Abstract
Background
Guidelines suggest referral for scoliosis when rib slope (scoliometer measurement, angle of trunk rotation [ATR]) is ≥7 degrees. We hypothesized that overweight and obese patients would have lower scoliometer measurements compared with normal-weight and underweight patients for a given spinal curvature, causing overweight and obese patients with adolescent idiopathic scoliosis to present for treatment later and with larger curves. Our goal was to determine the association between scoliometer readings and major curve magnitudes in relation to body mass index (BMI).
Methods
This retrospective cohort study at a tertiary referral center included 483 patients (420 girls) aged 10 to 18 years (mean age, 14±1.6 years) with thoracic adolescent idiopathic scoliosis who presented to 1 orthopaedic surgeon for initial evaluation of spinal deformity from 2010 to 2015. Records were reviewed for BMI percentile for age and sex (underweight, ≤4th percentile; normal weight, 5th to 84th percentile; overweight, 85th to 94th percentile; obese, ≥95th percentile), patient characteristics, thoracic scoliometer measurements, and thoracic major curves.
Results
Of the 483 patients, 23 were underweight, 372 were normal weight, 52 were overweight, and 36 were obese. Obese patients had a larger mean major curve (44 degrees) than normal-weight patients (34 degrees) (P = 0.004). The odds of presenting with a major curve ≥20 degrees were 4.9 (95% confidence interval, 1.1-22, P = 0.037) times higher for obese vs normal-weight patients. Receiver operating characteristic analysis of major curves (≥20 vs <20 degrees) estimated the scoliometer values with the greatest sensitivity and specificity to be 8 degrees for underweight patients, 7 degrees for normal-weight patients, 6 degrees for overweight patients, and 5 degrees for obese patients.
Conclusions
Obese patients presented with larger thoracic curves vs normal-weight patients. Differences in chest-wall thickness in patients with different BMI values may alter scoliometer measurements for a given rotational deformity. Our data suggest new referral criteria for the scoliometer test based on BMI values. Specifically, obese patients should be referred at an ATR of 5 degrees.
Keywords: adolescent idiopathic scoliosis, obesity, rib slope, scoliometer
Introduction
Scoliosis is defined as a spinal curvature with a coronal plane deformity of ≥10 degrees.1 The major classes are congenital, idiopathic, neuromuscular, and syndromic. Approximately 80% of scoliosis cases are adolescent idiopathic scoliosis (AIS), with a prevalence of 3% in the general population.2,3
Early detection and treatment of AIS are crucial; bracing has been shown to decrease the need for surgical intervention and slow progression of high-risk curves.4 Screening programs have been instituted in many countries to detect the deformity early while the spine is still amenable to orthotic treatment.5-7 Initial assessment for scoliosis involves the Adams forward bend test.8 If spinal asymmetry is noted, it can be quantified with a scoliometer to determine the angle of trunk rotation (ATR) for screening and referral purposes. Although it is impossible to reliably predict the major curve given a scoliometer value (because of large standard deviations), scoliometer values of 5 and 7 degrees are associated with mean radiographic major curves of 11 and 20 degrees, respectively.9 In the past, patients with an ATR ≥7 degrees were referred to an orthopaedic specialist for scoliosis evaluation.9 The current standard of care is to refer a patient with an ATR ≥10 degrees for immediate orthopaedic evaluation. Patients with an ATR <5 degrees should be dismissed without re-screening, whereas patients with an ATR of 5 to 9 degrees should be re-screened every 6 months until 1 year after the occurrence of menarche.10 To date, no studies have examined the relationship between scoliometer readings and major curve magnitude in the context of body habitus or body mass index (BMI).
Scoliometer measurements of ATR may be influenced by the amount of overlying tissue. Thus, we questioned whether patients with higher BMI values may have lower scoliometer measurements for the same spinal curvature. If so, this may lead to later diagnosis of AIS and larger scoliotic curves at the time of presentation compared with normal-weight patients.11
We analyzed the relationship of BMI category with major curve magnitudes and scoliometer measurements of ATR in patients referred for evaluation of spinal deformity. We hypothesized that scoliometer measurements would be lower for a given spinal curvature in overweight and obese patients compared with normal-weight and underweight patients.
Methods
Study Design, Setting, and Participants
This was an institutional review board–approved retrospective cohort study of patients aged 10 to 18 years with AIS who presented to the senior author, an orthopaedic surgeon at a tertiary referral center, for initial evaluation of scoliosis or spinal asymmetry between January 2010 and June 2015.
