Summary
Each year, the American Heart Association (AHA), in conjunction with the Centers for Disease Control and Prevention, the National Institutes of Health, and other government agencies, brings together the most up-to-date statistics on heart disease, stroke, other vascular diseases, and their risk factors and presents them in its Heart Disease and Stroke Statistical Update. The Statistical Update is a critical resource for researchers, clinicians, healthcare policy makers, media professionals, the lay public, and many others who seek the best available national data on heart disease, stroke, and other cardiovascular disease–related morbidity and mortality and the risks, quality of care, use of medical procedures and operations, and costs associated with the management of these diseases in a single document. Indeed, since 1999, the Statistical Update has been cited >10 500 times in the literature, based on citations of all annual versions. In 2012 alone, the various Statistical Updates were cited ≈3500 times (data from Google Scholar). In recent years, the Statistical Update has undergone some major changes with the addition of new chapters and major updates across multiple areas, as well as increasing the number of ways to access and use the information assembled.
For this year’s edition, the Statistics Committee, which produces the document for the AHA, updated all of the current chapters with the most recent nationally representative data and inclusion of relevant articles from the literature over the past year. This year’s edition includes a new chapter on peripheral artery disease, as well as new data on the monitoring and benefits of cardiovascular health in the population, with additional new focus on evidence-based approaches to changing behaviors, implementation strategies, and implications of the AHA’s 2020 Impact Goals. Below are a few highlights from this year’s Update.
The 2014 Update Expands Data Coverage of the Epidemic of Poor Cardiovascular Health Behaviors and Their Antecedents and Consequences
Adjusted estimated population attributable fractions for cardiovascular disease (CVD) mortality were as follows1: 40.6% (95% confidence interval [CI], 24.5%–54.6%) for high blood pressure; 13.7% (95% CI, 4.8%–22.3%) for smoking; 13.2% (95% CI, 3.5%–29.2%) for poor diet; 11.9% (95% CI, 1.3%–22.3%) for insufficient physical activity; and 8.8% (95% CI, 2.1%–15.4%) for abnormal blood glucose levels.
Although significant progress has been made over the past 4 decades, in 2012, among Americans ≥18 years of age, 20.5% of men and 15.9% of women continued to be cigarette smokers. In 2011, 18.1% of students in grades 9 through 12 reported current cigarette use.
The percentage of the nonsmoking population with exposure to secondhand smoke (as measured by serum cotinine levels ≥0.05 ng/mL) declined from 52.5% in 1999 to 2000 to 40.1% in 2007 to 2008. More than half of children 3 to 11 years of age (53.6%) and almost half of those 12 to 19 years of age (46.5%) had detectable levels, compared with just over a third of adults 20 years of age and older (36.7%).
The proportion of youth (≤18 years of age) who report engaging in no regular physical activity is high, and the proportion increases with age.
In 2011, among adolescents in grades 9 through 12, 17.7% of girls and 10.0% of boys reported that they had not engaged in ≥60 minutes of moderate to vigorous physical activity (defined as any activity that increased heart rate or breathing rate) at least once in the previous 7 days, despite recommendations that children engage in such activity 7 days per week.
In 2012, 29.9% of adults reported engaging in no aerobic leisure-time physical activity.
In 2009 to 2010, <1% of Americans met at least 4 of 5 healthy dietary goals. Among adults aged ≥20 years, only 12.3% met recommended goals for fruits and vegetables; 18.3% met goals for fish; 0.6% met goals for sodium; 51.9% met goals for sugar-sweetened beverages; and 7.3% met goals for whole grains. These proportions were even lower in children, with only 29.4% of adolescents aged 12 to 19 years meeting goals for low sugar-sweetened beverage intake.
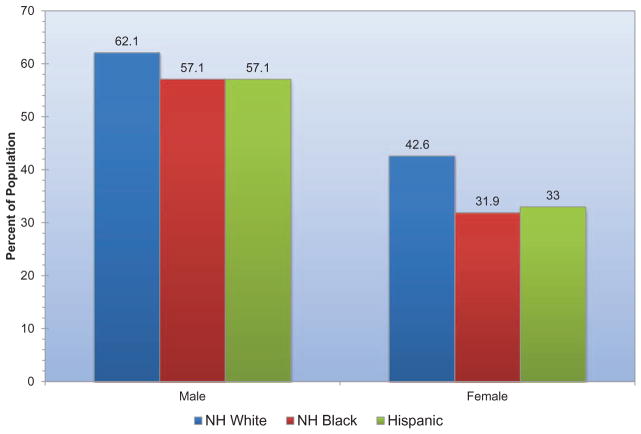
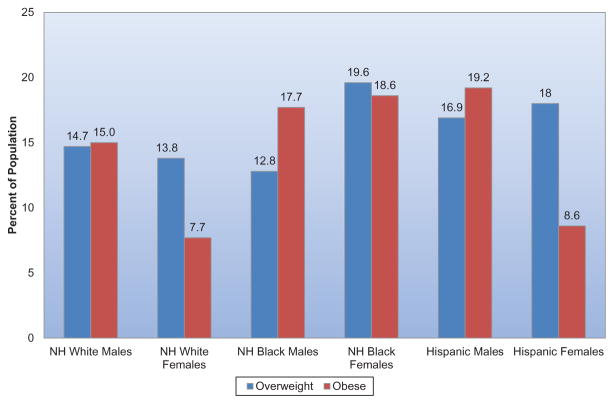
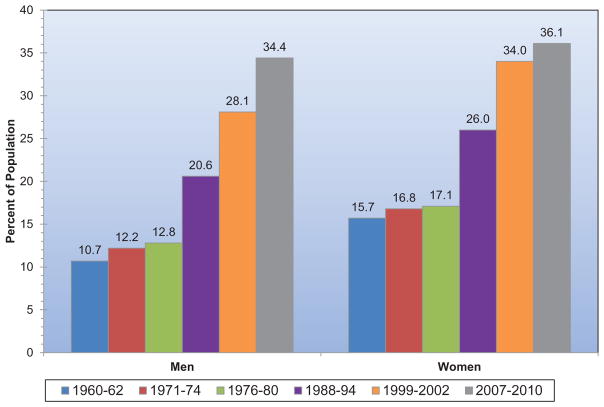
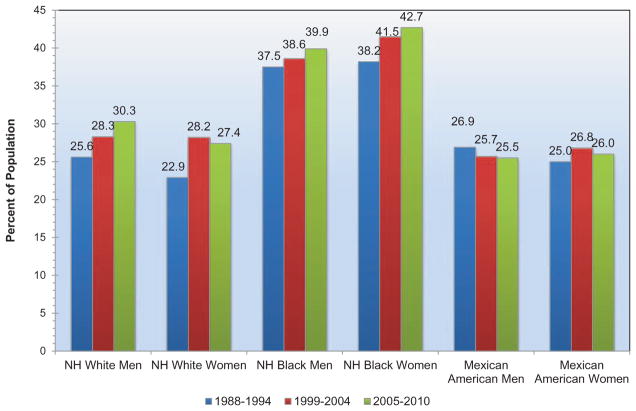
The estimated prevalence of overweight and obesity in US adults (≥20 years of age) is 154.7 million, which represented 68.2% of this group in 2010. Nearly 35% of US adults are obese (body mass index ≥30 kg/m2). Men and women of all race/ethnic groups in the population are affected by the epidemic of overweight and obesity.
Among children 2 to 19 years of age, 31.8% are overweight and obese (which represents 23.9 million children) and 16.9% are obese (12.7 million children). Mexican American boys and girls and African American girls are disproportionately affected. From 1971–1974 to 2007–2010, the prevalence of obesity in children 6 to 11 years of age has increased from 4.0% to 18.8%.
Obesity (body mass index ≥30 kg/m2) is associated with marked excess mortality in the US population. Even more notable is the excess morbidity associated with overweight and obesity in terms of risk factor development and incidence of diabetes mellitus, CVD end points (including coronary heart disease, stroke, and heart failure), and numerous other health conditions, including asthma, cancer, end-stage renal disease, degenerative joint disease, and many others.
Prevalence and Control of Cardiovascular Health Factors and Risks Remain an Issue for Many Americans
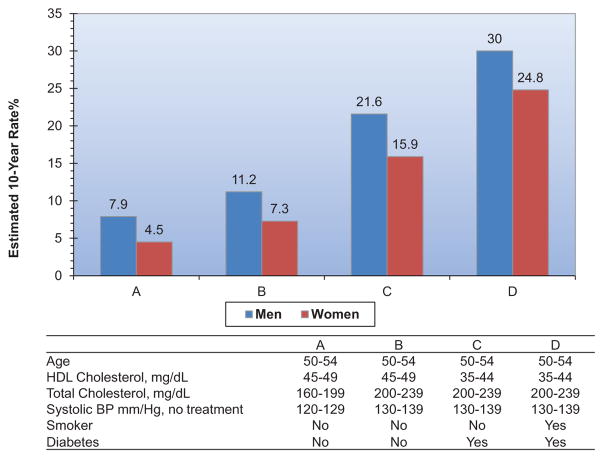
An estimated 31.9 million adults ≥20 years of age have total serum cholesterol levels ≥240 mg/dL, with a prevalence of 13.8%.
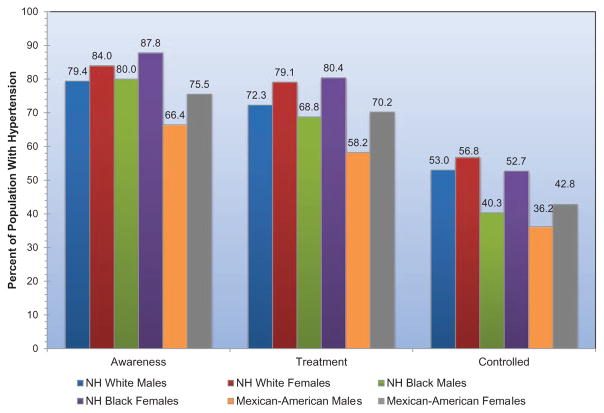
Based on 2007 to 2010 data, 33.0% of US adults ≥20 years of age have hypertension. This represents ≈78 million US adults with hypertension. The prevalence of hypertension is similar for men and women. African American adults have among the highest prevalence of hypertension (44%) in the world.
Among hypertensive Americans, ≈82% are aware of their condition and 75% are using antihypertensive medication, but only 53% of those with documented hypertension have their condition controlled to target levels.
In 2010, an estimated 19.7 million Americans had diagnosed diabetes mellitus, representing 8.3% of the adult population. An additional 8.2 million had undiagnosed diabetes mellitus, and 38.2% had prediabetes, with abnormal fasting glucose levels. African Americans, Mexican Americans, Hispanic/Latino individuals, and other ethnic minorities bear a strikingly disproportionate burden of diabetes mellitus in the United States.
The prevalence of diabetes mellitus is increasing dramatically over time, in parallel with the increases in prevalence of overweight and obesity.
Rates of Death Attributable to CVD Have Declined, but the Burden of Disease Remains High
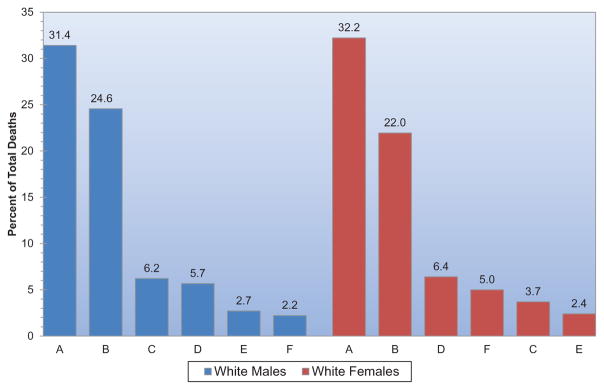
The 2010 overall rate of death attributable to CVD was 235.5 per 100 000. The rates were 278.4 per 100 000 for white males, 369.2 per 100 000 for black males, 192.2 per 100 000 for white females, and 260.5 per 100 000 for black females.
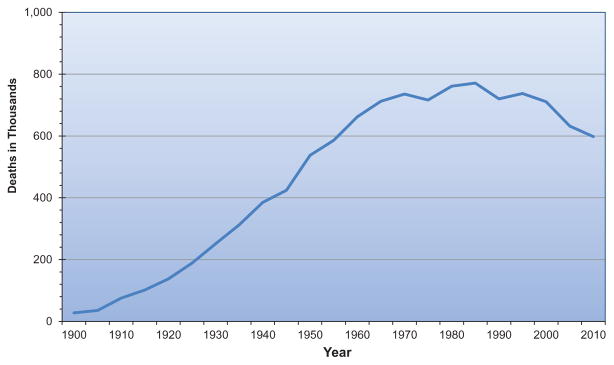
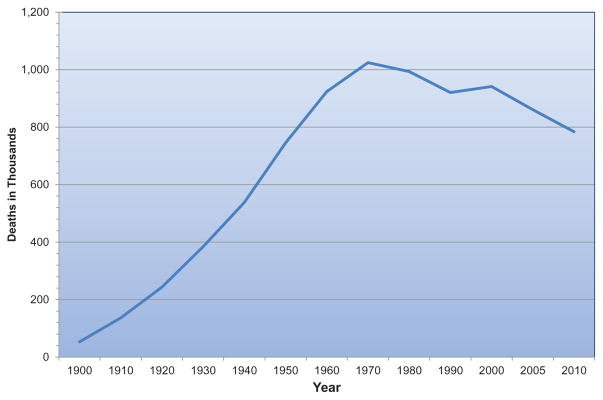
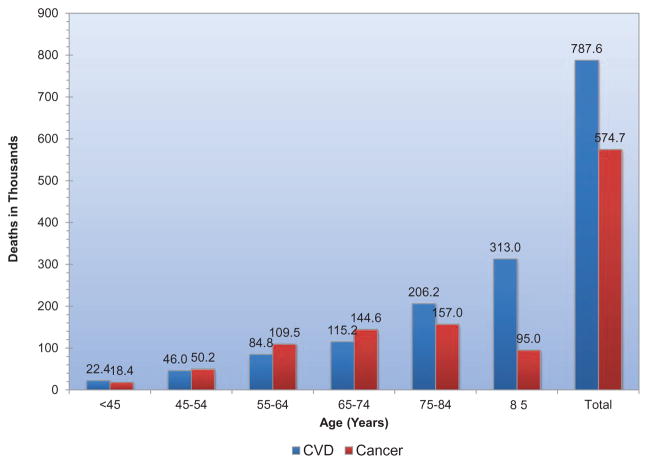
From 2000 to 2010, death rates attributable to CVD declined 31.0%. In the same 10-year period, the actual number of CVD deaths per year declined by 16.7%. Yet in 2010, CVD (I00–I99; Q20–Q28) still accounted for 31.9% (787 650) of all 2 468 435 deaths, or ≈1 of every 3 deaths in the United States.
On the basis of 2010 death rate data, >2150 Americans die of CVD each day, an average of 1 death every 40 seconds. About 150 000 Americans who died of CVD in 2010 were <65 years of age. In 2010, 34% of deaths attributable to CVD occurred before the age of 75 years, which is before the current average life expectancy of 78.7 years.
Coronary heart disease alone caused ≈1 of every 6 deaths in the United States in 2010. In 2010, 379 559 Americans died of CHD. Each year, an estimated ≈620 000 Americans have a new coronary attack (defined as first hospitalized myocardial infarction or coronary heart disease death) and ≈295 000 have a recurrent attack. It is estimated that an additional 150 000 silent first myocardial infarctions occur each year. Approximately every 34 seconds, 1 American has a coronary event, and approximately every 1 minute 23 seconds, an American will die of one.
From 2000 to 2010, the relative rate of stroke death fell by 35.8% and the actual number of stroke deaths declined by 22.8%. Yet each year, ≈795 000 people continue to experience a new or recurrent stroke (ischemic or hemorrhagic). Approximately 610 000 of these are first events and 185 000 are recurrent stroke events. In 2010, stroke caused ≈1 of every 19 deaths in the United States. On average, every 40 seconds, someone in the United States has a stroke, and someone dies of one approximately every 4 minutes.
The decline in stroke mortality over the past decades, a major improvement in population health observed for both sexes and all race and age groups, has resulted from reduced stroke incidence and lower case fatality rates. The significant improvements in stroke outcomes are concurrent with cardiovascular risk factor control interventions. The hypertension control efforts initiated in the 1970s appear to have had the most substantial influence on the accelerated decline in stroke mortality, with lower blood pressure distributions in the population. Control of diabetes mellitus and high cholesterol and smoking cessation programs, particularly in combination with hypertension treatment, also appear to have contributed to the decline in stroke mortality.2
In 2010, 1 in 9 death certificates (279 098 deaths) in the United States mentioned heart failure. Heart failure was the underlying cause in 57 757 of those deaths in 2010. The number of any-mention deaths attributable to heart failure was approximately as high in 1995 (287 000) as it was in 2010 (279 000). Additionally, hospital discharges for heart failure remained stable from 2000 to 2010, with first-listed discharges of 1 008 000 and 1 023 000, respectively.
The 2014 Update Provides Critical Data About Cardiovascular Quality of Care, Procedure Utilization, and Costs
In light of the current national focus on healthcare utilization, costs, and quality, it is critical to monitor and understand the magnitude of healthcare delivery and costs, as well as the quality of healthcare delivery, related to CVD risk factors and conditions. The Statistical Update provides these critical data in several sections.
Quality-of-Care Metrics for CVDs
Quality data are available from the AHA’s Get With The Guidelines programs for coronary heart disease, heart failure, and resuscitation and from the American Stroke Association/AHA’s Get With The Guidelines program for acute stroke. Similar data from the Veterans Healthcare Administration, national Medicare and Medicaid data, and Acute Coronary Treatment and Intervention Outcomes Network (ACTION)–Get With The Guidelines Registry data are also reviewed. These data show impressive adherence to guideline recommendations for many, but not all, metrics of quality of care for these hospitalized patients. Data are also reviewed on screening for CVD risk factor levels and control.
Cardiovascular Procedure Use and Costs
The total number of inpatient cardiovascular operations and procedures increased 28%, from 5 939 000 in 2000 to 7 588 000 in 2010 (National Heart, Lung, and Blood Institute computation based on National Center for Health Statistics annual data).
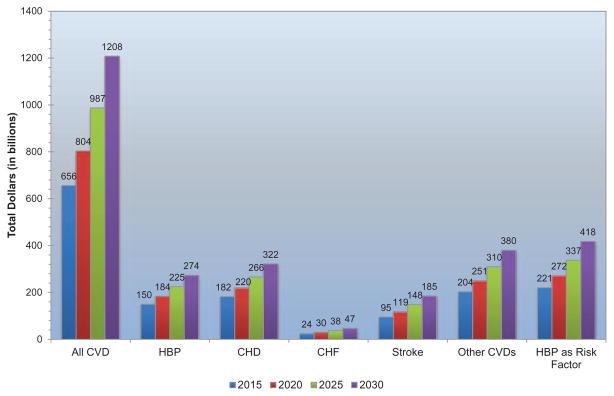
The total direct and indirect cost of CVD and stroke in the United States for 2010 is estimated to be $315.4 billion. This figure includes health expenditures (direct costs, which include the cost of physicians and other professionals, hospital services, prescribed medications, home health care, and other medical durables) and lost productivity that results from premature mortality (indirect costs).
By comparison, in 2008, the estimated cost of all cancer and benign neoplasms was $201.5 billion ($77.4 billion in direct costs, and $124 billion in mortality indirect costs). CVD costs more than any other diagnostic group.
The AHA, through its Statistics Committee, continuously monitors and evaluates sources of data on heart disease and stroke in the United States to provide the most current information available in the Statistics Update.
This annual Statistical Update is the product of an entire year’s worth of effort by dedicated professionals, volunteer physicians and scientists, and outstanding AHA staff members, without whom publication of this valuable resource would be impossible. Their contributions are gratefully acknowledged.
-
Alan S. Go, MD
Melanie B. Turner, MPH
On behalf of the American Heart Association Statistics
Committee and Stroke Statistics Subcommittee
Note: Population data used in the compilation of National Health and Nutrition Examination Survey (NHANES) prevalence estimates are for the latest year of the NHANES survey being used. Extrapolations for NHANES prevalence estimates are based on the census resident population for 2010 because this is the most recent year of NHANES data used in the Statistical Update.
- 1.Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, Gillespie C, Merritt R, Hu FB. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307:1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lackland DT, Roccella EJ, Deutsch A, Fornage M, George MG, Howard G, Kissela B, Kittner SJ, Lichtman JH, Lisabeth L, Schwamm LH, Smith EE, Towfighi A on behalf of the American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Quality of Care and Outcomes and Research, and Council on Functional Genomics and Translational Biology. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/ American Stroke Association. [Accessed December 5, 2013];Stroke. 2013 Dec 5; doi: 10.1161/01.str.0000437068.30550.cf. http://stroke.ahajournals.org/lookup/doi/10.1161/01.str.0000437068.30550.cf. [DOI]
Statistics 12.5% and 10.3% are statistically unreliable (relative standard error >30% and <50%). The statistic not shown has a relative standard error >50%.
The American Heart Association makes every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
Disclosures
| Writing Group Member |
Employment | Research Grant |
Other Research Support |
Speakers’ Bureau/ Honoraria |
Expert Witness |
Ownership Interest |
Consultant/ Advisory Board |
Other |
|---|---|---|---|---|---|---|---|---|
| Alan S. Go | Kaiser Permanente |
None | None | None | None | None | None | None |
| Dariush Mozaffarian |
Brigham and Women’s Hospital, Harvard Medical School, and Harvard School of Public Health | None | None | Ad hoc travel reimbursement and/ or honoraria for one-time scientific presentations or reviews on diet and cardiometabolic diseases from Life Sciences Research Organization (10/12) and Bunge (4/13) (each)* |
None | None | Ad hoc consulting fees from Amarin (9/13), Omthera (9/13), and Winston and Strawn LLP (9/13) (each)*; Advisory board: Unilever North America Scientific Advisory Board* |
Royalties from UpToDate, for an online chapter on fish oil*; Patent: Harvard University has filed a provisional patent application that has been assigned to Harvard University, listing Dr. Mozaffarian as a co-inventor to the US Patent and Trademark Office for use of trans-palmitoleic acid to prevent and treat insulin resistance, type 2 diabetes, and related conditions (no compensation)* |
| Véronique L. Roger |
Mayo Clinic | NIH† | None | None | None | None | None | None |
| Emelia J. Benjamin |
Boston University School of Medicine |
2R01HL092577-05†; 1R01HL102214†; HHSN26820130047C† |
None | None | None | None | NIH, NHLBI Outside Safety & Monitoring Board for the Coronary Artery Risk Development in Young Adults [CARDIA] Study*; Honorarium, American Heart Association, Associate Editor, Circulation† |
None |
| Jarett D. Berry |
UT Southwestern |
NHLBI†; AHA† |
None | Merck† | None | None | None | None |
| Michael J. Blaha |
Johns Hopkins | None | None | None | None | None | None | None |
| Shifan Dai |
Centers for Disease Control and Prevention |
None | None | None | None | None | None | None |
| Earl S. Ford |
Centers for Disease Control and Prevention |
None | None | None | None | None | None | None |
| Caroline S. Fox |
National Heart, Lung, and Blood Institute |
None | None | None | None | None | None | None |
| Sheila Franco | Centers for Disease Control and Prevention/ National Center for Health Statistics |
None | None | None | None | None | None | None |
| Heather J. Fullerton |
University of California, San Francisco |
NIH†; AHA† |
Private Philanthropy† |
None | None | None | None | None |
| Cathleen Gillespie |
Centers for Disease Control a nd Prevention |
None | None | None | None | None | None | None |
| Susan M. Hailpern |
Independent Consultant |
None | None | None | None | None | None | None |
| John A. Heit |
Mayo Clinic | NIH* | None | None | None | None | Daiichi Sankyo*; Janssen Pharmaceutical* | None |
| Virginia J. Howard |
University of Alabama at Birmingham |
NIH† | None | None | None | None | None | None |
| Mark D. Huffman |
Northwestern University Feinberg School of Medicine |
National Heart, Lung, and Blood Institute†; Eisenberg Foundation† |
Fogarty International Center (travel)*; World Heart Federation (conference, travel, and contract proposal under development)†; American Heart Association (travel)*; Cochrane Heart Group (travel)* |
None | None | None | None | None |
| Suzanne E. Judd |
University of Alabama at Birmingham |
NIH†; diaDexus† | None | None | None | None | diaDexus† | None |
| Brett M. Kissela |
University of Cincinnati |
NIH† | AbbVie and Reata* |
None | None | None | Allergan* | None |
| Steven J. Kittner |
University of Maryland School of Medicine and Veterans Administration Health Care System |
NINDS Ischemic Stroke Genetics Consortium (U01NS069208)† |
None | None | None | None | None | None |
| Daniel T. Lackland |
Medical University of South Carolina |
None | None | None | None | None | None | None |
| Judith H. Lichtman |
Yale University |
AHA†; NIH† |
None | None | None | None | None | None |
| Lynda D. Lisabeth |
University of Michigan |
R01 NS38916†; R01 NS062675*; R01 HL098065†; R01 NS070941† |
None | None | None | None | None | None |
| Rachel H. Mackey |
University of Pittsburgh |
LipoScience Inc.† | None | National Lipid Association* |
None | None | None | None |
| David J. Magid |
Colorado Permanente Medical Group |
NHLBI†; NIMH*; NIA*; AHRQ†; PCORI†; Amgen* |
None | None | None | None | None | None |
| Gregory M. Marcus |
University of California, San Francisco |
American Heart Association†; Gilead Sciences†; Medtronic†; SentreHeart† |
None | None | None | None | InCarda* | None |
| Ariane Marelli | McGill University Health Center |
None | None | None | None | None | None | None |
| David B. Matchar | Duke University Medical Center/ Duke-NUS Graduate Medical School |
Singapore National Medical Research Council (NMRC)† |
None | None | None | None | None | None |
| Darren K. McGuire |
UT South-western Medical Center |
None | Astra Zeneca*; Boehringer Ingelheim*; Bristol Myers Squibb*; Daiichi Sankyo*; Eli Lilly*; Genentech*; Glaxo Smith Kline*; F. Hoffmann LaRoche†; Merck*; Orexigen Therapeutic†; Takeda Pharmaceuticals North America* |
None | Takeda Pharmaceuticals North America† |
None | Boehringer Ingelheim*; Bristol Myers Squibb*; Genentech*; Janssen†; F. Hoffmann LaRoche*; Merck*; Sanofi Aventis* |
None |
| Emile R. Mohler III |
University of Pennsylvania |
GSK*; NIH*; Pluristem* |
None | None | None | Cytovas†; Floxmedical† |
Pfizer*; Takeda* |
None |
| Claudia S. Moy |
National Institutes of Health |
None | None | None | None | None | None | None |
| Michael E. Mussolino |
National Heart, Lung, and Blood Institute |
None | None | None | None | None | None | None |
| Robert W. Neumar | University of Michigan Health System |
None | None | None | None | None | None | None |
| Graham Nichol | University of Washington |
Resuscitation Outcomes Consortium (NIH U01 HL077863-06) 2010–2015, Co-PI†; Dynamic AED Registry (Food and Drug Administration, Cardiac Science Corp., Philips Healthcare Inc., Physio-Control Inc., HealthSine Technologies Inc., ZOLL Inc) 2012–2016, PI*; Velocity Pilot Study of Ultrafast Hypothermia in Patients with ST-elevation Myocardial Infarction (Velomedix Inc.) 2012–2014, National Co-PI (Waived personal compensation)* |
Novel method of tracking location of medical devices in time and space. (Patent pending, assigned to University of Washington)* |
None | None | None | Medic One Foundation Board of Directors (Money to Institution)* |
None |
| Dilip K. Pandey |
University of Illinois at Chicago |
None | None | None | None | None | None | None |
| Nina P. Paynter |
Brigham and Women’s Hospital |
Celera†; National Institutes of Health† |
None | None | None | None | None | None |
| Matthew J. Reeves |
Michigan State University |
None | None | None | None | None | None | None |
| Paul D. Sorlie |
National Heart , Lung, and Blood Institute, NIH |
None | None | None | None | None | None | None |
| Joel Stein |
Columbia University |
None | Myomo*; Tyromotion* |
QuantiaMD* | None | None | Myomo* | None |
| Amytis Towfighi |
University of Southern California |
AHA†; NIH/NINDS† |
None | None | None | None | None | None |
| Tanya N. Turan |
Medical University of South Carolina |
NIH/NINDS K23 – CHIASM PI† | None | None | Expert witness in Stroke-related medical malpractice cases* |
None | Boehringer Ingelheim, BI1356/BI 10773 Trials – Clinical Endpoint Adjudication Committee†; Gore REDUCE Trial-Clinical Endpoint Adjudication Committee*; NIH/NINDS VERITAS study – Clinical Endpoint Adjudication Committee* |
None |
| Melanie B. Turner |
American Heart Association |
None | None | None | None | None | None | None |
| Salim S. Virani |
Department of Veterans Affairs, Baylor College of Medicine |
Agency for Health Care Research and Quality*; Department of Veterans Affairs†; NIH*; Roderick D. MacDonald Research Foundation† |
None | None | None | None | None | None |
| Nathan D. Wong |
University of California, Irvine |
Bristol-Myers Squibb†; Regeneron† |
None | None | None | None | Genzyme* | None |
| Daniel Woo |
University of Cincinnati |
None | None | None | None | None | None | None |
1. About These Statistics
The AHA works with the CDC’s NCHS, the NHLBI, the NINDS, and other government agencies to derive the annual statistics in this Heart Disease and Stroke Statistical Update. This chapter describes the most important sources and the types of data we use from them. For more details, see Chapter 26 of this document, the Glossary.
The surveys used are:
BRFSS—ongoing telephone health survey system
GCNKSS—stroke incidence rates and outcomes within a biracial population
MEPS—data on specific health services that Americans use, how frequently they use them, the cost of these services, and how the costs are paid
NHANES—disease and risk factor prevalence and nutrition statistics
NHIS—disease and risk factor prevalence
NHDS—hospital inpatient discharges and procedures (discharged alive, dead, or status unknown)
NAMCS—physician office visits
NHHCS—staff, services, and patients of home health and hospice agencies
NHAMCS—hospital outpatient and ED visits
Nationwide Inpatient Sample of the AHRQ—hospital inpatient discharges, procedures, and charges
NNHS—nursing home residents
National Vital Statistics System—national and state mortality data
WHO—mortality rates by country
YRBSS—health-risk behaviors in youth and young adults
Abbreviations Used in Chapter 1
| AHA | American Heart Association |
| AHRQ | Agency for Healthcare Research and Quality |
| AP | angina pectoris |
| ARIC | Atherosclerosis Risk in Communities Study |
| BP | blood pressure |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CDC | Centers for Disease Control and Prevention |
| CHS | Cardiovascular Health Study |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| ED | emergency department |
| FHS | Framingham Heart Study |
| GCNKSS | Greater Cincinnati/Northern Kentucky Stroke Study |
| HD | heart disease |
| HF | heart failure |
| ICD | International Classification of Diseases |
| ICD-9-CM | International Classification of Diseases, Clinical Modification, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| MEPS | Medical Expenditure Panel Survey |
| MI | myocardial infarction |
| NAMCS | National Ambulatory Medical Care Survey |
| NCHS | National Center for Health Statistics |
| NHAMCS | National Hospital Ambulatory Medical Care Survey |
| NHANES | National Health and Nutrition Examination Survey |
| NHDS | National Hospital Discharge Survey |
| NHHCS | National Home and Hospice Care Survey |
| NHIS | National Health Interview Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| NINDS | National Institute of Neurological Disorders and Stroke |
| NNHS | National Nursing Home Survey |
| PAD | peripheral artery disease |
| WHO | World Health Organization |
| YRBSS | Youth Risk Behavior Surveillance System |
See Glossary (Chapter 26) for explanation of terms.
Disease Prevalence
Prevalence is an estimate of how many people have a disease at a given point or period in time. The NCHS conducts health examination and health interview surveys that provide estimates of the prevalence of diseases and risk factors. In this Update, the health interview part of the NHANES is used for the prevalence of CVDs. NHANES is used more than the NHIS because in NHANES, AP is based on the Rose Questionnaire; estimates are made regularly for HF; hypertension is based on BP measurements and interviews; and an estimate can be made for total CVD, including MI, AP, HF, stroke, and hypertension.
A major emphasis of this Statistical Update is to present the latest estimates of the number of people in the United States who have specific conditions to provide a realistic estimate of burden. Most estimates based on NHANES prevalence rates are based on data collected from 2007 to 2010 (in most cases, these are the latest published figures). These are applied to census population estimates for 2010. Differences in population estimates cannot be used to evaluate possible trends in prevalence because these estimates are based on extrapolations of rates beyond the data collection period by use of more recent census population estimates. Trends can only be evaluated by comparing prevalence rates estimated from surveys conducted in different years.
Risk Factor Prevalence
The NHANES 2007 to 2010 data are used in this Update to present estimates of the percentage of people with high lipid values, DM, overweight, and obesity. The NHIS is used for the prevalence of cigarette smoking and physical inactivity. Data for students in grades 9 through 12 are obtained from the YRBSS.
Incidence and Recurrent Attacks
An incidence rate refers to the number of new cases of a disease that develop in a population per unit of time. The unit of time for incidence is not necessarily 1 year, although we often discuss incidence in terms of 1 year. For some statistics, new and recurrent attacks or cases are combined. Our national incidence estimates for the various types of CVD are extrapolations to the US population from the FHS, the ARIC study, and the CHS, all conducted by the NHLBI, as well as the GCNKSS, which is funded by the NINDS. The rates change only when new data are available; they are not computed annually. Do not compare the incidence or the rates with those in past editions of the Heart Disease and Stroke Statistics Update (also known as the Heart and Stroke Statistical Update for editions before 2005). Doing so can lead to serious misinterpretation of time trends.
Mortality
Mortality data are generally presented according to the underlying cause of death. “Any-mention” mortality means that the condition was nominally selected as the underlying cause or was otherwise mentioned on the death certificate. For many deaths classified as attributable to CVD, selection of the single most likely underlying cause can be difficult when several major comorbidities are present, as is often the case in the elderly population. It is useful, therefore, to know the extent of mortality attributable to a given cause regardless of whether it is the underlying cause or a contributing cause (ie, its “any-mention” status). The number of deaths in 2010 with any mention of specific causes of death was tabulated by the NHLBI from the NCHS public-use electronic files on mortality.
The first set of statistics for each disease in this Update includes the number of deaths for which the disease is the underlying cause. Two exceptions are Chapter 9 (High Blood Pressure) and Chapter 19 (Cardiomyopathy and Heart Failure). High BP, or hypertension, increases the mortality risks of CVD and other diseases, and HF should be selected as an underlying cause only when the true underlying cause is not known. In this Update, hypertension and HF death rates are presented in 2 ways: (1) As nominally classified as the underlying cause and (2) as anymention mortality.
National and state mortality data presented according to the underlying cause of death were computed from the mortality tables of the NCHS World Wide Web site, the Health Data Interactive data system of the NCHS, or the CDC compressed mortality file. Any-mention numbers of deaths were tabulated from the electronic mortality files of the NCHS World Wide Web site and from Health Data Interactive.
Population Estimates
In this publication, we have used national population estimates from the US Census Bureau for 2010 in the computation of morbidity data. NCHS population estimates for 2010 were used in the computation of death rate data. The Census Bureau World Wide Web site1 contains these data, as well as information on the file layout.
Hospital Discharges and Ambulatory Care Visits
Estimates of the numbers of hospital discharges and numbers of procedures performed are for inpatients discharged from short-stay hospitals. Discharges include those discharged alive, dead, or with unknown status. Unless otherwise specified, discharges are listed according to the first-listed (primary) diagnosis, and procedures are listed according to all listed procedures (primary plus secondary). These estimates are from the NHDS of the NCHS unless otherwise noted. Ambulatory care visit data include patient visits to physician offices and hospital outpatient departments and EDs. Ambulatory care visit data reflect the first-listed (primary) diagnosis. These estimates are from NAMCS and NHAMCS of the NCHS.
International Classification of Diseases
Morbidity (illness) and mortality (death) data in the United States have a standard classification system: the ICD. Approximately every 10 to 20 years, the ICD codes are revised to reflect changes over time in medical technology, diagnosis, or terminology. Where necessary for comparability of mortality trends across the 9th and 10th ICD revisions, comparability ratios computed by the NCHS are applied as noted.2 Effective with mortality data for 1999, we are using the 10th revision (ICD-10). It will be a few more years before the 10th revision is systematically used for hospital discharge data and ambulatory care visit data, which are based on ICD-9-CM.3
Age Adjustment
Prevalence and mortality estimates for the United States or individual states comparing demographic groups or estimates over time either are age specific or are age adjusted to the 2000 standard population by the direct method.4 International mortality data are age adjusted to the European standard.5 Unless otherwise stated, all death rates in this publication are age adjusted and are deaths per 100 000 population.
Data Years for National Estimates
In this Update, we estimate the annual number of new (incidence) and recurrent cases of a disease in the United States by extrapolating to the US population in 2010 from rates reported in a community- or hospital-based study or multiple studies. Age-adjusted incidence rates by sex and race are also given in this report as observed in the study or studies. For US mortality, most numbers and rates are for 2010. For disease and risk factor prevalence, most rates in this report are calculated from the 2007 to 2010 NHANES. Because NHANES is conducted only in the noninstitutionalized population, we extrapolated the rates to the total US population in 2010, recognizing that this probably underestimates the total prevalence, given the relatively high prevalence in the institutionalized population. The numbers and rates of hospital inpatient discharges for the United States are for 2010. Numbers of visits to physician offices, hospital EDs, and hospital outpatient departments are for 2010. Except as noted, economic cost estimates are for 2010.
Cardiovascular Disease
For data on hospitalizations, physician office visits, and mortality, CVD is defined according to ICD codes given in Chapter 26 of the present document. This definition includes all diseases of the circulatory system, as well as congenital CVD. Unless so specified, an estimate for total CVD does not include congenital CVD. Prevalence of CVD includes people with hypertension, HD, stroke, PAD, and diseases of the veins.
Race
Data published by governmental agencies for some racial groups are considered unreliable because of the small sample size in the studies. Because we try to provide data for as many racial groups as possible, we show these data for informational and comparative purposes.
Contacts
If you have questions about statistics or any points made in this Update, please contact the AHA National Center, Office of Science & Medicine at statistics@heart.org. Direct all media inquiries to News Media Relations at inquiries@heart.org or 214-706-1173.
We do our utmost to ensure that this Update is error free. If we discover errors after publication, we will provide corrections at our World Wide Web site, http://www.heart.org/statistics, and in the journal Circulation.
- 1.US Census Bureau population estimates. Historical data: 2000s. [Accessed October 29, 2012];US Census Bureau Web site. http://www.census.gov/popest/data/historical/2000s/index.html.
- 2.National Center for Health Statistics. Health, United States, 2009, With Special Feature on Medical Technology. Hyattsville, MD: National Center for Health Statistics; 2010. [Accessed October 29, 2012]. http://www.cdc.gov/nchs/data/hus/hus09.pdf. [PubMed] [Google Scholar]
- 3.National Center for Health Statistics, Centers for Medicare and Medicaid Services. [Accessed October 29, 2012];ICD-9-CM Official Guidelines for Coding and Reporting. 2011 http://www.cdc.gov/nchs/data/icd9/icd9cm_guidelines_2011.pdf.
- 4.Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998;47:1–16. 20. [PubMed] [Google Scholar]
- 5.World Health Organization. World Health Statistics Annual. Geneva, Switzerland: World Health Organization; 1998. [Google Scholar]
2. Cardiovascular Health
See Tables 2-1 through 2-8 and Charts 2-1 through 2-13.
Table 2-1.
Definitions of Poor, Intermediate, and Ideal Cardiovascular Health for Each Metric in the AHA 2020 Goals
| Level of Cardiovascular Health for Each Metric
|
|||
|---|---|---|---|
| Poor | Intermediate | Ideal | |
| Current smoking | |||
| Adults ≥20 y of age | Yes | Former ≥12 mo | Never or quit >12 mo |
| Children 12–19 y of age | Tried during the prior 30 d | … | Never tried; never smoked whole cigarette |
| BMI* | |||
| Adults ≥20 y of age | ≥30 kg/m2 | 25–29.9 kg/m2 | <25 kg/m2 |
| Children 2–19 y of age | >95th percentile | 85th–95th percentile | <85th percentile |
| PA | |||
| Adults ≥20 y of age | None | 1–149 min/wk moderate or 1–74 min/wk vigorous or 1–149 min/wk moderate + 2×vigorous | ≥150 min/wk moderate or ≥75 min/wk vigorous or ≥150 min/wk moderate + 2×vigorous |
| Children 12–19 y of age | None | >0 and <60 min of moderate or vigorous every day | ≥60 min of moderate or vigorous every day |
| Healthy diet pattern, No. of components† | |||
| Adults ≥20 y of age | 0–1 | 2–3 | 4–5 |
| Children 5–19 y of age | 0–1 | 2–3 | 4–5 |
| Total cholesterol, mg/dL | |||
| Adults ≥20 y of age | ≥240 | 200–239 or treated to goal | <200 |
| Children 6–19 y of age | ≥200 | 170–199 | <170 |
| Blood pressure | |||
| Adults ≥20 y of age | SBP ≥140 mm Hg or DBP ≥90 mm Hg | SBP 120–139 mm Hg or DBP 80–89 mm Hg or treated to goal | <120 mm Hg/<80 mm Hg |
| Children 8–19 y of age | >95th percentile | 90th–95th percentile or SBP ≥120 mm Hg or DBP ≥80 mm Hg | <90th percentile |
| Fasting plasma glucose, mg/dL | |||
| Adults ≥20 y of age | ≥126 | 100–125 or treated to goal | <100 |
| Children 12–19 y of age | ≥126 | 100–125 | <100 |
AHA indicates American Heart Association; BMI, body mass index; DBP, diastolic blood pressure; ellipses (. . .), data not available; PA, physical activity; and SBP, systolic blood pressure.
Represents appropriate energy balance, that is, appropriate dietary quantity and PA to maintain normal body weight.
In the context of a healthy dietary pattern that is consistent with a Dietary Approaches to Stop Hypertension [DASH]–type eating pattern, to consume ≥4.5 cups/d of fruits and vegetables, ≥2 servings/wk of fish, and ≥3 servings/d of whole grains and no more than 36 oz/wk of sugar-sweetened beverages and 1500 mg/d of sodium.
Table 2-8.
AHA Advocacy and Policy Strategies Related to the 2020 Impact Goals for Ideal Cardiovascular Health
| Measure of Cardiovascular Health | Advocacy/Policy Solutions |
|---|---|
| Smoking status Ideal for cardiovascular health: Adults: Never smoked or quit more than a year ago Children: Never tried or never smoked a whole cigarette |
Federal
|
State
| |
| Physical activity Ideal for cardiovascular health: Adults: At least 150 min of moderate or 75 min of vigorous PA each week Children: >60 min of moderate to vigorous PA per day |
Federal
|
State
| |
| BMI Ideal for cardiovascular health: Adults: between 18.5 and 25 kg/m2 Children: between the 15th and 85th percentile Go to http://www.americanheart.org/obesitypolicy for additional policy resources |
Federal
|
State
| |
| Healthy diet Ideal for cardiovascular health: In the context of a DASH-type dietary pattern, adults and children should achieve at least 4 of the 5 following key components of a healthy diet:
|
Federal
|
State
| |
| Total cholesterol Ideal for cardiovascular health: Adults: Total cholesterol <200 mg/dL Children: <170 mg/dL |
Federal and state
|
| Blood pressure Ideal for cardiovascular health: Adults: <120/80 mm Hg Children: <90th percentile |
Federal
|
State
| |
| Fasting plasma glucose Ideal for cardiovascular health: Children and adults: Fasting blood glucose <100 mg/dL |
Federal and state
|
For AHA advocacy resources, including fact sheets, policy briefs, published papers, and position statements, go to http://www.heart.org/HEARTORG/Advocate/PolicyResources/Policy-Resources_UCM_001135_SubHomePage.jsp. At the time of press of this document, the AHA was in the process of updating its strategic policy agenda for 2014–2017.
AHA indicates American Heart Association; BMI, body mass index; CDC, Centers for Disease Control and Prevention; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension; FDA, US Food and Drug Administration; HD, heart disease; PA, physical activity; PE, physical education; UN, United Nations; and WHO, World Health Organization.
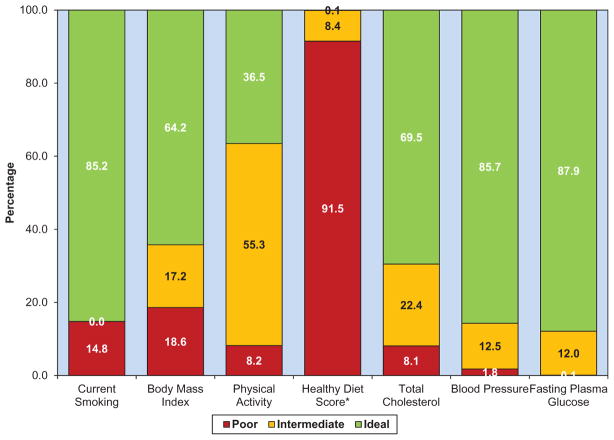
Chart 2-1.
Prevalence (unadjusted) estimates for poor, intermediate, and ideal cardiovascular health for each of the 7 metrics of cardiovascular health in the American Heart Association 2020 goals among US children aged 12 to 19 years, National Health and Nutrition Examination Survey 2009 to 2010.
Chart 2-13.
Incidence of cardiovascular disease according to the number of ideal health behaviors and health factors. Reprinted from Folsom et al7 with permission from Elsevier. Copyright © 2011, American College of Cardiology Foundation.
After achieving its major Impact Goals for 2010, the AHA created a new set of central organizational Impact Goals for the current decade1:
By 2020, to improve the cardiovascular health of all Americans by 20%, while reducing deaths from CVDs and stroke by 20%.1
These goals introduce a new concept, cardiovascular health, which is characterized by 7 health metrics. Ideal cardiovascular health is defined by the absence of clinically manifest CVD together with the simultaneous presence of optimal levels of all 7 metrics, including 4 health behaviors (not smoking and having sufficient PA, a healthy diet pattern, and appropriate energy balance as represented by normal body weight) and 3 health factors (optimal total cholesterol, BP, and fasting blood glucose, in the absence of drug treatment; Table 2-1). Because a spectrum of cardiovascular health can also be envisioned and the ideal cardiovascular health profile is known to be rare in the US population, a broader spectrum of cardiovascular health can also be represented as being “ideal,” “intermediate,” or “poor” for each of the health behaviors and health factors.1 Table 2-1 provides the specific definitions for ideal, intermediate, and poor cardiovascular health for each of the 7 metrics, both for adults (≥20 years of age) and children (age ranges for each metric depending on data availability).
Abbreviations Used in Chapter 2
| AHA | American Heart Association |
| ARIC | Atherosclerosis Risk in Communities Study |
| BMI | body mass index |
| BP | blood pressure |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CDC | Centers for Disease Control and Prevention |
| CHD | coronary heart disease |
| CHF | congestive heart failure |
| CI | confidence interval |
| CVD | cardiovascular disease |
| DASH | Dietary Approaches to Stop Hypertension |
| DBP | diastolic blood pressure |
| DM | diabetes mellitus |
| FDA | Food and Drug Administration |
| HbA1c | hemoglobin A1c |
| HBP | high blood pressure |
| HD | heart disease |
| HF | heart failure |
| HR | hazard ratio |
| ICD | International Classification of Diseases |
| ICD-10 | International Classification of Diseases, 10th Revision |
| MI | myocardial infarction |
| NHANES | National Health and Nutrition Examination Survey |
| NOMAS | Northern Manhattan Study |
| PA | physical activity |
| PE | physical education |
| REGARDS | Reasons for Geographic and Racial Differences in Stroke |
| SBP | systolic blood pressure |
| SE | standard error |
| UN | United Nations |
| WHO | World Health Organization |
This concept of cardiovascular health represents a new focus for the AHA, with 3 central and novel emphases:
An expanded focus on CVD prevention and promotion of positive “cardiovascular health,” in addition to the treatment of established CVD.
Efforts to promote both healthy behaviors (healthy diet pattern, appropriate energy intake, PA, and nonsmoking) and healthy biomarker levels (optimal blood lipids, BP, glucose levels) throughout the lifespan.
Population-level health promotion strategies to shift the majority of the public towards greater cardiovascular health, in addition to targeting those individuals at greatest CVD risk, since healthy lifestyles in all domains are uncommon throughout the US population.
Beginning in 2011, and recognizing the time lag in the nationally representative US data sets, this chapter in the annual Statistical Update evaluates and publishes metrics and information to provide insights into both progress toward meeting the 2020 AHA goals and areas that require greater attention to meet these goals.
Cardiovascular Health: Current Prevalence
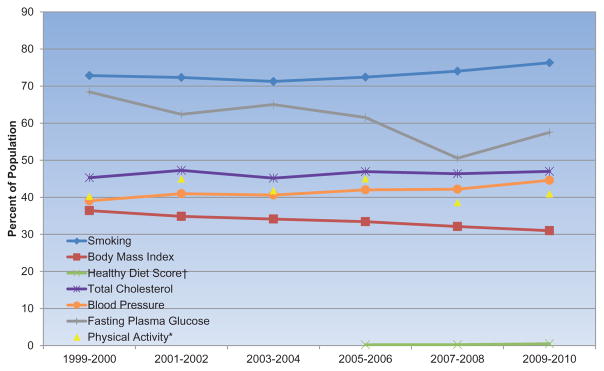
The most up-to-date data on national prevalence of ideal, intermediate, and poor levels of each of the 7 cardiovascular health metrics are shown for adolescents and teens 12 to 19 years of age (Chart 2-1) and for adults ≥20 years of age (Chart 2-2).
For most metrics, the prevalence of ideal levels of health behaviors and health factors is higher in US children than in US adults. Major exceptions are diet and PA, for which prevalence of ideal levels in children is similar to (for PA) or worse (for diet) than in adults.
Among children (Chart 2-1), the prevalence (unadjusted) of ideal levels of cardiovascular health behaviors and factors currently varies from <1% for the healthy diet pattern (ie, <1 in 100 US children meets at least 4 of the 5 dietary components) to >80% for the smoking, BP, and fasting glucose metrics.
Among US adults (Chart 2-2), the age-standardized prevalence of ideal levels of cardiovascular health behaviors and factors currently varies from 0.5% for having at least 4 of 5 components of the healthy diet pattern to up to 76% for never having smoked or being a former smoker who has quit for >12 months.
-
Age-standardized and age-specific prevalence estimates for ideal cardiovascular health and for ideal levels of each of its components are shown for 2007 to 2008 (baseline) and 2009 to 2010 in Table 2-2.
In 2009 to 2010, the prevalence of ideal levels across 7 health factors and health behaviors decreased dramatically from younger to older age groups. The same trend was seen in 2007 to 2008.
The prevalence of both children and adults meeting the dietary goals appeared to improve between 2007 to 2008 and 2009 to 2010, although this improvement should be viewed with caution given the challenges of accurately determining time trends across only 2 cycles of NHANES data collection. The improvement was attributable to the greater numbers of children and adults who met the whole grains goal, greater numbers of middle-aged and older adults who met the fruits and vegetables goal, and greater numbers of adults who met the fish goal.
-
Chart 2-3 displays the prevalence estimates for the population of US children (12–19 years of age) meeting different numbers of criteria for ideal cardiovascular health (out of 7 possible) in 2009 to 2010.
Few US children (<7%) meet only 0, 1, or 2 criteria for ideal cardiovascular health.
Nearly half of US children (45%) meet 3 or 4 criteria for ideal cardiovascular health, and about half meet 5 or 6 criteria (mostly 5 criteria).
Virtually no children meet all 7 criteria for ideal cardiovascular health.
Overall distributions are similar in boys and girls.
-
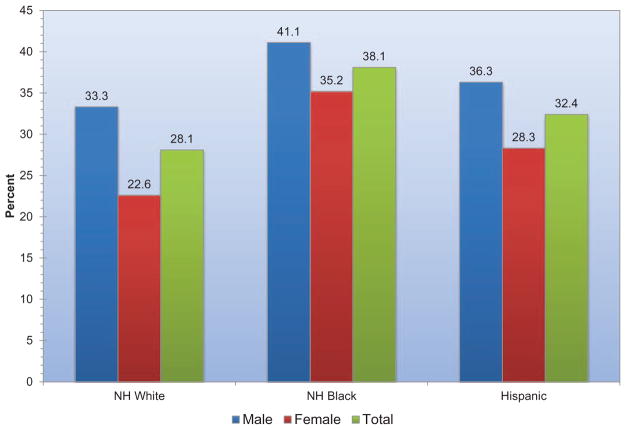
Charts 2-4 and 2-5 display the age-standardized prevalence estimates of US adults meeting different numbers of criteria for ideal cardiovascular health (out of 7 possible) in 2009 to 2010, overall and stratified by age, sex, and race.
Approximately 2% of US adults have 0 of the 7 criteria at ideal levels, and another 12% meet only 1 of 7 criteria. This is much worse than among children.
Most US adults (≥65%) have 2, 3, or 4 criteria at ideal cardiovascular health, with ≈1 in 5 adults within each of these categories.
Approximately 13% of US adults meet 5 criteria, 4% meet 6 criteria, and 0.1% meet 7 criteria at ideal levels.
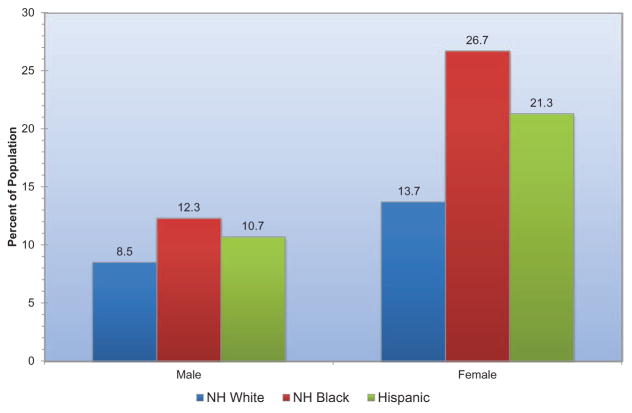
Presence of ideal cardiovascular health is both age and sex related (Chart 2-4). Younger adults are more likely to meet greater numbers of ideal metrics than are older adults. More than 60% of Americans >60 years of age have ≤2 metrics at ideal levels. At any age, women tend to have more metrics at ideal levels than do men.
Race is also related to presence of ideal cardiovascular health (Chart 2-5). Blacks and Mexican Americans tend to have fewer metrics at ideal levels than whites or other races. Approximately 6 in 10 white adults and 7 in 10 black or Mexican American adults have no more than 3 of 7 metrics at ideal levels.
-
Chart 2-6 displays the age-standardized percentages of US adults and percentages of children who have ≥5 of the metrics (out of 7 possible) at ideal levels.
Approximately 50% of US children 12 to 19 years of age have ≥5 metrics at ideal levels, with lower prevalence in girls (46%) than in boys (51%).
In comparison, only 17% of US adults have ≥5 metrics with ideal levels, with lower prevalence in men (11%) than in women (24%).
Among adults, whites are more likely to have ≥5 metrics at ideal levels (19%) than are Mexican Americans (12%) or blacks (10%).
-
Chart 2-7 displays the age-standardized percentages of US adults meeting different numbers of criteria for both poor and ideal cardiovascular health. Meeting the AHA 2020 Strategic Impact Goals is predicated on reducing the relative percentage of those with poor levels while increasing the relative percentage of those with ideal levels for each of the 7 metrics.
Approximately 92% of US adults have ≥1 metric at poor levels.
Approximately 35% of US adults have ≥3 metrics at poor levels.
Few US adults (<3%) have ≥5 metrics at poor levels.
More US adults have 4 to 6 ideal metrics than 4 to 6 poor metrics.
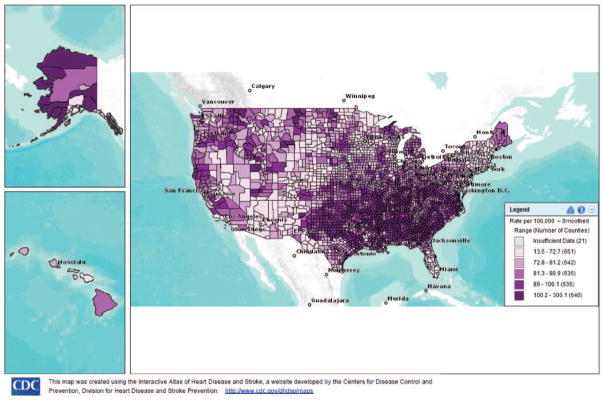
Using data from the BRFSS, Fang and colleagues2 estimated the prevalence of ideal cardiovascular health by state, which ranged from 1.2% (Oklahoma) to 6.9% (District of Columbia). Southern states tended to have higher rates of poor cardiovascular health, lower rates of ideal cardiovascular health, and lower mean cardiovascular health scores than New England and Western states (Chart 2-8).
-
The prevalence of poor health behaviors and health factors and their awareness, treatment, and control are displayed in Table 2-3 separately for those with and without self-reported CVD.
Americans with CVD are much more likely to be current or former smokers than Americans without CVD.
Approximately 20% of US adults are current smokers or have quit recently (<12 months ago).
As measured by self-reported data, Americans with CVD are very likely to have intermediate or poor levels of PA (74.1%), whereas Americans without CVD still commonly have such levels (58.4%). Furthermore, 64.5% of those with CVD and 47.3% of those without CVD report engaging in no moderate or vigorous activity at all.
Seventy percent of US adults with CVD and 79% of those without CVD meet 0 or only 1 of the 5 healthy diet metrics.
Two thirds of US adults are overweight, with little difference by prevalent CVD. Half of all US adults with CVD and one third without CVD are obese.
Hypertension is present in 28.5% of US adults without CVD and 51.0% of US adults with CVD. Of these, nearly all with CVD are aware of their hypertension (98.6%) and are receiving treatment (97.4%), but a much smaller proportion of those without CVD are aware (70.6%) or receiving treatment (61.4%).
Both presence of hypercholesterolemia (total cholesterol ≥240 mg/dL or receiving medication) and DM (fasting glucose ≥126 mg/dL or receiving medications) and awareness and treatment of these conditions are similarly higher among those with CVD than among those without CVD.
Chart 2-2.
Age-standardized prevalence estimates for poor, intermediate, and ideal cardiovascular health for each of the 7 metrics of cardiovascular health in the American Heart Association 2020 goals among US adults aged ≥20 years, National Health and Nutrition Examination Survey 2009 to 2010.
Table 2-2.
Prevalence of Ideal Cardiovascular Health and its Components in the US Population, Overall and in Selected Age Strata From NHANES 2007 to 2008 and 2009 to 2010
| Prevalence, %
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Ages 12–19 y, 2007–2008 | Ages 12–19 y, 2009–2010 | Ages ≥20 y,* 2007–2008 | Ages ≥20 y,* 2009–2010 | Ages 20–39 y, 2007–2008 | Ages 20–39 y, 2009–2010 | Ages 40–59 y, 2007–2008 | Ages 40–59 y, 2009–2010 | Ages ≥60 y, 2007–2008 | Ages ≥60 y, 2009–2010 | |
| Ideal cardiovascular health profile (composite–all 7) | 0.0 | 0.0 | 0.0 | 0.1 | 0.0 | 0.3 | 0.0 | 0.0 | 0.0 | 0.0 |
| ≥6 Ideal cardiovascular health composite score | 8.2 | 18.4 | 3.6 | 4.5 | 7.1 | 7.8 | 2.1 | 2.9 | 0.1 | 0.8 |
| ≥5 Ideal cardiovascular health composite score | 39.8 | 48.5 | 15.8 | 17.2 | 29.7 | 29.3 | 9.7 | 11.1 | 2.9 | 5.8 |
| Ideal health factors index (composite–all 4) | 35.5 | 48.4 | 13.9 | 15.8 | 27.7 | 29.5 | 7.3 | 9.2 | 1.0 | 2.4 |
| Total cholesterol <200 mg/dL (untreated) | 69.6 | 69.5 | 46.3 | 47.0 | 64.1 | 67.1 | 37.1 | 36.5 | 29.9 | 29.6 |
| SBP <120 mm Hg and DBP <80 mm Hg (untreated) | 82.3 | 85.7 | 43.8 | 44.6 | 63.8 | 65.2 | 36.9 | 40.5 | 14.6 | 15.8 |
| Not current smoker (never or quit ≥12 mo) | 83.7 | 85.2 | 72.9 | 76.3 | 66.4 | 69.7 | 72.9 | 75.5 | 86.1 | 88.3 |
| Fasting blood glucose <100 mg/dL | 76.2 | 87.9 | 52.0 | 57.5 | 67.4 | 74.0 | 45.6 | 54.0 | 31.9 | 35.4 |
| Ideal health behaviors index (composite–all 4) | 0.0 | 0.0 | 0.1 | 0.2 | 0.1 | 0.6 | 0.0 | 0.0 | 0.0 | 0.0 |
| PA at goal | 39.0 | 36.5 | 39.5 | 40.9 | 45.6 | 45.9 | 36.4 | 41.0 | 33.7 | 33.0 |
| Not current smoker (never or quit ≥12 mo) | 83.7 | 85.2 | 72.9 | 76.3 | 66.4 | 69.7 | 72.9 | 75.5 | 86.1 | 88.3 |
| BMI <25 kg/m2 | 62.5 | 64.2 | 31.9 | 31.0 | 39.1 | 37.7 | 28.0 | 27.7 | 25.3 | 25.3 |
| 4–5 Diet goals met† | 0.0 | 0.1 | 0.3 | 0.5 | 0.3 | 0.7 | 0.1 | 0.5 | 0.5 | 0.3 |
| Fruits and vegetables ≥4.5 cups/d | 7.9 | 7.6 | 12.3 | 13.7 | 11.7 | 11.5 | 11.4 | 13.7 | 15.8 | 17.0 |
| Fish ≥2 3.5-oz servings/wk | 9.2 | 8.5 | 18.3 | 23.7 | 16.8 | 21.9 | 19.7 | 24.4 | 19.4 | 26.0 |
| Sodium <1500 mg/d | 0.0 | 0.2 | 0.6 | 0.2 | 0.6 | 0.2 | 0.8 | 0.3 | 0.3 | 0.3 |
| Sugar-sweetened beverages <36 oz/wk | 32.0 | 29.5 | 51.9 | 55.5 | 41.0 | 42.7 | 54.6 | 58.2 | 71.2 | 73.5 |
| Whole grains (≥1.1 g of fiber per 10 g of carbohydrates) ≥3 1-oz equivalents/d | 3.2 | 5.8 | 7.3 | 11.2 | 7.0 | 11.2 | 7.1 | 10.4 | 8.4 | 11.9 |
| Secondary dietary metrics | ||||||||||
| Nuts, legumes, seeds ≥4 servings/wk | 8.7 | 12.2 | 21.7 | 23.6 | 19.6 | 21.3 | 22.5 | 25.4 | 24.7 | 24.8 |
| Processed meats <2 servings/wk | 56.3 | 53.2 | 57.6 | 58.0 | 54.0 | 54.7 | 59.7 | 58.7 | 61.1 | 62.3 |
| Saturated fat <7% of total energy intake (kcal) | 4.5 | 8.1 | 8.7 | 11.7 | 9.3 | 13.5 | 8.0 | 10.2 | 9.0 | 11.3 |
BMI indicates body mass index; DBP, diastolic blood pressure; NHANES, National Health and Nutrition Examination Survey; PA, physical activity; and SBP, systolic blood pressure.
Standardized to the age distribution of the 2000 US Standard population, except for dietary metrics.
Scaled for 2000 kcal/d and in the context of appropriate energy balance and a DASH (Dietary Approaches to Stop Hypertension)–type eating pattern.
Chart 2-3.
Proportion (unadjusted) of US children aged 12 to 19 years meeting different numbers of criteria for ideal cardiovascular health, overall and by sex, National Health and Nutrition Examination Survey 2009 to 2010.
Chart 2-4.
Age-standardized prevalence estimates of US adults aged ≥20 years meeting different numbers of criteria for ideal cardiovascular health, overall and by age and sex subgroups, National Health and Nutrition Examination Survey 2009 to 2010.
Chart 2-5.
Age-standardized prevalence estimates of US adults aged ≥20 years meeting different numbers of criteria for ideal cardiovascular health, overall and in selected race subgroups from National Health and Nutrition Examination Survey 2009 to 2010.
Chart 2-6.
Prevalence estimates of meeting ≥5 criteria for ideal cardiovascular health among US adults aged ≥20 years (age standardized), overall and by sex and race, and US children aged 12 to 19 years (unadjusted), by sex, National Health and Nutrition Examination Survey 2009 to 2010.
Chart 2-7.
Age-standardized prevalence estimates of US adults meeting different numbers of criteria for ideal and poor cardiovascular health for each of the 7 metrics of cardiovascular health in the American Heart Association 2020 goals, among US adults aged ≥20 years, National Health and Nutrition Examination Survey 2009 to 2010.
Chart 2-8.
Age-standardized cardiovascular health status by US states, Behavioral Risk Factor Surveillance System, 2009. A, Age-standardized prevalence of population with ideal cardiovascular health by states. B, Age-standardized percentage of population with 0 to 2 cardiovascular health metrics by states. C, Age-standardized mean score of cardiovascular health metrics by states. Reprinted from Fang et al2 with permission. Copyright © 2012, American Heart Association, Inc.
Table 2-3.
Selected Secondary Metrics for Monitoring CVD, NHANES 2009 to 2010
| In the Presence of CVD
|
In the Absence of CVD
|
|||
|---|---|---|---|---|
| No.* | % (SE)† | No.* | % (SE)† | |
| Total | 16 209 474 | 7.2 (0.4) | 199 590 596 | 92.8 (0.4) |
| CHD | 6 916 012 | 3.2 (0.3) | ||
| Stroke | 5 717 759 | 2.7 (0.2) | ||
| CHF | 4 320 227 | 2.0 (0.3) | ||
| Acute MI | 6 929 905 | 3.2 (0.3) | ||
| Health behaviors | ||||
| Smoking | ||||
| Current smoker or smokers who quit <12 mo ago | 3 127 273 | 37.2 (4.9) | 40 760 066 | 20.1 (0.9) |
| PA | ||||
| PA: intermediate or poor‡ | 11 813 011 | 74.1 (5.1) | 115 561 988 | 58.4 (1.5) |
| PA: none | 10 598 908 | 64.5 (5.5) | 93 459 556 | 47.3 (1.2) |
| Diet, No. of metrics | ||||
| Total diet score 0–3 of 5 | 12 665 860 | 100.0 (0.00) | 161 370 154 | 99.7 (0.11) |
| Total diet score 0–1 of 5 | 9 540 532 | 70.1 (4.69) | 127 156 293 | 78.8 (1.42) |
| Overweight/obesity | ||||
| Overweight or obese (BMI ≥25.0 kg/m2) | 12 621 701 | 69.4 (4.1) | 134 879 713 | 68.1 (1.3) |
| Obese (BMI ≥30.0 kg/m2) | 7 763 611 | 49.0 (5.2) | 68 655 702 | 34.7 (1.0) |
| Health factors | ||||
| Hypertension | ||||
| Prevalence of BP ≥140/90 mm Hg or taking medications | 10 591 170 | 51.0 (5.0) | 53 523 895 | 28.5 (0.9) |
| Awareness among those with hypertension | 10 071 343 | 98.6 (0.3) | 42 436 782 | 70.6 (3.2) |
| Treatment those with hypertension | 9 819 244 | 97.4 (0.4) | 39 194 948 | 61.4 (2.9) |
| BP control to <140/<90 mm Hg among treated | 6 886 176 | 64.2 (9.5) | 27 323 649 | 72.4 (2.4) |
| BP control to <140/<90 mm Hg among hypertensive | 6 886 176 | 62.3 (9.4) | 27 323 649 | 43.3 (2.8) |
| Hypercholesterolemia | ||||
| Prevalence of total cholesterol ≥240 mg/dL or taking medications | 8 201 829 | 37.1 (4.2) | 48 701 198 | 25.7 (0.7) |
| Awareness among those with hypercholesterolemia | 7 742 127 | 84.6 (8.0) | 35 174 931 | 59.9 (2.6) |
| Treatment among those with hypercholesterolemia | 7 219 078 | 79.3 (8.5) | 25 405 334 | 38.7 (2.4) |
| Cholesterol control to <200 mg/dL among treated | 6 659 732 | 95.0 (1.4) | 22 804 724 | 90.4 (1.2) |
| Cholesterol control to <200 mg/dL among hypercholesterolemia | 6 659 732 | 75.0 (8.9) | 22 804 724 | 34.7 (2.4) |
| Diabetes mellitus | ||||
| Prevalence of fasting glucose ≥125 mg/dL or taking medications | 4 769 759 | 15.2 (2.2) | 21 078 443 | 10.3 (1.1) |
| Awareness among diabetics | 4 006 153 | 90.4 (2.3) | 14 242 760 | 64.3 (4.6) |
| Treatment among diabetics | 3 935 446 | 87.1 (3.2) | 13 391 291 | 58.4 (5.3) |
| Blood glucose control among treated | 1 527 151 | 32.6 (9.9) | 5 878 676 | 45.0 (8.0) |
| Blood glucose control among diabetics | 1 527 151 | 27.2 (8.7) | 5 878 676 | 25.5 (5.9) |
BMI indicates body mass index; BP, blood pressure; CHD, coronary heart disease; CHF, congestive heart failure; CVD, cardiovascular disease; MI, myocardial infarction; NHANES, National Health and Nutrition Examination Survey; PA, physical activity; and SE, standard error.
Weighted sample size.
Standardized to the age distribution of the 2000 US Standard population.
Moderate <150 min/wk AND Vigorous <75 min/wk AND Combined <150 min/wk.
Cardiovascular Health: Trends Over Time
-
The trends over the past decade in each of the 7 cardiovascular health metrics (for diet, trends from 2005–2006 to 2009–2010) are shown in Chart 2-9 (for children 12–19 years of age) and Chart 2-10 (for adults ≥20 years of age).
Fewer children over time are meeting the BMI metric, whereas more are meeting the smoking and total cholesterol metrics. Other metrics do not show consistent trends over time in children.
More adults over time are meeting the smoking metric, whereas fewer are meeting the BMI and glucose metrics. Trends for other metrics are not evident over time in adults.
On the basis of NHANES data from 1988 to 2008, if current trends continue, estimated cardiovascular health is projected to improve by 6% between 2010 and 2020, short of the AHA’s goal of 20% improvement (Chart 2-11).3 On the basis of current trends among individual metrics, anticipated declines in prevalence of smoking, high cholesterol, and high BP (in men) would be offset by substantial increases in the prevalence of obesity and DM and small changes in ideal dietary patterns or PA.3
On the basis of these projections in cardiovascular health factors and behaviors, CHD deaths are projected to decrease by 30% between 2010 and 2020 because of projected improvements in total cholesterol, SBP, smoking and PA (≈167 000 fewer deaths), offset by increases in DM and BMI (≈24 000 more deaths).4
Chart 2-9.
Trends in prevalence (unadjusted) of meeting criteria for ideal cardiovascular health for each of the 7 metrics of cardiovascular health in the American Heart Association 2020 goals among US children aged 12 to 19 years, National Health and Nutrition Examination Survey (NHANES) 1999 to 2000 through 2009 to 2010. *Because of changes in the physical activity questionnaire between different cycles of the NHANES survey, trends over time for this indicator should be interpreted with caution and statistical comparisons should not be attempted. †Data for the Healthy Diet Score, based on a 2-day average intake, were only available for the 2005 to 2006, 2007 to 2008, and 2009 to 2010 NHANES cycles at the time of this analysis.
Chart 2-10.
Age-standardized trends in prevalence of meeting criteria for ideal cardiovascular health for each of the 7 metrics of cardiovascular health in the American Heart Association 2020 goals among US adults aged ≥20 years, National Health and Nutrition Examination Survey (NHANES) 1999 to 2000 through 2009 to 2010. *Because of changes in the physical activity questionnaire between different cycles of the NHANES survey, trends over time for this indicator should be interpreted with caution and statistical comparisons should not be attempted. †Data for the Healthy Diet Score, based on a 2-day average intake, were only available for the 2005 to 2006, 2007 to 2008, and 2009 to 2010 NHANES cycles at the time of this analysis.
Chart 2-11.
Prevalence of ideal, intermediate, and poor cardiovascular health metrics in 2006 (American Heart Association 2020 Impact Goals baseline year) and 2020 projections assuming current trends continue. The 2020 targets for each cardiovascular health metric assume a 20% relative increase in ideal cardiovascular health prevalence metrics and a 20% relative decrease in poor cardiovascular health prevalence metrics for men and women. Reprinted from Huffman et al3 with permission. Copyright © 2012, American Heart Association, Inc.
Cardiovascular Diseases
-
In 2010, the age-standardized death rate attributable to all CVD was 236.6 per 100 000 (includes congenital CVD [ICD-10 I00-I99, Q20-Q28]; Chart 2-12), down 8.8% from 259.4 per 100 000 in 2007 (baseline data for the 2020 Impact Goals on CVD and stroke mortality).5
Death rates in 2010 attributable to stroke, CHD, and other CVDs were 39.1, 113.6, and 82.7 per 100 000, respectively.5
Data from NHANES 2009 to 2010 reveal that overall, 7.2% of Americans self-reported having some type of CVD (Table 2-3), including 3.2% with CHD, 2.7% with stroke, and 2.0% with CHF (some individuals reported >1 condition).
Chart 2-12.
US age-standardized death rates* attributable to CVD, 2000 to 2010. *Directly standardized to the age distribution of the 2000 US standard population. †Total CVD: International Classification of Diseases, 10th Revision (ICD-10) I00 to I99 and Q20 to Q28. §Stroke (all cerebrovascular disease): ICD-10 I60 to I69. ¶CHD: ICD-10 I20 to I25. **Other CVD: ICD-10 I00 to I15, I26 to I51, I70 to I78, I80 to I89, and I95 to I99. CHD indicates coronary heart disease; and CVD, cardiovascular disease. Source: Centers for Disease Control and Prevention, National Center for Health Statistics.5
Relevance of Ideal Cardiovascular Health
Since the AHA announced its 2020 Impact Goals, multiple investigations have confirmed the importance of these metrics of cardiovascular health. Overall, these data demonstrate the relevance of the concept of cardiovascular health to the risk of future risk factors, disease, and mortality, including a strong inverse, stepwise association with all-cause, CVD, and ischemic HD mortality.
Bambs et al,6 Folsom et al,7 and Dong et al8 have all described the low prevalence (<1%) of ideal cardiovascular health, defined as being in the ideal category of all 7 AHA metrics in the Heart Strategies Concentrating on Risk Evaluation, ARIC, and NOMAS cohorts, respectively.
In ARIC and NOMAS, a stepwise inverse association was present between the number of ideal health metrics and incident CVD events (including CHD death, nonfatal MI, stroke, and HF) during 20 and 11 years of follow-up, respectively.7,8 For ARIC participants with 0, 1, 2, 3, 4, 5, 6, and 7 metrics at ideal levels, the age-, sex-, and race-adjusted rates of incident CVD incidence were 3.21, 2.19, 1.60, 1.20, 0.86, 0.64, 0.39, and 0 per 100 person-years, respectively.7 Findings were similar in the Aerobics Center Longitudinal Study, in which individuals with 6 to 7 ideal metrics had a 63% lower risk of CVD death (HR [95% CI], 0.37 [0.15, 0.95]) compared with individuals with 0 to 2 ideal metrics.9
A similar stepwise association was present between the number of ideal cardiovascular health metrics and risk of all-cause mortality, CVD mortality, and ischemic HD mortality after 14.5 years of follow-up based on NHANES 1988 to 2006 data.10 The HRs for individuals with 6 or 7 ideal health metrics compared with individuals with 0 ideal health metrics were 0.49 (95% CI, 0.33–0.74) for all-cause mortality, 0.24 (95% CI, 0.13–0.47) for CVD mortality, and 0.30 (95% CI, 0.13–0.68) for ischemic HD mortality.10 Ford et al11 demonstrated similar relationships.
-
The adjusted population attributable fractions for CVD mortality were as follows10:
40.6% (95% CI, 24.5%–54.6%) for HBP
13.7% (95% CI, 4.8%–22.3%) for smoking
13.2% (95% CI, 3.5%–29.2%) for poor diet
11.9% (95% CI, 1.3%–22.3%) for insufficient PA
8.8% (95% CI, 2.1%–15.4%) for abnormal glucose levels
-
The adjusted population attributable fractions for ischemic HD mortality were as follows10:
34.7% (95% CI, 6.6%–57.7%) for HBP
16.7% (95% CI, 6.4%–26.6%) for smoking
20.6% (95% CI, 1.2%–38.6%) for poor diet
7.8% (95% CI, 0%–22.2%) for insufficient PA
7.5% (95% CI, 3.0%–14.7%) for abnormal glucose levels
Data from the Cardiovascular Lifetime Risk Pooling Project indicate that adults with all-optimal risk factor levels (similar to having ideal cardiovascular health factor levels of cholesterol, blood sugar, and BP, as well as nonsmoking status) have substantially longer overall and CVD-free survival than those who have poor levels of ≥1 of these cardiovascular health factor metrics. For example, at an index age of 45 years, men with optimal risk factor profiles lived on average 14 years longer free of all CVD events, and ≈12 years longer overall, than individuals with ≥2 risk factors.12
Importantly, in many of these analyses, ideal health behaviors and ideal health factors were each independently associated with lower CVD risk in a stepwise fashion (Chart 2-13). Thus, across any levels of health behaviors, health factors were still associated with incident CVD, and across any levels of health factors, health behaviors were still associated with incident CVD.
Interestingly, based on NHANES 1999 to 2002, only modest intercorrelations are present between different cardiovascular health metrics. For example, these ranged from a correlation of −0.12 between PA and HbA1c to a correlation of 0.29 between BMI and HbA1c. Thus, although the 7 AHA cardiovascular health metrics appear modestly interrelated, substantial independent variation in each exists, and each is independently related to cardiovascular outcomes.11
The AHA metrics may also be related to risk of noncardiovascular conditions. Rasmussen-Torvik et al13 demonstrated a graded, inverse association between ideal cardiovascular health and cancer incidence, with 51% lower risk among individuals with 6 or 7 ideal cardiovascular health metrics than among those with 0 ideal metrics. These results were only partially attenuated (25% lower risk) when smoking was removed from the sum of metrics. In contrast, Artero et al9 did not find a significant association between ideal cardiovascular health and death attributable to cancer in the Aerobics Center Longitudinal Study. The AHA cardiovascular health metrics have also been cross-sectionally associated with lower prevalence of depressive symptoms in the REGARDS cohort.14
Recent analyses from the US Burden of Disease Collaborators demonstrated that each of the 7 health factors and behaviors causes substantial mortality and morbidity in the United States. The top risk factor related to overall disease burden was suboptimal diet, followed by tobacco smoking, high BMI, HBP, high fasting plasma glucose, and physical inactivity.14a
Achieving the 2020 Impact Goals
Taken together, these data continue to demonstrate both the tremendous relevance of the AHA 2020 Impact Goals for cardiovascular health and the substantial progress that will be needed to achieve these goals over the next decade.
-
A range of complementary strategies and approaches can lead to improvements in cardiovascular health. These include each of the following:
Individual-focused approaches, which target lifestyle and treatments at the individual level (Table 2-4)
Healthcare systems approaches, which encourage, facilitate, and reward efforts by providers to improve health behaviors and health factors (Table 2-5)
Population approaches, which target lifestyle and treatments in schools or workplaces, local communities, and states, as well as throughout the nation (Table 2-6)
Such approaches can focus on both (1) improving cardiovascular health among those who currently have less than optimal levels and (2) preserving cardiovascular health among those who currently have ideal levels (in particular, children, adolescents, and young adults) as they age.
The metrics with the greatest potential for improvement are health behaviors, including diet quality, PA, and body weight. However, each of the cardiovascular health metrics can be improved and deserves major focus.
Continued emphasis is also needed on the treatment of acute CVD events and secondary prevention through treatment and control of health behaviors and risk factors.
For each cardiovascular health metric, modest shifts in the population distribution toward improved health would produce relatively large increases in the proportion of Americans in both ideal and intermediate categories. For example, on the basis of NHANES 2009 to 2010, the current prevalence of ideal levels of BP among US adults is 44.3%. To achieve the 2020 goals, a 20% relative improvement would require an increase in this proportion to 53.1% by 2020 (44.3% × 1.20). On the basis of NHANES data, a reduction in population mean BP of just 2 mm Hg would result in 56.1% of US adults having ideal levels of BP, which represents a 26.8% relative improvement in this metric (Table 2-7). Larger population reductions in BP would lead to even larger numbers of people with ideal levels. Such small reductions in population BP could result from small health behavior changes at a population level, such as increased PA, increased fruit and vegetable consumption, decreased sodium intake, decreased adiposity, or some combination of these and other lifestyle changes, with resulting substantial projected decreases in CVD rates in US adults.15
The AHA has a broad range of policy initiatives to improve cardiovascular health and meet the 2020 Strategic Impact Goals (Table 2-8). Future Statistical Updates will update these initiatives and track progress toward the 2020 Impact Goals.
Table 2-4.
Evidence-Based Individual Approaches for Improving Health Behaviors and Health Factors in the Clinic Setting
|
Examples of approaches include mastery experiences (set a reasonable, proximal goal that the person can successfully achieve); vicarious experiences (have the person see someone with similar capabilities performing the behavior, such as walking on a treadmill or preparing a healthy meal); physiological feedback (explain to the patient when a change in their symptoms is related to worse or improved behaviors); and verbal persuasion (persuade the person that you believe in their capability to perform the behavior).
Motivational interviewing represents use of individual counseling to explore and resolve ambivalence toward changing behavior. Major principles include fostering the person’s own awareness and resolution of their ambivalence, as well as their own self-motivation to change, in a partnership with the counselor or provider.
Modified from Artinian et al16 with permission. Copyright © 2010, American Heart Association, Inc.
Table 2-5.
Evidence-Based Healthcare Systems Approaches to Support and Facilitate Improvements in Health Behaviors and Health Factors17–21
|
BP indicates blood pressure; and PA, physical activity.
Table 2-6.
Summary of Evidence-Based Population Approaches for Improving Diet, Increasing Physical Activity, and Reducing Tobacco Use*
| Diet | |
| Media and education | Sustained, focused media and educational campaigns, using multiple modes, for increasing consumption of specific healthful foods or reducing consumption of specific less healthful foods or beverages, either alone (IIa B) or as part of multicomponent strategies (I B)†‡§ |
| On-site supermarket and grocery store educational programs to support the purchase of healthier foods (IIa B)† | |
| Labeling and information | Mandated nutrition facts panels or front-of-pack labels/icons as a means to influence industry behavior and product formulations (IIa B)† |
| Economic incentives | Subsidy strategies to lower prices of more healthful foods and beverages (I A)† |
| Tax strategies to increase prices of less healthful foods and beverages (IIa B)† | |
| Changes in both agricultural subsidies and other related policies to create an infrastructure that facilitates production, transportation, and marketing of healthier foods, sustained over several decades (IIa B)† | |
| Schools | Multicomponent interventions focused on improving both diet and physical activity, including specialized educational curricula, trained teachers, supportive school policies, a formal PE program, healthy food and beverage options, and a parental/family component (I A)† |
| School garden programs, including nutrition and gardening education and hands-on gardening experiences (IIa A)† | |
| Fresh fruit and vegetable programs that provide free fruits and vegetables to students during the school day (IIa A)† | |
| Workplaces | Comprehensive worksite wellness programs with nutrition, physical activity, and tobacco cessation/prevention components (IIa A)† |
| Increased availability of healthier food/beverage options and/or strong nutrition standards for foods and beverages served, in combination with vending machine prompts, labels, or icons to make healthier choices (IIa B)† | |
| Local environment | Increased availability of supermarkets near homes (IIa B)†‡|| |
| Restrictions and mandates | Restrictions on television advertisements for less healthful foods or beverages advertised to children (I B)† |
| Restrictions on advertising and marketing of less healthful foods or beverages near schools and public places frequented by youths (IIa B)† | |
| General nutrition standards for foods and beverages marketed and advertised to children in any fashion, including on-package promotion (IIa B)† | |
| Regulatory policies to reduce specific nutrients in foods (eg, trans fats, salt, certain fats) (I B)†§ | |
| Physical activity | |
| Labeling and information | Point-of-decision prompts to encourage use of stairs (IIa A)† |
| Economic incentives | Increased gasoline taxes to increase active transport/commuting (IIa B)† |
| Schools | Multicomponent interventions focused on improving both diet and physical activity, including specialized educational curricula, trained teachers, supportive school policies, a formal PE program, serving of healthy food and beverage options, and a parental/family component (IIa A)† |
| Increased availability and types of school playground spaces and equipment (I B)† | |
| Increased number of PE classes, revised PE curricula to increase time in at least moderate activity, and trained PE teachers at schools (IIa A/IIb A¶)† | |
| Regular classroom physical activity breaks during academic lessons (IIa A)†§ | |
| Workplaces | Comprehensive worksite wellness programs with nutrition, physical activity, and tobacco cessation/prevention components (IIa A)† |
| Structured worksite programs that encourage activity and also provide a set time for physical activity during work hours (IIa B)† | |
| Improving stairway access and appeal, potentially in combination with “skip-stop” elevators that skip some floors (IIa B)† | |
| Adding new or updating worksite fitness centers (IIa B)† | |
| Local environment | Improved accessibility of recreation and exercise spaces and facilities (eg, building of parks and playgrounds, increasing operating hours, use of school facilities during nonschool hours) (IIa B)† |
| Improved land-use design (eg, integration and interrelationships of residential, school, work, retail, and public spaces) (IIa B)† | |
| Improved sidewalk and street design to increase active commuting (walking or bicycling) to school by children (IIa B)† | |
| Improved traffic safety (IIa B)† | |
| Improved neighborhood aesthetics (to increase activity in adults) (IIa B)† | |
| Improved walkability, a composite indicator that incorporates aspects of land-use mix, street connectivity, pedestrian infrastructure, aesthetics, traffic safety, and/or crime safety (IIa B)† | |
| Smoking | |
| Media and education | Sustained, focused media and educational campaigns to reduce smoking, either alone (IIa B) or as part of larger multicomponent population-level strategies (I A)† |
| Labeling and information | Cigarette package warnings, especially those that are graphic and health related (I B)†‡§ |
| Economic incentives | Higher taxes on tobacco products to reduce use and fund tobacco control programs (I A)†‡§ |
| Schools and workplaces | Comprehensive worksite wellness programs with nutrition, physical activity, and tobacco cessation/prevention components (IIa A)† |
| Local environment | Reduced density of retail tobacco outlets around homes and schools (I B)† |
| Development of community telephone lines for cessation counseling and support services (I A)† | |
| Restrictions and mandates | Community (city, state, or federal) restrictions on smoking in public places (I A)† |
| Local workplace-specific restrictions on smoking (I A)†‡§ | |
| Stronger enforcement of local school-specific restrictions on smoking (IIa B)† | |
| Local residence-specific restrictions on smoking (IIa B)†§ | |
| Partial or complete restrictions on advertising and promotion of tobacco products (I B)† | |
PE indicates physical education.
The specific population interventions listed here are either a Class I or IIa recommendation with an evidence grade of either A or B. The American Heart Association evidence grading system for class of recommendation and level of evidence is summarized in Table 2. Because implementation of population-level strategies does not require perfect evidence but rather consideration of risks versus benefits, associated costs, and alternate approaches, the absence of any specific strategy herein does not mean it should not also be considered for implementation. See the more detailed tables and text below for further information on the evidence for each of these interventions, as well as other strategies that were reviewed.
At least some evidence from studies conducted in high-income Western regions and countries (eg, North America, Europe, Australia, New Zealand).
At least some evidence from studies conducted in high-income non-Western regions and countries (eg, Japan, Hong Kong, South Korea, Singapore).
At least some evidence from studies conducted in low- or middle-income regions and countries (eg, Africa, China, Pakistan, India).
Based on cross-sectional studies only; only 2 longitudinal studies have been performed, with no significant relations seen.
Evidence IIa A for improving physical activity; evidence IIb B for reducing adiposity.
Reprinted from Mozaffarian et al17 with permission. Copyright © 2012, American Heart Association, Inc.
Table 2-7.
Reduction in BP Required to Increase Prevalence of Ideal BP Among Adults ≥20 Years of Age; NHANES 2009 to 2010
| % | |
|---|---|
| Percent BP ideal among adults, 2009–2010 | 44.26 |
| 20% Relative increase | 53.11 |
| Percent of US adults whose BP would be ideal if population mean BP were lowered by* | |
| 2 mm Hg | 56.13 |
| 3 mm Hg | 59.49 |
| 4 mm Hg | 61.59 |
| 5 mm Hg | 65.31 |
Standardized to the age distribution of the 2000 US standard population.
BP indicates blood pressure; and NHANES, National Health and Nutrition Examination Survey.
Reduction in BP=(observed average systolic-X mm Hg) AND (observed average diastolic-X mm Hg).
- 1.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 2.Fang J, Yang Q, Hong Y, Loustalot F. Status of cardiovascular health among adult Americans in the 50 states and the District of Columbia, 2009. J Am Heart Assoc. 2012;1:e005371. doi: 10.1161/JAHA.112.005371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM. Cardiovascular health behavior and health factor changes (1988–2008) and projections to 2020: results from the National Health and Nutrition Examination Surveys. Circulation. 2012;125:2595–2602. doi: 10.1161/CIRCULATIONAHA.111.070722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huffman MD, Lloyd-Jones DM, Ning H, Labarthe DR, Guzman Castillo M, O’Flaherty M, Ford ES, Capewell S. Quantifying options for reducing coronary heart disease mortality by 2020. Circulation. 2013;127:2477–2484. doi: 10.1161/CIRCULATIONAHA.112.000769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1999–2010. Series 20 No. 2P. [Accessed July 21, 2013];CDC WONDER Online Database [database online] Released January 2013. http://wonder.cdc.gov/cmf-icd10.html.
- 6.Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of “ideal cardiovascular health” in a community-based population: the Heart Strategies Concentrating on Risk Evaluation (Heart SCORE) study. Circulation. 2011;123:850–857. doi: 10.1161/CIRCULATIONAHA.110.980151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD ARIC Study Investigators. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dong C, Rundek T, Wright CB, Anwar Z, Elkind MS, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2012;125:2975–2984. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Artero EG, España-Romero V, Lee DC, Sui X, Church TS, Lavie CJ, Blair SN. Ideal cardiovascular health and mortality: Aerobics Center Longitudinal Study. Mayo Clin Proc. 2012;87:944–952. doi: 10.1016/j.mayocp.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, Gillespie C, Merritt R, Hu FB. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307:1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–995. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilkins JT, Ning H, Berry J, Zhao L, Dyer AR, Lloyd-Jones DM. Lifetime risk and years lived free of total cardiovascular disease. JAMA. 2012;308:1795–1801. doi: 10.1001/jama.2012.14312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rasmussen-Torvik LJ, Shay CM, Abramson JG, Friedrich CA, Nettleton JA, Prizment AE, Folsom AR. Ideal cardiovascular health is inversely associated with incident cancer: the Atherosclerosis Risk In Communities study. Circulation. 2013;127:1270–1275. doi: 10.1161/CIRCULATIONAHA.112.001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kronish IM, Carson AP, Davidson KW, Muntner P, Safford MM. Depressive symptoms and cardiovascular health by the American Heart Association’s definition in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. PLoS ONE. 2012;7:e52771. doi: 10.1371/journal.pone.0052771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14a.Murray CJ, Abraham J, Ali MK, Alvarado M, Atkinson C, Baddour LM, Bartels DH, Benjamin EJ, Bhalla K, Birbeck G, Bolliger I, Burstein R, Carnahan E, Chen H, Chou D, Chugh SS, Cohen A, Colson KE, Cooper LT, Couser W, Criqui MH, Dabhadkar KC, Dahodwala N, Danaei G, Dellavalle RP, Des Jarlais DC, Dicker D, Ding EL, Dorsey ER, Duber H, Ebel BE, Engell RE, Ezzati M, Felson DT, Finucane MM, Flaxman S, Flaxman AD, Fleming T, Forouzanfar MH, Freedman G, Freeman MK, Gabriel SE, Gakidou E, Gillum RF, Gonzalez-Medina D, Gosselin R, Grant B, Gutierrez HR, Hagan H, Havmoeller R, Hoffman H, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Kassebaum N, Khatibzadeh S, Knowlton LM, Lan Q, Leasher JL, Lim S, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Macintyre MF, Mallinger L, McDermott MM, Meltzer M, Mensah GA, Michaud C, Miller TR, Mock C, Moffitt TE, Mokdad AA, Mokdad AH, Moran AE, Mozaffarian D, Murphy T, Naghavi M, Narayan KM, Nelson RG, Olives C, Omer SB, Ortblad K, Ostro B, Pelizzari PM, Phillips D, Pope CA, Raju M, Ranganathan D, Razavi H, Ritz B, Rivara FP, Roberts T, Sacco RL, Salomon JA, Sampson U, Sanman E, Sapkota A, Schwebel DC, Shahraz S, Shibuya K, Shivakoti R, Silberberg D, Singh GM, Singh D, Singh JA, Sleet DA, Steenland K, Tavakkoli M, Taylor JA, Thurston GD, Towbin JA, Vavilala MS, Vos T, Wagner GR, Weinstock MA, Weisskopf MG, Wilkinson JD, Wulf S, Zabetian A, Lopez AD Collaborators USBoD. The State of US Health, 1990–2010: Burden of Diseases, Injuries, and Risk Factors. JAMA. 2013;310:591608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362:590–599. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Artinian NT, Fletcher GF, Mozaffarian D, Kris-Etherton P, Van Horn L, Lichtenstein AH, Kumanyika S, Kraus WE, Fleg JL, Redeker NS, Meininger JC, Banks J, Stuart-Shor EM, Fletcher BJ, Miller TD, Hughes S, Braun LT, Kopin LA, Berra K, Hayman LL, Ewing LJ, Ades PA, Durstine JL, Houston-Miller N, Burke LE on behalf of the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:406–441. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA, Jacobs DR, Jr, Kraus WE, Kris-Etherton PM, Krummel DA, Popkin BM, Whitsel LP, Zakai NA. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126:1514–1563. doi: 10.1161/CIR.0b013e318260a20b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bodenheimer T. Helping patients improve their health-related behaviors: what system changes do we need? Dis Manag. 2005;8:319–330. doi: 10.1089/dis.2005.8.319. [DOI] [PubMed] [Google Scholar]
- 19.Simpson LA, Cooper J. Paying for obesity: a changing landscape. Pediatrics. 2009;123(suppl 5):S301–S307. doi: 10.1542/peds.2008-2780I. [DOI] [PubMed] [Google Scholar]
- 20.Quist-Paulsen P. Cessation in the use of tobacco: pharmacologic and non-pharmacologic routines in patients. Clin Respir J. 2008;2:4–10. doi: 10.1111/j.1752-699X.2007.00038.x. [DOI] [PubMed] [Google Scholar]
- 21.Davis D, Galbraith R American College of Chest Physicians Health and Science Policy Committee. Continuing medical education effect on practice performance: effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest. 2009;135(suppl):42S–48S. doi: 10.1378/chest.08-2517. [DOI] [PubMed] [Google Scholar]
3. Smoking/Tobacco Use
See Table 3-1 and Charts 3-1 and 3-2.
Table 3-1.
Cigarette Smoking
| Population Group | Prevalence, 2012 Age ≥18 y*6 | Cost18 |
|---|---|---|
| Both sexes | 42 098 000 (18.1%) | $193 Billion per year |
| Males | 22 983 000 (20.5%) | … |
| Females | 19 115 000 (15.9%) | … |
| NH white males | 22.0% | … |
| NH white females | 19.2% | … |
| NH black males | 21.6% | … |
| NH black females | 14.2% | … |
| Hispanic or Latino males | 16.6% | … |
| Hispanic or Latino females | 7.5% | … |
| Asian only (both sexes) | 10.4% | … |
| American Indian/Alaska Native only (both sexes) | 18.8% | … |
Percentages are age adjusted. Estimates for Asian only and American Indian/Alaska Native only include non-Hispanic and Hispanic persons.
Ellipses (…) indicate data not available; and NH, non-Hispanic.
Rounded to the nearest thousand.
Chart 3-1.
Prevalence (%) of students in grades 9 to 12 reporting current cigarette use by sex and race/ethnicity (Youth Risk Behavior Surveillance System, 2011). NH indicates non-Hispanic. Data derived from MMWR: Morbidity and Mortality Weekly Report.3
Chart 3-2.
Prevalence (%) of current smoking for adults >18 years of age by race/ethnicity and sex (National Health Interview Survey: 2009–2011). All percentages are age adjusted. AIAN indicates American Indian/Alaska Native; and NH, non-Hispanic. *Includes both Hispanics and non-Hispanics. Data derived from Centers for Disease Control and Prevention/National Center for Health Statistics, Health Data Interactive.10
Smoking is a major risk factor for CVD and stroke.1 The AHA has identified never tried or never smoked a whole cigarette (for children) and never smoking or quitting >12 months ago (for adults) as 1 of the 7 components of ideal cardiovascular health.2 According to NHANES 2009 to 2010 data, 85.2% of children and 76.2% of adults met these criteria.
Prevalence
Youth
(See Chart 3-1.)
-
In 2011, in grades 9 through 12:
18.1% of students reported current cigarette use (on ≥1 day during the 30 days before the survey), 13.1% of students reported current cigar use, and 7.7% of students reported current smokeless tobacco use. Overall, 23.4% of students reported any current tobacco use (YRBS; Chart 3-1).3
Male students were more likely than female students to report current cigarette use (19.9% compared with 16.1%). Male students were also more likely than female students to report current cigar use (17.8% compared with 8.0%) and current smokeless tobacco use (12.8% compared with 2.2%; YRBS).3
Non-Hispanic white students were more likely than Hispanic or non-Hispanic black students to report any current tobacco use, which includes cigarettes, cigars, or smokeless tobacco (26.5% compared with 20.5% for Hispanic students and 15.4% for non-Hispanic black students; YRBS).3
Among youths 12 to 17 years of age in 2011, 2.4 million (10.0%) used a tobacco product (cigarettes, cigars, or smokeless tobacco) in the past month, and 1.9 million (7.8%) used cigarettes. Cigarette use in the past month in this age group declined significantly from 13.0% in 2002 to 7.8% in 2011 (NSDUH).4
-
Data from the YRBS5 for students in grades 9 to 12 indicated the following:
The percentage of students who reported ever trying cigarettes remained stable from 1991 to 1999 and then declined from 70.4% in 1999 to 44.7% in 2011.
The percentage who reported current cigarette use (on at least 1 day in the 30 days before the survey) increased between 1991 and 1997 and then declined from 36.4% in 1997 to 18.1% in 2011.
The percentage who reported current frequent cigarette use (smoked on ≥20 of the 30 days before the survey) increased from 1991 to 1999 and then declined from 16.8% in 1999 to 6.4% in 2011.
In 2011, 49.9% of students in grades 9 to 12 who currently smoked cigarettes had tried to quit smoking cigarettes during the previous 12 months. The prevalence of trying to quit smoking was higher among female student smokers (53.9%) than among male student smokers (47.0%) and among white females (54.0%) and Hispanic females (55.9%) than among white males (46.3%) and Hispanic males (44.7%; YRBS).3
Abbreviations Used in Chapter 3
| AHA | American Heart Association |
| AIAN | American Indian or Alaska Native |
| AMI | acute myocardial infarction |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CHD | coronary heart disease |
| CI | confidence interval |
| CVD | cardiovascular disease |
| NH | non-Hispanic |
| NHANES | National Health and Nutrition Examination Survey |
| NHIS | National Health Interview Survey |
| NSDUH | National Survey on Drug Use and Health |
| RR | relative risk |
| WHO | World Health Organization |
| YRBS | Youth Risk Behavior Survey |
Adults
(See Table 3-1 and Chart 3-2.)
-
In 2012, among adults ≥18 years of age:
20.5% of men and 15.9% of women were current cigarette smokers (NHIS).6
The percentage of current cigarette smokers (18.1%) declined 25% since 1998 (24.1%).6,7
The states with the highest percentage of current cigarette smokers were Kentucky (28.3%), West Virginia (28.2%), and Arkansas (25.0%). Utah had the lowest percentage of smokers (10.6%) (BRFSS).8
In 2011, an estimated 68.2 million Americans ≥12 years of age were current (past month) users of a tobacco product (cigarettes, cigars, smokeless tobacco, or tobacco in pipes). The rate of current use of any tobacco product in this age range declined from 2007 to 2011 (from 28.6% to 26.5%; NSDUH).4
From 1998 to 2007, cigarette smoking prevalence among adults ≥18 years of age decreased in 44 states and the District of Columbia. Six states had no substantial changes in prevalence after controlling for age, sex, and race/ethnicity (BRFSS).9
In 2009 to 2011, among people ≥65 years of age, 8.9% of men and 8.7% of women were current smokers. In this age group, men were more likely than women to be former smokers (53.0% compared with 30.6%) on the basis of age-adjusted estimates (NHIS).10
In 2009 to 2011, among adults ≥18 years of age, Asian men (15.1%) and Hispanic men (16.3%) were less likely to be current cigarette smokers than non-Hispanic black men (23.2%), non-Hispanic white men (23.6%), and American Indian or Alaska Native men (23.7%) on the basis of ageadjusted estimates (NHIS). Similarly, in 2009 to 2011, Asian women (5.7%) and Hispanic women (8.9%) were less likely to be current cigarette smokers than non-Hispanic black women (16.9%), non-Hispanic white women (20.3%), and American Indian or Alaska Native women (23.6%; NHIS).10
In 2010 to 2011, among women 15 to 44 years of age, past-month cigarette use was lower for those who were pregnant (17.6%) than among those who were not pregnant (25.4%). This pattern was found for women 18 to 25 years of age (22.4% versus 29.9% for pregnant and nonpregnant women, respectively) and for women 26 to 44 years of age (14.3% versus 25.7%, respectively; NSDUH).4
Incidence
-
In 2011:
Approximately 2.4 million people ≥12 years of age smoked cigarettes for the first time within the past 12 months, which was similar to the estimate in 2010. The 2011 estimate averages out to ≈6500 new cigarette smokers every day. Most new smokers (55.7%) in 2011 were <18 years of age when they first smoked cigarettes (NSDUH).4
The number of new smokers <18 years of age (1.3 million) was similar to that in 2002 (1.3 million); however, new smokers ≥18 years of age increased from ≈600 000 in 2002 to 1.1 million in 2011 (NSDUH).4
Among people 12 to 49 years of age who had started smoking within the past 12 months, the average age of first cigarette use was 17.2 years, similar to the average in 2010 (17.3 years).4
Data from 2002 to 2004 suggest that ≈1 in 5 nonsmokers 12 to 17 years of age is likely to start smoking. Youths in the Mexican subpopulations were significantly more susceptible (28.8%) to start smoking than those in non-Hispanic white (20.8%), non-Hispanic black (23.0%), Cuban (16.4%), Asian Indian (15.4%), Chinese (15.3%), and Vietnamese (13.8%) subpopulations. There was no significant difference in susceptibility to start smoking between boys and girls in any of the major populations or subpopulations (NSDUH).11
Morbidity
A 2010 report of the US Surgeon General on how tobacco causes disease summarizes an extensive body of literature on smoking and CVD and the mechanisms through which smoking is thought to cause CVD.12 Among its conclusions are the following:
There is a sharp increase in CVD risk with low levels of exposure to cigarette smoke, including secondhand smoke, and a less rapid further increase in risk as the number of cigarettes per day increases.
A meta-analysis comparing pooled data of ≈2.4 million smokers and nonsmokers found the RR ratio of smokers to nonsmokers for developing CHD was 25% higher in women than in men (95% CI, 1.12–1.39).13
Current smokers have a 2 to 4 times increased risk of stroke compared with nonsmokers or those who have quit for >10 years.14,15
Recent analysis has found that tobacco exposure is a top risk factor for disability in the United States, second only to dietary risks.16
Worldwide, tobacco smoking (including secondhand smoke) was 1 of the top 3 leading risk factors for disease in 2010.17
Mortality
In 2005, tobacco smoking was the cause of ≈467 000 adult deaths (19.1%) in the United States. Approximately one third of these deaths were related to CVD.18
During 2000 to 2004, ≈49 000 (11.1%) of cigarette smoking–related deaths were attributable to secondhand smoke.19
Each year from 2000 to 2004, smoking caused 3.1 million years of potential life lost for males and 2.0 million years for females, excluding deaths attributable to smoking-attributable residential fires and adult deaths attributable to secondhand smoke.19
From 2000 to 2004, smoking during pregnancy resulted in an estimated 776 infant deaths annually.17
During 2000 to 2004, cigarette smoking resulted in an estimated 269 655 deaths annually among males and 173 940 deaths annually among females.19
On average, male smokers die 13.2 years earlier than male nonsmokers, and female smokers die 14.5 years earlier than female nonsmokers.1
In 2010, tobacco smoking was the second-leading risk factor for deaths in the United States, after dietary risks.16
Overall mortality among US smokers is 3 times higher than that for never-smokers.20
Worldwide, tobacco smoking (including secondhand smoke) was estimated to contribute to 6.2 million deaths in 2010.17
Smoking Cessation
-
Smoking cessation reduces the risk of cardiovascular morbidity and mortality for smokers with and without CHD.
There is no evidence to date that reducing the amount smoked by smoking fewer cigarettes per day reduces the risk of CVD.12
Smokers who quit smoking at 25 to 34 years of age gained 10 years of life compared with those who continued to smoke. Those aged 35 to 44 years gained 9 years and those aged 45 to 54 years gained 6 years of life, on average, compared with those who continued to smoke.20
In 2010, 48.3% of adult current smokers ≥18 years of age who had a health checkup during the preceding year reported that they had been advised to quit. Smokers between 18 and 24 (31%) and 24 to 44 (44%) years of age were less likely to be advised to quit than those at older ages (57%; NHIS).21
Cessation medications (including sustained-release bupropion, varenicline, and nicotine gum, lozenge, nasal spray, and patch) are effective for helping smokers quit.22
In addition to medications, smoke-free policies, increases in tobacco prices, cessation advice from healthcare professionals, and quitlines and other counseling have contributed to smoking cessation.21
In 2010, 52.4% of adult smokers reported trying to quit smoking in the past year; 6.2% reported they recently quit smoking. Of those who tried to quit smoking, 30.0% used cessation medications.21
To help combat the global problem of tobacco exposure, in 2003 the WHO adopted the Framework Convention on Tobacco Control treaty. The WHO Framework Convention on Tobacco Control contains a set of universal standards to limit tobacco supply and demand worldwide. These standards include the use of tax policies to reduce tobacco consumption, a ban on the indoor use of tobacco products, implementation of educational programs about the dangers of tobacco use, and restrictions of the sale of tobacco products to international travelers. Since it came into force in 2005, >175 countries have ratified the WHO Framework Convention on Tobacco Control.23
Secondhand Smoke
-
Data from a 2006 report of the US Surgeon General on the consequences of involuntary exposure to tobacco smoke12 indicate the following:
Nonsmokers who are exposed to secondhand smoke at home or at work increase their risk of developing CHD by 25% to 30%.
Short exposures to secondhand smoke can cause blood platelets to become stickier, damage the lining of blood vessels, and decrease coronary flow velocity reserves, potentially increasing the risk of an AMI.
In 2008, data from 11 states showed that the majority of people surveyed in each state reported having smoke-free home rules, ranging from 68.8% in West Virginia to 85.6% in Arizona (BRFSS).24
As of December 31, 2010, 25 states and the District of Columbia had laws that prohibited smoking in indoor areas of worksites, restaurants, and bars; no states had such laws in 2000. As of December 31, 2010, an additional 10 states had laws that prohibited smoking in 1 or 2 but not all 3 venues.25
In 2012, 30 of the 50 largest US cities prohibited indoor smoking in private workplaces, either through state or local ordinances.26
Pooled data from 17 studies in North America, Europe, and Australasia suggest that smoke-free legislation can reduce the incidence of acute coronary events by 10%.27
The percentage of the US nonsmoking population with serum cotinine ≥0.05 ng/mL declined from 52.5% in 1999 to 2000 to 40.1% in 2007 to 2008, with declines occurring for both children and adults. During 2007 to 2008, the percentage of nonsmokers with detectable serum cotinine was 53.6% for those 3 to 11 years of age, 46.5% for those 12 to 19 years of age, and 36.7% for those ≥20 years of age. The percentage was also higher for non-Hispanic blacks (55.9%) than for non-Hispanic whites (40.1%) and Mexican Americans (28.5%; NHANES).28
Cost
Direct medical costs ($96 billion) and lost productivity costs ($97 billion) associated with smoking totaled an estimated $193 billion per year between 2000 and 2004.18
In 2008, $9.94 billion was spent on marketing cigarettes in the United States.29
Cigarette prices have increased 283% between the early 1980s and 2011, which contributed to decreased sales from ≈30 million packs sold in 1982 to ≈14 million packs sold in 2011.29
- 1.The 2004 United States Surgeon General’s Report: The Health Consequences of Smoking. N S W Public Health Bull. 2004;15:107. [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 3.Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Whittle L, Lim C, Wechsler H Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance: United States, 2011. MMWR Surveill Summ. 2012;61:1–162. [PubMed] [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration. [Accessed June 3, 2013];Results from the 2011 National Survey on Drug Use and Health: national findings and detailed tables. http://www.samhsa.gov/data/NSDUH.aspx. [PubMed]
- 5.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. [Accessed July 25, 2012];Trends in the prevalence of tobacco use, national YRBS: 1991–2011. http://www.cdc.gov/healthyyouth/yrbs/pdf/us_tobacco_trend_yrbs.pdf.
- 6.Blackwell D, Lucas J, Clarke T. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. National Center for Health Statistics. Vital Health Stat 10. In press. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults and trends in smoking cessation: United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:1227–1232. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2012. [Accessed September 17, 2013]. Prevalence and trends data, tobacco use. http://apps.nccd.cdc.gov/brfss/index.asp. [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC) State-specific prevalence and trends in adult cigarette smoking: United States, 1998–2007. MMWR Morb Mortal Wkly Rep. 2009;58:221–226. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention, National Center for Health Statistics. Health Data Interactive. [Accessed June 4, 2013];Centers for Disease Control and Prevention Web site. http://www.cdc.gov/nchs/hdi.htm.
- 11.Centers for Disease Control and Prevention (CDC) Racial/ethnic differences among youths in cigarette smoking and susceptibility to start smoking: United States, 2002–2004. MMWR Morb Mortal Wkly Rep. 2006;55:1275–1277. [PubMed] [Google Scholar]
- 12.US Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [Google Scholar]
- 13.Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. 2011;378:1297–1305. doi: 10.1016/S0140-6736(11)60781-2. [DOI] [PubMed] [Google Scholar]
- 14.Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, Creager MA, Culebras A, Eckel RH, Hart RG, Hinchey JA, Howard VJ, Jauch EC, Levine SR, Meschia JF, Moore WS, Nixon JV, Pearson TA on behalf of the American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention; Council for High Blood Pressure Research, Council on Peripheral Vascular Disease, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association [published correction appears in Stroke. 2011;42:e26] Stroke. 2011;42:517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 15.Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010;8:917–932. doi: 10.1586/erc.10.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.US Burden of Disease Collaborators. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;319:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD, 3rd, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Mohd Hanafiah K, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA, 3rd, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJ, Ezzati M, AlMazroa MA, Memish ZA. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010 [published corrections appear in Lancet. 2013;381:1276 and Lancet. 2013;381:628] Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors [published correction appears in PLoS Med. 2011;8. doi:10.1371/annotation/0ef47acd-9dcc-4296-a897-872d182cde57] PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) Smoking-attributable mortality, years of potential life lost, and productivity losses: United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57:1226–1228. [PubMed] [Google Scholar]
- 20.Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, McAfee T, Peto R. 21st-Century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368:341–350. doi: 10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease C, Prevention. Quitting smoking among adults: United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60:1513–1519. [PubMed] [Google Scholar]
- 22.Clinical Practice Guideline Treating Tobacco Use and Dependence Update Panel, Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update: a U.S. Public Health Service report. Am J Prev Med. 2008;35:158–176. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. [Accessed July 18, 2013];About the WHO Framework Convention on Tobacco Control. http://www.who.int/fctc/about/en/index.html.
- 24.Centers for Disease Control and Prevention (CDC) State-specific secondhand smoke exposure and current cigarette smoking among adults: United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:1232–1235. [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) State smoke-free laws for worksites, restaurants, and bars: United States, 2000–2010. MMWR Morb Mortal Wkly Rep. 2011;60:472–475. [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC) Comprehensive smoke-free laws: 50 largest U.S. cities, 2000 and 2012. MMWR Morb Mortal Wkly Rep. 2012;61:914–917. [PubMed] [Google Scholar]
- 27.Mackay DF, Irfan MO, Haw S, Pell JP. Meta-analysis of the effect of comprehensive smoke-free legislation on acute coronary events. Heart. 2010;96:1525–1530. doi: 10.1136/hrt.2010.199026. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention (CDC) Vital signs: nonsmokers’ exposure to secondhand smoke: United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2010;59:1141–1146. [PubMed] [Google Scholar]
- 29.US Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Accessed May 30, 2012]. http://www.surgeongeneral.gov/library/reports/preventing-youth-tobacco-use/prevent_youth_by_section.html. [Google Scholar]
4. Physical Inactivity
See Table 4-1 and Charts 4-1 through 4-5.
Table 4-1.
Met 2008 Federal PA Guidelines for Adults
| Population Group | Prevalence, 2012 (Age ≥18 y), % |
|---|---|
| Both sexes | 20.7 |
| Males | 24.6 |
| Females | 17.1 |
| NH white only | 22.9 |
| NH black only | 16.6 |
| Hispanic or Latino | 15.7 |
| American Indian/Alaska Native only | 18.7 |
| Asian only | 17.1 |
“Met 2008 federal PA guidelines for adults” is defined as engaging in ≥150 min of moderate or 75 min of vigorous aerobic leisure-time physical activity per wk (or an equivalent combination) and engaging in leisure-time strengthening physical activity at least twice a wk.
Data are age adjusted for adults ≥18 y of age.
PA indicates physical activity; NH, non-Hispanic.
Source: National Health Interview Survey 2012 (National Center for Health sStatistics).7
Chart 4-1.
Prevalence of students in grades 9 to 12 who did not participate in ≥60 minutes of physical activity on any day by race/ethnicity and sex (Youth Risk Behavior Surveillance: 2011). NH indicates non-Hispanic. Data derived from MMWR Surveillance Summaries.3
Chart 4-5.
Prevalence of meeting the aerobic guidelines of the 2008 Federal Physical Activity Guidelines among adults ≥18 years of age by race/ethnicity and sex (National Health Interview Survey: 2012). NH indicates non-Hispanic. Percentages are age adjusted. The aerobic guidelines of the 2008 Federal Physical Activity Guidelines recommend engaging in moderate leisure-time physical activity for ≥150 minutes per week or vigorous activity ≥75 minutes per week or an equivalent combination. Source: Blackwell et al.7
Physical inactivity is a major risk factor for CVD and stroke.1 The AHA has identified ≥60 minutes of moderate- or vigorous-intensity activity every day (for children) and ≥150 min/wk of moderate-intensity activity or ≥75 min/wk of vigorous-intensity activity or a combination thereof (for adults) as 1 of the 7 components of ideal cardiovascular health.2 In 2009 to 2010, 36.5% of children and 41.1% of adults met these criteria.
Prevalence
Youth
Inactivity
(See Chart 4-1.)
In 20113:
Nationwide, 13.8% of adolescents were inactive during the previous 7 days, as indicated by their response that they did not participate in ≥60 minutes of any kind of PA that increased their heart rate and made them breathe hard on any 1 of the previous 7 days.
Girls were more likely than boys to report inactivity (17.7% versus 10.0%).
The prevalence of inactivity was highest among black (26.7%) and Hispanic (21.3%) girls, followed by white girls (13.7%), black boys (12.3%), Hispanic boys (10.7%), and white boys (8.5%).
Abbreviations Used in Chapter 4
| AHA | American Heart Association |
| CARDIA | Coronary Artery Risk Development in Young Adults |
| CHD | coronary heart disease |
| CI | confidence interval |
| CRP | C-reactive protein |
| CVD | cardiovascular disease |
| DBP | diastolic blood pressure |
| DM | diabetes mellitus |
| EF | ejection fraction |
| FMD | flow-mediated dilation |
| HbA1c | hemoglobin AIc |
| HDL | high-density lipoprotein |
| HF | heart failure |
| HR | hazard ratio |
| MI | myocardial infarction |
| NH | non-Hispanic |
| NHANES | National Health and Nutrition Examination Survey |
| NHIS | National Health Interview Survey |
| PA | physical activity |
| PAD | peripheral artery disease |
| RR | relative risk |
| SBP | systolic blood pressure |
| WHO | World Health Organization |
Television/Video/Computers
(See Chart 4-2.)
Chart 4-2.
Percentage of students in grades 9 to 12 who used a computer for ≥3 hours a day by race/ethnicity and sex (Youth Risk Behavior Surveillance: 2011). NH indicates non-Hispanic. Data derived from MMWR Surveillance Summaries.3
In 20113:
Nationwide, 31.1% of adolescents used a computer for activities other than school work (eg, videogames or other computer games) for ≥3 hours per day on an average school day.
The prevalence of using computers or watching television ≥3 hours per day was highest among black (41.1%) and Hispanic (36.3%) boys, followed by white boys (33.3%), black girls (35.2%), Hispanic girls (28.3%), and white girls (22.6%).
32.4% of adolescents watched television for ≥3 hours per day.
The prevalence of watching television ≥3 hours per day was highest among black girls (54.9%) and boys (54.4%), followed by Hispanic boys (38.4%) and girls (37.2%) and white boys (27.3%) and girls (23.9%).
Increased television time has significant nutritional associations with weight gain (refer to Chapter 5, Nutrition).
Activity Recommendations
(See Charts 4-3 and 4-4.)
Chart 4-3.
Prevalence of students in grades 9 to 12 who met currently recommended levels of physical activity during the past 7 days by race/ethnicity and sex (Youth Risk Behavior Surveillance: 2011). “Currently recommended levels” was defined as activity that increased their heart rate and made them breathe hard some of the time for a total of ≥60 minutes per day on 5 of the 7 days preceding the survey. NH indicates non-Hispanic. Data derived from MMWR Surveillance Summaries.3
Chart 4-4.
Prevalence of children 6 to 19 years of age who attained sufficient moderate to vigorous physical activity to meet public health recommendations (≥60 minutes per day on 5 or more of the 7 days preceding the survey), by sex and age (National Health and Nutrition Examination Survey: 2003–2004). Source: Troiano et al.5
In 2011, the proportion of students who met activity recommendations of ≥60 minutes of PA on 7 days of the week was 28.7% nationwide and declined from 9th (30.7%) to 12th (25.1%) grades. At each grade level, the proportion was higher in boys than in girls.3
In 2011, more high school boys (38.3%) than girls (18.5%) self-reported having been physically active ≥60 minutes per day on all 7 days; self-reported rates of activity were higher in white (30.4%) than in black (26.0%) or Hispanic (26.5%) adolescents.3
The 2010 National Youth Physical Activity and Nutrition Study showed that a total of 15.3% of high school students met the recommendations for aerobic activity, 51.0% met the recommendations for muscle-strengthening activity, and 12.2% met the recommendations for both aerobic and muscle-strengthening activities.4
There was a marked discrepancy between the proportion of youth (ages 6–11 years) who reported engaging in ≥60 minutes of moderate-to-vigorous PA on most days of the week and those who actually engaged in moderate-to-vigorous PA for ≥60 minutes when activity was measured objectively with accelerometers (ie, portable motion sensors that record and quantify the duration and intensity of movements) in the NHANES 2003 to 2004 survey.5
On the basis of accelerometer counts per minute >2020, 42% of 6- to 11-year-olds accumulated ≥260 minutes of moderate-to-vigorous PA on ≥5 days per week, whereas only 8% of 12-to 15-year-olds and 7.6% of 16- to 19-year-olds achieved similar counts.5
More boys than girls met PA recommendations (≥60 minutes of moderate to vigorous activity on most days of the week) as measured by accelerometry.5
Structured Activity Participation
Despite recommendations from the National Association for Sport and Physical Education that schools should require daily physical education for students in kindergarten through 12th grade,6 only 51.8% of students attended physical education classes in school daily (56.7% of boys and 46.7% of girls).3
Physical education class participation declined from the 9th through the 12th grades among boys and girls.3
Little more than half (58.4%) of high school students played on at least 1 school or community sports team in the previous year; however, the prevalence declined with increasing grade level, from 61.4% in the 9th grade to 52.5% in the 12th grade.3
Adults
Inactivity
According to 2012 data from the NHIS, in adults ≥18 years of age:
29.9% do not engage in leisure-time PA (“no leisure-time PA/inactivity” refers to no sessions of light/moderate or vigorous PA of ≥10 minutes’ duration).7
Inactivity was higher among women than men (31.0% versus 28.6%, age adjusted) and increased with age from 24.5% to 31.8%, 35.7%, and 51.4% among adults 18 to 44, 45 to 64, 65 to 74, and ≥75 years of age, respectively.7
Non-Hispanic black and Hispanic adults were more likely to be inactive (39.4% and 39.8%, respectively) than were non-Hispanic white adults (26.2%) on the basis of age-adjusted estimates.7
Activity Recommendations
(See Table 4-1 and Chart 4-5.)
According to 2012 data from the NHIS, in adults ≥18 years of age:
20.7% met the 2008 federal PA guidelines for both aerobic and strengthening activity, an important component of overall physical fitness.7
The age-adjusted proportion who reported engaging in moderate or vigorous PA that met the 2008 aerobic PA guidelines for Americans (≥150 minutes of moderate PA or 75 minutes of vigorous PA or an equivalent combination each week) was 50.1%; 53.9% of men and 46.5% of women met the recommendations. Age-adjusted prevalence was 53.6% for non-Hispanic whites, 40.9% for non-Hispanic blacks, and 42.5% for Hispanics.7
The proportion of respondents who did not meet the federal aerobic PA guidelines increased with age from 43.8% of 18- to 44-year-olds to 71.9% of adults ≥75 years of age.7
Non-Hispanic black adults (59.1%) and Hispanic/Latino adults (57.4%) were more likely not to meet the federal aerobic PA guidelines than non-Hispanic white (46.4%) adults, according to age-adjusted estimates.7
The percentage of adults ≥25 years of age not meeting the full (aerobic and muscle-strengthening) federal PA guidelines was inversely associated with education; 66.4% of participants with no high school diploma, 57.6% of those with a high school diploma or a high school equivalency credential, 46.8% of those with some college, and 33.2% of those with a bachelor’s degree or higher did not meet the full federal PA guidelines.7
The proportion of adults ≥25 years of age who met the 2008 federal PA guidelines for aerobic activity was positively associated with education level: 62.9% of those with a college degree or higher met the PA guidelines compared with 31.5% of adults with less than a high school diploma.7
The proportion of adults reporting levels of PA consistent with the 2008 Physical Activity Guidelines for Americans remains low and decreases with age.8,9 Thirty-three percent of respondents in a study examining awareness of current US PA guidelines had direct knowledge of the recommended dosage of PA (ie, frequency/duration).10
The percentage of adults reporting ≥150 minutes of moderate PA or 75 minutes of vigorous PA or an equivalent combination weekly decreased with age from 55.8% for adults 18 to 44 years of age to 27.4% for those ≥75 years of age, on the basis of the 2011 NHIS.9
The percentage of men who engaged in both leisure-time aerobic and strengthening activities decreased with age, from 39.8% at age 18 to 24 years to 11.1% at ≥75 years of age. The percentage of women who engaged in both leisure-time aerobic and strengthening activities also decreased with age, from 20.7% at age 18 to 24 years to 5.3% at ≥75 years of age, on the basis of the 2011 NHIS.9
-
Using PA recommendations that existed at the time of the survey, adherence to PA recommendations was much lower when based on PA measured by accelerometer in NHANES 2003 to 20045:
Among adults 20 to 59 years of age, 3.8% of men and 3.2% of women met recommendations to engage in moderate-to-vigorous PA (accelerometer counts >2020/min) for 30 minutes (in sessions of ≥10 minutes) on ≥5 of 7 days.
Among those ≥60 years of age, adherence was 2.5% in men and 2.3% in women.
Accelerometry data from NHANES 2003 to 2006 showed that men engaged in 35 minutes of moderate activity per day, whereas for women, it was 21 minutes. More than 75% of moderate activity was accumulated in 1-minute bouts. Levels of activity declined sharply after the age of 50 years in all groups.11
In a review examining self-reported versus actual measured PA (eg, accelerometers, pedometers, indirect calorimetry, doubly labeled water, heart rate monitor), 60% of respondents self-reported higher values of activity than what was measured by use of direct methods.12
Among men, self-reported PA was 44% greater than actual measured values; among women, self-reported activity was 138% greater than actual measured PA.12
Trends
Youth
In 20113:
Among adolescents, there was a significant decrease in the prevalence of watching television ≥3 hours per day, from 42.8% in 1999 to 32.4%, although there was no significant decrease from the 2009 prevalence of 32.8%.
Among students nationwide, there was a significant increase in the prevalence of having participated in muscle-strengthening activities on ≥3 days per week, from 47.8% in 1991 to 55.6%.
Nationwide, the prevalence of adolescents using computers ≥3 hours per day increased from 21.1% in 2005 to 24.9% in 2009 and 31.1% in 2011.
Among adolescents nationwide, the prevalence of attending physical education classes at least once per week did not increase significantly, from 48.9% in 1991 to 51.8%.
The prevalence of adolescents playing ≥1 team sport in the past year increased from 55.1% in 1999 to 58.4%.
Adults
Between NHANES III (1988–1994) and NHANES 2001 to 2006, the non–age-adjusted proportion of adults who engaged in >12 bouts of PA per month declined from 57.0% to 43.3% in men and from 49.0% to 43.3% in women.13
The proportion of US adults who meet criteria for muscle strength has improved between 1998 and 2011. Annual estimates of the percentage of US adults who met the muscle-strengthening criteria increased from 17.7% in 1998 to 24.5% in 2011, and estimates of the percentage who met both the muscle-strengthening and aerobic criteria increased from 14.4% in 1998 to 21.0% in 2011.8,14
A 2.3% decline in physical inactivity between 1980 and 2000 was estimated to have prevented or postponed ≈17 445 deaths (≈5%) attributable to CHD in the United States.15
CVD and Metabolic Risk Factors
Youth
More girls (67.9%) than boys (55.7%) reported having exercised to lose weight or to keep from gaining weight.3
White girls (72.2%) were more likely than black (54.2%) and Hispanic (66.3%) girls to report exercising to lose weight or to keep from gaining weight.3
Total and vigorous PA are inversely correlated with body fat and the prevalence of obesity.16
Among children 4 to 18 years of age, increased time in moderate to vigorous PA was associated with improvements in waist circumference, SBP, fasting triglycerides, HDL cholesterol, and insulin. These findings were significant regardless of the amount of the children’s sedentary time.17
Among children aged 4 to 18 years, both higher activity levels and lower sedentary time measured by accelerometry were associated with more favorable metabolic risk factor profiles.17
Adults
Participants in the Diabetes Prevention Project randomized trial who met the PA goal of 150 minutes of PA per week were 44% less likely to develop DM after 3.2 years of follow-up, even if they did not meet the weight-loss target.18
Exercise for weight loss, without dietary interventions, was associated with significant reductions in DBP (−2 mm Hg; 95% CI, −4 to −1 mm Hg), triglycerides (−0.2 mmol/L; 95% CI, −0.3 to −0.1 mmol/L), and fasting glucose (−0.2 mmol/L; 95% CI, −0.3 to −0.1 mmol/L).19
A total of 120 to 150 minutes per week of moderate-intensity activity, compared with none, can reduce the risk of developing metabolic syndrome.20
In CARDIA, women who maintained high activity through young adulthood gained 6.1 fewer kilograms of weight and 3.8 fewer centimeters in waist circumference in middle age than those with lower activity. Highly active men gained 2.6 fewer kilograms and 3.1 fewer centimeters than their lower-activity counterparts.21
Self-reported low lifetime recreational activity has been associated with increased PAD.22
In 3 US cohort studies, men and women who increased their PA over time gained less weight in the long term, whereas those who decreased their PA over time gained more weight and those who maintained their current PA had intermediate weight gain.23
Among US men and women, every hour per day of increased television watching was associated with 0.3 lb of greater weight gain every 4 years, whereas every hour per day of decreased television watching was associated with a similar amount of relative weight loss.23
Morbidity and Mortality
Physical inactivity is responsible for 12.2% of the global burden of MI after accounting for other CVD risk factors such as cigarette smoking, DM, hypertension, abdominal obesity, lipid profile, no alcohol intake, and psychosocial factors.24
In a meta-analysis of longitudinal studies among women, RRs of incident CHD were 0.83 (95% CI, 0.69–0.99), 0.77 (95% CI, 0.64–0.92), 0.72 (95% CI, 0.59–0.87), and 0.57 (95% CI, 0.41–0.79) across increasing quintiles of PA compared with the lowest quintile.25
A 2003 meta-analysis of 23 studies on the association of PA with stroke indicated that compared with low levels of activity, high (RR, 0.79; 95% CI, 0.69–0.91) and moderate (RR, 0.91; 95% CI, 0.80–1.05) levels of activity were inversely associated with the likelihood of developing total stroke (ischemic and hemorrhagic).26
With television watching as a sedentary activity, 2 hours of television per day is associated with an RR for type 2 DM of 1.20 (95% CI, 1.14–1.27), an RR for fatal or nonfatal CVD of 1.15 (95% CI, 1.06–1.23), and an RR for all-cause mortality of 1.13 (95% CI, 1.07–1.18). The risk for all-cause mortality further increases with >3 hours of television daily.27
Longitudinal studies commonly report a graded, inverse association of PA amount and duration (ie, dose) with incident CHD and stroke.28
The PA guidelines for adults cite evidence that ≈150 minutes per week of moderate-intensity aerobic activity, compared with none, can reduce the risk of CVD.29
Adherence to PA guidelines for both aerobic and muscle-strengthening activities is associated with 27% lower all-cause mortality among adults without existing chronic conditions such as DM, cancer, MI, angina, CVD, stroke, or respiratory diseases and with 46% lower mortality among people with chronic comorbidities.29
In the Health Professionals Follow-Up Study, for every 3-hour-per-week increase in vigorous-intensity activity, the multivariate RR of MI was 0.78 (95% CI, 0.61–0.98) for men. This 22% reduction of risk can be explained in part by beneficial effects of PA on HDL cholesterol, vitamin D, apolipoprotein B, and HbA1c.30
In a 20-year study of older male veterans, an inverse, graded, and independent association between impaired exercise capacity and all-cause mortality risk was found. For each increase of 1 metabolic equivalent tasks in exercise capacity, mortality risk was 12% lower (HR, 0.88; 95% CI, 0.86–0.90). Unfit individuals who improved their fitness status had a 35% lower mortality risk (HR, 0.65; 95% CI, 0.46–0.93) than those who remained unfit.31
Secondary Prevention
PA improves inflammatory markers in people with existing stable CHD. After a 6-week training session, CRP levels declined by 23.7% (P<0.001), and plasma vascular cell adhesion molecule-1 levels declined by 10.23% (P<0.05); there was no difference in leukocyte count or levels of intercellular adhesion molecule-1.32
In a randomized trial of patients with PAD, supervised treadmill exercise training and lower-extremity resistance training were each associated with significant improvements in functional performance and quality of life compared with a usual-care control group. Exercise training was additionally associated with improved brachial artery FMD, whereas resistance training was associated with better stair-climbing ability versus control.33
On the basis of a meta-analysis of 34 randomized controlled trials, exercise-based cardiac rehabilitation after MI was associated with lower rates of reinfarction, cardiac mortality, and overall mortality.34
The benefit of intense exercise training for cardiac rehabilitation in people with HF was tested in a trial of 27 patients with stable, medically treated HF. Intense activity (an aerobic interval-training program 3 times per week for 12 weeks) was associated with a significant 35% improvement in left ventricular EF and decreases in pro-brain natriuretic peptide (40%), left ventricular end-diastolic volume (18%), and left ventricular end-systolic volume (25%) compared with control and endurance-training groups.35
Exercise training in patients with HF with preserved EF was associated with improved exercise capacity and favorable changes in diastolic function.36
Costs
The economic consequences of physical inactivity are substantial. In a summary of WHO data sources, the economic costs of physical inactivity were estimated to account for 1.5% to 3.0% of total direct healthcare expenditures in developed countries such as the United States.37
-
Interventions and community strategies to increase physical activity have been shown to be cost-effective in terms of reducing medical costs38:
Nearly $3 in medical cost savings is realized for every $1 invested in building bike and walking trails.
Incremental cost and incremental effectiveness ratios range from $14 000 to $69 000 per quality-adjusted life-year gained from interventions such as pedometer or walking programs compared with no intervention, especially in high-risk groups.
- 1.Artinian NT, Fletcher GF, Mozaffarian D, Kris-Etherton P, Van Horn L, Lichtenstein AH, Kumanyika S, Kraus WE, Fleg JL, Redeker NS, Meininger JC, Banks J, Stuart-Shor EM, Fletcher BJ, Miller TD, Hughes S, Braun LT, Kopin LA, Berra K, Hayman LL, Ewing LJ, Ades PA, Durstine JL, Houston-Miller N, Burke LE on behalf of the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:406–441. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 3.Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Whittle L, Lim C, Wechsler H Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance: United States, 2011. MMWR Surveill Summ. 2012;61:1–162. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Physical activity levels of high school students: United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:773–777. [PubMed] [Google Scholar]
- 5.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 6.National Association for Sport and Physical Education. Moving Into the Future: National Standards for Physical Education. 2. Reston, VA: NASPE Publications; 2004. [Google Scholar]
- 7.Blackwell D, Lucas J, Clarke T. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital Health Stat 10. In press. [PubMed] [Google Scholar]
- 8.Carlson SA, Fulton JE, Schoenborn CA, Loustalot F. Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. Am J Prev Med. 2010;39:305–313. doi: 10.1016/j.amepre.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Ward BW, Barnes PM, Freeman G, Schiller JS. Centers for Disease Control and Prevention Web site. National Center for Health Statistics; Jun, 2012. [Accessed July 20, 2012]. Early release of selected estimates based on data from the 2011 National Health Interview Survey. http://www.cdc.gov/nchs/nhis/released201206.htm. [Google Scholar]
- 10.Bennett GG, Wolin KY, Puleo EM, Mâsse LC, Atienza AA. Awareness of national physical activity recommendations for health promotion among US adults. Med Sci Sports Exerc. 2009;41:1849–1855. doi: 10.1249/MSS.0b013e3181a52100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luke A, Dugas LR, Durazo-Arvizu RA, Cao G, Cooper RS. Assessing physical activity and its relationship to cardiovascular risk factors: NHANES 2003–2006. BMC Public Health. 2011;11:387. doi: 10.1186/1471-2458-11-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.King DE, Mainous AG, 3rd, Carnemolla M, Everett CJ. Adherence to healthy lifestyle habits in US adults, 1988–2006. Am J Med. 2009;122:528–534. doi: 10.1016/j.amjmed.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Schiller J, Lucas J, Peregoy J. Summary health statistics for U.S. adults: National Health Interview Survey, 2011. [Accessed October 23, 2013];Vital Health Stat 10. 2012 (256) http://www.cdc.gov/nchs/data/series/sr_10/sr10_256.pdf. [PubMed]
- 15.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 16.Kim Y, Lee S. Physical activity and abdominal obesity in youth. Appl Physiol Nutr Metab. 2009;34:571–581. doi: 10.1139/H09-066. [DOI] [PubMed] [Google Scholar]
- 17.Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A International Children’s Accelerometry Database (ICAD) Collaborators. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents [published correction appears in JAMA. 2012;307:1915] JAMA. 2012;307:704–712. doi: 10.1001/jama.2012.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, Hoskin M, Kriska AM, Mayer-Davis EJ, Pi-Sunyer X, Regensteiner J, Venditti B, Wylie-Rosett J. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29:2102–2107. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaw K, Gennat H, O’Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006;(4):CD003817. doi: 10.1002/14651858.CD003817.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Department of Health and Human Services, Centers for Disease Control and Prevention. Physical activity for everyone: physical activity and health: the benefits of physical activity. [Accessed August 1, 2011];Centers for Disease Control and Prevention Web site. http://www.cdc.gov/physicalactivity/everyone/health/index.html#ReduceCardiovascularDisease.
- 21.Hankinson AL, Daviglus ML, Bouchard C, Carnethon M, Lewis CE, Schreiner PJ, Liu K, Sidney S. Maintaining a high physical activity level over 20 years and weight gain [published correction appears in JAMA. 2011;305:150] JAMA. 2010;304:2603–2610. doi: 10.1001/jama.2010.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson AM, Sadrzadeh-Rafie AH, Myers J, Assimes T, Nead KT, Higgins M, Gabriel A, Olin J, Cooke JP. Low lifetime recreational activity is a risk factor for peripheral arterial disease. J Vasc Surg. 2011;54:427–432. 432. e1–432.e4. doi: 10.1016/j.jvs.2011.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364:2392–2404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 25.Oguma Y, Shinoda-Tagawa T. Physical activity decreases cardiovascular disease risk in women: review and meta-analysis. Am J Prev Med. 2004;26:407–418. doi: 10.1016/j.amepre.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 26.Lee CD, Folsom AR, Blair SN. Physical activity and stroke risk: a meta-analysis. Stroke. 2003;34:2475–2481. doi: 10.1161/01.STR.0000091843.02517.9D. [DOI] [PubMed] [Google Scholar]
- 27.Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011;305:2448–2455. doi: 10.1001/jama.2011.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carnethon MR. Physical activity and cardiovascular disease: how much is enough? Am J Lifestyle Med. 2009;3(suppl):44S–49S. doi: 10.1177/1559827609332737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schoenborn CA, Stommel M. Adherence to the 2008 adult physical activity guidelines and mortality risk. Am J Prev Med. 2011;40:514–521. doi: 10.1016/j.amepre.2010.12.029. [DOI] [PubMed] [Google Scholar]
- 30.Chomistek AK, Chiuve SE, Jensen MK, Cook NR, Rimm EB. Vigorous physical activity, mediating biomarkers, and risk of myocardial infarction. Med Sci Sports Exerc. 2011;43:1884–1890. doi: 10.1249/MSS.0b013e31821b4d0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kokkinos P, Myers J, Faselis C, Panagiotakos DB, Doumas M, Pittaras A, Manolis A, Kokkinos JP, Karasik P, Greenberg M, Papademetriou V, Fletcher R. Exercise capacity and mortality in older men: a 20-year follow-up study. Circulation. 2010;122:790–797. doi: 10.1161/CIRCULATIONAHA.110.938852. [DOI] [PubMed] [Google Scholar]
- 32.Ranković G, Milicić B, Savić T, Dindić B, Mancev Z, Pesić G. Effects of physical exercise on inflammatory parameters and risk for repeated acute coronary syndrome in patients with ischemic heart disease. Vojnosanit Pregl. 2009;66:44–48. doi: 10.2298/vsp0901044r. [DOI] [PubMed] [Google Scholar]
- 33.McDermott MM, Ades P, Guralnik JM, Dyer A, Ferrucci L, Liu K, Nelson M, Lloyd-Jones D, Van Horn L, Garside D, Kibbe M, Domanchuk K, Stein JH, Liao Y, Tao H, Green D, Pearce WH, Schneider JR, McPherson D, Laing ST, McCarthy WJ, Shroff A, Criqui MH. Treadmill exercise and resistance training in patients with peripheral arterial disease with and without intermittent claudication: a randomized controlled trial [published correction appears in JAMA. 2012;307:1694] JAMA. 2009;301:165–174. doi: 10.1001/jama.2008.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am Heart J. 2011;162:571–584. e2. doi: 10.1016/j.ahj.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 35.Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM, Tjønna AE, Helgerud J, Slørdahl SA, Lee SJ, Videm V, Bye A, Smith GL, Najjar SM, Ellingsen Ø, Skjaerpe T. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115:3086–3094. doi: 10.1161/CIRCULATIONAHA.106.675041. [DOI] [PubMed] [Google Scholar]
- 36.Edelmann F, Gelbrich G, Düngen HD, Fröhling S, Wachter R, Stahrenberg R, Binder L, Töpper A, Lashki DJ, Schwarz S, Herrmann-Lingen C, Löffler M, Hasenfuss G, Halle M, Pieske B. Exercise training improves exercise capacity and diastolic function in patients with heart failure with preserved ejection fraction: results of the Ex-DHF (Exercise training in Diastolic Heart Failure) pilot study. J Am Coll Cardiol. 2011;58:1780–1791. doi: 10.1016/j.jacc.2011.06.054. [DOI] [PubMed] [Google Scholar]
- 37.Oldridge NB. Economic burden of physical inactivity: healthcare costs associated with cardiovascular disease. Eur J Cardiovasc Prev Rehabil. 2008;15:130–139. doi: 10.1097/HJR.0b013e3282f19d42. [DOI] [PubMed] [Google Scholar]
- 38.Weintraub WS, Daniels SR, Burke LE, Franklin BA, Goff DC, Jr, Hayman LL, Lloyd-Jones D, Pandey DK, Sanchez EJ, Schram AP, Whitsel LP on behalf of the American Heart Association Advocacy Coordinating Committee; Council on Cardiovascular Disease in the Young; Council on the Kidney in Cardiovascular Disease; Council on Epidemiology and Prevention; Council on Cardiovascular Nursing; Council on Arteriosclerosis; Thrombosis and Vascular Biology; Council on Clinical Cardiology, and Stroke Council. Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association. Circulation. 2011;124:967–990. doi: 10.1161/CIR.0b013e3182285a81. [DOI] [PubMed] [Google Scholar]
5. Nutrition
See Tables 5-1 and 5-2 and Charts 5-1 through 5-3.
Table 5-1.
Dietary Consumption in 2009 to 2010 Among US Adults ≥20 Years of Age of Selected Foods and Nutrients Related to Cardiometabolic Health103–106
| NH White Men
|
NH White Women
|
NH Black Men
|
NH Black Women
|
Mexican American Men
|
Mexican American Women |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* | Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) | % Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
|
| Foods | ||||||||||||
| Whole grains, servings/d |
1.1±0.9 | 10.4 | 1.1±0.8 | 8.4 | 0.8±0.7 | 7.4 | 0.8±0.7 | 8.1 | 2.2±1.4 | 29.0 | 2.1±1.5 | 26.9 |
| Fruits, servings/d | 1.6±1.8 | 11.0 | 1.8±1.5 | 12.7 | 1.2±1.8 | 7.8 | 1.3±1.2 | 6.9 | 1.7±1.3 | 14.1 | 1.9±2.1 | 14.3 |
| Fruits including 100% juices, servings/d |
2.6±2.3 | 25.9 | 2.7±2.0 | 26.5 | 3.0±2.4 | 28.6 | 2.9±2.1 | 27.1 | 3.2±2.3 | 29.3 | 3.4±2.6 | 36.9 |
| Vegetables including starch, servings/d |
2.1±0.4 | 6.2 | 2.2±1.4 | 8.1 | 1.3±0.8 | 2.1 | 1.6±1.0 | 5.0 | 1.3±0.9 | 2.1 | 1.6±1.0 | 3.8 |
| Vegetables including starch and juices /sauces, servings/d |
2.4±0.7 | 9.0 | 2.4±1.4 | 9.4 | 1.5±0.8 | 3.3 | 1.8±1.2 | 5.9 | 1.7±0.7 | 5.7 | 1.8±1.0 | 4.5 |
| Fish and shellfish, servings/wk |
1.6±1.7 | 22.4 | 1.4±1.7 | 22.2 | 1.6±1.7 | 23.2 | 2.1±01.3 | 27.7 | 1.9±1.3 | 25.7 | 1.2±1.3 | 21.3 |
| Nuts, legumes, and seeds, servings/wk |
2.6±2.9 | 21.7 | 2.8±4.2 | 22.8 | 2.4±4.2 | 17.3 | 2.6±4.6 | 19.3 | 7.5±4.6 | 44.2 | 5.3±4.6 | 37.4 |
| Processed meats, servings/wk |
3.0±1.7 | 49.2 | 2.1±1.4 | 60.8 | 3.3±1.4 | 49.0 | 2.3±1.0 | 57.7 | 2.0±1.0 | 63.4 | 1.2±1.0 | 75.2 |
| Sugar-sweetened beverages, servings/wk |
8.3±10.9 | 56.9 | 5.7±9.5 | 68.2 | 11.2±9.2 | 41.5 | 11.0±8.8 | 38.3 | 12.3±8.0 | 29.3 | 9.6±9.3 | 43.3 |
| Sweets and bakery desserts, servings/wk |
5.9±3.9 | 40.4 | 6.9±4.4 | 34.7 | 6.3±3.9 | 42.2 | 6.1±4.0 | 41.1 | 4.4±1.0 | 49.4 | 4.6±3.2 | 47.8 |
| Nutrients | ||||||||||||
| Total calories, kcal/d |
2532±705 | NA | 1766±414 | NA | 2365±699 | NA | 1785±476 | NA | 2367±664 | NA | 1690±502 | NA |
| EPA/DHA, g/d | 0.101±0.052 | 10.1 | 0.095±0.052 | 8.8 | 0.116±0.069 | 9.7 | 0.110±0.064 | 12.3 | 0.136±0.064 | 13.4 | 0.083±0.064 | 7.2 |
| ALA, g/d | 1.44±0.31 | 29.3 | 1.60±0.37 | 75.2 | 1.43±0.25 | 30.6 | 1.49±0.17 | 73.6 | 1.19±0.33 | 17.8 | 1.41±0.33 | 66.9 |
| n-6 PUFA, % energy | 7.4±1.5 | NA | 7.6±1.4 | NA | 7.4±1.2 | NA | 7.6±1.0 | NA | 6.3±1.4 | NA | 7,1±1.5 | NA |
| Saturated fat, % energy |
11.1±2.3 | 35.4 | 10.9±2.1 | 41.9 | 10.2±2.2 | 44.9 | 10.5±1.8 | 45.5 | 9.7±1.8 | 54.4 | 9.7±1.6 | 57.9 |
| Dietary cholesterol, mg/d |
263±106 | 71.5 | 260±104 | 71.1 | 311±83 | 56.2 | 306±83 | 57.8 | 293±75 | 65.6 | 300±60 | 63.0 |
| Total fat, % energy |
33.9±5.3 | 52.2 | 33.3±4.4 | 57.3 | 32.5±4.5 | 59.3 | 33.1±3.4 | 56.8 | 29.8±5.4 | 66.6 | 30.6±4.0 | 74.4 |
| Carbohydrate, % energy |
47.2±7.3 | NA | 50.1±6.6 | NA | 48.8±6.2 | NA | 51.1±5.4 | NA | 51.9±3.9 | NA | 54.3±5.6 | NA |
| Dietary fiber, g/d |
16.3±6.1 | 6.4 | 18.3±6.3 | 11.7 | 13.6±4.3 | 2.2 | 15.0±5.2 | 4.8 | 19.2±5.9 | 13.2 | 19.6±5.3 | 13.0 |
| Sodium, g/d | 3.4±0.6 | 6.5 | 3.6±0.5 | 4.6 | 3.3±0.6 | 11.5 | 3.5±0.4 | 6.0 | 3.2±0.5 | 10.3 | 3.4±0.5 | 9.5 |
Unpublished data from National Health and Nutrition Examination Survey 2009 to 2010, derived from two 24-h dietary recalls per person, with population SDs adjusted for within-person vs between-person variation. All values are energy adjusted by individual regressions or percent energy, and for comparability, means and proportions are reported for a 2000-kcal/d diet. To obtain actual mean consumption levels, the group means for each food or nutrient can be multiplied by the group-specific total calories (kcal/d) divided by 2000 kcal/d.
ALA indicates α-linoleic acid; DHA, docosahexaenoic acid; EPA, eicosapentaenoic acid; NA, not available; NH, non-Hispanic; n-6-PUFA, ω-6-polyunsaturatedfatty acid; and SD, standard deviation.
Guidelines adjusted to a 2000-kcal/d diet. Whole grains (characterized as minimum 1.1 g of fiber per 10 g of carbohydrate), 3 or more 1-oz equivalent (1 oz of bread; 1 cup of dry cereal; 1/2 cup of cooked rice, pasta, or cereal) servings per d (Dietary Guidelines for Americans)129; fish or shellfish, 2 or more 100-g (3.5-oz) servings per wk129; fruits, 2 cups per d125; vegetables, 2 1/2 cups per d, including up to 3 cups per wk of starchy vegetables125; nuts, legumes, and seeds, 4 or more 50-g servings per wk129; processed meats (bacon, hot dogs, sausage, processed deli meats), 2 or fewer 100-g (3.5-oz) servings per wk (1/4 of discretionary calories)125; sugar-sweetened beverages (defined as ≥50 cal/8 oz, excluding whole juices), ≤36 oz per wk (≈1/4 of discretionary calories)125, 129; sweets and bakery desserts, 2.5 or fewer 50-g servings per wk (≈1/4 of discretionary calories)125, 129; EPA/DHA, ≥0.250 g/d130; ALA, ≥1.6/1.1 g/d (men/women)126; saturated fat, <10% energy; dietary cholesterol, <300 mg/d125; total fat, 20% to 35% energy125; dietary fiber, ≥28/d125; and sodium, <2.3 g/d.125
Table 5-2.
Dietary Consumption in 2009 to 2010 Among US Children and Teenagers of Selected Foods and Nutrients Related to Cardiometabolic Health
| Boys (5–9 y)
|
Girls (5–9 y)
|
Boys (10–14 y)
|
Girls (10–14 y)
|
Boys (15–19 y)
|
Girls (15–19 y)
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
|
| Foods | ||||||||||||
| Whole grains, servings/d |
0.8±0.5 | 2.9 | 0.8±0.5 | 4.7 | 0.9±0.8 | 5.3 | 0.7±0.3 | 3.4 | 0.9±0.6 | 5.2 | 0.9±1.1 | 6.9 |
| Fruits, servings/d |
1.6±1.2 | 10.4 | 1.7±0.9 | 9.6 | 1.3±1.7 | 7.6 | 1.3±0.8 | 8.1 | 1.2±1.4 | 4.8 | 0.9±1.0 | 5.0 |
| Fruits including 100% juices, servings/d |
3.2±1.8 | 34.8 | 3.3±1.7 | 31.6 | 2.6±2.3 | 24.1 | 2.7±3.2 | 24.7 | 2.6±2.4 | 23.4 | 2.3±1.1 | 21.8 |
| Vegetables including starch, servings/d |
0.9±0.6 | 0.5 | 1.0±0.4 | 0.3 | 0.8±0.4 | 0.3 | 1.3±0.4 | 1.8 | 1.2±0.8 | 3.1 | 1.1±0.4 | 0.8 |
| Vegetables including starch and juices/sauces, servings/d |
1.1±0.6 | 1.1 | 1.2±0.4 | 0.1 | 1.0±0.4 | 0.3 | 1.5±0.4 | 2.5 | 1.4±0.9 | 3.9 | 1.3±0.2 | 0.8 |
| Fish and shellfish, servings/wk |
0.4±0.3 | 8.9 | 0.6±0.3 | 11.0 | 0.5±0.3 | 10.2 | 0.3±0.3 | 4.7 | 0.9±0.9 | 10.7 | 0.5±1.2 | 9.2 |
| Nuts, legumes, and seeds, servings/wk |
1.4±1.6 | 12.5 | 1.9±1.5 | 14.4 | 1.5±0.7 | 12.8 | 1.7±0.7 | 11.4 | 1.5±0.5 | 12.4 | 1.9±0.5 | 13.5 |
| Processed meats, servings/wk |
2.4±1.2 | 51.5 | 1.8±0.4 | 61.5 | 2.8±1.9 | 48.1 | 2.5±1.5 | 53.1 | 3.2±1.5 | 50.5 | 2.3±1.5 | 59.7 |
| Sugar-sweetened beverages, servings/wk |
7.6±4.6 | 46.8 | 7.1±5.5 | 42.9 | 10.2±6.2 | 31.1 | 8.7±3.5 | 33.0 | 16.4±12.5 | 24.2 | 12.5±10.0 | 30.2 |
| Sweets and bakery desserts, servings/wk |
8.9±2.3 | 24.5 | 9.6±2.3 | 20.8 | 7.3±2.5 | 24.9 | 7.7±2.5 | 26.6 | 5.3±2.9 | 38.6 | 7.6±3.9 | 36.9 |
| Nutrients | ||||||||||||
| Total calories, kcal/d |
1828±276 | NA | 1757±312 | NA | 2163±560 | NA | 1865±377 | NA | 2532±500 | NA | 1836±308 | NA |
| EPA/DHA, g/d | 0.045±0.049 | 3.2 | 0.051±0.048 | 4.6 | 0.048±0.049 | 2.5 | 0.039±0.048 | 0.9 | 0.063±0.052 | 6.2 | 0.058±0.067 | 3.7 |
| ALA, g/d | 1.18±0.16 | 10.7 | 1.24±0.17 | 57.1 | 1.17±0.24 | 12.9 | 1.33±0.21 | 63.0 | 1.28±0.16 | 22.3 | 1.37±0.32 | 63.0 |
| n-6 PUFA, % energy |
6.6±1.2 | NA | 6.8±1.2 | NA | 6.7±0.9 | NA | 7.1±0.8 | NA | 6.9±0.5 | NA | 7.6±1.8 | NA |
| Saturated fat, % energy |
11.3±1.7 | 31.0 | 11.2±1.1 | 33.2 | 11.3±0.9 | 37.8 | 11.4±1.6 | 33.5 | 11.0±1.4 | 34.7 | 10.7±1.5 | 40.2 |
| Dietary cholesterol, mg/d |
225±46 | 80.6 | 234±64 | 75.3 | 234±90 | 82.9 | 250±48 | 75.2 | 230±68 | 82.2 | 240±67 | 75.8 |
| Total fat, % energy |
32.1±2.4 | 69.6 | 32.0±1.8 | 72.6 | 32.4±1.8 | 62.3 | 32.9±1.7 | 64.5 | 32.2±3.4 | 62.6 | 32.4±3.0 | 65.4 |
| Carbohydrate, % energy |
54.4±2.4 | NA | 54.8±2.2 | NA | 53.1±3.3 | NA | 53.1±3.3 | NA | 52.5±4.8 | NA | 53.2±3.8 | NA |
| Dietary fiber, g/d |
14.7±3.5 | 1.9 | 15.4±3.5 | 1.5 | 13.9±2.6 | 0.5 | 14.7±3.2 | 0.7 | 13.9±2.8 | 0.7 | 14.1±4.7 | 2.2 |
| Sodium, g/d | 3.3±0.4 | 5.5 | 3.3±0.4 | 4.8 | 3.4±0.3 | 2.7 | 3.5±0.2 | 2.3 | 3.4±0.4 | 8.7 | 3.5±0.4 | 5.0 |
Unpublished data from National Health and Nutrition Examination Survey 2009 to 2010, derived from two 24-h dietary recalls per person, with population SDs adjusted for within-person vs between-person variation. All values are energy adjusted by individual regressions or percent energy, and for comparability, means and proportions are reported for a 2000-kcal/d diet. To obtain actual mean consumption levels, the group means for each food or nutrient can be multiplied by the group-specific total calories (kcal/d) divided by 2000 kcal/d.
