Abstract
Shared decision-making (SDM) and effective patient-provider communication are key and interrelated elements of patient-centered care that impact health and behavioral health outcomes. Measurement of SDM and communication from the patient’s perspective is necessary in order to ensure that health care systems and individual providers are responsive to patient views. However, there is a void of research addressing the psychometric properties of these measures with diverse patients, including non-English speakers, and in the context of behavioral health encounters. This study evaluated the psychometric properties of two patient-centered outcome measures, the Shared Decision Making Questionnaire-9 (SDM-Q) and the Kim Alliance Scale-Communication Subscale (KAS-CM), in a sample of 239 English and Spanish-speaking behavioral health patients. One dominant factor was found for each scale and this structure was used to examine whether there was measurement invariance across the two language groups. One SDM-Q item was inconsistent with the configural invariance comparison and was removed. The remaining SDM-Q items exhibited strong invariance, meaning that item loadings and item means were similar across the two groups. The KAS-CM items had limited variability, with most respondents indicating high communication levels, and the invariance analysis was done on binary versions of the items. These had metric invariance (loadings the same over groups) but several items violated the strong invariance test. In both groups, the SDM-Q had high internal consistency, whereas the KAS-CM was only adequate. These findings help interpret results for individual patients, taking into account cultural and linguistic differences in how patients perceive SDM and patient-provider communication.
Keywords: patient-provider communication, shared decision making, behavioral health, patient-centered, psychometrics
The Institute of Medicine (America, 2001) asserts that the quality chasm in healthcare services could be closed if providers sought the patient’s perspective about their illness, shared power and responsibility and improved their communication. Such shared decision making (SDM) and enhanced communication can improve the quality of behavioral health care (Patel, Bakken, & Ruland, 2008; Wills & Holmes-Rovner, 2006). SDM is “a form of patient-provider communication where both parties bring expertise to the process and work in partnership to make a decision” (Duncan, Best, & Hagen, 2010). SDM allows patients to report the “lived experience of their disorder” and the provider to bring to bear expertise about the “science informed processes of medical diagnosis and treatment” (Patel et al., 2008). Previous research shows that SDM augments patient satisfaction and positively corresponds with receipt of quality behavioral care (Swanson, Bastani, Rubenstein, Meredith, & Ford, 2007).
Nevertheless, a major obstacle for patients of color is that providers rarely receive training in how to motivate minority patients to voice their treatment concerns or preferences, nor engage them in the care-related decisions. Providers display fewer patient-centered behaviors (Cooper et al., 2003), are less receptive to question asking, and tend to demonstrate greater verbal dominance (Cooper et al., 2012) with minorities than with White patients. These actions often result in misunderstandings in communication, inadequate services, and failed treatment alliances (Kirmayer, Groleau, Guzder, Blake, & Jarvis, 2014). Minority patients may infer prejudice or perceive a negative attitude from their provider, thus reducing the likelihood that they perceive receiving quality care (Balsa & McGuire, 2003).
Language barriers can also be detrimental to patient-provider communication (Gilmer & Kronick, 2009); patients who do not speak the same language as their providers report worse outcomes (Pippins, Alegría, & Haas, 2007) and higher dropout rates (DuBard & Gizlice, 2008). It is fundamental that there be an understanding within patient-centered care to ensure that the patient can be actively engaged in health care decision making (Barry & Edgman-Levitan, 2012). Measuring shared decision making and communication between patients and providers requires consideration of three perspectives: the patient, the provider and an unbiased outside observer who simply codes the verbal and non-verbal behaviors. Special attention is needed when developing patient-reported measures and assessing patients’ perspectives, because patients might not understand the intent of questions about shared decision making, particularly if they have not been exposed to them, and might be reluctant to appear critical of their providers. Moreover, the psychometrics of measures need to be re-evaluated whenever new patient groups are studied, new languages are used in the assessment, or new clinical contexts are examined. In other words, a measure that is reliable and valid for measuring a patient-centered outcome for English-speaking patients may not be appropriate with Spanish-speaking patients (Mead & Bower, 2000). Yet there has been little research assessing the psychometric properties of patient-centered measures in behavioral health, especially among non-English speaking patients. This study addresses these two gaps in the literature. Using two measures to evaluate patient-centered outcomes, level of shared decision making (SDM) and quality of patient-provider-communication (KAS-CM), we assess the psychometric properties of these measures among English and Spanish-speaking patients receiving behavioral health treatment.
Shared Decision Making
One of the recent criticisms in the way that behavioral health care providers practice is their lack of shared-decision making (SDM) between patients and providers (Patel et al., 2008). There is some evidence of discomfort expressed by minority patients and providers regarding SDM and race due partly to the power that inherently exists in a patient-provider relationship (Peek et al., 2009). Providers are perceived to hold immense power, authority, and knowledge over their patients. This unequal distribution of power may be exacerbated by societal and racial hierarchies, especially between African-American patients and white providers (Peek et al., 2009). However, there is less research regarding how minority status might influence SDM in behavioral healthcare. One reason cited as the cause for an inadequate usage of SDM in behavioral healthcare settings has been the inability of patients to engage when suffering from severe behavioral health conditions such as schizophrenia (Hamann, Leucht, & Kissling, 2003; Hamann et al., 2009). Studies have shown that some patients with these disorders often report being pressured by their providers to agree to certain treatment recommendations without sufficient involvement in the decision (Quirk, Chaplin, Lelliott, & Seale, 2012). As a consequence of the authority and power that behavioral healthcare providers hold in these interactions, increasing attention has been given to patients with behavioral health conditions to help them better navigate and advocate for themselves during SDM interactions with their providers (Polo, Alegría, & Sirkin, 2012). Patients with behavioral health conditions have been noted to want greater access to information on diagnoses, symptoms, medications, and clinician’s rationale for treatment decisions (Patel et al., 2008). In a recent study involving patients with a variety of behavioral health disorders ranging from schizophrenia to depression, focus groups of providers and patients noted that patients’ openness with providers combined with active provider involvement during consultation sessions provided a safer and more comfortable environment that facilitated SDM (Hamann et al., 2015).
