Abstract
Obesity is a growing public health problem, which has now been considered as a pandemic non-communicable disease. However, the efficacy of several approaches for weight loss is limited and variable. Thus, alternative anti-obesity treatments are urgently warranted, which should be effective, safe, and widely available. Active compounds isolated from herbs are similar with the practice of Traditional Chinese Medicine, which has a holistic approach that can target to several organs and tissues in the whole body. Capsaicin, a major active compound from chili peppers, has been clearly demonstrated for its numerous beneficial roles in health. In this review, we will focus on the less highlighted aspect, in particular how dietary chili peppers and capsaicin consumption reduce body weight and its potential mechanisms of its anti-obesity effects. With the widespread pandemic of overweight and obesity, the development of more strategies for the treatment of obesity is urgent. Therefore, a better understanding of the role and mechanism of dietary capsaicin consumption and metabolic health can provide critical implications for the early prevention and treatment of obesity.
Keywords: adipogenesis, appetite, brown adipose tissue, Capsaicin, obesity, TRPV1
Introduction
The epidemic of obesity is a growing public health problem. The incidence of obesity has more than doubled since 1980, and has now reached worldwide epidemic status [1]. In 2014, the World Health Organization (WHO) estimated that 39% of the human adult population with 1.9 billion people were affected with overweight (body mass index (BMI) ≥25 kg/m2), and that obesity (BMI ≥30 kg/m2) affected approximately 13% with 600 million people [2,3]. Obesity is a serious risk factor as it is associated with chronic inflammation and metabolic syndrome [4], a cluster of morbidities that includes hypertension, hyperlipidemia, and Type 2 diabetes mellitus (T2DM) [5]. It can increase the risks of developing serious health problems, such as cardiovascular diseases, chronic kidney disease, and stroke [6,7]. Moreover, obese patients are more prone to contract several forms of cancer with reduced chances of survival [8]. Of particular concern is the incidence of overweight and obesity in children, with an estimated one-third of children and adolescents affected in the United States and over 41 million children are overweight before reaching puberty [2]. As such, obesity and its related diseases yield enormous tolls at individual, public health, and economic levels. In addition, genome-wide association studies (GWAS) have revealed compelling genetic signals influencing obesity risk, and genetic polymorphism plays a major role in determining obesity [9]. An updated randomized controlled trial indicated the higher body weight and waist circumference reductions in risk carriers than in non-risk carriers of the fat mass and obesity-associated (FTO) gene across different levels of personalized nutrition [10]. These data signify that the interventions should be personalized and vary with each individual [11]. Thus, the development of novel and personalized strategies for the early prevention and treatment of overweight and obesity is warranted.
Limitations in anti-obesity approaches
It has clearly established that weight loss will significantly diminish the complications of obesity [12]. Emerging human epidemiology studies indicated that reducing body weight, with weight loss of at least 5%, has long-term benefits on metabolic health and reduces the risks of developing insulin resistance, T2DM, and cardiovascular diseases [13]. However, weight loss is difficult and the obese individuals are struggling to achieve it, and the efficacy of several approaches for weight loss is limited and variable [14,15]. Firstly, it is widely accepted that a combination of physical exercise and low-calorie diet is the best approach to prevent and treat obesity. However, this strategy is difficult to implement and its compliance is poor. Gupta et al. [16] aimed to explore treatment satisfaction associated with different weight loss methods among patients with obesity. It showed that using self-modification weight loss techniques such as diet, exercise, and weight loss supplements has lowest treatment satisfaction, compared with gastric bypass and gastric banding, and prescription medication [16]. In addition, physical exercise and diet intervention also yield enormous tolls at economic level. It reported that retail sales of weight loss supplements were estimated to be more than $1.3 billion in 2001 in United States [17]. Thus, cheap, easily available therapies and supplements are urgently needed. The second approach is pharmaceutical drugs, such as orlistat, a potent and specific inhibitor of intestinal lipases. It can reduce body weight with an average weight loss of 3% during 1 year period [13]. However, its efficacy is variable and it can lead to gastrointestinal adverse effects, liver failure, and acute kidney injury [18]. Other anti-obesity drugs, such as rimonabant, fenfluramine, and sibutramine, have been withdrawn from the market due to severe adverse effects, including increased cardiovascular risks, mood disorders, and even suicidal susceptibility [14]. Thirdly, anti-diabetic agents, such as glucagon-like peptide 1 (GLP-1) analog, liraglutide has been shown its potential anti-obesity efficacy [19]. But it needs to be injected subcutaneously daily. Moreover, the weight loss is limited and it can increase the risk of pancreatitis [20]. Compared with aforementioned anti-obesity drugs, bariatric surgery such as Roux-en-Y gastric bypass or sleeve gastrectomy is more effective. However, it is physically invasive, relatively expensive, and its long-term effect is unclear [21]. Therefore, alternative anti-obesity treatments are urgently warranted, which should be effective, safe, and widely available [15].
