Abstract
Introduction
Interdisciplinary collaboration is a critical component of translation, dissemination, implementation, and improvement (TDII) science. Yet, little is known about effective frameworks and practices regarding interdisciplinary research in TDII.
Methods
This study drew on data collected from an expert panel during a regional symposium.
Results
Findings highlight facilitators and barriers to stimulating interdisciplinary TDII research in different domains: intrapersonal, interpersonal, organizational, power and hierarchy, physical environment, and communication and language.
Conclusions
Findings have significant implications for TDII of clinical practices.
Key words: Dissemination, implementation, interdisciplinary research
Introduction
Translation, dissemination, implementation, and improvement (TDII) research is a rapidly growing field that seeks to understand and develop systematic strategies to enhance the uptake of evidence-based practices (EBPs) that improve health-care delivery [1–4]. Health sciences researchers in multiple disciplines, including psychology, health services, epidemiology, social work, and medicine, are gradually recognizing the importance of using TDII methodologies to translate evidence into practice [3, 5]; however, researchers face significant barriers to working together and engaging in TDII research.
Interdisciplinarity—defined as interdisciplinary collaboration among stakeholders based in different institutions, ideologies, and methodological approaches—has been identified as critical to successfully overcoming barriers to the uptake of EBPs [2, 6–8]. The purpose of this manuscript is to discuss barriers to and facilitators of interdisciplinarity in TDII drawn from a multidisciplinary expert panel. By addressing this emerging emphasis, we seek to contribute to solutions to integrate various disciplines and settings that engage in team-based and cross-disciplinary research [9, 10], ultimately enhancing interdisciplinary TDII research.
Conceptual Framework
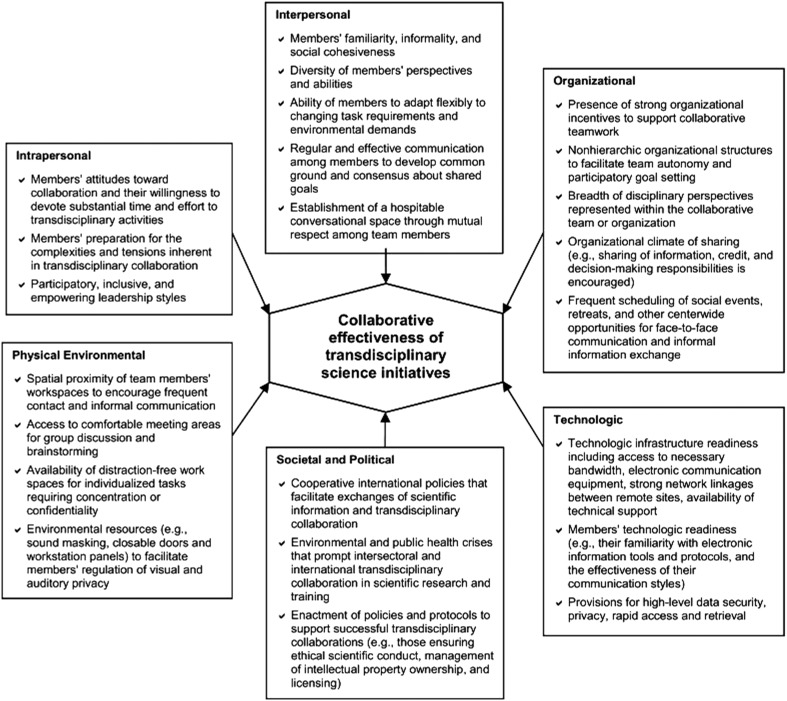
We rely on Stokols’ interdisciplinary team science framework (Fig. 1) to identify barriers and facilitators related to ideological, structural, and organizational dimensions of effective collaboration across disciplinary teams. Stokols’ work is informed by the science of team science (SciTS). SciTS is concerned with understanding multilevel factors that facilitate or hinder a wide range of collaborative, team-based research efforts [9, 11] and seeks to understand conditions, processes, and outcomes associated with successes and failures of interdisciplinary team science initiatives [11]. The fields of SciTS and TDII research are complementary; both focus on intrapersonal, interpersonal, organizational and institutional, physical and environmental, societal and political, and technological contextual factors that contribute to understanding the impact of interventions on team effectiveness, health intervention outcomes, or both. SciTS can be used to understand how to build effective team performance and interdisciplinary collaboration [11, 12] that may lead to effective translation of TDII research findings into practice [12].
Fig. 1.
Contextual factors influencing a transdisciplinary collaboration framework [11]. Reproduced from Stokols et al. (2008) [11], with permission from Elsevier.
