Abstract
The risk of autism spectrum disorder varies by maternal race–ethnicity, immigration status, and birth region. In this retrospective cohort study, Western Australian state registries and a study population of 134 204 mothers enabled us to examine the odds of autism spectrum disorder with intellectual disability in children born from 1994 to 2005 by the aforementioned characteristics. We adjusted for maternal age, parity, socioeconomic status, and birth year. Indigenous women were 50% less likely to have a child with autism spectrum disorder with intellectual disability than Caucasian, nonimmigrant women. Overall, immigrant women were 40% less likely to have a child with autism spectrum disorder with intellectual disability than nonimmigrant women. However, Black women from East Africa had more than 3.5 times the odds of autism spectrum disorder with intellectual disability in their children than Caucasian nonimmigrant women. Research is implicated on risk and protective factors for autism spectrum disorder with intellectual disability in the children of immigrant women.
Keywords: autism, developmental disability, epidemiology, immigrant, intellectual disability, race
Autism spectrum disorder is a lifelong neurodevelopmental disorder characterized by deficits in social communication and interaction and by restricted and repetitive behaviors, interests, or activities. These deficits originate in early childhood and impact everyday functioning.1 About 30% to 50% of persons with autism spectrum disorder have comorbid intellectual disability,2,3 defined as having an IQ of less than 70 and impairments in adaptive functioning occurring before age 18 years.1
In some countries, the prevalence of diagnosed autism spectrum disorder is lower among children of women from minority ethnic groups. For example, children of Indigenous women in Australia4 and Canada5 have a lower prevalence of diagnosed autism spectrum disorder than the children of Caucasian women. In the United States, children born to Hispanic and Black women have lower prevalence of diagnosed autism spectrum disorder than children born to Caucasian women.3 Additionally, some studies indicate the proportionate distribution of autism spectrum disorder with (vs without) intellectual disability is higher in the children of Hispanic, Asian, or Black women than the children of Caucasian women.6–8 Other studies4,9–14 have suggested that the prevalence of autism spectrum disorder, and especially autism spectrum disorder with intellectual disability,4,13 is higher among the children of immigrant than nonimmigrant women. In contrast, a United States population-based study reported that children born to immigrant Hispanic women had significantly lower rates of diagnosed autism spectrum disorder than children of nonimmigrant Hispanic or Caucasian women.15
Currently, it is not clear whether the association between maternal immigration status and the risk of having a child with autism spectrum disorder is primarily related to maternal race–ethnicity, immigrant status, or associated factors, such as the region of birth, the income status of the mother’s native country, the distance from the native country,16 maternal stress,17,18 nutrition,19 or other exposures of the mother. Although most studies have not separately examined race–ethnicity and immigration status, a few studies have shown that the prevalence of autism spectrum disorder among immigrant women can vary according to race–ethnicity and region of birth. For example, children born in Sweden16 and the United States20 to Black women from East Africa had higher rates of autism spectrum disorder with intellectual disability compared to children of native-born women. Likewise, children born in Western Australia and Malmö Sweden whose mothers were born in East Asia4 had higher autism spectrum disorder prevalence rates than children born in the same countries to nonimmigrant women.21
The estimated prevalence of autism spectrum disorder is increasing,22–24 and in Australia and other Western countries, the rate of immigration is also increasing. In Australia, the immigrant racial–ethnic composition25,26 is changing over time, and so year of birth should be considered in the analyses of prevalence differences according to race–ethnicity/immigration status.10,11,13,14 Therefore, while controlling for birth-year group and other demographic factors, we compared the prevalence of autism spectrum disorder with and without intellectual disability among children in Western Australia within subgroups defined by:
race–ethnicity,
immigrant status, and
region of birth for mothers of Asian race–ethnicity born in Asia and Black mothers born in East Africa.
Apart from providing insight into risk factors for autism spectrum disorder, differences in the prevalence of autism spectrum disorder among racial–ethnic groups might point to differences in ascertainment and thereby identify the need for enhanced screening in some population subgroups.
Data and Methods
Study Population and Data Collection
Our study population consisted of all women with a live-born child in Western Australia between 1994 and 2005 (inclusive). Our data were extracted from the Midwives Notification System,27 which provided birth dates, data to inform measures of maternal race–ethnicity, parity and socioeconomic status, and the Western Australia Birth Register27 which provided us with the maternal country of birth. Our third data source was the Intellectual Disability Exploring Answers Database28 which receives diagnostic information on children with autism spectrum disorder or intellectual disability from the state government organization, the Disability Services Commission,29 and the Western Australia Department of Education. Diagnoses of autism spectrum disorder and intellectual disability were made by clinicians or psychologists using criteria from the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) and Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision). The Intellectual Disability Exploring Answers Database provided records of children born between 1994 and 2005 (inclusive) and diagnosed with autism spectrum disorder, with and without intellectual disability, before 2011. An IQ test was performed in all cases unless the child obviously did not have intellectual disability or the child was unable to be assessed. For children within the latter group, an estimate was made on whether the child was vulnerable to intellectual disability. Linkage of the aforementioned data sets was enabled by the use of an encrypted alphanumeric code, which was created for each mother by personnel from Western Australia’s Data Linkage Branch.27
Maternal Groups
For women with at least one child identified with autism spectrum disorder, the index child was the eldest child with autism spectrum disorder born during the study period. Women in all comparison groups had no child identified with autism spectrum disorder, and the index child was the first-born child during the collection period. Case mothers were grouped into the case groups, autism spectrum disorder with intellectual disability and autism spectrum disorder without intellectual disability, according to the disability of their index child.
