiting further epithelial budding in regions where smooth muscle has already formed. DHT, dihydrotestosterone.
The andromedin hypothesis
In the andromedin model (Fig. 4A), ligand binding to AR in the UGM results in upregulation of the activity of a signaling factor(s) – an andromedin – that in turn acts directly upon the UGE to mediate prostate formation (Tenniswood, 1986; Thomson, 2008). Thus, in the simplest scenario, candidate andromedins should: (1) be expressed by the mesenchyme, (2) be upregulated by androgen signaling and (3) induce growth and prostate differentiation of the epithelium. Several candidate andromedins have been proposed over the years but, to date, no single candidate fully satisfies all of these criteria. However, it is conceivable that distinct signaling factors might provide andromedin function acting in combination, but this possibility has not yet been tested.
Fibroblast growth factor (FGF) 7 and FGF10 were among the first molecules to be suggested as candidate andromedins (Lu et al., 1999; Yan et al., 1992). Both Fgf7 and Fgf10 are expressed in the mouse UGM in vivo, and addition of exogenous FGF7 or FGF10 can promote epithelial growth and branching in UGS explants in culture (Finch et al., 1995; Sugimura et al., 1996; Thomson and Cunha, 1999). Despite these similarities, FGF7 and FGF10 also display notable differences, as FGF7 can stimulate epithelial budding and ductal branching in the absence of DHT in neonatal prostate organ culture (Sugimura et al., 1996), whereas FGF10 is unable to induce epithelial budding in the absence of DHT (Donjacour et al., 2003). Furthermore, although Fgf7 null mutants lack a prostate phenotype (Guo et al., 1996), Fgf10 null mutants either lack budding completely or occasionally form rudimentary prostate buds (Donjacour et al., 2003); interestingly, the epithelial-specific deletion of their cognate receptor Fgfr2 results in a small prostate that lacks anterior and ventral lobes (Lin et al., 2007). However, Fgf7 and Fgf10 do not appear to display sexually dimorphic expression and are not regulated by androgens (Thomson and Cunha, 1999; Thomson et al., 1997), suggesting that they are not andromedins. Instead, FGF10 might act to stabilize and promote the growth of nascent prostate buds, rather than be required for their initial formation (Donjacour et al., 2003).
There is evidence that at least some potential andromedins show sexually dimorphic expression. In particular, several Wnt ligands are upregulated during the period of prostatic bud formation (Mehta et al., 2011; Pritchard et al., 2009; Zhang et al., 2006). Furthermore, analyses using sensitive transgene reporters have shown that Wnt signaling activity is present in the mouse UGM prior to prostate budding and subsequently in both the mesenchyme and ductal tips during outgrowth (Kruithof-de Julio et al., 2013; Mehta et al., 2011). Consistent with these findings, downstream targets of canonical Wnt signaling such as Lef1 are expressed in epithelial cells of prostate ductal tips (Francis et al., 2013; Mehta et al., 2013; Wu et al., 2011). Notably, conditional targeting of β-catenin, the central mediator of canonical Wnt signaling, results in formation of prostate rudiments that lack expression of the early prostate-specific epithelial marker Nkx3.1 (Nkx3-1) (Francis et al., 2013; Mehta et al., 2013; Simons et al., 2012). However, there is currently no direct evidence that Wnt ligands are androgen regulated, and thus they do not currently fulfill all of the criteria for being considered andromedins. Interestingly, the Wnt inhibitor Wif1 is expressed at higher levels in the UGM of males and is androgen regulated, but Wif1 null mutants lack a prostate phenotype (Keil et al., 2012b), and consequently the role of Wif1 in prostate formation remains unclear.
It is possible that andromedins, although not showing sexually dimorphic expression themselves, might elicit sexually dimorphic responses through downstream components of their signaling pathways. For example, retinoic acid activity is high in the mouse UGM and can promote epithelial budding in culture (Vezina et al., 2008). Formation of retinoic acid is catalyzed by aldehyde dehydrogenases (ALDH), and ALDH inhibitors block prostate bud formation by the UGS in explant culture in the presence of DHT (Bryant et al., 2014). Interestingly, Aldh1a1 is only expressed in the male but not female UGS prior to prostate budding in vivo, whereas treatment of the female UGS with DHT in culture will induce Aldh1a1 expression (Bryant et al., 2014). Similarly, other candidate andromedins such as FGFs might also exert their effects through sex-specific expression of downstream pathway components (Schaeffer et al., 2008; Thomson and Cunha, 1999; Thomson et al., 1997).
The smooth muscle hypothesis
The smooth muscle hypothesis (Fig. 4B) proposes that androgen signaling has indirect effects on epithelial growth by regulating the differentiation of smooth muscle, which forms a barrier between the inductive mesenchyme and the UGE to block further epithelial budding and outgrowth (Hayward et al., 1996b; Thomson and Marker, 2006). This model could be particularly applicable for the formation of the ventral prostate lobe, in which the inductive capabilities of the UGM appear to be concentrated in a region of dense peripheral mesenchyme cells termed the ventral mesenchymal pad (VMP) (Timms, 2008; Timms et al., 1995). Androgen signaling reduces the extent of smooth muscle formation, which might allow signaling factors that are constitutively active in the VMP to reach the epithelium (Chrisman and Thomson, 2006; Thomson et al., 2002).
However, androgens also appear to be essential for the differentiation of smooth muscle during prostate development, and castration of adult hosts results in a loss of smooth muscle cells (Hayward et al., 1996b). Furthermore, at least some of the signals that control smooth muscle formation might be epithelial, as the UGE is essential for smooth muscle differentiation by the UGM in tissue recombinants (Cunha et al., 1983, 1992). Moreover, the species-specific properties of the smooth muscle in tissue recombinants are conferred by the species origin of the epithelium, rather than the mesenchyme (Hayward et al., 1998).
In summary, these two models for how androgens induce prostate epithelial budding are not mutually exclusive, and might even synergize. It is likely that the mesenchyme produces secreted factors that induce epithelial growth, and that androgen signaling regulates some of these factors or downstream pathway components. Moreover, the diffusion and/or activity of these secreted signaling factors could be blocked by the formation of smooth muscle. Notably, smooth muscle differentiation might reflect an inhibitory feedback loop mediated by androgen signaling within the stroma, or might instead correspond to a reciprocal paracrine feedback loop involving signaling from prostate epithelium that has responded to mesenchymal andromedins (Fig. 4B).
Mechanisms of epithelial specification
Although the studies described above have identified factors that might signal between the mesenchyme and epithelium during initial prostate budding, relatively little is known about how these paracrine signals regulate the activity of transcriptional regulators to mediate epithelial specification. However, studies in genetically engineered mice have implicated several transcriptional regulators as key players in the specification and differentiation of the prostate epithelium (Table 1).
Of particular interest is the winged-helix transcription factor Foxa1, which is broadly expressed in endodermal derivatives, including in the UGE prior to prostate induction and subsequently in the prostate luminal epithelium (Mirosevich et al., 2005). Although Foxa1 null mouse mutants have a neonatal lethal phenotype, prostate rudiments can be rescued by renal grafting, thereby allowing the analysis of prostate tissue phenotypes (Gao et al., 2005). Such rescued prostate tissue displays basal cell hyperplasia, loss of luminal secretory cells, absence of ductal canalization, and an increased number of intermediate cells co-expressing basal and luminal markers, suggesting a defect in epithelial differentiation (Gao et al., 2005). Furthermore, prostate-specific deletion of Foxa1 results in prostate epithelial hyperplasia, as well as expression of seminal vesicle marker genes, consistent with loss of terminal differentiation (DeGraff et al., 2014). In the prostate, Foxa1 functions at least in part as a ‘pioneer’ transcription factor that opens chromatin to recruit AR to target promoters (Cirillo et al., 2002; Gao et al., 2003). Although Foxa1 is broadly expressed in endodermal tissues, its activity in the prostate epithelium may be mediated by interactions with tissue-specific regulators, including members of the NFI family of transcription factors, which co-occupy many AR/Foxa1 binding sites on target promoters (Grabowska et al., 2014).
The homeodomain transcription factor Nkx3.1 is also important for prostate epithelial specification. In mice, Nkx3.1 null mutants display epithelial hyperplasia, altered prostate secretory protein expression, and expression of seminal vesicle markers, indicating a defect in epithelial differentiation (Bhatia-Gaur et al., 1999; Dutta et al., 2016). Nkx3.1 is the earliest known specific marker of the prostate epithelium (Bhatia-Gaur et al., 1999; Keil et al., 2012a). In the neonatal prostate epithelium, Nkx3.1 is expressed by all epithelial cells, whereas its expression in the adult prostate is found in all luminal cells as well as a subpopulation of basal cells (Bhatia-Gaur et al., 1999; Chen et al., 2005; Kruithof-de Julio et al., 2013; Wang et al., 2009). Interestingly, studies of a lacZ knock-in allele have shown that Nkx3.1 expression is strongest in the ductal tips and mediates a positive-feedback loop with canonical Wnt signaling during organogenesis, consistent with a central role for Nkx3.1 in prostate outgrowth and morphogenesis (Kruithof-de Julio et al., 2013). The similarity between Foxa1 and Nkx3.1 mutant phenotypes is consistent with biochemical studies that have shown that Foxa1 and Nkx3.1 can interact with AR to form components of an ‘enhanceosome’ that regulates expression of prostate epithelial target genes (He et al., 2010; Tan et al., 2012), although AR-independent roles of Nkx3.1 are also likely to be important. In particular, Nkx3.1 expression can re-specify seminal vesicle epithelium to form prostate in tissue recombinants; this activity is mediated by interaction of Nkx3.1 with the G9a histone methyltransferase (Ehmt2) to activate expression of the target gene Uty, which encodes a histone demethylase (Dutta et al., 2016).
The homeobox gene Hoxb13 encodes a transcriptional regulator that also plays a key role in prostate epithelial specification. Null mouse mutants for Hoxb13 display normal development of the anterior and dorsolateral lobes, but display defective luminal differentiation and secretory protein production in the ventral lobe, although Nkx3.1 expression is normal (Economides and Capecchi, 2003). Interestingly, Foxa1 is an essential positive regulator of Hoxb13 expression in the ventral prostate epithelium of mice (McMullin et al., 2010). It has also been shown that, in human prostate cancer cell lines, HOXB13 protein interacts with AR to either repress or activate downstream targets, depending on the presence of specific HOXB13 response elements, and that HOXB13 is an AR co-regulator that both positively and negatively regulates the recruitment of AR and other AR co-regulators to cognate targets, including the NKX3.1 enhancer (Norris et al., 2009).
Finally, recent evidence has identified Sox9 as a transcription factor that could play an essential early role in prostate epithelial specification. Sox9 expression precedes that of Nkx3.1 in the mouse UGE (Huang et al., 2012; Thomsen et al., 2008), and SOX9 is also expressed in early prostatic epithelium in human embryos (Wang et al., 2008). Conditional deletion of Sox9 in mice using a Cre recombinase driven by the Nkx3.1 promoter leads to severely defective ventral prostate formation and abnormal anterior prostate differentiation (Thomsen et al., 2008). However, deletion of Sox9 in the UGS prior to prostate budding results in loss of prostate formation in renal grafts, suggesting an essential role for Sox9 at early stages of prostate specification (Huang et al., 2012).