An overview of chili peppers and capsaicin
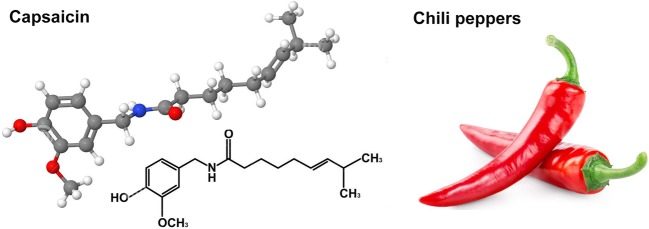
Chili pepper is generally used as a flavoring spice and is prominent in diets of various communities and cultures worldwide since 7000BC, with a long history of flavoring, coloring, preserving food as well as medication [26]. In chili pepper, more than 200 active constituents have been identified and some of its active constituents play multiple roles in the whole body [27]. Capsaicin, as a major active compound from chili pepper, has been established for its numerous beneficial roles in the human organism, including the treatment of pain inflammation, rheumatoid arthritis [28], and vasomotor rhinitis (Figure 1) [29]. Furthermore, capsaicin has proven an effective anti-cancer agent. Several preclinical studies showed that capsaicin could suppress various human neoplasia by generating reactive oxygen species and increasing apoptosis [30,31]. Finally, capsaicin demonstrated significant antioxidant properties, and it was postulated that this compound has important implications in the prevention or treatment of neurodegenerative diseases such as Alzheimer’s disease [32]. In addition to capsaicin as anti-obesity compounds, other types of natural products also have shown to be considered as anti-obesity compounds. Celastrol (from roots of the thunder god vine) can reduce appetite and food intake in mice that are fed a high-fat diet [33]. Stilbenoid resveratrol (from grapes and red wine), genistein (an isoflavone from soy), glycyrrhizin (from liquorice), quercetin, ethanolic extract (from ginseng roots), and green tea extract (including camellia sinensis, catechin, caffeine, and epigallocatechin gallate) play a role in adipogenesis inhibition, thus may have anti-obesity potency [15]. In this review, we will focus on the less highlighted aspect, in particular how dietary chili peppers and capsaicin consumption reduce body weight and the potential mechanisms of its anti-obesity effects. Figure 1 shows the molecular structure of capsaicin isolated from chili peppers.
Figure 1. The molecular structure of capsaicin isolated from chili peppers.
Clinical studies of the weight-loss effects of capsaicin
Weight-loss effects of capsaicin on lipid oxidation and energy expenditure
Epidemiological data revealed that the consumption of foods containing capsaicin was associated with a lower prevalence of obesity [34]. In one double-blind, randomized, placebo-controlled trial, it indicated that treatment of overweight or obese subjects with 6 mg/day capsinoid for 12 weeks was associated with abdominal fat loss measured by dual energy X-ray absorptiometry. Body weight was decreased as 0.9 and 0.5 kg in the capsinoid and placebo groups respectively. Moreover, none of the patients developed any adverse events (Table 1) [35]. Lejeune et al. [36] aimed to investigate whether capsaicin assists weight maintenance by limiting weight regain after weight loss of 5% to 10%. The results showed that capsaicin treatment caused sustained fat oxidation during weight maintenance compared with placebo (Table 1) [36]. Increase in the oxygen consumption (VO2) and body temperature reflecting increased energy expenditure, thus play critical role in weight loss. Fat oxidation was reported to be sustained together with elevation of the resting energy expenditure, and enhanced fat oxidation may contribute to increased energy expenditure. In another randomized double-blind study, it indicated that subjects between 30 and 65 years old with a BMI >23 kg/m2 treated with capsinoid (10 mg/kg per day) for 4 weeks safely and body weight tended to decrease during the 2- to 4-week period, with increased VO2, resting energy expenditure, and fat oxidation significantly (Table 1) [37]. Enhanced lipid oxidation and increased energy expenditure are potentially beneficial for weight management [38].
Table 1. Clinical studies of the weight-loss effects of capsaicin.
| Treatments | Year | Country | Study design | Subjects included | Baseline BMI | Sample size | Age (years) | Outcomes | Adverse events | Potential mechanism | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Capsinoids (6 mg per day for 12 weeks) | 2009 | U.S.A. | Double-blind, randomized, placebo-controlled trial | Overweight individuals | 30.6 ± 2.4 | N=80 | 42 ± 8 | Body weight decreased 0.92 kg; abdominal fat decreased 1.11% | None | Increase in fat oxidation and genetic polymorphisms | Snitker et al. [35] |
| Red pepper (capsaicin 10 g single meal) | 1999 | Canada | Prospective study | Healthy individuals | 25.3 ± 4.7 | N=23 | 25.8 ± 2.8 | Decreased appetite | None | Increase in sympathetic nervous system activity | Yoshioka et al. [40] |
| Capsinoids (10 mg/kg per day for 4 weeks) | 2007 | Japan | Double-blind, randomized, placebo-controlled trial | Men and postmenopausal women | >23 | N=48 | 30–65 | Body weight tended to decrease during the 2- to 4-week period | None | Increased VO2, energy expenditure, and fat oxidation | Inoue et al. [37] |
| Capsaicin (135 mg per day for 3 months) | 2003 | Netherlands | Randomized double-blind placebo-controlled study | Moderately overweight subjects | 29.3 ± 2.5 | N=140 | 18–60 | Significant increase in resting energy expenditure | None | More sustained fat oxidation | Lejeune et al. [36] |
| Capsinoids (9 mg per day for 8 weeks) | 2016 | Japan | Randomized double-blind placebo-controlled study | College students | 21.4 ± 1.8 | N=20 | 20.7 ± 1.2 | Increased brown adipose tissue (BAT) density | None | Increased BAT activity | Nirengi et al. [43] |
Weight-loss effects of capsaicin on appetite and brown adipose tissue
Dietary red pepper can suppress energy intake and modify macronutrient intake through appetite and satiety regulation [39]. One prospective study aimed to investigate the effects of capsaicin on feeding behavior and energy intake. It indicated that the addition of red pepper to the breakfast significantly decreased protein and fat intakes at lunch time, and the addition of red pepper to the appetizer significantly reduced the cumulative ad libitum energy and carbohydrate intakes during the rest of the lunch. These effects might be related to an increase in sympathetic nervous system activity (Table 1) [40]. BAT is known to play a critical role in cold-induced non-shivering thermogenesis to maintain body temperature, and it is expected to be a therapeutic target for obesity and related metabolic disorders in humans [41]. It showed chili pepper affects energy expenditure by triggering the BAT in the same way as low temperature does, leading to increased energy expenditure via non-shivering thermogenesis [42]. One recent clinical study showed that 9 mg of capsinoid for 8 weeks could increase BAT activity and increase thermogenesis in healthy subjects (Table 1) [43]. The results suggest that dietary capsaicin consumption could have a beneficial effect for weight management, by reducing energy intake and activation of BAT activity. The summary of the clinical studies about the weight-loss effects of capsaicin was shown Table 1.
