Abstract
Objective:
To evaluate the feasibility of conducting a randomized controlled trial comparing group-based outpatient physiotherapy with usual care in patients following total knee replacement.
Design:
A feasibility study for a randomized controlled trial.
Setting:
One secondary-care hospital orthopaedic centre, Bristol, UK.
Participants:
A total of 46 participants undergoing primary total knee replacement.
Interventions:
The intervention group were offered six group-based exercise sessions after surgery. The usual care group received standard postoperative care. Participants were not blinded to group allocation.
Outcome measures:
Feasibility was assessed by recruitment, reasons for non-participation, attendance, and completion rates of study questionnaires that included the Lower Extremity Functional Scale and Knee Injury and Osteoarthritis Outcome Score.
Results:
Recruitment rate was 37%. Five patients withdrew or were no longer eligible to participate. Intervention attendance was high (73%) and 84% of group participants reported they were ‘very satisfied’ with the exercises. Return of study questionnaires at six months was lower in the usual care (75%) than in the intervention group (100%). Mean (standard deviation) Lower Extremity Functional Scale scores at six months were 45.0 (20.8) in the usual care and 57.8 (15.2) in the intervention groups.
Conclusion:
Recruitment and retention of participants in this feasibility study was good. Group-based physiotherapy was acceptable to participants. Questionnaire return rates were lower in the usual care group, but might be enhanced by telephone follow-up. The Lower Extremity Functional Scale had high responsiveness and completion rates. Using this outcome measure, 256 participants would be required in a full-scale randomized controlled trial.
Keywords: Group-based exercise, total knee replacement, feasibility, randomized controlled trial
Introduction
Total knee replacement is a common surgical procedure for the management of knee osteoarthritis and between 2003 and 2014, 772,818 primary total knee replacements were performed in England and Wales.1 In 2012 it was reported that the average cost of a knee replacement and five year subsequent healthcare can exceed £7000 per patient.2 The provision of physiotherapy services available to patients after knee replacement varies across the United Kingdom,3 with little guidance on best practice. Studies indicate that functional exercises are widely used by physiotherapists for treating patients following knee replacement.3,4 However, function-based exercises may only provide short-term benefit to patients5 with limited evidence supporting long-term gains from physiotherapy interventions.6
Current trends in physiotherapy practice aim to address patients’ concerns and are orientated towards specific patient goals.7–11 This tailored approach is designed to enable patients to perform activities that they value and such interventions have been successfully delivered in group settings,11,12 The use of group-based interventions in research to investigate the most effective modality of delivering rehabilitation after knee replacement is of growing interest.13–16 Group-based physiotherapy may provide a cost-effective way of delivering treatment to a larger number of patients without compromising clinical effectiveness17,18 compared with one-to-one physiotherapy, and offers patients the opportunity to interact with other patients. The short-term benefits of group-based rehabilitation have been observed in patients with knee osteoarthritis19 and following total knee replacement.13 A combination of tailored and functional exercises for patients within a group setting integrates both individual and group benefits of rehabilitation, enhancing patients’ self-efficacy, empowerment,20 and outcome.21 In the context of joint replacement, higher levels of postoperative self-efficacy have been associated with better longer-term functional outcome22 and may enhance adherence with home exercises. In line with the Medical Research Council guidance on developing complex interventions,23 and similar feasibility studies in orthopaedics,24,25 the aims of this study were to evaluate the feasibility of conducting a definitive randomized controlled trial (RCT) comparing a novel group-based outpatient physiotherapy class, comprising functional and tailored exercises with that of usual care after total knee replacement and to determine the sample size required to conduct a definitive trial.
Methodology
This feasibility study for a RCT took place at a secondary care hospital in England in which over 500 primary total knee replacements are performed annually. Ethical approval for this study was provided by the South West-Cornwall and Plymouth Research Ethical Committee (reference 11/SW/0341), with sponsorship provided from North Bristol NHS Trust (reference 2713). The study was registered on the UK Clinical Research Network Portfolio Database (reference 12100) and the International Standard Randomized Controlled Trials Number (ISRCTN13579789).
Between July 2012 and February 2013, patients listed for total knee replacement surgery were posted a study information pack by a member of the clinical team. The study pack contained a letter of invitation detailing the recruitment process and a patient information booklet. These patients were then approached by a member of the research team during their preoperative assessment clinic to discuss the study in detail and assess eligibility. Patients undergoing a primary total knee replacement for osteoarthritis were eligible for participation in the study. Exclusion criteria included: knee replacement for conditions other than osteoarthritis, revision knee surgery, inability to participate in exercise for any medical reason such as unstable cardiovascular or cardio-respiratory disease, diagnosis of severe neurological disorders, inability to provide informed consent, and inability to complete study questionnaires in English as the study was using measures that had not all been validated in other languages. Patients not wishing to participate were asked for consent to ascertain their reason for not participating. A research nurse documented these reasons documented on a proforma at the preoperative assessment clinic.
After recruitment, a research nurse registered patients in the trial with a unique study identification number and recorded their details on the study database. Each participant was then randomized to receive either usual care or the physiotherapy intervention. Information including age and gender were inputted into a computer-generated randomization system (Minim)26 by the study administrator and participants were then randomized to receive either usual care or the physiotherapy intervention. Group allocation was minimised by gender and age to ensure equal distribution between groups. Participants were not blind to the group allocation and were informed of their allocation by telephone two weeks after their knee replacement surgery by a research physiotherapist (NA/SD). Participants randomized into the intervention arm were invited to attend an exercise group starting at the sixth week after surgery and running for a period of six weeks. Information about the date and location of the first class were then posted to the participant, along with an ‘activity goal form’ on which participants were asked to identify two activities to which they would like to return to after their knee replacement. Participants were instructed to bring the form with them to the first class with them. The weekly one-hour exercise classes were run by two experienced research physiotherapists (NA/SD) starting at six weeks after surgery and lasting a total of six weeks. The exercise class took place weekly in a physiotherapy gym at our centre and consisted of 12 separate stations with exercises designed to increase general fitness, lower-limb strength and function, balance, gait, and confidence. Two of these exercise stations included exercises to address two key functional goals identified by each participant on the ‘activity goal form’ as activities to which they would like to return to following their knee replacement. Participants spent four minutes at each station allowing sufficient time to carry out the exercises at their own pace with a focus on quality of movement rather than quantity. On completion of the exercise class, participants were provided with a list of exercises, including their individual exercises, to continue with at home on a regular basis. Travel and parking costs incurred by participants were refunded to a maximum of £20 per participant per session. Taxis were provided for participants unable to get to and from the class with public or personal transport.
