Abstract
The present study aims to explore the crisis of antibiotic resistance and discover more about the current challenges related to self-medication. The current challenges related to antibiotic resistance are unique and differ from the challenges of the past since new bacterial pathogens are involved and continue to evolve. Strains with resistance to multiple antibiotic classes have emerged which the discovery of new antibiotics has failed to match. The consequences of antibiotic resistance are grave with mortality and morbidity continually on the rise. This paper also highlights the possible interventions that can be effective at the micro or individual level in the prevention of development of antibiotic resistance.
Keywords: Antibiotics, Resistance, Drugs
1. Introduction
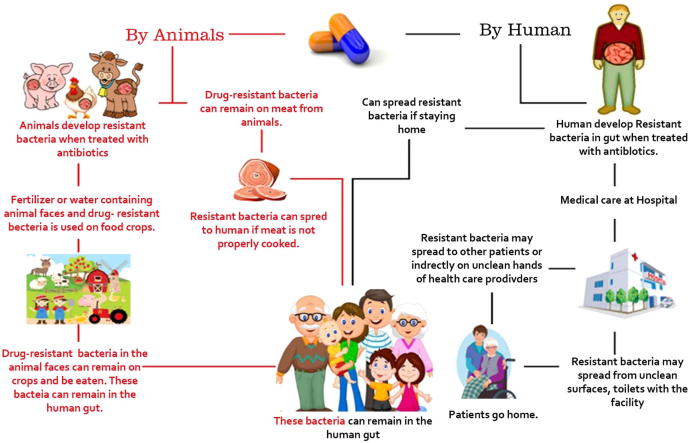
Poor infection control practices, negligent antibiotic use and the consistent dismissal of warnings against overuse of antibiotics often result in a condition where the body becomes more vulnerable to diseases and then treatment becomes difficult as the pathogens develop immunity against the antibiotic drugs that are administered more often than required (Gould and Bal, 2013, Wright, 2014, Sengupta et al., 2013). The Centers for Disease Control and Prevention (CDC) has classified a number of bacteria for developing multidrug resistance overtime against antibiotic drugs as a result of which an individual is exposed to greater risk of infection and a lack of treatment options make the recovery process difficult and dangerous (CDC, 2013). These antibiotic resistant bacteria can spread to humans or animals (Fig. 1). Some common antibiotic resistant pathogens are Meticillin-Resistant Staphylococcus aureus (MRSA), Glycopeptide-Resistant S. aureus, Toxin Hyperproducing Clostridium difficile, Extended-Spectrum β-lactamase- and carbapenemase-producing coliforms. Such antibiotic resistant pathogens are homogeneous, have increased virulence, and may spread even within the confines of a hospital or the community and prove to be a grave threat to health. There is an urgent need of discovering newer antibiotics to combat the drug-resistant pathogens and to reduce the mortality associated with drug resistance (Gould and Bal, 2013, Spellberg and Gilbert, 2014). This need can be fulfilled through collaborative research work at the international level and by spreading more awareness among the general population about self-medication and the side effects of antibiotic overuse. For instance, a dramatic decrease in the number of cases related to MRSA and C. difficile infections were recorded in England as a result of coordinated efforts at the international level (French, 2010).
Figure 1.
Development and spread of antibiotic resistant bacteria.
Bacterial resistance is so widespread and fatally dangerous that it has become a worldwide problem that presents therapeutic dilemmas to physicians from all regions. The ignorance of common people on such a vital subject and a lack of an alternative to these antibiotic treatments has turned it into a global crisis. Resistance against antibiotic drugs is an ecological phenomenon that results from the bacterial reaction that stems from the irrational overuse of antibiotic drugs (Nathan and Cars, 2014, French, 2010, Read and Woods, 2014). Self-medication is the most common reason for the development of human pathogen resistance to antibiotic drugs (Michael et al., 2014). Rampant irrational antibiotic use and ignorance of people about the complete knowledge of the course of antibiotics, their side effects, standard acceptable dosage limits, and antibiotic overdose issues are the potential reasons for inappropriate or incorrect treatment or even missed diagnosis and in most cases can lead to microbial resistance issues and increased morbidity (Michael et al., 2014). Antibiotic overdose can also cause some other health threats such as skin problems, severe allergies, hypersensitivity etc. Improved knowledge and more awareness among the non-medical population about allopathic drugs, especially an understanding of the usage of antibiotics can help in limiting the microbial resistance issues globally (Bennadi, 2014).
