Abstract
Objective
To investigate whether foot and/or ankle symptoms increase the risk of developing (i) knee symptoms and (ii) symptomatic radiographic knee osteoarthritis (OA).
Design
1020 Osteoarthritis Initiative participants who were at-risk of knee OA, but were without knee symptoms or radiographic knee OA, were investigated. Participants indicated the presence and laterality of foot/ankle symptoms at baseline. The main outcome was development of knee symptoms (pain, aching or stiffness in and around the knee on most days of the month for at least one month in the past year). A secondary outcome was development of symptomatic radiographic knee OA (symptoms plus Kellgren and Lawrence [KL] grade ≥2), over the subsequent four years. Associations between foot/ankle symptoms and study outcomes were assessed by logistic regression models.
Results
Foot/ankle symptoms in either or both feet significantly increased the odds of developing knee symptoms (adjusted odds ratio (OR) 1.55, 95% confidence interval (CI) 1.10 to 2.19), and developing symptomatic radiographic knee OA (adjusted OR 3.28, 95% CI 1.69 to 6.37). Based on laterality, contralateral foot/ankle symptoms were associated with developing both knee symptoms (adjusted OR 1.68, 95% CI 1.05 to 2.68) and symptomatic radiographic knee OA (adjusted OR 3.08, 95% CI 1.06 to 8.98), whilst bilateral foot/ankle symptoms were associated with developing symptomatic radiographic knee OA (adjusted OR 4.02, 95% CI 1.76 to 9.17).
Conclusion
In individuals at-risk of knee OA, the presence of contralateral foot/ankle symptoms in particular increases risk of developing both knee symptoms and symptomatic radiographic knee OA.
Keywords: Osteoarthritis, Knee Osteoarthritis, Arthritis, Epidemiology
INTRODUCTION
Knee osteoarthritis (OA) is a leading cause of joint pain1 and disability2 in middle- and older-aged individuals, and is one of the most commonly managed conditions in primary care3. Recent incidence rates suggest around 6% of people aged over 45 years develop knee symptoms each year, whilst 2% develop symptomatic radiographic knee OA4. Knee OA symptoms and radiographic change that worsen over time can lead to costly surgical intervention. Thus understanding risk factors associated with the onset of knee symptoms alone or in combination with structural change is a major research focus.
Symptoms in the foot and/or ankle is a potential risk factor for knee pain and OA that has received limited attention to date. Like knee OA, foot/ankle symptoms are very common in middle- and older-aged adults. They affect approximately 24% of people aged over 45 years5, and account for a substantial number of primary care consultations in this population6. Foot pain is highly disabling, reduces quality of life7, adversely affects walking and other daily functional abilities7 and increases the risk of falls8. To date, the majority of studies investigating symptoms at the foot/ankle and knee have examined these problems in isolation. However, isolated joint pain is rare9, and concurrent symptoms at the foot/ankle and knee is the most common multi-joint presentation10, occurring far greater than expected by chance alone. In a recent cross-sectional study using data from the Osteoarthritis Initiative (OAI), we found that people with both symptomatic radiographic knee OA and foot/ankle symptoms reported significantly worse general and knee OA specific health outcomes, and poorer physical function, than those with knee OA but without foot/ankle symptoms11. Despite the strong association between problems at these two sites, their temporal sequence has not yet been evaluated.
Investigating foot/ankle symptoms as a candidate risk factor for knee OA is attractive as it is simple to assess, and there is some evidence of potential modifiability using simple low-cost interventions such as off-the-shelf footwear12. Furthermore, there are a number of plausible biological mechanisms linking foot/ankle symptoms to knee OA development. For example, there may be shared biomechanical risk factors for the two problems, such as a pronated foot type13 or inappropriate footwear14. Alternatively, people with foot/ankle symptoms may walk differently to offload their painful foot15–17, altering knee function and increasing the risk of knee OA development. Finally, symptoms at these two sites may represent a widespread pain phenotype or an oligo- or polyarticular form of OA18.
The primary aim of this study was to use longitudinal data from the OAI to examine whether foot/ankle symptoms predict the development of knee symptoms over four years in people without knee symptoms or radiographic knee OA, but at-risk of knee OA, at baseline. A secondary aim was to examine whether foot/ankle symptoms also predict the development of symptomatic radiographic knee OA over four years. It was hypothesized that foot/ankle symptoms would increase the odds of developing knee symptoms and symptomatic radiographic knee OA in people at risk of knee OA.
METHODS
Study population
The OAI is an ongoing prospective multicentre cohort study designed to evaluate and identify biomarkers for the onset and/or progression of knee OA in people aged between 45–79 years. The study enrolled 4796 men and women from four sites in the United States, including Baltimore, Maryland; Columbus, Ohio; Pittsburgh, Pennsylvania; and Pawtucket, Rhode Island. All protocols and procedures were approved by the institutional review board at each site19 and all participants provided informed consent. Details regarding general exclusion criteria and the wider study protocols are available online for public access (http://www.oai.ucsf.edu/). In the current study, we analyzed OAI participants who were at risk of knee OA, defined as the presence of two or more established characteristics including: overweight, identified using age- and sex-specific criteria; a history of knee injury causing walking difficulties; any knee surgery; an immediate family history of a total knee replacement for OA; Heberden’s nodes; repetitive knee bending during occupational or recreation activities; or aged between 70–79 years. From this subcohort, we only included people who did not have frequent knee symptoms (defined as pain, aching or stiffness in and around the knee on most days of the month for at least one month in the past year) or radiographic evidence of knee OA (Kellgren and Lawrence [KL] grade ≥2) in either knee at baseline. We excluded people (rather than knees) with these outcomes because the presence of symptomatic knee OA in one knee greatly increases the risk of developing contralateral knee OA which may confound results20–22. Demographic, clinical and radiographic characteristics of both knees for all participants were evaluated at baseline and at 12, 24, 36 and 48-month follow-up visits.