Participants in the usual care arm of the study were instructed to continue with the routine care provided by the health service. All patients received standard inpatient care provided by our centre and upon discharge from hospital were provided with a knee replacement booklet. The booklet contained information about early and late stage postoperative exercises, functional activities, return to work and hobbies, precautions, expectations, and potential problems.27.In addition to this booklet, some patients were referred to physiotherapy services on an individual basis at the discretion of the hospital’s physiotherapy or orthopaedic team or by their GP. Services included referral to local outpatient physiotherapy or community physiotherapy at home. In such cases, patients may have received a variety of physiotherapy interventions, including specific knee strengthening and stretching exercises, functional exercise, manual therapy, or hydrotherapy.3
All participants were asked to complete study questionnaires before surgery and at two weeks, three months, and six months after surgery. The study questionnaires consisted of a series of patient-reported outcome measures to assess knee pain and function, recreational activity, balance, self-efficacy, participation, general health, and satisfaction with surgery and rehabilitation. We used two measures, the Knee Injury and Osteoarthritis Outcome Score28 and Lower Extremity Functional Scale,29 to assess outcomes. The Knee Injury and Osteoarthritis Outcome Score consists of five subscales that assess pain, symptoms, function in daily living, function in sport and recreation, and knee-related quality of life. The Lower Extremity Functional Scale is a 20-item questionnaire that assesses lower limb function and difficulty in performing everyday tasks. Questionnaires were posted to participants and reminders sent if no response was received two weeks after postage. If questionnaires were not received after reminders had been sent, then participants were contacted and asked to complete the Knee Injury and Osteoarthritis Outcome Score over the telephone by the research physiotherapist (NA/SD). The research physiotherapists were not blinded to participant group allocation and inputted all outcome measures into the study database.
Responsiveness of the Knee Injury and Osteoarthritis Outcome Score and Lower Extremity Functional Scale was also investigated to inform a decision on the most appropriate tool to power a future definitive trial.
Additional outcome measures included the University of California Los Angeles activity score,30 Aberdeen Impairment, Activity Limitation and Participation Restriction measure,31 Activities-specific Balance Confidence scale,32 and the Self-Efficacy for Rehabilitation questionnaire.33 A visual analogue scale for pain and questions regarding satisfaction with surgery and rehabilitation were also included. The Measure Yourself Medical Outcome Profile34 was recorded at six weeks, three months, and six months postoperatively by a research physiotherapist (NA/SD). Participants were asked to self-identify and score on initial symptom severity, wellbeing, and ability to undertake an activity, and then score this at each follow-up. Data on demographics, socioeconomic status, and comorbidities were collected in the preoperative questionnaire.
All participants were contacted by telephone at three months after surgery by a research physiotherapist (NA/SD) to complete a study evaluation survey. Participants were asked to answer yes/no to questions about the appropriateness of study information, understanding of the study processes and group allocation, and the suitability and timing of questionnaires. Participants randomized to the intervention group also completed an evaluation of the exercise class collected by the physiotherapists (NA/SD) after the final exercise class. Participants were asked to answer yes/no to questions about the information provided to prepare them for the exercise classes, such as location, duration, and content of the class with additional information recorded in free text. Participant satisfaction with the equipment, location, and range of exercises was recorded using a 4-point Likert-type scale ranging from ‘very dissatisfied’ to ‘very satisfied’. Usefulness of the exercises was scored on an 11-point numerical rating scale from 0 (not useful at all) to 10 (extremely useful). Adherence and barriers to attending the physiotherapy intervention, and reasons for non-attendance were also recorded.
Analysis of outcome data was descriptive with no comparison of outcome between the two groups as recommended for feasibility studies.35 Descriptive statistics about participant characteristics are presented as frequencies, percentages, and means. Patient-reported outcomes are reported as mean and standard deviation. Within-groups changes are reported as mean and 95% confidence intervals (95% CI).
Recruitment rates, questionnaire return and completion rates, and evaluation questionnaire results are reported as percentages. Reasons for non-participation were grouped into themes by one researcher (NA) and agreed by a second researcher (SD).
We assessed the responsiveness of the Lower Extremity Functional Scale and Knee Injury and Osteoarthritis Outcome Score questionnaires using the minimum important difference, the smallest change in a patient-reported outcome measure likely to be important from the patient’s or the clinician’s perspective. The minimum important difference is usually approximate by 0.5 standard deviation of the mean change between two measures of the studied outcome. Participants with a change larger than 0.5 standard deviation of the mean change of the studied score are deemed responders. We first derived the change between the preoperative assessment and the different postoperative assessments (at two weeks, three months, and six months after surgery) for each subscale of the Knee Injury and Osteoarthritis Outcome Score. Changes were then derived between the first postoperative assessment (two-weeks postsurgery) and the following ones for each of the Knee Injury and Osteoarthritis Outcome Score subscales and the Lower Extremity Functional Scale score.