Explanatory Variables
Researchers have previously demonstrated that socioeconomic status, maternal age, and parity are associated with autism spectrum disorder.4 The prevalence of autism spectrum disorder30 and the pattern of immigration to Western Australia from different regions25 have varied over time. Consequently, we included a binary measure of grouped birth year of the index child with the groups of 1994 to 1999 and 2000 to 2005. We derived our measure of maternal socioeconomic status from an Index of Relative Socioeconomic Disadvantage 31 and quartile boundaries from the original data set to define “low” pertaining to the lowest quartile, “medium” to the two inner quartiles, and “high” to the top quartile. We calculated maternal age at the index birth and defined a variable with the levels of 20 to 30 years, 31 to 40 years, and >40 years. Parity at the index birth was defined by 0 previous children, 1 previous child, 2 to 3 previous children, and >3 previous children. We did not include births after 2005, as a five-year period was needed for children with autism spectrum disorder without intellectual disability to have the opportunity to be diagnosed.
Variables Defining Maternal Groups
Race–ethnicity
We classified maternal race–ethnicity as Caucasian, Asian, Black, Indian, Maori or Polynesian, and Indigenous (Figure 1). In this article, Asian describes women identified as being of Asian race–ethnicity and not women from Asia who can be of other race–ethnicities as well. The Indigenous group included all women who self-identified as an Australian Aboriginal or Torres Strait Islander.
Figure 1.
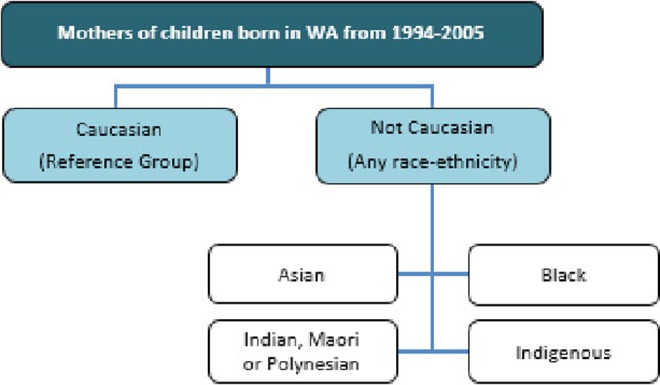
Comparison groups assessed in analyses according to race–ethnicity, independent of immigration status.
Immigration status and region of birth
A binary variable indicated maternal immigration status. Women who were born in an Australian state or mainland territory were categorized as nonimmigrant and all others as immigrant. We further divided the remainder of the world into the six regions of Central Asia, South Asia, Other Asia, East Africa, Other Africa, and Other regions. We chose these regions because we wanted to explore the odds of having a child identified with autism spectrum disorder in women of Asian race–ethnicity from Central Asia and South Asia and in Black women from East Africa, as other researchers had noted higher odds of autism spectrum disorder in children of women from these regions (Supplementary Table 1). We also grouped Asian and Black immigrant women according to their birth region (Figure 2).
Figure 2.
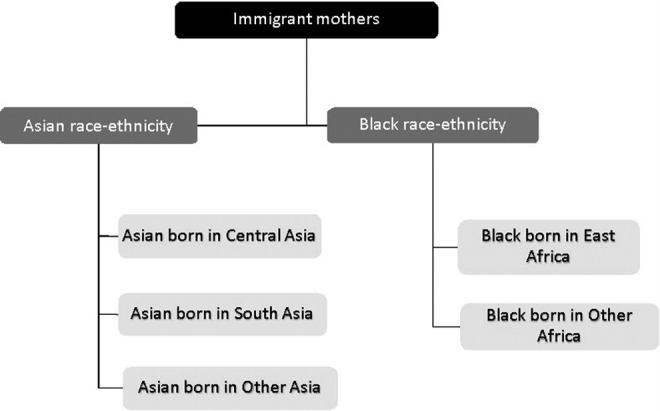
Categorization of mothers according to race–ethnicity and birthplace of interest.
Analyses
We used multinomial logistic regression where the dependent variable was the autism spectrum disorder case group. As stated earlier, both autism spectrum disorder and intellectual disability are based on a child receiving a diagnosis. The independent variables were one or more of maternal race–ethnicity, immigration status, and region of birth. We included covariates for maternal age, parity, socioeconomic status, and index birth year in the final model and report the unadjusted and adjusted odds ratios. We did not assess maternal groups with less than six observations due to the unreliability of these results.32 In case groups of size from six to nine, we calculated only the unadjusted odds ratios (or relative prevalence odds), as these groups were too small for the calculation of meaningful adjusted odds ratios.33 Since socioeconomic status is positively correlated with the prevalence of diagnosed autism spectrum disorder,4 we examined socioeconomic status in case groups where small numbers prevented us from calculating adjusted odds ratios. We tested the distribution of socioeconomic status in each of these groups compared to the comparator group using a χ2 test. In addition, we also tested proportions relating the demographic characteristics of parity and age to maternal groups using a χ2 test.
