Abstract
Objective
We sought to identify predictors and moderators of failure to engage (i.e., pretreatment attrition) and dropout in both Internet-based and traditional face-to-face cognitive-behavioral therapy (CBT) for bulimia nervosa. We also sought to determine if Internet-based treatment reduced failure to engage and dropout.
Method
Participants (N = 191, 98% female) were randomized to Internet-based CBT (CBT4BN) or traditional face-to-face group CBT (CBTF2F). Sociodemographics, clinical history, eating disorder severity, comorbid psychopathology, health status and quality of life, personality and temperament, and treatment-related factors were investigated as predictors.
Results
Failure to engage was associated with lower perceived treatment credibility and expectancy (odds ratio [OR] = 0.91, 95% CI: 0.82, 0.97) and body mass index (BMI) (OR = 1.10; 95% CI: 1.03, 1.18). Dropout was predicted by not having a college degree (hazard ratio [HR] = 0.55; 95% CI: 0.37, 0.81), novelty-seeking (HR = 1.02; 95% CI: 1.01, 1.03), previous CBT experience (HR = 1.77; 95% CI: 1.16, 2.71), and randomization to the individual's nonpreferred treatment format (HR = 1.95, 95% CI: 1.28, 2.96).
Discussion
Those most at risk of failure to engage had a higher BMI and perceived treatment as less credible and less likely to succeed. Dropout was associated with less education, higher novelty-seeking, previous CBT experience, and a mismatch between preferred and assigned treatment. Contrary to expectations, Internet-based CBT did not reduce failure to engage or dropout.
Keywords: bulimia nervosa, cognitive behavioral therapy, dropout, failure to engage, randomized controlled trial
Introduction
Evidence for the effectiveness of cognitive-behavioral therapy (CBT) as a front-line treatment for bulimia nervosa (BN) emerged in the 1980s and has consolidated over time.(1, 2) CBT has proven superior to waitlist, placebo, medication, and other forms of psychotherapy, with the exception of interpersonal psychotherapy which was found to be equally effective, but slower in achieving positive effects.(1, 2) CBT is consequently regarded as the treatment of choice for BN.(3) CBT can be delivered effectively in individual and group therapy settings and in self-help formats.(1) More recently, technological innovations have driven the online delivery of treatment to improve accessibility.(4) Studies of traditional CBT for BN report abstinence rates of ∼50% among completers, but lower rates of ∼30% in intent-to-treat analyses.(5) Even though the past 25 years have brought innovation in CBT delivery and accessibility, failure to engage in treatment remains problematic and dropout is unacceptably high.
Failure to engage refers to attrition before treatment has started. (6) In clinical settings and clinical trials 15-20% of BN patients fail to engage in individual or group CBT.(6-8) Some studies report higher failure rates (∼30%) from the point of referral rather than from the point of assessment,(9) but diagnostic status may be unconfirmed at referral. Two studies have examined the characteristics of patients who fail to engage (6, 7) and greater illness severity, clinical history complexity (e.g., greater duration of illness, impulsive behaviors, depression), and some measures of eating pathology, were predictors. On the majority of measures there were no significant differences between those who did and did not engage. Small sample sizes limit generalizability.
Although CBT is the frontline approach for treating BN, dropout attenuates patient outcomes. Dropout is a concern in all treatment modalities for eating disorders (10, 11) and ranges between 20% to 51% in inpatient settings and 29% to 73% in outpatient settings broadly.(10, 12) Some patients with BN may drop out because of symptom improvement(13) but according to long-term prospective studies BN is marked by a relapsing course and symptom persistence.(14) Eating disorder literature, broadly, suggests that premature treatment termination negatively impacts clinical improvement, relapse, and chronicity.(13, 15, 16) Dropout also has uncaptured consequences such as demoralization of therapists, burden on patients' loved ones, longer wait times for patients who desire treatment, and lost clinical time and administrative resources for clinics.
Several studies have considered whether baseline factors predict dropout from traditional CBT. More than fifty predictors across the domains of sociodemographics, clinical history, eating disorder severity, personality and temperament, health status and quality of life, and treatment factors have been examined; but no single factor has been a consistent predictor. (17-23) Mixed support exists for depression, body dissatisfaction, ineffectiveness, maturity fears, interpersonal distrust, and the presence of a comorbid disorder. Given recent extension of CBT into an online format, it is also timely to investigate predictors and moderators of engagement and outcome in this format, as this has not been done previously.
The data for the present study come from a multicenter non-inferiority randomized controlled trial (RCT) of face-to-face CBT (CBTF2F) vs. Internet-based CBT (CBT4BN) which was delivered by a therapist via a “chat” room.(24) The main finding of that trial was that Internet-based CBT was inferior to face-to-face CBT at post-treatment but non-inferior at 1-year follow-up on the primary outcome measure (i.e., abstinence from binge eating and purging), suggesting that Internet-based CBT might be as effective as face-to-face CBT though slower to achieve its effects. One of the hopes for Internet-based CBT was that it would reduce barriers in traveling to treatment and be more likely to keep people in treatment. In the present study, we predicted that Internet-based CBT would reduce failure to engage and treatment dropout relative to face-to-face CBT. We shied away from making hypotheses about predictors of the two outcomes because of inconsistent findings in previous research. Given the barriers to participation in Internet-based CBT are different from face-to-face CBT, we thought the predictors may be different such that moderator effects might also be observed. The tests of moderators were exploratory given the dearth of previous research.