Demographic characteristics and covariates
Demographic data collected included age, sex and race (White, Black/African American or Asian/other non-white). Covariates included body mass index (BMI),, comorbidities and depression. As well as recording BMI values, we also classified participants as obese (>30 kg/m2), overweight (≥25 and ≤30 kg/m2) or normal weight (<25 kg/m2). Comorbidities were assessed using the questionnaire version of the Charlson comorbidity index (CCI)23, and we dichotomized the cohort into those with ‘no comorbidities’ and those with ‘one or more comorbidities’. Depression was measured using the Centre for Epidemiological Studies Depression Scale (CES-D). Scores were summed and a score of ≥ 16 was used to indicate significant depressive symptoms24.
Risk factor
The primary risk factor was self-reported foot/ankle symptoms at baseline, defined as pain, aching or stiffness in the foot and/or ankle on more than half of the days during the past 30 days, consistent with definitions used in previous studies5, 10. In addition to classifying participants based on the presence or absence of symptoms in either foot/ankle, we further stratified foot/ankle symptoms as ipsilateral, contralateral or bilateral relative to each knee.
Incidence outcomes
Knee symptoms
Participants were asked about the presence of knee symptoms at baseline, and at the 12, 24, 36 and 48 month follow-up visits for each knee. Incident knee symptoms was defined as development of pain, aching or stiffness in and around the knee on most days of the month for at least one month in the previous year, reported at any of the follow up visits, consistent with the OAI definition and based on American College of Rheumatology criteria for clinical knee OA25.
Symptomatic radiographic knee osteoarthritis
Weightbearing fixed-flexion posteroanterior radiographs of both knees were taken at baseline and at the 12, 24, 36 and 48 month follow-up visits. Radiographs were evaluated using the KL grading system (grades range 0–4) by two central OAI senior musculoskeletal experts blinded to all other participant data and to each other’s readings. Incident symptomatic radiographic knee OA was defined as knee symptoms (as per definition above) and the presence of KL grade ≥2 based on the central OAI reading, at any of the follow up visits.
Statistical analysis
Baseline characteristics of participants with and without foot/ankle symptoms were summarised as number (%) for categorical variables and as mean (SD) or median (interquartile range) for continuous variables, as appropriate. Groups were compared using χ-squared tests, analysis of variance, Wilcoxon rank-sum or Kruskal-Wallis rank tests respectively.
To investigate the primary aim (development of knee symptoms), we analysed the association between any foot/ankle symptoms (i.e. symptoms in either or both feet/ankle) at baseline and the development of knee symptoms at any point within the four year follow-up period. For both aims, analyses were knee-specific (i.e. conducted at the knee level rather than at the participant level). Since most participants contributed two knees (8 participants with missing data contributed one knee only for the primary aim, and 3 participants with missing data contributed one knee only for the secondary aim), logistic regression models were fitted using generalized estimating equations to account for the correlation between left and right knees within participants. Two models were fitted, adjusting for sets of baseline covariates determined a priori. In the first model, only baseline foot/ankle symptoms were included to obtain unadjusted associations between baseline foot/ankle symptoms and the development of outcomes. The second model also included age, sex, race, BMI, Charlson Comorbidity index (dichotomised) and depression to adjust for variables known to be associated with both foot pain26 and knee OA27.
In addition to considering whether any foot/ankle symptoms were associated with the outcome (i.e. at the participant level), we also investigated the association with ipsilateral, contralateral or bilateral foot/ankle symptoms (i.e. at the limb level) to see if the association differed by laterality. Logistic regression models were again fitted using generalized estimating equations to adjust for clustering of knees within participants. Covariates were adjusted for in the same way as in the primary analysis. Similar analyses were conducted to address the secondary aim (the development of symptomatic radiographic knee OA), and the set of baseline variables was adjusted as per for the primary aim.
To assess the potential influence of confounders (both measured and unmeasured by the OAI) that were not accounted for in our analyses, we performed sensitivity analyses. More specifically, a causal inference-based approach adapted from Kasza et al28 was used. This approach varies a sensitivity parameter that quantifies the differences between participants with and without foot/ankle symptoms, had those without foot/ankle symptoms instead had symptoms. The sensitivity parameter compares the outcomes between two groups with the same exposure (where the exposure is hypothetical in those without foot/ankle symptoms), but with the possibility of differences that were unaccounted for in our analyses leading to differences in the development of knee symptoms and/or symptomatic radiographic knee OA. Values of the sensitivity parameter greater than 1 suggest that unaccounted confounders in those participants who actually had foot/ankle symptoms, such as widespread pain or generalised OA, contributed to the greater likelihood of those participants developing the outcome. Values of the sensitivity parameter equal to 1 suggest that there is no impact of unaccounted-for confounding on the results. Statistical significance was ascribed at p-value ≤ 0.05. Stata v12 (Stata Corporation, College Station, TX, USA) was used for all analyses.