2. Crisis of antibiotic resistance
There have been various reports published about the potential risks of antibiotic resistance in pathogens, for some time now. However, the current situation is dangerous as the present antibiotic-resistance crisis is different from the ones that have occurred in the past. Recent studies reveal that several different microbials are involved in antibiotic resistance and the available medicines to treat these new infections are limited. It is also important to note that there have not been many new discoveries of antibiotics to combat the antibiotic resistant pathogens (Piddock, 2012, Bartlett et al., 2013). One of the reasons could be that investment in the development of new antibiotics is no longer a wise investment for the pharmaceutical industries, compared to drugs for chronic diseases (Golkar et al., 2014, Gould and Bal, 2013, Wright, 2014, Piddock, 2012, Bartlett et al., 2013). The rise in antibiotic resistant bacteria is causing greater morbidity and higher mortality rates all over the world. An example of this can be observed among the children suffering from meningitis who may incur neurologic damage as the first line of antibiotic therapy is not of much consequence. An infection that involves antibiotic resistant microbial agents can slow down the recovery process and induce greater medical expenses (Murray, 1994).
Antibiotic resistance has turned into a severe global health crisis and yet people are not completely aware of the threat it poses at the individual level as well as the community level. Each year, in a developed country such as the Unites States, thousands of people are hospitalized with problems involving antibiotic resistant microbial infections out of which an estimated 23,000 patients die because of the lack of treatment options available for such patients and the complicated and fatal symptoms that these drug resistant microbials cause, that are difficult to diagnose. In the United States, alone, the direct healthcare expenditure involving the treatment of antibiotic resistant infections is about $20 billion a year (CDC, 2013). The costs are comparatively high in the developing countries where the healthcare system is not as advanced and the economies are not as powerful. In India, it is estimated that more than 58,000 infants died in the year 2013 as a result of antibiotic resistant bacteria infections, and over 40% of the world’s antibiotics are produced in India (Laxminarayan et al., 2013). The researchers and doctors from all over the world agree upon the severity of this crisis; however, the causes and solutions to antibiotic misuse are complicated. Many developing countries have poor antibiotic dispensing laws. Moreover, the provider and patient roles and contributions are intertwined in several cases that give rise to a need to understand different motivating factors in different populations, in a better way to solve this ever growing health issue (Barker et al., 2016).
A cause that is identified internationally as the most common and obvious contributing factor of antibiotic resistant pathogens is self-medication. The taking of medicines on one's own initiative or on another person's suggestion who is not a certified medical professional is termed as Self-medication. The most common and primary reason for people to start using medicines without professional help are advertisements on television, radio and print media in addition to advice from friends and family. People seem to have the innate desire to play an informed and self-sufficient role and demonstrate their independence by managing and treating their own illnesses. Another primary reason for people to indulge in self-medication is the expensive healthcare system. Some people are not economically strong and cannot afford to pay the consultation fees of the doctors. While some others think that going to a doctor's clinic or to the hospital is too much of a hassle and must be avoided if the disease is not of a serious nature. Some governments in the developing countries are also encouraging people to try to treat minor health problems on their own to reduce the cost of treatment and to save the country's limited economic resources and manpower (Nathan and Cars, 2014).
Wastage of economic resources and serious health hazards including prolonged illnesses and adverse reactions are few of the many problems that are related to self-medication. Anti-microbial resistance is a major crisis all over the world, especially in developing countries where antibiotics are sold as over the counter (OTC) medications. To combat this global crisis it is mandatory that the national governments show interest in this issue and formulate proper healthcare policies to combat the problem and regulate responsible self-medication. The general population should also be educated about the use, advantages and disadvantages of the common antibiotic drugs that are used most often. Antibiotics and other prescription medicine packages should have proper instructions about their usage and side effects so that people can be educated about the harmful effects of their overuse (Bennadi, 2014, Berendonk et al., 2015).
A trend that has become a common practice in some countries is ‘Rx-to-OTC’ switch where prescription medicines are given OTC status after a definite period of time. This switch usually happens after accumulating information about the use of the medicine, experience of different patients, and on the basis of some other scientific information. However, this is a dangerous switch as it encourages people to use potentially harmful drugs without any professional help, and correct knowledge for long periods of time (Piddock et al., 2016).