Method
Design and Participants
Participants were involved in an RCT conducted at two sites, University of North Carolina at Chapel Hill (UNC) and Western Psychiatric Institute and Clinic of the University of Pittsburgh (UP) Medical Center. Participants had BN, were 18+ years, English speaking, with reliable and private Internet access. Exclusion criteria were: a medical problem or developmental disability that would interfere with treatment, alcohol or drug dependence within the past three months, severe suicidal ideation, schizophrenia, psychosis, bipolar disorder, or pregnancy. All randomized individuals were included in this study, except three whose participation was terminated (two become pregnant; one lost weight rapidly and became medically unstable) and two who withdrew consent at post-treatment, giving a sample size of 191 (98% females) with 96 in CBTF2F and 95 in CBT4BN. Incentives were used to maximize data collection: $20 was given for completing the post-treatment assessment and $20 for completing the 12-month follow-up assessment.
The study was approved by the institutional review boards at UNC and UP. All participants provided written informed consent.
Procedures
The study design, treatment protocol development, and assessment schedule have been provided in full elsewhere.(24, 25) Assessments were administered at baseline prior to randomization, weekly during treatment, mid-treatment, post-treatment and at 3, 6-, and 12-month follow-up. BN diagnosis was obtained using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). (26) Post-treatment and follow-up assessments were conducted by trained therapists blind to treatment condition.
Treatment
Therapy groups had 3-8 participants and one therapist, and two sessions included a registered dietitian. CBTF2F and CBT4BN used the same CBT treatment manual, which was shown to be effective in a shorter-duration version of treatment. (27).
Patients in CBTF2F met the therapist and group members face-to-face, received a paper copy of the CBT modules, and completed weekly homework worksheets and daily self-monitoring via pen and paper. Patients in CBT4BN met with the therapist and group members in an online chat group. Each patient logged in to the chat group with an anonymous username used to identify them during the session at a pre-determined time with the therapist. The chat “room” was only open for 90-minute periods. All chat communication was through text and did not include video or audio. Participants completed weekly homework worksheets and daily self-monitoring via the CBT4BN website.
Measures
Predictors and moderators
On the basis of previous literature, we explored associations with: sociodemographics, clinical history and BMI, eating disorder severity, comorbid psychopathology, health status and quality of life, personality and temperament, and treatment-related factors.
Sociodemographic factors
These included age, marital status, employment status, number of children, and college education (0=completed, 1=absent). Sex was not included as the sample was predominantly (98%) female.
Clinical history and BMI
Age of BN onset, illness duration, previous psychiatric hospitalization for any diagnosis, and current use of psychiatric medication were collected during the clinical interview. Lifetime psychiatric diagnoses were established with the SCID. (26) Only the overarching categories of depressive disorder and anxiety disorder were sufficiently prevalent to analyze. Disorders were grouped in a manner consistent with their classification in the DSM-5;(28) thus lifetime depressive disorders included major depressive disorder and dysythmic disorder, and lifetime anxiety disorders included social anxiety disorder, specific phobia, panic disorder, and agoraphobia without panic disorder, but excluded obsessive-compulsive disorder and post-traumatic stress disorder. Baseline BMI (kg/m2) was computed from height and weight; height was measured with a stadiometer and weight with a digital scale.
Eating disorder severity
Frequency of binge eating (objective and subjective together) and purging episodes (self-induced vomiting, laxative misuse, diuretic misuse) over the past 28 days were measured with the Eating Disorder Examination (EDE),(29) as was global eating disorder psychopathology. Objective binge episodes involve the consumption of an objectively large amount of food with perceived loss of control, whereas subjective binge episodes involve eating smaller amounts of food with loss of control.
Comorbid psychopathology
Current psychiatric comorbidity was assessed with the SCID; due to prevalence only the major categories of depressive disorder and anxiety disorder were included in analyses. The Beck Depression Inventory (BDI) (30) and Beck Anxiety Inventory (BAI) (31) measured depression and anxiety symptoms.
Health status and quality of life
The Short-Form Health State Classification (SF-6D) (32) and the Eating Disorders Quality of Life Questionnaire (EDQOL) (33) assessed health status and quality of life. The SF-6D is derived from the SF-36 and is a briefer and valid measure which uses a quality-adjusted life years approach to derive a single score.(34) The EDQOL measures the impact of the eating disorder on psychological, physical/cognitive, financial, and work/school functioning.
Personality and temperament
The Temperament and Character Inventory (TCI) harm avoidance, novelty-seeking, self-directedness, reward dependence, persistence, cooperativeness, and self-transcendence subscales were administered(35) and the emotion dysregulation subscale of the Clinical and Research Inventory for Eating Disorders (CR-EAT).(36) The TCI has been translated into other languages and reliability and validity have been shown in many studies and across cultures. The CR-EAT emotion regulation subscale has acceptable test-retest reliability.(36)
Treatment-related factors
Previous CBT experience for any mental health problem was self-reported as yes/no during intake. A web self-efficacy scale (37) measured self-belief in competence using the Internet. Factor analysis has supported the validity of the web self-efficacy measure. (37) The Client Satisfaction Questionnaire (CSQ) based on Borkovec and Nau (38) assessed credibility (how logical the proposed treatment appeared), and expectancy (how confident participants were that treatment would succeed); individuals rated both treatment conditions, but for the current study the score for their allocated treatment was used. One item asked participants to nominate their preferred treatment format; responses were used to create a dummy variable characterizing whether they had been allocated to their nonpreferred treatment (1=nonpreferred, 0=preferred).