ALA indicates α-linoleic acid; DHA, docosahexaenoic acid; EPA, eicosapentaenoic acid; NA, not available; n-6-PUFA, ω-6-polyunsaturatedfatty acid; and SD, standard deviation.
For different age and sex subgroups here, the guideline cut points are standardized to a 2000-kcal/d diet to account for differences in caloric intake in these groups. Whole grains (characterized as minimum 1.1 g of fiber per 10 g of carbohydrate), 3 or more 1-oz equivalent (1 oz of bread; 1 cup of dry cereal; 1/2 cup of cooked rice, pasta, or cereal) servings per d (Dietary Guidelines for Americans)129; fish or shellfish, 2 or more 100-g (3.5-oz) servings per wk129; fruits, 2 cups per d125; vegetables, 2 1/2 cups per d, including up to 3 cups per wk of starchy vegetables125; nuts, legumes, and seeds, 4 or more 50-g servings per wk129; processed meats (bacon, hot dogs, sausage, processed deli meats), 2 or fewer 100-g (3.5-oz) servings per wk (1/4 of discretionary calories)125; sugar-sweetened beverages (defined as ≥50 cal/8 oz, excluding whole juices), ≤36 oz per wk (≈1/4 of discretionary calories)125,129; sweets and bakery desserts, 2.5 or fewer 50-g servings per wk (≈1/4 of discretionary calories)125,129; EPA/DHA, ≥0.250 g/d130; ALA, ≥1.6/1.1 g/d (men/women)126; saturated fat, <10% energy; dietary cholesterol, <300 mg/d125; total fat, 20% to 35% energy125; dietary fiber, ≥28/d125; and sodium, <2.3 g/d.125
Chart 5-1.
Age-adjusted trends in macronutrients and total calories consumed by US adults (20–74 years of age), 1971 to 2008. Data derived from National Center for Health Statistics14 and Wright and Wang.55
Chart 5-3.
Total US food expenditures away from home and at home, 1977 and 2007. Data derived from Davis and Saltos.66
This chapter of the Update highlights national dietary consumption data, focusing on key foods, nutrients, dietary patterns, and other dietary factors related to cardiometabolic health. It is intended to examine current intakes, trends and changes in intakes, and estimated effects on disease to support and further stimulate efforts to monitor and improve dietary habits in relation to cardiovascular health.
Abbreviations Used in Chapter 5
| ALA | α-linoleic acid |
| ARIC | Atherosclerosis Risk in Communities Study |
| BMI | body mass index |
| BP | blood pressure |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CHD | coronary heart disease |
| CHF | congestive heart failure |
| CI | confidence interval |
| CVD | cardiovascular disease |
| DASH | Dietary Approaches to Stop Hypertension |
| DBP | diastolic blood pressure |
| DHA | docosahexaenoic acid |
| DM | diabetes mellitus |
| EPA | eicosapentaenoic acid |
| GFR | glomerular filtration rate |
| GISSI | Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico |
| HD | heart disease |
| HDL | high-density lipoprotein |
| HEI | Healthy Eating Index |
| HF | heart failure |
| LDL | low-density lipoprotein |
| MI | myocardial infarction |
| n-6-PUFA | ω-6-polyunsaturated fatty acid |
| NA | not available |
| NH | non-Hispanic |
| NHANES | National Health and Nutrition Examination Survey |
| OR | odds ratio |
| PA | physical activity |
| RR | relative risk |
| SBP | systolic blood pressure |
| SD | standard deviation |
| WHI | Women’s Health Initiative |
Prevalence
Foods and Nutrients: Adults
(See Table 5-1; NHANES 2009–2010.)
The dietary consumption by US adults of selected foods and nutrients related to cardiometabolic health is detailed in Table 5-1 according to sex and race or ethnic subgroups:
Average consumption of whole grains was 1.1 servings per day by white men and women and 0.8 servings per day by black men and women, with only between 7% and 10% of white and black adults meeting guidelines of ≥3 servings per day. Average whole grain consumption by Mexican Americans was ≈2 servings per day, with 27% to 29% consuming ≥3 servings per day.
Average fruit consumption ranged from 1.2 to 1.9 servings per day in these sex and race or ethnic subgroups: 11% to 13% of whites, 7% to 8% of blacks, and 14% of Mexican Americans met guidelines of ≥2 cups per day. When 100% fruit juices were included, the number of servings increased, and the proportions of adults consuming ≥2 cups per day approximately doubled in whites and Mexican Americans and nearly quadrupled in blacks.
Average vegetable consumption ranged from 1.3 to 2.2 servings per day; 6% to 8% of whites, 2% to 5% of blacks, and 2 to 4% of Mexican Americans consumed ≥2.5 cups per day. The inclusion of vegetable juices and sauces generally produced little change in these consumption patterns.
Average consumption of fish and shellfish was lowest among Mexican American and white women (1.2 and 1.4 servings per week, respectively) and highest among black women (2.1 servings per week); ≈72% to 78% of all adults in each sex and race or ethnic subgroup consumed <2 servings per week. Approximately 9% to 10% of whites, 10% to 12% of blacks, and 7% to 13% of Mexican Americans consumed ≥250 mg of eicosapentaenoic acid and docosahexaenoic acid per day.
Average consumption of nuts, legumes, and seeds was ≈2.5 servings per week among whites and blacks and 5 to 8 servings per week among Mexican Americans. Approximately 22% of whites, 18% of blacks, and 40% of Mexican Americans met guidelines of ≥4 servings per week.
Average consumption of processed meats was lowest among Mexican American women (1.2 servings per week) and highest among black men (3.3 servings per week). Between 49% (black men) and 75% (Mexican American women) of adults consumed 2 or fewer servings per week.
Average consumption of sugar-sweetened beverages ranged from ≈6 servings per week among white women to 12 servings per week among Mexican American men. Women generally consumed less than men. From 29% (Mexican American men) to 68% (white women) of adults consumed no more than 36 oz (4.5 8-oz servings) per week.
Average consumption of sweets and bakery desserts ranged from ≈4.5 servings per day (Mexican Americans) to 7 servings per day (white women). Approximately two thirds of white women and more than half of all other sex and race groups consumed >2.5 servings per week.
Between 35% and 58% of adults in each sex and race or ethnic subgroup consumed <10% of total calories from saturated fat, and between 56% and 72% consumed <300 mg of dietary cholesterol per day.
Only 6% to 12% of whites, 2% to 5% of blacks, and 13% of Mexican Americans consumed ≥28 g of dietary fiber per day.
Only 5% to 7% of whites, 6% to 12% of blacks, and 10% of Mexican Americans consumed <2.3 g of sodium per day.
Foods and Nutrients: Children and Teenagers
(See Table 5-2; NHANES 2009–2010.)
The dietary consumption by US children and teenagers of selected foods and nutrients related to cardiometabolic health is detailed in Table 5-2:
Average whole grain consumption was low, <1 serving per day in all age and sex groups, with <7% of all children in different age and sex subgroups meeting guidelines of ≥3 servings per day.
Average fruit consumption was low and decreased with age: 1.6 to 1.7 servings per day in younger boys and girls (5–9 years of age), 1.3 servings per day in adolescent boys and girls (10–14 years of age), and 0.9 to 1.2 servings per day in teenage boys and girls (15–19 years of age). The proportion meeting guidelines of ≥2 cups per day was also low and decreased with age: ≈10% in those 5 to 9 years of age, 8% in those 10 to 14 years of age, and 5% in those 15 to 19 years of age. When 100% fruit juices were included, the number of servings consumed approximately doubled, and proportions consuming ≥2 cups per day increased to approximately one third of those 5 to 9 years of age and one fourth of those 10 to 14 years and 15 to 19 years of age.
Average vegetable consumption was low, ranging from 0.8 to 1.3 servings per day, with at most 3% of children in different age and sex subgroups meeting guidelines of ≥2.5 cups per day.
Average consumption of fish and shellfish was low, ranging between 0.3 and 0.9 servings per week in all age and sex groups. Among all ages, only 5% to 11% of youth consumed ≥2 servings per week.
Average consumption of nuts, legumes, and seeds ranged from 1.4 to 1.9 servings per week among different age and sex groups. Only between 11% and 14% of children in different age and sex subgroups consumed ≥4 servings per week.
Average consumption of processed meats ranged from ≈2 to 3 servings per week; was generally higher than the average consumption of nuts, legumes, and seeds; and was up to 8 times higher than the average consumption of fish and shellfish. Approximately 40% and 50% of children consumed >2 servings per week.
Average consumption of sugar-sweetened beverages was higher in boys than in girls and increased with age, from ≈7 to 8 servings per week in 5- to 9-year-olds, 9 to 10 servings per week in 10- to 14-year-olds, and 13 to 16 servings per week in 15- to 19-year-olds (each energy adjusted to 2000 kcal/d). This was generally considerably higher than the average consumption of whole grains, fruits, vegetables, fish and shellfish, or nuts, legumes, and seeds. Less than half of children 5 to 9 years of age and less than one quarter of boys 15 to 19 years of age consumed <4.5 servings per week.
Average consumption of sweets and bakery desserts was ≈9 to 10 servings per week in 5- to 9-year-olds, 7 to 8 servings per week in 10- to 14-year-olds, and 5 to 8 servings per week in 15- to 19-year-olds. From 61% (boys 15–19 years of age) to 79% (girls 5–9 years of age) of youths consumed >2.5 servings per week.
Average consumption of eicosapentaenoic acid and docosahexaenoic acid was low, ranging from 39 to 63 mg/d in boys and girls at all ages. Fewer than 6% of children and teenagers at any age consumed ≥250 mg/d.
Average consumption of saturated fat was ≈11% of calories, and average consumption of dietary cholesterol ranged from 225 to 250 mg/d. Approximately 30% to 40% of youth consumed <10% energy from saturated fat, and >75% consumed <300 mg of dietary cholesterol per day.
Average consumption of dietary fiber ranged from 14 to 15 g/d. Less than 2% of children in all age and sex subgroups consumed ≥28 g/d.
Average consumption of sodium ranged from 3.3 to 3.5 g/d. Only between 2% and 9% of children in different age and sex subgroups consumed <2.3 g/d.
Energy Balance
Energy balance, or consumption of total calories appropriate for needs, is determined by the balance of average calories consumed versus expended, with this balance depending on multiple factors, including calories consumed, PA, body size, age, sex, and underlying basal metabolic rate. Thus, one individual may consume relatively high calories but have negative energy balance (as a result of even greater calories expended), whereas another individual may consume relatively few calories but have positive energy balance (because of low calories expended). Given such variation, the most practical and reasonable method to assess energy balance in populations is to assess changes in weight over time (Trends section).
Average daily caloric intake in the United States is ≈2500 calories in adult men and 1800 calories in adult women (Table 5-1). In children and teenagers, average caloric intake is higher in boys than in girls and increases with age in boys (Table 5-2). Trends in energy balance are described below. The average US adult gains ≈1 lb per year. In an analysis of >120 000 US men and women in 3 separate US cohorts followed up for up to 20 years, changes in intakes of different foods and beverages were linked to long-term weight gain in different ways.1 Foods and beverages most positively linked to weight gain included refined grains, starches, and sugars, including potatoes, white bread, white rice, low-fiber breakfast cereals, sweets/desserts, and sugar-sweetened beverages, as well as red and processed meats. In contrast, increased consumption of several other foods, including nuts, whole grains, fruits, vegetables, and yogurt, was linked to relative weight loss over time. These findings indicate that attention to dietary quality, not simply counting total calories, is crucial for energy balance.1
Diet quality also appears to influence energy expenditure. After intentional weight loss, isocaloric diets higher in fat and lower in rapidly digestible carbohydrates produced significantly smaller declines in total energy expenditure than low-fat, high-carbohydrate diets.2 Similarly, isocaloric meals richer in rapidly digestible carbohydrate increased hunger and stimulated brain regions associated with reward and craving compared with isocaloric meals lower in rapidly digestible carbohydrate.3
Other nutritional determinants of positive energy balance (more calories consumed than expended), as determined by adiposity or weight gain, include larger portion sizes4,5 and greater consumption of fast food and commercially prepared meals.6–10
Preferences for portion size are associated with BMI, socioeconomic status, eating in fast food restaurants, and television watching.11,12 Portion sizes are larger at fast food restaurants than at home or at other restaurants.13
Between 1999 and 2004, 53% of Americans consumed an average of 1 to 3 restaurant meals per week, and 23% consumed ≥4 restaurant meals per week.14 Spending on food away from home, including restaurant meals, catered foods, and food eaten during out-of-town trips, increased from 26% of average annual food expenditures in 1970 to 42% in 2004.14
Macronutrient composition of the overall diet or of specific foods, such as percentage of calories from total fat, does not appear to be strongly associated with energy balance as ascertained by weight gain or loss.1,15–17 In contrast, dietary quality as characterized by higher or lower intakes of specific foods and beverages is strongly linked to weight gain (see above).1
Emerging evidence suggests that consumption of trans fat may be associated with energy imbalance as assessed by changes in adiposity or weight, as well as more specific adverse effects on visceral adiposity.18–20
Other individual factors associated with positive energy balance (weight gain) include greater television watching (with evidence that effects are mediated by diet, rather than physical inactivity, including greater snacking in front of the television and the influence of advertising on poor food choices)1,21–25 and lower average sleep duration.1,26
Randomized controlled trials of weight loss in obese individuals generally show modestly greater weight loss with low-carbohydrate (high-fat) diets than with low-fat diets at 6 months, but at 1 year, such differences diminish, and a diet that focuses on dietary quality and whole foods may be most successful in the long term.27–30
A comparison of BRFSS data in 1996 and 2003 suggested a shift in self-reported dietary strategies to lose weight, with the proportion focusing on calorie restriction increasing from 11.3% to 24.9% and the proportion focusing on restricting fat consumption decreasing from 41.6% to 29.1%.31
On the basis of BRFSS data from 2003, among all American adults who were overweight or obese, a higher proportion was trying to lose weight if also diagnosed with hypertension (58% trying to lose weight), DM (60%), or both diseases (72%) than adults with neither condition (50%).32
A 2007 to 2008 national survey of 1082 retail stores in 19 US cities found that energy-dense snack foods/beverages were present in 96% of pharmacies, 94% of gas stations, 22% of furniture stores, 16% of apparel stores, and 29% to 65% of other types of stores.33
Societal and environmental factors independently associated with energy imbalance (weight gain), via either increased caloric consumption or decreased expenditure, include education, income, race/ethnicity, and local conditions such as availability of grocery stores, types of restaurants, safety, parks and open spaces, and walking or biking paths.34–36 PA is covered in Chapter 4 of this update.
Dietary Patterns
In addition to individual foods and nutrients, overall dietary patterns can be used to assess more global dietary quality. Different dietary patterns have been defined, including the HEI, Alternative HEI, Western versus prudent dietary patterns, Mediterranean dietary pattern, and DASH-type diet. The higher-monounsaturated-fat DASH-type diet is generally similar to a traditional Mediterranean dietary pattern.37
In 1999 to 2004, only 19.4% of hypertensive US adults were following a DASH-type diet (based on intake of fiber, magnesium, calcium, sodium, potassium, protein, total fat, saturated fat, and cholesterol). This represented a decrease from 26.7% of hypertensive US adults in 1988 to 1994.38
Among older US adults (≥60 years of age) in 1999 to 2002, 72% met guidelines for dietary cholesterol intake, but only between 18% and 32% met guidelines for the HEI food groups (meats, dairy, fruits, vegetables, and grains). On the basis of the HEI score, only 17% of older US adults consumed a good-quality diet. Higher HEI scores were seen in white adults and individuals with greater education; lower HEI scores were seen in black adults and smokers.39
Dietary Supplements
Use of dietary supplements is common in the United States among both adults and children:
Approximately half of US adults in 2007 to 2010 used ≥1 dietary supplement, with the most common supplement being multivitamin-multimineral products (32% of men and women reporting use).40 It has been shown that most supplements are taken daily and for ≥2 years.41 Supplement use is associated with older age, higher education, greater PA, moderate alcohol consumption, lower BMI, abstinence from smoking, having health insurance, and white race.40,41 Previous research also suggests that supplement users have higher intakes of most vitamins and minerals from their food choices alone than nonusers.42,43 The primary reasons US adults in 2007 to 2010 reported for using dietary supplements were to “improve overall health” (45%) and to “maintain health” (33%).40
One third (32%) of US children (birth to 18 years of age) used dietary supplements in 1999 to 2002, with the highest use (48.5%) occurring among 4- to 8-year-olds. The most common supplements were multivitamins and multiminerals (58% of supplement users). The primary nutrients supplemented (either by multivitamins or individual vitamins) included vitamin C (29% of US children), vitamin A (26%), vitamin D (26%), calcium (21%), and iron (19%). Supplement use was associated with higher family income, a smoke-free home environment, lower child BMI, and less screen time (television, video games, or computers).44
In a 2005 to 2006 telephone survey of US adults, 41.3% were making or had made in the past a serious weight-loss attempt. Of these, one third (33.9%) had used a dietary supplement for weight loss, with such use being more common in women (44.9%) than in men (19.8%) and in blacks (48.7%) or Hispanics (41.6%) than in whites (31.2%); in those with high school education or less (38.4%) than in those with some college or more (31.1%); and in those with household income <$40 000 per year (41.8%) than in those with higher incomes (30.3%).45
Multiple trials of most dietary supplements, including folate, vitamin C, and vitamin E, have generally shown no significant benefits for CVD risk, and even potential for harm.36 For example, a multicenter randomized trial in patients with diabetic nephropathy found that B vitamin supplementation (folic acid 2.5 mg/d, vitamin B6 25 mg/d, and vitamin B12 1 mg/d) decreased GFR and increased risk of MI and stroke compared with placebo.46
Fish oil supplements at doses of 1 to 2 g/d have shown CVD benefits in 2 large randomized, open-label trials and 1 large randomized, placebo-controlled trial (GISSI-Prevenzione, Japan Eicosapentaenoic Acid Lipid Intervention Study, and GISSI-HF),47–49 but several other trials of fish oil have not shown significant effects on CVD risk.50 A meta-analysis of all randomized controlled clinical trials demonstrated a significant reduction for cardiac mortality but no statistically significant effects on other CVD end points.51
Trends
Energy Balance
(See Chart 5-1.)
Energy balance, or consumption of total calories appropriate for needs, has been steadily worsening in the United States over the past several decades, as evidenced by the dramatic increases over the past 30 years in overweight and obesity among both children and adults across broad cross sections of sex, race/ethnicity, geographic residence, and socioeconomic status. However, in more recent years, rates of obesity and overweight among both adults and children have begun to level off.52–54
The US obesity epidemic began in approximately 1980, accelerated from 1990 to 2005, and may be slowing in more recent years. Examining trends in diet, activity, and other factors from 1980 to present is important to elucidate the drivers of this remarkably recent epidemic.
Although trends in total calories consumed are difficult to quantify exactly because of differing methods of serial national dietary surveys over time, multiple lines of evidence indicate that average total energy consumption has increased by ≥200 kcal/d per person in the past 3 decades.
Data from NHANES indicate that between 1971 and 2004, average total energy consumption among US adults increased by 22% in women (from 1542 to 1886 kcal/d) and by 10% in men (from 2450 to 2693 kcal/d).14 These increases are supported by data from 2 older surveys, the Nationwide Food Consumption Survey (1977–1978) and the Continuing Surveys of Food Intake (1989–1998).13 However, recent data show that energy intake appeared relatively stable among US adults during 1999 to 2008.55
The increases in calories consumed between 1971 and 2004 are attributable primarily to greater average carbohydrate intake, particularly of starches, refined grains, and sugars (Foods and Nutrients section). Other specific changes related to increased caloric intake in the United States include larger portion sizes, greater food quantity and calories per meal, and increased consumption of sugar-sweetened beverages, snacks, commercially prepared (especially fast-food) meals, and higher-energy-density foods.7,13,56–60
Between 1977 and 1996, the average portion sizes for nearly all foods increased at fast-food outlets, other restaurants, and home. These included a 33% increase in the average portion of Mexican food (from 408 to 541 calories), a 34% increase in the average portion of cheeseburgers (from 397 to 533 calories), a 36% increase in the average portion of French fries (from 188 to 256 calories), and a 70% increase in the average portion of salty snacks such as crackers, potato chips, pretzels, puffed rice cakes, and popcorn (from 132 to 225 calories).13
Among US children 2 to 7 years of age, an estimated energy imbalance of only 110 to 165 kcal/d (the equivalent of one 12- to 16-oz bottle of soda/cola) was sufficient to account for the excess weight gain between 1988 and 1994 and 1999 and 2002.61
In a quantitative analysis using various US surveys between 1977 and 2006, the relations of changes in energy density, portion sizes, and number of daily eating/drinking occasions to changes in total energy intake were assessed.62 Decreases in energy density were actually linked to lower total energy intake over time, whereas increases in both portion size and number of eating occasions were linked to greater energy intake.
Among US children 2 to 18 years of age, increases in energy intake between 1977 and 2006 (179 kcal/d) were entirely attributable to substantial increases in energy eaten away from home (255 kcal/d).63 The percentage of energy eaten away from home increased from 23.4% to 33.9% during this time, with a shift toward energy from fast food as the largest contributor to foods away from home for all age groups.
A county-level investigation based on BRFSS and NHANES data found that prevalence of sufficient PA in the United States increased from 2001 to 2009 but that this was matched by increases in obesity in almost all counties during the same time period, with low correlation between level of PA and obesity in US counties.64
Foods and Nutrients
Several changes in foods and nutrients have occurred over time. Selected changes are highlighted below.
Macronutrients
(See Chart 5-1.)
Starting in 1977 and continuing until the most recent dietary guidelines revision in 2010, a major focus of US dietary guidelines was reduction of dietary fats.65 During this time, average total fat consumption declined as a percent of calories from 36.9% to 33.4% in men and from 36.1% to 33.8% in women.14 However, more recent analyses show that there were no significant trends in total fat intake among US adults from 1999 to 2008.55
Dietary guidelines during this time also emphasized carbohydrate consumption as the base of one’s dietary pattern66 and more recently specified the importance of complex rather than refined carbohydrates (eg, as the base of the Food Guide Pyramid).65 From 1971 to 2004, total carbohydrate intake increased from 42.4% to 48.2% of calories in men and from 45.4% to 50.6% of calories in women.14 Evaluated as absolute intakes, the increase in total calories consumed during this period was attributable primarily to the greater consumption of carbohydrates, both as foods (starches and grains) and as beverages.67,68 However, more recent analyses show that there has been a decrease in carbohydrate intake (expressed as percentage of energy) among US adults from 1999 to 2008.55
Sugar-Sweetened Beverages
(See Chart 5-2.)
Chart 5-2.
Per capita calories consumed from different beverages by US adults (≥19 years of age), 1965 to 2010. Source: Nationwide Food Consumption Surveys (1965, 1977–1978) and National Health and Nutrition Examination Survey (1988–2010), based on data from Duffey and Popkin62 and Kit et al.69 The 2010 data were only analyzed for soda/cola and sweetened fruit drinks.
Between 1965 and 2002, the average percentage of total calories consumed from beverages in the United States increased from 11.8% to 21.0% of energy, which represents an overall absolute increase of 222 kcal/d per person.59 This increase was largely caused by increased consumption of sugar-sweetened beverages and alcohol: Average consumption of fruit juices went from 20 to 39 kcal/d; of milk, from 125 to 94 kcal/d; of alcohol, from 26 to 99 kcal/d; of sweetened fruit drinks, from 13 to 38 kcal/d; and of soda/cola, from 35 to 143 kcal/d.62
In contrast, between 1999 and 2010, sugar-sweetened beverage intake decreased among both youth and adults in the United States, consistent with increased attention to their importance as a cause of obesity. In 2009 to 2010, youth and adults consumed a daily average of 155 and 151 kcal/d from sugar-sweetened beverages, respectively, a decrease from 1999 to 2000 of 68 and 45 kcal/d, respectively.69
In addition to increased overall consumption, the average portion size of a single sugar-sweetened beverage increased by >50% between 1977 and 1996, from 13.1 to 19.9 fl oz.13
Among children and teenagers (2–19 years of age), the largest increases in consumption of sugar-sweetened beverages between 1988 to 1994 and 1999 to 2004 were seen among black and Mexican American youths compared with white youths.60
Fruits and Vegetables
Between 1994 and 2005, the average consumption of fruits and vegetables declined slightly, from a total of 3.4 to 3.2 servings per day. The proportions of men and women consuming combined fruits and vegetables ≥5 times per day were low (≈20% and 29%, respectively) and did not change during this period.70
Morbidity and Mortality
Effects on Cardiovascular Risk Factors
Dietary habits affect multiple cardiovascular risk factors, including both established risk factors (SBP, DBP, LDL cholesterol levels, HDL cholesterol levels, glucose levels, and obesity/weight gain) and novel risk factors (eg, inflammation, cardiac arrhythmias, endothelial cell function, triglyceride levels, lipoprotein[a] levels, and heart rate):
A DASH dietary pattern with low sodium reduced SBP by 7.1 mm Hg in adults without hypertension and by 11.5 mm Hg in adults with hypertension.71
Compared with the low-fat DASH diet, DASH-type diets that increased consumption of either protein or unsaturated fat had similar or greater beneficial effects on CVD risk factors. Compared with a baseline usual diet, each of the DASH-type diets, which included various percentages (27%–37%) of total fat and focused on whole foods such as fruits, vegetables, whole grains, and fish, as well as potassium and other minerals and low sodium, reduced SBP by 8 to 10 mm Hg, DBP by 4 to 5 mm Hg, and LDL cholesterol by 12 to 14 mg/dL. The diets that had higher levels of protein and unsaturated fat also lowered triglyceride levels by 16 and 9 mg/dL, respectively.72 The DASH-type diet higher in unsaturated fat also improved glucose-insulin homeostasis compared with the low-fat/high-carbohydrate DASH diet.73
In a meta-analysis of randomized controlled trials, consumption of 1% of calories from trans fat in place of saturated fat, monounsaturated fat, or polyunsaturated fat, respectively, increased the ratio of total to HDL cholesterol by 0.031, 0.054, and 0.67; increased apolipoprotein B levels by 3, 10, and 11 mg/L; decreased apolipoprotein A-1 levels by 7, 5, and 3 mg/L; and increased lipoprotein(a) levels by 3.8, 1.4, and 1.1 mg/L.74
In meta-analyses of randomized controlled trials, consumption of eicosapentaenoic acid and docosahexaenoic acid for 212 weeks lowered SBP by 2.1 mm Hg75 and lowered resting heart rate by 2.5 beats per minute.76
In a pooled analysis of 25 randomized trials totaling 583 men and women both with and without hypercholesterolemia, nut consumption significantly improved blood lipid levels.77 For a mean consumption of 67 g of nuts per day, total cholesterol was reduced by 10.9 mg/dL (5.1%), LDL cholesterol by 10.2 mg/dL (7.4%), and the ratio of total cholesterol to HDL cholesterol by 0.24 (5.6% change; P<0.001 for each). Triglyceride levels were also reduced by 20.6 mg/dL (10.2%) in subjects with high triglycerides (2150 mg/dL). Different types of nuts had similar effects.77
A review of cross-sectional and prospective cohort studies suggests that higher intake of sugar-sweetened beverages is associated with greater visceral fat and higher risk of type 2 DM.78 Two randomized trials have confirmed that reducing intake of sugar-sweetened beverages reduces weight gain in children.79,80
In a randomized controlled trial, compared with a low-fat diet, 2 Mediterranean dietary patterns that included either virgin olive oil or mixed nuts lowered SBP by 5.9 and 7.1 mm Hg, plasma glucose by 7.0 and 5.4 mg/dL, fasting insulin by 16.7 and 20.4 pmol/L, the homeostasis model assessment index by 0.9 and 1.1, and the ratio of total to HDL cholesterol by 0.38 and 0.26 and raised HDL cholesterol by 2.9 and 1.6 mg/dL, respectively. The Mediterranean dietary patterns also lowered levels of C-reactive protein, interleukin-6, intercellular adhesion molecule-1, and vascular cell adhesion molecule-1.81
Effects on Cardiovascular Outcomes
Because dietary habits affect a broad range of established and novel risk factors, estimation of the impact of nutritional factors on cardiovascular health by considering only a limited number of pathways (eg, only effects on lipids, BP, and obesity) will systematically underestimate or even misconstrue the actual total impact on cardiovascular health. Randomized controlled trials and prospective observational studies have been used to quantify the total effects of dietary habits on clinical outcomes.
Fats and Carbohydrates
In the WHI randomized clinical trial (n=48 835), reduction of total fat consumption from 37.8% energy (baseline) to 24.3% energy (at 1 year) and 28.8% energy (at 6 years) had no effect on incidence of CHD (RR, 0.98; 95% CI, 0.88–1.09), stroke (RR, 1.02; 95% CI, 0.90–1.15), or total CVD (RR, 0.98; 95% CI, 0.92–1.05) over a mean of 8.1 years.82 This was consistent with null results of 4 prior randomized clinical trials and multiple large prospective cohort studies that indicated little effect of total fat consumption on CVD risk.83
In 3 separate meta-analyses of prospective cohort studies, the largest of which included 21 studies with up to 2 decades of follow-up, saturated fat consumption overall had no significant association with incidence of CHD, stroke, or total CVD.84–86 In comparison, in a pooled individual-level analysis of 11 prospective cohort studies, the specific exchange of polyunsaturated fat consumption in place of saturated fat was associated with lower CHD risk, with 13% lower risk for each 5% energy exchange (RR, 0.87; 95% CI, 0.70–0.97).87 These findings are consistent with a meta-analysis of randomized controlled trials in which increased polyunsaturated fat consumption in place of saturated fat reduced CHD events, with 10% lower risk for each 5% energy exchange (RR, 0.90; 95% CI, 0.83–0.97).88
In a pooled analysis of individual-level data from 11 prospective cohort studies in the United States, Europe, and Israel that included 344 696 participants, each 5% higher energy consumption of carbohydrate in place of saturated fat was associated with a 7% higher risk of CHD (RR, 1.07; 95% CI, 1.01–1.14).87 Each 5% higher energy consumption of monounsaturated fat in place of saturated fat was not significantly associated with CHD risk.87
Together these findings suggest that reducing saturated fat without specifying the replacement may have minimal effects on CHD risk, whereas increasing polyunsaturated fats from vegetable oils will reduce CHD.37
In a meta-analysis of prospective cohort studies, each 2% of calories from trans fat was associated with a 23% higher risk of CHD (RR, 1.23; 95% CI, 1.11–1.37).89
In meta-analyses of prospective cohort studies, greater consumption of refined complex carbohydrates, starches, and sugars, as assessed by glycemic index or load, was associated with significantly higher risk of CHD and DM. When the highest category was compared with the lowest category, risk of CHD was 36% greater (glycemic load: RR, 1.36; 95% CI, 1.13–1.63), and risk of DM was 40% greater (glycemic index: RR, 1.40; 95% CI, 1.23–1.59).90,91
Foods and Beverages
In meta-analyses of prospective cohort studies, each daily serving of fruits or vegetables was associated with a 4% lower risk of CHD (RR, 0.96; 95% CI, 0.93–0.99) and a 5% lower risk of stroke (RR, 0.95; 95% CI, 0.92–0.97).92,93
In a meta-analysis of prospective cohort studies, greater whole grain intake (2.5 compared with 0.2 servings per day) was associated with a 21% lower risk of CVD events (RR, 0.79; 95% CI, 0.73–0.85), with similar estimates in men and women and for various outcomes (CHD, stroke, and fatal CVD). In contrast, refined grain intake was not associated with lower risk of CVD (RR, 1.07; 95% CI, 0.94–1.22).94
In a meta-analysis of 16 prospective cohort studies that included 326 572 generally healthy individuals in Europe, the United States, China, and Japan, fish consumption was associated with significantly lower risk of CHD mortality.95 Compared with no consumption, an estimated 250 mg of long-chain omega-3 fatty acids per day was associated with 35% lower risk of CHD death (P<0.001).
In a meta-analysis of prospective cohort and case-control studies from multiple countries, consumption of unprocessed red meat was not significantly associated with incidence of CHD. In contrast, each 50-g serving per day of processed meats (eg, sausage, bacon, hot dogs, deli meats) was associated with a higher incidence of CHD (RR, 1.42; 95% CI, 1.07–1.89).96
In a meta-analysis of prospective cohort studies that included 442 101 participants and 28 228 DM cases, unprocessed red meat consumption was associated with a higher risk of DM (RR, 1.19; 95% CI, 1.04–1.37, per 100 g/d). On a per g/d basis, risk of DM was nearly 7-fold higher for processed meat consumption (RR, 1.51; 95% CI, 1.25–1.83, per 50 g/d).97
In a meta-analysis of 6 prospective observational studies, nut consumption was associated with significantly lower incidence of CHD (comparing higher to low intake: RR, 0.70; 95% CI, 0.57–0.82).85
Higher consumption of dairy or milk products is associated with lower incidence of DM and trends toward lower risk of stroke.77,90,91 Some limited evidence suggests that these associations are stronger for low-fat dairy or milk than for other dairy products. Dairy consumption is not significantly associated with higher or lower risk of CHD.85,98
Among 88 520 generally healthy women in the Nurses’ Health Study who were 34 to 59 years of age in 1980 and were followed up from 1980 to 2004, regular consumption of sugar-sweetened beverages was independently associated with higher incidence of CHD, with 23% and 35% higher risk with 1 and ≥2 servings per day, respectively, compared with <1 per month.99 Among the 15 745 participants in the ARIC study, the OR for developing CHD was 2.59 for participants who had a serum uric acid level >9.0 mg/dL and who drank >1 sugar-sweetened soda per day.100
Sodium and Potassium
Lower estimated consumption of dietary sodium was not associated with lower CVD mortality in NHANES,101 although such findings may be limited by changes in behaviors that result from underlying risk (reverse causation). In a post hoc analysis of the Trials of Hypertension Prevention, participants randomized to low-sodium interventions had a 25% lower risk of CVD (RR, 0.75; 95% CI, 0.57–0.99) after 10 to 15 years of follow-up after the original trials.102
In a meta-analysis of small randomized trials of sodium reduction of ≥6 months’ duration, nonsignificant trends were seen toward fewer CVD events in subjects with normal BP (RR, 0.71; 95% CI, 0.42–1.20; n=200 events) or hypertension (RR, 0.84; 95% CI, 0.57–1.23; n=93 events), but findings were not statistically significant, with relatively low statistical power because of the small numbers of events. Sodium restriction increased total mortality in trials of patients with CHF (RR, 2.59; 95% CI, 1.04–6.44), but these data were based on very few events (n=21 deaths).103
In a meta-analysis of 13 prospective cohorts that included 177 025 participants and >11 000 vascular events, higher sodium consumption was associated with greater risk of stroke (pooled RR, 1.23; 95% CI, 1.06–1.43; P=0.007) and a trend toward higher risk of CVD (1.14; 95% CI, 0.99–1.32; P=0.07). These associations were greater with larger differences in sodium intake and longer follow-up.104
In a meta-analysis of 15 prospective cohort samples that included 247 510 participants and 7066 strokes, 3058 CHD events, and 2497 total CVD events, each 1.64-g/d (42 mmol/d) higher potassium intake was associated with a 21% lower risk of stroke (RR, 0.79; 95% CI, 0.68–0.90) and trends toward lower risk of CHD and total CVD.105
Dietary Patterns
In a cohort of 380 296 US men and women, greater versus lower adherence to a Mediterranean dietary pattern, characterized by higher intakes of vegetables, legumes, nuts, fruits, whole grains, fish, and unsaturated fat and lower intakes of red and processed meat, was associated with a 22% lower cardiovascular mortality (RR, 0.78; 95% CI, 0.69–0.87).106 Similar findings have been seen for the Mediterranean dietary pattern and risk of incident CHD and stroke107 and for the DASH-type dietary pattern.108
In a cohort of 72 113 US female nurses, a dietary pattern characterized by higher intakes of vegetables, fruits, legumes, fish, poultry, and whole grains was associated with a 28% lower cardiovascular mortality (RR, 0.72; 95% CI, 0.60–0.87), whereas a dietary pattern characterized by higher intakes of processed meat, red meat, refined grains, French fries, and sweets/desserts was associated with a 22% higher cardiovascular mortality (RR, 1.22; 95% CI, 1.01–1.48).109 Similar findings have been seen in other cohorts and for other outcomes, including development of DM and metabolic syndrome.110–116
The observational findings for benefits of a healthy food–based dietary pattern have been confirmed in 2 randomized clinical trials, including a small secondary prevention trial in France among patients with recent MI117 and a large primary prevention trial in Spain among patients with CVD risk factors.118 The latter trial demonstrated a 30% reduction in the risk of stroke, MI, and death attributable to cardiovascular causes in those patients randomized to Mediterranean-style diets.
Impact on US Mortality
One report used consistent and comparable risk assessment methods and nationally representative data to estimate the impact of all major modifiable risk factors on mortality and morbidity in the United States in 1990 and 2010.119 Suboptimal dietary habits were the leading cause of both mortality and disability-adjusted life-years lost, exceeding even tobacco. In 2010, a total of 678 000 deaths of all causes were attributable to suboptimal diet.
A previous investigation reported the estimated mortality effects of several specific dietary risk factors in 2005 in the United States. High dietary salt consumption was estimated to be responsible for 102 000 annual deaths, low dietary omega-3 fatty acids for 84 000 annual deaths, high dietary trans fatty acids for 82 000 annual deaths, and low consumption of fruits and vegetables for 55 000 annual deaths.120
Cost
(See Chart 5-3.)
The US Department of Agriculture forecast that the Consumer Price Index for all food would increase 3.0% to 4.0% in 2013 as retailers continued to pass on higher commodity and energy costs to consumers in the form of higher retail prices. The Consumer Price Index for food increased 3.7% in 2011. Prices for foods eaten at home increased 4.8% in 2011, whereas prices for foods eaten away from home increased by 1.9%.121
The proportion of total US food expenditures for meals outside the home, as a share of total food dollars, increased from 27% in 1961 to 40% in 1981 to 49% in 2011.66
The proportion of sales of meals and snacks from fast-food restaurants compared with total meals and snacks away from home increased from 5% in 1958 to 29% in 1982 to 36% in 2011.121
As a proportion of income, food has become less expensive over time in the United States. As a share of personal disposable income, average (mean) total food expenditures by families and individuals have decreased from 22.3% (1949) to 18.1% (1961) to 14.9% (1981) to 11.3% (2011). For any given year, the share of disposable income spent on food is inversely proportional to absolute income. The share increases as absolute income levels decline.121
Among 153 forms of fruits and vegetables priced with 2008 Nielsen Homescan data, price and calorie per portion of 20 fruits and vegetables were compared with 20 common snack foods such as cookies, chips, pastries, and crackers. Average price per portion of fruits and vegetables was 31 cents with an average of 57 calories per portion, compared with 33 cents and 183 calories per portion for snack foods.121
An overview of the costs of various strategies for primary prevention of CVD determined that the estimated costs per year of life gained were between $9800 and $18 000 for statin therapy, ≈$1500 for nurse screening and lifestyle advice, $500 to $1250 for smoking cessation, and $20 to $900 for population-based healthy eating.122
Each year, >$33 billion in medical costs and $9 billion in lost productivity resulting from HD, cancer, stroke, and DM are attributed to poor nutrition.123–126
Two separate cost-effectiveness analyses estimated that population reductions in dietary salt would not only be cost-effective but actually cost-saving.127,128 In 1 analysis, a 1.2-g/d reduction in dietary sodium was projected to reduce US annual cases of incident CHD by 60 000 to 120 000, stroke by 32 000 to 66 000, and total mortality by 44 000 to 92 000.128 If accomplished through a regulatory intervention, estimated savings in healthcare costs would be $10 to $24 billion annually.128 Such an intervention would be more cost-effective than using medications to lower BP in all people with hypertension.
- 1.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364:2392–2404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ebbeling CB, Swain JF, Feldman HA, Wong WW, Hachey DL, Garcia-Lago E, Ludwig DS. Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA. 2012;307:2627–2634. doi: 10.1001/jama.2012.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lennerz BS, Alsop DC, Holsen LM, Stern E, Rojas R, Ebbeling CB, Goldstein JM, Ludwig DS. Effects of dietary glycemic index on brain regions related to reward and craving in men. Am J Clin Nutr. 2013;98:641–647. doi: 10.3945/ajcn.113.064113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ello-Martin JA, Ledikwe JH, Rolls BJ. The influence of food portion size and energy density on energy intake: implications for weight management. Am J Clin Nutr. 2005;82(suppl):236S–241S. doi: 10.1093/ajcn/82.1.236S. [DOI] [PubMed] [Google Scholar]
- 5.Fisher JO, Kral TV. Super-size me: portion size effects on young children’s eating. Physiol Behav. 2008;94:39–47. doi: 10.1016/j.physbeh.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Bowman SA, Vinyard BT. Fast food consumption of U.S. adults: impact on energy and nutrient intakes and overweight status. J Am Coll Nutr. 2004;23:163–168. doi: 10.1080/07315724.2004.10719357. [DOI] [PubMed] [Google Scholar]
- 7.Kant AK, Graubard BI. Eating out in America, 1987–2000: trends and nutritional correlates. Prev Med. 2004;38:243–249. doi: 10.1016/j.ypmed.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Duerksen SC, Elder JP, Arredondo EM, Ayala GX, Slymen DJ, Campbell NR, Baquero B. Family restaurant choices are associated with child and adult overweight status in Mexican-American families. J Am Diet Assoc. 2007;107:849–853. doi: 10.1016/j.jada.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 9.Duffey KJ, Gordon-Larsen P, Jacobs DR, Jr, Williams OD, Popkin BM. Differential associations of fast food and restaurant food consumption with 3-y change in body mass index: the Coronary Artery Risk Development in Young Adults Study. Am J Clin Nutr. 2007;85:201–208. doi: 10.1093/ajcn/85.1.201. [DOI] [PubMed] [Google Scholar]
- 10.Rosenheck R. Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev. 2008;9:535–547. doi: 10.1111/j.1467-789X.2008.00477.x. [DOI] [PubMed] [Google Scholar]
- 11.Burger KS, Kern M, Coleman KJ. Characteristics of self-selected portion size in young adults. J Am Diet Assoc. 2007;107:611–618. doi: 10.1016/j.jada.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Colapinto CK, Fitzgerald A, Taper LJ, Veugelers PJ. Children’s preference for large portions: prevalence, determinants, and consequences. J Am Diet Assoc. 2007;107:1183–1190. doi: 10.1016/j.jada.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 13.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977–1998. JAMA. 2003;289:450–453. doi: 10.1001/jama.289.4.450. [DOI] [PubMed] [Google Scholar]
- 14.National Center for Health Statistics. Health, United States, 2007: With Chartbook on Trends in the Health of Americans. Hyattsville, MD: National Center for Health Statistics; 2008. [Accessed July 20, 2011]. http://www.cdc.gov/nchs/data/hus/hus07.pdf. [Google Scholar]
- 15.Willett WC, Leibel RL. Dietary fat is not a major determinant of body fat. Am J Med. 2002;113(suppl 9B):47S–59S. doi: 10.1016/s0002-9343(01)00992-5. [DOI] [PubMed] [Google Scholar]
- 16.Brehm BJ, D’Alessio DA. Weight loss and metabolic benefits with diets of varying fat and carbohydrate content: separating the wheat from the chaff. Nat Clin Pract Endocrinol Metab. 2008;4:140–146. doi: 10.1038/ncpendmet0730. [DOI] [PubMed] [Google Scholar]
- 17.van Dam RM, Seidell JC. Carbohydrate intake and obesity. Eur J Clin Nutr. 2007;61(suppl 1):S75–S99. doi: 10.1038/sj.ejcn.1602939. [DOI] [PubMed] [Google Scholar]
- 18.Koh-Banerjee P, Chu NF, Spiegelman D, Rosner B, Colditz G, Willett W, Rimm E. Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16 587 US men. Am J Clin Nutr. 2003;78:719–727. doi: 10.1093/ajcn/78.4.719. [DOI] [PubMed] [Google Scholar]
- 19.Field AE, Willett WC, Lissner L, Colditz GA. Dietary fat and weight gain among women in the Nurses’ Health Study. Obesity (Silver Spring) 2007;15:967–976. doi: 10.1038/oby.2007.616. [DOI] [PubMed] [Google Scholar]
- 20.Kavanagh K, Jones KL, Sawyer J, Kelley K, Carr JJ, Wagner JD, Rudel LL. Trans fat diet induces abdominal obesity and changes in insulin sensitivity in monkeys. Obesity (Silver Spring) 2007;15:1675–1684. doi: 10.1038/oby.2007.200. [DOI] [PubMed] [Google Scholar]
- 21.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 22.Gable S, Chang Y, Krull JL. Television watching and frequency of family meals are predictive of overweight onset and persistence in a national sample of school-aged children. J Am Diet Assoc. 2007;107:53–61. doi: 10.1016/j.jada.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 23.Temple JL, Giacomelli AM, Kent KM, Roemmich JN, Epstein LH. Television watching increases motivated responding for food and energy intake in children. Am J Clin Nutr. 2007;85:355–361. doi: 10.1093/ajcn/85.2.355. [DOI] [PubMed] [Google Scholar]
- 24.Dubois L, Farmer A, Girard M, Peterson K. Social factors and television use during meals and snacks is associated with higher BMI among preschool children. Public Health Nutr. 2008;11:1267–1279. doi: 10.1017/S1368980008002887. [DOI] [PubMed] [Google Scholar]
- 25.Epstein LH, Roemmich JN, Robinson JL, Paluch RA, Winiewicz DD, Fuerch JH, Robinson TN. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med. 2008;162:239–245. doi: 10.1001/archpediatrics.2007.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nordmann AJ, Nordmann A, Briel M, Keller U, Yancy WS, Jr, Brehm BJ, Bucher HC. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials [published correction appears in Arch Intern Med. 2006;166:932] Arch Intern Med. 2006;166:285–293. doi: 10.1001/archinte.166.3.285. [DOI] [PubMed] [Google Scholar]
- 28.Gardner CD, Kiazand A, Alhassan S, Kim S, Stafford RS, Balise RR, Kraemer HC, King AC. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial [published correction appears in JAMA. 2007;298:178] JAMA. 2007;297:969–977. doi: 10.1001/jama.297.9.969. [DOI] [PubMed] [Google Scholar]
- 29.Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, Golan R, Fraser D, Bolotin A, Vardi H, Tangi-Rozental O, Zuk-Ramot R, Sarusi B, Brickner D, Schwartz Z, Sheiner E, Marko R, Katorza E, Thiery J, Fiedler GM, Blüher M, Stumvoll M, Stampfer MJ Dietary Intervention Randomized Controlled Trial (DIRECT) Group. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet [published correction appears in N Engl J Med. 2009;361:2681] N Engl J Med. 2008;359:229–241. doi: 10.1056/NEJMoa0708681. [DOI] [PubMed] [Google Scholar]
- 30.Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, McManus K, Champagne CM, Bishop LM, Laranjo N, Leboff MS, Rood JC, de Jonge L, Greenway FL, Loria CM, Obarzanek E, Williamson DA. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360:859–873. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andreyeva T, Long MW, Henderson KE, Grode GM. Trying to lose weight: diet strategies among Americans with overweight or obesity in 1996 and 2003. J Am Diet Assoc. 2010;110:535–542. doi: 10.1016/j.jada.2009.12.029. [DOI] [PubMed] [Google Scholar]
- 32.Zhao G, Ford ES, Li C, Mokdad AH. Weight control behaviors in overweight/obese U.S. adults with diagnosed hypertension and diabetes. Cardiovasc Diabetol. 2009;8:13. doi: 10.1186/1475-2840-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farley TA, Baker ET, Futrell L, Rice JC. The ubiquity of energy-dense snack foods: a national multicity study. Am J Public Health. 2010;100:306–311. doi: 10.2105/AJPH.2009.178681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kumanyika S, Grier S. Targeting interventions for ethnic minority and low-income populations. Future Child. 2006;16:187–207. doi: 10.1353/foc.2006.0005. [DOI] [PubMed] [Google Scholar]
- 35.Sallis JF, Glanz K. The role of built environments in physical activity, eating, and obesity in childhood. Future Child. 2006;16:89–108. doi: 10.1353/foc.2006.0009. [DOI] [PubMed] [Google Scholar]
- 36.Li F, Harmer PA, Cardinal BJ, Bosworth M, Acock A, Johnson-Shelton D, Moore JM. Built environment, adiposity, and physical activity in adults aged 50–75. Am J Prev Med. 2008;35:38–46. doi: 10.1016/j.amepre.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mozaffarian D, Appel LJ, Van Horn L. Components of a cardioprotective diet: new insights. Circulation. 2011;123:2870–2891. doi: 10.1161/CIRCULATIONAHA.110.968735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mellen PB, Gao SK, Vitolins MZ, Goff DC., Jr Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988–1994 and 1999–2004. Arch Intern Med. 2008;168:308–314. doi: 10.1001/archinternmed.2007.119. [DOI] [PubMed] [Google Scholar]
- 39.Ervin RB. Healthy Eating Index scores among adults, 60 years of age and over, by sociodemographic and health characteristics: United States, 1999–2002. Adv Data. 2008;(395):1–16. [PubMed] [Google Scholar]
- 40.Bailey RL, Gahche JJ, Miller PE, Thomas PR, Dwyer JT. Why US adults use dietary supplements. JAMA Intern Med. 2013;173:355–361. doi: 10.1001/jamainternmed.2013.2299. [DOI] [PubMed] [Google Scholar]
- 41.Radimer K, Bindewald B, Hughes J, Ervin B, Swanson C, Picciano MF. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999–2000. Am J Epidemiol. 2004;160:339–349. doi: 10.1093/aje/kwh207. [DOI] [PubMed] [Google Scholar]
- 42.Bailey RL, Fulgoni VL, 3rd, Keast DR, Dwyer JT. Dietary supplement use is associated with higher intakes of minerals from food sources. Am J Clin Nutr. 2011;94:1376–1381. doi: 10.3945/ajcn.111.020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bailey RL, Fulgoni VL, 3rd, Keast DR, Dwyer JT. Examination of vitamin intakes among US adults by dietary supplement use. J Acad Nutr Diet. 2012;112:657–663. e4. doi: 10.1016/j.jand.2012.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Picciano MF, Dwyer JT, Radimer KL, Wilson DH, Fisher KD, Thomas PR, Yetley EA, Moshfegh AJ, Levy PS, Nielsen SJ. Dietary supplement use among infants, children, and adolescents in the United States, 1999–2002. Arch Pediatr Adolesc Med. 2007;161:978–985. doi: 10.1001/archpedi.161.10.978. [DOI] [PubMed] [Google Scholar]
- 45.Pillitteri JL, Shiffman S, Rohay JM, Harkins AM, Burton SL, Wadden TA. Use of dietary supplements for weight loss in the United States: results of a national survey. Obesity (Silver Spring) 2008;16:790–796. doi: 10.1038/oby.2007.136. [DOI] [PubMed] [Google Scholar]
- 46.House AA, Eliasziw M, Cattran DC, Churchill DN, Oliver MJ, Fine A, Dresser GK, Spence JD. Effect of B-vitamin therapy on progression of diabetic nephropathy: a randomized controlled trial. JAMA. 2010;303:1603–1609. doi: 10.1001/jama.2010.490. [DOI] [PubMed] [Google Scholar]
- 47.Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial: Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico [published corrections appear in Lancet. 2001;357:642 and Lancet. 2007;369:106] Lancet. 1999;354:447–455. [PubMed] [Google Scholar]
- 48.Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, Oikawa S, Sasaki J, Hishida H, Itakura H, Kita T, Kitabatake A, Nakaya N, Sakata T, Shimada K, Shirato K Japan EPA Lipid Intervention Study (JELIS) Investigators. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis [published correction appears in Lancet. 2007;370:220] Lancet. 2007;369:1090–1098. doi: 10.1016/S0140-6736(07)60527-3. [DOI] [PubMed] [Google Scholar]
- 49.Tavazzi L, Maggioni A, Marchioli R, Barlera S, Franzosi M, Latini R, Lucci D, Nicolosi G, Porcu M, Tognoni G GISSI-HF Investigators. Effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372:1223–1230. doi: 10.1016/S0140-6736(08)61239-8. [DOI] [PubMed] [Google Scholar]
- 50.Mozaffarian D, Wu JH. Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol. 2011;58:2047–2067. doi: 10.1016/j.jacc.2011.06.063. [DOI] [PubMed] [Google Scholar]
- 51.Rizos EC, Ntzani EE, Bika E, Kostapanos MS, Elisaf MS. Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease events: a systematic review and meta-analysis. JAMA. 2012;308:1024–1033. doi: 10.1001/2012.jama.11374. [DOI] [PubMed] [Google Scholar]
- 52.Ford ES, Li C, Zhao G, Tsai J. Trends in obesity and abdominal obesity among adults in the United States from 1999–2008. Int J Obes (Lond) 2011;35:736–743. doi: 10.1038/ijo.2010.186. [DOI] [PubMed] [Google Scholar]
- 53.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 54.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wright JD, Wang CY. Trends in intake of energy and macronutrients in adults from 1999–2000 through 2007–2008. NCHS Data Brief. 2010;(49):1–8. [PubMed] [Google Scholar]
- 56.Briefel RR, Johnson CL. Secular trends in dietary intake in the United States. Annu Rev Nutr. 2004;24:401–431. doi: 10.1146/annurev.nutr.23.011702.073349. [DOI] [PubMed] [Google Scholar]
- 57.Kant AK, Graubard BI. Secular trends in patterns of self-reported food consumption of adult Americans: NHANES 1971–1975 to NHANES 1999–2002. Am J Clin Nutr. 2006;84:1215–1223. doi: 10.1093/ajcn/84.5.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Popkin BM, Armstrong LE, Bray GM, Caballero B, Frei B, Willett WC. A new proposed guidance system for beverage consumption in the United States [published correction appears in Am J Clin Nutr. 2007;86:525] Am J Clin Nutr. 2006;83:529. doi: 10.1093/ajcn.83.3.529. [DOI] [PubMed] [Google Scholar]
- 59.Duffey KJ, Popkin BM. Shifts in patterns and consumption of beverages between 1965 and 2002. Obesity (Silver Spring) 2007;15:2739–2747. doi: 10.1038/oby.2007.326. [DOI] [PubMed] [Google Scholar]
- 60.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics. 2008;121:e1604–e1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 61.Wang YC, Gortmaker SL, Sobol AM, Kuntz KM. Estimating the energy gap among US children: a counterfactual approach. Pediatrics. 2006;118:e1721–e1733. doi: 10.1542/peds.2006-0682. [DOI] [PubMed] [Google Scholar]
- 62.Duffey KJ, Popkin BM. Energy density, portion size, and eating occasions: contributions to increased energy intake in the United States, 1977–2006. PLoS Med. 2011;8:e1001050. doi: 10.1371/journal.pmed.1001050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Poti JM, Popkin BM. Trends in energy intake among US children by eating location and food source, 1977–2006. J Am Diet Assoc. 2011;111:1156–1164. doi: 10.1016/j.jada.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dwyer-Lindgren L, Freedman G, Engell RE, Fleming TD, Lim SS, Murray CJ, Mokdad AH. Prevalence of physical activity and obesity in US counties, 2001–2011: a road map for action. Popul Health Metr. 2013;11:7. doi: 10.1186/1478-7954-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7. Washington, DC: US Government Printing Office; 2010. [Accessed September 18, 2013]. http://www.health.gov/dietaryguidelines/dga2010/DietaryGuidelines2010.pdf. [Google Scholar]
- 66.Davis C, Saltos E. Dietary recommendations and how they have changed over time. In: Frazao E, editor. America’s Eating Habits: Changes and Consequences. Washington, DC: US Department of Agriculture; 1999. pp. 33–50. Agriculture Information Bulletin No. 750. [Google Scholar]
- 67.Centers for Disease Control and Prevention (CDC) Trends in intake of energy and macronutrients--United States, 1971–2000. MMWR Morb Mortal Wkly Rep. 2004;53:80–82. [PubMed] [Google Scholar]
- 68.Egan SK, Bolger PM, Carrington CD. Update of US FDA’s Total Diet Study food list and diets. J Expo Sci Environ Epidemiol. 2007;17:573–582. doi: 10.1038/sj.jes.7500554. [DOI] [PubMed] [Google Scholar]
- 69.Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr. 2013;98:180–188. doi: 10.3945/ajcn.112.057943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Blanck HM, Gillespie C, Kimmons JE, Seymour JD, Serdula MK. Trends in fruit and vegetable consumption among U.S. men and women, 1994–2005. Prev Chronic Dis. 2008;5:A35. [PMC free article] [PubMed] [Google Scholar]
- 71.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, 3rd, Simons-Morton DG, Karanja N, Lin PH DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet: DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 72.Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER, 3rd, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, Charleston J, McCarron P, Bishop LM OmniHeart Collaborative Research Group. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005;294:2455–2464. doi: 10.1001/jama.294.19.2455. [DOI] [PubMed] [Google Scholar]
- 73.Gadgil MD, Appel LJ, Yeung E, Anderson CA, Sacks FM, Miller ER., 3rd The effects of carbohydrate, unsaturated fat, and protein intake on measures of insulin sensitivity: results from the OmniHeart trial. Diabetes Care. 2013;36:1132–1137. doi: 10.2337/dc12-0869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Uauy R, Aro A, Clarke R, Ghafoorunissa, L’Abbé MR, Mozaffarian D, Skeaff CM, Stender S, Tavella M. WHO Scientific Update on trans fatty acids: summary and conclusions. Eur J Clin Nutr. 2009;63:S68–S75. [Google Scholar]
- 75.Geleijnse JM, Giltay EJ, Grobbee DE, Donders AR, Kok FJ. Blood pressure response to fish oil supplementation: metaregression analysis of randomized trials. J Hypertens. 2002;20:1493–1499. doi: 10.1097/00004872-200208000-00010. [DOI] [PubMed] [Google Scholar]
- 76.Mozaffarian D, Geelen A, Brouwer IA, Geleijnse JM, Zock PL, Katan MB. Effect of fish oil on heart rate in humans: a meta-analysis of randomized controlled trials. Circulation. 2005;112:1945–1952. doi: 10.1161/CIRCULATIONAHA.105.556886. [DOI] [PubMed] [Google Scholar]
- 77.Sabaté J, Oda K, Ros E. Nut consumption and blood lipid levels: a pooled analysis of 25 intervention trials. Arch Intern Med. 2010;170:821–827. doi: 10.1001/archinternmed.2010.79. [DOI] [PubMed] [Google Scholar]
- 78.Hu FB, Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav. 2010;100:47–54. doi: 10.1016/j.physbeh.2010.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med. 2012;367:1397–1406. doi: 10.1056/NEJMoa1203034. [DOI] [PubMed] [Google Scholar]
- 80.Ebbeling CB, Feldman HA, Chomitz VR, Antonelli TA, Gortmaker SL, Osganian SK, Ludwig DS. A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med. 2012;367:1407–1416. doi: 10.1056/NEJMoa1203388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, Fiol M, Gómez-Gracia E, López-Sabater MC, Vinyoles E, Arós F, Conde M, Lahoz C, Lapetra J, Sáez G, Ros E PREDIMED Study Investigators. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006;145:1–11. doi: 10.7326/0003-4819-145-1-200607040-00004. [DOI] [PubMed] [Google Scholar]
- 82.Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML, Wassertheil-Smoller S, Kuller LH, LaCroix AZ, Langer RD, Lasser NL, Lewis CE, Limacher MC, Margolis KL, Mysiw WJ, Ockene JK, Parker LM, Perri MG, Phillips L, Prentice RL, Robbins J, Rossouw JE, Sarto GE, Schatz IJ, Snetselaar LG, Stevens VJ, Tinker LF, Trevisan M, Vitolins MZ, Anderson GL, Assaf AR, Bassford T, Beresford SA, Black HR, Brunner RL, Brzyski RG, Caan B, Chlebowski RT, Gass M, Granek I, Greenland P, Hays J, Heber D, Heiss G, Hendrix SL, Hubbell FA, Johnson KC, Kotchen JM. Low-fat dietary pattern and risk of cardiovascular disease: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:655–666. doi: 10.1001/jama.295.6.655. [DOI] [PubMed] [Google Scholar]
- 83.World Health Organization, Food and Agriculture Organization of the United Nations. Diet, Nutrition and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation. Geneva, Switzerland: World Health Organization; 2003. WHO Technical Report Series 916. [Google Scholar]
- 84.Skeaff CM, Miller J. Dietary fat and coronary heart disease: summary of evidence from prospective cohort and randomised controlled trials. Ann Nutr Metab. 2009;55:173–201. doi: 10.1159/000229002. [DOI] [PubMed] [Google Scholar]
- 85.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169:659–669. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 86.Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr. 2010;91:535–546. doi: 10.3945/ajcn.2009.27725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jakobsen MU, O’Reilly EJ, Heitmann BL, Pereira MA, Bälter K, Fraser GE, Goldbourt U, Hallmans G, Knekt P, Liu S, Pietinen P, Spiegelman D, Stevens J, Virtamo J, Willett WC, Ascherio A. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr. 2009;89:1425–1432. doi: 10.3945/ajcn.2008.27124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7:e1000252. doi: 10.1371/journal.pmed.1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC. Trans fatty acids and cardiovascular disease. N Engl J Med. 2006;354:1601–1613. doi: 10.1056/NEJMra054035. [DOI] [PubMed] [Google Scholar]
- 90.Barclay AW, Petocz P, McMillan-Price J, Flood VM, Prvan T, Mitchell P, Brand-Miller JC. Glycemic index, glycemic load, and chronic disease risk: a meta-analysis of observational studies. Am J Clin Nutr. 2008;87:627–637. doi: 10.1093/ajcn/87.3.627. [DOI] [PubMed] [Google Scholar]
- 91.Dong JY, Zhang YH, Wang P, Qin LQ. Meta-analysis of dietary glycemic load and glycemic index in relation to risk of coronary heart disease. Am J Cardiol. 2012;109:1608–1613. doi: 10.1016/j.amjcard.2012.01.385. [DOI] [PubMed] [Google Scholar]
- 92.Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr. 2006;136:2588–2593. doi: 10.1093/jn/136.10.2588. [DOI] [PubMed] [Google Scholar]
- 93.Dauchet L, Amouyel P, Dallongeville J. Fruit and vegetable consumption and risk of stroke: a meta-analysis of cohort studies. Neurology. 2005;65:1193–1197. doi: 10.1212/01.wnl.0000180600.09719.53. [DOI] [PubMed] [Google Scholar]
- 94.Mellen PB, Walsh TF, Herrington DM. Whole grain intake and cardiovascular disease: a meta-analysis. Nutr Metab Cardiovasc Dis. 2008;18:283–290. doi: 10.1016/j.numecd.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 95.Harris WS, Mozaffarian D, Lefevre M, Toner CD, Colombo J, Cunnane SC, Holden JM, Klurfeld DM, Morris MC, Whelan J. Towards establishing dietary reference intakes for eicosapentaenoic and docosahexaenoic acids. J Nutr. 2009;139:804S–819S. doi: 10.3945/jn.108.101329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation. 2010;121:2271–2283. doi: 10.1161/CIRCULATIONAHA.109.924977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Willett WC, Hu FB. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr. 2011;94:1088–1096. doi: 10.3945/ajcn.111.018978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, Hu FB, Engberink MF, Willett WC, Geleijnse JM. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr. 2011;93:158–171. doi: 10.3945/ajcn.2010.29866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Fung TT, Malik V, Rexrode KM, Manson JE, Willett WC, Hu FB. Sweetened beverage consumption and risk of coronary heart disease in women. Am J Clin Nutr. 2009;89:1037–1042. doi: 10.3945/ajcn.2008.27140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bomback AS, Derebail VK, Shoham DA, Anderson CA, Steffen LM, Rosamond WD, Kshirsagar AV. Sugar-sweetened soda consumption, hyperuricemia, and kidney disease. Kidney Int. 2010;77:609–616. doi: 10.1038/ki.2009.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cohen HW, Hailpern SM, Alderman MH. Sodium intake and mortality follow-up in the Third National Health and Nutrition Examination Survey (NHANES III) J Gen Intern Med. 2008;23:1297–1302. doi: 10.1007/s11606-008-0645-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the Trials of Hypertension Prevention (TOHP) BMJ. 2007;334:885–888. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Taylor RS, Ashton KE, Moxham T, Hooper L, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease: a meta-analysis of randomized controlled trials (Cochrane review) Am J Hypertens. 2011;24:843–853. doi: 10.1038/ajh.2011.115. [DOI] [PubMed] [Google Scholar]
- 104.Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009;339:b4567. doi: 10.1136/bmj.b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.D’Elia L, Barba G, Cappuccio FP, Strazzullo P. Potassium intake, stroke, and cardiovascular disease a meta-analysis of prospective studies. J Am Coll Cardiol. 2011;57:1210–1219. doi: 10.1016/j.jacc.2010.09.070. [DOI] [PubMed] [Google Scholar]
- 106.Mitrou PN, Kipnis V, Thiébaut AC, Reedy J, Subar AF, Wirfält E, Flood A, Mouw T, Hollenbeck AR, Leitzmann MF, Schatzkin A. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP Diet and Health Study. Arch Intern Med. 2007;167:2461–2468. doi: 10.1001/archinte.167.22.2461. [DOI] [PubMed] [Google Scholar]
- 107.Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119:1093–1100. doi: 10.1161/CIRCULATIONAHA.108.816736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women [published correction appears in Arch Intern Med. 2008;168:1276] Arch Intern Med. 2008;168:713–720. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- 109.Heidemann C, Schulze MB, Franco OH, van Dam RM, Mantzoros CS, Hu FB. Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation. 2008;118:230–237. doi: 10.1161/CIRCULATIONAHA.108.771881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Osler M, Heitmann BL, Gerdes LU, Jørgensen LM, Schroll M. Dietary patterns and mortality in Danish men and women: a prospective observational study. Br J Nutr. 2001;85:219–225. doi: 10.1079/bjn2000240. [DOI] [PubMed] [Google Scholar]
- 111.van Dam RM, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Dietary patterns and risk for type 2 diabetes mellitus in U.S. men. Ann Intern Med. 2002;136:201–209. doi: 10.7326/0003-4819-136-3-200202050-00008. [DOI] [PubMed] [Google Scholar]
- 112.Heidemann C, Hoffmann K, Spranger J, Klipstein-Grobusch K, Möhlig M, Pfeiffer AF, Boeing H European Prospective Investigation into Cancer and Nutrition (EPIC)–Potsdam Study Cohort. A dietary pattern protective against type 2 diabetes in the European Prospective Investigation into Cancer and Nutrition (EPIC)–Potsdam Study cohort. Diabetologia. 2005;48:1126–1134. doi: 10.1007/s00125-005-1743-1. [DOI] [PubMed] [Google Scholar]
- 113.Brunner EJ, Mosdøl A, Witte DR, Martikainen P, Stafford M, Shipley MJ, Marmot MG. Dietary patterns and 15-y risks of major coronary events, diabetes, and mortality. Am J Clin Nutr. 2008;87:1414–1421. doi: 10.1093/ajcn/87.5.1414. [DOI] [PubMed] [Google Scholar]
- 114.Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation. 2008;117:754–761. doi: 10.1161/CIRCULATIONAHA.107.716159. [DOI] [PubMed] [Google Scholar]
- 115.Fitzgerald KC, Chiuve SE, Buring JE, Ridker PM, Glynn RJ. Comparison of associations of adherence to a Dietary Approaches to Stop Hypertension (DASH)-style diet with risks of cardiovascular disease and venous thromboembolism. J Thromb Haemost. 2012;10:189–198. doi: 10.1111/j.1538-7836.2011.04588.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Joosten MM, Grobbee DE, van der ADL, Verschuren WM, Hendriks HF, Beulens JW. Combined effect of alcohol consumption and lifestyle behaviors on risk of type 2 diabetes. Am J Clin Nutr. 2010;91:1777–1783. doi: 10.3945/ajcn.2010.29170. [DOI] [PubMed] [Google Scholar]
- 117.de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99:779–785. doi: 10.1161/01.cir.99.6.779. [DOI] [PubMed] [Google Scholar]
- 118.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA Martínez-González MA; PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–1290. doi: 10.1056/NEJMc1806491. [DOI] [PubMed] [Google Scholar]
- 119.US Burden of Disease Collaborators. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors [published correction appears in PLoS Med. 2011;8(1). doi:10.1371/annotation/0ef47acd-9dcc-4296-a897-872d182cde57] PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.US Department of Agriculture. Food expenditures. [Accessed July 21, 2011];US Department of Agriculture Web site. http://www.ers.usda.gov/Briefing/CPIFoodAndExpenditures/Data/
- 122.Brunner E, Cohen D, Toon L. Cost effectiveness of cardiovascular disease prevention strategies: a perspective on EU food based dietary guidelines. Public Health Nutr. 2001;4(2B):711–715. doi: 10.1079/phn2001161. [DOI] [PubMed] [Google Scholar]
- 123.Centers for Disease Control and Prevention. [Accessed July 21, 2011];Preventing chronic diseases: investing wisely in health: preventing obesity and chronic diseases through good nutrition and physical activity. http://www.cdc.gov/nccd-php/publications/factsheets/prevention/pdf/obesity.pdf. Revised 2008.
- 124.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B, Karanja N, Lefevre M, Rudel L, Sacks F, Van Horn L, Winston M, Wylie-Rosett J. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee [published corrections appear in Circulation. 2006;114:e629 and Circulation. 2006;114:e27] Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 125.International Society for the Study of Fatty Acids and Lipids. Recommendations for Intake of Polyunsaturated Fatty Acids in Healthy Adults. Devon, United Kingdom: International Society for the Study of Fatty Acids and Lipids; 2004. [Google Scholar]
- 126.Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) Washington, DC: Institute of Medicine, National Academies Press; 2005. [Google Scholar]
- 127.Smith-Spangler CM, Juusola JL, Enns EA, Owens DK, Garber AM. Population strategies to decrease sodium intake and the burden of cardiovascular disease: a cost-effectiveness analysis. Ann Intern Med. 2010;152:481–487. W170–W163. doi: 10.7326/0003-4819-152-8-201004200-00212. [DOI] [PubMed] [Google Scholar]
- 128.Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362:590–599. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.US Department of Health and Human Services and US Department of Agriculture. Dietary Guidelines for Americans, 2005. 6. Washington, DC: US Government Printing Office; 2005. [Accessed July 21, 2011]. http://www.health.gov/dietaryguidelines/dga2005/document/default.htm. [Google Scholar]
- 130.Interim summary of conclusions and dietary recommendations on total fat & fatty acids: from the Joint FAO/WHO Expert Consultation on fats and fatty acids in human nutrition. WHO; Geneva: 2008. [Accessed November 17, 2010]. pp. 10–14. http://www.who.int/nutrition/topics/FFA_summary_rec_conclusion.pdf. [Google Scholar]
6. Overweight and Obesity
See Table 6-1 and Charts 6-1 through 6-3.
Table 6-1.
Overweight and Obesity
| Prevalence of Overweight and Obesity, 2007–2010, Age >20 y | Prevalence of Obesity in Adults, 2007–2010, Age >20 y | Prevalence of Overweight and Obesity in Children, 2009–2010, Ages 2–19 y | Prevalence of Obesity in Children, 2009–2010, Ages 2–19 y | Cost, 2008* | |
|---|---|---|---|---|---|
| Both sexes, n (%) | 154 700 000 (68.2) | 78 400 000 (34.6) | 23 900 000 (31.8) | 12 700 000 (16.9) | $147 Billion |
| Males | 79 900 000 (72.9) | 36 800 000 (33.6) | 12 700 000 (33.0) | 7 200 000 (18.6) | … |
| Females | 74 800 000 (63.7) | 41 600 000 (35.6) | 11 200 000 (30.4) | 5 500 000 (15.0) | … |
| NH white males, % | 73.1 | 33.8 | 30.1 | 16.1 | … |
| NH white females, % | 60.2 | 32.5 | 25.6 | 11.7 | … |
| NH black males, % | 68.7 | 37.9 | 36.9 | 24.3 | … |
| NH black females, % | 79.9 | 53.9 | 41.3 | 24.3 | … |
| Mexican American males, % | 81.3 | 36.0 | 40.5 | 24.0 | … |
| Mexican American females, % | 78.2 | 44.8 | 38.2 | 18.2 | … |
Overweight and obesity in adults is defined as body mass index (BMI) ≥25 kg/m2. Obesity in adults is defined as BMI ≥30 kg/m2. In children, overweight and obesity are based on BMI-for-age values at or above the 85th percentile of the 2000 Centers for Disease Control and Prevention (CDC) growth charts. In children, obesity is based on BMI-for-age values at or above the 95th percentile of the CDC growth charts. In January 2007, the American Medical Association’s Expert Task Force on Childhood Obesity recommended new definitions for overweight and obesity in children and adolescents71; however, statistics based on this new definition are not yet available.
NH indicates non-Hispanic; ellipses (…), data not available.
Data from Finkelstein et al.57
Sources: National Health and Nutrition Examination Survey (NHANES) 2007 to 2010 (adults), unpublished National Heart, Lung, and Blood Institute (NHLBI) tabulation; NHANES 2009 to 2010 (ages 2–19 y) from Ogden et al.4 Extrapolation for ages 2 to 19 y from NHLBI tabulation of US Census resident population on April 1, 2010.
Chart 6-1.
Prevalence of overweight and obesity among students in grades 9 through 12 by sex and race/ethnicity. NH indicates non-Hispanic. Data derived from Eaton et al (Table 101).72
Chart 6-3.
Trends in the prevalence of obesity among US children and adolescents by age and survey year (National Health and Nutrition Examination Survey: 1971–1974, 1976–1980, 1988–1994, 1999–2002, 2003–2006, and 2007–2010). Data derived from Health, United States, 2011 (National Center for Health Statistics).73
Overweight and obesity are major risk factors for CVD and stroke.1,2 The AHA has identified BMI <85th percentile (for children) and <25 kg/m2 (for adults aged ≥20 years) as 1 of the 7 components of ideal cardiovascular health.3 In 2009 to 2010, 64.2% of children and 31.1% of adults met these criteria (see Chapter 2, Cardiovascular Health).
Abbreviations Used in Chapter 6
| AF | atrial fibrillation |
| AFFIRM | Atrial Fibrillation Follow-up Investigation of Rhythm Management |
| AHA | American Heart Association |
| BMI | body mass index |
| BP | blood pressure |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CAD | coronary artery disease |
| CARDIA | Coronary Artery Risk Development in Young Adults |
| CDC | Centers for Disease Control and Prevention |
| CHD | coronary heart disease |
| CHF | congestive heart failure |
| CI | confidence interval |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| FHS | Framingham Heart Study |
| HbA1c | hemoglobin A1c |
| HDL | high-density lipoprotein |
| HR | hazard ratio |
| HUNT 2 | Nord-Trøndelag Health Study |
| MEPS | Medical Expenditure Panel Survey |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| MI | myocardial infarction |
| NCDR | National Cardiovascular Data Registry |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHANES | National Health and Nutrition Examination Survey |
| NHDS | National Hospital Discharge Survey |
| NHIS | National Health Interview Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| OR | odds ratio |
| PA | physical activity |
| RR | relative risk |
| SBP | systolic blood pressure |
| SD | standard deviation |
| STEMI | ST-segment–elevation myocardial infarction |
Prevalence
Youth
(See Table 6-1 and Chart 6-1.)
The prevalence of overweight and obesity in children 2 to 5 years of age, based on a BMI-for-age value ≥85th percentile of the 2000 CDC growth charts, was 26% for non-Hispanic white boys and 21% for non-Hispanic white girls, 31% for non-Hispanic black boys and 27% for non-Hispanic black girls, and 34% for Mexican American boys and 33% for Mexican American girls according to 2009 to 2010 data from NHANES (NCHS). In children 6 to 11 years of age, the prevalence was 30% for non-Hispanic white boys and 25% for non-Hispanic white girls, 41% for non-Hispanic black boys and 44% for non-Hispanic black girls, and 39% for Mexican American boys and 40% for Mexican American girls. In children 12 to 19 years of age, the prevalence was 32% for non-Hispanic white boys and 28% for non-Hispanic white girls, 37% for non-Hispanic black boys and 45% for non-Hispanic black girls, and 46% for Mexican American boys and 41% for Mexican American girls.4
The national prevalence of obesity in children 2 to 5 years of age, based on BMI-for-age values ≥95th percentile of the 2000 CDC growth charts, was 12% for non-Hispanic white boys and 6% for non-Hispanic white girls, 21% for non-Hispanic black boys and 17% for non-Hispanic black girls, and 19% for Mexican American boys and 12% for Mexican American girls according to 2009 to 2010 data from NHANES (NCHS). In children 6 to 11 years of age, the prevalence was 17% for non-Hispanic white boys and 11% for non-Hispanic white girls, 30% for non-Hispanic black boys and 28% for non-Hispanic black girls, and 22% for Mexican American boys and 22% for Mexican American girls. In children 12 to 19 years of age, the prevalence was 18% for non-Hispanic white boys and 15% for non-Hispanic white girls, 23% for non-Hispanic black boys and 25% for non-Hispanic black girls, and 29% for Mexican American boys and 19% for Mexican American girls.4 Regional variation exists in these prevalences.
Overall, 18% of US children and adolescents 6 to 19 years of age have BMI-for-age values ≥95th percentile of the 2000 CDC growth charts for the United States (NHANES 2009–2010, NCHS).4
NHANES 2009 to 2010 found that 16.9% (95% CI, 15.4%–18.4%) of youth aged 2 to 19 years were obese, which was unchanged from NHANES 2007 to 2008. Rates of overweight and obesity (≥85th BMI percentile) were 39.1% for Hispanics, 39.4% for Mexican Americans, 27.9% for non-Hispanic whites, and 39.1% for non-Hispanic blacks.4
A study of >8500 4-year-olds in the Early Childhood Longitudinal Study, Birth Cohort (National Center for Education Statistics) found that 1 in 5 were obese. Almost 13% of Asian children, 16% of white children, nearly 21% of black children, 22% of Hispanic children, and 31% of American Indian children were obese. Children were considered obese if their BMI was ≥95th percentile on the basis of CDC BMI growth charts.5
Childhood sociodemographic factors may contribute to sex disparities in obesity prevalence. A study of data from the National Longitudinal Study of Adolescent Health (Add Health) found that parental education consistently modified sex disparity in blacks. The sex gap was largest in those with low parental education (16.7% of men compared with 45.4% of women were obese) and smallest in those with high parental education (28.5% of men compared with 31.4% of women were obese). In whites, there was little overall sex difference in obesity prevalence.6
The obesity epidemic is disproportionally more rampant among children living in low-income, low-education, and higher-unemployment households, according to data from the National Survey of Children’s Health.7
Data from 2011 show that among low-income preschool children, American Indians/Alaskan Natives have an obesity rate of 17.7%, whereas rates are 14.7% for Hispanics, 10.6% for non-Hispanic blacks, 10.3% for non-Hispanic whites, and 9.3% for Asian/Pacific Islanders.8
According to 1999 to 2008 NHANES survey data, lowest-income girls had an obesity prevalence of 17.9% compared with 13.1% among those with higher income; similar observations were observed for boys (20.6% versus 15.6%, respectively).9
According to the National Longitudinal Study of Adolescent Health, 1.0% of adolescents were severely obese in 1996 (defined as age <20 years and BMI ≥95th sex-specific BMI-for-age growth chart or BMI ≥30 kg/m2); the majority (70.5%) maintained this weight status into adulthood. Obese adolescents had a 16-fold increased risk of becoming severely obese adults compared with those with normal weight or those who were overweight.10
NHANES 2003 to 2004 and 2005 to 2006 data were used to determine overweight and obesity prevalence in rural versus urban youth; the results showed that 39% of rural versus 32% of urban children had BMI >85th percentile.11
Adults
(See Table 6-1 and Chart 6-2.)
Chart 6-2.
Age-adjusted prevalence of obesity in adults 20 to 74 years of age by sex and survey year (National Health Examination Survey: 1960–1962; National Health and Nutrition Examination Survey: 1971–1974, 1976–1980, 1988–1994, 1999–2002, and 2007–2010). Obesity is defined as body mass index of 30.0 kg/m2. Data derived from Health, United States, 2011 (National Center for Health Statistics).73
-
According to NHANES 2007 to 2010 (unpublished NHLBI tabulations):
Overall, 68% of US adults were overweight or obese (73% of men and 64% of women).
Among men, Mexican-Americans (81%) and non-Hispanic whites (73%) were more likely to be overweight or obese than non-Hispanic blacks (69%).
Among women, non-Hispanic blacks (80%) and Mexican-Americans (78%) were more likely to be overweight or obese than non-Hispanic whites (60%).
Among US adults, 35% were obese (35% of men and 36% of women).
Among men, non-Hispanic blacks (38%) and Mexican-Americans (36%) were more likely to be obese than non-Hispanic whites (34%).
Among women, non-Hispanic blacks (54%) and Mexican-Americans (45%) were more likely to be obese than non-Hispanic whites (33%).
When estimates were based on self-reported height and weight in the BRFSS/CDC survey in 2011, the prevalence of obesity ranged from 20.7% in Colorado to 34.9% in Mississippi. The median percentage by state was 27.8%.12 Additionally, no state met the Healthy People 2010 goal of reducing obesity to 15% of adults.13
-
On the basis of self-reported weights and heights from the 2012 NHIS14:
Blacks ≥18 years of age (27.9%), American Indians or Alaska Natives (26.6%), and whites (35.7%) were less likely than Asians (57.6%) to be at a healthy weight.
Blacks ≥18 years of age (36.2%) and American Indians or Alaska Natives (41.2%) were more likely to be obese than were whites (28.0%) and Asians (9.9%).
Most adults in Asian subgroups were in the healthy weight range, with rates ranging from 51% for Filipino adults to 68% for Chinese adults. Although the prevalence of obesity is low within the Asian adult population, Filipino adults (14%) were more than twice as likely to be obese (BMI ≥30 kg/m2) as Asian Indian (6%), Vietnamese (5%), or Chinese (4%) adults.15
-
According to the 2008 National Healthcare Disparities Report (based on NHANES 2003–2006)16:
Approximately 64.8% of obese adults were told by a doctor or health professional that they were overweight.
The proportion of obese adults told that they were overweight was significantly lower for non-Hispanic blacks (60.5%) and Mexican Americans (57.1%) than for non-Hispanic whites (66.4%), for middle-income people than for high-income people (62.4% versus 70.6%), and for adults with less than a high school education than for those with any college education (59.2% versus 70.3%).
As judged by an analysis of data from MESA, a large proportion of white, black, and Hispanic participants were overweight (60%–85%) or obese (30%–50%), whereas fewer Chinese American participants were overweight (33%) or obese (5%).17
According to NHANES 2007 to 2010 data, 35% of US adults >65 years of age were obese, which represents 13 million individuals.18
Trends
Youth
(See Chart 6-3.)
Among infants and children between 6 and 23 months of age, the prevalence of high weight for recumbent length was 7% in 1976 to 1980 and 12% in 2003 to 2006 (NHANES, NCHS).19
The obesity epidemic in children continues to grow on the basis of recent data from the Bogalusa Heart Study. Compared with 1973 to 1974, the proportion of children 5 to 17 years of age who were obese was 5 times higher in 2008 to 2009.20
A comparison of NHANES 2009 to 2010 data with 1999 to 2000 data demonstrates an increase in obesity prevalence in male youth of 5% (OR, 1.05; 95% CI, 1.01–1.10) but not in female youth (OR, 1.02; 95% CI, 0.98–1.07).4
Adults
On the basis of 2009 self-reported BRFSS data, overall obesity prevalence was 26.7% in the United States, with rates of 27.4% in men and 26.0% in women. By race/ethnicity, the prevalence of obesity among non-Hispanic whites was 25.2%, whereas it was 36.8% among non-Hispanic blacks and 30.7% among Hispanics. There was an inverse association by education level: College graduates had a 20.8% rate of obesity, whereas those who attained less than a high school education had an obesity prevalence of 32.9%.21
According to NHANES data, between 2009 and 2010, the prevalence of obesity remained steady among US adult men and women, with no significant change compared with 2003 to 2008.22 Among adults aged ≥65 years, the prevalence of obesity increased linearly for men between 1999 and 2010, but the increase among women was not statistically significant.18
Forecasts through 2030 using the BRFSS 1990 to 2008 data set suggest that by 2030, 51% of the population will be obese, with 11% with severe obesity, an increase of 33% for obesity and 130% for severe obesity.23
Morbidity
-
Overweight children and adolescents are at increased risk for future adverse health effects, including the following24:
Increased prevalence of traditional cardiovascular risk factors such as hypertension, hyperlipidemia, and DM.
Poor school performance, tobacco use, alcohol use, premature sexual behavior, and poor diet.
Other associated health conditions, such as asthma, hepatic steatosis, sleep apnea, stroke, some cancers (breast, colon, and kidney), renal insufficiency, musculoskeletal disorders, and gallbladder disease.
Data from 4 Finnish cohort studies examining childhood and adult BMI with a mean follow-up of 23 years found that overweight or obese children who remained obese in adulthood had increased risks of type 2 DM, hypertension, dyslipidemia, and carotid atherosclerosis. However, those who became normal weight by adulthood had risks comparable to individuals who were never obese.25
The CARDIA study showed that young adults who were overweight or obese had lower health-related quality of life than normal-weight participants 20 years later. On the basis of data from the Medical Outcomes Study 12-item short-form health survey, overweight and obese participants had lower multivariable-adjusted scores on the physical component summary score but not on the mental component summary score.25a
The increasing prevalence of obesity is driving an increased incidence of type 2 DM. Data from the FHS indicate a doubling in the incidence of DM over the past 30 years, most dramatically during the 1990s and primarily among individuals with a BMI >30 kg/m2.26
Among 68 070 participants across multiple NHANES surveys, the decline in BP in recent birth cohorts is slowing, mediated by BMI.27
In a meta-analysis from 58 cohorts, representing 221 934 people in 17 developed countries with 14 297 incident CVD outcomes, BMI, waist circumference, and waist-to-hip ratio were only minimally associated with cardiovascular outcomes after controlling for baseline SBP, DM, and total and HDL cholesterol in addition to age, sex, and smoking status. Measures of adiposity also did not improve risk discrimination or reclassification when risk factor data were included.28
The population attributable fraction for CHD associated with reducing current population mean BMI to 21 kg/m2 in the Asia-Pacific region ranged from 2% in India to 58% in American Samoa; the population attributable fraction for ischemic stroke ranged from 3% in India to 64% in American Samoa. These data from 15 countries show the proportion of CVD that would be prevented if the population mean BMI were reduced below the current overweight cut point.29
Obesity is also a strong predictor of sleep-disordered breathing, itself strongly associated with the development of CVD, as well as with myriad other health conditions, including numerous cancers, nonalcoholic fatty liver disease, gallbladder disease, musculoskeletal disorders, and reproductive abnormalities.30
A systematic review of prospective studies examining overweight and obesity as predictors of major stroke subtypes in >2 million participants over ≥4 years found an adjusted RR for ischemic stroke of 1.22 (95% CI, 1.05–1.41) in overweight individuals and an RR of 1.64 (95% CI, 1.36–1.99) for obese individuals relative to normal-weight individuals. RRs for hemorrhagic stroke were 1.01 (95% CI, 0.88–1.17) and 1.24 (95% CI, 0.99–1.54) for overweight and obese individuals, respectively. These risks were graded with increasing BMI and were independent of age, lifestyle, and other cardiovascular risk factors.31
A recent meta-analysis of 15 prospective studies demonstrated the increased risk for Alzheimer disease or vascular dementia and any dementia was 1.35 and 1.26 for overweight, respectively, and 2.04 and 1.64 for obesity, respectively.32 The inclusion of obesity in dementia forecast models increases the estimated prevalence of dementia through 2050 by 9% in the United States and 19% in China.33
Ten-year follow-up data from the Swedish Obese Subjects intervention study indicated that to maintain a favorable effect on cardiovascular risk factors, more than the short-term goal of 5% weight loss is needed to overcome secular trends and aging effects.34
A randomized clinical trial of 130 severely obese adult individuals randomized to either 12 months of diet and PA or only 6 months of PA resulted in 12.1 and 9.9 kg, respectively, of weight loss at 1 year, with improvements in waist circumference, visceral fat, BP, and insulin resistance.35
Mortality
Elevated childhood BMIs in the highest quartile were associated with premature death as an adult in a cohort of 4857 American Indian children during a median follow-up of 23.9 years.36
According to NHIS data, among young adults aged 18 to 39 years, the HR for all-cause mortality was 1.07 (95% CI, 0.91–1.26) for overweight individuals, 1.41 (95% CI, 1.16–1.73) for obese individuals, and 2.46 for extremely obese individuals (95% CI, 1.91–3.16).37
Among adults, obesity was associated with nearly 112 000 excess deaths (95% CI, 53 754–170 064) relative to normal weight in 2000. Grade 1 obesity (BMI 30 to <35 kg/m2) was associated with almost 30 000 of these excess deaths (95% CI, 8534–68 220) and grade 2 to 3 obesity (BMI ≥35 kg/m2) with >82 000 (95% CI, 44 843–119 289). Underweight was associated with nearly 34 000 excess deaths (95% CI, 15 726–51 766). As other studies have found,38 overweight (BMI 25 to <30 kg/m2) was not associated with excess deaths.39
A recent systematic review (2.88 million individuals and >270 000 deaths) showed that relative to normal BMI (18.5 to <25 kg/m2), all-cause mortality was lower for overweight (HR, 0.94; 95% CI, 0.91–0.96) but was not elevated for grade 1 obesity (HR, 0.95; 95% CI, 0.88–1.01). All-cause mortality was higher for obesity (all grades; HR, 1.18; 95% CI, 1.12–1.25) and grades 2 and 3 obesity (HR, 1.29; 95% CI, 1.18–1.41).40
In a collaborative analysis of data from almost 900 000 adults in 57 prospective studies, mostly in western Europe and North America, overall mortality was lowest at a BMI of ≈22.5 to 25 kg/m2 in both sexes and at all ages, after exclusion of early follow-up and adjustment for smoking status. Above this range, each 5-kg/m2-higher BMI was associated with ≈30% higher all-cause mortality, and no specific cause of death was inversely associated with BMI. Below 22.5 to 25 kg/m2, the overall inverse association with BMI was predominantly related to strong inverse associations for smoking-related respiratory disease, and the only clearly positive association was for ischemic heart disease.41
In a meta-analysis of 1.46 million white adults, over a mean follow-up period of 10 years, all-cause mortality was lowest at BMI levels of 20.0 to 24.9 kg/m2. Among women, compared with a BMI of 22.5 to 24.9 kg/m2, the HRs for death were as follows: BMI 15.0 to 18.4 kg/m2, 1.47; 18.5 to 19.9 kg/m2, 1.14; 20.0 to 22.4 kg/m2, 1.0; 25.0 to 29.9 kg/m2, 1.13; 30.0 to 34.9 kg/m2, 1.44; 35.0 to 39.9 kg/m2, 1.88; and 40.0 to 49.9 kg/m2, 2.51. Similar estimates were observed in men.42
Overweight was associated with significantly increased mortality resulting from DM or kidney disease and was not associated with increased mortality resulting from cancer or CVD in an analysis of 2004 data from NHANES. Obesity was associated with significantly increased mortality caused by CVD, some cancers, and DM or kidney disease. Obesity was associated with 13% of CVD deaths in 2004.43
A BMI paradox has been reported, with higher-BMI patients demonstrating favorable outcomes in CHF, hypertension, peripheral vascular disease, and CAD; similar findings have been seen for percent body fat. In AFFIRM, a multicenter trial of AF, obese patients had lower all-cause mortality (HR, 0.77; P=0.01) than normal-weight patients after multivariable adjustment over a 3-year follow-up period.44
Interestingly, among 2625 participants with new-onset DM, rates of total, CVD, and non-CVD mortality were higher among normal-weight people compared with overweight/obese participants, with adjusted HRs of 2.08 (95% CI, 1.52–2.85), 1.52 (95% CI, 0.89–2.58), and 2.32 (95% CI, 1.55–3.48), respectively.45
Calculations based on NHANES data from 1978 to 2006 suggest that the gains in life expectancy from smoking cessation are beginning to be outweighed by the loss of life expectancy related to obesity.46
Because of the increasing prevalence of obesity, the number of quality-adjusted life-years lost as a result of obesity is similar to or greater than that lost as a result of smoking, according to data from the BRFSS.47
Recent estimates suggest that reductions in smoking, cholesterol, BP, and physical inactivity levels resulted in a gain of 2 770 500 life-years; however, these gains were reduced by a loss of 715 000 life-years caused by the increased prevalence of obesity and DM.48
In a comparison of 5 different anthropometric variables (BMI, waist circumference, hip circumference, waist-to-hip ratio, and waist-to-height ratio) in 62 223 individuals from Norway with 12 years of follow-up from the HUNT 2 study, the risk of death per SD increase in each measure was 1.02 (95% CI, 0.99–1.06) for BMI, 1.10 (95% CI, 1.06–1.14) for waist circumference, 1.01 (95% CI, 0.97–1.05) for hip circumference, 1.15 (95% CI, 1.11–1.19) for waist-to-hip ratio, and 1.12 (95% CI, 1.08–1.16) for waist-to-height ratio. For CVD mortality, the risk of death per SD increase was 1.12 (95% CI, 1.06–1.20) for BMI, 1.19 (95% CI, 1.12–1.26) for waist circumference, 1.06 (95% CI, 1.00–1.13) for hip circumference, 1.23 (95% CI, 1.16–1.30) for waist-to-hip ratio, and 1.24 (95% CI, 1.16–1.31) for waist-to-height ratio.49
According to data from the NCDR, among patients presenting with STEMI and a BMI ≥40 kg/m2, in-hospital mortality rates were higher for patients with class III obesity (OR, 1.64; 95% CI, 1.32–2.03) when class I obesity was used as the referent.50
In a study of 22 203 women and men from England and Scotland, metabolically unhealthy obese individuals were at an increased risk of all-cause mortality compared with metabolically healthy obese individuals (HR, 1.72; 95% CI, 1.23–2.41).51
Cost
If current trends in the growth of obesity continue, total healthcare costs attributable to obesity could reach $861 to $957 billion by 2030, which would account for 16% to 18% of US health expenditures.52
According to NHANES I data linked to Medicare and mortality records, obese 45-year-olds had lifetime Medicare costs of $163 000 compared with $117 000 among those with normal weight by the time they reached 65 years of age.53
The total excess cost related to the current prevalence of adolescent overweight and obesity is estimated to be $254 billion ($208 billion in lost productivity secondary to premature morbidity and mortality and $46 billion in direct medical costs).54
According to 2006 MEPS and 2006 BRFSS data, annual medical expenditures would be 6.7% to 10.7% lower in the absence of obesity.55
According to data from the Medicare Current Beneficiary Survey from 1997 to 2006, in 1997, expenditures for a Part A and Part B services beneficiary were $6832 for a normal-weight individual, which was more than for overweight ($5473) or obese ($5790) individuals. However, over time, expenses increased more rapidly for overweight and obese individuals.56
The costs of obesity are high: Obese people pay on average $1429 (42%) more for healthcare costs than normal-weight individuals. For obese beneficiaries, Medicare pays $1723 more, Medicaid pays $1021 more, and private insurers pay $1140 more than for beneficiaries who are at normal weight. Similarly, obese people have 46% higher inpatient costs and 27% more outpatient visits and spend 80% more on prescription drugs.57
Bariatric Surgery
Patients with BMI >40 kg/m2 or >35 kg/m2 with an obesity-related comorbidity are eligible for gastric bypass surgery, which is typically performed as either a Roux-en-Y gastric bypass or a biliopancreatic diversion.
According to the 2006 NHDS, the incidence of bariatric surgery was estimated at 113 000 cases per year, with costs of nearly $1.5 billion annually.58
In a large bariatric surgery cohort, the prevalence of high 10-year predicted CVD risk was 36.5%,59 but 76% of those with low 10-year risk had high lifetime predicted CVD risk. The corresponding prevalence in US adults is 18% and 56%, respectively.60
Among obese Swedish patients undergoing bariatric surgery and followed up for up to 15 years, maximum weight loss was 32%. The risk of death was 0.76 among those who underwent bariatric surgery compared with matched control subjects.57 More recent data examining MI and stroke showed that bariatric surgery was associated with fewer CVD deaths (HR, 0.47; 95% CI, 0.29–0.76) and fewer strokes (HR, 0.67; 95% CI, 0.54–0.83) than in the control group. However, CVD risk was related to baseline CVD risk factors rather than to baseline BMI or 2-year weight change.61
Among 641 patients followed up for 10 years compared with 627 matched control subjects, after 2 years of follow-up, 72% of the surgically treated patients versus 21% of the control patients had remission of their DM; at 10 years of follow-up, results were 36% and 13%, respectively. Similar results have been observed for hypertension, elevated triglycerides, and low HDL cholesterol.62
According to retrospective data from the United States, among 9949 patients who underwent gastric bypass surgery, after a mean of 7 years, long-term mortality was 40% lower among the surgically treated patients than among obese control subjects. Specifically, cancer mortality was reduced by 60%, DM mortality by 92%, and CAD mortality by 56%. Nondisease death rates (eg, accidents, suicide) were 58% higher in the surgery group.63
A recent retrospective cohort from the Veterans Affairs medical system showed that in a propensity-matched analysis, bariatric surgery was not associated with reduced mortality compared with obese control subjects (time-adjusted HR, 0.94; 95% CI, 0.64–1.39).64
Two recent randomized controlled trials were performed that randomized bariatric surgery compared with intensive medical treatment among patients with type 2 DM. The first study randomized 150 patients and conducted 12-month follow-up; this study showed that glycemic control improved (6.4%) and weight loss was greater (29.4 versus 5.4 kg) in the surgical arm.65 The second trial randomized 60 patients to bariatric surgery versus medical therapy and conducted follow-up for 24 months. The results showed that DM remission occurred in 75% of the group that underwent gastric bypass surgery compared with 0% of those in the medical treatment arm, with HbA1c values of 6.35% in the surgical arm compared with 7.69% in the medical treatment arm.66
Of 120 patients with type 2 DM and a BMI between 30 and 39.9 kg/m2, 60 who were randomized to Roux-en-Y gastric bypass were almost 5-fold (OR, 4.8; 95% CI, 1.9–11.7) more likely to achieve an HbA1c <7.0% at 12-month follow-up. However, there were 22 serious adverse events in the intervention arm, including early and late perioperative complications and nutritional deficiencies.67
A recent cost-effectiveness study of laparoscopic adjustable gastric banding showed that after 5 years, $4970 was saved in medical expenses; if indirect costs were included (absenteeism and presenteeism), savings increased to $6180 and $10 960, respectively.68 However, when expressed per quality-adjusted life expectancy, only $6600 was gained for laparoscopic gastric bypass, $6200 for laparoscopic adjustable gastric band, and $17 300 for open Roux-en-Y gastric bypass, none of which exceeded the standard $50 000 per quality-adjusted life expectancy gained.69
Adolescents (aged 10–19 years old) underwent bariatric surgery at a rate of 0.8/100 000 procedures, which increased to 2.3/100 000 in 2003 and remained constant by 2009 at 2.4/100 000.70
- 1.Klein S, Burke LE, Bray GA, Blair S, Allison DB, Pi-Sunyer X, Hong Y, Eckel RH on behalf of the American Heart Association Council on Nutrition, Physical Activity, and Metabolism. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2004;110:2952–2967. doi: 10.1161/01.CIR.0000145546.97738.1E. [DOI] [PubMed] [Google Scholar]
- 2.Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 3.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch Pediatr Adolesc Med. 2009;163:344–348. doi: 10.1001/archpediatrics.2009.18. [DOI] [PubMed] [Google Scholar]
- 6.Robinson WR, Gordon-Larsen P, Kaufman JS, Suchindran CM, Stevens J. The female-male disparity in obesity prevalence among black American young adults: contributions of sociodemographic characteristics of the childhood family. Am J Clin Nutr. 2009;89:1204–1212. doi: 10.3945/ajcn.2007.25751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003–2007 [published correction appears in Ann Epidemiol. 2010;20:250] Ann Epidemiol. 2010;20:40–52. doi: 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Obesity Among Low-Income Preschool Children Fact Sheet. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention; 2012. [Accessed July 30, 2012]. http://www.cdc.gov/obesity/downloads/PedNSSFactSheet.pdf. [Google Scholar]
- 9.Ali MK, Bullard KM, Beckles GL, Stevens MR, Barker L, Narayan KM, Imperatore G. Household income and cardiovascular disease risks in U.S. children and young adults: analyses from NHANES 1999–2008. Diabetes Care. 2011;34:1998–2004. doi: 10.2337/dc11-0792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The NS, Suchindran C, North KE, Popkin BM, Gordon-Larsen P. Association of adolescent obesity with risk of severe obesity in adulthood. JAMA. 2010;304:2042–2047. doi: 10.1001/jama.2010.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis AM, Bennett KJ, Befort C, Nollen N. Obesity and related health behaviors among urban and rural children in the United States: data from the National Health and Nutrition Examination Survey 2003–2004 and 2005–2006. J Pediatr Psychol. 2011;36:669–676. doi: 10.1093/jpepsy/jsq117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Behavioral Risk Factor Surveillance System: prevalence and trends data. [Accessed July 5, 2011];Centers for Disease Control and Prevention Web site. http://apps.nccd.cdc.gov/brfss/index.asp.
- 13.Centers for Disease Control and Prevention (CDC) State-specific prevalence of obesity among adults: United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57:765–768. [PubMed] [Google Scholar]
- 14.Blackwell D, Lucas J, Clarke T. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. National Center for Health Statistics. Vital Health Stat 10. In press. [PubMed] [Google Scholar]
- 15.Barnes PM, Adams PF, Powell-Griner E. Advance Data From Vital and Health Statistics; No. 394. Hyattsville, MD: National Center for Health Statistics; 2008. Health characteristics of the Asian adult population: United States, 2004–2006. [PubMed] [Google Scholar]
- 16.Agency for Healthcare Research and Quality. 2008 National Healthcare Disparities Report. Rockville, MD: US Department of Health and Human Services, Agency for Healthcare Research and Quality; Mar, 2009. AHRQ publication No. 09-0002. [Google Scholar]
- 17.Burke GL, Bertoni AG, Shea S, Tracy R, Watson KE, Blumenthal RS, Chung H, Carnethon MR. The impact of obesity on cardiovascular disease risk factors and subclinical vascular disease: the Multi-Ethnic Study of Atherosclerosis. Arch Intern Med. 2008;168:928–935. doi: 10.1001/archinte.168.9.928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fakhouri TH, Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among older adults in the United States, 2007–2010. NCHS Data Brief. 2012;(106):1–8. [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention, National Center for Health Statistics. NCHS Health E-Stat: prevalence of overweight, infants and children less than 2 years of age: United States, 2003–2004. [Accessed September 28, 2010];Centers for Disease Control and Prevention Web site. http://www.cdc.gov/nchs/data/hestat/overweight/overweight_child_under02.htm. Updated April 7, 2010.
- 20.Broyles S, Katzmarzyk PT, Srinivasan SR, Chen W, Bouchard C, Freedman DS, Berenson GS. The pediatric obesity epidemic continues unabated in Bogalusa, Louisiana. Pediatrics. 2010;125:900–905. doi: 10.1542/peds.2009-2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention (CDC) Vital signs: state-specific obesity prevalence among adults: United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:951–955. [PubMed] [Google Scholar]
- 22.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 23.Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, Sherry B, Dietz W. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012;42:563–570. doi: 10.1016/j.amepre.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 24.Daniels SR, Jacobson MS, McCrindle BW, Eckel RH, Sanner BM. American Heart Association Childhood Obesity Research Summit: executive summary. Circulation. 2009;119:2114–2123. doi: 10.1161/CIRCULATIONAHA.109.192215. [DOI] [PubMed] [Google Scholar]
- 25.Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Sun C, Cheung M, Viikari JS, Dwyer T, Raitakari OT. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876–1885. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- 25a.Kozak AT, Daviglus ML, Chan C, Kiefe CI, Jacobs DR, Jr, Liu K. Relationship of body mass index in young adulthood and health-related quality of life two decades later: the Coronary Artery Risk Development in Young Adults study. Int J Obes (Lond) 2011;35:134–141. doi: 10.1038/ijo.2010.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fox CS, Pencina MJ, Meigs JB, Vasan RS, Levitzky YS, D’Agostino RB., Sr Trends in the incidence of type 2 diabetes mellitus from the 1970s to the 1990s: the Framingham Heart Study. Circulation. 2006;113:2914–2918. doi: 10.1161/CIRCULATIONAHA.106.613828. [DOI] [PubMed] [Google Scholar]
- 27.Goff DC, Jr, Gillespie C, Howard G, Labarthe DR. Is the obesity epidemic reversing favorable trends in blood pressure? Evidence from cohorts born between 1890 and 1990 in the United States. Ann Epidemiol. 2012;22:554–561. doi: 10.1016/j.annepidem.2012.04.021. [DOI] [PubMed] [Google Scholar]
- 28.Emerging Risk Factors Collaboration. Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, Sarwar N, Kizer JR, Lawlor DA, Nordestgaard BG, Ridker P, Salomaa V, Stevens J, Woodward M, Sattar N, Collins R, Thompson SG, Whitlock G, Danesh J. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown WV, Fujioka K, Wilson PW, Woodworth KA. Obesity: why be concerned? Am J Med. 2009;122(suppl 1):S4–S11. doi: 10.1016/j.amjmed.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Lee CM, Colagiuri S, Ezzati M, Woodward M. The burden of cardiovascular disease associated with high body mass index in the Asia-Pacific region. Obes Rev. 2011;12:e454–e459. doi: 10.1111/j.1467-789X.2010.00849.x. [DOI] [PubMed] [Google Scholar]
- 31.Strazzullo P, D’Elia L, Cairella G, Garbagnati F, Cappuccio FP, Scalfi L. Excess body weight and incidence of stroke: meta-analysis of prospective studies with 2 million participants. Stroke. 2010;41:e418–426. doi: 10.1161/STROKEAHA.109.576967. [DOI] [PubMed] [Google Scholar]
- 32.Anstey KJ, Cherbuin N, Budge M, Young J. Body mass index in midlife and late-life as a risk factor for dementia: a meta-analysis of prospective studies. Obes Rev. 2011;12:e426–e437. doi: 10.1111/j.1467-789X.2010.00825.x. [DOI] [PubMed] [Google Scholar]
- 33.Loef M, Walach H. Midlife obesity and dementia: meta-analysis and adjusted forecast of dementia prevalence in the United States and China. Obesity (Silver Spring) 2013;21:E51–E55. doi: 10.1002/oby.20037. [DOI] [PubMed] [Google Scholar]
- 34.Sjöström CD, Lystig T, Lindroos AK. Impact of weight change, secular trends and ageing on cardiovascular risk factors: 10-year experiences from the SOS study. Int J Obes (Lond) 2011;35:1413–1420. doi: 10.1038/ijo.2010.282. [DOI] [PubMed] [Google Scholar]
- 35.Goodpaster BH, Delany JP, Otto AD, Kuller L, Vockley J, South-Paul JE, Thomas SB, Brown J, McTigue K, Hames KC, Lang W, Jakicic JM. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. JAMA. 2010;304:1795–1802. doi: 10.1001/jama.2010.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ma J, Flanders WD, Ward EM, Jemal A. Body mass index in young adulthood and premature death: analyses of the US National Health Interview Survey linked mortality files. Am J Epidemiol. 2011;174:934–944. doi: 10.1093/aje/kwr169. [DOI] [PubMed] [Google Scholar]
- 38.McGee DL Diverse Populations Collaboration. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol. 2005;15:87–97. doi: 10.1016/j.annepidem.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 39.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 40.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prospective Studies Collaboration. Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, Moore SC, Tobias GS, Anton-Culver H, Freeman LB, Beeson WL, Clipp SL, English DR, Folsom AR, Freedman DM, Giles G, Hakansson N, Henderson KD, Hoffman-Bolton J, Hoppin JA, Koenig KL, Lee IM, Linet MS, Park Y, Pocobelli G, Schatzkin A, Sesso HD, Weiderpass E, Willcox BJ, Wolk A, Zeleniuch-Jacquotte A, Willett WC, Thun MJ. Body-mass index and mortality among 1.46 million white adults [published correction appears in N Engl J Med. 2011;365:869] N Engl J Med. 2010;363:2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 44.Badheka AO, Rathod A, Kizilbash MA, Garg N, Mohamad T, Afonso L, Jacob S. Influence of obesity on outcomes in atrial fibrillation: yet another obesity paradox. Am J Med. 2010;123:646–651. doi: 10.1016/j.amjmed.2009.11.026. [DOI] [PubMed] [Google Scholar]
- 45.Carnethon MR, De Chavez PJ, Biggs ML, Lewis CE, Pankow JS, Bertoni AG, Golden SH, Liu K, Mukamal KJ, Campbell-Jenkins B, Dyer AR. Association of weight status with mortality in adults with incident diabetes [published correction appears in JAMA. 2012;308:2085] JAMA. 2012;308:581–590. doi: 10.1001/jama.2012.9282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on U.S. life expectancy. N Engl J Med. 2009;361:2252–2260. doi: 10.1056/NEJMsa0900459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jia H, Lubetkin EI. Trends in quality-adjusted life-years lost contributed by smoking and obesity. Am J Prev Med. 2010;38:138–144. doi: 10.1016/j.amepre.2009.09.043. [DOI] [PubMed] [Google Scholar]
- 48.Capewell S, Hayes DK, Ford ES, Critchley JA, Croft JB, Greenlund KJ, Labarthe DR. Life-years gained among US adults from modern treatments and changes in the prevalence of 6 coronary heart disease risk factors between 1980 and 2000. Am J Epidemiol. 2009;170:229–236. doi: 10.1093/aje/kwp150. [DOI] [PubMed] [Google Scholar]
- 49.Petursson H, Sigurdsson JA, Bengtsson C, Nilsen TI, Getz L. Body configuration as a predictor of mortality: comparison of five anthropometric measures in a 12 year follow-up of the Norwegian HUNT 2 study. PLoS ONE. 2011;6:e26621. doi: 10.1371/journal.pone.0026621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Das SR, Alexander KP, Chen AY, Powell-Wiley TM, Diercks DB, Peterson ED, Roe MT, de Lemos JA. Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with ST-segment elevation myocardial infarction: results from the NCDR (National Cardiovascular Data Registry) J Am Coll Cardiol. 2011;58:2642–2650. doi: 10.1016/j.jacc.2011.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab. 2012;97:2482–2488. doi: 10.1210/jc.2011-3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring) 2008;16:2323–2330. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
- 53.Cai L, Lubitz J, Flegal KM, Pamuk ER. The predicted effects of chronic obesity in middle age on Medicare costs and mortality. Med Care. 2010;48:510–517. doi: 10.1097/MLR.0b013e3181dbdb20. [DOI] [PubMed] [Google Scholar]
- 54.Lightwood J, Bibbins-Domingo K, Coxson P, Wang YC, Williams L, Goldman L. Forecasting the future economic burden of current adolescent overweight: an estimate of the coronary heart disease policy model. Am J Public Health. 2009;99:2230–2237. doi: 10.2105/AJPH.2008.152595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Trogdon JG, Finkelstein EA, Feagan CW, Cohen JW. State- and payer-specific estimates of annual medical expenditures attributable to obesity. Obesity (Silver Spring) 2012;20:214–220. doi: 10.1038/oby.2011.169. [DOI] [PubMed] [Google Scholar]
- 56.Alley D, Lloyd J, Shaffer T, Stuart B. Changes in the association between body mass index and Medicare costs, 1997–2006. Arch Intern Med. 2012;172:277–278. doi: 10.1001/archinternmed.2011.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 58.Livingston EH. The incidence of bariatric surgery has plateaued in the U.S. Am J Surg. 2010;200:378–385. doi: 10.1016/j.amjsurg.2009.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mackey RH, Belle SH, Courcoulas AP, Dakin GF, Deveney CW, Flum DR, Garcia L, King WC, Kuller LH, Mitchell JE, Pomp A, Pories WJ, Wolfe BM Longitudinal Assessment of Bariatric Surgery Consortium Writing Group. Distribution of 10-year and lifetime predicted risk for cardiovascular disease prior to surgery in the longitudinal assessment of Bariatric Surgery-2 Study. Am J Cardiol. 2012;110:1130–1137. doi: 10.1016/j.amjcard.2012.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Marma AK, Berry JD, Ning H, Persell SD, Lloyd-Jones DM. Distribution of 10-year and lifetime predicted risks for cardiovascular disease in US adults: findings from the National Health and Nutrition Examination Survey 2003 to 2006. Circ Cardiovasc Qual Outcomes. 2010;3:8–14. doi: 10.1161/CIRCOUTCOMES.109.869727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H, Ahlin S, Anveden Å, Bengtsson C, Bergmark G, Bouchard C, Carlsson B, Dahlgren S, Karlsson J, Lindroos AK, Lönroth H, Narbro K, Näslund I, Olbers T, Svensson PA, Carlsson LM. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65. doi: 10.1001/jama.2011.1914. [DOI] [PubMed] [Google Scholar]
- 62.Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, Dahlgren S, Larsson B, Narbro K, Sjöström CD, Sullivan M, Wedel H Swedish Obese Subjects Study Scientific Group. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–2693. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 63.Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD, Lamonte MJ, Stroup AM, Hunt SC. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753–761. doi: 10.1056/NEJMoa066603. [DOI] [PubMed] [Google Scholar]
- 64.Maciejewski ML, Livingston EH, Smith VA, Kavee AL, Kahwati LC, Henderson WG, Arterburn DE. Survival among high-risk patients after bariatric surgery. JAMA. 2011;305:2419–2426. doi: 10.1001/jama.2011.817. [DOI] [PubMed] [Google Scholar]
- 65.Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, Thomas S, Abood B, Nissen SE, Bhatt DL. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–1576. doi: 10.1056/NEJMoa1200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Leccesi L, Nanni G, Pomp A, Castagneto M, Ghirlanda G, Rubino F. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–1585. doi: 10.1056/NEJMoa1200111. [DOI] [PubMed] [Google Scholar]
- 67.Ikramuddin S, Korner J, Lee WJ, Connett JE, Inabnet WB, Billington CJ, Thomas AJ, Leslie DB, Chong K, Jeffery RW, Ahmed L, Vella A, Chuang LM, Bessler M, Sarr MG, Swain JM, Laqua P, Jensen MD, Bantle JP. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA. 2013;309:2240–2249. doi: 10.1001/jama.2013.5835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Finkelstein EA, Allaire BT, Dibonaventura MD, Burgess SM. Incorporating indirect costs into a cost-benefit analysis of laparoscopic adjustable gastric banding. Value Health. 2012;15:299–304. doi: 10.1016/j.jval.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 69.Wang BC, Wong ES, Alfonso-Cristancho R, He H, Flum DR, Arterburn DE, Garrison LP, Sullivan SD. Cost-effectiveness of bariatric surgical procedures for the treatment of severe obesity. [Accessed June 14, 2013];Eur J Health Econ. 2013 Mar 24; doi: 10.1007/s10198-013-0472-5. http://link.springer.com/article/10.1007%2Fs10198-013-0472-5. [DOI] [PMC free article] [PubMed]
- 70.Kelleher DC, Merrill CT, Cottrell LT, Nadler EP, Burd RS. Recent national trends in the use of adolescent inpatient bariatric surgery: 2000 through 2009. JAMA Pediatr. 2013;167:126–132. doi: 10.1001/2013.jamapediatrics.286. [DOI] [PubMed] [Google Scholar]
- 71.American Medical Association Expert Task Force on Childhood Obesity. [Accessed September 20, 2012];Appendix: Expert Committee recommendations on the assessment, prevention, and treatment of child and adolescent overweight and obesity. 2007 Jan 25; http://www.ama-assn.org/ama1/pub/upload/mm/433/ped_obesity_recs.pdf.
- 72.Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Whittle L, Lim C, Wechsler H Centers for Disease Control and Prevention (CDC) Youth Risk Behavior Surveillance: United States, 2011. MMWR Surveill Summ. 2012;61:1–162. [PubMed] [Google Scholar]
- 73.National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD: National Center for Health Statistics; 2011. [Accessed August 1, 2012]. http://www.cdc.gov/nchs/data/hus/hus11.pdf. [PubMed] [Google Scholar]
7. Family History and Genetics
See Tables 7-1 through 7-3.
Table 7-1.
OR for Combinations of Parental Heart Attack History
| OR (95% CI) | |
|---|---|
| No family history | 1.00 |
| One parent with heart attack ≥50 y of age | 1.67 (1.55–1.81) |
| One parent with heart attack <50 y of age | 2.36 (1.89–2.95) |
| Both parents with heart attack ≥50 y of age | 2.90 (2.30–3.66) |
| Both parents with heart attack, one <50 y of age | 3.26 (1.72–6.18) |
| Both parents with heart attack, both <50 y of age | 6.56 (1.39–30.95) |
CI indicates confidence interval; OR, odds ratio.
Data derived from Chow et al.4
Table 7-3.
Heritability of CVD Risk Factors From the FHS
| Trait | Heritability |
|---|---|
| ABI | 0.2124 |
| SBP | 0.4225 |
| DBP | 0.3925 |
| Left ventricular mass | 0.24 to 0.3226 |
| BMI | 0.37 (mean age 40 y) to 0.52 (mean age 60 y)27 |
| Waist circumference | 0.4128 |
| Visceral abdominal fat | 0.3629 |
| Subcutaneous abdominal fat | 0.5729 |
| Fasting glucose | 0.3430 |
| HbA1c | 0.2730 |
| Triglycerides | 0.4831 |
| HDL cholesterol | 0.5231 |
| Total cholesterol | 0.5731 |
| LDL cholesterol | 0.5931 |
| Estimated GFR | 0.3332 |
ABI indicates ankle-brachial index; BMI, body mass index; CVD, cardiovascular disease; DBP, diastolic blood pressure; FHS, Framingham Heart Study; GFR, glomerular filtration rate; HbA1c, glycosylated hemoglobin; HDL, high-density lipoprotein; LDL, low-density lipoprotein; and SBP, systolic blood pressure.
Biologically related first-degree relatives (siblings, offspring and parents) share roughly 50% of their genetic variation with one another. This constitutes much greater sharing of genetic variation than with a randomly selected person from the population, and thus, when a trait aggregates within a family, this lends evidence for a genetic risk factor for the trait. Similarly, racial/ethnic minorities are more likely to share their genetic variation within their demographic than with other demographics. Familial aggregation of CVD may be related to aggregation of specific behaviors (eg, smoking, alcohol use) or risk factors (eg, hypertension, DM, obesity) that may themselves have environmental and genetic contributors. Unlike classic mendelian genetic risk factors, whereby usually 1 mutation directly causes 1 disease, a complex trait’s genetic contributors may increase risk without necessarily always causing the condition. The effect size of any specific contributor to risk may be small but widespread throughout a population, or may be large but affect only a small population, or may have an enhanced risk when an environmental contributor is present. Although the breadth of all genetic research into CVD is beyond the scope of this chapter, we present a summary of evidence that a genetic risk for CVD is likely, as well as a summary of evidence on the most consistently replicated genetic markers for HD and stroke identified to date.
Abbreviations Used in Chapter 7
| AAA | abdominal aortic aneurysm |
| ABI | ankle-brachial index |
| AF | atrial fibrillation |
| BMI | body mass index |
| CAC | coronary artery calcification |
| CAD | coronary artery disease |
| CARDIoGRAMplusC4D | Coronary Artery Disease Genome-wide Replication and Meta-Analysis (CARDIOGRAM) plus the Coronary Artery Disease (C4D) Genetics Consortium |
| CHD | coronary heart disease |
| CI | confidence interval |
| CVD | cardiovascular disease |
| DBP | diastolic blood pressure |
| DM | diabetes mellitus |
| FHS | Framingham Heart Study |
| GFR | glomerular filtration rate |
| HbA1c | hemoglobin A1c (glycosylated hemoglobin) |
| HD | heart disease |
| HDL | high-density lipoprotein |
| HF | heart failure |
| LDL | low-density lipoprotein |
| MI | myocardial infarction |
| NHANES | National Health and Nutrition Examination Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| OR | odds ratio |
| SBP | systolic blood pressure |
| SE | standard error |
| SNP | single-nucleotide polymorphism |
Family History
Prevalence
-
Among adults ≥20 years of age, 12.6% (SE 0.5%) reported having a parent or sibling with a heart attack or angina before the age of 50 years. The racial/ethnic breakdown is as follows (NHANES 2007–2010, unpublished NHLBI tabulation):
For non-Hispanic whites, 12.4% (SE 0.7%) for men, 14.9% (SE 0.9%) for women
For non-Hispanic blacks, 8.1% (SE 0.8%) for men, 13.0% (SE 0.9%) for women
For Mexican Americans, 8.1% (SE 0.9%) for men, 10.0% (SE 1.1%) for women
For other Hispanics, 8.8% (SE 1.5%) for men, 12.0% (SE 1.2%) for women
For other races, 8.7% (SE 2.1%) for men, 10.7% (SE 2.6%) for women
-
HD occurs as people age, and those without a family history of HD may survive longer, so the prevalence of family history will vary depending on the age at which it is assessed. The breakdown of reported family history of heart attack by age in the US population as measured by NHANES is as follows (NHANES 2007–2010, unpublished NHLBI tabulation):
Age 20 to 39 years, 8.4% (SE 0.9%) for men, 10.3% (SE 0.7%) for women
Age 40 to 59 years, 12.8% (SE 0.9%) for men, 15.3% (SE 1.1%) for women
Age 60 to 79 years, 13.7% (SE 0.9%) for men, 17.5% (SE 1.2%) for women
Age ≥80 years, 9.8% (SE 1.5%) for men, 13.7% (SE 0.6%) for women
In the multigenerational FHS, only 75% of participants with a documented parental history of a heart attack before age 55 years reported that history when asked.1
Impact of Family History
Premature paternal history of a heart attack has been shown to approximately double the risk of a heart attack in men and increase the risk in women by ≈70%.2,3
History of a heart attack in both parents increases the risk of heart attack, especially when 1 parent had a premature heart attack4 (Table 7-1).
Sibling history of HD has been shown to increase the odds of HD in men and women by ≈50%.5
Premature family history of angina, MI, angioplasty, or bypass surgery increased the lifetime risk by ≈50% for both HD (from 8.9% to 13.7%) and CVD mortality (from 14.1% to 21%).6
Similarly, parental history of AF is associated with ≈80% increased odds of AF in men and women,7 and a history of stroke in a first-degree relative increases the odds of stroke in men and women by ≈50%.8
Genetics
Heart Disease
Genome-wide association is a robust technique to identify associations between genotypes and phenotypes. Table 7-2 presents results from the CARDIoGRAMplusC4D Consortium, which represents the largest genetic study of CAD to date. Although the ORs are modest, ranging from 1.06 to 1.51 per copy of the risk allele (individuals may harbor up to 2 copies of a risk allele), these are common alleles, which suggests that the attributable risk may be substantial. Additional analysis suggested that loci associated with CAD were involved in lipid metabolism and inflammation pathways.9
The relationship between genetic variants associated with CHD and measured CHD risk factors is complex, with some genetic markers associated with multiple risk factors and other markers showing no association with risk factors.10
Genetic markers discovered thus far have not been shown to add to cardiovascular risk prediction tools beyond current models that incorporate family history.11 Genetic markers have also not been shown to improve prediction of subclinical atherosclerosis beyond traditional risk factors.12 However, an association between genetic markers and coronary calcification has been seen.13
The most consistently replicated genetic marker for HD in European-derived populations is located at 9p21.3. At this single-nucleotide polymorphism, ≈27% of the white population is estimated to have 0 risk alleles, 50% is estimated to have 1 risk allele, and the remaining 23% is estimated to have 2 risk alleles.14
The 10-year HD risk for a 65-year-old man with 2 risk alleles at 9p21.3 and no other traditional risk factors is ≈13.2%, whereas a similar man with 0 alleles would have a 10-year risk of ≈9.2%. The 10-year HD risk for a 40-year-old woman with 2 alleles and no other traditional risk factors is ≈2.4%, whereas a similar woman with 0 alleles would have a 10-year risk of ≈1.7%.14
Variation at the 9p21.3 region also increases the risk of HF15 and sudden death.16 Associations have also been observed between the 9p21.3 region and CAC.17,18 Additionally, stronger associations have been found between variation at 9p21.3 and earlier17,18 and more severe19 heart attacks. The biological mechanism underpinning the association of genetic variation in the 9p21 region with disease outcomes is still under investigation.
Table 7-2.
Validated SNPs for CAD, the Nearest Gene, and the OR From the CARDIoGRAMplusC4D Consortium
| SNP | Chromosome | Gene | Effect Size (OR) | Effect Allele Frequency |
|---|---|---|---|---|
| rs602633 | 1 | SORT1 | 1.12 | 0.77 |
| rs17464857 | 1 | MIA3 | 1.05 | 0.87 |
| rs17114036 | 1 | PPAP2B | 1.11 | 0.91 |
| rs11206510 | 1 | PCSK9 | 1.06 | 0.84 |
| rs4845625 | 1 | IL6R | 1.04 | 0.47 |
| rs6725887 | 2 | WDR12 | 1.12 | 0.11 |
| rs515135 | 2 | APOB | 1.08 | 0.82 |
| rs2252641 | 2 | ZEB2-AC074093.1 | 1.04 | 0.46 |
| rs1561198 | 2 | VAMP5-VAMP8-GGCX | 1.05 | 0.45 |
| rs6544713 | 2 | ABCG5-ABCG8 | 1.06 | 0.30 |
| rs9818870 | 3 | MRAS | 1.07 | 0.14 |
| rs7692387 | 4 | GUCY1A3 | 1.06 | 0.81 |
| rs1878406 | 4 | EDNRA | 1.06 | 0.15 |
| rs273909 | 5 | SLC22A4-SLC22A5 | 1.09 | 0.14 |
| rs12205331 | 6 | ANKS1A | 1.04 | 0.81 |
| rs9369640 | 6 | PHACTR1 | 1.09 | 0.65 |
| rs12190287 | 6 | TCF21 | 1.07 | 0.59 |
| rs3798220 | 6 | LPA | 1.28 | 0.01 |
| rs10947789 | 6 | KCNK5 | 1.06 | 0.76 |
| rs4252120 | 6 | PLG | 1.06 | 0.73 |
| rs11556924 | 7 | ZC3HC1 | 1.08 | 0.65 |
| rs12539895 | 7 | - | 1.08 | 0.19 |
| rs2023938 | 7 | HDAC9 | 1.07 | 0.10 |
| rs264 | 8 | LPL | 1.05 | 0.86 |
| rs2954029 | 8 | TRIB1 | 1.04 | 0.55 |
| rs1333049 | 9 | CDKN2A, CDKN2B | 1.23 | 0.47 |
| rs579459 | 9 | ABO | 1.07 | 0.21 |
| rs2505083 | 10 | KIAA1462 | 1.06 | 0.42 |
| rs501120 | 10 | CXCL12 | 1.07 | 0.83 |
| rs12413409 | 10 | CYP17A1-CNNM2-NT5C2 | 1.10 | 0.89 |
| rs2246833 | 10 | LIPA | 1.06 | 0.38 |
| rs9326246 | 11 | ZNF259-APOA5-A4-C3-A1 | 1.09 | 0.10 |
| rs974819 | 11 | PDGFD | 1.07 | 0.29 |
| rs3184504 | 12 | SH2B3 | 1.07 | 0.40 |
| rs4773144 | 13 | COL4A1-COL4A2 | 1.07 | 0.42 |
| rs9319428 | 13 | FLT1 | 1.05 | 0.32 |
| rs2895811 | 14 | HHIPL1 | 1.06 | 0.43 |
| rs7173743 | 15 | ADAMTS7 | 1.07 | 0.58 |
| rs17514846 | 15 | FURIN-FES | 1.05 | 0.44 |
| rs2281727 | 17 | SMG6-SRR | 1.05 | 0.36 |
| rs12936587 | 17 | RASD1-SMCR3-PEMT | 1.06 | 0.59 |
| rs15563 | 17 | UBE2Z-GIP-ATP5G1-SNF8 | 1.04 | 0.52 |
| rs1122608 | 19 | LDLR | 1.10 | 0.76 |
| rs2075650 | 19 | ApoE-ApoC1 | 1.11 | 0.14 |
| rs9982601 | 21 | KCNE2 | 1.13 | 0.13 |
CAD indicates coronary artery disease; CARDIoGRAMplusC4D, Coronary Artery Disease Genome-wide Replication and Meta-analysis (CARDIOGRAM) plus the Coronary Artery Disease (C4D) Genetics Consortium; OR, odds ratio; and SNP, single-nucleotide polymorphism.
Data derived from Deloukas et al.9
Stroke
The same 9p21.3 region has also been associated with intracranial aneurysm,20 AAA,21 and ischemic stroke.22
For large-vessel ischemic stroke, an association for large-vessel stroke with histone deacetylase 9 on chromosome 7p21.1 has been identified (>9000 subjects) and replicated (>12 000 subjects).22,23
CVD Risk Factors
Heritability is the ratio of genetically caused variation to the total variation of a trait or measure. Table 7-3 presents heritability estimates for standard CVD risk factors using data generated from the FHS. These data suggest that most CVD risk factors have at least moderate heritability.
- 1.Murabito JM, Nam BH, D’Agostino RB, Sr, Lloyd-Jones DM, O’Donnell CJ, Wilson PW. Accuracy of offspring reports of parental cardiovascular disease history: the Framingham Offspring Study. Ann Intern Med. 2004;140:434–440. doi: 10.7326/0003-4819-140-6-200403160-00010. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Nam BH, D’Agostino RB, Sr, Levy D, Murabito JM, Wang TJ, Wilson PW, O’Donnell CJ. Parental cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults: a prospective study of parents and offspring. JAMA. 2004;291:2204–2211. doi: 10.1001/jama.291.18.2204. [DOI] [PubMed] [Google Scholar]
- 3.Sesso HD, Lee IM, Gaziano JM, Rexrode KM, Glynn RJ, Buring JE. Maternal and paternal history of myocardial infarction and risk of cardiovascular disease in men and women. Circulation. 2001;104:393–398. doi: 10.1161/hc2901.093115. [DOI] [PubMed] [Google Scholar]
- 4.Chow CK, Islam S, Bautista L, Rumboldt Z, Yusufali A, Xie C, Anand SS, Engert JC, Rangarajan S, Yusuf S. Parental history and myocardial infarction risk across the world: the INTERHEART Study. J Am Coll Cardiol. 2011;57:619–627. doi: 10.1016/j.jacc.2010.07.054. [DOI] [PubMed] [Google Scholar]
- 5.Murabito JM, Pencina MJ, Nam BH, D’Agostino RB, Sr, Wang TJ, Lloyd-Jones D, Wilson PW, O’Donnell CJ. Sibling cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults. JAMA. 2005;294:3117–3123. doi: 10.1001/jama.294.24.3117. [DOI] [PubMed] [Google Scholar]
- 6.Bachmann JM, Willis BL, Ayers CR, Khera A, Berry JD. Association between family history and coronary heart disease death across long-term follow-up in men: the Cooper Center Longitudinal Study. Circulation. 2012;125:3092–3098. doi: 10.1161/CIRCULATIONAHA.111.065490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fox CS, Parise H, D’Agostino RB, Sr, Lloyd-Jones DM, Vasan RS, Wang TJ, Levy D, Wolf PA, Benjamin EJ. Parental atrial fibrillation as a risk factor for atrial fibrillation in offspring. JAMA. 2004;291:2851–2855. doi: 10.1001/jama.291.23.2851. [DOI] [PubMed] [Google Scholar]
- 8.Liao D, Myers R, Hunt S, Shahar E, Paton C, Burke G, Province M, Heiss G. Familial history of stroke and stroke risk: the Family Heart Study. Stroke. 1997;28:1908–1912. doi: 10.1161/01.str.28.10.1908. [DOI] [PubMed] [Google Scholar]
- 9.Deloukas P, Kanoni S, Willenborg C, Farrall M, Assimes TL, Thompson JR, Ingelsson E, Saleheen D, Erdmann J, Goldstein BA, Stirrups K, König IR, Cazier JB, Johansson A, Hall AS, Lee JY, Willer CJ, Chambers JC, Esko T, Folkersen L, Goel A, Grundberg E, Havulinna AS, Ho WK, Hopewell JC, Eriksson N, Kleber ME, Kristiansson K, Lundmark P, Lyytikäinen LP, Rafelt S, Shungin D, Strawbridge RJ, Thorleifsson G, Tikkanen E, Van Zuydam N, Voight BF, Waite LL, Zhang W, Ziegler A, Absher D, Altshuler D, Balmforth AJ, Barroso I, Braund PS, Burgdorf C, Claudi-Boehm S, Cox D, Dimitriou M, Do R, Doney AS, El Mokhtari N, Eriksson P, Fischer K, Fontanillas P, Franco-Cereceda A, Gigante B, Groop L, Gustafsson S, Hager J, Hallmans G, Han BG, Hunt SE, Kang HM, Illig T, Kessler T, Knowles JW, Kolovou G, Kuusisto J, Langenberg C, Langford C, Leander K, Lokki ML, Lundmark A, McCarthy MI, Meisinger C, Melander O, Mihailov E, Maouche S, Morris AD, Müller-Nurasyid M, Nikus K, Peden JF, Rayner NW, Rasheed A, Rosinger S, Rubin D, Rumpf MP, Schäfer A, Sivananthan M, Song C, Stewart AF, Tan ST, Thorgeirsson G, van der Schoot CE, Wagner PJ, Wells GA, Wild PS, Yang TP, Amouyel P, Arveiler D, Basart H, Boehnke M, Boerwinkle E, Brambilla P, Cambien F, Cupples AL, de Faire U, Dehghan A, Diemert P, Epstein SE, Evans A, Ferrario MM, Ferrières J, Gauguier D, Go AS, Goodall AH, Gudnason V, Hazen SL, Holm H, Iribarren C, Jang Y, Kähönen M, Kee F, Kim HS, Klopp N, Koenig W, Kratzer W, Kuulasmaa K, Laakso M, Laaksonen R, Lee JY, Lind L, Ouwehand WH, Parish S, Park JE, Pedersen NL, Peters A, Quertermous T, Rader DJ, Salomaa V, Schadt E, Shah SH, Sinisalo J, Stark K, Stefansson K, Trégouët DA, Virtamo J, Wallentin L, Wareham N, Zimmermann ME, Nieminen MS, Hengstenberg C, Sandhu MS, Pastinen T, Syvänen AC, Hovingh GK, Dedoussis G, Franks PW, Lehtimäki T, Metspalu A, Zalloua PA, Siegbahn A, Schreiber S, Ripatti S, Blankenberg SS, Perola M, Clarke R, Boehm BO, O’Donnell C, Reilly MP, März W, Collins R, Kathiresan S, Hamsten A, Kooner JS, Thorsteinsdottir U, Danesh J, Palmer CN, Roberts R, Watkins H, Schunkert H, Samani NJ Wellcome Trust Case Control Consortium, MuTHER Consortium, Diagram Consortium, CARDIOGENICS Consortium, CARDIoGRAMplusC4D Consortium. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet. 2013;45:25–33. doi: 10.1038/ng.2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Angelakopoulou A, Shah T, Sofat R, Shah S, Berry DJ, Cooper J, Palmen J, Tzoulaki I, Wong A, Jefferis BJ, Maniatis N, Drenos F, Gigante B, Hardy R, Laxton RC, Leander K, Motterle A, Simpson IA, Smeeth L, Thomson A, Verzilli C, Kuh D, Ireland H, Deanfield J, Caulfield M, Wallace C, Samani N, Munroe PB, Lathrop M, Fowkes FG, Marmot M, Whincup PH, Whittaker JC, de Faire U, Kivimaki M, Kumari M, Hypponen E, Power C, Humphries SE, Talmud PJ, Price J, Morris RW, Ye S, Casas JP, Hingorani AD. Comparative analysis of genome-wide association studies signals for lipids, diabetes, and coronary heart disease: Cardiovascular Biomarker Genetics Collaboration. Eur Heart J. 2012;33:393–407. doi: 10.1093/eurheartj/ehr225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holmes MV, Harrison S, Talmud PJ, Hingorani AD, Humphries SE. Utility of genetic determinants of lipids and cardiovascular events in assessing risk. Nat Rev Cardiol. 2011;8:207–221. doi: 10.1038/nrcardio.2011.6. [DOI] [PubMed] [Google Scholar]
- 12.Hernesniemi JA, Seppälä I, Lyytikäinen LP, Mononen N, Oksala N, Hutri-Kähönen N, Juonala M, Taittonen L, Smith EN, Schork NJ, Chen W, Srinivasan SR, Berenson GS, Murray SS, Laitinen T, Jula A, Kettunen J, Ripatti S, Laaksonen R, Viikari J, Kähönen M, Raitakari OT, Lehtimäki T. Genetic profiling using genome-wide significant coronary artery disease risk variants does not improve the prediction of subclinical atherosclerosis: the Cardiovascular Risk in Young Finns Study, the Bogalusa Heart Study and the Health 2000 Survey: a meta-analysis of three independent studies. PLoS One. 2012;7:e28931. doi: 10.1371/journal.pone.0028931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thanassoulis G, Peloso GM, Pencina MJ, Hoffmann U, Fox CS, Cupples LA, Levy D, D’Agostino RB, Hwang SJ, O’Donnell CJ. A genetic risk score is associated with incident cardiovascular disease and coronary artery calcium: the Framingham Heart Study. Circ Cardiovasc Genet. 2012;5:113–121. doi: 10.1161/CIRCGENETICS.111.961342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Palomaki GE, Melillo S, Bradley LA. Association between 9p21 genomic markers and heart disease: a meta-analysis. JAMA. 2010;303:648–656. doi: 10.1001/jama.2010.118. [DOI] [PubMed] [Google Scholar]
- 15.Yamagishi K, Folsom AR, Rosamond WD, Boerwinkle E ARIC Investigators. A genetic variant on chromosome 9p21 and incident heart failure in the ARIC study. Eur Heart J. 2009;30:1222–1228. doi: 10.1093/eurheartj/ehp087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Newton-Cheh C, Cook NR, VanDenburgh M, Rimm EB, Ridker PM, Albert CM. A common variant at 9p21 is associated with sudden and arrhythmic cardiac death. Circulation. 2009;120:2062–2068. doi: 10.1161/CIRCULATIONAHA.109.879049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Assimes TL, Knowles JW, Basu A, Iribarren C, Southwick A, Tang H, Absher D, Li J, Fair JM, Rubin GD, Sidney S, Fortmann SP, Go AS, Hlatky MA, Myers RM, Risch N, Quertermous T. Susceptibility locus for clinical and subclinical coronary artery disease at chromosome 9p21 in the multi-ethnic ADVANCE study. Hum Mol Genet. 2008;17:2320–2328. doi: 10.1093/hmg/ddn132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Donnell CJ, Cupples LA, D’Agostino RB, Fox CS, Hoffmann U, Hwang SJ, Ingellson E, Liu C, Murabito JM, Polak JF, Wolf PA, Demissie S. Genome-wide association study for subclinical atherosclerosis in major arterial territories in the NHLBI’s Framingham Heart Study. BMC Med Genet. 2007;8(suppl 1):S4. doi: 10.1186/1471-2350-8-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dandona S, Stewart AF, Chen L, Williams K, So D, O’Brien E, Glover C, Lemay M, Assogba O, Vo L, Wang YQ, Labinaz M, Wells GA, McPherson R, Roberts R. Gene dosage of the common variant 9p21 predicts severity of coronary artery disease. J Am Coll Cardiol. 2010;56:479–486. doi: 10.1016/j.jacc.2009.10.092. [DOI] [PubMed] [Google Scholar]
- 20.Foroud T, Koller DL, Lai D, Sauerbeck L, Anderson C, Ko N, Deka R, Mosley TH, Fornage M, Woo D, Moomaw CJ, Hornung R, Huston J, Meissner I, Bailey-Wilson JE, Langefeld C, Rouleau G, Connolly ES, Worrall BB, Kleindorfer D, Flaherty ML, Martini S, Mackey J, De Los Rios La Rosa F, Brown RD, Jr, Broderick JP FIA Study Investigators. Genome-wide association study of intracranial aneurysms confirms role of Anril and SOX17 in disease risk. Stroke. 2012;43:2846–2852. doi: 10.1161/STROKEAHA.112.656397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Helgadottir A, Thorleifsson G, Magnusson KP, Grétarsdottir S, Steinthorsdottir V, Manolescu A, Jones GT, Rinkel GJ, Blankensteijn JD, Ronkainen A, Jääskeläinen JE, Kyo Y, Lenk GM, Sakalihasan N, Kostulas K, Gottsäter A, Flex A, Stefansson H, Hansen T, Andersen G, Weinsheimer S, Borch-Johnsen K, Jorgensen T, Shah SH, Quyyumi AA, Granger CB, Reilly MP, Austin H, Levey AI, Vaccarino V, Palsdottir E, Walters GB, Jonsdottir T, Snorradottir S, Magnusdottir D, Gudmundsson G, Ferrell RE, Sveinbjornsdottir S, Hernesniemi J, Niemelä M, Limet R, Andersen K, Sigurdsson G, Benediktsson R, Verhoeven EL, Teijink JA, Grobbee DE, Rader DJ, Collier DA, Pedersen O, Pola R, Hillert J, Lindblad B, Valdimarsson EM, Magnadottir HB, Wijmenga C, Tromp G, Baas AF, Ruigrok YM, van Rij AM, Kuivaniemi H, Powell JT, Matthiasson SE, Gulcher JR, Thorgeirsson G, Kong A, Thorsteinsdottir U, Stefansson K. The same sequence variant on 9p21 associates with myocardial infarction, abdominal aortic aneurysm and intracranial aneurysm. Nat Genet. 2008;40:217–224. doi: 10.1038/ng.72. [DOI] [PubMed] [Google Scholar]
- 22.International Stroke Genetics Consortium (ISGC); Wellcome Trust Case Control Consortium 2 (WTCCC2) Bellenguez C, Bevan S, Gschwendtner A, Spencer CC, Burgess AI, Pirinen M, Jackson CA, Traylor M, Strange A, Su Z, Band G, Syme PD, Malik R, Pera J, Norrving B, Lemmens R, Freeman C, Schanz R, James T, Poole D, Murphy L, Segal H, Cortellini L, Cheng YC, Woo D, Nalls MA, Müller-Myhsok B, Meisinger C, Seedorf U, Ross-Adams H, Boonen S, Wloch-Kopec D, Valant V, Slark J, Furie K, Delavaran H, Langford C, Deloukas P, Edkins S, Hunt S, Gray E, Dronov S, Peltonen L, Gretarsdottir S, Thorleifsson G, Thorsteinsdottir U, Stefansson K, Boncoraglio GB, Parati EA, Attia J, Holliday E, Levi C, Franzosi MG, Goel A, Helgadottir A, Blackwell JM, Bramon E, Brown MA, Casas JP, Corvin A, Duncanson A, Jankowski J, Mathew CG, Palmer CN, Plomin R, Rautanen A, Sawcer SJ, Trembath RC, Viswanathan AC, Wood NW, Worrall BB, Kittner SJ, Mitchell BD, Kissela B, Meschia JF, Thijs V, Lindgren A, Macleod MJ, Slowik A, Walters M, Rosand J, Sharma P, Farrall M, Sudlow CL, Rothwell PM, Dichgans M, Donnelly P, Markus HS. Genome-wide association study identifies a variant in HDAC9 associated with large vessel ischemic stroke. Nat Genet. 2012;44:328–333. doi: 10.1038/ng.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Traylor M, Farrall M, Holliday EG, Sudlow C, Hopewell JC, Cheng YC, Fornage M, Ikram MA, Malik R, Bevan S, Thorsteinsdottir U, Nalls MA, Longstreth W, Wiggins KL, Yadav S, Parati EA, Destefano AL, Worrall BB, Kittner SJ, Khan MS, Reiner AP, Helgadottir A, Achterberg S, Fernandez-Cadenas I, Abboud S, Schmidt R, Walters M, Chen WM, Ringelstein EB, O’Donnell M, Ho WK, Pera J, Lemmens R, Norrving B, Higgins P, Benn M, Sale M, Kuhlenbäumer G, Doney AS, Vicente AM, Delavaran H, Algra A, Davies G, Oliveira SA, Palmer CN, Deary I, Schmidt H, Pandolfo M, Montaner J, Carty C, de Bakker PI, Kostulas K, Ferro JM, van Zuydam NR, Valdimarsson E, Nordestgaard BG, Lindgren A, Thijs V, Slowik A, Saleheen D, Paré G, Berger K, Thorleifsson G, Hofman A, Mosley TH, Mitchell BD, Furie K, Clarke R, Levi C, Seshadri S, Gschwendtner A, Boncoraglio GB, Sharma P, Bis JC, Gretarsdottir S, Psaty BM, Rothwell PM, Rosand J, Meschia JF, Stefansson K, Dichgans M, Markus HS Australian Stroke Genetics Collaborative, Wellcome Trust Case Control Consortium 2 (WTCCC2); International Stroke Genetics Consortium. Genetic risk factors for ischaemic stroke and its subtypes (the METASTROKE collaboration): a meta-analysis of genome-wide association studies. Lancet Neurol. 2012;11:951–962. doi: 10.1016/S1474-4422(12)70234-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
8. High Blood Cholesterol and Other Lipids
See Table 8-1 and Charts 8-1 through 8-3.
Table 8-1.
High Total and LDL Cholesterol and Low HDL Cholesterol
| Population Group | Prevalence of Total Cholesterol ≥200 mg/dL, 2010 Age ≥20 y | Prevalence of Total Cholesterol ≥240 mg/dL, 2010 Age ≥20 y | Prevalence of LDL Cholesterol ≥130 mg/dL, 2010 Age ≥20 y | Prevalence of HDL Cholesterol <40 mg/dL, 2010 Age ≥20 y |
|---|---|---|---|---|
| Both sexes, n (%)* | 98 900 000 (43.4) | 31 900 000 (13.8) | 71 000 000 (31.1) | 48 700 000 (21.8) |
| Males, n (%)* | 45 300 000 (41.3) | 14 000 000 (12.7) | 35 200 000 (31.9) | 34 600 000 (31.8) |
| Females, n (%)* | 53 600 000 (44.9) | 17 900 000 (14.7) | 35 800 000 (30.0) | 14 100 000 (12.3) |
| NH white males, % | 40.5 | 12.3 | 30.1 | 33.1 |
| NH white females, % | 45.8 | 15.6 | 29.3 | 12.4 |
| NH black males, % | 38.6 | 10.8 | 33.1 | 20.3 |
| NH black females, % | 40.7 | 11.7 | 31.2 | 10.2 |
| Mexican-American males, % | 48.1 | 15.2 | 39.9 | 34.2 |
| Mexican-American females, % | 44.7 | 13.5 | 30.4 | 15.1 |
Prevalence of total cholesterol ≥200 mg/dL includes people with total cholesterol ≥240 mg/dL. In adults, levels of 200 to 239 mg/dL are considered borderline high. Levels of ≥240 mg/dL are considered high.
HDL indicates high-density lipoprotein; LDL, low-density lipoprotein; and NH, non-Hispanic.
Total data for total cholesterol are for Americans ≥20 y of age. Data for LDL cholesterol, HDL cholesterol, and all racial/ethnic groups are age adjusted for age ≥20 y.
Source for total cholesterol ≥200 mg/dL, ≥240 mg/dL, LDL, and HDL: National Health and Nutrition Examination Survey (2007–2010), National Center for Health Statistics, and National Heart, Lung, and Blood Institute. Estimates from National Health and Nutrition Examination Survey 2007 to 2010 (National Center for Health Statistics) were applied to 2010 population estimates.
Chart 8-1.
Trends in mean serum total cholesterol among adolescents 12 to 17 years of age by race, sex, and survey year (National Health and Nutrition Examination Survey: 1976–1980,* 1988–1994,* 1999–2004, and 2005–2010). Values are in mg/dL. Mex. Am. indicates Mexican American; and NH, non-Hispanic. *Data for Mexican Americans not available. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 8-3.
Age-adjusted trends in the prevalence of serum total cholesterol ≥200 mg/dL in adults ≥20 years of age by sex, race/ethnicity, and survey year (National Health and Nutrition Examination Survey 2005–2006, 2007–2008, and 2009–2010). Mex. Am. indicates Mexican American; and NH, non-Hispanic.
High cholesterol is a major risk factor for CVD and stroke.1 The AHA has identified untreated total cholesterol <170 mg/dL (for children) and <200 mg/dL (for adults) as 1 of the 7 components of ideal cardiovascular health.2 In 2009 to 2010, 61.9% of children and 47.3% of adults met these criteria.
Prevalence
For information on dietary cholesterol, total fat, saturated fat, and other factors that affect blood cholesterol levels, see Chapter 5 (Nutrition).
Youth
(See Chart 8-1.)
-
Among children 6 to 11 years of age, the mean total cholesterol level is 161.9 mg/dL. For boys, it is 162.3 mg/dL; for girls, it is 161.5 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2007–2010, unpublished NHLBI tabulation):
For non-Hispanic whites, 160.9 mg/dL for boys and 161.6 mg/dL for girls
For non-Hispanic blacks, 165.2 mg/dL for boys and 157.9 mg/dL for girls
For Mexican Americans, 159.6 mg/dL for boys and 160.7 mg/dL for girls
-
Among adolescents 12 to 19 years of age, the mean total cholesterol level is 158.2 mg/dL. For boys, it is 156.1 mg/dL; for girls, it is 160.3 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2007–2010, unpublished NHLBI tabulation):
For non-Hispanic whites, 156.8 mg/dL for boys and 161.1 mg/dL for girls
For non-Hispanic blacks, 154.1 mg/dL for boys and 160.6 mg/dL for girls
For Mexican Americans, 157.8 mg/dL for boys and 158.0 mg/dL for girls
The prevalence of abnormal lipid levels among youths 12 to 19 years of age is 20.3%; 14.2% of normal-weight youths, 22.3% of overweight youths, and 42.9% of obese youths have ≥1 abnormal lipid level (NHANES 1999–2006, NCHS).3
Approximately 7.8% of adolescents 12 to 19 years of age have total cholesterol levels ≥200 mg/dL (NHANES 2007–2010, unpublished NHLBI tabulation).