Mechanisms and regulation of ductal outgrowth and branching morphogenesis
Following the formation of prostatic buds, the epithelium undergoes extensive proximal-distal outgrowth and branching morphogenesis, resulting in the morphologically distinct lobes of the rodent prostate or the zones of the human prostate. This phase of organogenesis is believed to be driven by a population of progenitor cells localized at the ductal tips, where the majority of proliferative cells are located and bifurcation of the branch points occurs (Sugimura et al., 1986b). In rodents, this stage of organogenesis is initiated during late fetal development, but the most prominent bud outgrowth occurs during the first two weeks postnatally. Analyses of genetically engineered mice, as well as of organ culture assays, have given us insight into the developmental pathways that drive prostate ductal outgrowth and branching morphogenesis. These pathways include the Notch and Activin signaling pathways, and additional studies have suggested roles for glial cell-derived neurotrophic factor (GDNF) and Ephrin signaling as well (Table 1). At present, however, the activities of the Hedgehog (Hh) and bone morphogenetic protein (BMP) signaling pathways in prostate ductal morphogenesis are best understood.
Early studies showed that Shh expression in the nascent prostate bud epithelium signals to the surrounding UGM by activating its receptor Ptc (Ptch1) and downstream Gli transcriptional regulators in the mesenchyme (Doles et al., 2006; Lamm et al., 2002; Wang et al., 2003). Organ culture experiments, together with phenotypic analyses of null mutant and transgenic overexpressing mice, have found that Shh is not required for the initial formation or outgrowth of prostate buds, but instead functions to mediate ductal branching and patterning in a stage-specific manner (Berman et al., 2004; Freestone et al., 2003; Yu and Bushman, 2013). Recent studies have also examined Hh signaling during androgen-mediated regeneration of the adult prostate, a process that has similarities with organogenesis, and have found that epithelial Hh activity induces the microRNAs miR26a and miR26b to repress stromal expression of hepatocyte growth factor (HGF), which induces epithelial branching (Lim et al., 2014). Thus, at least in the adult regenerating prostate, regions of low Hh signaling activity might correspond to the location of ductal branch points.
Parallel studies have shown that Bmp4 is expressed in the UGM and mediates ductal epithelial branching; the addition of BMP4 protein decreases the number of ductal tips in UGS culture, whereas Bmp4+/− heterozygotes display increased ductal branching (Lamm et al., 2001). Similarly, BMP7 treatment reduces ductal tip formation in organ culture, and null mutants for Bmp7 display significantly increased ductal branching (Grishina et al., 2005). Conversely, analyses of the BMP inhibitor noggin have shown that it is expressed in the UGM and that Nog mutant mice lack the ventral mesenchymal pad and fail to form the ventral prostate (Cook et al., 2007). Thus, both the Shh and BMP4/7 pathways appear to coordinate epithelial-mesenchymal interactions during prostate branching morphogenesis, but the precise mechanisms involved and their interactions with other relevant signaling pathways are still largely unresolved.
Although the majority of genes known to play a role in prostate branching morphogenesis are regulated by androgens (Table 1), there are likely to be genes and pathways important for this phase of prostate development that are independent of androgen signaling. Indeed, it has been shown that androgen ablation of neonates delays but does not completely abrogate further growth (Donjacour and Cunha, 1988; Lung and Cunha, 1981; Price, 1936). Conversely, administration of exogenous androgens to sexually mature male rodents does not promote further growth and branching of the prostate (Berry and Isaacs, 1984). At present, however, little is known about androgen-independent pathways that promote prostate branching morphogenesis. Estrogen signaling might represent one potential androgen-independent mechanism, as ERα (Esr1) null mice display reduced prostate branching morphogenesis (Chen et al., 2009, 2012), but it is not known whether estrogen signaling is truly independent of androgens at these stages of prostate development.
Differentiation of the prostate epithelium
During initial stages of branching morphogenesis, the nascent prostate is composed of solid epithelial cords. However, the epithelial cords subsequently undergo ductal canalization to form glandular structures, and the epithelial cells differentiate into basal, luminal and neuroendocrine lineages.
Mechanisms of epithelial canalization
Unlike the adjacent seminal vesicles that undergo branching morphogenesis as hollow tubes, the developing prostate epithelium undergoes significant branching morphogenesis as solid cords, which then canalize during later stages of development (Hayward et al., 1996a). Although ductal canalization has not been studied in detail in the prostate, it might share molecular similarities with canalization of other tissues such as the mammary and salivary glands (Mailleux et al., 2008). Mammary gland canalization is believed to occur primarily by anoikis, a process in which epithelial cells detach from the extracellular matrix and undergo apoptosis, although non-apoptotic cell death mechanisms might also play a role (Humphreys et al., 1996; Mailleux et al., 2007). Notably, studies of the rat prostate have shown that apoptosis occurs in the center of prostate epithelial cords during early canalization (Bruni-Cardoso and Carvalho, 2007). This process might be regulated by genes such as Dkk3 and Mmp2, which have been previously shown to play a role in normal prostate lumen formation (Table 1) (Bruni-Cardoso et al., 2010b; Kawano et al., 2006; Romero et al., 2013). Further studies are required to determine whether prostate ductal canalization occurs through anoikis and to elucidate the regulatory genes that drive lumen formation.
Lineage specification during organogenesis, homeostasis and regeneration
The transition of undifferentiated epithelial cords of the embryonic prostate into fully differentiated basal and luminal cells in the adult prostate has been an active area of investigation. Below, we describe studies of prostate epithelial progenitors and lineage hierarchy during organogenesis (summarized in Fig. 5). Prostate epithelial progenitors also maintain tissue homeostasis in adulthood, although studies of these progenitors have generally been limited because the adult epithelium is generally quiescent and displays slow turnover. Instead, adult prostate progenitors are more commonly analyzed in experimental contexts in which more rapid epithelial proliferation is induced (see Box 1). Thus, we also mention studies of lineage transitions during tissue homeostasis and androgen-mediated regeneration, but refer the reader to other recent reviews that discuss these studies in more detail (Kwon and Xin, 2014; Shibata and Shen, 2015; Wang and Shen, 2011).
Fig. 5.
Lineage relationships between cell types during prostate organogenesis. Lineage relationships between cell types during prostate organogenesis are depicted, showing known (solid arrows) and potential (dashed arrows) relationships. Upon induction of prostate budding, intermediate-like urogenital epithelial progenitors give rise to basal progenitors, which have multipotent and unipotent activity, as well as unipotent luminal progenitors. The origins of intermediate and neuroendocrine cells have not currently been resolved, although several studies suggest that neuroendocrine cells could either have neural crest or epithelial origins. Urogenital mesenchyme progenitors give rise to differentiated smooth muscle cells in the prostatic stroma, but it is not known whether these progenitors also give rise to prostate fibroblasts, or whether the fibroblasts originate from infiltrating mesenchymal stem cells. ChrA, chromogranin A; NSE, enolase 2 (Eno2); Syn, synaptophysin (Syp).
Box 1. Prostate gland homeostasis and regeneration.
The mature prostate is a relatively quiescent organ that exhibits slow epithelial turnover. Lineage-tracing studies in mice have shown that unipotent basal and luminal progenitors are largely responsible for the maintenance of their respective cell compartments during adult tissue homeostasis (Choi et al., 2012; Lu et al., 2013; Wang et al., 2013b). However, basal and luminal cells can display additional properties in other contexts. Notably, androgen deprivation by castration results in significant epithelial cell death in the prostate, whereas subsequent testosterone supplementation results in rapid tissue regeneration. During androgen-mediated regeneration, luminal castration-resistant Nkx3.1-expressing cells (CARNs) as well as basal cell populations can display bipotency and self-renewal indicative of stem cell activity (Lee et al., 2014; Wang et al., 2009, 2013b, 2015). Furthermore, during tissue damage and repair, such as in mouse models of prostatitis or luminal-specific anoikis, basal cells show significant capability to replace lost luminal cells (Kwon et al., 2014; Toivanen et al., 2016). Finally, when either basal and luminal cells are isolated from their native tissue microenvironment and grown as spheroids or organoids in culture, or in tissue reconstitution renal grafting assays in vivo, both cell types can show bipotency and reconstitution of epithelial architecture (Burger et al., 2005; Chua et al., 2014; Goldstein et al., 2008, 2010; Hofner et al., 2015; Karthaus et al., 2014; Lawson et al., 2007; Richardson et al., 2004; Wang et al., 2013b). Overall, although prostate epithelial progenitors appear to show limited stem cell properties during homeostasis, considerable plasticity can be activated in both basal and luminal cell compartments under circumstances when rapid epithelial growth is required.
In early studies, the prostate epithelium was reported to display a homogeneous phenotype prior to ductal canalization, displaying co-expression of basal and luminal markers as well as CK19, suggesting that the adult epithelium arises from a population of so-called ‘intermediate’ cells (Wang et al., 2001). By contrast, subsequent analyses of a more comprehensive set of cytokeratins found that the only such marker expressed throughout the developing UGS was the luminal marker CK8, raising the possibility that CK8-expressing cells give rise to the other differentiated cell types (Trompetter et al., 2008). However, these studies of cell type-specific marker expression are inherently limited in their ability to provide definitive information on lineage relationships.
More recently, lineage-tracing studies using specific Cre drivers to mark cell types in vivo have suggested that basal progenitors give rise to the mature prostate epithelium during organogenesis. In particular, inducible Cre drivers under the control of CK5, CK14 or CK8 promoters have been used to perform lineage tracing of basal and luminal epithelial cells during postnatal epithelial growth (Ousset et al., 2012). These analyses of early postnatal development showed that both luminal and basal compartments contain unipotent progenitors that only generate progeny of a single cell type, but that there are also multipotent basal progenitors that can give rise to basal, luminal and neuroendocrine cells (Ousset et al., 2012; Wuidart et al., 2016). Consistent with this interpretation, lineage-tracing studies of basal cells using deltaNp63cre mice have shown that p63-expressing basal cells in the UGS can give rise to all three prostate epithelial cell types (Pignon et al., 2013). However, there is significant co-expression of basal and luminal markers during early organogenesis, and basally located cells continue to express luminal markers well into postnatal development, which overlaps temporally with the time in which lineage marking occurs in these studies (Fig. 2). Therefore, it is unclear whether the progenitors of luminal and neuroendocrine cells are exclusively basal during early stages of organogenesis. Notably, although p63 null mutant mice are neonatal lethal, renal grafting of p63 mutant UGS results in prostate tissue that contains luminal cells but completely lacks basal cells, and can undergo serial androgen-mediated regeneration in the absence of basal cells, indicating tissue maintenance by a luminal progenitor (Kurita et al., 2004). The potential roles of luminal cells as progenitors during prostate organogenesis therefore requires further investigation, particularly given increasing evidence for luminal progenitor activity in adult prostate epithelium (Chua et al., 2014; Karthaus et al., 2014; Kwon et al., 2016; Wang et al., 2009).
Additional studies have focused on the localization of distinct progenitor populations within regions of the prostate lobes. Early studies of ductal outgrowth during organogenesis and androgen-mediated regeneration showed that cellular proliferation is highly enriched at ductal tips, suggesting a distal location for prostate epithelial progenitors (Sugimura et al., 1986a,b). Notably, a distal localization is consistent with the distribution of stem/progenitor cells during ductal outgrowth of tissues such as the lung and mammary gland (Hogan et al., 2014; Sreekumar et al., 2015). Furthermore, expression of Nkx3.1 is elevated in ductal tips (Kruithof-de Julio et al., 2013), and a role for Nkx3.1 in progenitor specification and maintenance has been suggested by the ductal morphogenesis defects in Nkx3.1 null mutants as well as by the stem cell properties of luminal Nkx3.1-expressing cells (termed CARNs; castration-resistant Nkx3.1-expressing cells) in the regressed adult prostate (Bhatia-Gaur et al., 1999; Wang et al., 2009). In contrast, studies of bromodeoxyuridine (BrdU) label-retaining cells have supported a proximal localization of epithelial progenitors during serial regeneration of the adult prostate (Tsujimura et al., 2002). This finding is also consistent with the recent identification of a luminal progenitor in the proximal region of the adult prostate epithelium (Kwon et al., 2016). Taken together, these findings suggest that the prostate epithelium might contain multiple stem/progenitor populations with distinct spatial distributions and functions during organogenesis and regeneration.