RESULTS
Sample characteristics
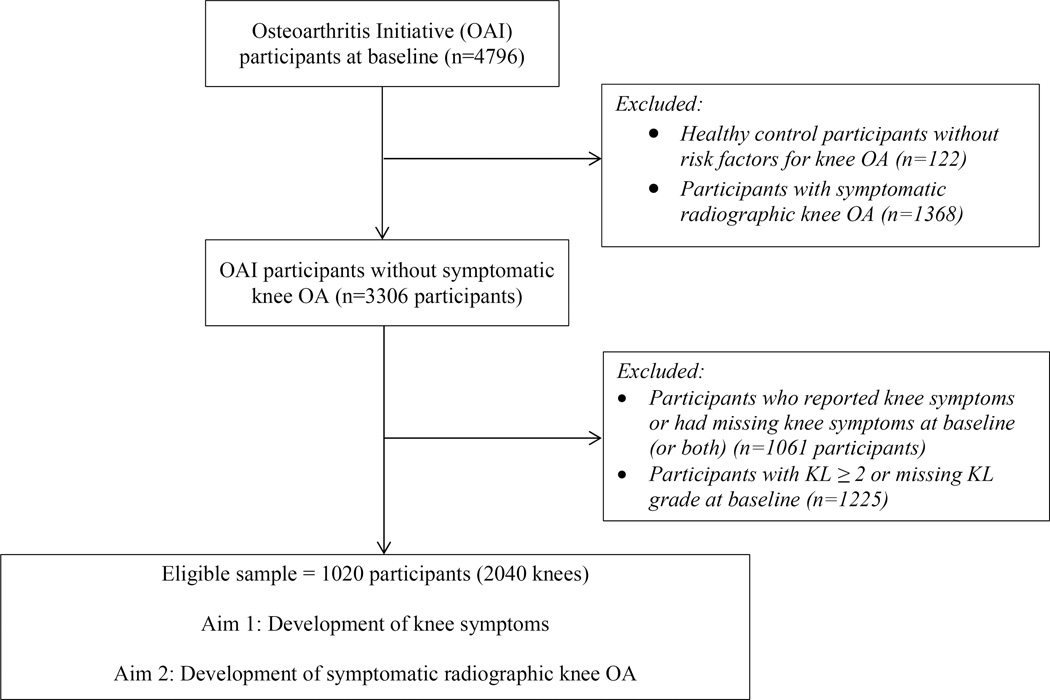
This study used OAI participants who did not have symptomatic radiographic knee OA (n=3306). Patients with knee symptoms (as defined previously) or radiographic knee OA (KL≥2) in one or both knees at baseline were excluded (n=2286) (Figure 1). Demographic data are presented in Table 1. Of the 1020 participants at baseline, 13% (n=133) reported symptoms in at least one foot/ankle. Those with foot/ankle symptoms were more likely to be female (p=0.014), younger (p=0.029), Black/African American (p<0.001) and have a higher BMI (p=0.003) at baseline. There were no differences in baseline measures of worst KL grade, comorbidities, depressive symptoms, shoulder pain, Heberden’s nodes, or previous knee injury or surgery between those with and without foot/ankle symptoms.
Figure 1.
Participants from the Osteoarthritis Initiative included in analysis.
Table 1.
Baseline characteristics of Osteoarthritis Initiative participants without knee pain classified based on the presence and side of foot/ankle symptoms. One participant had missing foot/ankle symptom status at baseline. Values are N (%) unless otherwise indicated.
| Characteristic | Missing (n) | No foot/ankle symptoms (n=887) | Any foot/ankle symptoms (n=133) | P value† |
|---|---|---|---|---|
| Mean (SD) age (years) | 0 | 60.9 (9.1) | 59.0 (9.3) | 0.029 |
| Sex | 0 | 0.014 | ||
| Male | 387 (43.6) | 43 (32.3) | ||
| Female | 500 (56.4) | 90 (67.7) | ||
| Race: | 0 | <0.001 | ||
| Asian and other non-white | 14 (1.6) | 10 (7.5) | ||
| White/Caucasian | 793 (89.4) | 107 (80.5) | ||
| Black/African American | 80 (9.0) | 16 (12.0) | ||
| Median (IQR) BMI kg/m2 | 1 | 26.4 (23.7, 30.0) | 27.7 (24.8, 32.0) | 0.003 |
| BMI categories: | 1 | 0.018 | ||
| Normal (BMI <25 kg/m2) |
317 (35.7) | 34 (25.6) | ||
| Overweight (BMI 25–30 kg/m2) |
347 (39.1) | 52 (39.1) | ||
| Obese (BMI >30 kg/m2) |
223 (25.1) | 47 (35.3) | ||
| Worst KL grade* | 0 | 0.937 | ||
| 0 | 568 (64.0) | 84 (63.2) | ||
| 1 | 319 (36.0) | 49 (36.8) | ||
| 2 | 0 (0) | 0 (0) | ||
| 3 | 0 (0) | 0 (0) | ||
| 4 | 0 (0) | 0 (0) | ||
| Comorbidities: | 0 | 0.134 | ||
| 0 | 692 (78.0) | 96 (72.2) | ||
| ≥1 | 195 (22.0) | 37 (27.8) | ||
| Depression | 8 | 0.351 | ||
| No | 827 (93.7) | 118 (91.5) | ||
| Yes | 56 (6.3) | 11 (8.5) |
SD, standard deviation; IQR, interquartile range; BMI, body mass index; KL, Kellgren Lawrence.
Baseline values
P-values from chi-squared test for binary and categorical variables, Wilcoxon rank-sum or Kruskal-Wallis rank tests for variables presented as median (IQR), and analysis of variance tests for variables presented as mean (SD).
Development of knee symptoms
Table 2 shows the odds of developing knee symptoms according to the presence and laterality of foot/ankle symptoms. After excluding knees with missing data, there were 1990 knees from 999 participants available for analysis. Baseline symptoms in any foot/ankle was associated with a significantly increased risk of developing knee symptoms in the subsequent four years (adjusted OR 1.55, 95% CI 1.10 to 2.19). Additional analyses of foot/ankle and knee symptom laterality showed that contralateral foot/ankle symptoms also increased the odds for developing knee symptoms (adjusted OR 1.68, 95% CI 1.05 to 2.68).
Table 2.