Fewer than 1% of adolescents are potentially eligible for pharmacological treatment on the basis of guidelines from the American Academy of Pediatrics.3,4
Abbreviations Used in Chapter 7
| AHA | American Heart Association |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CDC | Centers for Disease Control and Prevention |
| CHD | coronary heart disease |
| CVD | cardiovascular diseases |
| DM | diabetes mellitus |
| HD | heart disease |
| HDL | high-density lipoprotein |
| LDL | low-density lipoprotein |
| Mex. Am. | Mexican American |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHANES | National Health and Nutrition Examination Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
Adults
(See Table 8-1 and Charts 8-2 and 8-3.)
Chart 8-2.
Trends in mean serum total cholesterol among adults aged ≥20 years by race and survey year (National Health and Nutrition Examination Survey: 1988–1994, 1999–2002, 2003–2006, and 2007–2010). Values are in mg/dL. NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
An estimated 31.9 million adults ≥20 years of age have serum total cholesterol levels ≥240 mg/dL (extrapolated to 2010 by use of NCHS/NHANES 2007–2010 data), with a prevalence of 13.8% (Table 8-1; unpublished NHLBI tabulation).
Approximately 5.6% of adults ≥20 years of age have undiagnosed hypercholesterolemia, defined as a total cholesterol level ≥240 mg/dL and the participant having responded “no” to ever having been told by a doctor or other healthcare professional that the participant’s blood cholesterol level was high (NHANES 2007–2010, unpublished NHLBI tabulation).
Between the periods 1988 to 1994 and 1999 to 2002 (NHANES/NCHS), the age-adjusted mean serum total cholesterol level of adults ≥20 years of age decreased from 206 to 203 mg/dL, and LDL cholesterol levels decreased from 129 to 123 mg/dL.5
Data from NHANES 2003 to 2008 (NCHS) showed the serum total crude mean cholesterol level in adults ≥20 years of age was 195 mg/dL for men and 201 mg/dL for women.6
Data from the Minnesota Heart Survey (1980–1982 to 2000–2002) showed a decline in age-adjusted mean total cholesterol concentrations from 5.49 and 5.38 mmol/L (98.8 and 96.8 mg/dL) for men and women, respectively, in 1980 to 1982 to 5.16 and 5.09 mmol/L (92.8 and 91.6 mg/dL), respectively, in 2000 to 2002; however, the decline was not uniform across all age groups. Middle-aged to older people have shown substantial decreases, but younger people have shown little overall change and recently had increased total cholesterol values. Lipid-lowering drug use rose significantly for both sexes among those 35 to 74 years of age. Awareness, treatment, and control of hypercholesterolemia have increased; however, more than half of those at borderline-high risk remain unaware of their condition.7
According to data from NHANES 2005 to 2006, between the periods 1999 to 2000 and 2005 to 2006, mean serum total cholesterol levels in adults ≥20 years of age declined from 204 to 199 mg/dL. This decline was observed for men ≥40 years of age and for women ≥60 years of age. There was little change over this time period for other sex/age groups. In 2005 to 2006, ≈65% of men and 70% of women had been screened for high cholesterol in the past 5 years, and 16% of adults had serum total cholesterol levels ≥240 mg/dL.8
According to data from NHANES 2007 to 2008, mean serum total cholesterol levels in adults aged 20 to 74 years declined further to 197 mg/dL. Overall, the decline in cholesterol levels in recent years appears to reflect greater uptake of cholesterol-lowering medications rather than changes in dietary patterns.9
According to data from NHANES, from 1999 to 2006, the prevalence of elevated LDL cholesterol levels (as defined by levels higher than the specified Adult Treatment Panel III risk category) in adults ≥20 years of age has decreased by ≈33%.10
During the period from 1999 to 2006, 26.0% of adults had hypercholesterolemia, 9% of adults had both hypercholesterolemia and hypertension, 1.5% of adults had DM and hypercholesterolemia, and 3% of adults had all 3 conditions.11
Screening
Data from the BRFSS study of the CDC in 2011 showed that the percentage of adults who had been screened for high cholesterol in the preceding 5 years ranged from 66.3% in Utah to 83.7% in Massachusetts. The median percentage among all 50 states was 75.5%.12
The percentage of adults who reported having had a cholesterol check increased from 68.6% during 1999 to 2000 to 74.8% during 2005 to 2006.13
Awareness
Data from the BRFSS (CDC) survey in 2011 showed that among adults screened for high cholesterol, the percentage who had been told that they had high cholesterol ranged from 33.5% in Colorado to 42.3% in Mississippi. The median percentage among states was 38.4%.12
Among adults with hypercholesterolemia, the percentage who had been told that they had high cholesterol increased from 42.0% during 1999 to 2000 to 50.4% during 2005 to 2006.13
Treatment
Adherence
Youth
The American Academy of Pediatrics recommends screening for dyslipidemia in children and adolescents who have a family history of dyslipidemia or premature CVD, those whose family history is unknown, and those youths with risk factors for CVD, such as being overweight or obese, having hypertension or DM, or being a smoker.3
Analysis of data from NHANES 1999 to 2006 showed that the overall prevalence of abnormal lipid levels among youths 12 to 19 years of age was 20.3%.3
Adults
-
On the basis of data from the Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults1:
Fewer than half of all people who qualify for any kind of lipid-modifying treatment for CHD risk reduction are receiving it.
Fewer than half of even the highest-risk people (those with symptomatic CHD) are receiving lipid-lowering treatment.
Only approximately one third of treated patients are achieving their LDL goal; <20% of patients with CHD are at their LDL goal.
Data from NHANES 2005 to 2006 indicate that among those with elevated LDL cholesterol levels, 35.5% had not been screened previously, 24.9% were screened but not told they had elevated cholesterol, and 39.6% were treated inadequately.10
There were 33.2% of adults overall during 2005 to 2008 in NHANES who achieved LDL cholesterol goals. Among adults without health insurance, only 22.6% achieved LDL cholesterol goals; however, 82.8% of those adults with uncontrolled LDL cholesterol did have some form of health insurance.14
Lipid Levels
LDL (Bad) Cholesterol
Youth
There are limited data available on LDL cholesterol for children 6 to 11 years of age.
-
Among adolescents 12 to 19 years of age, the mean LDL cholesterol level is 89.5 mg/dL. For boys, it is 88.6 mg/dL, and for girls, it is 90.5 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2007–2010, unpublished NHLBI tabulation):
Among non-Hispanic whites, 90.4 mg/dL for boys and 90.9 mg/dL for girls
Among non-Hispanic blacks, 85.8 mg/dL for boys and 91.8 mg/dL for girls
Among Mexican Americans, 90.6 mg/dL for boys and 87.1 mg/dL for girls
High levels of LDL cholesterol occurred in 7.3% of male adolescents and 7.6% of female adolescents during 2007 to 2010.3
Adults
The mean level of LDL cholesterol for American adults ≥20 years of age was 115.8 mg/dL in 2007 to 2010.8 Levels of 130 to 159 mg/dL are considered borderline high, levels of 160 to 189 mg/dL are classified as high, and levels of ≥190 mg/dL are considered very high according to Adult Treatment Panel III.
-
According to NHANES 2007 to 2010 (unpublished NHLBI tabulation):
Among non-Hispanic whites, mean LDL cholesterol levels were 115.1 mg/dL for men and 115.7 mg/dL for women.
Among non-Hispanic blacks, mean LDL cholesterol levels were 115.9 mg/dL for men and 114.2 mg/dL for women.
Among Mexican Americans, mean LDL cholesterol levels were 119.7 mg/dL for men and 115.0 mg/dL for women.
The age-adjusted prevalence of high LDL cholesterol in US adults was 26.6% in 1988 to 1994 and 25.3% in 1999 to 2004 (NHANES/NCHS). Between 1988 to 1994 and 1999 to 2004, awareness increased from 39.2% to 63.0%, and use of pharmacological lipid-lowering treatment increased from 11.7% to 40.8%. LDL cholesterol control increased from 4.0% to 25.1% among those with high LDL cholesterol. In 1999 to 2004, rates of LDL cholesterol control were lower among adults 20 to 49 years of age than among those ≥65 years of age (13.9% versus 30.3%, respectively), among non-Hispanic blacks and Mexican Americans than among non-Hispanic whites (17.2% and 16.5% versus 26.9%, respectively), and among men than among women (22.6% versus 26.9%, respectively).15
Mean levels of LDL cholesterol decreased from 126.1 mg/dL during 1999 to 2000 to 116.1 mg/dL during 2009 to 2010. The prevalence of high LDL cholesterol decreased from 31.5% during 1999 to 2000 to 28.2% during 2009 to 2010 (unpublished NHLBI tabulation).
HDL (Good) Cholesterol
Youth
-
Among children 6 to 11 years of age, the mean HDL cholesterol level is 53.6 mg/dL. For boys, it is 55.1 mg/dL, and for girls, it is 51.9 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2007–2010, unpublished NHLBI tabulation):
Among non-Hispanic whites, 53.9 mg/dL for boys and 51.4 mg/dL for girls
Among non-Hispanic blacks, 59.9 mg/dL for boys and 55.3 mg/dL for girls
Among Mexican Americans, 53.5 mg/dL for boys and 50.5 mg/dL for girls
-
Among adolescents 12 to 19 years of age, the mean HDL cholesterol level is 51.4 mg/dL. For boys, it is 49.2 mg/dL, and for girls, it is 53.6 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2007–2010, unpublished NHLBI tabulation):
Among non-Hispanic whites, 48.4 mg/dL for boys and 53.0 mg/dL for girls
Among non-Hispanic blacks, 53.9 mg/dL for boys and 55.4 mg/dL for girls
Among Mexican Americans, 47.5 mg/dL for boys and 53.3 mg/dL for girls
Low levels of HDL cholesterol occurred in 21.7% of male adolescents and 10.7% of female adolescents during 2007 to 2010 (NHANES 2007–2010, unpublished NHLBI tabulation).
Adults
An HDL cholesterol level <40 mg/dL in adult males and <50 mg/dL in adult females is considered low and is a risk factor for HD and stroke.1 The mean level of HDL cholesterol for American adults ≥20 years of age is 52.5 mg/dL (NHANES 2007–2010, unpublished NHLBI tabulation).
-
According to NHANES 2007 to 2010 (unpublished NHLBI tabulation):
Among non-Hispanic whites, mean HDL cholesterol levels were 46.7 mg/dL for men and 58.1 mg/dL for women
Among non-Hispanic blacks, mean HDL cholesterol levels were 52.6 mg/dL for men and 58.7 mg/dL for women
Among Mexican Americans, mean HDL cholesterol levels were 45.4 mg/dL for men and 53.7 mg/dL for women
Triglycerides
Youth
There are limited data available on triglycerides for children 6 to 11 years of age.
-
Among adolescents 12 to 19 years of age, the geometric mean triglyceride level is 82.9 mg/dL. For boys, it is 85.6 mg/dL, and for girls, it is 80.1 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2007–2010, unpublished NHLBI tabulation):
Among non-Hispanic whites, 89.6 mg/dL for boys and 83.5 mg/dL for girls
Among non-Hispanic blacks, 66.7 mg/dL for boys and 58.6 mg/dL for girls
Among Mexican Americans, 97.1 mg/dL for boys and 83.5 mg/dL for girls
High levels of triglycerides occurred in 9.4% of male adolescents and 6.7% of female adolescents during 2007 to 2010.3
Adults
-
A fasting triglyceride level ≥150 mg/dL in adults is considered elevated and is a risk factor for HD and stroke. The geometric mean level of triglycerides for American adults ≥20 years of age is 130.3 mg/dL (NHANES 2007–2010, unpublished NHLBI tabulation).
-
Among men, the geometric mean triglyceride level is 141.7 mg/dL (NHANES 2007–2010, unpublished NHLBI tabulation). The racial/ethnic breakdown is as follows:
140.0 mg/dL for non-Hispanic white men
111.3 mg/dL for non-Hispanic black men
161.4 mg/dL for Mexican American men
-
Among women, the geometric mean triglyceride level is 119.1 mg/dL, with the following racial/ethnic breakdown:
121.5 mg/dL for non-Hispanic white women
94.4 mg/dL for non-Hispanic black women
134.1 mg/dL for Mexican American women
-
Approximately 27% of adults ≥20 years of age had a triglyceride level ≥150 mg/dL during 2007 to 2010 (NHANES 2007–2010, unpublished NHLBI tabulation).
Fewer than 3% of adults with a triglyceride level ≥150 mg/dL received pharmacological treatment during 1999 to 2004.16
- 1.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Prevalence of abnormal lipid levels among youths: United States, 1999–2006 [published correction appears in MMWR Morb Mortal Wkly Rep. 2010;59:78] MMWR Morb Mortal Wkly Rep. 2010;59:29–33. [PubMed] [Google Scholar]
- 4.Ford ES, Li C, Zhao G, Mokdad AH. Concentrations of low-density lipoprotein cholesterol and total cholesterol among children and adolescents in the United States. Circulation. 2009;119:1108–1115. doi: 10.1161/CIRCULATIONAHA.108.816769. [DOI] [PubMed] [Google Scholar]
- 5.Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, Wolz M, Grundy SM, Johnson CL. Trends in serum lipids and lipoproteins of adults, 1960–2002. JAMA. 2005;294:1773–1781. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 6.National Center for Health Statistics. Health, United States, 2010: With Special Feature on Death and Dying. Hyattsville, MD: National Center for Health Statistics; 2011. [Accessed July 5, 2011]. http://www.cdc.gov/nchs/data/hus/hus10.pdf. [PubMed] [Google Scholar]
- 7.Arnett DK, Jacobs DR, Jr, Luepker RV, Blackburn H, Armstrong C, Claas SA. Twenty-year trends in serum cholesterol, hypercholesterolemia, and cholesterol medication use: the Minnesota Heart Survey, 1980–1982 to 2000–2002. Circulation. 2005;112:3884–3891. doi: 10.1161/CIRCULATIONAHA.105.549857. [DOI] [PubMed] [Google Scholar]
- 8.Schober S, Carroll M, Lacher D, Hirsch R Division of Health and Nutrition Examination Surveys. High serum total cholesterol: an indicator for monitoring cholesterol lowering efforts: US adults, 2005–2006. NCHS Data Brief. 2007;(2):1–8. [PubMed] [Google Scholar]
- 9.Ford ES, Capewell S. Trends in total and low-density lipoprotein cholesterol among U.S. adults: contributions of changes in dietary fat intake and use of cholesterol-lowering medications. PLoS ONE. 2013;8:e65228. doi: 10.1371/journal.pone.0065228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuklina EV, Yoon PW, Keenan NL. Trends in high levels of low-density lipoprotein cholesterol in the United States, 1999–2006. JAMA. 2009;302:2104–2110. doi: 10.1001/jama.2009.1672. [DOI] [PubMed] [Google Scholar]
- 11.Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. Hypertension, high serum total cholesterol, and diabetes: racial and ethnic prevalence differences in U.S. adults, 1999–2006. NCHS Data Brief. 2010;(36):1–8. [PubMed] [Google Scholar]
- 12.Behavioral Risk Factor Surveillance System: prevalence and trends data. [Accessed July 5, 2011];Centers for Disease Control and Prevention Web site. http://apps.nccd.cdc.gov/brfss/index.asp.
- 13.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010;140:226–235. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC) Vital signs: prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol: United States, 1999–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep. 2011;60:109–114. [PubMed] [Google Scholar]
- 15.Hyre AD, Muntner P, Menke A, Raggi P, He J. Trends in ATP-III-defined high blood cholesterol prevalence, awareness, treatment and control among U.S. adults. Ann Epidemiol. 2007;17:548–555. doi: 10.1016/j.annepidem.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 16.Ford ES, Li C, Zhao G, Pearson WS, Mokdad AH. Hypertriglyceridemia and its pharmacologic treatment among US adults. Arch Intern Med. 2009;169:572–578. doi: 10.1001/archinternmed.2008.599. [DOI] [PubMed] [Google Scholar]
9. High Blood Pressure
ICD-9 401 to 404, ICD-10 I10 to I15. See Tables 9-1 and 9-2 and Charts 9-1 through 9-5.
Table 9-1.
High Blood Pressure
| Population Group | Prevalence, 2010, Age ≥20 y | Mortality,* 2010, All Ages | Hospital Discharges, 2010, All Ages | Estimated Cost, 2010 |
|---|---|---|---|---|
| Both sexes | 77 895 000 (33.0%) | 63 119 | 488 000 | $46.4 Billion |
| Males | 37 195 000 (33.6%) | 28 373 (45.0%)† | 216 000 | … |
| Females | 40 700 000 (32.2%) | 34 746 (55.0%)† | 272 000 | … |
| NH white males | 33.4% | 20 819 | … | … |
| NH white females | 30.7% | 26 798 | … | … |
| NH black males | 42.6% | 6670 | … | … |
| NH black females | 47.0% | 6923 | … | … |
| Mexican American males | 30.1% | … | … | … |
| Mexican American females | 28.8% | … | … | … |
| Asian | 21.2%‡ | 1578§ | … | … |
| American Indian or Alaska Native | 24.8%‡ | 331 | … | … |
Hypertension is defined in terms of National Health and Nutrition Examination Survey blood pressure measurements and health interviews. A subject was considered hypertensive if systolic blood pressure was ≥140 mm Hg or diastolic blood pressure was ≥90 mm Hg, if the subject said “yes” to taking antihypertensive medication, or if the subject was told on 2 occasions that he or she had hypertension.
Ellipses (…) indicate data not available; NH, non-Hispanic.
Mortality data for the white, black, Asian or Pacific Islander, and American Indian or Alaska Native populations include deaths among people of Hispanic and non-Hispanic origin. Numbers of deaths for the American Indian or Alaska Native and Asian or Pacific Islander populations are known to be underestimated.
These percentages represent the portion of total high blood pressure mortality that is for males vs females.
National Health Interview Survey (2010), National Center for Health Statistics; data are weighted percentages for Americans ≥18 y of age. Source: Blackwell et al.22
Includes Chinese, Filipino, Hawaiian, Japanese, and other Asian or Pacific Islander.
Sources: Prevalence: National Health and Nutrition Examination Survey (2007–2010), National Center for Health Statistics, and National Heart, Lung, and Blood Institute. Percentages for racial/ethnic groups are age adjusted for Americans ≥20 y of age. Age-specific percentages are extrapolated to the 2010 US population estimates. Mortality: Centers for Disease Control and Prevention/National Center for Health Statistics, 2010 Mortality Multiple Cause-of-Death–United States, version dated May 28, 2013. These data represent underlying cause of death only. Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics; data include those discharged alive, dead, or status unknown. Cost: Medical Expenditure Panel Survey data include estimated direct costs for 2010; indirect costs calculated by National Heart, Lung, and Blood Institute for 2010.
Table 9-2.
Hypertension Awareness, Treatment, and Control: NHANES 1999 to 2004 and 2005 to 2010, by Race/Ethnicity and Sex
| Awareness, %
|
Treatment, %
|
Control, %
|
||||
|---|---|---|---|---|---|---|
| 1999–2004 | 2005–2010 | 1999–2004 | 2005–2010 | 1999–2004 | 2005–2010 | |
| NH white males | 71.2 | 77.5 | 61.2 | 69.4 | 41.0 | 50.1 |
| NH white females | 74.4 | 84.0 | 65.3 | 78.2 | 37.2 | 53.9 |
| NH black male | 69.1 | 77.5 | 58.1 | 66.9 | 32.3 | 39.7 |
| NH black females | 83.5 | 88.5 | 73.9 | 81.5 | 40.4 | 52.8 |
| Mexican American males | 57.0 | 64.8 | 41.8 | 54.0 | 23.3 | 35.1 |
| Mexican American females | 67.9 | 75.5 | 56.3 | 68.1 | 29.6 | 41.6 |
NH indicates non-Hispanic; NHANES, National Health and Nutrition Examination Survey.
Sources: NHANES (1999–2004, 2005–2010) and National Heart, Lung, and Blood Institute.
Chart 9-1.
Prevalence of high blood pressure in adults ≥20 years of age by age and sex (National Health and Nutrition Examination Survey: 2007–2010). Hypertension is defined as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg, if the subject said “yes” to taking antihypertensive medication, or if the subject was told on 2 occasions that he or she had hypertension. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 9-5.
Extent of awareness, treatment, and control of high blood pressure by race/ethnicity and sex (National Health and Nutrition Examination Survey: 2007–2010). NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
High blood pressure is a major risk factor for CVD and stroke.1 The AHA has identified untreated BP <90th percentile (for children) and <120/<80 mm Hg (for adults aged ≥20 years) as 1 of the 7 components of ideal cardiovascular health.2 In 2009 to 2010, 85.8% of children and 44.3% of adults met these criteria (Chapter 2, Cardiovascular Health).
Abbreviations Used in Chapter 9
| AHA | American Heart Association |
| ARIC | Atherosclerosis Risk in Communities Study |
| BP | blood pressure |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CDC | Centers for Disease Control and Prevention |
| CHD | coronary heart disease |
| CHF | congestive heart failure |
| CHS | Cardiovascular Health Study |
| CRP | C-reactive protein |
| CVD | cardiovascular disease |
| DBP | diastolic blood pressure |
| DM | diabetes mellitus |
| ED | emergency department |
| FHS | Framingham Heart Study |
| HBP | high blood pressure |
| HD | heart disease |
| ICD-9 | International Classification of Diseases, 9th Revision |
| ICD-9-CM | International Classification of Diseases, Clinical Modification, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| LDL | low-density lipoprotein |
| MEPS | Medical Expenditure Panel Survey |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| NAMCS | National Ambulatory Medical Care Survey |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHAMCS | National Hospital Ambulatory Medical Care Survey |
| NHANES | National Health and Nutrition Examination Survey |
| NHDS | National Hospital Discharge Survey |
| NHES | National Health Examination Survey |
| NHIS | National Health Interview Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| NINDS | National Institute of Neurological Disorders and Stroke |
| NNHS | National Nursing Home Survey |
| PA | physical activity |
| REGARDS | Reasons for Geographic and Racial Differences in Stroke |
| SBP | systolic blood pressure |
| SEARCH | Search for Diabetes in Youth Study |
| WHI | Women’s Health Initiative |
Prevalence
(See Table 9-1 and Chart 9-1.)
-
HBP is defined as:
SBP ≥140 mm Hg or DBP ≥90 mm Hg or taking antihypertensive medicine, or
Having been told at least twice by a physician or other health professional that one has HBP.
One in 3 US adults has HBP (unpublished NHLBI tabulation).
Data from NHANES 2007 to 2010 found that ≈6% of US adults have undiagnosed hypertension. Data from the 2007 to 2008 BRFSS, NHIS, and NHANES surveys found 27.8%, 28.5%, and 30.7% US adults were told they had hypertension, respectively.3
-
Prevalence of hypertension (age adjusted) among US adults ≥18 years of age was estimated to be 28.6% in NHANES 2009 to 2010.
Among those 18 to 39 years of age, prevalence was 6.8%; among those 40 to 59 years of age, prevalence was 30.4%; and among those ≥60 years of age, prevalence was 66.7%. Furthermore, prevalence of hypertension among non-Hispanic blacks, non-Hispanic whites, and Hispanics was 40.4%, 27.4%, and 26.1%, respectively.4
An estimated 77.9 million adults ≥20 years of age have HBP, extrapolated to 2010 with NHANES 2007 to 2010 data (Table 9-1).
NHANES data show that a higher percentage of men than women have hypertension until 45 years of age. From 45 to 54 and from 55 to 64 years of age, the percentages of men and women with hypertension are similar. After that, a higher percentage of women have hypertension than men (Chart 9-1).
HBP is 2 to 3 times more common in women taking oral contraceptives than in women not taking them.1
Data from NHANES 1999 to 2008 and BRFSS 1997 to 2009 estimated the prevalence of hypertension in men and women ≥30 years of age to be 37.6% and 40.1%, respectively. Awareness, treatment, and control of hypertension varied across the country and were highest in the southeastern United States. Between 2001 and 2009, control of hypertension increased, as did prevalence of hypertension.5
Data from the 2011 BRFSS/CDC indicate that the percentage of adults ≥18 years of age who had been told that they had HBP ranged from 22.9% in Utah to 40.1% in Alabama. The median percentage was 30.8%.6
According to 2003 to 2008 NHANES data, among US adults with hypertension, 8.9% met the criteria for resistant hypertension (BP was ≥140/90 mm Hg, and they reported using antihypertensive medications from 3 different drug classes or drugs from ≥4 antihypertensive drug classes regardless of BP). This represents 12.8% of the population taking antihypertensive medication.7
According to data from NHANES 1988 to 1994 and 2007 to 2008, HBP control rates improved from 27.3% to 50.1%, treatment improved from 54.0% to 73.5%, and the control/treated rates improved from 50.6% to 72.3%.8
Projections show that by 2030, ≈41.4% of US adults will have hypertension, an increase of 8.4% from 2012 estimates (unpublished AHA computation, based on methodology described by Heidenreich et al9).
Older Adults
In 2009 to 2010, hypertension was among the diagnosed chronic conditions that were more prevalent among older (≥65 years of age) women than older men (57% for women, 54% for men). Ever-diagnosed conditions that were more prevalent among older men than older women included HD (37% for men, 26% for women) and DM (24% for men, 18% for women), on the basis of data from NHIS/NCHS.10
The age-adjusted prevalence of hypertension (both diagnosed and undiagnosed) in 2003 to 2006 was 75% for older women and 65% for older men on the basis of data from NHANES/NCHS.11
Data from the 2004 NNHS revealed the most frequent chronic medical condition among this nationally representative sample of long-term stay residents aged ≥65 years was hypertension (53% of men and 56% of women). In men, prevalence of hypertension decreased with increasing age.12
Among US adults ≥65 years of age (NHANES 1999–2004), prevalence of hypertension was 70.8%, awareness of hypertension was 75.9%, treatment for hypertension was 69.3%, and control of hypertension was 48.8%. Women had a slightly higher prevalence than men and a significantly lower rate of hypertension control.13
Children and Adolescents
Data from participants aged 12 to 19 years in the 2005 to 2010 NHANES found ideal blood pressure (<95th percentile) to be present in 78% of males and 90% of females; poor blood pressure (>95th percentile) was found in 2.9% of male and 3.7% of female participants.14
Analysis of data from participants aged 12 to 19 years in NHANES 1999 to 2008 found the prevalence of prehypertension/hypertension was 14%. Furthermore, there was no significant change in the prevalence of prehypertension/hypertension between 1999 to 2000 and 2007 to 2008 among this age group.15
Analysis of the NHES, the Hispanic Health and Nutrition Examination Survey, and the NHANES/NCHS surveys of the NCHS (1963–2002) found that the BP, pre-HBP, and HBP trends in children and adolescents 8 to 17 years of age moved downward from 1963 to 1988 and upward thereafter. Pre-HBP and HBP increased 2.3% and 1%, respectively, between 1988 and 1999. Increased obesity (abdominal obesity more so than general obesity) partially explained the HBP and pre-HBP rise from 1988 to 1999. BP and HBP reversed their downward trends 10 years after the increase in the prevalence of obesity. In addition, an ethnic and sex gap appeared in 1988 for pre-HBP and in 1999 for HBP: Non-Hispanic blacks and Mexican Americans had a greater prevalence of HBP and pre-HBP than non-Hispanic whites, and the prevalence was greater in boys than in girls. In that study, HBP in children and adolescents was defined as SBP or DBP that was, on repeated measurement, ≥95th percentile.16
A study in Ohio of >14 000 children and adolescents 3 to 18 years of age who were observed at least 3 times between 1999 and 2006 found that 507 children (3.6%) had hypertension. Of these, 131 (26%) had been diagnosed and 376 (74%) were undiagnosed. In addition, 3% of those with hypertension had stage 2 hypertension, and 41% of those with stage 2 hypertension were undiagnosed. Criteria for prehypertension were met by 485 children. Of these, 11% were diagnosed. In this study, HBP in children and adolescents was defined as SBP or DBP that was, on repeated measurement, ≥95th percentile.17
Analysis of data from the SEARCH study, which included children 3 to 17 years of age with type 1 and type 2 DM, found the prevalence of elevated BP to be 5.9% among those with type 1 DM and 23.7% among those with type 2 DM.18
A study of high school students in Houston, TX (mean age 15.4 years; 45.2% male, 49.3% Hispanic, 25.2% Caucasian, and 16.1% African American) found ≈30% of the students had ≥1 elevated BP measurement; elevated BP was significantly influenced by obesity.19
Longitudinal BP outcomes from the National Childhood Blood Pressure database (ages 13–15 years) were examined after a single BP measurement. Among those determined to have prehypertension, 14% of boys and 12% of girls had hypertension 2 years later; the overall rate of progression from prehypertension to hypertension was ≈7%.20
Race/Ethnicity and HBP
(See Table 9-1 and Chart 9-2.)
Chart 9-2.
Age-adjusted prevalence trends for high blood pressure in adults ≥20 years of age by race/ethnicity, sex, and survey (National Health and Nutrition Examination Survey: 1988–1994, 1999–2004, and 2005–2010). NH indicates non-Hispanic. Source: National Center for Health Statics and National Heart, Lung and Blood Institute.
The prevalence of hypertension in blacks in the United States is among the highest in the world, and it is increasing. From 1988 to 1994 through 1999 to 2002, the prevalence of HBP in adults increased from 35.8% to 41.4% among blacks, and it was particularly high among black women at 44.0%. Prevalence among whites also increased, from 24.3% to 28.1%.21
Compared with whites, blacks develop HBP earlier in life, and their average BPs are much higher. As a result, compared with whites, blacks have a 1.3-times greater rate of nonfatal stroke, a 1.8-times greater rate of fatal stroke, a 1.5-times greater rate of death attributable to HD, and a 4.2-times greater rate of end-stage kidney disease (fifth and sixth reports of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure).
Data from the 2012 NHIS showed that black adults 18 years of age were more likely (32.9%) to have been told on ≥2 occasions that they had hypertension than white adults (22.9%), American Indian/Alaska Native adults (24.8%), or Asian adults (21.2%).22
Trend analyses that used NHANES 1988 to 1994 and 1999 to 2004 data among non-Hispanic black and non-Hispanic white men and women found that non-Hispanic blacks had the highest prevalence of hypertension among both men and women during both time periods. The largest increase in prevalence of hypertension occurred among women (both non-Hispanic black and non-Hispanic white) compared with men. Racial/ethnic disparities did not change over time periods.23
Analysis from the REGARDS study of the NINDS suggests that efforts to raise awareness of prevalent hypertension among blacks apparently have been successful (31% greater odds in blacks relative to whites), and efforts to communicate the importance of receiving treatment for hypertension have been successful (69% greater odds among blacks relative to whites); however, substantial racial disparities remain with regard to the control of BP (SBP <140 mm Hg, DBP <90 mm Hg), with the odds of control being 27% lower in blacks than in whites. In contrast, geographic disparities in hypertension awareness, treatment, and control were minimal.24
The CDC analyzed death certificate data from 1995 to 2002 (any-mention mortality; ICD-9 codes 401–404 and ICD-10 codes I10–I13). The results indicated that Puerto Rican Americans had a consistently higher hypertension-related death rate than all other Hispanic subpopulations and non-Hispanic whites. The age-standardized hypertension-related mortality rate was 127.2 per 100 000 population for all Hispanics, similar to that of non-Hispanic whites (135.9). The age-standardized rate for Hispanic females (118.3) was substantially lower than that observed for Hispanic males (135.9). Hypertension-related mortality rates for males were higher than rates for females for all Hispanic subpopulations. Puerto Rican Americans had the highest hypertension-related death rate among all Hispanic subpopulations (154.0); Cuban Americans had the lowest (82.5).25
Some studies suggest that Hispanic Americans have rates of HBP similar to or lower than those of non-Hispanic white Americans. Findings from a new analysis of combined data from the NHIS of 2000 to 2002 point to a health disparity between black and white adults of Hispanic descent. Black Hispanics were at slightly greater risk than white Hispanics, although non-Hispanic black adults had by far the highest rate of HBP. The racial disparity among Hispanics also was evident in the fact that higher-income, better-educated black Hispanics still had a higher rate of HBP than lower-income, less-educated white Hispanics.26 Data from the NHLBI’s ARIC study found that hypertension was a particularly powerful risk factor for CHD in black people, especially black women.27
Data from MESA found that being born outside the United States, speaking a language other than English at home, and living fewer years in the United States were each associated with a decreased prevalence of hypertension.28
Filipino (27%) and Japanese (25%) adults were more likely than Chinese (17%) or Korean (17%) adults to have ever been told that they had hypertension.29
Mortality
(See Table 9-1.)
HBP mortality in 2010 was 63 119. Any-mention mortality in 2010 was 362 895. The 2010 death rate was 18.8.30
The 2010 overall death rate resulting from HBP was 18.8. Death rates were 17.2 for white males, 50.2 for black males, 15.0 for white females, and 37.1 for black females. When any-mention mortality for 2010 was used, the overall death rate was 108.9. Death rates were 112.5 for white males, 216.8 for black males, 90.6 for white females, and 161.9 for black females.30
From 2000 to 2010, the death rate attributable to HBP increased 16.0%, and the actual number of deaths rose 41.5% (AHA tabulation).31
A mathematical model was developed to estimate the number of deaths that potentially could be prevented annually by increasing the use of 9 clinical preventive services. The model predicted that a 10% increase in hypertension treatment would result in ≈14 000 deaths prevented.32
Analysis of NHANES I and II comparing hypertensive and nonhypertensive individuals found a reduction in age-adjusted mortality rate of 4.6 per 1000 person-years among people with hypertension compared with a reduction of 4.2 per 1000 person-years among those without hypertension.33
Assessment of 30-year follow-up of the Hypertension Detection and Follow-up Program identified the long-term benefit of stepped care, as well as the increased survival for hypertensive African Americans.34
Assessment of the Charleston Heart Study and Evans County Heart Study identified the excess burden of elevated BP for African Americans and its effect on long-term health outcomes.35
Data from the Harvard Alumni Health Study found that higher BP in early adulthood was associated several decades later with higher risk for all-cause mortality, CVD mortality, and CHD mortality but not stroke mortality.36
Risk Factors
Numerous risk factors and markers for development of hypertension have been identified, including age, ethnicity, family history of hypertension and genetic factors, lower education and socioeconomic status, greater weight, lower PA, tobacco use, psychosocial stressors, sleep apnea, and dietary factors (including dietary fats, higher sodium intake, lower potassium intake, and excessive alcohol intake).
A study of related individuals in the NHLBI’s FHS suggested that different sets of genes regulate BP at different ages.37
Recent data from the Nurses’ Health Study suggest that a large proportion of incident hypertension in women can be prevented by controlling dietary and lifestyle risk factors.38
A meta-analysis identified the benefit of a goal BP of 130/80 mm Hg for individuals with hypertension and type 2 DM but less evidence for treatment below this value.39
Aftermath
Approximately 69% of people who have a first heart attack, 77% of those who have a first stroke, and 74% of those who have CHF have BP >140/90 mm Hg (NHLBI unpublished estimates from ARIC, CHS, and FHS Cohort and Offspring studies).
Data from FHS/NHLBI indicate that recent (within the past 10 years) and remote antecedent BP levels may be an important determinant of risk over and above the current BP level.40
-
Data from the FHS/NHLBI indicate that hypertension is associated with shorter overall life expectancy, shorter life expectancy free of CVD, and more years lived with CVD.41
Total life expectancy was 5.1 years longer for normotensive men and 4.9 years longer for normotensive women than for hypertensive people of the same sex at 50 years of age.
Compared with hypertensive men at 50 years of age, men with untreated BP <140/90 mm Hg survived on average 7.2 years longer without CVD and spent 2.1 fewer years of life with CVD. Similar results were observed for women.
Hospital Discharges/Ambulatory Care Visits
(See Table 9-1.)
From 2000 to 2010, the number of inpatient discharges from short-stay hospitals with HBP as the first-listed diagnosis increased from 457 000 to 488 000 (no significant difference; NCHS, NHDS). The number of all-listed discharges increased from 8 034 000 to 11 282 000 (NHLBI, unpublished data from the NHDS, 2010; diagnoses in 2010 were truncated at 7 diagnoses for comparability with earlier year).
Data from the Nationwide Inpatient Sample from the years 2000 to 2007 found the frequency of hospitalizations for adults aged ≥18 years of age with a hypertensive emergency increased from 101 to 111 per 100 000 in 2007 (average increase of 1.11%). In contrast to the increased number of hospitalizations, the all-cause in-hospital mortality rate decreased during the same period from 2.8% to 2.6%.42
Data from ambulatory medical care use estimates for 2010 showed that the number of visits for essential hypertension was 43 436 000. Of these, 38 916 000 were physician office visits, 940 000 were ED visits, and 3 580 000 were outpatient department visits (NAMCS and NHAMCS, NHLBI tabulation).
In 2010, there were 280 000 hospitalizations with a first-listed diagnosis of essential hypertension (ICD-9-CM code 401), but essential hypertension was listed as either a primary or a secondary diagnosis on 11 048 000 hospitalized inpatient visits (unpublished data from the NHDS, NHLBI tabulation).
Awareness, Treatment, and Control
(See Table 9-2 and Charts 9-3 through 9-5.)
Chart 9-3.
Extent of awareness, treatment, and control of high blood pressure by race/ethnicity (National Health and Nutrition Examination Survey: 2007–2010). NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Data from NHANES 2007 to 2010 showed that of those with hypertension who were ≥20 years of age, 81.5% were aware of their condition, 74.9% were under current treatment, 52.5% had their hypertension under control, and 47.5% did not have it controlled (NHLBI tabulation).
Data from NHANES 2009 to 2010 showed that 81.9% of adults were aware of their hypertension. Furthermore, 76.4% self-reported that they were currently taking prescribed medication to control hypertension. Awareness of hypertension was lower among those aged 18 to 39 years than among aged 40 to 59 years and those aged ≥60 years of age. Non-Hispanic black adults were more aware of their hypertension than Hispanics (87.0% and 77.7%, respectively).4
Analysis of NHANES 2007 to 2008 and 2009 to 2010 found the proportion of adults with controlled hypertension increased from 48.4% to 53.3%, respectively. Medication use to lower hypertension was lowest for those aged 18 to 39 years (46.0%) compared with those aged 40 to 59 years (77.1%) and those aged ≥60 years (80.7%). Non-Hispanic black adults were more likely to take antihypertensive medication than non-Hispanic whites or Hispanic adults (79.7%, 76.6%, and 69.6%, respectively).4
Data from the FHS of the NHLBI show that among those ≥80 years of age, only 38% of men and 23% of women had BPs that met targets set forth in the National High Blood Pressure Education Program’s clinical guidelines. Control rates in men <60, 60 to 79, and ≥80 years of age were 38%, 36%, and 38%, respectively; for women in the same age groups, they were 38%, 28%, and 23%, respectively.43
Data from the WHI observational study of nearly 100 000 postmenopausal women across the country enrolled between 1994 and 1998 indicate that although prevalence rates ranged from 27% of women 50 to 59 years of age to 41% of women 60 to 69 years of age to 53% of women 70 to 79 years of age, treatment rates were similar across age groups: 64%, 65%, and 63%, respectively. Despite similar treatment rates, hypertension control is especially poor in older women, with only 29% of hypertensive women 70 to 79 years of age having clinic BPs <140/90 mm Hg compared with 41% and 37% of those 50 to 59 and 60 to 69 years of age, respectively.44
Among a cohort of postmenopausal women taking hormone replacement, hypertension was the most common comorbidity, with a prevalence of 34%.45
A study of >300 women in Wisconsin showed a need for significant improvement in BP and LDL levels. Of the screened participants, 35% were not at BP goal, 32.4% were not at LDL goal, and 53.5% were not at both goals.46
In 2005, a survey of people in 20 states conducted by the BRFSS of the CDC found that 19.4% of respondents had been told on ≥2 visits to a health professional that they had HBP. Of these, 70.9% reported changing their eating habits; 79.5% reduced the use of or were not using salt; 79.2% reduced the use of or eliminated alcohol; 68.8% were exercising; and 73.4% were taking antihypertensive medication.47
Among 1509 NHANES 2005 to 2006 participants aged ≥30 years with hypertension, 24% were categorized as low risk, 21% as intermediate risk, and 23% as high risk according to Framingham global risk. Furthermore, an additional 32% had CVD. Treatment for hypertension varied by risk category and ranged from 58% to 75%; hypertension control was 80% for those in the low-risk category and <50% for those in the high-risk category.48
According to data from NHANES 2001 to 2006, non-Hispanic blacks had 90% higher odds of poorly controlled BP than non-Hispanic whites. Among those who were hypertensive, non-Hispanic blacks and Mexican Americans had 40% higher odds of uncontrolled BP than non-Hispanic whites.49
According to data from NHANES 1998 to 2008 for adults with DM, prevalence of hypertension increased, whereas awareness, treatment, and control improved during these time periods; however, for adults 20 to 44 years of age, there was no evidence of improvement.50
“Resistant hypertension” is a treatment and control issue for nearly 1 in 10 hypertensive adults. This category of HBP represents individuals with uncontrolled HBP despite the use of ≥3 antihypertensive medications or with BP controlled with the use of ≥4 medications.51,52
Cost
(See Table 9-1.)
The estimated direct and indirect cost of HBP for 2010 is $46.4 billion (MEPS, NHLBI tabulation).
Projections show that by 2030, the total cost of HBP could increase to an estimated $274 billion (unpublished AHA computation, based on methodology described in Heidenreich et al9).
Prehypertension
Prehypertension is untreated SBP of 120 to 139 mm Hg or untreated DBP of 80 to 89 mm Hg and not having been told on 2 occasions by a physician or other health professional that one has hypertension.
Among disease-free participants in NHANES 1999 to 2006, the prevalence of prehypertension was 36.3%. Prevalence was higher in men than in women. Furthermore, prehypertension was correlated with an adverse cardiometabolic risk profile.53
Follow-up of 9845 men and women in the FHS/NHLBI who attended examinations from 1978 to 1994 revealed that at 35 to 64 years of age, the 4-year incidence of hypertension was 5.3% for those with baseline BP <120/80 mm Hg, 17.6% for those with SBP of 120 to 129 mm Hg or DBP of 80 to 84 mm Hg, and 37.3% for those with SBP of 130 to 139 mm Hg or DBP of 85 to 89 mm Hg. At 65 to 94 years of age, the 4-year incidences of hypertension were 16.0%, 25.5%, and 49.5% for these BP categories, respectively.54
Data from FHS/NHLBI also reveal that prehypertension is associated with elevated relative and absolute risks for CVD outcomes across the age spectrum. Compared with normal BP (<120/80 mm Hg), prehypertension was associated with a 1.5- to 2-fold increased risk for major CVD events in those <60, 60 to 79, and ≥80 years of age. Absolute risks for major CVD associated with prehypertension increased markedly with age: 6-year event rates for major CVD were 1.5% in prehypertensive people <60 years of age, 4.9% in those 60 to 79 years of age, and 19.8% in those ≥80 years of age.43
In a study of NHANES 1999 to 2000 (NCHS), people with prehypertension were more likely than those with normal BP levels to have above-normal cholesterol levels (≥200 mg/dL) and to be overweight or obese, whereas the probability of current smoking was lower. People with prehypertension were 1.65 times more likely to have ≥1 of these adverse risk factors than were those with normal BP.55
Assessment of the REGARDS data identified high risk of prehypertension to be associated with increased age and black race.56
A meta-analysis of 12 prospective cohort studies (including 518 520 participants) found prehypertension was associated with incident stroke. The risk was particularly noted in nonelderly people and for those with BP values in the higher prehypertension range.57
Prehypertension was found to be significantly associated with stroke.57
Prehypertension was highest in blacks with other risk factors, including DM and elevated CRP.56
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 3.Li C, Balluz LS, Ford ES, Okoro CA, Zhao G, Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the National Health and Nutrition Examination Survey, 2007–2008. Prev Med. 2012;54:381–387. doi: 10.1016/j.ypmed.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 4.Yoon SS, Burt V, Louis T, Carroll MD. Hypertension among adults in the United States, 2009–2010. NCHS Data Brief. 2012;(107):1–8. [PubMed] [Google Scholar]
- 5.Olives C, Myerson R, Mokdad AH, Murray CJ, Lim SS. Prevalence, awareness, treatment, and control of hypertension in United States counties, 2001–2009. PLoS ONE. 2013;8:e60308. doi: 10.1371/journal.pone.0060308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Behavioral Risk Factor Surveillance System: prevalence and trends data. [Accessed July 5, 2011];Centers for Disease Control and Prevention Web site. http://apps.nccd.cdc.gov/brfss/index.asp.
- 7.Persell SD. Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension. 2011;57:1076–1080. doi: 10.1161/HYPERTENSIONAHA.111.170308. [DOI] [PubMed] [Google Scholar]
- 8.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 9.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ on behalf of the American Heart Association Advocacy Coordinating Committee, Stroke Council, Council on Cardiovascular Radiology and Intervention, Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular Nursing, Council on the Kidney in Cardiovascular Disease, Council on Cardiovascular Surgery and Anesthesia, and Interdisciplinary Council on Quality of Care and Outcomes Research. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 10.Federal Interagency Forum on Aging-Related Statistics. Older Americans 2010 Key Indicators of Well-Being. Washington, DC: US Government Printing Office; 2010. [Accessed July 25, 2011]. http://www.agingstats.gov. [Google Scholar]
- 11.Crescioni M, Gorina Y, Bilheimer L, Gillum RF. Trends in health status and health care use among older men. Hyattsville, MD: National Center for Health Statistics; 2010. [Accessed July 20, 2011]. National Health Statistics Report No. 24. http://www.cdc.gov/nchs/data/nhsr/nhsr024.pdf. [PubMed] [Google Scholar]
- 12.Moore KL, Boscardin WJ, Steinman MA, Schwartz JB. Age and sex variation in prevalence of chronic medical conditions in older residents of U.S. nursing homes. J Am Geriatr Soc. 2012;60:756–764. doi: 10.1111/j.1532-5415.2012.03909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDonald M, Hertz RP, Unger AN, Lustik MB. Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol A Biol Sci Med Sci. 2009;64:256–263. doi: 10.1093/gerona/gln016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shay CM, Ning H, Daniels SR, Rooks CR, Gidding SS, Lloyd-Jones DM. Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005–2010. Circulation. 2013;127:1369–1376. doi: 10.1161/CIRCULATIONAHA.113.001559. [DOI] [PubMed] [Google Scholar]
- 15.May AL, Kuklina EV, Yoon PW. Prevalence of cardiovascular disease risk factors among US adolescents, 1999–2008. Pediatrics. 2012;129:1035–1041. doi: 10.1542/peds.2011-1082. [DOI] [PubMed] [Google Scholar]
- 16.Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488–1496. doi: 10.1161/CIRCULATIONAHA.106.683243. [DOI] [PubMed] [Google Scholar]
- 17.Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298:874–879. doi: 10.1001/jama.298.8.874. [DOI] [PubMed] [Google Scholar]
- 18.Rodriguez BL, Dabelea D, Liese AD, Fujimoto W, Waitzfelder B, Liu L, Bell R, Talton J, Snively BM, Kershnar A, Urbina E, Daniels S Imperatore G; SEARCH Study Group. Prevalence and correlates of elevated blood pressure in youth with diabetes mellitus: the SEARCH for Diabetes in Youth study. J Pediatr. 2010;157:245–251. e1. doi: 10.1016/j.jpeds.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 19.Acosta AA, Samuels JA, Portman RJ, Redwine KM. Prevalence of persistent prehypertension in adolescents. J Pediatr. 2012;160:757–761. doi: 10.1016/j.jpeds.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 20.Falkner B, Gidding SS, Portman R, Rosner B. Blood pressure variability and classification of prehypertension and hypertension in adolescence. Pediatrics. 2008;122:238–242. doi: 10.1542/peds.2007-2776. [DOI] [PubMed] [Google Scholar]
- 21.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 22.Blackwell D, Lucas J, Clarke T. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. National Center for Health Statistics. Vital Health Stat 10. In press. [PubMed] [Google Scholar]
- 23.Romero CX, Romero TE, Shlay JC, Ogden LG, Dabelea D. Changing trends in the prevalence and disparities of obesity and other cardiovascular disease risk factors in three racial/ethnic groups of USA adults. Adv Prev Med. 2012;2012:172423. doi: 10.1155/2012/172423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howard G, Prineas R, Moy C, Cushman M, Kellum M, Temple E, Graham A, Howard V. Racial and geographic differences in awareness, treatment, and control of hypertension: the REasons for Geographic And Racial Differences in Stroke study. Stroke. 2006;37:1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) Hypertension-related mortality among Hispanic subpopulations: United States, 1995–2002. MMWR Morb Mortal Wkly Rep. 2006;55:177–180. [PubMed] [Google Scholar]
- 26.Borrell LN. Self-reported hypertension and race among Hispanics in the National Health Interview Survey. Ethn Dis. 2006;16:71–77. [PubMed] [Google Scholar]
- 27.Jones DW, Chambless LE, Folsom AR, Heiss G, Hutchinson RG, Sharrett AR, Szklo M, Taylor HA., Jr Risk factors for coronary heart disease in African Americans: the Atherosclerosis Risk in Communities study, 1987–1997. Arch Intern Med. 2002;162:2565–2571. doi: 10.1001/archinte.162.22.2565. [DOI] [PubMed] [Google Scholar]
- 28.Moran A, Diez Roux AV, Jackson SA, Kramer H, Manolio TA, Shrager S, Shea S. Acculturation is associated with hypertension in a multiethnic sample. Am J Hypertens. 2007;20:354–363. doi: 10.1016/j.amjhyper.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 29.Barnes PM, Adams PF, Powell-Griner E. Advance Data From Vital and Health Statistics; No. 394. Hyattsville, MD: National Center for Health Statistics; 2008. Health characteristics of the Asian adult population: United States, 2004–2006. [PubMed] [Google Scholar]
- 30.Murphy SL, Xu JQ, Kochanek KD. National Vital Statistics Report. 4. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2013. Deaths: final data for 2010. [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1999–2010. Series 20 No. 2P. [Accessed July 21, 2013];CDC WONDER Online Database [database online] Released January 2013. http://wonder.cdc.gov/cmf-icd10.html.
- 32.Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the U.S. by improvements in use of clinical preventive services. Am J Prev Med. 2010;38:600–609. doi: 10.1016/j.amepre.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 33.Ford ES. Trends in mortality from all causes and cardiovascular disease among hypertensive and nonhypertensive adults in the United States. Circulation. 2011;123:1737–1744. doi: 10.1161/CIRCULATIONAHA.110.005645. [DOI] [PubMed] [Google Scholar]
- 34.Lackland DT, Egan BM, Mountford WK, Boan AD, Evans DA, Gilbert G, McGee DL. Thirty-year survival for black and white hypertensive individuals in the Evans County Heart Study and the Hypertension Detection and Follow-up Program. J Am Soc Hypertens. 2008;2:448–454. doi: 10.1016/j.jash.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gazes PC, Lackland DT, Mountford WK, Gilbert GE, Harley RA. Comparison of cardiovascular risk factors for high brachial pulse pressure in blacks versus whites (Charleston Heart Study, Evans County Study, NHANES I and II Studies) Am J Cardiol. 2008;102:1514–1517. doi: 10.1016/j.amjcard.2008.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gray L, Lee IM, Sesso HD, Batty GD. Blood pressure in early adulthood, hypertension in middle age, and future cardiovascular disease mortality: HAHS (Harvard Alumni Health Study) J Am Coll Cardiol. 2011;58:2396–2403. doi: 10.1016/j.jacc.2011.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kraft P, Bauman L, Yuan JY, Horvath S Framingham Heart Study. Multivariate variance-components analysis of longitudinal blood pressure measurements from the Framingham Heart Study. BMC Genet. 2003;4(suppl 1):S55. doi: 10.1186/1471-2156-4-S1-S55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302:401–411. doi: 10.1001/jama.2009.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123:2799–2810. doi: 10.1161/CIRCULATIONAHA.110.016337. [DOI] [PubMed] [Google Scholar]
- 40.Vasan RS, Massaro JM, Wilson PW, Seshadri S, Wolf PA, Levy D, D’Agostino RB Framingham Heart Study. Antecedent blood pressure and risk of cardiovascular disease: the Framingham Heart Study. Circulation. 2002;105:48–53. doi: 10.1161/hc0102.101774. [DOI] [PubMed] [Google Scholar]
- 41.Franco OH, Peeters A, Bonneux L, de Laet C. Blood pressure in adulthood and life expectancy with cardiovascular disease in men and women: life course analysis. Hypertension. 2005;46:280–286. doi: 10.1161/01.HYP.0000173433.67426.9b. [DOI] [PubMed] [Google Scholar]
- 42.Deshmukh A, Kumar G, Kumar N, Nanchal R, Gobal F, Sakhuja A, Mehta JL. Effect of Joint National Committee VII report on hospitalizations for hypertensive emergencies in the United States. Am J Cardiol. 2011;108:1277–1282. doi: 10.1016/j.amjcard.2011.06.046. [DOI] [PubMed] [Google Scholar]
- 43.Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294:466–472. doi: 10.1001/jama.294.4.466. [DOI] [PubMed] [Google Scholar]
- 44.Wassertheil-Smoller S, Anderson G, Psaty BM, Black HR, Manson J, Wong N, Francis J, Grimm R, Kotchen T, Langer R, Lasser N. Hypertension and its treatment in postmenopausal women: baseline data from the Women’s Health Initiative. Hypertension. 2000;36:780–789. doi: 10.1161/01.hyp.36.5.780. [DOI] [PubMed] [Google Scholar]
- 45.Hawkins K, Mittapally R, Chang J, Nahum GG, Gricar J. Burden of illness of hypertension among women using menopausal hormone therapy: a US perspective. Curr Med Res Opin. 2010;26:2823–2832. doi: 10.1185/03007995.2010.532543. [DOI] [PubMed] [Google Scholar]
- 46.Sanchez RJ, Khalil L. Badger Heart Program: health screenings targeted to increase cardiovascular awareness in women at four northern sites in Wisconsin. WMJ. 2005;104:24–29. [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention (CDC) Prevalence of actions to control high blood pressure: 20 states, 2005. MMWR Morb Mortal Wkly Rep. 2007;56:420–423. [PubMed] [Google Scholar]
- 48.Wong ND, Dede J, Chow VH, Wong KS, Franklin SS. Global cardiovascular risk associated with hypertension and extent of treatment and control according to risk group. Am J Hypertens. 2012;25:561–567. doi: 10.1038/ajh.2012.2. [DOI] [PubMed] [Google Scholar]
- 49.Redmond N, Baer HJ, Hicks LS. Health behaviors and racial disparity in blood pressure control in the National Health and Nutrition Examination Survey. Hypertension. 2011;57:383–389. doi: 10.1161/HYPERTENSIONAHA.110.161950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang J, Geiss LS, Cheng YJ, Imperatore G, Saydah SH, James C, Gregg EW. Long-term and recent progress in blood pressure levels among U.S. adults with diagnosed diabetes, 1988–2008. Diabetes Care. 2011;34:1579–1581. doi: 10.2337/dc11-0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sarafidis PA. Epidemiology of resistant hypertension. J Clin Hypertens (Greenwich) 2011;13:523–528. doi: 10.1111/j.1751-7176.2011.00445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KC. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation. 2011;124:1046–1058. doi: 10.1161/CIRCULATIONAHA.111.030189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gupta AK, McGlone M, Greenway FL, Johnson WD. Prehypertension in disease-free adults: a marker for an adverse cardiometabolic risk profile. Hypertens Res. 2010;33:905–910. doi: 10.1038/hr.2010.91. [DOI] [PubMed] [Google Scholar]
- 54.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–1686. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 55.Greenlund KJ, Croft JB, Mensah GA. Prevalence of heart disease and stroke risk factors in persons with prehypertension in the United States, 1999–2000. Arch Intern Med. 2004;164:2113–2118. doi: 10.1001/archinte.164.19.2113. [DOI] [PubMed] [Google Scholar]
- 56.Glasser SP, Judd S, Basile J, Lackland D, Halanych J, Cushman M, Prineas R, Howard V, Howard G. Prehypertension, racial prevalence and its association with risk factors: analysis of the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Am J Hypertens. 2011;24:194–199. doi: 10.1038/ajh.2010.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee M, Saver JL, Chang B, Chang KH, Hao Q, Ovbiagele B. Presence of baseline prehypertension and risk of incident stroke: a meta-analysis. Neurology. 2011;77:1330–1337. doi: 10.1212/WNL.0b013e3182315234. [DOI] [PMC free article] [PubMed] [Google Scholar]
10. Diabetes Mellitus
ICD-9 250; ICD-10 E10 to E14. See Table 10-1 and Charts 10-1 through 10-4.
Table 10-1.
Diabetes Mellitus
| Population Group | Prevalence of Physician-Diagnosed DM, 2010: Age ≥20 y | Prevalence of Undiagnosed DM, 2010: Age ≥20 y | Prevalence of Prediabetes, 2010: Age ≥20 y | Incidence of Diagnosed DM: Age ≥20 y* | Mortality (DM), 2010: All Ages† | Hospital Discharges, 2010: All Ages | Cost, 2012‡ |
|---|---|---|---|---|---|---|---|
| Both sexes | 19 700 000 (8.3%) | 8 200 000 (3.5%) | 87 300 000 (38.2%) | 1 900 000 | 69 071 | 630 000 | $245 Billion |
| Males | 9 600 000 (8.7%) | 5 300 000 (4.7%) | 50 700 000 (46.0%) | … | 35 490 (51.4%)§ | 311 000 | … |
| Females | 10 100 000 (7.9%) | 2 900 000 (2.3%) | 33 600 000 (30.5%) | … | 33 581 (48.6%)§ | 319 000 | … |
| NH white males, % | 7.7 | 4.5 | 47.7 | … | 28 486 | … | … |
| NH white females, % | 6.2 | 1.8 | 30.0 | … | 25 764 | … | … |
| NH black males, % | 13.5 | 4.8 | 35.7 | … | 5640 | … | … |
| NH black females, % | 15.4 | 2.9 | 29.0 | … | 6486 | … | … |
| Mexican American males, % | 11.4 | 6.6 | 47.0 | … | … | … | … |
| Mexican American females, % | 12.0 | 4.7 | 31.9 | … | … | … | … |
| Asian or Pacific Islander | … | … | … | … | 1838 | … | … |
| American Indian or Alaska Native | … | … | … | … | 857 | … | … |
Undiagnosed DM is defined as those whose fasting glucose is ≥126 mg/dL but who did not report being told by a healthcare provider that they had DM. Prediabetes is a fasting blood glucose of 100 to <126 mg/dL (impaired fasting glucose); prediabetes includes impaired glucose tolerance.
DM indicates diabetes mellitus; and NH, non-Hispanic. Ellipses (…) indicate data not available.
Centers for Disease Control and Prevention, National Diabetes Fact Sheet, 2011.5
Mortality data for the white, black, Asian or Pacific Islander, and American Indian or Alaska Native populations include deaths among people of Hispanic and NH origin. Numbers of deaths for the American Indian or Alaska Native and Asian or Pacific Islander populations are known to be underestimated.
Yang et al.72
These percentages represent the portion of total DM mortality that is for males vs females.
Sources: Prevalence: Prevalence of diagnosed and undiagnosed DM: National Health and Nutrition Examination Survey 2007 to 2010, National Center for Health Statistics (NCHS), and National Heart, Lung, and Blood Institute. Percentages for racial/ethnic groups are age adjusted for Americans ≥20 y of age. Age-specific percentages are extrapolations to the 2010 US population estimates. Mortality: Centers for Disease Control and Prevention/NCHS, 2010 Mortality Multiple Cause-of-Death–United States, version May 28, 2013. These data represent underlying cause of death only. Hospital discharges: National Hospital Discharge Survey, NCHS; data include those inpatients discharged alive, dead, or status unknown.
Chart 10-1.
Age-adjusted prevalence of physician-diagnosed diabetes mellitus in adults ≥20 years of age by race/ethnicity and sex (National Health and Nutrition Examination Survey: 2007–2010). NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 10-4.
Diabetes mellitus awareness, treatment, and control in adults ≥20 years of age (National Health and Nutrition Examination Survey: 2007–2010). Source: National Heart, Lung, and Blood Institute.
DM is a major risk factor for CVD and stroke.1 The AHA has identified untreated fasting blood glucose levels of <100 mg/dL for children and adults as 1 of the 7 components of ideal cardiovascular health.2 In 2009 to 2010, 88.2% of children and 57.4% of adults met these criteria.2
Prevalence
The prevalence of DM for all age groups worldwide was estimated to be 2.8% in 2000 and is projected to be 4.4% in 2030. The total number of people with DM is projected to rise from 171 million in 2000 to 366 million in 2030.3
Youths
Approximately 186 000 people <20 years of age have DM. Each year, ≈15 000 people <20 years of age are diagnosed with type 1 DM. Healthcare providers are finding more and more children with type 2 DM, a disease usually diagnosed in adults ≥40 years of age. Children who develop type 2 DM are typically overweight or obese and have a family history of the disease. Most are American Indian, black, Asian, or Hispanic/Latino.4
During the period from 2002 to 2005, 3600 youth (age <20 years) were diagnosed with type 2 DM annually.5
Among adolescents 10 to 19 years of age diagnosed with DM, 57.8% of blacks were diagnosed with type 2 versus type 1 DM compared with 46.1% of Hispanic youths and 14.9% of white youths.6
According to the Bogalusa Heart Study, a long-term follow-up study of youths aging into adulthood, youths who were prediabetic or who had DM were more likely to have a constellation of metabolic disorders in young adulthood (19–44 years of age), including obesity, hypertension, dyslipidemia, and metabolic syndrome, all of which predispose to CHD.7
Among youths with type 2 DM, 10.4% are overweight and 79.4% are obese.8
According to NHANES data from 1999 to 2007, among US adolescents aged 12 to 19 years, the prevalence of prediabetes and DM increased from 9% to 23%.9
The TODAY cohort comprised youths aged 10 to 17 years (41.1% Hispanic and 31.5% non-Hispanic black) participating in a randomized controlled study of new-onset type 2 DM; 41.5% of participants had household income <$25 000.10 The results of the clinical trial demonstrated that only half of the children maintained durable glycemic control with monotherapy,11 a higher rate of treatment failure than observed in adult cohorts.
In the TODAY cohort, youths who had type 2 DM were sedentary >56 minutes longer per day (via accelerometry) than obese youth from NHANES.12
Of 1514 SEARCH participants, 95% reported having undergone BP checks and 88% reported having had lipid-level checks, whereas slightly more than two thirds (68%) reported having had HbA1c testing or eye examinations (66%).13
Abbreviations Used in Chapter 10
| ACC | American College of Cardiology |
| ACCORD | Action to Control Cardiovascular Risk in Diabetes |
| ACS | acute coronary syndrome |
| ADVANCE | Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation |
| AF | atrial fibrillation |
| AHA | American Heart Association |
| AHRQ | Agency for Healthcare Research and Quality |
| AMI | acute myocardial infarction |
| ARIC | Atherosclerosis Risk in Communities study |
| BMI | body mass index |
| BP | blood pressure |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CDC | Centers for Disease Control and Prevention |
| CHD | coronary heart disease |
| CHS | Cardiovascular Health Study |
| CI | confidence interval |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| ED | emergency department |
| ESRD | end-stage renal disease |
| EVEREST | Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan |
| FHS | Framingham Heart Study |
| HbA1c | hemoglobin A1c |
| HD | heart disease |
| HDL | high-density lipoprotein |
| HF | heart failure |
| HR | hazard ratio |
| ICD-9 | International Classification of Diseases, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| IDDM | insulin-dependent diabetes mellitus |
| LDL | low-density lipoprotein |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| MI | myocardial infarction |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHANES | National Health and Nutrition Examination Survey |
| NHDS | National Hospital Discharge Survey |
| NHIS | National Health Interview Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| NSTEMI | non–ST-segment–elevation myocardial infarction |
| OR | odds ratio |
| PA | physical activity |
| PAR | population-attributable risk |
| RR | relative risk |
| SBP | systolic blood pressure |
| SEARCH | Search for Diabetes in Youth Study |
| STEMI | ST-segment–elevation myocardial infarction |
| TODAY | Treatment Options for Type 2 Diabetes in Adolescents and Youth |
| UA | unstable angina |
Adults
(See Table 10-1 and Charts 10-1 through 10-3.)
Chart 10-3.
Trends in diabetes mellitus prevalence in adults ≥20 years of age by sex (National Health and Nutrition Examination Survey: 1988–1994 and 2007–2010). Source: National Center for Health Statistics, National Heart, Lung, and Blood Institute.
On the basis of data from NHANES 2007 to 2010 (unpublished NHLBI tabulation), an estimated 19.7 million Americans ≥20 years of age have physician-diagnosed DM. An additional 8.2 million adults have undiagnosed DM, and 87.3 million adults have prediabetes (eg, fasting blood glucose of 100 to <126 mg/dL). The prevalence of prediabetes in the US adult population is 38%.
The prevalence of diagnosed DM in adults ≥65 years of age was 26.9% in 2010, and an additional 50% (>20 million) had prediabetes based on fasting glucose, oral glucose tolerance testing, or HbA1c. In addition, data from NHANES 2005 to 2006 show that 46% of DM cases remain undiagnosed in this group aged ≥65 years.14
According to the Bogalusa Heart Study, men >20 years of age have a slightly higher prevalence of DM (11.8%) than women (10.8%).6
After adjustment for population age differences, 2007 to 2009 national survey data for people >20 years of age indicate that 7.1% of non-Hispanic whites, 8.4% of Asian Americans, 11.8% of Hispanics, and 12.6% of non-Hispanic blacks had diagnosed DM.5
Compared with non-Hispanic white adults, the risk of diagnosed DM was 18% higher among Asian Americans, 66% higher among Hispanics/Latinos, and 77% higher among non-Hispanic blacks.5
In 2004 to 2006, the prevalence of diagnosed DM was more than twice as high for Asian Indian adults (14%) as for Chinese (6%) or Japanese (5%) adults.15
Type 2 DM accounts for 90% to 95% of all diagnosed cases of DM in adults.5
On the basis of 2012 BRFSS (CDC) data, the prevalence of adults in the United States who reported ever having been told by a physician that they had DM ranged from 6.9% in Alaska to 13.0% in West Virginia. The mean percentage among all states was 10.1%.16
The CDC analyzed data from 1994 to 2004 collected by the Indian Health Service that indicated that the age-adjusted prevalence of DM per 1000 population increased 101.2% among American Indian/Alaska Native adults <35 years of age (from 8.5% to 17.1%). During this time period, the prevalence of diagnosed DM was greater among females than males in all age groups.17
On the basis of projections from NHANES studies between 1984 and 2004, the total prevalence of DM in the United States is expected to more than double from 2005 to 2050 (from 5.6% to 12.0%) in all age, sex, and race/ethnicity groups. Increases are projected to be largest for the oldest age groups (for instance, projected to increase by 220% among those 65–74 years of age and by 449% among those ≥75 years of age). DM prevalence is projected to increase by 99% among non-Hispanic whites, by 107% among non-Hispanic blacks, and by 127% among Hispanics. The age/race/ethnicity group with the largest increase is expected to be blacks ≥75 years of age (projected increase of 606%).18
According to NHIS data from 1997 to 2008, the prevalence of DM was higher at both time points among Asian Americans (4.3%–8.2%) than among whites (3.8%–6.0%), with the Asian American group also having a greater proportional increase (1.9- versus 1.5-fold increase). This was observed despite lower BMI levels (23.6 versus 26.1 kg/m2 in the earliest time period) among Asians.19
According to international survey and epidemiologic data from 2.7 million participants, the prevalence of DM in adults increased from 8.3% in men and 7.5% in women in 1980 to 9.8% in men and 9.2% in women in 2008. The number of individuals affected with DM increased from 153 million in 1980 to 347 million in 2008.20
Incidence
Youths
In the SEARCH study, the incidence of DM in youths overall was 24.3 per 100 000 person-years. Among children <10 years of age, most had type 1 DM, regardless of race/ethnicity. The highest rates of incident type 1 DM were observed in non-Hispanic white youths (18.6, 28.1, and 32.9 per 100 000 person-years for age groups of 0–4, 5–9, and 10–14 years, respectively). Overall, type 2 DM was relatively infrequent, with the highest rates (17.0–49.4 per 100 000 person-years) seen among 15- to 19-year-old minority groups.6
Of 2291 individuals <20 years of age with newly diagnosed DM, slightly more than half (54.5%) had autoimmune, insulin-sensitive DM, and 15.9% had nonautoimmune, insulin-resistant DM.21
Projecting disease burden by 2050, the number of youths with type 1 DM will conservatively increase from 166 018 to 203 382, and the number with type 2 DM will increase from 20 203 to 30 111. Less conservative modeling projects the number of type 1 DM patients at 587 488 and of those with type 2 DM at 84 131 by 2050.22
Adults
(See Table 10-1.)
A total of 1.9 million new cases of DM (type 1 or type 2) were diagnosed in US adults ≥20 years of age in 2010.5
Data from the FHS indicate a doubling in the incidence of DM over the past 30 years, most dramatically during the 1990s. Among adults 40 to 55 years of age in each decade of the 1970s, 1980s, and 1990s, the age-adjusted 8-year incidence rates of DM were 2.0%, 3.0%, and 3.7% among women and 2.7%, 3.6%, and 5.8% among men, respectively. Compared with the 1970s, the age- and sex-adjusted OR for DM was 1.40 in the 1980s and 2.05 in the 1990s (P for trend=0.0006). Most of the increase in absolute incidence of DM occurred in individuals with a BMI ≥30 kg/m2 (P for trend=0.03).23
DM incidence in adults also varies markedly by race. Over 5 years of follow-up in 45- to 84-year-olds in MESA, 8.2% of the cohort developed DM. The cumulative incidence was highest in Hispanics (11.3%), followed by black (9.5%), Chinese (7.7%), and white (6.3%) participants.24
On the basis of meta-analyses of 4 longitudinal cohort studies comprising 175 938 individuals and 1.1 million person-years of follow-up, a statistically significant adjusted association was observed between net duration of television viewing and risk for incident type 2 DM, with a 20% increased risk per each 2-hour daily increment of exposure (adjusted RR, 1.20; 95% CI, 1.14–1.27).25
According to NHANES data from 1988 to 1994 compared with 2005 to 2010, the prevalence of DM increased from 8.4% to 12.1%. This increase was most pronounced among those ≥65 years of age (increase in prevalence from 18.6% to 28.5%).26
According to data from NHANES and BRFSS, up to 48.7% of individuals with self-reported DM did not meet glycemic, BP, and lipid targets, and only 14.3% met all 3 targets and did not smoke.27
Gestational DM complicates 2% to 10% of pregnancies and increases the risk of developing type 2 DM by 35% to 60%.5
Mortality
(See Table 10-1.)
DM mortality in 2010 was 69 071. Any-mention mortality in 2010 was 234 051.28
The 2010 overall underlying-cause death rate attributable to DM was 20.8. Death rates per 100 000 people were 23.1 for white males, 43.6 for black males, 15.6 for white females, and 35.1 for black females.28
-
According to data from the National Diabetes Information Clearinghouse, the National Institute of Diabetes and Digestive and Kidney Diseases, and the National Institutes of Health:
At least 68% of people >65 years of age with DM die of some form of HD; 16% die of stroke.
HD death rates among adults with DM are 2 to 4 times higher than the rates for adults without DM.5
In a collaborative meta-analysis of 820 900 individuals from 97 prospective studies, DM was associated with the following risks: all-cause mortality, HR 1.80 (95% CI, 1.71–1.90); cancer death, HR 1.25 (95% CI, 1.19–1.31); and vascular death, HR 2.32 (95% CI, 2.11–2.56). In particular, DM was associated with death attributable to the following cancers: liver, pancreas, ovary, colorectal, lung, bladder, and breast. A 50-year-old with DM died on average 6 years earlier than an individual without DM.29
FHS/NHLBI data show that having DM significantly increased the risk of developing CVD (HR 2.5 for women and 2.4 for men) and of dying when CVD was present (HR 2.2 for women and 1.7 for men). Diabetic men and women ≥50 years of age lived an average of 7.5 and 8.2 years less than their nondiabetic counterparts. The differences in life expectancy free of CVD were 7.8 and 8.4 years, respectively.30
Analysis of data from NHANES 1971 to 2000 found that men with DM experienced a 43% relative reduction in the age-adjusted mortality rate, which was similar to that of nondiabetic men. Among women with DM, however, mortality rates did not decrease, and the difference in mortality rates between diabetic and nondiabetic women doubled.31
During 1979 to 2004, DM death rates for black youths 1 to 19 years of age were approximately twice those for white youths. During 2003 to 2004, the annual average DM death rate per 1 million youths was 2.46 for black youths and 0.91 for white youths.32
Among individuals ≥65 years of age participating in the CHS, during follow-up for up to 16 years, adjusted CHD mortality risk was similar for those with prevalent CHD free of DM at study entry compared with participants with DM but free of CHD (HR, 1.04; 95% CI, 0.83–1.30).33
Analysis of data from the FHS from 1950 to 2005 found reductions in all-cause and CVD mortality among men and women with and without DM; however, all-cause and CVD mortality rates among individuals with DM remain ≈2-fold higher than for individuals without DM.34
According to NHIS data from 1997 to 2006, the rate of CVD death among adults with DM decreased by 40% (95% CI, 23%–54%). Similarly, all-cause mortality decreased by 23% (95% CI, 10%–35%). In contrast, over this same period among adults without DM, the CVD mortality rate decreased by 60%, and the all-cause mortality rate decreased by 44%.35
Awareness
(See Chart 10-4.)
Analysis of NHANES/NCHS data from 1988 to 1994 and from 2005 to 2006 in adults ≥20 years of age showed that 40% of those with DM did not know they had it.14 Although the prevalence of diagnosed DM has increased significantly over the past decade, the prevalence of undiagnosed DM and impaired fasting glucose has remained relatively stable. Minority groups remain disproportionately affected.36
Analysis of NHANES data collected during 2007 to 2010 indicated that the prevalence of DM was 8.3% among people ≥20 years of age. Prevalence of DM was defined as people who were told by a physician or other health professional that they had DM (NHANES 2007–2010, NHLBI tabulation).
Of the estimated 27.9 million adults with DM, 70.6% were told they had DM or were undergoing treatment, and 29.4% (8.2 million) were unaware of the diagnosis. Of 12.9 million people being treated (65.5% of the diagnosed diabetic population), 5.1 million (39.5%) had their hyperglycemia under control (ie, they were undergoing treatment and had fasting plasma glucose <126 mg/dL), and 7.8 million (60.5%) were being treated but did not have their hyperglycemia under control (fasting plasma glucose ≥126 mg/dL). An estimated 6.8 million individuals with diagnosed DM are not treated with glucose-lowering therapy (NHANES 2007–2010, NHLBI tabulation).
Aftermath
Although the exact date of DM onset can be difficult to determine, increasing duration of DM diagnosis is associated with increasing CVD risk. Longitudinal data from FHS suggest that the risk factor–adjusted RR of CHD is 1.38 (95% CI, 0.99–1.92) times higher and the risk for CHD death is 1.86 (95% CI, 1.17–2.93) times higher for each 10-year increase in duration of DM.37
-
On the basis of data from the NCHS/NHIS, 1997 to 200538
The estimated number of people ≥35 years of age with DM with a self-reported cardiovascular condition increased 36%, from 4.2 million in 1997 to 5.7 million in 2005; however, the respective age-adjusted prevalence decreased 11.2%, from 36.6% in 1997 to 32.5% in 2005, reflecting an increase in the number of patients diagnosed with DM that exceeded the increase in CVD prevalence.
Age-adjusted CVD prevalence was higher among men than women, among whites than blacks, and among non-Hispanics than Hispanics. Among women, the age-adjusted prevalence decreased by 11.2%; among men, it did not decrease significantly. Among blacks, the age-adjusted prevalence of self-reported CVD decreased by 25.3%; among whites, no significant decrease occurred; among non-Hispanics, the rate decreased by 12%. No clear trends were detected among Hispanics.
Because the total number of people with DM and self-reported CVD increased over this period but proportions with self-reported CVD declined, the data suggest that the mean age at which people are diagnosed with DM is decreasing, or the higher CVD mortality rate among older diabetic individuals is removing them from ability to self-report CVD. These and other data show a consistent increase over time in the United States of the number of people with DM and CVD.
-
Data from the FHS show that despite improvements in CVD morbidity and mortality over >4 decades of observation, DM continues to be associated with incremental CVD risk. Participants 45 to 64 years of age from the FHS original and offspring cohorts who attended examinations in 1950 to 1966 (“earlier” time period) and 1977 to 1995 (“later” time period) were followed up for incident MI, CHD death, and stroke. Among participants with DM, the age- and sex-adjusted CVD incidence rate was 286.4 per 10 000 person-years in the earlier period and 146.9 per 10 000 person-years in the later period, a 35.4% decline. HRs for DM as a predictor of incident CVD were not significantly different in the earlier (risk factor–adjusted HR, 2.68; 95% CI, 1.88–3.82) versus later (HR, 1.96; 95% CI, 1.44–2.66) period.39 Thus, although there was a 50% reduction in the rate of incident CVD events among adults with DM, the absolute risk of CVD remained 2-fold greater than among people without DM.39
Data from these earlier and later time periods in FHS also suggest that the increasing prevalence of DM is leading to an increasing rate of CVD, resulting in part from CVD risk factors that commonly accompany DM. The age- and sex-adjusted HR for DM as a CVD risk factor was 3.0 in the earlier time period and 2.5 in the later time period. Because the prevalence of DM has increased over time, the PAR for DM as a CVD risk factor increased from 5.4% in the earlier time period to 8.7% in the later time period (attributable risk ratio, 1.62; P=0.04). Adjustment for CVD risk factors (age, sex, hypertension, current smoking, high cholesterol, and obesity) weakened this attributable risk ratio to 1.5 (P=0.12).40
Other data from FHS show that over a 30-year period, CVD among women with DM was 54.8% among normal-weight women but 78.8% among obese women. Among normal-weight men with DM, the lifetime risk of CVD was 78.6%, whereas it was 86.9% among obese men.41
Other studies show that the increased prevalence of DM is being followed by an increasing prevalence of CVD morbidity and mortality. New York City death certificate data for 1989 to 1991 and 1999 to 2001 and hospital discharge data for 1988 to 2002 show increases in all-cause and cause-specific mortality between 1990 and 2000, as well as in annual hospitalization rates for DM and its complications among patients hospitalized with AMI and/or DM. During this decade, all-cause and cause-specific mortality rates declined, although not for patients with DM; rates increased 61% and 52% for diabetic men and women, respectively, as did hospitalization rates for DM and its complications. The percentage of all AMIs occurring in patients with DM increased from 21% to 36%, and the absolute number more than doubled, from 2951 to 6048. Although hospital days for AMI fell overall, for those with DM, they increased 51% (from 34 188 to 51 566). These data suggest that increases in DM rates threaten the long-established nationwide trend toward reduced coronary artery events.42
Data from the ARIC study of the NHLBI found that the magnitude of incremental CHD risk associated with DM was smaller in blacks than in whites.43
A subgroup analysis was conducted of patients with DM enrolled in randomized clinical trials that evaluated ACS therapies. The data included 62 036 patients from Thrombolysis in Myocardial Infarction studies (46 577 with STEMI and 15 459 with UA/NSTEMI). Of these, 17.1% had DM. Modeling showed that mortality at 30 days was significantly higher among patients with DM than among those without DM who presented with UA/NSTEMI (2.1% versus 1.1%; P≤0.001) and STEMI (8.5% versus 5.4%; P=0.001), with adjusted risks for 30-day mortality in DM versus no DM of 1.78 for UA/NSTEMI (95% CI, 1.24–2.56) and 1.40 (95% CI, 1.24–1.57) for STEMI. DM was also associated with significantly higher mortality 1 year after UA/NSTEMI or STEMI. By 1 year after ACS, patients with DM who presented with UA/NSTEMI had a risk of death that approached that of patients without DM who presented with STEMI (7.2% versus 8.1%).44
In analyses from the National Registry of Myocardial Infarction comprising data registered on 1 734 431 patients admitted with AMI to 1964 participating US hospitals, the incremental adjusted OR for hospital mortality associated with DM declined from 1.24 (95% CI, 1.16–1.32) in 1994 to 1.08 (95% CI, 0.99–1.19) in 2006, which demonstrates a closing of the acute hospital mortality gap associated with DM.45
In an analysis of provincial health claims data for adults living in Ontario, Canada, between 1992 and 2000, the rate of patients admitted for AMI and stroke decreased to a greater extent in the diabetic than the nondiabetic population (AMI, −15.1% versus −9.1%, P=0.0001; stroke, −24.2% versus −19.4%, P=0.0001). Patients with DM experienced reductions in case fatality rates related to AMI and stroke similar to those without DM (−44.1% versus −33.2%, P=0.1, and −17.1% versus −16.6%, P=0.9, respectively) and similarly comparable decreases in all-cause mortality. Over the same period, the number of DM cases increased by 165%, which translates to a marked increase in the proportion of CVD events occurring among patients with DM: AMI, 44.6%; stroke, 26.1%; AMI deaths, 17.2%; and stroke deaths, 13.2%.46
In the same data set, the transition to a high-risk category (an event rate equivalent to a 10-year risk of 20% or an event rate equivalent to that associated with previous MI) occurred at a younger age for men and women with DM than for those without DM (mean difference, 14.6 years). For the outcome of AMI, stroke, or death resulting from any cause, men and women with DM entered the high-risk category at 47.9 and 54.3 years of age, respectively. The data suggest that DM confers a risk equivalent to aging 15 years. In North America, diverse data show lower rates of CVD among people with DM, but as the prevalence of DM has increased, so has the absolute burden of CVD, especially among middle-aged and older individuals.47
-
DM increases the risk of HF and adversely affects outcomes among patients with HF.
DM alone qualifies for the most recent ACC Foundation/AHA diagnostic criteria for stages A and B HF, a classification of patients without HF but at notably high risk for its development.48
In MESA, DM was associated with a 2-fold increased adjusted risk of incident HF among 6814 individuals free of CVD at baseline over a mean follow-up of 4 years (HR, 1.99; 95% CI, 1.08–3.68).49
Post hoc analysis of data from the EVEREST randomized trial of patients hospitalized with decompensated systolic HF stratified by DM status, which evaluated cardiovascular outcomes over a follow-up period of 9.9 months, demonstrated an increased adjusted HR for the composite of cardiovascular mortality and HF rehospitalization associated with DM (HR, 1.17; 95% CI, 1.04–1.31).50
DM increases the risk of AF. On the basis of meta-analysis of published observational data comprising 11 studies and >1.6 million participants, DM was crudely associated with a 40% increased risk for AF (RR, 1.39; 95% CI, 1.10–1.75) with the association remaining significant after multivariable adjustment (adjusted RR, 1.24; 95% CI, 1.06–1.44), yielding an estimate of the population attributable fraction of AF attributable to DM of 2.5%.51
-
DM increases the risk of stroke, with the RR ranging from 1.8- to 6-fold increased risk.37,52
DM is associated with increased ischemic stroke incidence at all ages, with the incremental risk associated with DM being most prominent before 55 years of age in blacks and before 65 years of age in whites.52
Ischemic stroke patients with DM are younger, more likely to be black, and more likely to have hypertension, prior MI, and high cholesterol than nondiabetic patients.52
DM accounted for 44% of the new cases of ESRD in 2007.53
In 2011, the incidence rate of ESRD attributed to DM in adults ≥20 years increased with age from 5.02 per 100 000 in those aged 20 to 29 years to 109.81 per 100 000 in those ≥70 years, compared with rates of 2.41 and 83.19, respectively, in those without DM.54
According to NHANES data, the prevalence of diabetic kidney disease has increased from 2.2% in NHANES III to 3.3% in NHANES 2005 to 2008. These increases were observed in direct proportion to increases in DM.55
HbA1c levels ≥6.5% can be used to diagnose DM.55a In the population-based ARIC study, over a 14-year follow-up period that preceded the endorsement of HbA1c as a diagnostic criterion, HbA1c levels ≥6.5% at study entry were associated with a multivariable-adjusted HR of 16.5 (95% CI, 14.2–19.1) for diagnosed DM based on contemporaneous diagnostic criteria and 1.95 (95% CI, 1.53–2.48) for CHD relative to those with HbA1c <5.0%.56
According to data from the ARIC study and NHANES III, the sensitivity and specificity for diagnosing DM with HbA1c criteria (compared with a single fasting glucose measurement of ≥126 mg/dL) were 47% and 98%, respectively.
Risk Factors
DM, especially type 2 DM, is associated with clustered risk factors for CHD, with a prevalence of 75% to 85% for hypertension among adults with DM, 70% to 80% for elevated LDL, and 60% to 70% for obesity.57
Aggressive treatment of hypertension is recommended for adults with DM to prevent cardiovascular complications. Between NHANES III (1984–1992) and NHANES 1999 to 2004, the proportion of patients with DM whose BP was treated increased from 76.5% to 87.8%, and the proportion whose BP was controlled nearly doubled (from 15.9% to 29.6%).58
Aggressive treatment of hypercholesterolemia is recommended for adults with DM, with the cornerstone of treatment being statin therapy, which is recommended for all patients with DM >40 years of age independent of baseline cholesterol, with targeted LDL cholesterol <100 mg/dL and optimally <70 mg/dL.59
CHD risk factors among patients with DM remain suboptimally treated, although improvements have been observed over the past decade. Between 1999 and 2008, in up to 2623 adult participants with DM, data from NHANES showed that improvements were observed for the achieved targets for control of HbA1c (from 37.0% to 55.2%), BP (from 35.2% to 51.0%), and LDL cholesterol (from 32.5% to 52.9%).60
-
Data from the 2012 National Healthcare Disparities Report (AHRQ, US Department of Health and Human Services) found that only about 23% of adults over age 40 years with DM received all 4 interventions to reduce risk factors recommended for comprehensive DM care in 2009. The proportion receiving all 4 interventions was lower among blacks and Hispanics than whites.61
In multivariable models, among those aged 40 to 64 years, only about 65% had their blood pressure <140/80 mm Hg, with blacks less likely than whites to achieve this blood pressure level.61
-
In 1 large academic medical center, outpatients with type 2 DM were observed during an 18-month period for proportions of patients who had HbA1c levels, BP, or total cholesterol levels measured; who had been prescribed any drug therapy if HbA1c levels, SBP, or LDL cholesterol levels exceeded recommended treatment goals; and who had been prescribed greater-than-starting-dose therapy if these values were above treatment goals. Patients were less likely to have cholesterol levels measured (76%) than HbA1c levels (92%) or BP (99%; P<0.0001 for either comparison). The proportion of patients who received any drug therapy was greater for above-goal HbA1c (92%) than for above-goal SBP (78%) or LDL cholesterol (38%; P<0.0001 for each comparison). Similarly, patients whose HbA1c levels were above the treatment goal (80%) were more likely to receive greater-than-starting-dose therapy than were those who had above-goal SBP (62%) and LDL cholesterol levels (13%; P<0.0001).62
Data from the same academic medical center also showed that CVD risk factors among women with DM were managed less aggressively than among men with DM. Women were less likely than men to have HbA1c <7% (without CHD: adjusted OR for women versus men 0.84, P=0.005; with CHD: 0.63, P<0.0001). Women without CHD were less likely than men to be treated with lipid-lowering medication (0.82; P=0.01) or, when treated, to have LDL cholesterol levels <100 mg/dL (0.75; P=0.004) and were less likely than men to be prescribed aspirin (0.63; P<0.0001). Women with DM and CHD were less likely than men to be prescribed aspirin (0.70, P<0.0001) and, when treated for hypertension or hyperlipidemia, were less likely to have BP levels <130/80 mm Hg (0.75; P<0.0001) or LDL cholesterol levels <100 mg/dL (0.80; P=0.006).63
Analysis of data from the CHS of the NHLBI found that lifestyle risk factors, including PA level, dietary habits, smoking habits, alcohol use, and adiposity measures, assessed late in life, were each independently associated with risk of new-onset DM. Participants whose PA level and dietary, smoking, and alcohol habits were all in the low-risk group had an 82% lower incidence of DM than all other participants. When absence of adiposity was added to the other 4 low-risk lifestyle factors, incidence of DM was 89% lower.64
According to 2007 data from the BRFSS, only 25% of adults with DM achieved recommended levels of total PA based on the 2007 American Diabetes Association guidelines.65
Hospitalizations
(See Table 10-1.)
Youths
Nationwide Inpatient Sample data from 1993 to 2004 were analyzed for individuals 0 to 29 years of age with a diagnosis of DM. Rates of hospitalizations increased by 38%. Hospitalization rates were higher for females (42%) than for males (29%). Inflation-adjusted total charges for DM hospitalizations increased 130%, from $1.05 billion in 1993 to $2.42 billion in 2004.66
Adults
According to NHDS data reported by the CDC in an analysis of data from 2010, DM was a listed diagnosis in 16% of US adult hospital discharges. Of the 5.1 million discharges with DM listed, circulatory diseases was the most common first-listed diagnosis (24.1%; 1.3 million discharges) and DM the second most common (11.5%; 610 000 discharges).67
Hypoglycemia
Hypoglycemia is a common side effect of DM treatment, typically defined as a blood glucose level <50 mg/dL; severe hypoglycemia is additionally defined as patients needing assistance to treat themselves.
In the ADVANCE trial, 2.1% of patients had an episode of severe hypoglycemia.
Severe hypoglycemia was associated with an increased risk of major macrovascular events (HR, 2.88; 95% CI, 2.01–4.12), cardiovascular death (HR, 2.68; 95% CI, 1.72–4.19), and all-cause death (HR, 2.69; 95% CI, 1.97–3.67), including nonvascular outcomes. The lack of specificity of hypoglycemia with vascular outcomes suggests that it might be a marker for susceptibility. Risk factors for hypoglycemia included older age, DM duration, worse renal function, lower BMI, lower cognitive function, use of multiple glucose-lowering medications, and randomization to the intensive glucose control arm.68
According to data from the 2004 to 2008 MarketScan database of type 2 DM, which consisted of 536 581 individuals, the incidence rate of hypoglycemia was 153.8 per 10 000 person-years and was highest in adults aged 18 to 34 years (218.8 per 10 000 person-years).69
According to data from 2956 adults >55 years of age from the ACCORD trial, poor cognitive function, defined as a 5-point poorer baseline score on the Digit Symbol Substitution Test, was associated with a 13% increased risk of severe hypoglycemia that required medical assistance.70
In a sample of 813 adults with type 2 DM enrolled in commercial health plans, 71% reported experiencing symptoms of hypoglycemia.71
Cost
(See Table10-1.)
In 2012, the cost of DM was estimated at $245 billion, up from $174 billion in 2007, accounting for 1 in 5 healthcare dollars. Of these costs, $176 billion were direct medical costs and $69 billion resulted from reduced productivity. Inpatient care accounted for 43% of these costs, 18% were attributable to prescription costs to treat DM complications, and 12% were related to antidiabetes agents and supplies.72
After adjustment for age and sex, medical costs for patients with DM were 2.3 times higher than for people without DM.5
According to the insurance claims and MarketScan data from 7556 youths <19 years of age with insulin-treated DM, costs for youths with hypoglycemia were $12 850 compared with $8970 for youths without hypoglycemia. For diabetic ketoacidosis, costs were $14 236 for youths with versus $8398 for youths without diabetic ketoacidosis.73
The cost of hypoglycemia, according to data from 536 581 individuals with type 2 DM from the 2004 to 2008 MarketScan database, was $52 223 675, which accounted for 1.0% of inpatient costs, 2.7% of ED costs, and 0.3% of out-patient costs. This resulted in a mean cost of $17 564 for an inpatient admission, $1387 for an ED visit, and $394 for an outpatient visit.69
Type 1 DM
Type 1 DM constitutes 5% to 10% of DM in the United States.74
The Colorado IDDM Study Registry and SEARCH for Diabetes in Youth registry demonstrated an increasing incidence of type 1 DM among Colorado youths ≤17 years of age, with an increase in the incidence of 2.3% (95% CI, 1.6%–3.1%) per year over the past 26 years.75
Between 1996 and 2010, the number of youths with type 1 DM increased by 5.7% per year.76
Among youths with type 1 DM, the prevalence of overweight is 22.1% and the prevalence of obesity is 12.6%.8
A long-term study of patients with type 1 DM that began in 1966 showed that over 30 years of follow-up, overall risk of mortality associated with type 1 DM was 7 times greater than that of the general population. Females had a 13.2-fold incremental mortality risk compared with a 5.0-fold increased risk in males. During the course of study, the incremental mortality risk associated with type 1 DM declined from 9.3 to 5.6 times that of nondiabetic control subjects.77
According to 30-year mortality data from Allegheny County, PA, those with type 1 DM have a mortality rate 5.6 times higher than the general population.78
The leading cause of death among patients with type 1 DM is CVD, which accounted for 22% of deaths among those in the Allegheny County, PA, type 1 DM registry, followed by renal (20%) and infectious (18%) causes.79
Long-term follow-up data from the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study Research Group showed that intensive versus conventional treatment in the Diabetes Control and Complications Trial was associated with a 42% reduced risk of CVD (P=0.02) and a 57% reduced risk of the composite end point (P=0.02; included nonfatal MI, stroke, and CVD death).80
Observational data from the Swedish National Diabetes Register showed that most CVD risk factors were more adverse among patients with HbA1c between 8.0% and 11.9% than among those with HbA1c between 5.0% and 7.9%. Per 1% unit increase in HbA1c, the HR of fatal and nonfatal CHD was 1.30 in multivariable-adjusted models and 1.27 for fatal and nonfatal CVD. Among patients with HbA1c 8.0% to 11.9% compared with those with HbA1c 5.0% to 7.9%, the HR of fatal/nonfatal CHD was 1.71 and the risk of fatal/nonfatal CVD was 1.59.81
Among 2787 patients from the EURODIAB Prospective Complications Study, age, waist-hip ratio, pulse pressure, non-HDL cholesterol, microalbuminuria, and peripheral and autonomic neuropathy were risk factors for all-cause, CVD, and non-CVD mortality.81a
Among 3610 older patients (>60 years of age) with type 1 DM, the risk of severe hypoglycemia was twice as high as for those <60 years of age (40.1 versus 24.3 per 100 patient-years).82
- 1.Buse JB, Ginsberg HN, Bakris GL, Clark NG, Costa F, Eckel R, Fonseca V, Gerstein HC, Grundy S, Nesto RW, Pignone MP, Plutzky J, Porte D, Redberg R, Stitzel KF, Stone NJ. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Circulation. 2007;115:114–126. doi: 10.1161/CIRCULATIONAHA.106.179294. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 3.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 4.Liu LL, Yi JP, Beyer J, Mayer-Davis EJ, Dolan LM, Dabelea DM, Lawrence JM, Rodriguez BL, Marcovina SM, Waitzfelder BE, Fujimoto WY SEARCH for Diabetes in Youth Study Group. Type 1 and type 2 diabetes in Asian and Pacific Islander U.S. youth: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2009;32(suppl 2):S133–S140. doi: 10.2337/dc09-S205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 6.Dabelea D, Bell RA, D’Agostino RB, Jr, Imperatore G, Johansen JM, Linder B, Liu LL, Loots B, Marcovina S, Mayer-Davis EJ, Pettitt DJ, Waitzfelder B Writing Group for the SEARCH for Diabetes in Youth Study Group. Incidence of diabetes in youth in the United States. JAMA. 2007;297:2716–2724. doi: 10.1001/jama.297.24.2716. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen QM, Srinivasan SR, Xu JH, Chen W, Berenson GS. Changes in risk variables of metabolic syndrome since childhood in pre-diabetic and type 2 diabetic subjects: the Bogalusa Heart Study. Diabetes Care. 2008;31:2044–2049. doi: 10.2337/dc08-0898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu LL, Lawrence JM, Davis C, Liese AD, Pettitt DJ, Pihoker C, Dabelea D, Hamman R, Waitzfelder B, Kahn HS SEARCH for Diabetes in Youth Study Group. Prevalence of overweight and obesity in youth with diabetes in USA: the SEARCH for Diabetes in Youth study. Pediatr Diabetes. 2010;11:4–11. doi: 10.1111/j.1399-5448.2009.00519.x. [DOI] [PubMed] [Google Scholar]
- 9.May AL, Kuklina EV, Yoon PW. Prevalence of cardiovascular disease risk factors among US adolescents, 1999–2008. Pediatrics. 2012;129:1035–1041. doi: 10.1542/peds.2011-1082. [DOI] [PubMed] [Google Scholar]
- 10.Copeland KC, Zeitler P, Geffner M, Guandalini C, Higgins J, Hirst K, Kaufman FR, Linder B, Marcovina S, McGuigan P, Pyle L, Tamborlane W, Willi S TODAY Study Group. Characteristics of adolescents and youth with recent-onset type 2 diabetes: the TODAY cohort at baseline. J Clin Endocrinol Metab. 2011;96:159–167. doi: 10.1210/jc.2010-1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zeitler P, Hirst K, Pyle L, Linder B, Copeland K, Arslanian S, Cuttler L, Nathan DM, Tollefsen S, Wilfley D, Kaufman F TODAY Study Group. A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med. 2012;366:2247–2256. doi: 10.1056/NEJMoa1109333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kriska A, Delahanty L, Edelstein S, Amodei N, Chadwick J, Copeland K, Galvin B, El ghormli L, Haymond M, Kelsey M, Lassiter C, Mayer-Davis E, Milaszewski K, Syme A. Sedentary behavior and physical activity in youth with recent onset of type 2 diabetes. Pediatrics. 2013;131:e850–e856. doi: 10.1542/peds.2012-0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waitzfelder B, Pihoker C, Klingensmith G, Case D, Anderson A, Bell RA, Lawrence JM, Mayer-Davis EJ, Imperatore G, Standiford D, Rodriguez BL, Dabelea D, Seid M SEARCH for Diabetes in Youth Study Group. Adherence to guidelines for youths with diabetes mellitus. Pediatrics. 2011;128:531–538. doi: 10.1542/peds.2010-3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cowie CC, Rust KF, Ford ES, Eberhardt MS, Byrd-Holt DD, Li C, Williams DE, Gregg EW, Bainbridge KE, Saydah SH, Geiss LS. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988–1994 and 2005–2006 [published correction appears in Diabetes Care. 2011;34:2338] Diabetes Care. 2009;32:287–294. doi: 10.2337/dc08-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnes PM, Adams PF, Powell-Griner E. Advance Data From Vital and Health Statistics; No. 394. Hyattsville, MD: National Center for Health Statistics; 2008. Health characteristics of the Asian adult population: United States, 2004–2006. [PubMed] [Google Scholar]
- 16.Behavioral Risk Factor Surveillance System: prevalence and trends data. [Accessed June 4, 2013];Centers for Disease Control and Prevention Web site. http://apps.nccd.cdc.gov/brfss/index.asp.
- 17.Centers for Disease Control and Prevention (CDC) Diagnosed diabetes among American Indians and Alaska Natives aged <35 years: United States, 1994–2004. MMWR Morb Mortal Wkly Rep. 2006;55:1201–1203. [PubMed] [Google Scholar]
- 18.Narayan KM, Boyle JP, Geiss LS, Saaddine JB, Thompson TJ. Impact of recent increase in incidence on future diabetes burden: U.S., 2005–2050. Diabetes Care. 2006;29:2114–2116. doi: 10.2337/dc06-1136. [DOI] [PubMed] [Google Scholar]
- 19.Lee JW, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997–2008. Diabetes Care. 2011;34:353–357. doi: 10.2337/dc10-0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 21.Dabelea D, Pihoker C, Talton JW, D’Agostino RB, Jr, Fujimoto W, Klingensmith GJ, Lawrence JM, Linder B, Marcovina SM, Mayer-Davis EJ, Imperatore G, Dolan LM SEARCH for Diabetes in Youth Study. Etiological approach to characterization of diabetes type: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2011;34:1628–1633. doi: 10.2337/dc10-2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Imperatore G, Boyle JP, Thompson TJ, Case D, Dabelea D, Hamman RF, Lawrence JM, Liese AD, Liu LL, Mayer-Davis EJ, Rodriguez BL, Standiford D SEARCH for Diabetes in Youth Study Group. Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care. 2012;35:2515–2520. doi: 10.2337/dc12-0669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fox CS, Pencina MJ, Meigs JB, Vasan RS, Levitzky YS, D’Agostino RB., Sr Trends in the incidence of type 2 diabetes mellitus from the 1970s to the 1990s: the Framingham Heart Study. Circulation. 2006;113:2914–2918. doi: 10.1161/CIRCULATIONAHA.106.613828. [DOI] [PubMed] [Google Scholar]
- 24.Nettleton JA, Steffen LM, Ni H, Liu K, Jacobs DR., Jr Dietary patterns and risk of incident type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA) Diabetes Care. 2008;31:1777–1782. doi: 10.2337/dc08-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011;305:2448–2455. doi: 10.1001/jama.2011.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheng YJ, Imperatore G, Geiss LS, Wang J, Saydah SH, Cowie CC, Gregg EW. Secular changes in the age-specific prevalence of diabetes among U.S. adults: 1988–2010. Diabetes Care. 2013;36:2690–2696. doi: 10.2337/dc12-2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999–2010 [published correction appears in N Engl J Med. 2013;369:587] N Engl J Med. 2013;368:1613–1624. doi: 10.1056/NEJMsa1213829. [DOI] [PubMed] [Google Scholar]
- 28.Murphy SL, Xu JQ, Kochanek KD. National Vital Statistics Report. 4. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2013. Deaths: final data for 2010. [PubMed] [Google Scholar]
- 29.Seshasai SR, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, Whincup PH, Mukamal KJ, Gillum RF, Holme I, Njølstad I, Fletcher A, Nilsson P, Lewington S, Collins R, Gudnason V, Thompson SG, Sattar N, Selvin E, Hu FB, Danesh J Emerging Risk Factors Collaboration. Diabetes mellitus, fasting glucose, and risk of cause-specific death [published correction appears in N Engl J Med. 2011;364:1281] N Engl J Med. 2011;364:829–841. doi: 10.1056/NEJMoa1008862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Franco OH, Steyerberg EW, Hu FB, Mackenbach J, Nusselder W. Associations of diabetes mellitus with total life expectancy and life expectancy with and without cardiovascular disease. Arch Intern Med. 2007;167:1145–1151. doi: 10.1001/archinte.167.11.1145. [DOI] [PubMed] [Google Scholar]
- 31.Gregg EW, Gu Q, Cheng YJ, Narayan KM, Cowie CC. Mortality trends in men and women with diabetes, 1971 to 2000. Ann Intern Med. 2007;147:149–155. doi: 10.7326/0003-4819-147-3-200708070-00167. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention (CDC) Racial disparities in diabetes mortality among persons aged 1–19 years: United States, 1979–2004. MMWR Morb Mortal Wkly Rep. 2007;56:1184–1187. [PubMed] [Google Scholar]
- 33.Carnethon MR, Biggs ML, Barzilay J, Kuller LH, Mozaffarian D, Mukamal K, Smith NL, Siscovick D. Diabetes and coronary heart disease as risk factors for mortality in older adults. Am J Med. 2010;123:556.e1–556.e9. doi: 10.1016/j.amjmed.2009.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Preis SR, Hwang SJ, Coady S, Pencina MJ, D’Agostino RB, Sr, Savage PJ, Levy D, Fox CS. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation. 2009;119:1728–1735. doi: 10.1161/CIRCULATIONAHA.108.829176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gregg EW, Cheng YJ, Saydah S, Cowie C, Garfield S, Geiss L, Barker L. Trends in death rates among U.S. adults with and without diabetes between 1997 and 2006: findings from the National Health Interview Survey. Diabetes Care. 2012;35:1252–1257. doi: 10.2337/dc11-1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM, Saydah SH, Williams DE, Geiss LS, Gregg EW. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999–2002. Diabetes Care. 2006;29:1263–1268. doi: 10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 37.Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, Creager MA, Culebras A, Eckel RH, Hart RG, Hinchey JA, Howard VJ, Jauch EC, Levine SR, Meschia JF, Moore WS, Nixon JV, Pearson TA on behalf of the American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention; Council for High Blood Pressure Research, Council on Peripheral Vascular Disease, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association [published correction appears in Stroke. 2011;42:e26] Stroke. 2011;42:517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention (CDC) Prevalence of self-reported cardiovascular disease among persons aged > or =35 years with diabetes: United States, 1997–2005. MMWR Morb Mortal Wkly Rep. 2007;56:1129–1132. [PubMed] [Google Scholar]
- 39.Fox CS, Coady S, Sorlie PD, Levy D, Meigs JB, D’Agostino RB, Sr, Wilson PW, Savage PJ. Trends in cardiovascular complications of diabetes. JAMA. 2004;292:2495–2499. doi: 10.1001/jama.292.20.2495. [DOI] [PubMed] [Google Scholar]
- 40.Fox CS, Coady S, Sorlie PD, D’Agostino RB, Sr, Pencina MJ, Vasan RS, Meigs JB, Levy D, Savage PJ. Increasing cardiovascular disease burden due to diabetes mellitus: the Framingham Heart Study. Circulation. 2007;115:1544–1550. doi: 10.1161/CIRCULATIONAHA.106.658948. [DOI] [PubMed] [Google Scholar]
- 41.Fox CS, Pencina MJ, Wilson PW, Paynter NP, Vasan RS, D’Agostino RB., Sr Lifetime risk of cardiovascular disease among individuals with and without diabetes stratified by obesity status in the Framingham heart study. Diabetes Care. 2008;31:1582–1584. doi: 10.2337/dc08-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fang J, Alderman MH. Impact of the increasing burden of diabetes on acute myocardial infarction in New York City: 1990–2000. Diabetes. 2006;55:768–773. doi: 10.2337/diabetes.55.03.06.db05-1196. [DOI] [PubMed] [Google Scholar]
- 43.Jones DW, Chambless LE, Folsom AR, Heiss G, Hutchinson RG, Sharrett AR, Szklo M, Taylor HA., Jr Risk factors for coronary heart disease in African Americans: the Atherosclerosis Risk in Communities study, 1987–1997. Arch Intern Med. 2002;162:2565–2571. doi: 10.1001/archinte.162.22.2565. [DOI] [PubMed] [Google Scholar]
- 44.Donahoe SM, Stewart GC, McCabe CH, Mohanavelu S, Murphy SA, Cannon CP, Antman EM. Diabetes and mortality following acute coronary syndromes. JAMA. 2007;298:765–775. doi: 10.1001/jama.298.7.765. [DOI] [PubMed] [Google Scholar]
- 45.Gore MO, Patel MJ, Kosiborod M, Parsons LS, Khera A, de Lemos JA, Rogers WJ, Peterson ED, Canto JC, McGuire DK National Registry of Myocardial Infarction Investigators. Diabetes mellitus and trends in hospital survival after myocardial infarction, 1994 to 2006: data from the National Registry of Myocardial Infarction. Circ Cardiovasc Qual Outcomes. 2012;5:791–797. doi: 10.1161/CIRCOUTCOMES.112.965491. [DOI] [PubMed] [Google Scholar]
- 46.Booth GL, Kapral MK, Fung K, Tu JV. Recent trends in cardiovascular complications among men and women with and without diabetes. Diabetes Care. 2006;29:32–37. doi: 10.2337/diacare.29.01.06.dc05-0776. [DOI] [PubMed] [Google Scholar]
- 47.Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet. 2006;368:29–36. doi: 10.1016/S0140-6736(06)68967-8. [DOI] [PubMed] [Google Scholar]
- 48.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW. 2009 Focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation [published correction appears in Circulation. 2010;121:e258] Circulation. 2009;119:e391–e479. doi: 10.1161/CIRCULATIONAHA.109.192065. [DOI] [PubMed] [Google Scholar]
- 49.Bahrami H, Bluemke DA, Kronmal R, Bertoni AG, Lloyd-Jones DM, Shahar E, Szklo M, Lima JA. Novel metabolic risk factors for incident heart failure and their relationship with obesity: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;51:1775–1783. doi: 10.1016/j.jacc.2007.12.048. [DOI] [PubMed] [Google Scholar]
- 50.Sarma S, Mentz RJ, Kwasny MJ, Fought AJ, Huffman M, Subacius H, Nodari S, Konstam M, Swedberg K, Maggioni AP, Zannad F, Bonow RO, Gheorghiade M EVEREST Investigators. Association between diabetes mellitus and post-discharge outcomes in patients hospitalized with heart failure: findings from the EVEREST trial. Eur J Heart Fail. 2013;15:194–202. doi: 10.1093/eurjhf/hfs153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Huxley RR, Filion KB, Konety S, Alonso A. Meta-analysis of cohort and case-control studies of type 2 diabetes mellitus and risk of atrial fibrillation. Am J Cardiol. 2011;108:56–62. doi: 10.1016/j.amjcard.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kissela BM, Khoury J, Kleindorfer D, Woo D, Schneider A, Alwell K, Miller R, Ewing I, Moomaw CJ, Szaflarski JP, Gebel J, Shukla R, Broderick JP. Epidemiology of ischemic stroke in patients with diabetes: the Greater Cincinnati/Northern Kentucky Stroke Study. Diabetes Care. 2005;28:355–359. doi: 10.2337/diacare.28.2.355. [DOI] [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention (CDC) Incidence of end-stage renal disease attributed to diabetes among persons with diagnosed diabetes: United States and Puerto Rico, 1996–2007. MMWR Morb Mortal Wkly Rep. 2010;59:1361–1366. [PubMed] [Google Scholar]
- 54.Centers for Disease Control and Prevention. US Chronic Kidney Disease Surveillance System. Atlanta, GA: US Department of Health and Human Services; 2011. [Accessed September 20, 2013]. http://www.cdc.gov/ckd. [Google Scholar]
- 55.de Boer IH, Rue TC, Hall YN, Heagerty PJ, Weiss NS, Himmelfarb J. Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA. 2011;305:2532–2539. doi: 10.1001/jama.2011.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55a.American Diabetes Association. Diagnosis and classification of diabetes mellitus [published correction appears in Diabetes Care. 2010;33:e57] Diabetes Care. 2010;33(suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Selvin E, Steffes MW, Zhu H, Matsushita K, Wagenknecht L, Pankow J, Coresh J, Brancati FL. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 2010;362:800–811. doi: 10.1056/NEJMoa0908359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Preis SR, Pencina MJ, Hwang SJ, D’Agostino RB, Sr, Savage PJ, Levy D, Fox CS. Trends in cardiovascular disease risk factors in individuals with and without diabetes mellitus in the Framingham Heart Study. Circulation. 2009;120:212–220. doi: 10.1161/CIRCULATIONAHA.108.846519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Suh DC, Kim CM, Choi IS, Plauschinat CA, Barone JA. Trends in blood pressure control and treatment among type 2 diabetes with comorbid hypertension in the United States: 1988–2004. J Hypertens. 2009;27:1908–1916. doi: 10.1097/HJH.0b013e32832d4aee. [DOI] [PubMed] [Google Scholar]
- 59.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ National Heart, Lung, and Blood Institute; American College of Cardiology Foundation; American Heart Association. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines [published correction appears in Circulation. 2004;110:763] Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 60.Ford ES. Trends in the control of risk factors for cardiovascular disease among adults with diagnosed diabetes: findings from the National Health and Nutrition Examination Survey 1999–2008. J Diabetes. 2011;3:337–347. doi: 10.1111/j.1753-0407.2011.00148.x. [DOI] [PubMed] [Google Scholar]
- 61.US Department of Health and Human Services, Agency for Healthcare Research and Quality. National Healthcare Disparities Report, 2012. Rockville, MD: Agency for Healthcare Research and Quality; 2012. [Accessed October 30, 2013]. http://www.ahrq.gov/research/findings/nhqrdr/nhdr12/2012nhdr.pdf. [Google Scholar]
- 62.Grant RW, Cagliero E, Murphy-Sheehy P, Singer DE, Nathan DM, Meigs JB. Comparison of hyperglycemia, hypertension, and hypercholesterolemia management in patients with type 2 diabetes. Am J Med. 2002;112:603–609. doi: 10.1016/s0002-9343(02)01103-8. [DOI] [PubMed] [Google Scholar]
- 63.Wexler DJ, Grant RW, Meigs JB, Nathan DM, Cagliero E. Sex disparities in treatment of cardiac risk factors in patients with type 2 diabetes. Diabetes Care. 2005;28:514–520. doi: 10.2337/diacare.28.3.514. [DOI] [PubMed] [Google Scholar]
- 64.Mozaffarian D, Kamineni A, Carnethon M, Djoussé L, Mukamal KJ, Siscovick D. Lifestyle risk factors and new-onset diabetes mellitus in older adults: the cardiovascular health study. Arch Intern Med. 2009;169:798–807. doi: 10.1001/archinternmed.2009.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhao G, Ford ES, Li C, Balluz LS. Physical activity in U.S. older adults with diabetes mellitus: prevalence and correlates of meeting physical activity recommendations. J Am Geriatr Soc. 2011;59:132–137. doi: 10.1111/j.1532-5415.2010.03236.x. [DOI] [PubMed] [Google Scholar]
- 66.Lee JM, Okumura MJ, Freed GL, Menon RK, Davis MM. Trends in hospitalizations for diabetes among children and young adults: United States, 1993 2004. Diabetes Care. 2007;30:3035–3039. doi: 10.2337/dc07-0769. [DOI] [PubMed] [Google Scholar]
- 67.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics, Division of Health Care Statistics. Distribution of first-listed diagnoses among hospital discharges with diabetes as any listed diagnosis, adults aged 18 years and older, United States, 2010. [Accessed July 22, 2013];Centers for Disease Control and Prevention Web site. http://www.cdc.gov/diabetes/statistics/hosp/adulttable1.htm.
- 68.Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, Woodward M, Ninomiya T, Neal B, MacMahon S, Grobbee DE, Kengne AP, Marre M, Heller S ADVANCE Collaborative Group. Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010;363:1410–1418. doi: 10.1056/NEJMoa1003795. [DOI] [PubMed] [Google Scholar]
- 69.Quilliam BJ, Simeone JC, Ozbay AB, Kogut SJ. The incidence and costs of hypoglycemia in type 2 diabetes. Am J Manag Care. 2011;17:673–680. [PubMed] [Google Scholar]
- 70.Punthakee Z, Miller ME, Launer LJ, Williamson JD, Lazar RM, Cukierman-Yaffee T, Seaquist ER, Ismail-Beigi F, Sullivan MD, Lovato LC, Bergenstal RM, Gerstein HC ACCORD Group of Investigators; ACCORD-MIND Investigators. Poor cognitive function and risk of severe hypoglycemia in type 2 diabetes: post hoc epidemiologic analysis of the ACCORD trial. Diabetes Care. 2012;35:787–793. doi: 10.2337/dc11-1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Williams SA, Shi L, Brenneman SK, Johnson JC, Wegner JC, Fonseca V. The burden of hypoglycemia on healthcare utilization, costs, and quality of life among type 2 diabetes mellitus patients. J Diabetes Complications. 2012;26:399–406. doi: 10.1016/j.jdiacomp.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 72.Yang W, Dall T, Halder P, Gallo P, Kowal S, Hogan P American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36:1033–1046. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shrestha SS, Zhang P, Barker L, Imperatore G. Medical expenditures associated with diabetes acute complications in privately insured U.S. youth. Diabetes Care. 2010;33:2617–2622. doi: 10.2337/dc10-1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Redberg RF, Greenland P, Fuster V, Pyörälä K, Blair SN, Folsom AR, Newman AB, O’Leary DH, Orchard TJ, Psaty B, Schwartz JS, Starke R, Wilson PW. Prevention Conference VI: Diabetes and Cardiovascular Disease: Writing Group III: risk assessment in persons with diabetes. Circulation. 2002;105:e144–e152. doi: 10.1161/01.cir.0000013955.34262.af. [DOI] [PubMed] [Google Scholar]
- 75.Vehik K, Hamman RF, Lezotte D, Norris JM, Klingensmith G, Bloch C, Rewers M, Dabelea D. Increasing incidence of type 1 diabetes in 0- to 17-year-old Colorado youth. Diabetes Care. 2007;30:503–509. doi: 10.2337/dc06-1837. [DOI] [PubMed] [Google Scholar]
- 76.Hummel K, McFann KK, Realsen J, Messer LH, Klingensmith GJ, Chase HP. The increasing onset of type 1 diabetes in children. J Pediatr. 2012;161:652–657. e1. doi: 10.1016/j.jpeds.2012.03.061. [DOI] [PubMed] [Google Scholar]
- 77.Dorman JS, Laporte RE, Kuller LH, Cruickshanks KJ, Orchard TJ, Wagener DK, Becker DJ, Cavender DE, Drash AL. The Pittsburgh Insulin-Dependent Diabetes Mellitus (IDDM) morbidity and mortality study: mortality results. Diabetes. 1984;33:271–276. doi: 10.2337/diab.33.3.271. [DOI] [PubMed] [Google Scholar]
- 78.Secrest AM, Becker DJ, Kelsey SF, LaPorte RE, Orchard TJ. All-cause mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes: the Allegheny County Type 1 Diabetes Registry. Diabetes Care. 2010;33:2573–2579. doi: 10.2337/dc10-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Secrest AM, Becker DJ, Kelsey SF, Laporte RE, Orchard TJ. Cause-specific mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes. Diabetes. 2010;59:3216–3222. doi: 10.2337/db10-0862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643–2653. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Eeg-Olofsson K, Cederholm J, Nilsson PM, Zethelius B, Svensson AM, Gudbjörnsdóttir S, Eliasson B. Glycemic control and cardiovascular disease in 7,454 patients with type 1 diabetes: an observational study from the Swedish National Diabetes Register (NDR) Diabetes Care. 2010;33:1640–1646. doi: 10.2337/dc10-0398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81a.Soedamah-Muthu SS, Chaturvedi N, Witte DR, Stevens LK, Porta M, Fuller JH EURODIAB Prospective Complications Study Group. Relationship between risk factors and mortality in type 1 diabetic patients in Europe: the EURODIAB Prospective Complications Study (PCS) Diabetes Care. 2008;31:1360–1366. doi: 10.2337/dc08-0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Schutt M, Fach EM, Seufert J, Kerner W, Lang W, Zeyfang A, Welp R, Holl RW. DPV Initiative and the German BMBF Competence Network Diabetes Mellitus. Multiple complications and frequent severe hypoglycaemia in “elderly” and “old” patients with type 1 diabetes. Diabet Med. 2012;29:e176–e179. doi: 10.1111/j.1464-5491.2012.03681.x. [DOI] [PubMed] [Google Scholar]
11. Metabolic Syndrome
-
Metabolic syndrome is a multicomponent risk factor for CVD and type 2 DM that reflects the clustering of individual cardiometabolic risk factors related to abdominal obesity and insulin resistance. Although several different clinical definitions for metabolic syndrome have been proposed, the International Diabetes Federation, NHLBI, AHA, and others recently proposed a harmonized definition for metabolic syndrome.1 By this definition, metabolic syndrome is diagnosed when any 3 of the following 5 risk factors are present (most but not all people with DM will be classified as having metabolic syndrome by this definition because they will have ≥2 other factors besides the glucose criterion; many will prefer to separate those with DM into a separate group for risk stratification or treatment purposes):
Fasting plasma glucose ≥100 mg/dL or undergoing drug treatment for elevated glucose
HDL cholesterol <40 mg/dL in men or <50 mg/dL in women or undergoing drug treatment for reduced HDL cholesterol
Triglycerides ≥150 mg/dL or undergoing drug treatment for elevated triglycerides
Waist circumference >102 cm in men or >88 cm in women for people of most ancestries living in the United States. Ethnicity and country-specific thresholds can be used for diagnosis in other groups, particularly Asians and individuals of non-European ancestry who have predominantly resided outside the United States.
BP ≥130 mm Hg systolic or ≥85 mm Hg diastolic or undergoing drug treatment for hypertension or antihypertensive drug treatment in a patient with a history of hypertension.
Those with a fasting glucose level ≥126 mg/dL or a casual glucose value ≥200 mg/dL or taking hypoglycemic medication can normally be classified separately as having DM; many of these people will also have metabolic syndrome from the presence of additional risk factors noted above.
The new harmonized metabolic syndrome definition identifies a similar risk group and predicts CVD risk similarly to the prior metabolic syndrome definitions.2
There are many adverse health conditions that are related to metabolic syndrome but are not part of its clinical definition. These include nonalcoholic fatty liver disease, sexual dysfunction (erectile dysfunction in men and polycystic ovarian syndrome in women), and obstructive sleep apnea, as well as a general proinflammatory and pro-thrombotic state.3
Identification and treatment of metabolic syndrome fits closely with the current AHA 2020 Impact Goals, including emphasis on PA, healthy diet, and healthy weight for attainment of ideal BP, serum cholesterol, and fasting blood glucose. Metabolic syndrome should be considered largely a disease of unhealthy lifestyle. Prevalence of metabolic syndrome is a secondary metric in the 2020 Impact Goals. Identification of metabolic syndrome represents a call to action for the healthcare provider and patient to address the underlying lifestyle-related risk factors. A multidisciplinary team of healthcare professionals is desirable to adequately address these multiple issues in patients with metabolic syndrome.4
Abbreviations Used in Chapter 11
| AF | atrial fibrillation |
| AHA | American Heart Association |
| ARIC | Atherosclerosis Risk in Communities |
| BMI | body mass index |
| BP | blood pressure |
| CAC | coronary artery calcification |
| CAD | coronary artery disease |
| CHD | coronary heart disease |
| CI | confidence interval |
| COURAGE | Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation |
| CRP | C-reactive protein |
| CT | computed tomography |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| ECG | electrocardiogram |
| FRS | Framingham Risk Score |
| HDL | high-density lipoprotein |
| HF | heart failure |
| HIV | human immunodeficiency virus |
| HR | hazard ratio |
| IMT | intima-media thickness |
| LDL | low-density lipoprotein |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| MI | myocardial infarction |
| NCHS | National Center for Health Statistics |
| NHANES | National Health and Nutrition Examination Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| OR | odds ratio |
| PA | physical activity |
| PAR | population attributable risk |
| PCI | percutaneous coronary intervention |
| RR | relative risk |
| WHO | World Health Organization |
Prevalence
Adults
The following estimates include many of those who have DM, in addition to those with metabolic syndrome without DM:
Prevalence of metabolic syndrome varies by the definition used, with definitions such as that from the International Diabetes Federation and the harmonized definition suggesting lower thresholds for defining central obesity in European whites, Asians (in particular, South Asians), Middle Easterners, Sub-Saharan Africans, and Hispanics, which results in higher prevalence estimates.5
On the basis of NHANES 2003 to 2006 data and National Cholesterol Education Program/Adult Treatment Panel III guidelines, ≈34% of adults ≥20 years of age met the criteria for metabolic syndrome.6
-
Also based on NHANES 2003 to 2006 data6
The age-adjusted prevalence was 35.1% for men and 32.6% for women.
Among men, the age-specific prevalence ranged from 20.3% among people 20 to 39 years of age to 40.8% for people 40 to 59 years of age and 51.5% for people ≥60 years of age. Among women, the age-specific prevalence ranged from 15.6% among people 20 to 39 years of age to 37.2% for people 40 to 59 years of age and 54.4% for those ≥60 years of age.
The age-adjusted prevalences of people with metabolic syndrome were 37.2%, 25.3%, and 33.2% for non-Hispanic white, non-Hispanic black, and Mexican American men, respectively. Among women, the percentages were 31.5%, 38.8%, and 40.6%, respectively.
The age-adjusted prevalence was ≈53% higher among non-Hispanic black women than among non-Hispanic black men and ≈22% higher among Mexican American women than among Mexican American men.
The prevalence of metabolic syndrome is also high among immigrant Asian Indians, ranging between 26.8% and 38.2% depending on the definition used.7
Among American Indian and Alaska Native people living in the southwestern United States, the prevalence of metabolic syndrome was reported to be 43.2% in men and 47.3% in women; among Alaska Native people, prevalences were 26.5% and 31.2%, respectively.8
The prevalence of metabolic syndrome among pregnant women increased to 26.5% during 1999 to 2004 from 17.8% during 1988 to 1994.9
The prevalence of metabolic syndrome has been noted to be high among select special populations, including those taking atypical antipsychotic drugs,10 those receiving prior organ transplants,11 HIV-infected individuals,12 and individuals in select professions, including law enforcement13 and firefighters.14
There is a bidirectional relationship between metabolic syndrome and depression. In prospective studies, the presence of depression increases the risk of metabolic syndrome (OR, 1.49; 95% CI, 1.19–1.87), whereas metabolic syndrome increases the risk of depression (OR, 1.52; 95% CI, 1.20–1.91).15
Metabolic syndrome is becoming hyperendemic around the world. Recent evidence has described the prevalence of metabolic syndrome in Canada,16 Latin America,17 India,18 and China,19 as well as many other countries.
In the INTER-HEART case-control study of MI in 26 903 subjects from 52 countries, metabolic syndrome was present in 29.1% of case subjects and just 16.8% of control subjects. The age- and obesity-adjusted prevalence of metabolic syndrome was highest in cases among women (32.1%), South Asians (29.8%), and other Asians (28.7%).20
Despite its prevalence, the public’s recognition of metabolic syndrome is limited.21 A diagnosis of metabolic syndrome may increase risk perception and motivation toward a healthier behavior.22
Children/Adolescents
According to the 2009 AHA scientific statement about metabolic syndrome in children and adolescents, metabolic syndrome should be diagnosed with caution in this age group because metabolic syndrome categorization in adolescents is not stable.23 Approximately half of the 1098 adolescent participants in the Princeton School District Study diagnosed with pediatric Adult Treatment Panel III metabolic syndrome lost the diagnosis over 3 years of follow-up.24
Additional evidence of the instability of the diagnosis of metabolic syndrome in children exists. In children 6 to 17 years of age participating in research studies in a single clinical research hospital, the diagnosis of metabolic syndrome was unstable in 46% of cases after a mean of 5.6 years of follow-up.25
On the basis of NHANES 1999 to 2002 data, the prevalence of metabolic syndrome in adolescents 12 to 19 years of age was 9.4%, which represents ≈2.9 million people. It was 13.2% in boys, 5.3% in girls, 10.7% in whites, 5.2% in blacks, and 11.1% in Mexican Americans.26
In 1999 to 2004, ≈4.5% of US adolescents 12 to 17 years of age had metabolic syndrome according to the definition developed by the International Diabetes Federation.27 In 2006, this prevalence would have represented ≈1.1 million adolescents 12 to 17 years of age with metabolic syndrome. It increased from 1.2% among those 12 to 13 years of age to 7.1% among those 14 to 15 years of age and was higher among boys (6.7%) than girls (2.1%). Furthermore, 4.5% of white adolescents, 3.0% of black adolescents, and 7.1% of Mexican American adolescents had metabolic syndrome. The prevalence of metabolic syndrome remained relatively stable during successive 2-year periods: 4.5% for 1999 to 2000, 4.4% to 4.5% for 2001 to 2002, and 3.7% to 3.9% for 2003 to 2004.
Recent NHANES data among those aged 10 to 18 years in 2007 to 2008 showed an overall prevalence of metabolic syndrome of 3.9% in boys and 3.6% in girls, with the highest prevalence among Mexican Americans (7.6%) compared with African-Americans (2.1%) and whites (3.1%).28
In 1999 to 2002, among overweight or obese adolescents, 44% had metabolic syndrome.26 In 1988 to 1994, two thirds of all adolescents had ≥1 metabolic abnormality.29
Of 31 participants in the NHLBI Lipid Research Clinics Princeton Prevalence Study and the Princeton Follow-up Study who had metabolic syndrome at baseline, 21 (68%) had metabolic syndrome 25 years later.30 After adjustment for age, sex, and race, the baseline status of metabolic syndrome was significantly associated with an increased risk of having metabolic syndrome during adulthood (OR, 6.2; 95% CI, 2.8–13.8).
In the Bogalusa Heart Study, 4 variables (BMI, homeostasis model assessment of insulin resistance, ratio of triglycerides to HDL cholesterol, and mean arterial pressure) considered to be part of metabolic syndrome clustered together in blacks and whites and in children and adults.31 The degree of clustering was stronger among adults than among children. The clustering of rates of change in the components of metabolic syndrome in blacks exceeded that in whites. Cardiovascular abnormalities are associated with metabolic syndrome in children and adolescents.32,33
Risk
Adults
Consistent with 2 earlier meta-analyses, a recent meta-analysis of prospective studies concluded that metabolic syndrome increased the risk of developing CVD (summary RR, 1.78; 95% CI, 1.58–2.00).34 The risk of CVD tended to be higher in women (summary RR, 2.63) than in men (summary RR, 1.98; P=0.09). On the basis of results from 3 studies, metabolic syndrome remained a predictor of cardiovascular events after adjustment for the individual components of the syndrome (summary RR, 1.54; 95% CI, 1.32–1.79). A more recent meta-analysis among 87 studies comprising 951 083 subjects showed an even higher risk of CVD associated with metabolic syndrome (summary RR, 2.35; 95% CI, 2.02–2.73), with significant increased risks (RRs ranging from 1.6 to 2.9) for all-cause mortality, CVD mortality, MI, and stroke, as well as for those with metabolic syndrome without DM.35
In one of the earlier studies among US adults, mortality follow-up of the second NHANES showed a stepwise increase in risk of CHD, CVD, and total mortality across the spectrum of no disease, metabolic syndrome (without DM), DM, prior CVD, and those with CVD and DM, with an HR for CHD mortality of 2.02 (95% CI, 1.42–2.89) associated with metabolic syndrome. Increased risk was seen with increased numbers of metabolic syndrome risk factors.36
Several studies suggest that the FRS is a better predictor of incident CVD than metabolic syndrome.37–39 In the San Antonio Heart Study, the area under the receiver-operating characteristic curve was 0.816 for the FRS and 0.811 for the FRS plus metabolic syndrome.37 Furthermore, the sensitivity for CVD at a fixed specificity was significantly higher for the FRS than for metabolic syndrome. In ARIC, inclusion of metabolic syndrome did not improve the risk prediction achieved by the FRS.38 In the British Regional Heart Study, the area under the receiver-operating characteristic curve for the FRS was 0.73 for incident CHD during 10 years of follow-up, and the area under the receiver-operating characteristic curve for the number of metabolic syndrome components was 0.63.39 For CHD events during 20 years of follow-up, the areas under the receiver-operating characteristic curves were 0.68 for the FRS and 0.59 for the number of metabolic syndrome components.