Results
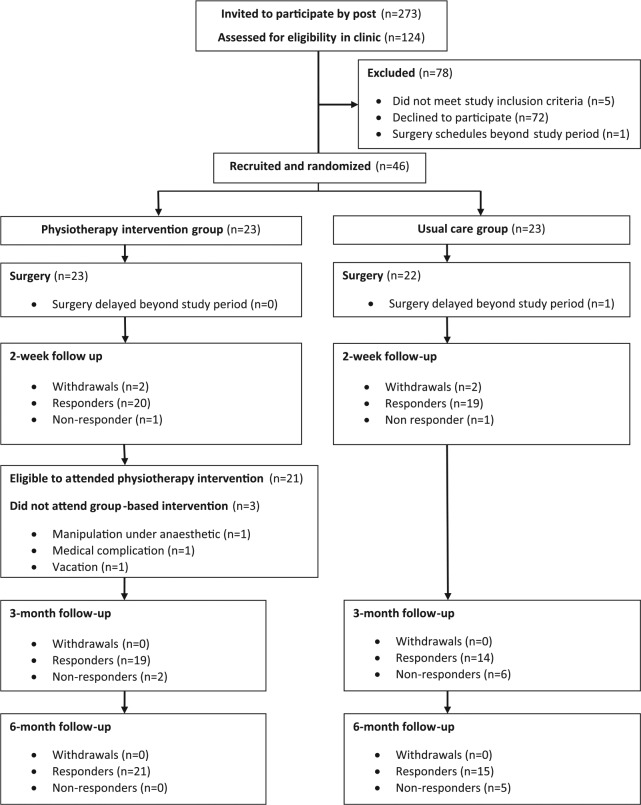
Figure 1 shows a CONSORT flow diagram for participants in this study. Study packs were posted to 238 potentially eligible patients, with 124 patients approached in the preassessment clinic during the study period. Of the 124 patients approached, 72 patients declined to participate, five patients were ineligible, and one patient had surgery arranged outside the study period. A total of 46 patients consented to participate, giving a recruitment rate of 37%. Of these patients, 23 were randomized to the intervention group and 23 to the usual care group. Baseline characteristics of participants are shown in Table 1. All patients who declined participation agreed to disclose their reasons for non-participation in the study.
Figure 1.
Study CONSORT flow diagram.
Table 1.
Baseline characteristics of participants recruited into the study.
| All | Intervention group | Usual care group | |
|---|---|---|---|
| Mean age (min-max) | 68.6 (51–82) | 70.0 (57–81) | 67.2 (51–82) |
| Gender (male/female) | 22/24 | 11/12 | 11/12 |
| Laterality of implant (left/right) | 19/27 | 9/14 | 10/13 |
| Mean distance (miles) residing from hospital (min–max) | 8.1 (1.3–18.6) | 9.2 (1.7–17.7) | 7.1 (1.3–18.6) |
| Living alone (n) | 12 | 4 | 8 |
| Retired (n) | 31 | 19 | 12 |
| Additional joint pains (n) | 38 | 23 | 15 |
| Back pain (n) | 15 | 8 | 7 |
| Diabetes (n) | 6 | 5 | 1 |
| Angina (n) | 3 | 3 | 0 |
| Mean (SD) KOOS pain | 42.4 (16.4) | 40.5 (16.5) | 44.5 (17.0) |
| Mean (SD) KOOS symptoms | 42.2 (16.7) | 40.7 (17.0) | 43.9 (16.3) |
| Mean (SD) KOOS activities of daily living | 46.3 (18.3) | 41.8 (15.7) | 51.2 (20.4) |
| Mean (SD) KOOS sport/recreation | 14.9 (20.9) | 12.2 (24.4) | 18.1 (15.8) |
| Mean (SD) KOOS quality of life | 15.6 (11.3) | 12.5 (12.6) | 18.4 (8.5) |
KOOS: Knee Injury and Osteoarthritis Outcome Score; SD: standard deviation; n: number of participants.
Reasons for non-participation were recorded for 72 patients. The most frequent reasons (54% of reported reasons) were related to travelling distance, transportation, and commitment to attend the exercise class if randomized to the intervention group. Other reasons included: Concerns around existing co-morbidities, caring responsibilities, dislike of completing questionnaires, planned vacations after surgery, unwillingness to exercise in a group, and anxiety about the forthcoming surgery at the time of approach about the study.
Four participants (9%) withdrew from the study: Two from the intervention group and three from the usual care group (Figure 1). In the usual care group, two patients self-withdrew and one patient did not undergo surgery during the study period. In the intervention group, one participant self-withdrew and one participant had postoperative complications that excluded them from continuing in the study. Three participants did not attend any of the classes, and one participant attended a single class before admission for a manipulation under anaesthetic for knee pain and stiffness, after which it was no longer clinically appropriate for them to continue class attendance. Of the three participants who did not attend any of the sessions, the reasons for non-attendance were a complication owing to a pre-existing medical condition, admission for manipulation under anaesthetic before the class start date, and an extended vacation. Overall, attendance-at-the-class rate was 73%, with 13 participants attending all six exercise classes and four participants attending five classes. Non-medical reasons for non-attendance were owing to participants’ social commitments on the day of the class. A total of 17 participants provided feedback about the exercise class. All participants felt that the one-hour duration of the session was the right amount of time to exercise, but three (18%) participants would have liked to receive more than six sessions. Overall, participants were satisfied with the range of exercises offered, with 15 (84%) participants reporting that they were ‘very satisfied’. All patients felt that the exercise class met their individual functional needs and many provided positive feedback about the exercise class.
Return rates of study questionnaires at two weeks after surgery were 19/20 (95%) in the usual care group and 20/21 (95%) in the intervention group. At three months after surgery, the rate of questionnaire return was lower with 14/20 (70%) in the usual care group compared with 19/21 (91%) in the intervention group. At six months after surgery, the questionnaire return rate improved to 15/20 (75%) in the usual care group and 21/21 (100%) and intervention group.