We identified patients by using the International Classification of Diseases, Ninth Revision, Clinical Modification, code 737.30 for scoliosis and excluding those who did not have AIS. We included patients who had documentation of age, sex, BMI value, main thoracic major curve as measured by the Cobb method on radiographs, and main thoracic ATR measured with a traditional scoliometer. No patient had undergone treatment for AIS, and all were self-referred or referred by primary care providers or general orthopaedic surgeons. We excluded patients with scoliosis secondary to syndromic, neuromuscular, or congenital causes, as well as patients with leg-length discrepancies >1 cm, disc disease, sciatica, or infections. Patients were categorized into 4 groups on the basis of BMI percentile for age and sex (underweight, ≤4th percentile; normal weight, 5th to 84th percentile; overweight, 85th to 94th percentile; and obese, ≥95th percentile).
Statistical Analysis
We used descriptive statistics for demographic information, analysis of variance to assess differences in major curves, ATR, and age at presentation, chi-squared test of independence to assess differences in sex distribution, and logistic regression to assess the relationship between ATR and major curves. We used receiver operating characteristic (ROC) analyses of dichotomous categories of major curve magnitude (≥20 vs <20 degrees) to determine the most sensitive and specific scoliometer values for each group (using the minimum Euclidean distance between the point [0,1] and the curve); this method minimizes false positives while maximizing true positives. ATR values were then plotted in relation to the estimated probabilities (based on logistic regression) of a patient presenting with a major curve of ≥20 degrees. Statistical significance was defined as a P value of .05 or less. Statistical analyses were performed with the statistical package R, version 2.15.1 (Free Software Foundation's GNU General Public License), and Stata, version 13 (StataCorp LP, College Station, TX).
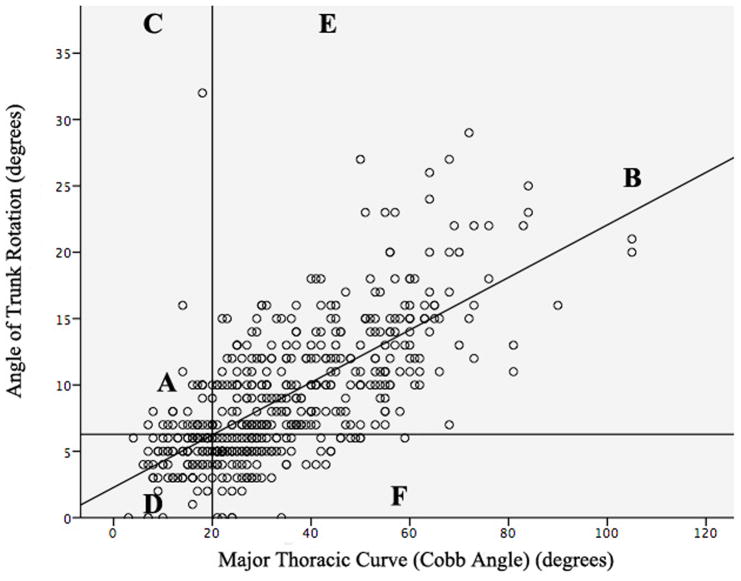
Results
This study included 483 patients (23 underweight, 372 normal weight, 52 overweight, and 36 obese). Mean (standard deviation [SD]) age was 14 (1.6) years, and 87% of patients were female (Table 1). Patients presented with a mean (SD) main thoracic major curve of 35 degrees (18 degrees) (range, 3 to 105 degrees) and a mean (SD) scoliometer value of 9 degrees (5 degrees) (range, 0 to 32 degrees) (Table 1). Post hoc comparisons using the Tukey honest significant difference test indicated that the mean major curve in the obese group was 10 degrees larger (95% confidence interval [CI], 3-15 degrees) than that in the normal-weight group (44 vs 34 degrees; P = 0.004). Linear regression between major thoracic curve and ATR demonstrated that the mean predicted ATR in patients with a 20-degree major curve was 6 degrees (95% CI, 5-7 degrees) with a correlation coefficient of 0.7 (P < 0.01) (Figs. 1, 2).