Logistic regression analyses for the risk of developing knee symptoms during the four year follow up period. GEEs fit to account for the clustering of knees within participants. 50 knees from 29 participants were excluded due to missing data.
| Laterality of foot/ankle symptoms |
Total number of knees (participants) |
No knee symptoms N (%) |
Knee symptoms N (%) |
Risk for knee symptoms | |||
|---|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) |
P value | Adjusted† OR (95% CI) |
P value | ||||
| No symptoms (ref) | 1742 (874) | 1135 (89.7) | 607 (83.8) | 1 | 1 | ||
| Any side | 248 (125) | 131 (10.3) | 117 (16.2) | 1.63 (1.16 to 2.27) | 0.004 | 1.55 (1.10 to 2.19) | 0.012 |
| Ipsilateral | 70 (70) | 40 (3.2) | 30 (4.1) | 1.34 (0.83 to 2.17) | 0.238 | 1.30 (0.80 to 2.12) | 0.294 |
| Contralateral | 72 (72) | 37 (2.9) | 35 (4.8) | 1.77 (1.11 to 2.84) | 0.017 | 1.68 (1.05 to 2.68) | 0.030 |
| Bilateral | 106 (53) | 54 (4.3) | 52 (7.2) | 1.74 (1.06 to 2.86) | 0.029 | 1.65 (0.98 to 2.78) | 0.060 |
OR, odds ratios; CI, confidence intervals.
Adjusted for age, sex, race, BMI, Charlson Comorbidity index (dichotomised) and depression.
Development of symptomatic radiographic knee OA
Table 3 shows the odds of developing symptomatic radiographic knee OA according to the presence and laterality of foot/ankle symptoms. After excluding knees with missing data, there were 1983 knees from 993 people available for analysis. Baseline symptoms in any foot/ankle was associated with a significantly increased risk of developing symptomatic radiographic knee OA at any time in the follow up period (adjusted OR 3.28, 95% CI 1.69 to 6.37). Subgroup analyses based on foot/ankle symptom laterality suggested bilateral foot/ankle symptoms had the highest odds for developing symptomatic radiographic knee OA (adjusted OR 4.02, 95% CI 1.76 to 9.17), and that foot/ankle symptoms that were contralateral to the affected knee also increased the risk of this outcome (adjusted OR 3.08, 95% CI 1.60 to 8.98).
Table 3.
Logistic regression analyses for the risk of developing symptomatic and radiographic knee OA, during the four year follow up period. GEEs fit to account for the clustering of knees within participants. 57 knees from 30 participants were excluded due to missing data.
| Laterality of foot/ankle symptoms |
Total number of knees (participants) |
No symptomatic knee ROA N (%) |
Symptomatic Knee ROA N (%) |
Risk for symptomatic knee ROA | |||
|---|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) |
P value | Adjusted† OR (95% CI) |
P value | ||||
| No symptoms (ref) | 1736 (869) | 1707 (88.1) | 29 (64.4) | 1 | 1 | ||
| Any side | 247 (124) | 231 (11.9) | 16 (35.6) | 4.26 (2.23 to 8.12) | <0.001 | 3.28 (1.69 to 6.37) | 0.0004 |
| Ipsilateral | 70 (70) | 67 (3.5) | 3 (6.7) | 2.57 (0.76 to 8.74) | 0.131 | 2.28 (0.70 to 7.37) | 0.171 |
| Contralateral | 71 (71) | 67 (3.5) | 4 (8.9) | 4.35 (1.61 to 11.74) | 0.004 | 3.08 (1.06 to 8.98) | 0.039 |
| Bilateral | 106 (53) | 97 (5.0) | 9 (20.0) | 5.38 (2.50 to 11.55) | <0.001 | 4.02 (1.76 to 9.17) | 0.001 |
OA, osteoarthritis; ROA, radiographic osteoarthritis; OR, odds ratios; CI, confidence intervals.
Adjusted for age, sex, race, BMI, Charlson Comorbidity index (dichotomised) and depression.
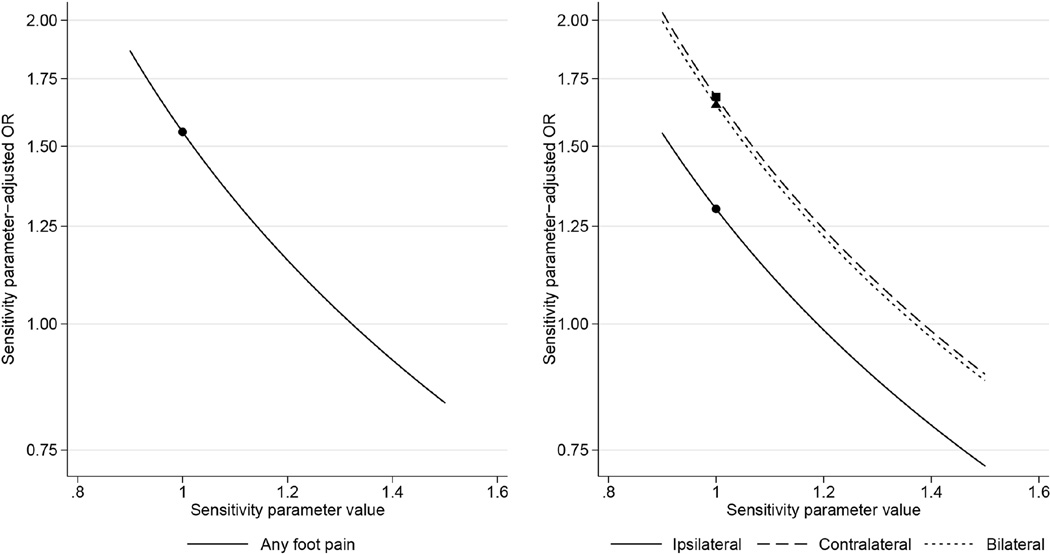
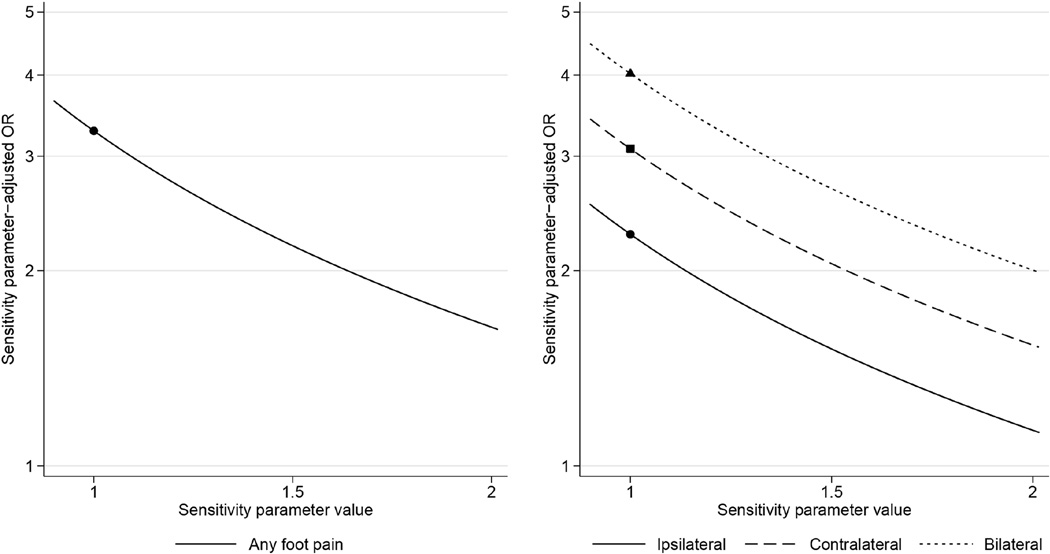
Sensitivity analyses
The results of our sensitivity analyses suggest that it is highly unlikely that any confounder not included in our analyses would have explained the observed association between foot/ankle symptoms and the development of knee symptoms and symptomatic radiographic knee OA. Specifically, the sensitivity analysis for developing knee symptoms (Figure 2) indicates that when the sensitivity parameter is about 1.3, the odds ratio reduces to 1. Hence, for the association to be entirely explained by unaccounted-for confounding, those with foot/ankle symptoms would need to be 30% more likely to develop the outcome