Abstract
Objectives
For patients with femoral neck fractures, total hip arthroplasty demonstrates superior outcomes compared to hemiarthroplasty. However hemiarthroplasty remains a common treatment for femoral neck fractures and the conversion rates are unknown. We compared the results of the two procedures utilizing a Medicare database.
Methods
We assembled a cohort of 70,242 patients age 65 to 90 with an ICD9 diagnosis and matching Current Procedure terminology (CPT) code for femoral neck fracture between 2008 and 2012. Patients were followed forward for two years minimum. Incidences of dislocation and mortality were measured. Reoperation for revision of total hip arthroplasty or conversion of hemiarthroplasty to total hip arthroplasty was assessed by CPT code. Groups were compared via proportional hazard models controlling for age, race, sex and comorbidity index.
Results
Hemiarthroplasty represented 95% of the patients treated using arthroplasty for femoral neck fracture. The proportional hazard of reoperation and dislocation were significantly lower for hemiarthroplasty than total hip arthroplasty (p<0.0001 for both). At two years, fewer than 2% of hemiarthroplasty patients underwent conversion to total hip replacement. Patients treated with total hip arthroplasty were more likely to be alive at two years (adjusted hazard ratio=1.67, 95% Confidence Interval: 1.59 to 1.92).
Conclusion
Patients treated with hemiarthroplasty following femoral neck fractures had significantly lower proportional hazard of reoperation than those treated with total hip arthroplasty. Total hip arthroplasty may be associated with lower mortality.
Level of Evidence
Therapeutic, Level III.(1)
Multiple randomized controlled trials have demonstrated that total hip arthroplasty (THA) for treatment of displaced femoral neck fractures results in superior functional outcomes over hemiarthroplasty(2-4). Previous studies have shown, however, that hemiarthroplasty (partial hip replacement) is the most common procedure used to treat femoral neck fractures in the United States(5).
The popularity of hemiarthroplasty may be related to higher risk of dislocation and higher mortality(2) seen in THA for femoral neck fracture compared to primary total hip arthroplasty(3). While a hemiarthroplasty may be later converted to a total hip arthroplasty, this is an additional surgery and not without risk of complications(6).
Given the low event rates for dislocation and reoperation, a large sample of patients is needed to compare the outcomes of arthroplasty for femoral neck fractures and control for differences in patient characteristics. We utilized a sample of US Medicare beneficiaries to study the utilization of hemiarthroplasty and total hip arthroplasty and investigate the choice of procedure on the outcomes and mortality. We hypothesized that total hip arthroplasty would have fewer reoperations that hemiarthroplasty.
Methods
We utilized the ENCLAVE system of the Center for Medicare and Medicaid Services, which has access to 100% of the Medicare beneficiaries in the US (see Figure, Supplemental Digital Content 1). The dataset was queried to generate a list of Medicare beneficiaries who were using fee-for-service during the observation period (2008-2012), underwent total arthroplasty or hemiarthroplasty following femoral neck fracture, at the age between 65 and 90 years old, and had minimum two years of follow up in the database (except patients who died). We used proportional hazard models of survival analysis to study the hazard of having a conversion, revision, dislocation, or death, whichever occurred first, comparing the two groups who underwent either total hip arthroplasty or hemiarthroplasty. Proportional hazard models control for differences in age or other covariates between the groups by producing adjusted hazard ratios.
Principal ICD9 codes were used to identify beneficiaries with femoral neck fractures, and total hip arthroplasty and hemiarthroplasty were identified using CPT codes 27130 and 27236 from physician claims files. Conversion from hemiarthroplasty to total arthroplasty (CPT code 27132) and revision of total arthroplasty (CPT 27134, 27137, or 27138) were treated as complications following hemiarthroplasty and total hip arthroplasty, respectively. Other outcomes included death and dislocation. Dislocation was identified by the CPT code for closed reduction (CPT 27266). We were not able to measure periprosthetic fractures.