Materials and Methods
The work presented here arose from formal presentations and small group discussions during the 2014 Southern California Dissemination, Implementation, and Improvement Science Symposium, sponsored by the University of California, Los Angeles Clinical Translational Science Institute; the University of Southern California Clinical and Translational Science Institute; and Kaiser Permanente. The goal of the day-long symposium was to accelerate the quantity and quality of TDII science programs and activities.
Participants were 12 senior and junior investigators, research fellows, leaders of local health-care delivery systems and public health agencies, and research partners in community-based organizations in Los Angeles. Participants represented a wide variety of disciplines including health services (7), sociology (3), and psychology (2). Participants also reported conducting research at different research institutions, including the US Department of Veteran Affairs, research universities (University of California, Los Angeles; University of Southern California; and Azusa Pacific University), and research centers in medical settings. Most participants were located in a medical organization.
Breakout sessions were moderated by a faculty member and a fellow who were selected based on their expertise and experience in the discussion topic. The session followed a semistructured question and answer format with open-ended questions posed by session leaders. The session began with initiation questions and moved to an iterative process in which new questions were developed and asked during the session. The session was audio recorded and transcribed, and written notes from attendees and session leaders were synthesized and reviewed for accuracy by the 2 session leaders. Semistructured questions used to initiate discussion included (1) How do we define interdisciplinary? (2) What are some challenges and barriers to working in interdisciplinary teams? (3) What are some potential solutions or facilitators to overcome these barriers? The identified topics spanned ideological (disciplinary orientations that prevent collaboration), structural (workplaces that isolate or limit collaboration), and organizational (poor leadership and communication that limit collaboration) domains, to an extent conforming to the Stokols et al.’s [11] framework of contextual factors that influence transdisciplinary collaboration.
Summary of Findings
Participants broadly defined discipline as an organized body of knowledge and methods. As such, the group identified >25 disciplines with direct relevance to building TDII research. Although participants represented fewer than half of those disciplines, they highlighted the importance of reaching out to scientists from those disciplines to strengthen interdisciplinary connections to develop TDII research in health and health care. Table 1 lists some of the stakeholders that participants said should be included in the discussion and execution of interdisciplinary TDII research.
Table 1.
Proposed disciplines with relevance to interdisciplinary dissemination and implementation research in health sciences
| Sociology | Education |
| Nursing | Psychology |
| Medicine | Social work |
| Health services research | Patients |
| Medical sociology | Behavioral health |
| Implementation science | Engineering |
| Health policy and management | Computer science |
| Organizational studies | Marketing |
| Economics | Urban planning |
| Industrial psychology | Parks and recreation |
| Communications | Community |
| Health-care operations | Biology and laboratory science |
| Ethnography | Health information technology |
Broadly, the identified issues fell into 4 of the 6 categories of the Stokols et al.’s [11] framework: intrapersonal, interpersonal, organizational, and physical environment. Subdomains were identified for each of these factors, including leadership, power and organizational hierarchy, accountability and responsibility, taxonomy and language, and exposure and isolation. Responding to iterative questioning, the group also provided a very thoughtful list of management practices, problems, and solutions for each of the 6 categories of the SciTS framework (see Table 2).
Table 2.
Management practices, problems, and solutions
| Management practices | Problems | Solutions | Examples |
|---|---|---|---|
| Intrapersonal | |||
| Accountability and responsibility | Challenges for team members related to time constraints, role confusion, limited motivation, and other contextual pressures | Emphasize structure and clarity in role definition, engage individual activities, foster collaboration among group members, and promote positive communication | Team members assigned to different tasks based on expertise in order to meet shared goals |
| Interpersonal | |||
| Leadership | Supportive leadership across disciplines may be a complex and lengthy process | Engage scholars in identifying goals and objectives at different levels of leadership. Set time frames and check progress regularly across team members | Institutional leaders can create synergies across professional schools by convening scientists and providing a vision, resources, and support for collaboration across a university setting |
| Organizational | |||
| Exposure to other disciplines | Exclusive focus on specialty journals, conferences, and training that challenge scholars to go beyond their discipline | Develop interdisciplinary team training early in graduate education and reshape conceptualized roles, influence the likelihood of future interdisciplinary interactions, and normalize those interactions | Medical and nursing schools that successfully implement programs for students to learn about patient care and health-care delivery in a team-based context |
| Power and hierarchy | Power hierarchies may negatively influence how members from different disciplines interact and engage when working toward a common goal | Achieving equal voice on the team and concurrent perceptions of safety when interacting across discipline is a necessary component of effective interdisciplinary DII research. Emphasis needs to be placed on diverse levels of institutions, policies, leaders, teams, and collaboration | Setting a team culture and practice whereby clinicians from diverse disciplines (pharmacy, nursing, medicine, social work, and allied health services) equally contribute to the research collaboration. This is also through team members’ appreciation and value of different training and experiences |
| Physical environment | |||
| Structure and isolation | Tendency of single disciplines to create structural and ideological silos decreasing opportunities for multidisciplinary teams to define accountability and responsibility that are meaningful | Emphasize collaboration in publications, revenue streams, quality metrics, memoranda of understanding, and tenure criteria. Aligning incentives to promote interdisciplinary partnerships | Large collaboration between HMO Research Network’s Virtual Data Warehouse and the University of California Research Data Exchange Scientist |
| Communication, taxonomy, and language | Structural content of communication across disciplines, which lacks congruence to develop coherent principles and paradigms | Develop consolidated frameworks for a variety of DII research areas by engaging different disciplines in the process of unifying conceptual and methodological approaches | Exploring National Institutes of Health resources on building interdisciplinary teams for potential solutions such as meetings with researchers from different departments in order to consolidate information under a unifying framework |
DII, dissemination, implementation, and improvement.