than those without symptoms would be had they also had foot/ankle symptoms. The sensitivity parameter required to explain the association between foot/ankle symptoms and symptomatic radiographic knee OA is even greater (Figure 3): those with foot/ankle symptoms need to be more than twice as likely to develop the outcome than those without symptoms would be had they also had foot/ankle symptoms. Figures 2 and 3 indicate as the value of the sensitivity parameter gets greater (corresponding to the greater tendency to develop the outcome among those with foot/ankle symptoms), the sensitivity parameter-adjusted OR is further reduced.
Figure 2.
Results of the sensitivity analysis for developing knee symptoms.
Figure 3.
Results of the sensitivity analysis for developing symptomatic radiographic knee OA.
DISCUSSION
This is the first study to investigate whether foot/ankle symptoms are a risk factor for the development of knee symptoms and symptomatic radiographic knee OA in people at-risk of the disease. Foot/ankle symptoms in either or both sides were found to increase the risk of developing knee symptoms over the subsequent four years, with contralateral foot/ankle symptoms the only side to show an association with knee symptom development in the laterality analysis. Foot/ankle symptoms in either or both sides were also found to increase the risk of developing symptomatic radiographic knee OA, with bilateral and contralateral foot/ankle symptoms both associated, however there were few cases who developed this outcome and confidence intervals were wide. These findings add to previous cross-sectional studies demonstrating strong associations between symptoms at the foot/ankle and knee10, 11, and they provide the first longitudinal evidence that foot/ankle symptoms are a risk factor for the development of knee symptoms, and symptomatic radiographic knee OA.
Few studies have investigated risk factors for the onset of knee symptoms. A large prospective cohort study previously identified previous knee injury as the strongest predictor of onset of future knee pain with similar odds ratios to ours (1.59 compared t0 1.60)29. Furthermore, although a number of other risk factors for the development of symptomatic radiographic knee OA have been previously reported, such as age and ethnicity, few are modifiable. Currently, the strongest known modifiable risk factors for developing knee OA are obesity and previous knee injury30. Our odds of around 3.3 for developing symptomatic radiographic knee OA are also comparable to these other potentially modifiable factors (pooled OR 2.6 for BMI and 3.9 for knee injury)30. However, some caution should be used when interpreting the outcomes of our symptomatic radiographic model. Firstly, despite our large cohort with several years' follow-up and our use of knee-level data, few cases developed symptomatic radiographic knee OA. This reduces the precision of the odds ratio for this model, as seen by the wide confidence intervals. With so few cases, and adjustment for six covariates, there is also some risk of over-fitting our regression models. However, our number of events per variable in the model (including covariates) was within recommendations31. Finally, our four year follow up may be too short to appropriately evaluate symptomatic radiographic outcomes. However, the OAI only has biennial radiographic data available after four years, and we felt that it would overly complicate our outcome definition to have annual outcomes up to four years and biennial data thereafter. Notwithstanding these points, the results for all of our models were broadly consistent which suggests that it is likely that there is some association between foot/ankle symptoms and symptomatic radiographic knee OA. The findings are also reasonably robust given our sensitivity analyses showed that it is unlikely that our conclusions would be changed had we adjusted for other confounders not included in our analyses.
