Abstract
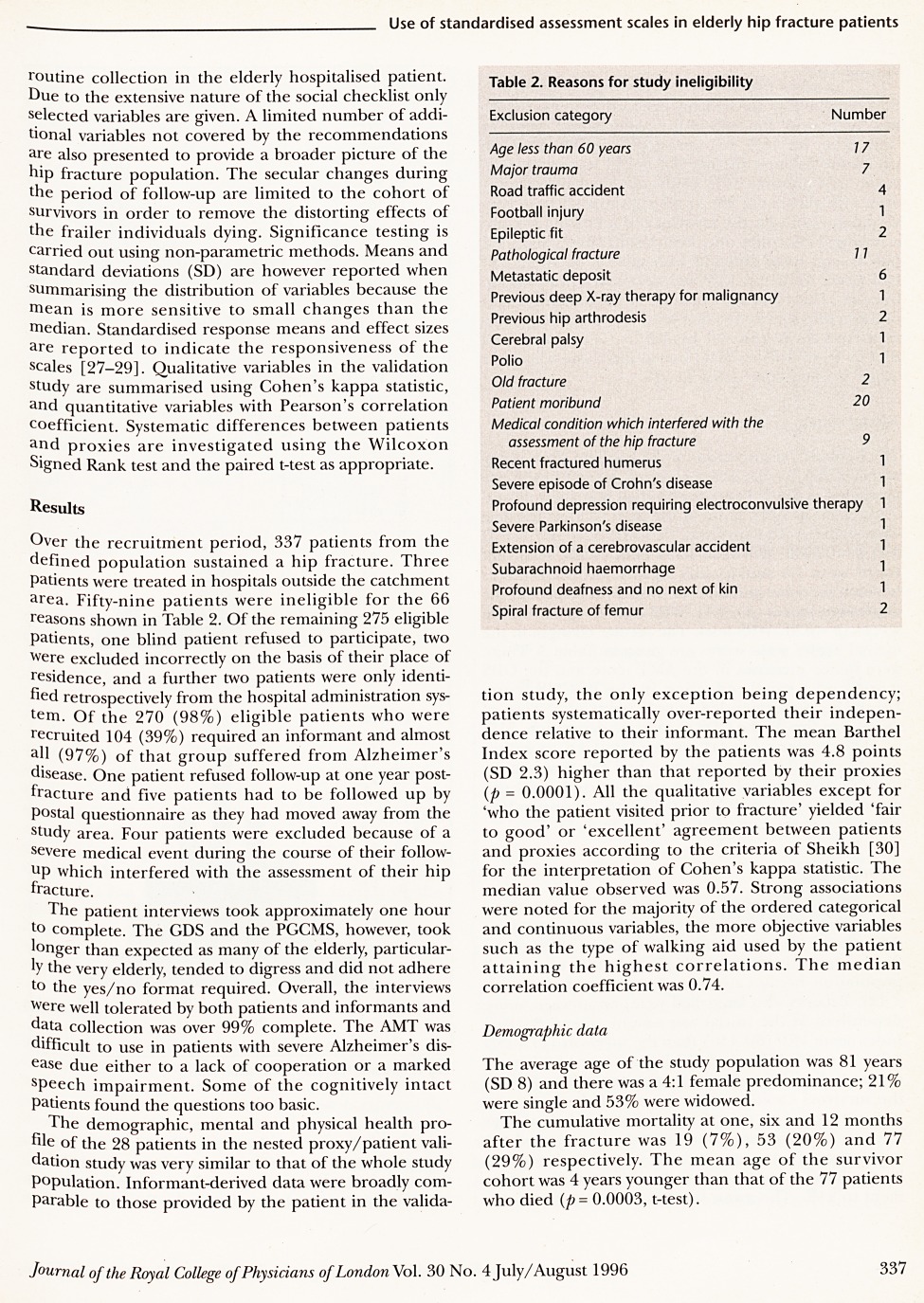
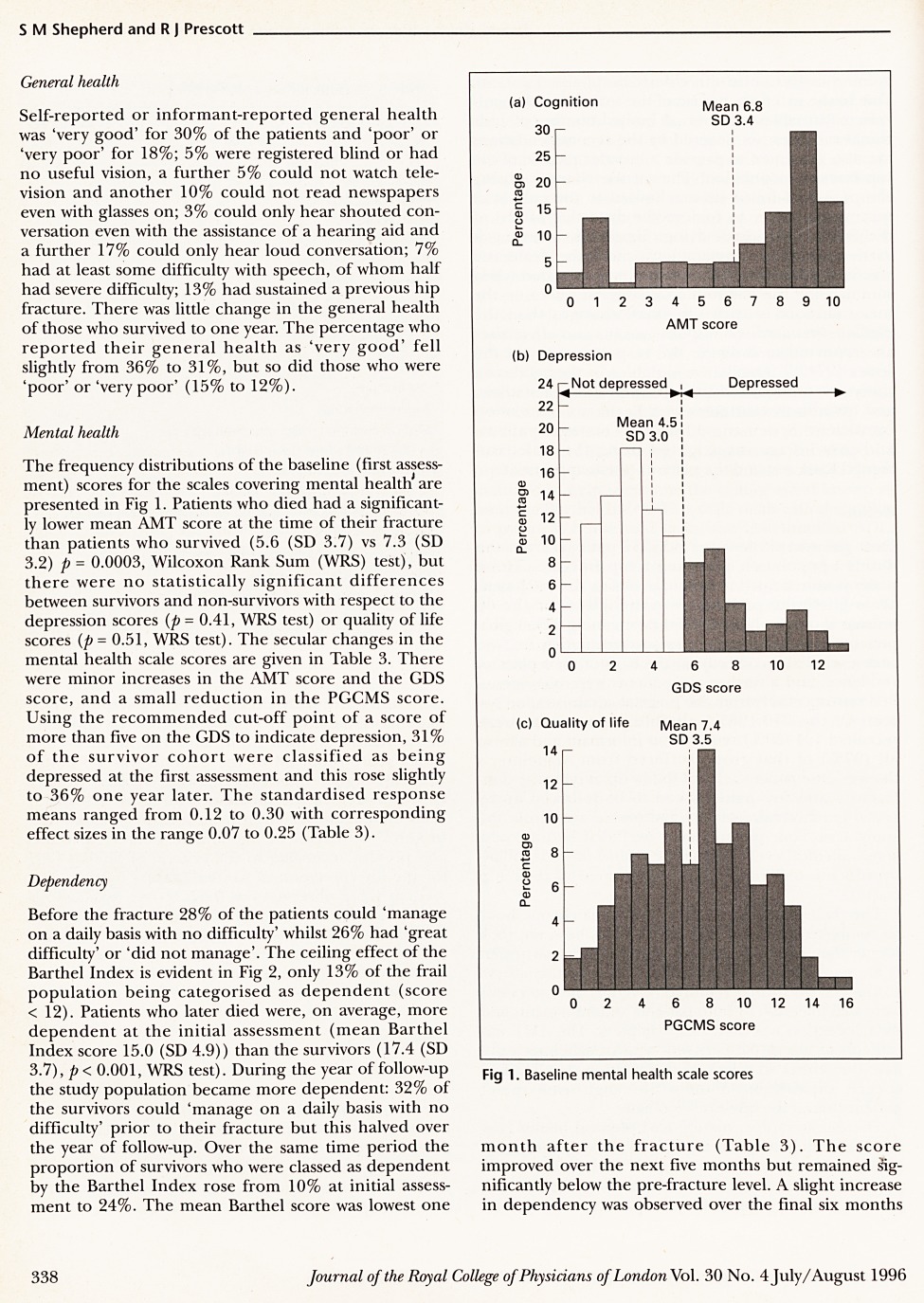
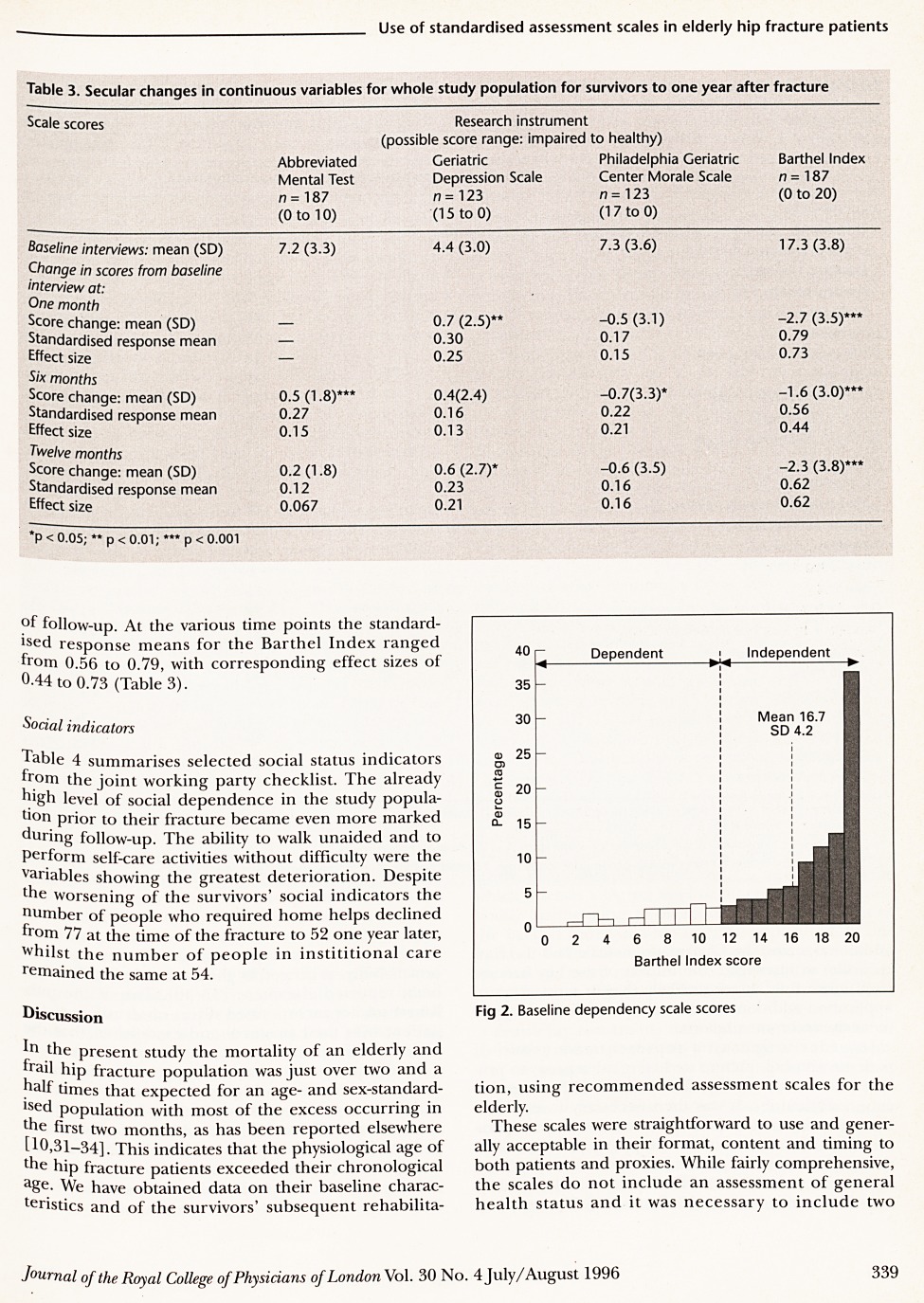
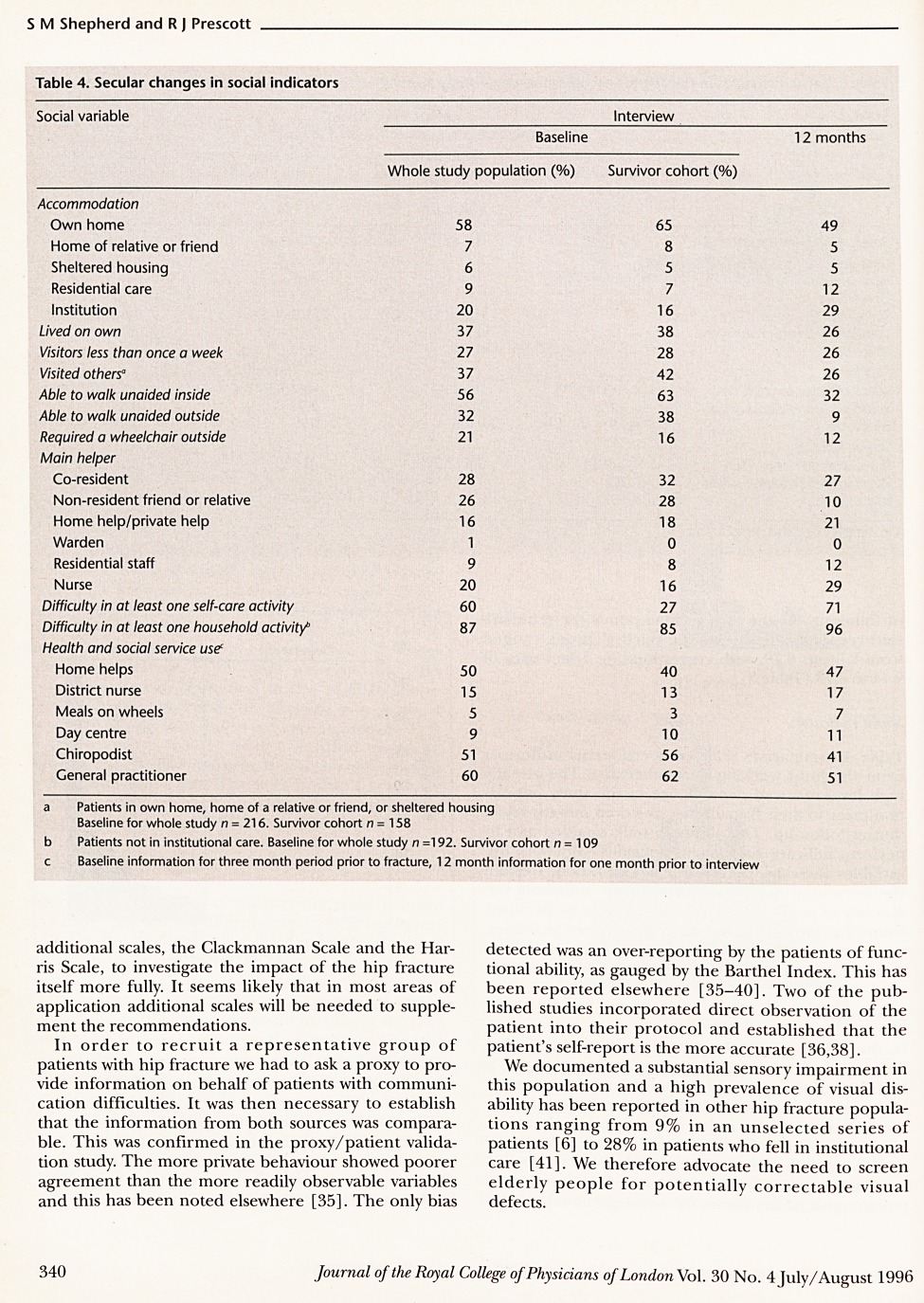
Standardised scales recommended by a joint working party from the Royal College of Physicians (RCP) and The British Geriatrics Society (BGS) in 1992 for the assessment of elderly hospitalised patients were employed in an elderly hip fracture population to investigate their feasibility and usefulness in this group. Patients were assessed at the time of their fracture and one, six and 12 months later. An informant was invited to provide information on behalf of patients (39%) who were classified as having significant memory and cognitive impairment (Abbreviated Mental Test score < 7) or if they had some other communication difficulty. Patients and informants found the format and content of the scales acceptable as well as the administration time of around one hour. Difficulties with the depression (Geriatric Depression Scale) and quality of life (Philadelphia Geriatric Center Morale Scale) scales were due to some patients' digressions, and the fact that little change was noted in the scores over the one-year period of follow-up questions their sensitivity. In the cohort of survivors 31% were classified as being depressed at baseline (score > 5) and this rose to 36% at one year. Ten per cent of the surviving patients were classed as dependent by the Barthel Index at the time of their fracture (score < 12) and this increased to 24% at one year. Despite exhibiting a ceiling effect, this scale was the most responsive of the scales at all time points. The social checklist highlighted important aspects for the management of hip fracture patients.
Full text
PDF


Contributor Information
S M Shepherd, Lecturer in Epidemiology, University of Edinburgh.
R J Prescott, Director of Medical Statistics Unit, University of Edinburgh.