Preclinical studies about anti-obesity effects of capsaicin and its potential mechanisms
Capsaicin and TRPV1 activation
Numerous epidemiology studies and animal studies indicated that capsaicin, as a transient receptor potential vanilloid 1 (TRPV1) agonist, may represent a potential strategy to treat obesity. Although it is well accepted that much of the effect is caused by stimulation of the TRPV1 receptor, the mechanism of action is not presently fully understood. Increasing evidence indicates that TRPV1 plays a critical role in the regulation of metabolic health for the whole body, including body weight, glucose and lipid metabolism, and cardiovascular system [44,45]. TRPV1 was deemed as a potential target for the prevention of obesity due to its effect on energy metabolism and balance [46,47]. Activation of TRPV1 by capsaicin can attenuate abnormal glucose homeostasis by stimulating insulin secretion and increasing GLP-1 levels (Table 2) [48,49]. Furthermore, capsaicin also plays its role in a receptor-independent manner. It reported that capsaicin was associated with nuclear factor-κB (NF-κB) inactivation and peroxisome proliferator-activated receptor-γ (PPARγ) activation, and then it could modulate the adipocyte function of adipose tissues in obese mouse and suppressed the inflammatory responses of adipose tissue macrophages, which are independent on TRPV1 [50]. Additionally, TRPV1 can play a critical role in cell proliferation and cancer. It showed that TRPV1 implicated as a regulator of growth factor signaling in the intestinal epithelium, which could subsequent suppress intestinal tumorgenesis [51].
Table 2. Preclinical studies about anti-obesity effects of capsaicin.
| Treatments | Species | Duration | Metabolic disorders | Potential mechanism | Reference |
|---|---|---|---|---|---|
| 0–250 μmol/l capsaicin | 3T3-L1 preadipocytes and adipocytes | 24–72 h | Decreased the amount of intracellular triglycerides, GPDH activity | Inhibited the expression of PPARγ, C/EBP-α, and leptin | Hsu et al. [52] |
| Induced apoptosis | Induced up-regulation of adiponectin at the protein level | ||||
| Inhibited adipogenesis | |||||
| 1 μmol/l capsaicin | 3T3-L1 preadipocytes | 3–8 days | Prevented the adipogenesis | Increased intracellular calcium | Zhang et al. [53] |
| 0.015% capsaicin | Male C57BL/6 mice | 10 weeks | Decreased triglyceride levels | Decreased TRPV-1 expression in adipose tissue | Kang et al. [54] |
| Lowered fasting glucose, insulin, and leptin levels | Increased mRNA/protein of adiponectin in the adipose tissue | ||||
| Increased PPARα/PGC-1α mRNA in the liver | |||||
| 10 mg/kg body weight capsaicin | Std ddY mice | 2 weeks | Lower body weight | Increased oxygen consumption | Ohnuki et al. [55] |
| Markedly suppressed body fat accumulation | Stimulated the secretion of adrenalin | ||||
| Decreased triglyceride levels | |||||
| 0.3% capsinoids | C57BL/6J mice | 8 weeks | Suppressed body weight gain under the HFD | Increased energy expenditure | Saito et al. [57], Ohyama et al. [58] |
| Decreased plasma cholesterol level | Activation of fat oxidation in skeletal muscle | ||||
| Prevented diet-induced liver steatosis | Activation lipolysis in BAT | ||||
| Increased cAMP levels and PKA activity in BAT | |||||
| 0.003%, 0.01%, and 0.03% capsaicin | wild-type and TRPV1−/− mice | 16 weeks | Promoted weight loss | Increased the expression of UCP-1, BMP8b, SIRT-1, PGC-1α, and PRDM-16 in BAT | Baskaran et al. [59] |
| Enhanced the respiratory exchange ratio | Increased the phosphorylation of SIRT-1 | ||||
| Countered hypercholesterolemia | |||||
| 0.01% capsaicin | wild-type and TRPV1−/− mice | 26 weeks | Countered obesity | Promoted SIRT-1 expression | Baskaran et al. [60] |
| Browning of WAT | Increased the expression of PGC-1α | ||||
| Facilitated PPARγ–PRDM-16 interaction | |||||
| 0.01% capsaicin | wild-type and TRPV1−/− mice | 24 weeks | Ameliorated abnormal glucose homeostasis | Activation of TRPV1-mediated GLP-1 secretion in the intestinal cells | Wang et al. [49] |
| Increased GLP-1 levels in the plasma and ileum | |||||
| 640 μmol/L, 2 ml/kg capsaicin | Sprague-Dawley rats | 15 min | Increased superior mesenteric artery blood flow | Induced a dichotomous pattern of blood flow changes | Leung et al. [68] |
| Reduction in hydrogen gas clearance | |||||
| 0.01% capsaicin | C57BL/6J male mice | 9 weeks | Reduced weight gain | Modest modulation of the gut microbiota | Shen et al. [69] |
| Improved glucose tolerance | Up-regulated the expression of Muc2 and antimicrobial protein gene Reg3g in the intestine |
BMP8b, bone morphogenetic protein-8b; cAMP, cyclic adenosine monophosphate; C/EBP-α, CCAAT-enhancer-binding protein-α; GPDH, glycerol-3-phosphate dehydrogenase; Muc2, mucin 2 gene; PGC1-α, PPARγ co-activator 1-α; PKA, protein kinase A; PRDM-16, positive regulatory domain containing 16; Reg3g, regenerating islet-derived protein 3γ; SIRT-1, sirtuin-1; UCP-1, uncoupling protein 1; WAT, white adipose tissue.