Patient-Provider Communication
Patient-provider communication is a key element impacting the outcomes of clinical care. Good communication between patients and providers has been associated with improved health outcomes (Stewart, 1995) and increased patient satisfaction (Clever, Jin, Levinson, & Meltzer, 2008). One meta-analysis found a 19% higher risk of non-adherence when providers communicated poorly, and indicated that physician communication training resulted in 1.62 times greater increase in the odds of patient adherence when compared to no physician training (Zolnierek & DiMatteo, 2009). However, fostering open communication between patients and providers has historically been a challenge. Patients tend not to state their concerns or ask necessary questions during medical visits (Beisecker & Beisecker, 1990; Korsch, Gozzi, & Francis, 1968; Roter et al., 1997). Minority patients in particular are less likely to engage in collaborative communication with providers (Alegría et al., 2008; Johnson, Roter, Powe, & Cooper, 2004) and to report lacking needed information about treatment (Levinson, Stiles, Inui, & Engle, 1993; Rooks, Wiltshire, Elder, BeLue, & Gary, 2012). Furthermore, once patients are trained to more actively engage in the clinical encounter, providers are not necessarily receptive to improving their own communication (Alegría et al., 2008). Providers have been found to be more verbally dominant and less patient-centered with African-American patients, with one study finding that physicians talked 43% more than African-American patients during the clinical encounter as compared to only 24% more than White patients (Johnson et al., 2004). Studies of Latino patients have found that a perception of the provider as an authority figure leads to less comfort taking an active role in the encounter and less likelihood the patient will engage in collaborative communication with a provider (Cortes, Mulvaney-Day, Fortuna, Reinfeld, & Alegría, 2008). Communication practices and perceptions on the part of patients ultimately influence the interpersonal dynamic of patient-provider encounters.
Poor functional health literacy has also been found to impact oral communication between patients and providers. English and Spanish-speaking patients with diabetes with poor functional health literacy reported significantly worse communication than those with adequate functional health literacy, particularly in the areas of clarity of the discussion, explanation of health condition, and explanation of processes of care (Schillinger, Bindman, Wang, Stewart, & Piette, 2004). Thus, the experience of patient-provider communication encompasses both functional (e.g., provision of key information) and affective (e.g., rapport between provider and patient) aspects of the encounter. Patient-provider communication is posited to impact health outcomes indirectly via its influence on patient and provider behaviors that directly impact health outcomes, such as identifying the correct diagnosis and treatment plan and increasing patient commitment to treatment (Street, Makoul, Arora, & Epstein, 2009), and can be considered a mechanism through which shared decision-making takes place.
Measures
The SDM-Q
The SDM-Q (also referred to as SDM-Q-9 in prior studies) was developed as a brief version of a longer questionnaire (Simon et al., 2006) The SDM-Q evaluates patient-reported SDM (Kriston et al., 2010) from a patient-provider visit based on the patient’s perception of nine steps deemed essential to SDM in the clinical encounter: disclosing that a decision needs to be made, establishing the equality of both parties, presenting treatment options, informing on benefits and risks of treatment, investigating patient’s understanding and expectations, identifying both parties’ preferences, negotiating, reaching a shared decision, and arrangement of follow-up. Representative items include, My provider wanted to know exactly how I want to be involved in making the decision. The nine-items are rated on six point scale from “0: completely disagree” to “5: completely agree.” The sum of the rating ranges between 0 and 45, but this is conventionally transformed to a scale that ranges from 0 to 100, where 0 indicates the lowest level and 100 the highest.
The psychometrics of the SDM-Q have been studied using a sample of German patients who reported on their interaction with primary care providers (Kriston et al., 2010). The scale had a Cronbach’s alpha of .98 in a sample used to develop the measure and an alpha of .94 in a separate cross-validation sample of German primary care patients. A factor analysis was conducted and a one-factor solution was found. The scale was translated into English and then was administered to a national U.S. sample of adults ages 21–70, who reported about decision making with their medical providers. Again Cronbach’s alpha was .94 (Glass et al., 2012). The measure has also been studied in Spanish and Dutch primary care samples (De Las Cuevas et al., 2014; Rodenburg-Vandenbussche et al., 2015). To our knowledge, the psychometrics of the scale have not been studied for patients who see a behavioral health provider.
The KAS Communication Subscale (KAS-CM)
The Kim Alliance Scale (KAS) (Kim, Boren, & Solen, 2001) was developed to measure therapeutic alliance between patient and provider from the patient’s perspective. It includes four subscales designed to measure aspects of alliance: 1) communication, 2) collaboration, 3) integration (equalizing power differential between provider and client), and 4) empowerment (Kim, Boren, & Solem, 2001). In this report we focus on the communication subscale, the KAS-CM, which measures communication from the perspective of the patient. The KAS-CM is intended to measure both instrumental and affective attributes of the patient-provider encounter such as bonding/rapport, provision of information, and expression of concerns. Sample items include I have a good rapport with my provider, I feel my provider gives me enough information, and I can express negative feelings freely. The responses to this 11-item measure are provided on a 4-point Likert scale ranging from “1: never” to “4: always,” with higher scores indicating higher quality of communication.
The KAS, including KAS-CM, was developed by nurse researchers by developing and rating items, assembling them into a scale based on conceptual consistency with the literature, and rating the items for content validity (Kim et al., 2001). The resulting scale was then validated using a convenience sample of 68 nurses (68% Caucasian, 88% female, and 67% with a master’s degree or above) who reported having had encounters as a patient in the prior two years. A factor analysis was conducted in which the initial factor in an unrotated factor solution was examined and items loading at .40 or above were retained within each factor. This resulted in a 30-item KAS (α = 0.94) which included an 11-item communication subscale (α = 0.87) with item-total correlations ranging from 0.38 to 0.73. The KAS subscales had high positive correlations with each other (r ranging from 0.74 to 0.86, p<.01). A later validation of the KAS used a 16-item revised version, the KAS-R, with only four of the original KAS communication items included (Kim, Kim, & Boren, 2008). To our knowledge, further psychometric analyses of the KAS or KAS subscales have not been conducted and the scale’s properties have not been investigated among behavioral health patients.
Methods
Study Patients and Setting
We recruited 351 patients from September 2013 through September 2015 through direct contact in waiting rooms at nine community outpatient behavioral health clinics in Massachusetts. Five clinics are a part of a public safety-net hospital system, two clinics are a part of private hospital system, and the remaining two clinics are a part of private, non-profit community health centers. These clinics generally serve a high proportion of low-income minority patients. Clinics offered individual and group therapy for a range of mental health and substance abuse issues. Behavioral health services offered in the clinics varied, but included psychotherapy, cognitive behavioral therapy, psychiatric medication management, substance abuse treatment, and case management. The study was presented to patients as helping them to ask questions and improve communication between the patient and their provider. Eligible patients were between the ages of 18 and 80, spoke English, Spanish or Mandarin, and were enrolled in individual behavioral health care treatment (e.g., psychotherapy or psychopharmacology). Exclusion criteria for patients included screening positive for mania, psychosis, or active suicidality. Patients over the age of 65 were assessed with a brief cognitive function screen and excluded if cognitive impairment was indicated. Based on these criteria and after providing written consent, 271 eligible patients were enrolled in the study. The sample used in this paper includes 160 English-speaking patients and 79 Spanish-speaking patients who enrolled in the study and completed the questionnaire, for a total of 239 patients in the study sample.
Any provider delivering behavioral health services (e.g., psychotherapy, psychopharmacology, and counseling) at participating clinics, with a minimum caseload of 6–8 patients, was eligible to participate in the study. Providers were recruited through presentations of the study at clinics by project staff. Forty-six providers agreed to participate. The study was approved by the Institutional Review Board of the Cambridge Health Alliance.