The covariates used for adjusted survival analysis included sex, age, race and comorbidity index. Age was determined at the index date, and race was classified as White, Black, or other. All the non-demographic variables were determined during the 12 months prior to the index date. Comorbidity index was developed using Gagne et al. 2011(7). Linearity and proportionality of hazard functions were tested using Martingale and Schoenfeld residuals, respectively. All analyses were conducted using SAS Enterprise Guide 4.3 with SAS 9.2 (SAS Institute, Inc., Cary, NC, USA) at α=0.05 significance level. We also performed a sub-analysis of patients age 75-84 and a comorbidity index of 1 or 2.
This study was reviewed and approved by CMS and the Institutional Review Board of NIH.
Results
The final cohort consisted of 70,242 patients who were treated with arthroplasty for a diagnosis of femoral neck fracture (Table 1). The mean age was 81.3 years (standard deviation 6.4 years). The vast majority (95%) of patients treated by arthroplasty for femoral neck fracture underwent hemiarthroplasty. Patients who underwent total hip arthroplasty tended to be younger (p<0.001), and have fewer co-morbid conditions (p<0.001). We observed a borderline trend towards total hip arthroplasty patients being more likely to be white (p=0.06) and male (p=0.06) but the actually percentage differences were small and less that 1.5%.
Table 1.
| Hemiarthroplasty | Total Hip Arthroplasty | p value | ||
|---|---|---|---|---|
| Number of Patients | 69,142 | 1,100 | ||
| Age(Years) | 65 to 69 | 6.4% | 14.6% | <0.001 |
| 70 to 74 | 10.5% | 18.5% | ||
| 75 to 79 | 17.5% | 21.0% | ||
| 80 to 84 | 27.8% | 24.3% | ||
| 85 to 90 | 37.9% | 21.7% | ||
| Race | Black | 3.6% | 3.1% | 0.0608 |
| Others | 5.1% | 4.5% | ||
| White | 91.3% | 92.4% | ||
| Sex | Male | 26.2% | 27.6% | 0.0616 |
| Female | 73.8% | 72.4% | ||
| Number of Comorbidities | 0 | 38.1% | 50.1% | <0.001 |
| 1 | 18.3% | 19.9% | ||
| 2 | 14.9% | 11.3% | ||
| 3+ | 28.7% | 18.8% |
Two year mortality incidence after femoral neck fracture for the entire cohort was 39%. After adjusting for age, sex, and comorbidity index in the proportional hazards model, the group treated with total hip arthroplasty had a lower mortality (Figure 1). Patients treated with total hip arthroplasty were 1.67 times more likely to be alive at two years (95% CI 1.59 to 1.92).
Figure 1. Mortality after Arthroplasty for Treatment of Femoral Neck Fracture. The dark line represents the cumulative incidence of mortality.
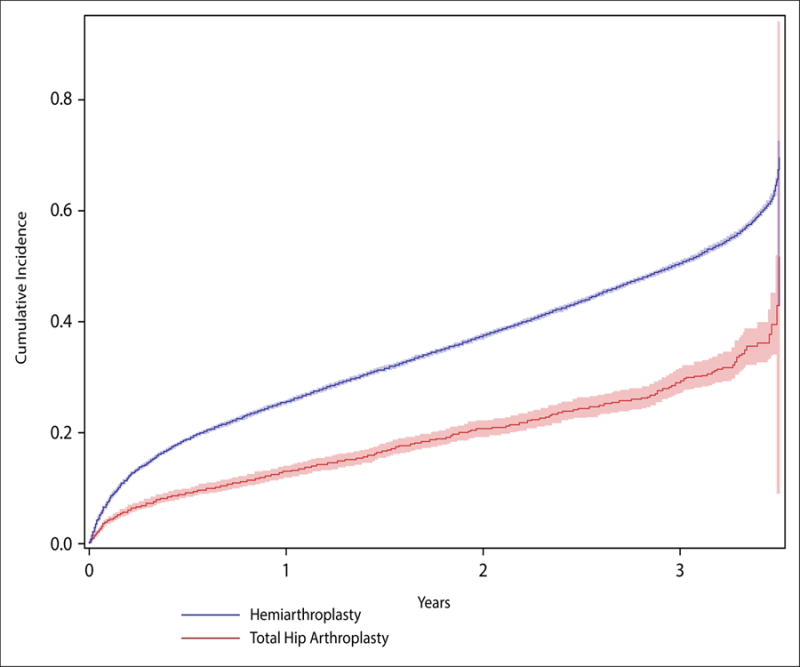
The shaded areas represent the 95% confidence interval.