There are several plausible mechanisms by which foot pain could be linked to the subsequent onset of knee symptoms in people at-risk of knee OA. First, people with foot/ankle symptoms alter their walking pattern7 and these biomechanical changes may increase the risk of developing knee OA. To date, the effects of foot/ankle symptoms on biomechanics relevant to knee OA have not been explored, however our findings of an association between contralateral but not ipsilateral foot symptoms suggest people with foot/ankle symptoms may shift weight away from the painful foot and increase load on the contralateral knee. Second, it has been suggested that a more pronated or “flatter” foot, which is associated with many painful foot conditions32–34, may increase rotational stress on the tibiofemoral joint13, due in part to the tight coupling between movement at the rearfoot and tibia35. Over time, this abnormal stress may damage the load-bearing tissues in the knee joint leading to pain and structural damage13. However, whilst some cross-sectional studies show increased foot pronation in people with knee OA36, and that a more pronated foot is associated with an increased prevalence of knee pain and medial tibiofemoral cartilage damage13, other research suggests increased pronation may instead be a compensatory mechanism designed to reduce knee load and pain37. Third, footwear may be a shared risk factor for both foot/ankle symptoms and knee OA. For example, inappropriate footwear is a risk factor for foot/ankle symptoms, and some types of footwear such as high heels may also alter knee biomechanics in a detrimental manner14, 38. Other researchers have suggested that pain in multiple joints in people with knee OA may reflect a more generalized (e.g. oligo- or polyarticular) OA presentation39 or a widespread pain phenotype18, partly due to changes in central pain processing40, 41. These central changes may lead to a generalized hypersensitivity to pain and therefore a greater likelihood of developing pain at multiple sites such as the knee and foot. However this does not appear to be explanatory in our findings given our conclusions remained unchanged after we performed sensitivity analyses to account for unaccounted-for confounders.
There is evidence that foot foot/ankle symptoms may be modifiable given studies have shown simple and relatively inexpensive conservative interventions are effective at treating common causes of foot foot/ankle symptoms. For example, off-the-shelf footwear was reported to improve general foot pain in older people12 and foot pain due to gout42, whilst foot orthoses have been shown to improve pain and function in people with plantar fasciitis43, pes cavus44 and rheumatoid arthritis45, amongst others. If the mechanism underpinning the association between foot/ankle symptoms and the development of knee symptoms is due to shifting weight to the contralateral limb to unload the painful foot/ankle, then simple analgesic interventions may also be helpful in reducing the need for this avoidance strategy. Further studies are now required to determine whether treating foot foot/ankle symptoms using conservative interventions also helps to reduce the incidence of knee pain and symptomatic radiographic knee OA in people at risk of the disease.
There are some limitations to our study. Firstly, although we found a relationship between foot/ankle symptoms and the development of symptomatic and radiographic knee OA, it cannot be determined whether this is an independent relationship to structural or radiographic knee OA as these participants are a subset of those who developed knee symptoms. The relationship between foot/ankle symptoms and the development of radiographic knee OA alone was not explored given that radiographic OA without symptoms is not clinically relevant. Second, participants were required to have reported knee symptoms at only one of the follow up visits similar to previous research46, thus it is possible our analyses included people whose knee symptoms were not sustained over time. We feel that this was appropriate given OAI data have shown knee pain profiles are stable over 6 years47. However, future studies may wish to examine whether foot/ankle symptoms are associated with more sustained knee pain. Third, we dichotomised BMI and the Charlson comorbidity index which can leave residual confounding48. However, we found no strong evidence of this when we re-ran the analyses using fractional polynomials to model the continuous scores for these covariates (see Table 1 in the supplementary analyses). It is also possible that our results were biased due to the exclusion of participants because of missing x-rays. However when we compared demographic characteristics and covariates between those with missing and non-missing x-rays, our results showed those with missing x-rays were more similar to OAI participants with KL≥2 at baseline than to those with KL grade 0 and 1 (see Table 2 in the supplementary analyses). Since those with KL≥2 were excluded from the study, it is possible that the participants with missing data would have been excluded regardless. Thus the impact of missing data on our outcomes is likely to be minimal. Finally, we tested a cohort who was already at an increased risk of developing knee OA and thus our results should not be generalised to the wider population. Further research is needed to determine whether foot/ankle symptoms also increase the risk of developing knee symptoms in a population that does not possess other knee OA risk factors.
In conclusion, our study showed that people with foot/ankle symptoms were at an increased risk of developing knee OA symptoms and symptomatic radiographic knee OA compared to those without foot/ankle symptoms. These findings have important clinical and research implications. Although it is unclear whether foot/ankle symptoms directly causes knee symptoms and radiographic changes, or whether its presence is an indirect clinical marker for another variable, our results have identified a potentially modifiable risk factor for knee OA in people at-risk of the disease. Future studies should now determine whether addressing foot/ankle symptoms using conservative interventions reduces the incidence of knee pain and symptomatic radiographic knee OA.
Supplementary Material
Acknowledgments
The authors would like to express their thanks to all participants, staff and funders from the Osteoarthritis Initiative for making the data publically available.
Role of the Funding Source: The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partner. KB, DH, and HBM are partly funded by the National Health and Medical Research Council (NHMRC), and RH is supported by an Australian Research Council Future Fellowship. KP is supported by a NHMRC Program Grant. HBM is currently a National Health and Medical Research Council Senior Research Fellow.
RSH and KLB, and the University of Melbourne, received royalties from sales of Gel Melbourne OA shoes from 2012–2014. The manufacturer of the shoes played no role in the study design nor had any input into the analysis and interpretation of data from this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
AUTHOR CONTRIBUTIONS
All authors were involved in conception and design of the study, or in acquisition analysis and interpretation of data, and in revising it critically for important intellectual content. All authors approved the final version to be published. Dr. Paterson takes responsibility for the integrity of of the work as a whole, from inception to finished article.
Conception and design. Paterson, Kasza, Hinman, Hunter, Bennell.
Analysis and interpretation of data. Paterson, Kasza, Hunter, Hinman, Menz, Peat, Bennell.
Drafting of the article. Paterson, Bennell.