Intrapersonal
Accountability and Responsibility
The panel participants emphasized the importance of development and recognition of boundaries and responsibilities regarding the processes of interdisciplinary TDII research. In collaborations, research team members are assigned to different tasks because it can be beneficial to build on the existing expertise of individual members to meet shared goals. It may become a challenge if team members face time constraints, role confusion, limited motivation, and other contextual pressures. These issues illustrate the need for solutions that help define ownership (accountability) and commitment (responsibility) and are focused on both individual and group needs and priorities. The literature on setting goals and teamwork may provide guidance in working with diverse team members and identifying overarching, beneficial, and common goals when engaging in interdisciplinary TDII research [13, 14]. This work design requires structure and clarity, so each member knows his or her role in accomplishing the overarching goal without overstepping boundaries or neglecting to engage in individual activities, fostering collaboration among groups, and promoting the health of the community.
Interpersonal
Leadership
We identified multiple issues and challenges related to leadership and facilitating or constraining interdisciplinary TDII research. Participants reported an example in which institutional leaders created synergies across 2 professional schools (social work and engineering) by convening scientists and providing a vision, resources, and support for collaboration across a university setting. A second example took place at Kaiser Permanente, where the leader of a department implemented a process for collaboration across specialists and allied health professionals to manage patients with heart failure. Overall, these examples and participant reports suggest that to engage relevant leaders in interdisciplinary TDII research, it is necessary to foster leadership commitment to interdisciplinary work by exposing leaders to models and teams from different disciplines and identifying visionary supportive leaders to act as local champions.
Leadership engagement and buy-in has been shown to be critical to success in organizational change, quality improvement, and effective implementation in health and social services [14–16]. Interdisciplinary TDII research involves leadership from multiple disciplines, potentially increasing the complexity of and need for engagement and buy-in [3]. Identifying appropriate supportive leadership across disciplines and achieving high-level agreement on goals and objectives may be a complex and lengthy process. In addition, different levels of leadership may be required to move interdisciplinary health sciences TDII research forward. For example, research in a health system setting may require regional and local leadership involvement, such as an area medical chief and a service line leader (eg, oncology, cardiology), and may need to represent both clinical and operational leaders. Leadership style may also vary across these levels and disciplines, but the common thread is leaders’ vision of how interdisciplinary work will improve TDII research.
Organizational
Exposure to Other Disciplines
Another important issue identified was the challenge of finding and connecting with partners and stakeholders in other disciplines. Participants suggested investing in and developing interdisciplinary team training early in graduate education. For example, some medical and nursing schools have successfully implemented programs for students to learn about patient care and health-care delivery in a team-based context. The expectation is that exposure during formative training will help reshape conceptualized roles, influence the likelihood of future interdisciplinary interactions, and normalize those interactions.
Scientists tend to focus on journals, conferences, and training that align with single-discipline silos, with limited opportunities for engagement in activities that cross silos. There may also be a limited number of role models who employ a multidisciplinary approach and model successful expansion beyond disciplinary silos and specialty boundaries. The main challenge is to find leaders in other disciplines who can expand the perspectives of potential collaborators.
Power and Hierarchy
Closely related to leadership are issues of power and organizational hierarchy related to engaging in interdisciplinary TDII activities. To decrease power differentials based on discipline status or other ideologies, participants suggested including leadership interventions to promote teamwork, active discouragement of use of status, and collaboration efforts across disciplines and within organizations to encourage effective interaction and communication among members. Specifically, interdisciplinary TDII research needs to focus on the different levels of institutions, policies, leaders, teams, and individuals that influence collaboration.