The unadjusted incidence of patients undergoing conversion from hemiarthroplasty within two years was 2.0%. We noted that the patients undergoing conversion tended be younger and more likely to be white (p<0.001). Patients undergoing hemiarthroplasty had a lower rate of reoperation than patients undergoing THA (Figure 2, p<0.0001)
Figure 2. Incidence of Reoperation after Total Hip Arthroplasty or Hemiarthroplasty for Treatment Femoral Neck Fracture.
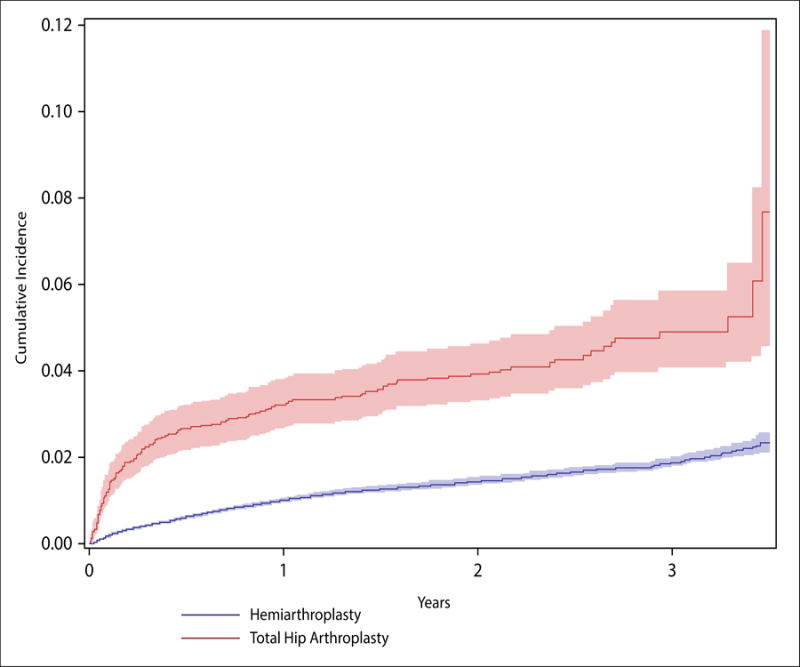
For the total hip arthroplasty cohort, reoperation represents revision arthroplasty. For the hemiarthroplasty cohort, reoperation represents conversation to total hip arthroplasty
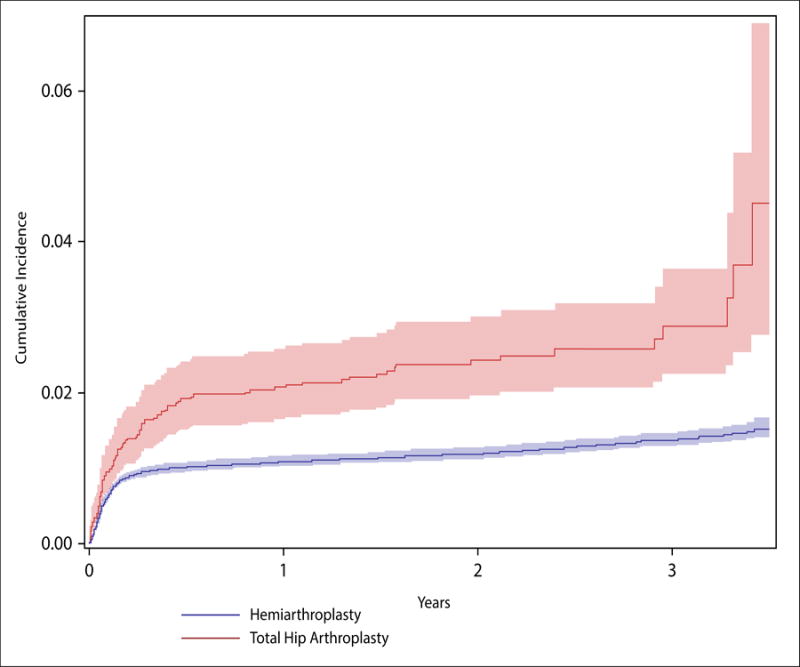
The rate of dislocation after hemiarthroplasty within 2 years was 1.5%, and the rate of dislocation after total hip arthroplasty was 2.9%. The hazard of dislocation was significantly higher after total hip arthroplasty (hazard ratio 2.02, 95% CI 1.62 to 2.52). The majority of dislocations occurred with 50 days after surgery (Figure 3). Reoperation was more common in the total hip arthroplasty group than the hemiarthroplasty group (hazard ratio 2.11, 95% CI 1.77 to 2.52). At two years 4.5% of the total hip arthroplasty group had undergone revision arthroplasty, whereas only 1.6% of the hemiarthroplasty group had undergone reoperation (p<0.0001). The ICD9 code for cause of revision was rarely coded beyond “mechanical complication of orthopaedic device.”