Potential moderators were selected a priori from the aforementioned predictors and included employment, number of children, web self-efficacy, and scores on EDE purging, BDI, BAI, EDQOL, TCI self-directedness, CR-EAT emotional dysregulation, CSQ, and treatment preference. Child care and work situations may interfere more with utilization of face-to-face treatment and web self-efficacy may be more relevant to outcomes from Internet-based treatment utilization; other tests were more exploratory in nature.
Cronbach alpha's for measures in the present study were: BDI (0.92), BAI (0.91), EDQOL (0.90), TCI novelty-seeking (0.89), TCI harm avoidance (0.91), TCI self-directedness (0.89), TCI reward dependence (0.88), TCI persistence (0.95), TCI cooperativeness (0.89), TCI self-transcendence (0.89), web self-efficacy (0.84), CR-EAT emotional regulation (0.92), and CSQ (0.76).
Covariates
All analyses adjusted for the blocking factor of treatment site. Treatment site was adjusted for rather than included as a predictor and moderator because it is of limited interest theoretically, and would not yield information relevant to clinical settings outside this study.
Failure to engage and dropout
Failure to engage referred to a failure to attend the first session following assessment completion and randomization. Dropout time was recorded as the session following the last attended session, unless the final session was attended in which case, a subject was censored. For CBT4BN, attendance was defined as showing up during the scheduled time, independent of number of statements or participation minutes.
Statistical Analysis
Prediction of failure to engage was examined using penalized likelihood logistic regression and prediction of dropout was examined with time-to-event analysis with the Cox proportional hazards model. Penalized regression was used because of the relatively low frequency of failure to engage (N = 31). Time-to-event analysis was chosen over logistic regression because it handles censored data and different times of dropout, avoids one having to choose an arbitrary definition of dropout (such as <50% of sessions attended), and is more statistically powerful because it does not limit the outcome to binary completion or dropout at a single time point.
Both analyses involved stepwise forward selection of variables meeting the inclusion criteria of: significance at the 0.15 level in univariable analysis with forced entry of the blocking factor of treatment site and the corresponding main effect terms (treatment condition, predictor) for tests of moderators. Predictors, briefly, will be associated with the response variable irrespective of the treatment, and thus were modeled with a single predictor term. Moderators will have associations that vary in strength and/or direction across treatments, and thus were modeled using treatment condition × predictor interaction terms. The alpha level was 0.05 for the multivariable analysis, and the false discovery rate (FDR) method addressed multiple testing. (39)
Prior to inferential analysis, missing data were imputed using multiple imputation with missingness on study variables of 3.8% (± 3.0%, range = 0%-10.9%) (M ± SD). Continuous variables were mean-centered, or median-centered in the presence of skew, and moderators were dummy coded -1/2 and +1/2 based on recommendations prior to creating interaction terms. In time-to-event models, checks were done to confirm functional form and proportional hazards. Prior to multivariable analysis, significant univariable predictors and moderators were assessed for collinearity. Parameter estimates from the multiple imputation datasets were combined using PROC MIANALYZE in SAS. Analyses were conducted with SAS 9.3.
Results
Descriptive Statistics
Table 1 presents the demographic and clinical characteristics of participants randomized to CBTF2F (N = 96) and CBT4BN (N = 95). Participants were predominantly women who were college-educated with a ten-year history of illness.
Table 1. Descriptive Statistics of Study Variables for Women with Bulimia Nervosa in CBTF2F and CBT4BN.