Critical revision of the article for important intellectual content. Paterson, Kasza, Hunter, Hinman, Menz, Peat, Bennell.
Final approval of the article. Paterson, Kasza, Hunter, Hinman, Menz, Peat, Bennell.
CONFLICT OF INTEREST
No authors report competing interests.
REFERENCES
- 1.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Annals of the Rheumatic Diseases. 2001;60:91–97. doi: 10.1136/ard.60.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. American Journal of Public Health. 1994;84:351–358. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Britt H, Miller GC, Henderson J, Bayram C, Valenti L, Harrison C, et al. A decade of Australian general practice activity 2004–05 to 2013–14. Sydney University Press; 2014. [Google Scholar]
- 4.Murphy LB, Moss S, Do BT, Helmick CG, Schwartz TA, Barbour KE, et al. Annual incidence of knee symptoms and four knee osteoarthritis outcomes in the Johnston County Osteoarthritis Project. Arthritis Care & Research. 2016;68:55–65. doi: 10.1002/acr.22641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas MJ, Roddy E, Zhang W, Menz HB, Hannan MT, Peat GM. The population prevalence of foot and ankle pain in middle and old age: A systematic review. Pain. 2011;152:2870–2880. doi: 10.1016/j.pain.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 6.Jordan K, Kadam U, Hayward R, Porcheret M, Young C, Croft P. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskeletal Disorders. 2010;11:144. doi: 10.1186/1471-2474-11-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mickle KJ, Munro BJ, Lord SR, Menz HB, Steele JR. Cross-sectional analysis of foot function, functional ability, and health-related quality of life in older people with disabling foot pain. Arthritis Care & Research. 2011;63:1592–1598. doi: 10.1002/acr.20578. [DOI] [PubMed] [Google Scholar]
- 8.Menz HB, Morris ME, Lord SR. Foot and ankle risk factors for falls in older people: A prospective study. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2006;61:866–870. doi: 10.1093/gerona/61.8.866. [DOI] [PubMed] [Google Scholar]
- 9.Ledingham J, Regan M, Jones A, Doherty M. Radiographic patterns and associations of osteoarthritis of the knee in patients referred to hospital. Annals of the Rheumatic Diseases. 1993;52:520–526. doi: 10.1136/ard.52.7.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keenan A-M, Tennant A, Fear J, Emery P, Conaghan PG. Impact of multiple joint problems on daily living tasks in people in the community over age fifty-five. Arthritis Care & Research. 2006;55:757–764. doi: 10.1002/art.22239. [DOI] [PubMed] [Google Scholar]
- 11.Paterson KL, Hinman RS, Hunter DJ, Wrigley TV, Bennell KL. Impact of concurrent foot pain on health and functional status in people with knee osteoarthritis: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2015;67:989–995. doi: 10.1002/acr.22537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Menz HB, Auhl M, Ristevski S, Frescos N, Munteanu SE. Effectiveness of off-the-shelf, extra-depth footwear in reducing foot pain in older people: a randomized controlled trial. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2015;70:511–517. doi: 10.1093/gerona/glu169. [DOI] [PubMed] [Google Scholar]
- 13.Gross KD, Felson DT, Niu J, Hunter DJ, Guermazi A, Roemer FW, et al. Association of flat feet with knee pain and cartilage damage in older adults. Arthritis Care & Research. 2011;63:937–944. doi: 10.1002/acr.20431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Titchenal MR, Asay JL, Favre J, Andriacchi TP, Chu CR. Effects of high heel wear and increased weight on the knee during walking. Journal of Orthopaedic Research. 2015;33:405–411. doi: 10.1002/jor.22775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levins AD, Skinner HB, Caiozzo VJ. Adaptive gait responses to plantar heel pain. Journal of rehabilitation research and development. 1998;35:289–293. [PubMed] [Google Scholar]
- 16.Sullivan J, Burns J, Adams R, Pappas E, Crosbie J. Plantar heel pain and foot loading during normal walking. Gait & Posture. 2015;41:688–693. doi: 10.1016/j.gaitpost.2015.01.025. [DOI] [PubMed] [Google Scholar]
- 17.Riskowski JL, Hagedorn TJ, Dufour AB, Hannan MT. Associations of region-specific foot pain and foot biomechanics: the Framingham Foot Study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2015 doi: 10.1093/gerona/glv067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suri P, Morgenroth DC, Kwoh CK, Bean JF, Kalichman L, Hunter DJ. Low back pain and other musculoskeletal pain comorbidities in individuals with symptomatic osteoarthritis of the knee: Data from the osteoarthritis initiative. Arthritis Care & Research. 2010;62:1715–1723. doi: 10.1002/acr.20324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Osteoarthritis Initiative. 2013 [Google Scholar]
- 20.Spector TD, Hart DJ, Doyle DV. Incidence and progression of osteoarthritis in women with unilateral knee disease in the general population: the effect of obesity. Annals of the Rheumatic Diseases. 1994;53:565–568. doi: 10.1136/ard.53.9.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Felson DT, Zhang Y, Hannan MT, Naimark A, Weissman BN, Aliabadi P, et al. The incidence and natural history of knee osteoarthritis in the elderly, the framingham osteoarthritis study. Arthritis & Rheumatism. 1995;38:1500–1505. doi: 10.1002/art.1780381017. [DOI] [PubMed] [Google Scholar]
- 22.Mont MA, Mitzner DL, Jones LC, Hungerford DS. History of the contralateral knee after primary knee arthroplasty for osteoarthritis. Clinical Orthopaedics and Related Research. 1995;321:145–150. [PubMed] [Google Scholar]