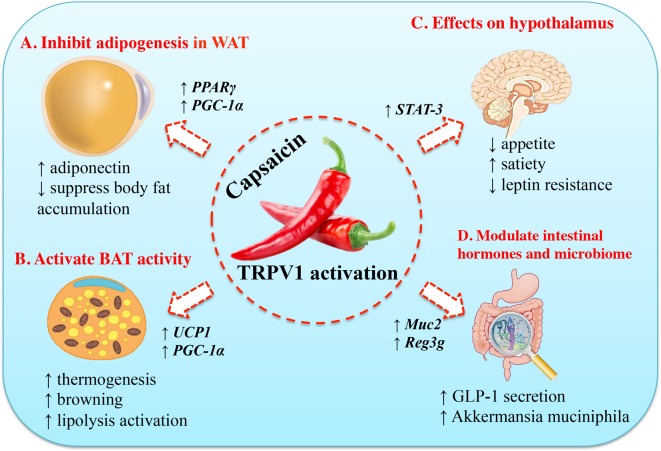
The potential mechanisms underlying the anti-obesity effects of capsaicin include: (1) increase lipid oxidation and inhibit adipogenesis; (2) activate BAT activity and induce thermogenesis; (3) suppress appetite and increase satiety regulated by neuronal circuits in the hypothalamus; (4) modulate the function of gastrointestinal tract and gut microbiome. The molecular mechanisms of the anti-obesity effects of capsaicin were summarized in Figure 2. In addition, we further collected most preclinical studies, including in vitro studies and rodent experiments about the anti-obesity effects of capsaicin (Table 2).
Figure 2. Molecular mechanisms of the anti-obesity effects of capsaicin.
(A) Capsaicin can inhibit adipogenesis in preadipocyte and adipocyte by up-regulating the expression of PPARγ and UCP-1. Thus, it will stimulate adiponectin secretion and increase body fat accumulation. (B) Capsaicin can activate BAT activity, accompanied by increased expression of UCP-1 and PGC-1α. (C) Capsaicin can suppress appetite, increase satiety, and ameliorate insulin resistance. (D) Capsaicin can modulate its function in gastrointestinal tract and gut microbiome, including stimulation of GLP-1 secretion and increase in population of the gut bacterium Akkermansia muciniphila. STAT-3, signal transducer and activator of transcription-3.
Capsaicin and its role in adipogenesis
Adipogenesis is the critical and original process of fatty adipose accumulation. It suggested that decreased preadipocyte differentiation, proliferation, and lipogenesis have the potential to reduce obesity. Hsu et al. [52] demonstrated that capsaicin inhibited the expression of PPARγ, C/EBP-α, and leptin, but induced up-regulation of adiponectin at the protein level. Thus, it efficiently induced apoptosis and inhibited adipogenesis in 3T3-L1 preadipocytes and adipocytes in vitro (Table 2, Figure 2) [52]. Zhang et al. [53] found that capsaicin treatment prevented adipogenesis of 3T3-L1-preadipocytes in vitro, with increased intracellular calcium (Figure 2). Male C57BL/6 obese mice fed a high-fat diet for 10 weeks received a supplement of 0.015% capsaicin showed decreased fasting glucose, insulin, leptin concentrations, and markedly improved glucose intolerance in obese mice, accompanied with decreased TRPV-1 expression in adipose tissue, increased adiponectin expression in the adipose tissue, and increased peroxisome proliferator-activated receptor-α (PPARα) and PGC-1α expression in the liver (Table 2, Figure 2) [54]. Ohnuki et al. [55] demonstrated that mice treated with 10 mg/kg body weight capsaicin could markedly suppressed body fat accumulation and promoted energy metabolism (Table 2). Hence, these studies supported that capsaicin could decrease adipogenensis and regulate genes function related with lipid metabolism, and then it can has the potential to lose weight.
Capsaicin and its role in brown adipose tissue
BAT is the main site of adaptive thermogenesis and experimental studies have associated BAT activity with protection against obesity and metabolic diseases [56]. A review illustrated that the activity of BAT can be activated and recruited not only by cold exposure but also by various food ingredients, such as capsaicin in chili pepper (Table 2) [57]. Capsinoids supplementation with exercise in C57BL/6J mice additively decreased body weight gain and fat accumulation, and increased whole body energy expenditure compared with exercise alone. The underlying mechanisms may be associated with increased energy expenditure, lipolysis activation in BAT, and increased cyclic adenosine monophosphate (cAMP) levels and PKA activity in BAT (Table 2, Figure 2) [58]. One up-to-date rodent experiment showed that capsaicin could counter the detrimental effects of high-fat diet, including glucose intolerance, hypercholesterolemia, and suppressed activity in BAT. These effects were mainly by increasing the expression of metabolically important thermogenic genes, including UCP-1, BMP8b, SIRT-1, PGC-1α, and positive regulatory domain containing zinc finger protein 16 (PRDM-16) in BAT. Furthermore, capsaicin supplementation, post high-fat diet, promoted weight loss and enhanced the respiratory exchange ratio. All these data suggested that capsaicin is a novel strategy to counter diet-induced obesity by enhancing metabolism and energy expenditure (Table 2, Figure 2) [59]. Baskaran et al. showed that activation of TRPV1 channels by dietary capsaicin triggered browning of adipose tissue to counteract obesity (Table 2) [60]. Collectively, these observations provide evidence that capsaicin can activate and recruit BAT, which would be a promising strategy to counter obesity.