| Study Variables | CBTF2F (N = 96) | CBT4BN (N = 95) |
|---|---|---|
| Sociodemographics | ||
| Age | 27.44 (8.84) | 28.82 (9.51) |
| Female, % (n) | 98% (94) | 98% (93) |
| White, % (n) | 86% (82) | 85% (81) |
| Married/de facto, % (n) | 22% (21) | 23% (21) |
| Employed, % (n) | 68% (64) | 71% (64) |
| Education, % (n) | ||
| Some high school or less | 0 (0) | 1% (1) |
| GED or high school graduate | 4% (4) | 0% (0) |
| Some college or technical school | 43% (40) | 36% (32) |
| College graduate | 35% (33) | 48% (43) |
| Post graduate degree | 18% (17) | 16% (14) |
| Number of children | 0.38 (1.02) | 0.47 (1.00) |
| Clinical history and BMI | ||
| Age of BN onset (years) | 18.32 (5.46) | 18.64 (5.70) |
| Duration of illness (years) | 9.49 (8.69) | 9.89 (9.03) |
| Previous psychiatric hospitalization, % (n) | 18% (16) | 13% (12) |
| Current psychiatric medication, % (n) | 43% (41) | 46% (44) |
| Lifetime psychiatric disorder, % (n) | ||
| Anorexia nervosa | 28% (27) | 33% (31) |
| Major depressive or dysthymic disorder | 71% (68) | 73% (69) |
| Any anxiety disorder | 15% (14) | 24% (23) |
| Social anxiety disorder | 10% (10) | 9% (9) |
| Panic disorder | 4% (4) | 12% (11) |
| Specific phobia | 3% (3) | 7% (7) |
| Agoraphobia | 1% (1) | 2% (2) |
| Bipolar disorder | 0 (0) | 1% (1) |
| Substance abuse | 10% (10) | 7% (7) |
| Alcohol abuse | 23% (22) | 13% (12) |
| Obsessive-compulsive disorder | 2% (2) | 6% (6) |
| Post-traumatic stress disorder | 12% (12) | 7% (7) |
| BMI | 24.03 (5.32) | 24.03 (5.59) |
| Eating disorder severity | ||
| EDE binge episodes | 25.73 (20.85) | 27.93 (21.91) |
| Objective | 15.61 (16.20) | 16.39 (14.74) |
| Subjective | 10.12 (13.95) | 11.83 (17.86) |
| EDE purging episodes | 32.02 (58.69) | 32.17 (33.94) |
| EDE global | 2.78 (1.17) | 2.91 (0.98) |
| Comorbid psychopathology | ||
| Current psychiatric disorder, % (n) | ||
| Major depressive disorder | 22% (21) | 24% (23) |
| Any anxiety disorder | 24% (23) | 28% (27) |
| Social anxiety disorder | 9% (9) | 6% (6) |
| Panic disorder | 1% (1) | 4% (4) |
| Specific phobia | 3% (3) | 5% (5) |
| Agoraphobia | 1% (1) | 2% (2) |
| Generalized anxiety disorder | 16% (15) | 17% (16) |
| Bipolar disorder | 0 (0) | 0 (0) |
| Substance abuse | 0 (0) | 0 (0) |
| Alcohol abuse | 4% (4) | 4% (4) |
| Obsessive-compulsive disorder | 1% (1) | 3% (3) |
| Post-traumatic stress disorder | 4% (4) | 1% (1) |
| BDI | 20.02 (12.06) | 20.44 (11.03) |
| BAI | 13.46 (9.75) | 14.32 (10.16) |
| Health status and quality of life | ||
| SF-6D | 0.66 (0.09) | 0.66 (0.10) |
| EDQOL | 1.58 (0.55) | 1.65 (0.63) |
| Temperament, character, and personality | ||
| TCI Harm avoidance | 104.25 (19.08) | 106.29 (19.07) |
| TCI Novelty-seeking | 107.47 (17.75) | 106.67 (19.85) |
| TCI Self-directedness | 124.31 (17.57) | 123.23 (20.68) |
| TCI Reward dependence | 105.21 (14.48) | 106.26 (17.26) |
| TCI Persistence | 121.78 (21.00) | 120.28 (23.01) |
| TCI Cooperativeness | 140.24 (16.00) | 140.56 (15.01) |
| TCI Self-transcendence | 63.91 (16.09) | 64.15 (15.81) |
| CR-EAT Emotional dysregulation | 3.48 (1.30) | 3.42 (1.23) |
| Treatment-related factors | ||
| Previous CBT experience, % (n) | 37% (34) | 33% (31) |
| Web self-efficacy | 3.46 (0.58) | 3.50 (0.48) |
| CSQ - credibility and expectancy | 26.45 (4.56) | 24.76 (5.33) |
| Randomization to nonpreferred treatment format, % (n) | 34% (31) | 64% (56) |
Note: Numbers are M (SD) unless otherwise indicated. Statistics are based on available data. BAI = Beck Anxiety Inventory. BDI = Beck Depression Inventory. BMI = body mass index. BN = bulimia nervosa. CBT = cognitive-behavioral therapy. CBTF2F = traditional face-to-face group CBT. CBT4BN = Internet-based group CBT. CR-EAT = Clinical Research Inventory for Eating Disorders. CSQ = Client Satisfaction Questionnaire. EDE = Eating Disorder Examination. EDQOL = Eating Disorders Quality of Life Questionnaire. GED = General Education Development. SF-6D = Short Form Health State Classification. TCI = Temperament and Character Inventory.
Description of Failure to Engage and Dropout
Overall, 16% (31/191) of participants failed to engage in treatment (CBTF2F: 21% [20/96]; CBT4BN: 12% [11/95]). A chi square goodness of fit test showed that failure to engage was not significantly different between the two groups, χ2(1) = 3.00, p = 0.08.
For those who engaged, the average number of treatment sessions attended was 10 (± 4.38, range = 2-16) for CBTF2F and 9 (± 5.25, range = 1-16) for CBT4BN. As shown in Figure 1, dropout appeared linear for both groups. A log-rank test showed that survival times from treatment commencement to dropout were not significantly different between the two groups (χ2[1] = 3.32, p = 0.07).
Figure 1.