Figure 3. Incidence of Dislocation after Total Hip Arthroplasty or Hemiarthroplasty for Treatment Femoral Neck Fracture.
When we subset the sample to those with age 75-84 and comorbidity scores in 1 or 2, we got a much smaller group (n=15,377) with comparable distribution in terms of age and comorbidities (p<0.6). The results were similar: the two-year mortality hazard ration comparing those treated with hemiarthroplasty with those with total hip arthroplasty was 1.89 (95% CI 1.55-2.29). As for dislocation, the hazard ratio comparing total hip arthroplasty to hemiarthroplasty was 2.19 (95% CI 1.40-3.41), whereas that for reoperation is 2.12 (95% CI 1.48-3.03).
Comparing the older (age>70) subgroup to the younger (age 65 to 69) subgroup, we found that older patients had a higher one year mortality (hazard ratio 1.87, 95% CI 1.82-2.13), but a lower revision rate (0.56, 95% CI 0.47-0.66) and lower dislocation rate (0.80, 95% CI 0.63 to 0.99) than younger patients.
Discussion
Our study of a large Medicare database shows that the majority of femoral neck fractures are treated with hemiarthroplasty, and that reoperations were significantly lower in the hemiarthroplasty group compared to the total hip group.
Randomized prospective studies have shown that total hip arthroplasty for femoral neck fractures results in the best functional outcome(2-4). Our study indicates that the vast majority of patients in the US are treated with hemiarthroplasty. Given that the preveleance of cognitive impairment in the hip fracture population is about 34%, and 82% or more are community ambulators, it would appear that total hip arthroplasty is underutilized it the United States.
Helping patients choose between total hip arthroplasty and hemiarthroplasty after a femoral neck fracture is difficult. The surgeon is often meeting the patient for the first time. There is some urgency to the surgery, because patients are in pain and outcomes are improved when surgery is performed without excessive delay(8). Finally there is no opportunity for the preoperative education on dislocation prevention.
Our study provides some useful information to aid patients and their surgeons in making the decision. While total hip results in the best functional outcome, hemiarthroplasty has a low complication rate: At 2 years, the rate of prosthetic dislocation is less than 2% and the rate of conversion to total hip replacement is less than 2%. Also, the 5% utilization rate of total hip arthroplasty is helpful for benchmarking in large care delivery systems.
The main drawback to performing total hip arthroplasty for femoral neck fractures is the risk of dislocation(9). While total hip arthroplasty patients had a higher hazard of dislocation than hemiarthroplasty, the cumulative incidence of dislocation at 2 years was 2.9%. We did note a fairly high incidence of revision in the total hip arthroplasty group at two years (7%). This may be related to the poor bone quality seen in this patient population or surgeon experience and deserves further study; our current dataset precludes analysis by surgeon volume.
We observed a significantly decreased proportional hazard of mortality in the group who underwent total hip arthroplasty, even after accounting for age and comorbidities. Other researchers have noticed total joint replacement to be associated with improved survival(10), and it is likely related to selection bias. The patients who undergo total hip arthroplasty after femoral neck fracture likely have some unmeasured factor (such as cognitive function or pre-injury activity level) which is not fully measured in a co-morbidity index. However one cannot rule out the possibility that the improved function of a total hip allows improved mobility and function, which then decreases medical complications. One randomized study of femoral neck fractures found lower mortality at seven year follow-up in the group randomized to total hip replacement(2).