Completion rates of the Knee Injury and Osteoarthritis Outcome Score and Lower Extremity Functional Scale are shown in Table 2. In both the usual care and intervention groups, completion rates of the Knee Injury and Osteoarthritis Outcome Score and Lower Extremity Functional Scale was high at each follow-up time point. Completion rates of all additional outcome measures are shown in Table 3. Results of all outcome measures scored at two weeks (six weeks for the Measure Yourself Medical Outcome Profile), three months, and six months are provided in Table 4. The three to six month within-groups changes for the Knee Injury and Osteoarthritis Outcome pain and activities of daily living scores were 8.3 (95% CI 0.7, 15.8) and 5.0 (95% CI −1.1, 11.1) in the usual care group and 8.8 (95% CI 1.1, 6.4) and 2.5 (95% CI −3.3, 8.4) in the physiotherapy intervention groups, respectively. The three- to six-month within-group changes for the Lower Extremity Functional Scale were 1.9 (95% CI −3.4, 7.3) and 6.2 (95% CI −2.0, 14.4) in the usual care and physiotherapy intervention groups, respectively.
Table 2.
Completion rate of the Lower Extremity Functional Scale and Knee Injury and Osteoarthritis Outcome Score subsections at two weeks, three months, and six months after surgery in both the usual care and physiotherapy intervention groups.
| Completion rates (x/n) (%) of (N) returned questionnairesx = number completedn = number of outcome returnedN = total number of potential returnable outcomes | 2-weeks after surgery |
3-months after surgery |
6-months after surgery |
||||
|---|---|---|---|---|---|---|---|
| Return rate n/N (%) | Completion rate x/n (%) | Return rate n/N (%) | Completion rate x/n (%) | Return rate n/N (%) | Completion rate x/n (%) | ||
| KOOS pain | Usual care | 19/20 (95) | 19/19 (100) | 14/20 (70) | 14/14 (100) | 15/20 (75) | 14/15 (93) |
| Physiotherapy intervention | 20/21 (95) | 20/20 (100) | 19/21 (90) | 19/19 (100) | 21/21 (100) | 21/21 (100) | |
| KOOS symptoms | Usual care | 19/20 (95) | 19/19 (100) | 14/20 (70) | 14/14 (100) | 15/20 (75) | 14/15 (93) |
| Physiotherapy intervention | 20/21 (95) | 20/20 (100) | 19/21 (90) | 19/19 (100) | 21/21 (100) | 21/21 (100) | |
| KOOS activities of daily living | Usual care | 19/20 (95) | 19/19 (100) | 14/20 (70) | 14/14 (100) | 15/20 (75) | 15/15 (100) |
| Physiotherapy intervention | 20/21 (95) | 20/20 (100) | 19/21 (90) | 19/19 (100) | 21/21 (100) | 21/21 (100) | |
| KOOS sport recreation | Usual care | 19/20 (95) | 18/19 (95) | 14/20 (70) | 13/14 (93) | 15/20 (75) | 15/15 (100) |
| Physiotherapy intervention | 20/21 (95) | 17/20 (85) | 19/21 (90) | 19/19 (100) | 21/21 (100) | 18/21 (86) | |
| KOOS quality of life | Usual care | 19/20 (95) | 19/19 (100) | 14/20 (70) | 13/14 (93) | 15/20 (75) | 14/15 (93) |
| Physiotherapy intervention | 20/21 (95) | 20/20 (100) | 19/21 (90) | 19/19 (100) | 21/21 (100) | 21/21 (100) | |
| LEFS | Usual care | 18/20 (90) | 17/18 (94) | 12/20 (60) | 11/12 (92) | 15/20 (75) | 14/15 (93) |
| Physiotherapy intervention | 20/21 (95) | 19/20 (95) | 19/21 (91) | 19/19 (100) | 21/21 (100) | 19/21 (91) | |
KOOS: Knee Injury and Osteoarthritis Outcome Score; LEFS: Lower Extremity Functional Scale.
Table 3.
Completion rate (%) of additional outcome measures at two-weeks (Measure Yourself Medical Outcome Profile six weeks), three months, and six months after surgery in both the usual care and physiotherapy intervention group.
| Completion rates (%) of additional outcome measures | 2-weeks after surgery | 3-months after surgery | 6-months after surgery | |
|---|---|---|---|---|
| ABC scale | Usual care | 17/20 (85) | 12/20 (60) | 15/20 (75) |
| Physiotherapy intervention | 20/21 (95) | 19/21 (91) | 21/21 (100) | |
| Pain (VAS) | Usual care | 17/20 (85) | 11/20 (55) | 10/20 (50) |
| Physiotherapy intervention | 20/21 (95) | 17/21 (76) | 18/21 (86) | |
| UCLA | Usual care | 18/20 (90) | 12/20 (60) | 15/20 (75) |
| Physiotherapy intervention | 20/21 (95) | 19/21 (91) | 20/21 (95) | |
| SER | Usual care | 18/20 (90) | 12/20 (60) | 14/20 (70) |
| Physiotherapy intervention | 20/21 (95) | 19/21 (91) | 20/21 (95) | |
| Ab-IAP | Usual care | 17/20 (85) | 12/20 (60) | 15/20 (75) |
| Physiotherapy intervention | 20/21 (95) | 19/21 (91) | 21/21 (100) | |
| MYMOP | Initial (6 weeks after surgery) | |||
| 20/20 (100) | 19/20 (95) | 17/20 (85) | ||
| Usual care Physiotherapy intervention | 21/21 (100) | 21/21 (100) | 19/20 (95) | |
ABC scale: activities-specific balance confidence scale; pain VAS: pain visual analogue scale; UCLA: UCLA activity score; SER: self-efficacy for rehabilitation; Ab-IAP: Aberdeen Measures of Impairment, Activities Limitation and Participation Restriction; MYMOP: Measure Yourself Medical Outcome Profile.
Table 4.