Research Procedures
Bilingual research assistants in each clinic approached patients prior to their appointments with their behavioral health providers and invited them to participate in the study in their preferred language. Since the screening tool included a suicidality assessment, patients provided written consent (including language about safety protocols) prior to being screened. Ineligible patients were compensated $10 for their time. Eligible participants who consented to participate in the study completed a 1–1.5 hour research interview in which they provided demographic information and completed self-report measures on their satisfaction with care, decision-making strategies, and general psychosocial well-being. Provider participants also provided written consent, and completed a 45-minute self-report assessment on corresponding measures. All interviews were audio-recorded. Patients received a $25 gift card for either a grocery store or discount retailer as compensation for their time. Providers received a $50 general gift card as compensation.
Process of Translation of Instruments
The Spanish translation of the patient SDM-Q measure was performed by De Las Cuevas and colleagues (2014), who translated the measure to Spanish from German using the 5-step methodology of cross-cultural adaptation of self-reported measures (Beaton, Bombardier, Guillemin, & Ferraz, 2000). This process includes having two independent translators, both competent in German and Spanish, translate the questionnaire from German into Spanish and then back-translated. This process also includes assessing the translated questionnaire for cultural appropriateness, content validity testing, and equivalence testing.
The English version of the KAS-CM used in this study was translated to Spanish and back-translated into English by trained Spanish-speaking research assistants and the study’s PI using the Matias-Carrelo et al. process (2003) to achieve semantic, construct, and technical equivalence. The Spanish translation was reviewed by the PI and team to ensure that the translation maintained a focus on the constructs of the English measure. The team reviewed the content equivalence of translated items to ensure they remained relevant to Spanish speakers. The Spanish translations were also pilot tested with Spanish-speaking behavioral health patients to confirm whether the translations were understood by the population with whom the measure would be used. After pilot-testing with Spanish-speaking patients, the PI and team simplified the translations in order to meet the literacy level of patients.
Study Design
Data for the current study came from an ongoing study (NCT01947283) assessing the effectiveness of psychoeducational interventions for patients and providers on question-asking and shared decision making in treatment.
All of the providers participating in the study completed the research interview in English. For the purposes of this paper, we excluded the Mandarin patient sample due to the small number of participants available for psychometric testing of the measures. Information regarding the Mandarin sample is available from the authors upon request.
Statistical Analysis
We describe sociodemographics (age, gender, education, socioeconomic status, and country of origin) for the full sample of patients and providers and for two patient subgroups, disaggregated by the language version of the measures (English or Spanish). We also provide descriptive statistics on household income, type of behavioral health services received in the past, and the average length of time the patient has seen their behavioral health provider for the patient sample only. We next report statistics on the distributions of the items in the SDM-Q and KAS-CM in each scale in the combined sample, and each language sample separately.
Our psychometric analysis followed the procedure outlined by (Gregorich, 2006), which focuses on the question of whether there is measurement invariance across English and Spanish samples. Measurement invariance, or equivalence, of a measure indicates that the same construct is being measured across different groups. Systematic testing of measurement invariance across at least two distinct groups (in this case, two language groups) allows for analysis of whether the measure and its component items measure the same construct in the two groups. When measurement invariance is established, differences in scores between the two groups can be interpreted as reflecting actual differences in the construct being measured (rather than reflecting bias due to language, cultural, and other group differences). We utilized confirmatory factor analysis to systematically assess configural invariance (the nature of the factor structure in each group), metric invariance (the equivalence of factor loadings after allowing latent variable variances to vary), strong invariance (the equivalence of item means, after allowing latent variable means to vary) and strict invariance (the equivalence of the item error variation). If strong or strict invariance is supported, it is appropriate to compare groups with the simple summed item responses. We carried out these analyses sequentially, first for SDM-Q and then for KAS-CM.
Mplus Version 7.4 (Muthén & Muthén, 1998–2015) was used to fit all the measurement invariance models with the two-group approach. When it was appropriate to treat the item responses as continuous variables, we used a robust maximum likelihood estimation method (MLMV) and when it was necessary to treat the item responses as categorical, we fit a probit item response model with weighted least squares (WLSMV). Mplus was used to make adjustments to the chi-square difference tests that were used to compare the nested measurement equivalence models. The robust estimation methods required listwise deletion of missing data (SDM) or pairwise deletion (KAS-CM), but the amount of missing data was minimal. Missing data in SDM-Q were less than 9% and less than 2% in KAS-CM. Data were sometimes missing due to patients correctly skipping a question because it was not applicable to them or because the patient felt that a particular item in the measure was not applicable to them.1 When we computed simple summed scale scores for the correlational analysis, we prorated the scaled measure of SDM-Q and KAS-CM, which essentially imputes the missing item to have the mean of the available items within the scale. When more than two items in a scale were missing, we assigned a missing value to the scale score. This entailed dropping 2 cases from the SDM-Q correlational analysis.
Results
Table 1 shows the demographic characteristics of the English and Spanish speaking patients, along with tests of group differences. The average length of time a patient saw their behavioral health provider (i.e., the provider who participated in the study) was 13 months. A little over 80 percent of the sample of patients lived near or below the U.S. poverty level. Roughly 76 percent of patients were hospitalized in the past for behavioral health issues and roughly 76 percent had past emergency room use for behavioral health issues. About 23 percent of patients used a prescription drug in the past for behavioral health issues. Compared to the English-speaking patients in the sample, there were more participants in the Spanish-speaking sample who were female, between ages 50–64, who had less education, and who were not employed. The majority of Spanish-speaking participants reported being from Central and South America, followed by those who reported being from the Caribbean islands. Table 2 summarizes the sociodemographic information of the providers in the study, who were mostly non-Latino White, between ages 18–34, and female. The providers were mostly psychologists, psychiatrist, and social workers.
Table 1.