Estimates of RR for CVD generally increase as the number of components of metabolic syndrome increases.39 Compared with men without an abnormal component in the Framingham Offspring Study, the HRs for CVD were 1.48 (95% CI, 0.69–3.16) for men with 1 or 2 components and 3.99 (95% CI, 1.89–8.41) for men with ≥3 components.40 Among women, the HRs were 3.39 (95% CI, 1.31–8.81) for 1 or 2 components and 5.95 (95% CI, 2.20–16.11) for ≥3 components. Compared with men without a metabolic abnormality in the British Regional Heart Study, the HRs were 1.74 (95% CI, 1.22–2.39) for 1 component, 2.34 (95% CI, 1.65–3.32) for 2 components, 2.88 (95% CI, 2.02–4.11) for 3 components, and 3.44 (95% CI, 2.35–5.03) for 4 or 5 components.39
The cardiovascular risk associated with metabolic syndrome varies on the basis of the combination of metabolic syndrome components present. Of all possible ways to have 3 metabolic syndrome components, the combination of central obesity, elevated BP, and hyperglycemia conferred the greatest risk for CVD (HR, 2.36; 95% CI, 1.54–3.61) and mortality (HR, 3.09; 95% CI, 1.93–4.94) in the Framingham Offspring Study.41
Data from the Aerobics Center Longitudinal Study indicate that risk for CVD mortality is increased in men without DM who have metabolic syndrome (HR, 1.8; 95% CI, 1.5–2.0); however, among those with metabolic syndrome, the presence of DM is associated with even greater risk for CVD mortality (HR, 2.1; 95% CI, 1.7–2.6).42 Analysis of data from NCHS was used to determine the number of disease-specific deaths attributable to all nonoptimal levels of each risk factor exposure by age and sex. The results of the analysis of dietary, lifestyle, and metabolic risk factors show that targeting a handful of risk factors has large potential to reduce mortality in the United States.43
Among stable CAD patients in the COURAGE trial, the presence of metabolic syndrome was associated with an increased risk of death or MI (unadjusted HR, 1.41; 95% CI, 1.15–1.73; P=0.001); however, after adjustment for its individual components, metabolic syndrome was no longer significantly associated with outcome (HR, 1.15; 95% CI, 0.79–1.68; P=0.46). Early PCI in addition to medical therapy did not significantly reduce the risk of death or MI regardless of metabolic syndrome or DM status.44
In the INTER-HEART case-control study of 26 903 subjects from 52 countries, metabolic syndrome was associated with an increased risk of MI, both according to the WHO (OR, 2.69; 95% CI, 2.45–2.95) and the International Diabetes Federation (OR, 2.20; 95% CI, 2.03–2.38) definitions, with a PAR of 14.5% (95% CI, 12.7%–16.3%) and 16.8% (95% CI, 14.8%–18.8%), respectively, and associations that were similar across all regions and ethnic groups. In addition, the presence of ≥3 risk factors with subthresh-old values was associated with increased risk of MI (OR, 1.50; 95% CI, 1.24–1.81) compared with having “normal” values. Similar results were observed when the International Diabetes Federation definition was used.20
In the Three-City Study, among 7612 participants aged ≥65 years who were followed up for 5.2 years, metabolic syndrome was associated with increased total CHD (HR, 1.78; 95% CI, 1.39–2.28) and fatal CHD (HR, 2.40; 95% CI, 1.41–4.09); however, metabolic syndrome was not associated with CHD beyond its individual risk components.45
In MESA, among 6603 people aged 45 to 84 years (1686 [25%] with metabolic syndrome without DM and 881 [13%] with DM), subclinical atherosclerosis assessed by CAC was more severe in people with metabolic syndrome and DM than in those without these conditions, and the extent of CAC was a strong predictor of CHD and CVD events in these groups.46 Furthermore, the progression of CAC was greater in people with metabolic syndrome and DM than in those without, and progression of CAC predicted future CVD event risk both in those with metabolic syndrome and in those with DM.47,48
In addition to CVD, metabolic syndrome has been associated with incident AF49 and HF.50
So-called metabolically benign obesity without metabolic syndrome is associated with similar all-cause mortality to lean individuals.51
Metabolic syndrome is associated with increased healthcare use and healthcare-related costs among individuals with and without DM. Overall, healthcare costs increase by ≈24% for each additional metabolic syndrome component present.52
Children
Few prospective pediatric studies have examined the future risk for CVD or DM according to baseline metabolic syndrome status. Data from 771 participants 6 to 19 years of age from the NHLBI’s Lipid Research Clinics Princeton Prevalence Study and the Princeton Follow-up Study showed that the risk of developing CVD was substantially higher among those with metabolic syndrome than among those without this syndrome (OR, 14.6; 95% CI, 4.8–45.3) who were followed up for 25 years.30
Another analysis of 814 participants in this cohort showed that those 5 to 19 years of age who had metabolic syndrome at baseline had an increased risk of having DM 25 to 30 years later compared with those who did not have the syndrome at baseline (OR, 11.5; 95% CI, 2.1–63.7).53
Additional data from the Princeton Follow-up Study, the Fels Longitudinal Study, and the Muscatine Study suggest that the absence of components of metabolic syndrome in childhood has a high negative predictive value for the development of metabolic syndrome or DM in adulthood.54
In a study of 6328 subjects from 4 prospective studies, compared with people with normal BMI as children and as adults, those with consistently high adiposity from childhood to adulthood had an increased risk of the following metabolic syndrome components: hypertension (RR, 2.7; 95% CI, 2.2–3.3), low HDL (RR, 2.1; 95% CI, 1.8–2.5), elevated triglycerides (RR, 3.0; 95% CI, 2.4–3.8), type 2 DM (RR, 5.4; 95% CI, 3.4–8.5), and increased carotid IMT (RR, 1.7; 95% CI, 1.4–2.2). Those who were overweight or obese during childhood but were not obese as adults had no increased risk compared with those with consistently normal BMI.55
In 1757 youths from the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study, those with metabolic syndrome in youth and adulthood were at 3.4 times increased risk of high carotid IMT and 12.2 times increased risk of type 2 DM in adulthood as those without metabolic syndrome at either time. Adults whose metabolic syndrome had resolved after their youth were at no increased risk of having high IMT or type 2 DM.56
Risk Factors
Risk of metabolic syndrome probably begins before birth. The Prediction of Metabolic Syndrome in Adolescence Study showed that the coexistence of low birth weight, small head circumference, and parental history of overweight or obesity places children at the highest risk for metabolic syndrome in adolescence. Other risk factors identified included parental history of DM, gestational hypertension in the mother, and lack of breastfeeding.57
In prospective or retrospective cohort studies, the following factors have been reported as being directly associated with incident metabolic syndrome, defined by one of the major definitions: age,35,37–39 low educational attainment,58,59 low socioeconomic status,60 smoking,59–62 parental smoking,63 low levels of PA,59–62, 64–66 low levels of physical fitness,64,67–70 intake of soft drinks,71 intake of diet soda,72 magnesium intake,73 energy intake,66 carbohydrate intake,58,61,74 total fat intake,37,53 Western dietary pattern,72 meat intake,72 intake of fried foods,72 skipping breakfast,70 heavy alcohol consumption,75 abstention from alcohol use,58 parental history of DM,53 long-term stress at work,76 pediatric metabolic syndrome,53 obesity or BMI,37,38,42,46,56 childhood obesity,77 waist circumference,74,78–82 intra-abdominal fat,83 gain in weight or BMI,37,63 change in weight or BMI,61,78,84 weight fluctuation,85 BP,74,78,81,86 heart rate,87 homeostasis model assessment,79,88 fasting insulin,79 2-hour insulin,79 proinsulin,79 fasting glucose or hyperglycemia,39,58,60 2-hour glucose,79 impaired glucose tolerance,79 triglycerides,74,78–81,89 low HDL cholesterol,74,77–79,81 oxidized LDL,88 uric acid,84,90 γ-glutamyltransferase,84,91,92 alanine transaminase,84,91,93,94 plasminogen activator inhibitor-1,95 aldosterone,95 leptin,96 CRP,97,98 adipocyte–fatty acid binding protein,99 free testosterone index,100 active periodontitis,101 and urinary bisphenol A levels.102
The following factors have been reported as being inversely associated with incident metabolic syndrome, defined by one of the major definitions, in prospective or retrospective cohort studies: muscular strength,103 change in PA or physical fitness,61,67 aerobic training,104 alcohol intake,40,46 Mediterranean diet,105 dairy consumption,72 vitamin D intake,106 intake of tree nuts,107 insulin sensitivity,79 ratio of aspartate aminotransferase to alanine transaminase,93 total testosterone,79,82,83 serum 25-hydroxyvitamin D,108 sex hormone–binding globulin,79,82,83 and Δ5-desaturase activity.109
In the Data From the Epidemiological Study on the Insulin Resistance Syndrome cohort, metabolic syndrome was associated with an unfavorable hemodynamic profile, including increased brachial central pulse pressure and increase pulse pressure amplification, compared with similar individuals with isolated hypertension but without metabolic syndrome.110 In MESA, metabolic syndrome was associated with major and minor ECG abnormalities, although this varied by sex.111
Individuals with metabolic syndrome have a higher degree of endothelial dysfunction than individuals with a similar burden of traditional cardiovascular risk factors.112 Metabolic syndrome is associated with increased thrombosis, including increased resistance to aspirin.113
In modern imaging studies using echocardiography, magnetic resonance imaging, cardiac CT, and positron emission tomography, metabolic syndrome has been shown to be closely related to increased epicardial adipose tissues,114 increased visceral fat in other locations,115 high-risk coronary plaque features including increased necrotic core,116 impaired coronary flow reserve,117 and left ventricular diastolic dysfunction.118
Men are more likely than women to develop metabolic syndrome,58,78 and blacks have been shown to be less likely to develop metabolic syndrome than whites.58
In >6 years of follow-up in the ARIC Study, 1970 individuals (25%) developed metabolic syndrome, and compared with the normal-weight group (BMI <25 kg/m2), the ORs of developing metabolic syndrome were 2.81 (95% CI, 2.50–3.17) and 5.24 (95% CI, 4.50–6.12) for the overweight (BMI 25–30 kg/m2) and obese (BMI ≥30 kg/m2) groups, respectively. Compared with the lowest quartile of leisure-time PA, the ORs of developing metabolic syndrome were 0.80 (95% CI, 0.71–0.91) and 0.92 (95% CI, 0.81–1.04) for people in the highest and middle quartiles, respectively.119
- 1.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC, Jr International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 2.Hari P, Nerusu K, Veeranna V, Sudhakar R, Zalawadiya S, Ramesh K, Afonso L. A gender-stratified comparative analysis of various definitions of metabolic syndrome and cardiovascular risk in a multiethnic U.S. population. Metab Syndr Relat Disord. 2012;10:47–55. doi: 10.1089/met.2011.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tota-Maharaj R, Defilippis AP, Blumenthal RS, Blaha MJ. A practical approach to the metabolic syndrome: review of current concepts and management. Curr Opin Cardiol. 2010;25:502–512. doi: 10.1097/HCO.0b013e32833cd474. [DOI] [PubMed] [Google Scholar]
- 4.Bagge E, Bjelle A, Edén S, Svanborg A. A longitudinal study of the occurrence of joint complaints in elderly people. Age Ageing. 1992;21:160–167. doi: 10.1093/ageing/21.3.160. [DOI] [PubMed] [Google Scholar]
- 5.Brown TM, Voeks JH, Bittner V, Safford MM. Variations in prevalent cardiovascular disease and future risk by metabolic syndrome classification in the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Am Heart J. 2010;159:385–391. doi: 10.1016/j.ahj.2009.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Natl Health Stat Report. 2009;(13):1–7. [PubMed] [Google Scholar]
- 7.Misra R, Patel T, Kotha P, Raji A, Ganda O, Banerji M, Shah V, Vijay K, Mudaliar S, Iyer D, Balasubramanyam A. Prevalence of diabetes, metabolic syndrome, and cardiovascular risk factors in US Asian Indians: results from a national study. J Diabetes Complications. 2010;24:145–153. doi: 10.1016/j.jdiacomp.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Schumacher C, Ferucci ED, Lanier AP, Slattery ML, Schraer CD, Raymer TW, Dillard D, Murtaugh MA, Tom-Orme L. Metabolic syndrome: prevalence among American Indian and Alaska native people living in the southwestern United States and in Alaska. Metab Syndr Relat Disord. 2008;6:267–273. doi: 10.1089/met.2008.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramos RG, Olden K. The prevalence of metabolic syndrome among US women of childbearing age. Am J Public Health. 2008;98:1122–1127. doi: 10.2105/AJPH.2007.120055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pramyothin P, Khaodhiar L. Metabolic syndrome with the atypical anti-psychotics. Curr Opin Endocrinol Diabetes Obes. 2010;17:460–466. doi: 10.1097/MED.0b013e32833de61c. [DOI] [PubMed] [Google Scholar]
- 11.Sorice GP, Di Pizio L, Sun VA, Schirò T, Muscogiuri G, Mezza T, Cefalo CM, Prioletta A, Pontecorvi A, Giaccari A. Metabolic syndrome in transplant patients: an updating point of view. Minerva Endocrinol. 2012;37:211–220. [PubMed] [Google Scholar]
- 12.van Wijk JP, Cabezas MC. Hypertriglyceridemia, metabolic syndrome, and cardiovascular disease in HIV-infected patients: effects of antiretroviral therapy and adipose tissue distribution. Int J Vasc Med. 2012;2012:201027. doi: 10.1155/2012/201027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zimmerman FH. Cardiovascular disease and risk factors in law enforcement personnel: a comprehensive review. Cardiol Rev. 2012;20:159–166. doi: 10.1097/CRD.0b013e318248d631. [DOI] [PubMed] [Google Scholar]
- 14.Donovan R, Nelson T, Peel J, Lipsey T, Voyles W, Israel RG. Cardiorespiratory fitness and the metabolic syndrome in firefighters. Occup Med (Lond) 2009;59:487–492. doi: 10.1093/occmed/kqp095. [DOI] [PubMed] [Google Scholar]
- 15.Pan A, Keum N, Okereke OI, Sun Q, Kivimaki M, Rubin RR, Hu FB. Bidirectional association between depression and metabolic syndrome: a systematic review and meta-analysis of epidemiological studies. Diabetes Care. 2012;35:1171–1180. doi: 10.2337/dc11-2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leiter LA, Fitchett DH, Gilbert RE, Gupta M, Mancini GB, McFarlane PA, Ross R, Teoh H, Verma S, Anand S, Camelon K, Chow CM, Cox JL, Després JP, Genest J, Harris SB, Lau DC, Lewanczuk R, Liu PP, Lonn EM, McPherson R, Poirier P, Qaadri S, Rabasa-Lhoret R, Rabkin SW, Sharma AM, Steele AW, Stone JA, Tardif JC, Tobe S, Ur E Cardiometabolic Risk Working Group: Executive Committee. Cardiometabolic risk in Canada: a detailed analysis and position paper by the Cardiometabolic Risk Working Group. Can J Cardiol. 2011;27:e1–e33. doi: 10.1016/j.cjca.2010.12.054. [DOI] [PubMed] [Google Scholar]
- 17.López-Jaramillo P, Sánchez RA, Diaz M, Cobos L, Bryce A, Parra Carrillo JZ, Lizcano F, Lanas F, Sinay I, Sierra ID, Peñaherrera E, Bendersky M, Schmid H, Botero R, Urina M, Lara J, Foss MC, Márquez G, Harrap S, Ramírez AJ, Zanchetti A Latin America Expert Group. Latin American consensus on hypertension in patients with diabetes type 2 and metabolic syndrome. J Hypertens. 2013;31:223–238. doi: 10.1097/HJH.0b013e32835c5444. [DOI] [PubMed] [Google Scholar]
- 18.Sawant A, Mankeshwar R, Shah S, Raghavan R, Dhongde G, Raje H, D’souza S, Subramanium A, Dhairyawan P, Todur S, Ashavaid TF. Prevalence of metabolic syndrome in urban India. Cholesterol. 2011;2011:920983. doi: 10.1155/2011/920983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shen J, Goyal A, Sperling L. The emerging epidemic of obesity, diabetes, and the metabolic syndrome in China. Cardiol Res Pract. 2012;2012:178675. doi: 10.1155/2012/178675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mente A, Yusuf S, Islam S, McQueen MJ, Tanomsup S, Onen CL, Rangarajan S, Gerstein HC, Anand SS INTERHEART Investigators. Metabolic syndrome and risk of acute myocardial infarction a case-control study of 26,903 subjects from 52 countries. J Am Coll Cardiol. 2010;55:2390–2398. doi: 10.1016/j.jacc.2009.12.053. [DOI] [PubMed] [Google Scholar]
- 21.Lewis SJ, Rodbard HW, Fox KM, Grandy S SHIELD Study Group. Self-reported prevalence and awareness of metabolic syndrome: findings from SHIELD. Int J Clin Pract. 2008;62:1168–1176. doi: 10.1111/j.1742-1241.2008.01770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jumean MF, Korenfeld Y, Somers VK, Vickers KS, Thomas RJ, Lopez-Jimenez F. Impact of diagnosing metabolic syndrome on risk perception. Am J Health Behav. 2012;36:522–532. doi: 10.5993/AJHB.36.4.9. [DOI] [PubMed] [Google Scholar]
- 23.Steinberger J, Daniels SR, Eckel RH, Hayman L, Lustig RH, McCrindle B, Mietus-Snyder ML. Progress and challenges in metabolic syndrome in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2009;119:628–647. doi: 10.1161/CIRCULATIONAHA.108.191394. [DOI] [PubMed] [Google Scholar]
- 24.Goodman E, Daniels SR, Meigs JB, Dolan LM. Instability in the diagnosis of metabolic syndrome in adolescents. Circulation. 2007;115:2316–2322. doi: 10.1161/CIRCULATIONAHA.106.669994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gustafson JK, Yanoff LB, Easter BD, Brady SM, Keil MF, Roberts MD, Sebring NG, Han JC, Yanovski SZ, Hubbard VS, Yanovski JA. The stability of metabolic syndrome in children and adolescents. J Clin Endocrinol Metab. 2009;94:4828–4834. doi: 10.1210/jc.2008-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cook S, Auinger P, Li C, Ford ES. Metabolic syndrome rates in United States adolescents, from the National Health and Nutrition Examination Survey, 1999–2002. J Pediatr. 2008;152:165–170. doi: 10.1016/j.jpeds.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Ford ES, Li C, Zhao G, Pearson WS, Mokdad AH. Prevalence of the metabolic syndrome among U.S. adolescents using the definition from the International Diabetes Federation. Diabetes Care. 2008;31:587–589. doi: 10.2337/dc07-1030. [DOI] [PubMed] [Google Scholar]
- 28.Basson SL, Luo Y, Li A, Perez A, Wong ND. Prevalence and trends in metabolic syndrome and associated cardiovascular risk factors among US adolescents between 1999 and 2008. Cardiovasc Endocrinol. 2013;2:23–30. [Google Scholar]
- 29.de Ferranti SD, Gauvreau K, Ludwig DS, Neufeld EJ, Newburger JW, Rifai N. Prevalence of the metabolic syndrome in American adolescents: findings from the Third National Health and Nutrition Examination Survey. Cir culation. 2004;110:2494–2497. doi: 10.1161/01.CIR.0000145117.40114.C7. [DOI] [PubMed] [Google Scholar]
- 30.Morrison JA, Friedman LA, Gray-McGuire C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: the Princeton Lipid Research Clinics Follow-up Study. Pediatrics. 2007;120:340–345. doi: 10.1542/peds.2006-1699. [DOI] [PubMed] [Google Scholar]
- 31.Chen W, Srinivasan SR, Li S, Xu J, Berenson GS. Clustering of long-term trends in metabolic syndrome variables from childhood to adulthood in Blacks and Whites: the Bogalusa Heart Study. Am J Epidemiol. 2007;166:527–533. doi: 10.1093/aje/kwm105. [DOI] [PubMed] [Google Scholar]
- 32.Chinali M, de Simone G, Roman MJ, Best LG, Lee ET, Russell M, Howard BV, Devereux RB. Cardiac markers of pre-clinical disease in adolescents with the metabolic syndrome: the Strong Heart Study. J Am Coll Cardiol. 2008;52:932–938. doi: 10.1016/j.jacc.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Toledo-Corral CM, Ventura EE, Hodis HN, Weigensberg MJ, Lane CJ, Li Y, Goran MI. Persistence of the metabolic syndrome and its influence on carotid artery intima media thickness in overweight Latino children. Atherosclerosis. 2009;206:594–598. doi: 10.1016/j.atherosclerosis.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–414. doi: 10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 35.Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, Rinfret S, Schiffrin EL, Eisenberg MJ. The metabolic syndrome and cardiovascular risk: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56:1113–1132. doi: 10.1016/j.jacc.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 36.Malik S, Wong ND, Franklin SS, Kamath TV, L’Italien GJ, Pio JR, Williams GR. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004;110:1245–1250. doi: 10.1161/01.CIR.0000140677.20606.0E. [DOI] [PubMed] [Google Scholar]
- 37.Stern MP, Williams K, González-Villalpando C, Hunt KJ, Haffner SM. Does the metabolic syndrome improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease? [published correction appears in Diabetes Care 2005;28:238] Diabetes Care. 2004;27:2676–2681. doi: 10.2337/diacare.27.11.2676. [DOI] [PubMed] [Google Scholar]
- 38.McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, Ballantyne CM, Heiss G. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the Atherosclerosis Risk in Communities study. Diabetes Care. 2005;28:385–390. doi: 10.2337/diacare.28.2.385. [DOI] [PubMed] [Google Scholar]
- 39.Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med. 2005;165:2644–2650. doi: 10.1001/archinte.165.22.2644. [DOI] [PubMed] [Google Scholar]
- 40.Wilson PW, D’Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–3072. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- 41.Franco OH, Massaro JM, Civil J, Cobain MR, O’Malley B, D’Agostino RB., Sr Trajectories of entering the metabolic syndrome: the Framingham Heart Study. Circulation. 2009;120:1943–1950. doi: 10.1161/CIRCULATIONAHA.109.855817. [DOI] [PubMed] [Google Scholar]
- 42.Church TS, Thompson AM, Katzmarzyk PT, Sui X, Johannsen N, Earnest CP, Blair SN. Metabolic syndrome and diabetes, alone and in combination, as predictors of cardiovascular disease mortality among men. Diabetes Care. 2009;32:1289–1294. doi: 10.2337/dc08-1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors [published correction appears in PLoS Med. 2011;8(1). doi:10.1371/annotation/0ef47acd-9dcc-4296-a897-872d182cde57.] PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maron DJ, Boden WE, Spertus JA, Hartigan PM, Mancini GB, Sedlis SP, Kostuk WJ, Chaitman BR, Shaw LJ, Berman DS, Dada M, Teo KK, Weintraub WS, O’Rourke RA COURAGE Trial Research Group. Impact of metabolic syndrome and diabetes on prognosis and outcomes with early percutaneous coronary intervention in the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial. J Am Coll Cardiol. 2011;58:131–137. doi: 10.1016/j.jacc.2011.02.046. [DOI] [PubMed] [Google Scholar]
- 45.Rachas A, Raffaitin C, Barberger-Gateau P, Helmer C, Ritchie K, Tzourio C, Amouyel P, Ducimetière P, Empana JP. Clinical usefulness of the metabolic syndrome for the risk of coronary heart disease does not exceed the sum of its individual components in older men and women: the Three-City (3C) Study. Heart. 2012;98:650–655. doi: 10.1136/heartjnl-2011-301185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Malik S, Budoff MJ, Katz R, Blumenthal RS, Bertoni AG, Nasir K, Szklo M, Barr RG, Wong ND. Impact of subclinical atherosclerosis on cardiovascular disease events in individuals with metabolic syndrome and diabetes: the Multi-Ethnic Study of Atherosclerosis. Diabetes Care. 2011;34:2285–2290. doi: 10.2337/dc11-0816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wong ND, Nelson JC, Granston T, Bertoni AG, Blumenthal RS, Carr JJ, Guerci A, Jacobs DR, Jr, Kronmal R, Liu K, Saad M, Selvin E, Tracy R, Detrano R. Metabolic syndrome, diabetes, and incidence and progression of coronary calcium: the Multiethnic Study of Atherosclerosis study. JACC Cardiovasc Imaging. 2012;5:358–366. doi: 10.1016/j.jcmg.2011.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Blaha MJ, DeFilippis AP, Rivera JJ, Budoff MJ, Blankstein R, Agatston A, Szklo M, Lakoski SG, Bertoni AG, Kronmal RA, Blumenthal RS, Nasir K. The relationship between insulin resistance and incidence and progression of coronary artery calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Diabetes Care. 2011;34:749–751. doi: 10.2337/dc10-1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chamberlain AM, Agarwal SK, Ambrose M, Folsom AR, Soliman EZ, Alonso A. Metabolic syndrome and incidence of atrial fibrillation among blacks and whites in the Atherosclerosis Risk in Communities (ARIC) Study. Am Heart J. 2010;159:850–856. doi: 10.1016/j.ahj.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Horwich TB, Fonarow GC. Glucose, obesity, metabolic syndrome, and diabetes relevance to incidence of heart failure. J Am Coll Cardiol. 2010;55:283–293. doi: 10.1016/j.jacc.2009.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Durward CM, Hartman TJ, Nickols-Richardson SM. All-cause mortality risk of metabolically healthy obese individuals in NHANES III. J Obes. 2012;2012:460321. doi: 10.1155/2012/460321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boudreau DM, Malone DC, Raebel MA, Fishman PA, Nichols GA, Feldstein AC, Boscoe AN, Ben-Joseph RH, Magid DJ, Okamoto LJ. Health care utilization and costs by metabolic syndrome risk factors. Metab Syndr Relat Disord. 2009;7:305–314. doi: 10.1089/met.2008.0070. [DOI] [PubMed] [Google Scholar]
- 53.Morrison JA, Friedman LA, Wang P, Glueck CJ. Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. J Pediatr. 2008;152:201–206. doi: 10.1016/j.jpeds.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 54.Schubert CM, Sun SS, Burns TL, Morrison JA, Huang TT. Predictive ability of childhood metabolic components for adult metabolic syndrome and type 2 diabetes. J Pediatr. 2009;155:S6.e1–S6.e7. doi: 10.1016/j.jpeds.2009.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Sun C, Cheung M, Viikari JS, Dwyer T, Raitakari OT. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876–1885. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- 56.Magnussen CG, Koskinen J, Juonala M, Chen W, Srinivasan SR, Sabin MA, Thomson R, Schmidt MD, Nguyen QM, Xu JH, Skilton MR, Kähönen M, Laitinen T, Taittonen L, Lehtimäki T, Rönnemaa T, Viikari JS, Berenson GS, Raitakari OT. A diagnosis of the metabolic syndrome in youth that resolves by adult life is associated with a normalization of high carotid intima-media thickness and type 2 diabetes mellitus risk: the Bogalusa Heart and Cardiovascular Risk in Young Finns studies. J Am Coll Cardiol. 2012;60:1631–1639. doi: 10.1016/j.jacc.2012.05.056. [DOI] [PubMed] [Google Scholar]
- 57.Efstathiou SP, Skeva II, Zorbala E, Georgiou E, Mountokalakis TD. Metabolic syndrome in adolescence: can it be predicted from natal and parental profile? The Prediction of Metabolic Syndrome in Adolescence (PREMA) study. Circulation. 2012;125:902–910. doi: 10.1161/CIRCULATIONAHA.111.034546. [DOI] [PubMed] [Google Scholar]
- 58.Carnethon MR, Loria CM, Hill JO, Sidney S, Savage PJ, Liu K Coronary Artery Risk Development in Young Adults study. Risk factors for the metabolic syndrome: the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985–2001. Diabetes Care. 2004;27:2707–2715. doi: 10.2337/diacare.27.11.2707. [DOI] [PubMed] [Google Scholar]
- 59.Wilsgaard T, Jacobsen BK. Lifestyle factors and incident metabolic syndrome: the Tromsø Study 1979–2001. Diabetes Res Clin Pract. 2007;78:217–224. doi: 10.1016/j.diabres.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 60.Chichlowska KL, Rose KM, Diez-Roux AV, Golden SH, McNeill AM, Heiss G. Life course socioeconomic conditions and metabolic syndrome in adults: the Atherosclerosis Risk in Communities (ARIC) Study. Ann Epidemiol. 2009;19:875–883. doi: 10.1016/j.annepidem.2009.07.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wannamethee SG, Shaper AG, Whincup PH. Modifiable lifestyle factors and the metabolic syndrome in older men: effects of lifestyle changes. J Am Geriatr Soc. 2006;54:1909–1914. doi: 10.1111/j.1532-5415.2006.00974.x. [DOI] [PubMed] [Google Scholar]
- 62.Holme I, Tonstad S, Sogaard AJ, Larsen PG, Haheim LL. Leisure time physical activity in middle age predicts the metabolic syndrome in old age: results of a 28-year follow-up of men in the Oslo study. BMC Public Health. 2007;7:154. doi: 10.1186/1471-2458-7-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Juonala M, Magnussen CG, Venn A, Gall S, Kähönen M, Laitinen T, Taittonen L, Lehtimäki T, Jokinen E, Sun C, Viikari JS, Dwyer T, Raitakari OT. Parental smoking in childhood and brachial artery flow-mediated dilatation in young adults: the Cardiovascular Risk in Young Finns study and the Childhood Determinants of Adult Health study. Arterioscler Thromb Vasc Biol. 2012;32:1024–1031. doi: 10.1161/ATVBAHA.111.243261. [DOI] [PubMed] [Google Scholar]
- 64.Laaksonen DE, Lakka HM, Salonen JT, Niskanen LK, Rauramaa R, Lakka TA. Low levels of leisure-time physical activity and cardiorespiratory fitness predict development of the metabolic syndrome. Diabetes Care. 2002;25:1612–1618. doi: 10.2337/diacare.25.9.1612. [DOI] [PubMed] [Google Scholar]
- 65.Ekelund U, Brage S, Franks PW, Hennings S, Emms S, Wareham NJ. Physical activity energy expenditure predicts progression toward the metabolic syndrome independently of aerobic fitness in middle-aged healthy Caucasians: the Medical Research Council Ely Study. Diabetes Care. 2005;28:1195–1200. doi: 10.2337/diacare.28.5.1195. [DOI] [PubMed] [Google Scholar]
- 66.Ferreira I, Twisk JW, van Mechelen W, Kemper HC, Stehouwer CD. Development of fatness, fitness, and lifestyle from adolescence to the age of 36 years: determinants of the metabolic syndrome in young adults: the Amsterdam Growth and Health Longitudinal Study. Arch Intern Med. 2005;165:42–48. doi: 10.1001/archinte.165.1.42. [DOI] [PubMed] [Google Scholar]
- 67.Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Jr, Liu K. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA. 2003;290:3092–3100. doi: 10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- 68.LaMonte MJ, Barlow CE, Jurca R, Kampert JB, Church TS, Blair SN. Cardiorespiratory fitness is inversely associated with the incidence of metabolic syndrome: a prospective study of men and women. Circulation. 2005;112:505–512. doi: 10.1161/CIRCULATIONAHA.104.503805. [DOI] [PubMed] [Google Scholar]
- 69.Ferreira I, Henry RM, Twisk JW, van Mechelen W, Kemper HC, Stehouwer CD Amsterdam Growth and Health Longitudinal Study. The metabolic syndrome, cardiopulmonary fitness, and subcutaneous trunk fat as independent determinants of arterial stiffness: the Amsterdam Growth and Health Longitudinal Study. Arch Intern Med. 2005;165:875–882. doi: 10.1001/archinte.165.8.875. [DOI] [PubMed] [Google Scholar]
- 70.Edwardson CL, Gorely T, Davies MJ, Gray LJ, Khunti K, Wilmot EG, Yates T, Biddle SJ. Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PLoS One. 2012;7:e34916. doi: 10.1371/journal.pone.0034916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs JB, D’Agostino RB, Gaziano JM, Vasan RS. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community [published correction appears in Circulation. 2007;116:e557] Circulation. 2007;116:480–488. doi: 10.1161/CIRCULATIONAHA.107.689935. [DOI] [PubMed] [Google Scholar]
- 72.Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation. 2008;117:754–761. doi: 10.1161/CIRCULATIONAHA.107.716159. [DOI] [PubMed] [Google Scholar]
- 73.He K, Liu K, Daviglus ML, Morris SJ, Loria CM, Van Horn L, Jacobs DR, Jr, Savage PJ. Magnesium intake and incidence of metabolic syndrome among young adults. Circulation. 2006;113:1675–1682. doi: 10.1161/CIRCULATIONAHA.105.588327. [DOI] [PubMed] [Google Scholar]
- 74.Mirmiran P, Noori N, Azizi F. A prospective study of determinants of the metabolic syndrome in adults. Nutr Metab Cardiovasc Dis. 2008;18:567–573. doi: 10.1016/j.numecd.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 75.Baik I, Shin C. Prospective study of alcohol consumption and metabolic syndrome. Am J Clin Nutr. 2008;87:1455–1463. doi: 10.1093/ajcn/87.5.1455. [DOI] [PubMed] [Google Scholar]
- 76.Chandola T, Brunner E, Marmot M. Chronic stress at work and the metabolic syndrome: prospective study. BMJ. 2006;332:521–525. doi: 10.1136/bmj.38693.435301.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sun SS, Liang R, Huang TT, Daniels SR, Arslanian S, Liu K, Grave GD, Siervogel RM. Childhood obesity predicts adult metabolic syndrome: the Fels Longitudinal Study. J Pediatr. 2008;152:191–200. doi: 10.1016/j.jpeds.2007.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cheung BM, Wat NM, Tam S, Thomas GN, Leung GM, Cheng CH, Woo J, Janus ED, Lau CP, Lam TH, Lam KS. Components of the metabolic syndrome predictive of its development: a 6-year longitudinal study in Hong Kong Chinese. Clin Endocrinol (Oxf) 2008;68:730–737. doi: 10.1111/j.1365-2265.2007.03110.x. [DOI] [PubMed] [Google Scholar]
- 79.Palaniappan L, Carnethon MR, Wang Y, Hanley AJ, Fortmann SP, Haffner SM, Wagenknecht L Insulin Resistance Atherosclerosis Study. Predictors of the incident metabolic syndrome in adults: the Insulin Resistance Atherosclerosis Study. Diabetes Care. 2004;27:788–793. doi: 10.2337/diacare.27.3.788. [DOI] [PubMed] [Google Scholar]
- 80.Morrison JA, Friedman LA, Harlan WR, Harlan LC, Barton BA, Schreiber GB, Klein DJ. Development of the metabolic syndrome in black and white adolescent girls: a longitudinal assessment. Pediatrics. 2005;116:1178–1182. doi: 10.1542/peds.2004-2358. [DOI] [PubMed] [Google Scholar]
- 81.Sheu WH, Chuang SY, Lee WJ, Tsai ST, Chou P, Chen CH. Predictors of incident diabetes, metabolic syndrome in middle-aged adults: a 10-year follow-up study from Kinmen, Taiwan. Diabetes Res Clin Pract. 2006;74:162–168. doi: 10.1016/j.diabres.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 82.Onat A, Uyarel H, Hergenç G, Karabulut A, Albayrak S, Can G. Determinants and definition of abdominal obesity as related to risk of diabetes, metabolic syndrome and coronary disease in Turkish men: a prospective cohort study. Atherosclerosis. 2007;191:182–190. doi: 10.1016/j.atherosclerosis.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 83.Tong J, Boyko EJ, Utzschneider KM, McNeely MJ, Hayashi T, Carr DB, Wallace TM, Zraika S, Gerchman F, Leonetti DL, Fujimoto WY, Kahn SE. Intra-abdominal fat accumulation predicts the development of the metabolic syndrome in non-diabetic Japanese-Americans. Diabetologia. 2007;50:1156–1160. doi: 10.1007/s00125-007-0651-y. [DOI] [PubMed] [Google Scholar]
- 84.Ryu S, Song J, Choi BY, Lee SJ, Kim WS, Chang Y, Kim DI, Suh BS, Sung KC. Incidence and risk factors for metabolic syndrome in Korean male workers, ages 30 to 39. Ann Epidemiol. 2007;17:245–252. doi: 10.1016/j.annepidem.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 85.Vergnaud AC, Bertrais S, Oppert JM, Maillard-Teyssier L, Galan P, Hercberg S, Czernichow S. Weight fluctuations and risk for metabolic syndrome in an adult cohort. Int J Obes (Lond) 2008;32:315–321. doi: 10.1038/sj.ijo.0803739. [DOI] [PubMed] [Google Scholar]
- 86.Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119:237–246. doi: 10.1542/peds.2006-2543. [DOI] [PubMed] [Google Scholar]
- 87.Tomiyama H, Yamada J, Koji Y, Yambe M, Motobe K, Shiina K, Yamamoto Y, Yamashina A. Heart rate elevation precedes the development of metabolic syndrome in Japanese men: a prospective study. Hypertens Res. 2007;30:417–426. doi: 10.1291/hypres.30.417. [DOI] [PubMed] [Google Scholar]
- 88.Holvoet P, Lee DH, Steffes M, Gross M, Jacobs DR., Jr Association between circulating oxidized low-density lipoprotein and incidence of the metabolic syndrome. JAMA. 2008;299:2287–2293. doi: 10.1001/jama.299.19.2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lim HS, Lip GY, Beevers DG, Blann AD. Factors predicting the development of metabolic syndrome and type II diabetes against a background of hypertension. Eur J Clin Invest. 2005;35:324–329. doi: 10.1111/j.1365-2362.2005.01495.x. [DOI] [PubMed] [Google Scholar]
- 90.Sui X, Church TS, Meriwether RA, Lobelo F, Blair SN. Uric acid and the development of metabolic syndrome in women and men. Metab Clin Exp. 2008;57:845–852. doi: 10.1016/j.metabol.2008.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.André P, Balkau B, Vol S, Charles MA, Eschwège E DESIR Study Group. Gamma-glutamyltransferase activity and development of the metabolic syndrome (International Diabetes Federation definition) in middle-aged men and women: Data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR) cohort. Diabetes Care. 2007;30:2355–2361. doi: 10.2337/dc07-0440. [DOI] [PubMed] [Google Scholar]
- 92.Lee DS, Evans JC, Robins SJ, Wilson PW, Albano I, Fox CS, Wang TJ, Benjamin EJ, D’Agostino RB, Vasan RS. Gamma glutamyl transferase and metabolic syndrome, cardiovascular disease, and mortality risk: the Framingham Heart Study. Arterioscler Thromb Vasc Biol. 2007;27:127–133. doi: 10.1161/01.ATV.0000251993.20372.40. [DOI] [PubMed] [Google Scholar]
- 93.Hanley AJ, Williams K, Festa A, Wagenknecht LE, D’Agostino RB, Jr, Haffner SM. Liver markers and development of the metabolic syndrome: the Insulin Resistance Atherosclerosis Study. Diabetes. 2005;54:3140–3147. doi: 10.2337/diabetes.54.11.3140. [DOI] [PubMed] [Google Scholar]
- 94.Schindhelm RK, Dekker JM, Nijpels G, Stehouwer CD, Bouter LM, Heine RJ, Diamant M. Alanine aminotransferase and the 6-year risk of the metabolic syndrome in Caucasian men and women: the Hoorn Study. Diabet Med. 2007;24:430–435. doi: 10.1111/j.1464-5491.2007.02100.x. [DOI] [PubMed] [Google Scholar]
- 95.Ingelsson E, Pencina MJ, Tofler GH, Benjamin EJ, Lanier KJ, Jacques PF, Fox CS, Meigs JB, Levy D, Larson MG, Selhub J, D’Agostino RB, Sr, Wang TJ, Vasan RS. Multimarker approach to evaluate the incidence of the metabolic syndrome and longitudinal changes in metabolic risk factors: the Framingham Offspring Study. Circulation. 2007;116:984–992. doi: 10.1161/CIRCULATIONAHA.107.708537. [DOI] [PubMed] [Google Scholar]
- 96.Galletti F, Barbato A, Versiero M, Iacone R, Russo O, Barba G, Siani A, Cappuccio FP, Farinaro E, della Valle E, Strazzullo P. Circulating leptin levels predict the development of metabolic syndrome in middle-aged men: an 8-year follow-up study. J Hypertens. 2007;25:1671–1677. doi: 10.1097/HJH.0b013e3281afa09e. [DOI] [PubMed] [Google Scholar]
- 97.Laaksonen DE, Niskanen L, Nyyssönen K, Punnonen K, Tuomainen TP, Valkonen VP, Salonen R, Salonen JT. C-reactive protein and the development of the metabolic syndrome and diabetes in middle-aged men. Diabetologia. 2004;47:1403–1410. doi: 10.1007/s00125-004-1472-x. [DOI] [PubMed] [Google Scholar]
- 98.Hassinen M, Lakka TA, Komulainen P, Gylling H, Nissinen A, Rauramaa R. C-reactive protein and metabolic syndrome in elderly women: a 12-year follow-up study. Diabetes Care. 2006;29:931–932. doi: 10.2337/diacare.29.04.06.dc05-2508. [DOI] [PubMed] [Google Scholar]
- 99.Xu A, Tso AW, Cheung BM, Wang Y, Wat NM, Fong CH, Yeung DC, Janus ED, Sham PC, Lam KS. Circulating adipocyte-fatty acid binding protein levels predict the development of the metabolic syndrome: a 5-year prospective study. Circulation. 2007;115:1537–1543. doi: 10.1161/CIRCULATIONAHA.106.647503. [DOI] [PubMed] [Google Scholar]
- 100.Rodriguez A, Muller DC, Metter EJ, Maggio M, Harman SM, Blackman MR, Andres R. Aging, androgens, and the metabolic syndrome in a longitudinal study of aging. J Clin Endocrinol Metab. 2007;92:3568–3572. doi: 10.1210/jc.2006-2764. [DOI] [PubMed] [Google Scholar]
- 101.Nibali L, Tatarakis N, Needleman I, Tu YK, D’Aiuto F, Rizzo M, Donos N. Clinical review: association between metabolic syndrome and periodontitis: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2013;98:913–920. doi: 10.1210/jc.2012-3552. [DOI] [PubMed] [Google Scholar]
- 102.Teppala S, Madhavan S, Shankar A. Bisphenol A and metabolic syndrome: results from NHANES. Int J Endocrinol. 2012;2012:598180. doi: 10.1155/2012/598180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Jurca R, Lamonte MJ, Barlow CE, Kampert JB, Church TS, Blair SN. Association of muscular strength with incidence of metabolic syndrome in men. Med Sci Sports Exerc. 2005;37:1849–1855. doi: 10.1249/01.mss.0000175865.17614.74. [DOI] [PubMed] [Google Scholar]
- 104.Bateman LA, Slentz CA, Willis LH, Shields AT, Piner LW, Bales CW, Houmard JA, Kraus WE. Comparison of aerobic versus resistance exercise training effects on metabolic syndrome (from the Studies of a Targeted Risk Reduction Intervention Through Defined Exercise: STRRIDE-AT/RT) Am J Cardiol. 2011;108:838–844. doi: 10.1016/j.amjcard.2011.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tortosa A, Bes-Rastrollo M, Sanchez-Villegas A, Basterra-Gortari FJ, Nuñez-Cordoba JM, Martinez-Gonzalez MA. Mediterranean diet inversely associated with the incidence of metabolic syndrome: the SUN prospective cohort. Diabetes Care. 2007;30:2957–2959. doi: 10.2337/dc07-1231. [DOI] [PubMed] [Google Scholar]
- 106.Maki KC, Fulgoni VL, 3rd, Keast DR, Rains TM, Park KM, Rubin MR. Vitamin D intake and status are associated with lower prevalence of metabolic syndrome in U.S. adults: National Health and Nutrition Examination Surveys 2003–2006. Metab Syndr Relat Disord. 2012;10:363–372. doi: 10.1089/met.2012.0020. [DOI] [PubMed] [Google Scholar]
- 107.O’Neil CE, Keast DR, Nicklas TA, Fulgoni VL., 3rd Nut consumption is associated with decreased health risk factors for cardiovascular disease and metabolic syndrome in U.S. adults: NHANES 1999–2004. J Am Coll Nutr. 2011;30:502–510. doi: 10.1080/07315724.2011.10719996. [DOI] [PubMed] [Google Scholar]
- 108.Chacko SA, Song Y, Manson JE, Van Horn L, Eaton C, Martin LW, Mc-Tiernan A, Curb JD, Wylie-Rosett J, Phillips LS, Plodkowski RA, Liu S. Serum 25-hydroxyvitamin D concentrations in relation to cardiometa-bolic risk factors and metabolic syndrome in postmenopausal women. Am J Clin Nutr. 2011;94:209–217. doi: 10.3945/ajcn.110.010272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Warensjö E, Risérus U, Vessby B. Fatty acid composition of serum lipids predicts the development of the metabolic syndrome in men. Diabetologia. 2005;48:1999–2005. doi: 10.1007/s00125-005-1897-x. [DOI] [PubMed] [Google Scholar]
- 110.Safar ME, Balkau B, Lange C, Protogerou AD, Czernichow S, Blacher J, Levy BI, Smulyan H. Hypertension and vascular dynamics in men and women with metabolic syndrome. J Am Coll Cardiol. 2013;61:12–19. doi: 10.1016/j.jacc.2012.01.088. [DOI] [PubMed] [Google Scholar]
- 111.Ebong IA, Bertoni AG, Soliman EZ, Guo M, Sibley CT, Chen YD, Rotter JI, Chen YC, Goff DC., Jr Electrocardiographic abnormalities associated with the metabolic syndrome and its components: the Multi-Ethnic Study of Atherosclerosis. Metab Syndr Relat Disord. 2012;10:92–97. doi: 10.1089/met.2011.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Li J, Flammer AJ, Lennon RJ, Nelson RE, Gulati R, Friedman PA, Thomas RJ, Sandhu NP, Hua Q, Lerman LO, Lerman A. Comparison of the effect of the metabolic syndrome and multiple traditional cardiovascular risk factors on vascular function. Mayo Clin Proc. 2012;87:968–975. doi: 10.1016/j.mayocp.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Smith JP, Haddad EV, Taylor MB, Oram D, Blakemore D, Chen Q, Boutaud O, Oates JA. Suboptimal inhibition of platelet cyclooxygenase-1 by aspirin in metabolic syndrome. Hypertension. 2012;59:719–725. doi: 10.1161/HYPERTENSIONAHA.111.181404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pierdomenico SD, Pierdomenico AM, Cuccurullo F, Iacobellis G. Meta-analysis of the relation of echocardiographic epicardial adipose tissue thickness and the metabolic syndrome. Am J Cardiol. 2013;111:73–78. doi: 10.1016/j.amjcard.2012.08.044. [DOI] [PubMed] [Google Scholar]
- 115.van der Meer RW, Lamb HJ, Smit JW, de Roos A. MR imaging evaluation of cardiovascular risk in metabolic syndrome. Radiology. 2012;264:21–37. doi: 10.1148/radiol.12110772. [DOI] [PubMed] [Google Scholar]
- 116.Marso SP, Mercado N, Maehara A, Weisz G, Mintz GS, McPherson J, Schiele F, Dudek D, Fahy M, Xu K, Lansky A, Templin B, Zhang Z, de Bruyne B, Serruys PW, Stone GW. Plaque composition and clinical outcomes in acute coronary syndrome patients with metabolic syndrome or diabetes. JACC Cardiovasc Imaging. 2012;5(suppl):S42–S52. doi: 10.1016/j.jcmg.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 117.Di Carli MF, Charytan D, McMahon GT, Ganz P, Dorbala S, Schelbert HR. Coronary circulatory function in patients with the metabolic syndrome. J Nucl Med. 2011;52:1369–1377. doi: 10.2967/jnumed.110.082883. [DOI] [PubMed] [Google Scholar]
- 118.Dinh W, Lankisch M, Nickl W, Gies M, Scheyer D, Kramer F, Scheffold T, Krahns T, Sause A, Füth R. Metabolic syndrome with or without diabetes contributes to left ventricular diastolic dysfunction. Acta Cardiol. 2011;66:167–174. doi: 10.1080/ac.66.2.2071247. [DOI] [PubMed] [Google Scholar]
- 119.Cheriyath P, Duan Y, Qian Z, Nambiar L, Liao D. Obesity, physical activity and the development of metabolic syndrome: the Atherosclerosis Risk in Communities study. Eur J Cardiovasc Prev Rehabil. 2010;17:309–313. doi: 10.1097/HJR.0b013e32833189b8. [DOI] [PubMed] [Google Scholar]
12. Chronic Kidney Disease
ICD-10 N18.0. See Tables 12-1 through 12-3.
Table 12-1.
BP and the Adjusted Risk of ESRD Among 316 675 Adults Without Evidence of Baseline Kidney Disease
| JNC V BP Category | Adjusted RR (95% CI) |
|---|---|
| Optimal | 1.00 (Reference) |
| Normal, not optimal | 1.62 (1.27–2.07) |
| High normal | 1.98 (1.55–2.52) |
| Hypertension | |
| Stage 1 | 2.59 (2.07–3.25) |
| Stage 2 | 3.86 (3.00–4.96) |
| Stage 3 | 3.88 (2.82–5.34) |
| Stage 4 | 4.25 (2.63–6.86) |
BP indicates blood pressure; CI, confidence interval; ESRD, end-stage renal disease; JNC V, fifth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; and RR, relative risk.
Table 12-3.
Adjusted HR for Death of Any Cause, Cardiovascular Events, and Hospitalization Among 1 120 295 Ambulatory Adults, According to eGFR*
| eGFR, mL·min−1·1.73 m−2 | Adjusted HR (95% CI)
|
||
|---|---|---|---|
| Death of Any Cause | Any Cardiovascular Event | Any Hospitalization | |
| ≥60† | 1.00 | 1.00 | 1.00 |
| 45–59 | 1.2 (1.1–1.2) | 1.4 (1.4–1.5) | 1.1 (1.1–1.1) |
| 30–44 | 1.8 (1.7–1.9) | 2.0 (1.9–2.1) | 1.5 (1.5–1.5) |
| 15–29 | 3.2 (3.1–3.4) | 2.8 (2.6–2.9) | 2.1 (2.0–2.2) |
| <15 | 5.9 (5.4–6.5) | 3.4 (3.1–3.8) | 3.1 (3.0–3.3) |
CI indicates confidence interval; eGFR, estimated glomerular filtration rate; and HR, hazard ratio.
The analyses were adjusted for age, sex, income, education, use or nonuse of dialysis, and presence or absence of prior coronary heart disease, prior chronic heart failure, prior ischemic stroke or transient ischemic attack, prior peripheral arterial disease, diabetes mellitus, hypertension, dyslipidemia, a serum albumin level of ≤3.5 g/dL, dementia, cirrhosis or chronic liver disease, chronic lung disease, documented proteinuria, and prior hospitalizations.
This group served as the reference group.
End-stage Renal Disease
Prevalence, Incidence, and Risk
(See Tables 12-1 and 12-2.)
Table 12-2.
Multivariable Association Between BMI and Risk of ESRD Among 320 252 Adults
| BMI, kg/m2 | Adjusted RR (95% CI) |
|---|---|
| 18.5–24.9 (Normal weight) | 1.00 (Reference) |
| 25.0–29.9 (Overweight) | 1.87 (1.64–2.14) |
| 30.0–34.9 (Class I obesity) | 3.57 (3.05–4.18) |
| 35.0–39.9 (Class II obesity) | 6.12 (4.97–7.54) |
| ≥40.0 (Extreme obesity) | 7.07 (5.37–9.31) |
BMI indicates body mass index; CI, confidence interval; ESRD, end-stage renal disease; and RR, relative risk.
ESRD is a condition that is most commonly associated with DM or HBP, occurs when the kidneys are functioning at a very low level, and is currently defined as the receipt of chronic renal replacement treatment such as hemodialysis, peritoneal dialysis, or kidney transplantation. The ESRD population is increasing in size and cost as those with CKD transition to ESRD and as a result of changing practice patterns in the United States.
Data from the 2010 annual report of the United States Renal Data System showed that in 2008, the prevalence of ESRD was 547 982, with 70% of these prevalent cases being treated with hemodialysis.1
In 2008, 112 476 new cases of ESRD were reported.1
In 2008, 17 413 kidney transplants were performed.1
Data from a large cohort of insured patients showed that in addition to established risk factors for ESRD, lower hemoglobin levels, higher serum uric acid levels, self-reported history of nocturia, and family history of kidney disease are independent risk factors for ESRD.2
Data from a large insured population revealed that among adults with a GFR >60 mL·min−1·1.73 m−2 and no evidence of proteinuria or hematuria at baseline, risks for ESRD increased dramatically with higher baseline BP level, and in this same patient population, BP-associated risks were greater in men than in women and in blacks than in whites.3
Compared with white patients with similar levels of kidney function, black patients are much more likely to progress to ESRD and are on average 10 years younger when they reach ESRD.4,5
Results from a large community-based population showed that higher BMI also independently increased the risk of ESRD. The higher risk of ESRD with overweight and obesity was consistent across age, sex, and race and in the presence or absence of DM, hypertension, or known baseline kidney disease.6
Abbreviations Used in Chapter 12
| ACTION | Acute Coronary Treatment and Intervention Outcomes Network |
| AF | atrial fibrillation |
| AMI | acute myocardial infarction |
| BMI | body mass index |
| BP | blood pressure |
| CHD | coronary heart disease |
| CHF | congestive heart failure |
| CI | confidence interval |
| CKD | chronic kidney disease |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| eGFR | estimated glomerular filtration rate |
| ESRD | end-stage renal disease |
| GFR | glomerular filtration rate |
| HBP | high blood pressure |
| HF | heart failure |
| HR | hazard ratio |
| ICD-10 | International Classification of Diseases, 10th Revision |
| JNC V | fifth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure |
| MI | myocardial infarction |
| NCHS | National Center for Health Statistics |
| NHANES | National Health and Nutrition Examination Survey |
| PAD | peripheral arterial disease |
| RR | relative risk |
Age, Sex, Race, and Ethnicity
The median age of the population with ESRD in 2008 varied across different racial/ethnic groups: 57.4 years for blacks, 58.0 years for Native Americans, 59.3 years for Asians, and 60.6 years for whites.1
Treatment of ESRD is more common in men than in women.1
Blacks, Hispanics, Asian Americans, and Native Americans have significantly higher rates of ESRD than do whites/Europeans. Blacks represent nearly 32% of treated patients with ESRD.1
Chronic Kidney Disease
Prevalence
CKD, defined as reduced GFR, excess urinary protein excretion, or both, is a serious health condition and a worldwide public health problem. The incidence and prevalence of CKD are increasing in the United States and are associated with poor outcomes and a high cost to the US healthcare system. Controversy exists about whether CKD itself independently causes incident CVD, but it is clear that people with CKD, as well as those with ESRD, represent a population at very high risk for CVD events. In fact, individuals with CKD are more likely to die of CVD than to transition to ESRD. The United States Renal Data System estimates that by 2020, >700 000 Americans will have ESRD, with >500 000 requiring dialysis and >250 000 receiving a transplant.
The National Kidney Foundation Kidney Disease Outcome Quality Initiative developed guidelines in 2002 that provided a standardized definition for CKD. Prevalence estimates may differ depending on assumptions used in obtaining estimates, including which equation is used to estimate GFR and methods for measuring proteinuria.7
-
The most recent US prevalence estimates of CKD come from NHANES 1988 to 1994 and 1999 to 2004 (NCHS) in adults ≥20 years of age.8
The prevalence of CKD in 1999 to 2004 (stages 1 to 5)9 was 13.1%. This represents an increase from the 10.0% prevalence estimate from NHANES 1988 to 1994 (NCHS).
The prevalence of stage 1 CKD (eGFR ≥90 mL·min−1· 1.73 m−2 with kidney damage, ie, presence of albuminuria) is 1.8%.
The prevalence of stage 2 CKD (eGFR 60–89 mL·min−1·1.73 m−2 with kidney damage) is 3.2%.
The prevalence of stage 3 CKD (eGFR 30–59 mL·min−1·1.73 m−2) is 7.7%.
The prevalence of stages 4 and 5 CKD (eGFR <29 mL·min−1·1.73 m−2) is 0.4%.
More than 26 million people (13%) in the United States have CKD, and most are undiagnosed.8 Another 20 million are at increased risk for CKD.10
Demographics
-
According to current definitions, the prevalence of CKD was higher with older age,1 as follows:
6.0% for those 20 to 39 years of age
11.6% for those 40 to 59 years of age
38.8% for those ≥60 years of age
CKD prevalence was greater among those with DM (43.8%) and hypertension (29.4%) than among those without these chronic conditions.1
The prevalence of CKD was slightly higher among Mexican Americans (18.7%) and non-Hispanic blacks (19.9%) than among non-Hispanic whites (16.1%). This disparity was most evident for those with stage 1 CKD; non-Hispanic whites had a CKD prevalence of 4.2% compared with prevalences among Mexican Americans and non-Hispanic blacks of 10.2% and 9.4%, respectively.11
Risk Factors
Many traditional CVD risk factors are also risk factors for CKD, including older age, male sex, hypertension, DM, smoking, and family history of CVD.
-
Recent evidence suggests that BMI is associated with worsening CKD.
In a cohort of 652 African American individuals with hypertensive nephrosclerosis, BMI was independently associated with urine total protein and albumin excretion.12
In addition, both the degree of CKD (ie, eGFR) and urine albumin are strongly associated with the progression from CKD to ESRD. Furthermore, urine albumin level is associated with progression to CKD across all levels of reduced eGFR.13
Other risk factors include systemic conditions such as auto-immune diseases, systemic infections, and drug exposure, as well as anatomically local conditions such as urinary tract infections, urinary stones, lower urinary tract obstruction, and neoplasia. Even after adjustment for these risk factors, excess CVD risk remains.14
ESRD/CKD and CVD
(See Table 12-3.)
-
CVD is the leading cause of death among those with ESRD, although the specific cardiovascular cause of death may be more likely to be arrhythmic than an AMI, end-stage HF, or stroke. CVD mortality is 5 to 30 times higher in dialysis patients than in subjects from the general population of the same age, sex, and race.15,16
Studies from a broad range of cohorts demonstrate an association between reduced eGFR and elevated risk of CVD, CVD outcomes, and all-cause death17,20–25 that appears to be largely independent of other known major CVD risk factors.
Although clinical practice guidelines recommend management of mineral and bone disorders secondary to CKD, a recent meta-analysis suggests that there is no consistent association between calcium and parathyroid hormone and the risk of death or cardiovascular events.26
Any degree of albuminuria, starting below the micro-albuminuria cut point, has been shown to be an independent risk factor for cardiovascular events, CHF hospitalization, PAD, and all-cause death in a wide variety of cohorts.27–32
-
A recent meta-analysis of 21 published studies of albuminuria involving 105 872 participants (730 577 person-years) from 14 studies with urine albumin/creatinine ratio measurements and 1 128 310 participants (4 732 110 person-years) from 7 studies with urine dipstick measurements showed that excess albuminuria or proteinuria is independently associated with a higher risk of CVD and all-cause mortality.33
People with both albuminuria/proteinuria and reduced eGFR are at particularly high risk for CVD, CVD outcomes, and death.34
The exact reasons why CKD and ESRD increase the risk of CVD have not been completely delineated but are clearly multifactorial and likely involve pathological alterations in multiple organ systems and pathways.
One potential explanation for the higher CVD event rate in patients with CKD is the low uptake of standard therapies for patients presenting with MI. In a recent analysis from the ACTION registry, patients presenting with CKD had a substantially higher mortality rate. In addition, patients with CKD were less likely to receive standard therapies for the treatment of MI.35
Cost: ESRD
The total annual cost of treating ESRD in the United States was $26.8 billion in 2008, which represents nearly 6% of the total Medicare budget.1
The total annual cost associated with CKD has not been determined accurately to date.
Cystatin C: Kidney Function and CVD
Serum cystatin C, another marker of kidney function, has been proposed to be a more sensitive indicator of kidney function than serum creatinine and creatinine-based estimating formulas at higher levels of GFR. It is a low-molecular-weight protein produced at a constant rate by all nucleated cells and appears not to be affected significantly across age, sex, and levels of muscle mass. Cystatin C is excreted by the kidneys, filtered through the glomerulus, and nearly completely reabsorbed by proximal tubular cells.36 Several equations have been proposed using cystatin C alone and in combination with serum creatinine to estimate kidney function.37,38
All-Cause Mortality
Elevated levels of cystatin C have been shown to be associated with increased risk for all-cause mortality in studies from a broad range of cohorts.39–41
-
In addition to GFR and urine albumin-to-creatinine ratio, cystatin C provides incremental information for the prediction of ESRD and mortality.
In a recent analysis of 26 643 US adults, the addition of cystatin C to the combination of creatinine and albumin-to-creatinine ratio resulted in a significant improvement in the prediction of both all-cause mortality and the development of ESRD.42
Cardiovascular Disease
Data from a large national cohort found higher values of cystatin C to be associated with prevalent stroke, angina, and MI,43 as well as higher BMI.44
Elevated cystatin C was an independent risk factor for HF,45,46 PAD events,47 clinical atherosclerosis, and subclinical measures of CVD in older adults,48 as well as for cardiovascular events among those with CHD.39,49
In several diverse cohorts, elevated cystatin C has been found to be associated with CVD-related mortality,41,50,51 including sudden cardiac death.52
In a recent clinical trial of 9270 patients with CKD, the effect of lipid-lowering therapy with simvastatin plus ezetimibe was associated with a lower risk for major atherosclerotic events compared with placebo.53
- 1.United States Renal Data System. USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2010. [Accessed July 26, 2011]. http://www.usrds.org/atlas10.aspx. [Google Scholar]
- 2.Hsu CY, Iribarren C, McCulloch CE, Darbinian J, Go AS. Risk factors for end-stage renal disease: 25-year follow-up. Arch Intern Med. 2009;169:342–350. doi: 10.1001/archinternmed.2008.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsu CY, McCulloch CE, Darbinian J, Go AS, Iribarren C. Elevated blood pressure and risk of end-stage renal disease in subjects without baseline kidney disease. Arch Intern Med. 2005;165:923–928. doi: 10.1001/archinte.165.8.923. [DOI] [PubMed] [Google Scholar]
- 4.Hsu CY, Lin F, Vittinghoff E, Shlipak MG. Racial differences in the progression from chronic renal insufficiency to end-stage renal disease in the United States. J Am Soc Nephrol. 2003;14:2902–2907. doi: 10.1097/01.asn.0000091586.46532.b4. [DOI] [PubMed] [Google Scholar]
- 5.Choi AI, Rodriguez RA, Bacchetti P, Bertenthal D, Hernandez GT, O’Hare AM. White/black racial differences in risk of end-stage renal disease and death. Am J Med. 2009;122:672–678. doi: 10.1016/j.amjmed.2008.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hsu CY, McCulloch CE, Iribarren C, Darbinian J, Go AS. Body mass index and risk for end-stage renal disease. Ann Intern Med. 2006;144:21–28. doi: 10.7326/0003-4819-144-1-200601030-00006. [DOI] [PubMed] [Google Scholar]
- 7.Snyder JJ, Foley RN, Collins AJ. Prevalence of CKD in the United States: a sensitivity analysis using the National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Kidney Dis. 2009;53:218–228. doi: 10.1053/j.ajkd.2008.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 9.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G National Kidney Foundation. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification [published correction appears in Ann Intern Med. 2003;139:605] Ann Intern Med. 2003;139:137–147. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Hospitalization discharge diagnoses for kidney disease: United States, 1980–2005. MMWR Morb Mortal Wkly Rep. 2008;57:309–312. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC) Prevalence of chronic kidney disease and associated risk factors: United States, 1999–2004. MMWR Morb Mortal Wkly Rep. 2007;56:161–165. [PubMed] [Google Scholar]
- 12.Toto RD, Greene T, Hebert LA, Hiremath L, Lea JP, Lewis JB, Pogue V, Sika M, Wang X AASK Collaborative Research Group. Relationship between body mass index and proteinuria in hypertensive nephrosclerosis: results from the African American Study of Kidney Disease and Hypertension (AASK) cohort. Am J Kidney Dis. 2010;56:896–906. doi: 10.1053/j.ajkd.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hallan SI, Ritz E, Lydersen S, Romundstad S, Kvenild K, Orth SR. Combining GFR and albuminuria to classify CKD improves prediction of ESRD. J Am Soc Nephrol. 2009;20:1069–1077. doi: 10.1681/ASN.2008070730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coresh J, Astor B, Sarnak MJ. Evidence for increased cardiovascular disease risk in patients with chronic kidney disease. Curr Opin Nephrol Hypertens. 2004;13:73–81. doi: 10.1097/00041552-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Sarnak MJ, Coronado BE, Greene T, Wang SR, Kusek JW, Beck GJ, Levey AS. Cardiovascular disease risk factors in chronic renal insufficiency. Clin Nephrol. 2002;57:327–335. doi: 10.5414/cnp57327. [DOI] [PubMed] [Google Scholar]
- 16.Weiner DE, Tabatabai S, Tighiouart H, Elsayed E, Bansal N, Griffith J, Salem DN, Levey AS, Sarnak MJ. Cardiovascular outcomes and all-cause mortality: exploring the interaction between CKD and cardiovascular disease. Am J Kidney Dis. 2006;48:392–401. doi: 10.1053/j.ajkd.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 17.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization [published correction appears in N Engl J Med. 2008;18:4] N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 18.Weiner DE, Tighiouart H, Stark PC, Amin MG, MacLeod B, Griffith JL, Salem DN, Levey AS, Sarnak MJ. Kidney disease as a risk factor for recurrent cardiovascular disease and mortality. Am J Kidney Dis. 2004;44:198–206. doi: 10.1053/j.ajkd.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 19.Alonso A, Lopez FL, Matsushita K, Loehr LR, Agarwal SK, Chen LY, Soliman EZ, Astor BC, Coresh J. Chronic kidney disease is associated with the incidence of atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2011;123:2946–2953. doi: 10.1161/CIRCULATIONAHA.111.020982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: the HOPE randomized trial. Ann Intern Med. 2001;134:629–636. doi: 10.7326/0003-4819-134-8-200104170-00007. [DOI] [PubMed] [Google Scholar]
- 21.Fried LF, Shlipak MG, Crump C, Bleyer AJ, Gottdiener JS, Kronmal RA, Kuller LH, Newman AB. Renal insufficiency as a predictor of cardiovascular outcomes and mortality in elderly individuals. J Am Coll Cardiol. 2003;41:1364–1372. doi: 10.1016/s0735-1097(03)00163-3. [DOI] [PubMed] [Google Scholar]
- 22.Shlipak MG, Fried LF, Cushman M, Manolio TA, Peterson D, Stehman-Breen C, Bleyer A, Newman A, Siscovick D, Psaty B. Cardiovascular mortality risk in chronic kidney disease: comparison of traditional and novel risk factors. JAMA. 2005;293:1737–1745. doi: 10.1001/jama.293.14.1737. [DOI] [PubMed] [Google Scholar]
- 23.Ruilope LM, Salvetti A, Jamerson K, Hansson L, Warnold I, Wedel H, Zanchetti A. Renal function and intensive lowering of blood pressure in hypertensive participants of the Hypertension Optimal Treatment (HOT) study. J Am Soc Nephrol. 2001;12:218–225. doi: 10.1681/ASN.V122218. [DOI] [PubMed] [Google Scholar]
- 24.Manjunath G, Tighiouart H, Ibrahim H, MacLeod B, Salem DN, Griffith JL, Coresh J, Levey AS, Sarnak MJ. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol. 2003;41:47–55. doi: 10.1016/s0735-1097(02)02663-3. [DOI] [PubMed] [Google Scholar]
- 25.Hailpern SM, Cohen HW, Alderman MH. Renal dysfunction and ischemic heart disease mortality in a hypertensive population. J Hypertens. 2005;23:1809–1816. doi: 10.1097/01.hjh.0000183120.92455.2a. [DOI] [PubMed] [Google Scholar]
- 26.Palmer SC, Hayen A, Macaskill P, Pellegrini F, Craig JC, Elder GJ, Strippoli GF. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: a systematic review and meta-analysis. JAMA. 2011;305:1119–1127. doi: 10.1001/jama.2011.308. [DOI] [PubMed] [Google Scholar]
- 27.Arnlöv J, Evans JC, Meigs JB, Wang TJ, Fox CS, Levy D, Benjamin EJ, D’Agostino RB, Vasan RS. Low-grade albuminuria and incidence of cardiovascular disease events in nonhypertensive and nondiabetic individuals: the Framingham Heart Study. Circulation. 2005;112:969–975. doi: 10.1161/CIRCULATIONAHA.105.538132. [DOI] [PubMed] [Google Scholar]
- 28.Klausen K, Borch-Johnsen K, Feldt-Rasmussen B, Jensen G, Clausen P, Scharling H, Appleyard M, Jensen JS. Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation. 2004;110:32–35. doi: 10.1161/01.CIR.0000133312.96477.48. [DOI] [PubMed] [Google Scholar]
- 29.Gerstein HC, Mann JF, Yi Q, Zinman B, Dinneen SF, Hoogwerf B, Hallé JP, Young J, Rashkow A, Joyce C, Nawaz S, Yusuf S HOPE Study Investigators. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001;286:421–426. doi: 10.1001/jama.286.4.421. [DOI] [PubMed] [Google Scholar]
- 30.Yuyun MF, Adler AI, Wareham NJ. What is the evidence that microalbuminuria is a predictor of cardiovascular disease events? Curr Opin Nephrol Hypertens. 2005;14:271–276. doi: 10.1097/01.mnh.0000165895.90748.3b. [DOI] [PubMed] [Google Scholar]
- 31.Wattanakit K, Folsom AR, Criqui MH, Kramer HJ, Cushman M, Shea S, Hirsch AT. Albuminuria and peripheral arterial disease: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Atherosclerosis. 2008;201:212–216. doi: 10.1016/j.atherosclerosis.2007.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brantsma AH, Bakker SJ, Hillege HL, de Zeeuw D, de Jong PE, Gansevoort RT PREVEND Study Group. Cardiovascular and renal outcome in subjects with K/DOQI stage 1–3 chronic kidney disease: the importance of urinary albumin excretion. Nephrol Dial Transplant. 2008;23:3851–3858. doi: 10.1093/ndt/gfn356. [DOI] [PubMed] [Google Scholar]
- 33.Chronic Kidney Disease Consortium. Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Gansevoort RT. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375:2073–2081. doi: 10.1016/S0140-6736(10)60674-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hemmelgarn BR, Manns BJ, Lloyd A, James MT, Klarenbach S, Quinn RR, Wiebe N, Tonelli M Alberta Kidney Disease Network. Relation between kidney function, proteinuria, and adverse outcomes. JAMA. 2010;303:423–429. doi: 10.1001/jama.2010.39. [DOI] [PubMed] [Google Scholar]
- 35.Fox CS, Muntner P, Chen AY, Alexander KP, Roe MT, Cannon CP, Saucedo JF, Kontos MC, Wiviott SD Acute Coronary Treatment and Intervention Outcomes Network registry. Use of evidence-based therapies in short-term outcomes of ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction in patients with chronic kidney disease: a report from the National Cardiovascular Data Acute Coronary Treatment and Intervention Outcomes Network registry. Circulation. 2010;121:357–365. doi: 10.1161/CIRCULATIONAHA.109.865352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Filler G, Bökenkamp A, Hofmann W, Le Bricon T, Martínez-Brú C, Grubb A. Cystatin C as a marker of GFR: history, indications, and future research. Clin Biochem. 2005;38:1–8. doi: 10.1016/j.clinbiochem.2004.09.025. [DOI] [PubMed] [Google Scholar]
- 37.Stevens LA, Coresh J, Schmid CH, Feldman HI, Froissart M, Kusek J, Rossert J, Van Lente F, Bruce RD, 3rd, Zhang YL, Greene T, Levey AS. Estimating GFR using serum cystatin C alone and in combination with serum creatinine: a pooled analysis of 3,418 individuals with CKD. Am J Kidney Dis. 2008;51:395–406. doi: 10.1053/j.ajkd.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20:629–637. doi: 10.1681/ASN.2008030287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ix JH, Shlipak MG, Chertow GM, Whooley MA. Association of cystatin C with mortality, cardiovascular events, and incident heart failure among persons with coronary heart disease: data from the Heart and Soul Study. Circulation. 2007;115:173–179. doi: 10.1161/CIRCULATIONAHA.106.644286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fried LF, Katz R, Sarnak MJ, Shlipak MG, Chaves PH, Jenny NS, Stehman-Breen C, Gillen D, Bleyer AJ, Hirsch C, Siscovick D, Newman AB. Kidney function as a predictor of noncardiovascular mortality. J Am Soc Nephrol. 2005;16:3728–3735. doi: 10.1681/ASN.2005040384. [DOI] [PubMed] [Google Scholar]
- 41.Shlipak MG, Wassel Fyr CL, Chertow GM, Harris TB, Kritchevsky SB, Tylavsky FA, Satterfield S, Cummings SR, Newman AB, Fried LF. Cystatin C and mortality risk in the elderly: the Health, Aging, and Body Composition study. J Am Soc Nephrol. 2006;17:254–261. doi: 10.1681/ASN.2005050545. [DOI] [PubMed] [Google Scholar]
- 42.Peralta CA, Shlipak MG, Judd S, Cushman M, McClellan W, Zakai NA, Safford MM, Zhang X, Muntner P, Warnock D. Detection of chronic kidney disease with creatinine, cystatin C, and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality. JAMA. 2011;305:1545–1552. doi: 10.1001/jama.2011.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Muntner P, Mann D, Winston J, Bansilal S, Farkouh ME. Serum cystatin C and increased coronary heart disease prevalence in US adults without chronic kidney disease. Am J Cardiol. 2008;102:54–57. doi: 10.1016/j.amjcard.2008.02.098. [DOI] [PubMed] [Google Scholar]
- 44.Muntner P, Winston J, Uribarri J, Mann D, Fox CS. Overweight, obesity, and elevated serum cystatin C levels in adults in the United States. Am J Med. 2008;121:341–348. doi: 10.1016/j.amjmed.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Djoussé L, Kurth T, Gaziano JM. Cystatin C and risk of heart failure in the Physicians’ Health Study (PHS) Am Heart J. 2008;155:82–86. doi: 10.1016/j.ahj.2007.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sarnak MJ, Katz R, Stehman-Breen CO, Fried LF, Jenny NS, Psaty BM, Newman AB, Siscovick D, Shlipak MG Cardiovascular Health Study. Cystatin C concentration as a risk factor for heart failure in older adults. Ann Intern Med. 2005;142:497–505. doi: 10.7326/0003-4819-142-7-200504050-00008. [DOI] [PubMed] [Google Scholar]
- 47.O’Hare AM, Newman AB, Katz R, Fried LF, Stehman-Breen CO, Seliger SL, Siscovick DS, Shlipak MG. Cystatin C and incident peripheral arterial disease events in the elderly: results from the Cardiovascular Health Study. Arch Intern Med. 2005;165:2666–2670. doi: 10.1001/archinte.165.22.2666. [DOI] [PubMed] [Google Scholar]
- 48.Shlipak MG, Katz R, Kestenbaum B, Fried LF, Siscovick D, Sarnak MJ. Clinical and subclinical cardiovascular disease and kidney function decline in the elderly. Atherosclerosis. 2009;204:298–303. doi: 10.1016/j.atherosclerosis.2008.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Koenig W, Twardella D, Brenner H, Rothenbacher D. Plasma concentrations of cystatin C in patients with coronary heart disease and risk for secondary cardiovascular events: more than simply a marker of glomerular filtration rate. Clin Chem. 2005;51:321–327. doi: 10.1373/clinchem.2004.041889. [DOI] [PubMed] [Google Scholar]
- 50.Keller T, Messow CM, Lubos E, Nicaud V, Wild PS, Rupprecht HJ, Bickel C, Tzikas S, Peetz D, Lackner KJ, Tiret L, Münzel TF, Blankenberg S, Schnabel RB. Cystatin C and cardiovascular mortality in patients with coronary artery disease and normal or mildly reduced kidney function: results from the AtheroGene study. Eur Heart J. 2009;30:314–320. doi: 10.1093/eurheartj/ehn598. [DOI] [PubMed] [Google Scholar]
- 51.Deo R, Fyr CL, Fried LF, Newman AB, Harris TB, Angleman S, Green C, Kritchevsky SB, Chertow GM, Cummings SR, Shlipak MG Health ABC study. Kidney dysfunction and fatal cardiovascular disease: an association independent of atherosclerotic events: results from the Health, Aging, and Body Composition (Health ABC) study. Am Heart J. 2008;155:62–68. doi: 10.1016/j.ahj.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 52.Deo R, Sotoodehnia N, Katz R, Sarnak MJ, Fried LF, Chonchol M, Kestenbaum B, Psaty BM, Siscovick DS, Shlipak MG. Cystatin C and sudden cardiac death risk in the elderly. Circ Cardiovasc Qual Outcomes. 2010;3:159–164. doi: 10.1161/CIRCOUTCOMES.109.875369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, Wanner C, Krane V, Cass A, Craig J, Neal B, Jiang L, Hooi LS, Levin A, Agodoa L, Gaziano M, Kasiske B, Walker R, Massy ZA, Feldt-Rasmussen B, Krairittichai U, Ophascharoensuk V, Fellström B, Holdaas H, Tesar V, Wiecek A, Grobbee D, de Zeeuw D, Grönhagen-Riska C, Dasgupta T, Lewis D, Herrington W, Mafham M, Majoni W, Wallendszus K, Grimm R, Pedersen T, Tobert J, Armitage J, Baxter A, Bray C, Chen Y, Chen Z, Hill M, Knott C, Parish S, Simpson D, Sleight P, Young A, Collins R SHARP Investigators. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet. 2011;377:2181–2192. doi: 10.1016/S0140-6736(11)60739-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
13. Total Cardiovascular Diseases
ICD-9 390 to 459, 745 to 747, ICD-10 I00 to I99, Q20 to Q28; see Glossary (Chapter 26) for details and definitions.
See Tables 13-1 through 13-4 and Charts 13-1 through 13-21.
Table 13-1.
Cardiovascular Diseases
| Population Group | Prevalence, 2010: Age ≥20 y | Mortality, 2010: All Ages* | Hospital Discharges, 2010: All Ages | Cost, 2010 |
|---|---|---|---|---|
| Both sexes | 83 600 000 (35.3%) | 787 650 | 5 802 000 | $315.4 Billion |
| Males | 40 700 000 (36.7%) | 387 318 (49.2%)† | 3 021 000 | … |
| Females | 42 900 000 (34.0%) | 400 332 (50.8%)† | 2 781 000 | … |
| NH white males | 36.6% | 330 330 | … | … |
| NH white females | 32.4% | 342 581 | … | … |
| NH black males | 44.4% | 46 266 | … | … |
| NH black females | 48.9% | 49 977 | … | … |
| Mexican American males | 33.4% | … | … | … |
| Mexican American females | 30.7% | … | … | … |
| Asian or Pacific Islander | … | 16 829‡ | … | … |
| American Indian or Alaska Native | … | 3667 | … | … |
Ellipses (…) indicate data not available; NH, non-Hispanic.
Mortality data for the white, black, Asian or Pacific Islander, and American Indian or Alaska Native populations include deaths among people of Hispanic and non-Hispanic origin. Numbers of deaths for the American Indian or Alaska Native and Asian or Pacific Islander populations are known to be underestimated.
These percentages represent the portion of total cardiovascular disease mortality that is attributable to males vs females.
Includes Chinese, Filipino, Hawaiian, Japanese, and other Asian or Pacific Islander.
Sources: Prevalence: National Health and Nutrition Examination Survey 2007 to 2010, National Center for Health Statistics (NCHS) and National Heart, Lung, and Blood Institute (NHLBI). Percentages for racial/ethnic groups are age adjusted for Americans ≥20 y of age. Age-specific percentages are extrapolated to the 2010 US population estimates. Mortality: Centers for Disease Control and Prevention/NCHS, 2010 Mortality Multiple Cause-of-Death–United States, version dated May 21, 2013. These data represent underlying cause of death only for International Classification of Diseases, 10th Revision codes I00 to I99 (diseases of the circulatory system) and Q20 to Q28 (congenital malformations of the circulatory system). Hospital discharges: National Hospital Discharge Survey, NCHS. Data include those inpatients discharged alive, dead, or of unknown status. Cost: NHLBI. Data include estimated direct and indirect costs for 2010.
Table 13-4.
Remaining Lifetime Risks for CVD and Other Diseases Among Men and Women Free of Disease at 40 and 70 Years of Age
| Diseases | Remaining Lifetime Risk at Age 40 y
|
Remaining Lifetime Risk at Age 70 y
|
||
|---|---|---|---|---|
| Men | Women | Men | Women | |
| Any CVD5a | 2 in 3* | 1 in 2* | 2 in 3† | 1 in 2 |
| CHD6 | 1 in 2 | 1 in 3 | 1 in 3 | 1 in 4 |
| AF56 | 1 in 4 | 1 in 4 | 1 in 4 | 1 in 4 |
| CHF57 | 1 in 5 | 1 in 5 | 1 in 5 | 1 in 5 |
| Stroke58 | 1 in 6‡ | 1 in 5‡ | 1 in 6 | 1 in 5 |
| Dementia58 | … | … | 1 in 7 | 1 in 5 |
| Hip fracture59 | 1 in 20 | 1 in 6 | … | … |
| Breast cancer60 | … | 1 in 8 | … | 1 in 15 |
| Prostate cancer60 | 1 in 6 | … | 1 in 9 | … |
| Lung cancer60 | 1 in 13 | 1 in 16 | 1 in 15 | 1 in 20 |
| Colon cancer60 | 1 in 19 | 1 in 21 | 1 in 25 | 1 in 27 |
| DM61 | 1 in 3 | 1 in 3 | 1 in 9 | 1 in 7 |
| Hypertension62 | 9 in 10‡ | 9 in 10‡ | 9 in 10† | 9 in 10† |
| Obesity63 | 1 in 3 | 1 in 3 | … | … |
AF indicates atrial fibrillation; CHD, coronary heart disease; CHF, congestive heart failure; CVD, cardiovascular disease; DM, diabetes mellitus; ellipses (…), not estimated.
Age 45 y.
Age 65 y.
Age 55 y.
Chart 13-1.
Prevalence of cardiovascular disease in adults ≥20 years of age by age and sex (National Health and Nutrition Examination Survey: 2007–2010). These data include coronary heart disease, heart failure, stroke, and hypertension. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-21.
Hospital discharges for the 10 leading diagnostic groups (United States: 2010). Source: National Hospital Discharge Survey/National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Prevalence
(See Table 13-1 and Chart 13-1.)
An estimated 83.6 million American adults (>1 in 3) have ≥ 1 types of CVD. Of these, 42.2 million are estimated to be ≥60 years of age. Total CVD includes diseases listed in the bullet points below, with the exception of congenital CVD. Because of overlap across conditions, it is not possible to add these conditions to arrive at a total.
HBP—77.9 million (defined as systolic pressure ≥140 mm Hg and/or diastolic pressure ≥90 mm Hg, use of anti-hypertensive medication, or being told at least twice by a physician or other health professional that one has HBP).
-
CHD—15.4 million
MI (heart attack)—7.6 million
AP (chest pain)—7.8 million
HF—5.1 million
Stroke (all types)—6.8 million
Congenital cardiovascular defects— 650 000 to 1.3 million
-
The following age-adjusted prevalence estimates from the NHIS, NCHS are for diagnosed conditions for people ≥18 years of age in 20121:
Among whites only, 10.9% have HD, 6.1% have CHD, 22.9% have hypertension, and 2.5% have had a stroke.
Among blacks or African Americans, 10.8% have HD, 6.5% have CHD, 32.9% have hypertension, and 3.9% have had a stroke.
Among Hispanics or Latinos, 7.8% have HD, 5.3% have CHD, 20.9% have hypertension, and 2.7% have had a stroke.
Among Asians, 6.8% have HD, 4.5% have CHD, 21.2% have hypertension, and 1.8% have had a stroke.
Among American Indians or Alaska Natives, 12.5% have HD, 8.1% have CHD, and 24.8% have hypertension. The statistic for stroke for this group is not shown because of unreliability.*
Among Native Hawaiians or other Pacific Islanders 12.5% have HD, 10.3% have CHD, and 36.5% have hypertension. The statistics for stroke for this group are not shown because of unreliability.*
-
Asian Indian adults (9%) are ≈2-fold more likely than Korean adults (4%) to have ever been told they have HD, based on data for 2004 to 2006.2
By 2030, 43.9% of the US population is projected to have some form of CVD (unpublished AHA tabulation, based on methodology described by Heidenreich et al).3
Abbreviations Used in Chapter 13
| AHA | American Heart Association |
| AMI | acute myocardial infarction |
| AP | angina pectoris |
| ARIC | Atherosclerosis Risk in Communities study |
| BMI | body mass index |
| BP | blood pressure |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CABG | cardiac revascularization (coronary artery bypass graft) |
| CAD | coronary artery disease |
| CARDIA | Coronary Artery Risk Development in Young Adults |
| CDC | Centers for Disease Control and Prevention |
| CHD | coronary heart disease |
| CHF | congestive heart failure |
| CLRD | chronic lower respiratory disease |
| CPR | cardiopulmonary resuscitation |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| ED | emergency department |
| FHS | Framingham Heart Study |
| HBP | high blood pressure |
| HCM | hypertrophic cardiomyopathy |
| HD | heart disease |
| HF | heart failure |
| HIV | human immunodeficiency virus |
| ICD-9 | International Classification of Diseases, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| LDL | low-density lipoprotein |
| MEPS | Medical Expenditure Panel Survey |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| MI | myocardial infarction |
| NAMCS | National Ambulatory Medical Care Survey |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHAMCS | National Hospital Ambulatory Medical Care Survey |
| NHANES | National Health and Nutrition Examination Survey |
| NHDS | National Hospital Discharge Survey |
| NHIS | National Health Interview Survey |
| NHHCS | National Home and Hospice Care Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| NNHS | National Nursing Home Survey |
| PA | physical activity |
| PCI | percutaneous coronary intervention |
| RR | relative risk |
| SBP | systolic blood pressure |
| UA | unstable angina |
| WONDER | Wide-ranging Online Data for Epidemiologic Research |
Incidence
(See Chart 13-2.)
Chart 13-2.
Incidence of cardiovascular disease (coronary heart disease, heart failure, stroke, or intermittent claudication; does not include hypertension alone) by age and sex (Framingham Heart Study, 1980–2003). Source: National Heart, Lung, and Blood Institute.4
-
On the basis of the NHLBI’s FHS original and offspring cohort data from 1980 to 20034
The average annual rate of first cardiovascular events rises from 3 per 1000 men at 35 to 44 years of age to 74 per 1000 men at 85 to 94 years of age. For women, comparable rates occur 10 years later in life. The gap narrows with advancing age.
Before 75 years of age, a higher proportion of CVD events attributable to CHD occur in men than in women, and a higher proportion of events attributable to stroke occur in women than in men.
Among American Indian men 45 to 74 years of age, the incidence of CVD ranges from 20 to 28 per 1000 population. Among women, it ranges from 9 to 15 per 1000.5
Data from the FHS indicate that the subsequent lifetime risk for all CVD in recipients starting free of known disease is almost 2 in 3 for men and >1 in 2 for women at 45 years of age (Table 13-4).5a
Analysis of FHS data among participants free of CVD at 50 years of age showed the lifetime risk for developing CVD was 51.7% for men and 39.2% for women. Median overall survival was 30 years for men and 36 years for women.6
Mortality
(See Table 13-1 through 13-3 and Charts 13-3 through 13-18.)
Table 13-3.
International Death Rates (Revised February 2012): Death Rates (per 100 000 Population) for Total CVD, CHD, Stroke, and Total Deaths in Selected Countries (Most Recent Year Available)
| Sorted Alphabetically by Country | Rate per 100 000 Population
|
Sorted by Descending CVD Death Rate | Rate per 100 000 Population
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| CVD | CHD | Stroke | Total | CVD | CHD | Stroke | Total | ||
| Men aged 35–74 y | |||||||||
| Argentina (2010) | 305.6 | 88.8 | 62.9 | 1062.8 | Russian Federation (2010) | 1173.3 | 654.8 | 299.2 | 2400.7 |
| Australia (2011) | 126.1 | 76.9 | 18.7 | 530.3 | Ukraine (2011) | 1080.0 | 732.9 | 220.8 | 2077.2 |
| Austria (2011) | 182.4 | 108.9 | 23.7 | 700.6 | Romania (2010) | 657.9 | 268.2 | 195.9 | 1548.4 |
| Belgium (2009) | 181.2 | 79.9 | 30.8 | 758.4 | Hungary (2011) | 564.8 | 302.6 | 108.6 | 1539.3 |
| Brazil (2010) | 347.7 | 134.5 | 95.8 | 1143.9 | Czech Republic (2011) | 374.0 | 200.2 | 55.6 | 1027.4 |
| Canada (2009) | 154.4 | 101.9 | 19.2 | 607.9 | Brazil (2010) | 347.7 | 134.5 | 95.8 | 1143.9 |
| Chile (2009) | 220.5 | 91.7 | 63.4 | 864.6 | Cuba (2010) | 347.5 | 175.4 | 80.1 | 957.5 |
| Cuba (2010) | 347.5 | 175.4 | 80.1 | 957.5 | Argentina (2010) | 305.6 | 88.8 | 62.9 | 1062.8 |
| Czech Republic (2011) | 374.0 | 200.2 | 55.6 | 1027.4 | Finland (2011) | 261.0 | 153.9 | 39.6 | 772.7 |
| Denmark (2011) | 146.0 | 62.0 | 29.1 | 722.0 | United States (2010) | 239.9 | 135.8 | 28.4 | 822.0 |
| Finland (2011) | 261.0 | 153.9 | 39.6 | 772.7 | Mexico (2010) | 224.1 | 130.9 | 46.0 | 1022.6 |
| France (2009) | 133.8 | 51.0 | 24.3 | 750.1 | Chile (2009) | 220.5 | 91.7 | 63.4 | 864.6 |
| Germany (2011) | 197.6 | 97.7 | 27.8 | 729.4 | Ireland (2009) | 210.0 | 140.6 | 29.2 | 701.3 |
| Hungary (2011) | 564.8 | 302.6 | 108.6 | 1539.3 | Germany (2011) | 197.6 | 97.7 | 27.8 | 729.4 |
| Ireland (2009) | 210.0 | 140.6 | 29.2 | 701.3 | United Kingdom (2010) | 197.5 | 121.1 | 29.8 | 673.6 |
| Israel (2010) | 121.5 | 60.6 | 24.0 | 580.4 | New Zealand (2009) | 184.4 | 121.1 | 26.5 | 605.2 |
| Italy (2010) | 145.6 | 68.4 | 27.8 | 585.1 | Austria (2011) | 182.4 | 108.9 | 23.7 | 700.6 |
| Japan (2011) | 142.7 | 47.0 | 49.0 | 611.5 | Belgium (2009) | 181.2 | 79.9 | 30.8 | 758.4 |
| Korea, South (2011) | 123.4 | 36.5 | 54.7 | 736.3 | Sweden (2010) | 165.1 | 93.1 | 26.3 | 556.1 |
| Mexico (2010) | 224.1 | 130.9 | 46.0 | 1022.6 | Canada (2009) | 154.4 | 101.9 | 19.2 | 607.9 |
| Netherlands (2011) | 136.8 | 53.1 | 21.9 | 586.6 | Spain (2010) | 149.6 | 69.8 | 28.1 | 668.3 |
| New Zealand (2009) | 184.4 | 121.1 | 26.5 | 605.2 | Portugal (2011) | 148.1 | 55.0 | 53.7 | 777.7 |
| Norway (2011) | 139.0 | 76.0 | 25.0 | 577.6 | Denmark (2011) | 146.0 | 62.0 | 29.1 | 722.0 |
| Portugal (2011) | 148.1 | 55.0 | 53.7 | 777.7 | Italy (2010) | 145.6 | 68.4 | 27.8 | 585.1 |
| Romania (2010) | 657.9 | 268.2 | 195.9 | 1548.4 | Japan (2011) | 142.7 | 47.0 | 49.0 | 611.5 |
| Russian Federation (2010) | 1173.3 | 654.8 | 299.2 | 2400.7 | Norway (2011) | 139.0 | 76.0 | 25.0 | 577.6 |
| Spain (2010) | 149.6 | 69.8 | 28.1 | 668.3 | Netherlands (2011) | 136.8 | 53.1 | 21.9 | 586.6 |
| Sweden (2010) | 165.1 | 93.1 | 26.3 | 556.1 | France (2009) | 133.8 | 51.0 | 24.3 | 750.1 |
| Switzerland (2010) | 131.6 | 67.7 | 16.3 | 538.1 | Switzerland (2010) | 131.6 | 67.7 | 16.3 | 538.1 |
| Ukraine (2011) | 1080.0 | 732.9 | 220.8 | 2077.2 | Australia (2011) | 126.1 | 76.9 | 18.7 | 530.3 |
| United Kingdom (2010) | 197.5 | 121.1 | 29.8 | 673.6 | Korea, South (2011) | 123.4 | 36.5 | 54.7 | 736.3 |
| United States (2010) | 239.9 | 135.8 | 28.4 | 822.0 | Israel (2010) | 121.5 | 60.6 | 24.0 | 580.4 |
| Women aged 35–74 y | |||||||||
| Argentina (2010) | 139.7 | 28.4 | 35.5 | 574.3 | Ukraine (2011) | 475.2 | 313.3 | 119.7 | 844.4 |
| Australia (2011) | 52.3 | 21.6 | 13.5 | 318.3 | Russian Federation (2010) | 466.0 | 226.3 | 155.0 | 915.7 |
| Austria (2011) | 69.7 | 32.0 | 14.4 | 361.3 | Romania (2010) | 312.2 | 105.8 | 111.4 | 692.3 |
| Belgium (2009) | 80.0 | 24.7 | 20.5 | 422.3 | Hungary (2011) | 223.5 | 105.4 | 52.1 | 692.0 |
| Brazil (2010) | 205.1 | 63.9 | 63.0 | 638.9 | Cuba (2010) | 209.2 | 90.1 | 61.0 | 613.8 |
| Canada (2009) | 65.9 | 33.1 | 14.5 | 388.1 | Brazil (2010) | 205.1 | 63.9 | 63.0 | 638.9 |
| Chile (2009) | 103.5 | 29.5 | 37.4 | 455.0 | Czech Republic (2011) | 149.0 | 63.6 | 30.1 | 483.3 |
| Cuba (2010) | 209.2 | 90.1 | 61.0 | 613.8 | Argentina (2010) | 139.7 | 28.4 | 35.5 | 574.3 |
| Czech Republic (2011) | 149.0 | 63.6 | 30.1 | 483.3 | Mexico (2010) | 137.0 | 59.6 | 36.0 | 638.8 |
| Denmark (2011) | 64.6 | 18.3 | 20.7 | 462.9 | United States (2010) | 119.6 | 53.0 | 21.6 | 520.3 |
| Finland (2011) | 74.8 | 31.4 | 20.8 | 358.6 | Chile (2009) | 103.5 | 29.5 | 37.4 | 455.0 |
| France (2009) | 48.2 | 10.9 | 13.8 | 343.3 | Ireland (2009) | 86.8 | 40.9 | 21.9 | 419.8 |
| Germany (2011) | 81.6 | 28.2 | 17.2 | 393.0 | United Kingdom (2010) | 84.7 | 36.8 | 21.6 | 431.5 |
| Hungary (2011) | 223.5 | 105.4 | 52.1 | 692.0 | Germany (2011) | 81.6 | 28.2 | 17.2 | 393.0 |
| Ireland (2009) | 86.8 | 40.9 | 21.9 | 419.8 | Belgium (2009) | 80.0 | 24.7 | 20.5 | 422.3 |
| Israel (2010) | 51.6 | 16.8 | 14.5 | 349.7 | New Zealand (2009) | 79.9 | 35.4 | 23.0 | 410.0 |
| Italy (2010) | 58.3 | 18.4 | 16.1 | 308.6 | Finland (2011) | 74.8 | 31.4 | 20.8 | 358.6 |
| Japan (2011) | 53.5 | 12.6 | 21.6 | 284.3 | Austria (2011) | 69.7 | 32.0 | 14.4 | 361.3 |
| Korea, South (2011) | 55.5 | 11.6 | 28.5 | 288.6 | Sweden (2010) | 67.8 | 31.1 | 16.2 | 357.1 |
| Mexico (2010) | 137.0 | 59.6 | 36.0 | 638.8 | Portugal (2011) | 66.6 | 16.5 | 29.0 | 343.2 |
| Netherlands (2011) | 65.9 | 18.0 | 16.7 | 408.8 | Canada (2009) | 65.9 | 33.1 | 14.5 | 388.1 |
| New Zealand (2009) | 79.9 | 35.4 | 23.0 | 410.0 | Netherlands (2011) | 65.9 | 18.0 | 16.7 | 408.8 |
| Norway (2011) | 53.4 | 20.2 | 15.8 | 355.5 | Denmark (2011) | 64.6 | 18.3 | 20.7 | 462.9 |
| Portugal (2011) | 66.6 | 16.5 | 29.0 | 343.2 | Italy (2010) | 58.3 | 18.4 | 16.1 | 308.6 |
| Romania (2010) | 312.2 | 105.8 | 111.4 | 692.3 | Korea, South (2011) | 55.5 | 11.6 | 28.5 | 288.6 |
| Russian Federation (2010) | 466.0 | 226.3 | 155.0 | 915.7 | Japan (2011) | 53.5 | 12.6 | 21.6 | 284.3 |
| Spain (2010) | 53.4 | 16.2 | 14.6 | 283.2 | Norway (2011) | 53.4 | 20.2 | 15.8 | 355.5 |
| Sweden (2010) | 67.8 | 31.1 | 16.2 | 357.1 | Spain (2010) | 53.4 | 16.2 | 14.6 | 283.2 |
| Switzerland (2010) | 49.3 | 19.4 | 11.1 | 308.9 | Australia (2011) | 52.3 | 21.6 | 13.5 | 318.3 |
| Ukraine (2011) | 475.2 | 313.3 | 119.7 | 844.4 | Israel (2010) | 51.6 | 16.8 | 14.5 | 349.7 |
| United Kingdom (2010) | 84.7 | 36.8 | 21.6 | 431.5 | Switzerland (2010) | 49.3 | 19.4 | 11.1 | 308.9 |
| United States (2010) | 119.6 | 53.0 | 21.6 | 520.3 | France (2009) | 48.2 | 10.9 | 13.8 | 343.3 |
Rates are adjusted to the European Standard population. International Classification of Diseases, 10th Revision codes used were I00 to I99 for CVD, I20 to I25 for CHD, and I60 to I69 for stroke.
CHD indicates coronary heart disease; and CVD, cardiovascular disease.
Sources: The World Health Organization, National Center for Health Statistics, and National Heart, Lung, and Blood Institute.
Chart 13-3.
Deaths attributable to diseases of the heart (United States: 1900–2010). See Glossary (Chapter 26) for an explanation of “diseases of the heart.” Note: In the years 1900 to 1920, the International Classification of Diseases codes were 77 to 80; for 1925, 87 to 90; for 1930 to 1945, 90 to 95; for 1950 to 1960, 402 to 404 and 410 to 443; for 1965, 402 to 404 and 410 to 443; for 1970 to 1975, 390 to 398 and 404 to 429; for 1980 to 1995, 390 to 398, 402, and 404 to 429; and for 2000 to 2009, I00 to I09, I11, I13, and I20 to I51. Before 1933, data are for a death registration area and not the entire United States. In 1900, only 10 states were in the death registration area, and this increased over the years, so part of the increase in numbers of deaths is attributable to an increase in the number of states. Source: National Center for Health Statistics.
Chart 13-18.
US maps corresponding to state death rates (including the District of Columbia), 2010.
ICD-10 I00 to I99, Q20 to Q28 for CVD; C00 to C97 for cancer; C33 to C34 for lung cancer; C50 for breast cancer; J40 to J47 for CLRD; G30 for Alzheimer disease; E10 to E14 for DM; and V01 to X59 and Y85 to Y86 for accidents.
Mortality data show that CVD as the listed underlying cause of death (including congenital cardiovascular defects) accounted for 31.9% (787 650) of all 2 468 435 deaths in 2010, or 1 of every 3 deaths in the United States. CVD any-mentions (1 344 185 deaths in 2010) constituted 54.5% of all deaths that year (NHLBI; NCHS public use data files).7
In every year since 1900 except 1918, CVD accounted for more deaths than any other major cause of death in the United States.8,9
On average, >2150 Americans die of CVD each day, an average of 1 death every 40 seconds. CVD currently claims more lives each year than cancer and CLRD combined.7
The 2010 death rate attributable to CVD was 235.5 (excluding congenital cardiovascular defects; NCHS). The death rates were 283.4 for males and 197.3 for females. The rates were 278.4 for white males, 369.2 for black males, 192.2 for white females, and 260.5 for black females. From 2000 to 2010, death rates attributable to CVD declined 31.0%. In the same 10-year period, the actual number of CVD deaths per year declined by 16.7% (AHA tabulation).7
Among other causes of death in 2010, cancer caused 574 743 deaths; CLRD, 138 080; accidents, 120 859; and Alzheimer disease, 83 494.7
On the basis of 2010 mortality data, CVD (including congenital cardiovascular defects) caused ≈1 death per minute among females, or 400 322 deaths. That represents approximately the same number of female lives as were claimed by cancer, CLRD, and Alzheimer disease combined (unpublished AHA tabulation). There were 40 996 deaths attributable to breast cancer in females in 2010; lung cancer claimed 70 550 females. Death rates for females were 22.1 for breast cancer and 38.1 for lung cancer. One in 30 deaths of females was attributable to breast cancer, whereas 1 in 7.2 was attributable to CHD. For comparison, 1 in 4.5 females died of cancer, whereas 1 in 3.1 died of CVD.7
Approximately 150 000 Americans died of CVD in 2010 who were <65 years of age, and 34% of deaths attributed to CVD occurred before the age of 75 years,7 which is well below the average life expectancy of 78.7 years.9
If all forms of major CVD were eliminated, life expectancy could rise by almost 7 years. If all forms of cancer were eliminated, the estimated gain could be 3 years. According to the same study, the probability at birth of eventually dying of major CVD (I00–I78) is 47%, and the chance of dying of cancer is 22%. Additional probabilities are 3% for accidents, 2% for DM (unrelated to CVD), and 0.7% for HIV.10
In 2010, the leading causes of death in women ≥65 years of age were diseases of the heart (No. 1), cancer (No. 2), stroke (No. 3), and CLRD (No. 4). In older men, they were diseases of the heart (No. 1), cancer (No. 2), CLRD (No. 3), and stroke (No. 4).7
A study of the decrease in US deaths attributable to CHD from 1980 to 2000 suggests that ≈47% of the decrease was attributable to increased use of evidence-based medical therapies and 44% to changes in risk factors in the population attributable to lifestyle and environmental changes.8
Analysis of data from NCHS was used to determine the number of disease-specific deaths attributable to all non-optimal levels of each risk factor exposure, by age and sex. In 2005, tobacco smoking and HBP were estimated to be responsible for 467 000 deaths, accounting for ≈1 in 5 or 6 deaths among US adults. Overweight/obesity and physical inactivity were each estimated to be responsible for nearly 1 in 10 deaths. High dietary salt, low dietary omega-3 fatty acids, and high dietary trans fatty acids were the dietary risks with the largest estimated excess mortality effects.10
Aftermath
Among an estimated 45 million people with functional disabilities in the United States, HD, stroke, and hypertension are among the 15 leading conditions that caused those disabilities. Disabilities were defined as difficulty with activities of daily living or instrumental activities of daily living, specific functional limitations (except vision, hearing, or speech), and limitation in ability to do housework or work at a job or business.11
Awareness of Warning Signs and Risk Factors for CVD
Surveys conducted every 3 years since 1997 by the AHA to evaluate trends in women’s awareness, knowledge, and perceptions related to CVD found most recently (in 2012) that awareness of HD as the leading cause of death among women was 56%, 30% higher than in 1997 (P<0.001). Awareness among black and Hispanic women in 2012 was similar to that of white women in 1997; however, awareness rates in 2012 among black and Hispanic women remained well below that of white women in 2012. Awareness of heart attack signs remained low for all racial/ethnic and age groups surveyed.12
A total of 875 students in 4 Michigan high schools were given a survey to obtain data on the perception of risk factors and other knowledge-based assessment questions about CVD. Accidents were rated as the greatest perceived lifetime health risk (39%). Nearly 17% selected CVD as the greatest lifetime risk, which made it the third most popular choice after accidents and cancer. When asked to identify the greatest cause of death for each sex, 42% correctly recognized CVD for men, and 14% correctly recognized CVD for women; 40% incorrectly chose abuse/use behavior with a substance other than cigarettes as the most important CVD risk behavior.13
Awareness of CPR
Seventy-nine percent of the lay public are confident that they know what actions to take in a medical emergency; 98% recognize an automated external defibrillator as something that administers an electric shock to restore a normal heart beat among victims of sudden cardiac arrest; and 60% are familiar with CPR (Harris Interactive survey conducted on behalf of the AHA among 1132 US residents >18 years of age, January 8, 2008–January 21, 2008).
Disparities in CVD Risk Factors
(See Chart 13-19.)
Chart 13-19.
Estimated average 10-year cardiovascular disease risk in adults 50 to 54 years of age according to levels of various risk factors (Framingham Heart Study). BP indicates blood pressure; and HDL, high-density lipoprotein. Data derived from D’Agostino et al.64
Data from the 2003 CDC BRFSS survey of adults ≥18 years of age showed the prevalence of respondents who reported having ≥2 risk factors for HD and stroke was successively higher at higher age groups. The prevalence of having ≥2 risk factors was highest among blacks (48.7%) and American Indian/Alaska Natives (46.7%) and lowest among Asians (25.9%); prevalence was similar in women (36.4%) and men (37.8%). The prevalence of multiple risk factors ranged from 25.9% among college graduates to 52.5% among those with less than a high school diploma (or its equivalent). People reporting household income of ≥$50 000 had the lowest prevalence (28.8%), and those reporting household income of <$10 000 had the highest prevalence (52.5%). Adults who reported being unable to work had the highest prevalence (69.3%) of ≥2 risk factors, followed by retired people (45.1%), unemployed adults (43.4%), homemakers (34.3%), and employed people (34.0%). Prevalence of ≥2 risk factors varied by state/ territory and ranged from 27.0% (Hawaii) to 46.2% (Kentucky). Twelve states and 2 territories had a multiple risk factor prevalence of ≥40%: Alabama, Arkansas, Georgia, Indiana, Kentucky, Louisiana, Mississippi, North Carolina, Ohio, Oklahoma, Tennessee, West Virginia, Guam, and Puerto Rico.14
Analysis of several data sets by the CDC showed that in adults ≥18 years of age, disparities were common in all risk factors examined. In men, the highest prevalence of obesity (29.7%) was found in Mexican Americans who had completed a high school education. Black women with or without a high school education had a high prevalence of obesity (48.4%). Hypertension prevalence was high among blacks (41.2%) regardless of sex or educational status. Hypercholesterolemia was high among white and Mexican American men and white women regardless of educational status. CHD and stroke were inversely related to education, income, and poverty status. Hospitalization for total HD and AMI was greater among men, but hospitalization for CHF and stroke was greater among women. Among Medicare enrollees, CHF hospitalization was higher among blacks, Hispanics, and American Indian/Alaska Natives than among whites, and stroke hospitalization was highest among blacks. Hospitalizations for CHF and stroke were highest in the southeastern United States. Life expectancy remains higher in women than in men and in whites than in blacks by ≈5 years. CVD mortality at all ages tended to be highest in blacks.15
Analysis of >14 000 middle-aged subjects in the ARIC study sponsored by the NHLBI showed that >90% of CVD events in black subjects, compared with ≈70% in white subjects, appeared to be explained by elevated or borderline risk factors. Furthermore, the prevalence of participants with elevated risk factors was higher in black subjects; after accounting for education and known CVD risk factors, the incidence of CVD was identical in black and white subjects. Thus, the observed higher CVD incidence rate in black subjects appears to be largely attributable to a greater prevalence of elevated risk factors. These results suggest that the primary prevention of elevated risk factors might substantially impact the future incidence of CVD, and these beneficial effects would likely be applicable not only for white but also for black subjects.16
-
Data from the MEPS 2004 Full-Year Data File showed that nearly 26 million US adults ≥18 years of age were told by a doctor that they had HD, stroke, or any other heart-related disease17:
38.6% maintained a healthy weight. Among those told that they had HD, 33.9% had a healthy weight compared with 39.3% who had never been told they had HD.
78.8% did not currently smoke. Among those ever told that they had indicators of HD, 18.3% continued to smoke.
More than 93% engaged in at least 1 recommended behavior for prevention of HD: 75.5% engaged in 1 or 2; 18% engaged in all 3; and 6.5% did not engage in any of the recommended behaviors.
-
Age-based variations:
Moderate to vigorous PA ≥3 times per week varied according to age. Younger people (18–44 years of age) were more likely (59.9%) than those who were older (45–64 and ≥65 years of age, 55.3% and 48.5%, respectively) to engage in regular PA.
A greater percentage of those 18 to 44 years of age had a healthy weight (43.7%) than did those 45 to 64 years of age and ≥65 years of age (31.4% and 37.3%, respectively).
People ≥65 years of age were more likely to be current nonsmokers (89.7%) than were people 18 to 44 years of age and 45 to 64 years of age (76.1% and 77.7%, respectively).
-
Race/ethnicity-based variations:
Non-Hispanic whites were more likely than Hispanics or non-Hispanic blacks to engage in moderate to vigorous PA (58.5% versus 51.4% and 52.5%, respectively).
Non-Hispanic whites were more likely to have maintained a healthy weight than were Hispanics or non-Hispanic blacks (39.8% versus 32.1% and 29.7%, respectively).
Hispanics were more likely to be nonsmokers (84.2%) than were non-Hispanic whites and non-Hispanic blacks (77.8% and 76.3%, respectively).
-
Sex-based variations:
Men were more likely to have engaged in moderate to vigorous PA ≥3 times per week than women (60.3% versus 53.1%, respectively).
Women were more likely than men to have maintained a healthy weight (45.1% versus 31.7%, respectively).
81.7% of women did not currently smoke, compared with 75.7% of men.
-
Variations based on education level:
A greater percentage of adults with at least some college education engaged in moderate to vigorous PA ≥3 times per week (60.8%) than did those with a high school education or less than a high school education (55.3% and 48.3%, respectively).
A greater percentage of adults with at least some college education had a healthy weight (41.2%) than did those with a high school or less than high school education (36.2% and 36.1%, respectively).
There was a greater percentage of nonsmokers among those with a college education (85.5%) than among those with a high school or less than high school education (73.8% and 69.9%, respectively).
A study of nearly 1500 participants in MESA found that Hispanics with hypertension, hypercholesterolemia, or DM who spoke Spanish at home or had spent less than half a year in the United States had higher SBP, LDL cholesterol, and fasting blood glucose, respectively, than Hispanics who spoke English and who had lived a longer period of time in the United States.18
Recent findings from >15 000 Hispanics of diverse background demonstrated that a sizeable proportion of both men and women had major CVD risk factors, with higher prevalence among Puerto Rican subgroups and those with lower socioeconomic status and a higher level of acculturation.19
Family History of CVD
A family history of CVD increases risk of CVD, with the largest increase in risk if the family member’s CVD was premature.20
There is consistent evidence from multiple large-scale prospective epidemiology studies for a strong and significant association of a reported family history of premature parental CHD with incident MI or CHD in offspring. In the FHS, the occurrence of a validated premature atherosclerotic CVD event in either a parent21 or a sibling22 was associated with an ≈2-fold elevated risk for CVD, independent of other traditional risk factors.
Addition of family history of premature CVD to a model that contained traditional risk factors provided modestly improved prognostic value in the FHS.21 Family history of premature MI is also an independent risk factor in other multivariable risk models that contain traditional risk factors in large cohorts of women23 and men.24
Parental history of premature CHD is associated with increased burden of subclinical atherosclerosis in the coronary arteries and the abdominal aorta.25,26
In the FHS, a parental history of validated HF is associated with a 1.7-fold higher risk of HF in offspring, after multivariable adjustment.27
A family history of early-onset sudden cardiac death in a first-degree relative is associated with a >2-fold higher risk for sudden cardiac death in offspring on the basis of available case-control studies.28
The 2004 HealthStyles survey of 4345 people in the United States indicated that most respondents believe that knowing their family history is important for their own health, but few are aware of the specific health information from relatives necessary to develop a family history.29
A family history of premature CVD was associated with a significant increase in lifetime risk for CVD mortality in men. The effect of a premature family history on lifetime risk was similar to that observed for other major CVD risk factors.30
An accurate and complete family history may identify rare mendelian conditions such as HCM, long-QT syndrome, or familial hypercholesterolemia. However, in the majority of people with a family history of a CVD event, a known rare mendelian condition is not identified.
Studies are under way to determine genetic variants that may help identify individuals at increased risk of CVD.
Impact of Healthy Lifestyle and Low Risk Factor Levels
Much of the literature on CVD has focused on factors associated with increasing risk for CVD and on factors associated with poorer outcomes in the presence of CVD; however, in recent years, a number of studies have defined the potential beneficial effects of healthy lifestyle factors and lower CVD risk factor burden on CVD outcomes and longevity. These studies suggest that prevention of risk factor development at younger ages may be the key to “successful aging,” and they highlight the need for evaluation of the potential benefits of intensive prevention efforts at younger and middle ages once risk factors develop to increase the likelihood of healthy longevity.
Data from the Cardiovascular Lifetime Risk Pooling Project, which involved 18 cohort studies and combined data on 257 384 black men and women and white men and women, indicate that at 45 years of age, participants with optimal risk factor profile had a substantially lower lifetime risk of CVD events than those with 1 major risk factor (1.4% versus 39.6% among men; 4.1% versus 20.2% among women). Having ≥2 major risk factors further increased lifetime risk to 49.5% in men and 30.7% in women.31
A recent study examined the association between low lifetime predicted risk for CVD (ie, having all optimal or near-optimal risk factor levels) and burden of subclinical atherosclerosis in younger adults in the CARDIA and MESA studies of the NHLBI. Among participants <50 years of age, nearly half had low and half had high predicted lifetime risk for CVD. Those with low predicted lifetime risk had lower prevalence and less severe amounts of coronary calcification and less carotid intima-media thickening, even at these younger ages, than those with high predicted lifetime risk. During follow-up, those with low predicted lifetime risk also had less progression of coronary calcium.32
Among >7900 men and women from the FHS followed up for 111 000 person-years, median survival was highly associated with risk factor presence and burden at 50 years of age. Men and women with optimal risk factors had a median life expectancy ≥10 years longer than those with ≥2 major risk factors at age 50 years.6
-
In another study, FHS investigators followed up 2531 men and women who were examined between the ages of 40 and 50 years and observed their overall rates of survival and survival free of CVD to 85 years of age and beyond. Low levels of the major risk factors in middle age were associated with overall survival and morbidity-free survival to ≥85 years of age.33
Overall, 35.7% survived to the age of 85 years, and 22% survived to that age free of major morbidities.
Factors associated with survival to the age of 85 years included female sex, lower SBP, lower total cholesterol, better glucose tolerance, absence of current smoking, and higher level of education attained. Factors associated with survival to the age of 85 years free of MI, UA, HF, stroke, dementia, and cancer were nearly identical.
When adverse levels of 4 of these factors were present in middle age, <5% of men and ≈15% of women survived to 85 years of age.
-
Data from the Chicago Heart Association Detection Project (1967–1973, with an average follow-up of 31 years) showed the following:
In younger women (18–39 years of age) with favorable levels for all 5 major risk factors (BP, serum cholesterol, BMI, DM, and smoking), future incidence of CHD and CVD is rare, and long-term and all-cause mortality are much lower than for those who have unfavorable or elevated risk factor levels at young ages. Similar findings applied to men in this study.34
Participants (18–64 years of age at baseline) without a history of MI were investigated to determine whether traditional CVD risk factors were similarly associated with CVD mortality in black and white men and women. In general, the magnitude and direction of associations were similar by race. Most traditional risk factors demonstrated similar associations with mortality in black and white adults of the same sex. Small differences were primarily in the strength and not the direction of the association.35
Remaining lifetime risks for CVD death were noted to increase substantially and in a graded fashion according to the number of risk factors present in middle age (40–59 years of age). However, remaining lifetime risks for non-CVD death also increased dramatically with increasing CVD risk factor burden. These data help to explain the markedly greater longevity experienced by those who reach middle age free of major CVD risk factors.36
Presence of a greater number of risk factors in middle age is associated with lower scores at older ages on assessment of social functioning, mental health, walking, and health perception in women, with similar findings in men.37
Risk factor burden in middle age is associated with better quality of life at follow-up in older age (≈25 years later) and lower average annual Medicare costs at older ages.37,38 Similarly, the existence of a greater number of risk factors in middle age is associated with higher average annual CVD-related and total Medicare costs (once Medicare eligibility is attained).38
A study of 84 129 women enrolled in the Nurses’ Health Study identified 5 healthy lifestyle factors, including absence of current smoking, drinking half a glass or more of wine per day (or equivalent alcohol consumption), ≥30 minutes of moderate or vigorous PA per day, BMI <25 kg/ m2, and dietary score in the top 40% (which included diets with lower amounts of trans fats, lower glycemic load, higher cereal fiber, higher marine omega-3 fatty acids, higher folate, and higher polyunsaturated to saturated fat ratio). When 3 of the 5 healthy lifestyle factors were present, the RR for CHD over a 14-year period was 57% lower; when 4 were present, the RR was 66% lower; and when all 5 factors were present, the RR was 83% lower.39 However, data from NHANES 1999 to 2002 showed that only approximately one third of adults complied with ≥6 of the recommended heart-healthy behaviors. Dietary recommendations in general and daily fruit intake recommendations in particular were least likely to be followed.40
Among individuals 70 to 90 years of age, adherence to a Mediterranean-style diet and greater PA are associated with 65% to 73% relatively lower rates of all-cause mortality, as well as lower mortality rates attributable to CHD, CVD, and cancer.41
Seventeen-year mortality data from the NHANES II Mortality Follow-Up Study indicated that the RR for fatal CHD was 51% lower for men and 71% lower for women with none of 3 major risk factors (hypertension, current smoking, and elevated total cholesterol [≥240 mg/dL]) than for those with ≥1 risk factor. Had all 3 major risk factors not occurred, it is hypothesized that 64% of all CHD deaths among women and 45% of CHD deaths in men could have been avoided.42
Hospital Discharges, Ambulatory Care Visits, Home Healthcare Patients, Nursing Home Residents, and Hospice Care Discharges
(See Table 13-1 and Charts 13-20 and 13-21.)
Chart 13-20.
Hospital discharges for cardiovascular disease (United States: 1970–2010). Hospital discharges include people discharged alive, dead, and “status unknown.” Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
From 2000 to 2010, the number of inpatient discharges from short-stay hospitals with CVD as the first-listed diagnosis decreased from 6 294 000 to 5 802 000 (NHDS, NCHS, and NHLBI). In 2010, CVD ranked highest among all disease categories in hospital discharges (NHDS, NCHS, and NHLBI).
In 2010, there were 75 432 000 physician office visits with a primary diagnosis of CVD (NCHS, NAMCS, NHLBI tabulation). In 2010, there were 4 640 000 ED visits and 7 829 000 hospital outpatient department visits with a primary diagnosis of CVD (NHAMCS, NHLBI tabulation).
In 2009, ≈1 of every 6 hospital stays, or 6 million, resulted from CVD (AHRQ, Nationwide Inpatient Sample). The total inpatient hospital cost for CVD was $71.2 billion, approximately one fourth of the total cost of inpatient hospital care in the United States. The average cost per hospitalization was ≈41% higher than the average cost for all stays. Hospital admissions that originated in the ED accounted for 60.7% of all hospital stays for CVD. This was 41% higher than the rate of 43.1% for all types of hospital stays; 3.3% of patients admitted to the hospital for CVD died in the hospital, which was significantly higher than the average in-hospital death rate of 2.1% for all hospitalized patients.43
In 2004, CAD was estimated to be responsible for 1.2 million hospital stays and was the most expensive condition treated. This condition resulted in >$44 billion in expenses. More than half of the hospital stays for CAD were among patients who also received PCI or CABG during their stay. AMI resulted in $31 billion in inpatient hospital charges for 695 000 hospital stays. The 1.1 million hospitalizations for CHF amounted to nearly $29 billion in hospital charges.44
In 2003, ≈48.3% of inpatient hospital stays for CVD were for women, who accounted for 42.8% of the national cost ($187 billion) associated with these conditions. Although only 40% of hospital stays for AMI and CAD were for women, more than half of all stays for nonspecific chest pain, CHF, and stroke were for women. There was no difference between men and women in hospitalizations for cardiac dysrhythmias.45
Circulatory disorders were the most frequent reason for admission to the hospital through the ED, accounting for 26.3% of all admissions through the ED. After pneumonia, the most common heart-related conditions (in descending order) were CHF, chest pain, hardening of the arteries, and heart attack, which together accounted for >15% of all admissions through the ED. Stroke and irregular heart beat ranked seventh and eighth, respectively.46
Among the 1 492 200 nursing home residents each day in 2004, CVD was the leading primary diagnosis; approximately one fourth of nursing home residents had a primary diagnosis of CVD at admission (23.7% or 353 100 residents) or at the time of interview (25% or 373 000 residents) (NCHS, NNHS).47
Among the 1 459 900 home healthcare patients each day in 2007, CVD was the leading primary diagnosis; almost one fifth of home healthcare patients had a primary diagnosis of CVD at admission into home health care (18.3% or 267 300 residents) or at the time of interview (18.9% or 275 700 residents) (NCHS, NHHCS). The majority (62.9% or 918 900 patients) of home healthcare patients each day in 2007 had any diagnosis of CVD at the time of interview.48
Among the 1 045 100 patients discharged from hospice in 2007, CVD was the primary diagnosis for 15.8% (or 165 100 discharges) at admission and 15.9% (or 165 700 discharges) at discharge. Half (50% or 523 000) of all hospice discharges had any diagnosis of CVD at the time of discharge.48
Operations and Procedures
In 2010, an estimated 7 588 000 inpatient cardiovascular operations and procedures were performed in the United States; 4.4 million were performed on males, and 3.2 million were performed on females (NHLBI tabulation of NHDS, NCHS).
Cost
The estimated direct and indirect cost of CVD for 2010 is $315.4 billion (MEPS, NHLBI tabulation).
By 2030, real (2012$) total direct medical costs of CVD are projected to increase to ≈$918 billion (unpublished AHA tabulation based on methodology described by Heidenreich et al3).
- 1.Blackwell D, Lucas J, Clarke T. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. National Center for Health Statistics. Vital Health Stat 10. In press. [PubMed] [Google Scholar]
- 2.Barnes PM, Adams PF, Powell-Griner E. Advance Data From Vital and Health Statistics; No. 394. Hyattsville, MD: National Center for Health Statistics; 2008. Health characteristics of the Asian adult population: United States, 2004–2006. [PubMed] [Google Scholar]
- 3.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ on behalf of the American Heart Association Advocacy Coordinating Committee; Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Cardiovascular Nursing; Council on the Kidney in Cardiovascular Disease; Council on Cardiovascular Surgery and Anesthesia, and Interdisciplinary Council on Quality of Care and Outcomes Research. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 4.Incidence and Prevalence: 2006 Chart Book on Cardiovascular and Lung Diseases. Bethesda, MD: National Heart, Lung, and Blood Institute; 2006. [Google Scholar]
- 5.Ali T, Jarvis B, O’Leary M. Strong Heart Study Data Book: A Report to American Indian Communities. Rockville, MD: National Institutes of Health, National Heart, Lung, and Blood Institute; 2001. NIH publication No. 01-3285. [Google Scholar]
- 5a.Wilkins JT, Ning H, Berry J, Zhao L, Dyer AR, Lloyd-Jones DM. Lifetime risk and years lived free of total cardiovascular disease. JAMA. 2012;308:1795–1801. doi: 10.1001/jama.2012.14312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, Wolf PA, Levy D. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1999–2010. Series 20 No. 2P. [Accessed July 21, 2013];CDC WONDER Online Database [database online] Released January 2013. http://wonder.cdc.gov/cmf-icd10.html.
- 8.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 9.Murphy SL, Xu JQ, Kochanek KD. National Vital Statistics Report. 4. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2013. Deaths: final data for 2010. [PubMed] [Google Scholar]
- 10.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors [published correction appears in PLoS Med. 2011;8(1). doi:10.1371/ annotation/0ef47acd-9dcc-4296-a897-872d182cde57] PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC) Prevalence and most common causes of disability among adults: United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58:421–426. [PubMed] [Google Scholar]
- 12.Mosca L, Hammond G, Mochari-Greenberger H, Towfighi A, Albert MA on behalf of the American Heart Association Cardiovascular Disease and Stroke in Women and Special Populations Committee of the Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Cardiovascular Nursing, Council on High Blood Pressure Research, and Council on Nutrition, Physical Activity and Metabolism. Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation. 2013;127:1254–1263. doi: 10.1161/CIR.0b013e318287cf2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vanhecke TE, Miller WM, Franklin BA, Weber JE, McCullough PA. Awareness, knowledge, and perception of heart disease among adolescents. Eur J Cardiovasc Prev Rehabil. 2006;13:718–723. doi: 10.1097/01.hjr.0000214611.91490.5e. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC) Racial/ethnic and socioeconomic disparities in multiple risk factors for heart disease and stroke: United States, 2003. MMWR Morb Mortal Wkly Rep. 2005;54:113–117. [PubMed] [Google Scholar]
- 15.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 16.Hozawa A, Folsom AR, Sharrett AR, Chambless LE. Absolute and attributable risks of cardiovascular disease incidence in relation to optimal and borderline risk factors: comparison of African American with white subjects: Atherosclerosis Risk in Communities Study. Arch Intern Med. 2007;167:573–579. doi: 10.1001/archinte.167.6.573. [DOI] [PubMed] [Google Scholar]
- 17.Soni A. Personal Health Behaviors for Heart Disease Prevention Among the U.S. Adult Civilian Noninstitutionalized Population, 2004. Rockville, MD: Agency for Healthcare Research and Quality; Mar, 2007. [Accessed August 3, 2011]. MEPS Statistical Brief No. 165. http://meps.ahrq.gov/mepsweb/data_files/publications/st165/stat165.pdf. [Google Scholar]
- 18.Eamranond PP, Legedza AT, Diez-Roux AV, Kandula NR, Palmas W, Siscovick DS, Mukamal KJ. Association between language and risk factor levels among Hispanic adults with hypertension, hypercholesterolemia, or diabetes. Am Heart J. 2009;157:53–59. doi: 10.1016/j.ahj.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daviglus ML, Talavera GA, Avilés-Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil-Smoller S, Sorlie PD, Stamler J. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chow CK, Islam S, Bautista L, Rumboldt Z, Yusufali A, Xie C, Anand SS, Engert JC, Rangarajan S, Yusuf S. Parental history and myocardial infarction risk across the world: the INTERHEART Study. J Am Coll Cardiol. 2011;57:619–627. doi: 10.1016/j.jacc.2010.07.054. [DOI] [PubMed] [Google Scholar]
- 21.Lloyd-Jones DM, Nam BH, D’Agostino RB, Sr, Levy D, Murabito JM, Wang TJ, Wilson PW, O’Donnell CJ. Parental cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults: a prospective study of parents and offspring. JAMA. 2004;291:2204–2211. doi: 10.1001/jama.291.18.2204. [DOI] [PubMed] [Google Scholar]
- 22.Murabito JM, Pencina MJ, Nam BH, D’Agostino RB, Sr, Wang TJ, Lloyd-Jones D, Wilson PW, O’Donnell CJ. Sibling cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults. JAMA. 2005;294:3117–3123. doi: 10.1001/jama.294.24.3117. [DOI] [PubMed] [Google Scholar]
- 23.Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score [published correction appears in JAMA. 2007;297:1433] JAMA. 2007;297:611–619. doi: 10.1001/jama.297.6.611. [DOI] [PubMed] [Google Scholar]
- 24.Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the prospective cardiovascular Münster (PROCAM) study [published correction appears in Circulation. 2002;105:900] Circulation. 2002;105:310–315. doi: 10.1161/hc0302.102575. [DOI] [PubMed] [Google Scholar]
- 25.Parikh NI, Hwang SJ, Larson MG, Cupples LA, Fox CS, Manders ES, Murabito JM, Massaro JM, Hoffmann U, O’Donnell CJ. Parental occurrence of premature cardiovascular disease predicts increased coronary artery and abdominal aortic calcification in the Framingham Offspring and Third Generation cohorts. Circulation. 2007;116:1473–1481. doi: 10.1161/CIRCULATIONAHA.107.705202. [DOI] [PubMed] [Google Scholar]
- 26.Nasir K, Budoff MJ, Wong ND, Scheuner M, Herrington D, Arnett DK, Szklo M, Greenland P, Blumenthal RS. Family history of premature coronary heart disease and coronary artery calcification: Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2007;116:619–626. doi: 10.1161/CIRCULATIONAHA.107.688739. [DOI] [PubMed] [Google Scholar]
- 27.Lee DS, Pencina MJ, Benjamin EJ, Wang TJ, Levy D, O’Donnell CJ, Nam BH, Larson MG, D’Agostino RB, Vasan RS. Association of parental heart failure with risk of heart failure in offspring. N Engl J Med. 2006;355:138–147. doi: 10.1056/NEJMoa052948. [DOI] [PubMed] [Google Scholar]
- 28.Friedlander Y, Siscovick DS, Arbogast P, Psaty BM, Weinmann S, Lemaitre RN, Raghunathan TE, Cobb LA. Sudden death and myocardial infarction in first degree relatives as predictors of primary cardiac arrest. Atherosclerosis. 2002;162:211–216. doi: 10.1016/s0021-9150(01)00701-8. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC) Awareness of family health history as a risk factor for disease: United States, 2004. MMWR Morb Mortal Wkly Rep. 2004;53:1044–1047. [PubMed] [Google Scholar]
- 30.Bachmann JM, Willis BL, Ayers CR, Khera A, Berry JD. Association between family history and coronary heart disease death across long-term follow-up in men: the Cooper Center Longitudinal Study. Circulation. 2012;125:3092–3098. doi: 10.1161/CIRCULATIONAHA.111.065490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, Greenland P, Van Horn L, Tracy RP, Lloyd-Jones DM. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–329. doi: 10.1056/NEJMoa1012848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Berry JD, Liu K, Folsom AR, Lewis CE, Carr JJ, Polak JF, Shea S, Sidney S, O’Leary DH, Chan C, Lloyd-Jones DM. Prevalence and progression of subclinical atherosclerosis in younger adults with low short-term but high lifetime estimated risk for cardiovascular disease: the Coronary Artery Risk Development in Young Adults Study and Multi-Ethnic Study of Atherosclerosis. Circulation. 2009;119:382–389. doi: 10.1161/CIRCULATIONAHA.108.800235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Terry DF, Pencina MJ, Vasan RS, Murabito JM, Wolf PA, Hayes MK, Levy D, D’Agostino RB, Benjamin EJ. Cardiovascular risk factors predictive for survival and morbidity-free survival in the oldest-old Framingham Heart Study participants. J Am Geriatr Soc. 2005;53:1944–1950. doi: 10.1111/j.1532-5415.2005.00465.x. [DOI] [PubMed] [Google Scholar]
- 34.Daviglus ML, Stamler J, Pirzada A, Yan LL, Garside DB, Liu K, Wang R, Dyer AR, Lloyd-Jones DM, Greenland P. Favorable cardiovascular risk profile in young women and long-term risk of cardiovascular and all-cause mortality. JAMA. 2004;292:1588–1592. doi: 10.1001/jama.292.13.1588. [DOI] [PubMed] [Google Scholar]
- 35.Carnethon MR, Lynch EB, Dyer AR, Lloyd-Jones DM, Wang R, Garside DB, Greenland P. Comparison of risk factors for cardiovascular mortality in black and white adults. Arch Intern Med. 2006;166:1196–1202. doi: 10.1001/archinte.166.11.1196. [DOI] [PubMed] [Google Scholar]
- 36.Lloyd-Jones DM, Dyer AR, Wang R, Daviglus ML, Greenland P. Risk factor burden in middle age and lifetime risks for cardiovascular and non-cardiovascular death (Chicago Heart Association Detection Project in Industry) Am J Cardiol. 2007;99:535–540. doi: 10.1016/j.amjcard.2006.09.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Daviglus ML, Liu K, Pirzada A, Yan LL, Garside DB, Feinglass J, Guralnik JM, Greenland P, Stamler J. Favorable cardiovascular risk profile in middle age and health-related quality of life in older age. Arch Intern Med. 2003;163:2460–2468. doi: 10.1001/archinte.163.20.2460. [DOI] [PubMed] [Google Scholar]
- 38.Daviglus ML, Liu K, Greenland P, Dyer AR, Garside DB, Manheim L, Lowe LP, Rodin M, Lubitz J, Stamler J. Benefit of a favorable cardiovascular risk-factor profile in middle age with respect to Medicare costs. N Engl J Med. 1998;339:1122–1129. doi: 10.1056/NEJM199810153391606. [DOI] [PubMed] [Google Scholar]
- 39.Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000;343:16–22. doi: 10.1056/NEJM200007063430103. [DOI] [PubMed] [Google Scholar]
- 40.Wright JD, Hirsch R, Wang CY. One-third of U.S adults embraced most heart healthy behaviors in 1999–2002. NCHS Data Brief. 2009;(17):1–8. [PubMed] [Google Scholar]
- 41.Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, van Staveren WA. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292:1433–1439. doi: 10.1001/jama.292.12.1433. [DOI] [PubMed] [Google Scholar]
- 42.Mensah GA, Brown DW, Croft JB, Greenlund KJ. Major coronary risk factors and death from coronary heart disease: baseline and follow-up mortality data from the Second National Health and Nutrition Examination Survey (NHANES II) Am J Prev Med. 2005;29(suppl 1):68–74. doi: 10.1016/j.amepre.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 43.Russo CA, Ho K, Elixhauser A. Hospital Stays for Circulatory Diseases, 2004. Rockville, MD: Agency for Healthcare Research and Quality; Feb, 2007. [Accessed August 3, 2011]. HCUP Statistical Brief 26. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb26.pdf. [PubMed] [Google Scholar]
- 44.Russo CA, Andrews RM. The National Hospital Bill: The Most Expensive Conditions, by Payer, 2004. Rockville, MD: Agency for Healthcare Research and Quality; Sep, 2006. [Accessed August 3, 2011]. HCUP Statistical Brief No. 13. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb13.pdf. [PubMed] [Google Scholar]
- 45.Elixhauser A, Jiang HJ. Hospitalizations for Women With Circulatory Disease, 2003. Rockville, MD: Agency for Healthcare Research and Quality; May, 2006. [Accessed August 3, 2011]. HCUP Statistical Brief No. 5. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb5.pdf. [PubMed] [Google Scholar]
- 46.Elixhauser A, Owens P. Reasons for Being Admitted to the Hospital Through the Emergency Department, 2003. Rockville, MD: Agency for Health Care Research and Quality; Feb, 2006. [Accessed June 27, 2011]. HCUP Statistical Brief No. 2. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb2.pdf. [PubMed] [Google Scholar]
- 47.Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 overview. Vital Health Stat 13. 2009;(167):1–155. [PubMed] [Google Scholar]
- 48.Caffrey C, Sengupta M, Moss A, Harris-Kojetin L, Valverde R. Home health care and discharged hospice care patients: United States, 2000 and 2007. Natl Health Stat Report. 2011;(38):1–27. [PubMed] [Google Scholar]
- 49.2007 State snapshots. [Accessed October 21, 2013];Agency for Healthcare Research and Quality Web site. http://statesnapshots.ahrq.gov/snaps07/index.jsp.
- 50.Brett KM, Hayes SG. Women’s Health and Mortality Chartbook. Washington, DC: US Department of Health and Human Services, Office on Women’s Health; 2004. [Accessed October 21, 2013]. DHHS publication No. 04-1032. http://www.cdc.gov/nchs/data/healthywomen/womenschartbook_aug2004.pdf. [Google Scholar]
- 51.SMART: BRFSS city and county data: selected metropolitan/micropolitan area risk trends. [Accessed October 21, 2013];Centers for Disease Control and Prevention Web site. http://apps.nccd.cdc.gov/BRFSS-SMART/
- 52.Behavioral Risk Factor Surveillance System: prevalence and trends data. [Accessed June 4, 2013];Centers for Disease Control and Prevention Web site. http://apps.nccd.cdc.gov/brfss/index.asp.
- 53.Geographic Information Systems (GIS) at CDC. [Accessed October 21, 2013];Centers for Disease Control and Prevention Web site. http://www.cdc.gov/gis/
- 54.Casper ML, Nwaise IA, Croft JB, Nilasena DS. Atlas of Stroke Hospitalizations Among Medicare Beneficiaries. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 55.Deleted in proof.
- 56.Lloyd-Jones DM, Wang TJ, Leip EP, Larson MG, Levy D, Vasan RS, D’Agostino RB, Massaro JM, Beiser A, Wolf PA, Benjamin EJ. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110:1042–1046. doi: 10.1161/01.CIR.0000140263.20897.42. [DOI] [PubMed] [Google Scholar]
- 57.Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D’Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ, Levy D Framingham Heart Study. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068–3072. doi: 10.1161/01.cir.0000039105.49749.6f. [DOI] [PubMed] [Google Scholar]
- 58.Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, Wolf PA. The lifetime risk of stroke: estimates from the Framingham Study. Stroke. 2006;37:345–350. doi: 10.1161/01.STR.0000199613.38911.b2. [DOI] [PubMed] [Google Scholar]
- 59.Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles’, or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149:2445–2448. [PubMed] [Google Scholar]
- 60.Howlader N, Noone AM, Krapcho M, Garshell J, Neyman N, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA, editors. SEER Cancer Statistics Review, 1975–2010. National Cancer Institute; Bethesda, MD: [Accessed July 22, 2013]. http://seer.cancer.gov/csr/1975_2010/. Based on November 2012 SEER data submission. SEER Web site. Posted April 2013. [Google Scholar]
- 61.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290:1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 62.Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D’Agostino RB, Levy D. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287:1003–1010. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 63.Vasan RS, Pencina MJ, Cobain M, Freiberg MS, D’Agostino RB. Estimated risks for developing obesity in the Framingham Heart Study. Ann Intern Med. 2005;143:473–480. doi: 10.7326/0003-4819-143-7-200510040-00005. [DOI] [PubMed] [Google Scholar]
- 64.D’Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
14. Stroke (Cerebrovascular Disease)
ICD-9 430 to 438; ICD-10 I60 to I69. See Tables 14-1 and 14-2 and Charts 14-1 through 14-12.
Table 14-1.
Stroke
| Population Group | Prevalence, 2010: Age ≥20 y | New and Recurrent Attacks, All Ages | Mortality, 2010: All Ages* | Hospital Discharges, 2010: All Ages | Cost, 2010 |
|---|---|---|---|---|---|
| Both sexes | 6 800 000 (2.8%) | 795 000 | 129 476 | 1 015 000 | $36.5 Billion |
| Males | 3 000 000 (2.6%) | 370 000 (46.5%)† | 52 367 (40.4%)† | 485 000 | … |
| Females | 3 800 000 (3.0%) | 425 000 (53.5%)† | 77 109 (59.6%)† | 530 000 | … |
| NH white males | 2.4% | 325 000‡ | 43 424 | … | … |
| NH white females | 2.9% | 365 000‡ | 65 695 | … | … |
| NH black males | 4.3% | 45 000‡ | 6938 | … | … |
| NH black females | 4.7% | 60 000‡ | 9027 | … | … |
| Mexican American males | 2.3% | … | … | … | … |
| Mexican American females | 1.4% | … | … | … | … |
| Hispanic or Latino | 2.7%§ | … | … | … | … |
| Asian | 1.8%§ | … | 3 833|| | … | … |
| American Indian or Alaska Native | 4.3%§¶ | … | 559 | … | … |
NH indicates non-Hispanic. Ellipses (…) indicate data not available.
Mortality data for the white, black, Asian or Pacific Islander, and American Indian or Alaska Native populations include deaths of people of Hispanic and non-Hispanic origin. Numbers of deaths for the American Indian or Alaska Native and Asian or Pacific Islander populations are known to be underestimated.
These percentages represent the portion of total stroke incidence or mortality that applies to males vs females.
Estimates include Hispanics and non-Hispanics. Estimates for whites include other nonblack races.
National Health Interview Survey (2012), National Center for Health Statistics; data are weighted percentages for Americans ≥18 y of age.218
Includes Chinese, Filipino, Hawaiian, Japanese, and other Asian or Pacific Islander.
Estimate considered unreliable or does not meet standards of reliability or precision.
Sources: Prevalence: National Health and Nutrition Examination Survey 2007 to 2010, National Center for Health Statistics (NCHS) and National Heart, Lung, and Blood Institute (NHLBI). Percentages for racial/ethnic groups are age adjusted for Americans ≥20 y of age. Age-specific percentages are extrapolated to the 2010 US population. Incidence: Greater Cincinnati/Northern Kentucky Stroke Study/National Institutes of Neurological Disorders and Stroke data for 1999 provided on August 1, 2007. US estimates compiled by NHLBI. See also Kissela et al.219 Data include children. Mortality: Centers for Disease Control and Prevention/NCHS, 2010 Mortality Multiple Cause-of-Death–United States, version dated May 21, 2013. These data represent underlying cause of death only. Mortality data for white and black males and females include Hispanics. Hospital discharges: National Hospital Discharge Survey, NCHS. Data include those inpatients discharged alive, dead, or status unknown. Cost: NHLBI. Data include estimated direct and indirect costs for 2010.
Table 14-2.
Modifiable Stroke Risk Factors
| Factor | Prevalence, % | PAR, %* | RR |
|---|---|---|---|
| Cigarette smoking | |||
| Overall | 19.8 | 12–14† | 1.9 |
| Men | 22.3 | ||
| Women | 17.4 | ||
| Hypertension | ‡ | 8 | |
| Ages 20–34 y | |||
| Men | 13.4 | 99 | |
| Women | 6.2 | 98 | |
| Ages 35–44 y | |||
| Men | 23.2 | 99 | |
| Women | 16.5 | 106 | |
| Ages 45–54 y | |||
| Men | 36.2 | 100 | |
| Women | 35.9 | 103 | |
| Ages 55–64 y | |||
| Men | 53.7 | 100 | |
| Women | 55.8 | 102 | |
| Ages 65–74 y | |||
| Men | 64.7 | 100 | |
| Women | 69.6 | 101 | |
| Ages ≥75 y | |||
| Men | 64.1 | 100 | |
| Women | 76.4 | 101 | |
| Diabetes | 7.3 | 5–27 | 1.8–6.0 |
| High total cholesterol | Data calculated for highest quintile (20%) vs lowest quintile | 9.1 (5.7–13.8) | 1.5 (95% CI, 1.3–1.8) |
| Continuous risk for ischemic stroke | … | 1.25 per 1-mmol/L (38.7 mg/dL) increase | |
| Low HDL cholesterol | |||
| <40 mg/dL | |||
| Men | 35 | ||
| Women | 15 | ||
| Data calculated for highest quintile (20%) vs lowest quintile | 23.7 | 0.4 | |
| <35 mg/dL | 26 | 20.6 (10.1–30.7) | 2.00 (95% CI, 1.43–2.70) |
| Continuous risk for ischemic stroke | ≈0.5–0.6 for each 1-mmol/L increase | ||
| AF (nonvalvular) | |||
| Overall age, y | |||
| 50–59 | 0.5 | 1.5 | 4.0 |
| 60–69 | 1.8 | 2.8 | 2.6 |
| 70–79 | 4.8 | 9.9 | 3.3 |
| 80–89 | 8.8 | 23.5 | 4.5 |
| Asymptomatic carotid stenosis | 2–8 | 2–7§ | 2.0 |
| Sickle cell disease | 0.25 (of blacks) | … | 200–400|| |
| Postmenopausal hormone therapy | 25 (Women 50–74 y of age) | 9 | 1.4 |
| Oral contraceptive use | 13 (women 25–44 y) | 9.4 | 2.3 |
| Dietary factors | |||
| Na intake >2300 mg | 75–90 | Unknown | Unknown |
| K intake <4700 mg | 90–99 | Unknown | Unknown |
| Physical inactivity | 25 | 30 | 2.7 |
| Obesity | 1.39 Stroke death per increase of 5 kg/m2 | ||
| Men | 33.3 | ||
| Women | 35.3 | ||
| CHD | |||
| Men | 8.4 | 5.8 | 1.73 (1.68–1.78) |
| Women | 5.6 | 3.9¶ | 1.55 (1.17–2.07) |
| Heart failure | |||
| Men | 2.6 | 1.4 | |
| Women | 2.1 | 1.1¶ | |
| Peripheral arterial disease | 4.9 | 3.0¶ | |
AF indicates atrial fibrillation; CHD, coronary heart disease; CI, confidence interval; HDL, high-density lipoprotein; PAR, population attributable risk; and RR, relative risk.
PAR is the proportion of ischemic stroke in the population that can be attributed to a particular risk factor (see Goldstein et al96 for formula).
PAR is for stroke deaths, not ischemic stroke incidence.
PAR percent=100×{[prevalence (RR-1)/prevalence (RR-1)+1]}.
Calculated on the basis of referenced data provided in the table or text.
Relative to stroke risk in children without sickle cell disease.
Calculated on the basis of point estimates of referenced data provided in the table. For peripheral arterial disease, calculation was based on average RR for men and women.
Adapted from Goldstein et al96 with permission. Copyright © 2011, American Heart Association, Inc.
Chart 14-1.
Prevalence of stroke by age and sex (National Health and Nutrition Examination Survey: 2007–2010). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 14-12.
Trends in carotid endarterectomy and carotid stenting procedures (United States: 1980–2010). Source: Nationwide Inpatient Sample, Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality.
Stroke Prevalence
(See Table 14-1 and Chart 14-1.)
An estimated 6.8 million Americans ≥20 years of age have had a stroke (extrapolated to 2010 by use of NHANES 2007–2010 data). Overall stroke prevalence during this period is an estimated 2.8% (NHANES, NHLBI).
According to data from the 2012 BRFSS (CDC), 2.9% of men and 2.9% of women ≥18 years of age had a history of stroke; 3.0% of non-Hispanic whites, 3.8% of non-Hispanic blacks, 1.9% of Asian/Pacific Islanders, 1.8% of Hispanics (of any race), 5.8% of American Indian/Alaska Natives, and 4.1% of other races or multiracial people had a history of stroke.1
Over the time period 2006 to 2010, data from BRFSS show that the overall self-reported stroke prevalence did not change. Older adults, blacks, people with lower levels of education, and people living in the southeastern United States had higher stroke prevalence.2
The prevalence of silent cerebral infarction is estimated to range from 6% to 28%, with higher prevalence with increasing age.3–5 The prevalence estimates also vary depending on the population studied (eg, ethnicity, sex, risk factor profile), definition of silent cerebral infarction, and imaging technique. It has been estimated that 13 million people had prevalent silent stroke in the 1998 US population.6,7
The prevalence of stroke-related symptoms was found to be relatively high in a general population free of a prior diagnosis of stroke or TIA. On the basis of data from 18 462 participants enrolled in a national cohort study, 17.8% of the population >45 years of age reported at least 1 symptom. Stroke symptoms were more likely among blacks than whites, among those with lower income and lower educational attainment, and among those with fair to poor perceived health status. Symptoms also were more likely in participants with higher Framingham stroke risk score (REGARDS, NINDS).8
Projections show that by 2030, an additional 3.4 million people aged ≥18 years will have had a stroke, a 20.5% increase in prevalence from 2012. The highest increase (29%) is projected to be in Hispanic men.9
Individuals with atherosclerotic stroke should be included among those deemed to be at high risk (20% over 10 years) of further atherosclerotic coronary events. For primary prevention, ischemic stroke should be included among CVD outcomes in absolute risk assessment algorithms. The inclusion of atherosclerotic ischemic stroke as a high-risk condition has important implications, because the number of patients considered to be at high risk will increase over time.10
Abbreviations Used in Chapter 14
| ACCORD | Action to Control Cardiovascular Risk in Diabetes |
| AF | atrial fibrillation |
| AHA | American Heart Association |
| AHI | apnea-hypopnea index |
| ARIC | Atherosclerosis Risk in Communities study |
| AHRQ | Agency for Healthcare Research and Quality |
| BASIC | Brain Attack Surveillance in Corpus Christi |
| BP | blood pressure |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CDC | Centers for Disease Control and Prevention |
| CHD | coronary heart disease |
| CHS | Cardiovascular Health Study |
| CI | confidence interval |
| CLRD | chronic lower respiratory disease |
| CREST | Carotid Revascularization Endarterectomy versus Stenting Trial |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| ED | emergency department |
| eGFR | estimated glomerular filtration rate |
| EMS | emergency medical services |
| FHS | Framingham Heart Study |
| FRS | Framingham Risk Score |
| FUTURE | Follow-up of TIA and Stroke Patients and Unelucidated Risk Factor Evaluation |
| GCNKSS | Greater Cincinnati/Northern Kentucky Stroke Study |
| GFR | glomerular filtration rate |
| GWTG | Get With The Guidelines |
| HBP | high blood pressure |
| HCUP | Healthcare Cost and Utilization Project |
| HD | heart disease |
| HDL | high-density lipoprotein |
| HF | heart failure |
| HR | hazard ratio |
| ICD-9 | International Classification of Diseases, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| ICH | intracerebral hemorrhage |
| MEPS | Medical Expenditure Panel Survey |
| MI | myocardial infarction |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHAMCS | National Hospital Ambulatory Medical Care Survey |
| NHANES | National Health and Nutrition Examination Survey |
| NHDS | National Hospital Discharge Survey |
| NHIS | National Health Interview Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| NINDS | National Institutes of Neurological Disorders and Stroke |
| NOMAS | Northern Manhattan Study |
| ONTARGET | Ongoing Telmisartan Alone and in Combination With Ramipril Global Endpoint Trial |
| OR | odds ratio |
| PA | physical activity |
| PAR | population attributable risk |
| REGARDS | Reasons for Geographic and Racial Differences in Stroke study |
| RR | relative risk |
| SAH | subarachnoid hemorrhage |
| SPS3 | Secondary Prevention of Small Subcortical Strokes |
| SBP | systolic blood pressure |
| SWITCH | Stroke With Transfusions Changing to Hydroxyurea |
| TIA | transient ischemic attack |
| tPA | tissue-type plasminogen activator |
Stroke Incidence
(See Table 14-1 and Charts 14-2 through 14-5.)
Chart 14-2.
Annual age-adjusted incidence of first-ever stroke by race. Hospital plus out-of-hospital ascertainment, 1993 to 1994, 1999, and 2005. ICH indicates intracerebral hemorrhage; and SAH, subarachnoid hemorrhage. Data derived from Kleindorfer et al.11
Chart 14-5.
Age-adjusted incidence of stroke/transient ischemic attack by race and sex, ages 45 to 74, Atherosclerosis Risk in Communities study cohort, 1987 to 2001. Data derived from the National Heart, Lung, and Blood Institute, Incidence and Prevalence: 2006 Chart Book.220
Each year, ≈795 000 people experience a new or recurrent stroke. Approximately 610 000 of these are first attacks, and 185 000 are recurrent attacks (GCNKSS, NINDS, and NHLBI; GCNKSS and NINDS data for 1999 provided July 9, 2008; estimates compiled by NHLBI).
Of all strokes, 87% are ischemic and 10% are ICH strokes, whereas 3% are SAH strokes (GCNKSS, NINDS, 1999).
On average, every 40 seconds, someone in the United States has a stroke (AHA computation based on the latest available data).
Each year, ≈55 000 more women than men have a stroke (GCNKSS, NINDS).11
Women have a higher lifetime risk of stroke than men. In the FHS, lifetime risk of stroke among those 55 to75 years of age was 1 in 5 for women (20% to 21%) and ≈1 in 6 for men (14% to 17%).12
Women have lower age-adjusted stroke incidence than men; however, sex differences in stroke risk may be modified by age.13 Data from FHS demonstrate that compared with white men, white women 45 to 84 years of age have lower stroke risk than men, but this association is reversed in older ages such that women >85 years of age have elevated risk compared with men.14 Similarly, a population-based study in Sweden found stroke incidence to be lower for women than for men at ages 55 to 64 years, but at 75 to 85 years of age, this association reversed, and women had a higher incidence than men.15 Other studies report an excess risk of stroke in men compared with women that persists throughout the life course or that diminishes but does not reverse with age.16–20
Temporal trend data from the BASIC Project for the time period 2000 through 2010 demonstrated that ischemic stroke rates declined significantly in people aged ≥60 years but remained largely unchanged over time in those aged 45 to 59 years. Rates of decline did not differ significantly for non-Hispanic whites and Mexican Americans in any age group. Therefore, ethnic disparities in stroke rates in the 45- to 59-year-old and 60- to 74-year-old age groups persist.21
In the national REGARDS cohort, in 27 744 participants followed up for 4.4 years (2003–2010), the overall age- and sex-adjusted black/white incidence rate ratio was 1.51, but for ages 45 to 54 years, it was 4.02, whereas for those ≥85 years of age, it was 0.86.22 Similar trends for decreasing black/white incidence rate ratio with age were seen in the GCNKSS.23
Analysis of data from the FHS suggests that stroke incidence is declining over time in this largely white cohort. Data from 1950 to 1977, 1978 to 1989, and 1990 to 2004 showed that the age-adjusted incidence of first stroke per 1000 person-years in each of the 3 periods was 7.6, 6.2, and 5.3 in men and 6.2, 5.8, and 5.1 in women, respectively. Lifetime risk for incident stroke at 65 years of age decreased significantly in the latest data period compared with the first, from 19.5% to 14.5% in men and from 18.0% to 16.1% in women.24
In a similar fashion, data from the most recent GCNKSS show that compared with the 1990s, when incidence rates of stroke were stable, stroke incidence in 2005 was decreased for whites. A similar decline was not seen in blacks. These changes for whites were driven by a decline in ischemic strokes. There were no changes in incidence of ischemic stroke for blacks or of hemorrhagic strokes in blacks or whites.11
In an analysis of temporal trends in ischemic stroke incidence stratified by age, the GCNKSS found an increased incidence of ischemic stroke over time for both blacks and whites aged 20 to 54 years, especially in 2005 compared with earlier time periods. There were declining incidence rates in the oldest age groups for both race groups.25
The BASIC Project (NINDS) demonstrated an increased incidence of stroke among Mexican Americans compared with non-Hispanic whites in a community in southeast Texas. The crude 3-year cumulative incidence (2000–2002) was 16.8 per 1000 in Mexican Americans and 13.6 per 1000 in non-Hispanic whites. Specifically, Mexican Americans had a higher cumulative incidence for ischemic stroke at younger ages (45–59 years of age: RR, 2.04; 95% CI, 1.55–2.69; 60–74 years of age: RR, 1.58; 95% CI, 1.31–1.91) but not at older ages (≥75 years of age: RR, 1.12; 95% CI, 0.94–1.32). Mexican Americans also had a higher incidence of ICH and SAH than non-Hispanic whites, after adjustment for age.26
The age-adjusted incidence of first ischemic stroke per 1000 was 0.88 in whites, 1.91 in blacks, and 1.49 in Hispanics according to data from NOMAS (NINDS) for 1993 to 1997. Among blacks, compared with whites, the relative rate of intracranial atherosclerotic stroke was 5.85; of extracranial atherosclerotic stroke, 3.18; of lacunar stroke, 3.09; and of cardioembolic stroke, 1.58. Among Hispanics (primarily Cuban and Puerto Rican), compared with whites, the relative rate of intracranial atherosclerotic stroke was 5.00; of extracranial atherosclerotic stroke, 1.71; of lacunar stroke, 2.32; and of cardioembolic stroke, 1.42.27
Among 4507 American Indian participants without a prior stroke in the Strong Heart Study in 1989 to 1992, the age- and sex-adjusted incidence of stroke through 2004 was 6.79 per 100 person-years, with 86% of incident strokes being ischemic.28
In the GCNKSS, the annual incidence of anticoagulant-associated ICH per 100 000 people increased from 0.8 (95% CI, 0.3–1.3) in 1988 to 1.9 (95% CI, 1.1–2.7) in 1993/1994 and 4.4 (95% CI, 3.2–5.5) in 1999 (P<0.001 for trend). Among people ≥80 years of age, the rate of anticoagulant-associated ICH increased from 2.5 (95% CI, 0–7.4) in 1988 to 45.9 (95% CI, 25.6–66.2) in 1999 (P<0.001 for trend).29
TIA: Prevalence, Incidence, and Prognosis
In a nationwide survey of US adults, the estimated prevalence of self-reported physician-diagnosed TIA was 2.3%, which translates to ≈5 million people. The true prevalence of TIA is greater, because many patients who experience neurological symptoms consistent with a TIA fail to report it to their healthcare provider.30
In the GCNKS, according to data from 1993 and 1994, the age-, sex-, and race-adjusted incidence rate for TIA was 0.83 per 10 000.31 The age- and sex-adjusted incidence rate for TIA in Rochester, MN, was estimated at 0.68 per 1000 for the years 1985 through 1989.32 In a more recent Italian community-based registry conducted in 2007 to 2009, the crude TIA incidence rate was 0.52 per 1000.33
The prevalence of physician-diagnosed TIA increases with age.30 Incidence of TIA increases with age and varies by sex and race/ethnicity. Men, blacks, and Mexican Americans have higher rates of TIA than their female and non-Hispanic white counterparts.26,31,33
Approximately 15% of all strokes are heralded by a TIA.34
TIAs confer a substantial short-term risk of stroke, hospitalization for CVD events, and death. Of 1707 TIA patients evaluated in the ED of Kaiser Permanente Northern California, a large, integrated healthcare delivery system, 180 (11%) experienced a stroke within 90 days. Ninety-one patients (5%) had a stroke within 2 days. Predictors of stroke included age >60 years, DM, focal symptoms of weakness or speech impairment, and TIA that lasted >10 minutes.35
Meta-analyses of cohorts of patients with TIA have shown the short-term risk of stroke after TIA to be ≈3% to 10% at 2 days and 9% to 17% at 90 days.36,37
Individuals who have a TIA and survive the initial high-risk period have a 10-year stroke risk of roughly 19% and a combined 10-year stroke, MI, or vascular death risk of 43% (4% per year).38
Within 1 year of TIA, ≈12% of patients will die.31
It is estimated that one third of episodes characterized as TIA according to the classic definition (ie, focal neurological deficits that resolve within 24 hours) would be considered infarctions on the basis of diffusion-weighted magnetic resonance imaging findings.39
Recurrent Stroke
In a cohort of 10 399 patients discharged with a primary diagnosis of stroke in the state of South Carolina in 2002, recurrent stroke rates were 1.8% at 1 month, 5% at 6 months, 8% at 1 year, and 18.1% at 4 years.40
In the REGARDS cohort with 5 years of follow-up, participants with self-reported stroke symptoms, TIA, distant stroke, or recent stroke all had increased risk of future stroke compared with those with no symptoms. After risk factor adjustment, there was a monotonically increasing risk of subsequent stroke across this symptomatic spectrum.41
Annual recurrent stroke rates in control arms of stroke prevention trials fell from 8.71% in trials launched in the 1960s to 6.10% in the 1970s, 5.41% in the 1980s, 4.04% in the 1990s, and 4.98% in the 2000s. Assuming a continued linear decline, the annual recurrent stroke rate in trial control arms in the coming decade is projected to be 2.25%.42
From 1994 to 2002, 1-year recurrent ischemic stroke rates declined by almost 5% among elderly Medicare beneficiaries, but declines were heterogeneous across geographic regions of the United States.43
Among 600 Scandinavian stroke patients followed up for 2 years, 55 (9.2%) had had a recurrent stroke, 15 (2.5%) had a TIA, 4 (0.7%) had a coronary event, and 24 (4.0%) had died. Recurrent stroke occurred in 19.2% of patients with index stroke caused by large-artery disease, 4.9% with small-vessel disease, 8.2% with cardioembolic cause, 5.6% with cryptogenic cause, and 12.8% of other and undetermined cause combined.44
Recurrent stroke is associated with a greater number of risk factors and a higher incidence of large-artery atherosclerosis than the first stroke.45
Among 1626 first-ever stroke patients in the South London Register,46 first stroke recurrence rates during the first, second, third, fourth, and fifth years were 8% (95% CI, 6.5%–9.8%), 3.3% (2.2%–4.9%), 3.5% (2.1%–5.8%), 1.2% (0.4%–3.7%), and 1.8% (0.4%–7.4%). Cumulative risks of first stroke recurrence were 2.6% (1.9%–3.7%) at 3 months, 8.0% (6.5%–9.8%) at 1 year, 14.1% (11.8 %–16.7%) at 3 years, and 16.6% (13.5%–20.4%) at 5 years.46
Stroke Mortality
(See Table 14-1 and Charts 14-6 and 14-7.)
Chart 14-6.
Age-adjusted death rates for stroke by sex and race/ethnicity, 2010. Death rates for the American Indian/Alaska Native and Asian or Pacific Islander populations are known to be underestimated. Stroke includes International Classification of Diseases, 10th Revision codes I60 to I69 (cerebrovascular disease). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 14-7.
Stroke death rates, 2008 through 2010. Adults ≥35 years of age, by county. Rates are spatially smoothed to enhance the stability of rates in counties with small populations. International Classification of Diseases, 10th Revision codes for stroke: I60 to I69. Data source: National Vital Statistics System and the US Census Bureau.
On average, every 4 minutes, someone dies of a stroke (NCHS, NHLBI).47
Stroke accounted for ≈1 of every 19 deaths in the United States in 2010.47
When considered separately from other CVDs, stroke ranks No. 4 among all causes of death, behind diseases of the heart, cancer, and CLRD (NCHS mortality data). The number of deaths with stroke as an underlying cause in 2010 was 129 476; any-mention mortality in 2010 was 217 621, and the age-adjusted death rate for stroke as an underlying cause of death was 39.1 per 100 000.47
Approximately 55% of stroke deaths in 2010 occurred out of the hospital (unpublished tabulation from NCHS 2010 mortality data set).
More women than men die of stroke each year because of the larger number of elderly women. Women accounted for almost 60% of US stroke deaths in 2010 (AHA tabulation).47
From 2000 to 2010, the annual stroke death rate decreased 35.8% and the actual number of stroke deaths declined 22.8% (AHA computation).47,48
-
Conclusions about changes in stroke death rates from 1981 to 2009 are as follows:
There was a greater decline in stroke death rates in men than in women, with a male-to-female ratio that decreased from 1.11 to 1.05 (age adjusted).
Stroke death rates declined more in people aged 45 to 64 years (−51.7%) than in those ≥65 years of age (−48.3%) or those aged 18 to 44 years (−37.8%).49
The decline in stroke mortality over the past several decades, a major improvement in population health observed for both sexes and all race and age groups, is the result of reduced stroke incidence and lower case fatality rates. The significant improvements in stroke outcomes are concurrent with cardiovascular risk factor control interventions. The hypertension control efforts initiated in the 1970s appear to have had the most substantial influence on the accelerated decline in stroke mortality, with lower blood pressure distributions in the population. Control of DM and dyslipidemia, as well as smoking cessation programs, particularly in combination with hypertension treatment, also appear to have contributed to the decline in stroke mortality.50
In examining trends in stroke mortality by US census divisions between 1999 and 2007 for people ≥45 years of age, the rate of decline varied by geographic region and race/ ethnic group. Among black and white women and white men, rates declined by ≥2% annually in every census division, but among black men, rates declined little in the East and West South Central divisions.51
From 1995 to 1998, age-standardized mortality rates for ischemic stroke, SAH, and ICH were higher among blacks than whites. Death rates attributable to ICH also were higher among Asians/Pacific Islanders than among whites. All minority populations had higher death rates attributable to SAH than did whites. Among adults 25 to 44 years of age, blacks and American Indian/Alaska Natives had higher risk ratios for stroke mortality than did whites for all 3 stroke subtypes. Age-standardized mortality rates for ischemic stroke and ICH were lower for Hispanics than for whites.52
In 2002, death certificate data showed that the mean age at stroke death was 79.6 years; however, males had a younger mean age at stroke death than females. Blacks, American Indian/Alaska Natives, and Asian/Pacific Islanders had younger mean ages than whites, and the mean age at stroke death was also younger among Hispanics than non-Hispanics.53
A report released by the CDC in collaboration with the Centers for Medicare & Medicaid Services, the Atlas of Stroke Hospitalizations Among Medicare Beneficiaries, found that in Medicare beneficiaries over the time period 1995 to 2002, the 30-day mortality rate varied by age: 9% in patients 65 to 74 years of age, 13.1% in those 74 to 84 years of age, and 23% in those ≥85 years of age.54
The Netherlands FUTURE study enrolled 959 consecutive patients aged 18 to 50 years who had been admitted to a single academic center with first-ever TIA (n=262), ischemic stroke (n=606), or ICH (n=91). Over a mean follow-up of 11.1 years (follow-up rate of 97%), among 30-day survivors, the observed 20-year mortality for each stroke type exceeded the expected mortality in the general population. Among the patients, mortality ranged from 1.2% to 2.9% at 1 year to 2.5% to 6.1% at 5 years, 9.2% to 12.4% at 10 years, and 13.7% to 26.8% at 20 years. Among the stroke cases, the relative excess of deaths compared with the general population was greatest among the youngest subjects, but the absolute excess of deaths was highest among the older subjects.55
There are substantial geographic disparities in stroke mortality, with higher rates in the southeastern United States, known as the “stroke belt.” This area is usually defined to include the 8 southern states of North Carolina, South Carolina, Georgia, Tennessee, Mississippi, Alabama, Louisiana, and Arkansas. These geographic differences have existed since at least 1940,56 and despite some minor shifts,57 they persist.54,58,59 Within the stroke belt, a “buckle” region along the coastal plain of North Carolina, South Carolina, and Georgia has been identified with an even higher stroke mortality rate than the remainder of the stroke belt. The overall average stroke mortality is ≈20% higher in the stroke belt than in the rest of the nation and ≈40% higher in the stroke buckle.60
Stroke Risk Factors
(See Table 14-2 and Chart 14-8.)
Chart 14-8.
Estimated 10-year stroke risk in adults 55 years of age according to levels of various risk factors (Framingham Heart Study). AF indicates atrial fibrillation; and CVD, cardiovascular disease. Data derived from Wolf et al.221
For prevalence and other information on any of these specific risk factors, refer to the specific risk factor chapters.
High Blood Pressure
(See Chapter 9 for more information.)
-
BP is a powerful determinant of risk for both ischemic stroke and intracranial hemorrhage.
Approximately 77% of those who have a first stroke have BP >140/90 mm Hg (NHLBI unpublished estimates from ARIC, CHS, and FHS Cohort and Offspring studies).
Diabetic subjects with BP <120/80 mm Hg have approximately half the lifetime risk of stroke of subjects with hypertension. The treatment and lowering of BP among diabetic hypertensive individuals was associated with a significant reduction in stroke risk.61
In the REGARDS study (NINDS), between the ages of 45 and 64 years (an age group in which African Americans are at 2 to 3 times the risk of stroke as whites), ≈40% of the excess stroke risk in African Americans is attributable to traditional stroke risk factors, with levels of SBP accounting for approximately one half of this impact.62 For each 10 mm Hg increase in levels of SBP, the increased stroke risk in whites is ≈8%; however, a similar 10 mm Hg increase in SBP in African Americans is associated with a 24% increase in stroke risk, an impact 3 times greater than in whites.63
Cross-sectional baseline data from the SPS3 trial showed that more than half of all symptomatic lacunar stroke patients had uncontrolled hypertension at 2.5 months after stroke.64
A meta-analysis of 12 prospective cohort studies (including 518 520 participants) found that prehypertension is associated with incident stroke. The risk is particularly noted in nonelderly people and for those with BP values in the higher prehypertension range.65
Blacks with hypertension were more aware and treated than whites, but were less likely than whites to have their BP controlled.66
The higher stroke risk for the stroke belt compared with other regions does not appear to be attributable to hypertension management, because treatment and control rates were similar for the 2 geographic areas.66
Several studies have shown significantly lower rates of recurrent stroke with lower BPs. Most recently, the BP-reduction component of the SPS3 trial showed that targeting an SBP <130 mm Hg was likely to reduce recurrent stroke by ≈20% (P=0.08) and significantly reduced ICH by two thirds.67,68
Diabetes Mellitus
(See Chapter 10 for more information.)
DM increases ischemic stroke incidence at all ages, but this risk is most prominent (risk ratio for ischemic stroke conferred by DM >5) before 65 years of age in both blacks and whites. According to data from the GCNKSS in 2005, the risk ratio for ischemic stroke in blacks <65 years of age was 5.2 compared with 12.0 for whites; the trend for greater risk conferred by DM at age <65 years in whites was noted in all 3 prior study periods. Overall, ischemic stroke patients with DM are younger, more likely to be black, and more likely to have HBP, MI, and high cholesterol than nondiabetic patients.69
In people with a history of TIA or minor stroke, impaired glucose tolerance nearly doubled the stroke risk compared with those with normal glucose levels and tripled the risks for those with DM.70
A meta-analysis of prospective randomized controlled trials of interventions that targeted prediabetic patients revealed a 24% relative risk reduction in fatal and nonfatal strokes (HR, 0.76; 95% CI, 0.58–0.99).71
Data from the US Nationwide Inpatient Sample revealed that from 1997 to 2006, the absolute number of acute ischemic stroke hospitalizations declined by 17% (from 489 766 in 1997 to 408 378 in 2006); however, the absolute number of acute ischemic stroke hospitalizations with comorbid DM rose by 27% (from 97 577 [20%] in 1997 to 124 244 [30%] in 2006). The rise in comorbid DM was more pronounced in individuals who were relatively younger, black or “other” race, on Medicaid, or admitted to hospitals located in the South. Factors independently associated with higher odds of DM in acute ischemic stroke patients were black or “other” (versus white) race, CHF, peripheral vascular disease, and history of MI, renal disease, or hypertension.72
A population-based study of 12 375 first-ever stroke patients 25 to 74 years old who were followed up for ≤23 years found that diabetic patients had a higher risk of death than nondiabetic patients (adjusted HR, 1.67; 95% CI, 1.58–1.76). The reduced survival of diabetic stroke patients was more pronounced in women (P=0.02) and younger individuals (P <0.001).73
A retrospective analysis of diabetic patients with acute ischemic stroke revealed that those who had been taking and continued taking sulfonylureas were less likely to experience symptomatic hemorrhagic transformation than those who did not take sulfonylureas (P=0.016).74
The ACCORD study showed that in patients with type 2 DM, targeting SBP to <120 mm Hg did not reduce the rate of cardiovascular events compared with subjects in whom the SBP target was <140 mm Hg, except for the end point of stroke, for which intensive therapy reduced the risk of any stroke (HR, 0.59; 95% CI, 0.39–0.89) and nonfatal stroke (HR, 0.63; 95% CI, 0.41–0.96).61
The ONTARGET trial revealed that in both patients with and without DM, the adjusted risk of stroke continued to decrease down to achieved SBP values of 115 mm Hg, whereas there was no benefit for other fatal or nonfatal cardiovascular outcomes below an SBP of 130 mm Hg.75
Disorders of Heart Rhythm
(See Chapter 16 for more information.)
AF is a powerful risk factor for stroke, independently increasing risk ≈5-fold throughout all ages. The percentage of strokes attributable to AF increases steeply from 1.5% at 50 to 59 years of age to 23.5% at 80 to 89 years of age.76,77
Because AF is often asymptomatic77a,77b and likely frequently undetected clinically,78 the stroke risk attributed to AF may be substantially underestimated.79 Screening for AF in patients with cryptogenic stroke or TIA by use of outpatient telemetry for 21 to 30 days has resulted in an AF detection rate of 12% to 23%.78–80
Among 2580 participants ≥65 years of age with hypertension in whom a cardiac rhythm device that included an atrial lead was implanted, 35% developed subclinical tachyarrhythmias (defined as an atrial rate ≥190 beats per minute that lasted ≥6 minutes). These subclinical events were independently associated with a 2.5-fold increased risk of ischemic stroke or systemic embolism.81
Important risk factors for stroke in the setting of AF include advancing age, hypertension, HF, DM, previous stroke or TIA, vascular disease, and female sex.82–84 Additional biomarkers, including high levels of troponin and B-type natriuretic peptide, increase the risk of stroke in the setting of AF independent of those well-established clinical characteristics.85
High Blood Cholesterol and Other Lipids
(See Chapter 8 for more information.)
For clarity, different types of cholesterol (total cholesterol, subfractions) are described here and are bolded in each bullet point.
An association between total cholesterol and ischemic stroke has been found in some prospective studies,86–88 but not others.89–91
Data from the Honolulu Heart Program//NHLBI found that in Japanese men 71 to 93 years of age, low concentrations of HDL cholesterol were more likely to be associated with a future risk of thromboembolic stroke than were high concentrations.92 However, a meta-analysis of 23 studies performed in the Asia-Pacific Region showed no significant association between low HDL cholesterol and stroke risk.93
In an analysis by the Emerging Risk Factors Collaboration of individual records on 302 430 people without initial vascular disease from 68 long-term prospective studies, HRs for ischemic stroke were 1.02 (95% CI, 0.94–1.11) with triglyceride, 0.93 (95% CI, 0.84–1.02) with HDL cholesterol, and 1.12 (95% CI, 1.04–1.20) with non-HDL cholesterol.94
A Finish study of 27 703 men and 30 532 women followed up for >20 years for ischemic stroke found an independent inverse association of HDL cholesterol with the risks of total and ischemic stroke in women.91
Among 13 951 patients in the Copenhagen Heart Study followed up for 33 years for ischemic stroke, increasing stepwise levels of nonfasting triglycerides were associated with increased risk of ischemic stroke in both men and women. Stepwise increasing levels of total cholesterol were not associated with risk of ischemic stroke in women, but levels >9.00 mmol/L were in men.95
Smoking
(See Chapter 3 for more information.)
Current smokers have a 2 to 4 times increased risk of stroke compared with nonsmokers or those who have quit for >10 years.96,97
Cigarette smoking is a risk factor for ischemic stroke and SAH, but the data for ICH are less consistent.96,97
Smoking is perhaps the most important modifiable risk factor in preventing SAH, with the highest PAR of any SAH risk factor.98
Data also support a dose-response relationship across old and young age groups.96,99
Discontinuation of smoking has been shown to reduce stroke risk across sex, race, and age groups.99
Exposure to secondhand smoke (also termed passive smoking or environmental tobacco smoke) is a risk factor for stroke. Meta-analyses have estimated a pooled RR of 1.25 for exposure to spousal smoking (or nearest equivalent) and risk of stroke. A dose-response relationship between exposure to secondhand smoke and stroke risk has also been reported.100,101
Physical Inactivity
(See Chapter 4 for more information.)
In NOMAS, a prospective cohort that included white, black, and Hispanic adults in an urban setting followed up for a median of 9 years, moderate to vigorous PA was associated with an overall 35% reduction in risk of ischemic stroke.102
The NOMAS study found that only moderate- to vigorous-intensity exercise was associated with reduced stroke incidence, whereas light exercise (such as walking) showed no benefit.102
Timing of PA in relation to stroke onset has also been examined in several studies. In a hospital-based case-control study from Heidelberg, Germany, recent activity (within the prior months) was associated with reduced odds of having a stroke or TIA, whereas sports activity during young adulthood that was not continued showed no benefit.104 In a Danish case-control study, ischemic stroke patients were less physically active in the week preceding the stroke than age- and sex-matched control subjects, with the highest activity scores associated with the greatest reduction in odds of stroke.105
Recent results from REGARDS found that participants reporting PA <4 times per week had a 20% increased risk of incident stroke over a mean of 5.7 years compared with those exercising ≥4 times per week. This relationship, which was more pronounced in men than in women, may be explained in large part by the effect of PA on reducing traditional risk factors, such as obesity and DM.106
Nutrition
(See Chapter 5 for more information.)