Table 1. Characteristics of 483 Adolescent Idiopathic Scoliosis Patients by Body Mass Index Category*.
| Mean (SD) | |||||
|---|---|---|---|---|---|
|
|
|||||
| Characteristic | Underweight (N = 23) | Normal Weight (N = 372) | Overweight (N = 52) | Obese (N = 36) | P |
| Age (y) | 14.8 (1.6) | 14.1 (1.6) | 13.6 (1.7) | 13.5 (1.5) | 0.182§ |
| Female sex | 12 (52)† | 333 (90)† | 41 (79)† | 32 (89)† | <0.001‡ |
| Main thoracic ATR (°) | 10 (7) | 9 (5) | 9 (5) | 10 (6) | 0.703§ |
| Main thoracic major curve (°) | 33 (22) | 34 (17) | 39 (22) | 44 (17) | 0.003§ |
ATR indicates angle of trunk rotation; SD, standard deviation.
Underweight, ≤4th percentile for age and sex; normal weight, 5th to 84th percentile for age; overweight, 85th to 94th percentile for age; obese, ≥95th percentile for age.
Expressed as number (%).
P values from χ2 analysis.
P values from analysis of variance.
Figure 1.
Linear regression of major thoracic curve vs angle of trunk rotation (ATR). A, 20-degree curve, ATR 6 degrees. B, Correlation coefficient: 0.7. C, 20% patients had <20-degree curves. D, 72% of these had ATR <7 degrees. E, 80% of patients had ≥20-degree curves. F, 73% of these had ATR ≥7 degrees.
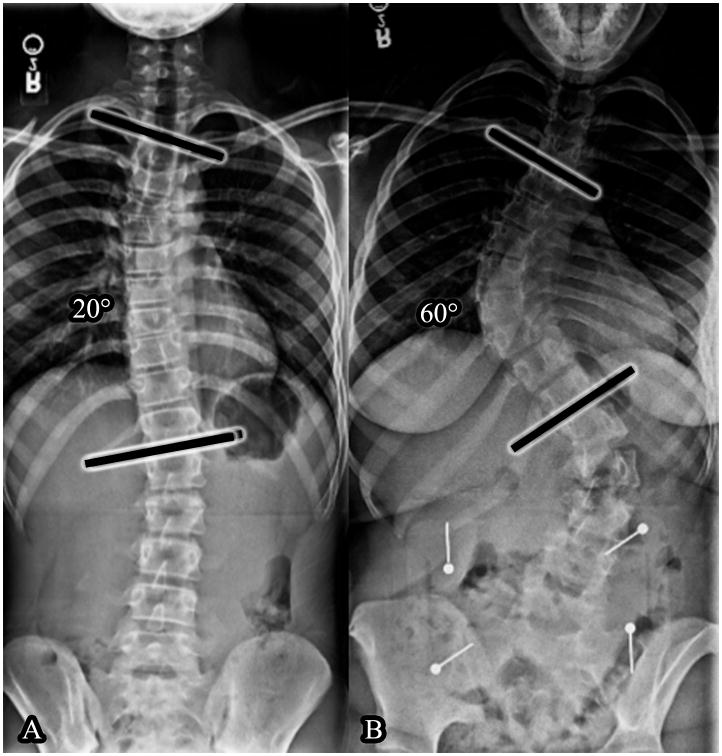
Figure 2.
Different body mass index and major curves as measured by the Cobb method, same scoliometer measurement. (A) Adolescent with body mass index value in the 47th percentile, 20 degree-curve, and 7 degree angle of trunk rotation. (B) Adolescent with body mass index value in the 96th percentile, 60-degree curve, and 7 degree angle of trunk rotation.
The odds of presenting with a major curve ≥20 degrees on radiography were 4.90 (95% CI, 1.12-21.80, P = 0.037) times higher for those in the obese group compared with those in the normal-weight group. There was no significant difference between the odds of the overweight (OR: 1.35 [95% CI, 0.60-3.04], P = 0.069) or underweight (OR: 0.50 [95% CI, 0.16-1.55], P = 0.31) patients compared with normal-weight patients.