Capsaicin and its role in appetite and satiety
Energy balance requires an ability of the brain to detect the status of energy stores and match energy intake with expenditure, and energy homeostasis is mainly controlled by neuronal circuits in the hypothalamus [61]. Hypothalamic endoplasmic reticulum stress occurs in individuals with obesity and is thought to induce low levels of leptin receptor signaling and play a central role in development of leptin resistance [62]. The adipose tissue-derived hormone leptin acts via its receptor in the brain to regulate energy balance and neuroendocrine function. Leptin resistance is a pathological condition, which means the lack of appetite reduction in response to leptin and the body fails to adequately respond to it [63]. Lee et al. [64] found that TRPV1 had a major role in regulating glucose metabolism and hypothalamic leptin’s effects in obesity, with hypothalamic STAT-3 activity blunted in the TRPV1 knockout mice (Figure 2). Addition of dietary capsaicin has been shown to increase satiety and it indicated that capsaicin increased sensation of fullness in energy balance, and decreased desire to eat after dinner in negative energy balance [65]. Although the studies about capsaicin and its role in appetite is limited, it inspired us that neuronal circuits in the hypothalamus may be a pivotal target of capsaicin.
Capsaicin and its role in gastrointestinal tract and gut microbiome
Capsaicin is passively absorbed in the stomach with greater than 80% efficiency and upper portion of the small intestine [66]. Thus, it may activate local TRPV1 channels in gastrointestinal tract to initiate a series of physiological effects. Dietary capsaicin consumption triggered the intestinal mucosal afferent nerves and increased intestinal blood flow [67]. Acute single administration of 640 μmol/l capsaicin into the duodenal lumen in anesthetized rats significantly increases superior mesenteric artery blood flow (Table 2) [68]. In addition, it showed that dietary capsaicin ameliorated abnormal glucose homeostasis and increased GLP-1 levels in the plasma and ileum through the activation of TRPV1-mediated GLP-1 secretion in the intestinal cells and tissues (Table 2, Figure 2) [49]. Recent study demonstrated that anti-obesity effect of capsaicin in mice fed with high-fat diet was associated with an increase in population of the gut bacterium Akkermansia muciniphila. Further studies found that capsaicin directly up-regulated the expression of Muc2 and antimicrobial protein gene Reg3g in the intestine (Table 2, Figure 2) [69]. These data suggested that the anti-obesity effect of capsaicin is associated with a modest modulation of the function in gastrointestinal tract and gut microbiome.
Conclusions
In summary, capsaicin plays a critical role in human and has multiple benefits for metabolic health, especially for weight loss in obese individuals. It is well accepted that the potential application of active compounds isolated from herbs are similar with the practice of traditional Chinese medicine, which has a holistic approach that can target to different organs and tissues in the whole body. More importantly, no adverse effects with capsaicin were observed in most studies. Thus, chili peppers and capsaicin are safely and easily applicable to our daily life. Considering that chili peppers have been a vital part of culinary cultures worldwide and have a long history of use for flavoring, so it is more feasible to be utilized to treat overweight and obesity, compare with medications or other interventions with certain side effects. Dietary chili peppers supplementation or to be food additives, with ideal dosage may be tentative methods for capsaicin to play its protective roles in metabolic health. With the widespread pandemic of overweight and obesity, the development of more strategies for the treatment of obesity is urgent. Therefore, a better understanding of the role and mechanism of dietary capsaicin consumption and metabolic health can provide critical implications for the early prevention and treatment of obesity.
Abbreviations
- BAT
brown adipose tissue
- BMI
body mass index
- BMP8b
bone morphogenetic protein-8b
- cAMP
cyclic adenosine monophosphate
- C/EBP-α
CCAAT-enhancer-binding protein-α
- HFD
high fat diet
- GLP-1
glucagon-like peptide-1
- GPDH
glycerol-3-phosphate dehydrogenase
- Muc2
mucin 2 gene
- NF-κB
nuclear factor-κB
- PGC1-α
PPARγ co-activator 1-α
- PKA
protein kinase A
- PPARα
peroxisome proliferator-activated receptor-α
- PPARγ
peroxisome proliferator-activated receptor-γ
- PRDM-16
positive regulatory domain containing 16
- PR
positive regulatory
- Reg3g
regenerating islet-derived protein 3γ
- SIRT-1
sirtuin-1
- STAT-3
signal transducer and activator of transcription-3
- T2DM
Type 2 diabetes mellitus
- TRPV1
transient receptor potential vanilloid 1
- UCP-1
uncoupling protein 1
- WAT
white adipose tissue
- WHO
World Health Organization
Funding
This work was supported by the National Natural Science Foundation of China [grant numbers 81170736 and 81570715]; National Key Research and Development Program of China [grant number 2016YFA0101002]; National Natural Science Foundation for Young Scholars of China [grant number 81300649]; and China Scholarship Council Foundation [grant number 201506210378]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests
The authors declare that there are no competing interests associated with the manuscript.
Author contribution
J.Z. and X.H.X. have made substantial contributions to ideas, conception, and design of the review. S.Z. and Q.Y.F. searched the databases, selected studies, extracted the data, and wrote the manuscript. S.Z. and Q.Z. reviewed and edited the manuscript. X.H.X. contributed to the design, reviewed, and edited the manuscript.