Results
Our study sample included 134 204 mothers, of whom 1028 had a child with autism spectrum disorder with intellectual disability and 347 had a child diagnosed with autism spectrum disorder without intellectual disability. Compared to mothers aged 20 to 29 years, mothers of children diagnosed with either autism spectrum disorder with intellectual disability or autism spectrum disorder without intellectual disability were less likely to be younger than 20 years (P < .00005 and P value = .0107), while mothers of children with autism spectrum disorder with intellectual disability were more likely to be 40 years or more (P < .00005) and mothers of children with autism spectrum disorder without intellectual disability were not (P = .0914). Further, mothers of children diagnosed with either autism spectrum disorder with intellectual disability or autism spectrum disorder without intellectual disability were more likely to have had a previous child (P < .00005 and P < .00005; Table 1). The distribution of socioeconomic status was similar within all maternal groups. The majority (90.2%) of children with autism spectrum disorder without intellectual disability were born from 1994 to 1999 (Table 1) and compared to the number born in 2000 to 2005, the difference is highly significant (P < .00005). This is likely due to the fact that, on average, higher functioning children with autism spectrum disorder without intellectual disability are diagnosed more than four years later than children with autism spectrum disorder with intellectual disability.34 At the end of the diagnostic period in 2010, the children in the second-year group were from five to ten years old, which means that many were less than 7.2 years, the average age of children receiving a diagnosis of Asperger syndrome, a form of autism spectrum disorder without intellectual disability.34
Table 1.
Demographic Characteristics of the Study Population According to ASD Status.
| No ASD (Comparator) | ASD With ID | ASD Without ID | Total | |
|---|---|---|---|---|
| Maternal age at the index birth | ||||
| Less than 20 years | 11 226 (8.5%) | 38 (3.7%) | 12 (3.5%) | 11 276 (8.4%) |
| 20-29 years | 67 079 (50.5%) | 426 (41.4%) | 154 (44.4%) | 67 659 (50.4%) |
| 30-39 years | 51 394 (38.7%) | 530 (51.6%) | 169 (48.7%) | 52 093 (38.8%) |
| 40 years or more | 3130 (2.4%) | 34 (3.3%) | 12 (3.5%) | 3176 (2.4%) |
| Parity at the index birth | ||||
| 0 previous child | 113 794 (85.7%) | 480 (46.7%) | 183 (52.7%) | 114 457 (85.3%) |
| 1 previous child | 11 696 (8.8%) | 345 (33.6%) | 105 (30.3%) | 12 146 (9.1%) |
| 2-3 previous children | 6448 (4.9%) | 175 (17.0%) | 52 (15.0%) | 6675 (5.0%) |
| >3 previous children | 891 (0.7%) | 28 (2.7%) | 7 (2.0%) | 926 (0.7%) |
| Maternal SES at the index birtha | ||||
| Low | 27 746 (20.9%) | 255 (22.8%) | 72 (20.8%) | 28 073 (20.9%) |
| Medium | 67 112 (50.5%) | 519 (50.5%) | 178 (51.3%) | 67 809 (50.5%) |
| High | 34 974 (26.3%) | 232 (22.6%) | 88 (25.4%) | 35 294 (26.3%) |
| Missing | 2997 (2.3%) | 22 (2.1%) | 9 (2.6%) | 3028 (2.3%) |
| Index birth-year group | ||||
| 1994-1999 | 65 460 (49.3%) | 452 (44.0%) | 313 (90.2%) | 66 225 (49.4%) |
| 2000-2005 | 67 369 (50.7%) | 576 (56.0%) | 34 (9.8%) | 67 979 (50.6%) |
| Total | 132 829 | 1028 | 347 | 134 204 |
Abbreviations: ASD, autism spectrum disorder; ID, intellectual disability; SES, socioeconomic status.
aWe derived our measure of maternal SES from an Index of Relative Socioeconomic Disadvantage (Australian Bureau of Statistics31) and quartile boundaries from the original data set to define “low” pertaining to the lowest quartile, “medium” to the 2 inner quartiles, and “high” to the top quartile.
The number of children diagnosed with autism spectrum disorder with intellectual disability or autism spectrum disorder without intellectual disability from Indian, Maori, or Polynesian mothers was too small for meaningful analysis (N < 6). Hence, these mothers will not be further referenced. Similarly, the numbers of children diagnosed with autism spectrum disorder without intellectual disability in mothers of Asian, Black, and Indigenous race–ethnicities were too small for analysis (N < 6), and these subgroups will not be further referenced (Table 2).
Table 2.
ASD by Race–Ethnicity and Immigration Status.
| Characteristic | No ASD (Comparator) | ASD With ID | ASD Without ID | Total | |
|---|---|---|---|---|---|
| Race–ethnicity | |||||
| Caucasian | 118 524 (89.2%) | 937 (91.2%) | 340 (98.0%) | 119 801 (89.3%) | |
| Asian | 6517 (4.9%) | 56 (5.5%) | 5 (1.4%) | 6578 (4.9%) | |
| Black | 594 (0.5%) | 7 (0.7%) | 0 (0.0%) | 601 (0.5%) | |
| Indian, Maori, or Polynesian | 1826 (1.4%) | 5 (0.5%) | 0 (0.0%) | 1831 (1.4%) | |
| Indigenous | 5368 (4.0%) | 23 (2.2%) | 2 (0.6%) | 5393 (4.0%) | |
| Immigration status | |||||
| Nonimmigrant | 96 717 (72.8%) | 752 (73.2%) | 262 (75.5%) | 97 731 (72.8%) | |
| Immigrant | 36 112 (27.2%) | 276 (26.9%) | 85 (24.5%) | 36 473 (27.2%) | |
| Race–ethnicity and immigration status | |||||
| Caucasian | Nonimmigrant | 90 959 (76.7%) | 725 (77.4%) | 260 (76.5%) | 91 944 (76.7%) |
| Immigrant | 27 565 (23.3%) | 212 (22.6%) | 80 (23.5%) | 27 857 (23.3%) | |
| Asian | Nonimmigrant | 287 (4.4%) | 2 (3.6%) | 0 (0.0%) | 289 (4.4%) |
| Immigrant | 6230 (95.6%) | 54 (96.4%) | 5 (100%) | 6289 (95.6%) | |
| Black | Nonimmigrant | 18 (3.0%) | 0 (0.0%) | 0 (NA) | 18 (3.0%) |
| Immigrant | 576 (97.0%) | 7 (100%) | 0 (NA) | 583 (97%) | |
| Indian, Maori, or Polynesian | Nonimmigrant | 165 (9.0%) | 2 (40%) | 0 (NA) | 167 (9.1%) |
| Immigrant | 1661 (91.0%) | 3 (60%) | 0 (NA) | 1664 (90.9%) | |
| Indigenous | Nonimmigrant | 5260 (97.9%) | 23 (100%) | 2 (100%) | 5285 (98.0%) |
| Immigrant | 108 (2.0%) | 0 (0.0%) | 0 (0.0%) | 108 (2.0%) | |
| Total | 132 829 (100%) | 1028 (100%) | 347 (100%) | 134 204 (100%) | |
Abbreviations: ASD, autism spectrum disorder; ID, intellectual disability; NA, percentage not able to be calculated.