Demographic Characteristics of Patients for the Overall Sample and Two Language Groups
| Variable | Total Sample (n=239) | English (n=160) | Spanish (n=79) | p value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Age | |||||||
| 18–34 | 69 | 28.99 | 54 | 33.96 | 15 | 18.99 | 0.124 |
| 35–49 | 71 | 29.83 | 44 | 27.67 | 27 | 34.18 | |
| 50–64 | 79 | 33.19 | 49 | 30.82 | 30 | 37.97 | |
| 65+ | 19 | 7.98 | 12 | 7.55 | 7 | 8.86 | |
| Gender | |||||||
| Male | 76 | 31.8 | 61 | 38.13 | 15 | 18.99 | 0.003 |
| Female | 163 | 68.2 | 99 | 61.88 | 64 | 81.01 | |
| Highest Education Level Completed | |||||||
| 0–6th grade | 21 | 8.79 | 1 | 0.63 | 20 | 25.32 | <0.001*** |
| 7–11 grade | 41 | 17.15 | 11 | 6.88 | 30 | 37.97 | |
| 12 grade | 36 | 15.06 | 26 | 16.25 | 10 | 12.66 | |
| >12 grade | 140 | 59 | 121 | 76.25 | 19 | 24.05 | |
| Employment Status | |||||||
| Employed | 113 | 47.48 | 87 | 54.72 | 26 | 32.91 | <0.01** |
| Not Employed | 125 | 52.52 | 72 | 45.28 | 53 | 67.09 | |
| Country of Origins | |||||||
| North America | 104 | 50.24 | 102 | 79.07 | 2 | 2.56 | <0.001*** |
| Central and South America | 64 | 30.92 | 14 | 10.85 | 50 | 64.1 | |
| Africa / Europe | 7 | 3.38 | 7 | 5.43 | 0 | 0 | |
| Asia / Pacific Islands | 3 | 1.45 | 3 | 2.33 | 0 | 0 | |
| Caribbean islands | 29 | 14.01 | 3 | 2.33 | 26 | 33.33 | |
| Household Income | |||||||
| <12K | 194 | 81.17 | 134 | 83.75 | 60 | 75.95 | 0.147 |
| >=12K | 45 | 18.83 | 26 | 16.25 | 19 | 24.05 | |
| Any past hospitalization for behavioral health issues | |||||||
| No | 56 | 23.43 | 30 | 18.75 | 26 | 32.91 | <0.05* |
| Yes | 183 | 76.57 | 130 | 81.25 | 53 | 67.09 | |
| Any past ER use for behavioral health issues | |||||||
| No | 57 | 23.85 | 40 | 25.00 | 17 | 21.52 | 0.552 |
| Yes | 182 | 76.15 | 120 | 75.00 | 62 | 78.48 | |
| Any prescription drugs for behavioral health issues | |||||||
| No | 185 | 77.41 | 125 | 78.13 | 60 | 75.95 | 0.705 |
| Yes | 54 | 22.59 | 35 | 21.88 | 19 | 24.05 | |
|
| |||||||
| mean | sd | mean | sd | mean | sd | p Value | |
|
| |||||||
| Number of months the patient has seen their behavioral health provider | 13.18 | (22.56) | 14.89 | (24.75) | 9.66 | (16.83) | 0.097 |
Table 2.
Demographic Characteristics of Provider Participants
| Variable | Total Sample (n=46) | |
|---|---|---|
|
| ||
| n | % | |
| Age | ||
| 18–34 | 18 | 39.13 |
| 35–49 | 12 | 26.09 |
| 50–64 | 11 | 23.91 |
| 65+ | 5 | 17.39 |
| Gender | ||
| Male | 11 | 23.91 |
| Female | 35 | 76.09 |
| Race | ||
| Non-Latino White | 33 | 71.74 |
| Latino | 4 | 8.70 |
| Non-Latino Black | 1 | 2.17 |
| Asian | 8 | 17.39 |
| Country of Origin | ||
| North America | 25 | 54.35 |
| Central/South America | 9 | 19.57 |
| Africa / Europe | 3 | 6.52 |
| Asia / Pacific Islands | 9 | 19.56 |
Table 3 shows the means, standard deviations, skewness/kurtosis, and minimum and maximum values for the SDM-Q and KAS-CM items in the total sample and each of two subgroups. For all items pertaining to SDM, participants in the Spanish speaking sample reported higher levels of shared-decision making than the English speaking sample (Spanish M: 82.0, English M: 72.7 ; p<0.001). The distributions of the responses generally had negative skew, with the majority of patients reporting 4 or 5 to the items. Patients reported the highest ratings for SDM 5 (My provider helped me understand all the information) (M: 4.28) and the lowest ratings for SDM 1 (My provider made clear that a decision needs to be made) (M: 3.23).
Table 3.
Descriptive Statistics of SDM-Q and KAS-CM Item Scores for the Overall Sample and Two Language Groups
| Variable | Total Sample (n=239) | English (n=160) | Spanish (n=79) | p-value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | Skew | Kurtosis | Range | M | SD | Skew | Kurtosis | M | SD | Skew | Kurtosis | ||
| SDM | ||||||||||||||
| SDM1 | 3.3 | 1.6 | −0.8 | 2.7 | 0–5 | 3.2 | 1.6 | −0.7 | 2.5 | 3.7 | 1.6 | −1.2 | 3.3 | |
| SDM2 | 3.9 | 1.4 | −1.5 | 4.7 | 0–5 | 3.8 | 1.4 | −1.4 | 4.2 | 4.0 | 1.3 | −1.9 | 6.3 | |
| SDM3 | 3.7 | 1.5 | −1.2 | 3.6 | 0–5 | 3.6 | 1.5 | −1.1 | 3.2 | 4.0 | 1.4 | −1.7 | 5.0 | |
| SDM4 | 3.6 | 1.5 | −1.1 | 3.2 | 0–5 | 3.4 | 1.6 | −0.8 | 2.5 | 4.1 | 1.2 | −1.9 | 6.9 | |
| SDM5 | 4.3 | 1.1 | −1.9 | 6.9 | 0–5 | 4.1 | 1.2 | −1.6 | 5.5 | 4.6 | 0.8 | −2.9 | 14.2 | |
| SDM6 | 3.7 | 1.6 | −1.3 | 3.6 | 0–5 | 3.6 | 1.6 | −1.1 | 3.1 | 4.0 | 1.4 | −1.7 | 5.5 | |
| SDM7 | 3.7 | 1.5 | −1.2 | 3.4 | 0–5 | 3.4 | 1.6 | −0.8 | 2.6 | 4.2 | 1.1 | −2.2 | 8.5 | |
| SDM8 | 3.9 | 1.5 | −1.4 | 4.1 | 0–5 | 3.6 | 1.5 | −1.1 | 3.2 | 4.3 | 1.1 | −2.4 | 8.8 | |
| SDM9 | 4.2 | 1.1 | −1.9 | 7.0 | 0–5 | 4.1 | 1.2 | −1.7 | 5.9 | 4.4 | 0.9 | −2.4 | 11.1 | |
| SDM total score | 76.0 | 20.7 | −1.0 | 3.7 | 8.9–100 | 72.7 | 21.4 | −0.8 | 3.1 | 82.8 | 17.3 | −1.7 | 6.6 | <0.001 |
| KAS-CM | ||||||||||||||
| KAS-CM1 | 4.0 | 0.2 | −8.6 | 91.3 | 1–4 | 4.0 | 0.1 | −8.8 | 78.0 | 3.9 | 0.4 | −5.6 | 38.5 | |
| KAS-CM2 | 3.9 | 0.3 | −5.5 | 34.7 | 2–4 | 3.9 | 0.3 | −5.0 | 29.4 | 4.0 | 0.3 | −6.9 | 51.9 | |
| KAS-CM3† | 3.9 | 0.4 | −4.5 | 27.0 | 1–4 | 3.9 | 0.3 | −2.7 | 8.0 | 3.9 | 0.5 | −4.3 | 21.2 | |
| KAS-CM4 | 3.2 | 1.0 | −1.0 | 3.0 | 1–4 | 2.9 | 1.0 | −0.6 | 2.4 | 3.8 | 0.6 | −4.1 | 19.4 | |