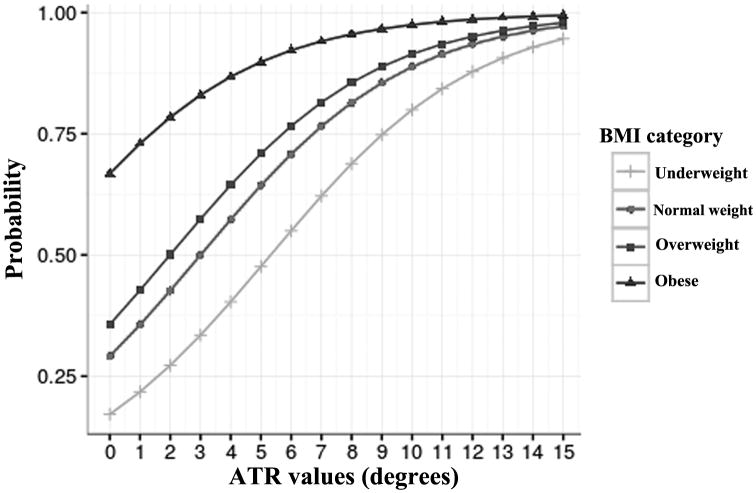
The optimal ATR cut-off values were 8 degrees for the underweight group, 7 degrees for the normal-weight group, 6 degrees for the overweight group, and 5 degrees for the obese group (sensitivities, specificities, positive predictive values, and negative predictive values shown in Table 2). Using these cut-off values, the probability of patients presenting with major curves of ≥20 degrees on radiography were 69% for underweight patients, 77% for normal-weight and overweight patients, and 90% for obese patients (Fig. 3). Given an ATR value of 5 degrees, the probabilities of presenting with a major curve of ≥20 degrees were 48% for underweight patients, 64% for normal-weight patients, 71% for overweight patients, and 90% for obese patients.
Table 2. Receiver Operating Characteristic Analysis of BMI in Relation to Major Curve ≥20° and Scoliometer Measurement.
| BMI Category* | No. of Patients | AUC (95% CI) | P | Scoliometer Measurement (°) | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|---|---|
| Underweight | 23 | 0.813 (0.639–0.986) | .019 | 8 | 75.0 | 85.7 | 92.3 | 60.0 |
| Normal weight | 372 | 0.793 (0.743–0.842) | <.001 | 7 | 72.8 | 71.8 | 90.7 | 41.2 |
| Overweight | 52 | 0.814 (0.652–0.976) | .002 | 6 | 78.6 | 80.0 | 94.3 | 47.1 |
| Obese | 36 | 0.934 (0.839–1.000) | .042 | 5 | 85.3 | 100† | 100† | 28.6 |
AUC indicates area under the curve; BMI, body mass index; CI, confidence interval; NPV, negative predictive value; PPV, positive predictive value.
Underweight, ≤4th percentile for age and sex; normal weight, 5th to 84th percentile for age; overweight, 85th to 94th percentile for age; obese, ≥95th percentile for age.
Limited because only 2 patients presented with major curves of <20°.
Figure 3.
Probability of presenting with a major curve ≥20 degrees based on body mass index (BMI) category. Angle of trunk rotation (ATR) in relation to probability of presenting with major curves ≥20 degrees. BMI categories (for age and sex): underweight, ≤4th percentile; normal weight, 5th to 84th percentile; overweight, 85th to 94th percentile; obese, ≥95th percentile.
Discussion
This study shows that scoliometer measurements for a given spinal curvature vary by patient body mass. Obese children had larger major curves at the time of presentation compared with their normal-weight counterparts. In patients overall, the mean ATR at a major curve of 20 degrees was approximately 6 degrees. We found a pattern indicating that patients with higher BMI values have lower scoliometer measurements of ATR for the same major curves.
Goodbody et al11 reported that overweight and obese patients with AIS presented with larger curve magnitudes (24- and 25-degree major curves, respectively) compared with normal-weight patients (18-degree major curve). In our study, there was a significant difference only between normal-weight (34-degree major curve) and obese (44-degree major curve) patients. Additionally, we found that obese patients had 4.9 times higher odds of presenting with a major curve ≥20 degrees compared with normal-weight patients. It is possible that patients, their parents, or their providers notice the scoliosis deformity later secondary to a patient's large body habitus. Additionally, Goodbody13 et al demonstrated that all patients in their study presenting with major curves in the surgical range of >45 degrees (15/150 patients) were overweight or obese. In our study, 127 of 483 patients had surgical-range curves. Of these patients, 5% were underweight, 65% were normal weight, 15% were overweight, and 15% were obese. Thus, although major curves were larger in obese patients, most patients requiring surgical intervention had BMI values within the normal range.