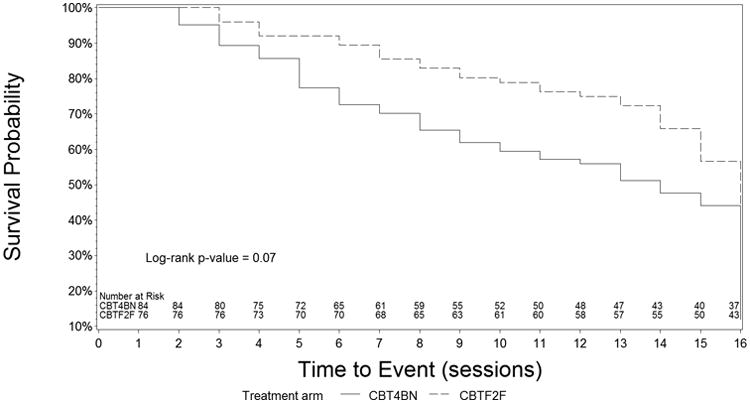
Time to Dropout in CBTF2F and CBT4BN (N = 160). CBTF2F = traditional face-to-face group CBT. CBT4BN = Internet-based group CBT
Predictors of Failure to Engage
The univariable analysis showed three significant predictors at the 0.15 level and no significant moderators (Table 2). Having a greater number of children, a higher BMI, and lower CSQ were associated with failure to engage. In multivariable analysis, only BMI and CSQ remained statistically significant at the 0.05 alpha level. With FDR correction, CSQ (FDR p = 0.01) and BMI (FDR p = 0.01) remained statistically significant.
Table 2. Significant Predictors and Moderators of Failure to Engage in CBTF2F and CBT4BN (N = 191).
| Firth penalized model | Variable | OR | 95% CI | FDR p | |
|---|---|---|---|---|---|
| Univariable | Predictors | Number of children | 1.32† | 0.95, 1.84 | |
| BMI | 1.09* | 1.02, 1.16 | |||
| CSQ - credibility and expectancy | 0.91* | 0.84, 0.98 | |||
| Moderators | - | - | - | ||
| Multivariable | Predictors | BMI | 1.10* | 1.03, 1.18 | 0.01* |
| CSQ - credibility and expectancy | 0.90* | 0.82, 0.97 | 0.01* | ||
| Moderators | - | - | - |
Note:
p < 0.15
p < 0.05
p < 0.01
p < 0.001.
All analyses are adjusted for treatment site. BMI = body mass index. CBTF2F = traditional face-to-face group CBT. CBT4BN = Internet-based group CBT. CSQ = Client Satisfaction Questionnaire.
Predictors of Dropout
The univariable analyses predicting dropout showed several statistically significant predictors at the 0.15 alpha threshold (Table 3). Dropout was associated with lower age, not having a college degree, younger age of onset, higher BMI, previous CBT experience, randomization to nonpreferred treatment, and higher TCI novelty-seeking and self-transcendence. Several moderators were statistically significant: employment, number of children, and purging.
Table 3. Significant Predictors and Moderators of Dropout in CBTF2F and CBT4BN (N = 160).
| Survival model | Variable | HR | 95% CI | FDR p | |
|---|---|---|---|---|---|
| Univariable | Predictors | Age | 0.98* | 0.96, 1.00 | |
| College education | 0.55*** | 0.39, 0.78 | |||
| Age of BN onset | 0.96* | 0.93, 0.99 | |||
| BMI | 1.03† | 0.99, 1.06 | |||
| TCI Novelty-seeking | 1.01** | 1.00, 1.02 | |||
| TCI Self-transcendence | 1.01† | 1.00, 1.02 | |||
| Previous CBT experience | 1.35† | 0.92, 1.97 | |||
| Nonpreferred treatment format | 1.69** | 1.19, 2.40 | |||
| Moderators | Employed | 0.49† | 0.23, 1.03 | ||
| Number of children | 1.40† | 0.95, 2.07 | |||
| Purging | 1.01† | 1.00,1.01 | |||
| Multivariable | Predictors | College education | 0.55** | 0.37, 0.81 | 0.01* |
| BMI | 1.02* | 1.00, 1.08 | 0.07 | ||
| TCI Novelty-seeking | 1.02** | 1.01, 1.03 | 0.01* | ||
| Previous CBT experience | 1.77** | 1.16, 2.71 | 0.02* | ||
| Nonpreferred treatment format | 1.95** | 1.28, 2.96 | 0.01* | ||
| Moderators | Employed | 0.36* | 0.17, 0.80 | 0.02* |
Note:
p < 0.15
p < 0.05
p < 0.01
p < 0.001.
All analyses are adjusted for treatment site. Post hoc probing with a stratified analysis showed that the moderator of employment status was not significantly associated with dropout in either treatment arm (ps > 0.05). BMI = body mass index. CBT = cognitive-behavioral therapy. CBTF2F = traditional face-to-face group CBT. CBT4BN = Internet-based group CBT. BN = bulimia nervosa. TCI = Temperament and Character Inventory.
Significant predictors and moderators were examined together in the multivariable analysis. College degree, BMI, TCI novelty-seeking, previous CBT treatment, and nonpreferred treatment were statistically significant, as well as the employment moderator, at the 0.05 level. With FDR correction, all effects except BMI remained statistically significant. Post hoc probing of the association between dropout and employment stratified by treatment format and adjusting for site and other multivariable predictors showed a non-significant association in both CBTF2F (HR = 1.03, 95% CI: 0.56, 1.20, p = 0.91) and CBT4BN (HR = 1.73, 95% CI: 0.96, 1.20, p = 0.07). We concluded that employment had no moderating effect.