Race–Ethnicity
The odds of having a child identified with autism spectrum disorder with intellectual disability were similar among women of Asian race–ethnicity and Caucasian women, unadjusted odds ratio 1.09 (95% confidence interval: 0.8-1.4); adjustment for demographic factors reduced the odds ratio slightly, 0.77 (95% confidence interval: 0.6-1.02). Black women were about 50% more likely to have a child diagnosed with autism spectrum disorder with intellectual disability than Caucasian women, although the difference was not statistically significant, odds ratio = 1.48 (0.7-3.1). For Indigenous women, the odds of having a child diagnosed with autism spectrum disorder with intellectual disability were about half the odds for Caucasian women both before, odds ratio = 0.54 (95% confidence interval: 0.4-0.8), and after adjustment, adjusted odds ratio = 0.52 (95% confidence interval: 0.3-0.8; Table 3).
Table 3.
The Odds of Having a Child With ASD With ID in Women by Race–Ethnicity.
| Race–Ethnicity | ASD With ID | |
|---|---|---|
| Unadjusted OR (95% CI) | Adjusted ORa (95% CI) | |
| Caucasian | 1 | 1 |
| Asian | 1.09 (0.8-1.4) | 0.77 (0.6-1.02) |
| Black | 1.48 (0.7-3.1) | b |
| Indigenous | 0.54 (0.4-0.8)c | 0.52 (0.3-0.8)c |
Abbreviations: ASD, autism spectrum disorder; CI, confidence interval; ID, intellectual disability; OR, odds ratio.
aCovariates were maternal age, parity, socioeconomic status, and birth-year group.
bNumbers were too small (N < 10) to produce reliable adjusted ORs.
c P < .005.
Immigrant Status
After adjustment for demographic factors and compared to nonimmigrant women, immigrant women were less likely to have a child diagnosed with either autism spectrum disorder with intellectual disability or autism spectrum disorder without intellectual disability, adjusted odds ratios 0.64 (95% confidence interval: 0.6-0.7) and 0.62 (95% confidence interval: 0.5-0.8), respectively.
Groups of Special Interest
Overall, the children of immigrant women from other Asia had a lower prevalence of diagnosed autism spectrum disorder with intellectual disability (P = .46), and the children of immigrant women from East Africa had a higher prevalence of diagnosed autism spectrum disorder with intellectual disability than the referent group (children of Caucasian, nonimmigrant women; Table 4), although neither differences were significant. Prior to adjustment and compared to Caucasian nonimmigrant women, women of Asian race–ethnicity from Central Asia and from South Asia each had about a 30% increased odds of having a child diagnosed with autism spectrum disorder with intellectual disability, odds ratios 1.28 (95% confidence interval: 0.8-2.0) and 1.37 (95% confidence interval: 0.9-2.0), respectively (Table 5). After adjustment for demographic factors, these odds ratios were reduced, adjusted odds ratios 0.83 (95% confidence interval: 0.5-1.3) and 0.83 (95% confidence interval: 0.6-1.2), respectively. Women of Asian race–ethnicity from other parts of Asia had less than half the odds of having a child identified with autism spectrum disorder with intellectual disability, odds ratio 0.44 (95% confidence interval: 0.2-0.98), P < .05; due to small case numbers (N < 10), we did not perform adjusted analyses for this group. Black women from East Africa had more than three-fold higher odds of having a child identified with autism spectrum disorder with intellectual disability, odds ratio 3.57 (1.7-7.6), P < .005; small case numbers also precluded adjusted analyses for this group. Indigenous women had about half the odds of having a child with autism spectrum disorder with intellectual disability, adjusted odds ratio 0.51 (0.3-0.8), P < .005.
Table 4.
Numbers of Select Immigrant Groups.a
| Racial–Ethnic Groups of Interest | Comparator Group | Total | ||
|---|---|---|---|---|
| No ASD | ASD With ID | ASD Without ID | ||
| Caucasian nonimmigrant women | 27 565 (99.0%) | 212 (0.8%) | 80 (0.3%) | 27 857 (100%) |
| Asian from Central Asia | 1763 (98.9%) | 18 (1.0%) | 1 (0.1%) | 1782 (100%) |
| Asian from South Asia | 2746 (98.9%) | 30 (1.1%) | 1 (0%) | 2777 (100%) |
| Asian from other Asia | 1721 (99.5%) | 6 (0.4%) | 3 (0.2%) | 1730 100% |
| Black from East Africa | 246 (97.2%) | 7 (2.8%) | 0 (0.0%) | 253 (100%) |
| Black from other Africa | 330 (100%) | 0 (0.0%) | 0 (0.0%) | 330 (100%) |
Abbreviations: ASD, autism spectrum disorder; ID, intellectual disability.
aShaded cells contain numbers that are too small for analysis.