References
- 1.Caballero B. (2007) The global epidemic of obesity: an overview. Epidemiol. Rev. 29, 1–5 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (2016) Obesity and overweight
- 3.Ogden C.L., Carroll M.D., Kit B.K. and Flegal K.M. (2014) Prevalence of childhood and adult obesity in the United States, 2011–2012. J. Am. Med. Assoc. 311, 806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Canale M.P., Manca di Villahermosa S., Martino G., Rovella V., Noce A., De Lorenzo A. et al. (2013) Obesity-related metabolic syndrome: mechanisms of sympathetic overactivity. Int. J. Endocrinol. 2013, 865965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khodabandehloo H., Gorgani-Firuzjaee S., Panahi G. and Meshkani R. (2016) Molecular and cellular mechanisms linking inflammation to insulin resistance and beta-cell dysfunction. Transl. Res. 167, 228–256 [DOI] [PubMed] [Google Scholar]
- 6.Kotsis V., Nilsson P., Grassi G., Mancia G., Redon J., Luft F. et al. (2015) New developments in the pathogenesis of obesity-induced hypertension. J. Hypertens. 33, 1499–1508 [DOI] [PubMed] [Google Scholar]
- 7.Mascali A., Franzese O., Nistico S., Campia U., Lauro D., Cardillo C. et al. (2016) Obesity and kidney disease: beyond the hyperfiltration. Int. J. Immunopathol. Pharmacol. 29, 354–363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basen-Engquist K. and Chang M. (2011) Obesity and cancer risk: recent review and evidence. Curr. Oncol. Rep. 13, 71–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chesi A. and Grant S.F. (2015) The genetics of pediatric obesity. Trends Endocrinol. Metab. 26, 711–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Celis-Morales C., Marsaux C.F., Livingstone K.M., Navas-Carretero S., San-Cristobal R., Fallaize R. et al. (2017) Can genetic-based advice help you lose weight? Findings from the Food4Me European randomized controlled trial [DOI] [PubMed]
- 11.Nielsen J. (2017) Systems biology of metabolism: a driver for developing personalized and precision medicine. Cell Metab. 25, 572–579 [DOI] [PubMed] [Google Scholar]
- 12.Kornet-van der Aa D.A., Altenburg T.M., van Randeraad-van der Zee C.H. and Chinapaw M.J. (2017) The effectiveness and promising strategies of obesity prevention and treatment programmes among adolescents from disadvantaged backgrounds: a systematic review. Obes. Rev. 18, 581-593 [DOI] [PubMed] [Google Scholar]
- 13.Yanovski S.Z. and Yanovski J.A. (2014) Long-term drug treatment for obesity: a systematic and clinical review. J. Am. Med. Assoc. 311, 74–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dietrich M.O. and Horvath T.L. (2012) Limitations in anti-obesity drug development: the critical role of hunger-promoting neurons. Nat. Rev. Drug Discov. 11, 675–691 [DOI] [PubMed] [Google Scholar]
- 15.Martel J., Ojcius D.M., Chang C.J., Lin C.S., Lu C.C., Ko Y.F. et al. (2017) Anti-obesogenic and antidiabetic effects of plants and mushrooms. Nat. Rev. Endocrinol. 13, 149–160 [DOI] [PubMed] [Google Scholar]
- 16.Gupta S. and Wang Z. (2016) Treatment satisfaction with different weight loss methods among respondents with obesity. Clin. Obes. 6, 161–170 [DOI] [PubMed] [Google Scholar]
- 17.Saper R.B., Eisenberg D.M. and Phillips R.S. (2004) Common dietary supplements for weight loss. Am. Fam. Physician. 70, 1731–1738 [PubMed] [Google Scholar]
- 18.Filippatos T.D., Derdemezis C.S., Gazi I.F., Nakou E.S., Mikhailidis D.P. and Elisaf M.S. (2008) Orlistat-associated adverse effects and drug interactions: a critical review. Drug Saf. 31, 53–65 [DOI] [PubMed] [Google Scholar]
- 19.Manigault K.R. and Thurston M.M. (2016) Liraglutide: a glucagon-like peptide-1 agonist for chronic weight management. Consult. Pharm. 31, 685–697 [DOI] [PubMed] [Google Scholar]
- 20.Prasad-Reddy L. and Isaacs D. (2015) A clinical review of GLP-1 receptor agonists: efficacy and safety in diabetes and beyond. Drugs Context 4, 212283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanipah Z.N. and Schauer P.R. (2017) Surgical treatment of obesity and diabetes. Gastrointest. Endosc. Clin. N. Am. 27, 191–211 [DOI] [PubMed] [Google Scholar]
- 22.Hao P.P., Jiang F., Chen Y.G., Yang J., Zhang K., Zhang M.X. et al. (2015) Traditional Chinese medication for cardiovascular disease. Nat. Rev. Cardiol. 12, 115–122 [DOI] [PubMed] [Google Scholar]
- 23.Kong L.Y. and Tan R.X. (2015) Artemisinin, a miracle of traditional Chinese medicine. Nat. Prod. Rep. 32, 1617–1621 [DOI] [PubMed] [Google Scholar]
- 24.Koehn F.E. and Carter G.T. (2005) The evolving role of natural products in drug discovery. Nat. Rev. Drug Discov. 4, 206–220 [DOI] [PubMed] [Google Scholar]
- 25.Fabricant D.S. and Farnsworth N.R. (2001) The value of plants used in traditional medicine for drug discovery. Environ. Health. Perspect. 109, 69–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kraft K.H., Brown C.H., Nabhan G.P., Luedeling E., Luna Ruiz Jde J., Coppens d’Eeckenbrugge G. et al. (2014) Multiple lines of evidence for the origin of domesticated chili pepper, Capsicum annuum, in Mexico. Proc. Natl. Acad. Sci. U.S.A. 111, 6165–6170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Varghese S., Kubatka P., Rodrigo L., Gazdikova K., Caprnda M., Fedotova J. et al. (2016) Chili pepper as a body weight-loss food. Int. J. Food Sci. Nutr. 1–10 [DOI] [PubMed] [Google Scholar]