| KAS-CM5 | 3.8 | 0.5 | −3.7 | 17.9 | 1–4 | 3.8 | 0.6 | −3.3 | 14.4 | 3.9 | 0.3 | −4.4 | 23.1 | |
| KAS-CM6 | 3.9 | 0.3 | −5.5 | 42.3 | 1–4 | 3.9 | 0.3 | −5.4 | 39.6 | 3.9 | 0.2 | −4.1 | 17.8 | |
| KAS-CM7 | 3.8 | 0.4 | −2.1 | 6.7 | 2–4 | 3.7 | 0.5 | −1.6 | 4.6 | 3.9 | 0.3 | −4.4 | 23.1 | |
| KAS-CM8† | 3.9 | 0.5 | −5.0 | 28.3 | 1–4 | 3.9 | 0.3 | −6.7 | 49.2 | 3.8 | 0.6 | −3.5 | 14.6 | |
| KAS-CM9 | 3.9 | 0.4 | −4.5 | 26.3 | 1–4 | 3.9 | 0.3 | −4.0 | 19.4 | 3.9 | 0.5 | −4.0 | 19.2 | |
| KAS-CM10 | 3.8 | 0.5 | −3.0 | 13.3 | 1–4 | 3.8 | 0.5 | −2.2 | 7.3 | 3.8 | 0.6 | −3.9 | 18.0 | |
| KAS-CM11 | 3.8 | 0.4 | −2.8 | 12.7 | 1–4 | 3.8 | 0.5 | −2.4 | 10.4 | 3.9 | 0.3 | −4.4 | 23.1 | |
| KAS-CM total score | 42.0 | 2.4 | −2.4 | 12.3 | 27–44 | 41.7 | 2.3 | −2.5 | 13.9 | 42.8 | 2.3 | −2.9 | 13.2 | <0.001 |
| KAS-CM total score - binary | 9.55 | 1.66 | 2–11 | 9.22 | 1.6 | 10.22 | 1.57 | |||||||
Note. The KAS factor analysis was conducted using the recoded binary responses by fitting a binary item factor model with a probit link function.
These items are reverse coded.
The distributions of the KAS-CM were even more skewed than the SDM-Q items. Although patients could use a scale ranging from 1 to 4, virtually all the means were larger than 3, and six of the 11 items had means greater than 3.9 in both English and Spanish samples. This pattern suggests that the primary decision that patients made regarding these items was whether to report a perfect communication score of 4 or a score that was less than perfect.2 The English speaking sample reported slightly lower ratings (relative to the Spanish speaking) of patient-provider communication on two items: KAS-CM 4 (My provider spends lots of time educating me) and KAS-CM 7 (I feel my provider gives me enough information). The mean KAS-CM score was significantly lower for the English-speaking sample (Spanish M: 42.8, English M: 41.7, p<0.001).
Measurement Invariance: SDM
We tested measurement invariance levels for SDM-Q by first assessing configural invariance across the English and Spanish samples, using exploratory factor analysis (EFA) and then we tested metric, strong and strict invariance models using confirmatory factor analysis (CFA). The initial one factor EFA revealed that the first item (My provider made it clear that a decision needed to be made) was unrelated to the general SDM dimension in the Spanish sample. This problem had also been reported in a different Spanish-speaking sample (De Las Cuevas et al., 2014), and so we removed this item to enable further tests of configural invariance.
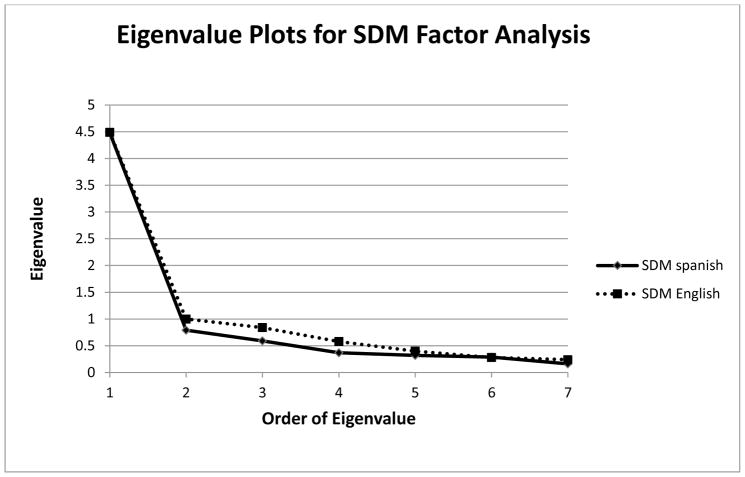
After dropping the first SDM item, the pattern of eigenvalues (“scree plot”) in both English and Spanish samples suggested one factor, as shown in Figure 1. All eight items had standardized loadings of .45 to .90 in magnitude in both samples. The fit of the one factor model, however, was not good according to conventional standards for formal fit statistics (statistics for English and Spanish samples are respectively, RMSEA bounds (0.15 to 0.21; 0.15 to 0.23), TLI (0.79; 0.86), CFI (0.85, 0.91). Hu and Bentler (1999) recommend RMSEA values less than .06 and TLI and CFI values greater than .95. We explored two and three factor models, and found that these had better fit statistics, but there was no coherent interpretation of the factors. For example, the two-factor solution resulted in only one item (SDM 9: My provider and I reached an agreement on how to proceed) loading onto a second factor. We also explored one factor models with correlated residuals, and were able to improve the fit, although the values continued to be worse than the recommended values (for the full sample, RMSEA bounds 0.04 to 0.12, TLI 0.88, CFI 0.93). When criteria for model selection disagree, Marsh, Hau, and Wen (2004) and Gregorich (2006) recommend taking theoretical and substantive concerns into account. For this reason, we continued the investigation of item invariance in the SDM with a one factor model, but we carried out sensitivity analyses with the one factor model with correlated residuals and found similar results. The one factor model allows us to adjust, at least approximately, for latent differences in English-speaking participants and Spanish-speaking participants when considering the item loadings, intercepts and residual variances. The one-factor solution was also consistent with prior research indicating that the SDM-Q scale represents a single latent construct of shared decision-making.
Figure 1.
Eigenvalue Plots for SDM Factor Analysis (Scree Plot)
We report the standardized factor loadings from one-factor models that were fit using robust maximum likelihood estimation in Table 4 (combined sample, English-language sample, and Spanish-language sample). For SDM-Q, the loadings ranged from .88 to .52, with a median loading of .72. The item with the highest loading was My provider and I thoroughly weighed the different treatment options, which is a canonical expression of shared decision making. The lowest loading item was the second, which was My provider wanted to know exactly how I want to be involved in making the decision. This pattern was seen in both the English and Spanish speaking samples.
Table 4.