Outcome measures at two weeks (six weeks for initial Measure Yourself Medical Outcome Profile), three months, and six months after surgery in both the physiotherapy intervention and usual care groups.
| 2-weeks after surgery | 3-months after surgery | 6-months after surgery | ||
|---|---|---|---|---|
| KOOS pain | Usual care | 52.9 (18.1) | 69.1 (19.5) | 70.9 (27.1) |
| Physiotherapy intervention | 46.7 (13.5) | 74.1 (19.9) | 78.6 (25.9) | |
| KOOS symptoms | Usual care | 42.9 (10.6) | 54.8 (16.9) | 56.7 (14.3) |
| Physiotherapy intervention | 52.2 (13.9) | 59.6 (16.4) | 58.4 (18.9) | |
| KOOS activities of daily living | Usual care | 60.8 (19.8) | 76.1 (18.5) | 73.5 (26.4) |
| Physiotherapy intervention | 54.4 (17.6) | 81.2 (15.9) | 79.6 (23.4) | |
| KOOS sport recreation | Usual care | 12.9 (11.9) | 27.9 (20.2) | 37.1 (25.7) |
| Physiotherapy intervention | 16.2 (25.9) | 39.2 (29.4) | 46.3 (35.4) | |
| KOOS quality of life | Usual care | 16.7 (7.5) | 36.1 (17.3) | 45.1 (29.2) |
| Physiotherapy intervention | 23.8 (17.6) | 52.4 (27.1) | 61.5 (32.3) | |
| LEFS | Usual care | 30.1 (13.4) | 48.8 (17.4) | 45.0 (20.8) |
| Physiotherapy intervention | 26.1 (11.5) | 55.8 (15.6) | 57.8 (15.2) | |
| ABC scale | Usual care | 58.4 (21.1) | 79.0 (19.4) | 80.7 (19.8) |
| Physiotherapy intervention | 43.7 (23.3) | 84.3 (15.2) | 84.1 (17.3) | |
| Pain (VAS) | Usual care | 5.7 (2.2) | 3.6 (2.2) | 3.9 (3.6) |
| Physiotherapy intervention | 5.3 (2.5) | 3.5 (3.1) | 2.9 (3.4) | |
| UCLA | Usual care | 2.5 (0.8) | 4.3 (1.1) | 4.5 (1.9) |
| Physiotherapy intervention | 2.8 (0.8) | 4.9 (1.7) | 5.2 (1.5) | |
| SER | Usual care | 91.2 (16.9) | 99.9 (23.5) | 103.8 (18.3) |
| Physiotherapy intervention | 90.2 (20.1) | 108.7 (13.0) | 110.7 (10.7) | |
| Ab-IAP | Usual care | 20.0 (4.4) | 13.9 (6.1) | 15.4 (9.8) |
| Physiotherapy intervention | 18.3 (5.1) | 11.5 (4.2) | 10.9 (3.1) | |
| MYMOP | Initial (6 weeks after surgery) | |||
| Usual care | 3.7 (0.7) | 2.8 (0.9) | 2.4 (1.3) | |
| Physiotherapy intervention | 3.2 (0.8) | 1.9 (1.3) | 1.9 (1.4) |
KOOS: Knee Injury and Osteoarthritis Outcome Score; LEFS: Lower Extremity Functional Scale; ABC scale: activities-specific balance confidence scale; Pain VAS: pain visual analogue scale; UCLA: UCLA activity score; SER: self-efficacy for rehabilitation; Ab-IAP: Aberdeen Measures of Impairment, Activity Limitation and Participation Restriction; MYMOP: Measure Yourself Medical Outcome Profile.
Responsiveness between the preoperative period and the successive postoperative periods improved over time (Table 5). For each of the Knee Injury and Osteoarthritis Outcome Score subscales, nearly all patients were responsive at six months postsurgery. Postoperative responsiveness as measured by the change in Knee Injury and Osteoarthritis Outcome Score subscales between the two weeks postoperative period and the longer postoperative assessments, also improved over time. At six month postoperative, all patients were perceiving change in the pain, symptoms, and quality of life subscales of the Knee Injury and Osteoarthritis Outcome Score. Most patients also had experienced perceptible change in their functional ability, and sport and recreation activities. For the Lower Extremity Functional Scale, an activity-based score, the proportion of responders was higher at three months than six months postoperative, although the number of responders on the Lower Extremity Functional Scale was consistently higher than on the Knee Injury and Osteoarthritis Outcome Score function in the daily living subscale.
Table 5.
Responsiveness of the Knee Injury and Osteoarthritis Outcome Score and Lower Extremity Functional Scale. Minimum important difference: Respondent (patients with a pre–postsurgery change score greater than 0.5 standard deviation of the change score).
| Respondents n/N (%) |
|||
|---|---|---|---|
| 2 weeks | 3 months | 6 months | |
| Change from preoperative assessmenta | |||
| KOOS pain | 39 (15/39) | 27/33 (82) | 35/35 (100) |
| KOOS symptoms | 44 (17/39) | 19/33 (58) | 35/35 (100) |
| KOOS activities of daily living | 51 (20/39) | 25/33 (76) | 34/36 (94) |
| KOOS sport/recreation | 15 (5/39) | 15/23 (48) | 31/32 (97) |
| KOOS quality of life | 33 (13/39) | 25/32 (78) | 35/35 (100) |
| Change from 2-weeks postoperative assessmentb | |||
| KOOS pain | – | 24/33 (73) | 34/34 (100) |
| KOOS symptoms | – | 19/33 (58) | 34/34 (100) |
| KOOS activities of daily living | – | 23/33 (70) | 27/35 (77) |
| KOOS sport/recreation | – | 14/28 (50) | 27/28 (96) |
| KOOS quality of life | – | 22/32 (69) | 34/34 (100) |
| LEFS | – | 27/28 (96) | 25/30 (83) |
Change between the preoperative assessment and the specific postoperative assessment.
Change between the two-weeks postoperative assessment and the specific postoperative assessment.
KOOS: Knee Injury and Osteoarthritis Outcome Score; LEFS: Lower Extremity Functional Scale.
Discussion
This study was designed to evaluate the feasibility of conducting a RCT and to inform the design of a future fully powered trial. Our findings indicate that a future trial would be feasible to implement at our centre with acceptable recruitment and retention rates, high rates of study questionnaire return and completion, and high levels of attendance and satisfaction with the group-based physiotherapy intervention.