Demonstrating appreciation for and the value of team members with different training, experience, and expectations regarding research evidence, statistical analyses, and theoretical and conceptual methods is critical to the success of interdisciplinary TDII research. However, power hierarchies may play a role in how members from different disciplines (eg, medicine and social work) interact and engage when working toward a common goal. The organizational literature has relied on leadership and managerial interventions that seek to alter the norms and values of organizational culture to reduce conflict among team members [17–19]. The effectiveness of these interventions is enhanced through experience and competence at individual, group, and organizational levels [17]. Knowledge and experience that is highly valued in one discipline may not be as valued, or even regarded unfavorably, in another. Achieving equal voice on the team, and concurrent perceptions of safety when interacting across disciplines, is a necessary component of effective interdisciplinary TDII research [14].
Physical Environment
Structure and Isolation
Another important theme of this discussion involved silos—specifically, the tendency of single disciplines to create structural and ideological silos. Participants agreed that this is a significant barrier to collaboration. To promote communication across disciplines, they said it is important to invest in and develop robust data infrastructures to facilitate collaboration. Examples of such efforts include the Health Maintenance Organization (HMO) Research Network’s Virtual Data Warehouse and the University of California Research Data Exchange. Having common data standards facilitates multisite interdisciplinary research and provides a common language for clinicians and researchers from diverse backgrounds to easily communicate and engage in research.
Formally discussing differing incentives and developing a structured approach to aligning incentives across disciplines are crucial steps in developing interdisciplinary partnerships. The importance of factors such as publications, revenue streams, quality metrics, memoranda of understanding, and tenure must be explicitly discussed during the formation of interdisciplinary TDII teams and creation of specific incentives for collaboration in partnership agreements. These recommendations are a first step toward reducing structural and ideological silos and have the potential to influence the amount, content, and impact of interdisciplinary translational TDII research.
Communication, Taxonomy, and Language
Another challenge to promoting interdisciplinary TDII research is the structural content of communication across disciplines. Scientists from different disciplines may refer to the same phenomena with different terms. To respond to these issues, the group suggested the use of interdisciplinary language to develop consolidated frameworks for a variety of TDII research areas. This approach can draw from the development of the consolidated framework for implementation research led by researchers at the US Department of Veterans Affairs [20], which organized meetings with researchers at different departments and staff members at different levels to consolidate information under a unifying framework. To pursue approaches such as concept mapping (ie, a graphic organizer for representing concepts), participants recommended exploring National Institutes of Health resources on building interdisciplinary teams and relying on information science to allow rapid, reproducible mapping of concepts and definitions, and continuous consolidation of related concepts.
Discussion
Interdisciplinary TDII research is important to enhance the use of EBPs across multiple disciplines and is a critical part of knowledge translation. The exploration and use of the SciTS collaboration framework provides a useful context to invest in understanding and addressing contextual factors that promote multidisciplinary work in TDII research. The findings fall broadly into 4 of the 6 domains of the Stokols et al.’s [11] framework: intrapersonal, interpersonal, organizational, and physical environment. Although not directly addressed, participants recommended approaches that incorporated the technological, social, and political domains. In particular, participants implicitly alluded to these domains when describing ways to enhance communication, methods, and interpersonal relationships among scientists. The topics and urgency in panel reports were consistent with the extant literature in terms of the importance of relationships, leadership, power, physical environment, and the use of technology to improve interdisciplinary collaboration.
Findings from this exploratory study should be interpreted with caution. This was a preliminary descriptive study that relied on a small nonprobability sample of experts in TDII research who volunteered to participate; hence, findings have limited generalizability. However, this is an appropriate first step to identify relevant concepts, scenarios, and related solutions to enhance transdisciplinary collaborations in TDII research and practice.
These preliminary findings have significant implications for TDII practice. Changes in policy and practice should focus on the role of leadership, power, and organizational hierarchy with the goal of fostering commitment and developing a vision to support leadership and incentives in administering joint projects in TDII research. Please refer to Table 2 for examples. Another component to consider is the significance of universities or organizations in developing credibility, building accountability and responsibility, and focusing efforts on improving communication strategies. Future work should examine domains, problems, and solutions to improve process and proximate outcomes, such as communication, coordination, collaboration, and problem solving among researchers from different backgrounds conducting TDII research.