Adherence to a Mediterranean-style diet that was higher in nuts and olive oil was associated with a reduced risk of stroke (HR, 0.54; 95% CI, 0.35–0.84) in a randomized clinical trial conducted in Spain. The protective benefit of the Mediterranean diet observed was greater for strokes than for MI, but stroke subtype was not available.107
In the Nurses Health and Health Professionals Follow-up Studies, each 1-serving increase in sugar-sweetened soda beverage was associated with a 13% increased risk of ischemic stroke but not hemorrhagic stroke. Conversely, each 1-serving increase in low-calorie or diet soda was associated with a 7% increased risk of ischemic stroke and 27% increased risk of hemorrhagic stroke.108
A meta-analysis of >94 000 people with 34 817 stroke events demonstrated that eating ≥5 servings of fish per week versus eating <1 serving per week was associated with a 12% reduction in stroke risk; however, these results were not consistent across all cohort studies.109
Using registry data from Sweden, people eating ≥7 servings of fruits and vegetables per day had a 19% reduced risk of stroke compared with those only eating 1 serving per day. This effect was only seen in people who did not have hypertension.110
Family History and Genetics
(See Chapter 7 for more information.)
In the FHS, a documented parental ischemic stroke by the age of 65 years was associated with a 3-fold increase in ischemic stroke risk in offspring, even after adjustment for other known stroke risk factors. The absolute magnitude of the increased risk was greatest in those in the highest quintile of the FRS. By age 65 years, people in the highest FRS quintile with an early parental ischemic stroke had a 25% risk of stroke compared with a 7.5% risk of ischemic stroke for those without such a history.111
Chronic Kidney Disease
(See Chapter 12 for more information.)
The CHS (NHLBI) showed that people with creatinine ≥1.5 mg/dL were at increased risk for stroke, with an adjusted HR of 1.77 (95% CI, 1.08–2.91).112
Participants in REGARDS with a reduced eGFR were also shown to have increased risk of stroke symptoms,113 and a meta-analysis of >280 000 patients showed a 43% increased incident stroke risk among patients with a GFR <60 mL·min−1·1.73 m−2.114
In a study of 539 287 Swedish men and women followed up for 12 years,115 HRs for ICH were as follows: for GFR 60 to 90 mL·min−1·1.73 m−2 (mild), 1.04 (95% CI, 0.93–1.15); for GFR 30 to 60 mL·min−1·1.73 m−2 (moderate), 1.26 (95% CI, 0.96–1.64); and for GFR 15 to 30 mL·min−1·1.73 m−2 (severe impairment), 2.31 (95% CI, 1.10–4.87). Among 128 patients with ICH, the presence of GFR <45 mL·min−1·1.73 m−2 is associated with larger, lobar hematomas and poor outcome.116
A urinary albumin to creatinine ratio >30 mg/g was associated with a 40% increased risk of stroke in black participants but not white participants in the REGARDS study.117
Risk Factor Issues Specific to Women
On average, women are older at stroke onset than men (≈75 years compared with 71 years).14
In the setting of AF, women have a significantly higher risk of stroke than men.118–122
Analysis of data from the FHS found that women with natural menopause before 42 years of age had twice the ischemic stroke risk of women with natural menopause after 42 years of age.123
Investigators from the Nurse’s Health Study, however, did not find an association between age at natural menopause and risk of ischemic or hemorrhagic stroke.124
Overall, randomized clinical trial data indicate that the use of estrogen plus progestin, as well as estrogen alone, increases stroke risk in postmenopausal, generally healthy women and provides no protection for postmenopausal women with established CHD125–128 and recent stroke or TIA.129
In a nested case-control study of the United Kingdom’s General Practice Research Database, stroke risk was not increased for users of low-dose (≤50 μg) estrogen patches (RR, 0.81; 95% CI, 0.62–1.05) but was increased for users of high-dose (>50 μg) patches (RR, 1.89; 95% CI, 1.15–3.11) compared with nonusers.130
Low-estrogen-dose oral contraceptives are associated with a 93% increased risk of ischemic stroke, but the absolute increased risk is small, (4.1 ischemic strokes per 100 000 nonsmoking, normotensive women).131,132
Migraine with aura is associated with ischemic stroke in younger women, particularly if they smoke or use oral contraceptives. The combination of all 3 factors increases the risk ≈9-fold compared with women without any of these factors.133,134
The risk of ischemic stroke or ICH during pregnancy and the first 6 weeks after giving birth was 2.4 times greater than for nonpregnant women of similar age and race, according to the Baltimore-Washington Cooperative Young Stroke Study. The risk of ischemic stroke during pregnancy was not increased during pregnancy per se but was increased 8.7-fold during the first 6 postpartum weeks. ICH showed a small RR of 2.5 during pregnancy that increased dramatically to an RR of 28.3 in the first 6 postpartum weeks. The excess risk of stroke (all types except SAH) attributable to the combined pregnancy/postpregnancy period was 8.1 per 100 000 pregnancies.135
Analyses of the US Nationwide Inpatient Sample from 1994 to 1995 and from 2006 to 2007 show a temporal increase in the proportion of pregnancy hospitalizations that were associated with a stroke, with a 47% increase for antenatal hospitalizations and an 83% increase for postpartum hospitalizations, but no increase for delivery hospitalizations. Increases in the prevalence of HD and hypertensive disorders accounted for almost all the increase in postpartum stroke hospitalizations but not the antenatal stroke hospitalizations.86
Preeclampsia is a risk factor for ischemic stroke remote from pregnancy.136 The subsequent stroke risk of pre-eclampsia maybe mediated by a 3.6- to 6.1-fold higher later risk of hypertension and a 3.1- to 3.7-fold higher later risk of DM, depending on whether the preeclampsia was mild or severe.137
Sleep Apnea
The prevalence of sleep-disordered breathing, defined as an AHI >5, has been estimated to be 24% for men and 9% for women aged 30 to 60 years.138
In the Sleep Heart Health Study, obstructive sleep apnea measured by the obstructive AHI was associated with risk of incident ischemic stroke in men after adjustment for confounders (P=0.016 for linear trend associated with quartiles of AHI) but not in women. Compared with men in the lowest quartile of AHI, men in the highest quartile (AHI >19) had an adjusted HR of 2.9 (95% CI, 1.1–7.4).139
In the Victoria Sleep Project, severe sleep apnea (AHI ≥30) was associated with increased risk of incident ischemic stroke in community-dwelling elderly (HR, 2.5; 95% CI, 1.0–6.0).140
Obstructive sleep apnea is associated with poststroke mortality.141–143
Sleep apnea is common after stroke, with prevalence in excess of 50%.144
No definitive study has been conducted to determine whether treatment with continuous positive airway pressure prevents stroke or improves poststroke outcomes.
Awareness of Stroke Warning Signs and Risk Factors
Correct knowledge of at least 1 stroke warning sign increased from 48% in 1995 to 68% in 2000, with no significant improvement to 2005 (68%) on the basis of a telephone survey conducted in a biracial population in the greater Cincinnati/Northern Kentucky region. Knowledge of 3 correct warning signs was low but increased over time: 5.4% in 1995, 12.0% in 2000, and 15.7% in 2005. Knowledge of at least 1 stroke risk factor increased from 59% in 1995 to 71% in 2000, but there was no improvement to 2005 (71%). Only 3.6% of those surveyed were able to independently identify tPA as an available drug therapy, and only 9% of these were able to identify a window of <3 hours for treatment.145
In the 2009 NHIS, 51.2% of subjects were aware of 5 stroke warning symptoms and would first call 9-1-1 if they thought that someone was having a stroke. Awareness of all 5 stroke warning symptoms and calling 9-1-1 was higher among whites than blacks and Hispanics (55.9%, 47.1%, and 36.5%, respectively), women than men (53.6% versus 48.6%), and people with higher versus lower educational attainment (59.0% for people with a bachelor’s degree or more compared with 51.4% for people with a high school diploma or some college and 36.7% for those who had not received a high school diploma; unpublished NHLBI tabulation).
A study was conducted of patients admitted to an ED with possible stroke to determine their knowledge of the signs, symptoms, and risk factors of stroke. Of the 163 patients able to respond, 39% did not know a single sign or symptom. Patients ≥65 years of age were less likely than those <65 years old to know a sign or symptom of stroke (28% versus 47%), and 43% did not know a single risk factor. Overall, almost 40% of patients did not know the signs, symptoms, and risk factors for stroke.146
In 2004, 800 adults ≥45 years of age were surveyed to assess their perceived risk for stroke and their history of stroke risk factors. Overall, 39% perceived themselves to be at risk. Younger age, current smoking, a history of DM, HBP, high cholesterol, HD, and stroke/TIA were independently associated with perceived risk for stroke. Respondents with AF were no more likely to report being at risk than were respondents without AF. Perceived risk for stroke increased as the number of risk factors increased; however, 46% of those with ≥3 risk factors did not perceive themselves to be at risk.147
A study of patients who had experienced a stroke found that only 60.5% were able to accurately identify 1 stroke risk factor and that 55.3% were able to identify 1 stroke symptom. Patients’ median delay time from onset of symptoms to admission in the ED was 16 hours, and only 31.6% accessed the ED in <2 hours. Analysis showed that the appearance of nonmotor symptoms as the primary symptom and nonuse of the 9-1-1 system were significant predictors of delay >2 hours. Someone other than the patient made the decision to seek treatment in 66% of the cases.148
Spanish-speaking Hispanics are less likely to know all stroke symptoms than English-speaking Hispanics, non-Hispanic blacks, and non-Hispanic whites. Lack of English proficiency is strongly associated with lack of stroke knowledge among Hispanics.149
Aftermath
(See Charts 14-9 through 14-11.)
Chart 14-9.
Proportion of patients dead 1 year after first stroke. Source: pooled data from the Framingham Heart Study, Atherosclerosis Risk in Communities study, and Cardiovascular Health Study of the National Heart, Lung, and Blood Institute.
Chart 14-11.
Proportion of patients with recurrent stroke within 5 years after first stroke. Source: pooled data from the Framingham Heart Study, Atherosclerosis Risk in Communities study, and Cardiovascular Health Study of the National Heart, Lung, and Blood Institute.
Stroke is a leading cause of serious long-term disability in the United States (Survey of Income and Program Participation, a survey of the US Census Bureau).150
Stroke was among the top 18 diseases contributing to years lived with disability in 2010; of these 18 causes, only the age-standardized rates for stroke increased significantly between 1990 and 2010 (P<0.05).151
Among Medicare patients discharged from the hospital after stroke, ≈45% return directly home, 24% are discharged to inpatient rehabilitation facilities, and 31% are discharged to skilled nursing facilities. Of stroke patients returning directly home, 32% use home healthcare services.152 For Medicare patients (including, but not limited to, stroke survivors), the likelihood of receiving inpatient rehabilitation facility care versus skilled nursing facility care is substantially influenced by the distance to and availability of inpatient rehabilitation facility beds.153
Approximately one third of stroke survivors experience poststroke depression.154
-
In the NHLBI’s FHS, among ischemic stroke survivors who were ≥65 years of age, the following disabilities were observed at 6 months after stroke155:
50% had some hemiparesis
30% were unable to walk without some assistance
46% had cognitive deficits
35% had depressive symptoms
19% had aphasia
26% were dependent in activities of daily living
26% were institutionalized in a nursing home
Visual impairments persist in 21% of stroke survivors 90 days after stroke.156
Initial severity of upper limb weakness is the best predictor of ultimate recovery of upper limb motor function.157
Data from the BRFSS (CDC) 2005 survey on stroke survivors in 21 states and the District of Columbia found that 30.7% of stroke survivors received outpatient rehabilitation. The findings indicated that the prevalence of stroke survivors receiving outpatient stroke rehabilitation was lower than would be expected if clinical practice guideline recommendations for all stroke patients had been followed.158
After stroke, women have greater disability than men. A cross-sectional analysis of 5888 community-living elderly people (>65 years of age) in the CHS who were ambulatory at baseline found that women were half as likely to be independent in activities of daily living after stroke, even after controlling for age, race, education, and marital status.159 A prospective study from a Michigan-based stroke registry found that women had a 63% lower probability of achieving independence in activities of daily living 3 months after discharge, even after controlling for age, race, subtype, prestroke ambulatory status, and other patient characteristics.160
Black stroke survivors had greater limitations in ambulation than did white stroke survivors, after adjustment for age, sex, and educational attainment but not stroke subtype, according to data from the NHIS (2000–2001, NCHS) as analyzed by the CDC.161 A national study of inpatient rehabilitation after first stroke found that blacks were younger, had a higher proportion of hemorrhagic stroke, and were more disabled on admission. Compared with non-Hispanic whites, blacks and Hispanics also had a poorer functional status at discharge but were more likely to be discharged to home rather than to another institution, even after adjustment for age and stroke subtype. After adjustment for the same covariates, compared with non-Hispanic whites, blacks also had less improvement in functional status per inpatient day.162
Stroke in Children
On the basis of pathogenic differences, pediatric strokes are typically classified as either perinatal (occurring at ≤28 days of life and including in utero strokes) or (later) childhood.
Estimates of the overall annual incidence of stroke in US children are 6.4 per 100 000 children (0 to 15 years) in 1999 in the GCNKSS163 and 4.6 per 100 000 children (0 to 19 years) in 1997 to 2003 according to data from Kaiser Permanente of Northern California, a large, integrated health-care delivery system.164 Approximately half of all incident childhood strokes are hemorrhagic.163–165
The prevalence of perinatal strokes is 29 per 100 000 live births, or 1 per 3500 live births in the 1997 to 2003 Kaiser Permanente of Northern California population.164
A history of infertility, preeclampsia, prolonged rupture of membranes, and chorioamnionitis are independent maternal risk factors for perinatal arterial ischemic stroke.166 However, maternal health and pregnancies are normal in most cases.167
The most common cause of arterial ischemic stroke in children is a cerebral arteriopathy, found in more than half of all cases.168,169
HD confers an 8- to 16-fold increased risk of arterial ischemic stroke but was present in only 8% of children with stroke in a population-based cohort.170
Exposure to minor infection in the prior month is an independent risk factor for childhood arterial ischemic stroke, present in one third of cases (adjusted OR, 3.9; 95% CI, 2.0–7.4). Head or neck trauma in the prior week is an even stronger risk factor (adjusted OR, 36; 95% CI, 5–281), present in 10% of cases.170
Thrombophilias (genetic and acquired) are risk factors for childhood stroke, with summary ORs ranging from 1.6 to 8.8 in a meta-analysis.171
In a prospective Swiss registry,172 atherosclerotic risk factors were less common in children with arterial ischemic stroke than in young adults; the most common of these factors in children was hyperlipidemia (15%). However, an analysis of the Nationwide Inpatient Sample suggests a low but rising prevalence of these factors among US adolescents and young adults hospitalized for ischemic stroke (1995 versus 2008).173
From 1979 to 1998 in the United States, childhood mortality resulting from stroke declined by 58% overall, with reductions in all major subtypes.174
The incidence of stroke in children has been stable over the past 10 years, whereas 30-day case fatality rates declined from 18% in 1988 to 1989 to 9% in 1993 to 1994 and 9% in 1999 in the GCNKSS population.163
Compared with girls, boys have a 1.28-fold higher risk of stroke.175 Compared with white children, black children have a 2-fold risk of both incident stroke and death attributable to stroke.174,175 The increased risk among blacks is not fully explained by the presence of sickle cell disease, nor is the excess risk among boys fully explained by trauma.175
Among young adult survivors of childhood stroke, 37% had a normal modified Rankin score, 42% had mild deficits, 8% had moderate deficits, and 15% had severe deficits.176 Concomitant involvement of the basal ganglia, cerebral cortex, and posterior limb of the internal capsule predicts a persistent hemiparesis.177 Basilar artery thrombosis is found in <5% of children with arterial ischemic strokes, but half result in a poor outcome (moderate or severe disability or death).178
Despite current treatment, 1 of 10 children with ischemic or hemorrhagic stroke will have a recurrence within 5 years.178a,178b The 5-year recurrence risk is as high as 60% among children with cerebral arteriopathy. The recurrence risk after perinatal stroke, however, is negligible.179
Among 59 long-term survivors of pediatric brain aneurysms, 41% developed new or recurrent aneurysm during a median follow-up of 34 years; of those, one third developed multiple aneurysms.180
More than 25% of survivors of perinatal ischemic strokes develop delayed seizures within 3 years; children with larger strokes are at higher risk.181 The cumulative risk of delayed seizures after later childhood stroke is 13% at 5 years and 30% at 10 years.182
The SWITCH trial reported that chronic blood transfusion therapy remains the superior option (over hydroxyurea) for secondary stroke prevention in children with sickle cell disease.183 A similar trial of hydroxyurea as an alternative to blood transfusion for primary stroke prevention is near completion.
Stroke in the Very Elderly
Stroke patients >85 years of age make up 17% of all stroke patients.184
Very elderly patients have a higher risk-adjusted mortality,185 have higher disability,185 have longer hospitalizations,186 receive less evidenced-based care,186a,186b and are less likely to be discharged to their original place of residence.186,187
According to analyses from the US Nationwide Inpatient Sample, over the past decade, in-hospital mortality rates after stroke have declined for every age/sex group except men aged >84 years.188
Over the next 40 years (2010–2050), the number of incident strokes is expected to more than double, with the majority of the increase among the elderly (aged ≥75 years) and minority groups.189
Barriers to Stroke Care
On the basis of NHIS data from 2000 to 2006, elderly Mexican American and non-Hispanic black stroke survivors had less access to physician care (generalist and specialist physician visits) and medications than whites; however, for patients aged 45 to 64 years, these differences were present only for specialist care. Lack of health insurance conferred the highest adjusted odds for reduced access in both age groups.190
GWTG data from 2003 to 2009 found that less than half of patients presenting with stroke symptoms received imaging within the recommended 25 minutes of hospital arrival. Factors significantly associated with longer time to imaging included older age, being female, non-white race, having DM, and arrival by means other than EMS.191
Data from the Paul Coverdell National Acute Stroke Registry found that more patients were transported by ambulance than by other means (43.6%). Significantly fewer blacks (42.4%) arrived within 2 hours of symptom onset than did whites (49.5%), and significantly fewer nonambulance patients (36.2%) arrived within 2 hours of symptom onset than did patients transported by ambulance (58.6%).192
Data from the GWTG-Stroke program examining trends in time from symptom onset to hospital arrival between 2002 and 2009 found that there had been little overall improvement in the proportion of ischemic stroke patients arriving within 2 hours of symptom onset during this time period; only 20.6% of the 413 000 subjects arrived within 2 hours, although this increased to 26.9% when the time period was extended to 3.5 hours.193
Recent data have shown a steady increase in the proportion of ischemic stroke patients who are treated with tPA therapy. For example, data from 2 US administrative databases in 2009 found that between 3.4% and 5.2% of acute ischemic strokes were treated with tPA, which was approximately double the treatment rate observed in the same data sources in 2005.194
Data obtained from the Nationwide Inpatient Sample between 2004 and 2009 from 25 states showed that tPA treatment rates were higher in Joint Commission–certified primary stroke centers (6.7%) compared with noncertified hospitals (2.2%); however, over this 6-year period, tPA treatment rates increased faster in noncertified hospitals (1.4%–3.3%) than in primary stroke centers (6.5%–6.7%).195
NHIS data from 1998 to 2002 found that younger stroke survivors (aged 45–64 years) self-reported worse access to physician care and medication affordability than older stroke survivors. Compared with older patients, younger stroke survivors were more likely to be male (52% versus 47%), to be black (19% versus 10%), and to lack health insurance (11% versus 0.4%). Lack of health insurance was associated with reduced access to care.196
Results from the BASIC project found that women were less likely to arrive at the ED within 3 hours of stroke symptom onset than men (OR, 0.7; 95% CI, 0.5–0.9). Mexican Americans were 40% less likely to arrive by EMS than non-Hispanic whites, even after adjustment for age, National Institutes of Health Stroke Scale score, education, history of stroke, and insurance status. Language fluency was not associated with time to hospital arrival or use of EMS. The receipt of tPA was low (1.5%) but did not differ by sex or ethnicity.197
Hospital Discharges/Ambulatory Care Visits
(See Table 14-1.)
From 2000 to 2010, the number of inpatient discharges from short-stay hospitals with stroke as the first-listed diagnosis remained about the same, with discharges of 981 000 and 1 015 000, respectively (NHDS, NHLBI tabulation).198
Data from 2010 from the NHDS of the NCHS showed that the average length of stay for discharges with stroke as the first-listed diagnosis was 6.1 days (median, 3 days) compared with 9.5 days (median, 6 days) in 1990 (NHDS, NHLBI tabulation).198
In 2010, men and women accounted for roughly the same number of hospital stays for stroke in the 18- to 44-year-old age group. Among people 45 to 64 years of age, 57.1% of stroke patients were men. After 65 years of age, women were the majority. Among people 65 to 84 years of age, 53.4% of stroke patients were women, whereas among those ≥85 years of age, women constituted 66.2% of all stroke patients.199
A first-ever county-level Atlas of Stroke Hospitalizations Among Medicare Beneficiaries was released in 2008 by the CDC in collaboration with the Centers for Medicare & Medicaid Services. It found that the stroke hospitalization rate for blacks was 27% higher than for the US population in general, 30% higher than for whites, and 36% higher than for Hispanics. In contrast to whites and Hispanics, the highest percentage of strokes in blacks (42.3%) occurred in the youngest Medicare age group (65–74 years of age).54
In 2010, there were 671 000 ED visits and 257 000 out-patient department visits with stroke as the first-listed diagnosis. In 2010, physician office visits for a first-listed diagnosis of stroke totaled 2 207 000 (NHAMCS, unpublished NHLBI tabulation).200
Operations and Procedures
(See Chart 14-12.)
In 2010, an estimated 100 000 inpatient endarterectomy procedures were performed in the United States. Carotid endarterectomy is the most frequently performed surgical procedure to prevent stroke (NHDS, NHLBI tabulation).
Although rates of carotid endarterectomy have decreased between 1997 and 2010, the use of carotid stenting has increased dramatically (Nationwide Inpatient Sample, HCUP, AHRQ).
The practice of carotid stenting in the United States is expanding, from <3% of all carotid artery revascularization procedures in 1998 to 13% in 2008.201
The randomized CREST study compared carotid endarterectomy and stenting for symptomatic and asymptomatic carotid stenosis. There was no overall difference in the primary end point of stroke, MI, or death; however, carotid endarterectomy showed superiority with increasing age, with the crossover point at approximately age 70, and was associated with fewer strokes, which had a greater impact on quality of life than MI.202,203
In-hospital mortality for carotid endarterectomy has decreased steadily from 1993 to 2010 (Nationwide Inpatient Sample, HCUP, AHRQ).
In the Medicare population, in-hospital stroke rate and mortality are similar for carotid endarterectomy and carotid stenting.204
Carotid stenting is associated with significantly higher costs than carotid endarterectomy in asymptomatic patients205 and may be less cost-effective in general.206
The percentage of patients undergoing carotid endarterectomy within 2 weeks of the onset of stroke increased from 13% in 2007 to 47% in 2010.207
Cost
(See Table 14-1.)
The direct and indirect cost of stroke in 2010 was $36.5 billion (MEPS, NHLBI tabulation).
The estimated direct medical cost of stroke for 2010 is $20.6 billion. This includes hospital outpatient or office-based provider visits, hospital inpatient stays, ED visits, prescribed medicines, and home health care.208
The mean expense per patient for direct care for any type of service (including hospital inpatient stays, outpatient and office-based visits, ED visits, prescribed medicines, and home health care) in the United States in 2010 was estimated at $5455.208
The mean lifetime cost of ischemic stroke in the United States is estimated at $140 048. This includes inpatient care, rehabilitation, and follow-up care necessary for lasting deficits. (All numbers were converted to 1999 dollars by use of the medical component of the Consumer Price Index.)209
Between 2012 and 2030, total direct medical stroke-related costs are projected to triple, from $71.6 billion to $184.1 billion, with the majority of the projected increase in costs arising from those 65 to 79 years of age.9
Inpatient hospital costs for an acute stroke event account for 70% of first-year poststroke costs.209
The largest components of short-term care costs were room charges (50%), medical management (21%), and diagnostic costs (19%).210
Death within 7 days, SAH, and stroke while hospitalized for another condition are associated with higher costs in the first year. Lower costs are associated with mild cerebral infarctions or residence in a nursing home before the stroke.211
Demographic variables (age, sex, and insurance status) are not associated with stroke cost. Severe strokes (National Institutes of Health Stroke Scale score >20) cost twice as much as mild strokes, despite similar diagnostic testing. Comorbidities such as ischemic HD and AF predict higher costs.210,211a
The total cost of stroke from 2005 to 2050, in 2005 dollars, is projected to be $1.52 trillion for non-Hispanic whites, $313 billion for Hispanics, and $379 billion for blacks. The per capita cost of stroke estimate is highest in blacks ($25 782), followed by Hispanics ($17 201) and non-Hispanic whites ($15 597). Loss of earnings is expected to be the highest cost contributor in each race/ ethnic group.212
During 2001 to 2005, the average cost for outpatient stroke rehabilitation services and medications the first year after inpatient rehabilitation discharge was $11 145. The corresponding average yearly cost of medication was $3376, whereas the average cost of yearly rehabilitation service utilization was $7318.212a
Recurrent stroke patients had 38% higher costs per patient 1 year after discharge from index hospitalization than new stroke patients.213
In adjusted models that controlled for relevant covariates, the attributable 1-year cost of poststroke aphasia was estimated at $1703 in 2004 dollars.214
Data from Sweden show that healthcare costs associated with stroke survivors with spasticity are 4-fold higher than for stroke survivors without spasticity.215
The estimated cost of acute pediatric stroke in the United States was $42 million in 2003. The mean cost of short-term hospital care was $20 927 per discharge.216
After adjustment for routine healthcare costs, the average 5-year cost of a neonatal stroke was $51 719 and that of a childhood stroke was $135 161. Costs among children with stroke continued to exceed those in age-matched control children even in the fifth year by an average of $2016.217
- 1.Behavioral Risk Factor Surveillance System: prevalence and trends data. [Accessed June 4, 2013];Centers for Disease Control and Prevention Web site. http://apps.nccd.cdc.gov/brfss/index.asp.
- 2.Centers for Disease Control and Prevention. Prevalence of stroke: United States, 2006–2010. MMWR Morb Mortal Wkly Rep. 2012;61:379–382. [PubMed] [Google Scholar]
- 3.Vermeer SE, Longstreth WT, Jr, Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007;6:611–619. doi: 10.1016/S1474-4422(07)70170-9. [DOI] [PubMed] [Google Scholar]
- 4.Prabhakaran S, Wright CB, Yoshita M, Delapaz R, Brown T, DeCarli C, Sacco RL. Prevalence and determinants of subclinical brain infarction: the Northern Manhattan Study. Neurology. 2008;70:425–430. doi: 10.1212/01.wnl.0000277521.66947.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Das RR, Seshadri S, Beiser AS, Kelly-Hayes M, Au R, Himali JJ, Kase CS, Benjamin EJ, Polak JF, O’Donnell CJ, Yoshita M, D’Agostino RB, Sr, DeCarli C, Wolf PA. Prevalence and correlates of silent cerebral infarcts in the Framingham offspring study. Stroke. 2008;39:2929–2935. doi: 10.1161/STROKEAHA.108.516575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howard G, Wagenknecht LE, Cai J, Cooper L, Kraut MA, Toole JF. Cigarette smoking and other risk factors for silent cerebral infarction in the general population. Stroke. 1998;29:913–917. doi: 10.1161/01.str.29.5.913. [DOI] [PubMed] [Google Scholar]
- 7.Bryan RN, Wells SW, Miller TJ, Elster AD, Jungreis CA, Poirier VC, Lind BK, Manolio TA. Infarctlike lesions in the brain: prevalence and anatomic characteristics at MR imaging of the elderly: data from the Cardiovascular Health Study. Radiology. 1997;202:47–54. doi: 10.1148/radiology.202.1.8988191. [DOI] [PubMed] [Google Scholar]
- 8.Howard VJ, McClure LA, Meschia JF, Pulley L, Orr SC, Friday GH. High prevalence of stroke symptoms among persons without a diagnosis of stroke or transient ischemic attack in a general population: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Arch Intern Med. 2006;166:1952–1958. doi: 10.1001/archinte.166.18.1952. [DOI] [PubMed] [Google Scholar]
- 9.Ovbiagele B, Goldstein LB, Higashida RT, Howard VJ, Johnston SC, Khavjou OA, Lackland DT, Lichtman JH, Mohl S, Sacco RL, Saver JL, Trogdon JG on behalf of the American Heart Association Advocacy Coordinating Committee and Stroke Council. Forecasting the future of stroke in the United States: a policy statement from the American Heart Association and American Stroke Association. Stroke. 2013;44:2361–2375. doi: 10.1161/STR.0b013e31829734f2. [DOI] [PubMed] [Google Scholar]
- 10.Lackland DT, Elkind MS, D’Agostino R, Sr, Dhamoon MS, Goff DC, Jr, Higashida RT, McClure LA, Mitchell PH, Sacco RL, Sila CA, Smith SC, Jr, Tanne D, Tirschwell DL, Touzé E, Wechsler LR on behalf of the American Heart Association Stroke Council; Council on Epidemiology and Prevention; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Quality of Care and Outcomes Research. Inclusion of stroke in cardiovascular risk prediction instruments: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012;43:1998–2027. doi: 10.1161/STR.0b013e31825bcdac. [DOI] [PubMed] [Google Scholar]
- 11.Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, Khatri P, Adeoye O, Ferioli S, Broderick JP, Kissela BM. Stroke incidence is decreasing in whites but not in blacks: a population-based estimate of temporal trends in stroke incidence from the Greater Cincinnati/Northern Kentucky Stroke Study. Stroke. 2010;41:1326–1331. doi: 10.1161/STROKEAHA.109.575043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, Wolf PA. The lifetime risk of stroke: estimates from the Framingham Study. Stroke. 2006;37:345–350. doi: 10.1161/01.STR.0000199613.38911.b2. [DOI] [PubMed] [Google Scholar]
- 13.Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, Khatiwoda A, Lisabeth L. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7:915–926. doi: 10.1016/S1474-4422(08)70193-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petrea RE, Beiser AS, Seshadri S, Kelly-Hayes M, Kase CS, Wolf PA. Gender differences in stroke incidence and poststroke disability in the Framingham heart study. Stroke. 2009;40:1032–1037. doi: 10.1161/STROKEAHA.108.542894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Löfmark U, Hammarström A. Evidence for age-dependent education-related differences in men and women with first-ever stroke: results from a community-based incidence study in northern Sweden. Neuroepidemiology. 2007;28:135–141. doi: 10.1159/000102141. [DOI] [PubMed] [Google Scholar]
- 16.Rothwell PM, Coull AJ, Silver LE, Fairhead JF, Giles MF, Lovelock CE, Redgrave JN, Bull LM, Welch SJ, Cuthbertson FC, Binney LE, Gutnikov SA, Anslow P, Banning AP, Mant D, Mehta Z Oxford Vascular Study. Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study) Lancet. 2005;366:1773–1783. doi: 10.1016/S0140-6736(05)67702-1. [DOI] [PubMed] [Google Scholar]
- 17.Hollander M, Koudstaal PJ, Bots ML, Grobbee DE, Hofman A, Breteler MM. Incidence, risk, and case fatality of first ever stroke in the elderly population: the Rotterdam Study. J Neurol Neurosurg Psychiatry. 2003;74:317–321. doi: 10.1136/jnnp.74.3.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vega T, Zurriaga O, Ramos JM, Gil M, Alamo R, Lozano JE, López A, Miralles MT, Vaca P, Alvarez MdM Group of Research for the RECENT Project. Stroke in Spain: epidemiologic incidence and patterns: a health sentinel network study. J Stroke Cerebrovasc Dis. 2009;18:11–16. doi: 10.1016/j.jstrokecerebrovasdis.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 19.Sealy-Jefferson S, Wing JJ, Sánchez BN, Brown DL, Meurer WJ, Smith MA, Morgenstern LB, Lisabeth LD. Age- and ethnic-specific sex differences in stroke risk. Gend Med. 2012;9:121–128. doi: 10.1016/j.genm.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lewsey JD, Gillies M, Jhund PS, Chalmers JW, Redpath A, Briggs A, Walters M, Langhorne P, Capewell S, McMurray JJ, Macintyre K. Sex differences in incidence, mortality, and survival in individuals with stroke in Scotland, 1986 to 2005. Stroke. 2009;40:1038–1043. doi: 10.1161/STROKEAHA.108.542787. [DOI] [PubMed] [Google Scholar]
- 21.Morgenstern LB, Smith MA, Sánchez BN, Brown DL, Zahuranec DB, Garcia N, Kerber KA, Skolarus LE, Meurer MJ, Burke JF, Adelman EA, Baek J, Lisabeth LD. Persistent ischemic stroke disparities despite declining incidence in Mexican Americans. [Accessed July 16, 2013];Ann Neurol. 2013 Jul 13; doi: 10.1002/ana.23972. http://onlinelibrary.wiley.com/doi/10.1002/ana.23972/abstract;jsessionid=093BDB7E007BADCD9CDE0E88765C879E.f04t01. [DOI] [PMC free article] [PubMed]
- 22.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, Cushman M, Moy CS, Soliman EZ, Kissela BM, Howard G. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol. 2011;69:619–627. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kleindorfer D, Broderick J, Khoury J, Flaherty M, Woo D, Alwell K, Moomaw CJ, Schneider A, Miller R, Shukla R, Kissela B. The unchanging incidence and case-fatality of stroke in the 1990s: a population-based study. Stroke. 2006;37:2473–2478. doi: 10.1161/01.STR.0000242766.65550.92. [DOI] [PubMed] [Google Scholar]
- 24.Carandang R, Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Kannel WB, Wolf PA. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. JAMA. 2006;296:2939–2946. doi: 10.1001/jama.296.24.2939. [DOI] [PubMed] [Google Scholar]
- 25.Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, Adeoye O, Flaherty ML, Khatri P, Ferioli S, De Los Rios La Rosa F, Broderick JP, Kleindorfer DO. Age at stroke: temporal trends in stroke incidence in a large, biracial population. Neurology. 2012;79:1781–1787. doi: 10.1212/WNL.0b013e318270401d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morgenstern LB, Smith MA, Lisabeth LD, Risser JM, Uchino K, Garcia N, Longwell PJ, McFarling DA, Akuwumi O, Al-Wabil A, Al-Senani F, Brown DL, Moyé LA. Excess stroke in Mexican Americans compared with non-Hispanic Whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2004;160:376–383. doi: 10.1093/aje/kwh225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White H, Boden-Albala B, Wang C, Elkind MS, Rundek T, Wright CB, Sacco RL. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005;111:1327–1331. doi: 10.1161/01.CIR.0000157736.19739.D0. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Y, Galloway JM, Welty TK, Wiebers DO, Whisnant JP, Devereux RB, Kizer JR, Howard BV, Cowan LD, Yeh J, Howard WJ, Wang W, Best L, Lee ET. Incidence and risk factors for stroke in American Indians: the Strong Heart Study. Circulation. 2008;118:1577–1584. doi: 10.1161/CIRCULATIONAHA.108.772285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flaherty ML, Kissela B, Woo D, Kleindorfer D, Alwell K, Sekar P, Moomaw CJ, Haverbusch M, Broderick JP. The increasing incidence of anticoagulant-associated intracerebral hemorrhage. Neurology. 2007;68:116–121. doi: 10.1212/01.wnl.0000250340.05202.8b. [DOI] [PubMed] [Google Scholar]
- 30.Johnston SC, Fayad PB, Gorelick PB, Hanley DF, Shwayder P, van Husen D, Weiskopf T. Prevalence and knowledge of transient ischemic attack among US adults. Neurology. 2003;60:1429–1434. doi: 10.1212/01.wnl.0000063309.41867.0f. [DOI] [PubMed] [Google Scholar]
- 31.Kleindorfer D, Panagos P, Pancioli A, Khoury J, Kissela B, Woo D, Schneider A, Alwell K, Jauch E, Miller R, Moomaw C, Shukla R, Broderick JP. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke. 2005;36:720–723. doi: 10.1161/01.STR.0000158917.59233.b7. [DOI] [PubMed] [Google Scholar]
- 32.Brown RD, Jr, Petty GW, O’Fallon WM, Wiebers DO, Whisnant JP. Incidence of transient ischemic attack in Rochester, Minnesota, 1985–1989. Stroke. 1998;29:2109–2113. doi: 10.1161/01.str.29.10.2109. [DOI] [PubMed] [Google Scholar]
- 33.Cancelli I, Janes F, Gigli GL, Perelli A, Zanchettin B, Canal G, D’Anna L, Russo V, Barbone F, Valente M. Incidence of transient ischemic attack and early stroke risk: validation of the ABCD2 score in an Italian population-based study. Stroke. 2011;42:2751–2757. doi: 10.1161/STROKEAHA.110.612705. [DOI] [PubMed] [Google Scholar]
- 34.Hankey GJ. Impact of treatment of people with transient ischemic attacks on stroke incidence and public health. Cerebrovasc Dis. 1996;6(suppl 1):26–33. [Google Scholar]
- 35.Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA. 2000;284:2901–2906. doi: 10.1001/jama.284.22.2901. [DOI] [PubMed] [Google Scholar]
- 36.Wu CM, McLaughlin K, Lorenzetti DL, Hill MD, Manns BJ, Ghali WA. Early risk of stroke after transient ischemic attack: a systematic review and meta-analysis. Arch Intern Med. 2007;167:2417–2422. doi: 10.1001/archinte.167.22.2417. [DOI] [PubMed] [Google Scholar]
- 37.Giles MF, Rothwell PM. Risk of stroke early after transient ischaemic attack: a systematic review and meta-analysis. Lancet Neurol. 2007;6:1063–1072. doi: 10.1016/S1474-4422(07)70274-0. [DOI] [PubMed] [Google Scholar]
- 38.Clark TG, Murphy MF, Rothwell PM. Long term risks of stroke, myocardial infarction, and vascular death in “low risk” patients with a non-recent transient ischaemic attack. J Neurol Neurosurg Psychiatry. 2003;74:577–580. doi: 10.1136/jnnp.74.5.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ovbiagele B, Kidwell CS, Saver JL. Epidemiological impact in the United States of a tissue-based definition of transient ischemic attack. Stroke. 2003;34:919–924. doi: 10.1161/01.STR.0000064323.65539.A7. [DOI] [PubMed] [Google Scholar]
- 40.Feng W, Hendry RM, Adams RJ. Risk of recurrent stroke, myocardial infarction, or death in hospitalized stroke patients. Neurology. 2010;74:588–593. doi: 10.1212/WNL.0b013e3181cff776. [DOI] [PubMed] [Google Scholar]
- 41.Judd SE, Kleindorfer DO, McClure LA, Rhodes JD, Howard G, Cushman M, Howard VJ. Self-report of stroke, transient ischemic attack, or stroke symptoms and risk of future stroke in the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Stroke. 2013;44:55–60. doi: 10.1161/STROKEAHA.112.675033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hong KS, Yegiaian S, Lee M, Lee J, Saver JL. Declining stroke and vascular event recurrence rates in secondary prevention trials over the past 50 years and consequences for current trial design. Circulation. 2011;123:2111–2119. doi: 10.1161/CIRCULATIONAHA.109.934786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Allen NB, Holford TR, Bracken MB, Goldstein LB, Howard G, Wang Y, Lichtman JH. Trends in one-year recurrent ischemic stroke among the elderly in the USA: 1994–2002. Cerebrovasc Dis. 2010;30:525–532. doi: 10.1159/000319028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Redfors P, Jood K, Holmegaard L, Rosengren A, Blomstrand C, Jern C. Stroke subtype predicts outcome in young and middle-aged stroke sufferers. Acta Neurol Scand. 2012;126:329–335. doi: 10.1111/j.1600-0404.2012.01653.x. [DOI] [PubMed] [Google Scholar]
- 45.Lee BI, Nam HS, Heo JH, Kim DI Yonsei Stroke Team. Yonsei Stroke Registry: analysis of 1,000 patients with acute cerebral infarctions. Cerebrovasc Dis. 2001;12:145–151. doi: 10.1159/000047697. [DOI] [PubMed] [Google Scholar]
- 46.Hillen T, Coshall C, Tilling K, Rudd AG, McGovern R, Wolfe CD South London Stroke Register. Cause of stroke recurrence is multifactorial: patterns, risk factors, and outcomes of stroke recurrence in the South London Stroke Register. Stroke. 2003;34:1457–1463. doi: 10.1161/01.STR.0000072985.24967.7F. [DOI] [PubMed] [Google Scholar]
- 47.Murphy SL, Xu JQ, Kochanek KD. National Vital Statistics Report. 4. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2013. Deaths: final data for 2010. [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1999–2010. Series 20 No. 2P. [Accessed July 21, 2013];CDC WONDER Online Database [database online] Released January 2013. http://wonder.cdc.gov/cmf-icd10.html.
- 49.National Center for Health Statistics. Health Data Interactive. [Accessed July 15, 2013];Centers for Disease Control and Prevention Web site. http://www.cdc.gov/nchs/hdi.htm.
- 50.Lackland DT, Roccella EJ, Deutsch A, Fornage M, George MG, Howard G, Kissela B, Kittner SJ, Lichtman JH, Lisabeth L, Schwamm LH, Smith EE, Towfighi A on behalf of the American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Quality of Care and Outcomes and Research, and Council on Functional Genomics and Translational Biology. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. [Accessed December 5, 2013];Stroke. 2013 Dec 5; doi: 10.1161/01.str.0000437068.30550.cf. http://stroke.ahajournals.org/lookup/doi/10.1161/01.str.0000437068.30550.cf. [DOI]
- 51.Gillum RF, Kwagyan J, Obisesan TO. Ethnic and geographic variation in stroke mortality trends. Stroke. 2011;42:3294–3296. doi: 10.1161/STROKEAHA.111.625343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ayala C, Greenlund KJ, Croft JB, Keenan NL, Donehoo RS, Giles WH, Kittner SJ, Marks JS. Racial/ethnic disparities in mortality by stroke subtype in the United States, 1995–1998. Am J Epidemiol. 2001;154:1057–1063. doi: 10.1093/aje/154.11.1057. [DOI] [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention (CDC) Disparities in deaths from stroke among persons aged <75 years: United States, 2002. MMWR Morb Mortal Wkly Rep. 2005;54:477–481. [PubMed] [Google Scholar]
- 54.Casper ML, Nwaise IA, Croft JB, Nilasena DS. Atlas of Stroke Hospitalizations Among Medicare Beneficiaries. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 55.Rutten-Jacobs LC, Arntz RM, Maaijwee NA, Schoonderwaldt HC, Dorresteijn LD, van Dijk EJ, de Leeuw FE. Long-term mortality after stroke among adults aged 18 to 50 years. JAMA. 2013;309:1136–1144. doi: 10.1001/jama.2013.842. [DOI] [PubMed] [Google Scholar]
- 56.Lanska DJ. Geographic distribution of stroke mortality in the United States: 1939–1941 to 1979–1981. Neurology. 1993;43:1839–1851. doi: 10.1212/wnl.43.9.1839. [DOI] [PubMed] [Google Scholar]
- 57.Casper ML, Wing S, Anda RF, Knowles M, Pollard RA. The shifting stroke belt: changes in the geographic pattern of stroke mortality in the United States, 1962 to 1988. Stroke. 1995;26:755–760. doi: 10.1161/01.str.26.5.755. [DOI] [PubMed] [Google Scholar]
- 58.Howard G, Evans GW, Pearce K, Howard VJ, Bell RA, Mayer EJ, Burke GL. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke. 1995;26:1153–1158. doi: 10.1161/01.str.26.7.1153. [DOI] [PubMed] [Google Scholar]
- 59.Perry HM, Roccella EJ. Conference report on stroke mortality in the southeastern United States. Hypertension. 1998;31:1206–1215. doi: 10.1161/01.hyp.31.6.1206. [DOI] [PubMed] [Google Scholar]
- 60.Howard G, Anderson R, Johnson NJ, Sorlie P, Russell G, Howard VJ. Evaluation of social status as a contributing factor to the stroke belt region of the United States. Stroke. 1997;28:936–940. doi: 10.1161/01.str.28.5.936. [DOI] [PubMed] [Google Scholar]
- 61.Cushman WC, Evans GW, Byington RP, Goff DC, Jr, Grimm RH, Jr, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, Rhodes JD, Soliman EZ, Moy CS, Judd SE, Howard VJ REasons for Geographic And Racial Differences in Stroke (REGARDS) Investigators. Traditional risk factors as the underlying cause of racial disparities in stroke: lessons from the half-full (empty?) glass. Stroke. 2011;42:3369–3375. doi: 10.1161/STROKEAHA.111.625277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, Safford MM, Cushman M, Glasser SP, Howard VJ. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med. 2013;173:46–51. doi: 10.1001/2013.jamainternmed.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.White CL, Pergola PE, Szychowski JM, Talbert R, Cervantes-Arriaga A, Clark HD, Del Brutto OH, Godoy IE, Hill MD, Pelegri A, Sussman CR, Taylor AA, Valdivia J, Anderson DC, Conwit R, Benavente OR SPS3 Investigators. Blood pressure after recent stroke: baseline findings from the Secondary Prevention of Small Subcortical Strokes Trial. Am J Hypertens. 2013;26:1114–1122. doi: 10.1093/ajh/hpt076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lee M, Saver JL, Chang B, Chang KH, Hao Q, Ovbiagele B. Presence of baseline prehypertension and risk of incident stroke: a meta-analysis. Neurology. 2011;77:1330–1337. doi: 10.1212/WNL.0b013e3182315234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Howard G, Prineas R, Moy C, Cushman M, Kellum M, Temple E, Graham A, Howard V. Racial and geographic differences in awareness, treatment, and control of hypertension: the REasons for Geographic And Racial Differences in Stroke study. Stroke. 2006;37:1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 67.Freis ED. The Veterans Administration Cooperative Study on antihypertensive agents: implications for stroke prevention. Stroke. 1974;5:76–77. doi: 10.1161/01.str.5.1.76. [DOI] [PubMed] [Google Scholar]
- 68.The Dutch TIA Trial Study Group. A comparison of two doses of aspirin (30 mg vs. 283 mg a day) in patients after a transient ischemic attack or minor ischemic stroke. N Engl J Med. 1991;325:1261–1266. doi: 10.1056/NEJM199110313251801. [DOI] [PubMed] [Google Scholar]
- 69.Khoury JC, Kleindorfer D, Alwell K, Moomaw CJ, Woo D, Adeoye O, Flaherty ML, Khatri P, Ferioli S, Broderick JP, Kissela BM. Diabetes mellitus: a risk factor for ischemic stroke in a large biracial population. Stroke. 2013;44:1500–1504. doi: 10.1161/STROKEAHA.113.001318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vermeer SE, Sandee W, Algra A, Koudstaal PJ, Kappelle LJ, Dippel DW Dutch TIA Trial Study Group. Impaired glucose tolerance increases stroke risk in nondiabetic patients with transient ischemic attack or minor ischemic stroke. Stroke. 2006;37:1413–1417. doi: 10.1161/01.STR.0000221766.73692.0b. [DOI] [PubMed] [Google Scholar]
- 71.Hopper I, Billah B, Skiba M, Krum H. Prevention of diabetes and reduction in major cardiovascular events in studies of subjects with prediabetes: meta-analysis of randomised controlled clinical trials. Eur J Cardiovasc Prev Rehabil. 2011;18:813–823. doi: 10.1177/1741826711421687. [DOI] [PubMed] [Google Scholar]
- 72.Towfighi A, Markovic D, Ovbiagele B. Current national patterns of comorbid diabetes among acute ischemic stroke patients. Cerebrovasc Dis. 2012;33:411–418. doi: 10.1159/000334192. [DOI] [PubMed] [Google Scholar]
- 73.Eriksson M, Carlberg B, Eliasson M. The disparity in long-term survival after a first stroke in patients with and without diabetes persists: the Northern Sweden MONICA study. Cerebrovasc Dis. 2012;34:153–160. doi: 10.1159/000339763. [DOI] [PubMed] [Google Scholar]
- 74.Kunte H, Busch MA, Trostdorf K, Vollnberg B, Harms L, Mehta RI, Castellani RJ, Mandava P, Kent TA, Simard JM. Hemorrhagic transformation of ischemic stroke in diabetics on sulfonylureas. Ann Neurol. 2012;72:799–806. doi: 10.1002/ana.23680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Redon J, Mancia G, Sleight P, Schumacher H, Gao P, Pogue J, Fagard R, Verdecchia P, Weber M, Böhm M, Williams B, Yusoff K, Teo K, Yusuf S ONTARGET Investigators. Safety and efficacy of low blood pressures among patients with diabetes: subgroup analyses from the ONTARGET (ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial) J Am Coll Cardiol. 2012;59:74–83. doi: 10.1016/j.jacc.2011.09.040. [DOI] [PubMed] [Google Scholar]
- 76.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–988. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 77.Wang TJ, Massaro JM, Levy D, Vasan RS, Wolf PA, D’Agostino RB, Larson MG, Kannel WB, Benjamin EJ. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA. 2003;290:1049–1056. doi: 10.1001/jama.290.8.1049. [DOI] [PubMed] [Google Scholar]
- 77a.Page RL, Wilkinson WE, Clair WK, McCarthy EA, Pritchett EL. Asymptomatic arrhythmias in patients with symptomatic paroxysmal atrial fibrillation and paroxysmal supraventricular tachycardia. Circulation. 1994;89:224–227. doi: 10.1161/01.cir.89.1.224. [DOI] [PubMed] [Google Scholar]
- 77b.Strickberger SA, Ip J, Saksena S, Curry K, Bahnson TD, Ziegler PD. Relationship between atrial tachyarrhythmias and symptoms. Heart Rhythm. 2005;2:125–131. doi: 10.1016/j.hrthm.2004.10.042. [DOI] [PubMed] [Google Scholar]
- 78.Tayal AH, Tian M, Kelly KM, Jones SC, Wright DG, Singh D, Jarouse J, Brillman J, Murali S, Gupta R. Atrial fibrillation detected by mobile cardiac outpatient telemetry in cryptogenic TIA or stroke. Neurology. 2008;71:1696–1701. doi: 10.1212/01.wnl.0000325059.86313.31. [DOI] [PubMed] [Google Scholar]
- 79.Elijovich L, Josephson SA, Fung GL, Smith WS. Intermittent atrial fibrillation may account for a large proportion of otherwise cryptogenic stroke: a study of 30-day cardiac event monitors. J Stroke Cerebrovasc Dis. 2009;18:185–189. doi: 10.1016/j.jstrokecerebrovasdis.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 80.Flint AC, Banki NM, Ren X, Rao VA, Go AS. Detection of paroxysmal atrial fibrillation by 30-day event monitoring in cryptogenic ischemic stroke: the Stroke and Monitoring for PAF in Real Time (SMART) Registry. Stroke. 2012;43:2788–2790. doi: 10.1161/STROKEAHA.112.665844. [DOI] [PubMed] [Google Scholar]
- 81.Healey JS, Connolly SJ, Gold MR, Israel CW, Van Gelder IC, Capucci A, Lau CP, Fain E, Yang S, Bailleul C, Morillo CA, Carlson M, Themeles E, Kaufman ES, Hohnloser SH ASSERT Investigators. Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. 2012;366:120–129. doi: 10.1056/NEJMoa1105575. [DOI] [PubMed] [Google Scholar]
- 82.Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–2870. doi: 10.1001/jama.285.22.2864. [DOI] [PubMed] [Google Scholar]
- 83.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on Atrial Fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 84.Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, Selmer C, Ahlehoff O, Olsen AM, Gislason GH, Torp-Pedersen C. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124. doi: 10.1136/bmj.d124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hijazi Z, Oldgren J, Andersson U, Connolly SJ, Ezekowitz MD, Hohnloser SH, Reilly PA, Vinereanu D, Siegbahn A, Yusuf S, Wallentin L. Cardiac biomarkers are associated with an increased risk of stroke and death in patients with atrial fibrillation: a Randomized Evaluation of Long-term Anticoagulation Therapy (RE-LY) substudy. Circulation. 2012;125:1605–1616. doi: 10.1161/CIRCULATIONAHA.111.038729. [DOI] [PubMed] [Google Scholar]
- 86.Kurth T, Everett BM, Buring JE, Kase CS, Ridker PM, Gaziano JM. Lipid levels and the risk of ischemic stroke in women. Neurology. 2007;68:556–562. doi: 10.1212/01.wnl.0000254472.41810.0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Eastern Stroke and Coronary Heart Disease Collaborative Research Group. Blood pressure, cholesterol, and stroke in eastern Asia. Lancet. 1998;352:1801–1807. [PubMed] [Google Scholar]
- 88.Tirschwell DL, Smith NL, Heckbert SR, Lemaitre RN, Longstreth WT, Jr, Psaty BM. Association of cholesterol with stroke risk varies in stroke subtypes and patient subgroups. Neurology. 2004;63:1868–1875. doi: 10.1212/01.wnl.0000144282.42222.da. [DOI] [PubMed] [Google Scholar]
- 89.Prospective Studies Collaboration. Cholesterol, diastolic blood pressure, and stroke: 13,000 strokes in 450,000 people in 45 prospective cohorts. Lancet. 1995;346:1647–1653. [PubMed] [Google Scholar]
- 90.Amarenco P, Labreuche J, Touboul PJ. High-density lipoprotein-cholesterol and risk of stroke and carotid atherosclerosis: a systematic review. Atherosclerosis. 2008;196:489–496. doi: 10.1016/j.atherosclerosis.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 91.Zhang Y, Tuomilehto J, Jousilahti P, Wang Y, Antikainen R, Hu G. Total and high-density lipoprotein cholesterol and stroke risk. Stroke. 2012;43:1768–1774. doi: 10.1161/STROKEAHA.111.646778. [DOI] [PubMed] [Google Scholar]
- 92.Curb JD, Abbott RD, Rodriguez BL, Masaki KH, Chen R, Popper JS, Petrovitch H, Ross GW, Schatz IJ, Belleau GC, Yano K. High density lipoprotein cholesterol and the risk of stroke in elderly men: the Honolulu Heart Program. Am J Epidemiol. 2004;160:150–157. doi: 10.1093/aje/kwh177. [DOI] [PubMed] [Google Scholar]
- 93.Huxley RR, Barzi F, Lam TH, Czernichow S, Fang X, Welborn T, Shaw J, Ueshima H, Zimmet P, Jee SH, Patel JV, Caterson I, Perkovic V, Woodward M Asia Pacific Cohort Studies Collaboration and the Obesity in Asia Collaboration. Isolated low levels of high-density lipoprotein cholesterol are associated with an increased risk of coronary heart disease: an individual participant data meta-analysis of 23 studies in the Asia-Pacific region. Circulation. 2011;124:2056–2064. doi: 10.1161/CIRCULATIONAHA.111.028373. [DOI] [PubMed] [Google Scholar]
- 94.Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, Thompson A, Wood AM, Lewington S, Sattar N, Packard CJ, Collins R, Thompson SG, Danesh J Emerging Risk Factors Collaboration. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302:1993–2000. doi: 10.1001/jama.2009.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Varbo A, Nordestgaard BG, Tybjaerg-Hansen A, Schnohr P, Jensen GB, Benn M. Nonfasting triglycerides, cholesterol, and ischemic stroke in the general population. Ann Neurol. 2011;69:628–634. doi: 10.1002/ana.22384. [DOI] [PubMed] [Google Scholar]
- 96.Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, Creager MA, Culebras A, Eckel RH, Hart RG, Hinchey JA, Howard VJ, Jauch EC, Levine SR, Meschia JF, Moore WS, Nixon JV, Pearson TA on behalf of the American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention; Council for High Blood Pressure Research, Council on Peripheral Vascular Disease, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association [published correction appears in Stroke. 2011;42:e26] Stroke. 2011;42:517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 97.Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010;8:917–932. doi: 10.1586/erc.10.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kissela BM, Sauerbeck L, Woo D, Khoury J, Carrozzella J, Pancioli A, Jauch E, Moomaw CJ, Shukla R, Gebel J, Fontaine R, Broderick J. Subarachnoid hemorrhage: a preventable disease with a heritable component. Stroke. 2002;33:1321–1326. doi: 10.1161/01.str.0000014773.57733.3e. [DOI] [PubMed] [Google Scholar]
- 99.Bhat VM, Cole JW, Sorkin JD, Wozniak MA, Malarcher AM, Giles WH, Stern BJ, Kittner SJ. Dose-response relationship between cigarette smoking and risk of ischemic stroke in young women. Stroke. 2008;39:2439–2443. doi: 10.1161/STROKEAHA.107.510073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lee PN, Forey BA. Environmental tobacco smoke exposure and risk of stroke in nonsmokers: a review with meta-analysis. J Stroke Cerebrovasc Dis. 2006;15:190–201. doi: 10.1016/j.jstrokecerebrovasdis.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 101.Oono IP, Mackay DF, Pell JP. Meta-analysis of the association between secondhand smoke exposure and stroke. J Public Health (Oxf) 2011;33:496–502. doi: 10.1093/pubmed/fdr025. [DOI] [PubMed] [Google Scholar]
- 102.Willey JZ, Moon YP, Paik MC, Boden-Albala B, Sacco RL, Elkind MS. Physical activity and risk of ischemic stroke in the Northern Manhattan Study. Neurology. 2009;73:1774–1779. doi: 10.1212/WNL.0b013e3181c34b58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Deleted in proof.
- 104.Grau AJ, Barth C, Geletneky B, Ling P, Palm F, Lichy C, Becher H, Buggle F. Association between recent sports activity, sports activity in young adulthood, and stroke. Stroke. 2009;40:426–431. doi: 10.1161/STROKEAHA.108.527978. [DOI] [PubMed] [Google Scholar]
- 105.Krarup LH, Truelsen T, Pedersen A, Lerke H, Lindahl M, Hansen L, Schnohr P, Boysen G. Level of physical activity in the week preceding an ischemic stroke. Cerebrovasc Dis. 2007;24:296–300. doi: 10.1159/000105683. [DOI] [PubMed] [Google Scholar]
- 106.McDonnell MN, Hillier SL, Hooker SP, Le A, Judd SE, Howard VJ. Physical activity frequency and risk of incident stroke in a national US study of blacks and whites. Stroke. 2013;44:2519–2524. doi: 10.1161/STROKEAHA.113.001538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA Martínez-González MA; PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–1290. doi: 10.1056/NEJMc1806491. [DOI] [PubMed] [Google Scholar]
- 108.Bernstein AM, de Koning L, Flint AJ, Rexrode KM, Willett WC. Soda consumption and the risk of stroke in men and women. Am J Clin Nutr. 2012;95:1190–1199. doi: 10.3945/ajcn.111.030205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chowdhury R, Stevens S, Gorman D, Pan A, Warnakula S, Chowdhury S, Ward H, Johnson L, Crowe F, Hu FB, Franco OH. Association between fish consumption, long chain omega 3 fatty acids, and risk of cerebrovascular disease: systematic review and meta-analysis. BMJ. 2012;345:e6698. doi: 10.1136/bmj.e6698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Larsson SC, Virtamo J, Wolk A. Total and specific fruit and vegetable consumption and risk of stroke: a prospective study. Atherosclerosis. 2013;227:147–152. doi: 10.1016/j.atherosclerosis.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 111.Seshadri S, Beiser A, Pikula A, Himali JJ, Kelly-Hayes M, Debette S, DeStefano AL, Romero JR, Kase CS, Wolf PA. Parental occurrence of stroke and risk of stroke in their children: the Framingham study. Circulation. 2010;121:1304–1312. doi: 10.1161/CIRCULATIONAHA.109.854240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Manolio TA, Kronmal RA, Burke GL, O’Leary DH, Price TR. Short-term predictors of incident stroke in older adults: the Cardiovascular Health Study. Stroke. 1996;27:1479–1486. doi: 10.1161/01.str.27.9.1479. [DOI] [PubMed] [Google Scholar]
- 113.Muntner P, Judd SE, McClellan W, Meschia JF, Warnock DG, Howard VJ. Incidence of stroke symptoms among adults with chronic kidney disease: results from the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Nephrol Dial Transplant. 2012;27:166–173. doi: 10.1093/ndt/gfr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lee M, Saver JL, Chang KH, Liao HW, Chang SC, Ovbiagele B. Low glomerular filtration rate and risk of stroke: meta-analysis. BMJ. 2010;341:c4249. doi: 10.1136/bmj.c4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Holzmann MJ, Aastveit A, Hammar N, Jungner I, Walldius G, Holme I. Renal dysfunction increases the risk of ischemic and hemorrhagic stroke in the general population. Ann Med. 2012;44:607–615. doi: 10.3109/07853890.2011.582136. [DOI] [PubMed] [Google Scholar]
- 116.Molshatzki N, Orion D, Tsabari R, Schwammenthal Y, Merzeliak O, Toashi M, Tanne D. Chronic kidney disease in patients with acute intracerebral hemorrhage: association with large hematoma volume and poor outcome. Cerebrovasc Dis. 2011;31:271–277. doi: 10.1159/000322155. [DOI] [PubMed] [Google Scholar]
- 117.Gutiérrez OM, Judd SE, Muntner P, Rizk DV, McClellan WM, Safford MM, Cushman M, Kissela BM, Howard VJ, Warnock DG. Racial differences in albuminuria, kidney function, and risk of stroke. Neurology. 2012;79:1686–1692. doi: 10.1212/WNL.0b013e31826e9af8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Friberg J, Scharling H, Gadsbøll N, Truelsen T, Jensen GB Copenhagen City Heart Study. Comparison of the impact of atrial fibrillation on the risk of stroke and cardiovascular death in women versus men (The Copenhagen City Heart Study) Am J Cardiol. 2004;94:889–894. doi: 10.1016/j.amjcard.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 119.Fang MC, Singer DE, Chang Y, Hylek EM, Henault LE, Jensvold NG, Go AS. Gender differences in the risk of ischemic stroke and peripheral embolism in atrial fibrillation: the AnTicoagulation and Risk factors In Atrial fibrillation (ATRIA) study. Circulation. 2005;112:1687–1691. doi: 10.1161/CIRCULATIONAHA.105.553438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Dagres N, Nieuwlaat R, Vardas PE, Andresen D, Lévy S, Cobbe S, Kremastinos DT, Breithardt G, Cokkinos DV, Crijns HJ. Gender-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: a report from the Euro Heart Survey on Atrial Fibrillation. J Am Coll Cardiol. 2007;49:572–577. doi: 10.1016/j.jacc.2006.10.047. [DOI] [PubMed] [Google Scholar]
- 121.Poli D, Antonucci E, Grifoni E, Abbate R, Gensini GF, Prisco D. Gender differences in stroke risk of atrial fibrillation patients on oral anticoagulant treatment. Thromb Haemost. 2009;101:938–942. [PubMed] [Google Scholar]
- 122.Avgil Tsadok M, Jackevicius CA, Rahme E, Humphries KH, Behlouli H, Pilote L. Sex differences in stroke risk among older patients with recently diagnosed atrial fibrillation. JAMA. 2012;307:1952–1958. doi: 10.1001/jama.2012.3490. [DOI] [PubMed] [Google Scholar]
- 123.Lisabeth LD, Beiser AS, Brown DL, Murabito JM, Kelly-Hayes M, Wolf PA. Age at natural menopause and risk of ischemic stroke: the Framingham Heart Study. Stroke. 2009;40:1044–1049. doi: 10.1161/STROKEAHA.108.542993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hu FB, Grodstein F, Hennekens CH, Colditz GA, Johnson M, Manson JE, Rosner B, Stampfer MJ. Age at natural menopause and risk of cardiovascular disease. Arch Intern Med. 1999;159:1061–1066. doi: 10.1001/archinte.159.10.1061. [DOI] [PubMed] [Google Scholar]
- 125.Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, Kooperberg C, Baird A, Kotchen T, Curb JD, Black H, Rossouw JE, Aragaki A, Safford M, Stein E, Laowattana S, Mysiw WJ WHI Investigators. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA. 2003;289:2673–2684. doi: 10.1001/jama.289.20.2673. [DOI] [PubMed] [Google Scholar]
- 126.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 127.Hendrix SL, Wassertheil-Smoller S, Johnson KC, Howard BV, Kooperberg C, Rossouw JE, Trevisan M, Aragaki A, Baird AE, Bray PF, Buring JE, Criqui MH, Herrington D, Lynch JK, Rapp SR, Torner J WHI Investigators. Effects of conjugated equine estrogen on stroke in the Women’s Health Initiative. Circulation. 2006;113:2425–2434. doi: 10.1161/CIRCULATIONAHA.105.594077. [DOI] [PubMed] [Google Scholar]
- 128.Simon JA, Hsia J, Cauley JA, Richards C, Harris F, Fong J, Barrett-Connor E, Hulley SB. Postmenopausal hormone therapy and risk of stroke: the Heart and Estrogen-progestin Replacement Study (HERS) Circulation. 2001;103:638–642. doi: 10.1161/01.cir.103.5.638. [DOI] [PubMed] [Google Scholar]
- 129.Viscoli CM, Brass LM, Kernan WN, Sarrel PM, Suissa S, Horwitz RI. A clinical trial of estrogen-replacement therapy after ischemic stroke. N Engl J Med. 2001;345:1243–1249. doi: 10.1056/NEJMoa010534. [DOI] [PubMed] [Google Scholar]
- 130.Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: a nested case-control study. BMJ. 2010;340:c2519. doi: 10.1136/bmj.c2519. [DOI] [PubMed] [Google Scholar]
- 131.Gillum LA, Mamidipudi SK, Johnston SC. Ischemic stroke risk with oral contraceptives: a meta-analysis. JAMA. 2000;284:72–78. doi: 10.1001/jama.284.1.72. [DOI] [PubMed] [Google Scholar]
- 132.Gillum LA, Johnston SC. Oral contraceptives and stroke risk: the debate continues. Lancet Neurol. 2004;3:453–454. doi: 10.1016/S1474-4422(04)00819-1. [DOI] [PubMed] [Google Scholar]
- 133.MacClellan LR, Giles W, Cole J, Wozniak M, Stern B, Mitchell BD, Kittner SJ. Probable migraine with visual aura and risk of ischemic stroke: the stroke prevention in young women study. Stroke. 2007;38:2438–2445. doi: 10.1161/STROKEAHA.107.488395. [DOI] [PubMed] [Google Scholar]
- 134.Schürks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ. 2009;339:b3914. doi: 10.1136/bmj.b3914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kittner SJ, Stern BJ, Feeser BR, Hebel R, Nagey DA, Buchholz DW, Earley CJ, Johnson CJ, Macko RF, Sloan MA, Wityk RJ, Wozniak MA. Pregnancy and the risk of stroke. N Engl J Med. 1996;335:768–774. doi: 10.1056/NEJM199609123351102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Brown DW, Dueker N, Jamieson DJ, Cole JW, Wozniak MA, Stern BJ, Giles WH, Kittner SJ. Preeclampsia and the risk of ischemic stroke among young women: results from the Stroke Prevention in Young Women Study [published correction appears in Stroke. 2006;37:2862] Stroke. 2006;37:1055–1059. doi: 10.1161/01.STR.0000206284.96739.ee. [DOI] [PubMed] [Google Scholar]
- 137.Lykke JA, Langhoff-Roos J, Sibai BM, Funai EF, Triche EW, Paidas MJ. Hypertensive pregnancy disorders and subsequent cardiovascular morbidity and type 2 diabetes mellitus in the mother. Hypertension. 2009;53:944–951. doi: 10.1161/HYPERTENSIONAHA.109.130765. [DOI] [PubMed] [Google Scholar]
- 138.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–1239. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 139.Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O’Connor GT, Resnick HE, Diener-West M, Sanders MH, Wolf PA, Geraghty EM, Ali T, Lebowitz M, Punjabi NM. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182:269–277. doi: 10.1164/rccm.200911-1746OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Munoz R, Duran-Cantolla J, Martínez-Vila E, Gallego J, Rubio R, Aizpuru F, De La Torre G. Severe sleep apnea and risk of ischemic stroke in the elderly. Stroke. 2006;37:2317–2321. doi: 10.1161/01.STR.0000236560.15735.0f. [DOI] [PubMed] [Google Scholar]
- 141.Martínez-García MA, Soler-Cataluña JJ, Ejarque-Martínez L, Soriano Y, Román-Sánchez P, Illa FB, Canal JM, Durán-Cantolla J. Continuous positive airway pressure treatment reduces mortality in patients with ischemic stroke and obstructive sleep apnea: a 5-year follow-up study. Am J Respir Crit Care Med. 2009;180:36–41. doi: 10.1164/rccm.200808-1341OC. [DOI] [PubMed] [Google Scholar]
- 142.Parra O, Arboix A, Montserrat JM, Quintó L, Bechich S, García-Eroles L. Sleep-related breathing disorders: impact on mortality of cerebrovascular disease. Eur Respir J. 2004;24:267–272. doi: 10.1183/09031936.04.00061503. [DOI] [PubMed] [Google Scholar]
- 143.Sahlin C, Sandberg O, Gustafson Y, Bucht G, Carlberg B, Stenlund H, Franklin KA. Obstructive sleep apnea is a risk factor for death in patients with stroke: a 10-year follow-up. Arch Intern Med. 2008;168:297–301. doi: 10.1001/archinternmed.2007.70. [DOI] [PubMed] [Google Scholar]
- 144.Broadley SA, Jorgensen L, Cheek A, Salonikis S, Taylor J, Thompson PD, Antic R. Early investigation and treatment of obstructive sleep apnoea after acute stroke. J Clin Neurosci. 2007;14:328–333. doi: 10.1016/j.jocn.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 145.Kleindorfer D, Khoury J, Broderick JP, Rademacher E, Woo D, Flaherty ML, Alwell K, Moomaw CJ, Schneider A, Pancioli A, Miller R, Kissela BM. Temporal trends in public awareness of stroke: warning signs, risk factors, and treatment. Stroke. 2009;40:2502–2506. doi: 10.1161/STROKEAHA.109.551861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kothari R, Sauerbeck L, Jauch E, Broderick J, Brott T, Khoury J, Liu T. Patients’ awareness of stroke signs, symptoms, and risk factors. Stroke. 1997;28:1871–1875. doi: 10.1161/01.str.28.10.1871. [DOI] [PubMed] [Google Scholar]
- 147.Harwell TS, Blades LL, Oser CS, Dietrich DW, Okon NJ, Rodriguez DV, Burnett AM, Russell JA, Allen MJ, Fogle CC, Helgerson SD, Gohdes D. Perceived risk for developing stroke among older adults. Prev Med. 2005;41:791–794. doi: 10.1016/j.ypmed.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 148.Zerwic J, Hwang SY, Tucco L. Interpretation of symptoms and delay in seeking treatment by patients who have had a stroke: exploratory study. Heart Lung. 2007;36:25–34. doi: 10.1016/j.hrtlng.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 149.DuBard CA, Garrett J, Gizlice Z. Effect of language on heart attack and stroke awareness among U.S. Hispanics. Am J Prev Med. 2006;30:189–196. doi: 10.1016/j.amepre.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 150.Centers for Disease Control and Prevention (CDC) Prevalence and most common causes of disability among adults: United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58:421–426. [PubMed] [Google Scholar]
- 151.Murray CJ, Abraham J, Ali MK, Alvarado M, Atkinson C, Baddour LM, Bartels DH, Benjamin EJ, Bhalla K, Birbeck G, Bolliger I, Burstein R, Carnahan E, Chen H, Chou D, Chugh SS, Cohen A, Colson KE, Cooper LT, Couser W, Criqui MH, Dabhadkar KC, Dahodwala N, Danaei G, Dellavalle RP, Des Jarlais DC, Dicker D, Ding EL, Dorsey ER, Duber H, Ebel BE, Engell RE, Ezzati M, Felson DT, Finucane MM, Flaxman S, Flaxman AD, Fleming T, Forouzanfar MH, Freedman G, Freeman MK, Gabriel SE, Gakidou E, Gillum RF, Gonzalez-Medina D, Gosselin R, Grant B, Gutierrez HR, Hagan H, Havmoeller R, Hoffman H, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Kassebaum N, Khatibzadeh S, Knowlton LM, Lan Q, Leasher JL, Lim S, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Macintyre MF, Mallinger L, McDermott MM, Meltzer M, Mensah GA, Michaud C, Miller TR, Mock C, Moffitt TE, Mokdad AA, Mokdad AH, Moran AE, Mozaffarian D, Murphy T, Naghavi M, Narayan KM, Nelson RG, Olives C, Omer SB, Ortblad K, Ostro B, Pelizzari PM, Phillips D, Pope CA, Raju M, Ranganathan D, Razavi H, Ritz B, Rivara FP, Roberts T, Sacco RL, Salomon JA, Sampson U, Sanman E, Sapkota A, Schwebel DC, Shahraz S, Shibuya K, Shivakoti R, Silberberg D, Singh GM, Singh D, Singh JA, Sleet DA, Steenland K, Tavakkoli M, Taylor JA, Thurston GD, Towbin JA, Vavilala MS, Vos T, Wagner GR, Weinstock MA, Weisskopf MG, Wilkinson JD, Wulf S, Zabetian A, Lopez AD US Burden of Disease Collaborators. The state of US Health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Buntin MB, Colla CH, Deb P, Sood N, Escarce JJ. Medicare spending and outcomes after postacute care for stroke and hip fracture. Med Care. 2010;48:776–784. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Buntin MB, Garten AD, Paddock S, Saliba D, Totten M, Escarce JJ. How much is postacute care use affected by its availability? Health Serv Res. 2005;40:413–434. doi: 10.1111/j.1475-6773.2005.00365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke. 2005;36:1330–1340. doi: 10.1161/01.STR.0000165928.19135.35. [DOI] [PubMed] [Google Scholar]
- 155.Kelly-Hayes M, Beiser A, Kase CS, Scaramucci A, D’Agostino RB, Wolf PA. The influence of gender and age on disability following ischemic stroke: the Framingham study. J Stroke Cerebrovasc Dis. 2003;12:119–126. doi: 10.1016/S1052-3057(03)00042-9. [DOI] [PubMed] [Google Scholar]
- 156.Ali M, Hazelton C, Lyden P, Pollock A, Brady M VISTA Collaboration. Recovery from poststroke visual impairment: evidence from a clinical trials resource. Neurorehabil Neural Repair. 2013;27:133–141. doi: 10.1177/1545968312454683. [DOI] [PubMed] [Google Scholar]
- 157.Coupar F, Pollock A, Rowe P, Weir C, Langhorne P. Predictors of upper limb recovery after stroke: a systematic review and meta-analysis. Clin Rehabil. 2012;26:291–313. doi: 10.1177/0269215511420305. [DOI] [PubMed] [Google Scholar]
- 158.Centers for Disease Control and Prevention (CDC) Outpatient rehabilitation among stroke survivors: 21 states and the District of Columbia, 2005. MMWR Morb Mortal Wkly Rep. 2007;56:504–507. [PubMed] [Google Scholar]
- 159.Whitson HE, Landerman LR, Newman AB, Fried LP, Pieper CF, Cohen HJ. Chronic medical conditions and the sex-based disparity in disability: the Cardiovascular Health Study. J Gerontol A Biol Sci Med Sci. 2010;65:1325–1331. doi: 10.1093/gerona/glq139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Gargano JW, Reeves MJ Paul Coverdell National Acute Stroke Registry Michigan Prototype Investigators. Sex differences in stroke recovery and stroke-specific quality of life: results from a statewide stroke registry. Stroke. 2007;38:2541–2548. doi: 10.1161/STROKEAHA.107.485482. [DOI] [PubMed] [Google Scholar]
- 161.Centers for Disease Control and Prevention (CDC) Differences in disability among black and white stroke survivors: United States, 2000–2001. MMWR Morb Mortal Wkly Rep. 2005;54:3–6. [PubMed] [Google Scholar]
- 162.Ottenbacher KJ, Campbell J, Kuo YF, Deutsch A, Ostir GV, Granger CV. Racial and ethnic differences in postacute rehabilitation outcomes after stroke in the United States. Stroke. 2008;39:1514–1519. doi: 10.1161/STROKEAHA.107.501254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kleindorfer D, Khoury J, Kissela B, Alwell K, Woo D, Miller R, Schneider A, Moomaw C, Broderick JP. Temporal trends in the incidence and case fatality of stroke in children and adolescents. J Child Neurol. 2006;21:415–418. doi: 10.1177/08830738060210050301. [DOI] [PubMed] [Google Scholar]
- 164.Agrawal N, Johnston SC, Wu YW, Sidney S, Fullerton HJ. Imaging data reveal a higher pediatric stroke incidence than prior US estimates. Stroke. 2009;40:3415–3421. doi: 10.1161/STROKEAHA.109.564633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Broderick J, Brott T, Kothari R, Miller R, Khoury J, Pancioli A, Gebel J, Mills D, Minneci L, Shukla R. The Greater Cincinnati/Northern Kentucky Stroke Study: preliminary first-ever and total incidence rates of stroke among blacks. Stroke. 1998;29:415–421. doi: 10.1161/01.str.29.2.415. [DOI] [PubMed] [Google Scholar]
- 166.Lee J, Croen LA, Backstrand KH, Yoshida CK, Henning LH, Lindan C, Ferriero DM, Fullerton HJ, Barkovich AJ, Wu YW. Maternal and infant characteristics associated with perinatal arterial stroke in the infant. JAMA. 2005;293:723–729. doi: 10.1001/jama.293.6.723. [DOI] [PubMed] [Google Scholar]
- 167.Kirton A, Armstrong-Wells J, Chang T, Deveber G, Rivkin MJ, Hernandez M, Carpenter J, Yager JY, Lynch JK, Ferriero DM International Pediatric Stroke Study Investigators. Symptomatic neonatal arterial ischemic stroke: the International Pediatric Stroke Study. Pediatrics. 2011;128:e1402–1410. doi: 10.1542/peds.2011-1148. [DOI] [PubMed] [Google Scholar]
- 168.Mackay MT, Wiznitzer M, Benedict SL, Lee KJ, Deveber GA, Ganesan V International Pediatric Stroke Study Group. Arterial ischemic stroke risk factors: the International Pediatric Stroke Study. Ann Neurol. 2011;69:130–140. doi: 10.1002/ana.22224. [DOI] [PubMed] [Google Scholar]
- 169.Ganesan V, Prengler M, McShane MA, Wade AM, Kirkham FJ. Investigation of risk factors in children with arterial ischemic stroke. Ann Neurol. 2003;53:167–173. doi: 10.1002/ana.10423. [DOI] [PubMed] [Google Scholar]
- 170.Hills NK, Johnston SC, Sidney S, Zielinski BA, Fullerton HJ. Recent trauma and acute infection as risk factors for childhood arterial ischemic stroke. Ann Neurol. 2012;72:850–858. doi: 10.1002/ana.23688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Kenet G, Lütkhoff LK, Albisetti M, Bernard T, Bonduel M, Brandao L, Chabrier S, Chan A, deVeber G, Fiedler B, Fullerton HJ, Goldenberg NA, Grabowski E, Günther G, Heller C, Holzhauer S, Iorio A, Journeycake J, Junker R, Kirkham FJ, Kurnik K, Lynch JK, Male C, Manco-Johnson M, Mesters R, Monagle P, van Ommen CH, Raffini L, Rostásy K, Simioni P, Sträter RD, Young G, Nowak-Göttl U. Impact of thrombophilia on risk of arterial ischemic stroke or cerebral sinovenous thrombosis in neonates and children: a systematic review and meta-analysis of observational studies. Circulation. 2010;121:1838–1847. doi: 10.1161/CIRCULATIONAHA.109.913673. [DOI] [PubMed] [Google Scholar]
- 172.Bigi S, Fischer U, Wehrli E, Mattle HP, Boltshauser E, Bürki S, Jeannet PY, Fluss J, Weber P, Nedeltchev K, El-Koussy M, Steinlin M, Arnold M. Acute ischemic stroke in children versus young adults. Ann Neurol. 2011;70:245–254. doi: 10.1002/ana.22427. [DOI] [PubMed] [Google Scholar]
- 173.George MG, Tong X, Kuklina EV, Labarthe DR. Trends in stroke hospitalizations and associated risk factors among children and young adults, 1995–2008. Ann Neurol. 2011;70:713–721. doi: 10.1002/ana.22539. [DOI] [PubMed] [Google Scholar]
- 174.Fullerton HJ, Chetkovich DM, Wu YW, Smith WS, Johnston SC. Deaths from stroke in US children, 1979 to 1998. Neurology. 2002;59:34–39. doi: 10.1212/wnl.59.1.34. [DOI] [PubMed] [Google Scholar]
- 175.Fullerton HJ, Wu YW, Zhao S, Johnston SC. Risk of stroke in children: ethnic and gender disparities. Neurology. 2003;61:189–194. doi: 10.1212/01.wnl.0000078894.79866.95. [DOI] [PubMed] [Google Scholar]
- 176.Elbers J, Deveber G, Pontigon AM, Moharir M. Long-term outcomes of pediatric ischemic stroke in adulthood. [Accessed June 5, 2013];J Child Neurol. 2013 Apr 15; doi: 10.1177/0883073813484358. http://jcn.sagepub.com/content/early/2013/04/12/0883073813484358.long. [DOI] [PubMed]
- 177.Boardman JP, Ganesan V, Rutherford MA, Saunders DE, Mercuri E, Cowan F. Magnetic resonance image correlates of hemiparesis after neonatal and childhood middle cerebral artery stroke. Pediatrics. 2005;115:321–326. doi: 10.1542/peds.2004-0427. [DOI] [PubMed] [Google Scholar]
- 178.Lagman-Bartolome AM, Pontigon AM, Moharir M, MacGregor DL, Askalan R, Yau I, Deveber G. Basilar artery strokes in children: good outcomes with conservative medical treatment. Dev Med Child Neurol. 2013;55:434–439. doi: 10.1111/dmcn.12092. [DOI] [PubMed] [Google Scholar]
- 178a.Sträter R, Becker S, von Eckardstein A, Heinecke A, Gutsche S, Junker R, Kurnik K, Schobess R, Nowak-Göttl U. Prospective assessment of risk factors for recurrent stroke during childhood–a 5-year follow-up study. Lancet. 2002;360:1540–1545. doi: 10.1016/S0140-6736(02)11520-0. [DOI] [PubMed] [Google Scholar]
- 178b.Fullerton HJ, Wu YW, Sidney S, Johnston SC. Recurrent hemorrhagic stroke in children: a population-based cohort study. Stroke. 2007;38:2658–2662. doi: 10.1161/STROKEAHA.107.481895. [DOI] [PubMed] [Google Scholar]
- 179.Fullerton HJ, Wu YW, Sidney S, Johnston SC. Risk of recurrent childhood arterial ischemic stroke in a population-based cohort: the importance of cerebrovascular imaging. Pediatrics. 2007;119:495–501. doi: 10.1542/peds.2006-2791. [DOI] [PubMed] [Google Scholar]
- 180.Koroknay-Pál P, Niemelä M, Lehto H, Kivisaari R, Numminen J, Laakso A, Hernesniemi J. De novo and recurrent aneurysms in pediatric patients with cerebral aneurysms. Stroke. 2013;44:1436–1439. doi: 10.1161/STROKEAHA.111.676601. [DOI] [PubMed] [Google Scholar]
- 181.Wusthoff CJ, Kessler SK, Vossough A, Ichord R, Zelonis S, Halperin A, Gordon D, Vargas G, Licht DJ, Smith SE. Risk of later seizure after perinatal arterial ischemic stroke: a prospective cohort study. Pediatrics. 2011;127:e1550–e1557. doi: 10.1542/peds.2010-1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Fox CK, Glass HC, Sidney S, Lowenstein DH, Fullerton HJ. Acute seizures predict epilepsy after childhood stroke. [Accessed June 5, 2013];Ann Neurol. 2013 Apr 24; doi: 10.1002/ana.23916. http://onlinelibrary.wiley.com/doi/10.1002/ana.23916/abstract;jsessionid=A336EA5F9B96EB6EF021CC2AAD90DC19.f01t04. [DOI] [PMC free article] [PubMed]
- 183.Ware RE, Helms RW SWiTCH Investigators. Stroke With Transfusions Changing to Hydroxyurea (SWiTCH) Blood. 2012;119:3925–3932. doi: 10.1182/blood-2011-11-392340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Russo T, Felzani G, Marini C. Stroke in the very old: a systematic review of studies on incidence, outcome, and resource use. J Aging Res. 2011;2011:108785. doi: 10.4061/2011/108785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Forti P, Maioli F, Procaccianti G, Nativio V, Lega MV, Coveri M, Zoli M, Sacquegna T. Independent predictors of ischemic stroke in the elderly: prospective data from a stroke unit. Neurology. 2013;80:29–38. doi: 10.1212/WNL.0b013e31827b1a41. [DOI] [PubMed] [Google Scholar]
- 186.Saposnik G, Black S Stroke Outcome Research Canada (SORCan) Working Group. Stroke in the very elderly: hospital care, case fatality and disposition. Cerebrovasc Dis. 2009;27:537–543. doi: 10.1159/000214216. [DOI] [PubMed] [Google Scholar]
- 186a.Palnum KD, Petersen P, Sørensen HT, Ingeman A, Mainz J, Bartels P, Johnsen SP. Older patients with acute stroke in Denmark: quality of care and short-term mortality: a nationwide follow-up study. Age Ageing. 2008;37:90–95. doi: 10.1093/ageing/afm134. [DOI] [PubMed] [Google Scholar]
- 186b.Lichtman JH, Naert L, Allen NB, Watanabe E, Jones SB, Barry LC, Bravata DM, Goldstein LB. Use of antithrombotic medications among elderly ischemic stroke patients. Circ Cardiovasc Qual Outcomes. 2011;4:30–38. doi: 10.1161/CIRCOUTCOMES.109.850883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Kammersgaard LP, Jørgensen HS, Reith J, Nakayama H, Pedersen PM, Olsen TS Copenhagen Stroke Study. Short- and long-term prognosis for very old stroke patients: the Copenhagen Stroke Study. Age Ageing. 2004;33:149–154. doi: 10.1093/ageing/afh052. [DOI] [PubMed] [Google Scholar]
- 188.Ovbiagele B, Markovic D, Towfighi A. Recent age- and gender-specific trends in mortality during stroke hospitalization in the United States. Int J Stroke. 2011;6:379–387. doi: 10.1111/j.1747-4949.2011.00590.x. [DOI] [PubMed] [Google Scholar]
- 189.Howard G, Goff DC. Population shifts and the future of stroke: forecasts of the future burden of stroke. Ann NY Acad Sci. 2012;1268:14–20. doi: 10.1111/j.1749-6632.2012.06665.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Levine DA, Neidecker MV, Kiefe CI, Karve S, Williams LS, Allison JJ. Racial/ethnic disparities in access to physician care and medications among US stroke survivors. Neurology. 2011;76:53–61. doi: 10.1212/WNL.0b013e318203e952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Kelly AG, Hellkamp AS, Olson D, Smith EE, Schwamm LH. Predictors of rapid brain imaging in acute stroke: analysis of the Get With the Guidelines-Stroke program. Stroke. 2012;43:1279–1284. doi: 10.1161/STROKEAHA.111.626374. [DOI] [PubMed] [Google Scholar]
- 192.Centers for Disease Control and Prevention (CDC) Prehospital and hospital delays after stroke onset: United States, 2005–2006. MMWR Morb Mortal Wkly Rep. 2007;56:474–478. [PubMed] [Google Scholar]
- 193.Tong D, Reeves MJ, Hernandez AF, Zhao X, Olson DM, Fonarow GC, Schwamm LH, Smith EE. Times from symptom onset to hospital arrival in the Get With The Guidelines–Stroke Program 2002 to 2009: temporal trends and implications. Stroke. 2012;43:1912–1917. doi: 10.1161/STROKEAHA.111.644963. [DOI] [PubMed] [Google Scholar]
- 194.Adeoye O, Hornung R, Khatri P, Kleindorfer D. Recombinant tissue-type plasminogen activator use for ischemic stroke in the United States: a doubling of treatment rates over the course of 5 years. Stroke. 2011;42:1952–1955. doi: 10.1161/STROKEAHA.110.612358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Mullen MT, Kasner SE, Kallan MJ, Kleindorfer DO, Albright KC, Carr BG. Joint Commission primary stroke centers utilize more rt-PA in the nationwide inpatient sample. J Am Heart Assoc. 2013;2:e000071. doi: 10.1161/JAHA.112.000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Levine DA, Kiefe CI, Houston TK, Allison JJ, McCarthy EP, Ayanian JZ. Younger stroke survivors have reduced access to physician care and medications: National Health Interview Survey from years 1998 to 2002. Arch Neurol. 2007;64:37–42. doi: 10.1001/archneur.64.1.noc60002. [DOI] [PubMed] [Google Scholar]
- 197.Smith MA, Lisabeth LD, Bonikowski F, Morgenstern LB. The role of ethnicity, sex, and language on delay to hospital arrival for acute ischemic stroke. Stroke. 2010;41:905–909. doi: 10.1161/STROKEAHA.110.578112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Centers for Disease Control and Prevention, National Center for Health Statistics. 2010 National Ambulatory Medical Care Survey and 2010 National Hospital Ambulatory Medical Care Survey. [Accessed July 17, 2013];Ambulatory health care data: questionnaires, datasets, and related documentation. For methodology, see National Center for Health Statistics, Public Use Data File Documentation: 2010 National Ambulatory Medical Care Survey and Public Use Data File Documentation: 2010 National Hospital Ambulatory Medical Care Survey. http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
- 199.Elixhauser A, Jiang H. Hospitalizations for Women With Circulatory Disease, 2003. Rockville, MD: Agency for Healthcare Research and Quality; May, 2006. [Accessed August 3, 2011]. HCUP Statistical Brief No. 5. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb5.pdf. [PubMed] [Google Scholar]
- 200.Centers for Disease Control and Prevention, National Center for Health Statistics. 2009 National Ambulatory Medical Care Survey and 2009 National Hospital Ambulatory Medical Care Survey. [Accessed August 12, 2011];Ambulatory health care data: questionnaires, datasets, and related documentation. For methodology, see National Center for Health Statistics, Public Use Data File Documentation: 2009 National Ambulatory Medical Care Survey and Public Use Data File Documentation: 2009 National Hospital Ambulatory Medical Care Survey http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
- 201.Dumont TM, Rughani AI. National trends in carotid artery revascularization surgery. J Neurosurg. 2012;116:1251–1257. doi: 10.3171/2012.3.JNS111320. [DOI] [PubMed] [Google Scholar]
- 202.Brott TG, Hobson RW, 2nd, Howard G, Roubin GS, Clark WM, Brooks W, Mackey A, Hill MD, Leimgruber PP, Sheffet AJ, Howard VJ, Moore WS, Voeks JH, Hopkins LN, Cutlip DE, Cohen DJ, Popma JJ, Ferguson RD, Cohen SN, Blackshear JL, Silver FL, Mohr JP, Lal BK, Meschia JF CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis [published corrections appear in N Engl J Med. 2010;363:198 and N Engl J Med. 2010;363:498] N Engl J Med. 2010;363:11–23. doi: 10.1056/NEJMoa0912321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Voeks JH, Howard G, Roubin GS, Malas MB, Cohen DJ, Sternbergh WC, 3rd, Aronow HD, Eskandari MK, Sheffet AJ, Lal BK, Meschia JF, Brott TG CREST Investigators. Age and outcomes after carotid stenting and endarterectomy: the Carotid Revascularization Endarterectomy Versus Stenting Trial. Stroke. 2011;42:3484–3490. doi: 10.1161/STROKEAHA.111.624155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Wang FW, Esterbrooks D, Kuo YF, Mooss A, Mohiuddin SM, Uretsky BF. Outcomes after carotid artery stenting and endarterectomy in the Medicare population. Stroke. 2011;42:2019–2025. doi: 10.1161/STROKEAHA.110.608992. [DOI] [PubMed] [Google Scholar]
- 205.McDonald RJ, Kallmes DF, Cloft HJ. Comparison of hospitalization costs and Medicare payments for carotid endarterectomy and carotid stenting in asymptomatic patients. AJNR Am J Neuroradiol. 2012;33:420–425. doi: 10.3174/ajnr.A2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Sternbergh WC, 3rd, Crenshaw GD, Bazan HA, Smith TA. Carotid endarterectomy is more cost-effective than carotid artery stenting. J Vasc Surg. 2012;55:1623–1628. doi: 10.1016/j.jvs.2011.12.045. [DOI] [PubMed] [Google Scholar]
- 207.Witt AH, Johnsen SP, Jensen LP, Hansen AK, Hundborg HH, Andersen G. Reducing delay of carotid endarterectomy in acute ischemic stroke patients: a nationwide initiative. Stroke. 2013;44:686–690. doi: 10.1161/STROKEAHA.111.678565. [DOI] [PubMed] [Google Scholar]
- 208.Medical Expenditure Panel Survey: household component summary data table: table 4: total expenses and percent distribution for selected conditions by source of payment: United States, 2008. [Accessed September 9, 2013];Agency for Healthcare Research and Quality Web site. http://meps.ahrq.gov/data_stats/tables_compendia_hh_interactive.jsp?_SERVICE=MEPSSocket0&_PROGRAM=MEPSPGM.TC.SAS&File=HCFY2008&Table=HCFY2008_CNDXP_D&_Debug=
- 209.Taylor TN, Davis PH, Torner JC, Holmes J, Meyer JW, Jacobson MF. Lifetime cost of stroke in the United States. Stroke. 1996;27:1459–1466. doi: 10.1161/01.str.27.9.1459. [DOI] [PubMed] [Google Scholar]
- 210.Diringer MN, Edwards DF, Mattson DT, Akins PT, Sheedy CW, Hsu CY, Dromerick AW. Predictors of acute hospital costs for treatment of ischemic stroke in an academic center. Stroke. 1999;30:724–728. doi: 10.1161/01.str.30.4.724. [DOI] [PubMed] [Google Scholar]
- 211.Leibson CL, Hu T, Brown RD, Hass SL, O’Fallon WM, Whisnant JP. Utilization of acute care services in the year before and after first stroke: A population-based study. Neurology. 1996;46:861–869. [PubMed] [Google Scholar]
- 211a.Matz R. Cost-effective, risk-free, evidence-based medicine. Arch Intern Med. 2003;163:2795. doi: 10.1001/archinte.163.22.2795-a. [DOI] [PubMed] [Google Scholar]
- 212.Brown DL, Boden-Albala B, Langa KM, Lisabeth LD, Fair M, Smith MA, Sacco RL, Morgenstern LB. Projected costs of ischemic stroke in the United States. Neurology. 2006;67:1390–1395. doi: 10.1212/01.wnl.0000237024.16438.20. [DOI] [PubMed] [Google Scholar]
- 212a.Godwin KM, Wasserman J, Ostwald SK. Cost associated with stroke: outpatient rehabilitative services and medication. Top Stroke Rehabil. 2011;18(suppl 1):676–684. doi: 10.1310/tsr18s01-676. [DOI] [PubMed] [Google Scholar]
- 213.Engel-Nitz NM, Sander SD, Harley C, Rey GG, Shah H. Costs and outcomes of noncardioembolic ischemic stroke in a managed care population. Vasc Health Risk Manag. 2010;6:905–913. doi: 10.2147/VHRM.S10851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Ellis C, Simpson AN, Bonilha H, Mauldin PD, Simpson KN. The one-year attributable cost of poststroke aphasia. Stroke. 2012;43:1429–1431. doi: 10.1161/STROKEAHA.111.647339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Lundström E, Smits A, Borg J, Terént A. Four-fold increase in direct costs of stroke survivors with spasticity compared with stroke survivors without spasticity: the first year after the event. Stroke. 2010;41:319–324. doi: 10.1161/STROKEAHA.109.558619. [DOI] [PubMed] [Google Scholar]
- 216.Perkins E, Stephens J, Xiang H, Lo W. The cost of pediatric stroke acute care in the United States [published correction appears in Stroke. 2010;41:e600] Stroke. 2009;40:2820–2827. doi: 10.1161/STROKEAHA.109.548156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Gardner MA, Hills NK, Sidney S, Johnston SC, Fullerton HJ. The 5-year direct medical cost of neonatal and childhood stroke in a population-based cohort. Neurology. 2010;74:372–378. doi: 10.1212/WNL.0b013e3181cbcd48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Blackwell D, Lucas J, Clarke T. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. National Center for Health Statistics. Vital Health Stat 10. In press. [PubMed] [Google Scholar]
- 219.Kissela BM, Khoury J, Kleindorfer D, Woo D, Schneider A, Alwell K, Miller R, Ewing I, Moomaw CJ, Szaflarski JP, Gebel J, Shukla R, Broderick JP. Epidemiology of ischemic stroke in patients with diabetes: the Greater Cincinnati/Northern Kentucky Stroke Study. Diabetes Care. 2005;28:355–359. doi: 10.2337/diacare.28.2.355. [DOI] [PubMed] [Google Scholar]
- 220.Incidence and Prevalence: 2006 Chart Book on Cardiovascular and Lung Diseases. Bethesda, MD: National Heart, Lung, and Blood Institute; 2006. [Google Scholar]
- 221.Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22:312–318. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
15. Congenital Cardiovascular Defects and Kawasaki Disease
ICD-9 745 to 747, ICD-10 Q20 to Q28. See Tables 15-1 through 15-4.
Table 15-1.
Congenital Cardiovascular Defects
| Population Group | Estimated Prevalence, 2002, All Ages | Mortality, 2010, All Ages* | Hospital Discharges, 2010, All Ages |
|---|---|---|---|
| Both sexes | 650 000 to 1.3 million16 | 3196 | 62 000 |
| Males | … | 1718 (53.8%)† | 38 000 |
| Females | … | 1478 (46.2%)† | 24 000 |
| NH white males | … | 1333 | … |
| NH white females | … | 1120 | … |
| NH black males | … | 311 | … |
| NH black females | … | 271 | … |
| Asian or Pacific Islander | … | 120 | … |
| American Indian or Alaska Native | … | 41 | … |
Ellipses (…) indicate data not available; and NH, non-Hispanic.
Mortality data for the white, black, Asian or Pacific Islander, and American Indian or Alaska Native populations include deaths among people of Hispanic and non- Hispanic origin. Numbers of deaths for the American Indian or Alaska Native and Asian or Pacific Islander populations are known to be underestimated.
These percentages represent the portion of total congenital cardiovascular mortality that is for males vs females.
Sources: Mortality: Centers for Disease Control and Prevention/National Center for Health Statistics, 2010 Mortality Multiple Cause-of-Death—United States, version dated May 23, 2013. These data represent underlying cause of death only; data include Hispanics. Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics; data include those inpatients discharged alive, dead, or status unknown.
Table 15-4.
Surgery for Congenital Heart Disease
| Sample | Population, Weighted | |
|---|---|---|
| Surgery for congenital heart disease, n | 14 888 | 25 831 |
| Deaths, n | 736 | 1253 |
| Mortality rate, % | 4.9 | 4.8 |
| By sex (81 missing in sample) | ||
| Male, n | 8127 | 14 109 |
| Deaths, n | 420 | 714 |
| Mortality rate, % | 5.2 | 5.1 |
| Female, n | 6680 | 11 592 |
| Deaths, n | 315 | 539 |
| Mortality rate, % | 4.7 | 4.6 |
| By type of surgery | ||
| ASD secundum surgery, n | 834 | 1448 |
| Deaths, n | 3 | 6 |
| Mortality rate, % | 0.4 | 0.4 |
| Norwood procedure for HPLHS, n | 161 | 286 |
| Deaths, n | 42 | 72 |
| Mortality rate, % | 26.1 | 25.2 |
In 2003, 25 000 cardiovascular operations for congenital cardiovascular defects were performed on children <20 y of age. Inpatient mortality rate after all types of cardiac surgery was 4.8%. Nevertheless, mortality risk varies substantially for different defect types, from 0.4% for ASD repair to 25.2% for first-stage palliation for HPLHS. Fifty-five percent of operations were performed in males. In unadjusted analysis, mortality after cardiac surgery was somewhat higher for males than for females (5.1% vs 4.6%).
ASD indicates atrial septal defect; and HPLHS, hypoplastic left heart syndrome.
Source: Reprinted from Ma et al65 with permission from Elsevier. Copyright © 2007, The Society of Thoracic Surgeons.
Congenital cardiovascular defects, also known as congenital heart defects, are structural problems that arise from abnormal formation of the heart or major blood vessels. ICD-9 lists 25 congenital heart defect codes, of which 21 designate specific anatomic or hemodynamic lesions.
Defects range in severity from tiny pinholes between chambers that may resolve spontaneously to major malformations that can require multiple surgical procedures before school age and may result in death in utero, in infancy, or in childhood. The common complex defects include the following:
TOF
TGA
AV septal defects
Coarctation of the aorta
HPLHS
Congenital heart defects are serious and common conditions that have a significant impact on morbidity, mortality, and healthcare costs in children and in adults.1 As health outcomes improve and survival increases for children living with congenital HD, the burden of care is shifting toward adult populations.2,3
Incidence
The most commonly reported incidence of congenital heart defects in the United States is between 4 and 10 per 1000, clustering around 8 per 1000 live births.4,5 Continental variations in birth prevalence have been reported, from 6.9 per 1000 births in Europe to 9.3 per 1000 in Asia.6 Variations in reported number of incident cases are largely accounted for by the age at detection and the method of diagnosis. Major defects may be apparent in the prenatal or neonatal period, but minor defects may not be detected until adulthood. Detection rates have increased since the advent of cardiac ultrasound7 and pulse oximetry.8 Thus, true measures of the incidence of congenital HD would need to record new cases of defects that present from fetal life onward. Because most estimates are available for new cases detected between birth and the first year of life, birth prevalence is the best proxy for incidence of congenital heart defects. These are typically reported as cases per 1000 live births per year and do not distinguish between tiny defects that resolve without treatment and major malformations. To distinguish more serious defects, some studies also report new cases of sufficient severity to require an invasive procedure or that result in death within the first year of life. Despite the absence of true incidence figures, some data are available and are provided in Table 15-2.
Table 15-2.
| Type of Presentation | Rate per 1000 Live Births | Estimated Number (Variable With Yearly Birth Rate) |
|---|---|---|
| Fetal loss | Unknown | Unknown |
| Invasive procedure during the first year | 2.4 | 9200 |
| Detected during first year* | 8 | 36 000 |
| Bicuspid aortic valve | 13.7 | 54 800 |
Includes stillbirths and pregnancy termination at <20 wk gestation; includes some defects that resolve spontaneously or do not require treatment.
Abbreviations Used in Chapter 15
| ASD | atrial septal defect |
| AV | atrioventricular |
| BMI | body mass index |
| CDC | Centers for Disease Control and Prevention |
| CHD | coronary heart disease |
| CI | confidence interval |
| DM | diabetes mellitus |
| HCUP | Healthcare Cost and Utilization Project |
| HD | heart disease |
| HPLHS | hypoplastic left heart syndrome |
| ICD-9 | International Classification of Diseases, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| MACDP | Metropolitan Atlanta Congenital Defects Program |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHLBI | National Heart, Lung, and Blood Institute |
| OR | odds ratio |
| RR | relative risk |
| STS | Society of Thoracic Surgeons |
| TGA | transposition of the great arteries |
| TOF | tetralogy of Fallot |
| VSD | ventricular septal defect |
Using population-based data from the MACDP in metropolitan Atlanta, GA, congenital heart defects occurred in 1 of every 111 to 125 births (live, still, or >20 weeks’ gestation) from 1995 to 1997 and from 1998 to 2005, with variations in sex and racial distribution of some lesions.4
Data collected in Alberta, Canada, found the total prevalence of CHD to be 12.42 per 1000 total births (live, still, or >20 weeks’ gestation).9
The National Birth Defects Prevention Network for 13 states from 2004 to 2006 showed the average prevalence of 21 selected major birth defects. These data indicated that there are >6100 estimated annual cases of 5 cardiovascular defects: truncus arteriosus (0.7/10 000 births), TGA (3.0/10 000 births), TOF (4.0/10 000 births), AV septal defect (4.7/10 000 births), and HPLHS (2.3/10 000 births).10
Analysis of contemporary birth cohorts with MACDP data revealed that the most common defects at birth were VSD (4.2/1000 births), ASD (1.3/1000 births), valvar pulmonic stenosis (0.6/1000 births); TOF (0.5/1000 births), aortic coarctation (0.4/1000 births), AV septal defect (0.4/1000 births), and TGA (0.2/1000 births).4,11
An estimated minimum of 32 000 infants are expected to be affected with congenital HD each year in the United States. Of these, an approximate 25%, or 2.4 per 1000 live births, require invasive treatment in the first year of life.12
Estimates also are available for bicuspid aortic valves, which occur in 13.7 per 1000 people; these defects may not require treatment in infancy but can cause problems later in adulthood.13
Prevalence
(See Tables 15-1 through 15-3.)
Table 15-3.
Estimated Prevalence of Congenital Cardiovascular Defects and Percent Distribution by Type, United States, 2002* (in Thousands)
| Type | Prevalence, n
|
Percent of Total
|
||||
|---|---|---|---|---|---|---|
| Total | Children | Adults | Total | Children | Adults | |
| Total | 994 | 463 | 526 | 100 | 100 | 100 |
| VSD† | 199 | 93 | 106 | 20.1 | 20.1 | 20.1 |
| ASD | 187 | 78 | 109 | 18.8 | 16.8 | 20.6 |
| Patent ductus arteriosus | 144 | 58 | 86 | 14.2 | 12.4 | 16.3 |
| Valvular pulmonic stenosis | 134 | 58 | 76 | 13.5 | 12.6 | 14.4 |
| Coarctation of aorta | 76 | 31 | 44 | 7.6 | 6.8 | 8.4 |
| Valvular aortic stenosis | 54 | 25 | 28 | 5.4 | 5.5 | 5.2 |
| TOF | 61 | 32 | 28 | 6.1 | 7 | 5.4 |
| AV septal defect | 31 | 18 | 13 | 3.1 | 3.9 | 2.5 |
| TGA | 26 | 17 | 9 | 2.6 | 3.6 | 1.8 |
| Hypoplastic right heart syndrome | 22 | 12 | 10 | 2.2 | 2.5 | 1.9 |
| Double-outlet right ventricle | 9 | 9 | 0 | 0.9 | 1.9 | 0.1 |
| Single ventricle | 8 | 6 | 2 | 0.8 | 1.4 | 0.3 |
| Anomalous pulmonary venous connection | 9 | 5 | 3 | 0.9 | 1.2 | 0.6 |
| Truncus arteriosus | 9 | 6 | 2 | 0.7 | 1.3 | 0.5 |
| HPLHS | 3 | 3 | 0 | 0.3 | 0.7 | 0 |
| Other | 22 | 12 | 10 | 2.1 | 2.6 | 1.9 |
Average of the low and high estimates, two thirds from low estimate.16
ASD indicates atrial septal defect; AV, atrioventricular; HPLHS, hypoplastic left heart syndrome; TGA, transposition of the great arteries; TOF, tetralogy of Fallot; and VSD, ventricular septal defect.
Excludes an estimated 3 million bicuspid aortic valve prevalence (2 million in adults and 1 million in children).
Small VSD, 117 000 (65 000 adults and 52 000 children); large VSD, 82 000 (41 000 adults and 41 000 children).
Source: Reprinted from Hoffman et al16 with permission from Elsevier. Copyright © 2004, Mosby, Inc.
The 32nd Bethesda Conference estimated that the total number of adults living with congenital HD in the United States in 2000 was 800 000.1,14 In the United States, 1 in 150 adults are expected to have some form of congenital HD.3 In population data from Canada, the measured prevalence of congenital cardiac defects in the general population was 11.89 per 1000 children and 4.09 per 1000 adults in the year 2000.15 Extrapolated to the US population in the same year, this yields published estimates of 859 000 children and 850 000 adults for the year 2000.11 The expected growth rates of the congenital heart defects population vary from 1% to 5% per year depending on the age and distribution of lesions.13
Estimates of the distribution of lesions in the congenital heart defects population using available data vary with assumptions made. If all those born with lesions between 1940 and 2002 were treated, there would be 750 000 survivors with simple lesions, 400 000 with moderate lesions, and 180 000 with complex lesions; in addition, there would be 3.0 million subjects alive with bicuspid aortic valves.16 Without treatment, the number of survivors in each group would be 400 000, 220 000, and 30 000, respectively. The actual numbers surviving were projected to be between these 2 sets of estimates as of 1 decade ago.16 Using measurements from population data in Canada, the prevalence of severe forms of congenital heart defects increased 85% in adults and 22% in children from 1985 to 2000.15 The most common types of defects in children are (at a minimum) VSD, 620 000 people; ASD, 235 000 people; valvular pulmonary stenosis, 185 000 people; and patent ductus arteriosus, 173 000 people.16 The most common lesions seen in adults are ASD and TOF.14
Risk Factors
Numerous intrinsic and extrinsic nongenetic risk factors contribute to CHD.17
Attributable risks or fractions have been shown to include paternal anesthesia in TOF (3.6%), sympathomimetic medication for coarctation of the aorta (5.8%), pesticides for VSD (5.5%), and solvents for HPLHS (4.6%).18
A study of infants born with heart defects unrelated to genetic syndromes who were included in the National Birth Defects Prevention Study found that women who reported smoking in the month before becoming pregnant or in the first trimester were more likely to give birth to a child with a septal defect. Compared with the infants of mothers who did not smoke during pregnancy, infants of mothers who were heavy smokers (≥25 cigarettes daily) were twice as likely to have a septal defect.19
Data from the Baltimore-Washington Infant Study showed that maternal smoking during the first trimester of pregnancy was associated with a ≥30% increased risk of the following lesions in the fetus: ASD, pulmonary valvar stenosis, truncus arteriosus, and TGA.20
Maternal periconceptional smoking, exposure to secondhand smoke,21 and binge drinking22 are associated with an increased risk of congenital cardiac defects. Mothers who smoke and report any binge drinking in the 3 months before pregnancy are at an increased risk of giving birth to a child with a congenital cardiac defect (adjusted OR, 12.65).22 A greater risk of congenital heart defects is also seen in women who both have a high BMI and report periconceptional smoking.23
Associations between exposure to air pollutants during first-trimester pregnancy and risks of congenital heart defects were documented from 1986 to 2003 by the MACDP that related carbon monoxide, nitrogen dioxide, and sulfur dioxide measurements to the risk of ASD, VSD, TGA, and TOF.24
The results of a population-based study examining pregnancy obesity found a weak to moderate positive association of maternal obesity with 7 of 16 categories of birth defects, including heart defects.25
Although folic acid supplementation is recommended during pregnancy to potentially reduce the risk of congenital heart defects,17 there has been only 1 US population-based case-control study, performed with the Baltimore-Washington Infant Study between 1981 and 1989, that showed an inverse relationship between folic acid use and the risk of TGA.26 A study from Quebec, Canada, that analyzed 1.3 million births from 1990 to 2005 found a significant 6% per year reduction in severe congenital heart defects using a time-trend analysis before and after public health measures were instituted that mandated folic acid fortification of grain and flour products in Canada.27
Pregestational DM was significantly associated with cardiac defects, both isolated and multiple. Gestational DM was associated with a limited group of birth defects.28
Paternal risk of occupational exposure was addressed in a study published in 2012 that documented a higher incidence of congenital HD with paternal exposure to phthalates.29
Mortality
(See Tables 15-1 and 15-4.)
Mortality related to congenital cardiovascular defects in 2010 was 3196 deaths. Any-mention mortality related to congenital cardiovascular defects in 2010 was 5018 deaths.30
In 2010, congenital cardiovascular defects were the most common cause of infant death resulting from birth defects; 26.6% of infants who died of a birth defect had a heart defect.31
The 2010 age-adjusted death rate (deaths per 100 000 people) attributable to congenital cardiovascular defects was 1.1. Death rates were 1.1 for white males, 1.4 for black males, 0.9 for white females, and 1.2 for black females. Crude infant (<1 year of age) mortality rates were 32.5 for white infants and 43.2 for black infants.31,32
Death rates attributed to congenital heart defects decrease as gestational age advances toward 40 weeks,33 and similarly, in-hospital death of infants with major congenital HDs is independently associated with late-preterm birth (OR, 2.70; 95% CI, 1.69–4.33) compared with delivery at later gestational ages.34
In a study that investigated mortality in very low-birth-weight infants, the mortality rate of very low-birth-weight infants with serious congenital HD was 44% compared with 12.7% in very low-birth-weight infants without serious congenital HD.35
The death rate attributable to congenital heart defects in the United States has continued to decline from 1979 to 1997 and from 1999 to 2006. Age-adjusted death rates attributable to all congenital heart defects declined 21% to 39%, and deaths tended to occur at progressively older ages. Although 1-year survival for infants with congenital heart defects has increased from 67.4% (1979–1993) to 82.5% (1994–2005),36 mortality in infants <1 year of age continues to account for nearly half of the deaths associated with congenital heart defects.36a
When CDC data on multiple causes of death were used to examine mortality in cyanotic and acyanotic lesions between 1979 and 2005, all-age death rates had declined by 60% for VSD and 40% for TOF.37
In population-based data from Canada, 8123 deaths occurred in 71 686 congenital HD patients followed up for nearly 1 million patient-years. Overall mortality decreased by 31%, and the median age of death increased from 2 to 23 years between 1987 and 2005.3
Mortality after congenital heart surgery also differs between races/ethnicities after adjustment for access to care. The risk of in-hospital mortality for minority patients compared with white patients is 1.22 (95% CI, 1.05–1.41) for Hispanics, 1.27 (95% CI, 1.09–1.47) for non-Hispanic blacks, and 1.56 (95% CI, 1.37–1.78) for other non-Hispanics.38 Similarly, another study found that a higher risk of in-hospital mortality was associated with nonwhite race (OR, 1.36; 95% CI, 1.19–1.54), as well as Medicaid insurance (OR, 1.26; 95% CI, 1.09–1.46).39
According to CDC multiple-cause death data, from 1999 to 2006, sex differences in mortality over time varied with age. Between the ages of 18 and 34 years, mortality over time decreased significantly in females but not in males.40
On the basis of data from HCUP’s Kids’ Inpatient Database from 2000, 2003, and 2006, male children had more congenital heart defect surgeries in infancy, more high-risk surgeries, and more procedures to correct multiple congenital heart defects. Female infants with high-risk congenital heart defects had a 39% higher adjusted mortality.41
In 2007, 189 000 life-years were lost before 55 years of age because of deaths attributable to congenital cardiovascular defects. This is almost as many life-years as were lost from leukemia and asthma combined (NHLBI tabulation of NCHS mortality data).
Data from studies conducted in 15 North American centers by the Pediatric Heart Network revealed that even in lesions associated with the highest mortality among congenital lesions, such as HPLHS, aggressive palliation can lead to an increase in the 12-month survival rate, from 64% to 74%.42
Data analysis for the STS Congenital Heart Surgery Database, a voluntary registry with self-reported data for a 4-year cycle (2007–2010) from 103 centers performing congenital heart surgery (98 from the United States, 3 from Canada, and 1 from Japan),43 showed that of 95 357 total operations, the overall aggregate hospital discharge mortality rate was 3.5%.44 Specifically, the mortality rate was 10.1% for neonates (0–30 days of age),45 2.9% for infants (31 days to 1 year of age),46 1.1% for children (>1 year to 18 years of age),47 and 1.9% for adults (>18 years of age).48
Using the Nationwide Inpatient Sample 1988 to 2003, mortality was examined for 12 congenital heart defect procedures. A total of 30 250 operations were identified, which yielded a national estimate of 152 277±7875 operations. Of these, 27% were performed in patients ≥18 years of age. The overall in-hospital mortality rate for adult patients with congenital heart defects was 4.71% (95% CI, 4.19%– 5.23%), with a significant reduction in mortality observed when surgery was performed on such adult patients by pediatric versus nonpediatric heart surgeons (1.87% versus 4.84%; P<0.0001).49
Hospitalizations
(See Table 15-1.)
In 2004, birth defects accounted for >139 000 hospitalizations, representing 47.4 stays per 100 000 people. Cardiac and circulatory congenital anomalies accounted for 34% of all hospital stays for birth defects. Although the most common congenital lesions were shunts, including patent ductus arteriosus, VSDs, and ASDs, TOF accounted for a higher proportion of in-hospital death than any other birth defect. Between 1997 and 2004, hospitalization rates increased by 28.5% for cardiac and circulatory congenital anomalies.50
Cost
From data from the HCUP 2003 Kids’ Inpatient Database and 2003 information on birth defects in the Congenital Malformations Surveillance Report, it was found that the most expensive average neonatal hospital charges were for 2 congenital heart defects: HPLHS ($199 597) and common truncus arteriosus ($192 781). Two other cardiac defects, coarctation of the aorta and TGA, were associated with average hospital charges in excess of $150 000. For the 11 selected cardiovascular congenital defects (of 35 birth defects considered), there were 11 578 hospitalizations in 2003 and 1550 in-hospital deaths (13.4%). Estimated total hospital charges for these 11 conditions were $1.4 billion.51
In 2004, hospital costs for congenital cardiovascular defect conditions totaled $2.6 billion. The highest aggregate costs were for stays related to cardiac and circulatory congenital anomalies, which accounted for ≈$1.4 billion, more than half of all hospital costs for birth defects.50
Data from 1941 neonates with HPLHS showed a median cost of $99 070 for stage 1 palliation (Norwood or Sano procedure), $35 674 for stage 2 palliation (Glenn procedure), $36 928 for stage 3 palliation (Fontan procedure), and $289 292 for transplantation.52
In 2124 patients undergoing congenital heart operations between 2001 and 2007, total costs for the surgeries were $12 761 (ASD repair), $18 834 (VSD repair), $28 223 (TOF repair), and $55 430 (arterial switch operation).53
Kawasaki Disease
ICD-9 446.1; ICD-10 M30.3.
Mortality—8. Any-mention mortality—12.
The incidence of Kawasaki disease is rising worldwide, including in the United States, where the hospitalization rate rose from 17.5/100 000 children aged <5 years to 20.8/100 000 children <5 years in 2006.54 In 2010, Japan experienced its highest-ever incidence rate of 239.6 cases per 100 000 children aged <4 years,55 and in Korea, the rate reached 113.1/100 000 children <5 years old in 2008.56 A recent study reports a rate of 164.6/100 000 in children <5 years old in Taiwan.57
In addition to geographic variation in the incidence of Kawasaki disease, the age of children affected may also differ. In northern Europe (Finland, Sweden, and Norway), 67.8% of patients with Kawasaki disease were <5 years of age, compared with 86.4% of patients in Japan (P<0.001).58
US states with higher Asian American populations have higher rates of Kawasaki disease; for example, rates are 2.5-fold higher in Hawaii than in the continental United States.59
Boys have a 1.5-fold higher incidence of Kawasaki disease than girls.59
An estimated 5523 hospitalizations for Kawasaki disease occurred in the United States in 2006, with a mean patient age of 3 years. Race-specific incidence rates indicate that Kawasaki disease is most common among Americans of Asian and Pacific Island descent (30.3/100 000 children <5 years of age), occurs with intermediate frequency in non- Hispanic blacks (17.5/100 000 children <5 years of age) and Hispanics (15.7/100 000 children <5 years of age), and is least common in whites (12.0/100 000 children <5 years of age).60
Kawasaki disease is more common during the winter and early spring months, except in Hawaii, where no clear seasonal trend is seen61; it occurs more often in boys than girls at a ratio of ≈1.5:1, and 76.8% of children with Kawasaki disease are <5 years of age.54,59,60
-
Data from the Kids’ Inpatient Database59 show a hospitalization rate for Kawasaki disease for children <5 years of
19 per 100 000 in 2009
20.8 per 100 000 in 2006
17.3 per 100 000 in 2003
17.5 per 100 000 in 2000
Addition of prednisolone to the standard regimen of intravenous immunoglobulin for patients with severe Kawasaki disease appears to result in a substantial reduction in the incidence of coronary artery anomalies (RR, 0.20; 95% CI, 0.12–0.28).62
- 1.Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, del Nido P, Fasules JW, Graham TP, Jr, Hijazi ZM, Hunt SA, King ME, Landzberg MJ, Miner PD, Radford MJ, Walsh EP, Webb GD. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease) Circulation. 2008;118:e714–e833. doi: 10.1161/CIRCULATIONAHA.108.190690. [DOI] [PubMed] [Google Scholar]
- 2.Sable C, Foster E, Uzark K, Bjornsen K, Canobbio MM, Connolly HM, Graham TP, Gurvitz MZ, Kovacs A, Meadows AK, Reid GJ, Reiss JG, Rosenbaum KN, Sagerman PJ, Saidi A, Schonberg R, Shah S, Tong E, Williams RG on behalf of the American Heart Association Congenital Heart Defects Committee of the Council on Cardiovascular Disease in the Young, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Best practices in managing transition to adulthood for adolescents with congenital heart disease: the transition process and medical and psychosocial issues: a scientific statement from the American Heart Association. Circulation. 2011;123:1454–1485. doi: 10.1161/CIR.0b013e3182107c56. [DOI] [PubMed] [Google Scholar]
- 3.Khairy P, Ionescu-Ittu R, Mackie AS, Abrahamowicz M, Pilote L, Marelli AJ. Changing mortality in congenital heart disease. J Am Coll Cardiol. 2010;56:1149–1157. doi: 10.1016/j.jacc.2010.03.085. [DOI] [PubMed] [Google Scholar]
- 4.Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A. Prevalence of congenital heart defects in metropolitan Atlanta, 1998–2005. J Pediatr. 2008;153:807–813. doi: 10.1016/j.jpeds.2008.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roguin N, Du ZD, Barak M, Nasser N, Hershkowitz S, Milgram E. High prevalence of muscular ventricular septal defect in neonates. J Am Coll Cardiol. 1995;26:1545–1548. doi: 10.1016/0735-1097(95)00358-4. [DOI] [PubMed] [Google Scholar]
- 6.van der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, Roos-Hesselink JW. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58:2241–2247. doi: 10.1016/j.jacc.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 7.Botto LD, Correa A, Erickson JD. Racial and temporal variations in the prevalence of heart defects. Pediatrics. 2001;107:E32. doi: 10.1542/peds.107.3.e32. [DOI] [PubMed] [Google Scholar]
- 8.Koppel RI, Druschel CM, Carter T, Goldberg BE, Mehta PN, Talwar R, Bierman FZ. Effectiveness of pulse oximetry screening for congenital heart disease in asymptomatic newborns. Pediatrics. 2003;111:451–455. doi: 10.1542/peds.111.3.451. [DOI] [PubMed] [Google Scholar]
- 9.Bedard T, Lowry RB, Sibbald B, Harder JR, Trevenen C, Horobec V, Dyck JD. Congenital heart defect case ascertainment by the Alberta Congenital Anomalies Surveillance System. Birth Defects Res Part A Clin Mol Teratol. 2012;94:449–458. doi: 10.1002/bdra.23007. [DOI] [PubMed] [Google Scholar]
- 10.Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, Anderson P, Mason CA, Collins JS, Kirby RS, Correa A National Birth Defects Prevention Network. Updated national birth prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin Mol Teratol. 2010;88:1008–1016. doi: 10.1002/bdra.20735. [DOI] [PubMed] [Google Scholar]
- 11.Marelli AJ, Therrien J, Mackie AS, Ionescu-Ittu R, Pilote L. Planning the specialized care of adult congenital heart disease patients: from numbers to guidelines: an epidemiologic approach. Am Heart J. 2009;157:1–8. doi: 10.1016/j.ahj.2008.08.029. [DOI] [PubMed] [Google Scholar]
- 12.Moller JH. Perspectives in Pediatric Cardiology: Surgery of Congenital Heart Disease: Pediatric Cardiac Care Consortium, 1984–1995. Armonk, NY: Futura Publishing; 1998. Prevalence and incidence of cardiac malformation; pp. 19–26. [Google Scholar]
- 13.Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–1900. doi: 10.1016/s0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 14.Warnes CA, Liberthson R, Danielson GK, Dore A, Harris L, Hoffman JI, Somerville J, Williams RG, Webb GD. Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 2001;37:1170–1175. doi: 10.1016/s0735-1097(01)01272-4. [DOI] [PubMed] [Google Scholar]
- 15.Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E, Pilote L. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007;115:163–172. doi: 10.1161/CIRCULATIONAHA.106.627224. [DOI] [PubMed] [Google Scholar]
- 16.Hoffman JI, Kaplan S, Liberthson RR. Prevalence of congenital heart disease. Am Heart J. 2004;147:425–439. doi: 10.1016/j.ahj.2003.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Jenkins KJ, Correa A, Feinstein JA, Botto L, Britt AE, Daniels SR, Elixson M, Warnes CA, Webb CL on behalf of the American Heart Association Council on Cardiovascular Disease in the Young. Noninherited risk factors and congenital cardiovascular defects: current knowledge: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young. Circulation. 2007;115:2995–3014. doi: 10.1161/CIRCULATIONAHA.106.183216. [DOI] [PubMed] [Google Scholar]
- 18.Wilson PD, Loffredo CA, Correa-Villaseñor A, Ferencz C. Attributable fraction for cardiac malformations. Am J Epidemiol. 1998;148:414–423. doi: 10.1093/oxfordjournals.aje.a009666. [DOI] [PubMed] [Google Scholar]
- 19.Malik S, Cleves MA, Honein MA, Romitti PA, Botto LD, Yang S, Hobbs CA National Birth Defects Prevention Study. Maternal smoking and congenital heart defects. Pediatrics. 2008;121:e810–e816. doi: 10.1542/peds.2007-1519. [DOI] [PubMed] [Google Scholar]
- 20.Alverson CJ, Strickland MJ, Gilboa SM, Correa A. Maternal smoking and congenital heart defects in the Baltimore-Washington Infant Study. Pediatrics. 2011;127:e647–e653. doi: 10.1542/peds.2010-1399. [DOI] [PubMed] [Google Scholar]
- 21.Patel SS, Burns TL, Botto LD, Riehle-Colarusso TJ, Lin AE, Shaw GM, Romitti PA National Birth Defects Prevention Study. Analysis of selected maternal exposures and non-syndromic atrioventricular septal defects in the National Birth Defects Prevention Study, 1997–2005. Am J Med Genet A. 2012;158A:2447–2455. doi: 10.1002/ajmg.a.35555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mateja WA, Nelson DB, Kroelinger CD, Ruzek S, Segal J. The association between maternal alcohol use and smoking in early pregnancy and congenital cardiac defects. J Womens Health (Larchmt) 2012;21:26–34. doi: 10.1089/jwh.2010.2582. [DOI] [PubMed] [Google Scholar]
- 23.Baardman ME, Kerstjens-Frederikse WS, Corpeleijn E, de Walle HE, Hofstra RM, Berger RM, Bakker MK. Combined adverse effects of maternal smoking and high body mass index on heart development in offspring: evidence for interaction? Heart. 2012;98:474–479. doi: 10.1136/heartjnl-2011-300822. [DOI] [PubMed] [Google Scholar]
- 24.Strickland MJ, Klein M, Correa A, Reller MD, Mahle WT, Riehle-Colarusso TJ, Botto LD, Flanders WD, Mulholland JA, Siffel C, Marcus M, Tolbert PE. Ambient air pollution and cardiovascular malformations in Atlanta, Georgia, 1986–2003. Am J Epidemiol. 2009;169:1004–1014. doi: 10.1093/aje/kwp011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waller DK, Shaw GM, Rasmussen SA, Hobbs CA, Canfield MA, Siega-Riz AM, Gallaway MS, Correa A National Birth Defects Prevention Study. Prepregnancy obesity as a risk factor for structural birth defects. Arch Pediatr Adolesc Med. 2007;161:745–750. doi: 10.1001/archpedi.161.8.745. [DOI] [PubMed] [Google Scholar]
- 26.Scanlon KS, Ferencz C, Loffredo CA, Wilson PD, Correa-Villaseñor A, Khoury MJ, Willett WC. Preconceptional folate intake and malformations of the cardiac outflow tract: Baltimore-Washington Infant Study Group. Epidemiology. 1998;9:95–98. [PubMed] [Google Scholar]
- 27.Ionescu-Ittu R, Marelli AJ, Mackie AS, Pilote L. Prevalence of severe congenital heart disease after folic acid fortification of grain products: time trend analysis in Quebec, Canada. BMJ. 2009;338:b1673. doi: 10.1136/bmj.b1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Correa A, Gilboa SM, Besser LM, Botto LD, Moore CA, Hobbs CA, Cleves MA, Riehle-Colarusso TJ, Waller DK, Reece EA. Diabetes mellitus and birth defects. Am J Obstet Gynecol. 2008;199:237.e1–237.e9. doi: 10.1016/j.ajog.2008.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Snijder CA, Vlot IJ, Burdorf A, Obermann-Borst SA, Helbing WA, Wildhagen MF, Steegers EA, Steegers-Theunissen RP. Congenital heart defects and parental occupational exposure to chemicals. Hum Reprod. 2012;27:1510–1517. doi: 10.1093/humrep/des043. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1999–2010. Series 20 No. 2P. [Accessed July 21, 2013];CDC WONDER Online Database [database online] Released January 2013. http://wonder.cdc.gov/cmf-icd10.html.
- 31.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File: Underlying Cause-of-Death. [Accessed July 18, 2012];CDC WONDER Online Database [database online] Released January 2013. http://wonder.cdc.gov/mortSQl.html.
- 32.Centers for Disease Control and Prevention, National Center for Health Statistics. Linked Birth/Infant Death Records. [Accessed September 16, 2013];CDC WONDER Online Database [database online] Released January 2013. http://wonder.cdc.gov/lbd.html.
- 33.Cnota JF, Gupta R, Michelfelder EC, Ittenbach RF. Congenital heart disease infant death rates decrease as gestational age advances from 34 to 40 weeks. J Pediatr. 2011;159:761–765. doi: 10.1016/j.jpeds.2011.04.020. [DOI] [PubMed] [Google Scholar]
- 34.Swenson AW, Dechert RE, Schumacher RE, Attar MA. The effect of late preterm birth on mortality of infants with major congenital heart defects. J Perinatol. 2012;32:51–54. doi: 10.1038/jp.2011.50. [DOI] [PubMed] [Google Scholar]
- 35.Archer JM, Yeager SB, Kenny MJ, Soll RF, Horbar JD. Distribution of and mortality from serious congenital heart disease in very low birth weight infants. Pediatrics. 2011;127:293–299. doi: 10.1542/peds.2010-0418. [DOI] [PubMed] [Google Scholar]
- 36.Oster ME, Lee KA, Honein MA, Riehle-Colarusso T, Shin M, Correa A. Temporal trends in survival among infants with critical congenital heart defects. Pediatrics. 2013;131:e1502–e1508. doi: 10.1542/peds.2012-3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36a.Boneva RS, Botto LD, Moore CA, Yang Q, Correa A, Erickson JD. Mortality associated with congenital heart defects in the United States: trends and racial disparities, 1979–1997. Circulation. 2001;103:2376–2381. doi: 10.1161/01.cir.103.19.2376. [DOI] [PubMed] [Google Scholar]
- 37.Pillutla P, Shetty KD, Foster E. Mortality associated with adult congenital heart disease: trends in the US population from 1979 to 2005. Am Heart J. 2009;158:874–879. doi: 10.1016/j.ahj.2009.08.014. [DOI] [PubMed] [Google Scholar]
- 38.Oster ME, Strickland MJ, Mahle WT. Racial and ethnic disparities in post-operative mortality following congenital heart surgery. J Pediatr. 2011;159:222–226. doi: 10.1016/j.jpeds.2011.01.060. [DOI] [PubMed] [Google Scholar]
- 39.Chan T, Pinto NM, Bratton SL. Racial and insurance disparities in hospital mortality for children undergoing congenital heart surgery. Pediatr Cardiol. 2012;33:1026–1039. doi: 10.1007/s00246-012-0221-z. [DOI] [PubMed] [Google Scholar]
- 40.Gilboa SM, Salemi JL, Nembhard WN, Fixler DE, Correa A. Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation. 2010;122:2254–2263. doi: 10.1161/CIRCULATIONAHA.110.947002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marelli A, Gauvreau K, Landzberg M, Jenkins K. Sex differences in mortality in children undergoing congenital heart disease surgery: a United States population-based study. Circulation. 2010;122(suppl):S234–S240. doi: 10.1161/CIRCULATIONAHA.109.928325. [DOI] [PubMed] [Google Scholar]
- 42.Ohye RG, Sleeper LA, Mahony L, Newburger JW, Pearson GD, Lu M, Goldberg CS, Tabbutt S, Frommelt PC, Ghanayem NS, Laussen PC, Rhodes JF, Lewis AB, Mital S, Ravishankar C, Williams IA, Dunbar-Masterson C, Atz AM, Colan S, Minich LL, Pizarro C, Kanter KR, Jaggers J, Jacobs JP, Krawczeski CD, Pike N, McCrindle BW, Virzi L, Gaynor JW Pediatric Heart Network Investigators. Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med. 2010;362:1980–1992. doi: 10.1056/NEJMoa0912461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Society of Thoracic Surgeons. The Society of Thoracic Surgeons (STS) National Database: congenital heart surgery database participants. [Accessed July 30, 2012];Society of Thoracic Surgeons Web site. http://www.sts.org/sites/default/files/documents/DatabaseMap%20-%20CONGENITAL%2012.31.pdf.
- 44.Society of Thoracic Surgeons. STS congenital heart surgery data summary: July 2006-June 2010 procedures: all patients. [Accessed July 18, 2011];Society of Thoracic Surgeons Web site. http://www.sts.org/sites/default/files/documents/STSCONG-AllPatientsSummary_Fall2010.pdf.
- 45.Society of Thoracic Surgeons. STS congenital heart surgery data summary: July 2006-June 2010 procedures: neonates (0–30 days) [Accessed July 18, 2011];Society of Thoracic Surgeons Web site. http://www.sts.org/sites/default/files/documents/STSCONG-NeonatesSummary_Fall2010.pdf.
- 46.Society of Thoracic Surgeons. STS congenital heart surgery data summary: July 2006-June 2010 procedures: infants (31 days-1 year) [Accessed July 18, 2011];Society of Thoracic Surgeons Web site. http://www.sts.org/sites/default/files/documents/STSCONG-InfantsSummary_Fall2010.pdf.
- 47.Society of Thoracic Surgeons. STS congenital heart surgery data summary: July 2006-June 2010 procedures: children (>1 year to <18 years) [Accessed July 18, 2011];Society of Thoracic Surgeons Web site. http://www.sts.org/sites/default/files/documents/STSCONG-ChildrenSummary_Fall2010.pdf.
- 48.Society of Thoracic Surgeons. STS congenital heart surgery data summary: July 2006-June 2010 procedures: adult (18 years+) [Accessed July 18, 2011];Society of Thoracic Surgeons Web site. http://www.sts.org/sites/default/files/documents/STSCONG-AdultsSummary_Fall2010.pdf.
- 49.Karamlou T, Diggs BS, Person T, Ungerleider RM, Welke KF. National practice patterns for management of adult congenital heart disease: operation by pediatric heart surgeons decreases in-hospital death. Circulation. 2008;118:2345–2352. doi: 10.1161/CIRCULATIONAHA.108.776963. [DOI] [PubMed] [Google Scholar]
- 50.Russo CA, Elixhauser A. Hospitalizations for Birth Defects, 2004. Rockville, MD: US Agency for Healthcare Research and Quality; Jan, 2007. [Accessed July 18, 2011]. HCUP Statistical Brief No. 24. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb24.pdf. [PubMed] [Google Scholar]
- 51.Centers for Disease Control and Prevention (CDC) Hospital stays, hospital charges, and in-hospital deaths among infants with selected birth defects: United States, 2003. MMWR Morb Mortal Wkly Rep. 2007;56:25–29. [PubMed] [Google Scholar]
- 52.Dean PN, Hillman DG, McHugh KE, Gutgesell HP. Inpatient costs and charges for surgical treatment of hypoplastic left heart syndrome. Pediatrics. 2011;128:e1181–e1186. doi: 10.1542/peds.2010-3742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pasquali SK, Sun JL, d’Almada P, Jaquiss RD, Lodge AJ, Miller N, Kemper AR, Lannon CM, Li JS. Center variation in hospital costs for patients undergoing congenital heart surgery. Circ Cardiovasc Qual Outcomes. 2011;4:306–312. doi: 10.1161/CIRCOUTCOMES.110.958959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Luca NJ, Yeung RS. Epidemiology and management of Kawasaki disease. Drugs. 2012;72:1029–1038. doi: 10.2165/11631440-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 55.Nakamura Y, Yashiro M, Uehara R, Sadakane A, Tsuboi S, Aoyama Y, Kotani K, Tsogzolbaatar EO, Yanagawa H. Epidemiologic features of Kawasaki disease in Japan: results of the 2009–2010 nationwide survey. J Epidemiol. 2012;22:216–221. doi: 10.2188/jea.JE20110126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Park YW, Han JW, Hong YM, Ma JS, Cha SH, Kwon TC, Lee SB, Kim CH, Lee JS, Kim CH. Epidemiological features of Kawasaki disease in Korea, 2006–2008. Pediatr Int. 2011;53:36–39. doi: 10.1111/j.1442-200X.2010.03178.x. [DOI] [PubMed] [Google Scholar]
- 57.Wu MH, Chen HC, Yeh SJ, Lin MT, Huang SC, Huang SK. Prevalence and the long-term coronary risks of patients with Kawasaki disease in a general population <40 years: a national database study. Circ Cardiovasc Qual Outcomes. 2012;5:566–570. doi: 10.1161/CIRCOUTCOMES.112.965194. [DOI] [PubMed] [Google Scholar]
- 58.Salo E, Griffiths EP, Farstad T, Schiller B, Nakamura Y, Yashiro M, Uehara R, Best BM, Burns JC. Incidence of Kawasaki disease in northern European countries. Pediatr Int. 2012;54:770–772. doi: 10.1111/j.1442-200X.2012.03692.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Uehara R, Belay ED. Epidemiology of Kawasaki disease in Asia, Europe, and the United States. J Epidemiol. 2012;22:79–85. doi: 10.2188/jea.JE20110131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Holman RC, Belay ED, Christensen KY, Folkema AM, Steiner CA, Schonberger LB. Hospitalizations for Kawasaki syndrome among children in the United States, 1997–2007. Pediatr Infect Dis J. 2010;29:483–488. doi: 10.1097/INF.0b013e3181cf8705. [DOI] [PubMed] [Google Scholar]
- 61.Holman RC, Christensen KY, Belay ED, Steiner CA, Effler PV, Miyamura J, Forbes S, Schonberger LB, Melish M. Racial/ethnic differences in the incidence of Kawasaki syndrome among children in Hawaii. Hawaii Med J. 2010;69:194–197. [PMC free article] [PubMed] [Google Scholar]
- 62.Kobayashi T, Saji T, Otani T, Takeuchi K, Nakamura T, Arakawa H, Kato T, Hara T, Hamaoka K, Ogawa S, Miura M, Nomura Y, Fuse S, Ichida F, Seki M, Fukazawa R, Ogawa C, Furuno K, Tokunaga H, Takatsuki S, Hara S, Morikawa A RAISE Study Group Investigators. Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (RAISE study): a randomised, open-label, blinded-endpoints trial. Lancet. 2012;379:1613–1620. doi: 10.1016/S0140-6736(11)61930-2. [DOI] [PubMed] [Google Scholar]
- 63.Sands AJ, Casey FA, Craig BG, Dornan JC, Rogers J, Mulholland HC. Incidence and risk factors for ventricular septal defect in “low risk” neonates. Arch Dis Child Fetal Neonatal Ed. 1999;81:F61–F63. doi: 10.1136/fn.81.1.f61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Larson EW, Edwards WD. Risk factors for aortic dissection: a necropsy study of 161 cases. Am J Cardiol. 1984;53:849–855. doi: 10.1016/0002-9149(84)90418-1. [DOI] [PubMed] [Google Scholar]
- 65.Ma M, Gauvreau K, Allan CK, Mayer JE, Jr, Jenkins KJ. Causes of death after congenital heart surgery. Ann Thorac Surg. 2007;83:1438–1445. doi: 10.1016/j.athoracsur.2006.10.073. [DOI] [PubMed] [Google Scholar]
16. Disorders of Heart Rhythm
See Tables 16-1 and 16-2.
Table 16-1.
Incidence and Outcome of Out-of-Hospital Cardiac Arrest in the United States, 2011
| Incidence per 100 000, Point Estimate (95% CI) | Annual Number of Cases in United States, Point Estimate (Quasi CI) | Annual Number of Fatalities in United States, Point Estimate (Quasi CI) | Survival, Point Estimate (95% CI), % | |
|---|---|---|---|---|
| EMS assessed | ||||
| Overall | 134.1 (131.7–136.6) | 424 000 (417 000–432 000) | 401 000 (392 000–410 000) | 5.2 (4.8–5.6) |
| Adults | 135.8 (133.0–138.7) | 322 000 (315 000–328 000) | 299 000 (291 000–307 000) | 6.7 (6.2–7.2) |
| Children | 11.9 (10.5–13.4) | 9500 (8400–10 700) | 8800 (7500–10 200) | 4.4 (2.0–6.9) |
| EMS treated | ||||
| Overall | 66.7 (64.9–68.4) | 211 000 (205 000–216 000) | 187 000 (181 000–194 000) | 10.4 (9.7–11.2) |
| Adults | 84.8 (82.5–87.0) | 201 000 (195 000–206 000) | 178 000 (172 000–184 000) | 10.7 (9.9–11.5) |
| Children | 9.7 (8.4–11.1) | 7700 (6700–8800) | 7000 (5800–8400) | 5.4 (2.4–8.4) |
| Shockable rhythm | ||||
| Overall | 13.4 (12.6–14.2) | 42 000 (40 000–45 000) | 30 000 (27 000–33 000) | 28.3 (25.7–30.8) |
| Adults | 17.4 (16.4–18.5) | 41 000 (39 000–44 000) | 29 000 (26 000–32 000) | 28.4 (25.9–30.9) |
| Children | 0.7 (0.3–1.0) | 560 (240–800) | 370 (100–720) | 26.7 (4.3–49.1) |
| Bystander-witnessed shockable rhythm | ||||
| Overall | 7.7 (7.1–8.3) | 24 000 (22 000–26 000) | 16 000 (14 000–18 000) | 31.7 (28.3–35.2) |
| Adults | 10.1 (9.3–10.9) | 24 000 (22 000–26 000) | 16 000 (14 000–18 000) | 31.7 (28.2–35.1) |
| Children | 0.3 (0.1–0.5) | 240 (80–400) | 160 (30–360) | 26.7 (4.3–49.0) |
US sites only; 2011 cases.
CI indicates confidence interval; and EMS, emergency medical services.
Source: Resuscitation Outcomes Consortium Investigators, unpublished data, July 23, 2013.
Table 16-2.
Outcome of In-Hospital Cardiac Arrest in United States, 2011
| Survival, % | Point Estimate (95% CI) | |
|---|---|---|
| Treated IHCA | ||
| Adults | 22.7 | 22.0–23.4 |
| Children | 36.8 | 32.6–41 |
| Shockable rhythm | ||
| Adults | 41.5 | 39.3–43.7 |
| Children | 33.3 | 15.5–51.1 |
CI indicates confidence interval; and IHCA, in-hospital cardiac arrest.
Source: Get With The Guidelines–Resuscitation Investigators, unpublished data, July 27, 2013.
Bradyarrhythmias
ICD-9 426.0, 426.1, 427.81; ICD-10 I44.0 to I44.3, I49.5.
Mortality—841. Any-mention mortality—4927. Hospital discharges—110 000.
AV Block
Prevalence and Incidence
The prevalence of first-degree AV block in NHANES III was 3.7%.1
In a healthy sample of subjects from the ARIC study (mean age 53 years), the prevalence of first-degree AV block was 7.8% in black men, 3.0% in black women, 2.1% in white men, and 1.3% in white women.2 Lower prevalence estimates were noted in the relatively younger population (mean age 45 years) of the CARDIA study at its year 20 follow-up examination: 2.6% in black men, 1.9% in black women, 1.2% in white men, and 0.1% in white women.2
Mobitz II second-degree AV block is rare in healthy individuals (≈0.003%), whereas Mobitz I (Wenckebach) is observed in 1% to 2% of healthy young people, especially during sleep.2
The prevalence of third-degree AV block in the general adult population is ≈0.02% to 0.04%.3,4
Third-degree AV block is very rare in apparently healthy individuals. Johnson et al5 found only 1 case among >67 000 symptom-free individuals; Rose et al,6 in their study of >18 000 civil servants, did not find any cases. On the other hand, among 293 124 patients with DM and 552 624 with hypertension enrolled with Veterans Health Administration hospitals, third-degree AV block was present in 1.1% and 0.6% of those patients, respectively.7
Congenital complete AV block is estimated to occur in 1 of 15 000 to 25 000 live births.2
Abbreviations Used in Chapter 16
| AF | atrial fibrillation |
| AHA | American Heart Association |
| AMI | acute myocardial infarction |
| ARIC | Atherosclerosis Risk in Communities study |
| ASSERT | Asymptomatic Atrial Fibrillation and Stroke Evaluation in Pacemaker Patients and the Atrial Fibrillation Reduction Atrial Pacing Trial |
| AV | atrioventricular |
| BMI | body mass index |
| BP | blood pressure |
| CABG | coronary artery bypass graft |
| CAD | coronary artery disease |
| CARDIA | Coronary Artery Risk Development in Young Adults |
| CASQ2 | calsequestrin 2 |
| CHD | coronary heart disease |
| CHS | Cardiovascular Health Study |
| CI | confidence interval |
| CKD | chronic kidney disease |
| CPR | cardiopulmonary resuscitation |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| ECG | electrocardiogram |
| ED | emergency department |
| EMPHASIS-HF | Eplerenone in MildPatients Hospitalization And Survival Study in Heart Failure |
| EMS | emergency medical services |
| FHS | Framingham Heart Study |
| GBD | Global Burden of Diseases, Injuries, and Risk Factors Study |
| GWTG | Get With The Guidelines |
| HCM | hypertrophic cardiomyopathy |
| HD | heart disease |
| HF | heart failure |
| HR | hazard ratio |
| ICD-9 | International Classification of Diseases, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| MI | myocardial infarction |
| IHCA | in-hospital cardiac arrest |
| NCHS | National Center for Health Statistics |
| NHANES | National Health and Nutrition Examination Survey |
| NHDS | National Hospital Discharge Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| OR | odds ratio |
| PA | physical activity |
| PAR | population attributable risk |
| PVT | polymorphic ventricular tachycardia |
| RR | relative risk |
| RYR2 | ryanodine type 2 receptor |
| SBP | systolic blood pressure |
| SD | standard deviation |
| SVT | supraventricular tachycardia |
| TdP | torsade de pointes |
| VF | ventricular fibrillation |
| VT | ventricular tachycardia |
| YLL | years of life lost |
Risk Factors
Although first-degree AV block and Mobitz type I second-degree AV block can occur in apparently healthy individuals, presence of Mobitz II second-degree or third-degree AV block usually indicates underlying HD, including CHD and HF.2
Reversible causes of AV block include electrolyte abnormalities, drug-induced AV block, perioperative AV block attributable to hypothermia, or inflammation near the AV conduction system after surgery in this region. Some conditions may warrant pacemaker implantation because of the possibility of disease progression even if the AV block reverses transiently (eg, sarcoidosis, amyloidosis, and neuromuscular diseases).8
Long sinus pauses and AV block can occur during sleep apnea. In the absence of symptoms, these abnormalities are reversible and do not require pacing.9
Prevention
Aftermath
In the FHS, PR interval prolongation (>200 ms) was associated with an increased risk of AF (HR, 2.06; 95% CI, 1.36–3.12),11,12 pacemaker implantation (HR, 2.89; 95% CI, 1.83–4.57),12 and all-cause mortality (HR, 1.44; 95% CI, 1.09–1.91).12 Compared with individuals with a PR ≤200 ms, individuals with a PR interval >200 ms had an absolute increased risk per year of 1.04% for AF, 0.55% for pacemaker implantation, and 2.05% for death.
Patients with abnormalities of AV conduction may be asymptomatic or may experience serious symptoms related to bradycardia, ventricular arrhythmias, or both.
Decisions about the need for a pacemaker are influenced by the presence or absence of symptoms directly attributable to bradycardia. Permanent pacing improves survival in patients with third-degree AV block, especially if syncope has occurred.8 Nevertheless, the overall prognosis depends to a large extent on the underlying HD.
Although there is little evidence to suggest that pacemakers improve survival in patients with isolated first-degree AV block,13 it is now recognized that marked first-degree AV block (PR >300 ms) can lead to symptoms even in the absence of higher degrees of AV block.14
Prognosis
Investigators at Northwestern University compared older adult (age >60 years) outpatients with (n=470) and without (n=2090) asymptomatic bradycardia. Over a mean followup of 7.2 years, patients with asymptomatic bradycardia had a higher adjusted incidence of pacemaker insertion (HR, 2.14; 95% CI, 1.30–3.51; P=0.003), which appeared after a lag time of 4 years. However, the absolute rate of pacemaker implantation was low (<1% per year), and asymptomatic bradycardia was not associated with a higher risk of death.15
Sinus Node Dysfunction
Prevalence and Incidence
The prevalence of sinus node dysfunction has been estimated to be between 403 and 666 per million, with an incidence rate of 63 per million per year requiring pacemaker therapy.16
Sinus node dysfunction occurs in 1 of every 600 cardiac patients >65 years of age and accounts for ≈50% of implantations of pacemakers in the United States.17,17a
Sinus node dysfunction is commonly present with other causes of bradyarrhythmias (carotid sinus hypersensitivity in 33% of patients and advanced AV conduction abnormalities in 17%).18,19
Risk Factors
The causes of sinus node dysfunction can be classified as intrinsic (secondary to pathological conditions involving the sinus node) or extrinsic (caused by depression of sinus node function by external factors such as drugs or autonomic influences).20
Sinus node dysfunction may occur at any age but is primarily a disease of the elderly, with the average being ≈68 years of age.17
Idiopathic degenerative disease is probably the most common cause of sinus node dysfunction.21
Collected data from 28 different studies on atrial pacing for sinus node dysfunction showed a median annual incidence of complete AV block of 0.6% (range, 0%–4.5%) with a total prevalence of 2.1% (range, 0%–11.9%). This suggests that the degenerative process also affects the specialized conduction system, although the rate of progression is slow and does not dominate the clinical course of disease.22
Ischemic HD can be responsible for one third of cases of sinus node dysfunction. Transient sinus node dysfunction can complicate MI; it is common during inferior MI and is caused by autonomic influences. Cardiomyopathy, long-standing hypertension, infiltrative disorders (eg, amyloidosis and sarcoidosis), collagen vascular disease, and surgical trauma can also result in sinus node dysfunction.23,24
Aftermath
The course of sinus node dysfunction is typically progressive, with 57% of patients experiencing symptoms over a 4-year period if untreated, and a 23% prevalence of syncope over the same time frame.25
Approximately 50% of patients with sinus node dysfunction develop tachy-brady syndrome over a lifetime; such patients have a higher risk of stroke and death. The survival of patients with sinus node dysfunction appears to depend primarily on the severity of underlying cardiac disease and is not significantly changed by pacemaker therapy.26–28
In a retrospective study,29 patients with sinus node dysfunction who had pacemaker therapy were followed up for 12 years; at 8 years, mortality among those with ventricular pacing was 59% compared with 29% among those with atrial pacing. This discrepancy may be attributed to selection bias. For instance, the physiological or anatomic disorder (eg, fibrosis of conductive tissue) that led to the requirement for the particular pacemaker may have influenced prognosis, rather than the type of pacemaker used.
The incidence of sudden death is extremely low, and sinus node dysfunction does not appear to affect survival whether untreated or treated with pacemaker therapy.8
SVT including AF occurs in 47% to 53% of patients with sinus node dysfunction.28,30
On the basis of records from the NHDS, age-adjusted pacemaker implantation rates increased progressively from 370 per million in 1990 to 612 per million in 2002. This escalating implantation rate is attributable to increasing implantation for isolated sinus node dysfunction; implantation for sinus node dysfunction increased by 102%, whereas implantation for all other indications did not increase.31
SVT (Excluding AF and Atrial Flutter)
ICD-9 427.0; ICD-10 I47.1.
Mortality—132. Any-mention mortality—1206. Hospital discharges—23 000.