- 28.Richards B.L., Whittle S.L. and Buchbinder R. (2012) Neuromodulators for pain management in rheumatoid arthritis. Cochrane Database Syst. Rev. 1, Cd008921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh U. and Bernstein J.A. (2014) Intranasal capsaicin in management of nonallergic (vasomotor) rhinitis. Prog. Drug Res. 68, 147–170 [DOI] [PubMed] [Google Scholar]
- 30.Zheng L., Chen J., Ma Z., Liu W., Yang F., Yang Z. et al. (2016) Capsaicin enhances anti-proliferation efficacy of pirarubicin via activating TRPV1 and inhibiting PCNA nuclear translocation in 5637 cells. Mol. Med. Rep. 13, 881–887 [DOI] [PubMed] [Google Scholar]
- 31.Liu Y.P., Dong F.X., Chai X., Zhu S., Zhang B.L. and Gao D.S. (2016) Role of autophagy in capsaicin-induced apoptosis in U251 glioma cells. Cell. Mol. Neurobiol. 36, 737–743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dairam A., Fogel R., Daya S. and Limson J.L. (2008) Antioxidant and iron-binding properties of curcumin, capsaicin, and S-allylcysteine reduce oxidative stress in rat brain homogenate. J. Agric. Food Chem. 56, 3350–3356 [DOI] [PubMed] [Google Scholar]
- 33.Liu J., Lee J., Salazar Hernandez M.A., Mazitschek R. and Ozcan U. (2015) Treatment of obesity with celastrol. Cell 161, 999–1011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wahlqvist M.L. and Wattanapenpaiboon N. (2001) Hot foods–unexpected help with energy balance? Lancet 358, 348–349 [DOI] [PubMed] [Google Scholar]
- 35.Snitker S., Fujishima Y., Shen H., Ott S., Pi-Sunyer X., Furuhata Y. et al. (2009) Effects of novel capsinoid treatment on fatness and energy metabolism in humans: possible pharmacogenetic implications. Am. J. Clin. Nutr. 89, 45–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lejeune M.P., Kovacs E.M. and Westerterp-Plantenga M.S. (2003) Effect of capsaicin on substrate oxidation and weight maintenance after modest body-weight loss in human subjects. Br. J. Nutr. 90, 651–659 [DOI] [PubMed] [Google Scholar]
- 37.Inoue N., Matsunaga Y., Satoh H. and Takahashi M. (2007) Enhanced energy expenditure and fat oxidation in humans with high BMI scores by the ingestion of novel and non-pungent capsaicin analogues (capsinoids). Biosci. Biotechnol. Biochem. 71, 380–389 [DOI] [PubMed] [Google Scholar]
- 38.Whiting S., Derbyshire E. and Tiwari B.K. (2012) Capsaicinoids and capsinoids. A potential role for weight management? A systematic review of the evidence Appetite 59, 341–348 [DOI] [PubMed] [Google Scholar]
- 39.Whiting S., Derbyshire E.J. and Tiwari B. (2014) Could capsaicinoids help to support weight management? A systematic review and meta-analysis of energy intake data Appetite 73, 183–188 [DOI] [PubMed] [Google Scholar]
- 40.Yoshioka M., St-Pierre S., Drapeau V., Dionne I., Doucet E., Suzuki M. et al. (1999) Effects of red pepper on appetite and energy intake. Br. J. Nutr. 82, 115–123 [PubMed] [Google Scholar]
- 41.Yoneshiro T. and Saito M. (2015) Activation and recruitment of brown adipose tissue as anti-obesity regimens in humans. Ann. Med. 47, 133–141 [DOI] [PubMed] [Google Scholar]
- 42.Saito M. and Yoneshiro T. (2013) Capsinoids and related food ingredients activating brown fat thermogenesis and reducing body fat in humans. Curr. Opin. Lipidol. 24, 71–77 [DOI] [PubMed] [Google Scholar]
- 43.Nirengi S., Homma T., Inoue N., Sato H., Yoneshiro T., Matsushita M. et al. (2016) Assessment of human brown adipose tissue density during daily ingestion of thermogenic capsinoids using near-infrared time-resolved spectroscopy. J. Biomed. Opt. 21, 091305. [DOI] [PubMed] [Google Scholar]
- 44.Chen J., Li L., Li Y., Liang X., Sun Q., Yu H. et al. (2015) Activation of TRPV1 channel by dietary capsaicin improves visceral fat remodeling through connexin43-mediated Ca2+ influx. Cardiovasc. Diabetol. 14, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sun F., Xiong S. and Zhu Z. (2016) Dietary capsaicin protects cardiometabolic organs from dysfunction. Nutrients 8, 1-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ludy M.J. and Mattes R.D. (2012) Comparison of sensory, physiological, personality, and cultural attributes in regular spicy food users and non-users. Appetite 58, 19–27 [DOI] [PubMed] [Google Scholar]
- 47.Ma L., Zhong J., Zhao Z., Luo Z., Ma S., Sun J. et al. (2011) Activation of TRPV1 reduces vascular lipid accumulation and attenuates atherosclerosis. Cardiovasc. Res. 92, 504–513 [DOI] [PubMed] [Google Scholar]
- 48.Gram D.X., Ahren B., Nagy I., Olsen U.B., Brand C.L., Sundler F. et al. (2007) Capsaicin-sensitive sensory fibers in the islets of Langerhans contribute to defective insulin secretion in Zucker diabetic rat, an animal model for some aspects of human type 2 diabetes. Eur. J. Neurosci. 25, 213–223 [DOI] [PubMed] [Google Scholar]