Although studies of prostate epithelial progenitors have focused mostly on basal and luminal cells, they have also given insight into the origin of neuroendocrine cells. Several studies have addressed whether neuroendocrine cells are of epithelial origin, or instead could be derived from the caudal neural crest. In particular, tissue reconstitution experiments have shown that adult epithelial progenitors can generate neuroendocrine cells (Goldstein et al., 2008; Wang et al., 2009, 2013b), and this has been further supported by lineage tracing during prostate organogenesis (Ousset et al., 2012). Consistent with this interpretation, lineage tracing has shown that neuroendocrine cells in the lung and thyroid have an epithelial origin (Johansson et al., 2015; Song et al., 2012). However, descriptive analyses have revealed that cells positive for chromogranin A, which marks neuroendocrine cells, can migrate into the UGS during development, suggesting that prostate neuroendocrine cells are derived from the neural crest ectoderm (Aumüller et al., 1999, 2001); notably, this conclusion has been supported by a recent lineage-tracing study (Szczyrba et al., 2017). Thus, additional work will be required to clarify these apparent discrepancies concerning the origin of prostate neuroendocrine cells.
Stromal progenitors and differentiation during prostate development
During organogenesis, differentiation of the prostate stroma occurs in parallel with that of the epithelium, and the two processes are coordinated by reciprocal epithelial-stromal signaling. The UGM differentiates from a fibroblastic inductive mesenchyme that promotes epithelial growth into a mature stromal compartment containing multiple specialized cell types. To date, the constituent cell types of the mouse prostate stroma have been characterized to a limited extent during organogenesis (Abler et al., 2011; Georgas et al., 2015), but their precise origin and functions have not been clearly elucidated. In the adult mouse prostate, recent work has defined at least four distinct populations of stromal cells: subepithelial cells, smooth muscle cells, wrapping cells and interstitial fibroblasts (Peng et al., 2013). Subepithelial cells are fibroblast-like cells that lie adjacent to the basement membrane beneath the basal epithelial cells, and are covered by a layer of smooth muscle cells. Wrapping cells are also fibroblast-like, and are tightly associated with the outer part of the smooth muscle layer, whereas interstitial fibroblasts are located between prostate ducts (Peng et al., 2013). In the case of the human prostate, ultrastructural analyses of subepithelial cells have resulted in their subdivision into fibroblasts, interstitial Cajal-like cells and spindle-shaped cells with myoid differentiation (Gevaert et al., 2014).
Tissue recombination studies have suggested that the differentiation of smooth muscle cells from the UGM is regulated by signaling from the adjacent epithelium during organogenesis (Hayward et al., 1997). In particular, the combination of human prostate epithelium with rodent UGM resulted in a smooth muscle phenotype that reflected human and not rodent tissue (Hayward et al., 1998). Interestingly, lineage-tracing studies indicate that these smooth muscle cells are maintained by a unipotent progenitor population during adult tissue homeostasis and regeneration (Peng et al., 2013). However, less is known about the origin of the fibroblast-like populations, which might also differentiate from the UGM or alternatively could be derived from infiltrating mesenchymal stem cells (Shaw et al., 2008).
Concluding remarks
Overall, the study of prostate organogenesis provides a rich and fertile area of investigation, at the intersection of multiple topics of interest to developmental biologists, including: the generation of secondary sexual dimorphism, the relationship of androgen signaling to tissue morphogenesis, the role of reciprocal epithelial-mesenchymal interactions, and the properties of epithelial progenitors and their role in lineage specification, tissue homeostasis and regeneration. However, the relationship between normal development and prostate tumorigenesis is also of particular interest to cancer biologists, as many of the key transcriptional regulators of normal prostate development have also been implicated in prostate cancer, including Nkx3.1, Foxa1, Hoxb13, Sox9, and of course AR (Baca et al., 2013; Barbieri et al., 2012; Bhatia-Gaur et al., 1999; Ewing et al., 2012; Kim et al., 2002; Network, 2015; Shen and Abate-Shen, 2010; Wang et al., 2008, 2013a; Watson et al., 2015). Moreover, key signaling pathways, such as the canonical Wnt and FGF pathways, that function in the prostate are also known to play crucial roles during tumor progression (Acevedo et al., 2007; Corn et al., 2013; Grasso et al., 2012; Kypta and Waxman, 2012; Memarzadeh et al., 2007; Sun et al., 2012). Elucidating how these signaling pathways and transcriptional regulators are integrated at the molecular and functional levels to mediate prostate specification and differentiation will be of particular relevance for understanding their roles in prostate cancer. For example, mechanisms that drive progenitor cell plasticity in the context of epithelial regeneration and repair could also play a role in prostate tumor plasticity in mediating resistance to cancer therapies. Thus, the field of prostate development is likely to remain of vital interest and importance for continuing investigation.
Acknowledgements
We thank Maho Shibata for insightful comments on the manuscript.
Footnotes
Competing interests
The authors declare no competing or financial interests.
Funding
This work was supported by an Australian National Health and Medical Research Council Early Career Fellowship (R.T.) and by the National Institutes of Health (R01DK076602 to M.M.S.). Deposited in PMC for release after 12 months.
References
- Abate-Shen C. and Shen M. M. (2000). Molecular genetics of prostate cancer. Genes Dev. 14, 2410-2434. 10.1101/gad.819500 [DOI] [PubMed] [Google Scholar]
- Abler L. L., Keil K. P., Mehta V., Joshi P. S., Schmitz C. T. and Vezina C. M. (2011). A high-resolution molecular atlas of the fetal mouse lower urogenital tract. Dev. Dyn. 240, 2364-2377. 10.1002/dvdy.22730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrahamsson P. A. (1999). Neuroendocrine cells in tumour growth of the prostate. Endocr Relat. Cancer 6, 503-519. 10.1677/erc.0.0060503 [DOI] [PubMed] [Google Scholar]
- Acevedo V. D., Gangula R. D., Freeman K. W., Li R., Zhang Y., Wang F., Ayala G. E., Peterson L. E., Ittmann M. and Spencer D. M. (2007). Inducible FGFR-1 activation leads to irreversible prostate adenocarcinoma and an epithelial-to-mesenchymal transition. Cancer Cell 12, 559-571. 10.1016/j.ccr.2007.11.004 [DOI] [PubMed] [Google Scholar]
- Allgeier S. H., Lin T.-M., Vezina C. M., Moore R. W., Fritz W. A., Chiu S. Y., Zhang C. and Peterson R. E. (2008). WNT5A selectively inhibits mouse ventral prostate development. Dev. Biol. 324, 10-17. 10.1016/j.ydbio.2008.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashley G. R., Grace O. C., Vanpoucke G. and Thomson A. A. (2010). Identification of EphrinB1 expression in prostatic mesenchyme and a role for EphB-EphrinB signalling in prostate development. Differentiation 80, 89-98. 10.1016/j.diff.2010.06.003 [DOI] [PubMed] [Google Scholar]
- Attard G., Parker C., Eeles R. A., Schröder F., Tomlins S. A., Tannock I., Drake C. G. and de Bono J. S. (2016). Prostate cancer. Lancet 387, 70-82. 10.1016/S0140-6736(14)61947-4 [DOI] [PubMed] [Google Scholar]
- Aumüller G., Leonhardt M., Janssen M., Konrad L., Bjartell A. and Abrahamsson P.-A. (1999). Neurogenic origin of human prostate endocrine cells. Urology 53, 1041-1048. 10.1016/S0090-4295(98)00631-1 [DOI] [PubMed] [Google Scholar]
- Aumüller G., Leonhardt M., Renneberg H., von Rahden B., Bjartell A. and Abrahamsson P.-A. (2001). Semiquantitative morphology of human prostatic development and regional distribution of prostatic neuroendocrine cells. Prostate 46, 108-115. [DOI] [PubMed] [Google Scholar]
- Baca S. C., Prandi D., Lawrence M. S., Mosquera J. M., Romanel A., Drier Y., Park K., Kitabayashi N., Macdonald T. Y., Ghandi M. et al. (2013). Punctuated evolution of prostate cancer genomes. Cell 153, 666-677. 10.1016/j.cell.2013.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbieri C. E., Baca S. C., Lawrence M. S., Demichelis F., Blattner M., Theurillat J.-P., White T. A., Stojanov P., Van Allen E., Stransky N. et al. (2012). Exome sequencing identifies recurrent SPOP, FOXA1 and MED12 mutations in prostate cancer. Nat. Genet. 44, 685-689. 10.1038/ng.2279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartsch G. and Rohr H. P. (1980). Comparative light and electron microscopic study of the human, dog and rat prostate. An approach to an experimental model for human benign prostatic hyperplasia (light and electron microscopic analysis) – a review. Urol. Int. 35, 91-104. 10.1159/000280309 [DOI] [PubMed] [Google Scholar]
- Berman D. M., Tian H. and Russell D. W. (1995). Expression and regulation of steroid 5 alpha-reductase in the urogenital tract of the fetal rat. Mol. Endocrinol. 9, 1561-1570. [DOI] [PubMed] [Google Scholar]
- Berman D. M., Desai N., Wang X., Karhadkar S. S., Reynon M., Abate-Shen C., Beachy P. A. and Shen M. M. (2004). Roles for Hedgehog signaling in androgen production and prostate ductal morphogenesis. Dev. Biol. 267, 387-398. 10.1016/j.ydbio.2003.11.018 [DOI] [PubMed] [Google Scholar]
- Berquin I. M., Min Y., Wu R., Wu H. and Chen Y. Q. (2005). Expression signature of the mouse prostate. J. Biol. Chem. 280, 36442-36451. 10.1074/jbc.M504945200 [DOI] [PubMed] [Google Scholar]
- Berry S. J. and Isaacs J. T. (1984). Comparative aspects of prostatic growth and androgen metabolism with aging in the dog versus the rat. Endocrinology 114, 511-520. 10.1210/endo-114-2-511 [DOI] [PubMed] [Google Scholar]