Discussion
In this investigation of predictors and moderators of failure to engage and dropout from face-to-face and Internet-based CBT for BN, failure to engage was predicted by lower credibility and expectancy for treatment and a higher BMI, whereas dropout was predicted by less education, higher novelty-seeking, prior experience of CBT, and randomization to a delivery format that was not the individual's preference. It was envisaged that Internet-based CBT would reduce failure to engage and dropout relative to face-to-face CBT by removing barriers related to attending the clinic; however, contrary to expectations, there were no differences. No moderators differentially predicted failure to engage or dropout among the treatment formats.
Internet-based CBT was expected to reduce barriers to attending traditional treatment at the clinic (e.g., travel, gas money, childcare), and was anticipated to have a positive effect on failure to engage and time to dropout, but this was not confirmed in the present study. Internet-based CBT had similar dropout survival time as face-to-face CBT. To our knowledge this is the only existing study to address this important issue. (4) Prior to randomization, patient's preferences for the two treatment formats were measured, and there was a majority preference for face-to-face therapy. Dropout was predicted by randomization to one's nonpreferred delivery format, which could explain the higher than anticipated dropout in CBT4BN. Reasons for failure to engage and dropout may be different among face-to-face and Internet-based treatment, which may also account for the findings. For instance, a lack of reliable computer and Internet access and suitably quiet surroundings may be barriers to online participation.
Failure to engage occurred among 16% who agreed to participate in the treatment trial, consistent with other documented estimates in eating disorder clinics and clinical trials. (6-8) Previous limited research has suggested that a more severe, complex lifetime and acute illness presentation on certain indices characterizes this subgroup. (6, 7) The present study included the broadest range of predictors to date, examining more participants than the previous studies combined, but results did not support this premise. The mixed findings may be attributable to the preliminary sample in Coker et al. (N = 6), univariable analysis and failure to account for multiple testing in previous studies, study differences in measures, or to other differences in methodology. We found no differences on sociodemographics, clinical characteristics, eating disorder severity, comorbidity, health status and quality of life, and personality and temperament between those who did and did not engage. Two positive associations were observed in our study; in contrast to Waller, (6) we found that a higher BMI predicted failure to engage. Higher BMI could be a marker of clinical severity, weight-related stigma, feeling uncomfortable in group therapy with patients who are on the lower weight spectrum, or could indicate a preference to seek out weight loss treatment rather than a BN intervention. (40) Alternatively, changes in the demographics of individuals with BN presenting for treatment may make higher BMI a more important factor in treatment choice and outcome. (40) We found support for perceived credibility and expectancy for treatment, which has not been measured in previous research.
The success rate of each treatment format could be higher if failure to engage and dropout were prevented. In the trial, based on intent-to-treat methods 21% and 26% in CBTF2F and 14% and 30% in CBT4BN were binge-purge abstinent at post-treatment and 1-year follow-up, respectively.(25) Yet, 16% of the whole sample failed to engage, and of the remainder, dropout was a linear function of time (Figure 1) with an average “dose” of only ∼60% of treatment sessions, which is suboptimal. In the past, low motivation for change has been a popular therapeutic target for enhancing retention in eating disorders, but results have been disappointing. This study imparts fresh knowledge on new therapeutic targets and at-risk characteristics that may be considered for future retention interventions. Regarding education, it is possible that participants without a college degree were students with hectic schedules, or that therapy materials were more attractive or tailored to those with a college degree. In conjunction with the findings of Agras et al., (18) novelty-seeking increased the risk of dropout, which may support earlier targeting of bulimic cognitions among this subgroup given that early focus on eating and meal regularity often intensifies weight and shape concerns. More intensive strategies (i.e., psychoeducation, between-session contact) to guide expectations, support, and mastery during more difficult phases of treatment, may prove helpful. Prior experience of CBT increased the risk of dropout, which may mean these patients commence treatment thinking they have already tried the treatment and thus more readily dropout, or this may be a marker of previous treatment failures. There was empirical support for considering patient preference when treatment options are presented. There was a slight moderator effect, suggesting that those who were employed were better suited to CBTF2F.
This study has several limitations that warrant consideration. There is assessment bias given that we were not able to look at all potential predictors of dropout, only those assessed, and selection bias because we recruited individuals willing to be randomized to either treatment. There may be differences between dropout under trial conditions versus routine care (e.g., differences in motivation, payment, reminders). The way dropout was defined, a person who attended every second session up to the 10th session would be characterized in the same way as a person who attended all 10 sessions then dropped out. A future research question is whether heterogeneity across individuals exists according to attendance pattern. Also, except for Waller's(6) research, studies have not ruled out patients who fail to engage (or dropout) for unavoidable reasons, which would lead to more precise estimates of “preventable” failure to engage, increased statistical power, and less measurement error. Studies that have recorded reasons for dropout have a large amount of missing reports,(18) so this information may be difficult to get. The investigation of process variables could give additional information to formulate clinical strategies to retain patients in treatment. Because of mixed findings in previous literature no specific hypotheses were made regarding predictor variables, and a large number of potential predictors and moderators were examined on an exploratory basis. We therefore suggest caution in accepting positive findings before they are replicated. In addition, CBT4BN represented a complete suite of Internet-based CBT including therapist guided chat sessions, and online materials, self-monitoring, and feedback. Our results may not generalize to less comprehensive Internet-based approaches.
This study provides promising avenues for improving retention in CBT for BN by identifying people at high risk of failure to engage and dropout. Replication of these findings, and formulating and evaluating clinical strategies to enhance retention, are important next steps.