Recently, screening of 3537 articles published from Europe, Asia, and North America, were roughly 55,225 people participated to help researchers systematically assess quantitative and qualitative public beliefs and knowledge about antibiotic resistance (McCullough et al., 2016). It was seen that about 70% of the participants had heard about antibiotic resistance in the past, 88% of the participants believed that it referred to some sort of physical changes in the body while the rest of them believed that excessive use of antibiotics and not completing antibiotic courses led to the resistance problem (McCullough et al., 2016). A shocking 84% suggested that antibiotic resistance could be reduced by limiting the use of antibiotics and seeking help from a clinician (McCullough et al., 2016). The qualitative data indicate that people considered the emerging antibiotic resistance crisis development as the consequence of other people's actions and suggested that clinicians should find a remedy to this growing crisis. The researchers concluded that the public is not fully aware of what exactly the antibiotic resistance crisis entails and have an incomplete knowledge about antibiotic use. The results of this study clearly indicate that the public needs to be updated on the antibiotic resistance crisis and the safe use of antibiotic drugs (McCullough et al., 2016).
3. Current challenges of antibiotics resistance
The infections related to antibiotic resistant pathogens generally occur in hospitals as highly vulnerable patients are clustered together and there is a high use of antibiotics in such settings along with invasive procedures. Data suggest that as many as 50,000 Americas died in the year 2006 alone, due to two common antibacterial-resistant pathogen infections, sepsis and pneumonia and it cost the U.S government around $8 billion (Ventola, 2015).
A trend of indulging in self-medication has also been noticed among the educated population of some developing countries such as India (Verma et al., 2010, Shveta and Jagmohan, 2011). In a study that was conducted to evaluate this trend, a surprising 73% of the population of Punjab (a state in India) resorted to self-medication for the treatment of minor health problems to chronic and recurrent illnesses (Joshi and Shalini, 2011, Sharma et al., 2005, Phalke et al., 2006). These reports suggest that even after the diagnosis of a chronic ailment, patients seek only occasional professional advice, and consider them competent to manage and maintain their own health. Apart from the frequent use of antibiotics, a large part of the population is estimated to be using drugs such as histamine H2-receptor blocker, topical corticosteroid, antifungal, and oral contraceptive without taking advice from clinicians. This trend demonstrates a lack of understanding, knowledge about the use of antibiotics, and other drugs to escape the inconvenience of visiting the doctor (Barker et al., 2016).
Recent studies suggest that self-medication is especially prevalent in economically deprived communities. In many developing countries the health care facilities do not meet the standard benchmark and are even quite expensive, making self-medication an easy and necessary medical choice. Another factor that contributes to the promotion of self-medication in developing countries is the availability of prescription drugs as OTC medicines and can be easily purchased from any pharmaceutical store. Moreover, lax medical regulations lead to a proliferation of counter free drugs that are available for the treatment and management of prevalent diseases (Bennadi, 2014).
The biggest challenge for the healthcare sector is to educate people about antibiotics, its side effects, and to encourage them to stop the misuse of antibiotics. The lack of knowledge about self-medication is the prime reason for mass scale antibiotic resistance tragedy. To curb it from emerging as an even bigger global crisis it is important to educate people about the emergence of antibiotic resistance in bacterial pathogens and the limited treatment options available for infections related to drug resistance. Antibiotic resistance crisis is not just a concern related to the health care industry, but the emerging crisis if not controlled can be potentially harmful to a country's economic growth as well (Woolhouse et al., 2016).
Another important challenge that the pharmaceutical industry needs to overcome is a lack of new drug development to treat bacterial infections. The efficacy of currently available antibiotic drugs is in grave danger as the resistance crisis is growing and bacterial infections are on the verge of becoming fatal again. Stringent regulatory requirements and a lack of monetary incentives for research are two major reasons why there has not been any new discovery of drugs to treat life-threatening bacterial infections (Ventola, 2015).
4. Prevention of antibiotic resistance
If resistance gene frequency is decreased at the local level and antibiotic use is regulated, it can prevent the global antibiotic crisis from growing even bigger (Littmann et al., 2015). Incomplete knowledge and misperceptions about the use of antibiotic and the subsequent consequences of its misuse must be highlighted to successfully tackle the issue (McCullough et al., 2016). Health professionals can play a vital role in prevention by educating people about the potential risks of antibiotic use as people are more likely to trust and consider their therapeutic advice and medical knowledge. When a patient is diagnosed with an infection that needs to be treated with antibiotic drugs, the medical professional should provide proper instructions on its usage such as dose, frequency of dose, treatment course and the harmful effects of its misuse. Lack of compliance to the antibiotic treatment course and improper self-medication are major reasons for the increase in drug-induced diseases and development of antibiotic resistance crisis. (Bennadi, 2014). Health professionals should also educate their patients and caregivers about the psychological factors that can assist them in enhancing the adherence to medication such as enhancing motivation, patient education, formulating health goals and increasing social support.