Standardized Factor Loadings for Single Factor Models of SDM-Q and KAS-CM for 2 Language Groups
| Item | Total Sample (n=239) | English (n=160) | Spanish (n=79) |
|---|---|---|---|
| Factor loading | Factor loading | Factor loading | |
| SDM (with SDM1 excluded) | |||
| SDM2 | 0.52 | 0.51 | 0.48 |
| SDM3 | 0.60 | 0.58 | 0.56 |
| SDM4 | 0.82 | 0.80 | 0.80 |
| SDM5 | 0.64 | 0.67 | 0.70 |
| SDM6 | 0.81 | 0.80 | 0.82 |
| SDM7 | 0.88 | 0.87 | 0.89 |
| SDM8 | 0.80 | 0.77 | 0.89 |
| SDM9 | 0.60 | 0.55 | 0.58 |
| KAS-CM | |||
| KAS-CM1 | 0.47 | 0.54 | 0.73 |
| KAS-CM2 | 0.72 | 0.67 | 0.83 |
| KAS-CM3† | 0.40 | 0.45 | 0.65 |
| KAS-CM4 | 0.41 | 0.25 | 0.40 |
| KAS-CM5 | 0.72 | 0.77 | 0.90 |
| KAS-CM6 | 0.94 | 0.96 | 0.98 |
| KAS-CM7 | 0.76 | 0.70 | 0.85 |
| KAS-CM8† | 0.38 | 0.49 | 0.69 |
| KAS-CM9 | 0.63 | 0.66 | 0.83 |
| KAS-CM10 | 0.68 | 0.64 | 0.81 |
| KAS-CM11 | 0.68 | 0.50 | 0.70 |
Note. All coefficients were significantly different from zero at p<.05.
These items are reverse coded.
As seen in Table 5, we found evidence that the SDM-Q factor loadings were equivalent across groups (metric invariance; indicated in the table by a indicated by a non-significant chi-square difference test comparing nested models) and that the individual item means were equivalent across groups, after adjusting for latent variable differences (strong invariance). In other words, the Spanish-language sample reported overall higher levels of shared decision-making, but this was not due to differential item functioning. Variation of item errors (strict invariance) was not equivalent across groups. The summed item responses can therefore be used to compare groups.
Table 5.
Factorial Invariance Tests
| SDM (with SDM1 Removed) | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Model | MLMVχ2 | df | Δχ2 | Δdf | ΔP | RMSEA | CFI |
| Configural | 99.302 | 40 | 0.117 | 0.815 | |||
| Metric | 97.895 | 47 | 7.33 | 7 | 0.395 | 0.100 | 0.842 |
| Strong | 105.189 | 54 | 6.769 | 7 | 0.453 | 0.093 | 0.841 |
| Strict | 119.5 | 62 | 18.03 | 8 | 0.021 | 0.092 | 0.821 |
|
| |||||||
| KAS | |||||||
|
| |||||||
| Model | WLSMVχ2 | df | Δχ2 | Δdf | ΔP | RMSEA | CFI |
|
| |||||||
| Configural | 92.724 | 88 | 0.022 | 0.988 | |||
| Metric | 111.308 | 98 | 16.988 | 10 | 0.075 | 0.034 | 0.967 |
| Strong | 149.078 | 108 | 73.707 | 10 | 0.000 | 0.058 | 0.897 |
| Partial strong invariance | 119.845 | 105 | 10.891 | 7 | 0.144 | 0.035 | 0.963 |
| Strict | - | - | - | - | - | - | - |
Note: When robust methods are used to estimate the model, the chi square difference tests are not simple differences in the model chi square fits, but are instead computed using scaled differences (Muthén & Muthén, 1998–2015).
Measurement Invariance: KAS-CM
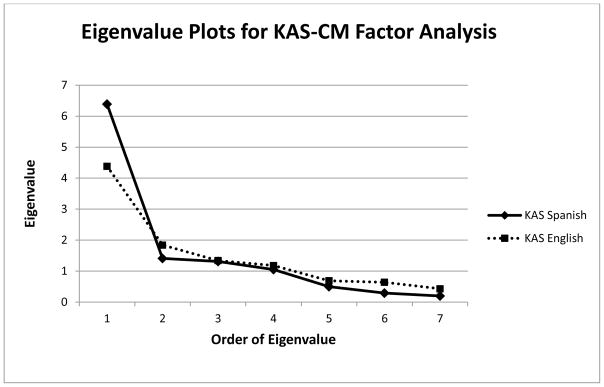
Just as we did for SDM, we first examined configural invariance issues in KAS-CM. Because the variation in responses to the KAS-CM items was concentrated in the distinction between less than best and best response, we carried out the factor analysis treating all eleven items as binary. We used Mplus Version 7.4 to fit a binary item factor model with a probit link function, which essentially fit tetrachoric correlations based on the binary items. These correlations represent the associations of latent continuous processes reflecting the likelihood of endorsing the KAS-CM items with the best possible endorsement. A one-factor model for the KAS-CM demonstrated good model fit according to fit statistics for the Spanish sample (RMSEA bounds 0 to 0.06, TLI 1.02, CFI 1.00), but good to poor model fit depending on the fit statistics interpreted for the English sample (RMSEA bounds 0.03 to 0.07, TLI 0.88, CFI 0.91). Again, a two-factor solution provided slightly improved fit, but the results were not easily interpretable (for example, two of the items had equivalent loadings on both factors) and did not result in a clinically meaningful scale. Like the SDM-9, the one factor model for the KAS-CM accounted for the majority of the shared variance (see Figure 2). Interpreting theoretical, practical, and statistical significance of the potential solutions, we selected a one-factor solution for subsequent analyses of measurement invariance. We also carried out sensitivity analyses with the one factor model with correlated residuals, finding good fit across groups and similar results to the original one-factor solution on subsequent tests of measurement invariance.
Figure 2.
Eigenvalue Plots for KAS-CM Factor Analysis (Scree Plot)
The factor loadings for the one-factor solution ranged from .94 to .38 with a median of .68. The highest loading was for KAS-CM 6 (My provider listens to me without judgment) which is prototypic of effective communication. The lowest loading was for KAS-CM 8 (My provider does not allow me to state my opinion) which is one of the two reverse coded items. The loadings for the Spanish language sample appeared to be somewhat larger (median .81 vs. .64 in the English language sample) since the residual variances were smaller in the Spanish sample for all items.
We continued measurement invariance analyses and first found equivalent factor loadings across English and Spanish language groups (metric invariance). However, we next found that item means were not all equivalent across the groups (strong factorial invariance was not supported), indicating that influences other than the latent factor of patient-provider communication might be causing higher or lower item responses for one group when compared to the other.3 In order to identify if particular items might be affected more than others, we examined differences in item thresholds and found 3 large differences. Even adjusting for the latent variable, Spanish-speaking patients were more likely to endorse KAS-CM 4 (My provider spends a lot of time educating me), than English-speaking patients, whereas English speakers were relatively more likely to endorse KAS-CM 1 (Plain/clear language is used by my provider) and KAS-CM 8 (My provider does not allow me to state my opinion, reverse-coded) than Spanish speakers with the same level of overall communication. We hypothesized that these items might account for the systematic difference in item means across groups, and proceeded with an additional test of partial strong invariance in which we found that the means for the remaining items are equivalent across groups once Items 1, 4, and 8 are excluded.4 The summed item responses of the 8 remaining items can be used to compare groups.