Our study has a number of limitations. First, the Medicare dataset may be large, but it is purely administrative data without any clinical information about patient functional status or demands. A large part of the hemiarthroplasty cohort may be unhappy with their hip function but unwilling to undergo reoperation. Second, because relatively few patients underwent total hip arthroplasty, our ability to assess that group is limited. However our large sample sizes leads to narrow confidence intervals for the main outcome, reoperation. Third, we chose to measure outcome at the first event (dislocation or reoperation). Some patients may have had a dislocation followed by a reoperation, so our estimate of the revision rate likely underestimates the revision rate. If 100% of the patients who sustained a dislocation underwent revision, the revision rate for THA would go up by two percentage points. Finally, we did not have any functional outcome data in this database. Functional outcome data would strongly helpful in guiding the decision making.
In summary, we found that total hip arthroplasty was utilized less often than hemiarthroplasty, and was associated with higher incidence of revision but lower mortality over two years. While total hip arthroplasty remains the procedure of choice for healthier patients with femoral neck fractures, reoperation or conversion surgery after hemiarthroplasty is uncommon.
Supplementary Material
Overview of cohort construction.
Footnotes
Investigation performed at National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health, Bethesda MD
References
- 1.Woodward LM, Clemson L, Moseley AM, et al. Most functional outcomes are similar for men and women after hip fracture: a secondary analysis of the enhancing mobility after hip fracture trial. BMC Geriatr. 2014;14:140. doi: 10.1186/1471-2318-14-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avery PP, Baker RP, Walton MJ, et al. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a seven- to ten-year follow-up report of a prospective randomised controlled trial. J Bone Joint Surg Br. 2011;93:1045–1048. doi: 10.1302/0301-620X.93B8.27132. [DOI] [PubMed] [Google Scholar]
- 3.Baker RP, Squires B, Gargan MF, et al. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006;88:2583–2589. doi: 10.2106/JBJS.E.01373. [DOI] [PubMed] [Google Scholar]
- 4.Blomfeldt R, Törnkvist H, Eriksson K, et al. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint Surg Br. 2007;89:160–165. doi: 10.1302/0301-620X.89B2.18576. [DOI] [PubMed] [Google Scholar]
- 5.Lieberman JR, Romano PS, Mahendra G, et al. The treatment of hip fractures: variations in care. Clin Orthop Relat Res. 2006;442:239–244. doi: 10.1097/01.blo.0000188558.67172.4e. [DOI] [PubMed] [Google Scholar]
- 6.Sah AP, Estok DM. Dislocation rate after conversion from hip hemiarthroplasty to total hip arthroplasty. J Bone Joint Surg Am. 2008;90:506–516. doi: 10.2106/JBJS.G.00479. [DOI] [PubMed] [Google Scholar]
- 7.Gagne JJ, Glynn RJ, Avorn J, et al. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64:749–759. doi: 10.1016/j.jclinepi.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nyholm AM, Gromov K, Palm H, et al. Time to Surgery Is Associated with Thirty-Day and Ninety-Day Mortality After Proximal Femoral Fracture: A Retrospective Observational Study on Prospectively Collected Data from the Danish Fracture Database Collaborators. J Bone Joint Surg Am. 2015;97:1333–1339. doi: 10.2106/JBJS.O.00029. [DOI] [PubMed] [Google Scholar]
- 9.Bhandari M, Devereaux PJ, Einhorn TA, et al. Hip fracture evaluation with alternatives of total hip arthroplasty versus hemiarthroplasty (HEALTH): protocol for a multicentre randomised trial. BMJ Open. 2015;5:e006263. doi: 10.1136/bmjopen-2014-006263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barrett J, Losina E, Baron JA, et al. Survival following total hip replacement. J Bone Joint Surg Am. 2005;87:1965–1971. doi: 10.2106/JBJS.D.02440. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Overview of cohort construction.