Table 5.
Odds Ratios for Having a Child With ASD With ID in Select Immigrant Groups.
| Racial–Ethnic Group | ASD With ID | |
|---|---|---|
| Unadjusted OR (95% CI) | Adjusted ORa (95% CI) | |
| Caucasian nonimmigrant women | 1 | 1 |
| Asian from Central Asia | 1.28 (0.8-2.0) | 0.83 (0.5-1.3) |
| Asian from South Asia | 1.37 (0.9-2.0) | 0.83 (0.6-1.2) |
| Asian from Other Asia | 0.44 (0.2-0.98)b | c |
| Black from East Africa | 3.57 (1.7-7.6)d | c |
| Indigenous women | 0.54 (0.4-0.8)d | 0.51 (0.3-0.8)d |
Abbreviations: ASD, autism spectrum disorder; CI, confidence interval; ID, intellectual disability; OR, odds ratio.
aCovariates were maternal age, parity, socioeconomic status, and birth year group.
b P < .05.
cNumbers were too small (N < 10) to produce reliable adjusted ORs.
d P < .005.
Although small case numbers prevented us from performing adjusted analyses, we compared the socioeconomic status of immigrant women from both Other Asia and East Africa to nonimmigrant Caucasian women. Differences were significant between groups (P < .0005). Women of Asian race–ethnicity from Other Asia had a higher proportion of high socioeconomic status than nonimmigrant Caucasian women (P = .0012), and Black women from East Africa had a higher proportion of low socioeconomic status than nonimmigrant Caucasian women (P = .0022; Table 6).
Table 6.
SES Distribution by Maternal Region of Birth and Race–Ethnicity.
| SES at Time of Index Birtha | Asian From Other Asia | Black From East Africa | Nonimmigrant Caucasian |
|---|---|---|---|
| Low | 276 (16.0%) | 85 (33.6%) | 18 560 (20.2%) |
| Medium | 894 (51.7%) | 138 (54.6%) | 47 791 (52.0%) |
| High | 547 (31.6%) | 28 (11.1%) | 23 417 (25.5%) |
| Missing | 13 (0.8%) | 2 (0.8%) | 2176 (2.4%) |
| Total | 1730 (100%) | 253 (100%) | 91 944 (100%) |
Abbreviation: SES, socioeconomic status.
aWe derived our measure of maternal SES from an Index of Relative Socioeconomic Disadvantage (Australian Bureau of Statistics31) and quartile boundaries from the original data-set to define “low” pertaining to the lowest quartile, “medium” to the 2 inner quartiles, and “high” to the top quartile.
Discussion
We found that children born to Indigenous mothers were about half as likely to receive a diagnosis of autism spectrum disorder with or without intellectual disability as children born to Caucasian mothers. Children born to immigrant mothers overall were about 40% less likely to receive a diagnosis of autism spectrum disorder with or without intellectual disability. However, there were notable differences among children of immigrant mothers. Children born to Asian women from other Asia were less than half as likely to receive a diagnosis of autism spectrum disorder with intellectual disability, and children born to Black women from East Africa were more than 3.5 times as likely to have a child diagnosed with autism spectrum disorder with intellectual disability.
Others have shown that older mothers are more likely to have a child with autism spectrum disorder and less likely to be of young age. For example, Leonard et al4 showed that compared to mothers aged 25 to 29 years, mothers younger than 20 years were less likely to have a child with autism spectrum disorder with intellectual disability, and mothers older than 39 years were more likely to have a child with autism spectrum disorder with intellectual disability. We found similar associations of a decreased likelihood of autism spectrum disorder with intellectual disability in mothers younger than 20 years and an increased likelihood in mothers more than 39 years. However, Leonard et al4 found no significant association with age in mothers of children with autism spectrum disorder without intellectual disability. In contrast, we found that compared to mothers of 20 to 29 years, mothers of children with autism spectrum disorder without intellectual disability were less likely to be less than 20 years (P value = .107) but not more likely to be 40 years or more (P value = .0914). We suggest that our failure to find an association with mothers aged 40 years or older is due to the smaller number of mothers in this group and that due to the later age of diagnosis of autism spectrum disorder without intellectual disability, some of their children were not diagnosed before the deadline of January 1, 2011. The lower likelihood of autism spectrum disorder in the children of younger mothers might be due to underascertainment in this group. Due to our definition of the index child as the eldest child in comparator mothers and the eldest child with a disability in case mothers, we needed to adjust for parity in models but could not assess true parity differences for these children.
Indigenous women had about half the odds of a child diagnosed with autism spectrum disorder with intellectual disability. This is similar to the odds ratios described by others.4,5 As in the United States,35–37 this might be due to poorer access to health care and consequent underascertainment of autism spectrum disorder. In Western Australia, many Indigenous people live in remote areas,38 where diagnosis is difficult to obtain. Moreover, there can be less motivation to seek a diagnosis since few services are available.