We next estimated Cronbach’s alpha for each of the scales (Table 5). The alpha for SDM-Q is 0.89 for the combined sample, and was similar in the individual samples (English, α = 0.88; Spanish, α = 0.90). Alphas were lower for KAS-CM, with items scored as binary (total sample α =0.66; English, α = 0.61; Spanish, α = 0.78). Correlation between SDM-Q and KAS-CM revealed that the two constructs of shared decision making and patient-provider communication are related (r = 0.39, p < .001). The correlation is almost the same in the English speaking sample (r = 0.40, p < .001) and lower in the Spanish speaking group (r = 0.23, p <.05); however, this difference is not statistically significant.
We investigated the convergence of the patient’s reported SDM measure with the provider’s reported SDM on the equivalent scale, the SDM-Q-Doc (Scholl, Kriston, Dirmaier, Buchholz, & Härter, 2012). In parallel, we examined the convergence of the patient’s reported KAS-CM with the provider’s report using a modified KAS-CM (the one item that was added for the provider measure was not included). In both cases, the correlations between providers’ reports and patients’ reports appeared low for the overall sample (r = 0.04 for SDM-Q and r = 0.02 for KAS-CM). The trend was for patients to report higher ratings than their provider did in the same encounter.
Discussion
Minority patients face new demands connecting with providers with different customs, values and experiences, and addressing these challenges by improving SDM and patient-centered communication could lead to better quality care. Our findings suggest that a revised 8-item version of the SDM-Q (first item deleted) performs well in both English and Spanish with behavioral health patients, and is a useful patient-centered measures for clinical practice with both Spanish and English-speaking populations. We also found that the KAS-CM is a promising measure for collecting information about patient-provider communication among behavioral health patients, but that in our sample most respondents were near the ceiling of perceived good communication. We identified three KAS-CM items that should be excluded from group comparisons of Spanish and English speaking patients due to differential item functioning across groups. Given that patient perceptions of the patient-provider encounter have been linked to overall health and behavioral health outcomes (Little et al., 2001; Oates, Weston, & Jordan, 2000), use of these measures is a time-efficient way to collect data necessary to improve the clinical encounter for both English and Spanish-speaking patients.
Psychometric results for the SDM-Q are consistent with what has been previously reported in the literature for English-speaking, Dutch, German, and Spanish primary care patients (De Las Cuevas et al., 2014; Glass et al., 2012; Kriston et al., 2010; Rodenburg-Vandenbussche et al., 2015). Similar to these studies but with a more diverse population, the factor analyses for our English and Spanish-speaking samples indicated a one-dimensional structure for the patient’s measure. Our finding that Item 1 on the scale did not have a significant loading for Spanish-speaking patients and that an 8-item version of the SDM-Q demonstrated better fit is consistent with the results in a Spanish sample of primary care patients from Spain (De Las Cuevas et al., 2014). Factor loadings were above 0.48 for all SDM-Q items in both languages. Our results suggest that the scale has factorial validity in both languages, and that Item 1 (My provider made clear that a decision needs to be made) does not correlate well with the overall scale for Spanish speaking patients, independently of site or sector of care. The finding that this item showed the lowest mean score when compared to other items on the scale was not surprising, given that patients may not view the clinical encounter as a setting where they can make decisions about their care. As has been previously described in the literature (Hamann et al., 2015), patients, particularly non-English speaking patients, rarely get an opportunity to evaluate decisions in care, and even the conceptualization of sharing power can seem alien in behavioral healthcare visits (Cortes et al., 2008). This item also seems to diverge from the others in the scale given that it does not describe a decision-making process but rather a direct communication from a provider.
Nevertheless, Spanish speaking patients rate their providers higher in terms of overall SDM as compared to their English counterparts. This might be tied to a more pronounced barrier to access to behavioral health care for Spanish speaking patients (DuBard & Gizlice, 2008), who might find that having a provider who offers respect and warmth is a more salient feature of communication than attempting SDM with them (Eliacin, Salyers, Kukla, & Matthias, 2015). As a consequence of the power that behavioral healthcare providers hold in these interactions and the cultural value of respeto (respect) for Spanish speaking patients, some behavioral dimensions of SDM (like asking the patient about what should be covered in the session or what are his/her options in treatment) might be experienced and rated differently depending the cultural values and expectations for empowerment of diverse patients (Cortes et al., 2008).
The SDM-Q demonstrated strong factorial invariance, leading us to conclude that the summed item means of the SDM-Q scale can be compared across English and Spanish-speaking patient groups. The reliability of the SDM patient measure was also confirmed, with acceptable alphas in both languages and comparable results to those observed for English-speaking primary care patients (Glass et al., 2012). This seems to expand the generalizability of the SDM measure for behavioral health patients in both English and Spanish. Yet there was no convergent validity with provider ratings, as illustrated by the low correlations of the patient SDM measure with the provider SDM measure for the same encounter. These differences of perspectives reinforce the importance of having a patient’s perspective separate from that of the provider’s when evaluating SDM in the clinical encounter. Several explanations could account for our results. It is possible that patients who would rate their providers low on SDM quickly drop out of care and were not represented in our study. Alternatively, these patients may stay and accept what is offered, without discriminating on specific behavioral dimensions of shared decision making. Some prior data seem to indicate the tension inherent between the patient and the provider’s view of what constitutes optimal shared decision-making in the clinical encounter. For example, one study found that while both patients and providers were in favor of collaborating in the decision-making process, patients viewed providers as responsible for final decisions in treatment, and vice versa (De Las Cuevas, Rivero-Santana, Perestelo-Pérez, Pérez-Ramos, & Serrano-Aguilar, 2012). The low correlation between measures by providers and patients in our study indicate that providers perceived less decision-making and communication in the same encounter when compared to patients, which may reflect differing views of what specific behaviors constitute patient-centered care.
The KAS-CM subscale also demonstrated a one-factor structure of the underlying construct for the total sample and for both language groups, and partial strong factorial invariance, indicating that the summed item means of eight of the scale items can be compared across English and Spanish-speaking patient groups. While the KAS-CM has not been studied as a stand-alone scale, this finding is consistent with the conceptual framework of the Kim Alliance Scale as containing a separate communication construct (Kim et al., 2008). Similar to results of Kim and colleagues (2008), where 58% of patients gave perfect scores on the Communication subscale, we also encountered highly skewed endorsements of KAS-CM items from behavioral health patients, indicating that patients tend to rate their providers highly on communication. This led us to modify the measure as a binary item scale rather than treat item responses as a continuous in the outcome measure. While we consider that it is possible that our ceiling effect is related to our average patient having seen their provider for more than a year at the time of data collection, we also note that expanding the number of response options for the KAS-CM may provider more variability in responses and improve the scale’s psychometric properties.