Acknowledgments
This research was supported by the National Institute of Health grant (R01MH080065), the Alexander von Humboldt Stiftung (PIs: Kordy and Bulik), and the Global Foundation for Eating Disorders (PIs: Bulik and Baucom). Benjamin Zimmer was supported by a Fellowship for Postdoctoral Researchers from the German Academic Exchange Service (DAAD). We would like to thank Hans Kordy for his contribution to the project and his thoughtful comments on this manuscript.
Footnotes
Potential Conflict of Interest: Bulik and Peat are Consultants for Shire Pharmaceuticals.
References
- 1.Hay P, Bacaltchuk J, Stefano S, Kashyap P. Psychological treatments for bulimia nervosa and binging. Cochrane Database of Systematic Reviews. 2009;4:CD000562. doi: 10.1002/14651858.CD000562.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hay PP, Claudino AM, Kaio MH. Antidepressants versus psychological treatments and their combination for bulimia nervosa. Cochrane Database of Systematic Reviews. 2001;4 doi: 10.1002/14651858.CD003385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Practice guideline for the treatment of patients with eating disorders. 3rd. American Psychiatric Association; 2006. [DOI] [PubMed] [Google Scholar]
- 4.Aardoom JJ, Dingemans AE, Spinhoven P, Furth EF. Treating eating disorders over the internet: A systematic review and future research directions. International Journal of Eating Disorders. 2013;46(6):539–52. doi: 10.1002/eat.22135. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell JE, Crosby RD, Wonderlich SA, Crow S, Lancaster K, Simonich H, et al. A randomized trial comparing the efficacy of cognitive–behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face. Behaviour research and therapy. 2008;46(5):581–92. doi: 10.1016/j.brat.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waller G. Drop-out and failure to engage in individual outpatient cognitive behavior therapy for bulimic disorders. International Journal of Eating Disorders. 1997;22(1):35–41. doi: 10.1002/(sici)1098-108x(199707)22:1<35::aid-eat4>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 7.Coker S, Vize C, Wade T, Cooper PJ. Patients with bulimia nervosa who fail to engage in cognitive behavior therapy. International Journal of Eating Disorders. 1993;13(1):35–40. doi: 10.1002/1098-108x(199301)13:1<35::aid-eat2260130105>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 8.Chen E, Touyz SW, Beumont PJ, Fairburn CG, Griffiths R, Butow P, et al. Comparison of group and individual cognitive-behavioral therapy for patients with bulimia nervosa. International Journal of Eating Disorders. 2003;33(3):241–54. doi: 10.1002/eat.10137. [DOI] [PubMed] [Google Scholar]
- 9.Burket RC, Hodgin JD. Factors predicting reluctance to seek treatment in patients with eating disorders. Southern medical journal. 1993;86(5):529–32. doi: 10.1097/00007611-199305000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Fassino S, Pierò A, Tomba E, Abbate-Daga G. Factors associated with dropout from treatment for eating disorders: A comprehensive literature review. BMC psychiatry. 2009;9(1):67. doi: 10.1186/1471-244X-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beintner I, Jacobi C, Schmidt UH. Participation and outcome in manualized self-help for bulimia nervosa and binge eating disorder: A systematic review and metaregression analysis. Clinical Psychology Review. 2014;34(2):158–76. doi: 10.1016/j.cpr.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Hatchett GT, Park HL. Comparison of four operational definitions of premature termination. Psychotherapy: Theory, Research, Practice, Training. 2003;40(3):226. [Google Scholar]
- 13.Di Pietro G, Valoroso L, Fichele M, Bruno C, Sorge F. What happens to eating disorder outpatients who withdrew from therapy? Eating and Weight Disorders. 2002;7(4):298–303. doi: 10.1007/BF03324976. [DOI] [PubMed] [Google Scholar]
- 14.Fairburn CG, Stice E, Cooper Z, Doll HA, Norman PA, O'Connor ME. Understanding persistence in bulimia nervosa: A 5-year naturalistic study. Journal of Consulting and Clinical Psychology. 2003;71(1):103. [PubMed] [Google Scholar]
- 15.Björk T, Björck C, Clinton D, Sohlberg S, Norring C. What happened to the ones who dropped out? Outcome in eating disorder patients who complete or prematurely terminate treatment. European eating disorders review. 2009;17(2):109–19. doi: 10.1002/erv.911. [DOI] [PubMed] [Google Scholar]
- 16.Baran SA, Weltzin TE, Kaye WH. Low discharge weight and outcome in anorexia nervosa. American Journal of Psychiatry. 1995;152(7):1070–2. doi: 10.1176/ajp.152.7.1070. [DOI] [PubMed] [Google Scholar]
- 17.Blouin J, Schnarre K, Carter J, Blouin A, Tener L, Zuro C, Barlow J. Factors affecting dropout rate from cognitive-behavioral group treatment for bulimia nervosa. International Journal of Eating Disorders. 1995;17(4):323–9. doi: 10.1002/1098-108x(199505)17:4<323::aid-eat2260170403>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 18.Agras WS, Crow SJ, Halmi KA, Mitchell JE, Wilson GT, Kraemer HC. Outcome predictors for the cognitive behavior treatment of bulimia nervosa: Data from a multisite study. American Journal of Psychiatry. 2000;157(8):1302–8. doi: 10.1176/appi.ajp.157.8.1302. [DOI] [PubMed] [Google Scholar]