Children born to Black immigrant mothers have a higher prevalence of diagnosed autism spectrum disorder with intellectual disability than the referent group, nonimmigrant Caucasian mothers. These findings are in line with those of researchers in Sweden and the United States.16,20 We further subdivided this group of immigrants and found that all cases of autism spectrum disorder identified in Black immigrant mothers were from mothers born in East Africa, with four born in Ethiopia and one each from Eritrea, Kenya, and Somalia, which are adjacent counties found within a localized region of East Africa and termed the Horn of Africa. Furthermore, all autism spectrum disorder diagnoses in the children of Black mothers were of autism spectrum disorder with intellectual disability, and these women were the only Black women from Africa to have a child with autism spectrum disorder. Additionally, in contrast to the Asian women who migrated from other Asia, the socioeconomic status of Black women who migrated from East Africa was lower than Caucasian nonimmigrant women. Thus, while the healthy immigrant effect might have explained the low diagnosed autism spectrum disorder prevalence in children born to Asian women who had migrated from Other Asia, it is unlikely that it was a driving force among this select group of women who migrated from East Africa.
To date, all studies exploring autism spectrum disorder in children of Black women from Africa have had the limitation of small numbers.16,20 We were faced with similar difficulties. For example, due to small numbers, we were unable to perform adjusted regression analyses for either of the two immigrant groups with autism spectrum disorder prevalence rates that differed significantly from the referent group.
The lack of data has resulted in an inability of researchers to conduct studies to assess proposed mechanisms that might explain the higher prevalence of autism spectrum disorder with intellectual disability in Black immigrant mothers from East Africa. We raise three hypotheses and suggest that each, to some degree, can be affecting the prevalence of autism spectrum disorder. First, there can be an ascertainment effect with Black mothers more likely to get early diagnoses for their children. This could occur if in close-knit communities, diagnoses in a few families might influence other families to have a child with apparent development delays assessed in order to get needed services. Second, the severity of symptoms might be affecting the likelihood of diagnosis. In other words, almost all of the autism spectrum disorder in the children of Black mothers could be due to intellectual disability being the driving force of the children getting comprehensive developmental assessments. Finally, cultural factors might affect the accuracy of specific diagnostic tests for autism spectrum disorder, since cultural norms and expectations influence eye contact, language, and socialization in young children.34
In Black women from East Africa, it is difficult to identify unique environmental risk factors that would not be operating in many other African populations, although some have been proposed, such as nutritional factors and vitamin D deficiency. The latter hypothesis is supported by the fact that both male and female immigrants from Horn of Africa to Australia were deficient in vitamin D.39 Prenatal stress has been associated with autism spectrum disorder.40 Hence, another hypothesis is that the stress associated with lifestyle changes, which might be exacerbated in Black immigrant women from East Africa where many have had negative extremes, such as war, famine, and consequent refugee status,41 has resulted in increased rates of autism spectrum disorder. Furthermore, in Australia, women from East Africa are reported to be the victims of increased domestic violence.41,42 Stress is associated with the increased risk of a child with autism spectrum disorder.43,44 A plausible mechanism is alteration in a woman’s cortisol profile due to stress and that changes the fetal environment.45
Strength and Limitations
Our study was enabled by the availability of population-based data on children with autism spectrum disorder or intellectual disability. Important variables, such as race–ethnicity and birth dates, were collected by midwives in conjunction with the mothers, and immigration status was provided by the Birth Registry. This reduced bias and enhanced the accuracy of our results. Another strength is our separation of Asian race–ethnicity from the trait of being born in Asia.
Nonetheless, one study limitation is the likelihood of some incorrect categorizations of ethnicity. Moreover, the numbers of mothers of some ethnicities were small. This, combined with the small number of children with autism spectrum disorder, limited the groups available for analysis. The number of children with a diagnosis of autism spectrum disorder without intellectual disability was especially small; it is very likely that this group is incomplete, since younger children might not yet have been assessed for either autism spectrum disorder or intellectual disability and those children with milder symptoms of autism spectrum disorder without intellectual disability might not be recognized as such before they have entered school. This greatly limited our ability to assess autism spectrum disorder without intellectual disability. Overall, only 25% of children identified as having autism spectrum disorder were classified as autism spectrum disorder without intellectual disability, and the proportion among non-Caucasian groups was markedly lower.
Conclusion
Our comprehensive assessment of the Western Australia population revealed three groups of children whose prevalence of diagnosed autism spectrum disorder , particularly autism spectrum disorder with intellectual disability, diverged from the referent group—Caucasian children with nonimmigrant Caucasian mothers. Children born to Indigenous women had significantly lower prevalence of diagnosed autism spectrum disorder than the referent group, possibly associated with low socioeconomic status and poor access to diagnostic services. Children of women of Asian race–ethnicity who migrated from parts of other Asia also had significantly lower prevalence of diagnosed autism spectrum disorder; however, the underlying reason is likely different from that for children born to Indigenous women. These Asian immigrant women were of higher than average socioeconomic status, suggesting the possibility of a healthy immigrant effect. Finally, the high prevalence of diagnosed autism spectrum disorder in children born to Black women from East Africa is in line with a few other small studies. However, neither our study nor previous studies could explore the possible underlying reasons. We hypothesize that at least some of this difference could be the result of various factors leading to higher ascertainment of autism spectrum disorder in this group of children; however, we cannot rule out the possibility of some biological risk factor, such as nutrition or stress. Further study is needed to disentangle possible ascertainment versus biologic reasons for the disparities we observed. Such study will present challenges, given the need to aggregate data across many years and possibly combine data from multiple locations in order to have sufficient numbers to study children within immigrant subgroups. Nonetheless, in light of the improved outcomes of early intervention,46 improved methods of ascertainment and access to services, particularly for Indigenous children, are indicated.