- Bhatia-Gaur R., Donjacour A. A., Sciavolino P. J., Kim M., Desai N., Young P., Norton C. R., Gridley T., Cardiff R. D., Cunha G. R. et al. (1999). Roles for Nkx3.1 in prostate development and cancer. Genes Dev. 13, 966-977. 10.1101/gad.13.8.966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branam A. M., Davis N. M., Moore R. W., Schneider A. J., Vezina C. M. and Peterson R. E. (2013). TCDD inhibition of canonical Wnt signaling disrupts prostatic bud formation in mouse urogenital sinus. Toxicol. Sci. 133, 42-53. 10.1093/toxsci/kft027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brechka H., McAuley E. M., Lamperis S. M., Paner G. P. and Vander Griend D. J. (2016). Contribution of caudal Müllerian duct mesenchyme to prostate development. Stem Cells Dev. 25, 1733-1741. 10.1089/scd.2016.0088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T. R., Lubahn D. B., Wilson E. M., Joseph D. R., French F. S. and Migeon C. J. (1988). Deletion of the steroid-binding domain of the human androgen receptor gene in one family with complete androgen insensitivity syndrome: evidence for further genetic heterogeneity in this syndrome. Proc. Natl. Acad. Sci. USA 85, 8151-8155. 10.1073/pnas.85.21.8151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruni-Cardoso A. and Carvalho H. F. (2007). Dynamics of the epithelium during canalization of the rat ventral prostate. Anat Rec (Hoboken) 290, 1223-1232. 10.1002/ar.20591 [DOI] [PubMed] [Google Scholar]
- Bruni-Cardoso A., Lynch C. C., Rosa-Ribeiro R., Matrisian L. M. and Carvalho H. F. (2010a). MMP-2 contributes to the development of the mouse ventral prostate by impacting epithelial growth and morphogenesis. Dev. Dyn. 239, 2386-2392. 10.1002/dvdy.22382 [DOI] [PubMed] [Google Scholar]
- Bruni-Cardoso A., Rosa-Ribeiro R., Pascoal V. D. B., De Thomaz, A. A., Cesar C. L. and Carvalho H. F. (2010b). MMP-2 regulates rat ventral prostate development in vitro. Dev. Dyn. 239, 737-746. 10.1002/dvdy.22222 [DOI] [PubMed] [Google Scholar]
- Bryant S. L., Francis J. C., Lokody I. B., Wang H., Risbridger G. P., Loveland K. L. and Swain A. (2014). Sex specific retinoic acid signaling is required for the initiation of urogenital sinus bud development. Dev. Biol. 395, 209-217. 10.1016/j.ydbio.2014.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buresh R. A., Kuslak S. L., Rusch M. A., Vezina C. M., Selleck S. B. and Marker P. C. (2010). Sulfatase 1 is an inhibitor of ductal morphogenesis with sexually dimorphic expression in the urogenital sinus. Endocrinology 151, 3420-3431. 10.1210/en.2009-1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burger P. E., Xiong X., Coetzee S., Salm S. N., Moscatelli D., Goto K. and Wilson E. L. (2005). Sca-1 expression identifies stem cells in the proximal region of prostatic ducts with high capacity to reconstitute prostatic tissue. Proc. Natl. Acad. Sci. USA 102, 7180-7185. 10.1073/pnas.0502761102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cancilla B., Jarred R. A., Wang H., Mellor S. L., Cunha G. R. and Risbridger G. P. (2001). Regulation of prostate branching morphogenesis by activin A and follistatin. Dev. Biol. 237, 145-158. 10.1006/dbio.2001.0364 [DOI] [PubMed] [Google Scholar]
- Chen H., Mutton L. N., Prins G. S. and Bieberich C. J. (2005). Distinct regulatory elements mediate the dynamic expression pattern of Nkx3.1. Dev. Dyn. 234, 961-973. 10.1002/dvdy.20596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M., Hsu I., Wolfe A., Radovick S., Huang K. H., Yu S., Chang C., Messing E. M. and Yeh S. (2009). Defects of prostate development and reproductive system in the estrogen receptor-alpha null male mice. Endocrinology 150, 251-259. 10.1210/en.2008-0044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M., Yeh C.-R., Shyr C.-R., Lin H.-H., Da J. and Yeh S. (2012). Reduced prostate branching morphogenesis in stromal fibroblast, but not in epithelial, estrogen receptor alpha knockout mice. Asian J. Androl. 14, 546-555. 10.1038/aja.2011.181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi N., Zhang B., Zhang L., Ittmann M. and Xin L. (2012). Adult murine prostate basal and luminal cells are self-sustained lineages that can both serve as targets for prostate cancer initiation. Cancer Cell 21, 253-265. 10.1016/j.ccr.2012.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrisman H. and Thomson A. A. (2006). Regulation of urogenital smooth muscle patterning by testosterone and estrogen during prostatic induction. Prostate 66, 696-707. 10.1002/pros.20378 [DOI] [PubMed] [Google Scholar]
- Chua C. W., Shibata M., Lei M., Toivanen R., Barlow L. M. J., Bergren S. K., Badani K. K., McKiernan J. M., Benson M. C., Hibshoosh H. et al. (2014). Single luminal epithelial progenitors can generate prostate organoids in culture. Nat. Cell Biol. 16, 951-961. 10.1038/ncb3047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirillo L. A., Lin F. R., Cuesta I., Friedman D., Jarnik M. and Zaret K. S. (2002). Opening of compacted chromatin by early developmental transcription factors HNF3 (FoxA) and GATA-4. Mol. Cell 9, 279-289. 10.1016/S1097-2765(02)00459-8 [DOI] [PubMed] [Google Scholar]
- Cook C., Vezina C. M., Allgeier S. H., Shaw A., Yu M., Peterson R. E. and Bushman W. (2007). Noggin is required for normal lobe patterning and ductal budding in the mouse prostate. Dev. Biol. 312, 217-230. 10.1016/j.ydbio.2007.09.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corn P. G., Wang F., McKeehan W. L. and Navone N. (2013). Targeting fibroblast growth factor pathways in prostate cancer. Clin. Cancer Res. 19, 5856-5866. 10.1158/1078-0432.CCR-13-1550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunha G. R. (1975). Age-dependent loss of sensitivity of female urogenital sinus to androgenic conditions as a function of the epithelia-stromal interaction in mice. Endocrinology 97, 665-673. 10.1210/endo-97-3-665 [DOI] [PubMed] [Google Scholar]
- Cunha G. R. and Lung B. (1978). The possible influence of temporal factors in androgenic responsiveness of urogenital tissue recombinants from wild-type and androgen-insensitive (Tfm) mice. J. Exp. Zool. 205, 181-193. 10.1002/jez.1402050203 [DOI] [PubMed] [Google Scholar]
- Cunha G. R. and Young P. (1991). Inability of Tfm (testicular feminization) epithelial cells to express androgen-dependent seminal vesicle secretory proteins in chimeric tissue recombinants. Endocrinology 128, 3293-3298. 10.1210/endo-128-6-3293 [DOI] [PubMed] [Google Scholar]
- Cunha G. R., Fujii H., Neubauer B. L., Shannon J. M., Sawyer L. and Reese B. A. (1983). Epithelial-mesenchymal interactions in prostatic development. I. Morphological observations of prostatic induction by urogenital sinus mesenchyme in epithelium of the adult rodent urinary bladder. J. Cell Biol. 96, 1662-1670. 10.1083/jcb.96.6.1662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunha G. R., Donjacour A. A., Cooke P. S., Mee S., Bigsby R. M., Higgins S. J. and Sugimura Y. (1987). The endocrinology and developmental biology of the prostate. Endocr. Rev. 8, 338-362. 10.1210/edrv-8-3-338 [DOI] [PubMed] [Google Scholar]
- Cunha G. R., Battle E., Young P., Brody J., Donjacour A., Hayashi N. and Kinbara H. (1992). Role of epithelial-mesenchymal interactions in the differentiation and spatial organization of visceral smooth muscle. Epithelial Cell Biol 1, 76-83. [PubMed] [Google Scholar]
- De Marzo A. M., Nelson W. G., Meeker A. K. and Coffey D. S. (1998). Stem cell features of benign and malignant prostate epithelial cells. J. Urol. 160, 2381-2392. 10.1016/S0022-5347(01)62196-7 [DOI] [PubMed] [Google Scholar]
- DeGraff D. J., Grabowska M. M., Case T. C., Yu X., Herrick M. K., Hayward W. J., Strand D. W., Cates J. M., Hayward S. W., Gao N. et al. (2014). FOXA1 deletion in luminal epithelium causes prostatic hyperplasia and alteration of differentiated phenotype. Lab. Invest. 94, 726-739. 10.1038/labinvest.2014.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietrich W., Susani M., Stifter L. and Haitel A. (2011). The human female prostate-immunohistochemical study with prostate-specific antigen, prostate-specific alkaline phosphatase, and androgen receptor and 3-D remodeling. J. Sex. Med. 8, 2816-2821. 10.1111/j.1743-6109.2011.02408.x [DOI] [PubMed] [Google Scholar]
- Doles J., Cook C., Shi X., Valosky J., Lipinski R. and Bushman W. (2006). Functional compensation in Hedgehog signaling during mouse prostate development. Dev. Biol. 295, 13-25. 10.1016/j.ydbio.2005.12.002 [DOI] [PubMed] [Google Scholar]
- Donjacour A. A. and Cunha G. R. (1988). The effect of androgen deprivation on branching morphogenesis in the mouse prostate. Dev. Biol. 128, 1-14. 10.1016/0012-1606(88)90260-6 [DOI] [PubMed] [Google Scholar]
- Donjacour A. A. and Cunha G. R. (1993). Assessment of prostatic protein secretion in tissue recombinants made of urogenital sinus mesenchyme and urothelium from normal or androgen-insensitive mice. Endocrinology 132, 2342-2350. [DOI] [PubMed] [Google Scholar]
- Donjacour A. A. and Cunha G. R. (1995). Induction of prostatic morphology and secretion in urothelium by seminal vesicle mesenchyme. Development 121, 2199-2207. [DOI] [PubMed] [Google Scholar]
- Donjacour A. A., Thomson A. A. and Cunha G. R. (2003). FGF-10 plays an essential role in the growth of the fetal prostate. Dev. Biol. 261, 39-54. 10.1016/S0012-1606(03)00250-1 [DOI] [PubMed] [Google Scholar]
- Dutta A., Le Magnen C., Mitrofanova A., Ouyang X., Califano A. and Abate-Shen C. (2016). Identification of an NKX3.1-G9a-UTY transcriptional regulatory network that controls prostate differentiation. Science 352, 1576-1580. 10.1126/science.aad9512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Economides K. D. and Capecchi M. R. (2003). Hoxb13 is required for normal differentiation and secretory function of the ventral prostate. Development 130, 2061-2069. 10.1242/dev.00432 [DOI] [PubMed] [Google Scholar]
- Ekman P. (2000). The prostate as an endocrine organ: androgens and estrogens. Prostate Suppl. 10, 14-18. [DOI] [PubMed] [Google Scholar]
- El-Alfy M., Luu-The V., Huang X. F., Berger L., Labrie F. and Pelletier G. (1999). Localization of type 5 17beta-hydroxysteroid dehydrogenase, 3beta-hydroxysteroid dehydrogenase, and androgen receptor in the human prostate by in situ hybridization and immunocytochemistry. Endocrinology 140, 1481-1491. [DOI] [PubMed] [Google Scholar]
- El-Alfy M., Pelletier G., Hermo L. S. and Labrie F. (2000). Unique features of the basal cells of human prostate epithelium. Microsc. Res. Tech. 51, 436-446. [DOI] [PubMed] [Google Scholar]
- Ewing C. M., Ray A. M., Lange E. M., Zuhlke K. A., Robbins C. M., Tembe W. D., Wiley K. E., Isaacs S. D., Johng D., Wang Y. et al. (2012). Germline mutations in HOXB13 and prostate-cancer risk. N. Engl. J. Med. 366, 141-149. 10.1056/NEJMoa1110000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraldeschi R., Sharifi N., Auchus R. J. and Attard G. (2013). Molecular pathways: Inhibiting steroid biosynthesis in prostate cancer. Clin. Cancer Res. 19, 3353-3359. 10.1158/1078-0432.CCR-12-0931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch P. W., Cunha G. R., Rubin J. S., Wong J. and Ron D. (1995). Pattern of keratinocyte growth factor and keratinocyte growth factor receptor expression during mouse fetal development suggests a role in mediating morphogenetic mesenchymal-epithelial interactions. Dev. Dyn. 203, 223-240. 10.1002/aja.1002030210 [DOI] [PubMed] [Google Scholar]