Prevalence and Incidence
Data from the Marshfield Epidemiologic Study Area in Wisconsin suggested the incidence of documented paroxysmal SVT is 35 per 100 000 person-years. The mean age at SVT onset was 57 years, and both female sex and age >65 years were significant risk factors.32
A review of ED visits from 1993 to 2003 revealed that 550 000 visits were for SVT (0.05% of all visits; 95% CI, 0.04%–0.06%), or ≈50 000 visits per year. Of these patients, 24% (95% CI, 15%–34%) were admitted to the hospital, and 44% (95% CI, 32%–56%) were discharged without specific follow-up.33
The prevalence of SVT that is clinically undetected is likely much greater than the estimates from ED visits and electrophysiology procedures would suggest. For example, among a random sample of 604 participants in Finland, 7 (1.2%) fulfilled the diagnostic criteria for inappropriate sinus tachycardia.34
Of 1383 participants in the Baltimore Longitudinal Study of Aging undergoing maximal exercise testing, 6% exhibited SVT during the test; increasing age was a significant risk factor. Only 16% exhibited >10 beats of SVT, only 4% were symptomatic, and the SVT participants were more likely to develop spontaneous SVT or AF.35
From the surface ECG, the prevalence of atrial tachycardia is estimated to be 0.34% in asymptomatic patients and 0.46% in symptomatic patients.36
Aftermath
Specific Types
Among those presenting for invasive electrophysiological study and ablation, AV nodal reentrant tachycardia (a circuit that requires 2 AV nodal pathways) is the most common mechanism of SVT40,41 and usually represents the majority of cases (56% of 1 series of 1754 cases from Loyola University Medical Center).41
AV reentrant tachycardia (an arrhythmia that requires the presence of an extranodal connection between the atria and ventricles or specialized conduction tissue) is the second most common42,43 type of SVT (27% in the Loyola series),41 and atrial tachycardia is the third most common (17% in the Loyola series).41
In the pediatric population, AV reentrant tachycardia is the most common SVT mechanism, followed by AV nodal reentrant tachycardia and then atrial tachycardia.44
AV reentrant tachycardia prevalence decreases with age, whereas AV nodal reentrant tachycardia and atrial tachycardia prevalences increase with advancing age.41
The majority of AV reentrant tachycardia patients in the Loyola series were men (55%), whereas the majority of patients with AV nodal reentrant tachycardia (70%) or atrial tachycardia (62%) were women.41
Multifocal atrial tachycardia is an arrhythmia that is commonly confused with AF and is characterized by 3 distinct P-wave morphologies, irregular R-R intervals, and a rate >100 beats per minute. It is uncommon in both children42 and adults,43 with a prevalence in hospitalized adults estimated at 0.05% to 0.32%.45,46 The average age in adults is 70 to 72 years. Adults with multifocal atrial tachycardia have a mortality rate that is high, with estimates around 45%, but this is generally ascribed to the underlying condition(s).43,47
Wolff-Parkinson-White Syndrome
Wolff-Parkinson-White syndrome, a diagnosis reserved for those with both ventricular preexcitation (evidence of an anterograde conducting AV accessory pathway on a 12-lead ECG) and tachyarrhythmias,37 deserves special attention because of the associated risk of sudden death. Sudden death is generally attributed to rapid heart rates in AF conducting down an accessory pathway and leading to VF.48,49 Of note, AF is common in Wolff-Parkinson-White patients, and surgical or catheter ablation of the accessory pathway often results in elimination of the AF.50
Ventricular preexcitation with or without tachyarrhythmia was observed in 0.11% of 47 358 ECGs in adults participating in 4 large Belgian epidemiological studies45 and in 0.17% of 32 837 Japanese high school students in ECGs obtained by law before the students entered school.46
Asymptomatic adults with ventricular preexcitation appear to be at no increased risk of sudden death compared with the general population,48,49,51,52 although certain characteristics found during invasive electrophysiological study (including inducibility of AV reentrant tachycardia or AF, accessory pathway refractory period, and the shortest R-R interval during AF) can help risk stratify these patients.49,53
In a meta-analysis of 20 studies involving 1869 asymptomatic patients with a Wolff-Parkinson-White ECG pattern followed up for a total of 11 722 person-years, the risk of sudden death in a random effects model that was used because of heterogeneity across studies was estimated to be 1.25 (95% CI, 0.57–2.19) per 1000 person-years. Risk factors for sudden death included male sex, inclusion in a study of children (<18 years of age), and inclusion in an Italian study.54
Symptomatic adult patients with the Wolff-Parkinson-White syndrome are at a higher risk of sudden death. In a study of 60 symptomatic patients in Olmsted County, MN, including some who underwent curative surgery, 2 (3.3%) experienced sudden death over a 13-year period. Of 690 Wolff-Parkinson- White syndrome patients referred to a single hospital in the Netherlands, 15 (2.2%) had aborted sudden death, and VF was the first manifestation of the disease in 8 patients.55
Of 379 Wolff-Parkinson-White patients with induced AV reentrant tachycardia during electrophysiology study who did not undergo ablation, 29 (8%) exhibited a “malignant presentation” over a mean 3.6 years of follow-up: syncope/presyncope in 25 patients, rapid preexcited AF causing hemodynamic collapse in 3 patients, and VF in 1 patient.56 Those with such a presentation were more often male, had a shorter accessory pathway effective refractory period during electrophysiology study, more often had AV reentrant tachycardia that triggered AF during electrophysiology study, and more often had >1 accessory pathway.
Although some studies in asymptomatic children with ventricular preexcitation suggest a benign prognosis,51,57 others suggest that electrophysiological testing can identify a group of asymptomatic children with a risk of sudden death or VF as high as 11% over 19 months of follow-up.58
Subclinical Atrial Tachyarrhythmias and Unrecognized AF
Pacemakers and defibrillators have increased clinician awareness of the frequency of subclinical AF and atrial high-rate episodes in individuals without a documented history of AF. Several studies have suggested that device-detected high-rate atrial tachyarrhythmias are surprisingly frequent and are associated with an increased risk of AF,53 thromboembolism,53,59 and total mortality.53
-
Investigators in the ASSERT study prospectively enrolled 2580 patients with a recent pacemaker or defibrillator implantation who were ≥65 years of age, had a history of hypertension, and had no history of AF. They classified individuals by presence versus absence of subclinical atrial tachyarrhythmias (defined as atrial rate >190 beats per minute for >6 minutes in the first 3 months) and conducted follow- up for 2.5 years.60 Subclinical atrial tachyarrhythmias in the first 3 months occurred in 10.1% of the patients and were associated with the following:
An almost 6-fold higher risk of clinical AF (HR, 5.56; 95% CI, 3.78–8.17; P<0.001)
A more than doubling in the adjusted risk of the primary end point, ischemic stroke or systemic embolism (HR, 2.50; 95% CI, 1.28–4.89; P<0.008)
An annual ischemic stroke or systemic embolism rate of 1.69% (versus 0.69% in those without)
A 13% PAR for ischemic stroke or systemic embolism
Over the subsequent 2.5 years of follow-up, an additional 34.7% of the patients had subclinical atrial tachyarrhythmias, which were 8-fold more frequent than clinical AF episodes.
The appropriate therapy of subclinical atrial tachyarrhythmias has not been rigorously studied.
In a community-based study in Sweden, all inhabitants aged 75 to 76 years were invited to a stepwise screening program for AF. Of 848 participants, 10 had clinically unrecognized AF diagnosed on a 12-lead ECG. Of 403 individuals with ≥2 stroke risk factors who completed a 2-week once-a-day handheld ECG event recorder, an additional 30 were diagnosed with paroxysmal AF. The study suggests that the burden of unrecognized AF in the community is higher than appreciated.61
AF and Atrial Flutter
ICD-9 427.3; ICD-10 I48.
Prevalence
Estimates of the prevalence of AF in the United States ranged from ≈2.7 million to 6.1 million in 2010, and AF prevalence is expected to rise to between ≈5.6 and 12 million in 2050.62,63
Data from a California health plan suggest that compared with whites, blacks (OR, 0.49; 95% CI, 0.47–0.52), Asians (OR, 0.68; 95% CI, 0.64–0.72), and Hispanics (OR, 0.58; 95% CI, 0.55–0.61) have significantly lower adjusted prevalences of AF.64
-
Data from the NHDS/NCHS (1996–2001) on cases that included AF as a primary discharge diagnosis found the following:
Approximately 44.8% of patients were men.
The mean age for men was 66.8 years versus 74.6 years for women.
The racial breakdown for admissions was 71.2% white, 5.6% black, and 2.0% other races (20.8% were not specified).
Black patients were much younger than patients of other races.
Among Medicare patients aged ≥65 years, diagnosed from 1993 to 2007, the prevalence of AF increased ≈5% per year, from ≈41.1 per 1000 beneficiaries to 85.5 per 1000 beneficiaries.65
Incidence
-
Data from the NHDS/NCHS (1996–2001) on cases that included AF as a primary discharge diagnosis found the following:
The incidence in men ranged from 20.6 per 100 000 people per year for patients between 15 and 44 years of age to 1077.4 per 100 000 people per year for patients ≥85 years of age.
In women, the incidence ranged from 6.6 per 100 000 people per year for patients between 15 and 44 years of age to 1203.7 per 100 000 people per year for those ≥85 years of age.
-
In Olmsted County, MN
In a Medicare sample, the incidence of AF was ≈28 per 1000 person-years and did not change substantively between 1993 and 2007. Of individuals with incident AF in 2007, ≈55% were women, 91% were white, 84% had hypertension, 36% had HF, and 30% had cerebrovascular disease.65
Mortality
In 2010, AF was mentioned on 107 335 US death certificates and was the underlying cause in 16 454 of those deaths (NCHS, NHLBI).
In adjusted analyses from the FHS, AF was associated with an increased risk of death in both men (OR, 1.5; 95% CI, 1.2–1.8) and women (OR, 1.9; 95% CI, 1.5–2.2).68 Furthermore, there was an interaction with sex, such that AF appeared to diminish the survival advantage typically observed in women.
In Medicare beneficiaries ≥65 years of age with new-onset AF, mortality decreased modestly but significantly between 1993 and 2007. In 2007, the age- and sex-adjusted mortality at 30 days was 11%, and at 1 year, it was 25%.65
A study of >4600 patients diagnosed with first AF showed that risk of death within the first 4 months after the AF diagnosis was high. The most common causes of CVD death were CAD, HF, and ischemic stroke, which accounted for 22%, 14%, and 10%, respectively, of the early deaths (within the first 4 months) and 15%, 16%, and 7%, respectively, of the late deaths.69
AF is also associated with mortality in individuals with other cardiovascular conditions and procedures, including HF,66,70 MI,67,71 CABG,72,73 and stroke,74 and with noncardiovascular conditions such as sepsis75 and noncardiac surgery.76
Lifetime Risk and Cumulative Risk
Participants in the NHLBI-sponsored FHS were followed up from 1968 to 1999. At 40 years of age, remaining lifetime risks for AF were 26.0% for men and 23.0% for women. At 80 years of age, lifetime risks for AF were 22.7% for men and 21.6% for women. In further analysis, counting only those who had development of AF without prior or concurrent HF or MI, lifetime risk for AF was ≈16%.77
Investigators from the NHLBI-sponsored ARIC study observed that the cumulative risk of AF was 21% in white men, 17% in white women, and 11% in African Americans of both sexes by 80 years of age.78
Risk Factors
-
Standard risk factors
Both ARIC71 and FHS (http://www.framinghamheart-study.org/risk/atrial.html)11,79 have developed risk prediction models to predict new-onset AF. Predictors of increased risk of new-onset AF include advancing age, European ancestry, body size (greater height and BMI), electrocardiography features (left ventricular hypertrophy, left atrial enlargement), DM, BP (SBP and hypertension treatment), and presence of CVD (CHD, HF, valvular HD).
More recently, the ARIC, CHS, and FHS investigators developed and validated a risk prediction model.73
Other consistently reported risk factors for AF include clinical and subclinical hyperthyroidism,80,81 CKD,82 and heavy alcohol consumption.83
-
Family history
Although unusual, early-onset familial lone AF has long been recognized as a risk factor.84,85
-
In the past decade, the heritability of AF in the community has been appreciated. In studies from the FHS
Adjusted for coexistent risk factors, having at least 1 parent with AF was associated with a 1.85-fold increased risk of AF in the adult offspring (multivariable- adjusted 95% CI, 1.12–3.06; P=0.02).86
A history of a first-degree relative with AF also was associated with an increased risk of AF (HR, 1.40; 95% CI, 1.13–1.74).72 The risk was greater if the first-degree relative’s age of onset was ≤65 years (HR, 2.01; 95% CI, 1.49–2.71) and with each additional affected first-degree relative (HR, 1.24; 95% CI, 1.05–1.46).87
-
Genetics
Mutations in genes coding channels (sodium and potassium), gap junction proteins, and signaling have been described, often in lone AF or familial AF series, but they are responsible for few cases of AF in the community.88
Meta-analyses of genome-wide association studies have revealed single-nucleotide polymorphisms on chromosomes 4q25 (upstream of PITX2),89–91 16q22 (ZFHX3),90,92 and 1q21 (KCNN3),91 as well as 6 other novel susceptibility loci (near PRRX1, CAV1, C9orf3, SYNPO2L, SYNE2, and HCN4).93 Although an area of intensive inquiry, the causative single-nucleotide polymorphisms and the functional basis of the associations have not been revealed.
Awareness
In a US national biracial study of individuals with AF, compared with whites, blacks had approximately one third the likelihood (OR, 0.32; 95% CI, 0.20–0.52) of being aware that they had AF.94
Prevention
Data from the ARIC study indicated that having at least 1 elevated risk factor explained 50% and having at least 1 borderline risk factor explained 6.5% of incident AF cases. The estimated overall incidence rate per 1000 person-years at a mean age of 54.2 years was 2.19 for those with optimal risk, 3.68 for those with borderline risk, and 6.59 for those with elevated risk factors.95
Observational data from the CHS suggested that moderate-intensity exercise (such as regular walking) was associated with a lower risk of AF (HR, 0.72).97 However, data from many studies suggested that vigorous-intensity exercise 5 to 7 days a week was associated with a slightly increased risk of AF (HR, 1.20; P=0.04).98
Meta-analyses have suggested that renin-angiotensin system blockers may be useful in primary and secondary (recurrences) prevention of AF in trials of hypertension, after MI, in HF, and after cardioversion.74,99 However, the studies were primarily secondary or post hoc analyses, and the results were fairly heterogeneous. Recently, in an analysis of the EMPHASIS-HF trial, in one of many secondary outcomes, eplerenone was nominally observed to reduce the incidence of new-onset AF.100
Although heterogeneous in their findings, modest-sized short-term studies suggested that the use of statins might prevent AF; however, larger longer-term studies do not provide support that statins are effective in AF prevention.101
The NHLBI sponsored a workshop highlighting important research areas to advance the prevention of AF.102
Aftermath
-
Hospitalization
-
Hospital discharges—479 000.
-
-
Stroke
Stroke rates per 1000 patient-years declined in AF patients taking anticoagulants, from 46.7 in 1992 to 19.5 in 2002, for ischemic stroke but remained fairly steady for hemorrhagic stroke (1.6–2.9).105
When standard stroke risk factors were accounted for, AF was associated with a 4- to 5-fold increased risk of ischemic stroke.106
Although the RR of stroke associated with AF did not vary (≈3–5-fold increased risk) substantively with advancing age, the proportion of strokes attributable to AF increased significantly. In FHS, AF accounted for ≈1.5% of strokes in individuals 50 to 59 years of age and ≈23.5% in those 80 to 89 years of age.106
Paroxysmal, persistent, and permanent AF all appeared to increase the risk of ischemic stroke to a similar degree.99
AF was also an independent risk factor for ischemic stroke severity, recurrence, and mortality.74 In one study, people who had AF and were not treated with anticoagulants had a 2.1-fold increase in risk for recurrent stroke and a 2.4- fold increase in risk for recurrent severe stroke.107
Studies have demonstrated an underutilization of warfarin therapy. In a recent meta-analysis, men and individuals with prior stroke were more likely to receive warfarin, whereas factors associated with lower use included alcohol and drug abuse, noncompliance, warfarin contraindications, dementia, falls, both gastrointestinal and intracranial hemorrhage, renal impairment, and advancing age.108
-
Cognition
Individuals with AF have an adjusted 2-fold increased risk of dementia.109
A meta-analysis suggested that the risk was consistently high in the 7 studies of patients with recent stroke and a history of AF (OR, 2.4; 95% CI, 1.7–3.5; P<0.001; I2=87%). There was significant heterogeneity in the 7 studies of individuals without a history of stroke (OR, 1.6; 95% CI, 1.0–2.7; P=0.05; I2=87%).110
In individuals with AF in Olmsted County, MN, the cumulative rate of dementia at 1 and 5 years was 2.7% and 10.5%, respectively.100
-
Heart failure
Global Burden
-
The vast majority of research on the epidemiology of AF has been conducted in Europe and North America. The GBD study estimated annual deaths and disability-adjusted life-years globally for hundreds of diseases, including AF.
Standardizing by age, the investigators estimated that between 1990 and 2010, the death rate (per 100 000) increased 89.6%, from 0.9 (0.7–1.1) to 1.7 (1.4–2.1) over all ages.112
The investigators estimated that between 1990 and 2010, the disability-adjusted life-years (summing the YLL and the years lived with disability; in 1000s) increased 94.5%, from 1854 (95% CI, 1377–2429) to 3598 (95% CI, 2756–4578).113
Cost
Investigators examined Medicare and MarketScan databases (2004–2006) to estimate costs attributed to AF in 2008 US dollars:
Annual total direct costs for AF patients were ≈$20 670 versus ≈$11 965 in the control group, for an incremental per-patient cost of $8705.104
Extrapolating to the US population, it is estimated that the incremental cost of AF was ≈$26 billion, of which $6 billion was attributed to AF, $9.9 billion to other cardiovascular expenses, and $10.1 billion to noncardiovascular expenses.104
Tachycardia
ICD-9 427.0, 427.1, 427.2.
Mortality—599. Any-mention mortality—5994. Hospital discharges—78 000.
Monomorphic VT
Prevalence and Incidence
Of 150 consecutive patients with wide-complex tachycardia subsequently studied by invasive electrophysiological study, 122 (81%) had VT; the remainder had SVT.114
Of patients with ventricular arrhythmias presenting for invasive electrophysiological studies, 11% to 21% had no structural HD, and the majority of those with structural HD had CAD.115,116
In 634 patients with implantable cardioverter-defibrillators who had structural HD (including both primary and secondary prevention patients) followed up for a mean 11±3 months, ≈80% of potentially clinically relevant ventricular tachyarrhythmias were attributable to VT amenable to antitachycardia pacing (implying a stable circuit and therefore monomorphic VT).117 Because therapy may have been delivered before spontaneous resolution occurred, the proportion of these VT episodes with definite clinical relevance is not known.
Of those with VT in the absence of structural HD, right ventricular outflow tract VT is the most common form.118
Aftermath
Although the prognosis of those with VT or frequent premature ventricular contractions in the absence of structural HD is good,115,118 a potentially reversible cardiomyopathy may develop in patients with very frequent premature ventricular contractions,119,120 and some cases of sudden death attributable to short-coupled premature ventricular contractions have been described.121,122
Polymorphic VT
Prevalence and Incidence
The true prevalence and incidence of PVT in the US general population are not known.
During ambulatory cardiac monitoring, PVT prevalence ranged from 0.01% to 0.15%123,124; however, among patients who developed sudden cardiac death during ambulatory cardiac monitoring, PVT was detected in 30% to 43%.124–126
A prevalence range of 15% to 19% was reported during electrophysiological study in patients resuscitated from cardiac arrest.126–128
In the setting of AMI, the prevalence of PVT ranged from 1.2% to 2%.129,130
Out-of-hospital PVT is estimated to be present in ≈25% of all cardiac arrest cases involving VT.131,132
Risk Factors
PVT in the setting of a normal QT interval is most frequently seen in the context of acute ischemia or MI.133,134
Less frequently, PVT with a normal QT interval can occur in patients without apparent structural HD. Catecholaminergic PVT, which is discussed under inherited arrhythmic syndromes, is one such disorder.
A prolonged QT interval, whether acquired (drug induced) or congenital, is a common cause of PVT. Drug-induced prolongation of the QT interval that causes PVT is discussed under TdP, whereas congenital prolonged QT interval is discussed under inherited arrhythmic syndromes.
Aftermath
Prevention
Prompt detection and correction of myocardial ischemia would potentially minimize the risk of PVT with normal QT interval in the setting of AMI.
Torsade de Pointes
Prevalence and Incidence
The true incidence and prevalence of drug-induced TdP in the US general population are largely unknown.
By extrapolating data from non-US registries,137 it has been estimated that 12 000 cases of drug-induced TdP occur annually in the United States.129
The prevalence of drug-induced prolongation of QT interval and TdP is 2 to 3 times higher in women than in men.130
With the majority of QT-interval–prolonging drugs, drug-induced TdP may occur in 3% to 15% of patients.126
Antiarrhythmic drugs with QT-interval–prolonging potential carry a 1% to 3% risk of TdP over 1 to 2 years of exposure.138
Risk Factors
TdP is usually related to administration of QT-interval– prolonging drugs.139 An up-to-date list of drugs with the potential to cause TdP may be found at http://www.azcert.org/medical-pros/drug-lists/drug-lists.cfm, a Web site maintained by the University of Arizona Center for Education and Research on Therapeutics.
Specific risk factors for drug-induced TdP include prolonged QT interval, female sex, advanced age, bradycardia, hypokalemia, hypomagnesemia, left ventricular systolic dysfunction, and conditions that lead to elevated plasma concentrations of causative drugs, such as kidney disease, liver disease, drug interactions, or some combination of these.129,140,141
Predisposition was also noted in patients who had a history of ventricular arrhythmia and who experienced a recent symptomatic increase in the frequency and complexity of ectopy.142
Drug-induced TdP rarely occurs in patients without concomitant risk factors. An analysis of 144 published articles describing TdP associated with noncardiac drugs revealed that 100% of the patients had at least 1 risk factor, and 71% had at least 2 risk factors.143
Both common and rare genetic variants have been shown to increase the propensity to drug-induced QT interval prolongation.144,145
Aftermath
Drug-induced TdP may result in morbidity that requires hospitalization and in mortality attributable to sudden cardiac death in ≤31% of patients.129,146
Patients with advanced HF with a history of drug-induced TdP had a significantly higher risk of sudden cardiac death during therapy with amiodarone than amiodarone-treated patients with no history of drug-induced TdP (55% versus 15%).147 Current use of antipsychotic drugs was associated with a significant increase in the risk of sudden cardiac death attributable to TdP (OR, 3.3; 95% CI, 1.8–6.2).148
Hospitalization was required in 47% and death occurred in 8% of patients with QT interval prolongation and TdP caused by administration of methadone.149
Prevention
Keys to reducing the incidence of drug-induced cardiac arrhythmias include increased awareness among the medical, pharmaceutical, and nursing professions of the potential problems associated with the use of certain agents.
Appropriate monitoring when a QT-interval–prolonging drug is administered is essential. Also, prompt withdrawal of the offending agent should be initiated.150
VF and Ventricular Flutter
ICD-9 427.4; ICD-10 I49.0.
Mortality—1090. Any-mention mortality—9076.
Out-of-Hospital Cardiac Arrest: Adults
Out-of-hospital cardiac arrest is defined as a sudden and unexpected pulseless condition attributable to cessation of cardiac mechanical activity.151 There are wide variations in the reported incidence of and outcomes for out-of-hospital cardiac arrest. These differences are caused in part by differences in definition and ascertainment of cardiac arrest data, as well as differences in treatment after the onset of cardiac arrest.
For additional details on out-of-hospital cardiac arrest treatment, please refer to Chapter 22, Quality of Care.
Incidence
(See Table 16-1.)
The incidence of nontraumatic EMS-assessed, EMS-treated cardiac arrest and bystander-witnessed VF among individuals of any age during 2011 in the United States is best characterized by an ongoing registry from the Resuscitation Outcomes Consortium.
The total resident population of the United States is 316 302 564 individuals (www.census.gov, accessed July 23, 2013). Extrapolation of the incidence and case-fatality rate of EMS-assessed out-of-hospital cardiac arrest reported by the Resuscitation Outcomes Consortium (Resuscitation Outcomes Consortium Investigators, unpublished data, July 23, 2013) to the total population of the United States suggests that each year, 424 000 (quasi CI, 417 000–432 000) people experience EMS-assessed out-of-hospital cardiac arrests in the United States.
Approximately 60% of out-of-hospital cardiac arrests are treated by EMS personnel.152
Twenty-five percent of those with EMS-treated out-of-hospital cardiac arrest have no symptoms before the onset of arrest.153
Among EMS-treated out-of-hospital cardiac arrests, 23% have an initial rhythm of VF or VT or are shockable by an automated external defibrillator.154
The incidence of cardiac arrest with an initial rhythm of VF is decreasing over time; however, the incidence of cardiac arrest with any initial rhythm is not decreasing.155
Risk Factors
A study conducted in New York City found the age-adjusted incidence of out-of-hospital cardiac arrest per 10 000 adults was 10.1 among blacks, 6.5 among Hispanics, and 5.8 among whites.156
Prior HD is a major risk factor for cardiac arrest. A study of 1275 health maintenance organization enrollees 50 to 79 years of age who had cardiac arrest showed that the incidence of out-of-hospital cardiac arrest was 6.0 per 1000 person-years in subjects with any clinically recognized HD compared with 0.8 per 1000 person-years in subjects without HD. In subgroups with HD, incidence was 13.6 per 1000 person-years in subjects with prior MI and 21.9 per 1000 person-years in subjects with HF.157
A family history of cardiac arrest in a first-degree relative is associated with an ≈2-fold increase in risk of cardiac arrest.158,159
In a study of 81 722 women in the Nurses’ Health Study, the PAR of sudden death associated with 4 lifestyle factors (smoking, PA, diet, and weight) was 81% (95% CI, 52%–93%).160
Aftermath
Survival to hospital discharge in 2011 after EMS-treated nontraumatic cardiac arrest with any first recorded rhythm was 10.4% (95% CI, 9.7%–11.2%) for patients of any age, 10.7% (95% CI, 9.9%–11.5%) for adults, and 5.4% (2.4%–8.4%) for children (Resuscitation Outcomes Consortium Investigators, unpublished data, July 23, 2013). Survival after bystander-witnessed VF was 31.7% (95% CI, 28.3%–35.2%) for patients of any age, 31.7% (95% CI, 28.2%–35.1%) for adults, and 26.7% (95% CI, 4.3%–49.0%) for children (Resuscitation Outcomes Consortium Investigators, unpublished data, July 23, 2013).
In a study using US Nationwide Inpatient Sample data, inhospital mortality for patients hospitalized for cardiac arrest declined 11.8%, from 69.6% in 2001 to 57.8% in 2009.161
A 9-year retrospective cohort study of 5958 people who received EMS-initiated resuscitation demonstrated that 16.8% (n=1001) were alive at hospital discharge. In people discharged alive, 5-year survival was better in those who received percutaneous intervention (78.7% versus 54.4% for those not treated) and in those who received therapeutic hypothermia (77.5% versus 60.4% in those not treated).162
In a retrospective follow-up study of 2 randomized trials of EMS dispatcher CPR instruction, 5-year survival was higher in people who received chest compressions alone (10.2%) than in those who received chest compressions and rescue breathing (8.5%).163
A study conducted in New York City found the age-adjusted survival to 30 days after discharge was more than twice as poor for blacks as for whites, and survival among Hispanics was also lower than among whites.156
Seventy-nine percent of the lay public are confident that they know what actions to take in a medical emergency; 98% recognize an automated external defibrillator as something that administers an electric shock to restore a normal heartbeat among victims of sudden cardiac arrest; and 60% are familiar with CPR (Harris Interactive survey conducted on behalf of the AHA among 1132 US residents ≥18 years of age, January 8, 2008–January 21, 2008).
A nationwide prospective Danish study observed that family members of individuals who had premature (age <60 years) sudden cardiac death had a significantly elevated 1.72 standardized risk of subsequent CVD compared with the general population.164
Out-of-Hospital Cardiac Arrest: Athletics
Among 10.9 million registered participants in 40 marathons and 19 half marathons, the overall incidence of cardiac arrest was 0.54 per 100 000 participants (95% CI, 0.41–0.70).165 Those with cardiac arrest were more often male and were running a marathon versus a half marathon. Seventy-one percent of those with cardiac arrest died; those who died were younger (mean 39±9 years of age) than those who did not die (mean 49±10 years of age), were more often male, and were more often running a full marathon.
Out-of-Hospital Cardiac Arrest: Children
(See Table 16-1.)
The incidence of out-of-hospital cardiac arrest among individuals <18 years of age in the United States is best characterized by an ongoing registry (Resuscitation Outcomes Consortium Investigators, unpublished data, July 23, 2013).
Most sudden deaths in young athletes were attributable to CVD (56%). Of the cardiovascular deaths that occurred, 29% occurred in blacks, 54% in high school students, and 82% with physical exertion during competition/training; only 11% occurred in females, although this proportion has increased over time.158
A longitudinal study of students 17 to 24 years of age participating in National Collegiate Athletic Association sports showed that the incidence of nontraumatic out-of-hospital cardiac arrest was 1 per 22 903 athlete participant-years. The incidence of cardiac arrest tended to be higher among blacks than among whites and among men than among women.159
In-Hospital Cardiac Arrest
(See Table 16-2.)
Extrapolation of the incidence of in-hospital cardiac arrest reported by GWTG-Resuscitation to the total population of hospitalized patients in the United States suggests that each year, 209 000 (quasi CI, 192 000–211 000) people are treated for in-hospital cardiac arrest.166
According to the GWTG-Resuscitation Investigators (unpublished data, July 27, 2013), 22.7% (95% CI, 22.0%– 23.4%) of adults and 36.8% (95% CI, 32.6%–41.0%) of children (excluding neonates) who experienced in-hospital cardiac arrest with any first recorded rhythm in 2011 survived to discharge.
In 2011, 41.5% (95% CI, 39.3%–43.7%) of adults and 33.3% (95% CI, 15.5%–51.1%) of children (excluding neonates) survived to discharge after in-hospital cardiac arrest with VF or pulseless VT as the first recorded rhythm (GWTG-Resuscitation Investigators, unpublished data, July 27, 2013). For additional details on in-hospital arrest treatment, please refer to Chapter 22, Quality of Care.
Inherited Syndromes Associated With Sudden Cardiac Death
Long-QT Syndrome
The hereditary long-QT syndrome is a genetic channelopathy characterized by prolongation of the QT interval (typically >460 ms) and susceptibility to ventricular tachyarrhythmias that lead to syncope and sudden cardiac death. Investigators have identified mutations in 13 genes leading to this phenotype (LQT1 through LQT13). LQT1 (KCNQ1), LQT2 (KCNH2), and LQT3 (SCN5A) mutations account for the majority (≈80%) of the typed mutations.167,168
Prevalence of long-QT syndrome is estimated at 1 per 2000 live births from ECG-guided molecular screening of ≈44 000 mostly white infants born in Italy.169 A similar prevalence was found among nearly 8000 Japanese school children screened by use of an ECG-guided molecular screening approach.170
Long-QT syndrome has been reported among those of African descent, but its prevalence is not well assessed.171
There is variable penetrance and a sex-time interaction for long-QT syndrome symptoms. Risk of cardiac events is higher among boys than girls (21% among boys and 14% among girls by age 12 years). Risk of events during adolescence is equivalent between sexes (≈25% for both sexes from ages 12–18 years). Conversely, risk of cardiac events in young adulthood is higher among women than men (39% among women from ages 18–40 years and 16% among men).168
In addition to age and sex, the clinical course is influenced by prior syncope or aborted cardiac arrest, family history, QT-interval duration, genotype, number of mutations, and congenital deafness.167,168,172
Risk of cardiac events is decreased during pregnancy but increased during the 9-month postpartum period.173
The mainstay of therapy and prevention is β-blockade treatment.172,174 Implantable defibrillators are considered for high-risk individuals.175
Individuals may be risk-stratified for increased risk of sudden cardiac death176 according to their specific long-QT mutation and their response to β-blockers.174
Short-QT Syndrome
Short-QT syndrome is a recently described inherited mendelian condition characterized by shortening of the QT interval (typically QT <320 ms) and predisposition to AF and ventricular tachyarrhythmias and sudden death. Mutations in 5 ion channel genes have been described (SQT1–SQT5).177
In a population of 41 767 young predominantly male Swiss transcripts, 0.02% of the population had a QT interval shorter than 320 ms.178
Among 53 patients from the European Short QT Syndrome Registry (75% males, median age 26 years), a familial or personal history of cardiac arrest was present in 89%. Twenty-four patients received an implantable cardioverter-defibrillator, and 12 received long-term prophylaxis with hydroquinidine. During a median follow-up of 64 months, 2 patients received an appropriate implantable cardioverter-defibrillator shock, and 1 patient experienced syncope. Nonsustained PVT was recorded in 3 patients.179
The Brugada Syndrome
The Brugada syndrome is an inherited channelopathy characterized by persistent ST-segment elevation in the precordial leads (V1–V3), right bundle-branch block, and susceptibility to ventricular arrhythmias and sudden cardiac death.180
Mutations in several ion channel–related genes have been identified that lead to Brugada syndrome.180
Prevalence is estimated at 1 to 5 per 10 000 individuals. Prevalence is higher in Southeast Asian countries, including Thailand and the Philippines. There is a strong male predominance (80% male).180–185
Cardiac event rates for Brugada syndrome patients followed up prospectively in northern Europe (31.9 months) and Japan (48.7 months) were similar: 8% to 10% in patients with prior aborted sudden death, 1% to 2% in those with history of syncope, and 0.5% in asymptomatic patients.186,187 Predictors of poor outcome included family history of sudden death and early repolarization pattern on ECG.188,189
Catecholaminergic PVT
Catecholaminergic PVT is a familial condition characterized by adrenergically induced ventricular arrhythmias associated with syncope and sudden death. It is associated with frequent ectopy, bidirectional VT, and PVT with exercise or catecholaminergic stimulation (such as emotion, or medicines such as isoproterenol).
Mutations in genes encoding RYR2190,191 are found in the majority, and mutations in genes encoding CASQ2192,193 are found in a small minority.186 However, a substantial proportion of individuals with catecholaminergic PVT do not have an identified mutation.
Statistics regarding catecholaminergic PVT are primarily from case series. Of 101 patients with catecholaminergic PVT, the majority had experienced symptoms before 21 years of age.186
In small series (n=27 to n=101) of patients followed up over a mean of 6.8 to 7.9 years, 27% to 62% experienced cardiac symptoms, and fatal or near-fatal events occurred in 13% to 31%.186,187,190
Risk factors for cardiac events included younger age of diagnosis and absence of β-blocker therapy. A history of aborted cardiac arrest and absence of β-blocker therapy were risk factors for fatal or near-fatal events.186
Arrhythmogenic Right Ventricular Cardiomyopathy
Arrhythmogenic right ventricular cardiomyopathy is a form of genetically inherited structural HD that presents with fibrofatty replacement of the myocardium, with clinical presentation of palpitations, syncope, and sudden death.191
Twelve arrhythmogenic right ventricular cardiomyopathy loci have been described (ARVC1–ARVC12). Disease-causing genes for 8 of these loci have been identified, the majority of which are in desmosomally related proteins.191
Prevalence is estimated at 2 to 10 per 10 000 individuals. 194,195 Of 100 patients reported on from the Johns Hopkins Arrhythmogenic Right Ventricular Dysplasia Registry, 51 were men and 95 were white, with the rest being of black, Hispanic, or Middle Eastern origin. Twenty-two percent of index cases had evidence of the familial form of arrhythmogenic right ventricular cardiomyopathy.192
The most common presenting symptoms were palpitations (27%), syncope (26%), and sudden cardiac death (23%).192
During a median follow-up of 6 years, 47 patients received an implantable cardioverter-defibrillator, 29 of whom received appropriate implantable cardioverter-defibrillator shocks. At the end of follow-up, 66 patients were alive. Twenty-three patients died at study entry, and 11 died during follow-up (91% of deaths were attributable to sudden cardiac arrest).192 Similarly, the annual mortality rate was 2.3% for 130 patients with arrhythmogenic right ventricular cardiomyopathy from Paris, France, who were followed up for a mean of 8.1 years.193
Hypertrophic Cardiomyopathy
(Please refer to Chapter 19, Cardiomyopathy and Heart Failure, for statistics regarding the general epidemiology of HCM.)
Over a mean follow-up of 8±7 years, 6% of HCM patients experienced sudden cardiac death.196
Among 1866 sudden deaths in athletes between 1980 and 2006, HCM was the most common cause of cardiovascular sudden death (in 251 cases, or 36% of the 690 deaths that could be reliably attributed to a cardiovascular cause).158
The risk of sudden death increases with increasing maximum left ventricular wall thickness,197,198 and the risk for those with wall thickness ≥30 mm is 18.2 per 1000 patient-years (95% CI, 7.3–37.6),197 or approximately twice that of those with maximal wall thickness <30 mm.197,198 Of note, an association between maximum wall thickness and sudden death has not been found in every HCM population.194
Nonsustained VT is a risk factor for sudden death,195,199 particularly in younger patients. Nonsustained VT in those ≤30 years of age is associated with a 4.35-greater odds of sudden death (95% CI, 1.5–12.3).195
A history of syncope is also a risk factor for sudden death in these patients,200 particularly if the syncope was recent before the initial evaluation and not attributable to a neurally mediated event.201
The presence of left ventricular outflow tract obstruction ≥30 mm Hg appears to increase the risk of sudden death by ≈2-fold.202,203 The presence of left ventricular outflow tract obstruction has a low positive predictive value (7%–8%) but a high negative predictive value (92%–95%) for predicting sudden death.202,204
The rate of malignant ventricular arrhythmias detected by implantable cardioverter-defibrillators appears to be similar between those with a family history of sudden death in ≥1 first-degree relatives and those with at least 1 of the risk factors described above.205
The risk of sudden death increases with the number of risk factors.206,207
Early Repolarization Syndrome
Early repolarization, observed in ≈4% to 19% of the population208– 211 (more commonly in young men121,208,210 and in athletes209) has conventionally been considered a benign finding.
A clinically relevant syndrome was initially described in which ≥1-mm positive deflections (sometimes referred to as “J waves”) in the S wave of ≥2 consecutive inferior or lateral leads were found in 31% of 206 patients with idiopathic VF compared with 5% of control subjects (P<0.001).208 These findings have been validated in a second study demonstrating similar J-point elevation in 42% of 45 patients with idiopathic VF compared with 13% of age and sex-matched control subjects (P=0.001).209 Given an estimated risk of idiopathic VF in the general population (among those aged 35–45 years) of 3.4 per 100 000, the positive predictive value of such J-wave findings in a person 35 to 45 years of age increases the chances of having idiopathic VF to 11 of 100 000.209
In an analysis of the Social Insurance Institution’s Coronary Disease Study in Finland, J-point elevation was identified in 5.8% of 10 864 people.210 Those with inferior lead J-point elevation more often were male and more often were smokers; had a lower resting heart rate, lower BMI, lower BP, shorter corrected QT interval, and longer QRS duration; and were more likely to have ECG evidence of CAD. Those with lateral J-point elevation were more likely to have left ventricular hypertrophy. Before and after multivariable adjustment, subjects with J-point elevation of ≥1 mm in the inferior leads (n=384) had a higher risk of cardiac death (adjusted RR, 1.28; 95% CI, 1.04–1.59; P=0.03) and arrhythmic death (adjusted RR, 1.43; 95% CI, 1.06–1.94; P=0.03). However, these patients did not have a significantly higher rate of all-cause mortality. Before and after multivariable adjustment, subjects with J-point elevation >2 mm (n=36) had an increased risk of cardiac death (adjusted RR, 2.98; 95% CI, 1.85–4.92; P=0.03), arrhythmic death (adjusted RR, 3.94; 95% CI, 1.96–7.90; P=0.03), and death of any cause (adjusted RR, 1.54; 95% CI, 1.06–2.24; P=0.03).
In CARDIA, 18.6% of 5069 participants had early repolarization restricted to the inferior and lateral leads at baseline; by year 20, only 4.8% exhibited an early repolarization pattern. 211 Younger age, black race, male sex, longer exercise duration and QRS duration, and lower BMI, heart rate, QT index, and Cornell voltage were associated cross-sectionally with the presence of baseline early repolarization. Predictors of maintenance of the ECG pattern from baseline to year 20 were black race (OR, 2.62; 95% CI, 1.61–4.25), BMI (OR, 0.62 per 1 SD; 95% CI, 0.40–0.94), serum triglyceride levels (OR, 0.66 per 1 SD; 95% CI, 0.45–0.98), and QRS duration (OR, 1.68 per 1 SD; 95% CI, 1.37–2.06) at baseline.
Evidence from families with a high penetrance of the early repolarization syndrome associated with a high risk of sudden death suggests that the syndrome can be inherited in an autosomal dominant fashion.212 A meta-analysis of genome-wide association studies performed in population-based cohorts failed to identify any genetic variants that met criteria for statistical significance213 (Table 16-1).
- 1.US Department of Health and Human Services, National Center for Health Statistics. Third National Health and Nutrition Examination Survey (NHANES III), 1988–1994. Hyattsville, MD: Centers for Disease Control and Prevention; 1998. [Accessed July 6, 2011]. Electrocardiography data file documentation. CDROM, Series 11, No. 2A. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/nhanes/nhanes3/2A/NH3ECG-acc.pdf. [Google Scholar]
- 2.Wolbrette DL, Naccarelli GV. Bradycardias: sinus nodal dysfunction and atrioventricular conduction disturbances. In: Topol EJ, editor. Textbook of Cardiovascular Medicine. 3. Baltimore, MD: Lippincott Williams & Wilkins; 2007. pp. 1038–1049. [Google Scholar]
- 3.Kojic EM, Hardarson T, Sigfusson N, Sigvaldason H. The prevalence and prognosis of third-degree atrioventricular conduction block: the Reykjavik study. J Intern Med. 1999;246:81–86. doi: 10.1046/j.1365-2796.1999.00521.x. [DOI] [PubMed] [Google Scholar]
- 4.Quin EM, Wharton JM, Gold MR. Bradyarrhythmias. In: Yan G-X, Kowey PR, editors. Management of Cardiac Arrhythmias. New York, NY: Springer Humana Press; 2010. pp. 305–322. [Google Scholar]
- 5.Johnson RL, Averill KH, Lamb LE. Electrocardiographic findings in 67,375 asymptomatic subjects, VII: atrioventricular block. Am J Cardiol. 1960;6:153–177. doi: 10.1016/0002-9149(60)90044-8. [DOI] [PubMed] [Google Scholar]
- 6.Rose G, Baxter PJ, Reid DD, McCartney P. Prevalence and prognosis of electrocardiographic findings in middle-aged men. Br Heart J. 1978;40:636–643. doi: 10.1136/hrt.40.6.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Movahed MR, Hashemzadeh M, Jamal MM. Increased prevalence of third-degree atrioventricular block in patients with type II diabetes mellitus. Chest. 2005;128:2611–2614. doi: 10.1378/chest.128.4.2611. [DOI] [PubMed] [Google Scholar]
- 8.Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, 3rd, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Faxon DP, Halperin JL, Hiratzka LF, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura RA, Ornato JP, Page RL, Riegel B, Tarkington LG, Yancy CW American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices); American Association for Thoracic Surgery; Society of Thoracic Surgeons. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons [published correction appears in Circulation. 2009;120:e34–e35] Circulation. 2008;117:e350–e408. doi: 10.1161/CIRCUALTIONAHA.108.189742. [DOI] [PubMed] [Google Scholar]
- 9.Grimm W, Koehler U, Fus E, Hoffmann J, Menz V, Funck R, Peter JH, Maisch B. Outcome of patients with sleep apnea-associated severe bradyarrhythmias after continuous positive airway pressure therapy. Am J Cardiol. 2000;86:688–692. A9. doi: 10.1016/s0002-9149(00)01055-9. [DOI] [PubMed] [Google Scholar]
- 10.Glickstein JS, Buyon J, Friedman D. Pulsed Doppler echocardiographic assessment of the fetal PR interval. Am J Cardiol. 2000;86:236–239. doi: 10.1016/s0002-9149(00)00867-5. [DOI] [PubMed] [Google Scholar]
- 11.Schnabel RB, Sullivan LM, Levy D, Pencina MJ, Massaro JM, D’Agostino RB, Sr, Newton-Cheh C, Yamamoto JF, Magnani JW, Tadros TM, Kannel WB, Wang TJ, Ellinor PT, Wolf PA, Vasan RS, Benjamin EJ. Lancet. 2009;373:739–745. doi: 10.1016/S0140-6736(09)60443-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng S, Keyes MJ, Larson MG, McCabe EL, Newton-Cheh C, Levy D, Benjamin EJ, Vasan RS, Wang TJ. Long-term outcomes in individuals with prolonged PR interval or first-degree atrioventricular block. JAMA. 2009;301:2571–2577. doi: 10.1001/jama.2009.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mymin D, Mathewson FA, Tate RB, Manfreda J. The natural history of primary first-degree atrioventricular heart block. N Engl J Med. 1986;315:1183–1187. doi: 10.1056/NEJM198611063151902. [DOI] [PubMed] [Google Scholar]
- 14.Barold SS. Indications for permanent cardiac pacing in first-degree AV block: class I, II, or III? Pacing Clin Electrophysiol. 1996;19:747–751. doi: 10.1111/j.1540-8159.1996.tb03355.x. [DOI] [PubMed] [Google Scholar]
- 15.Goldberger JJ, Johnson NP, Gidea C. Significance of asymptomatic bradycardia for subsequent pacemaker implantation and mortality in patients >60 years of age. Am J Cardiol. 2011;108:857–861. doi: 10.1016/j.amjcard.2011.04.035. [DOI] [PubMed] [Google Scholar]
- 16.Brignole M, Menozzi C, Lolli G, Oddone D, Gianfranchi L, Bertulla A. Pacing for carotid sinus syndrome and sick sinus syndrome. Pacing Clin Electrophysiol. 1990;13(pt 2):2071–2075. doi: 10.1111/j.1540-8159.1990.tb06944.x. [DOI] [PubMed] [Google Scholar]
- 17.Adán V, Crown LA. Diagnosis and treatment of sick sinus syndrome. Am Fam Physician. 2003;67:1725–1732. [PubMed] [Google Scholar]
- 17a.Rodriguez RD, Schocken DD. Update on sick sinus syndrome, a cardiac disorder of aging. Geriatrics. 1990;45:26–30. 33. [PubMed] [Google Scholar]
- 18.Sutton R, Kenny RA. The natural history of sick sinus syndrome. Pacing Clin Electrophysiol. 1986;9(pt 2):1110–1114. doi: 10.1111/j.1540-8159.1986.tb06678.x. [DOI] [PubMed] [Google Scholar]
- 19.Brignole M. Sick sinus syndrome. Clin Geriatr Med. 2002;18:211–227. doi: 10.1016/s0749-0690(02)00006-x. [DOI] [PubMed] [Google Scholar]
- 20.Issa Z, Miller J, Zipes D. Clinical Arrhythmology and Electrophysiology: A Companion to Braunwald’s Heart Disease. Philadelphia, PA: Saunders Elsevier; 2008. [Google Scholar]
- 21.Dobrzynski H, Boyett MR, Anderson RH. New insights into pacemaker activity: promoting understanding of sick sinus syndrome. Circulation. 2007;115:1921–1932. doi: 10.1161/CIRCULATIONAHA.106.616011. [DOI] [PubMed] [Google Scholar]
- 22.Rosenqvist M, Obel IW. Atrial pacing and the risk for AV block: is there a time for change in attitude? Pacing Clin Electrophysiol. 1989;12(pt 1):97–101. doi: 10.1111/pace.1989.12.p1.97. [DOI] [PubMed] [Google Scholar]
- 23.Kistler PM, Sanders P, Fynn SP, Stevenson IH, Spence SJ, Vohra JK, Sparks PB, Kalman JM. Electrophysiologic and electroanatomic changes in the human atrium associated with age. J Am Coll Cardiol. 2004;44:109–116. doi: 10.1016/j.jacc.2004.03.044. [DOI] [PubMed] [Google Scholar]
- 24.Sanders P, Kistler PM, Morton JB, Spence SJ, Kalman JM. Remodeling of sinus node function in patients with congestive heart failure: reduction in sinus node reserve. Circulation. 2004;110:897–903. doi: 10.1161/01.CIR.0000139336.69955.AB. [DOI] [PubMed] [Google Scholar]
- 25.Menozzi C, Brignole M, Alboni P, Boni L, Paparella N, Gaggioli G, Lolli G. The natural course of untreated sick sinus syndrome and identification of the variables predictive of unfavorable outcome. Am J Cardiol. 1998;82:1205–1209. doi: 10.1016/s0002-9149(98)00605-5. [DOI] [PubMed] [Google Scholar]
- 26.Simon AB, Janz N. Symptomatic bradyarrhythmias in the adult: natural history following ventricular pacemaker implantation. Pacing Clin Electrophysiol. 1982;5:372–383. doi: 10.1111/j.1540-8159.1982.tb02245.x. [DOI] [PubMed] [Google Scholar]
- 27.Alt E, Völker R, Wirtzfeld A, Ulm K. Survival and follow-up after pacemaker implantation: a comparison of patients with sick sinus syndrome, complete heart block, and atrial fibrillation. Pacing Clin Electrophysiol. 1985;8:849–855. doi: 10.1111/j.1540-8159.1985.tb05904.x. [DOI] [PubMed] [Google Scholar]
- 28.Lamas GA, Lee KL, Sweeney MO, Silverman R, Leon A, Yee R, Marinchak RA, Flaker G, Schron E, Orav EJ, Hellkamp AS, Greer S, McAnulty J, Ellenbogen K, Ehlert F, Freedman RA, Estes NA, 3rd, Greenspon A, Goldman L Mode Selection Trial in Sinus-Node Dysfunction. Ventricular pacing or dual-chamber pacing for sinus-node dysfunction. N Engl J Med. 2002;346:1854–1862. doi: 10.1056/NEJMoa013040. [DOI] [PubMed] [Google Scholar]
- 29.McComb JM, Gribbin GM. Effect of pacing mode on morbidity and mortality: update of clinical pacing trials. Am J Cardiol. 1999;83(5B):211D–213D. doi: 10.1016/s0002-9149(98)01030-3. [DOI] [PubMed] [Google Scholar]
- 30.Lamas GA, Lee K, Sweeney M, Leon A, Yee R, Ellenbogen K, Greer S, Wilber D, Silverman R, Marinchak R, Bernstein R, Mittleman RS, Lieberman EH, Sullivan C, Zorn L, Flaker G, Schron E, Orav EJ, Goldman L. The Mode Selection Trial (MOST) in sinus node dysfunction: design, rationale, and baseline characteristics of the first 1000 patients. Am Heart J. 2000;140:541–551. doi: 10.1067/mhj.2000.109652. [DOI] [PubMed] [Google Scholar]
- 31.Birnie D, Williams K, Guo A, Mielniczuk L, Davis D, Lemery R, Green M, Gollob M, Tang A. Reasons for escalating pacemaker implants. Am J Cardiol. 2006;98:93–97. doi: 10.1016/j.amjcard.2006.01.069. [DOI] [PubMed] [Google Scholar]
- 32.Orejarena LA, Vidaillet H, Jr, DeStefano F, Nordstrom DL, Vierkant RA, Smith PN, Hayes JJ. Paroxysmal supraventricular tachycardia in the general population. J Am Coll Cardiol. 1998;31:150–157. doi: 10.1016/s0735-1097(97)00422-1. [DOI] [PubMed] [Google Scholar]
- 33.Murman DH, McDonald AJ, Pelletier AJ, Camargo CA., Jr U.S. emergency department visits for supraventricular tachycardia, 1993–2003. Acad Emerg Med. 2007;14:578–581. doi: 10.1197/j.aem.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 34.Still AM, Raatikainen P, Ylitalo A, Kauma H, Ikäheimo M, Antero Kesäniemi Y, Huikuri HV. Prevalence, characteristics and natural course of inappropriate sinus tachycardia. Europace. 2005;7:104–112. doi: 10.1016/j.eupc.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 35.Maurer MS, Shefrin EA, Fleg JL. Prevalence and prognostic significance of exercise-induced supraventricular tachycardia in apparently healthy volunteers. Am J Cardiol. 1995;75:788–792. doi: 10.1016/s0002-9149(99)80412-3. [DOI] [PubMed] [Google Scholar]
- 36.Poutiainen AM, Koistinen MJ, Airaksinen KE, Hartikainen EK, Kettunen RV, Karjalainen JE, Huikuri HV. Prevalence and natural course of ectopic atrial tachycardia. Eur Heart J. 1999;20:694–700. doi: 10.1053/euhj.1998.1313. [DOI] [PubMed] [Google Scholar]
- 37.Blomström-Lundqvist C, Scheinman MM, Aliot EM, Alpert JS, Calkins H, Camm AJ, Campbell WB, Haines DE, Kuck KH, Lerman BB, Miller DD, Shaeffer CW, Jr, Stevenson WG, Tomaselli GF, Antman EM, Smith SC, Jr, Alpert JS, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Hiratzka LF, Hunt SA, Jacobs AK, Russell RO, Jr, Priori SG, Blanc JJ, Budaj A, Burgos EF, Cowie M, Deckers JW, Garcia MA, Klein WW, Lekakis J, Lindahl B, Mazzotta G, Morais JC, Oto A, Smiseth O, Trappe HJ American College of Cardiology; American Heart Association Task Force on Practice Guidelines; European Society of Cardiology Committee for Practice Guidelines; Writing Committee to Develop Guidelines for the Management of Patients With Supraventricular Arrhythmias. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Supraventricular Arrhythmias) Circulation. 2003;108:1871–1909. doi: 10.1161/01.CIR.0000091380.04100.84. [DOI] [PubMed] [Google Scholar]
- 38.Wu EB, Chia HM, Gill JS. Reversible cardiomyopathy after radiofrequency ablation of lateral free-wall pathway-mediated incessant supraventricular tachycardia. Pacing Clin Electrophysiol. 2000;23:1308–1310. doi: 10.1111/j.1540-8159.2000.tb00951.x. [DOI] [PubMed] [Google Scholar]
- 39.Wang YS, Scheinman MM, Chien WW, Cohen TJ, Lesh MD, Griffin JC. Patients with supraventricular tachycardia presenting with aborted sudden death: incidence, mechanism and long-term follow-up. J Am Coll Cardiol. 1991;18:1711–1719. doi: 10.1016/0735-1097(91)90508-7. [DOI] [PubMed] [Google Scholar]
- 40.Brembilla-Perrot B, Houriez P, Beurrier D, Claudon O, Burger G, Vançon AC, Mock L. Influence of age on the electrophysiological mechanism of paroxysmal supraventricular tachycardias. Int J Cardiol. 2001;78:293–298. doi: 10.1016/s0167-5273(01)00392-8. [DOI] [PubMed] [Google Scholar]
- 41.Porter MJ, Morton JB, Denman R, Lin AC, Tierney S, Santucci PA, Cai JJ, Madsen N, Wilber DJ. Influence of age and gender on the mechanism of supraventricular tachycardia. Heart Rhythm. 2004;1:393–396. doi: 10.1016/j.hrthm.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 42.Bradley DJ, Fischbach PS, Law IH, Serwer GA, Dick M., 2nd The clinical course of multifocal atrial tachycardia in infants and children. J Am Coll Cardiol. 2001;38:401–408. doi: 10.1016/s0735-1097(01)01390-0. [DOI] [PubMed] [Google Scholar]
- 43.Kastor JA. Multifocal atrial tachycardia. N Engl J Med. 1990;322:1713–1717. doi: 10.1056/NEJM199006143222405. [DOI] [PubMed] [Google Scholar]
- 44.Anand RG, Rosenthal GL, Van Hare GF, Snyder CS. Is the mechanism of supraventricular tachycardia in pediatrics influenced by age, gender or ethnicity? Congenit Heart Dis. 2009;4:464–468. doi: 10.1111/j.1747-0803.2009.00336.x. [DOI] [PubMed] [Google Scholar]
- 45.De Bacquer D, De Backer G, Kornitzer M. Prevalences of ECG findings in large population based samples of men and women. Heart. 2000;84:625–633. doi: 10.1136/heart.84.6.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sano S, Komori S, Amano T, Kohno I, Ishihara T, Sawanobori T, Ijiri H, Tamura K. Prevalence of ventricular preexcitation in Japanese schoolchildren. Heart. 1998;79:374–378. doi: 10.1136/hrt.79.4.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McCord J, Borzak S. Multifocal atrial tachycardia. Chest. 1998;113:203–209. doi: 10.1378/chest.113.1.203. [DOI] [PubMed] [Google Scholar]
- 48.Munger TM, Packer DL, Hammill SC, Feldman BJ, Bailey KR, Ballard DJ, Holmes DR, Jr, Gersh BJ. A population study of the natural history of Wolff-Parkinson-White syndrome in Olmsted County, Minnesota, 1953- 1989. Circulation. 1993;87:866–873. doi: 10.1161/01.cir.87.3.866. [DOI] [PubMed] [Google Scholar]
- 49.Leitch JW, Klein GJ, Yee R, Murdock C. Prognostic value of electrophysiology testing in asymptomatic patients with Wolff-Parkinson-White pattern [published correction appears in Circulation. 1991;83:1124] Circulation. 1990;82:1718–1723. doi: 10.1161/01.cir.82.5.1718. [DOI] [PubMed] [Google Scholar]
- 50.Dagres N, Clague JR, Lottkamp H, Hindricks G, Breithardt G, Borggrefe M. Impact of radiofrequency catheter ablation of accessory pathways on the frequency of atrial fibrillation during long-term follow-up: high recurrence rate of atrial fibrillation in patients older than 50 years of age. Eur Heart J. 2001;22:423–427. doi: 10.1053/euhj.2000.2429. [DOI] [PubMed] [Google Scholar]
- 51.Goudevenos JA, Katsouras CS, Graekas G, Argiri O, Giogiakas V, Sideris DA. Ventricular pre-excitation in the general population: a study on the mode of presentation and clinical course. Heart. 2000;83:29–34. doi: 10.1136/heart.83.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Krahn AD, Manfreda J, Tate RB, Mathewson FA, Cuddy TE. The natural history of electrocardiographic preexcitation in men: the Manitoba Follow- up Study. Ann Intern Med. 1992;116:456–460. doi: 10.7326/0003-4819-116-6-456. [DOI] [PubMed] [Google Scholar]
- 53.Glotzer TV, Hellkamp AS, Zimmerman J, Sweeney MO, Yee R, Marinchak R, Cook J, Paraschos A, Love J, Radoslovich G, Lee KL, Lamas GA MOST Investigators. Atrial high rate episodes detected by pacemaker diagnostics predict death and stroke: report of the Atrial Diagnostics Ancillary Study of the MOde Selection Trial (MOST) Circulation. 2003;107:1614–1619. doi: 10.1161/01.CIR.0000057981.70380.45. [DOI] [PubMed] [Google Scholar]
- 54.Obeyesekere MN, Leong-Sit P, Massel D, Manlucu J, Modi S, Krahn AD, Skanes AC, Yee R, Gula LJ, Klein GJ. Risk of arrhythmia and sudden death in patients with asymptomatic preexcitation: a meta-analysis. Circulation. 2012;125:2308–2315. doi: 10.1161/CIRCULATIONAHA.111.055350. [DOI] [PubMed] [Google Scholar]
- 55.Timmermans C, Smeets JL, Rodriguez LM, Vrouchos G, van den Dool A, Wellens HJ. Aborted sudden death in the Wolff-Parkinson-White syndrome. Am J Cardiol. 1995;76:492–494. doi: 10.1016/s0002-9149(99)80136-2. [DOI] [PubMed] [Google Scholar]
- 56.Pappone C, Vicedomini G, Manguso F, Baldi M, Pappone A, Petretta A, Vitale R, Saviano M, Ciaccio C, Giannelli L, Calovic Z, Tavazzi L, Santinelli V. Risk of malignant arrhythmias in initially symptomatic patients with Wolff-Parkinson-White syndrome: results of a prospective long-term electrophysiological follow-up study. Circulation. 2012;125:661–668. doi: 10.1161/CIRCULATIONAHA.111.065722. [DOI] [PubMed] [Google Scholar]
- 57.Inoue K, Igarashi H, Fukushige J, Ohno T, Joh K, Hara T. Long-term prospective study on the natural history of Wolff-Parkinson-White syndrome detected during a heart screening program at school. Acta Paediatr. 2000;89:542–545. doi: 10.1080/080352500750027817. [DOI] [PubMed] [Google Scholar]
- 58.Pappone C, Manguso F, Santinelli R, Vicedomini G, Sala S, Paglino G, Mazzone P, Lang CC, Gulletta S, Augello G, Santinelli O, Santinelli V. Radiofrequency ablation in children with asymptomatic Wolff-Parkinson- White syndrome. N Engl J Med. 2004;351:1197–1205. doi: 10.1056/NEJMoa040625. [DOI] [PubMed] [Google Scholar]
- 59.Glotzer TV, Daoud EG, Wyse DG, Singer DE, Ezekowitz MD, Hilker C, Miller C, Qi D, Ziegler PD. The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythm Electrophysiol. 2009;2:474–480. doi: 10.1161/CIRCEP.109.849638. [DOI] [PubMed] [Google Scholar]
- 60.Healey JS, Connolly SJ, Gold MR, Israel CW, Van Gelder IC, Capucci A, Lau CP, Fain E, Yang S, Bailleul C, Morillo CA, Carlson M, Themeles E, Kaufman ES, Hohnloser SH ASSERT Investigators. Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. 2012;366:120–129. doi: 10.1056/NEJMoa1105575. [DOI] [PubMed] [Google Scholar]
- 61.Engdahl J, Andersson L, Mirskaya M, Rosenqvist M. Stepwise screening of atrial fibrillation in a 75-year-old population: implications for stroke prevention. Circulation. 2013;127:930–937. doi: 10.1161/CIRCULATIONAHA.112.126656. [DOI] [PubMed] [Google Scholar]
- 62.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 63.Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TS. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence [published correction appears in Circulation. 2006;114:e498] Circulation. 2006;114:119–125. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 64.Shen AY, Contreras R, Sobnosky S, Shah AI, Ichiuji AM, Jorgensen MB, Brar SS, Chen W. Racial/ethnic differences in the prevalence of atrial fibrillation among older adults–a cross-sectional study. J Natl Med Assoc. 2010;102:906–913. doi: 10.1016/s0027-9684(15)30709-4. [DOI] [PubMed] [Google Scholar]
- 65.Piccini JP, Hammill BG, Sinner MF, Jensen PN, Hernandez AF, Heckbert SR, Benjamin EJ, Curtis LH. Incidence and prevalence of atrial fibrillation and associated mortality among Medicare beneficiaries, 1993–2007. Circ Cardiovasc Qual Outcomes. 2012;5:85–93. doi: 10.1161/CIRCOUTCOMES.111.962688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, Wolf PA, D’Agostino RB, Murabito JM, Kannel WB, Benjamin EJ. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation. 2003;107:2920–2925. doi: 10.1161/01.CIR.0000072767.89944.6E. [DOI] [PubMed] [Google Scholar]
- 67.Jabre P, Jouven X, Adnet F, Thabut G, Bielinski SJ, Weston SA, Roger VL. Atrial fibrillation and death after myocardial infarction: a community study. Circulation. 2011;123:2094–2100. doi: 10.1161/CIRCULATIONAHA.110.990192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98:946–952. doi: 10.1161/01.cir.98.10.946. [DOI] [PubMed] [Google Scholar]
- 69.Miyasaka Y, Barnes ME, Bailey KR, Cha SS, Gersh BJ, Seward JB, Tsang TS. Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based study. J Am Coll Cardiol. 2007;49:986–992. doi: 10.1016/j.jacc.2006.10.062. [DOI] [PubMed] [Google Scholar]
- 70.Mamas MA, Caldwell JC, Chacko S, Garratt CJ, Fath-Ordoubadi F, Neyses L. A meta-analysis of the prognostic significance of atrial fibrillation in chronic heart failure. Eur J Heart Fail. 2009;11:676–683. doi: 10.1093/eurjhf/hfp085. [DOI] [PubMed] [Google Scholar]
- 71.Jabre P, Roger VL, Murad MH, Chamberlain AM, Prokop L, Adnet F, Jouven X. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review and meta-analysis. Circulation. 2011;123:1587–1593. doi: 10.1161/CIRCULATIONAHA.110.986661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chamberlain AM, Agarwal SK, Folsom AR, Soliman EZ, Chambless LE, Crow R, Ambrose M, Alonso A. A clinical risk score for atrial fibrillation in a biracial prospective cohort (from the Atherosclerosis Risk in Communities [ARIC] study) Am J Cardiol. 2011;107:85–91. doi: 10.1016/j.amjcard.2010.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Alonso A, Krijthe BP, Aspelund T, Stepas KA, Pencina MJ, Moser CB, Sinner MF, Sotoodehnia N, Fontes JD, Janssens AC, Kronmal RA, Magnani JW, Witteman JC, Chamberlain AM, Lubitz SA, Schnabel RB, Agarwal SK, McManus DD, Ellinor PT, Larson MG, Burke GL, Launer LJ, Hofman A, Levy D, Gottdiener JS, Kääb S, Couper D, Harris TB, Soliman EZ, Stricker BH, Gudnason V, Heckbert SR, Benjamin EJ. Simple risk model predicts incidence of atrial fibrillation in a racially and geographically diverse population: the CHARGE-AF consortium. J Am Heart Assoc. 2013;2:e000102. doi: 10.1161/JAHA.112.000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lin HJ, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, D’Agostino RB. Stroke severity in atrial fibrillation: the Framingham Study. Stroke. 1996;27:1760–1764. doi: 10.1161/01.str.27.10.1760. [DOI] [PubMed] [Google Scholar]
- 75.Walkey AJ, Wiener RS, Ghobrial JM, Curtis LH, Benjamin EJ. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. JAMA. 2011;306:2248–2254. doi: 10.1001/jama.2011.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.van Diepen S, Bakal JA, McAlister FA, Ezekowitz JA. Mortality and read-mission of patients with heart failure, atrial fibrillation, or coronary artery disease undergoing noncardiac surgery: an analysis of 38 047 patients. Circulation. 2011;124:289–296. doi: 10.1161/CIRCULATIONAHA.110.011130. [DOI] [PubMed] [Google Scholar]
- 77.Lloyd-Jones DM, Wang TJ, Leip EP, Larson MG, Levy D, Vasan RS, D’Agostino RB, Massaro JM, Beiser A, Wolf PA, Benjamin EJ. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110:1042–1046. doi: 10.1161/01.CIR.0000140263.20897.42. [DOI] [PubMed] [Google Scholar]
- 78.Alonso A, Agarwal SK, Soliman EZ, Ambrose M, Chamberlain AM, Prineas RJ, Folsom AR. Incidence of atrial fibrillation in whites and African- Americans: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2009;158:111–117. doi: 10.1016/j.ahj.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schnabel RB, Aspelund T, Li G, Sullivan LM, Suchy-Dicey A, Harris TB, Pencina MJ, D’Agostino RB, Sr, Levy D, Kannel WB, Wang TJ, Kronmal RA, Wolf PA, Burke GL, Launer LJ, Vasan RS, Psaty BM, Benjamin EJ, Gudnason V, Heckbert SR. Arch Intern Med. 2010;170:1909–1917. doi: 10.1001/archinternmed.2010.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sawin CT, Geller A, Wolf PA, Belanger AJ, Baker E, Bacharach P, Wilson PW, Benjamin EJ, D’Agostino RB. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med. 1994;331:1249–1252. doi: 10.1056/NEJM199411103311901. [DOI] [PubMed] [Google Scholar]
- 81.Cappola AR, Fried LP, Arnold AM, Danese MD, Kuller LH, Burke GL, Tracy RP, Ladenson PW. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA. 2006;295:1033–1041. doi: 10.1001/jama.295.9.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Alonso A, Lopez FL, Matsushita K, Loehr LR, Agarwal SK, Chen LY, Soliman EZ, Astor BC, Coresh J. Chronic kidney disease is associated with the incidence of atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2011;123:2946–2953. doi: 10.1161/CIRCULATIONAHA.111.020982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kodama S, Saito K, Tanaka S, Horikawa C, Saito A, Heianza Y, Anasako Y, Nishigaki Y, Yachi Y, Iida KT, Ohashi Y, Yamada N, Sone H. Alcohol consumption and risk of atrial fibrillation: a meta-analysis. J Am Coll Cardiol. 2011;57:427–436. doi: 10.1016/j.jacc.2010.08.641. [DOI] [PubMed] [Google Scholar]
- 84.Wolff L. Familial auricular fibrillation. N Engl J Med. 1943;229:396–398. [Google Scholar]
- 85.Ellinor PT, Yoerger DM, Ruskin JN, MacRae CA. Familial aggregation in lone atrial fibrillation. Hum Genet. 2005;118:179–184. doi: 10.1007/s00439-005-0034-8. [DOI] [PubMed] [Google Scholar]
- 86.Fox CS, Parise H, D’Agostino RB, Sr, Lloyd-Jones DM, Vasan RS, Wang TJ, Levy D, Wolf PA, Benjamin EJ. Parental atrial fibrillation as a risk factor for atrial fibrillation in offspring. JAMA. 2004;291:2851–2855. doi: 10.1001/jama.291.23.2851. [DOI] [PubMed] [Google Scholar]
- 87.Lubitz SA, Yin X, Fontes JD, Magnani JW, Rienstra M, Pai M, Villalon ML, Vasan RS, Pencina MJ, Levy D, Larson MG, Ellinor PT, Benjamin EJ. Association between familial atrial fibrillation and risk of new-onset atrial fibrillation. JAMA. 2010;304:2263–2269. doi: 10.1001/jama.2010.1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ellinor PT, MacRae CA. Ion channel mutations in AF: signal or noise? Heart Rhythm. 2008;5:436–437. doi: 10.1016/j.hrthm.2008.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gudbjartsson DF, Arnar DO, Helgadottir A, Gretarsdottir S, Holm H, Sigurdsson A, Jonasdottir A, Baker A, Thorleifsson G, Kristjansson K, Palsson A, Blondal T, Sulem P, Backman VM, Hardarson GA, Palsdottir E, Helgason A, Sigurjonsdottir R, Sverrisson JT, Kostulas K, Ng MC, Baum L, So WY, Wong KS, Chan JC, Furie KL, Greenberg SM, Sale M, Kelly P, Mac-Rae CA, Smith EE, Rosand J, Hillert J, Ma RC, Ellinor PT, Thorgeirsson G, Gulcher JR, Kong A, Thorsteinsdottir U, Stefansson K. Variants conferring risk of atrial fibrillation on chromosome 4q25. Nature. 2007;448:353–357. doi: 10.1038/nature06007. [DOI] [PubMed] [Google Scholar]
- 90.Benjamin EJ, Rice KM, Arking DE, Pfeufer A, van Noord C, Smith AV, Schnabel RB, Bis JC, Boerwinkle E, Sinner MF, Dehghan A, Lubitz SA, D’Agostino RB, Sr, Lumley T, Ehret GB, Heeringa J, Aspelund T, Newton-Cheh C, Larson MG, Marciante KD, Soliman EZ, Rivadeneira F, Wang TJ, Eiríksdottir G, Levy D, Psaty BM, Li M, Chamberlain AM, Hofman A, Vasan RS, Harris TB, Rotter JI, Kao WH, Agarwal SK, Stricker BH, Wang K, Launer LJ, Smith NL, Chakravarti A, Uitterlinden AG, Wolf PA, Sotoodehnia N, Köttgen A, van Duijn CM, Meitinger T, Mueller M, Perz S, Steinbeck G, Wichmann HE, Lunetta KL, Heckbert SR, Gudnason V, Alonso A, Kääb S, Ellinor PT, Witteman JC. Variants in ZFHX3 are associated with atrial fibrillation in individuals of European ancestry. Nat Genet. 2009;41:879–881. doi: 10.1038/ng.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ellinor PT, Lunetta KL, Glazer NL, Pfeufer A, Alonso A, Chung MK, Sinner MF, de Bakker PI, Mueller M, Lubitz SA, Fox E, Darbar D, Smith NL, Smith JD, Schnabel RB, Soliman EZ, Rice KM, Van Wagoner DR, Beckmann BM, van Noord C, Wang K, Ehret GB, Rotter JI, Hazen SL, Steinbeck G, Smith AV, Launer LJ, Harris TB, Makino S, Nelis M, Milan DJ, Perz S, Esko T, Köttgen A, Moebus S, Newton-Cheh C, Li M, Möhlenkamp S, Wang TJ, Kao WH, Vasan RS, Nöthen MM, MacRae CA, Stricker BH, Hofman A, Uitterlinden AG, Levy D, Boerwinkle E, Metspalu A, Topol EJ, Chakravarti A, Gudnason V, Psaty BM, Roden DM, Meitinger T, Wichmann HE, Witteman JC, Barnard J, Arking DE, Benjamin EJ, Heckbert SR, Kääb S. Common variants in KCNN3 are associated with lone atrial fibrillation. Nat Genet. 2010;42:240–244. doi: 10.1038/ng.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gudbjartsson DF, Holm H, Gretarsdottir S, Thorleifsson G, Walters GB, Thorgeirsson G, Gulcher J, Mathiesen EB, Njølstad I, Nyrnes A, Wilsgaard T, Hald EM, Hveem K, Stoltenberg C, Kucera G, Stubblefield T, Carter S, Roden D, Ng MC, Baum L, So WY, Wong KS, Chan JC, Gieger C, Wichmann HE, Gschwendtner A, Dichgans M, Kuhlenbäumer G, Berger K, Ringelstein EB, Bevan S, Markus HS, Kostulas K, Hillert J, Sveinbjörnsdóttir S, Valdimarsson EM, Løchen ML, Ma RC, Darbar D, Kong A, Arnar DO, Thorsteinsdottir U, Stefansson K. A sequence variant in ZFHX3 on 16q22 associates with atrial fibrillation and ischemic stroke. Nat Genet. 2009;41:876–878. doi: 10.1038/ng.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ellinor PT, Lunetta KL, Albert CM, Glazer NL, Ritchie MD, Smith AV, Arking DE, Müller-Nurasyid M, Krijthe BP, Lubitz SA, Bis JC, Chung MK, Dörr M, Ozaki K, Roberts JD, Smith JG, Pfeufer A, Sinner MF, Lohman K, Ding J, Smith NL, Smith JD, Rienstra M, Rice KM, Van Wagoner DR, Magnani JW, Wakili R, Clauss S, Rotter JI, Steinbeck G, Launer LJ, Davies RW, Borkovich M, Harris TB, Lin H, Völker U, Völzke H, Milan DJ, Hofman A, Boerwinkle E, Chen LY, Soliman EZ, Voight BF, Li G, Chakravarti A, Kubo M, Tedrow UB, Rose LM, Ridker PM, Conen D, Tsunoda T, Furukawa T, Sotoodehnia N, Xu S, Kamatani N, Levy D, Nakamura Y, Parvez B, Mahida S, Furie KL, Rosand J, Muhammad R, Psaty BM, Meitinger T, Perz S, Wichmann HE, Witteman JC, Kao WH, Kathiresan S, Roden DM, Uitterlinden AG, Rivadeneira F, McKnight B, Sjögren M, Newman AB, Liu Y, Gollob MH, Melander O, Tanaka T, Stricker BH, Felix SB, Alonso A, Darbar D, Barnard J, Chasman DI, Heckbert SR, Benjamin EJ, Gudnason V, Kääb S. Meta-analysis identifies six new susceptibility loci for atrial fibrillation. Nat Genet. 2012;44:670–675. doi: 10.1038/ng.2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Meschia JF, Merrill P, Soliman EZ, Howard VJ, Barrett KM, Zakai NA, Kleindorfer D, Safford M, Howard G. Racial disparities in awareness and treatment of atrial fibrillation: the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Stroke. 2010;41:581–587. doi: 10.1161/STROKEAHA.109.573907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Huxley RR, Lopez FL, Folsom AR, Agarwal SK, Loehr LR, Soliman EZ, Maclehose R, Konety S, Alonso A. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2011;123:1501–1508. doi: 10.1161/CIRCULATIONAHA.110.009035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort: the Framingham Heart Study. JAMA. 1994;271:840–844. [PubMed] [Google Scholar]
- 97.Mozaffarian D, Furberg CD, Psaty BM, Siscovick D. Physical activity and incidence of atrial fibrillation in older adults: the Cardiovascular Health Study. Circulation. 2008;118:800–807. doi: 10.1161/CIRCULATIONAHA.108.785626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Aizer A, Gaziano JM, Cook NR, Manson JE, Buring JE, Albert CM. Relation of vigorous exercise to risk of atrial fibrillation. Am J Cardiol. 2009;103:1572–1577. doi: 10.1016/j.amjcard.2009.01.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hart RG, Pearce LA, Rothbart RM, McAnulty JH, Asinger RW, Halperin JL Stroke Prevention in Atrial Fibrillation Investigators. Stroke with intermittent atrial fibrillation: incidence and predictors during aspirin therapy. J Am Coll Cardiol. 2000;35:183–187. doi: 10.1016/s0735-1097(99)00489-1. [DOI] [PubMed] [Google Scholar]
- 100.Swedberg K, Zannad F, McMurray JJ, Krum H, van Veldhuisen DJ, Shi H, Vincent J, Pitt B EMPHASIS-HF Study Investigators. Eplerenone and atrial fibrillation in mild systolic heart failure: results from the EMPHASIS- HF (Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure) study. J Am Coll Cardiol. 2012;59:1598–1603. doi: 10.1016/j.jacc.2011.11.063. [DOI] [PubMed] [Google Scholar]
- 101.Rahimi K, Emberson J, McGale P, Majoni W, Merhi A, Asselbergs FW, Krane V, Macfarlane PW PROSPER Executive. Effect of statins on atrial fibrillation: collaborative meta-analysis of published and unpublished evidence from randomised controlled trials. BMJ. 2011;342:d1250. doi: 10.1136/bmj.d1250. [DOI] [PubMed] [Google Scholar]
- 102.Benjamin EJ, Chen PS, Bild DE, Mascette AM, Albert CM, Alonso A, Calkins H, Connolly SJ, Curtis AB, Darbar D, Ellinor PT, Go AS, Goldschlager NF, Heckbert SR, Jalife J, Kerr CR, Levy D, Lloyd-Jones DM, Massie BM, Nattel S, Olgin JE, Packer DL, Po SS, Tsang TS, Van Wagoner DR, Waldo AL, Wyse DG. Prevention of atrial fibrillation: report from a National Heart, Lung, and Blood Institute workshop. Circulation. 2009;119:606–618. doi: 10.1161/CIRCULATIONAHA.108.825380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Khairallah F, Ezzedine R, Ganz LI, London B, Saba S. Epidemiology and determinants of outcome of admissions for atrial fibrillation in the United States from 1996 to 2001. Am J Cardiol. 2004;94:500–504. doi: 10.1016/j.amjcard.2004.04.068. [DOI] [PubMed] [Google Scholar]
- 104.Kim MH, Johnston SS, Chu BC, Dalal MR, Schulman KL. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4:313–320. doi: 10.1161/CIRCOUTCOMES.110.958165. [DOI] [PubMed] [Google Scholar]
- 105.Lakshminarayan K, Solid CA, Collins AJ, Anderson DC, Herzog CA. Atrial fibrillation and stroke in the general Medicare population: a 10- year perspective (1992 to 2002) Stroke. 2006;37:1969–1974. doi: 10.1161/01.STR.0000230607.07928.17. [DOI] [PubMed] [Google Scholar]
- 106.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–988. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 107.Penado S, Cano M, Acha O, Hernández JL, Riancho JA. Atrial fibrillation as a risk factor for stroke recurrence. Am J Med. 2003;114:206–210. doi: 10.1016/s0002-9343(02)01479-1. [DOI] [PubMed] [Google Scholar]
- 108.Baczek VL, Chen WT, Kluger J, Coleman CI. Predictors of warfarin use in atrial fibrillation in the United States: a systematic review and meta-analysis. BMC Fam Pract. 2012;13:5. doi: 10.1186/1471-2296-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ott A, Breteler MM, de Bruyne MC, van Harskamp F, Grobbee DE, Hofman A. Atrial fibrillation and dementia in a population-based study: the Rotterdam Study. Stroke. 1997;28:316–321. doi: 10.1161/01.str.28.2.316. [DOI] [PubMed] [Google Scholar]
- 110.Kwok CS, Loke YK, Hale R, Potter JF, Myint PK. Atrial fibrillation and incidence of dementia: a systematic review and meta-analysis. Neurology. 2011;76:914–922. doi: 10.1212/WNL.0b013e31820f2e38. [DOI] [PubMed] [Google Scholar]
- 111.Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna W, Seward JB, Iwasaka T, Tsang TS. Incidence and mortality risk of congestive heart failure in atrial fibrillation patients: a community-based study over two decades. Eur Heart J. 2006;27:936–941. doi: 10.1093/eurheartj/ehi694. [DOI] [PubMed] [Google Scholar]
- 112.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O’Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA, 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010 [published correction appears in Lancet. 2013;381:628] Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fèvre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gonzalez-Medina D, Gosselin R, Grainger R, Grant B, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Laden F, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Levinson D, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mock C, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O’Donnell M, O’Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA, 3rd, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leòn FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiebe N, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AK, Zheng ZJ, Zonies D, Lopez AD, AlMazroa MA, Memish ZA. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010 [published correction appears in Lancet. 2013;381:628] Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 114.Akhtar M, Shenasa M, Jazayeri M, Caceres J, Tchou PJ. Wide QRS complex tachycardia: reappraisal of a common clinical problem. Ann Intern Med. 1988;109:905–912. doi: 10.7326/0003-4819-109-11-905. [DOI] [PubMed] [Google Scholar]
- 115.Sacher F, Tedrow UB, Field ME, Raymond JM, Koplan BA, Epstein LM, Stevenson WG. Ventricular tachycardia ablation: evolution of patients and procedures over 8 years. Circ Arrhythm Electrophysiol. 2008;1:153–161. doi: 10.1161/CIRCEP.108.769471. [DOI] [PubMed] [Google Scholar]
- 116.Swerdlow CD, Winkle RA, Mason JW. Determinants of survival in patients with ventricular tachyarrhythmias. N Engl J Med. 1983;308:1436–1442. doi: 10.1056/NEJM198306163082402. [DOI] [PubMed] [Google Scholar]
- 117.Wathen MS, DeGroot PJ, Sweeney MO, Stark AJ, Otterness MF, Adkisson WO, Canby RC, Khalighi K, Machado C, Rubenstein DS, Volosin KJ PainFREE Rx II Investigators. Prospective randomized multicenter trial of empirical antitachycardia pacing versus shocks for spontaneous rapid ventricular tachycardia in patients with implantable cardioverter-defibrillators: Pacing Fast Ventricular Tachycardia Reduces Shock Therapies (PainFREE Rx II) trial results. Circulation. 2004;110:2591–2596. doi: 10.1161/01.CIR.0000145610.64014.E4. [DOI] [PubMed] [Google Scholar]
- 118.Lemery R, Brugada P, Bella PD, Dugernier T, van den Dool A, Wellens HJ. Nonischemic ventricular tachycardia: clinical course and long-term follow-up in patients without clinically overt heart disease. Circulation. 1989;79:990–999. doi: 10.1161/01.cir.79.5.990. [DOI] [PubMed] [Google Scholar]
- 119.Yarlagadda RK, Iwai S, Stein KM, Markowitz SM, Shah BK, Cheung JW, Tan V, Lerman BB, Mittal S. Reversal of cardiomyopathy in patients with repetitive monomorphic ventricular ectopy originating from the right ventricular outflow tract. Circulation. 2005;112:1092–1097. doi: 10.1161/CIRCULATIONAHA.105.546432. [DOI] [PubMed] [Google Scholar]
- 120.Baman TS, Lange DC, Ilg KJ, Gupta SK, Liu TY, Alguire C, Armstrong W, Good E, Chugh A, Jongnarangsin K, Pelosi F, Jr, Crawford T, Ebinger M, Oral H, Morady F, Bogun F. Relationship between burden of premature ventricular complexes and left ventricular function. Heart Rhythm. 2010;7:865–869. doi: 10.1016/j.hrthm.2010.03.036. [DOI] [PubMed] [Google Scholar]
- 121.Viskin S, Rosso R, Rogowski O, Belhassen B. The “short-coupled” variant of right ventricular outflow ventricular tachycardia: a not-so-benign form of benign ventricular tachycardia? J Cardiovasc Electrophysiol. 2005;16:912–916. doi: 10.1111/j.1540-8167.2005.50040.x. [DOI] [PubMed] [Google Scholar]
- 122.Noda T, Shimizu W, Taguchi A, Aiba T, Satomi K, Suyama K, Kurita T, Aihara N, Kamakura S. Malignant entity of idiopathic ventricular fibrillation and polymorphic ventricular tachycardia initiated by premature extrasystoles originating from the right ventricular outflow tract. J Am Coll Cardiol. 2005;46:1288–1294. doi: 10.1016/j.jacc.2005.05.077. [DOI] [PubMed] [Google Scholar]
- 123.Denes P, Gabster A, Huang SK. Clinical, electrocardiographic and follow-up observations in patients having ventricular fibrillation during Holter monitoring. Role of quinidine therapy. Am J Cardiol. 1981;48:9–16. doi: 10.1016/0002-9149(81)90566-x. [DOI] [PubMed] [Google Scholar]
- 124.Panidis IP, Morganroth J. Sudden death in hospitalized patients: cardiac rhythm disturbances detected by ambulatory electrocardiographic monitoring. J Am Coll Cardiol. 1983;2:798–805. doi: 10.1016/s0735-1097(83)80225-3. [DOI] [PubMed] [Google Scholar]
- 125.Kempf FC, Jr, Josephson ME. Cardiac arrest recorded on ambulatory electrocardiograms. Am J Cardiol. 1984;53:1577–1582. doi: 10.1016/0002-9149(84)90582-4. [DOI] [PubMed] [Google Scholar]
- 126.DiMarco JP, Haines DE. Sudden cardiac death. Curr Probl Cardiol. 1990;15:183–232. doi: 10.1016/0146-2806(90)90021-h. [DOI] [PubMed] [Google Scholar]
- 127.Roy D, Waxman HL, Kienzle MG, Buxton AE, Marchlinski FE, Josephson ME. Clinical characteristics and long-term follow-up in 119 survivors of cardiac arrest: relation to inducibility at electrophysiologic testing. Am J Cardiol. 1983;52:969–974. doi: 10.1016/0002-9149(83)90514-3. [DOI] [PubMed] [Google Scholar]
- 128.Stevenson WG, Brugada P, Waldecker B, Zehender M, Wellens HJ. Clinical, angiographic, and electrophysiologic findings in patients with aborted sudden death as compared with patients with sustained ventricular tachycardia after myocardial infarction. Circulation. 1985;71:1146–1152. doi: 10.1161/01.cir.71.6.1146. [DOI] [PubMed] [Google Scholar]
- 129.Tisdale JE, Miler DA. Drug-Induced Diseases: Prevention, Detection and Management. 2. Bethesda, MD: American Society of Health System Pharmacists; 2010. [Google Scholar]
- 130.Lehmann MH, Timothy KW, Frankovich D, Fromm BS, Keating M, Locati EH, Taggart RT, Towbin JA, Moss AJ, Schwartz PJ, Vincent GM. Age-gender influence on the rate-corrected QT interval and the QT-heart rate relation in families with genotypically characterized long QT syndrome. J Am Coll Cardiol. 1997;29:93–99. doi: 10.1016/s0735-1097(96)00454-8. [DOI] [PubMed] [Google Scholar]
- 131.White RD, Wood DL. Out-of-hospital pleomorphic ventricular tachycardia and resuscitation: association with acute myocardial ischemia and infarction. Ann Emerg Med. 1992;21:1282–1287. doi: 10.1016/s0196-0644(05)81767-6. [DOI] [PubMed] [Google Scholar]
- 132.Brady W, Meldon S, DeBehnke D. Comparison of prehospital monomorphic and polymorphic ventricular tachycardia: prevalence, response to therapy, and outcome. Ann Emerg Med. 1995;25:64–70. doi: 10.1016/s0196-0644(95)70357-8. [DOI] [PubMed] [Google Scholar]
- 133.Wolfe CL, Nibley C, Bhandari A, Chatterjee K, Scheinman M. Polymorphous ventricular tachycardia associated with acute myocardial infarction. Circulation. 1991;84:1543–1551. doi: 10.1161/01.cir.84.4.1543. [DOI] [PubMed] [Google Scholar]
- 134.Pellegrini CN, Scheinman MM. Clinical management of ventricular tachycardia. Curr Probl Cardiol. 2010;35:453–504. doi: 10.1016/j.cpcardiol.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 135.Passman R, Kadish A. Polymorphic ventricular tachycardia, long Q-T syndrome, and torsades de pointes. Med Clin North Am. 2001;85:321–341. doi: 10.1016/s0025-7125(05)70318-7. [DOI] [PubMed] [Google Scholar]
- 136.Brady WJ, DeBehnke DJ, Laundrie D. Prevalence, therapeutic response, and outcome of ventricular tachycardia in the out-of-hospital setting: a comparison of monomorphic ventricular tachycardia, polymorphic ventricular tachycardia, and torsades de pointes. Acad Emerg Med. 1999;6:609–617. doi: 10.1111/j.1553-2712.1999.tb00414.x. [DOI] [PubMed] [Google Scholar]
- 137.Darpö B. Spectrum of drugs prolonging QT interval and the incidence of torsades de pointes. Eur Heart J Suppl. 2001;3(suppl K):K70–K80. [Google Scholar]
- 138.Kannankeril P, Roden DM, Darbar D. Drug-induced long QT syndrome. Pharmacol Rev. 2010;62:760–781. doi: 10.1124/pr.110.003723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Camm AJ, Janse MJ, Roden DM, Rosen MR, Cinca J, Cobbe SM. Congenital and acquired long QT syndrome. Eur Heart J. 2000;21:1232–1237. doi: 10.1053/euhj.2000.2222. [DOI] [PubMed] [Google Scholar]
- 140.Gupta A, Lawrence AT, Krishnan K, Kavinsky CJ, Trohman RG. Current concepts in the mechanisms and management of drug-induced QT prolongation and torsade de pointes. Am Heart J. 2007;153:891–899. doi: 10.1016/j.ahj.2007.01.040. [DOI] [PubMed] [Google Scholar]
- 141.Kannankeril PJ, Roden DM. Drug-induced long QT and torsade de pointes: recent advances. Curr Opin Cardiol. 2007;22:39–43. doi: 10.1097/HCO.0b013e32801129eb. [DOI] [PubMed] [Google Scholar]
- 142.Lewis BH, Antman EM, Graboys TB. Detailed analysis of 24 hour ambulatory electrocardiographic recordings during ventricular fibrillation or torsade de pointes. J Am Coll Cardiol. 1983;2:426–436. doi: 10.1016/s0735-1097(83)80268-x. [DOI] [PubMed] [Google Scholar]
- 143.Zeltser D, Justo D, Halkin A, Prokhorov V, Heller K, Viskin S. Torsade de pointes due to noncardiac drugs: most patients have easily identifiable risk factors. Medicine (Baltimore) 2003;82:282–290. doi: 10.1097/01.md.0000085057.63483.9b. [DOI] [PubMed] [Google Scholar]
- 144.Jamshidi Y, Nolte IM, Dalageorgou C, Zheng D, Johnson T, Bastiaenen R, Ruddy S, Talbott D, Norris KJ, Snieder H, George AL, Marshall V, Shakir S, Kannankeril PJ, Munroe PB, Camm AJ, Jeffery S, Roden DM, Behr ER. Common variation in the NOS1AP gene is associated with drug-induced QT prolongation and ventricular arrhythmia. J Am Coll Cardiol. 2012;60:841–850. doi: 10.1016/j.jacc.2012.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ramirez AH, Shaffer CM, Delaney JT, Sexton DP, Levy SE, Rieder MJ, Nickerson DA, George AL, Jr, Roden DM. Novel rare variants in congenital cardiac arrhythmia genes are frequent in drug-induced torsades de pointes. Pharmacogenomics J. 2013;13:325–329. doi: 10.1038/tpj.2012.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Faber TS, Zehender M, Just H. Drug-induced torsade de pointes. Incidence, management and prevention. Drug Saf. 1994;11:463–476. doi: 10.2165/00002018-199411060-00007. [DOI] [PubMed] [Google Scholar]
- 147.Middlekauff HR, Stevenson WG, Saxon LA, Stevenson LW. Amiodarone and torsades de pointes in patients with advanced heart failure. Am J Cardiol. 1995;76:499–502. doi: 10.1016/s0002-9149(99)80138-6. [DOI] [PubMed] [Google Scholar]
- 148.Straus SM, Bleumink GS, Dieleman JP, van der Lei J, ‘t Jong GW, Kingma JH, Sturkenboom MC, Stricker BH. Antipsychotics and the risk of sudden cardiac death [published correction appears in Arch Intern Med. 2004;164:1839] Arch Intern Med. 2004;164:1293–1297. doi: 10.1001/archinte.164.12.1293. [DOI] [PubMed] [Google Scholar]
- 149.Pearson EC, Woosley RL. QT prolongation and torsades de pointes among methadone users: reports to the FDA spontaneous reporting system. Pharmacoepidemiol Drug Saf. 2005;14:747–753. doi: 10.1002/pds.1112. [DOI] [PubMed] [Google Scholar]
- 150.Doig JC. Drug-induced cardiac arrhythmias: incidence, prevention and management. Drug Saf. 1997;17:265–275. doi: 10.2165/00002018-199717040-00006. [DOI] [PubMed] [Google Scholar]
- 151.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 152.Chugh SS, Jui J, Gunson K, Stecker EC, John BT, Thompson B, Ilias N, Vickers C, Dogra V, Daya M, Kron J, Zheng ZJ, Mensah G, McAnulty J. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44:1268–1275. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 153.Müller D, Agrawal R, Arntz HR. How sudden is sudden cardiac death? Circulation. 2006;114:1146–1150. doi: 10.1161/CIRCULATIONAHA.106.616318. [DOI] [PubMed] [Google Scholar]
- 154.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I Resuscitation Outcomes Consortium Investigators. Regional variation in out-of-hospital cardiac arrest incidence and outcome [published correction appears in JAMA. 2008;300:1763] JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Cobb LA, Fahrenbruch CE, Olsufka M, Copass MK. Changing incidence of out-of-hospital ventricular fibrillation, 1980–2000. JAMA. 2002;288:3008–3013. doi: 10.1001/jama.288.23.3008. [DOI] [PubMed] [Google Scholar]
- 156.Galea S, Blaney S, Nandi A, Silverman R, Vlahov D, Foltin G, Kusick M, Tunik M, Richmond N. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007;166:534–543. doi: 10.1093/aje/kwm102. [DOI] [PubMed] [Google Scholar]
- 157.Rea TD, Pearce RM, Raghunathan TE, Lemaitre RN, Sotoodehnia N, Jouven X, Siscovick DS. Incidence of out-of-hospital cardiac arrest. Am J Cardiol. 2004;93:1455–1460. doi: 10.1016/j.amjcard.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 158.Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119:1085–1092. doi: 10.1161/CIRCULATIONAHA.108.804617. [DOI] [PubMed] [Google Scholar]
- 159.Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of sudden cardiac death in National Collegiate Athletic Association athletes. Circulation. 2011;123:1594–1600. doi: 10.1161/CIRCULATIONAHA.110.004622. [DOI] [PubMed] [Google Scholar]
- 160.Chiuve SE, Fung TT, Rexrode KM, Spiegelman D, Manson JE, Stampfer MJ, Albert CM. Adherence to a low-risk, healthy lifestyle and risk of sudden cardiac death among women. JAMA. 2011;306:62–69. doi: 10.1001/jama.2011.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Fugate JE, Brinjikji W, Mandrekar JN, Cloft HJ, White RD, Wijdicks EF, Rabinstein AA. Post-cardiac arrest mortality is declining: a study of the US National Inpatient Sample 2001 to 2009. Circulation. 2012;126:546–550. doi: 10.1161/CIRCULATIONAHA.111.088807. [DOI] [PubMed] [Google Scholar]
- 162.Dumas F, White L, Stubbs BA, Cariou A, Rea TD. Long-term prognosis following resuscitation from out of hospital cardiac arrest: role of percutaneous coronary intervention and therapeutic hypothermia. J Am Coll Cardiol. 2012;60:21–27. doi: 10.1016/j.jacc.2012.03.036. [DOI] [PubMed] [Google Scholar]
- 163.Dumas F, Rea TD, Fahrenbruch C, Rosenqvist M, Faxén J, Svensson L, Eisenberg MS, Bohm K. Chest compression alone cardiopulmonary resuscitation is associated with better long-term survival compared with standard cardiopulmonary resuscitation. Circulation. 2013;127:435–441. doi: 10.1161/CIRCULATIONAHA.112.124115. [DOI] [PubMed] [Google Scholar]
- 164.Ranthe MF, Carstensen L, Oyen N, Tfelt-Hansen J, Christiansen M, McKenna WJ, Wohlfahrt J, Melbye M, Boyd HA. Family history of premature death and risk of early onset cardiovascular disease. J Am Coll Cardiol. 2012;60:814–821. doi: 10.1016/j.jacc.2012.06.018. [DOI] [PubMed] [Google Scholar]
- 165.Kim JH, Malhotra R, Chiampas G, d’Hemecourt P, Troyanos C, Cianca J, Smith RN, Wang TJ, Roberts WO, Thompson PD, Baggish AL Race Associated Cardiac Arrest Event Registry (RACER) Study Group. Cardiac arrest during long-distance running races. N Engl J Med. 2012;366:130–140. doi: 10.1056/NEJMoa1106468. [DOI] [PubMed] [Google Scholar]
- 166.Merchant RM, Yang L, Becker LB, Berg RA, Nadkarni V, Nichol G, Carr BG, Mitra N, Bradley SM, Abella BS, Groeneveld PW American Heart Association Get With The Guidelines-Resuscitation Investigators. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39:2401–2406. doi: 10.1097/CCM.0b013e3182257459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Wedekind H, Burde D, Zumhagen S, Debus V, Burkhardtsmaier G, Mönnig G, Breithardt G, Schulze-Bahr E. QT interval prolongation and risk for cardiac events in genotyped LQTS-index children. Eur J Pediatr. 2009;168:1107–1115. doi: 10.1007/s00431-008-0896-6. [DOI] [PubMed] [Google Scholar]
- 168.Goldenberg I, Zareba W, Moss AJ. Long QT Syndrome. Curr Probl Cardiol. 2008;33:629–694. doi: 10.1016/j.cpcardiol.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 169.Schwartz PJ, Stramba-Badiale M, Crotti L, Pedrazzini M, Besana A, Bosi G, Gabbarini F, Goulene K, Insolia R, Mannarino S, Mosca F, Nespoli L, Rimini A, Rosati E, Salice P, Spazzolini C. Prevalence of the congenital long-QT syndrome. Circulation. 2009;120:1761–1767. doi: 10.1161/CIRCULATIONAHA.109.863209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Hayashi K, Fujino N, Uchiyama K, Ino H, Sakata K, Konno T, Masuta E, Funada A, Sakamoto Y, Tsubokawa T, Nakashima K, Liu L, Higashida H, Hiramaru Y, Shimizu M, Yamagishi M. Long QT syndrome and associated gene mutation carriers in Japanese children: results from ECG screening examinations. Clin Sci (Lond) 2009;117:415–424. doi: 10.1042/CS20080528. [DOI] [PubMed] [Google Scholar]
- 171.Fugate T, 2nd, Moss AJ, Jons C, McNitt S, Mullally J, Ouellet G, Goldenberg I, Zareba W, Robinson JL U S. portion of International Long QT Syndrome Registry Investigators. Long QT syndrome in African- Americans. Ann Noninvasive Electrocardiol. 2010;15:73–76. doi: 10.1111/j.1542-474X.2009.00342.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Goldenberg I, Bradley J, Moss A, McNitt S, Polonsky S, Robinson JL, Andrews M, Zareba W International LQTS Registry Investigators. Beta-blocker efficacy in high-risk patients with the congenital long-QT syndrome types 1 and 2: implications for patient management. J Cardiovasc Electrophysiol. 2010;21:893–901. doi: 10.1111/j.1540-8167.2010.01737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Seth R, Moss AJ, McNitt S, Zareba W, Andrews ML, Qi M, Robinson JL, Goldenberg I, Ackerman MJ, Benhorin J, Kaufman ES, Locati EH, Napolitano C, Priori SG, Schwartz PJ, Towbin JA, Vincent GM, Zhang L. Long QT syndrome and pregnancy. J Am Coll Cardiol. 2007;49:1092–1098. doi: 10.1016/j.jacc.2006.09.054. [DOI] [PubMed] [Google Scholar]
- 174.Barsheshet A, Goldenberg I, O-Uchi J, Moss AJ, Jons C, Shimizu W, Wilde AA, McNitt S, Peterson DR, Zareba W, Robinson JL, Ackerman MJ, Cypress M, Gray DA, Hofman N, Kanters JK, Kaufman ES, Platonov PG, Qi M, Towbin JA, Vincent GM, Lopes CM. Mutations in cytoplasmic loops of the KCNQ1 channel and the risk of life-threatening events: implications for mutation-specific response to β-blocker therapy in type 1 long-QT syndrome. Circulation. 2012;125:1988–1996. doi: 10.1161/CIRCULATIONAHA.111.048041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Zareba W, Moss AJ, Daubert JP, Hall WJ, Robinson JL, Andrews M. Implantable cardioverter defibrillator in high-risk long QT syndrome patients. J Cardiovasc Electrophysiol. 2003;14:337–341. doi: 10.1046/j.1540-8167.2003.02545.x. [DOI] [PubMed] [Google Scholar]
- 176.Jons C, O-Uchi J, Moss AJ, Reumann M, Rice JJ, Goldenberg I, Zareba W, Wilde AA, Shimizu W, Kanters JK, McNitt S, Hofman N, Robinson JL, Lopes CM. Use of mutant-specific ion channel characteristics for risk stratification of long QT syndrome patients. Sci Transl Med. 2011;3:76ra28. doi: 10.1126/scitranslmed.3001551. [DOI] [PubMed] [Google Scholar]
- 177.Cross B, Homoud M, Link M, Foote C, Garlitski AC, Weinstock J, Estes NA., 3rd The short QT syndrome. J Interv Card Electrophysiol. 2011;31:25–31. doi: 10.1007/s10840-011-9566-0. [DOI] [PubMed] [Google Scholar]
- 178.Kobza R, Roos M, Niggli B, Abächerli R, Lupi GA, Frey F, Schmid JJ, Erne P. Prevalence of long and short QT in a young population of 41,767 predominantly male Swiss conscripts. Heart Rhythm. 2009;6:652–657. doi: 10.1016/j.hrthm.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 179.Giustetto C, Schimpf R, Mazzanti A, Scrocco C, Maury P, Anttonen O, Probst V, Blanc JJ, Sbragia P, Dalmasso P, Borggrefe M, Gaita F. Long-term follow-up of patients with short QT syndrome. J Am Coll Cardiol. 2011;58:587–595. doi: 10.1016/j.jacc.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 180.Benito B, Brugada J, Brugada R, Brugada P. Brugada syndrome [published correction appears in Rev Esp Cardiol. 2010;63:620] Rev Esp Cardiol. 2009;62:1297–1315. doi: 10.1016/s1885-5857(09)73357-2. [DOI] [PubMed] [Google Scholar]
- 181.Miyasaka Y, Tsuji H, Yamada K, Tokunaga S, Saito D, Imuro Y, Matsumoto N, Iwasaka T. Prevalence and mortality of the Brugada-type electrocardiogram in one city in Japan. J Am Coll Cardiol. 2001;38:771–774. doi: 10.1016/s0735-1097(01)01419-x. [DOI] [PubMed] [Google Scholar]
- 182.Baron RC, Thacker SB, Gorelkin L, Vernon AA, Taylor WR, Choi K. Sudden death among Southeast Asian refugees: an unexplained nocturnal phenomenon. JAMA. 1983;250:2947–2951. [PubMed] [Google Scholar]
- 183.Nademanee K, Veerakul G, Nimmannit S, Chaowakul V, Bhuripanyo K, Likittanasombat K, Tunsanga K, Kuasirikul S, Malasit P, Tansupasawadikul S, Tatsanavivat P. Arrhythmogenic marker for the sudden unexplained death syndrome in Thai men. Circulation. 1997;96:2595–2600. doi: 10.1161/01.cir.96.8.2595. [DOI] [PubMed] [Google Scholar]
- 184.Gilbert J, Gold RL, Haffajee CI, Alpert JS. Sudden cardiac death in a southeast Asian immigrant: clinical, electrophysiologic, and biopsy characteristics. Pacing Clin Electrophysiol. 1986;9(pt 1):912–914. doi: 10.1111/j.1540-8159.1986.tb06640.x. [DOI] [PubMed] [Google Scholar]
- 185.Hermida JS, Lemoine JL, Aoun FB, Jarry G, Rey JL, Quiret JC. Prevalence of the Brugada syndrome in an apparently healthy population. Am J Cardiol. 2000;86:91–94. doi: 10.1016/s0002-9149(00)00835-3. [DOI] [PubMed] [Google Scholar]
- 186.Hayashi M, Denjoy I, Extramiana F, Maltret A, Buisson NR, Lupoglazoff JM, Klug D, Hayashi M, Takatsuki S, Villain E, Kamblock J, Messali A, Guicheney P, Lunardi J, Leenhardt A. Incidence and risk factors of arrhythmic events in catecholaminergic polymorphic ventricular tachycardia. Circulation. 2009;119:2426–2434. doi: 10.1161/CIRCULATIONAHA.108.829267. [DOI] [PubMed] [Google Scholar]
- 187.Sumitomo N, Harada K, Nagashima M, Yasuda T, Nakamura Y, Aragaki Y, Saito A, Kurosaki K, Jouo K, Koujiro M, Konishi S, Matsuoka S, Oono T, Hayakawa S, Miura M, Ushinohama H, Shibata T, Niimura I. Catecholaminergic polymorphic ventricular tachycardia: electrocardiographic characteristics and optimal therapeutic strategies to prevent sudden death. Heart. 2003;89:66–70. doi: 10.1136/heart.89.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Probst V, Veltmann C, Eckardt L, Meregalli PG, Gaita F, Tan HL, Babuty D, Sacher F, Giustetto C, Schulze-Bahr E, Borggrefe M, Haissaguerre M, Mabo P, Le Marec H, Wolpert C, Wilde AA. Long-term prognosis of patients diagnosed with Brugada syndrome: results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635–643. doi: 10.1161/CIRCULATIONAHA.109.887026. [DOI] [PubMed] [Google Scholar]
- 189.Kamakura S, Ohe T, Nakazawa K, Aizawa Y, Shimizu A, Horie M, Ogawa S, Okumura K, Tsuchihashi K, Sugi K, Makita N, Hagiwara N, Inoue H, Atarashi H, Aihara N, Shimizu W, Kurita T, Suyama K, Noda T, Satomi K, Okamura H, Tomoike H Brugada Syndrome Investigators in Japan. Long-term prognosis of probands with Brugada-pattern ST-elevation in leads V1-V3. Circ Arrhythm Electrophysiol. 2009;2:495–503. doi: 10.1161/CIRCEP.108.816892. [DOI] [PubMed] [Google Scholar]
- 190.Sy RW, Gollob MH, Klein GJ, Yee R, Skanes AC, Gula LJ, Leong-Sit P, Gow RM, Green MS, Birnie DH, Krahn AD. Arrhythmia characterization and long-term outcomes in catecholaminergic polymorphic ventricular tachycardia. Heart Rhythm. 2011;8:864–871. doi: 10.1016/j.hrthm.2011.01.048. [DOI] [PubMed] [Google Scholar]
- 191.Hamilton RM. Arrhythmogenic right ventricular cardiomyopathy. Pacing Clin Electrophysiol. 2009;32(suppl 2):S44–S51. doi: 10.1111/j.1540-8159.2009.02384.x. [DOI] [PubMed] [Google Scholar]
- 192.Dalal D, Nasir K, Bomma C, Prakasa K, Tandri H, Piccini J, Roguin A, Tichnell C, James C, Russell SD, Judge DP, Abraham T, Spevak PJ, Bluemke DA, Calkins H. Arrhythmogenic right ventricular dysplasia: a United States experience. Circulation. 2005;112:3823–3832. doi: 10.1161/CIRCULATIONAHA.105.542266. [DOI] [PubMed] [Google Scholar]
- 193.Hulot JS, Jouven X, Empana JP, Frank R, Fontaine G. Natural history and risk stratification of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circulation. 2004;110:1879–1884. doi: 10.1161/01.CIR.0000143375.93288.82. [DOI] [PubMed] [Google Scholar]
- 194.Olivotto I, Gistri R, Petrone P, Pedemonte E, Vargiu D, Cecchi F. Maximum left ventricular thickness and risk of sudden death in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2003;41:315–321. doi: 10.1016/s0735-1097(02)02713-4. [DOI] [PubMed] [Google Scholar]
- 195.Monserrat L, Elliott PM, Gimeno JR, Sharma S, Penas-Lado M, McKenna WJ. Non-sustained ventricular tachycardia in hypertrophic cardiomyopathy: an independent marker of sudden death risk in young patients. J Am Coll Cardiol. 2003;42:873–879. doi: 10.1016/s0735-1097(03)00827-1. [DOI] [PubMed] [Google Scholar]
- 196.Maron BJ, Olivotto I, Spirito P, Casey SA, Bellone P, Gohman TE, Graham KJ, Burton DA, Cecchi F. Epidemiology of hypertrophic cardiomyopathy- related death: revisited in a large non-referral-based patient population. Circulation. 2000;102:858–864. doi: 10.1161/01.cir.102.8.858. [DOI] [PubMed] [Google Scholar]
- 197.Spirito P, Bellone P, Harris KM, Bernabo P, Bruzzi P, Maron BJ. Magnitude of left ventricular hypertrophy and risk of sudden death in hypertrophic cardiomyopathy. N Engl J Med. 2000;342:1778–1785. doi: 10.1056/NEJM200006153422403. [DOI] [PubMed] [Google Scholar]
- 198.Elliott PM, Gimeno Blanes JR, Mahon NG, Poloniecki JD, McKenna WJ. Relation between severity of left-ventricular hypertrophy and prognosis in patients with hypertrophic cardiomyopathy. Lancet. 2001;357:420–424. doi: 10.1016/S0140-6736(00)04005-8. [DOI] [PubMed] [Google Scholar]
- 199.Adabag AS, Casey SA, Kuskowski MA, Zenovich AG, Maron BJ. Spectrum and prognostic significance of arrhythmias on ambulatory Holter electrocardiogram in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2005;45:697–704. doi: 10.1016/j.jacc.2004.11.043. [DOI] [PubMed] [Google Scholar]
- 200.Kofflard MJ, Ten Cate FJ, van der Lee C, van Domburg RT. Hypertrophic cardiomyopathy in a large community-based population: clinical outcome and identification of risk factors for sudden cardiac death and clinical deterioration. J Am Coll Cardiol. 2003;41:987–993. doi: 10.1016/s0735-1097(02)03004-8. [DOI] [PubMed] [Google Scholar]
- 201.Spirito P, Autore C, Rapezzi C, Bernabò P, Badagliacca R, Maron MS, Bongioanni S, Coccolo F, Estes NA, Barillà CS, Biagini E, Quarta G, Conte MR, Bruzzi P, Maron BJ. Syncope and risk of sudden death in hypertrophic cardiomyopathy. Circulation. 2009;119:1703–1710. doi: 10.1161/CIRCULATIONAHA.108.798314. [DOI] [PubMed] [Google Scholar]
- 202.Maron MS, Olivotto I, Betocchi S, Casey SA, Lesser JR, Losi MA, Cecchi F, Maron BJ. Effect of left ventricular outflow tract obstruction on clinical outcome in hypertrophic cardiomyopathy. N Engl J Med. 2003;348:295–303. doi: 10.1056/NEJMoa021332. [DOI] [PubMed] [Google Scholar]
- 203.Elliott PM, Gimeno JR, Tomé MT, Shah J, Ward D, Thaman R, Mogensen J, McKenna WJ. Left ventricular outflow tract obstruction and sudden death risk in patients with hypertrophic cardiomyopathy. Eur Heart J. 2006;27:1933–1941. doi: 10.1093/eurheartj/ehl041. [DOI] [PubMed] [Google Scholar]
- 204.Efthimiadis GK, Parcharidou DG, Giannakoulas G, Pagourelias ED, Charalampidis P, Savvopoulos G, Ziakas A, Karvounis H, Styliadis IH, Parcharidis GE. Left ventricular outflow tract obstruction as a risk factor for sudden cardiac death in hypertrophic cardiomyopathy. Am J Cardiol. 2009;104:695–699. doi: 10.1016/j.amjcard.2009.04.039. [DOI] [PubMed] [Google Scholar]
- 205.Bos JM, Maron BJ, Ackerman MJ, Haas TS, Sorajja P, Nishimura RA, Gersh BJ, Ommen SR. Role of family history of sudden death in risk stratification and prevention of sudden death with implantable defibrillators in hypertrophic cardiomyopathy. Am J Cardiol. 2010;106:1481–1486. doi: 10.1016/j.amjcard.2010.06.077. [DOI] [PubMed] [Google Scholar]
- 206.Elliott PM, Poloniecki J, Dickie S, Sharma S, Monserrat L, Varnava A, Mahon NG, McKenna WJ. Sudden death in hypertrophic cardiomyopathy: identification of high risk patients. J Am Coll Cardiol. 2000;36:2212–2218. doi: 10.1016/s0735-1097(00)01003-2. [DOI] [PubMed] [Google Scholar]
- 207.Maron BJ, Spirito P, Shen WK, Haas TS, Formisano F, Link MS, Epstein AE, Almquist AK, Daubert JP, Lawrenz T, Boriani G, Estes NA, 3rd, Favale S, Piccininno M, Winters SL, Santini M, Betocchi S, Arribas F, Sherrid MV, Buja G, Semsarian C, Bruzzi P. Implantable cardioverter-defibrillators and prevention of sudden cardiac death in hypertrophic cardiomyopathy [published correction appears in JAMA. 2007;298:1516] JAMA. 2007;298:405–412. doi: 10.1001/jama.298.4.405. [DOI] [PubMed] [Google Scholar]
- 208.Haïssaguerre M, Derval N, Sacher F, Jesel L, Deisenhofer I, de Roy L, Pasquié JL, Nogami A, Babuty D, Yli-Mayry S, De Chillou C, Scanu P, Mabo P, Matsuo S, Probst V, Le Scouarnec S, Defaye P, Schlaepfer J, Rostock T, Lacroix D, Lamaison D, Lavergne T, Aizawa Y, Englund A, Anselme F, O’Neill M, Hocini M, Lim KT, Knecht S, Veenhuyzen GD, Bordachar P, Chauvin M, Jais P, Coureau G, Chene G, Klein GJ, Clémenty J. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008;358:2016–2023. doi: 10.1056/NEJMoa071968. [DOI] [PubMed] [Google Scholar]
- 209.Rosso R, Kogan E, Belhassen B, Rozovski U, Scheinman MM, Zeltser D, Halkin A, Steinvil A, Heller K, Glikson M, Katz A, Viskin S. J-point elevation in survivors of primary ventricular fibrillation and matched control subjects: incidence and clinical significance. J Am Coll Cardiol. 2008;52:1231–1238. doi: 10.1016/j.jacc.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 210.Tikkanen JT, Anttonen O, Junttila MJ, Aro AL, Kerola T, Rissanen HA, Reunanen A, Huikuri HV. Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med. 2009;361:2529–2537. doi: 10.1056/NEJMoa0907589. [DOI] [PubMed] [Google Scholar]
- 211.Walsh JA, 3rd, Ilkhanoff L, Soliman EZ, Prineas R, Liu K, Ning H, Lloyd-Jones DM. Natural history of the early repolarization pattern in a biracial cohort: CARDIA (Coronary Artery Risk Development in Young Adults) Study. J Am Coll Cardiol. 2013;61:863–869. doi: 10.1016/j.jacc.2012.11.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Gourraud JB, Le Scouarnec S, Sacher F, Chatel S, Derval N, Portero V, Chavernac P, Sandoval JE, Mabo P, Redon R, Schott JJ, Le Marec H, Haïssaguerre M, Probst V. Identification of large families in early repolarization syndrome. J Am Coll Cardiol. 2013;61:164–172. doi: 10.1016/j.jacc.2012.09.040. [DOI] [PubMed] [Google Scholar]
- 213.Sinner MF, Porthan K, Noseworthy PA, Havulinna AS, Tikkanen JT, Müller-Nurasyid M, Peloso G, Ulivi S, Beckmann BM, Brockhaus AC, Cooper RR, Gasparini P, Hengstenberg C, Hwang SJ, Iorio A, Junttila MJ, Klopp N, Kähönen M, Laaksonen MA, Lehtimäki T, Lichtner P, Lyytikäinen LP, Martens E, Meisinger C, Meitinger T, Merchant FM, Nieminen MS, Peters A, Pietilä A, Perz S, Oikarinen L, Raitakari O, Reinhard W, Silander K, Thorand B, Wichmann HE, Sinagra G, Viikari J, O’Donnell CJ, Ellinor PT, Huikuri HV, Kääb S, Newton-Cheh C, Salomaa V. A meta-analysis of genome-wide association studies of the electrocardiographic early repolarization pattern. Heart Rhythm. 2012;9:1627–1634. doi: 10.1016/j.hrthm.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
17. Subclinical Atherosclerosis
See Table 17-1 and Charts 17-1 through 17-6.
Table 17-1.
CAC Scores for the 75th Percentile of Men and Women of Different Race/Ethnic Groups, at Specified Ages
| Age, y | 75th Percentile CAC Scores*
|
|||
|---|---|---|---|---|
| Black | Chinese | Hispanic | White | |
| Women | ||||
| 45 | 0 | 0 | 0 | 0 |
| 55 | 0 | 2 | 0 | 1 |
| 65 | 26 | 45 | 19 | 54 |
| 75 | 138 | 103 | 116 | 237 |
| Men | ||||
| 45 | 0 | 3 | 0 | 0 |
| 55 | 15 | 34 | 27 | 68 |
| 65 | 95 | 121 | 141 | 307 |
| 75 | 331 | 229 | 358 | 820 |
CAC indicates coronary artery calcification.
The 75th percentile CAC score is the score at which 75% of people of the same age, sex, and race have a score at or below this level and 25% of people of the same age, sex, and race have a higher score. (Source: MESA CAC Tools Web site.42)
Chart 17-1.
Prevalence (%) of coronary calcium: US adults 33 to 45 years of age. P<0.0001 across race-sex groups. Data derived from Loria et al.5
Chart 17-6.
Mean values of carotid intima-media thickness (IMT) for different carotid artery segments in older adults, by race. Data derived from Manolio et al.32
Atherosclerosis, a systemic disease process in which fatty deposits, inflammation, cells, and scar tissue build up within the walls of arteries, is the underlying cause of the majority of clinical cardiovascular events. Individuals who develop atherosclerosis tend to develop it in a number of different types of arteries (large and small arteries and those feeding the heart, brain, kidneys, and extremities), although they may have much more in some parts of the body than others. In recent decades, advances in imaging technology have allowed for improved ability to detect and quantify atherosclerosis at all stages and in multiple different vascular beds. Two modalities, CT of the chest for evaluation of CAC and B-mode ultrasound of the neck for evaluation of carotid artery IMT, have been used in large studies with outcomes data and may help define the burden of atherosclerosis in individuals before they develop clinical events such as heart attack or stroke. Another commonly used method for detecting and quantifying atherosclerosis in the peripheral arteries is the ABI. Data on cardiovascular outcomes are beginning to emerge for additional modalities that measure anatomic and functional measures of subclinical disease, including brachial artery reactivity testing, aortic and carotid magnetic resonance imaging, and tonometric methods of measuring vascular compliance or microvascular reactivity. Further research may help to define the role of these techniques in cardiovascular risk assessment. Some guidelines have recommended screening for subclinical atherosclerosis, especially by CAC, or IMT may be appropriate in people at intermediate risk for HD (eg, 10-year estimated risk of 10% to 20%) but not for lower-risk general population screening or for people with preexisting HD or most other high-risk conditions.1,2 However, a recent guideline notes those with DM who are ≥40 years of age may be suitable for screening of risk by coronary calcium. There are still limited data demonstrating whether screening with these and other imaging modalities can improve patient outcomes or whether it only increases downstream medical care costs. A recently published report in a large cohort randomly assigned to coronary calcium screening or not showed such screening to result in an improved risk factor profile without increasing downstream medical costs.3
Abbreviations Used in Chapter 17
| ABI | ankle-brachial index |
| AF | atrial fibrillation |
| ARIC | Atherosclerosis Risk in Communities study |
| BMI | body mass index |
| BP | blood pressure |
| CAC | coronary artery calcification |
| CAD | coronary artery disease |
| CARDIA | Coronary Artery Risk Development in Young Adults |
| CHD | coronary heart disease |
| CHS | Cardiovascular Health Study |
| CI | confidence interval |
| CONFIRM | Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry |
| CRP | C-reactive protein |
| CT | computed tomography |
| CVD | cardiovascular disease |
| DBP | diastolic blood pressure |
| DM | diabetes mellitus |
| FHS | Framingham Heart Study |
| FMD | flow-mediated dilation |
| FRS | Framingham Risk Score |
| HDL | high-density lipoprotein |
| HD | heart disease |
| HR | hazard ratio |
| IMT | intima-media thickness |
| JUPITER | Justification for the Use of Statins in Primary Prevention: An Intervention Trial Evaluating Rosuvastatin |
| LDL | low-density lipoprotein |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| MI | myocardial infarction |
| NHLBI | National Heart, Lung, and Blood Institute |
| RR | relative risk |
| SBP | systolic blood pressure |
| SD | standard deviation |
Coronary Artery Calcification
Background
CAC is a measure of the burden of atherosclerosis in the heart arteries and is measured by CT. Other components of the atherosclerotic plaque, including fatty (eg, cholesterol- rich components) and fibrotic components, often accompany CAC and may be present even in the absence of CAC.
The presence of any CAC, which indicates that at least some atherosclerotic plaque is present, is defined by an Agatston score >0. Clinically significant plaque, frequently an indication for more aggressive risk factor management, is often defined by an Agatston score ≥100 or a score ≥75th percentile for one’s age and sex. An Agatston score ≥400 has been noted to be an indication for further diagnostic evaluation (eg, exercise testing or myocardial perfusion imaging) for CAD.
Prevalence
(See Table 17-1 and Charts 17-1 and 17-2.)
Chart 17-2.
Prevalence (%) of coronary calcium: US adults 45 to 84 years of age. P<0.0001 across ethnic groups in both men and women. Data derived from Bild et al.6
-
The NHLBI’s FHS reported CAC measured in 3238 white adults in age groups ranging from <45 years of age to ≥75 years of age.4
Overall, 32.0% of women and 52.9% of men had prevalent CAC.
Among participants at intermediate risk according to FRS, 58% of women and 67% of men had prevalent CAC.
-
The NHLBI’s CARDIA study measured CAC in 3043 black and white adults 33 to 45 years of age (at the CARDIA year 15 examination).5
Overall, 15.0% of men and 5.1% of women, 5.5% of those 33 to 39 years of age and 13.3% of those 40 to 45 years of age, had prevalent CAC. Overall, 1.6% of participants had an Agatston score that exceeded 100.
Chart 17-1 shows the prevalence of CAC by ethnicity and sex. The prevalence of CAC was lower in black men than in white men but was similar in black and white women at these ages.
-
The NHLBI’s MESA measured CAC in 6814 participants 45 to 84 years of age, including white (n=2619), black (n=1898), Hispanic (n=1494), and Chinese (n=803) men and women.6
Chart 17-2 shows the prevalence of CAC by sex and ethnicity.
The prevalence and 75th percentile levels of CAC were highest in white men and lowest in black and Hispanic women. Significant ethnic differences persisted after adjustment for risk factors, with the RR of coronary calcium being 22% less in blacks, 15% less in Hispanics, and 8% less in Chinese than in whites.
Table 17-1 shows the 75th percentile levels of CAC by sex and race at selected ages. These might be considered cut points above which more aggressive efforts to control risk factors (eg, elevated cholesterol or BP) could be implemented and/or at which treatment goals might be more aggressive (eg, LDL cholesterol <100 mg/dL instead of <130 mg/dL).
The prevalence of CAC varies widely according to FRS. In a report from MESA,7 the prevalence of CAC among individuals with very low FRS (10-year risk <5%) was low. These findings may have important implications for population screening for subclinical atherosclerosis.
Investigators from the NHLBI’s CARDIA study examined the association between neighborhood attributes and subclinical atherosclerosis in younger adult populations. Using 2000 US Census block-group-level data, among women, higher odds of CAC were associated with higher neighborhood deprivation and lower neighborhood cohesion. Among all men, neither neighborhood deprivation nor neighborhood cohesion was associated with CAC, whereas among men in deprived neighborhoods, low cohesion was associated with higher odds of CAC.8
CAC and Incidence of Cardiovascular Events
(See Charts 17-3 and 17-4.)
Chart 17-3.
Hazard ratios (HR) for coronary heart disease (CHD) events associated with coronary calcium scores: US adults 45 to 84 years of age (reference group, coronary artery calcification [CAC]=0). All HRs P<0.0001. Major CHD events included myocardial infarction and death attributable to CHD; any CHD events included major CHD events plus definite angina or definite or probable angina followed by revascularization. Data derived from Detrano et al.9
Chart 17-4.
Hazard ratios (HR) for coronary heart disease events associated with coronary calcium scores: US adults (reference group, coronary artery calcification [CAC]=0 and Framingham Risk Score <10%). Coronary heart disease events included nonfatal myocardial infarction and death attributable to coronary heart disease. Data derived from Greenland et al.10
-
The NHLBI’s MESA recently reported on the association of CAC scores with first CHD events over a median followup of 3.9 years among a population-based sample of 6722 men and women (39% white, 27% black, 22% Hispanic, and 12% Chinese).9
Chart 17-3 shows the HRs associated with CAC scores of 1 to 100, 101 to 300, and >300 compared with those without CAC (score=0), after adjustment for standard risk factors. People with CAC scores of 1 to 100 had ≈4 times greater risk and those with CAC scores >100 were 7 to 10 times more likely to experience a coronary event than those without CAC.
CAC provided similar predictive value for coronary events in whites, Chinese, blacks, and Hispanics (HRs ranging from 1.15–1.39 for each doubling of coronary calcium).
-
In another report of a community-based sample, not referred for clinical reasons, the South Bay Heart Watch examined CAC in 1461 adults (average age 66 years) with coronary risk factors, with a median of 7.0 years of follow-up.10
Chart 17-4 shows the HRs associated with increasing CAC scores (relative to CAC=0 and <10% risk category) in low-risk (<10%), intermediate-risk (10%–15% and 16%–20%), and high-risk (>20%) FRS categories of estimated risk for CHD in 10 years. Increasing CAC scores further predicted risk in intermediate- and highrisk groups.
In a study of healthy adults 60 to 72 years of age who were free of clinical CAD, predictors of the progression of CAC were assessed. Predictors tested included age, sex, race/ethnicity, smoking status, BMI, family history of CAD, CRP, several measures of DM, insulin levels, BP, and lipids. Insulin resistance, in addition to the traditional cardiac risk factors, independently predicts progression of CAC.11 Clinically, however, it is not yet recommended to conduct serial scanning of CAC to measure effects of therapeutic interventions.
A recent publication from MESA also used CAC, in particular, and carotid IMT to stratify CHD and CVD event risk in people with metabolic syndrome and DM; those with low levels of CAC or carotid IMT have CHD and CVD event rates as low as many people without metabolic syndrome and DM. Those with DM who have CAC scores <100 have annual CHD event rates of <1%.12
It is noteworthy, as recently demonstrated in MESA in 5878 participants with a median of 5.8 years of follow-up, that the addition of CAC to standard risk factors resulted in significant improvement of classification of risk for incident CHD events, placing 77% of people in the highest or lowest risk categories compared with 69% based on risk factors alone. An additional 23% of those who experienced events were reclassified as high risk, and 13% with events were reclassified as low risk.13
The contribution of CAC to risk prediction has also been observed in other cohorts, including both the Heinz Nixdorf Recall Study14 and the Rotterdam Study.15
An absence of CAC, observed in 40% to 50% of individuals, confers a very low risk for future cardiovascular events. In a recent meta-analysis of 13 studies assessing the relationship of CAC with adverse cardiovascular outcomes that included 71 595 asymptomatic patients, 29 312 patients (41%) did not have any evidence of CAC.16 In a follow-up that averaged 3 to 5 years, 154 of 29 312 patients without CAC (0.47%) experienced a cardiovascular event compared with 1749 of 42 283 patients with CAC (4.14%). The cumulative RR ratio was 0.15 (95% CI, 0.11–0.21; P<0.001). These findings were confirmed in MESA, which reported a rate of 0.52% for CHD events during a median of 4 years of follow-up among people with no detectable CAC.17
A recent meta-analysis18 also highlighted the utility of CAC testing in the diabetic population. In this meta-analysis, 8 studies were included (n=6521; 802 events; mean followup, 5.18 years). The RR for all-cause mortality or cardiovascular events or both comparing a total CAC score ≥10 with a score <10 was 5.47 (95% CI, 2.59–11.53; I2=82.4%, P<0.001). For people with a CAC score <10, the posttest probability of the composite outcome was ≈1.8%, which represents a 6.8-fold reduction from the pretest probability, which suggests that those with low or absent CAC may facilitate risk stratification by enabling the identification of people at low risk within this high-risk population.18
In the Heinz Nixdorf Recall Study,19 CAC independently predicted stroke during a mean follow-up of 7.9 years. Cox proportional hazards regressions were used to examine CAC as a predictor of stroke in addition to established vascular risk factors (age, sex, SBP, LDL, HDL, DM, smoking, and AF). Study participants who had a stroke had significantly higher CAC values at baseline than the remaining subjects (median, 104.8 [quartile 1, 14.0; quartile 3, 482.2] versus 11.2 [quartile 1, 0; quartile 3, 106.2]; P<0.001). In a multivariable Cox regression, log10(CAC+1) was an independent stroke predictor (HR, 1.52; 95% CI, 1.19–1.92; P=0.001). CAC discriminated stroke risk specifically in participants in the low (<10%) and intermediate (10%– 20%) FRS categories.19
CAC Progression and Risk
A recent report in 4609 individuals who had baseline and repeat cardiac CT found that progression of CAC provided incremental information over baseline score, demographics, and cardiovascular risk factors in predicting future allcause mortality.20
More recently, data from 6778 people in MESA showed annual CAC progression was an average of 25 Agatston units, and among those without CAC at baseline, a 5-U annual change in CAC was associated with HRs of 1.4 and 1.5 for total and hard CHD events, respectively. Among those with CAC >0 at baseline, HRs per 100-U annual change in CAC were 1.2 and 1.3, respectively, and for those with annual progression ≥300 versus no progression, HRs were 3.8 and 6.3, respectively.21 Progression of CAC in MESA was also shown to be greater in those with metabolic syndrome and DM than in those with neither condition, and progression of CAC in each of these conditions was associated with a greater future risk of CHD events.22
In MESA, greater adherence to a healthy lifestyle based on a healthy lifestyle score was associated with slower progression of CAC and lower mortality rates relative to those with the most unhealthy lifestyle.23
Carotid IMT
Background
Carotid IMT measures the thickness of 2 layers (the intima and media) of the wall of the carotid arteries, the largest conduits of blood going to the brain. Carotid IMT is thought to be an even earlier manifestation of atherosclerosis than CAC, because thickening precedes the development of frank atherosclerotic plaque. Carotid IMT methods are still being refined, so it is important to know which part of the artery was measured (common carotid, internal carotid, or bulb) and whether near and far walls were both measured. This information can affect the average-thickness measurement that is usually reported.
Unlike CAC, everyone has some thickness to the layers of their arteries, but people who develop atherosclerosis have greater thickness. Ultrasound of the carotid arteries can also detect plaques and determine the degree of narrowing of the artery they may cause. Epidemiological data, including the data discussed below, have indicated that high-risk levels of thickening might be considered as those in the highest quartile or quintile for one’s age and sex, or ≥1 mm.
Although ultrasound is commonly used to diagnose plaque in the carotid arteries in people who have had strokes or who have bruits (sounds of turbulence in the artery), guidelines are limited as to screening of asymptomatic people with carotid IMT to quantify atherosclerosis or predict risk. However, some organizations have recognized that carotid IMT measurement by B-mode ultrasonography may provide an independent assessment of coronary risk.24
Prevalence and Association With Incident Cardiovascular Events
(See Charts 17-5 and 17-6.)
Chart 17-5.
Mean values of carotid intima-media thickness (IMT) for different carotid artery segments in younger adults by race and sex (Bogalusa Heart Study). Data derived from Urbina et al.25
-
The Bogalusa Heart Study measured carotid IMT in 518 black and white men and women at a mean age of 32±3 years. These men and women were healthy but overweight.25
The mean values of carotid IMT for the different segments are shown in Chart 17-5 by sex and race. Men had significantly higher carotid IMT in all segments than women, and blacks had higher common carotid and carotid bulb IMTs than whites.
Even at this young age, after adjustment for age, race, and sex, carotid IMT was associated significantly and positively with waist circumference, SBP, DBP, and LDL cholesterol. Carotid IMT was inversely correlated with HDL cholesterol levels. Participants with greater numbers of adverse risk factors (0, 1, 2, 3, or more) had stepwise increases in mean carotid IMT levels.
In a subsequent analysis, the Bogalusa investigators examined the association of risk factors measured since childhood with carotid IMT measured in these young adults.26 Higher BMI and LDL cholesterol levels measured at 4 to 7 years of age were associated with increased risk for being >75th percentile for carotid IMT in young adulthood. Higher SBP and LDL cholesterol and lower HDL cholesterol in young adulthood were also associated with having high carotid IMT. These data highlight the importance of adverse risk factor levels in early childhood and young adulthood in the early development of atherosclerosis.
Among both women and men in MESA, blacks had the highest common carotid IMT, but they were similar to whites and Hispanics in internal carotid IMT. Chinese participants had the lowest carotid IMT, in particular in the internal carotid, of the 4 ethnic groups (Chart 17-6).
-
The NHLBI’s CHS reported follow-up of 4476 men and women ≥65 years of age (mean age 72 years) who were free of CVD at baseline.27
Mean maximal common carotid IMT was 1.03±0.20 mm, and mean internal carotid IMT was 1.37±0.55 mm.
After a mean follow-up of 6.2 years, those with maximal combined carotid IMT in the highest quintile had a 4- to 5-fold greater risk for incident heart attack or stroke than those in the bottom quintile. After adjustment for other risk factors, there was still a 2- to 3-fold greater risk for the top versus the bottom quintile.
A study of 441 individuals ≤65 years of age without a history of CAD, DM, or hyperlipidemia who were examined for carotid IMT found 42% had high-risk carotid ultrasound findings (carotid IMT ≥75th percentile, adjusted for age, sex, and race or presence of plaque). Among those with an FRS ≤5%, 38% had high-risk carotid ultrasound findings.28
Conflicting data have been reported on the contribution of carotid IMT to risk prediction. In 13 145 participants in the NHLBI’s ARIC study, the addition of carotid IMT combined with identification of plaque presence or absence to traditional risk factors reclassified risk in 23% of individuals overall, with a net reclassification improvement of 9.9%. There was a modest but statistically significant improvement in the area under the receiver operating characteristic curve, from 0.742 to 0.755.29 In contrast, data reported recently from the Carotid Atherosclerosis Progression Study observed a net reclassification improvement of −1.4% that was not statistically significant.30
A recent study from a consortium of 14 population-based cohorts consisting of 45 828 individuals followed up for a median of 11 years demonstrated little additive value of common carotid IMT to FRS for purposes of discrimination and reclassification as far as incident MI and stroke were concerned. The C statistics of the model with FRS alone (0.757; 95% CI, 0.749–0.764) and with addition of common carotid IMT (0.759; 95% CI, 0.752–0.766) were similar. The net reclassification improvement with the addition of common carotid IMT was small (0.8%; 95% CI, 0.1%–1.6%). In those at intermediate risk, the net reclassification improvement was 3.6% among all individuals (95% CI, 2.7%–4.6%).31
CAC and Carotid IMT
-
In the NHLBI’s MESA, a study of white, black, Chinese, and Hispanic adults 45 to 84 years of age, carotid IMT and CAC were found to be commonly associated, but patterns of association differed somewhat by sex and race.32
Common and internal carotid IMT were greater in women and men who had CAC than in those who did not, regardless of ethnicity.
Overall, CAC prevalence and scores were associated with carotid IMT, but associations were somewhat weaker in blacks than in other ethnic groups.
In general, blacks had the thickest carotid IMT of all 4 ethnic groups, regardless of the presence of CAC.
Common carotid IMT differed little by race/ethnicity in women with any CAC, but among women with no CAC, IMT was higher among blacks (0.86 mm) than in the other 3 groups (0.76–0.80 mm).
-
In a more recent analysis from the NHLBI’s MESA study, the investigators reported on follow-up of 6698 men and women in 4 ethnic groups over 5.3 years and compared the predictive utility of carotid IMT and CAC.33
CAC was associated more strongly than carotid IMT with the risk of incident CVD.
After adjustment for each other (CAC score and IMT) and for traditional CVD risk factors, the HR for CVD increased 2.1-fold for each 1-SD increment of log-transformed CAC score versus 1.3-fold for each 1-SD increment of the maximum carotid IMT.
For CHD events, the HRs per 1-standard deviation increment increased 2.5-fold for CAC score and 1.2-fold for IMT.
A receiver operating characteristic curve analysis also suggested that CAC score was a better predictor of incident CVD than was IMT, with areas under the curve of 0.81 versus 0.78, respectively.
Investigators from the NHLBI’s CARDIA and MESA studies examined the burden and progression of subclinical atherosclerosis among adults <50 years of age. Ten-year and lifetime risks for CVD were estimated for each participant, and the participants were stratified into 3 groups: (1) those with low 10-year (<10%) and low lifetime (<39%) predicted risk for CVD; (2) those with low 10-year (<10%) but high lifetime (≥39%) predicted risk; and (3) those with high 10-year risk (>10%). The latter group had the highest burden and greatest progression of subclinical atherosclerosis. Given the young age of those studied, ≈90% of participants were at low 10-year risk, but of these, half had high predicted lifetime risk. Compared with those with low short-term/low lifetime predicted risks, those with low short-term/high lifetime predicted risk had significantly greater burden and progression of CAC and significantly greater burden of carotid IMT, even at these younger ages. These data confirm the importance of early exposure to risk factors for the onset and progression of subclinical atherosclerosis.34
CT Angiography
CT angiography is widely used by cardiologists to aid in the diagnosis of CAD, particularly when other test results may be equivocal. It is also of interest because of its ability to detect and possibly quantitate overall plaque burden and certain characteristics of plaques that may make them prone to rupture, such as positive remodeling or low attenuation.
Compared with the established value of CAC scanning for risk reclassification in asymptomatic patients, there are limited data regarding the utility of CT angiography in asymptomatic people. This was recently assessed by the investigators of the CONFIRM registry,35 from which >7500 asymptomatic subjects with CAC and CT angiography were followed up for death and nonfatal MI for a median of 2 years. Overall, 2.2% either died or experienced nonfatal MI, and in multivariable models, compared with those without atherosclerosis, there was increasing risk across groups with increasing degrees of atherosclerosis measured by CT angiography. However, after the inclusion of CAC in the multivariable risk model, CT angiography did not provide incremental prognostic value over this short period of follow-up.35
Because of the limited outcome data in asymptomatic people, as well as the associated expense and risk of CT angiography (including generally higher radiation levels than CT scanning to detect CAC), current guidelines do not recommend its use as a screening tool for assessment of cardiovascular risk in asymptomatic people.2
Measures of Vascular Function and Incident CVD Events
Background
Measures of arterial tonometry (stiffness) are based on the concept that pulse pressure has been shown to be an important risk factor for CVD. Arterial tonometry offers the ability to directly and noninvasively measure central pulse wave velocity in the thoracic and abdominal aorta.
Brachial FMD is a marker for nitric oxide release from the endothelium that can be measured by ultrasound. Impaired FMD is an early marker of CVD.
Recommendations have not been specific, however, as to which, if any, measures of vascular function may be useful for CVD risk stratification in selected patient subgroups. Because of the absence of significant prospective data relating these measures to outcomes, latest guidelines do not currently recommend measuring either FMD or arterial stiffness for cardiovascular risk assessment in asymptomatic adults.2
Arterial Tonometry and CVD
The Rotterdam Study measured arterial stiffness in 2835 elderly participants (mean age 71 years).36 They found that as aortic pulse wave velocity increased, the risk of CHD was 1.72 (second versus first tertile) and 2.45 (third versus first tertile). Results remained robust even after accounting for carotid IMT, ABI, and pulse pressure.
A study from Denmark of 1678 individuals aged 40 to 70 years found that each 1-SD increment in aortic pulse wave velocity (3.4 m/s) increased CVD risk by 16% to 20%.37
The FHS measured several indices of arterial stiffness, including pulse wave velocity, wave reflection, and central pulse pressure.38 They found that not only was higher pulse wave velocity associated with a 48% increased risk of incident CVD events, but pulse wave velocity additionally improved CVD risk prediction (integrated discrimination improvement of 0.7%, P<0.05).
FMD and CVD
MESA measured FMD in 3026 participants (mean age 61 years) who were free of CVD. As FMD increased (ie, improved brachial function), the risk of CVD was 16% lower.39 FMD also improved CVD risk prediction compared with the FRS by improving net reclassification by 29%.
Comparison of Measures
In MESA, a comparison of 6 risk markers—CAC, ABI, high-sensitivity CRP, carotid IMT, brachial FMD, and family history of CHD—and their clinical utility over FRS was evaluated in 1330 intermediate-risk individuals. After 7.6 years of follow-up, CAC, ABI, high-sensitivity CRP, and family history were independently associated with incident CHD in multivariable analyses (HRs of 2.6, 0.79, 1.28, and 2.18, respectively), but carotid IMT and brachial FMD were not. CAC provided the highest incremental improvement over the FRS (0.784 for both CAC and FRS versus 0.623 for FRS alone), as well as the greatest net reclassification improvement (0.659).40
Utility for Risk Stratification for Treatment
CAC has been examined for its potential to identify those most likely to benefit from treatment.
In a recent report, 950 participants from MESA who met JUPITER clinical trial entry criterion (risk factors plus LDL cholesterol <130 mg/dL and CRP ≥2 mg/L) were identified and stratified according to CAC scores of 0, 1 to 100, or >100; CHD event rates were calculated, and the number needed to treat was calculated by applying the benefit found in JUPITER to the event rates found in each of these groups. For CHD, the predicted 5-year number needed to treat was 549 for those with CAC of 0, 94 for scores of 1 to 100, and 24 for scores >100, thus showing the utility of CAC in identifying those most likely to benefit from statin treatment with an appropriate number needed to treat..41
- 1.Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, Guerci AD, Lima JA, Rader DJ, Rubin GD, Shaw LJ, Wiegers SE. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 2.Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, Foster E, Hlatky MA, Hodgson JM, Kushner FG, Lauer MS, Shaw LJ, Smith SC, Jr, Taylor AJ, Weintraub WS, Wenger NK, Jacobs AK, Smith SC, Jr, Anderson JL, Albert N, Buller CE, Creager MA, Ettinger SM, Guyton RA, Halperin JL, Hochman JS, Kushner FG, Nishimura R, Ohman EM, Page RL, Stevenson WG, Tarkington LG, Yancy CW American College of Cardiology Foundation; American Heart Association. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;56:e50–e103. doi: 10.1016/j.jacc.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Rozanski A, Gransar H, Shaw LJ, Kim J, Miranda-Peats L, Wong ND, Rana JS, Orakzai R, Hayes SW, Friedman JD, Thomson LE, Polk D, Min J, Budoff MJ, Berman DS. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing: the EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) prospective randomized trial. J Am Coll Cardiol. 2011;57:1622–1632. doi: 10.1016/j.jacc.2011.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoffmann U, Massaro JM, Fox CS, Manders E, O’Donnell CJ. Defining normal distributions of coronary artery calcium in women and men (from the Framingham Heart Study) Am J Cardiol. 2008;102:1136–1141. 1141.e1. doi: 10.1016/j.amjcard.2008.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loria CM, Liu K, Lewis CE, Hulley SB, Sidney S, Schreiner PJ, Williams OD, Bild DE, Detrano R. Early adult risk factor levels and subsequent coronary artery calcification: the CARDIA Study. J Am Coll Cardiol. 2007;49:2013–2020. doi: 10.1016/j.jacc.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 6.Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, Ouyang P, Jackson S, Saad MF. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 7.Okwuosa TM, Greenland P, Ning H, Liu K, Bild DE, Burke GL, Eng J, Lloyd-Jones DM. Distribution of coronary artery calcium scores by Framingham 10-year risk strata in the MESA (Multi-Ethnic Study of Atherosclerosis): potential implications for coronary risk assessment. J Am Coll Cardiol. 2011;57:1838–1845. doi: 10.1016/j.jacc.2010.11.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim D, Diez Roux AV, Kiefe CI, Kawachi I, Liu K. Do neighborhood socioeconomic deprivation and low social cohesion predict coronary calcification? The CARDIA study. Am J Epidemiol. 2010;172:288–298. doi: 10.1093/aje/kwq098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O’Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 10.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals [published correction appears in JAMA. 2004;291:563] JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 11.Lee KK, Fortmann SP, Fair JM, Iribarren C, Rubin GD, Varady A, Go AS, Quertermous T, Hlatky MA. Insulin resistance independently predicts the progression of coronary artery calcification. Am Heart J. 2009;157:939–945. doi: 10.1016/j.ahj.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Malik S, Budoff MJ, Katz R, Blumenthal RS, Bertoni AG, Nasir K, Szklo M, Barr RG, Wong ND. Impact of subclinical atherosclerosis on cardiovascular disease events in individuals with metabolic syndrome and diabetes: the Multi-Ethnic Study of Atherosclerosis. Diabetes Care. 2011;34:2285–2290. doi: 10.2337/dc11-0816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, Greenland P. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–1616. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erbel R, Möhlenkamp S, Moebus S, Schmermund A, Lehmann N, Stang A, Dragano N, Grönemeyer D, Seibel R, Kälsch H, Bröcker-Preuss M, Mann K, Siegrist J, Jöckel KH Heinz Nixdorf Recall Study Investigative Group. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol. 2010;56:1397–1406. doi: 10.1016/j.jacc.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 15.Elias-Smale SE, Proença RV, Koller MT, Kavousi M, van Rooij FJ, Hunink MG, Steyerberg EW, Hofman A, Oudkerk M, Witteman JC. Coronary calcium score improves classification of coronary heart disease risk in the elderly: the Rotterdam study. J Am Coll Cardiol. 2010;56:1407–1414. doi: 10.1016/j.jacc.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 16.Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffmann U, Hoffman U, Cury RC, Abbara S, Brady TJ, Budoff MJ, Blumenthal RS, Nasir K. Diagnostic and prognostic value of absence of coronary artery calcification [published correction appears in JACC Cardiovasc Imaging. 2010;3:1089] JACC Cardiovasc Imaging. 2009;2:675–688. doi: 10.1016/j.jcmg.2008.12.031. [DOI] [PubMed] [Google Scholar]
- 17.Budoff MJ, McClelland RL, Nasir K, Greenland P, Kronmal RA, Kondos GT, Shea S, Lima JA, Blumenthal RS. Cardiovascular events with absent or minimal coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Am Heart J. 2009;158:554–561. doi: 10.1016/j.ahj.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kramer CK, Zinman B, Gross JL, Canani LH, Rodrigues TC, Azevedo MJ, Retnakaran R. Coronary artery calcium score prediction of all cause mortality and cardiovascular events in people with type 2 diabetes: systematic review and meta-analysis. BMJ. 2013;346:f1654. doi: 10.1136/bmj.f1654. [DOI] [PubMed] [Google Scholar]
- 19.Hermann DM, Gronewold J, Lehmann N, Moebus S, Jöckel KH, Bauer M, Erbel R Heinz Nixdorf Recall Study Investigative Group. Coronary artery calcification is an independent stroke predictor in the general population. Stroke. 2013;44:1008–1013. doi: 10.1161/STROKEAHA.111.678078. [DOI] [PubMed] [Google Scholar]
- 20.Budoff MJ, Hokanson JE, Nasir K, Shaw LJ, Kinney GL, Chow D, Demoss D, Nuguri V, Nabavi V, Ratakonda R, Berman DS, Raggi P. Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovasc Imaging. 2010;3:1229–1236. doi: 10.1016/j.jcmg.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 21.Budoff MJ, Young R, Lopez VA, Kronmal RA, Nasir K, Blumenthal RS, Detrano RC, Bild DE, Guerci AD, Liu K, Shea S, Szklo M, Post W, Lima J, Bertoni A, Wong ND. Progression of coronary calcium and incident coronary heart disease events: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2013;61:1231–1239. doi: 10.1016/j.jacc.2012.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong ND, Nelson JC, Granston T, Bertoni AG, Blumenthal RS, Carr JJ, Guerci A, Jacobs DR, Jr, Kronmal R, Liu K, Saad M, Selvin E, Tracy R, Detrano R. Metabolic syndrome, diabetes, and incidence and progression of coronary calcium: the Multiethnic Study of Atherosclerosis study. JACC Cardiovasc Imaging. 2012;5:358–366. doi: 10.1016/j.jcmg.2011.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmed HM, Blaha MJ, Nasir K, Jones SR, Rivera JJ, Agatston A, Blankstein R, Wong ND, Lakoski S, Budoff MJ, Burke GL, Sibley CT, Ouyang P, Blumenthal RS. Low-risk lifestyle, coronary calcium, cardiovascular events, and mortality: results from MESA. Am J Epidemiol. 2013;178:12–21. doi: 10.1093/aje/kws453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith SC, Jr, Greenland P, Grundy SM. AHA Conference Proceedings. Prevention Conference V: Beyond Secondary Prevention: Identifying the high-Risk Patient for Primary Prevention: executive summary: American Heart Association. Circulation. 2000;101:111–116. doi: 10.1161/01.cir.101.1.111. [DOI] [PubMed] [Google Scholar]
- 25.Urbina EM, Srinivasan SR, Tang R, Bond MG, Kieltyka L, Berenson GS Bogalusa Heart Study. Impact of multiple coronary risk factors on the intima-media thickness of different segments of carotid artery in healthy young adults (the Bogalusa Heart Study) Am J Cardiol. 2002;90:953–958. doi: 10.1016/s0002-9149(02)02660-7. [DOI] [PubMed] [Google Scholar]
- 26.Li S, Chen W, Srinivasan SR, Bond MG, Tang R, Urbina EM, Berenson GS. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA. 2003;290:2271–2276. doi: 10.1001/jama.290.17.2271. [DOI] [PubMed] [Google Scholar]
- 27.O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 28.Eleid MF, Lester SJ, Wiedenbeck TL, Patel SD, Appleton CP, Nelson MR, Humphries J, Hurst RT. Carotid ultrasound identifies high risk subclinical atherosclerosis in adults with low Framingham risk scores. J Am Soc Echocardiogr. 2010;23:802–808. doi: 10.1016/j.echo.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Nambi V, Chambless L, Folsom AR, He M, Hu Y, Mosley T, Volcik K, Boerwinkle E, Ballantyne CM. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (Atherosclerosis Risk In Communities) study. J Am Coll Cardiol. 2010;55:1600–1607. doi: 10.1016/j.jacc.2009.11.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lorenz MW, Schaefer C, Steinmetz H, Sitzer M. Is carotid intima media thickness useful for individual prediction of cardiovascular risk? Ten-year results from the Carotid Atherosclerosis Progression Study (CAPS) Eur Heart J. 2010;31:2041–2048. doi: 10.1093/eurheartj/ehq189. [DOI] [PubMed] [Google Scholar]
- 31.Den Ruijter HM, Peters SA, Anderson TJ, Britton AR, Dekker JM, Eijkemans MJ, Engström G, Evans GW, de Graaf J, Grobbee DE, Hedblad B, Hofman A, Holewijn S, Ikeda A, Kavousi M, Kitagawa K, Kitamura A, Koffijberg H, Lonn EM, Lorenz MW, Mathiesen EB, Nijpels G, Okazaki S, O’Leary DH, Polak JF, Price JF, Robertson C, Rembold CM, Rosvall M, Rundek T, Salonen JT, Sitzer M, Stehouwer CD, Witteman JC, Moons KG, Bots ML. Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis [published correction appears in JAMA. 2013;310:1739] JAMA. 2012;308:796–803. doi: 10.1001/jama.2012.9630. [DOI] [PubMed] [Google Scholar]
- 32.Manolio TA, Arnold AM, Post W, Bertoni AG, Schreiner PJ, Sacco RL, Saad MF, Detrano RL, Szklo M. Ethnic differences in the relationship of carotid atherosclerosis to coronary calcification: the Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2008;197:132–138. doi: 10.1016/j.atherosclerosis.2007.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Folsom AR, Kronmal RA, Detrano RC, O’Leary DH, Bild DE, Bluemke DA, Budoff MJ, Liu K, Shea S, Szklo M, Tracy RP, Watson KE, Burke GL. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) [published correction appears in Arch Intern Med. 2008;168:1782] Arch Intern Med. 2008;168:1333–1339. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berry JD, Liu K, Folsom AR, Lewis CE, Carr JJ, Polak JF, Shea S, Sidney S, O’Leary DH, Chan C, Lloyd-Jones DM. Prevalence and progression of subclinical atherosclerosis in younger adults with low short-term but high lifetime estimated risk for cardiovascular disease: the Coronary Artery Risk Development in Young Adults Study and Multi-Ethnic Study of Atherosclerosis. Circulation. 2009;119:382–389. doi: 10.1161/CIRCULATIONAHA.108.800235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cho I, Chang HJ, Sung JM, Pencina MJ, Lin FY, Dunning AM, Achenbach S, Al-Mallah M, Berman DS, Budoff MJ, Callister TQ, Chow BJ, Delago A, Hadamitzky M, Hausleiter J, Maffei E, Cademartiri F, Kaufmann P, Shaw LJ, Raff GL, Chinnaiyan KM, Villines TC, Cheng V, Nasir K, Gomez M, Min JK CONFIRM Investigators. Coronary computed tomographic angiography and risk of all-cause mortality and nonfatal myocardial infarction in subjects without chest pain syndrome from the CONFIRM Registry (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) Circulation. 2012;126:304–313. doi: 10.1161/CIRCULATIONAHA.111.081380. [DOI] [PubMed] [Google Scholar]
- 36.Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA, Asmar R, Reneman RS, Hoeks AP, Breteler MM, Witteman JC. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation. 2006;113:657–663. doi: 10.1161/CIRCULATIONAHA.105.555235. [DOI] [PubMed] [Google Scholar]
- 37.Willum-Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation. 2006;113:664–670. doi: 10.1161/CIRCULATIONAHA.105.579342. [DOI] [PubMed] [Google Scholar]
- 38.Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ. Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation. 2010;121:505–511. doi: 10.1161/CIRCULATIONAHA.109.886655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, Post W, Lima JA, Crouse JR, Herrington DM. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the Multi-Ethnic Study of Atherosclerosis. Circulation. 2009;120:502–509. doi: 10.1161/CIRCULATIONAHA.109.864801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary D, Carr JJ, Goff DC, Greenland P, Herrington DM. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate- risk individuals. JAMA. 2012;308:788–795. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blaha MJ, Budoff MJ, DeFilippis AP, Blankstein R, Rivera JJ, Agatston A, O’Leary DH, Lima J, Blumenthal RS, Nasir K. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet. 2011;378:684–692. doi: 10.1016/S0140-6736(11)60784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.MESA CAC score reference values. [Accessed June 17, 2013];MESA CAC Tools Web site. http://www.mesa-nhlbi.org/Calcium/input.aspx.