Supplementary Material
Acknowledgments
The authors are grateful to Jenny Bourke for her assistance in the early stages of this project and thank the Disability Services Commission, the Telethon Kids Institute, the Western Australia Department of Education, the Catholic Education Office, and the Association of Independent Schools of Western Australia for assistance with data collection for the Intellectual Disability Exploring Answers Database.
Footnotes
Author Contributions: JF wrote the initial manuscript and performed the initial statistical calculations. All coauthors read and had the opportunity to contribute to subsequent drafts and NdK advised on subsequent statistical calculations. JF, HML, and NdK had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Authors’ Note: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease and Control and Prevention.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr Fairthorne was funded by an Australian Post-graduate Award and a University of Western Australia PhD Completion Scholarship.
Ethics Approval: Ethical approval for this study was granted by the Western Australian Department of Health Human Research Ethics Committee (#2011/64). Approval to analyze the data by Indigenous status was granted by the Western Australian Aboriginal Health Ethics Committee (#613).
Supplemental Material: The online supplements are available at http://journals.sagepub.com/doi/suppl/10.1177/2329048X16688125.
References
- 1. American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders: DSM 5. Arlington, VA: Bookpoint US; 2013. [Google Scholar]
- 2. Braun KVN, Christensen D, Doernberg N, et al. Trends in the prevalence of autism spectrum disorder, cerebral palsy, hearing loss, intellectual disability, and vision impairment, metropolitan Atlanta, 1991–2010. PLoS One. 2015;10(4):e0124120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2012. Morb Mortal Wkly Rep. 2016;65(3):1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leonard H, Glasson E, Nassar N, et al. Autism and intellectual disability are differentially related to sociodemographic background at birth. PloS One. 2011;6(3): e17875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burstyn I, Sithole F, Zwaigenbaum L. Autism spectrum disorders, maternal characteristics and obstetric complications among singletons born in Alberta, Canada. Chronic Dis Can. 2010;30(4):125–134. [PubMed] [Google Scholar]
- 6. Croen L, Grether J, Selvin S. Descriptive epidemiology of autism in a California population: who is at risk? J Autism Dev Disord. 2002;32(3):217–224. [DOI] [PubMed] [Google Scholar]
- 7. Dealberto MJ. Prevalence of autism according to maternal immigrant status and ethnic origin. Acta Psychiatr Scand. 2011;123(5):339–348. [DOI] [PubMed] [Google Scholar]
- 8. Jelliffe-Pawlowski L, Shaw G, Nelson V, Harris J. Risks for severe mental retardation occurring in isolation and with other developmental disabilities. Am J Med Genet. 2005;136(2):152–157. [DOI] [PubMed] [Google Scholar]
- 9. Hultman C, Sandin S, Levine S, Lichtenstein P, Reichenberg A. Advancing paternal age and risk of autism: new evidence from a population-based study and a meta-analysis of epidemiological studies. Mol Psychiatry. 2011;16(12):1203–1212. [DOI] [PubMed] [Google Scholar]
- 10. Hultman C, Sparen P, Cnattingius S. Perinatal risk factors for infantile autism. Epidemiology. 2002;13(4):417–423. [DOI] [PubMed] [Google Scholar]
- 11. Keen D, Reid F, Arnone D. Autism, ethnicity and maternal immigration. Br J Psychiatry. 2010;196(4):274–281. [DOI] [PubMed] [Google Scholar]
- 12. Lauritsen M, Pedersen C, Mortensen P. Effects of familial risk factors and place of birth on the risk of autism: a nationwide register-based study. J Child Psychol Psychiatry. 2005;46(9):963–971. [DOI] [PubMed] [Google Scholar]
- 13. Magnusson C, Rai D, Goodman A, et al. Migration and autism spectrum disorder: population-based study. Br J Psychiatry. 2012;201:109–115. [DOI] [PubMed] [Google Scholar]
- 14. Williams K, Helmer M, Duncan G, Peat J, Mellis C. Perinatal and maternal risk factors for autism spectrum disorders in New South Wales, Australia. Child Care Health Dev. 2008;34(2):249–256. [DOI] [PubMed] [Google Scholar]
- 15. Schieve L, Boulet S, Blumberg S, et al. Association between parental nativity and autism spectrum disorder among US-born non-Hispanic white and Hispanic children, 2007 National Survey of Children’s Health. Disabil Health J. 2012;5(1):18–25. [DOI] [PubMed] [Google Scholar]
- 16. Gillberg C, Schaumann H, Gillberg I. Autism in immigrants: children born in Sweden to mothers born in Uganda. J Intellect Disabil Res. 1995;39(2):141–144. [DOI] [PubMed] [Google Scholar]
- 17. Rai D, Golding J, Magnusson C, Steer C, Lewis G, Dalman C. Prenatal and early life exposure to stressful life events and risk of autism spectrum disorders: population-based studies in Sweden and England. PloS One. 2012;7(6): e38893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ronald A, Pennell C, Whitehouse A. Prenatal maternal stress associated with ADHD and autistic traits in early childhood. Front Psychol. 2011;1(223):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schmidt R, Tancredi D, Ozonoff S, et al. Maternal periconceptional folic acid intake and risk of autism spectrum disorders and developmental delay in the CHARGE (CHildhood Autism Risks from Genetics and Environment) case-control study. Am J Clin Nutr. 2012;96(1):80–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hewitt A, Gulaid A, Hamre K, et al. Minneapolis Somali Autism Spectrum Disorder Prevalence Project, Community Report 2013. Minneapolis, MN: University of Minnesota; Published 2013. [Google Scholar]
- 21. Haglund N, Källén K. Risk factors for autism and Asperger syndrome. Autism. 2011;15(2):163–183. [DOI] [PubMed] [Google Scholar]
- 22. King M, Bearman P. Diagnostic change and the increased prevalence of autism. Int J Epidemiol. 2009;38(5):1224–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Matson J, Kozlowski A. The increasing prevalence of autism spectrum disorders. Res Autism Spectr Disord. 2011;5(1):418–425. [Google Scholar]
- 24. Waterhouse L. Autism overflows: increasing prevalence and proliferating theories. Neuropsychol Rev. 2008;18(4):273–286. [DOI] [PubMed] [Google Scholar]
- 25. Australian Bureau of Statistics. Australia’s population by country of birth. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/3412.0Chapter12011-12%20and%202012-13. Updated 2013. Accessed September 1, 2015.