- 19.Agüera Z, Riseco N, Jiménez-Murcia S, Islam MA, Granero R, Vicente E, et al. Cognitive behaviour therapy response and dropout rate across purging and nonpurging bulimia nervosa and binge eating disorder: DSM-5 implications. BMC psychiatry. 2013;13:285. doi: 10.1186/1471-244X-13-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Steel Z, Jones J, Adcock S, Clancy R, Bridgford-West L, Austin J. Why the high rate of dropout from individualized cognitive-behavior therapy for bulimia nervosa? International Journal of Eating Disorders. 2000;28(2):209–14. doi: 10.1002/1098-108x(200009)28:2<209::aid-eat10>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 21.Waller G, Gray E, Hinrichsen H, Mountford V, Lawson R, Patient E. Cognitive-behavioral therapy for bulimia nervosa and atypical bulimic nervosa: Effectiveness in clinical settings. International Journal of Eating Disorders. 2014;47(1):13–7. doi: 10.1002/eat.22181. [DOI] [PubMed] [Google Scholar]
- 22.Schnicker K, Hiller W, Legenbauer T. Drop-out and treatment outcome of outpatient cognitive–behavioral therapy for anorexia nervosa and bulimia nervosa. Comprehensive Psychiatry. 2013;54(7):812–23. doi: 10.1016/j.comppsych.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Peñas-Lledó E, Agüera Z, Sánchez I, Gunnard K, Jiménez-Murcia S, Fernández-Aranda F. Differences in cognitive behavioral therapy dropout rates between bulimia nervosa subtypes based on drive for thinness and depression. Psychotherapy and psychosomatics. 2012;82(2):125–6. doi: 10.1159/000339620. [DOI] [PubMed] [Google Scholar]
- 24.Zerwas SC, Watson HJ, Hofmeier SM, Levine MD, Hamer RM, Crosby RD, et al. A randomized controlled trial of online chat and face-to-face group therapy for bulimia nervosa. Psychotherapy and Psychosomatics. doi: 10.1159/000449025. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bulik CM, Marcus MD, Zerwas S, Levine MD, Hofmeier S, Trace SE, et al. CBT4BN versus CBTF2F: Comparison of online versus face-to-face treatment for bulimia nervosa. Contemporary clinical trials. 2012;33(5):1056–64. doi: 10.1016/j.cct.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical interview for DSM-4-TR Axis 1 disorders, research version, patient edition (SCID-1/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 27.Bulik CM, Sullivan PF, Carter F, McIntosh V, Joyce P. The role of exposure with response prevention in the cognitive-behavioural therapy for bulimia nervosa. Psychological Medicine. 1998;28(03):611–23. doi: 10.1017/s0033291798006618. [DOI] [PubMed] [Google Scholar]
- 28.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 29.Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. 12th. New York: Guilford Press; 1993. pp. 317–60. [Google Scholar]
- 30.Beck A, Steer R, Brown G. Manual for Beck Depression Inventory II (BDI-II) San Antonio, TX: Psychology Corporation; 1996. [Google Scholar]
- 31.Borden J, Peterson D, Jackson E. The Beck Anxiety Inventory in nonclinical samples: initial psychometric properties. Journal of Psychopathology and Behavioral Assessment. 1991;13(4):345–56. [Google Scholar]
- 32.Brazier J, Usherwood T, Harper R, Thomas K. Deriving a preference-based single index from the UK SF-36 Health Survey. Journal of clinical epidemiology. 1998;51(11):1115–28. doi: 10.1016/s0895-4356(98)00103-6. [DOI] [PubMed] [Google Scholar]
- 33.Engel SG, Wittrock DA, Crosby RD, Wonderlich SA, Mitchell JE, Kolotkin RL. Development and psychometric validation of an eating disorder-specific health-related quality of life instrument. International Journal of Eating Disorders. 2006;39(1):62–71. doi: 10.1002/eat.20200. [DOI] [PubMed] [Google Scholar]
- 34.Petrou S, Hockley C. An investigation into the empirical validity of the EQ-5D and SF-6D based on hypothetical preferences in a general population. Health economics. 2005;14(11):1169–89. doi: 10.1002/hec.1006. [DOI] [PubMed] [Google Scholar]
- 35.Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD. The Temperament and Character Inventory (TCI): A guide to its development and use. St. Louis, MO: Center for Psychobiology of Personality. Washington University; 1994. [Google Scholar]
- 36.Moessner M, Fassnacht D, Bauer S. Online assessment of eating disorders: The Clinical and Research Inventory for Eating Disorders (CR-EAT) [Google Scholar]
- 37.Anandarajan M, Simmers C, Igbaria M. An exploratory investigation of the antecedents and impact of internet usage: An individual perspective. Behaviour and Information Technology. 2000;19:69–85. [Google Scholar]
- 38.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry. 1972;3(4):257–60. [Google Scholar]
- 39.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the royal statistical society Series B (Methodological) 1995:289–300. [Google Scholar]
- 40.Bulik CM, Marcus MD, Zerwas S, Levine MD, La Via M. The changing “weightscape” of bulimia nervosa. American Journal of Psychiatry. 2012;169(10):1031–6. doi: 10.1176/appi.ajp.2012.12010147. [DOI] [PMC free article] [PubMed] [Google Scholar]