18. Coronary Heart Disease, Acute Coronary Syndrome, and Angina Pectoris
See Tables 18-1 and 18-2 and Charts 18-1 through 18-10; see Glossary (Chapter 26) for details and definitions.
Table 18-1.
Coronary Heart Disease
| Population Group | Prevalence, CHD, 2010 Age ≥20 y | Prevalence, MI, 2010 Age ≥20 y | New and Recurrent MI and Fatal CHD, Age ≥35 y | New and Recurrent MI, Age ≥35 y | Mortality,* CHD, 2010 All Ages | Mortality,* MI, 2010 All Ages | Hospital Discharges CHD, 2010 All Ages |
|---|---|---|---|---|---|---|---|
| Both sexes | 15 400 000 (6.4%) | 7 600 000 (2.9%) | 915 000 | 720 000 | 379 559 | 122 071 | 1 346 000 |
| Males | 8 800 000 (7.9%) | 5 000 000 (4.2%) | 530 000 | 420 000 | 207 580 (54.7%)† | 67 435 (55.2%)† | 828 000 |
| Females | 6 600 000 (5.1%) | 2 600 000 (1.7%) | 385 000 | 300 000 | 171 979 (45.3%)† | 54 636 (44.8%)† | 518 000 |
| NH white males | 8.2% | 4.4% | 465 000‡ | … | 181 386 | 59 181 | … |
| NH white females | 4.6% | 1.5% | 330 000‡ | … | 148 891 | 47 023 | … |
| NH black males | 6.8% | 3.9% | 65 000‡ | … | 20 615 | 6445 | … |
| NH black females | 7.1% | 2.3% | 55 000‡ | … | 19 015 | 6298 | … |
| Mexican American males | 6.7% | 3.6% | … | … | … | … | … |
| Mexican American females | 5.3% | 1.7% | … | … | … | … | … |
| Asian | 4.5%§ | … | … | … | 7821|| | 2530|| | … |
| American Indian/Alaska Native | 8.1%§¶ | … | … | … | 1831 | 594 | … |
CHD includes people who responded “yes” to at least 1 of the questions in “Has a doctor or other health professional ever told you that you had coronary heart disease, angina or angina pectoris, heart attack, or myocardial infarction?” Those who answered “no” but were diagnosed with Rose angina are also included (the Rose questionnaire is only administered to survey participants >40 y of age).
CHD indicates coronary heart disease; ellipses (…), data not available; MI, myocardial infarction; and NH, non-Hispanic.
Mortality data for the white, black, Asian or Pacific Islander, and American Indian/Alaska Native populations include deaths of people of Hispanic and non-Hispanic origin. Numbers of deaths for the American Indian/Alaska Native and Asian or Pacific Islander populations are known to be underestimated.
These percentages represent the portion of total CHD and MI mortality that is for males vs females.
Estimates include Hispanics and non-Hispanics. Estimates for whites include other nonblack races.
National Health Interview Survey, National Center for Health Statistics 2012; data are weighted percentages for Americans ≥18 y of age.1
Includes Chinese, Filipino, Hawaiian, Japanese, and Other Asian or Pacific Islander.
Estimate considered unreliable or does not meet standards of reliability or precision.
Sources: Prevalence: National Health and Nutrition Examination Survey 2007 to 2010 (National Center for Health Statistics) and National Heart, Lung, and Blood Institute. Percentages for racial/ethnic groups are age adjusted for Americans ≥20 y of age. Age-specific percentages are extrapolated to the 2010 US population estimates. These data are based on self-reports. Incidence: Atherosclerosis Risk in Communities study (2005–2010), National Heart, Lung, and Blood Institute. Mortality: Centers for Disease Control and Prevention/National Center for Health Statistics, 2010 Mortality Multiple Cause-of-Death–United States, version dated May 29, 2013. Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics (data include those inpatients discharged alive, dead, or status unknown).
Table 18-2.
Angina Pectoris
| Population Group | Prevalence, 2010, Age ≥20 y | Incidence of Stable AP, Age ≥45 y | Hospital Discharges, 2010, All Ages* |
|---|---|---|---|
| Both sexes | 7 800 000 (3.2%) | 565 000 | 22 000 |
| Males | 3 700 000 (3.3%) | 370 000 | 12 000 |
| Females | 4 100 000 (3.2%) | 195 000 | 10 000 |
| NH white males | 3.3% | … | … |
| NH white females | 2.8% | … | … |
| NH black males | 2.4% | … | … |
| NH black females | 5.4% | … | … |
| Mexican American males | 3.4% | … | … |
| Mexican American females | 3.3% | … | … |
AP is chest pain or discomfort that results from insufficient blood flow to the heart muscle. Stable AP is predictable chest pain on exertion or under mental or emotional stress. The incidence estimate is for AP without myocardial infarction.
AP indicates angina pectoris; ellipses, data not available; and NH, non-Hispanic.
There were 56 000 days of care for discharges of patients with AP from short-stay hospitals in 2010.
Sources: Prevalence: National Health and Nutrition Examination Survey 2007 to 2010 (National Center for Health Statistics) and National Heart, Lung, and Blood Institute; percentages for racial/ethnic groups are age adjusted for US adults ≥20 y of age. AP includes people who either answered “yes” to the question of ever having angina or AP or who were diagnosed with Rose angina (the Rose questionnaire is only administered to survey participants >40 y of age). Estimates from National Health and Nutrition Examination Survey 2007 to 2010 (National Center for Health Statistics) were applied to 2010 population estimates (≥20 y of age). Incidence: AP uncomplicated by a myocardial infarction or with no myocardial infarction (Framingham Heart Study [the original cohort and the Offspring Cohort 1986–2009], National Heart, Lung, and Blood Institute). Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics; data include those inpatients discharged alive, dead, or status unknown.
Chart 18-1.
Prevalence of coronary heart disease by age and sex (National Health and Nutrition Examination Survey: 2007–2010). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 18-10.
Incidence of angina pectoris (deemed uncomplicated on the basis of physician interview of patient) by age and sex (Framingham Heart Study 1986–2009). Data derived from National Heart, Lung, and Blood Institute.
Coronary Heart Disease
ICD-9 410 to 414, 429.2; ICD-10 I20 to I25; including MI ICD-10 I21 to I22.
Abbreviations Used in Chapter 18
| ACC | American College of Cardiology ACS acute coronary syndrome |
| ACTION | Acute Coronary Treatment and Intervention Outcomes Network |
| AHA | American Heart Association |
| AMI | acute myocardial infarction |
| AP | angina pectoris |
| ARIC | Atherosclerosis Risk in Communities study |
| BMI | body mass index |
| BP | blood pressure |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CABG | coronary artery bypass graft |
| CAD | coronary artery disease |
| CDC | Centers for Disease Control and Prevention |
| CHD | coronary heart disease |
| CHS | Cardiovascular Health Study |
| CI | confidence interval |
| CRUSADE | Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| ECG | electrocardiogram/electrocardiographic |
| ED | emergency department |
| EHS-ACS-II | second Euro Heart Survey on ACS |
| EMS | emergency medical services |
| FHS | Framingham Heart Study |
| GRACE | Global Registry of Acute Coronary Events |
| GWTG | Get With The Guidelines |
| HCUP | Healthcare Cost and Utilization Project |
| HD | heart disease |
| HDL-C | high-density lipoprotein-cholesterol |
| HF | heart failure |
| ICD-9 | International Classification of Diseases, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| MEPS | Medical Expenditure Panel Survey |
| MI | myocardial infarction |
| NAMCS | National Ambulatory Medical Care Survey |
| NCDR | National Cardiovascular Data Registry |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHAMCS | National Hospital Ambulatory Medical Care Survey |
| NHANES | National Health and Nutrition Examination Survey |
| NHDS | National Hospital Discharge Survey |
| NHIS | National Health Interview Study |
| NHLBI | National Heart, Lung, and Blood Institute |
| NRMI-4 | National Registry of Myocardial Infarction 4 |
| NSTEMI | non–ST-segment–elevation myocardial infarction |
| OR | odds ratio |
| PCI | percutaneous coronary intervention |
| SBP | systolic blood pressure |
| STEMI | ST-segment–elevation myocardial infarction |
| UA | unstable angina |
| WISE | Women’s Ischemia Syndrome Evaluation |
| YLL | years of life lost |
Prevalence
(See Table 18-1 and Charts 18-1 and 18-2.)
Chart 18-2.
Prevalence of myocardial infarction by age and sex (National Health and Nutrition Examination Survey: 2007–2010). Myocardial infarction includes people who answered “yes” to the question of ever having had a heart attack or myocardial infarction. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
-
On the basis of data from NHANES 2007 to 2010 (NHLBI tabulation), an estimated 15.4 million Americans ≥20 years of age have CHD.
Total CHD prevalence is 6.4% in US adults ≥20 years of age. CHD prevalence is 7.9% for men and 5.1% for women.
Among non-Hispanic whites, CHD prevalence is 8.2% for men and 4.6% for women.
Among non-Hispanic blacks, CHD prevalence is 6.8% for men and 7.1% for women.
Among Mexican Americans, CHD prevalence is 6.7% for men and 5.3% for women.
-
On the basis of data from the 2012 NHIS
-
According to data from NHANES 2007 to 2010 (NHLBI tabulation), the overall prevalence for MI is 2.9% in US adults ≥20 years of age. MI prevalence is 4.2% for men and 1.7% for women.
Among non-Hispanic whites, MI prevalence is 4.4% for men and 1.5% for women.
Among non-Hispanic blacks, MI prevalence is 3.9% for men and 2.3% for women.
Among Mexican Americans, MI prevalence is 3.6% for men and 1.7% for women.
Data from the BRFSS 2011 survey indicated that 4.3% of respondents had been told that they had had an MI. The highest prevalence was in Arkansas (6.4%) and West Virginia (6.2%). The lowest prevalence was in Colorado (2.7%) and Utah (3.0%). In the same survey, 4.2% of respondents were told that they had angina or CHD. The highest prevalence was in West Virginia (6.6%), and the lowest was in Colorado (2.4%).2
Projections show that by 2030, prevalence of CHD will increase ≈18% from 2013 estimates (AHA computation, based on methodology described in Heidenreich et al).3
Incidence
(See Table 18-1 and Charts 18-3 through 18-5.)
Chart 18-3.
Annual number of adults per 1000 having diagnosed heart attack or fatal coronary heart disease (CHD) by age and sex (Atherosclerosis Risk in Communities Surveillance: 2005–2010 and Cardiovascular Health Study). These data include myocardial infarction (MI) and fatal CHD but not silent MI. Source: National Heart, Lung, and Blood Institute.
Chart 18-5.
Incidence of myocardial infarction by age, sex, and race (Atherosclerosis Risk in Communities Surveillance: 2005-2010). Source: Unpublished data from Atherosclerosis Risk in Communities study, National Heart, Lung, and Blood Institute.
Approximately every 44 seconds, an American will have an MI (AHA computation).
-
On the basis of data from the ARIC study4 of the NHLBI
This year, ≈620 000 Americans will have a new coronary attack (defined as first hospitalized MI or CHD death), and ≈295 000 will have a recurrent attack. It is estimated that an additional 150 000 silent MIs occur each year. That assumes that ≈21% of the 720 000 first and recurrent MIs are silent.5,6
The estimated annual incidence of MI is 515 000 new attacks and 205 000 recurrent attacks.
Average age at first MI is 64.9 years for men and 72.3 years for women.
-
On the basis of the NHLBI-sponsored FHS
In the NHLBI-sponsored ARIC study, in participants 35 to 84 years of age, the average age-adjusted first MI or fatal CHD rates per 1000 population were as follows: white men, 3.6; black men, 5.6; white women, 2.1; and black women, 3.8 (unpublished data from ARIC Surveillance 2005–2010, NHLBI).
Incidence rates for MI in the NHLBI-sponsored ARIC study are displayed in Charts 18-3 and 18-4, stratified by age, race, and sex. The annual age-adjusted rates per 1000 population of first MI (2005–2010) were 4.8 in black men, 3.2 in white men, 3.3 in black women, and 1.9 in white women (unpublished data from ARIC Surveillance 2005– 2010, NHLBI).
Among American Indians 65 to 74 years of age, the annual rates per 1000 population of new and recurrent MIs were 7.6 for men and 4.9 for women.7
On the basis of data from the NHDS, since the mid-1990s, the rate of hospitalization for MI and in-hospital case fatality rates have decreased.8
From 2002 to 2007, the rates of hospitalization for MI decreased among Medicare beneficiaries; however, the degree of reduction was more significant in whites than in African Americans.9
Chart 18-4.
Incidence of heart attack or fatal coronary heart disease by age, sex, and race (Atherosclerosis Risk in Communities Surveillance: 2005–2010). Source: National Heart, Lung, and Blood Institute.
Trends in Incidence
Analysis of >40 years of physician-validated AMI data in the NHLBI’s FHS found that AMI rates diagnosed by electrocardiographic criteria declined ≈50%, with a concomitant 2-fold increase in rates of AMI diagnosed by blood markers. These findings may explain the paradoxical stability of AMI rates in the United States despite concomitant improvements in CHD risk factors.10
Data from the Worcester Heart Attack Study showed that incidence rates for AMI were 277 per 100 000 person-years in 1975 and 209 per 100 000 person-years in 2005 (P=0.42 for overall trend). The incidence rate rose from 1975 to 1981, decreased from 1981 to 1988, increased from 1981 to 2001, and decreased from 2001 to 2005.11
In Olmsted County, MN, no significant change in the overall age- and sex-adjusted incidence rate for hospitalized MI was noted (186 per 100 000 person-years in 1987 and 180 per 100 000 person-years in 2006; P=0.171), but a significant decline in the age- and sex-adjusted incidence rate for hospitalized MI based on creatine kinase/creatine kinase- MB markers, to 141 per 100 000 person-years (P=0.020), was observed in 2006, which represents a 20% decrease during the study period.12
Data from Kaiser Permanente Northern California showed that the age- and sex-adjusted incidence rate of hospitalizations for MI changed from 274 per 100 000 person-years in 1999 to 208 per 100 000 person-years in 2008. Furthermore, the age- and sex-adjusted incidence rate of hospitalizations for STEMI changed from 133 per 100 000 person-years in 1999 to 50 per 100 000 person-years in 2008 (P linear trend <0.001). The trajectory of the age- and sex-adjusted incidence rate of hospitalizations for NSTEMI did not change significantly.13
From 1987 to 2008, the age- and biomarker-adjusted incidence rates of hospitalization for AMI or fatal CHD decreased by 4.9% per year (95% CI, 5.3%–4.5%) among white men, 3.9% per year (95% CI, 4.5%–3.4%) among white women, 1.8% per year (95% CI, 2.6%–1.0%) among black men, and 3.5% per year (95% CI, 4.4%–2.6%) among black women in the ARIC study.14
Predicted Risk
Ten-Year Predicted Risk
Analysis of data from NHANES III (1988–1994) and NHANES 1999 to 2002 (NCHS) showed that in adults 20 to 74 years of age, the overall distribution of 10-year risk of developing CHD changed little during this time. Among the 3 racial/ethnic groups, blacks had the highest proportion of participants in the high-risk group.15
Another analysis of NHANES data concluded that 10-year predicted risk for CHD among adults 30 to 74 years of age decreased from 10.0% during 1976 to 1980 to 7.9% during 1988 to 1994 (P<0.001) and to 7.4% during 1999 to 2004 (P <0.001).16
More recently, it was reported that the mean predicted 10-year risk for CHD among adults aged 30 to 74 years decreased from 7.2% during 1999 to 2000 to 6.5% during 2009 to 2010 (P=0.005).17 Mean predicted risk declined among men, women, whites, and adults 40 to 59, 50 to 59, and 60 to 74 years of age. Risk increased nonsignificantly among African American adults.
A survey of US family physicians, general internists, and cardiologists found that 41% of respondents reported using global CHD risk assessment at least occasionally.18
Lifetime Risk
The lifetime risk of developing CHD after 40 years of age is 49% for men and 32% for women.19
Lifetime risk for CHD varies drastically as a function of risk factor profile. With an optimal risk factor profile, lifetime risk for CHD is 3.6% for men and <1% for women; with ≥2 major risk factors, it is 37.5% for men and 18.3% for women.20
Mortality
CHD was an underlying cause of death in ≈1 of every 6 deaths in the United States in 2010.
In 2010, CHD mortality was 379 559,21 and CHD any-mention mortality was 545 259.22
In 2010, MI mortality was 122 071.21 MI any-mention mortality was 158 998 (NCHS, NHLBI tabulation).22
In 2010, the overall CHD death rate per 100 000 was 113.6.21 From 2000 to 2010, the annual death rate attributable to CHD declined 39.2% and the actual number of deaths declined 26.3% (CDC computation).21,22 CHD death rates per 100 000 were 151.9 for white males and 169.0 for black males; for white females, the rate was 83.8, and for black females, it was 104.9.21
In 2010, 73% of CHD deaths occurred out of the hospital. According to NCHS mortality data, 278 000 CHD deaths occur out of the hospital or in hospital EDs annually (NCHS, AHA tabulation).22
Approximately every 34 seconds, an American will experience a coronary event, and approximately every 1 minute 23 seconds, someone will die of one (AHA computation).
Approximately 34% of the people who experience a coronary attack in a given year will die of it, and ≈15% who experience a heart attack (MI) will die of it (AHA computation).
A study of 1275 health maintenance organization enrollees 50 to 79 years of age who had cardiac arrest showed that the incidence of out-of-hospital cardiac arrest was 6.0/1000 subject-years in subjects with any clinically recognized HD compared with 0.8/1000 subject-years in subjects without HD. Among enrollees with HD, incidence was 13.6 and 21.9 per1000 subject-years in those with prior MI and with HF, respectively.23
Approximately 80% of people who die of CHD are ≥65 years of age (NCHS; AHA computation).
The estimated average number of YLL because of an MI death is 17.2 (NCHS, NHLBI tabulation).
-
On the basis of data from the FHS of the NHLBI5
Fifty percent of men and 64% of women who die suddenly of CHD have no previous symptoms of this disease. Between 70% and 89% of sudden cardiac deaths occur in men, and the annual incidence is 3 to 4 times higher in men than in women; however, this disparity decreases with advancing age.
People who have had an MI have a sudden death rate 4 to 6 times that of the general population.
Researchers investigating variation in hospital-specific 30-day risk-stratified mortality rates for patients with AMI found teaching status, number of hospital beds, AMI volume, cardiac facilities available, urban/rural location, geographic region, hospital ownership type, and socioeconomic status profile of the patients were all significantly associated with mortality rates. However, a substantial proportion of variation in outcomes for patients with AMI between hospitals remains unexplained by measures of hospital characteristics.24
Temporal Trends in CHD Mortality
The decline in CHD mortality rates in part reflects the shift in the pattern of clinical presentations of AMI. In the past decade, there has been a marked decline in STEMI (from 133 to 50 cases per 100 000 person-years).13
-
According to data from the National Registry of Myocardial Infarction:
From 1990 to 1999, in-hospital AMI mortality declined from 11.2% to 9.4%.25
From 1990 to 2006, in-hospital AMI mortality declined from 10.4% to 6.3% (P<0.001; STEMI: 11.5% to 8.0%, P<0.001; NSTEMI: 7.1% to 5.2%, P<0.001). Approximately 37% of the decline in annual mortality for patients with NSTEMI and 21% for patients with STEMI was judged to be attributable to improvements in acute treatments.26
Mortality rate increases for every 30 minutes that elapses before a patient with ST-segment elevation is recognized and treated.25
-
Other studies also reported declining case fatality rates after MI:
In Olmsted County, MN, the age- and sex-adjusted 30-day case fatality rate decreased by 56% from 1987 to 2006.12
In Worcester, MA, the hospital case fatality rates, 30-day postadmission case fatality rates, and 1-year postdischarge case fatality rates for STEMI were 11.1%, 13.2%, and 10.6%, respectively, in 1997 and 9.7%, 11.4%, and 8.4%, respectively, in 2005. The hospital case fatality rates, 30-day postadmission case fatality rates, and 1-year postdischarge case fatality rates for NSTEMI were 12.9%, 16.0%, and 23.1%, respectively, in 1997 and 9.5%, 14.0%, and 18.7%, respectively, in 2005.27
Among enrollees of the Kaiser Permanente Northern California healthcare delivery system, the age- and sex-adjusted 30-day mortality rate for MI dropped from 10.5% in 1999 to 7.8% in 2008, and the 30-day mortality rate for NSTEMI dropped from 10.0% in 1999 to 7.6% in 2008.13
A recent analysis of Centers for Medicare & Medicaid Services data suggests that between 1995 and 2006, the 30-day mortality rate attributable to MI decreased, as did hospital variation in mortality attributable to MI.28
Data from the Nationwide Inpatient Sample database suggest that mortality attributable to MI has decreased since 1988.29
-
CHD death rates have fallen from 1968 to the present. Analysis of NHANES (NCHS) data compared CHD death rates between 1980 and 2000 to determine how much of the decline in deaths attributable to CHD over that period could be explained by the use of medical and surgical treatments versus changes in CVD risk factors (resulting from lifestyle/behavior). After 1980 and 2000 data were compared, it was estimated that ≈47% of the decrease in CHD deaths was attributable to treatments, including the following30:
Secondary preventive therapies after MI or revascularization (11%)
Initial treatments for AMI or UA (10%)
Treatments for HF (9%)
Revascularization for chronic angina (5%)
Other therapies (12%), including antihypertensive and lipid-lowering primary prevention therapies
-
It was also estimated that a similar amount of the reduction in CHD deaths, ≈44%, was attributable to changes in risk factors, including the following30:
Lower total cholesterol (24%)
Lower SBP (20%)
Lower smoking prevalence (12%)
Decreased physical inactivity (5%)
Nevertheless, these favorable improvements in risk factors were offset in part by increases in BMI and in DM prevalence, which accounted for an increased number of deaths (8% and 10%, respectively).
Between 1980 and 2002, death rates attributable to CHD among men and women ≥35 years of age fell by 52% in men and 49% in women. Among men, the death rate declined on average by 2.9% per year in the 1980s, 2.6% per year during the 1990s, and 4.4% per year from 2000 to 2002. Among women, death rates fell by 2.6%, 2.4%, and 4.4%, respectively; however, when stratified by age, among men 35 to 54 years of age, the average annual rate of death fell by 6.2%, 2.3%, and 0.5%, respectively. Among women 35 to 54 years of age, the average annual rate of death fell by 5.4% and 1.2% and then increased by 1.5%, respectively. This increase was not statistically significant; however, in even younger women (35–44 years of age), the rate of death has been increasing by an average of 1.3% annually between 1997 and 2002, which is statistically significant.31
In an analysis of 28 studies published from 1977 to 2007, significantly improved survival was described in patients with nonacute CAD treated with revascularization by CABG or PCI in conjunction with medical therapy compared with patients treated with medical therapy alone.32
Risk Factors
Risk factors for CHD act synergistically to increase CHD risk, as shown in the examples in Charts 18-6 and 18-7.
Chart 18-6.
Estimated 10-year coronary heart disease risk in adults 55 years of age according to levels of various risk factors (Framingham Heart Study). HDL-C indicates high-density lipoprotein-cholesterol. Data derived from Wilson et al.59
Chart 18-7.
Prevalence of low coronary heart disease risk, overall and by sex (National Health and Nutrition Examination Survey: 1971–2006). Low risk is defined as systolic blood pressure <120 mm Hg and diastolic blood pressure <80 mm Hg; cholesterol <200 mg/dL; body mass index <25 kg/m2; currently not smoking cigarettes; and no prior myocardial infarction or diabetes mellitus. Source: Personal communication with the National Heart, Lung, and Blood Institute, June 28, 2007.
Awareness of Warning Signs and Risk Factors for HD
Among people in 14 states and Washington, DC, participating in the 2005 BRFSS, only 27% were aware of 5 heart attack warning signs and symptoms (1, pain in jaw, neck, or back; 2, weak, lightheaded, or faint; 3, chest pain or discomfort; 4, pain or discomfort in arms or shoulder; and 5, shortness of breath) and indicated that they would first call 9-1-1 if they thought someone was having a heart attack or stroke. Significant variation in the percentage of participants who were aware of all 5 heart attack warning signs and symptoms and who would call 9-1-1 as their initial action varied by race or ethnicity (30.2% for non-Hispanic whites, 16.2% for non-Hispanic blacks and 14.3% for Hispanics), sex (30.8% for women and 22.5% for men), and educational status (33.4% for those with a college education or more and 15.7% for those with less than a high school education). In addition, significant interstate variation was also present (highest in West Virginia [35.5%] and lowest in Washington, DC [16.0%]).33
Data from the Women Veterans Cohort showed that 42% of women ≥35 years of age were concerned about HD.34
-
Women’s awareness that CVD is their leading cause of death increased from 30% in 1997 to 56% in 2012.
Depending on age, 44% to 50% identified HD/heart attack as the leading cause of death for women, a significant increase from 16% to 34% in the original 1997 survey.
The percentages of women identifying warning signs for a heart attack were as follows: pain in the chest, neck, shoulder, and arm—56%; shortness of breath—38%; chest tightness—17%; nausea—18%; and fatigue—10%.
The 5 most commonly cited HD prevention strategies in 2012 were maintaining a healthy BP (78%), seeing the doctor (78%), and increasing fiber intake, eating food with antioxidants, and maintaining healthy cholesterol levels (each 66%).
Among online survey participants, 21% responded that their doctor had talked to them about HD risk. Rates were lower among Hispanic women (12%) than whites (22%) or blacks (22%) and increased with age from 6% (25–34 years) to 33% (≥65 years).35
A 2004 national study of physician awareness and adherence to CVD prevention guidelines showed low awareness that the annual number of deaths from CVD among women exceeded that among men (fewer than 1 in 5 physicians knew this).36
Delays Between Symptom Onset and Arrival at Hospital
A recent community surveillance study in 4 US communities reported that in 2000, 49.5% of people arrived at the hospital ≥4 hours after the onset of AMI symptoms. From 1987 to 2000, the percentage of patients arriving at the hospital ≥4 hours after symptoms began did not change significantly, indicating that there had been little improvement in the speed at which patients with MI symptoms arrived at the hospital after symptom onset. Although the proportion of patients with MI who arrived at the hospital by EMS increased over this period, from 37.1% in 1987 to 44.5% in 2000, the total time between onset and hospital arrival did not change appreciably.37
System improvements in Dallas County, TX, resulted in decreases in the median time from symptom onset to balloon (catheterization) from the fourth quarter of 2010 to the first quarter of 2012.38
Data from CRUSADE and the NCDR ACTION Registry–GWTG showed a longer median time to hospital presentation in men (3 hours) than in women (2.8 hours; P<0.001). From 2002 to 2007, presentation time did not change significantly in men or women.39
Individuals with documented CHD have 5 to 7 times the risk of having a heart attack or dying as the general population. Survival rates improve after a heart attack if treatment begins within 1 hour; however, most patients are admitted to the hospital 2.5 to 3 hours after symptoms begin. More than 3500 patients with a history of CHD were asked to identify possible symptoms of heart attack. Despite their history of CHD, 44% had low knowledge levels. Among these high-risk participants, 43% underestimated their risk for a future AMI (men 47%, women 36%).40
Data from Worcester, MA, indicate that the average time from symptom onset to hospital arrival has not improved and that delays in hospital arrival are associated with less receipt of guidelines-based care. Mean and median prehospital delay times from symptom onset to arrival at the hospital were 4.1 and 2.0 hours in 1986 and 4.6 and 2.0 hours in 2005, respectively. Receipt of thrombolytic therapy and PCI within 90 minutes of hospital arrival was less likely among patients who arrived within ≥2 hours of symptom onset than among those who arrived <2 hours after onset.41
In an analysis from ARIC, low neighborhood household income (OR, 1.46; 95% CI, 1.09–1.96) and being a Medicaid recipient (OR, 1.87; 95% CI, 1.10–3.19) were associated with increased odds of having prolonged prehospital delays from symptom onset to hospital arrival for AMI compared with individuals with higher neighborhood household income and other insurance providers, respectively.42
An analysis of data from the NCDR ACTION Registry–GWTG showed that 60% of 37 634 STEMI patients used EMS to get to the hospital. Older adults, women, adults with comorbidities, and sicker patients were more likely to use EMS than their counterparts. Hospital arrival time was shorter for those who used EMS (89 minutes) than self-transport (120 minutes).43
Aftermath
Depending on their sex and clinical outcome, people who survive the acute stage of an MI have a chance of illness and death 1.5 to 15 times higher than that of the general population. Among these people, the risk of another MI, sudden death, AP, HF, and stroke—for both men and women—is substantial (FHS, NHLBI).5
-
On the basis of pooled data from the FHS, ARIC, and CHS studies of the NHLBI (1986–2007), within 1 year after a first MI:
At ≥45 years of age, 19% of men and 26% of women will die.
At 45 to 64 years of age, 5% of white men, 8% of white women, 14% of black men, and 9% of black women will die.
At ≥65 years of age, 25% of white men, 30% of white women, 25% of black men, and 30% of black women will die.
In part because women have MIs at older ages than men, they are more likely to die of MIs within a few weeks.
-
Within 5 years after a first MI:
At ≥45 years of age, 36% of men and 47% of women will die.
At 45 to 64 years of age, 11% of white men, 18% of white women, 22% of black men, and 28% of black women will die.
At ≥65 years of age, 46% of white men, 53% of white women, 54% of black men, and 58% of black women will die.
-
Of those who have a first MI, the percentage with a recurrent MI or fatal CHD within 5 years is as follows:
At 45 to 64 years of age, 15% of men and 22 of women
At ≥65 years of age, 22% of men and women
At 45 to 64 years of age, 14% of white men, 18% of white women, 22% of black men, and 28% of black women
At ≥65 years of age, 21% of white men and women, 33% of black men, and 26% of black women
-
The percentage of people with a first MI who will have HF in 5 years is as follows:
At 45 to 64 years of age, 8% of men and 18% of women
At ≥65 years of age, 20% of men and 23% of women
At 45 to 64 years of age, 7% of white men, 15% of white women, 13% of black men, and 25% of black women
At ≥65 years of age, 19% of white men, 23% of white women, 31% of black men, and 24% of black women
-
The percentage of people with a first MI who will have a stroke within 5 years is as follows:
At 45 to 64 years of age, 2% of men and 6% of women
At ≥65 years of age, 5% of men and 8% of women
At 45 to 64 years of age, 2% of white men, 4% of white women, 3% of black men, and 10% of black women
At ≥65 years of age, 5% of white men, 8% of white women, 9% of black men, and 10% of black women
-
The median survival time (in years) after a first MI is
At 55 to 64 years of age, 17.0 for men and 13.3 for women
At 65 to 74 years of age, 9.3 for men and 8.8 for women
At ≥75 years of age, 3.2 for men and 3.2 for women
A Mayo Clinic study found that cardiac rehabilitation after an MI is underused, particularly in women and the elderly. Women were 55% less likely than men to participate in cardiac rehabilitation, and older study patients were less likely to participate than younger participants. Only 32% of men and women ≥70 years of age participated in cardiac rehabilitation compared with 66% of those 60 to 69 years of age and 81% of those <60 years of age.44
Among survivors of an MI, in 2005, 34.7% of BRFSS respondents participated in outpatient cardiac rehabilitation. The prevalence of cardiac rehabilitation was higher among older age groups (≥50 years of age), among men versus women, among Hispanics, among those who were married, among those with higher education, and among those with higher levels of household income.45
A recent analysis of Medicare claims data revealed that only 13.9% of Medicare beneficiaries enroll in cardiac rehabilitation after an AMI, and only 31% enroll after CABG. Older people, women, nonwhites, and individuals with comorbidities were less likely to enroll in cardiac rehabilitation programs.46
Hospital Discharges and Ambulatory Care Visits
(See Table 18-1 and Chart 18-8.)
Chart 18-8.
Hospital discharges for coronary heart disease by sex (United States: 1970–2010). Hospital discharges include people discharged alive, dead, and “status unknown.” Source: National Hospital Discharge Survey/National Center for Health Statistics and National Heart, Lung, and Blood Institute.
From 2000 to 2010, the number of inpatient discharges from short-stay hospitals with CHD as the first-listed diagnosis decreased from 2 165 000 to 1 346 000 (NHDS, NHLBI tabulation).
In 2010, there were 11 921 000 ambulatory care visits with CHD as the first-listed diagnosis (NCHS, NAMCS, NHAMCS). There were 10 570 000 physician office visits, 587 000 ED visits, and 764 000 outpatient department visits with a primary diagnosis of CHD (NHAMCS, NHLBI tabulation). The majority of these visits (77.7%) were for coronary atherosclerosis.47
The age-adjusted hospitalization rate for MI per 100 000 people was 215 in 1979 to 1981, increased to 342 in 1985 to 1987, stabilized for the next decade, and then declined after 1996 to 242 during the period from 2003 to 2005. The rate for men exceeded that for women by almost a factor of 2. Hospitalization rates increased strongly with age.8
An analysis of data from HCUP found that 48.3% of hospitalizations for circulatory disease in 2003 occurred among women, but among patients >65 years of age, women constituted the majority. Furthermore, the percentage of hospitalized patients who were female increased from 24.1% of those 18 to 44 years of age to 63.7% of those ≥85 years of age for MI, from 31.4% of people 18 to 44 years of age to 60.7% of those ≥85 years of age for coronary atherosclerosis, and from 45.1% of those 18 to 44 years of age to 73.9% of those ≥85 years of age for nonspecific chest pain. For MI, in-hospital mortality was 9.3% among women and 6.2% among men.48
Operations and Procedures
In 2010, an estimated 954 000 inpatient PCI procedures, 397 000 inpatient bypass procedures, 1 029 000 inpatient diagnostic cardiac catheterizations, 97 000 inpatient implantable defibrillator procedures, and 370 000 pacemaker procedures were performed for inpatients in the United States (NHLBI tabulation).
Cost
(See Table 18-1.)
The estimated direct and indirect cost of heart disease in 2010 was $204.4 billion (MEPS, NHLBI tabulation).
In 2006, $11.7 billion was paid to Medicare beneficiaries for in-hospital costs when CHD was the principal diagnosis ($14 009 per discharge for AMI, $12 977 per discharge for coronary atherosclerosis, and $10 630 per discharge for other ischemic HD).42
-
Between 2013 and 2030, medical costs of CHD (real 2010$) are projected to increase by ≈100%
Indirect costs for all CVD (real 2010$) are projected to increase 52% (from $202.5 billion to $308.2 billion) between 2013 and 2030. Of these indirect costs, CHD is projected to account for ≈43% and has the largest indirect costs (AHA computation, based on methodology described by Heidenreich et al3).
Acute Coronary Syndrome
ICD-9 410, 411; ICD-10 I20.0, I21, I22.
The term acute coronary syndrome is increasingly used to describe patients who present with either AMI or UA. (UA is chest pain or discomfort that is accelerating in frequency or severity and may occur while at rest but does not result in myocardial necrosis.) The discomfort may be more severe and prolonged than typical AP, or it may be the first time a person has had AP. UA, NSTEMI, and STEMI share common pathophysiological origins related to coronary plaque progression, instability, or rupture with or without luminal thrombosis and vasospasm.
A conservative estimate for the number of discharges with ACS from hospitals in 2010 is 625 000. Of these, an estimated 363 000 are males and 262 000 are females. This estimate is derived by adding the first-listed inpatient hospital discharges for MI (595 000) to those for UA (30 000; NHDS, NHLBI).
When secondary discharge diagnoses in 2010 were included, the corresponding number of inpatient hospital discharges was 1 141 000 unique hospitalizations for ACS; 653 000 were males, and 488 000 were females. Of the total, 813 000 were for MI alone, 322 000 were for UA alone, and 6000 hospitalizations received both diagnoses (NHDS, NHLBI).
Among commercially insured adults 18 to 64 years of age, the 1-year medical costs for an ACS event during 2004 to 2005 were $34 087 for those who were treated with medical management, $52 673 for those who were treated with percutaneous intervention, and $86 914 for those who had coronary artery bypass surgery. The 1-year short-term disability costs were $6048, $9221, and $17 335, respectively, and the 1-year absenteeism costs were $9826, $9460, and $14 960, respectively.49 Another study of the same database using adults 18 to 64 years of age who had a principal inpatient diagnosis of ACS during 2003 to 2006 estimated that the incremental annual direct cost was $40 671 and the incremental short-term disability cost was $999.50
Decisions about medical and interventional treatments are based on specific findings noted when a patient presents with ACS. Such patients are classified clinically into 1 of 3 categories according to the presence or absence of ST-segment elevation on the presenting ECG and abnormal (“positive”) elevations of myocardial biomarkers, such as troponins, as follows:
STEMI
NSTEMI
UA
The percentage of ACS or MI cases with ST-segment elevation varies in different registries/databases and depends heavily on the age of patients included and the type of surveillance used. According to NRMI-4, ≈29% of patients with MI are patients with STEMI.51 The AHA GWTG project found that 32% of the patients with MI in the CAD module were patients with STEMI (personal communication from AHA GWTG staff, October 1, 2007). The GRACE study, which includes US patient populations, found that 38% of ACS patients have STEMI, whereas the EHS-ACS-II reported that ≈47% of patients with ACS have STEMI.52
In addition, the percentage of ACS or MI cases with ST-segment elevation appears to be declining. In an analysis of 46 086 hospitalizations for ACS in the Kaiser Permanente Northern California study, the percentage of MI cases with ST-segment elevation decreased from 47.0% to 22.9% between 1999 and 2008.13
Analysis of data from the GRACE multinational observational cohort study of patients with ACS found evidence of a change in practice for both pharmacological and interventional treatments in patients with either STEMI or non–ST-segment–elevation ACS. These changes have been accompanied by nonsignificant decreases in the rates of in-hospital death, cardiogenic shock, and new MI among patients with non–ST-segment–elevation ACS. The use of evidence-based therapies and PCI interventions increased in the STEMI population. This increase was matched by a statistically significant decrease in the rates of death, cardiogenic shock, and HF or pulmonary edema.53
A study of hospital process performance in 350 centers of nearly 65 000 patients enrolled in the CRUSADE National Quality Improvement Initiative found that ACC/AHA guideline– recommended treatments were adhered to in 74% of eligible instances.54 A better composite guideline adherence rate was significantly associated with decreased in-hospital mortality among all patients with ACS and those with NSTEMI.
After adjustment for clinical differences and the severity of CAD by angiogram, 30-day mortality after ACS is similar in men and women.55
Angina Pectoris
ICD-9 413; ICD-10 I20.1 to I20.9.
Prevalence
(See Table 18-2 and Chart 18-9.)
Chart 18-9.
Prevalence of angina pectoris by age and sex (National Health and Nutrition Examination Survey: 2007–2010). Angina pectoris includes people who either answered “yes” to the question of ever having angina or angina pectoris or were diagnosed with Rose Angina. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
A study of 4 national cross-sectional health examination studies found that among Americans 40 to 74 years of age, the age-adjusted prevalence of AP was higher among women than men. Increases in the prevalence of AP occurred for Mexican American men and women and African American women but were not statistically significant for the latter.56
Incidence
(See Table 18-2 and Chart 18-10.)
Only 18% of coronary attacks are preceded by long-standing AP (NHLBI computation of FHS follow-up since 1986).
The annual rates per 1000 population of new episodes of AP for nonblack men are 28.3 for those 65 to 74 years of age, 36.3 for those 75 to 84 years of age, and 33.0 for those ≥85 years of age. For nonblack women in the same age groups, the rates are 14.1, 20.0, and 22.9, respectively. For black men, the rates are 22.4, 33.8, and 39.5, and for black women, the rates are 15.3, 23.6, and 35.9, respectively (CHS, NHLBI).57
On the basis of 1987 to 2001 data from the ARIC study of the NHLBI, the annual rates per 1000 population of new episodes of AP for nonblack men are 8.5 for those 45 to 54 years of age, 11.9 for those 55 to 64 years of age, and 13.7 for those 65 to 74 years of age. For nonblack women in the same age groups, the rates are 10.6, 11.2, and 13.1, respectively. For black men, the rates are 11.8, 10.6, and 8.8, and for black women, the rates are 20.8, 19.3, and 10.0, respectively.57
Mortality
A small number of deaths resulting from CHD are coded as being attributable to AP. These are included as a portion of total deaths attributable to CHD.
Cost
For women with nonobstructive CHD enrolled in the WISE study of the NHLBI, the average lifetime cost estimate was ≈$770 000 and ranged from $1.0 to $1.1 million for women with 1- to 3-vessel CHD.58
- 1.Blackwell D, Lucas J, Clarke T. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. National Center for Health Statistics. Vital Health Stat 10. In press. [PubMed] [Google Scholar]
- 2.Behavioral Risk Factor Surveillance System: prevalence and trends data. [Accessed July 5, 2011];Centers for Disease Control and Prevention Web site. http://apps.nccd.cdc.gov/brfss/index.asp.
- 3.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ on behalf of the American Heart Association Advocacy Coordinating Committee; Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Cardiovascular Nursing; Council on the Kidney in Cardiovascular Disease; Council on Cardiovascular Surgery and Anesthesia, and Interdisciplinary Council on Quality of Care and Outcomes Research. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 4.Community surveillance event rates. [Accessed August 30, 2012];Atherosclerosis Risk in Communities (ARIC) Study Website. http://www.cscc.unc.edu/aric/displaydata.php?pg_id=37.
- 5.Thom TJ, Kannel WB, Silbershatz H, D’Agostino RB., Sr . Cardiovascular diseases in the United States and prevention approaches. In: Fuster V, Alexander RW, O’Rourke RA, Roberts R, King SB 3rd, Wellens HJJ, editors. Hurst’s the Heart. 10. New York, NY: McGraw-Hill; 2001. pp. 3–18. [Google Scholar]
- 6.Boland LL, Folsom AR, Sorlie PD, Taylor HA, Rosamond WD, Chambless LE, Cooper LS. Occurrence of unrecognized myocardial infarction in subjects aged 45 to 65 years (the ARIC study) Am J Cardiol. 2002;90:927–931. doi: 10.1016/s0002-9149(02)02655-3. [DOI] [PubMed] [Google Scholar]
- 7.Ali T, Jarvis B, O’Leary M. Strong Heart Study Data Book: A Report to American Indian Communities. Rockville, MD: National Institutes of Health, National Heart, Lung, and Blood Institute; 2001. NIH publication No. 01-3285. [Google Scholar]
- 8.Fang J, Alderman MH, Keenan NL, Ayala C. Acute myocardial infarction hospitalization in the United States, 1979 to 2005. Am J Med. 2010;123:259–266. doi: 10.1016/j.amjmed.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 9.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 10.Parikh NI, Gona P, Larson MG, Fox CS, Benjamin EJ, Murabito JM, O’Donnell CJ, Vasan RS, Levy D. Long-term trends in myocardial infarction incidence and case fatality in the National Heart, Lung, and Blood Institute’s Framingham Heart study. Circulation. 2009;119:1203–1210. doi: 10.1161/CIRCULATIONAHA.108.825364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30-year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roger VL, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, Bell MR, Kors J, Yawn BP, Jacobsen SJ. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010;121:863–869. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 14.Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, Wagenknecht L, Ni H, Folsom AR. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012;125:1848–1857. doi: 10.1161/CIRCULATIONAHA.111.047480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ajani UA, Ford ES. Has the risk for coronary heart disease changed among U.S adults? J Am Coll Cardiol. 2006;48:1177–1182. doi: 10.1016/j.jacc.2006.05.055. [DOI] [PubMed] [Google Scholar]
- 16.Lopez-Jimenez F, Batsis JA, Roger VL, Brekke L, Ting HH, Somers VK. Trends in 10-year predicted risk of cardiovascular disease in the United States, 1976 to 2004. Circ Cardiovasc Qual Outcomes. 2009;2:443–450. doi: 10.1161/CIRCOUTCOMES.108.847202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ford ES. Trends in predicted 10-year risk of coronary heart disease and cardiovascular disease among U.S. adults from 1999 to 2010. J Am Coll Cardiol. 2013;61:2249–2252. doi: 10.1016/j.jacc.2013.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shillinglaw B, Viera AJ, Edwards T, Simpson R, Sheridan SL. Use of global coronary heart disease risk assessment in practice: a cross-sectional survey of a sample of U.S. physicians. BMC Health Serv Res. 2012;12:20. doi: 10.1186/1472-6963-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–92. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]
- 20.Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, Greenland P, Van Horn L, Tracy RP, Lloyd-Jones DM. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–329. doi: 10.1056/NEJMoa1012848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy SL, Xu JQ, Kochanek KD. National Vital Statistics Report. 4. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2013. Deaths: final data for 2010. [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1999–2010. Series 20 No. 2P. [Accessed July 21, 2013];CDC WONDER Online Database [database online] Released January 2013. http://wonder.cdc.gov/cmf-icd10.html.
- 23.Rea TD, Pearce RM, Raghunathan TE, Lemaitre RN, Sotoodehnia N, Jouven X, Siscovick DS. Incidence of out-of-hospital cardiac arrest. Am J Cardiol. 2004;93:1455–1460. doi: 10.1016/j.amjcard.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 24.Bradley EH, Herrin J, Curry L, Cherlin EJ, Wang Y, Webster TR, Drye EE, Normand SL, Krumholz HM. Variation in hospital mortality rates for patients with acute myocardial infarction. Am J Cardiol. 2010;106:1108–1112. doi: 10.1016/j.amjcard.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 25.Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid B, Shoultz DA, Frederick PD, Every N. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;36:2056–2063. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 26.Peterson ED, Shah BR, Parsons L, Pollack CV, Jr, French WJ, Canto JG, Gibson CM, Rogers WJ. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1045–1055. doi: 10.1016/j.ahj.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 27.McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124:40–47. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krumholz HM, Wang Y, Chen J, Drye EE, Spertus JA, Ross JS, Curtis JP, Nallamothu BK, Lichtman JH, Havranek EP, Masoudi FA, Radford MJ, Han LF, Rapp MT, Straube BM, Normand SL. Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995–2006. JAMA. 2009;302:767–773. doi: 10.1001/jama.2009.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Movahed MR, John J, Hashemzadeh M, Jamal MM, Hashemzadeh M. Trends in the age adjusted mortality from acute ST segment elevation myocardial infarction in the United States (1988–2004) based on race, gender, infarct location and comorbidities. Am J Cardiol. 2009;104:1030–1034. doi: 10.1016/j.amjcard.2009.05.051. [DOI] [PubMed] [Google Scholar]
- 30.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 31.Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50:2128–2132. doi: 10.1016/j.jacc.2007.05.056. [DOI] [PubMed] [Google Scholar]
- 32.Jeremias A, Kaul S, Rosengart TK, Gruberg L, Brown DL. The impact of revascularization on mortality in patients with nonacute coronary artery disease. Am J Med. 2009;122:152–161. doi: 10.1016/j.amjmed.2008.07.027. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC) Disparities in adult awareness of heart attack warning signs and symptoms: 14 states, 2005. MMWR Morb Mortal Wkly Rep. 2008;57:175–179. [PubMed] [Google Scholar]
- 34.Biswas MS, Calhoun PS, Bosworth HB, Bastian LA. Are women worrying about heart disease? Womens Health Issues. 2002;12:204–211. doi: 10.1016/s1049-3867(02)00136-6. [DOI] [PubMed] [Google Scholar]
- 35.Mosca L, Hammond G, Mochari-Greenberger H, Towfighi A, Albert MA on behalf of the American Heart Association Cardiovascular Disease and Stroke in Women and Special Populations Committee of the Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Cardiovascular Nursing, Council on High Blood Pressure Research, and Council on Nutrition, Physical Activity and Metabolism. Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation. 2013;127:1254–1263. e1–e29. doi: 10.1161/CIR.0b013e318287cf2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, Fabunmi RP, Kwan J, Mills T, Simpson SL. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111:499–510. doi: 10.1161/01.CIR.0000154568.43333.82. [DOI] [PubMed] [Google Scholar]
- 37.McGinn AP, Rosamond WD, Goff DC, Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987–2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 38.DelliFraine J, Langabeer J, 2nd, Segrest W, Fowler R, King R, Moyer P, Henry TD, Koenig W, Warner J, Stuart L, Griffin R, Fathiamini S, Emert J, Roettig ML, Jollis J. Developing an ST-elevation myocardial infarction system of care in Dallas County. Am Heart J. 2013;165:926–931. doi: 10.1016/j.ahj.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 39.Diercks DB, Owen KP, Kontos MC, Blomkalns A, Chen AY, Miller C, Wiviott S, Peterson ED. Gender differences in time to presentation for myocardial infarction before and after a national women’s cardiovascular awareness campaign: a temporal analysis from the Can Rapid Risk Stratification of Unstable Angina Patients Suppress ADverse Outcomes with Early Implementation (CRUSADE) and the National Cardiovascular Data Registry Acute Coronary Treatment and Intervention Outcomes Network-Get with the Guidelines (NCDR ACTION Registry-GWTG) Am Heart J. 2010;160:80–87. e3. doi: 10.1016/j.ahj.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 40.Dracup K, McKinley S, Doering LV, Riegel B, Meischke H, Moser DK, Pelter M, Carlson B, Aitken L, Marshall A, Cross R, Paul SM. Acute coronary syndrome: what do patients know? Arch Intern Med. 2008;168:1049–1054. doi: 10.1001/archinte.168.10.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saczynski JS, Yarzebski J, Lessard D, Spencer FA, Gurwitz JH, Gore JM, Goldberg RJ. Trends in prehospital delay in patients with acute myocardial infarction (from the Worcester Heart Attack Study) Am J Cardiol. 2008;102:1589–1594. doi: 10.1016/j.amjcard.2008.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Foraker RE, Rose KM, McGinn AP, Suchindran CM, Goff DC, Jr, Whitsel EA, Wood JL, Rosamond WD. Neighborhood income, health insurance, and prehospital delay for myocardial infarction: the atherosclerosis risk in communities study. Arch Intern Med. 2008;168:1874–1879. doi: 10.1001/archinte.168.17.1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mathews R, Peterson ED, Li S, Roe MT, Glickman SW, Wiviott SD, Saucedo JF, Antman EM, Jacobs AK, Wang TY. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction: findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get With The Guidelines. Circulation. 2011;124:154–163. doi: 10.1161/CIRCULATIONAHA.110.002345. [DOI] [PubMed] [Google Scholar]
- 44.Witt BJ, Jacobsen SJ, Weston SA, Killian JM, Meverden RA, Allison TG, Reeder GS, Roger VL. Cardiac rehabilitation after myocardial infarction in the community. J Am Coll Cardiol. 2004;44:988–996. doi: 10.1016/j.jacc.2004.05.062. [DOI] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention (CDC) Receipt of outpatient cardiac rehabilitation among heart attack survivors: United States, 2005. MMWR Morb Mortal Wkly Rep. 2008;57:89–94. [PubMed] [Google Scholar]
- 46.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention, National Center for Health Statistics. 2010 National Ambulatory Medical Care Survey and 2010 National Hospital Ambulatory Medical Care Survey. [Accessed July 17, 2013];Ambulatory health care data: questionnaires, datasets, and related documentation. For methodology, see National Center for Health Statistics, Public Use Data File Documentation: 2010 National Ambulatory Medical Care Survey and Public Use Data File Documentation: 2010 National Hospital Ambulatory Medical Care Survey. http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
- 48.Elixhauser A, Jiang H. Hospitalizations for Women With Circulatory Disease, 2003. Rockville, MD: Agency for Healthcare Research and Quality; May, 2006. [Accessed August 3, 2011]. HCUP Statistical Brief 5. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb5.pdf. [PubMed] [Google Scholar]
- 49.Zhao Z, Winget M. Economic burden of illness of acute coronary syndromes: medical and productivity costs. BMC Health Serv Res. 2011;11:35. doi: 10.1186/1472-6963-11-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Johnston SS, Curkendall S, Makenbaeva D, Mozaffari E, Goetzel R, Burton W, Maclean R. The direct and indirect cost burden of acute coronary syndrome. J Occup Environ Med. 2011;53:2–7. doi: 10.1097/JOM.0b013e31820290f4. [DOI] [PubMed] [Google Scholar]
- 51.Roe MT, Parsons LS, Pollack CV, Jr, Canto JG, Barron HV, Every NR, Rogers WJ, Peterson ED National Registry of Myocardial Infarction Investigators. Quality of care by classification of myocardial infarction: treatment patterns for ST-segment elevation vs non-ST-segment elevation myocardial infarction. Arch Intern Med. 2005;165:1630–1636. doi: 10.1001/archinte.165.14.1630. [DOI] [PubMed] [Google Scholar]
- 52.Mandelzweig L, Battler A, Boyko V, Bueno H, Danchin N, Filippatos G, Gitt A, Hasdai D, Hasin Y, Marrugat J, Van de Werf F, Wallentin L, Behar S Euro Heart Survey Investigators. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27:2285–2293. doi: 10.1093/eurheartj/ehl196. [DOI] [PubMed] [Google Scholar]
- 53.Fox KA, Steg PG, Eagle KA, Goodman SG, Anderson FA, Jr, Granger CB, Flather MD, Budaj A, Quill A, Gore JM GRACE Investigators. Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA. 2007;297:1892–1900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]
- 54.Peterson ED, Roe MT, Mulgund J, DeLong ER, Lytle BL, Brindis RG, Smith SC, Jr, Pollack CV, Jr, Newby LK, Harrington RA, Gibler WB, Ohman EM. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006;295:1912–1920. doi: 10.1001/jama.295.16.1912. [DOI] [PubMed] [Google Scholar]
- 55.Berger JS, Elliott L, Gallup D, Roe M, Granger CB, Armstrong PW, Simes RJ, White HD, Van de Werf F, Topol EJ, Hochman JS, Newby LK, Harrington RA, Califf RM, Becker RC, Douglas PS. Sex differences in mortality following acute coronary syndromes. JAMA. 2009;302:874–882. doi: 10.1001/jama.2009.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ford ES, Giles WH. Changes in prevalence of nonfatal coronary heart disease in the United States from 1971–1994. Ethn Dis. 2003;13:85–93. [PubMed] [Google Scholar]
- 57.Incidence and Prevalence: 2006 Chart Book on Cardiovascular and Lung Diseases. Bethesda, MD: National Heart, Lung, and Blood Institute; 2006. [Google Scholar]
- 58.Shaw LJ, Merz CN, Pepine CJ, Reis SE, Bittner V, Kip KE, Kelsey SF, Olson M, Johnson BD, Mankad S, Sharaf BL, Rogers WJ, Pohost GM, Sopko G Women’s Ischemia Syndrome Evaluation (WISE) Investigators. The economic burden of angina in women with suspected ischemic heart disease: results from the National Institutes of Health–National Heart, Lung, and Blood Institute–sponsored Women’s Ischemia Syndrome Evaluation. Circulation. 2006;114:894–904. doi: 10.1161/CIRCULATIONAHA.105.609990. [DOI] [PubMed] [Google Scholar]
- 59.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
19. Cardiomyopathy and Heart Failure
See Table 19-1 and Charts 19-1 through 19-3.
Table 19-1.
Heart Failure
| Population Group | Prevalence, 2010, Age ≥20 y | Incidence (New Cases), Age ≥45 y | Mortality, 2010, All Ages* | Hospital Discharges, 2010, All Ages | Cost, 2012† |
|---|---|---|---|---|---|
| Both sexes | 5 100 000 (2.1%) | 825 000 | 57 757 | 1 023 000 | 30.7 billion |
| Males | 2 700 000 (2.5%) | 395 000 | 24 385 (42.2%)‡ | 501 000 | … |
| Females | 2 400 000 (1.8%) | 430 000 | 33 372 (57.8%)‡ | 522 000 | … |
| NH white males | 2.2% | 350 000 | 21 540 | … | … |
| NH white females | 1.7% | 375 000 | 29 750 | … | … |
| NH black males | 4.1% | 45 000 | 2444 | … | … |
| NH black females | 3.0% | 55 000 | 3084 | … | … |
| Mexican American males | 1.9% | … | … | … | … |
| Mexican American females | 1.1% | … | … | … | … |
| Asian or Pacific Islander | … | … | 714 | … | … |
| American Indian or Alaska Native | … | … | 225 | … | … |
Heart failure includes people who answered “yes” to the question of ever having congestive heart failure.
Ellipses (…) indicate data not available; and NH, non-Hispanic.
Mortality data for the white, black, Asian or Pacific Islander, and American Indian or Alaska Native populations include deaths among people of Hispanic and non-Hispanic origin. Numbers of deaths for the American Indian or Alaska Native and Asian or Pacific Islander populations are known to be underestimated.
Cost data are from Heidenreich et al.9
These percentages represent the portion of total mortality attributable to heart failure that is for males vs females.
Sources: Prevalence: National Health and Nutrition Examination Survey 2007 to 2010 (National Center for Health Statistics) and National Heart, Lung, and Blood Institute. Percentages are age adjusted for Americans ≥20 y of age. Age-specific percentages are extrapolated to the 2010 US population estimates. These data are based on self-reports. Incidence: Atherosclerosis Risk in Communities Study Community Surveillance, 2005 to 2010 from National Heart, Lung, and Blood Institute. Mortality: Centers for Disease Control and Prevention/National Center for Health Statistics, 2010 Mortality Multiple Cause-of-Death–United States, version dated May 29, 2013.
Chart 19-1.
Prevalence of heart failure by sex and age (National Health and Nutrition Examination Survey: 2007–2010). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 19-3.
Hospital discharges for heart failure by sex (United States: 1980–2010). Note: Hospital discharges include people discharged alive, dead, and status unknown. Source: National Hospital Discharge Survey/National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Abbreviations Used in Chapter 19
| ABC | Health Aging, and Body Composition Study |
| ARIC | Atherosclerosis Risk in Communities Study |
| BMI | body mass index |
| BP | blood pressure |
| CAD | coronary artery disease |
| CARDIA | Coronary Artery Risk Development in Young Adults Study |
| CHS | Cardiovascular Health Study |
| CI | confidence interval |
| CRP | C-reactive protein |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| ED | emergency department |
| EF | ejection fraction |
| FHS | Framingham Heart Study |
| HbA1c | hemoglobin A1c (glycosylated hemoglobin) |
| HBP | high blood pressure |
| HCM | hypertrophic cardiomyopathy |
| HF | heart failure |
| HR | hazard ratio |
| ICD-9 | International Classification of Diseases, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| MI | myocardial infarction |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHAMCS | National Hospital Ambulatory Medical Care Survey |
| NHANES | National Health and Nutrition Examination Survey |
| NHDS | National Hospital Discharge Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| PAR | population attributable risk |
Cardiomyopathy
ICD-9 425; ICD-10 I42.
Mortality—23 712. Any-mention mortality—46 821. Hospital discharges—34 000.
-
Since 1996, the NHLBI-sponsored Pediatric Cardiomyopathy Registry has collected data on all children with newly diagnosed cardiomyopathy in New England and the Central Southwest (Texas, Oklahoma, and Arkansas).1
The overall incidence of cardiomyopathy is 1.13 cases per 100 000 among children <18 years of age.
Among children <1 year of age, the incidence is 8.34, and among children 1 to 18 years of age, it is 0.70 per 100 000.
The annual incidence is lower in white than in black children, higher in boys than in girls, and higher in New England (1.44 per 100 000) than in the Central Southwest (0.98 per 100 000).
HCM is the most common inherited heart defect, occurring in 1 of 500 individuals. In the United States, ≈500 000 people have HCM, yet most are unaware of it.2 See Chapter 16, Disorders of Heart Rhythm, for statistics regarding sudden death in HCM.
In a recent report of the Pediatric Cardiomyopathy Registry, the overall annual incidence of HCM in children was 4.7 per 1 million children. There was a higher incidence in the New England than in the Central Southwest region, in boys than in girls, and in children diagnosed at <1 year of age than in older children.3
Dilated cardiomyopathy is the most common form of cardiomyopathy. The Pediatric Cardiomyopathy Registry recently reported an annual incidence of dilated cardiomyopathy in children <18 years of age of 0.57 per 100 000 overall. The annual incidence was higher in boys than in girls (0.66 versus 0.47 cases per 100 000), in blacks than in whites (0.98 versus 0.46 cases per 100 000), and in infants (<1 year of age) than in children (4.40 versus 0.34 cases per 100 000). The majority of children (66%) had idiopathic disease. The most common known causes were myocarditis (46%) and neuromuscular disease (26%).4
Risk factors for death and transplantation in children varied by cause of dilated cardiomyopathy. For idiopathic dilated cardiomyopathy, increased left ventricular end-diastolic dimension was associated with increased transplantation risk but not mortality. Short stature was significantly related to death but not transplantation.5
The 5-year incidence rate of sudden cardiac death among children with dilated cardiomyopathy is 3%.6
Tachycardia-induced cardiomyopathy develops slowly and appears reversible, but recurrent tachycardia causes rapid decline in left ventricular function and development of HF. Sudden death is possible.7
Data from Kaiser Permanente indicate that the incidence of peripartum cardiomyopathy is 4.84 per 10 000 live births (95% CI, 3.98–5.83), and peripartum cardiomyopathy is associated with higher maternal and neonatal death rates and worse neonatal outcomes.8
Heart Failure
ICD-9 428; ICD-10 I50.
Prevalence
(See Table 19-1 and Chart 19-1.)
On the basis of data from NHANES 2007 to 2010, an estimated 5.1 million Americans ≥20 years of age have HF (NHLBI tabulation).
Projections show that the prevalence of HF will increase 46% from 2012 to 2030, resulting in >8 million people ≥18 years of age with HF.9
Incidence
(See Table 19-1 and Chart 19-2.)
Chart 19-2.
First acute decompensated heart failure annual event rates per 1000 (from ARIC Community Surveillance 2005–2010). Source: National Heart, Lung, and Blood Institute.
-
On the basis of data from the community surveillance component of the ARIC study of the NHLBI:
There are 825 000 new HF cases annually.
At ages <75 years, HF incidence is higher in blacks than whites.
-
Data from the NHLBI-sponsored FHS10 indicate the following:
HF incidence approaches 10 per 1000 population after 65 years of age.
Seventy-five percent of HF cases have antecedent hypertension.
At 40 years of age, the lifetime risk of developing HF for both men and women is 1 in 5. At 80 years of age, remaining lifetime risk for development of new HF remains at 20% for men and women, even in the face of a much shorter life expectancy.
At 40 years of age, the lifetime risk of HF occurring without antecedent MI is 1 in 9 for men and 1 in 6 for women.
The lifetime risk for people with BP >160/90 mm Hg is double that of those with BP <140/90 mm Hg.
The annual rates per 1000 population of new HF events for white men are 15.2 for those 65 to 74 years of age, 31.7 for those 75 to 84 years of age, and 65.2 for those ≥85 years of age. For white women in the same age groups, the rates are 8.2, 19.8, and 45.6, respectively. For black men, the rates are 16.9, 25.5, and 50.6 (unreliable estimate), and for black women, the estimated rates are 14.2, 25.5, and 44.0 (unreliable estimate), respectively (CHS, NHLBI).11
In MESA, African Americans had the highest risk of developing HF, followed by Hispanic, white, and Chinese Americans (4.6, 3.5, 2.4, and 1.0 per 1000 person-years, respectively). This higher risk reflected differences in the prevalence of hypertension, DM, and socioeconomic status. African Americans had the highest proportion of incident HF not preceded by clinical MI (75%).12
In Olmsted County, MN, the incidence of HF did not decline between 1979 and 2000.13
In the NHLBI’s ARIC study, the age-adjusted incidence rate per 1000 person-years was 3.4 for white women, less than for all other groups, that is, white men (6.0), black women (8.1), and black men (9.1). The 30-day, 1-year, and 5-year case fatality rates after hospitalization for HF were 10.4%, 22%, and 42.3%, respectively. Blacks had a greater 5-year case fatality rate than whites (P<0.05). HF incidence rates in black women were more similar to those of men than of white women. The greater HF incidence in blacks than in whites is explained largely by blacks’ greater levels of atherosclerotic risk factors.14
Data from Kaiser Permanente indicated an increase in the incidence of HF among the elderly, with the effect being greater in men.15
Data from hospitals in Worcester, MA, indicate that during 2000, the incidence and attack rates for HF were 219 per 100 000 and 897 per 100 000, respectively. HF was more frequent in women and the elderly. The hospital fatality rate was 5.1%.16
In the CARDIA study, HF before 50 years of age was more common among blacks than whites. Hypertension, obesity, and systolic dysfunction are important risk factors that may be targets for prevention.17
The lifetime risks of HF were assessed in a diverse large group of 39 578 participants in several cohorts (Chicago Heart Association Detection Project in Industry, ARIC, and CHS). At age 45 years, lifetime risks for HF through age 75 or 95 years were 30% to 42% in white men, 20% to 29% in black men, 32% to 39% in white women, and 24% to 46% in black women. HBP and higher BMI at all ages in both blacks and whites led to higher lifetime risks.18
Mortality
(See Table 19-1.)
In 2010, HF any-mention mortality was 279 098 (126 776 males and 152 322 females). HF was the underlying cause in 57 757 of those deaths in 2010.19 Table 19-1 shows the numbers of these deaths that are coded for HF as the underlying cause.
The 2010 overall any-mention death rate for HF was 84.0. Any-mention death rates were 99.9 for white males, 101.7 for black males, 74.1 for white females, and 79.1 for black females.19
One in 9 deaths has HF mentioned on the death certificate (NCHS, NHLBI).
The number of any-mention deaths attributable to HF was approximately as high in 1995 (287 000) as it was in 2010 (279 000; NCHS, NHLBI).20
Survival after HF diagnosis has improved over time, as shown by data from the FHS21 and the Olmsted County Study.13 However, the death rate remains high: ≈50% of people diagnosed with HF will die within 5 years.13,19
In the elderly, data from Kaiser Permanente indicate that survival after the onset of HF has also improved.15
In the CHS, depression and amino-terminal pro-B-type natriuretic peptide were independent risk factors for CVD-related and all-cause mortality.22
Among Medicare beneficiaries, the overall 1-year mortality rate declined slightly over the past decade but remains high.23 Changes were uneven across states.
Risk Factors
In the NHLBI-sponsored FHS, B-type natriuretic peptide, urinary albumin-to-creatinine ratio, elevated serum γ-glutamyl transferase, and higher levels of hematocrit were identified as risk factors for HF.24–26
In the Framingham Offspring Study, among 2739 participants, increased circulating concentrations of resistin were associated with incident HF independent of prevalent coronary disease, obesity, insulin resistance, and inflammation.27
Among 20 900 male physicians in the Physicians Health Study, the lifetime risk of HF was higher in men with hypertension; healthy lifestyle factors (normal weight, not smoking, regular exercise, moderate alcohol intake, consumption of breakfast cereals, and consumption of fruits and vegetables) were related to lower risk of HF.28 Adiponectin was also associated with risk of HF (J-shaped relationship).29
Among 2934 participants in the ABC study, the incidence of HF was 13.6 per 1000 person-years. Men and black participants were more likely to develop HF. Coronary disease (PAR 23.9% for white participants, 29.5% for black participants) and uncontrolled BP (PAR 21.3% for white participants, 30.1% for black participants) had the highest PARs in both races. There was a higher proportion of HF attributable to modifiable risk factors in black than in white participants (67.8% versus 48.9%).30 Inflammatory markers (interleukin-6 and tumor necrosis factor-α), serum albumin levels, and cigarette smoking exposure were also associated with HF risk.31–33
In the CHS, baseline cardiac troponin and changes in cardiac troponin levels measured by a sensitive assay were significantly associated with incident HF.34 Circulating individual and total omega-3 fatty acid concentrations were associated with lower incidence of HF.35
In the ARIC study, white blood cell count, CRP, albuminuria, HbA1c among individuals without DM, cardiac troponin measured with a sensitive assay, ventricular premature complexes, and socioeconomic position over the life course were all identified as risk factors for HF.36–41
In the MESA study, plasma N-terminal pro-B-type natriuretic peptide provided incremental prognostic information beyond the traditional risk factors and the magnetic resonance imaging–determined left ventricular mass index for incident symptomatic HF.42
Left Ventricular Function
-
Data from Olmsted County, MN, indicate the following:
Among asymptomatic individuals, the prevalence of left ventricular diastolic dysfunction was 21% for mild diastolic dysfunction and 7% for moderate or severe diastolic dysfunction. The prevalence of systolic dysfunction was 6%. The presence of any left ventricular dysfunction (systolic or diastolic) was associated with an increased risk of developing overt HF, and diastolic dysfunction was predictive of all-cause death.43 After 4 years of follow-up, the prevalence of diastolic dysfunction increased to 39.2%. Diastolic dysfunction was associated with development of HF during 6 years of subsequent follow-up after adjustment for age, hypertension, DM, and CAD (HR, 1 .81; 95% CI, 1.01–3.48).44
Among individuals with symptomatic HF, the prevalence of left ventricular diastolic dysfunction was 6% for mild diastolic dysfunction and 75% for moderate or severe diastolic dysfunction.45 The proportion of people with HF and preserved EF increased over time. Survival improved over time among individuals with reduced EF but not among those with preserved EF.46
Hospital Discharges/Ambulatory Care Visits
(See Table 19-1 and Chart 19-3.)
Hospital discharges for HF were essentially unchanged from 2000 to 2010, with first-listed discharges of 1 008 000 and 1 023 000, respectively (NHDS, NHLBI tabulation).47
In 2010, there were 1 801 000 physician office visits with a primary diagnosis of HF.47 In 2010, there were 676 000 ED visits and 236 000 outpatient department visits for HF (NHAMCS, NHLBI tabulation).48
Among 1077 patients with HF in Olmsted County, MN, hospitalizations were common after HF diagnosis, with 83% patients hospitalized at least once and 43% hospitalized at least 4 times. More than one half of all hospitalizations were related to noncardiovascular causes.49
Among Medicare beneficiaries, the overall HF hospitalization rate declined substantially from 1998 to 2008 but at a lower rate for black men.23 Changes were uneven across states.
Cost
In 2012, total cost for HF was estimated to be $30.7 million. Of this total, 68% was attributable to direct medical costs.9
Projections show that by 2030, the total cost of HF will increase almost 127% to $69.7 billion from 2012. This equals ≈$244 for every US adult.9
- 1.Lipshultz SE, Sleeper LA, Towbin JA, Lowe AM, Orav EJ, Cox GF, Lurie PR, McCoy KL, McDonald MA, Messere JE, Colan SD. The incidence of pediatric cardiomyopathy in two regions of the United States. N Engl J Med. 2003;348:1647–1655. doi: 10.1056/NEJMoa021715. [DOI] [PubMed] [Google Scholar]
- 2.Maron BJ, McKenna WJ, Danielson GK, Kappenberger LJ, Kuhn HJ, Seidman CE, Shah PM, Spencer WH, 3rd, Spirito P, Ten Cate FJ, Wigle ED Task Force on Clinical Expert Consensus Documents, American College of Cardiology, Committee for Practice Guidelines, European Society of Cardiology. American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines. J Am Coll Cardiol. 2003;42:1687–1713. doi: 10.1016/s0735-1097(03)00941-0. [DOI] [PubMed] [Google Scholar]
- 3.Colan SD, Lipshultz SE, Lowe AM, Sleeper LA, Messere J, Cox GF, Lurie PR, Orav EJ, Towbin JA. Epidemiology and cause-specific outcome of hypertrophic cardiomyopathy in children: findings from the Pediatric Cardiomyopathy Registry. Circulation. 2007;115:773–781. doi: 10.1161/CIRCULATIONAHA.106.621185. [DOI] [PubMed] [Google Scholar]
- 4.Towbin JA, Lowe AM, Colan SD, Sleeper LA, Orav EJ, Clunie S, Messere J, Cox GF, Lurie PR, Hsu D, Canter C, Wilkinson JD, Lipshultz SE. Incidence, causes, and outcomes of dilated cardiomyopathy in children. JAMA. 2006;296:1867–1876. doi: 10.1001/jama.296.15.1867. [DOI] [PubMed] [Google Scholar]
- 5.Alvarez JA, Orav EJ, Wilkinson JD, Fleming LE, Lee DJ, Sleeper LA, Rusconi PG, Colan SD, Hsu DT, Canter CE, Webber SA, Cox GF, Jefferies JL, Towbin JA, Lipshultz SE Pediatric Cardiomyopathy Registry Investigators. Competing risks for death and cardiac transplantation in children with dilated cardiomyopathy: results from the Pediatric Cardiomyopathy Registry. Circulation. 2011;124:814–823. doi: 10.1161/CIRCULATIONAHA.110.973826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pahl E, Sleeper LA, Canter CE, Hsu DT, Lu M, Webber SA, Colan SD, Kantor PF, Everitt MD, Towbin JA, Jefferies JL, Kaufman BD, Wilkinson JD, Lipshultz SE Pediatric Cardiomyopathy Registry Investigators. Incidence of and risk factors for sudden cardiac death in children with dilated cardiomyopathy: a report from the Pediatric Cardiomyopathy Registry. J Am Coll Cardiol. 2012;59:607–615. doi: 10.1016/j.jacc.2011.10.878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nerheim P, Birger-Botkin S, Piracha L, Olshansky B. Heart failure and sudden death in patients with tachycardia-induced cardiomyopathy and recurrent tachycardia. Circulation. 2004;110:247–252. doi: 10.1161/01.CIR.0000135472.28234.CC. [DOI] [PubMed] [Google Scholar]
- 8.Gunderson EP, Croen LA, Chiang V, Yoshida CK, Walton D, Go AS. Epidemiology of peripartum cardiomyopathy: incidence, predictors, and outcomes. Obstet Gynecol. 2011;118:583–591. doi: 10.1097/AOG.0b013e318229e6de. [DOI] [PubMed] [Google Scholar]
- 9.Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Piña IL, Trogdon JG on behalf of the American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D’Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ, Levy D Framingham Heart Study. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068–3072. doi: 10.1161/01.cir.0000039105.49749.6f. [DOI] [PubMed] [Google Scholar]
- 11.Incidence and Prevalence: 2006 Chart Book on Cardiovascular and Lung Diseases. Bethesda, MD: National Heart, Lung, and Blood Institute; 2006. [Google Scholar]
- 12.Bahrami H, Kronmal R, Bluemke DA, Olson J, Shea S, Liu K, Burke GL, Lima JA. Differences in the incidence of congestive heart failure by ethnicity: the Multi-Ethnic Study of Atherosclerosis. Arch Intern Med. 2008;168:2138–2145. doi: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, Jacobsen SJ. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292:344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 14.Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study) Am J Cardiol. 2008;101:1016–1022. doi: 10.1016/j.amjcard.2007.11.061. [DOI] [PubMed] [Google Scholar]
- 15.Barker WH, Mullooly JP, Getchell W. Changing incidence and survival for heart failure in a well-defined older population, 1970–1974 and 1990–1994. Circulation. 2006;113:799–805. doi: 10.1161/CIRCULATIONAHA.104.492033. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg RJ, Spencer FA, Farmer C, Meyer TE, Pezzella S. Incidence and hospital death rates associated with heart failure: a community-wide perspective. Am J Med. 2005;118:728–734. doi: 10.1016/j.amjmed.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 17.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huffman MD, Berry JD, Ning H, Dyer AR, Garside DB, Cai X, Daviglus ML, Lloyd-Jones DM. Lifetime risk for heart failure among white and black Americans: cardiovascular lifetime risk pooling project. J Am Coll Cardiol. 2013;61:1510–1517. doi: 10.1016/j.jacc.2013.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murphy SL, Xu JQ, Kochanek KD. National Vital Statistics Report. 4. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2013. Deaths: final data for 2010. [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention, National Center for Health Statistics. CDC WONDER Online Database [database online] Atlanta, GA: Centers for Disease Control and Prevention; [Accessed July 18, 2012]. Compressed mortality file: underlying cause of death. Released January 2013. http://wonder.cdc.gov/mortSQl.html. [Google Scholar]
- 21.Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, Murabito JM, Vasan RS. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347:1397–1402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 22.van den Broek KC, Defilippi CR, Christenson RH, Seliger SL, Gottdiener JS, Kop WJ. Predictive value of depressive symptoms and B-type natriuretic peptide for new-onset heart failure and mortality. Am J Cardiol. 2011;107:723–729. doi: 10.1016/j.amjcard.2010.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011;306:1669–1678. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Velagaleti RS, Gona P, Larson MG, Wang TJ, Levy D, Benjamin EJ, Selhub J, Jacques PF, Meigs JB, Tofler GH, Vasan RS. Multimarker approach for the prediction of heart failure incidence in the community. Circulation. 2010;122:1700–1706. doi: 10.1161/CIRCULATIONAHA.109.929661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dhingra R, Gona P, Wang TJ, Fox CS, D’Agostino RB, Sr, Vasan RS. Serum gamma-glutamyl transferase and risk of heart failure in the community. Arterioscler Thromb Vasc Biol. 2010;30:1855–1860. doi: 10.1161/ATVBAHA.110.207340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coglianese EE, Qureshi MM, Vasan RS, Wang TJ, Moore LL. Usefulness of the blood hematocrit level to predict development of heart failure in a community. Am J Cardiol. 2012;109:241–245. doi: 10.1016/j.amjcard.2011.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frankel DS, Vasan RS, D’Agostino RB, Sr, Benjamin EJ, Levy D, Wang TJ, Meigs JB. Resistin, adiponectin, and risk of heart failure: the Framingham offspring study. J Am Coll Cardiol. 2009;53:754–762. doi: 10.1016/j.jacc.2008.07.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Djoussé L, Driver JA, Gaziano JM. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA. 2009;302:394–400. doi: 10.1001/jama.2009.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Djoussé L, Wilk JB, Hanson NQ, Glynn RJ, Tsai MY, Gaziano JM. Association between adiponectin and heart failure risk in the Physicians’ Health Study. Obesity (Silver Spring) 2013;21:831–834. doi: 10.1002/oby.20260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalogeropoulos A, Georgiopoulou V, Kritchevsky SB, Psaty BM, Smith NL, Newman AB, Rodondi N, Satterfield S, Bauer DC, Bibbins-Domingo K, Smith AL, Wilson PW, Vasan RS, Harris TB, Butler J. Epidemiology of incident heart failure in a contemporary elderly cohort: the Health, Aging, and Body Composition Study. Arch Intern Med. 2009;169:708–715. doi: 10.1001/archinternmed.2009.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kalogeropoulos A, Georgiopoulou V, Psaty BM, Rodondi N, Smith AL, Harrison DG, Liu Y, Hoffmann U, Bauer DC, Newman AB, Kritchevsky SB, Harris TB, Butler J Health ABC Study Investigators. Inflammatory markers and incident heart failure risk in older adults: the Health ABC (Health, Aging, and Body Composition) study. J Am Coll Cardiol. 2010;55:2129–2137. doi: 10.1016/j.jacc.2009.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gopal DM, Kalogeropoulos AP, Georgiopoulou VV, Tang WW, Methvin A, Smith AL, Bauer DC, Newman AB, Kim L, Harris TB, Kritchevsky SB, Butler J Health ABC Study. Serum albumin concentration and heart failure risk: the Health, Aging, and Body Composition Study. Am Heart J. 2010;160:279–285. doi: 10.1016/j.ahj.2010.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gopal DM, Kalogeropoulos AP, Georgiopoulou VV, Smith AL, Bauer DC, Newman AB, Kim L, Bibbins-Domingo K, Tindle H, Harris TB, Tang WW, Kritchevsky SB, Butler J. Cigarette smoking exposure and heart failure risk in older adults: the Health, Aging, and Body Composition Study. Am Heart J. 2012;164:236–242. doi: 10.1016/j.ahj.2012.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.deFilippi CR, de Lemos JA, Christenson RH, Gottdiener JS, Kop WJ, Zhan M, Seliger SL. Association of serial measures of cardiac troponin T using a sensitive assay with incident heart failure and cardiovascular mortality in older adults. JAMA. 2010;304:2494–2502. doi: 10.1001/jama.2010.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mozaffarian D, Lemaitre RN, King IB, Song X, Spiegelman D, Sacks FM, Rimm EB, Siscovick DS. Circulating long-chain ω-3 fatty acids and incidence of congestive heart failure in older adults: the Cardiovascular Health Study: a cohort study. Ann Intern Med. 2011;155:160–170. doi: 10.1059/0003-4819-155-3-201108020-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Blecker S, Matsushita K, Köttgen A, Loehr LR, Bertoni AG, Boulware LE, Coresh J. High-normal albuminuria and risk of heart failure in the community. Am J Kidney Dis. 2011;58:47–55. doi: 10.1053/j.ajkd.2011.02.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Matsushita K, Blecker S, Pazin-Filho A, Bertoni A, Chang PP, Coresh J, Selvin E. The association of hemoglobin A1c with incident heart failure among people without diabetes: the Atherosclerosis Risk in Communities study. Diabetes. 2010;59:2020–2026. doi: 10.2337/db10-0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saunders JT, Nambi V, de Lemos JA, Chambless LE, Virani SS, Boerwinkle E, Hoogeveen RC, Liu X, Astor BC, Mosley TH, Folsom AR, Heiss G, Coresh J, Ballantyne CM. Cardiac troponin T measured by a highly sensitive assay predicts coronary heart disease, heart failure, and mortality in the Atherosclerosis Risk in Communities Study. Circulation. 2011;123:1367–1376. doi: 10.1161/CIRCULATIONAHA.110.005264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roberts CB, Couper DJ, Chang PP, James SA, Rosamond WD, Heiss G. Influence of life-course socioeconomic position on incident heart failure in blacks and whites: the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2010;172:717–727. doi: 10.1093/aje/kwq193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bekwelem W, Lutsey PL, Loehr LR, Agarwal SK, Astor BC, Guild C, Ballantyne CM, Folsom AR. White blood cell count, C-reactive protein, and incident heart failure in the Atherosclerosis Risk in Communities (ARIC) Study. Ann Epidemiol. 2011;21:739–748. doi: 10.1016/j.annepidem.2011.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Agarwal SK, Simpson RJ, Jr, Rautaharju P, Alonso A, Shahar E, Massing M, Saba S, Heiss G. Relation of ventricular premature complexes to heart failure (from the Atherosclerosis Risk In Communities [ARIC] Study) Am J Cardiol. 2012;109:105–109. doi: 10.1016/j.amjcard.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Choi EY, Bahrami H, Wu CO, Greenland P, Cushman M, Daniels LB, Almeida AL, Yoneyama K, Opdahl A, Jain A, Criqui MH, Siscovick D, Darwin C, Maisel A, Bluemke DA, Lima JA. N-terminal pro-B-type natriuretic peptide, left ventricular mass, and incident heart failure: Multi-Ethnic Study of Atherosclerosis. Circ Heart Fail. 2012;5:727–734. doi: 10.1161/CIRCHEARTFAILURE.112.968701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Redfield MM, Jacobsen SJ, Burnett JC, Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289:194–202. doi: 10.1001/jama.289.2.194. [DOI] [PubMed] [Google Scholar]
- 44.Kane GC, Karon BL, Mahoney DW, Redfield MM, Roger VL, Burnett JC, Jr, Jacobsen SJ, Rodeheffer RJ. Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA. 2011;306:856–863. doi: 10.1001/jama.2011.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bursi F, Weston SA, Redfield MM, Jacobsen SJ, Pakhomov S, Nkomo VT, Meverden RA, Roger VL. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–2216. doi: 10.1001/jama.296.18.2209. [DOI] [PubMed] [Google Scholar]
- 46.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention, National Center for Health Statistics. 2010 National Ambulatory Medical Care Survey and 2010 National Hospital Ambulatory Medical Care Survey. [Accessed July 17, 2013];Ambulatory health care data: questionnaires, datasets, and related documentation. For methodology, see National Center for Health Statistics, Public Use Data File Documentation: 2010 National Ambulatory Medical Care Survey and Public Use Data File Documentation: 2010 National Hospital Ambulatory Medical Care Survey. http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
- 48.Centers for Disease Control and Prevention, National Center for Health Statistics. 2009 National Ambulatory Medical Care Survey and 2009 National Hospital Ambulatory Medical Care Survey. [Accessed August 12, 2011];Ambulatory health care data: questionnaires, datasets, and related documentation. For methodology, see National Center for Health Statistics, Public Use Data File Documentation: 2009 National Ambulatory Medical Care Survey and Public Use Data File Documentation: 2009 National Hospital Ambulatory Medical Care Survey. http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
- 49.Dunlay SM, Redfield MM, Weston SA, Therneau TM, Hall Long K, Shah ND, Roger VL. Hospitalizations after heart failure diagnosis a community perspective. J Am Coll Cardiol. 2009;54:1695–1702. doi: 10.1016/j.jacc.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
20. Valvular, Venous, and Aortic Diseases
See Tables 20-1 and 20-2 and Chart 20-1.
Table 20-1.
Pooled Prevalence of Valvular Heart Disease From CARDIA, ARIC, and CHS Cohorts
| Age, y
|
P Value for Trend | Frequency Adjusted to 2000 US Adult Population | |||||
|---|---|---|---|---|---|---|---|
| 18–44 | 45–54 | 55–64 | 65–74 | ≥75 | |||
| Participants, n | 4351 | 696 | 1240 | 3879 | 1745 | … | 209 128 094 |
| Male | 1959 (45) | 258 (37) | 415 (33) | 1586 (41) | 826 (47) | … | 100 994 367 (48) |
| Mitral regurgitation (n=449) | 23 (0.5) | 1 (0.1) | 12 (1.0) | 250 (6.4) | 163 (9.3) | <0.0001 | 1.7% (95% CI, 1.5%–1.9%) |
| Mitral stenosis (n=15) | 0 (0) | 1 (0.1) | 3 (0.2) | 7 (0.2) | 4 (0.2) | 0.006 | 0.1% (95% CI, 0.02%–0.2%) |
| Aortic regurgitation (n=90) | 10 (0.2) | 1 (0.1) | 8 (0.7) | 37 (1.0) | 34 (2.0) | <0.0001 | 0.5% (95% CI, 0.3%–0.6%) |
| Aortic stenosis (n=102) | 1 (0.02) | 1 (0.1) | 2 (0.2) | 50 (1.3) | 48 (2.8) | <0.0001 | 0.4% (95% CI, 0.3%–0.5%) |
| Any valve disease | |||||||
| Overall (n=615) | 31 (0.7) | 3 (0.4) | 23 (1.9) | 328 (8.5) | 230 (13.2) | <0.0001 | 2.5% (95% CI, 2.2%–2.7%) |
| Women (n=356) | 19 (0.8) | 1 (0.2) | 13 (1.6) | 208 (9.1) | 115 (12.6) | <0.0001 | 2.4% (95% CI, 2.1%–2.8%) |
| Men (n=259) | 12 (0.6) | 2 (0.8) | 10 (2.4) | 120 (7.6) | 115 (14.0) | <0.0001 | 2.5% (95% CI, 2.1%–2.9%) |
Values are n (%) unless otherwise indicated.
ARIC indicates Atherosclerosis Risk in Communities study; CARDIA, Coronary Artery Risk Development in Young Adults; CHS, Cardiovascular Health Study; CI, confidence interval; and ellipses (…), not applicable.
Source: Reprinted from The Lancet, Nkomo et al1 with permission from Elsevier. Copyright © 2006, Elsevier Ltd.
Table 20-2.
Rheumatic Fever/Rheumatic Heart Disease
| Population Group | Mortality, 2010: All Ages* | Hospital Discharges, 2010: All Ages |
|---|---|---|
| Both sexes | 2987 | 20 000 |
| Males | 996 (33.3%)† | 5000 |
| Females | 1991 (66.7%)† | 15 000 |
| NH white males | 885 | … |
| NH white females | 1759 | … |
| NH black males | 79 | … |
| NH black females | 153 | … |
| Asian or Pacific Islander‡ | 97 | … |
| American Indian or Alaska Native‡ | 14 | … |
Ellipses (…) indicate data not available; and NH, non-Hispanic.
Mortality data include Hispanics.
These percentages represent the portion of total mortality that is for males vs females.
Number of deaths shown may be lower than actual because of underreporting in this population.
Sources: Mortality: Centers for Disease Control and Prevention/National Center for Health Statistics, 2010 Mortality Multiple Cause-of-Death–United States, version dated May 29, 2013; data represent underlying cause of death only. Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics, and National Heart, Lung, and Blood Institute; data include those inpatients discharged alive, dead, or of unknown status.
Chart 20-1.
Rheumatic heart disease prevalence trends per 1000 people for each World Health Organization region: A, The Americas; B, Europe; C, Africa; D, Eastern Mediterranean; E, Western Pacific; and F, Southeast Asia. Reprinted from Seckeler and Hoke14 with permission of Dove Medical Press; permission conveyed through Copyright Clearance Center, Inc. Copyright © 2011, Seckeler and Hoke,
Mortality and any-mention mortality in this section are for 2010. “Mortality” is the number of deaths in 2010 for the given underlying cause based on ICD-10. Prevalence data are for 2006. Hospital discharge data are from the NHDS/NCHS; data include inpatients discharged alive, dead, or status unknown. Hospital discharge data for 2010 are based on ICD-9 codes.
Valvular Heart Disease
(See Table 20-1.)
ICD-9 424; ICD-10 I34 to I38.
Mortality—22 777. Any-mention mortality—46 426. Hospital discharges—85 000.
Two important factors have contributed to the changing epidemiology of valvular heart disease in the United States over the past few decades: aging of the population and the increased ability to diagnose valvular heart disease by echocardiography.
A large population-based epidemiological study with systematic use of echocardiography on 16 501participants from Olmsted County, MN, showed an overall age-adjusted prevalence of clinically diagnosed (moderate or greater) valvular heart disease of 1.8%.1
-
Prevalence of any valve disease increased with age1
18 to 44 years: 0.3% (95% CI, 0.2%–0.3%)
45 to 54 years: 0.7% (95% CI, 0.6%–0.9%)
55 to 64 years: 1.6% (95% CI, 1.4%–1.9%)
65 to 75 years: 4.4% (95% CI, 3.9%–4.9%)
≥75 years: 11.7% (95% CI, 11.0%–12.5%)
-
Pooled echocardiographic data from 11 911 participants from CARDIA (4351), ARIC (2435), and CHS (5125) demonstrated a similar increase in prevalence with age (Table 20-1).1
18 to 44 years: 0.7% (95% CI, 0.5%–1.0%)
45 to 54 years: 0.4% (95% CI, 0.1%–1.3%)
55 to 64 years: 1.9% (95% CI, 1.2%–2.8%)
65 to 75 years: 8.5% (95% CI, 7.6%–9.4%)
≥75 years: 13.3% (95% CI, 11.7%–15.0%)
Adjusted to the entire US population, these data suggest that the prevalence of any valve disease is 2.5% (95% CI, 2.2%–2.7%), with no difference between men (2.4% [95% CI, 2.1%–2.8%]) and women (2.5% [95% CI, 2.1%–2.9%]). Within this sample, 0.4% had aortic stenosis, 0.5% had aortic regurgitation, 0.1% had mitral stenosis, and 1.7% had mitral regurgitation.1
In CARDIA, ARIC, and CHS, survival of participants with valve disease was 79% (SE 2%) at 5 years and 68% (1.9%) at 8 years compared with 93% (0.2%) and 86% (0.4%) in participants without valve disease.
Abbreviations Used in Chapter 20
| AAA | abdominal aortic aneurysm |
| AHA | American Heart Association |
| AVR | aortic valve replacement |
| ARIC | Atherosclerosis Risk in Communities study |
| BMI | body mass index |
| CARDIA | Coronary Artery Risk Development in Young Adults |
| CHD | coronary heart disease |
| CHS | Cardiovascular Health Study |
| CI | confidence interval |
| CT | computed tomography |
| DM | diabetes mellitus |
| DVT | deep vein thrombosis |
| GBD | Global Burden of Diseases, Injuries, and Risk Factors Study |
| HD | heart disease |
| HR | hazard ratio |
| ICD | International Classification of Diseases |
| ICD-9 | International Classification of Diseases, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| IE | infective endocarditis |
| IRAD | International Registry of Acute Aortic Dissection |
| MESA | Multi-Ethnic Study of Atherosclerosis |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHDS | National Hospital Discharge Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| OVER | Open Versus Endovascular Repair |
| PAD | peripheral artery disease |
| PARTNER | Placement of Aortic Transcatheter Valves |
| PE | pulmonary embolism |
| RR | relative risk |
| SD | standard deviation |
| STS | Society of Thoracic Surgeons |
| TAVR | transcatheter aortic valve replacement |
| TIA | transient ischemic attack |
| VTE | venous thromboembolism |
| WHO | World Health Organization |
| YLL | years of life lost |
Aortic Valve Disorders
ICD-9 424.1; ICD-10 I35.
Mortality—15 276 Any-mention mortality—30 736. Hospital discharges—55 000.
The prevalence of moderate or severe aortic stenosis in patients ≥75 years old is 2.8% (95% CI, 2.1%–3.7%), and the prevalence of moderate or severe aortic regurgitation in patients ≥75 years is 2.0% (95% CI, 1.4%–2.7%).1
In MESA participants aged 45 to 84 years (n=5880), aortic valve calcium was quantified with serial CT images. During a mean follow-up of 2.4 years, 210 (4.1%) of the 5142 participants with no aortic valve calcium had a mean incidence rate of progression of 1.7% per year, which increased with age. Incident aortic valve calcium was associated with several conventional cardiovascular risk factors, including age, male sex, BMI, and smoking.2
Approximately 50% of patients with severe aortic stenosis are referred for cardiothoracic surgery, and ≈40% undergo AVR according to data from 10 US centers of various sizes and geographic distribution. Reasons for not undergoing AVR included high perioperative risk, age, lack of symptoms, and patient/family refusal.3
On the basis of data from the PARTNER B cohort that compared TAVR with medical therapy in patients who were not surgical candidates for AVR, 2-year mortality rates were 43.3% and 68% (P<0.001) and 2-year hospitalization rates were 35% and 72.5% (P<0.001), respectively.4
One-year costs of TAVR were higher than with medical therapy ($106 076 versus $53 621), with an incremental cost-effectiveness of $50 200 per life-year gained and $61 889 per quality-adjusted life-year gained.5
In a cohort of 416 community-based participants from Olmsted County, MN, with bicuspid aortic valves followed up for a mean (SD) of 16 (7) years, the incidence of aortic dissection in individuals ≥50 years of age at baseline was 17.4 (95% CI, 2.9–53.6) cases per 10 000 patient years. For patients aged ≥50 years with a bicuspid valve and a baseline aortic aneurysm, the incidence of aortic dissection was 44.9 (95% CI, 7.5–138.5) cases per 10 000 patient-years. In the remaining participants without baseline aortic aneurysm, the incidence of aneurysm was 84.9 (95% CI, 63.3–110.9) cases per 10 000 patient-years, for an age-adjusted RR of 86.2 (95% CI, 65.1–114) compared with the general population.6
Aortic Valve Interventions
Lipid-lowering therapy does not appear to reduce aortic stenosis progression on the basis of any echocardiographic measures of aortic stenosis, as reported by a meta-analysis of 4 randomized controlled trials by Teo and colleagues.7
Immediate postoperative and 1-, 3-, 5-, and 10-year pooled survival rates from 48 studies of 13 216 octogenarians were 93.7%, 87.6%, 78.7%, 65.4%, and 29.7%, respectively.8
-
TAVR has emerged as an innovative technology for treatment of aortic stenosis in patients at high risk for perioperative complications.
-
A systematic review9 of TAVR from 16 studies that included 3519 patients and reported at least 1 outcome using the Valve Academic Research Consortium’s definitions demonstrated the following:
Device success 92.1% (88.7–95.5%)
30-day all-cause mortality 7.8% (5.5%-11.1%)
1-year all-cause mortality 22.1% (17.9–26.9%)
Major vascular complications 11.9% (8.6%-16.4%)
Major stroke 3.2% (2.1%-4.8%)
More recent data from the PARTNER A cohort that compared TAVR with surgical AVR showed that 2-year mortality rates were 33.9% and 35% (P=0.78), respectively. Stroke or TIA rates were higher in the TAVR arm (11.2% versus 6.5%, P=0.05) than in the surgical AVR arm, as were major vascular complications (11.6% versus 3.8%, P<0.001).10
-
Mitral Valve Disorders
ICD-9 424.0; ICD-10 I34.
Mortality—2279. Any-mention mortality—5185. Hospital discharges—22 000.
Prevalence
(See Table 20-1.)
In pooled data from CARDIA, ARIC, and CHS, mitral valve disease was the most common valvular lesion. At least moderate mitral regurgitation occurred at a frequency of 1.7% as adjusted to the US adult population of 2000, increasing from 0.5% in participants aged 18 to 44 years to 9.3% in participants aged ≥75 years.1
-
A systematic review by de Marchena and colleagues11 found that in the US population, the prevalence of mitral regurgitation according to Carpentier’s functional classification system was as follows:
Type I (congenital mitral regurgitation and endocarditis): <20 per 1 million
Type II (myxomatous mitral regurgitation): 15 000 per 1 million
Type IIIa (rheumatic HD, systemic lupus erythematosus, antiphospholipid syndrome): 10 520 per 1 million
Type IIIb (ischemic mitral regurgitation, left ventricular dysfunction, dilated cardiomyopathy): 23 250 per 1 million
Data from the STS adult cardiac surgery database of 14 604 isolated, nonemergent mitral valve repair operations demonstrate an operative mortality rate of 2.59%. Over a mean (SD) follow-up of 5.9 (3.9) years and a mean (SD) age of 73.3 (5.5) years, survival was 74.9%. The 10-year actuarial survival rate of 57.4% was similar to the matched US population.12
Pulmonary Valve Disorders
ICD-9 424.3; ICD-10 I37.
Mortality—17. Any-mention mortality—44.
Tricuspid Valve Disorders
ICD-9 424.2; ICD-10 I36.
Mortality—9. Any-mention mortality—93.
Rheumatic Fever/Rheumatic HD
(See Table 20-2 and Chart 20-1.)
ICD-9 390 to 398; ICD-10 I00 to I09.
Mortality—2987. Any-mention mortality—5747. Hospital discharges—20 000.
Rheumatic HD is uncommon in high-income countries such as the United States but remains endemic in Africa, Asia, and the Pacific, affecting >15 million individuals and causing 233 000 deaths annually.13
The reported prevalence of rheumatic HD is increasing in all regions of the world except Europe.14
-
Recent echocardiography-based screening studies in schoolchildren have demonstrated rheumatic HD prevalence rates ranging from 14.8 (95% CI, 7.3–22.3) per 1000 (Uganda)15 to 20.4 (95% CI, 16.9–23.9) per 1000 in northern India16 to 21.5 (95% CI, 16.8–26.2) per 1000 in Cambodia and 30.4 (95% CI, 23.2–37.6) per 1000 (Mozambique).17
Acute rheumatic fever incidence is decreasing in all WHO regions except for the Americas, where it appears to be increasing slightly, and the Western Pacific, where it appears to be increasing steadily.14
In 1950, ≈15 000 Americans (adjusted for changes in ICD codes) died of rheumatic fever/rheumatic HD compared with ≈3100 annually in the present era (NCHS/NHLBI).
The 2009 overall death rate for rheumatic fever/rheumatic HD was 1.1 per 100 000. Death rates varied across race/ethnic groups but were generally low: white, 1.2 per 100 000; black or African American, 0.7 per 100 000; Asian or Pacific Islander, 0.6 per 100 000; American Indian or Alaska Native, 0.6 per 100 000; and Hispanic or Latino origin individuals, 0.4 per 100 000.18
Bacterial Endocarditis
ICD-9 421.0; ICD-10 I33.0.
Mortality—1060. Any-mention mortality—2197. Hospital discharges—34 000, primary plus secondary diagnoses.
The 2007 AHA guidelines on prevention of IE15 state that IE is thought to result from the following sequence of events: (1) Formation of nonbacterial thrombotic endocarditis on the surface of a cardiac valve or elsewhere that endothelial damage occurs; (2) bacteremia; and (3) adherence of the bacteria in the bloodstream to nonbacterial thrombotic endocarditis and proliferation of bacteria within a vegetation. Viridans group streptococci are part of the normal skin, oral, respiratory, and gastrointestinal tract flora, and they cause ≥50% of cases of community-acquired native valve IE not associated with intravenous drug use.19
-
Although the absolute risk for acquiring IE from a dental procedure is impossible to measure precisely, the best available estimates are as follows: If dental treatment causes 1% of all cases of viridans group streptococcal IE annually in the United States, the overall risk in the general population is estimated to be as low as 1 case of IE per 14 million dental procedures. The estimated absolute risk rates for acquiring IE from a dental procedure in patients with underlying cardiac conditions are as follows20:
Mitral valve prolapse: 1 per 1.1 million procedures
CHD: 1 per 475 000
Rheumatic HD: 1 per 142 000
Presence of a prosthetic cardiac valve: 1 per 114 000
Previous IE: 1 per 95 000 dental procedures
Cessation of antibiotic prophylaxis for IE before dental procedures has not led to a change in pediatric cases of endocarditis. Using 2003 to 2010 data from 37 centers in the Pediatric Health Information Systems Database, Pasquali and colleagues21 did not demonstrate a significant difference in the number of IE hospitalizations after the guidelines were implemented in 2007 (1.6% difference after versus before guideline implementation; 95% CI, −6.4% to 10.3%; P=0.7).
A systematic review that included 161 studies and 27 354 patients from 1960 to 2011 demonstrated that in hospital-based studies (143 studies; 23 877 patients), staphylococcal endocarditis has increased over time (coagulase-negative Staphylococcus 2% to 10%, P<0.001), with recent increases in Staphylococcus aureus (21% to 30%, P<0.05) over the past decade and a corresponding decrease in streptococcal endocarditis (32% to 17%) over the same time period.22
Cardiac device IE appears to be present in 6.4% (95% CI, 5.5%–7.4%) of patients with definite IE, according to data from the International Collaboration on Endocarditis–Prospective Cohort Study (2000–2006). Nearly half (45.8%; 95% CI, 38.3%–53.4%) of such cases are associated with healthcare-associated infection. In-hospital and 1-year mortality rates for these patients were 14.7% (26/177; 95% CI, 9.8%–20.8%) and 23.2% (41/177; 95% CI, 17.2%–30.1%), respectively.23
Endocarditis, Valve Unspecified
ICD-9 424.9; ICD-10 I38.
Mortality—5196. Any-mention mortality—10 582.
VTE Epidemiology (Including DVT and PE)24
Pulmonary Embolism
ICD-9 415.1; ICD-10 I26.
Mortality—7322. Any-mention mortality—29 392. Hospital discharges—186 000.
Deep Vein Thrombosis
ICD-9 451.1; ICD-10 I80.2.
Mortality—2484. Any-mention mortality—12 952.
Incidence
The average annual incidence of VTE among whites is 108 per 100 000 person-years, with 250 000 incident cases occurring annually among US whites.
VTE incidence appears to be similar or higher among African Americans and lower among Asian Americans and Native Americans than among whites.
After adjustment for the different age and sex distribution of African Americans, VTE incidence is 78 per 100 000, which suggests that 27 000 incident VTE cases occur annually among US blacks.
VTE incidence has not changed significantly over the past 25 years.
Incidence rates increase exponentially with age for both men and women and for both DVT and PE.
Incidence rates are higher in women during childbearing years, whereas incidence rates after age 45 years are higher in men.
PE accounts for an increasing proportion of VTE with increasing age in both sexes.
VTE event type (DVT versus PE) has a common familial background and shared genetic susceptibility.25
Survival
For almost one quarter of PE patients, the initial clinical presentation is sudden death.
Thirty-day VTE survival is 74 .8% (DVT alone, 96 .2%; PE with or without DVT, 59.1%).26
PE is an independent predictor of reduced survival for ≤3 months.
Because most PE deaths are sudden and usually attributed to underlying disease (eg, cancer; other chronic heart, lung, or renal disease), secular trends in VTE survival are confounded by autopsy rates.
Recurrence
VTE is a chronic disease with episodic recurrence; ≈30% of patients develop recurrence within the next 10 years.
Independent predictors of early (within 180 days) recurrence include active cancer, proportion of time spent taking heparin with a heparin level ≥0.2 anti-Xa U/mL, and proportion of time spent taking warfarin with an international normalized ratio ≥2. Two-week case fatality for recurrent DVT alone and recurrent PE with or without DVT is 2% and 11%, respectively.27
Complications
The 20-year cumulative incidence of venous stasis syndrome and venous ulcer after proximal DVT is 40% and 3.7%, respectively.
The incidence of chronic thromboembolic pulmonary hypertension is 6.5 per million person-years; ≈1400 incident cases occur annually among US whites.
Risk Factors
Independent VTE risk factors include increasing patient age, surgery, trauma/fracture, hospital or nursing home confinement, active cancer, central vein catheterization or transvenous pacemaker, prior superficial vein thrombosis, infection, varicose veins, and neurological disease with leg paresis, and among women, use of oral contraceptives, pregnancy/postpartum period, and hormone therapy.28
Together, these risk factors account for >75% of all incident VTE that occurs in the community.
Compared with residents in the community, hospitalized residents have a >130-fold higher VTE incidence (71 versus 9605 per 100 000 person-years).29
Hospitalization and nursing home residence together account for almost 60% of incident VTE events that occur in the community.
Among patients hospitalized for acute medical illness, independent risk factors for VTE include prior VTE, thrombophilia, cancer, age >60 years, leg paralysis, immobilization ≥7 days, and admission to an intensive care unit or coronary care unit.30
Among cancer patients beginning chemotherapy, tumor site, BMI, hemoglobin, platelet and white blood cell count, and plasma D-dimer and soluble P-selectin levels are predictors of VTE in the next 6 months.31
In a large cohort study of middle-aged women, including women undergoing surgery, current smoking increased the risk for hospitalization for or death attributable to VTE.32 However, whether smoking represents an independent VTE risk factor remains uncertain.
In a case-crossover study, novel predictors of hospitalization for VTE included recent infection, erythropoiesis-stimulating agents, and blood transfusion.33
Hospitalization for an autoimmune disorder (particularly immune thrombocytopenia, polyarteritis nodosa, polymyositis or dermatomyositis, systemic lupus erythematosus, and rheumatoid arthritis34) is associated with an increased risk for VTE in the year after hospitalization.35
An association between systemic, intestinal, or inhaled glucocorticoids and VTE was reported recently36; however, this association may be spurious because of residual confounding.
Among patients with immune thrombocytopenia, splenectomy was associated with an increased incidence of abdominal vein thrombosis within 90 days after surgery and an increased incidence of leg DVT and PE.37 Whether these associations are independent of immune thrombocytopenia disease activity is uncertain.
Pregnancy-associated VTE incidence is 200 per 100 000 woman-years; compared with nonpregnant women of childbearing age, the RR for VTE is increased 4-fold. VTE risk appears to be higher for pregnancies after in vitro fertilization compared with natural pregnancies.38
VTE risk during the postpartum period is ≈5-fold higher than during pregnancy.
Arteries, Diseases of
ICD-9 440 to 448; ICD-10 I70 to I78. Includes PAD.
Penetrating Aortic Ulcers
A single-center evaluation of 388 penetrating aortic ulcers found on CT angiography (2003–2009) demonstrated penetrating aortic ulcers in the aortic arch (6.8%), descending thoracic aorta (61.2%), and abdominal aorta (29.7%). Nearly 2 of every 3 penetrating aortic ulcers (57.7%) did not have a saccular aneurysm or intramural hematoma, whereas ≈1 in 4 (27.8%) had associated saccular aneurysms, and ≈1 in 7 (14.4%) had an associated intramural hematoma. Rupture was present in ≈1 in 25 penetrating aortic ulcers (4.1%).39
Aortic Aneurysm
ICD-9 441; ICD-10 I71.
Mortality—10 431. Any-mention mortality—16 877. Hospital discharges—64 000.
According to the GBD, the age-standardized death rate attributable to aortic aneurysm was 3.4 (95% CI, 2.5–4.8), with a 27% median decrease since 1990. The YLL because of aortic aneurysms was 57.4 (95% CI, 43.8–80.4), with a 29% median decrease since 1990.40
Although the definition varies somewhat by age and body surface area, generally an AAA is considered to be present when the anteroposterior diameter of the aorta reaches 3.0 cm.41
The prevalence of AAAs that are 2.9 to 4.9 cm in diameter ranges from 1.3% in men 45 to 54 years of age to 12.5% in men 75 to 84 years of age. For women, the prevalence ranges from 0% in the youngest to 5.2% in the oldest age groups.41
A meta-analysis of 15 475 individuals from 18 studies on small AAAs (3.0–5.4 cm) demonstrated that mean aneurysm growth rate was 2.21 mm per year and was independent of age and sex. Growth rates were higher in smokers (by 0.35 mm/y) and lower in patients with DM (by 0.51 mm/y).42
Rupture rates range from 0.71 to 11.03 per 1000 person-years, with higher rupture rates in smokers (pooled HR, 2.02; 95% CI, 1.33–3.06) and women (pooled HR, 3.76; 95% CI, 2.58–5.47).42
Data from IRAD demonstrate that the rate of mesenteric malperfusion in 1809 patients with type A acute dissections was 3.7%, with a higher mortality rate than for patients without malperfusion (63.2% versus 23.8%, P<0.001).43
Data from IRAD suggest that patients with acute type B aortic dissection have heterogeneous in-hospital outcomes. In-hospital mortality in patients with and without complications (such as mesenteric ischemia, renal failure, limb ischemia, or refractory pain) was 20.0% and 6.1%, respectively. In patients with complications, in-hospital mortality associated with surgical and endovascular repair was 28.6% and 10.1% (P=0.006), respectively.44
Thoracic Aortic Aneurysm Treatment
A sample of 12 573 and 2732 Medicare patients who underwent open thoracic aortic aneurysm and endovascular repair demonstrated higher perioperative mortality for open repair in both intact (7.1% versus 6.1%, P=0.07) and ruptured (46% versus 28%, P<0.01) thoracic aortic aneurysms but higher 1-year (87% versus 82%, P=0.001) and 5-year (72% versus 62%, P=0.001) survival rates.45
Perioperative mortality rates for open thoracic aortic aneurysms were higher for black Medicare patients than for white Medicare patients (18% versus 10%, P<0.001), but rates were similar for endovascular repair (8% versus 9%, P=0.56).46
AAA Treatment
A 2011 meta-analysis of 46 studies that included 1397 studies of patients with ruptured AAA demonstrated that endovascular repair was associated with a perioperative mortality rate of 24.3%.47
Long-term results from the OVER trial that compared open AAA repair to endovascular repair demonstrated no survival difference between open and endovascular repair at a median follow-up of 9 years (HR, 0.97; 95% CI, 0.77–1.22) despite reductions in mortality from endovascular repair at 2 years (HR, 0.63; 95% CI, 0.40–0.98) and 3 years (HR, 0.72; 95% CI, 0.51–1.00).48
After multivariable adjustment, Medicare patients who underwent open AAA repair had a higher risk of all-cause mortality (HR, 1.24; 95% CI, 1.05–1.47) and AAA-related mortality (HR, 4.37; 95% CI, 2.51–7.66) at 1 year than patients who underwent endovascular repair.49
- 1.Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005–1011. doi: 10.1016/S0140-6736(06)69208-8. [DOI] [PubMed] [Google Scholar]
- 2.Owens DS, Katz R, Takasu J, Kronmal R, Budoff MJ, O’Brien KD. Incidence and progression of aortic valve calcium in the Multi-Ethnic Study of Atherosclerosis (MESA) Am J Cardiol. 2010;105:701–708. doi: 10.1016/j.amjcard.2009.10.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bach DS. Prevalence and characteristics of unoperated patients with severe aortic stenosis. J Heart Valve Dis. 2011;20:284–291. [PubMed] [Google Scholar]
- 4.Makkar RR, Fontana GP, Jilaihawi H, Kapadia S, Pichard AD, Douglas PS, Thourani VH, Babaliaros VC, Webb JG, Herrmann HC, Bavaria JE, Kodali S, Brown DL, Bowers B, Dewey TM, Svensson LG, Tuzcu M, Moses JW, Williams MR, Siegel RJ, Akin JJ, Anderson WN, Pocock S, Smith CR, Leon MB PARTNER Trial Investigators. Transcatheter aortic-valve replacement for inoperable severe aortic stenosis [published correction appears in N Engl J Med. 2012;367:881] N Engl J Med. 2012;366:1696–1704. doi: 10.1056/NEJMoa1202277. [DOI] [PubMed] [Google Scholar]
- 5.Reynolds MR, Magnuson EA, Wang K, Lei Y, Vilain K, Walczak J, Kodali SK, Lasala JM, O’Neill WW, Davidson CJ, Smith CR, Leon MB, Cohen DJ PARTNER Investigators. Cost-effectiveness of transcatheter aortic valve replacement compared with standard care among inoperable patients with severe aortic stenosis: results from the Placement of Aortic Transcatheter Valves (PARTNER) trial (Cohort B) Circulation. 2012;125:1102–1109. doi: 10.1161/CIRCULATIONAHA.111.054072. [DOI] [PubMed] [Google Scholar]
- 6.Michelena HI, Khanna AD, Mahoney D, Margaryan E, Topilsky Y, Suri RM, Eidem B, Edwards WD, Sundt TM, 3rd, Enriquez-Sarano M. Incidence of aortic complications in patients with bicuspid aortic valves. JAMA. 2011;306:1104–1112. doi: 10.1001/jama.2011.1286. [DOI] [PubMed] [Google Scholar]
- 7.Teo KK, Corsi DJ, Tam JW, Dumesnil JG, Chan KL. Lipid lowering on progression of mild to moderate aortic stenosis: meta-analysis of the randomized placebo-controlled clinical trials on 2344 patients. Can J Cardiol. 2011;27:800–808. doi: 10.1016/j.cjca.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Vasques F, Messori A, Lucenteforte E, Biancari F. Immediate and late outcome of patients aged 80 years and older undergoing isolated aortic valve replacement: a systematic review and meta-analysis of 48 studies. Am Heart J. 2012;163:477–485. doi: 10.1016/j.ahj.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 9.Généreux P, Head SJ, Van Mieghem NM, Kodali S, Kirtane AJ, Xu K, Smith C, Serruys PW, Kappetein AP, Leon MB. Clinical outcomes after transcatheter aortic valve replacement using Valve Academic Research Consortium definitions: a weighted meta-analysis of 3,519 patients from 16 studies. J Am Coll Cardiol. 2012;59:2317–2326. doi: 10.1016/j.jacc.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 10.Kodali SK, Williams MR, Smith CR, Svensson LG, Webb JG, Makkar RR, Fontana GP, Dewey TM, Thourani VH, Pichard AD, Fischbein M, Szeto WY, Lim S, Greason KL, Teirstein PS, Malaisrie SC, Douglas PS, Hahn RT, Whisenant B, Zajarias A, Wang D, Akin JJ, Anderson WN, Leon MB PARTNER Trial Investigators. Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med. 2012;366:1686–1695. doi: 10.1056/NEJMoa1200384. [DOI] [PubMed] [Google Scholar]
- 11.de Marchena E, Badiye A, Robalino G, Junttila J, Atapattu S, Nakamura M, De Canniere D, Salerno T. Respective prevalence of the different Carpentier classes of mitral regurgitation: a stepping stone for future therapeutic research and development. J Card Surg. 2011;26:385–392. doi: 10.1111/j.1540-8191.2011.01274.x. [DOI] [PubMed] [Google Scholar]
- 12.Badhwar V, Peterson ED, Jacobs JP, He X, Brennan JM, O’Brien SM, Dokholyan RS, George KM, Bolling SF, Shahian DM, Grover FL, Edwards FH, Gammie JS. Longitudinal outcome of isolated mitral repair in older patients: results from 14,604 procedures performed from 1991 to 2007. Ann Thorac Surg. 2012;94:1870–1877. doi: 10.1016/j.athoracsur.2012.05.105. [DOI] [PubMed] [Google Scholar]
- 13.Carapetis JR, McDonald M, Wilson NJ. Acute rheumatic fever. Lancet. 2005;366:155–168. doi: 10.1016/S0140-6736(05)66874-2. [DOI] [PubMed] [Google Scholar]
- 14.Seckeler MD, Hoke TR. The worldwide epidemiology of acute rheumatic fever and rheumatic heart disease. Clin Epidemiol. 2011;3:67–84. doi: 10.2147/CLEP.S12977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beaton A, Okello E, Lwabi P, Mondo C, McCarter R, Sable C. Echocardiography screening for rheumatic heart disease in Ugandan schoolchildren. Circulation. 2012;125:3127–3132. doi: 10.1161/CIRCULATIONAHA.112.092312. [DOI] [PubMed] [Google Scholar]
- 16.Saxena A, Ramakrishnan S, Roy A, Seth S, Krishnan A, Misra P, Kalaivani M, Bhargava B, Flather MD, Poole-Wilson PP. Prevalence and outcome of subclinical rheumatic heart disease in India: the RHEUMATIC (Rheumatic Heart Echo Utilisation and Monitoring Actuarial Trends in Indian Children) study. Heart. 2011;97:2018–2022. doi: 10.1136/heartjnl-2011-300792. [DOI] [PubMed] [Google Scholar]
- 17.Marijon E, Ou P, Celermajer DS, Ferreira B, Mocumbi AO, Jani D, Paquet C, Jacob S, Sidi D, Jouven X. Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med. 2007;357:470–476. doi: 10.1056/NEJMoa065085. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention, National Center for Health Statistics. CDC WONDER Online Database [database online] Atlanta, GA: Centers for Disease Control and Prevention; [Accessed July 18, 2012]. Compressed mortality file: underlying cause of death. Released January 2013. http://wonder.cdc.gov/mortSQl.html. [Google Scholar]
- 19.Fowler V, Scheld W, Bayer A. Endocarditis and intravascular infections. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and Practices of Infectious Diseases. 6. New York, NY: Elsevier; 2005. pp. 975–1021. [Google Scholar]
- 20.Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, Bolger A, Cabell CH, Takahashi M, Baltimore RS, Newburger JW, Strom BL, Tani LY, Gerber M, Bonow RO, Pallasch T, Shulman ST, Rowley AH, Burns JC, Ferrieri P, Gardner T, Goff D, Durack DT. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group [published correction appears in Circulation. 2007;116:e376– e377] Circulation. 2007;116:1736–1754. doi: 10.1161/CIRCULATIONAHA.106.183095. [DOI] [PubMed] [Google Scholar]
- 21.Pasquali SK, He X, Mohamad Z, McCrindle BW, Newburger JW, Li JS, Shah SS. Trends in endocarditis hospitalizations at US children’s hospitals: impact of the 2007 American Heart Association Antibiotic Prophylaxis Guidelines. Am Heart J. 2012;163:894–899. doi: 10.1016/j.ahj.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Slipczuk L, Codolosa NJ, Carlos D, Romero-Corral A, Pressman GS, Figueredo VM. Systematic review & meta-analysis of infective endocarditis microbiology over 5 decades. Circulation. 2012;126:A15138. Abstract. [Google Scholar]
- 23.Athan E, Chu VH, Tattevin P, Selton-Suty C, Jones P, Naber C, Miró JM, Ninot S, Fernández-Hidalgo N, Durante-Mangoni E, Spelman D, Hoen B, Lejko-Zupanc T, Cecchi E, Thuny F, Hannan MM, Pappas P, Henry M, Fowler VG, Jr, Crowley AL, Wang A ICE-PCS Investigators. Clinical characteristics and outcome of infective endocarditis involving implantable cardiac devices. JAMA. 2012;307:1727–1735. doi: 10.1001/jama.2012.497. [DOI] [PubMed] [Google Scholar]
- 24.Heit JA. The epidemiology of venous thromboembolism in the community. Arterioscler Thromb Vasc Biol. 2008;28:370–372. doi: 10.1161/ATVBAHA.108.162545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zöller B, Li X, Sundquist J, Sundquist K. Shared familial aggregation of susceptibility to different manifestations of venous thromboembolism: a nationwide family study in Sweden. Br J Haematol. 2012;157:146–148. doi: 10.1111/j.1365-2141.2011.08927.x. [DOI] [PubMed] [Google Scholar]
- 26.Heit JA, Silverstein MD, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ., 3rd Predictors of survival after deep vein thrombosis and pulmonary embolism: a population-based, cohort study. Arch Intern Med. 1999;159:445–453. doi: 10.1001/archinte.159.5.445. [DOI] [PubMed] [Google Scholar]
- 27.Heit JA, Lahr BD, Petterson TM, Bailey KR, Ashrani AA, Melton LJ., 3rd Heparin and warfarin anticoagulation intensity as predictors of recurrence after deep vein thrombosis or pulmonary embolism: a population-based cohort study. Blood. 2011;118:4992–4999. doi: 10.1182/blood-2011-05-357343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parkin L, Sweetland S, Balkwill A, Green J, Reeves G, Beral V Million Women Study Collaborators. Body mass index, surgery, and risk of venous thromboembolism in middle-aged women: a cohort study. Circulation. 2012;125:1897–1904. doi: 10.1161/CIRCULATIONAHA.111.063354. [DOI] [PubMed] [Google Scholar]
- 29.Heit JA, Melton LJ, 3rd, Lohse CM, Petterson TM, Silverstein MD, Mohr DN, O’Fallon WM. Incidence of venous thromboembolism in hospitalized patients vs community residents. Mayo Clin Proc. 2001;76:1102–1110. doi: 10.4065/76.11.1102. [DOI] [PubMed] [Google Scholar]
- 30.Spyropoulos AC, Anderson FA, Jr, Fitzgerald G, Decousus H, Pini M, Chong BH, Zotz RB, Bergmann JF, Tapson V, Froehlich JB, Monreal M, Merli GJ, Pavanello R, Turpie AG, Nakamura M, Piovella F, Kakkar AK, Spencer FA IMPROVE Investigators. Predictive and associative models to identify hospitalized medical patients at risk for VTE. Chest. 2011;140:706–714. doi: 10.1378/chest.10-1944. [DOI] [PubMed] [Google Scholar]
- 31.Ay C, Dunkler D, Marosi C, Chiriac AL, Vormittag R, Simanek R, Quehenberger P, Zielinski C, Pabinger I. Prediction of venous thromboembolism in cancer patients. Blood. 2010;116:5377–5382. doi: 10.1182/blood-2010-02-270116. [DOI] [PubMed] [Google Scholar]
- 32.Sweetland S, Parkin L, Balkwill A, Green J, Reeves G, Beral V Million Women Study Collaborators. Smoking, surgery, and venous thromboembolism risk in women: United Kingdom cohort study. Circulation. 2013;127:1276–1282. doi: 10.1161/CIRCULATIONAHA.113.001428. [DOI] [PubMed] [Google Scholar]
- 33.Rogers MA, Levine DA, Blumberg N, Flanders SA, Chopra V, Langa KM. Triggers of hospitalization for venous thromboembolism. Circulation. 2012;125:2092–2099. doi: 10.1161/CIRCULATIONAHA.111.084467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holmqvist ME, Neovius M, Eriksson J, Mantel Ä, Wållberg-Jonsson S, Jacobsson LT, Askling J. Risk of venous thromboembolism in patients with rheumatoid arthritis and association with disease duration and hospitalization. JAMA. 2012;308:1350–1356. doi: 10.1001/2012.jama.11741. [DOI] [PubMed] [Google Scholar]
- 35.Zöller B, Li X, Sundquist J, Sundquist K. Risk of pulmonary embolism in patients with autoimmune disorders: a nationwide follow-up study from Sweden. Lancet. 2012;379:244–249. doi: 10.1016/S0140-6736(11)61306-8. [DOI] [PubMed] [Google Scholar]
- 36.Johannesdottir SA, Horváth-Puhó E, Dekkers OM, Cannegieter SC, Jørgensen JO, Ehrenstein V, Vandenbroucke JP, Pedersen L, Sørensen HT. Use of glucocorticoids and risk of venous thromboembolism: a nationwide population- based case-control study. JAMA Intern Med. 2013;173:743–752. doi: 10.1001/jamainternmed.2013.122. [DOI] [PubMed] [Google Scholar]
- 37.Boyle S, White RH, Brunson A, Wun T. Splenectomy and the incidence of venous thromboembolism and sepsis in patients with immune thrombocytopenia. Blood. 2013;121:4782–4790. doi: 10.1182/blood-2012-12-467068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Henriksson P, Westerlund E, Wallén H, Brandt L, Hovatta O, Ekbom A. Incidence of pulmonary and venous thromboembolism in pregnancies after in vitro fertilisation: cross sectional study. BMJ. 2013;346:e8632. doi: 10.1136/bmj.e8632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nathan DP, Boonn W, Lai E, Wang GJ, Desai N, Woo EY, Fairman RM, Jackson BM. Presentation, complications, and natural history of penetrating atherosclerotic ulcer disease. J Vasc Surg. 2012;55:10–15. doi: 10.1016/j.jvs.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 40.Murray CJ, Abraham J, Ali MK, Alvarado M, Atkinson C, Baddour LM, Bartels DH, Benjamin EJ, Bhalla K, Birbeck G, Bolliger I, Burstein R, Carnahan E, Chen H, Chou D, Chugh SS, Cohen A, Colson KE, Cooper LT, Couser W, Criqui MH, Dabhadkar KC, Dahodwala N, Danaei G, Dellavalle RP, Des Jarlais DC, Dicker D, Ding EL, Dorsey ER, Duber H, Ebel BE, Engell RE, Ezzati M, Felson DT, Finucane MM, Flaxman S, Flaxman AD, Fleming T, Forouzanfar MH, Freedman G, Freeman MK, Gabriel SE, Gakidou E, Gillum RF, Gonzalez-Medina D, Gosselin R, Grant B, Gutierrez HR, Hagan H, Havmoeller R, Hoffman H, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Kassebaum N, Khatibzadeh S, Knowlton LM, Lan Q, Leasher JL, Lim S, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Macintyre MF, Mallinger L, McDermott MM, Meltzer M, Mensah GA, Michaud C, Miller TR, Mock C, Moffitt TE, Mokdad AA, Mokdad AH, Moran AE, Mozaffarian D, Murphy T, Naghavi M, Narayan KM, Nelson RG, Olives C, Omer SB, Ortblad K, Ostro B, Pelizzari PM, Phillips D, Pope CA, Raju M, Ranganathan D, Razavi H, Ritz B, Rivara FP, Roberts T, Sacco RL, Salomon JA, Sampson U, Sanman E, Sapkota A, Schwebel DC, Shahraz S, Shibuya K, Shivakoti R, Silberberg D, Singh GM, Singh D, Singh JA, Sleet DA, Steenland K, Tavakkoli M, Taylor JA, Thurston GD, Towbin JA, Vavilala MS, Vos T, Wagner GR, Weinstock MA, Weisskopf MG, Wilkinson JD, Wulf S, Zabetian A, Lopez AD US Burden of Disease Collaborators. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM, Jr, White CJ, White J, White RA. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease. Circulation. 2006;113:e463–e654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- 42.Sweeting MJ, Thompson SG, Brown LC, Powell JT RESCAN Collaborators. Meta-analysis of individual patient data to examine factors affecting growth and rupture of small abdominal aortic aneurysms. Br J Surg. 2012;99:655–665. doi: 10.1002/bjs.8707. [DOI] [PubMed] [Google Scholar]
- 43.Di Eusanio M, Trimarchi S, Patel HJ, Hutchison S, Suzuki T, Peterson MD, Di Bartolomeo R, Folesani G, Pyeritz RE, Braverman AC, Montgomery DG, Isselbacher EM, Nienaber CA, Eagle KA, Fattori R. Clinical presentation, management, and short-term outcome of patients with type A acute dissection complicated by mesenteric malperfusion: observations from the International Registry of Acute Aortic Dissection. J Thorac Cardiovasc Surg. 2013;145:385–390. e1. doi: 10.1016/j.jtcvs.2012.01.042. [DOI] [PubMed] [Google Scholar]
- 44.Trimarchi S, Tolenaar JL, Tsai TT, Froehlich J, Pegorer M, Upchurch GR, Fattori R, Sundt TM, 3rd, Isselbacher EM, Nienaber CA, Rampoldi V, Eagle KA. Influence of clinical presentation on the outcome of acute B aortic dissection: evidences from IRAD. J Cardiovasc Surg (Torino) 2012;53:161–168. [PubMed] [Google Scholar]
- 45.Goodney PP, Travis L, Lucas FL, Fillinger MF, Goodman DC, Cronenwett JL, Stone DH. Survival after open versus endovascular thoracic aortic aneurysm repair in an observational study of the Medicare population. Circulation. 2011;124:2661–2669. doi: 10.1161/CIRCULATIONAHA.111.033944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Goodney PP, Brooke BS, Wallaert J, Travis L, Lucas FL, Goodman DC, Cronenwett JL, Stone DH. Thoracic endovascular aneurysm repair, race, and volume in thoracic aneurysm repair. J Vasc Surg. 2013;57:56–63. 63.e1. doi: 10.1016/j.jvs.2012.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Karkos CD, Sutton AJ, Bown MJ, Sayers RD. A meta-analysis and metaregression analysis of factors influencing mortality after endovascular repair of ruptured abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2011;42:775–786. doi: 10.1016/j.ejvs.2011.07.028. [DOI] [PubMed] [Google Scholar]
- 48.Lederle FA, Freischlag JA, Kyriakides TC, Matsumura JS, Padberg FT, Jr, Kohler TR, Kougias P, Jean-Claude JM, Cikrit DF, Swanson KM OVER Veterans Affairs Cooperative Study Group. Long-term comparison of endovascular and open repair of abdominal aortic aneurysm. N Engl J Med. 2012;367:1988–1997. doi: 10.1056/NEJMoa1207481. [DOI] [PubMed] [Google Scholar]
- 49.Jackson RS, Chang DC, Freischlag JA. Comparison of long-term survival after open vs endovascular repair of intact abdominal aortic aneurysm among Medicare beneficiaries. JAMA. 2012;307:1621–1628. doi: 10.1001/jama.2012.453. [DOI] [PubMed] [Google Scholar]
21. Peripheral Artery Disease
ICD-9: 440.20 to 440.24, 440.30 to 440.32, 440.4, 440.9, 443.9, 445.02; ICD-10: I70.2, I70.9, I73.9, I74.3, I74.4. See Table 21-1 and Charts 21-1 and 21-2.
Table 21-1.
Peripheral Artery Disease Table 21-1. Peripheral Artery Disease
| Population Group | Prevalence, Age ≥40 y | Mortality, 2010, All Ages* | Hospital Discharges, 2010, All Ages |
|---|---|---|---|
| Both sexes | ≥6.8 Million | 13 854 | 146 000 |
| Males | … | 5826 (42.1%)† | 84 000 |
| Females | … | 8028 (57.9%)† | 62 000 |
| NH white males | … | 5074 | … |
| NH white females | … | 7045 | … |
| NH black males | … | 648 | … |
| NH black females | … | 868 | … |
| Asian or Pacific Islander | … | 172 | … |
| American Indian/Alaska Native | … | 47 | … |
Ellipses (…) indicate data not available; and NH, non-Hispanic.
Mortality data for the white, black, Asian or Pacific Islander, and American Indian or Alaska Native populations include deaths among people of Hispanic and non-Hispanic origin. Numbers of deaths for the American Indian or Alaska Native and Asian or Pacific Islander populations are known to be underestimated.
These percentages represent the portion of total mortality attributable to heart failure that is for males vs females.
Sources: Prevalence: Allison et al.1 Prevalence of peripheral arterial disease is based on an ankle-brachial index <0.9 or a previous revascularization for peripheral arterial disease. Mortality: Centers for Disease Control and Prevention/National Center for Health Statistics, 2010 Mortality Multiple Cause-of-Death–United States, version dated May 21, 2013.
Chart 21-1.
Prevalence estimates for peripheral arterial disease in males by age and ethnicity. Amer. indicates American; and NH, non-Hispanic. Source: Reprinted from Allison et al1 with permission from Elsevier. Copyright © 2007, American Journal of Preventive Medicine.
Chart 21-2.
Prevalence estimates for peripheral arterial disease in females by age and ethnicity. Amer. indicates American; and NH, non-Hispanic. Source: Reprinted from Allison et al1 with permission from Elsevier. Copyright © 2007, American Journal of Preventive Medicine.
Prevalence and Incidence
(See Table 21-1 and Charts 21-1 and 21-2.)
PAD affects ≈8.5 million Americans aged ≥40 years and is associated with significant morbidity and mortality.1
The age-standardized prevalence rate of PAD per 100 000 in 2010 was 185.6 (95% CI, 150.3–226.1), with minimal change (median percent change, 0.19% [95% CI, −24.1% to 31.6%]) since 1990. The age-standardized disability-adjusted life-year rate of PAD per 100 000 in 2010 was 23.9 (95% CI, 15.7–38.3), with a median change of 24.9% since 1990.2
The highest prevalence of PAD has been observed among elderly people, non-Hispanic blacks, and women. In a multivariable age-, sex-, and race/ethnicity-adjusted regression model, hypertension, DM, CKD, and smoking were associated with incident PAD (P≤0.05 for each).3,4
A 2003 to 2008 sample of US national insurance claims of adults aged >40 years demonstrated that 263 270 eligible individuals had a PAD diagnosis, with an annual incidence and prevalence of 2.76% (95% CI, 2.75%–2.77%) and 12.29% (95% CI, 12.8%–12.31%), respectively.5
In the general population, only ≈10% of people with PAD have the classic symptom of intermittent claudication. Approximately 40% do not complain of leg pain, whereas the remaining 50% have a variety of leg symptoms different from classic claudication.6,7 Data from NHANES 1999 to 2002 suggest that up to two thirds of US adults with PAD who are ≥40 years old are asymptomatic, with one fourth having severe PAD (ABI <0.7).8 In an older, disabled population of women, as many as two thirds of individuals with PAD had no exertional leg symptoms.9
Abbreviations Used in Chapter 21
| ABI | ankle brachial index |
| AHA | American Heart Association |
| Amer. | American |
| CHD | coronary heart disease |
| CI | confidence interval |
| CKD | chronic kidney disease |
| CVD | cardiovascular disease |
| DM | diabetes mellitus |
| ED | emergency department |
| GBD | Global Burden of Diseases, Injuries, and Risk Factors Study |
| HR | hazard ratio |
| ICD-9 | International Classification of Diseases, 9th Revision |
| ICD-10 | International Classification of Diseases, 10th Revision |
| MI | myocardial infarction |
| NCHS | National Center for Health Statistics |
| NH | non-Hispanic |
| NHANES | National Health and Nutrition Examination Survey |
| NHAMCS | National Hospital Ambulatory Medical Care Survey |
| NHDS | National Hospital Discharge Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| OR | odds ratio |
| PA | physical activity |
| PAD | peripheral artery disease |
| REACH | Reduction of Atherothrombosis for Continued Health |
| RR | relative risk |
| YLL | years of life lost |
Mortality
(See Table 21-1.)
In 2010, PAD any-mention mortality was 62 955 (29 213 males and 33 742 females). PAD was the underlying cause in 13 854 of those deaths in 2010.10 Table 21-1 shows the numbers of these deaths that were coded for PAD as the underlying cause.
The 2010 overall any-mention age-adjusted death rate for PAD was 18.9 per 100 000. Any-mention death rates were 22.3 for white males, 26.9 for black males, 16.4 for white females, and 19.6 for black females.11
The number of any-mention deaths attributable to PAD was higher in 2000 (96 551) than in 2010 (62 955; NCHS, AHA).11
Data from the GBD project suggest that the age-standardized death rate attributable to PAD was 1.7 (95% CI, 1.0–2.9) per 100 000, with a 42% median increase since 1990. The YLL because of PAD was 21.2 (95% CI, 13.4–35.9), with a 29% median increase since 1990.2
A 2008 meta-analysis of 24 955 men and 23 339 women demonstrated that the association of the ABI with mortality has a reverse J-shaped distribution in which participants with an ABI of 1.11 to 1.40 are at lowest risk for mortality. Low ABI (≤0.9) carried a 3-fold (RR, 3.33; 95% CI, 2.74–4.06) risk of all-cause death compared with men with normal ABI (1.11–1.40) and a similar risk in women (RR, 2.71; 95% CI, 2.03–3.62).12
Among 508 patients (449 men) identified from 2 vascular laboratories in San Diego, CA, a decline in ABI of >0.15 within a 10-year period was associated with a subsequent increased risk of all-cause mortality (RR, 2.4; 95% CI, 1.2–4.8) and CVD mortality (RR, 2.8; 95% CI, 1.3–6.0) at 3 years’ follow-up.13
Among 440 patients with PAD, male sex and smoking were more associated with aortoiliac (proximal) disease than with infrailiac (distal) disease. In addition, aortoiliac disease was associated with an increased risk of mortality or cardiovascular events compared with infrailiac disease (adjusted HR, 3.28; 95% CI, 1.87–5.75).14
Risk Factors
The risk factors for PAD are similar but not identical to those for CHD. DM and cigarette smoking are stronger risk factors for PAD than for CHD.15 ORs for associations of DM and smoking with symptomatic PAD are ≈3.0 to 4.0. Most studies suggest that the prevalence of PAD is similar in men and women.16
Pooled data from 11 studies in 6 countries found that PAD (defined by ABI <0.9) is a marker for systemic atherosclerotic disease. The pooled age-, sex-, risk factor–, and CVD-adjusted RR for all-cause death was 1.60 (95% CI, 1.32–1.95), the RR for cardiovascular mortality was 1.96 (95% CI, 1.46–2.64), the RR for CHD was 1.45 (95% CI, 1.08–1.93), and the RR for stroke was 1.35 (95% CI, 1.10–1.65).17
Awareness and Aftermath
A cross-sectional, population-based telephone survey of >2500 adults ≥50 years of age, with oversampling of blacks and Hispanics, found that 26% expressed familiarity with PAD. Of these, half were not aware that DM and smoking increase the risk of PAD. One in 4 knew that PAD is associated with increased risk of MI and stroke, and only 14% were aware that PAD could lead to amputation. All knowledge domains were lower in individuals with lower income and education levels.18
People with PAD have impaired function and quality of life. This is true even for people who do not report leg symptoms. Furthermore, patients with PAD, including those who are asymptomatic, experience a significant decline in lower-extremity functioning over time.19–21
Among patients with established PAD, higher PA levels during daily life are associated with better overall survival rate, a lower risk of death because of CVD, and slower rates of functional decline.22,23 In addition, better 6-minute walk performance and faster walking speed are associated with lower rates of all-cause mortality, cardiovascular mortality, and mobility loss.24,25
From 2000 to 2008, the overall use of lower-extremity amputation decreased significantly during the study period, from 7258 to 5790 per 100 000 Medicare beneficiaries with PAD. There was significant geographic variation in the rate of lower-extremity amputation, from 8400 amputations per 100 000 patients with PAD in the East South Central region to 5500 amputations per 100 000 patients with PAD in the Mountain region. After adjustment for clustering at the US Census Bureau level, geographic variation in lower-extremity amputations remained. Lower-extremity amputation was performed more often in the East South Central region (adjusted OR, 1.152; 95% CI, 1.131–1.174; P< 0.001) and West South Central region (adjusted OR, 1.115; 95% CI, 1.097–1.133; P<0.001) and less often in the Middle Atlantic region (OR, 0.833; 95% CI, 0.820–0.847; P<0.001) than in the South Atlantic region.26
A 2003 to 2008 sample of US national insurance claims of adults >40 years of age demonstrated that 44 431 patients had a critical limb ischemic diagnosis over the study period, with an annual incidence and prevalence of 0.47% (95% CI, 0.46–0.47) and 1.90% (95% CI, 1.89–1.91), respectively.5
Interventions
Data from the REACH registry of 8273 PAD participants suggest that only 70% of PAD patients receive lipid-lowering therapy and only 82% receive antiplatelet therapy for secondary CVD prevention.27
-
A 2011 systematic review evaluated lower-extremity aerobic exercise against usual care and demonstrated a range of benefits, including the following28:
Increased claudication time by 71 seconds (79%) to 918 seconds (422%)
Increased claudication distance by 15 m (5.6%) to 232 m (200%)
Increased walking distance/time by 67% to 101% after 40 minutes of walking 2 to 3 times per week
Hospital Discharges
(See Table 21-1.)
Hospital discharges for PAD slightly increased from 2000 to 2010, with first-listed discharges of 135 000 and 146 000, respectively (unreliable estimate, NHDS, NHLBI tabulation).29
In 2010, there were 1 539 000 physician office visits with a primary diagnosis of PAD.29 In 2010, there were 20 000 ED visits and 109 000 outpatient department visits for PAD (NHAMCS, NHLBI tabulation).30
- 1.Allison MA, Ho E, Denenberg JO, Langer RD, Newman AB, Fabsitz RR, Criqui MH. Ethnic-specific prevalence of peripheral arterial disease in the United States. Am J Prev Med. 2007;32:328–333. doi: 10.1016/j.amepre.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 2.Murray CJ, Abraham J, Ali MK, Alvarado M, Atkinson C, Baddour LM, Bartels DH, Benjamin EJ, Bhalla K, Birbeck G, Bolliger I, Burstein R, Carnahan E, Chen H, Chou D, Chugh SS, Cohen A, Colson KE, Cooper LT, Couser W, Criqui MH, Dabhadkar KC, Dahodwala N, Danaei G, Dellavalle RP, Des Jarlais DC, Dicker D, Ding EL, Dorsey ER, Duber H, Ebel BE, Engell RE, Ezzati M, Felson DT, Finucane MM, Flaxman S, Flaxman AD, Fleming T, Forouzanfar MH, Freedman G, Freeman MK, Gabriel SE, Gakidou E, Gillum RF, Gonzalez-Medina D, Gosselin R, Grant B, Gutierrez HR, Hagan H, Havmoeller R, Hoffman H, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Kassebaum N, Khatibzadeh S, Knowlton LM, Lan Q, Leasher JL, Lim S, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Macintyre MF, Mallinger L, McDermott MM, Meltzer M, Mensah GA, Michaud C, Miller TR, Mock C, Moffitt TE, Mokdad AA, Mokdad AH, Moran AE, Mozaffarian D, Murphy T, Naghavi M, Narayan KM, Nelson RG, Olives C, Omer SB, Ortblad K, Ostro B, Pelizzari PM, Phillips D, Pope CA, Raju M, Ranganathan D, Razavi H, Ritz B, Rivara FP, Roberts T, Sacco RL, Salomon JA, Sampson U, Sanman E, Sapkota A, Schwebel DC, Shahraz S, Shibuya K, Shivakoti R, Silberberg D, Singh GM, Singh D, Singh JA, Sleet DA, Steenland K, Tavakkoli M, Taylor JA, Thurston GD, Towbin JA, Vavilala MS, Vos T, Wagner GR, Weinstock MA, Weisskopf MG, Wilkinson JD, Wulf S, Zabetian A, Lopez AD US Burden of Disease Collaborators. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eraso LH, Fukaya E, Mohler ER, 3rd, Xie D, Sha D, Berger JS. Peripheral arterial disease, prevalence and cumulative risk factor profile analysis. [Accessed June 27, 2013];Eur J Prev Cardiol. 2012 Jun 27; doi: 10.1177/2047487312452968. http://cpr.sagepub.com/content/early/2012/06/26/2047487312452968.full.pdf. [DOI] [PMC free article] [PubMed]
- 4.Ostchega Y, Paulose-Ram R, Dillon CF, Gu Q, Hughes JP. Prevalence of peripheral arterial disease and risk factors in persons aged 60 and older: data from the National Health and Nutrition Examination Survey 1999–2004. J Am Geriatr Soc. 2007;55:583–589. doi: 10.1111/j.1532-5415.2007.01123.x. [DOI] [PubMed] [Google Scholar]
- 5.Nehler MR, Duval S, Zakharyan A, Annex BH, Diao L, Hiatt WR, Hirsch AT. Incidence and prevalence of peripheral artery disease and critical limb ischemia in an insured national population. Circulation. 2012;126:A12761. doi: 10.1016/j.jvs.2014.03.290. Abstract. [DOI] [PubMed] [Google Scholar]
- 6.Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, Krook SH, Hunninghake DB, Comerota AJ, Walsh ME, McDermott MM, Hiatt WR. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286:1317–1324. doi: 10.1001/jama.286.11.1317. [DOI] [PubMed] [Google Scholar]
- 7.McDermott MM, Greenland P, Liu K, Guralnik JM, Criqui MH, Dolan NC, Chan C, Celic L, Pearce WH, Schneider JR, Sharma L, Clark E, Gibson D, Martin GJ. Leg symptoms in peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA. 2001;286:1599–1606. doi: 10.1001/jama.286.13.1599. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Lower extremity disease among persons aged > or =40 years with and without diabetes: United States, 1999–2002. MMWR Morb Mortal Wkly Rep. 2005;54:1158–1160. [PubMed] [Google Scholar]
- 9.McDermott MM, Fried L, Simonsick E, Ling S, Guralnik JM. Asymptomatic peripheral arterial disease is independently associated with impaired lower extremity functioning: the Women’s Health and Aging Study [published correction appears in Circulation. 2001;104:504] Circulation. 2000;101:1007–1012. doi: 10.1161/01.cir.101.9.1007. [DOI] [PubMed] [Google Scholar]
- 10.Murphy SL, Xu JQ, Kochanek KD. National Vital Statistics Report. 4. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2013. Deaths: final data for 2010. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention, National Center for Health Statistics. CDC WONDER Online Database [database online] Atlanta, GA: Centers for Disease Control and Prevention; [Accessed July 18, 2012]. Compressed mortality file: underlying cause of death. Released January 2013. http://wonder.cdc.gov/mortSQl.html. [Google Scholar]
- 12.Fowkes FG, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, Folsom AR, Hirsch AT, Dramaix M, deBacker G, Wautrecht JC, Kornitzer M, Newman AB, Cushman M, Sutton-Tyrrell K, Lee AJ, Price JF, d’Agostino RB, Murabito JM, Norman PE, Jamrozik K, Curb JD, Masaki KH, Rodriguez BL, Dekker JM, Bouter LM, Heine RJ, Nijpels G, Stehouwer CD, Ferrucci L, McDermott MM, Stoffers HE, Hooi JD, Knottnerus JA, Ogren M, Hedblad B, Witteman JC, Breteler MM, Hunink MG, Hofman A, Criqui MH, Langer RD, Fronek A, Hiatt WR, Hamman R, Resnick HE, Guralnik J, McDermott MM Ankle Brachial Index Collaboration. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA. 2008;300:197–208. doi: 10.1001/jama.300.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Criqui MH, Ninomiya JK, Wingard DL, Ji M, Fronek A. Progression of peripheral arterial disease predicts cardiovascular disease morbidity and mortality. J Am Coll Cardiol. 2008;52:1736–1742. doi: 10.1016/j.jacc.2008.07.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aboyans V, Desormais I, Lacroix P, Salazar J, Criqui MH, Laskar M. The general prognosis of patients with peripheral arterial disease differs according to the disease localization. J Am Coll Cardiol. 2010;55:898–903. doi: 10.1016/j.jacc.2009.09.055. [DOI] [PubMed] [Google Scholar]
- 15.Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM, Jr, White CJ, White J, White RA. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease. Circulation. 2006;113:e463–e654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- 16.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) J Vasc Surg. 2007;45(suppl S):S5–S67. doi: 10.1016/j.jvs.2006.12.037. [DOI] [PubMed] [Google Scholar]
- 17.Heald CL, Fowkes FG, Murray GD, Price JF Ankle Brachial Index Collaboration. Risk of mortality and cardiovascular disease associated with the ankle-brachial index: systematic review. Atherosclerosis. 2006;189:61–69. doi: 10.1016/j.atherosclerosis.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 18.Hirsch AT, Murphy TP, Lovell MB, Twillman G, Treat-Jacobson D, Harwood EM, Mohler ER, 3rd, Creager MA, Hobson RW, 2nd, Robertson RM, Howard WJ, Schroeder P, Criqui MH Peripheral Arterial Disease Coalition. Gaps in public knowledge of peripheral arterial disease: the first national PAD public awareness survey. Circulation. 2007;116:2086–2094. doi: 10.1161/CIRCULATIONAHA.107.725101. [DOI] [PubMed] [Google Scholar]
- 19.McDermott MM, Greenland P, Liu K, Guralnik JM, Celic L, Criqui MH, Chan C, Martin GJ, Schneider J, Pearce WH, Taylor LM, Clark E. The ankle brachial index is associated with leg function and physical activity: the Walking and Leg Circulation Study [published correction appears in Ann Intern Med. 2003;139:306] Ann Intern Med. 2002;136:873–883. doi: 10.7326/0003-4819-136-12-200206180-00008. [DOI] [PubMed] [Google Scholar]
- 20.McDermott MM, Liu K, Greenland P, Guralnik JM, Criqui MH, Chan C, Pearce WH, Schneider JR, Ferrucci L, Celic L, Taylor LM, Vonesh E, Martin GJ, Clark E. Functional decline in peripheral arterial disease: associations with the ankle brachial index and leg symptoms. JAMA. 2004;292:453–461. doi: 10.1001/jama.292.4.453. [DOI] [PubMed] [Google Scholar]
- 21.McDermott MM, Guralnik JM, Tian L, Liu K, Ferrucci L, Liao Y, Sharma L, Criqui MH. Associations of borderline and low normal ankle-brachial index values with functional decline at 5-year follow-up: the WALCS (Walking and Leg Circulation Study) J Am Coll Cardiol. 2009;53:1056–1062. doi: 10.1016/j.jacc.2008.09.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garg PK, Tian L, Criqui MH, Liu K, Ferrucci L, Guralnik JM, Tan J, McDermott MM. Physical activity during daily life and mortality in patients with peripheral arterial disease. Circulation. 2006;114:242–248. doi: 10.1161/CIRCULATIONAHA.105.605246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garg PK, Liu K, Tian L, Guralnik JM, Ferrucci L, Criqui MH, Tan J, McDermott MM. Physical activity during daily life and functional decline in peripheral arterial disease. Circulation. 2009;119:251–260. doi: 10.1161/CIRCULATIONAHA.108.791491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McDermott MM, Guralnik JM, Tian L, Ferrucci L, Liu K, Liao Y, Criqui MH. Baseline functional performance predicts the rate of mobility loss in persons with peripheral arterial disease. J Am Coll Cardiol. 2007;50:974–982. doi: 10.1016/j.jacc.2007.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McDermott MM, Tian L, Liu K, Guralnik JM, Ferrucci L, Tan J, Pearce WH, Schneider JR, Criqui MH. Prognostic value of functional performance for mortality in patients with peripheral artery disease. J Am Coll Cardiol. 2008;51:1482–1489. doi: 10.1016/j.jacc.2007.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones WS, Patel MR, Dai D, Subherwal S, Stafford J, Calhoun S, Peterson ED. Temporal trends and geographic variation of lower-extremity amputation in patients with peripheral artery disease: results from U.S. Medicare 2000–2008. J Am Coll Cardiol. 2012;60:2230–2236. doi: 10.1016/j.jacc.2012.08.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, Goto S, Liau CS, Richard AJ, Röther J, Wilson PW REACH Registry Investigators. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006;295:180–189. doi: 10.1001/jama.295.2.180. [DOI] [PubMed] [Google Scholar]
- 28.Parmenter BJ, Raymond J, Dinnen P, Singh MA. A systematic review of randomized controlled trials: walking versus alternative exercise prescription as treatment for intermittent claudication. Atherosclerosis. 2011;218:1–12. doi: 10.1016/j.atherosclerosis.2011.04.024. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention, National Center for Health Statistics. 2010 National Ambulatory Medical Care Survey and 2010 National Hospital Ambulatory Medical Care Survey. [Accessed July 17, 2013];Ambulatory health care data: questionnaires, datasets, and related documentation. For methodology, see National Center for Health Statistics, Public Use Data File Documentation: 2010 National Ambulatory Medical Care Survey and Public Use Data File Documentation: 2010 National Hospital Ambulatory Medical Care Survey. http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
- 30.Centers for Disease Control and Prevention, National Center for Health Statistics. 2009 National Ambulatory Medical Care Survey and 2009 National Hospital Ambulatory Medical Care Survey. [Accessed August 12, 2011];Ambulatory health care data: questionnaires, datasets, and related documentation. For methodology, see National Center for Health Statistics, Public Use Data File Documentation: 2009 National Ambulatory Medical Care Survey and Public Use Data File Documentation: 2009 National Hospital Ambulatory Medical Care Survey. http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
22. Quality of Care
See Tables 22-1 through 22-14.