- 26. Office of Immigration Statistics. Yearbook of Immigration Statistics: 2012. Washington, DC: United States Department of Homeland Security; 2013. [Google Scholar]
- 27. Department of Health of Western Australia. What we collect and manage. 2011. http://www.health.wa.gov.au/healthdata/statewide/index.cfm. Published 2011. Accessed September 13, 2015.
- 28. Petterson B, Leonard H, Bourke J, et al. IDEA (Intellectual Disability Exploring Answers): a population-based database for intellectual disability in Western Australia. Ann Hum Biol. 2005;32(2):237–243. [DOI] [PubMed] [Google Scholar]
- 29. Government of Western Australia. Disability Services Commission. 2014. http://www.disability.wa.gov.au/. Published 2014. Accessed September 13, 2015.
- 30. Bourke J, de Klerk N, Smith T, Leonard H. Population-based prevalence of intellectual disability and autism spectrum disorders in Western Australia: a comparison with previous estimates. Medicine (Baltimore). 2016;95(21):e3737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Australian Bureau of Statistics. Information paper: an introduction to socio-economic indexes for areas (SEIFA). 2009. http://www.abs.gov.au/ausstats/abs@.nsf/mf/2039.0. Published 2009. Accessed September 13, 2015.
- 32. Woodward M. Epidemiology: Study Design and Analysis. 2nd ed Boca Raton, US: Chapman and Hall; 2005. [Google Scholar]
- 33. Schwab JA. Multinomial Logistic Regression: Basic Relationships and Complete Problems. Austin, Texas: University of Texas; 2002. [Google Scholar]
- 34. Mandell D, Novak M, Zubritsky C. Factors associated with age of diagnosis among children with autism spectrum disorders. Pediatrics. 2005;116(6):1480–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Liptak G, Benzoni L, Mruzek D, et al. Disparities in diagnosis and access to health services for children with autism: data from the National Survey of Children’s Health. J Dev Behav Pediatr. 2008;29(3):152–160. [DOI] [PubMed] [Google Scholar]
- 36. Pinborough-Zimmerman J, Bilder D, Bakian A, et al. Sociodemographic risk factors associated with autism spectrum disorders and intellectual disability. Autism Res. 2011;4(6):438–448. [DOI] [PubMed] [Google Scholar]
- 37. Windham G, Anderson M, Croen L, Smith K, Collins J, Grether J. Birth prevalence of autism spectrum disorders in the San Francisco Bay area by demographic and ascertainment source characteristics. J Autism Dev Disord. 2011;41(10):1362–1372. [DOI] [PubMed] [Google Scholar]
- 38. Baxter J, Gray M, Hayes A. Families in regional, rural and remote Australia. Aust Bureau Stat. 2010;3. [Google Scholar]
- 39. Skull S, Ngeow J, Biggs B, Street A, Ebeling P. Vitamin D deficiency is common and unrecognized among recently arrived adult immigrants from the Horn of Africa. Intern Med J. 2003;33(1-2):47–51. [DOI] [PubMed] [Google Scholar]
- 40. Walder DJ, Laplante DP, Sousa-Pires A, Veru F, Brunet A, King S. Prenatal maternal stress predicts autism traits in 6½ year-old children: Project Ice Storm. Psychiatry Res. 2014;219(2):353–360. [DOI] [PubMed] [Google Scholar]
- 41. Fisher CM. Changed and changing gender and family roles and domestic violence in African refugee background communities post-settlement in Perth, Australia. Violence Against Women. 2013;19(7):833–847. [DOI] [PubMed] [Google Scholar]
- 42. McMichael C, Manderson L. Somali women and well-being: Social networks and social capital among immigrant women in Australia. Hum Organ. 2004;63(1):88–99. [Google Scholar]
- 43. Kinney D, Munir K, Crowley D, Miller A. Prenatal stress and risk for autism. Neurosci Biobehav Rev. 2008;32(8):1519–1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Roberts A, Koenen K, Lyall K, Ascherio A, Weisskopf M. Women’s posttraumatic stress symptoms and autism spectrum disorder in their children. Res Autism Spectr Disord. 2014;8(6):608–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Scheinost D, Sinha R, Cross SN, et al. Does prenatal stress alter the developing connectome? [Published online November 2, 2016] Pediatric Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Makrygianni MK, Reed P. A meta-analytic review of the effectiveness of behavioural early intervention programs for children with autistic spectrum disorders. Res Autism Spectr Disord. 2010;4:577–593. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