The recruitment rate of this study was 37%. This is similar to a feasibility trial by Minns Lowe and colleagues36 where recruitment was 34%, but lower than other physiotherapy trials where recruitment rates range from 47%–63%.18,37,38 The main reasons reported by patients for not participating in the study were travel-related issues, which have been highlighted in previous studies,36,39 and the inability to commit to the intervention if allocated into this group. The offer to reimburse travel cost, particularly for patients after orthopaedic surgery, may help to maximise participation in future studies in which participants are invited to attend additional appointments or exercise sessions. However, it is evident that despite the offer of travel assistance, such as taxis or reimbursement of expenses, a large proportion of participants still declined to participate in this study. This indicates that a combination of factors may influence the decision to take part. For example, patients were approached at the preassessment clinic in which they underwent a number of clinical processes prior to confirmation of surgery. This is a busy clinic and potentially stressful time for the patient and therefore may not be the most appropriate time for recruitment. Nevertheless, retention was good in our study, suggesting that participants in both the intervention and usual care group found the trial processes acceptable. However, it is important to note that reimbursement of travel costs is not standard practice in healthcare provision in the United Kingdom, and therefore the recruitment and retention of participants into the exercise group may not reflect that of clinical practice.
The group-based physiotherapy exercise class was generally well received, with a high attendance rate for the six group sessions (73%). This finding is similar to a previous study that involved repeated appointments for a physiotherapy intervention38 and reported that 81% of participants attended eight out of a possible 12 treatment sessions. Although satisfaction after knee replacement is high,21 patients often report lower levels of physical function40 and greater need for physiotherapy input than patients after other types of joint replacement.41 Some participants reported that attendance at classes increased their confidence. Health professional support42 and engagement with peers is important20 and can have a positive impact on functional attainment and quality of life after joint replacement.43 Group-based physiotherapy can be enjoyable and allows patients to compare their progress with that of their peers, and offers interaction between patients who have experienced knee replacement.21
Offering a one-to-one component and devising strategies to involve patients in their own rehabilitation may be important to assist in adherence, empowerment, and self-efficacy.20,44 Incorporating one-to-one physiotherapy within the group setting has been highlighted by Naylor and colleagues21 as potentially beneficial to allow identification of persistent postoperative problems and influence adherence. Futures studies should aim to include an element of individualised treatment to enhance patient care within group-based exercise.
Our study design was feasible, and lessons were learnt for a future trial. Return rates were higher in the intervention group than the usual care group, suggesting that more contact with the research team may have influenced adherence. The higher return rates in the intervention group are not unexpected and may reflect closer relationships developed between participants attending the group and the research physiotherapists, compared with those not invited to attend the class. This highlights a major limitation of the study and using postal questionnaires in a future trial may benefit from additional follow-up telephone contact to improve rates of data collection. One participant in the usual care group noted in the study evaluation document that ‘if I was in the group (referring to the exercise class) I would have probably filled out the forms’ (P09) suggesting that receipt of the intervention may influence response rates. In this study, participants could not be blinded to the group allocation and steps to reduce the influence of group allocation on return rates should be evaluated in future trials.
In this study, both the Knee Injury and Osteoarthritis Outcome Score and Lower Extremity Functional Scale had acceptable completion rates and good rates of responsiveness. The Knee Injury and Osteoarthritis Outcome Score is a 42-item questionnaire with five-subsections, with acceptable psychometric properties.45 However, the sport and recreational, and other symptoms subscales, demonstrate low reliability in total knee replacement45 and the applicability of the sport and recreation subscale in patients that are less physically active, has been questioned.46 The Lower Extremity Functional Scale is a shorter, 20-item validated questionnaire that reliably assesses lower limb functional impairment and difficulty in performing everyday tasks.47 In terms of measuring changes in physical functioning and activities of daily living, the Lower Extremity Functional Scale demonstrating greater response than the Knee Injury and Osteoarthritis Outcome Score activities of daily living subscale at six months after surgery in our study. This suggests that the Lower Extremity Functional Scale may be more applicable in this context for measuring physical functioning in future trials. The Lower Extremity Functional Scale has a minimal clinically important difference of nine scale points,29 and using data obtained from this study, a sample size of 256 would be required to detect a minimal clinically important difference in the Lower Extremity Functional Scale between the usual care and intervention group. This calculation is based on a total group standard deviation of 18.4 at six months with the assumption of 80% power, a two-sided 5% significance level, up to 35% missing data (in usual care group), and an inflation factor of 1.122 derived from the 80% upper confidence limit of the standard deviation estimate.48
Owing to the nature of the trial, it was not possible to blind participants to their allocation and further work would need to consider how to minimise the impact of this on data collection. For instance, allocation to the usual care group appeared to impact on willingness to complete questionnaires and there is a need to consider how best to maximise questionnaire completion in future studies. Another limitation was that the physiotherapists delivering the intervention were also responsible for data collection. Familiarity of the participants with the research physiotherapist in the group may have influenced their participation and how they reported their views about the acceptability of the exercise group and exercises provided. Any future full-scale study should have assessors that are not involved in delivering the intervention.
Our results indicate that a full-scale RCT to determine the effectiveness of a group-based physiotherapy class six weeks after total knee replacement is feasible. A group-based physiotherapy intervention that focuses on function and individual needs was found to be acceptable to patients and a feasible method of delivering a physiotherapy intervention after total knee replacement. Postal questionnaire return rates were lower in the usual care group than the intervention group, although they may be improved with additional telephone follow-up. Both the Knee Injury and Osteoarthritis Outcome Score and Lower Extremity Functional Scale had acceptable completion rates, with the Lower Extremity Functional Scale demonstrating higher responsiveness than the Knee Injury and Osteoarthritis Outcome Score function in daily living scale.
Clinical message.
Group-based physiotherapy is acceptable to patients as a method of delivering outpatient rehabilitation after total knee replacement.