In 1984, Bunnell12 reported on 1065 patients who had been referred from screening programs for orthopaedic evaluation of scoliosis, showing that greater ATR was positively correlated with greater curve magnitude. Bunnell's study has defined the referral criterion for scoliosis for more than 3 decades, which is to refer a patient with a scoliometer value of ≥7 degrees to an orthopaedic surgeon.9 However, the mean predicted ATR at a major curve of 20 degrees was 6 degrees in our study (correlation coefficient, 0.70) compared with 7 degrees in Bunnell's study (correlation coefficient, 0.89). This may be because we have a larger proportion of overweight and obese patients in our study; the rate of adolescent obesity has more than quadrupled in the US in the last 3 decades.13,14 Ng et al15 reported global obesity data, showing a rise of 47% in the prevalence of overweight and obesity among children from 1980 to 2013, with the largest increase observed between 1992 and 2002.
The most important qualities of a screening test are sensitivity, specificity, reproducibility, and accuracy. The test should have well-defined cutoff values, and it should be safe, noninvasive, easy to perform, and inexpensive.16-18 We show a range of sensitivities from 73% to 85% and a range of specificities from 72% to 100%. Of note, the value of 100% specificity found in the obese population using a cut-off of 5 degrees is limited, because only 2 patients presented with major curves of <20 degrees in the obese cohort. Historically, for an ATR ≥7 degrees, the scoliometer test is characterized by a sensitivity of 83% and a specificity of 87%.19 These values are comparable to those found in our study by BMI cohort.
Our ROC analysis suggests a trend that for the same spinal curvature, patients with higher BMI values may have lower scoliometer measurements of ATR. This means that scoliosis may be diagnosed later in patients with higher BMI values. For example, an obese child who presents with a scoliometer measurement of 5 degrees would not undergo radiography or receive a referral to an orthopaedic surgeon on the basis of conventional guidelines, although the patient, according to this study, would have a 90% probability of having a major curve ≥20 degrees. In addition, a patient's large body habitus may mask physical examination findings. With new referral values, cases like these may be diagnosed earlier, resulting in earlier treatment.
Although these referral values may detect a higher prevalence of scoliosis in the obese and overweight population, bracing may not be as beneficial in preventing curve progression in these patients compared with normal-weight and underweight patients. O'Neill et al.20 found that overweight patients (BMI ≥85th percentile) were 3.1 times as likely to have unsuccessful orthotic treatment compared with patients who were not overweight. This may be attributable to the inability of the orthoses to transmit corrective forces effectively through increased soft tissue. However, 55% (17/31) of obese patients did not have curve progression. Of the patients who were not overweight, 28% (69/245) had curve progression. Although being overweight may undermine the success of bracing, overweight patients still benefited. Furthermore, earlier identification of scoliosis may enable patients to undergo lifestyle modifications with accompanying weight loss, making bracing more effective. Over the long term, these patients may not require surgery if diagnosed early and treated appropriately.
We found that when measuring ATR in underweight patients, the scoliometer had optimal sensitivity and specificity at 8 degrees, compared with 5 degrees in obese patients with the same major curve. This suggests that extra soft tissue objectively decreases the rotational deformity measured during the Adams forward bend test using the scoliometer.
Our study is limited by several factors. Sample sizes in the underweight, overweight, and obese groups were small compared with the normal-weight group. All patients were referred to an orthopaedic specialist; it is unknown how many of these referrals were made on the basis of scoliometer measurements. At our institution, scoliometer values were measured by 1 pediatric orthopaedic surgeon; therefore, interobserver and intraobserver reliability were not assessed. Future research may include examining the general adolescent population (eg, using samples of children screened in schools) to help define appropriate referral thresholds for patients in different BMI categories. Because of differences in sagittal alignment, the distribution of overlying soft tissue may differ between the kyphotic thoracic vertebra and the lordotic lumbar vertebra. Only main thoracic curves were assessed in this study; lumbar curves should be evaluated in future studies.
Despite these limitations, our results provide valuable information about BMI values in relation to spinal curvatures and scoliometer measurements of ATR. We demonstrated that obese patients present with larger thoracic curves, which may be attributable to later diagnosis because of having a larger body habitus. We recommend the modification of referral criteria based on scoliometer measurements to account for the increasing prevalence of obesity. We advocate that the conventional 7 degrees referral criterion be used for normal-weight patients, but that 8 degrees be used for underweight patients, 6 degrees for overweight patients, and 5 degrees for obese patients. These criteria may reduce unnecessary referrals for underweight patients while allowing earlier identification and treatment of scoliosis in overweight and obese adolescents.