- Francis J. C., Thomsen M. K., Taketo M. M. and Swain A. (2013). beta-catenin is required for prostate development and cooperates with Pten loss to drive invasive carcinoma. PLoS Genet. 9, e1003180 10.1371/journal.pgen.1003180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freestone S. H., Marker P., Grace O. C., Tomlinson D. C., Cunha G. R., Harnden P. and Thomson A. A. (2003). Sonic hedgehog regulates prostatic growth and epithelial differentiation. Dev. Biol. 264, 352-362. 10.1016/j.ydbio.2003.08.018 [DOI] [PubMed] [Google Scholar]
- Gamat M., Malinowski R. L., Parkhurst L. J., Steinke L. M. and Marker P. C. (2015). Ornithine decarboxylase activity is required for prostatic budding in the developing mouse prostate. PLoS ONE 10, e0139522 10.1371/journal.pone.0139522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao N., Zhang J., Rao M. A., Case T. C., Mirosevich J., Wang Y., Jin R., Gupta A., Rennie P. S. and Matusik R. J. (2003). The role of hepatocyte nuclear factor-3 alpha (Forkhead Box A1) and androgen receptor in transcriptional regulation of prostatic genes. Mol. Endocrinol. 17, 1484-1507. 10.1210/me.2003-0020 [DOI] [PubMed] [Google Scholar]
- Gao N., Ishii K., Mirosevich J., Kuwajima S., Oppenheimer S. R., Roberts R. L., Jiang M., Yu X., Shappell S. B., Caprioli R. M. et al. (2005). Forkhead box A1 regulates prostate ductal morphogenesis and promotes epithelial cell maturation. Development 132, 3431-3443. 10.1242/dev.01917 [DOI] [PubMed] [Google Scholar]
- Georgas K. M., Armstrong J., Keast J. R., Larkins C. E., McHugh K. M., Southard-Smith E. M., Cohn M. J., Batourina E., Dan H., Schneider K. et al. (2015). An illustrated anatomical ontology of the developing mouse lower urogenital tract. Development 142, 1893-1908. 10.1242/dev.117903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gevaert T., Lerut E., Joniau S., Franken J., Roskams T. and De Ridder D. (2014). Characterization of subepithelial interstitial cells in normal and pathological human prostate. Histopathology 65, 418-428. 10.1111/his.12402 [DOI] [PubMed] [Google Scholar]
- Ghosh S., Lau H., Simons B. W., Powell J. D., Meyers D. J., De Marzo A. M., Berman D. M. and Lotan T. L. (2011). PI3K/mTOR signaling regulates prostatic branching morphogenesis. Dev. Biol. 360, 329-342. 10.1016/j.ydbio.2011.09.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein A. S., Lawson D. A., Cheng D., Sun W., Garraway I. P. and Witte O. N. (2008). Trop2 identifies a subpopulation of murine and human prostate basal cells with stem cell characteristics. Proc. Natl. Acad. Sci. USA 105, 20882-20887. 10.1073/pnas.0811411106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein A. S., Huang J., Guo C., Garraway I. P. and Witte O. N. (2010). Identification of a cell of origin for human prostate cancer. Science 329, 568-571. 10.1126/science.1189992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowska M. M., Elliott A. D., DeGraff D. J., Anderson P. D., Anumanthan G., Yamashita H., Sun Q., Friedman D. B., Hachey D. L., Yu X. et al. (2014). NFI transcription factors interact with FOXA1 to regulate prostate-specific gene expression. Mol. Endocrinol. 28, 949-964. 10.1210/me.2013-1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasso C. S., Wu Y.-M., Robinson D. R., Cao X., Dhanasekaran S. M., Khan A. P., Quist M. J., Jing X., Lonigro R. J., Brenner J. C. et al. (2012). The mutational landscape of lethal castration-resistant prostate cancer. Nature 487, 239-243. 10.1038/nature11125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grishina I. B., Kim S. Y., Ferrara C., Makarenkova H. P. and Walden P. D. (2005). BMP7 inhibits branching morphogenesis in the prostate gland and interferes with Notch signaling. Dev. Biol. 288, 334-347. 10.1016/j.ydbio.2005.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo L., Degenstein L. and Fuchs E. (1996). Keratinocyte growth factor is required for hair development but not for wound healing. Genes Dev. 10, 165-175. 10.1101/gad.10.2.165 [DOI] [PubMed] [Google Scholar]
- Hayward S. W. (2002). Approaches to modeling stromal-epithelial interactions. J. Urol. 168, 1165-1172. 10.1016/S0022-5347(05)64620-4 [DOI] [PubMed] [Google Scholar]
- Hayward S. W., Baskin L. S., Haughney P. C., Cunha A. R., Foster B. A., Dahiya R., Prins G. S. and Cunha G. R. (1996a). Epithelial development in the rat ventral prostate, anterior prostate and seminal vesicle. Acta Anat (Basel) 155, 81-93. 10.1159/000147793 [DOI] [PubMed] [Google Scholar]
- Hayward S. W., Baskin L. S., Haughney P. C., Foster B. A., Cunha A. R., Dahiya R., Prins G. S. and Cunha G. R. (1996b). Stromal development in the ventral prostate, anterior prostate and seminal vesicle of the rat. Acta Anat (Basel) 155, 94-103. 10.1159/000147794 [DOI] [PubMed] [Google Scholar]
- Hayward S. W., Brody J. R. and Cunha G. R. (1996c). An edgewise look at basal epithelial cells: three-dimensional views of the rat prostate, mammary gland and salivary gland. Differentiation 60, 219-227. 10.1046/j.1432-0436.1996.6040219.x [DOI] [PubMed] [Google Scholar]
- Hayward S. W., Rosen M. A. and Cunha G. R. (1997). Stromal-epithelial interactions in the normal and neoplastic prostate. Br J Urol 79 Suppl. 2, 18-26. 10.1111/j.1464-410X.1997.tb16917.x [DOI] [PubMed] [Google Scholar]
- Hayward S. W., Haughney P. C., Rosen M. A., Greulich K. M., Weier H.-U. G., Dahiya R. and Cunha G. R. (1998). Interactions between adult human prostatic epithelium and rat urogenital sinus mesenchyme in a tissue recombination model. Differentiation 63, 131-140. 10.1046/j.1432-0436.1998.6330131.x [DOI] [PubMed] [Google Scholar]
- He H. H., Meyer C. A., Shin H., Bailey S. T., Wei G., Wang Q., Zhang Y., Xu K., Ni M., Lupien M. et al. (2010). Nucleosome dynamics define transcriptional enhancers. Nat. Genet. 42, 343-347. 10.1038/ng.545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Höfner T., Eisen C., Klein C., Rigo-Watermeier T., Goeppinger S. M., Jauch A., Schoell B., Vogel V., Noll E., Weichert W. et al. (2015). Defined conditions for the isolation and expansion of basal prostate progenitor cells of mouse and human origin. Stem Cell Reports 4, 503-518. 10.1016/j.stemcr.2015.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan B. L. M., Barkauskas C. E., Chapman H. A., Epstein J. A., Jain R., Hsia C. C. W., Niklason L., Calle E., Le A., Randell S. H. et al. (2014). Repair and regeneration of the respiratory system: complexity, plasticity, and mechanisms of lung stem cell function. Cell Stem Cell 15, 123-138. 10.1016/j.stem.2014.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L., Pu Y., Alam S., Birch L. and Prins G. S. (2005). The role of Fgf10 signaling in branching morphogenesis and gene expression of the rat prostate gland: lobe-specific suppression by neonatal estrogens. Dev. Biol. 278, 396-414. 10.1016/j.ydbio.2004.11.020 [DOI] [PubMed] [Google Scholar]
- Huang L., Pu Y., Hu W. Y., Birch L., Luccio-Camelo D., Yamaguchi T. and Prins G. S. (2009). The role of Wnt5a in prostate gland development. Dev. Biol. 328, 188-199. 10.1016/j.ydbio.2009.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Z., Hurley P. J., Simons B. W., Marchionni L., Berman D. M., Ross A. E. and Schaeffer E. M. (2012). Sox9 is required for prostate development and prostate cancer initiation. Oncotarget 3, 651-663. 10.18632/oncotarget.531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y. C., Chen F. and Li X. (2016). Clarification of mammalian cloacal morphogenesis using high-resolution episcopic microscopy. Dev. Biol. 409, 106-113. 10.1016/j.ydbio.2015.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman J. W. (1948). The detailed anatomy of the para-urethral ducts in the adult human female. Am. J. Obstet. Gynecol. 55, 86-101. 10.1016/0002-9378(48)90157-4 [DOI] [PubMed] [Google Scholar]
- Humphreys R. C., Krajewska M., Krnacik S., Jaeger R., Weiher H., Krajewski S., Reed J. C. and Rosen J. M. (1996). Apoptosis in the terminal endbud of the murine mammary gland: a mechanism of ductal morphogenesis. Development 122, 4013-4022. [DOI] [PubMed] [Google Scholar]
- Hynes P. J. and Fraher J. P. (2004). The development of the male genitourinary system. I. The origin of the urorectal septum and the formation of the perineum. Br. J. Plast. Surg. 57, 27-36. 10.1016/j.bjps.2003.08.019 [DOI] [PubMed] [Google Scholar]
- Ittmann M., Huang J., Radaelli E., Martin P., Signoretti S., Sullivan R., Simons B. W., Ward J. M., Robinson B. D., Chu G. C. et al. (2013). Animal models of human prostate cancer: the consensus report of the New York meeting of the Mouse Models of Human Cancers Consortium Prostate Pathology Committee. Cancer Res. 73, 2718-2736. 10.1158/0008-5472.CAN-12-4213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerde T. J. and Bushman W. (2009). IL-1 induces IGF-dependent epithelial proliferation in prostate development and reactive hyperplasia. Sci. Signal. 2, ra49 10.1126/scisignal.2000338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joesting M. S., Cheever T. R., Volzing K. G., Yamaguchi T. P., Wolf V., Naf D., Rubin J. S. and Marker P. C. (2008). Secreted frizzled related protein 1 is a paracrine modulator of epithelial branching morphogenesis, proliferation, and secretory gene expression in the prostate. Dev. Biol. 317, 161-173. 10.1016/j.ydbio.2008.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson E., Andersson L., Örnros J., Carlsson T., Ingeson-Carlsson C., Liang S., Dahlberg J., Jansson S., Parrillo L., Zoppoli P. et al. (2015). Revising the embryonic origin of thyroid C cells in mice and humans. Development 142, 3519-3528. 10.1242/dev.126581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karthaus W. R., Iaquinta P. J., Drost J., Gracanin A., van Boxtel R., Wongvipat J., Dowling C. M., Gao D., Begthel H., Sachs N. et al. (2014). Identification of multipotent luminal progenitor cells in human prostate organoid cultures. Cell 159, 163-175. 10.1016/j.cell.2014.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawano Y., Kitaoka M., Hamada Y., Walker M. M., Waxman J. and Kypta R. M. (2006). Regulation of prostate cell growth and morphogenesis by Dickkopf-3. Oncogene 25, 6528-6537. 10.1038/sj.onc.1209661 [DOI] [PubMed] [Google Scholar]