Acknowledgments
The research described was supported in part by the National Institutes of Health and National Center for Advancing Translational Sciences through UCLA CTSI grant no. UL1TR000124, Southern California CTSI grant no. UL1TR000130, and Kaiser Permanente Southern California. Funding for E. G.’s role in this study was provided by a National Institute of Drug Abuse research grant (R33DA035634-03, principal investigator (PI): E. G.) and an implementation fellowship training grant (R25 MH080916, PI: Enola Proctor). Funders had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
The Dissemination and Implementation Science Workgroup: Brian S. Mittman; Moira Inkelas; Ibrahima C. Sankaré; Stefanie D. Vassar; and Arturo B. Martinez.
Contributor Information
Collaborators: the Dissemination and Implementation Science Workgroup
Declaration of Interest
None.
Previous Presentations
The work is based on preliminary findings, stakeholder engagement efforts, and forum discussions presented at the 2014 Southern California Regional Dissemination, Implementation and Improvement Science Symposium, sponsored in part by the National Institutes of Health and National Center for Advancing Translational Sciences through UCLA CTSI grant no. UL1TR000124, Southern California CTSI grant no. UL1TR000130, and Kaiser Permanente Southern California.
References
- 1. Aarons GA, et al. The role of organizational processes in dissemination and implementation research In: Brownson RC, Colditz GA, Proctor E, eds. Dissemination and Implementation Research in Health: Translating Science to Practice. New York: Oxford University Press, 2012, pp. 128–158. [Google Scholar]
- 2. Brownson RC, et al. Fostering more-effective public health by identifying administrative evidence-based practices: a review of the literature. American Journal of Preventive Medicine 2012; 43: 309–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brownson R, Colditz G, Proctor E. Dissemination and Implementation Research in Health: Translating Science to Practice New York: Oxford University Press, 2012. [Google Scholar]
- 4. Rabin BA, et al. A glossary for dissemination and implementation research in health. Journal of Public Health Management and Practice 2008; 14: 117–123. [DOI] [PubMed] [Google Scholar]
- 5. Woolf SH. The meaning of translational research and why it matters. JAMA 2008; 299: 211–213. [DOI] [PubMed] [Google Scholar]
- 6. Curran GM, et al. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care 2012; 50: 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McMillen C. Dissemination and implementation in social service settings In: Brownson RC, Colditz GA, Proctor E, eds. Dissemination and Implementation Research in Health: Translating Science to Practice. New York: Oxford University Press, 2012, pp. 384–399. [Google Scholar]
- 8. Proctor EK, et al. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Administration and Policy in Mental Health 2009; 36: 24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Börner K, et al. A multi-level systems perspective for the science of team science. Science Translational Medicine 2010; 2: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fiore SM. Interdisciplinarity as teamwork: how the science of teams can inform team science. Small Group Research 2008; 39: 251–277. [Google Scholar]
- 11. Stokols D, et al. The science of team science: overview of the field and introduction to the supplement. American Journal of Preventive Medicine 2008; 35: S77–S89. [DOI] [PubMed] [Google Scholar]
- 12. Emmons KM, Viswanath K, Colditz GC. The role of transdisciplinary collaboration in translating and disseminating health research: lessons learned and exemplars of success. American Journal of Preventive Medicine 2008; 35: S204–S210. [DOI] [PubMed] [Google Scholar]
- 13. Green LW, Kreuter MW. Health Program Planning: An Educational and Ecological Approach (4th edition) New York: McGraw-Hill, 2005. [Google Scholar]
- 14. Tabak RG, et al. Bridging research and practice: models for dissemination and implementation research. American Journal of Preventive Medicine 2012; 43: 337–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aarons GA, Sommerfeld DH, Walrath-Greene C. Evidence-based practice implementation: the impact of private versus public sector organizations on organizational support, provider attitudes, and adoption of evidence-based practice. Implementation Science 2009; 4: 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guerrero EG, Kim A. Organizational structure, leadership and readiness for change and the implementation of organizational cultural competence in addiction health services. Evaluation and Program Planning 2013; 40: 74–81. [DOI] [PubMed] [Google Scholar]
- 17. Collins DB, Holton EF. The effectiveness of managerial leadership development programs: a meta-analysis of studies from 1982 to 2001. Human Resource Development Quarterly 2004; 15: 217–248. [Google Scholar]
- 18. Dreachslin JL, Weech-Maldonado R, Dansky KH. Racial and ethnic diversity and organizational behavior: a focused research agenda for health services management. Social Science and Medicine 2004; 59: 961–971. [DOI] [PubMed] [Google Scholar]
- 19. Jayne MEA, Dipboye RL. Leveraging diversity to improve business performance: research findings and recommendations for organizations. Human Resource Management 2004; 43: 409–424. [Google Scholar]
- 20. Damschroder LJ, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science 2009; 4: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]