Table 22-1.
ACS Quality-of-Care Measures, 2012
| Quality-of-Care Measure | VHA* | National Data From HIQR Program† | ACTION-GWTG STEMI‡ | ACTION-GWTG NSTEMI‡ |
|---|---|---|---|---|
| Aspirin within 24 h of admission | 99 | 99.2 | 98.3 | 97.5 |
| Aspirin at discharge | 99 | 99.1 | 98.9 | 98.1 |
| β-Blockers at discharge | 99 | 98.9 | 97.8 | 96.7 |
| Lipid-lowering medication at discharge§ | 99 | 97.7 | 99.1 | 98.5 |
| ARB/ACEI at discharge for patients with LVEF <40% | 97 | 97.5 | 91.4 | 88.3 |
| ACEI at discharge for AMI patients | NM | NM | 71.6 | 59.6 |
| ARB at discharge for AMI patients | NM | NM | 9.2 | 13.3 |
| Adult smoking cessation advice/counseling | Retired | 99.7|| | 98.6 | 98.2 |
| Cardiac rehabilitation referral for AMI patients | NM | NM | 82.5 | 73.7 |
Values are percentages.
ACEI indicates angiotensin-converting enzyme inhibitor; ACS, acute coronary syndrome; ACTION-GWTG, Acute Coronary Treatment and Intervention Outcomes Network Registry–Get With The Guidelines; AMI, acute myocardial infarction; ARB, angiotensin receptor blocker; HIQR, Hospital Inpatient Quality Reporting; LVEF, left ventricular ejection fraction; NM, not measured; NSTEMI, non–ST-segment–elevation myocardial infarction; STEMI, ST-segment–elevation myocardial infarction; and VHA, Veterans Health Administration.
VHA: AMI patients. Data reported include data from October 1, 2011, to September 30, 2012.
HIQR Program includes data from all payers, including Medicare and Medicaid. Data reported include data from the third quarter of 2011 to the second quarter of 2012.
ACTION Registry: STEMI and NSTEMI patients are reported separately. Patients must be admitted with acute ischemic symptoms within the previous 24 h, typically reflected by a primary diagnosis of STEMI or NSTEMI. Patients who are admitted for any other clinical condition are not eligible. Data reported include data from the second quarter of 2012 to the first quarter of 2013.
Denotes statin use at discharge. Use of nonstatin lipid-lowering agent was 8.1% for STEMI patients and 11.7% for NSTEMI patients in the ACTION registry.
Measure was retired in January 2012.
Table 22-14.
Quality of Care by Race/Ethnicity and Sex in the GWTG-Stroke Program, 2012
| Quality-of-Care Measure | White | Black | Hispanic | Male | Female |
|---|---|---|---|---|---|
| IV tPA in patients who arrived ≤2 h after symptom onset, treated ≤3 h* | 81.9 | 80.8 | 84.8 | 82.5 | 81.6 |
| IV tPA in patients who arrived <3.5 h after symptom onset, treated ≤4.5 h | 59.9 | 60.0 | 63.0 | 61.3 | 59.6 |
| IV tPA door-to-needle time ≤60 min | 40.0 | 37.6 | 40.8 | 42.0 | 37.8 |
| Thrombolytic complications: IV tPA and life-threatening, serious systemic hemorrhage | 17.0 | 14.8 | 15.2 | 16.4 | 16.5 |
| Antithrombotics <48 h after admission* | 97.0 | 96.6 | 96.5 | 97.1 | 96.7 |
| DVT prophylaxis by second hospital day* | 98.5 | 98.2 | 97.9 | 98.4 | 98.3 |
| Antithrombotics at discharge* | 98.0 | 97.6 | 97.0 | 98.0 | 97.6 |
| Anticoagulation for AF at discharge* | 93.5 | 93.4 | 92.3 | 93.6 | 93.1 |
| Therapy at discharge if LDL cholesterol >100 mg/dL or LDL cholesterol not measured or on therapy at admission* | 94.3 | 94.9 | 94.4 | 95.4 | 93.6 |
| Counseling for smoking cessation* | 97.0 | 96.6 | 96.5 | 96.9 | 96.7 |
| Lifestyle changes recommended for BMI >25 kg/m2 | 56.8 | 56.8 | 63.5 | 57.3 | 57.1 |
| Composite quality-of-care measure | 96.3 | 96.3 | 95.9 | 96.6 | 96.0 |
Values are percentages.
Quality-of-care measures stratified by race/ethnicity and sex are reported for hospitals participating in GWTG from January 1, 2012 through December 31, 2012.
AF indicates atrial fibrillation; BMI, body mass index; DVT, deep vein thrombosis; GWTG-Stroke, Get With The Guidelines–Stroke; IV, intravenous; LDL, low-density lipoprotein; and tPA, tissue-type plasminogen activator.
Indicates the 7 key performance measures targeted in GWTG-Stroke.
The Institute of Medicine defines quality of care as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.”1 The Institute of Medicine has defined 6 specific domains for improving health care, including care that is safe, effective, patient-centered, timely, efficient, and equitable.
In the following sections, data on quality of care will be presented based on the 6 domains of quality as defined by the Institute of Medicine. This is intended to highlight current care and to stimulate efforts to improve the quality of cardiovascular care nationally. Where possible, data are reported from recently published literature or standardized quality indicators from quality-improvement registries (ie, those consistent with the methods for quality performance measures endorsed by the ACC and the AHA).2 Additional data on aspects of quality of care, such as adherence to ACC/AHA clinical practice guidelines, are also included to provide a spectrum of quality-of-care data. The data selected are meant to provide examples of the current quality of care as reflected by the Institute of Medicine domains and are not meant to be comprehensive given the sheer number of publications yearly.
Abbreviations Used in Chapter 22
| ACC | American College of Cardiology |
| ACE | angiotensin-converting enzyme |
| ACEI | angiotensin-converting enzyme inhibitor |
| ACS | acute coronary syndrome |
| ACTION | Acute Coronary Treatment and Intervention Outcomes Network |
| AED | automated external defibrillator |
| AF | atrial fibrillation |
| AHA | American Heart Association |
| AMI | acute myocardial infarction |
| ARB | angiotensin receptor blocker |
| BMI | body mass index |
| BP | blood pressure |
| CABG | coronary artery bypass grafting |
| CAD | coronary artery disease |
| CHD | coronary heart disease |
| CHF | congestive heart failure |
| CI | confidence interval |
| COURAGE | Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation |
| CPR | cardiopulmonary resuscitation |
| CRUSADE | Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines |
| CVD | cardiovascular disease |
| D2B | Door-to-Balloon (Alliance) |
| DES | drug-eluting stent |
| DM | diabetes mellitus |
| DVT | deep vein thrombosis |
| ECG | electrocardiogram |
| ED | emergency department |
| EF | ejection fraction |
| EMS | emergency medical services |
| GBD | Global Burden of Diseases, Injuries, and Risk Factors Study |
| GWTG | Get With The Guidelines |
| HbA1c | hemoglobin A1c (glycosylated hemoglobin) |
| HD | heart disease |
| HF | heart failure |
| HIQR | Hospital Inpatient Quality Reporting |
| HR | hazard ratio |
| IV | intravenous |
| LDL | low-density lipoprotein |
| LV | left ventricular |
| LVEF | left ventricular ejection fraction |
| LVSD | left ventricular systolic dysfunction |
| MI | myocardial infarction |
| N/A | not available or not applicable |
| NCDR | National Cardiovascular Data Registry |
| NHANES | National Health and Nutrition Examination Survey |
| NM | not measured |
| NSTEMI | non–ST-segment–elevation myocardial infarction |
| OR | odds ratio |
| PAD | peripheral artery disease |
| PCI | percutaneous coronary intervention |
| PINNACLE | Practice Innovation and Clinical Excellence |
| RR | relative risk |
| SBP | systolic blood pressure |
| SCD-HeFT | Sudden Cardiac Death in Heart Failure Trial |
| STEMI | ST-segment–elevation myocardial infarction |
| STS | Society of Thoracic Surgeons |
| TAVR | transcatheter aortic valve replacement |
| tPA | tissue-type plasminogen activator |
| TVR | target-vessel revascularization |
| TVT | transcatheter valve therapy |
| UFH | unfractionated heparin |
| VHA | Veterans Health Administration |
| YLL | years of life lost |
-
The safety domain has been defined as avoiding injuries to patients from the care that is intended to help them. The following are several publications that have focused on safety issues:
In a small, single-center study conducted over a 2-month period in the cardiac care unit of a tertiary center, Rahim et al3 demonstrated that iatrogenic adverse events were common (99 of 194 patients), of which bleeding (27%) was the most common preventable iatrogenic adverse event.
Using the NCDR CathPCI Registry, Tsai et al4 found that almost one fourth of dialysis patients undergoing PCI (n=22 778) received a contraindicated antithrombotic agent, specifically enoxaparin, eptifibatide, or both. Patients who received a contraindicated antithrombotic agent had an increased risk of in-hospital bleeding (OR, 1.63; 95% CI, 1.35–1.98) and a trend toward increased mortality (OR, 1.15; 95% CI, 0.97–1.36).4
Using data from the ACTION Registry-GWTG, Mathews and colleagues developed a contemporary model to stratify in-hospital bleeding risk for patients after STEMI and NSTEMI.5 The 12 factors associated with major bleeding in the model were heart rate, baseline hemoglobin, female sex, baseline serum creatinine, age, electrocardiographic changes, HF or shock, DM, PAD, body weight, SBP, and home warfarin use. The risk model discriminated well in the derivation (C statistic= 0.73) and validation (C statistic=0.71) cohorts, and the risk score for major bleeding corresponded well with observed bleeding.5
In a random sample of medical and surgical long-term care adult patients in Massachusetts hospitals, López et al6 assessed the association between disclosure of an adverse event and patients’ perception of quality of care. Overall, only 40% of adverse events were disclosed. Higher quality ratings were associated with disclosure of an adverse event. Conversely, lower patient perception of quality of care was associated with events that were preventable and with events that caused discomfort.6
Using prospective propensity-matched cohort analysis of 7 newly introduced cardiovascular devices, Resnic et al7 showed the feasibility of automated prospective surveillance to identify low-frequency safety signals in a cardiovascular registry. In this study, 3 of the 21 safety alerts triggered sustained alerts in 2 implantable devices.7
-
Effective care has been defined as providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit. It also encompasses monitoring results of the care provided and using them to improve care for all patients.1 There are many quality-improvement registries that have been developed for inpatient cardiovascular/stroke care, and the data on these are provided in subsequent tables. Similar efforts are under way for quality-of-care registries in the outpatient setting.
According to data from NHANES 1988 to 1994 and 1999 to 2008, prevalence of hypertension increased from 23.9% in 1988 to 1994 to 29.0% in 2007 to 2008, and hypertension control among hypertensive adults has increased from 27.3% in 1988 to 1994 to 50.1% in 2007 to 2008. In addition, among people with hypertension, BP has decreased from 143.0/80.4 to 135.2/74.1 mm Hg.8
Weintraub et al9 reported results from a comparative effectiveness study of PCI versus CABG using observational data among patients ≥65 years of age with 2- or 3-vessel CAD without AMI. Their results showed that at 1 year, there was no significant difference in adjusted mortality between groups (6.24% in the CABG group versus 6.55% in the PCI group). At 4 years, there was lower mortality in the CABG group than in the PCI group (16.4% versus 20.8%; RR, 0.79; 95% CI, 0.76–0.82).9
Appel et al10 reported results of a randomized controlled trial comparing the effectiveness of 2 behavioral weight loss interventions with controls. The interventions included either remote weight loss intervention (delivered through the telephone, a study-specific Web site, and e-mail) or in-person support (individual and group sessions along with the 3 means of remote support). At 24 months, the mean change in weight from baseline was −0.8 kg in the control group, −4.6 kg in the group with remote support only (P<0.001 for comparison with the control group), and −5.1 kg in the group receiving in-person support (P<0.001 for comparison with the control group). The change in weight from baseline did not differ significantly between the 2 intervention groups at the end of the trial.
Choudhry et al11 reported results of a cluster randomized trial that evaluated the impact of eliminating out-of-pocket costs (full prescription coverage) on medication adherence and cardiovascular outcomes in patients discharged after MI. Compared with the usual prescription coverage, rates of adherence to statins, β-blockers, ACE inhibitors, and ARBs were on average 4% to 6% higher in the full-coverage group. There was no significant difference in the primary outcome (first major vascular event or revascularization) between the 2 groups (17.6 per 100 person years in the full-coverage group versus 18.8 in the usual-coverage group; HR, 0.93; 95% CI, 0.82–1.04). The rates of secondary outcomes of total major vascular events or revascularization were significantly reduced in the full-coverage group (21.5 versus 23.3; HR, 0.89; 95% CI, 0.90–0.99), as was the rate of first major vascular event (11 versus 12.8; HR, 0.86; 95% CI, 0.74–0.99). The elimination of copayments did not increase total spending, although patient costs were reduced for drugs and other services.
Data from the ACC PINNACLE outpatient registry12 of patients with CAD (n=38 775) showed that 77.8% of the patients (30 160) were prescribed statins, 2042 (5.3%) were treated only with nonstatin lipid-lowering medications, and 6573 (17%) were not taking any lipid-lowering medication. Lack of medical insurance (RR, 0.94; 95% CI, 0.89–1.00) was associated with a lower likelihood of statin treatment, whereas male sex (RR, 1.10; 95% CI, 1.07–1.13), coexisting hypertension (RR, 1.07; 95% CI, 1.02–1.12), prior CABG (RR, 1.09; 95% CI, 1.05–1.14), and prior PCI (RR, 1.11; 95% CI, 1.06–1.16) were associated with a higher likelihood of statin treatment.
In patients recently hospitalized with HF, a randomized clinical trial did not show improvement in the primary end point (readmission for any reason or death of any cause within 180 days after enrollment) or the secondary end points (hospitalization for HF, number of days in the hospital, and number of hospitalizations) with the use of telemonitoring.13 Similar results were seen in a randomized clinical trial of remote telemedical management in patients with chronic HF.14
Heisler et al15 reported results of a prospective, multisite, cluster randomized trial that evaluated the effectiveness of a pharmacist-led intervention that targeted medication management and adherence counseling to improve BP control in patients with DM in 2 high-performing integrated healthcare systems. Although the mean SBP of patients in the intervention arm was 2.4 mm Hg lower (95% CI, −3.4 to −1.5; P<0.001) immediately after the intervention than that of patients in the control arm, the mean SBP decrease from 6 months before to 6 months after the intervention (primary outcome) was similar in magnitude (≈9 mm Hg) in both arms.15
In 2013, investigators from the GBD 2010 study described their findings of a systematic analysis of disease burden, injuries, and leading risk factors in the United States and compared them with those of 34 countries in the Organisation for Economic Co-operation and Development.16 Their findings showed that the US life expectancy for both sexes combined increased from 75.2 years in 1990 to 78.2 years in 2010. During the same time period, healthy life expectancy (the number of years that a person at a given age can expect to live in good health, taking into account mortality and disability) increased from 65.8 years to 68.1 years in the United States. Despite declines in the YLLs because of premature mortality secondary to ischemic HD and stroke, 15.9% of YLLs were related to ischemic HD and 4.3% of YLLs were related to stroke in the United States in 2010, which highlights the continued dominance of CVD in causing premature death. Despite these absolute improvements, the US rank among 34 countries in the Organisation for Economic Co-operation and Development changed from 18th to 27th for the age-standardized death rate, from 20th to 27th for life expectancy at birth, from 14th to 26th for healthy life expectancy, and from 23rd to 28th for the age-standardized YLL. These results indicate that improvements in population health in the United States have not kept pace with advances in population health in other wealthy nations.
Outcome measures of 30-day mortality and 30-day readmission after hospitalization for AMI or HF have been developed that adjust for patient mix (eg, comorbidities) so that comparisons can be made across hospitals.17 Using national Medicare data from 2008 through 2010, the median (10th, 90th percentile) hospital risk-standardized mortality rate was 15.7% (13.7%, 17.7%) for AMI and 11.5% (9.7%, 13.5%) for HF. The median risk-standardized readmission rate was 19.7% (18.0%, 21.7%) for AMI and 24.7% (22.6%, 27.3%) for HF. Distinct regional patterns were seen for both measures and both conditions. The median risk-standardized mortality rate for AMI decreased by 0.7% from 2008 to 2010, whereas the median risk-standardized mortality rate for HF increased by 0.4%. The median risk-standardized readmission rate for AMI and HF declined by 0.5% and 0.3%, respectively, from 2008 to 2010.17
A study of 30 947 patients admitted with ischemic strokes showed that admission to a designated stroke center compared with admission to a nondesignated hospital was associated with more frequent use of thrombolytic therapy (4.8% versus 1.7%, P<0.001) and lower 30-day all-cause mortality (10.1% versus 12.5%, P<0.001).18
A study of 458 hospitals participating in the STS National Cardiac Database showed that an intervention of receiving quality-improvement educational material designed to influence the prescription rates of 4 medication classes (aspirin, β-blockers, lipid-lowering therapy, and ACE inhibitors) after CABG discharge in addition to site-specific feedback reports led to a significant improvement in adherence for all 4 secondary prevention medications at the intervention sites compared with the control sites.19
In 2011, the ACC Foundation/AHA/American Medical Association–Physician Consortium for Performance Improvement published a joint report on performance measures for CAD and hypertension.20 The 9 performance measures for CAD care included BP control, lipid control, symptom and activity assessment, symptom management, tobacco use (screening, cessation, and intervention), antiplatelet therapy, β-blocker therapy, ACE inhibitor/ARB therapy, and cardiac rehabilitation patient referral from an outpatient setting. For hypertension care, the performance measures included BP control. This set was an update to the 2005 ACC Foundation/AHA performance measures for CAD and hypertension and included modifications to 7 of the 2005 performance measures. Screening for DM was retired from the CAD set published in 2005, whereas symptom management and cardiac rehabilitation referral were added to the 2011 CAD set. Similarly, the ACC Foundation/AHA/American Medical Association–Physician Consortium for Performance Improvement published a report on performance measures for HF,21 which was an update to the 2005 report.22 Eight measures from the 2005 report were retired, β-blocker use in patients with HF was expanded as a performance measure for the inpatient setting, symptom management and counseling about implantable cardioverter-defibrillators were added as new quality metrics, and patient education was changed from a performance measure to a quality metric.
A study from the PINNACLE registry of NCDR showed that uninsured patients with CAD were 9%, 12%, and 6% less likely to receive treatment with a β-blocker, an ACE inhibitor/ARB, and lipid-lowering therapy, respectively, than privately insured CAD patients, and CAD patients with public insurance were 9% less likely to be prescribed ACE inhibitor/ARB therapy. Most of the differences were attenuated after adjustment for the site providing care.23
A randomized controlled trial of Transcendental Meditation or health education in 201 black men and women with CHD showed that the Transcendental Meditation program was associated with a 48% reduction in RR (11.2% absolute risk reduction) for the composite primary end point of all-cause mortality, MI, or stroke (HR, 0.52; 95% CI, 0.29–0.92) during an average follow-up of 5.4 years.24
In 2013, a TVT registry was created through a partnership between the STS and the ACC.25 The objective of this registry is to provide an “objective, comprehensive, and scientifically based resource to improve the quality of patient care, to monitor the safety and effectiveness of TVT devices, to serve as an analytic resource for TVT research, and to enhance communication among key stake holders.”
Inpatient ACS, HF, and stroke quality-of-care measures data, including trends in care data, where available from national registries, are given in Tables 22-1 through 22-6.
Selected outpatient quality-of-care measures from the National Committee for Quality Assurance for 2011 appear in Table 22-7.
Quality-of-care measures for patients who had out-of-hospital cardiac arrest and were enrolled in the Resuscitation Outcomes Consortium cardiac arrest registry in 2011 (Resuscitation Outcomes Consortium Investigators, unpublished data, July 25, 2013) are given in Tables 22-8 and 22-9.
Quality-of-care measures for patients who had inhospital cardiac arrest and were enrolled in the AHA’s GWTG-Resuscitation quality-improvement project in 2012 (GWTG-Resuscitation Investigators, unpublished data, July 27, 2013) are given in Table 22-10.
-
Patient-centered care has been defined as the provision of care that is respectful of and responsive to individual patient preferences, needs, and values and that ensures that patient values guide all clinical decisions. Dimensions of patient-centered care include the following: (1) Respect for patients’ values, preferences, and expressed needs; (2) coordination and integration of care; (3) information, communication, and education; (4) physical comfort; (5) emotional support; and (6) involvement of family and friends. Studies that focused on some of these aspects of patient-centered care are highlighted below.
The COURAGE trial,26 which investigated a strategy of PCI plus optimal medical therapy versus optimal medical therapy alone, demonstrated that both groups had significant improvement in health status during follow-up. By 3 months, health status scores had increased in the PCI group compared with the medical therapy group, to 76±24 versus 72±23 for physical limitation (P=0.004), 77±28 versus 73±27 for angina stability (P=0.002), 85±22 versus 80±23 for angina frequency (P<0.001), 92±12 versus 90±14 for treatment satisfaction (P<0.001), and 73±22 versus 68±23 for quality of life (P<0.001). The PCI plus optimal medical therapy group had a small but significant incremental benefit compared with the optimal medical therapy group early on, but this benefit disappeared by 36 months.
In SCD-HeFT,27 a study of a single-lead implantable cardioverter-defibrillator versus amiodarone for moderately symptomatic HF, patients with implantable cardioverter-defibrillators had improvement in quality of life compared with patients who received medical therapy at 3 and 12 months but not at 30 months. Implantable cardioverter-defibrillator shocks in the month preceding a scheduled assessment were associated with a decrease in quality of life in multiple domains. The authors concluded that the presence of a single-lead implantable cardioverter-defibrillator was not associated with any detectably adverse quality of life during 30 months of follow-up.
Peikes et al28 reported on 15 care-coordination programs as part of a Medicare demonstration project for patients with CHF, CAD, DM, and other conditions. Thirteen of the 15 programs did not show a difference in hospitalization rates, and none of the programs demonstrated net savings. The interventions tested varied significantly, but the majority of the interventions included patient education to improve adherence to medication, diet, exercise, and self-care regimens and improving care coordination through various approaches. These programs overall had favorable effects on none of the adherence measures and only a few of the many quality-of-care indicators examined. The authors concluded that programs with substantial in-person contact that target moderately to severely ill patients can be cost-neutral and improve some aspects of care.
Hernandez et al29 showed that patients with outpatient follow-up within 7 days of discharge for an HF hospitalization were less likely to be readmitted within 30 days in the GWTG-HF registry of patients who were ≥65 years of age. The median length of stay was 4 days (interquartile range, 2–6 days), and 21.3% of patients were readmitted within 30 days. At the hospital level, the median percentage of patients who had early follow-up after discharge from the index hospitalization was 38.3% (interquartile range, 32.4%–44.5%).
Smolderen et al30 assessed whether health insurance status affects decisions to seek care for AMI. Uninsured and insured patients with financial concerns were more likely to delay seeking care during AMI and had prehospital delays of >6 hours (48.6% of uninsured patients and 44.6% of insured patients with financial concerns compared with 39.3% of insured patients without financial concerns). Lack of health insurance and financial concerns about accessing care among those with health insurance were each associated with delays in seeking emergency care for AMI.
Using a cohort (n=192) nested within a randomized trial at a university-affiliated ambulatory practice, Murray et al31 demonstrated that refill adherence of <40% was associated with a 3-fold higher incidence of HF hospitalization than refill adherence of ≥80% (P=0.002). In multivariable analysis, prescription label–reading skills were associated with a lower incidence of HF-specific emergency care (incidence rate ratio, 0.76; 95% CI, 0.19–0.69), and participants with adequate health literacy had a lower risk of HF hospitalization (incidence rate ratio, 0.34; 95% CI, 0.15–0.76).
Reynolds et al32 reported results on health-related quality of life after TAVR in inoperable patients with severe aortic stenosis compared with those receiving standard therapy. Health-related quality of life was assessed at baseline and at 1, 6, and 12 months with the Kansas City Cardiomyopathy Questionnaire and the 12-item Short Form-12 General Health Survey. Although the Kansas City Cardiomyopathy Questionnaire summary scores improved in both groups, the extent of improvement was greater in the TAVR group than in the standard-care group at 1 month (mean between-group difference, 13 points; 95% CI, 8–19), with larger benefits at 6 months (mean difference, 21 points; 95% CI, 15–27 points) and 12 months (mean difference, 26 points; 95% CI, 19–33). At 12 months, TAVR patients also reported higher physical and mental health scores on the 12-item Short Form-12 General Health Survey, with a mean difference of 5.7 and 6.4 points, respectively (P<0.001 for both comparisons) compared with standard care.32
In 2012, the AHA published a scientific statement on decision making in advanced HF. This statement discusses the clinical trajectory of HF, importance and process of shared decision making in advanced HF, timing of discussion, discussion on outcomes beyond survival (ie, major adverse events, symptom burden, functional limitations, loss of independence, quality of life, and obligations for caregivers), discussions regarding end-of-life issues, and assessment and integration of emotional readiness of the patient and family in these discussions.33
In 2013, the AHA published a scientific statement on the importance of measuring patient-reported health status across 3 domains (symptom burden, functional status, and health-related quality of life).34 The statement discusses why it is important to measure patient-reported health status measures, the association between measures of patient-reported health status and cardiovascular outcomes, and the currently available tools to measure health status of patients with CVD.
In 2012, the ACC Foundation published a policy statement on patient-centered care in cardiovascular medicine. This policy statement discusses and provides recommendations on topics such as enhanced clinician-patient communication, health literacy, clinician-directed patient education, assessment of patient-centered outcomes, process of shared decision making, collaborative care planning and goal setting, and patient empowerment and self-management. The policy statement also discusses newer paradigms and challenges in patient-centered care, such as the impact of technology, complexity of care strategies with self-care, a systemic approach to episodic care, and barriers to patient-centered care.35
-
The timely care domain relates to reducing waits and sometimes harmful delays for both those who receive and those who give care. Timeliness is an important characteristic of any service and is a legitimate and valued focus of improvement in health care and other industries.
Data from the CRUSADE national quality-improvement initiative showed that median delay from onset of symptoms to hospital presentation for patients presenting with NSTEMI was 2.6 hours and was significantly associated with in-hospital mortality but did not change over time from 2001 to 2006.36
Bradley et al37 demonstrated that participation in the D2B Alliance led to a reduction in door-to-balloon time to within 90 minutes for patients with STEMI. By March 2008, >75% of patients had door-to-balloon times of ≤90 minutes compared with only approximately one fourth of patients in April 2005.
Using data between 2005 and 2007 from the NCDR CathPCI Registry, Wang et al38 demonstrated that among STEMI patients, only 10% of the transfer patients received PCI within 90 minutes (versus 63% for direct-arrival patients; P<0.0001).
Glickman et al39 showed that a year-long implementation of standardized protocols as part of a statewide regionalization program was associated with a significant improvement in median door-in–door-out times among 436 STEMI patients who presented at non-PCI hospitals who required transfer (before intervention: 97 minutes, interquartile range 56–160 minutes; after intervention: 58 minutes, interquartile range 35–90 minutes; P<0.0001).
A recent study40 of 204 591 patients with ischemic and hemorrhagic strokes admitted to 1563 GTWG-Stroke participating hospitals between April 1, 2003, and June 30, 2010, showed that 63.7% of the patients arrived by EMS in the hospital. Older patients, those with Medicaid and Medicare, and those with severe strokes were more likely to activate EMS. Conversely, minority race/ethnicity (black, Hispanic, Asian) and living in rural communities were associated with a lower likelihood of EMS use. EMS transport was independently associated with an onset-to-door time ≤3 hours, a higher proportion of patients meeting door-to-imaging time of ≤25 minutes, more patients meeting a door-to-needle time of ≤60 minutes, and more eligible patients being treated with tPA if onset of symptoms was ≤2 hours. The authors concluded that although EMS use was associated with rapid evaluation and treatment of stroke, more than one third of stroke patients fail to use EMS.
Data on time to reperfusion for STEMI or ischemic stroke are provided from national registries in Table 22-11.
-
Efficiency has been defined as avoiding waste, in particular waste of equipment, supplies, ideas, and energy. In an efficient healthcare system, resources are used to get the best value for the money spent.
The AHA and ACC have jointly developed a scientific statement that outlines standards for measures to be used for public reporting of efficiency in health care. The group identified 4 standards important to the development of any efficiency performance measure, including (1) integration of quality and cost, (2) valid cost measurement and analysis, (3) no or minimal incentive to provide poor-quality care, and (4) no or proper attribution of the measure. In the statement, 4 examples were provided of hospital-based efficiency measures, as well as information on how each of the measures fared within the 4 domains recommended. The examples were length of stay, 30-day readmission, hospitalization costs, and nonrecommended imaging tests.41
Using data from the NCDR CathPCI registry from 2004 through 2010, Amin et al42 examined the association between risk of TVR and use of DES and the cost-effectiveness of lower use of DES in patients at low risk of TVR (<10% TVR risk). The authors showed a marked variation in physicians’ use of DES (range, 2%–100%). Even in groups with low TVR risk, 73.9% of the patients received DES. The authors projected that by reducing the use of DES by 50% in patients at low risk of TVR, US health-care costs could be lowered by $205 million, whereas the overall TVR event rate would be increased by 0.5%.
At an urban, tertiary care, academic medical center ED, elements of departmental work flow were redesigned to streamline patient throughput before implementation of a fully integrated ED information system with patient tracking, computerized charting and order entry, and direct access to patient historical data from the hospital data repository. Increasing the clinical information available at the bedside and improving departmental work flow through ED information system implementation and process redesign led to decreased patient throughput times and improved ED efficiency (eg, the length of stay for all patients [from arrival to time patient left the ED] decreased by 1.94 hours, from 6.69 hours [n=508] before the intervention to 4.75 hours [n=691] after the intervention; P<0.001).43
Himmelstein et al44 analyzed whether more-computerized hospitals had lower costs of care or administration or better quality, to address a common belief that computerization improves healthcare quality, reduces costs, and increases administrative efficiency. They found that hospitals that increased computerization faster had more rapid administrative cost increases (P=0.0001); however, higher overall computerization scores correlated weakly with better quality scores for AMI (r=0.07, P=0.003) but not for HF, pneumonia, or the 3 conditions combined. In multivariate analyses, more-computerized hospitals had slightly better quality. The authors concluded that hospital computing might modestly improve process measures of quality but does not reduce administrative or overall costs.
In a retrospective cohort study of cases (111 707) submitted to the NCDR ICD (implantable cardioverter-defibrillator) Registry between January 1, 2006, and June 30, 2009, 25 145 (22.5%) received non–evidence-based implantable cardioverter-defibrillator therapy. Patients who received non–evidence-based implantable cardioverter-defibrillator therapy had a significantly higher risk of in-hospital death (0.57% versus 0.18%, P<0.001) and any postprocedure complication (3.23% versus 2.41%, P<0.001) than those who received evidence-based implantable cardioverter-defibrillator therapy.45
In a multicenter study of patients within the NCDR undergoing PCI, Chan et al46 reported results of the appropriateness of PCI for both acute and nonacute indications. Among patients undergoing PCI for acute indications (71.1% of the cohort), 98.5% of the procedures were classified as appropriate, 0.3% as uncertain, and 1.1% as inappropriate. Among patients undergoing PCI for nonacute indications (28.9% of the cohort), 50.4% of the procedures were classified as appropriate, 38% as uncertain, and 11.6% as inappropriate. There was also substantial variation for inappropriate nonacute PCI across hospitals (median hospital rate 10.8%; interquartile range 6.0%–16.7%).
-
Equitable care means the provision of care that does not vary in quality because of personal characteristics such as sex, ethnicity, geographic location, and socioeconomic status. The aim of equity is to secure the benefits of quality health care for all the people of the United States. With regard to equity in caregiving, all individuals rightly expect to be treated fairly by local institutions, including health-care organizations.
Chan et al47 demonstrated that rates of survival to discharge were lower for black patients (25.2%) than for white patients (37.4%) after in-hospital cardiac arrest. Lower rates of survival to discharge for blacks reflected lower rates of both successful resuscitation (55.8% versus 67.4%) and postresuscitation survival (45.2% versus 55.5%). Adjustment for the hospital site at which patients received care explained a substantial portion of the racial differences in successful resuscitation (adjusted RR, 0.92; 95% CI, 0.88–0.96; P<0.001) and eliminated the racial differences in postresuscitation survival (adjusted RR, 0.99; 95% CI, 0.92–1.06; P=0.68). The authors concluded that much of the racial difference was associated with the hospital center in which black patients received care.
Kapoor et al48 evaluated 99 058 HF admissions from 244 sites between January 2005 and September 2009. Patients were grouped on the basis of payer status (private/health maintenance organization, no insurance, Medicare, or Medicaid). Compared with private/health maintenance organization group, the other 3 groups were less likely to receive evidence-based therapies (β-blockers, implantable cardioverter-defibrillators, anticoagulation for AF, ACE inhibitors, or ARBs) and had longer hospital stays. Higher adjusted rates of in-hospital mortality were also seen in patients with Medicaid (OR, 1.22; 95% CI, 1.06–1.41) and in patients with reduced EF and no insurance (OR, 1.61; 95% CI, 1.15–2.25).
Cohen et al49 demonstrated that among hospitals engaged in a national quality monitoring and improvement program, evidence-based care for AMI appeared to improve over time for patients irrespective of race/ethnicity, and differences in care by race/ethnicity care were reduced or eliminated. They analyzed 142 593 patients with AMI (121 528 whites, 10 882 blacks, and 10 183 Hispanics) at 443 hospitals participating in the GWTG-CAD program. Overall, defect-free care was 80.9% for whites, 79.5% for Hispanics (adjusted OR versus whites, 1.00; 95% CI, 0.94–1.06; P=0.94), and 77.7% for blacks (adjusted OR versus whites, 0.93; 95% CI, 0.87–0.98; P=0.01). A significant gap in defect-free care was observed for blacks during the first half of the study but was no longer present during the remainder of the study. Overall, progressive improvements in defect-free care were observed regardless of race/ethnic groups.
Thomas et al50 analyzed data among hospitals that voluntarily participated in the AHA’s GWTG-HF program from January 2005 through December 2008. Relative to white patients, Hispanic and black patients hospitalized with HF were significantly younger (median age 78, 63, and 64 years, respectively) but had lower EFs (mean EF 41.1%, 38.8%, and 35.7%, respectively) with a higher prevalence of DM (40.2%, 55.7%, and 43.8%, respectively) and hypertension (70.6%, 78.4%, and 82.8%, respectively). The provision of guideline-based care was comparable for white, black, and Hispanic patients. Black (1.7%) and Hispanic (2.4%) patients had lower in-hospital mortality than white patients (3.5%). Improvement in adherence to all-or-none HF measures increased annually from year 1 to year 3 for all 3 racial/ethnic groups.50
Al-Khatib et al51 analyzed implantable cardioverter-defibrillator use for primary prevention among 11 880 patients with a history of HF, left ventricular EF<35%, and age >65 years enrolled in the GWTG-HF registry from January 2005 through December 2009. From 2005 to 2007, overall implantable cardioverter-defibrillator use increased from 30.2% to 42.4% and then remained unchanged in 2008 to 2009. After adjustment for confounders, implantable cardioverter-defibrillator use increased significantly in the overall study population during 2005 to 2007 (OR, 1.28; 95% CI, 1.11–1.48 per year; P=0.0008) and in black women (OR, 1.82; 95% CI, 1.28–2.58 per year; P=0.0008), white women (OR, 1.30; 95% CI, 1.06–1.59 per year; P=0.010), black men (OR, 1.54; 95% CI, 1.19–1.99 per year; P=0.0009), and white men (OR, 1.25; 95% CI, 1.06–1.48 per year; P=0.0072). The increase in implantable cardioverter-defibrillator use was greatest among blacks. They concluded that although previously described racial disparities in the use of implantable cardioverter-defibrillators were no longer present in their study by the end of the study period, a sex difference in their use persisted.51
In 2013, the AHA published an advisory that provided a recommendation on improving bystander CPR in communities with low bystander CPR rates (in the United States, rates ranged from 10%–65%) and the metrics to evaluate the impact of community-based CPR training programs.52
GWTG data by race, sex, and ethnicity are provided in Tables 22-12 through 22-14.
Table 22-6.
Additional ACTION-GWTG Quality-of-Care Metrics for ACS Care, 2012*
| Quality Metrics | Overall | STEMI | NSTEMI |
|---|---|---|---|
| ECG within 10 min of arrival | 64.5 | 75.0 | 59.8 |
| Aspirin within 24 h of arrival | 97.8 | 98.3 | 97.5 |
| Any anticoagulant use† | 93.4 | 95.9 | 91.7 |
| Dosing error | |||
| UFH dose | 47.0 | 47.3 | 47.0 |
| Enoxaparin dose | 11.0 | 11.2 | 11.0 |
| Glycoprotein IIb/IIIa inhibitor dose | 6.7 | 7.1 | 6.0 |
| Aspirin at discharge | 98.4 | 98.9 | 98.1 |
| Prescribed statins on discharge | 98.8 | 99.1 | 98.5 |
| Adult smoking cessation advice/counseling | 98.4 | 98.6 | 98.2 |
| Cardiac rehabilitation referral | 77.3 | 82.5 | 73.7 |
| In-hospital mortality‡ (95% CI) | 4.8 (4.6–4.9) | 6.5 (6.3–6.7) | 3.6 (3.5–3.7) |
Values are percentages.
ACS indicates acute coronary syndrome; ACTION-GWTG, Acute Coronary Treatment and Intervention Outcomes Network Registry–Get With The Guidelines; CI, confidence interval; ECG, electrocardiogram; NSTEMI, non–ST-segment–elevation myocardial infarction; STEMI, ST-segment–elevation myocardial infarction; and UFH, unfractionated heparin.
2012 data reported include data from second quarter of 2012 to first quarter of 2013.
Includes UFH, low-molecular-weight heparin, or direct thrombin inhibitor use.
Excludes transfer-out patients.
Table 22-7.
National Committee for Quality Assurance Health Plan Employer Data and Information Set Measures of Care, 2011
| Commercial | Medicare | Medicaid | |
|---|---|---|---|
| AMI | |||
| β-Blocker persistence* | 81.3 | 87.3 | 80.5 |
| Cholesterol management for patients with CVD | |||
| Cholesterol screening | 88.1 | 88.8 | 82.0 |
| LDL cholesterol control (<100 mg/dL) | 59.8 | 56.5 | 42.1 |
| Hypertension | |||
| BP <140/90 mm Hg | 65.4 | 64.0 | 56.8 |
| DM | |||
| HbA1c testing | 90.0 | 91 | 82.5 |
| HbA1c >9.0% | 28.3 | 26.5 | 43.0 |
| Eye examination performed | 56.9 | 66.0 | 53.3 |
| LDL cholesterol screening | 85.3 | 88.3 | 75.0 |
| LDL cholesterol <100 mg/dL | 48.1 | 52.5 | 35.2 |
| Monitoring nephropathy | 83.8 | 89.9 | 77.8 |
| BP <140/90 mm Hg | 65.8 | 63.1 | 60.9 |
| Advising smokers and tobacco users to quit | 77.6 | 81.5 | 74.6 |
| BMI percentile assessment in children and adolescents | 44.7 | N/A | 46 |
| Nutrition counseling (children and adolescents) | 46.4 | N/A | 50.1 |
| Counseling for physical activity (children and adolescents) | 43.0 | N/A | 40.6 |
| BMI assessment for adults | 55.4 | 68.2 | 52.6 |
| Physical activity discussion in older adults (≥65 y of age) | N/A | 53.0 | N/A |
| Physical activity advice in older adults (≥65 y of age) | N/A | 48.7 | N/A |
Values are percentages.
AMI indicates acute myocardial infarction; BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; DM, diabetes mellitus; HbA1c, hemoglobin A1c; LDL, low-density lipoprotein; and N/A, not available or not applicable.
β-Blocker persistence: Received persistent β-blocker treatment for 6 mo after AMI hospital discharge.
Table 22-8.
Quality of Care for EMS-Treated Out-of-Hospital Cardiac Arrest
| Overall | Adults | Children | |
|---|---|---|---|
| Bystander CPR, %* | 40.8 (39.6–42.0) | 40.4 (39.1–41.7) | 53.9 (47.3–60.4) |
| Shocked by AED before EMS, %* | 2.1 (1.7–2.4) | 2.1 (1.8–2.5) | 0 (0–0) |
| Time from dispatch to first EMS defibrillator applied, min* | 8.9 (4.7) | 8.9 (4.7) | 9.0 (3.7) |
| Chest compression fraction, %*† | 0.75 (0.16) | 0.75 (0.16) | 0.80 (0.15) |
| Compression depth, mm*‡ | 39.5 (14.9) | 39.6 (14.9) | 35.9 (16.5) |
| Preshock pause duration, s§ | 18.5 (8.6) | 18.5 (8.6) | N/A |
Values are mean (95% confidence interval) or mean (standard deviation).
US sites only; 2011 cases.
AED indicates automated external defibrillator; CPR, cardiopulmonary resuscitation; EMS indicates emergency medical services; and N/A, not available.
Denominator is EMS-treated cardiac arrest.
During first 5 min of resuscitation.
During first 10 min of resuscitation.
Up to and including first 6 shocks.
Source: Unpublished data, Resuscitation Outcomes Consortium Investigators, July 23, 2013.
Table 22-9.
Quality of Postresuscitation Hospital Care for Out-of-Hospital Cardiac Arrests
| Overall | Adults | Children | |
|---|---|---|---|
| Hypothermia induced* | 55.7 (50.5–61.0) | 55.8 (50.6–61.1) | 66.7 (13.3–100) |
| Care not withdrawn during hospitalization† | 44.8 (41.7–47.9) | 44.7 (41.5–47.8) | 51.5 (34.5–68.6) |
| Assessed for implantable defibrillator‡ | 31.3 (23.7–38.8) | 31.2 (23.6–38.9) | 50.0 (0–100) |
Values are mean percentages (95% confidence interval).
US sites only; 2011 cases.
Denominator is admitted to hospital after cardiac arrest with first rhythm of ventricular tachycardia/ventricular fibrillation.
Denominator is all cases admitted to hospital.
Denominator is all cases admitted to hospital with first rhythm of ventricular tachycardia/ventricular fibrillation and no acute myocardial injury.
Source: Unpublished data, Resuscitation Outcomes Consortium Investigators, July 23, 2013.
Table 22-10.
Quality of Care for In-Hospital Cardiac Arrest, 2012
| Adults | Children | |
|---|---|---|
| Monitored before arrest, % | 86.6 (86.0–87.2) | 90.0 (87.8–92.8) |
| ETCO2 used during arrest, % | 4.5 (4.1–4.9) | 9.1 (6.8–11.8) |
| Induced hypothermia after resuscitation from shockable rhythm, % | 7.6 (6.2–9.1) | 17.7 (3.8–43.4) |
| Achieved temperature between 32°C and 34°C if cooled, % | 54.2 (43.5–64.9) | N/A |
Values are mean percentages (95% confidence interval).
ETCO2 indicates end-tidal carbon dioxide; N/A, not applicable.
Source: Unpublished data, Get With the Guidelines–Resuscitation Investigators, July 27, 2013.
Table 22-11.
Timely Reperfusion for ACS and Stroke, 2012
| Quality-of-Care Measure | VHA (for STEMI) or GWTG-Stroke (for Stroke) | National Data From HIQR Program* | ACTION-GWTG STEMI† |
|---|---|---|---|
| STEMI | |||
| tPA within 30 min | 50‡ | 60.1 | 44.6‡ |
| PCI within 90 min | 69 | 94.5 | 95.3 |
| Stroke | |||
| IV tPA in patients who arrived <2 h after symptom onset, treated ≤3 h | 82.0 | N/A | N/A |
| IV tPA in patients who arrived <3.5 h after symptom onset, treated ≤4.5 h | 60.4 | N/A | N/A |
| IV tPA door-to-needle time ≤60 min | 39.9 | N/A | N/A |
Values are percentages.
ACS indicates acute coronary syndrome; ACTION-GWTG, Acute Coronary Treatment and Intervention Outcomes Network Registry–Get With The Guidelines; GWTG-Stroke, Get With The Guidelines–Stroke; HIQR, Hospital Inpatient Quality Reporting; IV, intravenous; N/A, not applicable; PCI, percutaneous coronary intervention; STEMI, ST-segment–elevation myocardial infarction; tPA, tissue-type plasminogen activator; and VHA, Veterans Health Administration.
HIQR Program includes data from all payers, including Medicare and Medicaid. Data reported include data from third quarter of 2011 to second quarter of 2012.
ACTION Registry: Data reported include data from second quarter of 2012 to first quarter of 2013.
Indicates low number.
Table 22-12.
Quality of Care by Race/Ethnicity and Sex in the ACTION Registry, 2012
| Quality-of-Care Measure | White | Black | Other | Men | Women |
|---|---|---|---|---|---|
| Aspirin at admission | 97.9 | 97.8 | 97.6 | 98.1 | 97.3 |
| Aspirin at discharge | 98.5 | 97.8 | 98.5 | 98.7 | 98.0 |
| β-Blockers at discharge | 97.2 | 96.8 | 97.6 | 97.4 | 96.5 |
| Time to PCI ≤90 min for STEMI patients | 95.5 | 94.1 | 93.9 | 95.7 | 94.1 |
| ARB/ACEI at discharge for patients with LVEF <40% | 89.6 | 90.4 | 89.1 | 89.9 | 89.3 |
| Statins at discharge | 98.8 | 98.5 | 98.9 | 99.0 | 98.3 |
Values are percentages.
Data reported include data from second quarter of 2012 to first quarter of 2013.
ACTION indicates Acute Coronary Treatment and Intervention Outcomes Network; ARB/ACEI angiotensin receptor blocker/angiotensin-converting enzyme inhibitor; LVEF, left ventricular ejection fraction; PCI, percutaneous coronary intervention; and STEMI, ST-segment–elevation myocardial infarction.
- 1.Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 2.Spertus JA, Eagle KA, Krumholz HM, Mitchell KR, Normand SL American College of Cardiology; American Heart Association Task Force on Performance Measures. American College of Cardiology and American Heart Association methodology for the selection and creation of performance measures for quantifying the quality of cardiovascular care. Circulation. 2005;111:1703–1712. doi: 10.1161/01.CIR.0000157096.95223.D7. [DOI] [PubMed] [Google Scholar]
- 3.Rahim SA, Mody A, Pickering J, Devereaux PJ, Yusuf S. Iatrogenic adverse events in the coronary care unit. Circ Cardiovasc Qual Outcomes. 2009;2:437–442. doi: 10.1161/CIRCOUTCOMES.108.846493. [DOI] [PubMed] [Google Scholar]
- 4.Tsai TT, Maddox TM, Roe MT, Dai D, Alexander KP, Ho PM, Messenger JC, Nallamothu BK, Peterson ED, Rumsfeld JS National Cardiovascular Data Registry. Contraindicated medication use in dialysis patients undergoing percutaneous coronary intervention. JAMA. 2009;302:2458–2464. doi: 10.1001/jama.2009.1800. [DOI] [PubMed] [Google Scholar]
- 5.Mathews R, Peterson ED, Chen AY, Wang TY, Chin CT, Fonarow GC, Cannon CP, Rumsfeld JS, Roe MT, Alexander KP. In-hospital major bleeding during ST-elevation and non-ST-elevation myocardial infarction care: derivation and validation of a model from the ACTION Registry®-GWTG™. Am J Cardiol. 2011;107:1136–1143. doi: 10.1016/j.amjcard.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 6.López L, Weissman JS, Schneider EC, Weingart SN, Cohen AP, Epstein AM. Disclosure of hospital adverse events and its association with patients’ ratings of the quality of care. Arch Intern Med. 2009;169:1888–1894. doi: 10.1001/archinternmed.2009.387. [DOI] [PubMed] [Google Scholar]
- 7.Resnic FS, Gross TP, Marinac-Dabic D, Loyo-Berrios N, Donnelly S, Normand SL, Matheny ME. Automated surveillance to detect post-procedure safety signals of approved cardiovascular devices. JAMA. 2010;304:2019–2027. doi: 10.1001/jama.2010.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 9.Weintraub WS, Grau-Sepulveda MV, Weiss JM, O’Brien SM, Peterson ED, Kolm P, Zhang Z, Klein LW, Shaw RE, McKay C, Ritzenthaler LL, Popma JJ, Messenger JC, Shahian DM, Grover FL, Mayer JE, Shewan CM, Garratt KN, Moussa ID, Dangas GD, Edwards FH. Comparative effectiveness of revascularization strategies. N Engl J Med. 2012;366:1467–1476. doi: 10.1056/NEJMoa1110717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Appel LJ, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G, Miller ER, 3rd, Dalcin A, Jerome GJ, Geller S, Noronha G, Pozefsky T, Charleston J, Reynolds JB, Durkin N, Rubin RR, Louis TA, Brancati FL. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365:1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choudhry NK, Avorn J, Glynn RJ, Antman EM, Schneeweiss S, Toscano M, Reisman L, Fernandes J, Spettell C, Lee JL, Levin R, Brennan T, Shrank WH Post-Myocardial Infarction Free Rx Event and Economic Evaluation (MI FREEE) Trial. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365:2088–2097. doi: 10.1056/NEJMsa1107913. [DOI] [PubMed] [Google Scholar]
- 12.Arnold SV, Spertus JA, Tang F, Krumholz HM, Borden WB, Farmer SA, Ting HH, Chan PS. Statin use in outpatients with obstructive coronary artery disease. Circulation. 2011;124:2405–2410. doi: 10.1161/CIRCULATIONAHA.111.038265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, Phillips CO, Hodshon BV, Cooper LS, Krumholz HM. Telemonitoring in patients with heart failure [published correction appears in N Engl J Med. 2011;364:490] N Engl J Med. 2010;363:2301–2309. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Böhm M, Boll H, Baumann G, Honold M, Koehler K, Gelbrich G, Kirwan BA, Anker SD Telemedical Interventional Monitoring in Heart Failure Investigators. Impact of remote telemedical management on mortality and hospitalizations in ambulatory patients with chronic heart failure: the Telemedical Interventional Monitoring in Heart Failure Study. Circulation. 2011;123:1873–1880. doi: 10.1161/CIRCULATIONAHA.111.018473. [DOI] [PubMed] [Google Scholar]
- 15.Heisler M, Hofer TP, Schmittdiel JA, Selby JV, Klamerus ML, Bosworth HB, Bermann M, Kerr EA. Improving blood pressure control through a clinical pharmacist outreach program in patients with diabetes mellitus in 2 high-performing health systems: the adherence and intensification of medications cluster randomized, controlled pragmatic trial. Circulation. 2012;125:2863–2872. doi: 10.1161/CIRCULATIONAHA.111.089169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murray CJ, Abraham J, Ali MK, Alvarado M, Atkinson C, Baddour LM, Bartels DH, Benjamin EJ, Bhalla K, Birbeck G, Bolliger I, Burstein R, Carnahan E, Chen H, Chou D, Chugh SS, Cohen A, Colson KE, Cooper LT, Couser W, Criqui MH, Dabhadkar KC, Dahodwala N, Danaei G, Dellavalle RP, Des Jarlais DC, Dicker D, Ding EL, Dorsey ER, Duber H, Ebel BE, Engell RE, Ezzati M, Felson DT, Finucane MM, Flaxman S, Flaxman AD, Fleming T, Forouzanfar MH, Freedman G, Freeman MK, Gabriel SE, Gakidou E, Gillum RF, Gonzalez-Medina D, Gosselin R, Grant B, Gutierrez HR, Hagan H, Havmoeller R, Hoffman H, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Kassebaum N, Khatibzadeh S, Knowlton LM, Lan Q, Leasher JL, Lim S, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Macintyre MF, Mallinger L, McDermott MM, Meltzer M, Mensah GA, Michaud C, Miller TR, Mock C, Moffitt TE, Mokdad AA, Mokdad AH, Moran AE, Mozaffarian D, Murphy T, Naghavi M, Narayan KM, Nelson RG, Olives C, Omer SB, Ortblad K, Ostro B, Pelizzari PM, Phillips D, Pope CA, Raju M, Ranganathan D, Razavi H, Ritz B, Rivara FP, Roberts T, Sacco RL, Salomon JA, Sampson U, Sanman E, Sapkota A, Schwebel DC, Shahraz S, Shibuya K, Shivakoti R, Silberberg D, Singh GM, Singh D, Singh JA, Sleet DA, Steenland K, Tavakkoli M, Taylor JA, Thurston GD, Towbin JA, Vavilala MS, Vos T, Wagner GR, Weinstock MA, Weisskopf MG, Wilkinson JD, Wulf S, Zabetian A, Lopez AD US Burden of Disease Collaborators. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services. [Accessed June 6, 2013];Medicare Hospital Quality Chartbook 2012: Performance Report on Outcome Measures. http://cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Downloads/MedicareHospitalQualityChartbook2012.pdf.
- 18.Xian Y, Holloway RG, Chan PS, Noyes K, Shah MN, Ting HH, Chappel AR, Peterson ED, Friedman B. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011;305:373–380. doi: 10.1001/jama.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams JB, Delong ER, Peterson ED, Dokholyan RS, Ou FS, Ferguson TB, Jr Society of Thoracic Surgeons and the National Cardiac Database. Secondary prevention after coronary artery bypass graft surgery: findings of a national randomized controlled trial and sustained society-led incorporation into practice. Circulation. 2011;123:39–45. doi: 10.1161/CIRCULATIONAHA.110.981068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drozda J, Jr, Messer JV, Spertus J, Abramowitz B, Alexander K, Beam CT, Bonow RO, Burkiewicz JS, Crouch M, Goff DC, Jr, Hellman R, James T, 3rd, King ML, Machado EA, Jr, Ortiz E, O’Toole M, Persell SD, Pines JM, Rybicki FJ, Sadwin LB, Sikkema JD, Smith PK, Torcson PJ, Wong JB. ACCF/AHA/AMA-PCPI 2011 performance measures for adults with coronary artery disease and hypertension: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement [published correction appears in Circulation. 2011;124:e39] Circulation. 2011;124:248–270. doi: 10.1161/CIR.0b013e31821d9ef2. [DOI] [PubMed] [Google Scholar]
- 21.Bonow RO, Ganiats TG, Beam CT, Blake K, Casey DE, Jr, Goodlin SJ, Grady KL, Hundley RF, Jessup M, Lynn TE, Masoudi FA, Nilasena D, Piña IL, Rockswold PD, Sadwin LB, Sikkema JD, Sincak CA, Spertus J, Torcson PJ, Torres E, Williams MV, Wong JB American College of Cardiology Foundation; American Heart Association Task Force on Performance Measures; American Medical Association-Physician Consortium for Performance Improvement. ACCF/AHA/AMA-PCPI 2011 performance measures for adults with heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement. Circulation. 2012;125:2382–2401. doi: 10.1161/CIR.0b013e3182507bec. [DOI] [PubMed] [Google Scholar]
- 22.Bonow RO, Bennett S, Casey DE, Jr, Ganiats TG, Hlatky MA, Konstam MA, Lambrew CT, Normand SL, Pina IL, Radford MJ, Smith AL, Stevenson LW, Burke G, Eagle KA, Krumholz HM, Linderbaum J, Masoudi FA, Ritchie JL, Rumsfeld JS, Spertus JA American College of Cardiology; American Heart Association Task Force on Performance Measures; Heart Failure Society of America. ACC/AHA clinical performance measures for adults with chronic heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Heart Failure Clinical Performance Measures. Circulation. 2005;112:1853–1887. doi: 10.1161/CIRCULATIONAHA.105.170072. [DOI] [PubMed] [Google Scholar]
- 23.Smolderen KG, Spertus JA, Tang F, Oetgen W, Borden WB, Ting HH, Chan PS. Treatment differences by health insurance among outpatients with coronary artery disease: insights from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2013;61:1069–1075. doi: 10.1016/j.jacc.2012.11.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schneider RH, Grim CE, Rainforth MV, Kotchen T, Nidich SI, Gaylord-King C, Salerno JW, Kotchen JM, Alexander CN. Stress reduction in the secondary prevention of cardiovascular disease: randomized, controlled trial of transcendental meditation and health education in Blacks. Circ Cardiovasc Qual Outcomes. 2012;5:750–758. doi: 10.1161/CIRCOUTCOMES.112.967406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carroll JD, Edwards FH, Marinac-Dabic D, Brindis RG, Grover FL, Peterson ED, Tuzcu EM, Shahian DM, Rumsfeld JS, Shewan CM, Hewitt K, Holmes DR, Jr, Mack MJ. The STS-ACC Transcatheter Valve Therapy National Registry: a new partnership and infrastructure for the introduction and surveillance of medical devices and therapies. J Am Coll Cardiol. 2013;62:1026–1034. doi: 10.1016/j.jacc.2013.03.060. [DOI] [PubMed] [Google Scholar]
- 26.Weintraub WS, Spertus JA, Kolm P, Maron DJ, Zhang Z, Jurkovitz C, Zhang W, Hartigan PM, Lewis C, Veledar E, Bowen J, Dunbar SB, Deaton C, Kaufman S, O’Rourke RA, Goeree R, Barnett PG, Teo KK, Boden WE, Mancini GB COURAGE Trial Research Group. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med. 2008;359:677–687. doi: 10.1056/NEJMoa072771. [DOI] [PubMed] [Google Scholar]
- 27.Mark DB, Anstrom KJ, Sun JL, Clapp-Channing NE, Tsiatis AA, Davidson-Ray L, Lee KL, Bardy GH Sudden Cardiac Death in Heart Failure Trial Investigators. Quality of life with defibrillator therapy or amiodarone in heart failure. N Engl J Med. 2008;359:999–1008. doi: 10.1056/NEJMoa0706719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301:603–618. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 29.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, Peterson ED, Curtis LH. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 30.Smolderen KG, Spertus JA, Nallamothu BK, Krumholz HM, Tang F, Ross JS, Ting HH, Alexander KP, Rathore SS, Chan PS. Health care insurance, financial concerns in accessing care, and delays to hospital presentation in acute myocardial infarction. JAMA. 2010;303:1392–1400. doi: 10.1001/jama.2010.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther. 2009;85:651–658. doi: 10.1038/clpt.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reynolds MR, Magnuson EA, Lei Y, Leon MB, Smith CR, Svensson LG, Webb JG, Babaliaros VC, Bowers BS, Fearon WF, Herrmann HC, Kapadia S, Kodali SK, Makkar RR, Pichard AD, Cohen DJ Placement of Aortic Transcatheter Valves (PARTNER) Investigators. Health-related quality of life after transcatheter aortic valve replacement in inoperable patients with severe aortic stenosis. Circulation. 2011;124:1964–1972. doi: 10.1161/CIRCULATIONAHA.111.040022. [DOI] [PubMed] [Google Scholar]
- 33.Allen LA, Stevenson LW, Grady KL, Goldstein NE, Matlock DD, Arnold RM, Cook NR, Felker GM, Francis GS, Hauptman PJ, Havranek EP, Krumholz HM, Mancini D, Riegel B, Spertus JA on behalf of the American Heart Association Council on Quality of Care and Outcomes Research, Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Cardiovascular Radiology and Intervention, and Council on Cardiovascular Surgery and Anesthesia. Decision making in advanced heart failure: a scientific statement from the American Heart Association. Circulation. 2012;125:1928–1952. doi: 10.1161/CIR.0b013e31824f2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rumsfeld JS, Alexander KP, Goff DC, Jr, Graham MM, Ho PM, Masoudi FA, Moser DK, Roger VL, Slaughter MS, Smolderen KG, Spertus JA, Sullivan MD, Treat-Jacobson D, Zerwic JJ on behalf of the American Heart Association Council on Quality of Care and Outcomes Research, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Prevention, Council on Peripheral Vascular Disease, and Stroke Council. Cardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart Association. Circulation. 2013;127:2233–2249. doi: 10.1161/CIR.0b013e3182949a2e. [DOI] [PubMed] [Google Scholar]
- 35.Walsh MN, Bove AA, Cross RR, Ferdinand KC, Forman DE, Freeman AM, Hughes S, Klodas E, Koplan M, Lewis WR, MacDonnell B, May DC, Messer JV, Pressler SJ, Sanz ML, Spertus JA, Spinler SA, Teichholz LE, Wong JB, Byrd KD American College of Cardiology Foundation. ACCF 2012 health policy statement on patient-centered care in cardiovascular medicine: a report of the American College of Cardiology Foundation Clinical Quality Committee. J Am Coll Cardiol. 2012;59:2125–2143. doi: 10.1016/j.jacc.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 36.Ting HH, Chen AY, Roe MT, Chan PS, Spertus JA, Nallamothu BK, Sullivan MD, DeLong ER, Bradley EH, Krumholz HM, Peterson ED. Delay from symptom onset to hospital presentation for patients with non-ST-segment elevation myocardial infarction. Arch Intern Med. 2010;170:1834–1841. doi: 10.1001/archinternmed.2010.385. [DOI] [PubMed] [Google Scholar]
- 37.Bradley EH, Nallamothu BK, Herrin J, Ting HH, Stern AF, Nembhard IM, Yuan CT, Green JC, Kline-Rogers E, Wang Y, Curtis JP, Webster TR, Masoudi FA, Fonarow GC, Brush JE, Jr, Krumholz HM. National efforts to improve door-to-balloon time results from the Door-to-Balloon Alliance. J Am Coll Cardiol. 2009;54:2423–2429. doi: 10.1016/j.jacc.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 38.Wang TY, Peterson ED, Ou FS, Nallamothu BK, Rumsfeld JS, Roe MT. Door-to-balloon times for patients with ST-segment elevation myocardial infarction requiring interhospital transfer for primary percutaneous coronary intervention: a report from the National Cardiovascular Data Registry. Am Heart J. 2011;161:76–83. e1. doi: 10.1016/j.ahj.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 39.Glickman SW, Lytle BL, Ou FS, Mears G, O’Brien S, Cairns CB, Garvey JL, Bohle DJ, Peterson ED, Jollis JG, Granger CB. Care processes associated with quicker door-in-door-out times for patients with ST-elevation-myocardial infarction requiring transfer: results from a statewide regionalization program. Circ Cardiovasc Qual Outcomes. 2011;4:382–388. doi: 10.1161/CIRCOUTCOMES.110.959643. [DOI] [PubMed] [Google Scholar]
- 40.Ekundayo OJ, Saver JL, Fonarow GC, Schwamm LH, Xian Y, Zhao X, Hernandez AF, Peterson ED, Cheng EM. Patterns of emergency medical services use and its association with timely stroke treatment: findings from get with the guidelines-stroke. Circ Cardiovasc Qual Outcomes. 2013;6:262–269. doi: 10.1161/CIRCOUTCOMES.113.000089. [DOI] [PubMed] [Google Scholar]
- 41.Krumholz HM, Keenan PS, Brush JE, Jr, Bufalino VJ, Chernew ME, Epstein AJ, Heidenreich PA, Ho V, Masoudi FA, Matchar DB, Normand SL, Rumsfeld JS, Schuur JD, Smith SC, Jr, Spertus JA, Walsh MN. Standards for measures used for public reporting of efficiency in health care: a scientific statement from the American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research and the American College of Cardiology Foundation. Circulation. 2008;118:1885–1893. doi: 10.1161/CIRCULATIONAHA.108.190500. [DOI] [PubMed] [Google Scholar]
- 42.Amin AP, Spertus JA, Cohen DJ, Chhatriwalla A, Kennedy KF, Vilain K, Salisbury AC, Venkitachalam L, Lai SM, Mauri L, Normand SL, Rumsfeld JS, Messenger JC, Yeh RW. Use of drug-eluting stents as a function of predicted benefit: clinical and economic implications of current practice. Arch Intern Med. 2012;172:1145–1152. doi: 10.1001/archinternmed.2012.3093. [DOI] [PubMed] [Google Scholar]
- 43.Baumlin KM, Shapiro JS, Weiner C, Gottlieb B, Chawla N, Richardson LD. Clinical information system and process redesign improves emergency department efficiency. Jt Comm J Qual Patient Saf. 2010;36:179–185. doi: 10.1016/s1553-7250(10)36030-2. [DOI] [PubMed] [Google Scholar]
- 44.Himmelstein DU, Wright A, Woolhandler S. Hospital computing and the costs and quality of care: a national study. Am J Med. 2010;123:40–46. doi: 10.1016/j.amjmed.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 45.Al-Khatib SM, Hellkamp A, Curtis J, Mark D, Peterson E, Sanders GD, Heidenreich PA, Hernandez AF, Curtis LH, Hammill S. Non-evidence-based ICD implantations in the United States. JAMA. 2011;305:43–49. doi: 10.1001/jama.2010.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chan PS, Patel MR, Klein LW, Krone RJ, Dehmer GJ, Kennedy K, Nallamothu BK, Weaver WD, Masoudi FA, Rumsfeld JS, Brindis RG, Spertus JA. Appropriateness of percutaneous coronary intervention. JAMA. 2011;306:53–61. doi: 10.1001/jama.2011.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chan PS, Nichol G, Krumholz HM, Spertus JA, Jones PG, Peterson ED, Rathore SS, Nallamothu BK American Heart Association National Registry of Cardiopulmonary Resuscitation (NRCPR) Investigators. Racial differences in survival after in-hospital cardiac arrest. JAMA. 2009;302:1195–1201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kapoor JR, Kapoor R, Hellkamp AS, Hernandez AF, Heidenreich PA, Fonarow GC. Payment source, quality of care, and outcomes in patients hospitalized with heart failure. J Am Coll Cardiol. 2011;58:1465–1471. doi: 10.1016/j.jacc.2011.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cohen MG, Fonarow GC, Peterson ED, Moscucci M, Dai D, Hernandez AF, Bonow RO, Smith SC., Jr Racial and ethnic differences in the treatment of acute myocardial infarction: findings from the Get With the Guidelines-Coronary Artery Disease program. Circulation. 2010;121:2294–2301. doi: 10.1161/CIRCULATIONAHA.109.922286. [DOI] [PubMed] [Google Scholar]
- 50.Thomas KL, Hernandez AF, Dai D, Heidenreich P, Fonarow GC, Peterson ED, Yancy CW. Association of race/ethnicity with clinical risk factors, quality of care, and acute outcomes in patients hospitalized with heart failure. Am Heart J. 2011;161:746–754. doi: 10.1016/j.ahj.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 51.Al-Khatib SM, Hellkamp AS, Hernandez AF, Fonarow GC, Thomas KL, Al-Khalidi HR, Heidenreich PA, Hammill S, Yancy C, Peterson ED Get With the Guidelines Steering Committee and Hospitals. Trends in use of implantable cardioverter-defibrillator therapy among patients hospitalized for heart failure: have the previously observed sex and racial disparities changed over time? Circulation. 2012;125:1094–1101. doi: 10.1161/CIRCULATIONAHA.111.066605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sasson C, Meischke H, Abella BS, Berg RA, Bobrow BJ, Chan PS, Root ED, Heisler M, Levy JH, Link M, Masoudi F, Ong M, Sayre MR, Rumsfeld JS, Rea TD on behalf of the American Heart Association Council on Quality of Care and Outcomes Research, Emergency Cardiovascular Care Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Clinical Cardiology, and Council on Cardiovascular Surgery and Anesthesia. Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a science advisory from the American Heart Association for healthcare providers, policymakers, public health departments, and community leaders. Circulation. 2013;127:1342–1350. doi: 10.1161/CIR.0b013e318288b4dd. [DOI] [PubMed] [Google Scholar]
23. Medical Procedures
See Tables 23-1 and 23-2 and Charts 23-1 through 23-4.
Table 23-1.
2011 National HCUP Statistics: Mean Hospital Charges, In-Hospital Death Rates, and Mean Length of Stay for Various Cardiovascular Procedures
| Procedure | Mean Hospital Charges, $ | In-Hospital Death Rate, % | Mean Length of Stay, d | ICD-9-CM Procedure Codes |
|---|---|---|---|---|
| Total vascular and cardiac surgery and procedures | 75 746 | 2.88 | 6.1 | 35–39, 00.50–00.51, 00.53–00.55, 00.61–00.66 |
| Cardiac revascularization (bypass) | 147 435 | 1.63 | 9.2 | 36.1–36.3 |
| PCI | 70 176 | 1.13 | 3.2 | 00.66 |
| Cardiac catheterization | 42 337 | 0.93 | 3.7 | 37.21–37.23 |
| Pacemakers | 69 205 | 1.21 | 5.0 | 37.7–37.8, 00.50, 00.53 |
| Implantable defibrillators | 146 210 | 0.61 | 5.3 | 37.94–37.99, 00.51, 00.54 |
| Endarterectomy | 38 500 | 0.34 | 2.5 | 38.12 |
| Valves | 203 009 | 3.63 | 11.0 | 35.1–35.2, 35.99 |
| Heart transplantation | 706 199 | 5.28 | 41.0 | 37.51 |
HCUP indicates Healthcare Cost and Utilization Project; ICD-9-CM, International Classification of Diseases, Clinical Modification, 9th Revision; and PCI, percutaneous coronary intervention.
Data derived from the Agency for Healthcare Research and Quality, HCUP Nationwide Inpatient Sample, 2011.
Table 23-2.
Estimated* Inpatient Cardiovascular Operations, Procedures, and Patient Data by Sex and Age: United States, 2010 (in Thousands)
| Operation/Procedure/Patients | ICD-9-CM Procedure Codes | All | Sex
|
Age, y
|
||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | <15 | 15–44 | 45–64 | ≥65 | |||
| Valves | 35.1, 35.2, 35.99 | 106 | 64 | 42 | 4† | 5† | 32 | 65 |
| Angioplasty | 36.0, 0.66 | 955 | 642 | 313 | … | 44 | 421 | 489 |
| PCI (patients) | 36.06, 36.07, 0.66 | 492 | 330 | 162 | … | 23 | 216 | 253 |
| PCI | 0.66 | 500 | 334 | 166 | … | 23 | 220 | 257 |
| PCI with stents | 36.06, 36.07 | 454 | 308 | 146 | … | 21 | 201 | 233 |
| Cardiac revascularization‡ | 36.1–36.3 | 397 | 298 | 99 | … | 9† | 157 | 231 |
| Cardiac revascularization (patients) | 36.1–36.3 | 219 | 164 | 55 | … | 5† | 86 | 128 |
| Cardiac catheterization | 37.21–37.23 | 1029 | 638 | 391 | 7† | 64 | 456 | 502 |
| Pacemakers | 37.7, 37.8, 00.50, 00.53 | 370 | 196 | 174 | 3† | 6† | 57 | 305 |
| Pacemaker devices | 37.8, 00.53 | 159 | 81 | 78 | 1† | 3† | 20 | 135 |
| Pacemaker leads | 37.7, 00.50 | 212 | 115 | 96 | 1† | 3† | 36 | 171 |
| Implantable defibrillators | 37.94–37.99, 00.51, 00.54 | 97 | 71 | 26 | … | 8† | 31 | 58 |
| Endarterectomy | 38.12 | 100 | 55 | 45 | … | … | 29 | 71 |
| Total vascular and cardiac surgery and procedures§|| | 35–39, 00.50–00.51, 00.53–00.55, 00.61–00.66 | 7588 | 4397 | 3191 | 310 | 681 | 2706 | 3891 |
These data do not reflect any procedures performed on an outpatient basis. Many more procedures are being performed on an outpatient basis. Some of the lower numbers in this table compared with 2006 probably reflect this trend. Data include procedures performed on newborn infants.
Ellipses (…) indicate data not available; ICD-9-CM, International Classification of Diseases, Clinical Modification, 9th Revision; and PCI, percutaneous coronary intervention.
Breakdowns are not available for some procedures, so entries for some categories do not add to totals. These data include codes for which the estimated number of procedures is <5000. Categories with such small numbers are considered unreliable by the National Center for Health Statistics and in some cases may have been omitted.
Estimate should be used with caution because it may be unreliable or does not meet standards of reliability or precision.
Because ≥1 procedure codes are required to describe the specific bypass procedure performed, it is impossible from these (mixed) data to determine the average number of grafts per patient.
Totals include procedures not shown here.
This estimate includes angioplasty and stent insertions for noncoronary arteries.
Data derived from the National Hospital Discharge Survey/National Center for Health Statistics, 2010. Estimates are based on a sample of inpatient records from short-stay hospitals in the United States.
Chart 23-1.
Trends in cardiovascular procedures, United States: 1979 to 2010. Note: Inpatient procedures only. PCI indicates percutaneous coronary intervention. Source: National Hospital Discharge Survey, National Center for Health Statistics, and National Heart, Lung, and Blood Institute.
Chart 23-4.
Heart transplantations in the United States by recipient age, 2012. Source: Organ Procurement and Transplantation Network data as of April 11, 2013.
Trends in Operations and Procedures
(See Tables 23-1 and 23-2 and Charts 23-1 and 23-2.)
Chart 23-2.
Number of surgical procedures in the 10 leading diagnostic groups, United States: 2010. Source: National Hospital Discharge Survey/National Center for Health Statistics and National Heart, Lung, and Blood Institute.
-
The total number of inpatient cardiovascular operations and procedures increased 28%, from 5 939 000 in 2000 to 7 588 000 in 2010 (NHLBI computation based on NCHS annual data). Data from the NHDS were examined for trends from 1990 to 2004 for use of PCI and CABG and in-hospital mortality rate attributable to PCI and CABG by sex1:
Discharge rates (per 10 000 population) for PCI increased 58%, from 37.2 in 1990 to 1992 to 59.2 in 2002 to 2004.
Discharge rates for CABG increased from 34.1 in 1990 to 1992 to 38.6 in 1996 to 1998, then declined to 25.2 in 2002 to 2004.
In 1990 to 1992, discharge rates for CABG were 53.5 for males and 18.1 for females; these rates increased through 1996 to 1998, then declined to 38.8 and 13.6, respectively, in 2002 to 2004. The magnitude of these declines decreased by age decile and were essentially flat for both men and women ≥75 years of age.
PCI discharge rates increased from 54.5 for males and 23.0 for females to 83.0 and 38.7, respectively, over the 15-year time interval. In 2002 to 2004, discharge rates for men and women 65 to 74 years of age were 135.1 and 64.0, respectively. For those ≥75 years of age, the rates were 128.7 and 69.0, respectively.
In-hospital mortality rate (deaths per 100 CABG discharges) declined from 4.3 to 3.5 between 1990 to 1992 and 2002 to 2004 despite an increase in Charlson comorbidity index. The mortality rate declined in all age and sex subsets, but especially in women.
-
Data from the Acute Care Tracker database were used to estimate the population-based rates per 100 000 population for PCI and CABG procedures from 2002 to 2005, standardized to the 2005 US population2:
Adjusted for age and sex, the overall rate for coronary revascularization declined from 382 to 358 per 100 000. PCI rates during hospitalization increased from 264 to 267 per 100 000, whereas CABG rates declined from 121 to 94.
-
Data from men and women enrolled in Medicare from 1992 to 2001 suggest that efforts to eliminate racial disparities in the use of high-cost cardiovascular procedures (PCI, CABG, and carotid endarterectomy) were unsuccessful.3
In 1992, among women, the age-standardized rates of carotid endarterectomy were 1.59 per 1000 enrollees for whites and 0.64 per 1000 enrollees for blacks. By 2002, the rates were 2.42 per 1000 enrollees among white women and 1.15 per 1000 enrollees among black women. For men, the difference in rates between whites and blacks remained the same. In 1992, the rates were 3.13 per 1000 enrollees among white men and 0.82 per 1000 enrollees among black men; in 2001, the rates were 4.42 and 1.44, respectively.
Abbreviations Used in Chapter 23
| CABG | coronary artery bypass graft |
| CHF | congestive heart failure |
| D2B | Door-to-Balloon Alliance |
| DES | drug-eluting stent |
| GWTG-CAD | Get With The Guidelines–Coronary Artery Disease |
| HCUP | Healthcare Cost and Utilization Project |
| HD | heart disease |
| HPLHS | hypoplastic left heart syndrome |
| ICD-9-CM | International Classification of Diseases, 9th Revision, Clinical Modification |
| NCHS | National Center for Health Statistics |
| NHDS | National Hospital Discharge Survey |
| NHLBI | National Heart, Lung, and Blood Institute |
| PCI | percutaneous coronary intervention |
| PTCA | percutaneous transluminal coronary angioplasty |
| STEMI | ST-segment–elevation myocardial infarction |
| STS | Society of Thoracic Surgeons |
| TOF | tetralogy of Fallot |
| VSD | ventricular septal defect |
Cardiac Catheterization and PCI
(See Tables 23-1 and 23-2.)
From 2000 to 2010, the number of cardiac catheterizations decreased slightly, from 1 221 000 to 1 029 000 annually (NHDS, NHLBI tabulation).
In 2010, an estimated 492 000 patients underwent PCI (previously referred to as percutaneous transluminal coronary angioplasty, or PTCA) procedures in the United States (NHDS, NHLBI tabulation).
In 2010, ≈67% of PCI procedures were performed on men, and ≈51% were performed on people ≥65 years of age (NHDS, NHLBI tabulation).
In-hospital death rates for PCI have remained stable, although comorbidities increased for patients who received the procedure.1
In 2010, ≈75% of stents implanted during PCI were DES compared with 25% that were bare-metal stents (NHDS, NHLBI computation).
In a study of nontransferred patients with STEMI treated with primary PCI from July 2006 to March 2008, there was significant improvement over time in the percentage of patients receiving PCI within 90 minutes, from 54.1% from July to September 2006 to 74.1% from January to March 2008, among hospitals participating in the GWTG-CAD program. This improvement was seen whether or not hospitals joined the D2B Alliance during that period.4
The rate of any cardiac stent procedure rose by 61% from 1999 to 2006, then declined by 27% between 2006 and 2009.5
Cardiac Open Heart Surgery
The NHDS (NCHS) estimates that in 2010, in the United States, 219 000 patients underwent a total of 397 000 coronary artery bypass procedures (defined by procedure codes). CABG volumes have declined nationally since 1998. Risk-adjusted mortality for CABG has declined significantly over the past decade.
Data from the STS Adult Cardiac Surgery Database, which voluntarily collects data from ≈80% of all hospitals that perform CABG in the United States, indicate that a total of 158 008 procedures involved CABG in 2010.6
Data from the STS Adult Cardiac Surgery Database document a 50% decline in the risk-adjusted mortality rate despite a significant increase in preoperative surgical risk.7
Congenital Heart Surgery, 1998 to 2002 (From STS)
There were 103 664 procedures performed from July 2006 to June 2010. The in-hospital mortality rate was 3.2% in 2010. The 5 most common diagnoses were the following: patent ductus arteriosus (7.4%); HPLHS (6.9%); VSD, type 2 (6.3%); cardiac, other (5.3%); and TOF (4.9%).8
There were 16 920 procedures performed from 1998 to 2002 at 18 centers. In 2002, there were 4208 procedures performed. The in-hospital mortality rate ranged from 5.7% in 1998 to 4.3% in 2002. Of these procedures, ≈46% were performed in children >1 year old, ≈32% in infants between 29 days and 1 year of age, and ≈22% in neonates (<29 days old). The conditions for which these procedures were most commonly performed were the following: patent ductus arteriosus (6.5%), VSD (6.4%), and TOF (6.0%).8
Heart Transplantations
(See Charts 23-3 and 23-4.)
Chart 23-3.
Trends in heart transplantations (United Network for Organ Sharing: 1975–2012). Source: United Network for Organ Sharing, scientific registry data.
In 2012, 2378 heart transplantations were performed in the United States (Chart 23-3). There are 247 transplant hospitals in the United States, 129 of which performed heart transplantations (based on Organ Procurement and Transplantation Network data as of April 10, 2013).
Of the recipients in 2012, 69.7% were male, and 65.9% were white; 19.6% were black, whereas 9.0% were Hispanic. Heart transplantations by recipient age are shown in Chart 23-4.
As of April 11, 2013, for transplants that occurred between 2009 and 2010, the 1-year survival rate was 90.8% for males and 90.6% for females; the 5-year rates between 2005 and 2010 were 77.5% for males and 75.6% for females; and the 10-year rates between 2000 and 2010 were 58.9% for males and 57.6% for females. The 1-, 5-, and 10-year survival rates for white cardiac transplant patients were 91.2%, 79.1%, and 61.0%, respectively. For black patients, they were 88.3%, 68.6%, and 47.5%, respectively. For Hispanic patients, they were 91.9%, 76.3%, and 59.7%, respectively.
As of June 4, 2013, 3497 patients were on the transplant waiting list for a heart transplant, and 50 patients were on the list for a heart/lung transplant.
Cardiovascular Healthcare Expenditures
An analysis of claims and enrollment data from the Continuous Medicare History Sample and from physician claims from 1995 to 2004 was used to evaluate the conditions that contributed to the most expensive 5% of Medicare beneficiaries.8
Ischemic HD, CHF, and cerebrovascular disease, respectively, constituted 13.8%, 5.9%, and 5.7% of the conditions of all beneficiaries in 2004. In patients in the top 5% overall for all expenditures, the respective figures were 39.1%, 32.7%, and 22.3% for these cardiovascular conditions.
- 1.Holmes JS, Kozak LJ, Owings MF. Use and in-hospital mortality associated with two cardiac procedures, by sex and age: national trends, 1990–2004. Health Aff (Millwood) 2007;26:169–177. doi: 10.1377/hlthaff.26.1.169. [DOI] [PubMed] [Google Scholar]
- 2.Nallamothu BK, Young J, Gurm HS, Pickens G, Safavi K. Recent trends in hospital utilization for acute myocardial infarction and coronary revascularization in the United States. Am J Cardiol. 2007;99:749–753. doi: 10.1016/j.amjcard.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353:683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 4.Nallamothu BK, Krumholz HM, Peterson ED, Pan W, Bradley E, Stern AF, Masoudi FA, Janicke DM, Hernandez AF, Cannon CP, Fonarow GC D2B Alliance and the American Heart Association Get-With-The-Guidelines Investigators. Door-to-balloon times in hospitals within the Get-With-The-Guidelines registry after initiation of the Door-to-Balloon (D2B) Alliance. Am J Cardiol. 2009;103:1051–1055. doi: 10.1016/j.amjcard.2008.12.030. [DOI] [PubMed] [Google Scholar]
- 5.Auerbach DI, Maeda JL, Steiner C. Hospital Stays with Cardiac Stents, 2009. Rockville, MD: Agency for Healthcare Research and Quality; Apr, 2012. [Accessed July 23, 2012]. HCUP Statistical Brief 128. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb128.pdf. [PubMed] [Google Scholar]
- 6.Society of Thoracic Surgeons. STS Adult Cardiac Surgery Database: Executive Summary: 10 Years. [Accessed July 25, 2011];Society of Thoracic Surgeons Web site. http://www.sts.org/sites/default/files/documents/2011%20-%20Adult%20Cardiac%20Surgery%20-1stHarvestExecutiveSummary.pdf.
- 7.Ferguson TB, Jr, Hammill BG, Peterson ED, DeLong ER, Grover FL STS National Database Committee. A decade of change: risk profiles and outcomes for isolated coronary artery bypass grafting procedures, 1990–1999: a report from the STS National Database Committee and the Duke Clinical Research Institute. Ann Thorac Surg. 2002;73:480–489. doi: 10.1016/s0003-4975(01)03339-2. [DOI] [PubMed] [Google Scholar]
- 8.Riley GF. Long-term trends in the concentration of Medicare spending. Health Aff (Millwood) 2007;26:808–816. doi: 10.1377/hlthaff.26.3.808. [DOI] [PubMed] [Google Scholar]
24. Economic Cost of Cardiovascular Disease
See Tables 24-1 and 24-2 and Charts 24-1 through 24-5.
Table 24-1.
Estimated Direct and Indirect Costs (in Billions of Dollars) of CVD and Stroke: United States, 2010
| Heart Disease* | Stroke | Hypertensive Disease† | Other Circulatory Conditions | Total CVD | |
|---|---|---|---|---|---|
| Direct costs‡ | |||||
| Hospital inpatient stays | 67.4 | 12.2 | 5.4 | 13.0 | 98.0 |
| Hospital emergency department visits | 5.6 | 1.7 | 0.9 | 0.5 | 8.7 |
| Hospital outpatient or office-based provider visits | 19.3 | 2.6 | 13.0 | 7.3 | 42.2 |
| Home health care | 5.0 | 2.9 | 3.3 | 0.5 | 11.7 |
| Prescribed medicines | 9.9 | 1.2 | 20.3 | 1.4 | 32.8 |
| Total expenditures | 107.2 | 20.6 | 42.9 | 22.7 | 193.4 |
| Indirect costs§ | |||||
| Lost productivity/mortality|| | 97.2 | 15.9 | 3.5 | 5.3 | 122.0 |
| Grand totals | 204.4 | 36.5 | 46.4 | 28.0 | 315.4 |
Numbers do not add to total because of rounding.
CVD indicates cardiovascular disease.
This category includes coronary heart disease, heart failure, part of hypertensive disease, cardiac dysrhythmias, rheumatic heart disease, cardiomyopathy, pulmonary heart disease, and other or ill-defined heart diseases.
Costs attributable to hypertensive disease are limited to hypertension without heart disease.
Medical Expenditure Panel Survey healthcare expenditures are estimates of direct payments for care of a patient with the given disease provided during the year, including out-of-pocket payments and payments by private insurance, Medicaid, Medicare, and other sources. Payments for over-the-counter drugs are not included. These estimates of direct costs do not include payments attributed to comorbidities. Total CVD costs are the sum of costs for the 4 diseases but with some duplication.
The Statistics Committee agreed to suspend the presentation of estimates of lost productivity attributable to morbidity until a better estimating method can be developed.
Lost future earnings of people who died in 2010, discounted at 3%.
Sources: Estimates from the Household Component of the Medical Expenditure Panel Survey of the Agency for Healthcare Research and Quality for direct costs (2010).1 Indirect mortality costs are based on 2010 counts of deaths by the National Center for Health Statistics and an estimated present value of lifetime earnings furnished for 2009 by Wendy Max (Institute for Health and Aging, University of California, San Francisco, April 25, 2012) and inflated to 2010 from change in worker compensation reported by the US Bureau of Labor Statistics.
All estimates prepared by Michael Mussolino, National Heart, Lung, and Blood Institute.
Table 24-2.
Costs of Total CVD in Billions of Dollars by Age and Sex: United States, 2010
| Total | Sex
|
Age, y
|
|||
|---|---|---|---|---|---|
| Male | Female | <65 | ≥65 | ||
| Direct | 193.4 | 96.4 | 97.0 | 95.4 | 98.0 |
| Indirect mortality | 122.0 | 89.6 | 32.4 | 105.0 | 17.0 |
| Total | 315.4 | 186.0 | 129.4 | 200.4 | 115.0 |
Numbers may not add to total because of rounding.
CVD indicates cardiovascular diseases and stroke.
Source: Medical Expenditure Panel Survey, 2010 (direct costs), mortality data from the National Center for Health Statistics, present value of lifetime earnings from the Institute for Health and Aging, University of California, San Francisco, and hourly compensation data from the US Bureau of Labor Statistics (indirect costs).
All estimates prepared by Michael Mussolino, National Heart, Lung, and Blood Institute.
Chart 24-1.
Direct and indirect costs of cardiovascular disease (CVD) and stroke (in billions of dollars), United States, 2010. Source: Prepared by the National Heart, Lung, and Blood Institute.1,3
Chart 24-5.
Projected direct costs of total cardiovascular disease by type of cost (2012 $ in billions). Unpublished data tabulated by the American Heart Association using methods described by Heidenreich et al.8
The annual direct and indirect cost of CVD and stroke in the United States is an estimated $315.4 billion (Table 24-1; Chart 24-1). This figure includes $193.4 billion in expenditures (direct costs, which include the cost of physicians and other professionals, hospital services, prescribed medication, and home health care, but not the cost of nursing home care) and $122.0 billion in lost future productivity attributed to premature CVD and stroke mortality in 2010 (indirect costs).
The direct costs for CVD and stroke are the healthcare expenditures for 2010 available on the Web site of the nationally representative MEPS of the AHRQ.1 Details on the advantages or disadvantages of using MEPS data are provided in the “Heart Disease and Stroke Statistics–2011 Update.”2 Indirect mortality costs are estimated for 2010 by multiplying the number of deaths that year attributable to CVD and strokes, in age and sex groups, by estimates of the present value of lifetime earnings for those age and sex groups as of 2010. Mortality data are from the National Vital Statistics System of the NCHS.3 The present values of lifetime earnings are unpublished estimates furnished by the Institute on Health and Aging, University of California at San Francisco, by Wendy Max, PhD, on April 25, 2012. Those estimates have a 3% discount rate, the recommended percentage.4 The discount rate removes the effect of inflation in income over the lifetime of earnings. The estimates are for 2009, inflated to 2010 by 3% to account for the 2009 to 2010 change in hourly worker compensation in the business sector reported by the US Bureau of Labor Statistics.5
The indirect costs exclude lost productivity costs attributable to CVD and stroke illness during 2010 among workers, people keeping house, people in institutions, and people unable to work. Those morbidity costs were substantial in very old studies, but an adequate update could not be made.
Most Costly Diseases
(See Table 24-2 and Chart 24-2.)
Chart 24-2.
The 22 leading diagnoses for direct health expenditures, United States, 2010 (in billions of dollars). COPD indicates chronic obstructive pulmonary disease; and GI, gastrointestinal tract. Source: National Heart, Lung, and Blood Institute; estimates are from the Medical Expenditure Panel Survey, Agency for Healthcare Research and Quality, and exclude nursing home costs.
CVD and stroke accounted for 15% of total health expenditures in 2010, more than any major diagnostic group.1,6 That is also the case for indirect mortality costs. By way of comparison, CVD total direct and indirect costs shown in Table 24-1 are higher than the official National Cancer Institute estimates for cancer and benign neoplasms in 2008, which were cited as $228 billion total ($93 billion in direct costs, $19 billion in indirect morbidity costs, and $116 billion in indirect mortality costs).7
Table 24-2 shows direct and indirect costs for CVD by sex and by 2 broad age groups. Chart 24-2 shows total direct costs for the 14 leading chronic diseases in the MEPS list. HD is the most costly condition.1
Abbreviations Used in Chapter 24
| AHA | American Heart Association |
| AHRQ | Agency for Healthcare Research and Quality |
| CHD | coronary heart disease |
| CHF | congestive heart failure |
| COPD | chronic obstructive pulmonary disease |
| CVD | cardiovascular disease |
| GI | gastrointestinal (tract) |
| HBP | high blood pressure |
| HD | heart disease |
| HF | heart failure |
| MEPS | Medical Expenditure Panel Survey |
| NCHS | National Center for Health Statistics |
Projections
(See Charts 24-3 through 24-5.)
Chart 24-3.
Projected total costs of cardiovascular disease (CVD), 2015 to 2030 (2012 $ in billions) in the United States. CHD indicates coronary heart disease; CHF, congestive heart failure; and HBP, high blood pressure. Unpublished data tabulated by the American Heart Association using methods described by Heidenreich et al.8
The AHA developed methodology to project future costs of care for HBP, CHD, HF, stroke, and all other CVD.8
By 2030, 43.9% of the US population is projected to have some form of CVD.
Between 2012 and 2030, total direct medical costs of CVD are projected to increase from $396 billion to $918 billion (2012 $ in billions). Of this total, 60.5% is attributable to hospital costs, 15.6% to medications, 10.8% to physicians, 6.8 % to nursing home care, 5.3% to home health care, and 1.1% to other costs.
Indirect costs (attributable to lost productivity) for all CVDs are estimated to increase from $183 billion in 2012 to $290 billion in 2030 (2012 $ in billions), an increase of 58%.
These data indicate that CVD prevalence and costs are projected to increase substantially.
- 1.Medical Expenditure Panel Survey: household component summary data table. Table 4: total expenses and percent distribution for selected conditions by source of payment: United States, 2008. [Accessed June 12, 2013];Agency for Healthcare Research and Quality Web site. http://www.meps.ahrq.gov/mepsweb/data_stats/tables_compendia_hh_interactive.jsp?
- 2.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2011 update: a report from the American Heart Association [published correction appears in Circulation. 2011;124:e426 and Circulation. 2011;123:e240] Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murphy SL, Xu JQ, Kochanek KD. National Vital Statistics Report. 4. Vol. 61. Hyattsville, MD: National Center for Health Statistics; 2013. Deaths: final data for 2010. [PubMed] [Google Scholar]
- 4.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in Health and Medicine. New York, NY: Oxford University Press; 1996. [Google Scholar]
- 5.Bureau of Labor Statistics, Office of Compensation Levels and Trends. Employment Cost Index, Historical Listing: Volume V: Continuous Occupational and Industry Series: September 1975–March 2013 (December 2005=100). Table 4: employment cost index for total compensation, for civilian workers, by occupation and industry: Continuous Occupational and Industry Series. [Accessed June 6, 2013];US Bureau of Labor Statistics Web site. http://www.bls.gov/web/eci/ecicois.pdf.
- 6.Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey. Household component summary tables. Table 1: total health services: median and mean expenses per person with expense and distribution of expenses by source of payment: United States, 2008. [Accessed November 23, 2011];Agency for Healthcare Research and Quality Web site. http://www.meps.ahrq.gov/mepsweb/data_stats/tables_compendia_hh_interactive.jsp?
- 7.American Cancer Society. Economic impact of cancer. [Accessed May 25, 2011];American Cancer Society Web site. http://www.cancer.org/Cancer/CancerBasics/economic-impact-of-cancer.
- 8.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ on behalf of the American Heart Association Advocacy Coordinating Committee, Stroke Council, Council on Cardiovascular Radiology and Intervention, Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular Nursing, Council on the Kidney in Cardiovascular Disease, Council on Cardiovascular Surgery and Anesthesia, and Interdisciplinary Council on Quality of Care and Outcomes Research. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
25. At-a-Glance Summary Tables
See Tables 25-1 through 25-4.
Table 25-1.
Males and CVD: At-a-Glance Table
| Diseases and Risk Factors | Both Sexes | Total Males | White Males | Black Males | Mexican American Males |
|---|---|---|---|---|---|
| Smoking | |||||
| Prevalence, 2012* | 42.1 M (18.1%) | 23.0 M (20.5%) | 22.0% | 21.6% | 16.6%† |
| PA‡ | |||||
| Prevalence, 2012* | 20.7% | 24.6% | 26.0% | 23.7% | 19.3%† |
| Overweight and obesity | |||||
| Prevalence, 2010 | |||||
| Overweight and obesity, BMI >25.0 kg/m2§ | 154.7 M (68.2%) | 79.9 M (72.9%) | 73.1% | 68.7% | 81.3% |
| Obesity, BMI >30.0 kg/m2§ | 78.4 M (34.6%) | 36.8 M (33.6%) | 33.8% | 37.9% | 36.0% |
| Blood cholesterol | |||||
| Prevalence, 2010 | |||||
| Total cholesterol >200 mg/dL§ | 98.9 M (43.4%) | 45.3 M (41.3%) | 40.5% | 38.6% | 48.1% |
| Total cholesterol >240 mg/dL§ | 31.9 M (13.8%) | 14.0 M (12.7%) | 12.3% | 10.8% | 15.2% |
| LDL cholesterol >130 mg/dL§ | 71.0 M (31.1%) | 35.2 M (31.9%) | 30.1% | 33.1% | 39.9% |
| HDL cholesterol <40 mg/dL§ | 48.7 M (21.8%) | 34.6 M (31.8%) | 33.1% | 20.3% | 34.2% |
| HBP | |||||
| Prevalence, 2010§ | 77.9 M (33.0%) | 37.2 M (33.6%) | 33.4% | 42.6% | 30.1% |
| Mortality, 2010|| | 63 119 | 28 373 | 20 819 | 6670 | N/A |
| DM | |||||
| Prevalence, 2010 | |||||
| Physician-diagnosed DM§ | 19.7 M (8.3%) | 9.6 M (8.7%) | 7.7% | 13.5% | 11.4% |
| Undiagnosed DM§ | 8.2 M (3.5%) | 5.3 M (4.7%) | 4.5% | 4.8% | 6.6% |
| Prediabetes§ | 87.3 M (38.2%) | 50.7 M (46.0%) | 47.7% | 35.7% | 47.0% |
| Incidence, diagnosed DM§ | 1.9 M | N/A | N/A | N/A | N/A |
| Mortality, 2010|| | 69 071 | 35 490 | 28 486 | 5640 | N/A |
| Total CVD | |||||
| Prevalence, 2010§ | 83.6 M (35.3%) | 40.7 M (36.7%) | 36.6% | 44.4% | 33.4% |
| Mortality, 2010||¶ | 787 650 | 387 318 | 330 330 | 46 266 | N/A |
| Stroke | |||||
| Prevalence, 2010§ | 6.8 M (2.8%) | 3.0 M (2.6%) | 2.4% | 4.3% | 2.3% |
| New and recurrent strokes|| | 795.0 K | 370.0 K | 325.0 K | 45.0 K | N/A |
| Mortality, 2010|| | 129 476 | 52 367 | 43 424 | 6938 | N/A |
| CHD | |||||
| Prevalence, CHD, 2010§ | 15.4 M (6.4%) | 8.8 M (7.9%) | 8.2% | 6.8% | 6.7% |
| Prevalence, MI, 2010§ | 7.6 M (2.9%) | 5.0 M (4.2%) | 4.4% | 3.9% | 3.6% |
| Prevalence, AP, 2010§ | 7.8 M (3.2%) | 3.7 M (3.3%) | 3.3% | 2.4% | 3.4% |
| New and recurrent CHD#** | 915.0 K | 530.0 K | 465.0 K | 65.0 K | N/A |
| New and recurrent MI** | 720.0 K | 420.0 K | N/A | N/A | N/A |
| Incidence, AP (stable angina)‡‡ | 565.0 K | 370.0 K | N/A | N/A | N/A |
| Mortality, 2010, CHD|| | 379 559 | 207 580 | 181 386 | 20 615 | N/A |
| Mortality, 2010, MI|| | 122 071 | 67 435 | 59 181 | 6445 | N/A |
| HF | |||||
| Prevalence, 2010§ | 5.1 M (2.1%) | 2.7 M (2.5%) | 2.5% | 4.1% | 1.9% |
| Incidence, 2010‡‡ | 825 000 | 395 000 | 350 000 | 45 000 | N/A |
| Mortality, 2010|| | 57 757 | 24 385 | 21 540 | 2444 | N/A |
AP indicates angina pectoris (chest pain); BMI, body mass index; CHD, coronary heart disease (includes heart attack, angina pectoris chest pain, or both); CVD, cardiovascular disease; DM, diabetes mellitus; HBP, high blood pressure; HDL, high-density lipoprotein; HF, heart failure; K, thousands; LDL, low-density lipoprotein; M, millions; MI, myocardial infarction (heart attack); N/A, data not available; and PA, physical activity.
Age ≥18 y (National Health Interview Survey).
All Hispanic (National Health Interview Survey).
Met 2008 full Federal PA guidelines for adults.
Age ≥20 y.
All ages.
Total CVD mortality includes deaths from congenital heart disease.
New and recurrent MI and fatal CHD.
Age ≥35 y.
Age ≥45 y.
Table 25-4.
Children, Youth, and CVD: At-a-Glance Table
| Diseases and Risk Factors | Both Sexes | Total Males | Total Females | NH Whites
|
NH Blacks
|
Mexican Americans
|
|||
|---|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | ||||
| Smoking, % | |||||||||
| High school students, grades 9–12 | |||||||||
| Current cigarette smoking, 2011 | 18.1 | 19.9 | 16.1 | 21.5 | 18.9 | 13.7 | 7.4 | 19.5* | 15.2* |
| Current cigar smoking, 2011 | 13.1 | 17.8 | 8.0 | 19.0 | 7.5 | 15.1 | 8.5 | 17.2* | 9.1* |
| PA† | |||||||||
| Prevalence, grades 9–12, 2011‡ | |||||||||
| Met currently recommended levels of PA, % | 49.5 | 59.9 | 38.5 | 62.1 | 42.6 | 57.1 | 31.9 | 57.1* | 33.0* |
| Overweight and obesity | |||||||||
| Prevalence, 2010 | |||||||||
| Children and adolescents, ages 2–19 y, overweight or obese | 23.9 M (31.8%) | 12.7 M (33.0%) | 11.2 M (30.4%) | 30.1% | 25.6% | 36.9% | 41.3% | 40.5% | 38.2% |
| Children and adolescents, age 2–19 y, obese‡ | 12.7 M (16.9%) | 7.2 M (18.6%) | 5.5 M (15.0%) | 16.1% | 11.7% | 24.3% | 24.3% | 24.0% | 18.2% |
| Blood cholesterol, mg/dL, 2010 | |||||||||
| Mean total cholesterol | |||||||||
| Ages 4–11 y | 161.9 | 162.3 | 161.5 | 160.9 | 161.6 | 165.2 | 157.9 | 159.6 | 160.7 |
| Ages 12–19 y | 158.2 | 156.1 | 160.3 | 156.8 | 161.1 | 154.1 | 160.6 | 157.8 | 158.0 |
| Mean HDL cholesterol | |||||||||
| Ages 4–11 y | 53.6 | 55.1 | 51.9 | 53.9 | 51.4 | 59.9 | 55.3 | 53.5 | 50.5 |
| Ages 12–19 y | 51.4 | 49.2 | 53.6 | 48.4 | 53.0 | 53.9 | 55.4 | 47.5 | 53.3 |
| Mean LDL cholesterol | |||||||||
| Ages 12–19 y | 89.5 | 88.6 | 90.5 | 90.4 | 90.9 | 85.8 | 91.8 | 90.6 | 87.1 |
| Congenital cardiovascular defects | |||||||||
| Mortality, 2010§ | 3196 | 1718 | 1478 | 1333 | 1120 | 311 | 271 | N/A | N/A |
Overweight indicates a body mass index in the 95th percentile of the Centers for Disease Control and Prevention 2000 growth chart.
CVD indicates cardiovascular disease; HDL, high-density lipoprotein; LDL, low-density lipoprotein; M, millions; N/A, data not available; NH, non-Hispanic; and PA, physical activity.
All Hispanic subgroups.
Regular leisure-time PA.
Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Whittle L, Lim C, Wechsler H; Centers for Disease Control and Prevention. Youth risk behavior surveillance: United States, 2011. MMWR Surveill Summ. 2012;61:1–162.
All ages.
Sources: See the following summary tables and charts for complete details:
Smoking—Table 3-1
Physical activity —Table 4-1
Blood cholesterol—Table 8-1
High blood pressure—Table 9-1
Diabetes mellitus—Table 10-1
Total cardiovascular diseases—Table 13-1
Stroke—Table 14-1
Congenital heart defects—Table 15-1
Coronary heart disease—Table 18-1
Heart failure—Table 19-1
26. Glossary
| Age-adjusted rates | Used mainly to compare the rates of ≥2 communities or population groups or the nation as a whole over time. The American Heart Association (AHA) uses a standard population (2000), so these rates are not affected by changes or differences in the age composition of the population. Unless otherwise noted, all death rates in this publication are age adjusted per 100 000 population and are based on underlying cause of death. |
| Agency for Healthcare Research and Quality (AHRQ) | A part of the US Department of Health and Human Services, this is the lead agency charged with supporting research designed to improve the quality of health care, reduce the cost of health care, improve patient safety, decrease the number of medical errors, and broaden access to essential services. The Agency for Healthcare Research and Quality sponsors and conducts research that provides evidence-based information on healthcare outcomes, quality, cost, use, and access. The information helps healthcare decision makers (patients, clinicians, health system leaders, and policy makers) make more informed decisions and improve the quality of health-care services. The Agency for Healthcare Research and Quality conducts the Medical Expenditure Panel Survey (MEPS; ongoing). |
| Bacterial endocarditis | An infection of the heart’s inner lining (endocardium) or of the heart valves. The bacteria that most often cause endocarditis are streptococci, staphylococci, and enterococci. |
| Body mass index (BMI) | A mathematical formula to assess body weight relative to height. The measure correlates highly with body fat. It is calculated as weight in kilograms divided by the square of the height in meters (kg/m2). |
| Centers for Disease Control and Prevention/National Center for Health Statistics (CDC/NCHS) | CDC is an agency within the US Department of Health and Human Services. The CDC conducts the Behavioral Risk Factor Surveillance System (BRFSS), an ongoing survey. The CDC/NCHS conducts or has conducted these surveys (among others):
|
| Centers for Medicare & Medicaid Services, formerly Health Care Financing Administration | The federal agency that administers the Medicare, Medicaid, and Child Health Insurance programs. |
| Comparability ratio | Provided by the NCHS to allow time-trend analysis from one International Classification of Diseases (ICD) revision to another. It compensates for the “shifting” of deaths from one causal code number to another. Its application to mortality based on one ICD revision means that mortality is “comparability modified” to be more comparable to mortality coded to the other ICD revision. |
| Coronary heart disease (CHD) (ICD-10 codes I20–I25) | This category includes acute myocardial infarction (I21–I22), other acute ischemic (coronary) heart disease (I24), angina pectoris (I20), atherosclerotic cardiovascular disease (I25.0), and all other forms of chronic ischemic coronary heart disease (I25.1–I25.9). |
| Death rate | The relative frequency with which death occurs within some specified interval of time in a population. National death rates are computed per 100 000 population. Dividing the total number of deaths by the total population gives a crude death rate for the total population. Rates calculated within specific subgroups, such as age-specific or sex-specific rates, are often more meaningful and informative. They allow well-defined subgroups of the total population to be examined. Unless otherwise stated, all death rates in this publication are age adjusted and are per 100 000 population. |
| Diseases of the circulatory system (ICD codes I00–I99) | Included as part of what the AHA calls “cardiovascular disease.” (“Total cardiovascular disease” in this Glossary.) |
| Diseases of the heart | Classification the NCHS uses in compiling the leading causes of death. Includes acute rheumatic fever/chronic rheumatic heart diseases (I00–I09), hypertensive heart disease (I11), hypertensive heart and renal disease (I13), coronary heart disease (I20–I25), pulmonary heart disease and diseases of pulmonary circulation (I26–I28), heart failure (I50), and other forms of heart disease (I29–I49, I50.1–I51). “Diseases of the heart” are not equivalent to “total cardiovascular disease,” which the AHA prefers to use to describe the leading causes of death. |
| Health Care Financing Administration | See Centers for Medicare & Medicaid Services. |
| Hispanic origin | In US government statistics, “Hispanic” includes people who trace their ancestry to Mexico, Puerto Rico, Cuba, Spain, the Spanish-speaking countries of Central or South America, the Dominican Republic, or other Spanish cultures, regardless of race. It does not include people from Brazil, Guyana, Suriname, Trinidad, Belize, or Portugal, because Spanish is not the first language in those countries. Most of the data in this update are for Mexican Americans or Mexicans, as reported by government agencies or specific studies. In many cases, data for all Hispanics are more difficult to obtain. |
| Hospital discharges | The number of inpatients (including newborn infants) discharged from short-stay hospitals for whom some type of disease was the first-listed diagnosis. Discharges include those discharged alive, dead, or “status unknown.” |
| International Classification of Diseases (ICD) codes | A classification system in standard use in the United States. The International Classification of Diseases is published by the World Health Organization. This system is reviewed and revised approximately every 10 to 20 years to ensure its continued flexibility and feasibility. The 10th revision (ICD-10) began with the release of 1999 final mortality data. The ICD revisions can cause considerable change in the number of deaths reported for a given disease. The NCHS provides “comparability ratios” to compensate for the “shifting” of deaths from one ICD code to another. To compare the number or rate of deaths with that of an earlier year, the “comparability-modified” number or rate is used. |
| Incidence | An estimate of the number of new cases of a disease that develop in a population, usually in a 1-year period. For some statistics, new and recurrent attacks, or cases, are combined. The incidence of a specific disease is estimated by multiplying the incidence rates reported in community- or hospital-based studies by the US population. The rates in this report change only when new data are available; they are not computed annually. |
| Major cardiovascular diseases | Disease classification commonly reported by the NCHS; represents ICD codes I00 to I78. The AHA does not use “major cardiovascular diseases” for any calculations. See “Total cardiovascular disease” in this Glossary. |
| Metabolic syndrome | Metabolic syndrome is defined* as the presence of any 3 of the following 5 diagnostic measures: Elevated waist circumference (≥102 cm in men or ≥88 cm in women), elevated triglycerides (≥150 mg/dL [1.7 mmol/L] or drug treatment for elevated triglycerides), reduced high-density lipoprotein cholesterol (<40 mg/dL [0.9 mmol/L] in men, <50 mg/dL [1.1 mmol/L] in women, or drug treatment for reduced high-density lipoprotein cholesterol), elevated blood pressure (≥130 mm Hg systolic blood pressure, ≥85 mm Hg diastolic blood pressure, or drug treatment for hypertension), and elevated fasting glucose (≥100 mg/dL or drug treatment for elevated glucose). |
| Morbidity | Incidence and prevalence rates are both measures of morbidity (ie, measures of various effects of disease on a population). |
| Mortality | Mortality data for states can be obtained from the NCHS Web site (http://cdc.gov/nchs/), by direct communication with the CDC/NCHS, or from the AHA on request. The total number of deaths attributable to a given disease in a population during a specific interval of time, usually 1 year, are reported. These data are compiled from death certificates and sent by state health agencies to the NCHS. The process of verifying and tabulating the data takes ≈2 years. |
| National Heart, Lung, and Blood Institute (NHLBI) | An institute in the National Institutes of Health in the US Department of Health and Human Services. The National Heart, Lung, and Blood Institute conducts such studies as the following:
|
| National Institute of Neurological Disorders and Stroke (NINDS) | An institute in the National Institutes of Health of the US Department of Health and Human Services. The National Institute of Neurological Disorders and Stroke sponsors and conducts research studies such as these:
|
| Physical activity | Any bodily movement produced by the contraction of skeletal muscle that increases energy expenditure above a basal level. |
| Physical fitness | The ability to perform daily tasks with vigor and alertness, without undue fatigue, and with ample energy to enjoy leisure-time pursuits and respond to emergencies. Physical fitness includes a number of components consisting of cardiorespiratory endurance (aerobic power), skeletal muscle endurance, skeletal muscle strength, skeletal muscle power, flexibility, balance, speed of movement, reaction time, and body composition. |
| Prevalence | An estimate of the total number of cases of a disease existing in a population during a specified period. Prevalence is sometimes expressed as a percentage of population. Rates for specific diseases are calculated from periodic health examination surveys that government agencies conduct. Annual changes in prevalence as reported in this statistical update reflect changes in the population size. Changes in rates can be evaluated only by comparing prevalence rates estimated from surveys conducted in different years. Note: In the data tables, which are located in the different disease and risk factor categories, if the percentages shown are age adjusted, they will not add to the total. |
| Race and Hispanic origin | Race and Hispanic origin are reported separately on death certificates. In this publication, unless otherwise specified, deaths of people of Hispanic origin are included in the totals for whites, blacks, American Indians or Alaska Natives, and Asian or Pacific Islanders according to the race listed on the decedent’s death certificate. Data for Hispanic people include all people of Hispanic origin of any race. See “Hispanic origin” in this Glossary. |
| Stroke (ICD-10 codes I60–I69) | This category includes subarachnoid hemorrhage (I60); intracerebral hemorrhage (I61); other nontraumatic intracranial hemorrhage (I62); cerebral infarction (I63); stroke, not specified as hemorrhage or infarction (I64); occlusion and stenosis of pre-cerebral arteries not resulting in cerebral infarction (I65); occlusion and stenosis of cerebral arteries not resulting in cerebral infarction (I66); other cerebrovascular diseases (I67); cerebrovascular disorders in diseases classified elsewhere (I68); and sequelae of cerebrovascular disease (I69). |
| Total cardiovascular disease (ICD-10 codes I00–I99, Q20–Q28) | This category includes rheumatic fever/rheumatic heart disease (I00–I09); hypertensive diseases (I10–I15); ischemic (coronary) heart disease (I20–I25); pulmonary heart disease and diseases of pulmonary circulation (I26–I28); other forms of heart disease (I30–I52); cerebrovascular disease (stroke) (I60–I69); atherosclerosis (I70); other diseases of arteries, arterioles, and capillaries (I71–I79); diseases of veins, lymphatics, and lymph nodes not classified elsewhere (I80–I89); and other and unspecified disorders of the circulatory system (I95–I99). When data are available, we include congenital cardiovascular defects (Q20–Q28). |
| Underlying cause of death or any-mention cause of death | These terms are used by the NCHS when defining mortality. Underlying cause of death is defined by the World Health Organization as “the disease or injury which initiated the chain of events leading directly to death, or the circumstances of the accident or violence which produced the fatal injury.” Contributing cause of death would be any other disease or condition that the decedent may also have had and that was reported on the death certificate but was not part of the chain of events leading directly to death. |
According to criteria established by the American Heart Association/National Heart, Lung, and Blood Institute and published in Circulation (Circulation. 2005;112:2735–2752).
Chart 9-4.
Extent of awareness, treatment, and control of high blood pressure by age (National Health and Nutrition Examination Survey: 2007–2010). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 10-2.
Age-adjusted prevalence of physician-diagnosed type 2 diabetes mellitus in adults ≥20 years of age by race/ethnicity and years of education (National Health and Nutrition Examination Survey: 2007–2010). NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-4.
Deaths attributable to cardiovascular disease (United States: 1900–2010). Cardiovascular disease (International Classification of Diseases, 10th Revision codes I00–I99) does not include congenital. Before 1933, data are for a death registration area and not the entire United States. Source: National Center for Health Statistics.
Chart 13-5.
Percentage breakdown of deaths attributable to cardiovascular disease (United States: 2010). Total may not add to 100 because of rounding. Coronary heart disease includes International Classification of Diseases, 10th Revision (ICD-10) codes I20 to I25; stroke, I60 to I69; heart failure, I50; high blood pressure, I10 to I15; diseases of the arteries, I70 to I78; and other, all remaining ICD-I0 I categories. *Not a true underlying cause. With any-mention deaths, heart failure accounts for 35% of cardiovascular disease deaths. Source: National Heart, Lung, and Blood Institute from National Center for Health Statistics reports and data sets.
Chart 13-6.
Cardiovascular disease (CVD) deaths vs cancer deaths by age (United States: 2010). CVD includes International Classification of Diseases, 10th Revision codes I00 to I99 and Q20 to Q28; cancer, C00 to C97. Source: National Center for Health Statistics.
Chart 13-7.
Cardiovascular disease (CVD) and other major causes of death: total, <85 years of age, and ≥85 years of age. Deaths among both sexes, United States, 2010. Heart disease includes International Classification of Diseases, 10th Revision codes I00 to I09, I11, I13, and I20 to I51; stroke, I60 to I69; all other CVD, I10, I12, I15, and I70 to I99; cancer, C00 to C97; chronic lower respiratory disease (CLRD), J40 to J47; Alzheimer disease, G30; and accidents, V01 to X59 and Y85 to Y86. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-8.
Cardiovascular disease (CVD) and other major causes of death in males: total, <85 years of age, and ≥85 years of age. Deaths among males, United States, 2010. Heart disease includes International Classification of Diseases, 10th Revision codes I00 to I09, I11, I13, and I20 to I51; stroke, I60 to I69; all other CVD, I10, I12, I15, and I70 to I99; cancer, C00 to C97; chronic lower respiratory disease (CLRD), J40 to J47; and accidents, V01 to X59 and Y85 to Y86. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-9.
Cardiovascular disease (CVD) and other major causes of death in females: total, <85 years of age, and ≥85 years of age. Deaths among females, United States, 2010. Heart disease includes International Classification of Diseases, 10th Revision codes I00 to I09, I11, I13, and I20 to I51; stroke, I60 to I69; all other CVD, I10, I12, I15, and I70 to I99; cancer, C00 to C97; chronic lower respiratory disease (CLRD), J40 to J47; and Alzheimer disease, G30. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-10.
Cardiovascular disease and other major causes of death for all males and females (United States: 2010). A indicates cardiovascular disease plus congenital cardiovascular disease (International Classification of Diseases, 10th Revision codes I00–I99 and Q20–Q28); B, cancer (C00–C97); C, accidents (V01–X59 and Y85–Y86); D, chronic lower respiratory disease (J40–J47); E, diabetes mellitus (E10–E14); and F, Alzheimer disease (G30). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-11.
Cardiovascular disease and other major causes of death for white males and females (United States: 2010). A indicates cardiovascular disease plus congenital cardiovascular disease (International Classification of Diseases, 10th Revision codes I00–I99 and Q20–Q28); B, cancer (C00–C97); C, accidents (V01–X59 and Y85–Y86); D, chronic lower respiratory disease (J40–J47); E, diabetes mellitus (E10–E14); and F, Alzheimer disease (G30). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-12.
Cardiovascular disease and other major causes of death for black males and females (United States: 2010). A indicates cardiovascular disease plus congenital cardiovascular disease (International Classification of Diseases, 10th Revision codes I00–I99 and Q20–Q28); B, cancer (C00–C97); C, accidents (V01–X59 and Y85–Y86); D, diabetes mellitus (E10–E14); E, chronic lower respiratory disease (J40–J47); F, nephritis (N00–N07, N17–N19, and N25–N27). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-13.
Cardiovascular disease and other major causes of death for Hispanic or Latino males and females (United States: 2010). A indicates cardiovascular disease plus congenital cardiovascular disease (International Classification of Diseases, 10th Revision codes I00–I99 and Q20–Q28); B, cancer (C00–C97); C, accidents (V01–X59 and Y85–Y86); D, diabetes mellitus (E10–E14); E, chronic lower respiratory disease (J40–J47); and F, nephritis (N00–N07, N17–N19, and N25–N27). Number of deaths shown may be lower than actual because of underreporting in this population. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-14.
Cardiovascular disease and other major causes of death for Asian or Pacific Islander males and females (United States: 2010). “Asian or Pacific Islander” is a heterogeneous category that includes people at high cardiovascular disease risk (eg, South Asian) and people at low cardiovascular disease risk (eg, Japanese). More specific data on these groups are not available. A indicates cardiovascular disease plus congenital cardiovascular disease (International Classification of Diseases, 10th Revision codes I00–I99 and Q20–Q28); B, cancer (C00–C97); C, accidents (V01–X59 and Y85–Y86); D, diabetes mellitus (E10–E14); E, chronic lower respiratory disease (J40–J47); and F, influenza and pneumonia (J09–J18). Number of deaths shown may be lower than actual because of underreporting in this population. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-15.
Cardiovascular disease and other major causes of death for American Indian or Alaska Native males and females (United States: 2010). A indicates cardiovascular disease plus congenital cardiovascular disease (International Classification of Diseases, 10th Revision codes I00–I99 and Q20–Q28); B, cancer (C00–C97); C, accidents (V01–X59 and Y85–Y86); D, diabetes mellitus (E10–E14); E, chronic liver disease (K70 and K73–K74); and F, chronic lower respiratory disease (J40–J47). Number of deaths shown may be lower than actual because of underreporting in this population. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-16.
Age-adjusted death rates for coronary heart disease (CHD), stroke, and lung and breast cancer for white and black females (United States: 2010). CHD includes International Classification of Diseases, 10th Revision codes I20 to I25; stroke, I60 to I69; lung cancer, C33 to C34; and breast cancer, C50. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-17.
Cardiovascular disease mortality trends for males and females (United States: 1979–2010). Cardiovascular disease excludes congenital cardiovascular defects (International Classification of Diseases [ICD], 10th Revision codes I00–I99). The overall comparability for cardiovascular disease between the ICD, 9th Revision codes (1979–1998) and ICD, 10th Revision codes (1999–2010) is 0.9962. No comparability ratios were applied. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 14-3.
Annual rate of first cerebral infarction by age, sex, and race (Greater Cincinnati/Northern Kentucky Stroke Study: 1999). Rates for black men and women 45 to 54 years of age and for black men ≥75 years of age are considered unreliable. Source: unpublished data from the Greater Cincinnati/Northern Kentucky Stroke Study.
Chart 14-4.
Annual rate of all first-ever strokes by age, sex, and race (Greater Cincinnati/Northern Kentucky Stroke Study: 1999). Rates for black men and women 45 to 54 years of age and for black men ≥75 years of age are considered unreliable.
Chart 14-10.
Proportion of patients dead within 5 years after first stroke. Source: pooled data from the Framingham Heart Study, Atherosclerosis Risk in Communities study, and Cardiovascular Health Study of the National Heart, Lung, and Blood Institute.
Chart 24-4.
Projected total (direct and indirect) costs of total cardiovascular disease by age (2012 $ in billions). Unpublished data tabulated by the American Heart Association using methods described by Heidenreich et al.8
Table 13-2.
Age-adjusted Death Rates per 100 000 Population for CVD, CHD, and Stroke by State, 2008 to 2010
| State | CVD*
|
CHD†
|
Stroke‡
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Rank§ | Death Rate | % Change, 1999–2001 to 2008–2010 | Rank§ | Death Rate | % Change, 1999–2001 to 2008–2010 | Rank§ | Death Rate | % Change, 1999–2001 to 2008–2010 | |
| Alabama | 51 | 314.8 | −19.2 | 25 | 110.3 | −32.6 | 52 | 54.4 | −21.8 |
| Alaska | 13 | 209.1 | −26.7 | 8 | 88.1 | −31.1 | 34 | 42.4 | −34.4 |
| Arizona | 6 | 204.0 | −28.7 | 27 | 111.9 | −31.0 | 4 | 32.5 | −37.7 |
| Arkansas | 49 | 299.4 | −21.8 | 48 | 149.7 | −20.0 | 51 | 53.7 | −30.2 |
| California | 25 | 226.0 | −31.2 | 30 | 116.0 | −39.0 | 19 | 39.2 | −37.9 |
| Colorado | 3 | 190.1 | −31.1 | 5 | 82.7 | −35.3 | 11 | 36.2 | −35.9 |
| Connecticut | 10 | 206.0 | −31.2 | 11 | 93.2 | −41.7 | 2 | 31.3 | −37.8 |
| Delaware | 29 | 235.1 | −29.7 | 33 | 119.9 | −39.3 | 24 | 40.4 | −22.3 |
| District of Columbia | 45 | 283.9 | −25.0 | 51 | 159.0 | −21.4 | 7 | 33.6 | −26.6 |
| Florida | 18 | 215.2 | −30.4 | 29 | 114.8 | −39.1 | 45 | 47.6 | −31.7 |
| Georgia | 41 | 265.9 | −29.4 | 10 | 91.7 | −43.2 | 18 | 39.1 | −33.4 |
| Hawaii | 4 | 196.2 | −27.6 | 3 | 77.1 | −32.1 | 33 | 41.7 | −36.6 |
| Idaho | 17 | 214.6 | −27.9 | 12 | 95.3 | −35.2 | 27 | 40.6 | −35.4 |
| Illinois | 31 | 243.7 | −30.0 | 32 | 117.1 | −38.7 | 39 | 44.9 | −34.0 |
| Indiana | 40 | 261.2 | −28.0 | 34 | 120.6 | −35.4 | 31 | 40.9 | −34.1 |
| Iowa | 30 | 238.1 | −24.8 | 42 | 132.6 | −28.7 | 38 | 44.3 | −31.5 |
| Kansas | 28 | 234.8 | −26.7 | 16 | 99.1 | −35.8 | 41 | 46.1 | −27.1 |
| Kentucky | 44 | 281.4 | −28.3 | 43 | 132.9 | −33.6 | 43 | 46.9 | −31.7 |
| Louisiana | 48 | 298.4 | −21.4 | 39 | 127.7 | −32.2 | 15 | 37.6 | −28.4 |
| Maine | 14 | 209.7 | −32.3 | 15 | 98.2 | −40.0 | 23 | 39.9 | −34.7 |
| Maryland | 32 | 245.1 | −28.1 | 38 | 127.1 | −32.8 | 5 | 33.0 | −35.8 |
| Massachusetts | 8 | 204.5 | −29.4 | 14 | 97.3 | −33.5 | 30 | 40.9 | −34.2 |
| Michigan | 42 | 270.0 | −27.2 | 45 | 140.7 | −33.3 | 10 | 36.1 | −33.3 |
| Minnesota | 1 | 175.2 | −32.7 | 1 | 70.3 | −41.4 | 50 | 51.6 | −35.6 |
| Mississippi | 52 | 335.7 | −22.7 | 41 | 131.6 | −36.8 | 40 | 46.0 | −27.7 |
| Missouri | 43 | 272.5 | −26.9 | 46 | 141.1 | −31.2 | 25 | 40.5 | −28.3 |
| Montana | 16 | 214.3 | −25.2 | 9 | 90.7 | −26.8 | 26 | 40.5 | −32.5 |
| Nebraska | 19 | 215.8 | −28.6 | 7 | 85.8 | −35.4 | 13 | 36.9 | −29.8 |
| Nevada | 36 | 254.3 | −25.7 | 19 | 101.8 | −37.8 | 8 | 33.9 | −35.1 |
| New Hampshire | 9 | 205.4 | −34.3 | 18 | 100.5 | −44.7 | 6 | 33.0 | −38.8 |
| New Jersey | 26 | 232.7 | −29.6 | 37 | 122.9 | −37.9 | 14 | 37.3 | −29.6 |
| New Mexico | 11 | 207.1 | −25.4 | 21 | 105.6 | −30.6 | 1 | 27.7 | −26.8 |
| New York | 37 | 257.6 | −27.1 | 52 | 160.2 | −32.6 | 44 | 47.5 | −31.6 |
| North Carolina | 33 | 246.0 | −31.1 | 28 | 112.7 | −38.2 | 21 | 39.5 | −37.3 |
| North Dakota | 20 | 216.7 | −28.6 | 26 | 111.6 | −32.7 | 37 | 43.2 | −33.8 |
| Ohio | 38 | 259.6 | −28.6 | 40 | 129.4 | −35.9 | 49 | 51.3 | −28.4 |
| Oklahoma | 50 | 309.5 | −23.9 | 49 | 156.3 | −31.9 | 35 | 42.6 | −24.8 |
| Oregon | 7 | 204.3 | −30.9 | 6 | 84.1 | −37.3 | 28 | 40.7 | −41.8 |
| Pennsylvania | 35 | 250.5 | −28.2 | 36 | 122.4 | −35.8 | 29 | 40.7 | −29.1 |
| Puerto Rico | 2 | 179.6 | −30.6 | 4 | 80.5 | −35.4 | 12 | 36.2 | −30.1 |
| Rhode Island | 23 | 223.8 | −28.4 | 44 | 135.9 | −35.1 | 3 | 32.3 | −32.4 |
| South Carolina | 39 | 260.0 | −29.1 | 24 | 109.5 | −37.8 | 48 | 50.6 | −36.7 |
| South Dakota | 22 | 222.1 | −26.6 | 35 | 122.1 | −26.7 | 22 | 39.7 | −31.5 |
| Tennessee | 46 | 289.8 | −26.0 | 50 | 157.5 | −28.1 | 47 | 50.2 | −33.8 |
| Texas | 34 | 248.5 | −29.1 | 31 | 116.9 | −39.4 | 42 | 46.3 | −29.3 |
| Utah | 5 | 197.1 | −27.2 | 2 | 72.1 | −36.1 | 16 | 38.1 | −37.3 |
| Vermont | 12 | 207.5 | −30.3 | 23 | 108.7 | −33.5 | 9 | 34.4 | −35.8 |
| Virginia | 27 | 232.8 | −29.7 | 17 | 100.2 | −36.3 | 36 | 43.0 | −35.9 |
| Washington | 15 | 212.9 | −29.0 | 22 | 105.8 | −32.9 | 20 | 39.3 | −42.8 |
| West Virginia | 47 | 291.9 | −26.5 | 47 | 144.0 | −34.5 | 46 | 47.6 | −22.4 |
| Wisconsin | 21 | 221.5 | −30.6 | 20 | 103.7 | −36.3 | 17 | 38.8 | −39.2 |
| Wyoming | 24 | 224.8 | −24.2 | 13 | 96.5 | −33.7 | 32 | 41.3 | −29.1 |
| Total United States | 242.4 | −28.6 | 119.1 | −36.0 | 40.3 | −32.9 | |||
CHD indicates coronary heart disease; and CVD, cardiovascular disease.
CVD is defined here as International Classification of Diseases, 10th Revision (ICD–10) codes I00 to I99.
CHD is defined here as ICD-10 codes I20 to I25.
Stroke is defined here as ICD-10 codes I60 to I69.
Rank is lowest to highest.
Source: Centers for Disease Control and Prevention (CDC) Wide-ranging Online Data for Epidemiologic Research (WONDER), 2008 to 2010. Data provided by personal communication with the National Heart, Lung, and Blood Institute. The Agency for Healthcare Research and Quality has released state-level data for heart disease for all 50 states and the District of Columbia; the data are taken from the congressionally mandated National Healthcare Quality Report.49 In addition, the Women’s Health and Mortality Chartbook of the National Center for Health Statistics has state-related data for women.50 Metropolitan/micropolitan area risk data are available for 500 such areas nationwide.51 Behavioral Risk Factor Surveillance System data are also collected within each state.52 The CDC has the Geographic Information Systems, which provides mortality rates down to the county level, by sex and ethnicity.53 The 2008 Atlas of Stroke Hospitalizations Among Medicare Beneficiaries is a new resource that provides data down to the county level, by sex and race.54
Table 22-2.
HF Quality-of-Care Measures, 2012
| Quality-of-Care Measure | National Data From HIQR Program* | AHA GWTG-HF | VHA |
|---|---|---|---|
| LVEF assessment | 98.7 | 96.5 | 100 |
| ARB/ACEI at discharge for patients with LVSD | 96.4 | 95.4 | 97 |
| Complete discharge instructions | 92.9 | 93.4 | 97 |
| Adult smoking cessation advice/counseling | 99† | 97.3 | 99 |
| β-Blockers at discharge for patients with LVSD, no contraindications | NM | 97.2 | NM |
| Anticoagulation for AF or atrial flutter, no contraindications | NM | 78.7 | Retired |
Values are percentages.
In the GWTG registry, mechanical ventilation was required in 0.9% of patients. In-hospital mortality was 2.5%, and mean length of hospital stay was 5.0 d (median 4.0 d).
AF indicates atrial fibrillation; AHA GWTG-HF, American Heart Association’s Get With The Guidelines–Heart Failure; ARB/ACEI, angiotensin receptor blocker/angiotensin-converting enzyme inhibitor; HF, heart failure; HIQR, Hospital Inpatient Quality Reporting; LVEF, left ventricular ejection fraction; LVSD, left ventricular systolic dysfunction; NM, not measured; and VHA, Veterans Health Administration.
HIQR Program includes data from all payers, including Medicare and Medicaid. Data reported include data from the third quarter of 2011 to the second quarter of 2012.
Measure was retired in January 2012.
Table 22-3.
Time Trends in GWTG-ACS Quality-of-Care Measures, 2006 to 2012
| Quality-of-Care Measure | 2006 | 2007 | 2008 | 2009 | 2010* | 2011* | 2012* |
|---|---|---|---|---|---|---|---|
| Aspirin within 24 h of admission | 94.7 | 92.8 | 91.2 | 90.9 | 97 | 97.6 | 97.8 |
| Aspirin at discharge | 94.4 | 95.8 | 94.9 | 95.5 | 98 | 98.3 | 98.4 |
| β-Blockers at discharge | 92.8 | 94.6 | 94.5 | 94.9 | 96 | 96.7 | 97.1 |
| Lipid-lowering medication at discharge | 84.5 | 85.6 | 81.6 | 86.8 | 92† | 98.4† | 98.8† |
| Lipid therapy at discharge if LDL cholesterol >100 mg/dL | 89.1 | 90.7 | 91.9 | 92.5 | NM | NM | NM |
| ARB/ACEI at discharge for patients with LVEF <40% | 87.3 | 91.1 | 91.9 | 91.9 | 86 | 87.8 | 89.7 |
| Adult smoking cessation advice/counseling | 94.3 | 97.4 | 98.4 | 98.4 | 98 | 98.4 | 98.4 |
| Cardiac rehabilitation referral for AMI patients | 71.1 | 63.6 | 52.0 | 49.1 | 75 | 76.5 | 77.3 |
Values are percentages.
In the ACTION (Acute Coronary Treatment and Intervention Outcomes Network) registry, the unadjusted in-hospital mortality rate for 2012 was 4.8% (95% confidence interval, 4.6%–4.9%; excludes transfer-out patients). The American Heart Association’s Get With The Guidelines–Coronary Artery Disease (GWTG-CAD) program has merged into the ACTION registry.
AMI indicates acute myocardial infarction; ARB/ACEI, angiotensin receptor blocker/angiotensin-converting enzyme inhibitor; GWTG-ACS, Get With The Guidelines–Acute Coronary Syndrome; LDL, low-density lipoprotein; LVEF, left ventricular ejection fraction; and NM, not measured.
Measures from 2006 to 2009 are from the American Heart Association’s GWTG-CAD registry. The 2010 to 2012 measures are from the American Heart Association’s ACTION registry. The 2012 data reported include data from the second quarter of 2012 to the first quarter of 2013.
Represents statin use.
Table 22-4.
Time Trends in GWTG-HF Quality-of-Care Measures, 2006 to 2012
| Quality-of-Care Measure | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|---|
| LVEF assessment* | 93.8 | 96.2 | 96.8 | 98.2 | 98 | 99.2 | 96.5 |
| ARB/ACEI at discharge for patients with LVSD* | 85.5 | 89.1 | 91.6 | 93.0 | 94.2 | 95.4 | 95.4 |
| Complete discharge instructions† | 78.8 | 84.8 | 88.5 | 90.9 | 93.3 | 93.5 | 93.4 |
| Postdischarge appointment (new for 2011)* | … | … | … | … | … | 13.3 | 47.4 |
| Adult smoking cessation advice/counseling† | 90.8 | 94.7 | 97.1 | 97.6 | 99.3 | 99.2 | 97.3 |
| β-Blockers at discharge for patients with LVSD, no contraindications† | 89.9 | 90.2 | 92.5 | 92.7 | 94.8 | 96.2 | 97.2 |
| Evidence-based specific β-blockers* | 67.7 | 58.9 | 54.1 | 45.2 | 48.4 | 58.4 | 82.6 |
| Anticoagulation for AF or atrial flutter, no contraindications | 62.9 | 61.6 | 60.7 | 68.9 | 70.2 | 75.4 | 78.7 |
Values are percentages.
In the GWTG registry, mechanical ventilation was required in 0.9% of patients. In-hospital mortality was 2.5%, and mean length of hospital stay was 5.0 d (median 4.0 d).
AF indicates atrial fibrillation; ARB/ACEI, angiotensin receptor blocker/angiotensin-converting enzyme inhibitor; GWTG-HF, Get With The Guidelines–Heart Failure; LVEF, left ventricular ejection fraction; and LVSD, left ventricular systolic dysfunction.
Indicates the 4 key achievement measures targeted in GWTG-HF. The composite quality-of-care measure for 2012 was 93.5%. The composite quality-of-care measure indicates performance on the provision of several elements of care. It is computed by summing the numerators for each key achievement measure across the population of interest to create a composite numerator (all the care that was given), summing the denominators for each measure to form a composite denominator (all the care that should have been given), and reporting the ratio (the percentage of all the needed care that was given). The composite performance measure includes β-blocker at discharge instead of evidence-based specific β-blockers and complete discharge instructions instead of postdischarge appointment until data collection for the new achievement measures stabilizes.
Indicates historical key achievement measures in GWTG-HF. The composite quality-of-care measure for 2012 for the historical key achievement measures was 64.9%.
Table 22-5.
Time Trends in GWTG-Stroke Quality-of-Care Measures, 2006 to 2012
| Quality-of-Care Measure | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|---|
| IV tPA in patients who arrived ≤2 h after symptom onset, treated ≤3 h* | 55.8 | 60.2 | 63.9 | 73.1 | 76.2 | 78.3 | 82.0 |
| IV tPA in patients who arrived <3.5 h after symptom onset, treated ≤4.5 h | … | … | … | … | 42.5 | 57.9 | 60.4 |
| IV tPA door-to-needle time ≤60 min | 22.5 | 24.9 | 25.9 | 28.0 | 29.5 | 33.8 | 39.9 |
| Thrombolytic complications: IV tPA and life-threatening, serious systemic hemorrhage | 20.8 | 17.3 | 16.1 | 15.1 | 13.1 | 15.7 | 16.5 |
| Antithrombotics <48 h after admission* | 94.8 | 95.8 | 96.0 | 96.2 | 96.3 | 96.7 | 96.9 |
| DVT prophylaxis by second hospital day* | 85.3 | 88.9 | 92.2 | 92.7 | 92.2 | 93.5 | 98.4 |
| Antithrombotics at discharge* | 94.1 | 95.1 | 97.0 | 97.8 | 97.7 | 98.1 | 97.8 |
| Anticoagulation for AF at discharge* | 88.2 | 89.5 | 93.1 | 93.5 | 93.5 | 93.1 | 93.4 |
| Therapy at discharge if LDL cholesterol >100 mg/dL or LDL cholesterol not measured or on therapy at admission* | 70.3 | 76.3 | 82.1 | 86.2 | 88.1 | 89.8 | 94.5 |
| Counseling for smoking cessation* | 86.1 | 92.2 | 94.3 | 96.2 | 96.7 | 97.0 | 96.8 |
| Lifestyle changes recommended for BMI >25 kg/m2 | 42.5 | 45.7 | 51.7 | 57.3 | 57.8 | 57.8 | 57.2 |
| Composite quality-of-care measure | 85.9 | 88.9 | 91.7 | 93.3 | 93.7 | 94.4 | 96.3 |
Values are percentages.
In-hospital mortality for the 2012 patient population was 6.4%, and mean length of hospital stay was 5.2 d (median 3.0 d).
AF indicates atrial fibrillation; BMI, body mass index; DVT, deep vein thrombosis; GWTG-Stroke, Get With The Guidelines–Stroke; IV, intravenous; LDL, low-density lipoprotein; and tPA, tissue-type plasminogen activator.
Indicates the 7 key achievement measures targeted in GWTG-Stroke.
Table 22-13.
Quality of Care by Race/Ethnicity and Sex in the GWTG-HF Program, 2012
| Quality-of-Care Measure | White | Black | Hispanic | Men | Women |
|---|---|---|---|---|---|
| Postdischarge appointment (new for 2011)* | 48.4 | 53.6 | 41.7 | 49.9 | 48.4 |
| Complete set of discharge instructions† | 93.2 | 94.3 | 93.2 | 93.9 | 92.9 |
| Measure of LV function* | 96.4 | 96.4 | 92.7 | 96.8 | 95.9 |
| ACEI or ARB at discharge for patients with LVSD, no contraindications* | 95.0 | 96.5 | 95.3 | 95.5 | 95.3 |
| Smoking cessation counseling, current smokers† | 97.1 | 97.9 | 95.9 | 97.3 | 97.1 |
| Evidence-based specific β-blockers* | 82.0 | 86.4 | 84.2 | 83.9 | 82.8 |
| β-Blockers at discharge for patients with LVSD, no contraindications† | 97.4 | 97.6 | 96.2 | 97.3 | 97.3 |
| Hydralazine/nitrates at discharge for patients with LVSD, no contraindications‡ | … | 20.1 | … | 21.3 | 17.0 |
| Anticoagulation for AF or atrial flutter, no contraindications | 79.8 | 76.0 | 69.2 | 80.6 | 76.7 |
| Composite quality-of-care measure (with discharge instructions and β-blocker at discharge) | 93.3 | 93.8 | 89.9 | 93.9 | 92.9 |
Values are percentages.
Quality-of-care measures stratified by race/ethnicity and sex are reported for hospitals participating in GWTG from January 1, 2012, through December 31, 2012.
ACEI indicates angiotensin-converting enzyme inhibitor; AF, atrial fibrillation; ARB, angiotensin receptor blocker; ellipses (…), no data; GWTG-HF, Get With The Guidelines–Heart Failure; LV, left ventricular; and LVSD, left ventricular systolic dysfunction.
Indicates the 4 key achievement measures targeted in GWTG-HF.
Indicates historical key achievement measures in GWTG-HF.
For black patients only.
Table 25-2.
Females and CVD: At-a-Glance Table
| Diseases and Risk Factors | Both Sexes | Total Females | White Females | Black Females | Mexican American Females |
|---|---|---|---|---|---|
| Smoking | |||||
| Prevalence, 2012* | 42.1 M (18.1%) | 19.1 M (15.9%) | 19.2% | 14.2% | 7.5%† |
| PA‡ | |||||
| Prevalence, 2012* | 20.7% | 17.1% | 19.9% | 10.8% | 12.2%† |
| Overweight and obesity | |||||
| Prevalence, 2010 | |||||
| Overweight and obesity, BMI >25.0 kg/m2§ | 154.7 M (68.2%) | 74.8 M (63.7%) | 60.2% | 79.9% | 78.2% |
| Obesity, BMI >30.0 kg/m2§ | 78.4 M (34.6%) | 41.6 M (35.6%) | 32.5% | 53.9% | 44.8% |
| Blood cholesterol | |||||
| Prevalence, 2010 | |||||
| Total cholesterol >200 mg/dL§ | 98.9 M (43.4%) | 53.6 M (44.9%) | 45.8% | 40.7% | 44.7% |
| Total cholesterol >240 mg/dL§ | 31.9 M (13.8%) | 17.9 M (14.7%) | 15.6% | 11.7% | 13.5% |
| LDL cholesterol >130 mg/dL§ | 71.0 M (31.1%) | 35.8 M (30.0%) | 29.3% | 31.2% | 30.4% |
| HDL cholesterol <40 mg/dL§ | 48.7 M (21.8%) | 14.1 M (12.3%) | 12.4% | 10.2% | 15.1% |
| HBP | |||||
| Prevalence, 2010§ | 77.9 M (33.0%) | 40.7 M (32.2%) | 30.7% | 47.0% | 28.8% |
| Mortality, 2010|| | 63 119 | 34 746 | 26 798 | 6923 | N/A |
| DM | |||||
| Prevalence, 2010 | |||||
| Physician-diagnosed DM§ | 19.7 M (8.3%) | 10.1 M (7.9%) | 6.2% | 15.4% | 12.0% |
| Undiagnosed DM§ | 8.2 M (3.5%) | 2.9 M (2.3%) | 1.8% | 2.9% | 4.7% |
| Prediabetes§ | 87.3 M (38.2%) | 33.6 M (30.5%) | 30.0% | 29.0% | 31.9% |
| Incidence, diagnosed DM§ | 1.9 M | N/A | N/A | N/A | N/A |
| Mortality, 2010|| | 69 071 | 33 581 | 25 764 | 6486 | N/A |
| Total CVD | |||||
| Prevalence, 2010§ | 83.6 M (35.3%) | 42.9 M (34.0%) | 32.4% | 48.9% | 30.7% |
| Mortality, 2010||¶ | 787 650 | 400 332 | 342 581 | 49 977 | N/A |
| Stroke | |||||
| Prevalence, 2010§ | 6.8 M (2.8%) | 3.8 M (3.0%) | 2.9% | 4.7% | 1.4% |
| New and recurrent strokes|| | 795.0 K | 425.0 K | 365.0 K | 60.0 K | N/A |
| Mortality, 2010|| | 129 476 | 77 109 | 65 695 | 9027 | N/A |
| CHD | |||||
| Prevalence, CHD, 2010§ | 15.4 M (6.4%) | 6.6 M (5.1%) | 4.6% | 7.1% | 5.3% |
| Prevalence, MI, 2010§ | 7.6 M (2.9%) | 2.6 M (1.7%) | 1.5% | 2.3% | 1.7% |
| Prevalence, AP, 2010§ | 7.8 M (3.2%) | 4.1 M (3.2%) | 2.8% | 5.4% | 3.3% |
| New and recurrent CHD#** | 915.0 K | 385.0 K | 330.0 K | 55.0 K | N/A |
| New and recurrent MI** | 720.0 K | 300.0 K | N/A | N/A | N/A |
| Incidence, AP (stable angina)‡‡ | 565.0 K | 195.0 K | N/A | N/A | N/A |
| Mortality, 2010, CHD|| | 379 559 | 171 979 | 148 891 | 19 015 | N/A |
| Mortality, 2010, MI|| | 122 071 | 54 636 | 47 023 | 6298 | N/A |
| HF | |||||
| Prevalence, 2010§ | 5.1 M (2.1%) | 2.4 M (1.8%) | 1.8% | 3.0% | 1.1% |
| Incidence, 2010‡‡ | 825 000 | 430 000 | 375 000 | 55 000 | N/A |
| Mortality, 2010|| | 57 757 | 33 372 | 29 750 | 3084 | N/A |
AP indicates angina pectoris (chest pain); BMI, body mass index; CHD, coronary heart disease (includes heart attack, angina pectoris chest pain, or both); CVD, cardiovascular disease; DM, diabetes mellitus; HBP, high blood pressure; HDL, high-density lipoprotein; HF, heart failure; K, thousands; LDL, low-density lipoprotein; M, millions; MI, myocardial infarction (heart attack); N/A, data not available; and PA, physical activity.
Age ≥18 y (National Health Interview Survey).
All Hispanic (National Health Interview Survey).
Met 2008 full Federal PA guidelines for adults.
Age ≥20 y.
All ages.
Total CVD mortality includes deaths from congenital heart disease.
New and recurrent MI and fatal CHD.
Age ≥35 y.
Age ≥45 y.
Table 25-3.
Race/Ethnicity and CVD: At-a-Glance Table
| Diseases and Risk Factors | Both Sexes | Whites
|
Blacks
|
Mexican Americans
|
Hispanics/Latinos
|
Asians: Both Sexes | American Indian/Alaska Native: Both Sexes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | Males | Females | ||||
| Smoking | |||||||||||
| Prevalence, 2012* | 42.1 M (18.1%) | 22.0% | 19.2% | 21.6% | 14.2% | 11.3% | 16.6% | 7.5% | 10.4% | 18.8% | |
| PA† | |||||||||||
| Prevalence, 2012* | 20.7% | 20.6% | 21.4% | 14.9% | 15.7% | 18.7% | 16.8% | ||||
| Overweight and obesity | |||||||||||
| Prevalence, 2010 | |||||||||||
| Overweight and obesity, BMI >25.0 kg/m2‡ | 154.7 M (68.2%) | 73.1% | 60.2% | 68.7% | 79.9% | 81.3% | 78.2% | N/A | N/A | N/A | N/A |
| Overweight and obesity, BMI >30.0 kg/m2‡ | 78.4 M (34.6%) | 33.8% | 32.5% | 37.9% | 53.9% | 36.0% | 44.8% | N/A | N/A | N/A | N/A |
| Blood cholesterol | |||||||||||
| Prevalence, 2010 | |||||||||||
| Total cholesterol >200 mg/dL‡ | 98.9 M (43.4%) | 40.5% | 45.8% | 38.6% | 40.7% | 48.1% | 44.7% | N/A | N/A | N/A | N/A |
| Total cholesterol >240 mg/dL‡ | 31.9 M (13.8%) | 12.3% | 15.6% | 10.8% | 11.7% | 15.2% | 13.5% | N/A | N/A | N/A | N/A |
| LDL cholesterol >130 mg/dL‡ | 71.0 M (31.1%) | 30.1% | 29.3% | 33.1% | 31.2% | 39.9% | 30.4% | N/A | N/A | N/A | N/A |
| HDL cholesterol <40 mg/dL‡ | 48.7 M (21.8%) | 33.1% | 12.4% | 20.3% | 10.2% | 34.2% | 15.1% | N/A | N/A | N/A | N/A |
| HBP | |||||||||||
| Prevalence, 2010‡ | 77.9 M (33.0%) | 33.4% | 30.7% | 42.6% | 47.0% | 30.1% | 28.8% | 20.9%* | 21.27%* | 24.8%* | |
| Mortality, 2010§ | 63 119 | 20 819 | 26 798 | 6670 | 6923 | N/A | N/A | N/A | N/A | 1578 | 331 |
| DM | |||||||||||
| Prevalence, 2010 | |||||||||||
| Physician-diagnosed DM‡ | 19.7 M (8.3%) | 7.7% | 6.2% | 13.5% | 15.4% | 11.4% | 12.0% | N/A | N/A | N/A | N/A |
| Undiagnosed DM‡ | 8.2 M (3.5%) | 4.5% | 1.8% | 4.8% | 2.9% | 6.6% | 4.7% | N/A | N/A | N/A | N/A |
| Prediabetes‡ | 87.3 M (38.2%) | 47.7% | 30.0% | 35.7% | 29.0% | 47.0% | 31.9% | N/A | N/A | N/A | N/A |
| Incidence, diagnosed DM‡ | 1.9 M | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Mortality, 2010§ | 69 071 | 28 486 | 25 764 | 5640 | 6486 | N/A | N/A | N/A | N/A | 1838 | 857 |
| Total CVD | |||||||||||
| Prevalence, 2010‡ | 83.6 M (35.3%) | 36.6% | 32.4% | 44.4% | 48.9% | 33.4% | 30.7% | N/A | N/A | N/A | N/A |
| Mortality, 2010§|| | 787 650 | 330 330 | 342 581 | 46 266 | 49 977 | N/A | N/A | N/A | N/A | 16 829 | 3667 |
| Stroke | |||||||||||
| Prevalence, 2010‡ | 6.8 M (2.8%) | 2.4% | 2.9% | 4.3% | 4.7% | 2.3% | 1.4% | 2.7%* | 1.8%* | 4.3%*¶ | |
| New and recurrent strokes§ | 795.0 K | 325.0 K | 365.0 K | 45.0 K | 60.0 K | N/A | N/A | N/A | N/A | N/A | N/A |
| Mortality, 2010§ | 129 476 | 43 424 | 65 695 | 6938 | 9027 | N/A | N/A | N/A | N/A | 3833 | 559 |
| CHD | |||||||||||
| Prevalence, CHD, 2010‡ | 15.4 M (6.4%) | 8.2% | 4.6% | 6.8% | 7.1% | 6.7% | 5.3% | N/A | N/A | N/A | N/A |
| Prevalence, MI, 2010‡ | 7.6 M (2.9%) | 4.4% | 1.5% | 3.9% | 2.3% | 3.6% | 1.7% | N/A | N/A | N/A | N/A |
| Prevalence, AP, 2010‡ | 7.8 M (3.2%) | 3.3% | 2.8% | 2.4% | 5.4% | 3.4% | 3.3% | N/A | N/A | N/A | N/A |
| New and recurrent CHD#** | 915.0 K | 465.0 K | 330.0 K | 65.0 K | 55.0 K | N/A | N/A | N/A | N/A | N/A | N/A |
| Mortality, CHD, 2010§ | 379 559 | 181 386 | 148 891 | 20 615 | 19 015 | N/A | N/A | N/A | N/A | 7821 | 1831 |
| Mortality, MI, 2010§ | 122 071 | 59 181 | 47 023 | 6445 | 6298 | N/A | N/A | N/A | N/A | 2530 | 594 |
| HF | |||||||||||
| Prevalence, 2010‡ | 5.1 M (2.1%) | 2.5% | 1.8% | 4.1% | 3.0% | 1.9% | 1.1% | N/A | N/A | N/A | N/A |
| Incidence, 2010‡‡ | 825 000 | 350 000 | 375 000 | 45 000 | 55 000 | N/A | N/A | N/A | N/A | N/A | N/A |
| Mortality, 2010§ | 57 757 | 21 540 | 29 750 | 2444 | 3084 | N/A | N/A | N/A | N/A | 714 | 225 |
AP, angina pectoris (chest pain); BMI, body mass index; CHD, coronary heart disease (includes heart attack, angina pectoris chest pain, or both); CVD, cardiovascular disease; DM, diabetes mellitus; HBP, high blood pressure; HDL, high-density lipoprotein; HF, heart failure; K, thousands; LDL, low-density lipoprotein; M, millions; MI, myocardial infarction (heart attack); N/A, data not available; and PA, physical activity;.
Age ≥18 y (National Health Interview Survey, 2012).
Met 2008 full Federal PA guidelines for adults.
Age ≥20 y.
All ages.
Total CVD mortality includes deaths from congenital heart disease.
Figure not considered reliable.
New and recurrent MI and fatal CHD.
Age ≥35 y.
Age ≥45 y.
Acknowledgments
We wish to thank Lucy Hsu, Michael Wolz, Sean Coady, and Khurram Nasir for their valuable comments and contributions. We would like to acknowledge Lauren Rowell for her administrative assistance.