- Keil K. P., Mehta V., Abler L. L., Joshi P. S., Schmitz C. T. and Vezina C. M. (2012a). Visualization and quantification of mouse prostate development by in situ hybridization. Differentiation 84, 232-239. 10.1016/j.diff.2012.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keil K. P., Mehta V., Branam A. M., Abler L. L., Buresh-Stiemke R. A., Joshi P. S., Schmitz C. T., Marker P. C. and Vezina C. M. (2012b). Wnt inhibitory factor 1 (Wif1) is regulated by androgens and enhances androgen-dependent prostate development. Endocrinology 153, 6091-6103. 10.1210/en.2012-1564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keil K. P., Abler L. L., Mehta V., Altmann H. M., Laporta J., Plisch E. H., Suresh M., Hernandez L. L. and Vezina C. M. (2014). DNA methylation of E-cadherin is a priming mechanism for prostate development. Dev. Biol. 387, 142-153. 10.1016/j.ydbio.2014.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellokumpu-Lehtinen P., Santti R. and Pelliniemi L. J. (1980). Correlation of early cytodifferentiation of the human fetal prostate and Leydig cells. Anat. Rec. 196, 263-273. 10.1002/ar.1091960302 [DOI] [PubMed] [Google Scholar]
- Kim M. J., Bhatia-Gaur R., Banach-Petrosky W. A., Desai N., Wang Y., Hayward S. W., Cunha G. R., Cardiff R. D., Shen M. M. and Abate-Shen C. (2002). Nkx3.1 mutant mice recapitulate early stages of prostate carcinogenesis. Cancer Res.. 62, 2999-3004. [PubMed] [Google Scholar]
- Kruithof-de Julio M., Shibata M., Desai N., Reynon M., Halili M. V., Hu Y.-P., Price S. M., Abate-Shen C. and Shen M. M. (2013). Canonical Wnt signaling regulates Nkx3.1 expression and luminal epithelial differentiation during prostate organogenesis. Dev. Dyn. 242, 1160-1171. 10.1002/dvdy.24008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurita T., Medina R. T., Mills A. A. and Cunha G. R. (2004). Role of p63 and basal cells in the prostate. Development 131, 4955-4964. 10.1242/dev.01384 [DOI] [PubMed] [Google Scholar]
- Kwon O. J. and Xin L. (2014). Prostate epithelial stem and progenitor cells. Am J Clin Exp Urol 2, 209-218. [PMC free article] [PubMed] [Google Scholar]
- Kwon O. J., Zhang L., Ittmann M. M. and Xin L. (2014). Prostatic inflammation enhances basal-to-luminal differentiation and accelerates initiation of prostate cancer with a basal cell origin. Proc. Natl. Acad. Sci. USA 111, E592-E600. 10.1073/pnas.1318157111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon O.-J., Zhang L. and Xin L. (2016). Stem Cell Antigen-1 identifies a distinct androgen-independent murine prostatic luminal cell lineage with bipotent potential. Stem Cells 34, 191-202. 10.1002/stem.2217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kypta R. M. and Waxman J. (2012). Wnt/beta-catenin signalling in prostate cancer. Nat Rev Urol 9, 418-428. 10.1038/nrurol.2012.116 [DOI] [PubMed] [Google Scholar]
- Lai K.-P., Yamashita S., Vitkus S., Shyr C.-R., Yeh S. and Chang C. (2012). Suppressed prostate epithelial development with impaired branching morphogenesis in mice lacking stromal fibromuscular androgen receptor. Mol. Endocrinol. 26, 52-66. 10.1210/me.2011-1189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamm M. L. G., Podlasek C. A., Barnett D. H., Lee J., Clemens J. Q., Hebner C. M. and Bushman W. (2001). Mesenchymal factor bone morphogenetic protein 4 restricts ductal budding and branching morphogenesis in the developing prostate. Dev. Biol. 232, 301-314. 10.1006/dbio.2001.0187 [DOI] [PubMed] [Google Scholar]
- Lamm M. L. G., Catbagan W. S., Laciak R. J., Barnett D. H., Hebner C. M., Gaffield W., Walterhouse D., Iannaccone P. and Bushman W. (2002). Sonic hedgehog activates mesenchymal Gli1 expression during prostate ductal bud formation. Dev. Biol. 249, 349-366. 10.1006/dbio.2002.0774 [DOI] [PubMed] [Google Scholar]
- Lasnitzki I. and Mizuno T. (1977). Induction of the rat prostate gland by androgens in organ culture. J. Endocrinol. 74, 47-55. 10.1677/joe.0.0740047 [DOI] [PubMed] [Google Scholar]
- Lawson D. A., Xin L., Lukacs R. U., Cheng D. and Witte O. N. (2007). Isolation and functional characterization of murine prostate stem cells. Proc. Natl. Acad. Sci. USA 104, 181-186. 10.1073/pnas.0609684104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee D.-K., Liu Y., Liao L., Wang F. and Xu J. (2014). The prostate basal cell (BC) heterogeneity and the p63-positive BC differentiation spectrum in mice. Int. J. Biol. Sci. 10, 1007-1017. 10.7150/ijbs.9997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. H., Johnson D. T., Luong R., Yu E. J., Cunha G. R., Nusse R. and Sun Z. (2015). Wnt/beta-catenin-responsive cells in prostatic development and regeneration. Stem Cells 33, 3356-3367. 10.1002/stem.2096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim A., Shin K., Zhao C., Kawano S. and Beachy P. A. (2014). Spatially restricted Hedgehog signalling regulates HGF-induced branching of the adult prostate. Nat. Cell Biol. 16, 1135-1145. 10.1038/ncb3057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y., Liu G., Zhang Y., Hu Y.-P., Yu K., Lin C., McKeehan K., Xuan J. W., Ornitz D. M., Shen M. M. et al. (2007). Fibroblast growth factor receptor 2 tyrosine kinase is required for prostatic morphogenesis and the acquisition of strict androgen dependency for adult tissue homeostasis. Development 134, 723-734. 10.1242/dev.02765 [DOI] [PubMed] [Google Scholar]
- Liu A. Y., True L. D., LaTray L., Nelson P. S., Ellis W. J., Vessella R. L., Lange P. H., Hood L. and van den Engh G. (1997). Cell-cell interaction in prostate gene regulation and cytodifferentiation. Proc. Natl. Acad. Sci. USA 94, 10705-10710. 10.1073/pnas.94.20.10705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowsley O. S. (1912). The development of the human prostate gland with reference to the development of other structures at the neck of the urinary bladder. . Am. J. Anat. 13, 299-349. 10.1002/aja.1000130303 [DOI] [Google Scholar]
- Lu W., Luo Y., Kan M. and McKeehan W. L. (1999). Fibroblast growth factor-10. A second candidate stromal to epithelial cell andromedin in prostate. J. Biol. Chem. 274, 12827-12834. 10.1074/jbc.274.18.12827 [DOI] [PubMed] [Google Scholar]
- Lu T.-L., Huang Y.-F., You L.-R., Chao N.-C., Su F.-Y., Chang J.-L. and Chen C.-M. (2013). Conditionally ablated Pten in prostate basal cells promotes basal-to-luminal differentiation and causes invasive prostate cancer in mice. Am. J. Pathol. 182, 975-991. 10.1016/j.ajpath.2012.11.025 [DOI] [PubMed] [Google Scholar]
- Lubahn D. B., Brown T. R., Simental J. A., Higgs H. N., Migeon C. J., Wilson E. M. and French F. S. (1989). Sequence of the intron/exon junctions of the coding region of the human androgen receptor gene and identification of a point mutation in a family with complete androgen insensitivity. Proc. Natl. Acad. Sci. USA 86, 9534-9538. 10.1073/pnas.86.23.9534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lung B. and Cunha G. R. (1981). Development of seminal vesicles and coagulating glands in neonatal mice. I. The morphogenetic effects of various hormonal conditions. Anat. Rec. 199, 73-88. 10.1002/ar.1091990108 [DOI] [PubMed] [Google Scholar]
- Luo W., Rodriguez M., Valdez J. M., Zhu X., Tan K., Li D., Siwko S., Xin L. and Liu M. (2013). Lgr4 is a key regulator of prostate development and prostate stem cell differentiation. Stem Cells 31, 2492-2505. 10.1002/stem.1484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon M. F. and Hawkes S. G. (1970). X-linked gene for testicular feminization in the mouse. Nature 227, 1217-1219. 10.1038/2271217a0 [DOI] [PubMed] [Google Scholar]
- Mahoney J. J. (1940). The embryology and postnatal development of the prostate gland in the female rat. Anat. Rec. (Hoboken) 77, 375-395. 10.1002/ar.1090770309 [DOI] [Google Scholar]
- Mailleux A. A., Overholtzer M., Schmelzle T., Bouillet P., Strasser A. and Brugge J. S. (2007). BIM regulates apoptosis during mammary ductal morphogenesis, and its absence reveals alternative cell death mechanisms. Dev. Cell 12, 221-234. 10.1016/j.devcel.2006.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mailleux A. A., Overholtzer M. and Brugge J. S. (2008). Lumen formation during mammary epithelial morphogenesis: insights from in vitro and in vivo models. Cell Cycle 7, 57-62. 10.4161/cc.7.1.5150 [DOI] [PubMed] [Google Scholar]
- McMullin R. P., Dobi A., Mutton L. N., Orosz A., Maheshwari S., Shashikant C. S. and Bieberich C. J. (2010). A FOXA1-binding enhancer regulates Hoxb13 expression in the prostate gland. Proc. Natl. Acad. Sci. USA 107, 98-103. 10.1073/pnas.0902001107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeal J. E. (1969). Origin and development of carcinoma in the prostate. Cancer 23, 24-34. [DOI] [PubMed] [Google Scholar]
- McNeal J. E. (1978). Evolution of benign prostatic enlargement. Invest. Urol. 15, 340-345. [PubMed] [Google Scholar]
- McNeal J. E. (1981). Normal and pathologic anatomy of prostate. Urology 17, 11-16. [PubMed] [Google Scholar]
- McNeal J. E. (1983). The prostate gland – morphology and pathobiology. Monographs Urol. 4, 3. [Google Scholar]
- McNeal J. E. (1988). Normal histology of the prostate. Am. J. Surg. Pathol. 12, 619-633. 10.1097/00000478-198808000-00003 [DOI] [PubMed] [Google Scholar]
- Mehta V., Abler L. L., Keil K. P., Schmitz C. T., Joshi P. S. and Vezina C. M. (2011). Atlas of Wnt and R-spondin gene expression in the developing male mouse lower urogenital tract. Dev. Dyn. 240, 2548-2560. 10.1002/dvdy.22741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta V., Schmitz C. T., Keil K. P., Joshi P. S., Abler L. L., Lin T.-M., Taketo M. M., Sun X. and Vezina C. M. (2013). Beta-catenin (CTNNB1) induces Bmp expression in urogenital sinus epithelium and participates in prostatic bud initiation and patterning. Dev. Biol. 376, 125-135. 10.1016/j.ydbio.2013.01.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memarzadeh S., Xin L., Mulholland D. J., Mansukhani A., Wu H., Teitell M. A. and Witte O. N. (2007). Enhanced paracrine FGF10 expression promotes formation of multifocal prostate adenocarcinoma and an increase in epithelial androgen receptor. Cancer Cell 12, 572-585. 10.1016/j.ccr.2007.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirosevich J., Bentel J. M., Zeps N., Redmond S. L., D'Antuono M. F. and Dawkins H. J. (1999). Androgen receptor expression of proliferating basal and luminal cells in adult murine ventral prostate. J. Endocrinol. 162, 341-350. 10.1677/joe.0.1620341 [DOI] [PubMed] [Google Scholar]
- Mirosevich J., Gao N. and Matusik R. J. (2005). Expression of Foxa transcription factors in the developing and adult murine prostate. Prostate 62, 339-352. 10.1002/pros.20131 [DOI] [PubMed] [Google Scholar]