- 23.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Medical care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 25.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis: Classification of osteoarthritis of the knee. Arthritis & Rheumatism. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 26.Hill C, Gill T, Menz H, Taylor A. Prevalence and correlates of foot pain in a population-based study: the North West Adelaide health study. Journal of Foot and Ankle Research. 2008;1:2. doi: 10.1186/1757-1146-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bastick A, Runhaar J, Belo J, Bierma-Zeinstra S. Prognostic factors for progression of clinical osteoarthritis of the knee: a systematic review of observational studies. Arthritis Research & Therapy. 2015;17:152. doi: 10.1186/s13075-015-0670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kasza J, Polkinghorne KR, Marshall MR, McDonald SP, Wolfe R. Clustering and residual confounding in the application of marginal structural models: dialysis modality, vascular access, and mortality. American Journal of Epidemiology. 2015;182:535–543. doi: 10.1093/aje/kwv090. [DOI] [PubMed] [Google Scholar]
- 29.Jinks C, Jordan KP, Blagojevic M, Croft P. Predictors of onset and progression of knee pain in adults living in the community. A prospective study. Rheumatology. 2008;47:368–374. doi: 10.1093/rheumatology/kem374. [DOI] [PubMed] [Google Scholar]
- 30.Blagojevic M, Jinks C, Jeffery A, Jordan KP. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis and Cartilage. 2010;18:24–33. doi: 10.1016/j.joca.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 31.Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and cox regression. American Journal of Epidemiology. 2007;165:710–718. doi: 10.1093/aje/kwk052. [DOI] [PubMed] [Google Scholar]
- 32.Irving D, Cook J, Young M, Menz H. Obesity and pronated foot type may increase the risk of chronic plantar heel pain: a matched case-control study. BMC Musculoskeletal Disorders. 2007;8:41. doi: 10.1186/1471-2474-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Golightly YM, Hannan MT, Dufour AB, Hillstrom HJ, Jordan JM. Foot disorders associated with overpronated and oversupinated foot function: The Johnston County Osteoarthritis Project. Foot & ankle international. 2014;35:1159–1165. doi: 10.1177/1071100714543907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Menz HB, Dufour AB, Riskowski JL, Hillstrom HJ, Hannan MT. Association of planus foot posture and pronated foot function with foot pain: the Framingham Foot Study. Arthritis Care & Research. 2013;65:1991–1999. doi: 10.1002/acr.22079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Souza TR, Pinto RZ, Trede RG, Kirkwood RN, Fonseca ST. Temporal couplings between rearfoot–shank complex and hip joint during walking. Clinical Biomechanics. 2010;25:745–748. doi: 10.1016/j.clinbiomech.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 36.Levinger P, Menz HB, Morrow AD, Feller JA, Bartlett JR, Bergman NR. Foot kinematics in people with medial compartment knee osteoarthritis. Rheumatology. 2012;51:2191–2198. doi: 10.1093/rheumatology/kes222. [DOI] [PubMed] [Google Scholar]
- 37.Levinger P, Menz H, Morrow A, Bartlett J, Feller J, Bergman N. Relationship between foot function and medial knee joint loading in people with medial compartment knee osteoarthritis. Journal of Foot and Ankle Research. 2013;6:33. doi: 10.1186/1757-1146-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Radzimski AO, Mündermann A, Sole G. Effect of footwear on the external knee adduction moment — A systematic review. The Knee. 2012;19:163–175. doi: 10.1016/j.knee.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 39.Croft P, Jordan K, Jinks C. “Pain elsewhere” and the impact of knee pain in older people. Arthritis & Rheumatism. 2005;52:2350–2354. doi: 10.1002/art.21218. [DOI] [PubMed] [Google Scholar]
- 40.Kulkarni B, Bentley DE, Elliott R, Julyan PJ, Boger E, Watson A, et al. Arthritic pain is processed in brain areas concerned with emotions and fear. Arthritis & Rheumatism. 2007;56:1345–1354. doi: 10.1002/art.22460. [DOI] [PubMed] [Google Scholar]
- 41.Kosek E, Ordeberg G. Lack of pressure pain modulation by heterotopic noxious conditioning stimulation in patients with painful osteoarthritis before, but not following, surgical pain relief. Pain. 2000;88:69–78. doi: 10.1016/S0304-3959(00)00310-9. [DOI] [PubMed] [Google Scholar]
- 42.Rome K, Stewart S, Vandal A, Gow P, McNair P, Dalbeth N. The effects of commercially available footwear on foot pain and disability in people with gout: a pilot study. BMC Musculoskeletal Disorders. 2013;14:278. doi: 10.1186/1471-2474-14-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee SY, McKeon P, Hertel J. Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis. Physical Therapy in Sport. 2009;10:12–18. doi: 10.1016/j.ptsp.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 44.Burns J, Crosbie J, Ouvrier R, Hunt A. Effective orthotic therapy for the painful cavus foot: a randomized controlled trial. Journal of the American Podiatric Medical Association. 2006;96:205–211. doi: 10.7547/0960205. [DOI] [PubMed] [Google Scholar]
- 45.Woodburn J, Barker S, Helliwell PS. A randomized controlled trial of foot orthoses in rheumatoid arthritis. The Journal of Rheumatology. 2002;29:1377–1383. [PubMed] [Google Scholar]
- 46.Segal NA, Torner JC, Felson DT, Niu J, Sharma L, Lewis CE, et al. Knee extensor strength does not protect against incident knee symptoms at 30 months in the Multicenter Knee Osteoarthritis (MOST) cohort. PM&R. 2009;1:459–465. doi: 10.1016/j.pmrj.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Collins JE, Katz JN, Dervan EE, Losina E. Trajectories and risk profiles of pain in persons with radiographic, symptomatic knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis and Cartilage. 2014;22:622–630. doi: 10.1016/j.joca.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brenner H, Blettner M. Controlling for continuous confounders in epidemiologic research. Epidemiology. 1997;8:429–434. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.