5. Future prospects
Research studies and popular mass media articles have raised alarm about the crisis of antibiotic resistance time and again. Researchers have expressed concern over the increase in the number of patients who are developing untreatable invasive infections due to multidrug-resistant bacteria (MDR) each year, and the increase in the mortality rate resulting from such conditions. It is therefore important to highlight that there is an imminent need to develop new antibiotics since there has been an increase in pan-drug-resistant bacteria worldwide which is a dangerous crisis leading to millions of death worldwide.
However, there is another side to this debate since the level of resistance to some classes of antibiotics of the MDR phenotype has been found to be consistently stable and relatively low over the years and some options are available for older antibiotics. The death rates that can be attributed to MDR bacteria are controversial since all cases are not reported and mortality is high due to non-MDR infections as well. Some experts assert that the currently available antibiotics are sufficient for tackling the menace of emerging bacterial resistance if the disease is managed on a non-profit basis and as per international regulations.
6. Conclusion
The fast emerging antibiotic resistance crisis threatens the extraordinary health benefits that have been achieved through antibiotic medication. The pharmaceutical companies are failing to address the challenge with the discovery of new drugs to treat microbial infections, while the antibiotics continue to be overused and misused throughout the world, turning the antibiotic resistance problem into a global health crisis. This crisis is not only a health threat and a grave challenge for the pharmaceutical and the healthcare industry, but also an economic burden for both developed and developing economies (Ventola, 2015). A major reason responsible for antibiotic resistance crisis is over dosage and self-medication. Factors such as limited health education, poverty and inadequate access to a doctor are the determinant cause for people to seek advice from a local pharmacist or to indulge in self-medication instead of taking advice from a certified medical professional (Piddock et al., 2016). The government needs to implement new policies to tackle this issue. There is a need for more collaborative research efforts to manage the crisis. The general public's involvement as an active contributor to antibiotic resistance crisis needs to be solved through proper awareness initiatives. The cries for progress in new drug development in this area should not be ignored (Ventola, 2015).
Acknowledgments
This work was supported by Korea Institute of Planning and Evaluation for Technology in Food, Agriculture, Forestry and Fisheries (IPET) through High Value-added Food Technology Development Program, funded by Ministry of Agriculture, Food and Rural Affairs (MAFRA) (115043-1).
Footnotes
Peer review under responsibility of King Saud University.
References
- Barker A., Verhoeven K., Ahsan M., Alam S., Sharma P., Sengupta S., Safdar N. Social determinants of patient antibiotic misuse in Haryana, India. J. Invest. Med. 2016;64(4) 935-935. [Google Scholar]
- Bartlett J.G., Gilbert D.N., Spellberg B. Seven ways to preserve the miracle of antibiotics. Clin. Infect. Dis. 2013;56(10):1445–1450. doi: 10.1093/cid/cit070. [DOI] [PubMed] [Google Scholar]
- Bennadi D. Self-medication: a current challenge. J Basic Clin. Pharm. 2014;5:19. doi: 10.4103/0976-0105.128253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berendonk T.U., Manaia C.M., Merlin C., Fatta-Kassinos D., Cytryn E., Walsh F., Kreuzinger N. Tackling antibiotic resistance: the environmental framework. Nat. Rev. Microbiol. 2015;13:310–317. doi: 10.1038/nrmicro3439. [DOI] [PubMed] [Google Scholar]
- CDC, 2013. Antibiotics resistance threats in the United States. U.S department of health and human services centers for disease control and prevention. Centers for Disease Control and Prevention, Office of Infectious Disease Antibiotic resistance threats in the United States, 2013. Apr, 2013. Available at: <http://www.cdc.gov/drugresistance/threat-report-2013>. Accessed January 28, 2015.