- Network C. G. A. R. (2015). The molecular taxonomy of primary prostate cancer. Cell 163, 1011-1025. 10.1016/j.cell.2015.10.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris J. D., Chang C.-Y., Wittmann B. M., Kunder R. S., Cui H., Fan D., Joseph J. D. and McDonnell D. P. (2009). The homeodomain protein HOXB13 regulates the cellular response to androgens. Mol. Cell 36, 405-416. 10.1016/j.molcel.2009.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omori A., Miyagawa S., Ogino Y., Harada M., Ishii K., Sugimura Y., Ogino H., Nakagata N. and Yamada G. (2014). Essential roles of epithelial bone morphogenetic protein signaling during prostatic development. Endocrinology 155, 2534-2544. 10.1210/en.2013-2054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr B., Vanpoucke G., Grace O. C., Smith L., Anderson R. A., Riddick A. C. P., Franco O. E., Hayward S. W. and Thomson A. A. (2011). Expression of pleiotrophin in the prostate is androgen regulated and it functions as an autocrine regulator of mesenchyme and cancer associated fibroblasts and as a paracrine regulator of epithelia. Prostate 71, 305-317. 10.1002/pros.21244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ousset M., Van Keymeulen A., Bouvencourt G., Sharma N., Achouri Y., Simons B. D. and Blanpain C. (2012). Multipotent and unipotent progenitors contribute to prostate postnatal development. Nat. Cell Biol. 14, 1131-1138. 10.1038/ncb2600 [DOI] [PubMed] [Google Scholar]
- Park H.-J. and Bolton E. C. (2015). Glial cell line-derived neurotrophic factor induces cell proliferation in the mouse urogenital sinus. Mol. Endocrinol. 29, 289-306. 10.1210/me.2014-1312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng Y.-C., Levine C. M., Zahid S., Wilson E. L. and Joyner A. L. (2013). Sonic hedgehog signals to multiple prostate stromal stem cells that replenish distinct stromal subtypes during regeneration. Proc. Natl. Acad. Sci. USA 110, 20611-20616. 10.1073/pnas.1315729110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce G. B. and Speers W. C. (1988). Tumors as caricatures of the process of tissue renewal: prospects for therapy by directing differentiation. Cancer Res. 48, 1996-2004. [PubMed] [Google Scholar]
- Pignon J.-C., Grisanzio C., Geng Y., Song J., Shivdasani R. A. and Signoretti S. (2013). p63-expressing cells are the stem cells of developing prostate, bladder, and colorectal epithelia. Proc. Natl. Acad. Sci. USA 110, 8105-8110. 10.1073/pnas.1221216110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podlasek C. A., Duboule D. and Bushman W. (1997). Male accessory sex organ morphogenesis is altered by loss of function of Hoxd-13. Dev. Dyn. 208, 454-465. [DOI] [PubMed] [Google Scholar]
- Podlasek C. A., Barnett D. H., Clemens J. Q., Bak P. M. and Bushman W. (1999a). Prostate development requires Sonic hedgehog expressed by the urogenital sinus epithelium. Dev. Biol. 209, 28-39. 10.1006/dbio.1999.9229 [DOI] [PubMed] [Google Scholar]
- Podlasek C. A., Clemens J. Q. and Bushman W. (1999b). Hoxa-13 gene mutation results in abnormal seminal vesicle and prostate development. J. Urol. 161, 1655-1661. 10.1016/S0022-5347(05)68999-9 [DOI] [PubMed] [Google Scholar]
- Podlasek C. A., Seo R. M., Clemens J. Q., Ma L., Maas R. L. and Bushman W. (1999c). Hoxa-10 deficient male mice exhibit abnormal development of the accessory sex organs. Dev. Dyn. 214, 1-12. [DOI] [PubMed] [Google Scholar]
- Pointis G., Latreille M.-T., Mignot T.-M., Janssens Y. and Cedard L. (1979). Regulation of testosterone synthesis in the fetal mouse testis. J Steroid Biochem 11, 1609-1612. 10.1016/0022-4731(79)90357-1 [DOI] [PubMed] [Google Scholar]
- Pointis G., Latreille M.-T. and Cedard L. (1980). Gonado-pituitary relationships in the fetal mouse at various times during sexual differentiation. J. Endocrinol. 86, 483-488. 10.1677/joe.0.0860483 [DOI] [PubMed] [Google Scholar]
- Price D. (1936). Normal development of the prostate and seminal vesicles of the rat with a study of experimental postnatal modifications. Am. J. Anat. 60, 79-128. 10.1002/aja.1000600105 [DOI] [Google Scholar]
- Price D. (1963). Comparative aspects of development and structure in the prostate. Natl. Cancer Inst. Monogr. 12, 1-27. [PubMed] [Google Scholar]
- Pritchard C., Mecham B., Dumpit R., Coleman I., Bhattacharjee M., Chen Q., Sikes R. A. and Nelson P. S. (2009). Conserved gene expression programs integrate mammalian prostate development and tumorigenesis. Cancer Res. 69, 1739-1747. 10.1158/0008-5472.CAN-07-6817 [DOI] [PubMed] [Google Scholar]
- Richardson G. D., Robson C. N., Lang S. H., Neal D. E., Maitland N. J. and Collins A. T. (2004). CD133, a novel marker for human prostatic epithelial stem cells. J. Cell Sci. 117, 3539-3545. 10.1242/jcs.01222 [DOI] [PubMed] [Google Scholar]
- Romero D., Kawano Y., Bengoa N., Walker M. M., Maltry N., Niehrs C., Waxman J. and Kypta R. (2013). Downregulation of Dickkopf-3 disrupts prostate acinar morphogenesis through TGF-beta/Smad signalling. J. Cell Sci. 126, 1858-1867. 10.1242/jcs.119388 [DOI] [PubMed] [Google Scholar]
- Ruan W., Powell-Braxton L., Kopchick J. J. and Kleinberg D. L. (1999). Evidence that insulin-like growth factor I and growth hormone are required for prostate gland development. Endocrinology 140, 1984-1989. 10.1210/en.140.5.1984 [DOI] [PubMed] [Google Scholar]
- Schaeffer E. M., Marchionni L., Huang Z., Simons B., Blackman A., Yu W., Parmigiani G. and Berman D. M. (2008). Androgen-induced programs for prostate epithelial growth and invasion arise in embryogenesis and are reactivated in cancer. Oncogene 27, 7180-7191. 10.1038/onc.2008.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifert A. W., Harfe B. D. and Cohn M. J. (2008). Cell lineage analysis demonstrates an endodermal origin of the distal urethra and perineum. Dev. Biol. 318, 143-152. 10.1016/j.ydbio.2008.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shappell S. B., Thomas G. V., Roberts R. L., Herbert R., Ittmann M. M., Rubin M. A., Humphrey P. A., Sundberg J. P., Rozengurt N., Barrios R. et al. (2004). Prostate pathology of genetically engineered mice: definitions and classification. The consensus report from the Bar Harbor meeting of the Mouse Models of Human Cancer Consortium Prostate Pathology Committee. Cancer Res. 64, 2270-2305. 10.1158/0008-5472.CAN-03-0946 [DOI] [PubMed] [Google Scholar]
- Shaw A., Attia S. and Bushman W. (2008). Prostate stromal and urogenital sinus mesenchymal cell lines for investigations of stromal-epithelial interactions. Differentiation 76, 599-605. 10.1111/j.1432-0436.2008.00275.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen M. M. and Abate-Shen C. (2010). Molecular genetics of prostate cancer: new prospects for old challenges. Genes Dev. 24, 1967-2000. 10.1101/gad.1965810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibata M. and Shen M. M. (2015). Stem cells in genetically-engineered mouse models of prostate cancer. Endocr Relat. Cancer 22, T199-T208. 10.1530/ERC-15-0367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel R. L., Miller K. D. and Jemal A. (2016). Cancer statistics, 2016. CA Cancer J. Clin. 66, 7-30. 10.3322/caac.21332 [DOI] [PubMed] [Google Scholar]
- Signoretti S., Waltregny D., Dilks J., Isaac B., Lin D., Garraway L., Yang A., Montironi R., McKeon F. and Loda M. (2000). p63 is a prostate basal cell marker and is required for prostate development. Am. J. Pathol. 157, 1769-1775. 10.1016/S0002-9440(10)64814-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Signoretti S., Pires M. M., Lindauer M., Horner J. W., Grisanzio C., Dhar S., Majumder P., McKeon F., Kantoff P. W., Sellers W. R. et al. (2005). p63 regulates commitment to the prostate cell lineage. Proc. Natl. Acad. Sci. USA. 102, 11355-11360. 10.1073/pnas.0500165102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siiteri P. K. and Wilson J. D. (1974). Testosterone formation and metabolism during male sexual differentiation in the human embryo. J. Clin. Endocrinol. Metab. 38, 113-125. 10.1210/jcem-38-1-113 [DOI] [PubMed] [Google Scholar]
- Simons B. W., Hurley P. J., Huang Z., Ross A. E., Miller R., Marchionni L., Berman D. M. and Schaeffer E. M. (2012). Wnt signaling though beta-catenin is required for prostate lineage specification. Dev. Biol. 371, 246-255. 10.1016/j.ydbio.2012.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song H., Yao E., Lin C., Gacayan R., Chen M.-H. and Chuang P.-T. (2012). Functional characterization of pulmonary neuroendocrine cells in lung development, injury, and tumorigenesis. Proc. Natl. Acad. Sci. USA 109, 17531-17536. 10.1073/pnas.1207238109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sreekumar A., Roarty K. and Rosen J. M. (2015). The mammary stem cell hierarchy: a looking glass into heterogeneous breast cancer landscapes. Endocr Relat. Cancer 22, T161-T176. 10.1530/ERC-15-0263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugimura Y., Cunha G. R. and Donjacour A. A. (1986a). Morphological and histological study of castration-induced degeneration and androgen-induced regeneration in the mouse prostate. Biol. Reprod. 34, 973-983. 10.1095/biolreprod34.5.973 [DOI] [PubMed] [Google Scholar]
- Sugimura Y., Cunha G. R., Donjacour A. A., Bigsby R. M. and Brody J. R. (1986b). Whole-mount autoradiography study of DNA synthetic activity during postnatal development and androgen-induced regeneration in the mouse prostate. Biol. Reprod. 34, 985-995. 10.1095/biolreprod34.5.985 [DOI] [PubMed] [Google Scholar]
- Sugimura Y., Foster B. A., Hom Y. K., Lipschutz J. H., Rubin J. S., Finch P. W., Aaronson S. A., Hayashi N., Kawamura J. and Cunha G. R. (1996). Keratinocyte growth factor (KGF) can replace testosterone in the ductal branching morphogenesis of the rat ventral prostate. Int. J. Dev. Biol. 40, 941-951. [PubMed] [Google Scholar]
- Sun Y., Campisi J., Higano C., Beer T. M., Porter P., Coleman I., True L. and Nelson P. S. (2012). Treatment-induced damage to the tumor microenvironment promotes prostate cancer therapy resistance through WNT16B. Nat. Med. 18, 1359-1368. 10.1038/nm.2890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szczyrba J., Niesen A., Wagner M., Wandernoth P. M., Aumüller G. and Wennemuth G. (2017). Neuroendocrine cells of the prostate derive from the neural crest. J. Biol. Chem. 292, 2021-2031. 10.1074/jbc.M116.755082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeda H., Lasnitzki I. and Mizuno T. (1986). Analysis of prostatic bud induction by brief androgen treatment in the fetal rat urogenital sinus. J. Endocrinol. 110, 467-470. 10.1677/joe.0.1100467 [DOI] [PubMed] [Google Scholar]