This feasibly study highlighted that questionnaire return rates were lower in the usual care group than the intervention group. This indicates a need to improve methods of data collection.
A total of 256 patients would be required to perform a full scale RCT comparing group-based exercise.
Acknowledgments
The views expressed in this article are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. The research team acknowledge the support of the NIHR, through the Comprehensive Clinical Research Network.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This article presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research programme [RP-PG-0407-10070].
References
- 1. National Joint Registry, 12th Annual Report 2014. Hemel Hempstead: NJR Centre. [Google Scholar]
- 2. Dakin H, Gray A, Fitzpatrick R, Maclennan G, Murray D; KAT Trial Group. Rationing of total knee replacement: A cost-effectiveness analysis on a large trial data set. BMJ Open. 2012; 2(1): e000332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Artz N, Dixon S, Wylde V, Beswick A, Blom A, Gooberman-Hill R. Physiotherapy provision following discharge after total hip and total knee replacement: A survey of current practice at high-volume NHS hospitals in England and Wales. Musculoskel Care 2013; 11: 31–38. [DOI] [PubMed] [Google Scholar]
- 4. Peter WF, Nelissen RG, Vliet Vlieland TP. Guideline recommendations for post-acute postoperative physiotherapy in total hip and knee arthroplasty: Are they used in daily clinical practice? Musculoskel Care 2014; 12: 125–131. [DOI] [PubMed] [Google Scholar]
- 5. Minns Lowe CJ, Barker KL, Dewey M, Sackley CM. Effectiveness of physiotherapy exercise after knee arthroplasty for osteoarthritis: Systematic review and meta-analysis of randomised controlled trials. BMJ 2007; 335: 812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Artz N, Elvers KT, Minns Lowe C, Sackley C, Jepson P, Beswick AD. Effectiveness of physiotherapy exercise following total knee replacement: Systematic review and meta-analysis. BMC Musculoskel Disord 2015; 16(1): 15 DOI: 10.1186/s12891-015-0469-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Luoma ML, Hakamies-Blomqvist L, Blomqvist C, Nikander R, Gustavsson-Lilius M, Saarto T. Experiences of breast cancer survivors participating in a tailored exercise intervention – a qualitative study. Anticancer Res 2014; 34: 1193–1199. [PubMed] [Google Scholar]
- 8. Foster NE, Healey EL, Holden MA, et al. A multicentre, pragmatic, parallel group, randomised controlled trial to compare the clinical and cost-effectiveness of three physiotherapy-led exercise interventions for knee osteoarthritis in older adults: The BEEP trial protocol (ISRCTN: 93634563). BMC Musculoskel Disord 2014; 15: 254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wesson J, Clemson L, Brodaty H, et al. A feasibility study and pilot randomised trial of a tailored prevention program to reduce falls in older people with mild dementia. BMC Geriatr 2013; 13: 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gronstedt H, Frandin K, Bergland A, et al. Effects of individually tailored physical and daily activities in nursing home residents on activities of daily living, physical performance and physical activity level: A randomized controlled trial. Gerontology 2013; 59: 220–229. [DOI] [PubMed] [Google Scholar]
- 11. Rasotto C, Bergamin M, Simonetti A, et al. Tailored exercise program reduces symptoms of upper limb work-related musculoskeletal disorders in a group of metalworkers: A randomized controlled trial. Man Ther 2015; 1: 56–62. [DOI] [PubMed] [Google Scholar]
- 12. Hurley MV, Walsh NE, Mitchell HL, et al. Clinical effectiveness of a rehabilitation program integrating exercise, self-management, and active coping strategies for chronic knee pain: A cluster randomized trial. Arthritis Rheum 2007; 57(7): 1211–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Han AS, Nairn L, Harmer AR, et al. Early rehabilitation after total knee replacement surgery: A multicenter, noninferiority, randomized clinical trial comparing a home exercise program with usual outpatient care. Arthritis Care Res 2015; 67(2): 196–202. [DOI] [PubMed] [Google Scholar]
- 14. Negus JJ, Cawthorne DP, Chen JS, Scholes CJ, Parker DA, March LM. Patient outcomes using Wii-enhanced rehabilitation after total knee replacement – the TKR-POWER study. Contemp Clin Trials 2015; 40: 47–53. [DOI] [PubMed] [Google Scholar]
- 15. Piva SR, Moore CG, Schneider M, Gil AB, Almeida GJ, Irrgang JJ. A randomized trial to compare exercise treatment methods for patients after total knee replacement: Protocol paper. BMC Musculoskel Disord 2015; 16: 303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Madsen M, Larsen K, Madsen IK, Søe H, Hansen TB. Late group-based rehabilitation has no advantages compared with supervised home-exercises after total knee arthroplasty. Dan Med J 2013; 60(4): A4607. [PubMed] [Google Scholar]
- 17. Hurley MV, Walsh NE, Mitchell HL, et al. Economic evaluation of a rehabilitation program integrating exercise, self-management, and active coping strategies for chronic knee pain. Arthritis and Rheumatism 2007; 57: 1220–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mitchell C, Walker J, Walters S, Morgan AB, Binns T, Mathers N. Costs and effectiveness of pre- and post-operative home physiotherapy for total knee replacement: Randomized controlled trial. J Eval Clin Pract 2005; 11: 283–292. [DOI] [PubMed] [Google Scholar]
- 19. da Silva FS, de Melo FE, do Amaral MM, et al. Efficacy of simple integrated group rehabilitation program for patients with knee osteoarthritis: Single-blind randomized controlled trial. J Rehabil Res Dev 2015; 52(3): 309–322. [DOI] [PubMed] [Google Scholar]
- 20. Westby M, Backman C. Patient and health professional views on rehabilitation practices and outcomes following total hip and knee arthroplasty for osteoarthritis: A focus group study. BMC Health Serv Res 2010; 10: 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Naylor JM, Mittal R, Carroll K, Harris IA. Introductory insights into patient preferences for outpatient rehabilitation after knee replacement: Implications for practice and future research. J Eval Clin Pract 2012; 18: 586–592. [DOI] [PubMed] [Google Scholar]
- 22. Orbell S, Johnston M, Rowley D, Davey P, Espley A. Self-efficacy and goal importance in the prediction of physical disability in people following hospitalization: A prospective study. Br J Health Psychol 2001; 6: 25–40. [DOI] [PubMed] [Google Scholar]
- 23. Craig P, Dieppe P, Macintyre S, Mitchie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: The new medical research council guidance. BMJ 2008, 337: a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brock TM, Sprowson AP, Muller S, Reed MR. Short-stretch inelastic compression bandage in knee swelling following total knee arthroplasty study (STICKS): Study protocol for a randomised controlled feasibility study. Trials 2015; 16: 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jepson P, Sands G, Beswick AD, Davis ET, Blom AW, Sackley CM. A feasibility randomized controlled trial of pre-operative occupational therapy to optimise recovery for patients undergoing primary total hip replacement for osteoarthritis (PROOF-THR). Clin Rehabil 2016; 30(2): 156–166. [DOI] [PubMed] [Google Scholar]
- 26. Evans S, Royston P, Day S. Minim: Allocation by minimisation in clinical trials. Available at: http://www-usersyorkacuk/~mb55/guide/minimhtm (accessed 2 March 2012).