- French G.L. The continuing crisis in antibiotic resistance. Int. J. Antimicrob. Agents. 2010;36:S3–S7. doi: 10.1016/S0924-8579(10)70003-0. [DOI] [PubMed] [Google Scholar]
- Golkar Z., Bagazra O., Pace D.G. Bacteriophage therapy: a potential solution for the antibiotic resistance crisis. J. Infect Dev. Ctries. 2014;8(2):129–136. doi: 10.3855/jidc.3573. [DOI] [PubMed] [Google Scholar]
- Gould I.M., Bal A.M. New antibiotic agents in the pipeline and how they can overcome microbial resistance. Virulence. 2013;4(2):185–191. doi: 10.4161/viru.22507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi M.C., Shalini Agarwal.S. A questionnaire based study of self-medication practices among young population. Res. J. Pharm. Biol. Chem. Sci. 2011;2:761–766. [Google Scholar]
- Laxminarayan R., Duse A., Wattal C., Zaidi A.K., Wertheim H.F., Sumpradit N. Antibiotic resistance-the need for global solutions. Lancet Infect. Dis. 2013;13:1057–1098. doi: 10.1016/S1473-3099(13)70318-9. [DOI] [PubMed] [Google Scholar]
- Littmann J., Buyx A., Cars O. Antibiotic resistance: an ethical challenge. Int. J. Antimicrob. Agents. 2015;46:359–361. doi: 10.1016/j.ijantimicag.2015.06.010. [DOI] [PubMed] [Google Scholar]
- McCullough A.R., Parekh S., Rathbone J., Del Mar C.B., Hoffmann T.C. A systematic review of the public's knowledge and beliefs about antibiotic resistance. J. Antimicrob. Chemother. 2016;71(1):27–33. doi: 10.1093/jac/dkv310. [DOI] [PubMed] [Google Scholar]
- Michael C.A., Dominey-Howes D., Labbate M. The antibiotic resistance crisis: causes, consequences, and management. Front. Public Health. 2014;2:145. doi: 10.3389/fpubh.2014.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray B.E. Can antibiotic resistance be controlled? N. Engl. J. Med. 1994;330:1229–1230. doi: 10.1056/NEJM199404283301710. [DOI] [PubMed] [Google Scholar]
- Nathan C., Cars O. Antibiotic resistance—problems, progress, and prospects. N. Engl. J. Med. 2014;371:1761–1763. doi: 10.1056/NEJMp1408040. [DOI] [PubMed] [Google Scholar]
- Phalke V.D., Phalke D.B., Durgawale P.M. Self-medication practices in rural Maharashtra. Indian J. Community Med. 2006;31:34–35. [Google Scholar]
- Piddock L., Garneau-Tsodikova S., Garner C. Ask the experts: how to curb antibiotic resistance and plug the antibiotics gap? Future Med. Chem. 2016;8:1027–1032. doi: 10.4155/fmc-2014-0032. [DOI] [PubMed] [Google Scholar]
- Piddock L.J. The crisis of no new antibiotics—what is the way forward? Lancet Infect. Dis. 2012;12(3):249–253. doi: 10.1016/S1473-3099(11)70316-4. [DOI] [PubMed] [Google Scholar]
- Read A.F., Woods R.J. Antibiotic resistance management. Evol. Med. Public Health. 2014;2014(1):147. doi: 10.1093/emph/eou024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sengupta S., Chattopadhyay M.K., Grossart H.P. The multifaceted roles of antibiotics and antibiotic resistance in nature. Front. Microbiol. 2013;4:47. doi: 10.3389/fmicb.2013.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma R., Verma U., Sharma C.L., Kapoor B. Self-medication among urban population of Jammu city. Indian J. Pharmacol. 2005;37:37–45. [Google Scholar]
- Shveta S., Jagmohan S. A study of self-medication pattern in Punjab. Indian J. Pharm. Pract. 2011;4:43–48. [Google Scholar]
- Spellberg B., Gilbert D.N. The future of antibiotics and resistance: a tribute to a career of leadership by John Bartlett. Clin. Infect. Dis. 2014;59(suppl 2):S71–S75. doi: 10.1093/cid/ciu392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventola C.L. The antibiotic resistance crisis: part 1: causes and threats. Pharm. Ther. 2015;40:277. [PMC free article] [PubMed] [Google Scholar]
- Verma R.K., Mohan L., Pandey M. Evaluation of self-medication among professional students in North India: proper statutory drug control must be implemented. Asian J. Pharm. Clin. Res. 2010;3:60–64. [Google Scholar]
- Woolhouse M., Waugh C., Perry M.R., Nair H. Global disease burden due to antibiotic resistance–state of the evidence. J. Global Health. 2016;6:1. doi: 10.7189/jogh.06.010306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright G.D. Something new: revisiting natural products in antibiotic drug discovery. Can. J. Microbiol. 2014;60(3):147–154. doi: 10.1139/cjm-2014-0063. [DOI] [PubMed] [Google Scholar]