- Tan P. Y., Chang C. W., Chng K. R., Wansa K. D. S. A., Sung W.-K. and Cheung E. (2012). Integration of regulatory networks by NKX3-1 promotes androgen-dependent prostate cancer survival. Mol. Cell. Biol. 32, 399-414. 10.1128/MCB.05958-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor R. A., Wang H., Wilkinson S. E., Richards M. G., Britt K. L., Vaillant F., Lindeman G. J., Visvader J. E., Cunha G. R., St John J. et al. (2009). Lineage enforcement by inductive mesenchyme on adult epithelial stem cells across developmental germ layers. Stem Cells 27, 3032-3042. 10.1002/stem.244 [DOI] [PubMed] [Google Scholar]
- Tenniswood M. (1986). Role of epithelial-stromal interactions in the control of gene expression in the prostate: an hypothesis. Prostate 9, 375-385. 10.1002/pros.2990090407 [DOI] [PubMed] [Google Scholar]
- Thomsen M. K., Butler C. M., Shen M. M. and Swain A. (2008). Sox9 is required for prostate development. Dev. Biol. 316, 302-311. 10.1016/j.ydbio.2008.01.030 [DOI] [PubMed] [Google Scholar]
- Thomson A. A. (2008). Mesenchymal mechanisms in prostate organogenesis. Differentiation 76, 587-598. 10.1111/j.1432-0436.2008.00296.x [DOI] [PubMed] [Google Scholar]
- Thomson A. A. and Cunha G. R. (1999). Prostatic growth and development are regulated by FGF10. Development 126, 3693-3701. [DOI] [PubMed] [Google Scholar]
- Thomson A. A. and Marker P. C. (2006). Branching morphogenesis in the prostate gland and seminal vesicles. Differentiation 74, 382-392. 10.1111/j.1432-0436.2006.00101.x [DOI] [PubMed] [Google Scholar]
- Thomson A. A., Foster B. A. and Cunha G. R. (1997). Analysis of growth factor and receptor mRNA levels during development of the rat seminal vesicle and prostate. Development 124, 2431-2439. [DOI] [PubMed] [Google Scholar]
- Thomson A. A., Timms B. G., Barton L., Cunha G. R. and Grace O. C. (2002). The role of smooth muscle in regulating prostatic induction. Development 129, 1905-1912. [DOI] [PubMed] [Google Scholar]
- Timms B. G. (2008). Prostate development: a historical perspective. Differentiation 76, 565-577. 10.1111/j.1432-0436.2008.00278.x [DOI] [PubMed] [Google Scholar]
- Timms B. G. and Hofkamp L. E. (2011). Prostate development and growth in benign prostatic hyperplasia. Differentiation 82, 173-183. 10.1016/j.diff.2011.08.002 [DOI] [PubMed] [Google Scholar]
- Timms B. G., Lee C. W., Aumüller G. and Seitz J. (1995). Instructive induction of prostate growth and differentiation by a defined urogenital sinus mesenchyme. Microsc. Res. Tech. 30, 319-332. 10.1002/jemt.1070300407 [DOI] [PubMed] [Google Scholar]
- Timms B. G., Petersen S. L. and vom Saal F. S. (1999). Prostate gland growth during development is stimulated in both male and female rat fetuses by intrauterine proximity to female fetuses. J. Urol. 161, 1694-1701. 10.1016/S0022-5347(05)69007-6 [DOI] [PubMed] [Google Scholar]
- Toivanen R., Mohan A. and Shen M. M. (2016). Basal progenitors contribute to repair of the prostate epithelium following induced luminal anoikis. Stem Cell Reports 6, 660-667. 10.1016/j.stemcr.2016.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trompetter M., Smedts F., van der Wijk J., Schoots C., de Jong H. J., Hopman A. and de la Rosette J. (2008). Keratin profiling in the developing human prostate. A different approach to understanding epithelial lineage. Anticancer Res. 28, 237-243. [PubMed] [Google Scholar]
- Tsujimura A., Koikawa Y., Salm S., Takao T., Coetzee S., Moscatelli D., Shapiro E., Lepor H., Sun T. T. and Wilson E. L. (2002). Proximal location of mouse prostate epithelial stem cells: a model of prostatic homeostasis. J. Cell Biol. 157, 1257-1265. 10.1083/jcb.200202067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuxhorn J. A., Ayala G. E. and Rowley D. R. (2001). Reactive stroma in prostate cancer progression. J. Urol. 166, 2472-2483. 10.1016/S0022-5347(05)65620-0 [DOI] [PubMed] [Google Scholar]
- Verhagen A. P. M., Aalders T. W., Ramaekers F. C. S., Debruyne F. M. J. and Schalken J. A. (1988). Differential expression of keratins in the basal and luminal compartments of rat prostatic epithelium during degeneration and regeneration. Prostate 13, 25-38. 10.1002/pros.2990130104 [DOI] [PubMed] [Google Scholar]
- Verhagen A. P., Ramaekers F. C., Aalders T. W., Schaafsma H. E., Debruyne F. M. and Schalken J. A. (1992). Colocalization of basal and luminal cell-type cytokeratins in human prostate cancer. Cancer Res. 52, 6182-6187. [PubMed] [Google Scholar]
- Vezina C. M., Allgeier S. H., Fritz W. A., Moore R. W., Strerath M., Bushman W. and Peterson R. E. (2008). Retinoic acid induces prostatic bud formation. Dev. Dyn. 237, 1321-1333. 10.1002/dvdy.21526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z. A. and Shen M. M. (2011). Revisiting the concept of cancer stem cells in prostate cancer. Oncogene 30, 1261-1271. 10.1038/onc.2010.530 [DOI] [PubMed] [Google Scholar]
- Wang Y., Hayward S., Cao M., Thayer K. and Cunha G. (2001). Cell differentiation lineage in the prostate. Differentiation 68, 270-279. 10.1046/j.1432-0436.2001.680414.x [DOI] [PubMed] [Google Scholar]
- Wang B. E., Shou J., Ross S., Koeppen H., De Sauvage F. J. and Gao W.-Q. (2003). Inhibition of epithelial ductal branching in the prostate by sonic hedgehog is indirectly mediated by stromal cells. J. Biol. Chem. 278, 18506-18513. 10.1074/jbc.M300968200 [DOI] [PubMed] [Google Scholar]
- Wang X.-D., Shou J., Wong P., French D. M. and Gao W.-Q. (2004). Notch1-expressing cells are indispensable for prostatic branching morphogenesis during development and re-growth following castration and androgen replacement. J. Biol. Chem. 279, 24733-24744. 10.1074/jbc.M401602200 [DOI] [PubMed] [Google Scholar]
- Wang X.-D., Leow C. C., Zha J., Tang Z., Modrusan Z., Radtke F., Aguet M., de Sauvage F. J. and Gao W.-Q. (2006). Notch signaling is required for normal prostatic epithelial cell proliferation and differentiation. Dev. Biol. 290, 66-80. 10.1016/j.ydbio.2005.11.009 [DOI] [PubMed] [Google Scholar]
- Wang H., Leav I., Ibaragi S., Wegner M., Hu G. F., Lu M. L., Balk S. P. and Yuan X. (2008). SOX9 is expressed in human fetal prostate epithelium and enhances prostate cancer invasion. Cancer Res. 68, 1625-1630. 10.1158/0008-5472.CAN-07-5915 [DOI] [PubMed] [Google Scholar]
- Wang X., Kruithof-de Julio M., Economides K. D., Walker D., Yu H. L., Halili M. V., Hu Y. P., Price S. M., Abate-Shen C. and Shen M. M. (2009). A luminal epithelial stem cell that is a cell of origin for prostate cancer. Nature 461, 495-500. 10.1038/nature08361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Lunardi A., Zhang J., Chen Z., Ala U., Webster K. A., Tay Y., Gonzalez-Billalabeitia E., Egia A., Shaffer D. R. et al. (2013a). Zbtb7a suppresses prostate cancer through repression of a Sox9-dependent pathway for cellular senescence bypass and tumor invasion. Nat. Genet. 45, 739-746. 10.1038/ng.2654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z. A., Mitrofanova A., Bergren S. K., Abate-Shen C., Cardiff R. D., Califano A. and Shen M. M. (2013b). Lineage analysis of basal epithelial cells reveals their unexpected plasticity and supports a cell-of-origin model for prostate cancer heterogeneity. Nat. Cell Biol. 15, 274-283. 10.1038/ncb2697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B. E., Wang X., Long J. E., Eastham-Anderson J., Firestein R. and Junttila M. R. (2015). Castration-resistant Lgr5+ cells are long-lived stem cells required for prostatic regeneration. Stem Cell Rep. 4, 768-779. 10.1016/j.stemcr.2015.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warot X., Fromental-Ramain C., Fraulob V., Chambon P. and Dolle P. (1997). Gene dosage-dependent effects of the Hoxa-13 and Hoxd-13 mutations on morphogenesis of the terminal parts of the digestive and urogenital tracts. Development 124, 4781-4791. [DOI] [PubMed] [Google Scholar]
- Watson P. A., Arora V. K. and Sawyers C. L. (2015). Emerging mechanisms of resistance to androgen receptor inhibitors in prostate cancer. Nat. Rev. Cancer 15, 701-711. 10.1038/nrc4016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Daniels G., Shapiro E., Xu K., Huang H., Li Y., Logan S., Greco M. A., Peng Y., Monaco M. E. et al. (2011). LEF1 identifies androgen-independent epithelium in the developing prostate. Mol. Endocrinol. 25, 1018-1026. 10.1210/me.2010-0513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wuidart A., Ousset M., Rulands S., Simons B. D., Van Keymeulen A. and Blanpain C. (2016). Quantitative lineage tracing strategies to resolve multipotency in tissue-specific stem cells. Genes Dev. 30, 1261-1277. 10.1101/gad.280057.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu B., Hariharan A., Rakshit S., Dressler G. R. and Wellik D. M. (2012). The role of Pax2 in mouse prostate development. Prostate 72, 217-224. 10.1002/pros.21424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue Y., Smedts F., Debruyne F. M. J., de la Rosette J. J. and Schalken J. A. (1998). Identification of intermediate cell types by keratin expression in the developing human prostate. Prostate 34, 292-301. [DOI] [PubMed] [Google Scholar]
- Yan G., Fukabori Y., Nikolaropoulos S., Wang F. and McKeehan W. L. (1992). Heparin-binding keratinocyte growth factor is a candidate stromal-to-epithelial-cell andromedin. Mol. Endocrinol. 6, 2123-2128. [DOI] [PubMed] [Google Scholar]
- Yu M. and Bushman W. (2013). Differential stage-dependent regulation of prostatic epithelial morphogenesis by Hedgehog signaling. Dev. Biol. 380, 87-98. 10.1016/j.ydbio.2013.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaviacic M. and Ablin R. J. (1998). The female prostate. J. Natl. Cancer Inst. 90, 713-714. 10.1093/jnci/90.9.713 [DOI] [PubMed] [Google Scholar]
- Zaviacic M. and Ablin R. J. (2000). The female prostate and prostate-specific antigen. Immunohistochemical localization, implications of this prostate marker in women and reasons for using the term ‘prostate’ in the human female. Histol. Histopathol. 15, 131-142. [DOI] [PubMed] [Google Scholar]
- Zhang T.-J., Hoffman B. G., Ruiz de Algara T. and Helgason C. D. (2006). SAGE reveals expression of Wnt signalling pathway members during mouse prostate development. Gene Expr. Patterns 6, 310-324. 10.1016/j.modgep.2005.07.005 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Zhang J., Lin Y., Lan Y., Lin C., Xuan J. W., Shen M. M., McKeehan W. L., Greenberg N. M. and Wang F. (2008). Role of epithelial cell fibroblast growth factor receptor substrate 2alpha in prostate development, regeneration and tumorigenesis. Development 135, 775-784. 10.1242/dev.009910 [DOI] [PubMed] [Google Scholar]