- 49.Wang P., Yan Z., Zhong J., Chen J., Ni Y., Li L. et al. (2012) Transient receptor potential vanilloid 1 activation enhances gut glucagon-like peptide-1 secretion and improves glucose homeostasis. Diabetes 61, 2155–2165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kang J.H., Kim C.S., Han I.S., Kawada T. and Yu R. (2007) Capsaicin, a spicy component of hot peppers, modulates adipokine gene expression and protein release from obese-mouse adipose tissues and isolated adipocytes, and suppresses the inflammatory responses of adipose tissue macrophages. FEBS Lett. 581, 4389–4396 [DOI] [PubMed] [Google Scholar]
- 51.de Jong P.R., Takahashi N., Harris A.R., Lee J., Bertin S., Jeffries J. et al. (2014) Ion channel TRPV1-dependent activation of PTP1B suppresses EGFR-associated intestinal tumorigenesis. J. Clin. Invest. 124, 3793–3806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hsu C.L. and Yen G.C. (2007) Effects of capsaicin on induction of apoptosis and inhibition of adipogenesis in 3T3-L1 cells. J. Agric. Food Chem. 55, 1730–1736 [DOI] [PubMed] [Google Scholar]
- 53.Zhang L.L., Yan Liu D., Ma L.Q., Luo Z.D., Cao T.B., Zhong J. et al. (2007) Activation of transient receptor potential vanilloid type-1 channel prevents adipogenesis and obesity. Circ. Res. 100, 1063–1070 [DOI] [PubMed] [Google Scholar]
- 54.Kang J.H., Goto T., Han I.S., Kawada T., Kim Y.M. and Yu R. (2010) Dietary capsaicin reduces obesity-induced insulin resistance and hepatic steatosis in obese mice fed a high-fat diet. Obesity (Silver Spring) 18, 780–787 [DOI] [PubMed] [Google Scholar]
- 55.Ohnuki K., Haramizu S., Oki K., Watanabe T., Yazawa S. and Fushiki T. (2001) Administration of capsiate, a non-pungent capsaicin analog, promotes energy metabolism and suppresses body fat accumulation in mice. Biosci. Biotechnol. Biochem. 65, 2735–2740 [DOI] [PubMed] [Google Scholar]
- 56.Villarroya F., Cereijo R., Villarroya J. and Giralt M. (2017) Brown adipose tissue as a secretory organ. Nat. Rev. Endocrinol. 13, 26–35 [DOI] [PubMed] [Google Scholar]
- 57.Saito M., Yoneshiro T. and Matsushita M. (2015) Food ingredients as anti-obesity agents. Trends Endocrinol. Metab. 26, 585–587 [DOI] [PubMed] [Google Scholar]
- 58.Ohyama K., Nogusa Y., Suzuki K., Shinoda K., Kajimura S. and Bannai M. (2015) A combination of exercise and capsinoid supplementation additively suppresses diet-induced obesity by increasing energy expenditure in mice. Am. J. Physiol. Endocrinol. Metab. 308, E315–E323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baskaran P., Krishnan V., Fettel K., Gao P., Zhu Z., Ren J. et al. (2017) TRPV1 activation counters diet-induced obesity through sirtuin-1 activation and PRDM-16 deacetylation in brown adipose tissue. Int. J. Obes. (Lond.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Baskaran P., Krishnan V., Ren J. and Thyagarajan B. (2016) Capsaicin induces browning of white adipose tissue and counters obesity by activating TRPV1 channel-dependent mechanisms. Br. J. Pharmacol. 173, 2369–2389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ahima R.S. and Antwi D.A. (2008) Brain regulation of appetite and satiety. Endocrinol. Metab. Clin. North Am. 37, 811–823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ozcan L., Ergin A.S., Lu A., Chung J., Sarkar S., Nie D. et al. (2009) Endoplasmic reticulum stress plays a central role in development of leptin resistance. Cell Metab. 9, 35–51 [DOI] [PubMed] [Google Scholar]
- 63.Myers M.G., Cowley M.A. and Munzberg H. (2008) Mechanisms of leptin action and leptin resistance. Annu. Rev. Physiol. 70, 537–556 [DOI] [PubMed] [Google Scholar]
- 64.Lee E., Jung D.Y., Kim J.H., Patel P.R., Hu X., Lee Y. et al. (2015) Transient receptor potential vanilloid type-1 channel regulates diet-induced obesity, insulin resistance, and leptin resistance. FASEB J. 29, 3182–3192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Janssens P.L., Hursel R. and Westerterp-Plantenga M.S. (2014) Capsaicin increases sensation of fullness in energy balance, and decreases desire to eat after dinner in negative energy balance. Appetite 77, 44–49 [DOI] [PubMed] [Google Scholar]
- 66.Kawada T., Suzuki T., Takahashi M. and Iwai K. (1984) Gastrointestinal absorption and metabolism of capsaicin and dihydrocapsaicin in rats. Toxicol. Appl. Pharmacol. 72, 449–456 [DOI] [PubMed] [Google Scholar]
- 67.Leung F.W. (2008) Capsaicin-sensitive intestinal mucosal afferent mechanism and body fat distribution. Life Sci. 83, 1–5 [DOI] [PubMed] [Google Scholar]
- 68.Leung F.W., Golub M., Tuck M., Yip I., Leung J.W. and Go V.L. (2001) Stimulation of intestinal mucosal afferent nerves increases superior mesenteric artery and decreases mesenteric adipose tissue blood flow. Dig. Dis. Sci. 46, 1217–1222 [DOI] [PubMed] [Google Scholar]
- 69.Shen W., Shen M., Zhao X., Zhu H., Yang Y., Lu S. et al. (2017) Anti-obesity effect of capsaicin in mice fed with high-fat diet is associated with an increase in population of the gut bacterium Akkermansia muciniphila. Front. Microbiol. 8, 272. [DOI] [PMC free article] [PubMed] [Google Scholar]