Acknowledgments
Funding Statement: Funding was received for partial statistical analysis from the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health through Grant Number 1UL1TR001079.
Footnotes
Conflict of Interest Disclosures: The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- 1.Kane WJ. Scoliosis prevalence: a call for a statement of terms. Clin Orthop Relat Res. 1977;126:43–46. [PubMed] [Google Scholar]
- 2.Goldstein LA, Waugh TR. Classification and terminology of scoliosis. Clin Orthop Relat Res. 1973:10–22. doi: 10.1097/00003086-197306000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Riseborough EJ, Wynne-Davies R. A genetic survey of idiopathic scoliosis in Boston, Massachusetts. J Bone Joint Surg Am. 1973;55:974–982. [PubMed] [Google Scholar]
- 4.Weinstein SL, Dolan LA, Wright JG, et al. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. 2013;369:1512–1521. doi: 10.1056/NEJMoa1307337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lonstein JE, Bjorklund S, Wanninger MH, et al. Voluntary school screening for scoliosis in Minnesota. J Bone Joint Surg Am. 1982;64:481–488. [PubMed] [Google Scholar]
- 6.Pruijs JE, van der Meer R, Hageman MA, et al. The benefits of school screening for scoliosis in the central part of The Netherlands. Eur Spine J. 1996;5:374–379. doi: 10.1007/BF00301964. [DOI] [PubMed] [Google Scholar]
- 7.Soucacos PN, Soucacos PK, Zacharis KC, et al. School-screening for scoliosis. A prospective epidemiological study in northwestern and central Greece. J Bone Joint Surg Am. 1997;79:1498–1503. doi: 10.2106/00004623-199710000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Cote P, Kreitz BG, Cassidy JD, et al. A study of the diagnostic accuracy and reliability of the Scoliometer and Adam's forward bend test. Spine (Phila Pa 1976) 1998;23:796–802. doi: 10.1097/00007632-199804010-00011. discussion 803. [DOI] [PubMed] [Google Scholar]
- 9.Bunnell WP. Outcome of spinal screening. Spine (Phila Pa 1976) 1993;18:1572–1580. doi: 10.1097/00007632-199309000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Bunnell WP. Selective screening for scoliosis. Clin Orthop Relat Res. 2005:40–45. doi: 10.1097/01.blo.0000163242.92733.66. [DOI] [PubMed] [Google Scholar]
- 11.Goodbody CM, Sankar WN, Flynn JM. Presentation of Adolescent Idiopathic Scoliosis: The Bigger the Kid, the Bigger the Curve. J Pediatr Orthop. 2015 doi: 10.1097/BPO.0000000000000580. [DOI] [PubMed] [Google Scholar]
- 12.Bunnell WP. An objective criterion for scoliosis screening. J Bone Joint Surg Br. 1984;66:1381–1387. [PubMed] [Google Scholar]
- 13.National Center for Health Statistics (US) Hyattsville (MD): National Center for Health Statistics (US); 2012. May, Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Available from: http://www.ncbi.nlm.nih.gov/books/NBK98752/ [PubMed] [Google Scholar]
- 14.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grivas TB, Vasiliadis ES, Maziotou C, et al. The direct cost of “Thriasio” school screening program. Scoliosis. 2007;2:7. doi: 10.1186/1748-7161-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morrissy RT. School screening for scoliosis. A statement of the problem. Spine (Phila Pa 1976) 1988;13:1195–1197. doi: 10.1097/00007632-198810000-00028. [DOI] [PubMed] [Google Scholar]
- 18.Williams JI. Criteria for screening: are the effects predictable? Spine (Phila Pa 1976) 1988;13:1178–1186. doi: 10.1097/00007632-198810000-00023. [DOI] [PubMed] [Google Scholar]
- 19.Ashworth MA, Hancock JA, Ashworth L, et al. Scoliosis screening. An approach to cost/benefit analysis. Spine (Phila Pa 1976) 1988;13:1187–1188. doi: 10.1097/00007632-198810000-00024. [DOI] [PubMed] [Google Scholar]
- 20.O'Neill PJ, Karol LA, Shindle MK, et al. Decreased orthotic effectiveness in overweight patients with adolescent idiopathic scoliosis. The Journal of bone and joint surgery American volume. 2005;87:1069–1074. doi: 10.2106/JBJS.C.01707. [DOI] [PubMed] [Google Scholar]