- 27. North Bristol NHS Trust. Knee replacement a guide for patients. Available at: https://www.nbt.nhs.uk/sites/default/files/attachments/Your%20knee%20replacement_NBT002048.pdf (accessed 15 December 2011).
- 28. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther 1998; 28: 88–96. [DOI] [PubMed] [Google Scholar]
- 29. Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): Scale development, measurement properties, and clinical application. Physical Therapy 1999; 79: 371–383. [PubMed] [Google Scholar]
- 30. Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am 1984; 66: 228–241. [PubMed] [Google Scholar]
- 31. Pollard B, Dixon D, Dieppe P, Johnston M. Measuring the ICF components of impairment, activity limitation and participation restriction: An item analysis using classical test theory and item response theory. Health Qual Life Outcomes 2009; 7: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci 1995; 50A: M28–34. [DOI] [PubMed] [Google Scholar]
- 33. Waldrop D, Lightsey R, Ethington C, Woemmel C, Coke A. Self-efficacy, optimism, health competence, and recovery from orthopedic surgery. J Couns Psychol 2001; 48: 233–238. [Google Scholar]
- 34. Paterson C. Measuring outcomes in primary care: A patient generated measure, MYMOP, compared with the SF-36 health survey. BMJ 1996; 312: 1016–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: Recommendations for good practice. J Eval Clin Pract 2004; 10: 307–312. [DOI] [PubMed] [Google Scholar]
- 36. Minns Lowe CJ, Barker KL, Holder R, Sackley CM. Comparison of postdischarge physiotherapy versus usual care following primary total knee arthroplasty for osteoarthritis: An exploratory pilot randomized clinical trial. Clin Rehabil 2012; 26: 629–641. [DOI] [PubMed] [Google Scholar]
- 37. Moffet H, Collet JP, Shapiro SH, Paradis G, Marquis F, Roy L. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: A single-blind randomized controlled trial. Arch Phys Med Rehabil 2004; 85: 546–556. [DOI] [PubMed] [Google Scholar]
- 38. Harmer AR, Naylor JM, Crosbie J, Russell T. Land-based versus water-based rehabilitation following total knee replacement: A randomized, single-blind trial. Arthritis Rheum 2009; 61: 184–191. [DOI] [PubMed] [Google Scholar]
- 39. Wylde V, Marques E, Artz N, Blom A, Gooberman-Hill R. Effectiveness and cost-effectiveness of a group-based pain self-management intervention for patients undergoing total hip replacement: Feasibility study for a randomized controlled trial. Trials 2014; 15: 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rogers KD, Blyth FM, March LM, Jorm L. A nested case-control analysis of self-reported physical functioning after total knee replacement surgery in the 45 and Up Study Cohort. BMJ Open 2013; 3: e002291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. de Beer J, Petruccelli D, Adili A, Piccirillo L, Wismer D, Winemaker M. Patient perspective survey of total hip vs total knee arthroplasty surgery. J Arthroplasty 2012; 27: 865–869, e1–5. [DOI] [PubMed] [Google Scholar]
- 42. Westby MD, Brittain A, Backman CL. Expert consensus on best practices for post-acute rehabilitation after total hip and knee arthroplasty: A Canada and United States Delphi study. Arthritis Care Res 2014; 66: 411–423. [DOI] [PubMed] [Google Scholar]
- 43. Young NL, Cheah D, Waddell JP, Wright JG. Patient characteristics that affect the outcome of total hip arthroplasty: A review. Can J Surg 1998; 41: 188–195. [PMC free article] [PubMed] [Google Scholar]
- 44. Orbell S, Johnston M, Rowley D, Davey P, Espley A. Self-efficacy and goal importance in the prediction of physical disability in people following hospitalization: A prospective study. Br J Health Psychol 2001; 6: 25–40. [DOI] [PubMed] [Google Scholar]
- 45. Peer MA, Lane J. The Knee Injury and Osteoarthritis Outcome Score (KOOS): A review of its psychometric properties in people undergoing total knee arthroplasty.J Orthop Sports Phys Ther 2013; 43: 20–28. [DOI] [PubMed] [Google Scholar]
- 46. Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC), Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arth Care & Res 2011; 63(Suppl 11): S208–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Stratford PW, Kennedy DM, Maly MR, Macintyre NJ. Quantifying self-report measures’ overestimation of mobility scores post arthroplasty. Phys Ther 2010; 90: 1288–1296. [DOI] [PubMed] [Google Scholar]
- 48. Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol 2012; 65: 301–308. [DOI] [PubMed] [Google Scholar]