Based on our results, we presume that the KAS-CM subscale represents a unidimensional construct, with adequate reliability in both languages. The factor loadings for the KAS-CM subscale were acceptable (greater than 0.4) for both Spanish and English speaking patients. However, we find that three items on the KAS-CM may reflect differences in cultural or language characteristics of the two groups, rather than true differences in latent construct of patient-provider communication. As a result, we see loadings that are different across the two language subgroups, emphasizing how the experience of the communication might vary by language groups. For example, Spanish-speaking patients reported more frequently that their provider spent time educating them and less frequently that their provider allowed them to state their opinion. English-speaking patients reported more frequently that their provider uses plain/clear language.
One potential way of explaining this finding is that communication in healthcare visits itself varies by language of the patient (Alegría et al., 2013). Perhaps bilingual U.S. providers treating monolingual Spanish-speakers have more difficulty employing easily understood wording in behavioral health sessions, due to less proficiency in the language when compared to the patient or to differences in colloquial terms depending on the patient’s country of origin. A more thought-provoking explanation might be that what is valued of communication diverges by language or cultural group (Alegría, Sribney, Perez, Laderman, & Keefe, 2009; Mulvaney-Day, Earl, Diaz-Linhart, & Alegría, 2011). In the case of the KAS-CM, it may be that cultural expectations about the provider’s role influence patient’s ratings of individual items but not of the patients’ overall perception of their level of communication. In the case of whether or not a provider spends time educating the patient, this connotes a one-way communication from the provider (as expert) to the patient (as student). In a qualitative study of communication preferences among patients with depression receiving outpatient behavioral health care, the overall themes expressed by African-American, Latino, and White patients did not differ, and centered on good relationships in which patients felt listened to and felt understood (Mulvaney-Day, Earl, Diaz-Linhart, & Alegría, 2011). However, the descriptions and understandings of how these qualities were expressed in the clinical encounter were different across the different ethnic and racial groups. Notably with regards to our findings, Latino patients preferred a directive, authoritative approach from their providers when compared to African-American and non-Latino White respondents, who preferred that providers actively work to diminish the power differential inherent in the provider-patient relationship.
This study has several limitations. Patients represented in the study sample agreed to participate in an intervention study aimed at helping them ask questions and make decisions with their providers; thus, the study sample may have been more interested than the average patient in the constructs measured by the study. The sample is predominantly minority patients receiving behavioral care in safety-net clinics, which allows us to present novel results regarding the validity of measures in this population and care setting; however, results may differ in other patient populations. Additionally, the ceiling effect observed on the KAS-CM indicates that a measure with additional response options might better capture variability among patient perceptions of communication with providers. Another limitation has to do with the limited Mandarin speaking sample participating in the study, restricting the possibility of estimating the psychometric properties with this group. The lack of instruments to evaluate the convergent validity of these measures also is considered a limitation. Future studies may further address the reasons why patient and provider reports were not significantly correlated, perhaps by completing an item analysis to identify specific behaviors viewed differently by the two groups.
It is important to note that the one-factor models selected for each measure demonstrated poorer fit than potential two and three-factor models; however, we took into account theoretical and practical considerations along with statistical considerations in selecting the one-factor models. We did find improved fit when allowing some residuals to correlate, indicating the influence of background factors other than the latent constructs of SDM and KAS, respectively, on these variables. Given that our question of interest was the evaluation of whether the scales can be accurately used in clinical practice with the two language groups, we concluded that the factor structure for each scale was sufficiently established to allow for comparison across groups and recommendations for clinical practice.
Not withstanding these limitations, our study emphasizes the importance of evaluating the psychometric properties of patient-centered outcomes with diverse patients and in different languages. Our results provide evidence of the suitability of revised 8-item versions of both the SDM and the KAS-CM for identifying patient perceptions of shared decision making and patient-provider communication among both Spanish and English speaking respondents receiving behavioral healthcare. The findings are also suggestive of the need to carefully examine how self-report measures perform among non-English speaking patients, in order to ensure that self-report measures used to track patient outcomes in health services research and clinical practice accurately reflect the experiences of diverse patient populations.
Table 6.
Internal Consistency (Cronbach's α) of SDM-Q and KAS-CM for 2 Language Groups
| Total Sample (n=239) | English (n=160) | Spanish (n=79) | |
|---|---|---|---|
| SDM-Q(with SDM1 excluded) | 0.89 | 0.88 | 0.90 |
| KAS-CM | 0.66 | 0.61 | 0.78 |
Acknowledgments
Funding: The Effectiveness of DECIDE in Patient-Provider Communication, Therapeutic Alliance & Care Continuation study was supported by the Patient-Centered Outcomes Research Institute (PCORI) research grant #CD-12-11-4187. Dr. Alvarez was supported by Research Grant R01MH098374-03S1, funded by the National Institute of Mental Health.
Appendix 1: SDM-Q
| Item | English | Spanish |
|---|---|---|
| SDM1 | My provider made clear that a decision needs to be made. | Mi proveedor me dijo expresamente que debía tomarse una decisión. |
| SDM2 | My provider wanted to know exactly how I want to be involved in making the decision. | Mi proveedor quería saber exactamente cómo me gustaría participar en la toma de decisiones. |
| SDM3 | My provider told me that there are different options for treating my behavioral health or substance abuse condition. | Mi proveedor me informó de que existen distintas opciones de tratamiento para mi problema de salud. |
| SDM4 | My provider explained the advantages and disadvantages of the treatment options. | Mi proveedor me explicó con exactitud las ventajas y desventajas de las distintas opciones de tratamiento. |
| SDM5 | My provider helped me understand all the information. | Mi proveedor me ayudó a entender toda la información. |
| SDM6 | My provider asked me which treatment option I prefer. | Mi proveedor me preguntó qué opción de tratamiento prefiero. |
| SDM7 | My provider and I thoroughly weighed the different treatment options. | Mi proveedor y yo valoramos con detenimiento las distintas opciones de tratamiento. |
| SDM8 | My provider and I selected a treatment option together. | Mi proveedor y yo elegimos juntos/as una opción de tratamiento. |
| SDM9 | My provider and I reached an agreement on how to proceed. | Mi proveedor y yo llegamos a un acuerdo sobre el modo de proceder. |
Note. This measure was introduced with the following verbal introduction (English version): “Now I’m going to ask you some questions about how decisions were made with your mental health care or substance abuse provider during the last visit you had with your provider. If you didn’t see your provider today, think back to the last appointment you had with your provider. For each statement, please indicate how much you agree or disagree.”
Appendix 2: KAS-CM
| Item | English | Spanish |
|---|---|---|
| KAS-CM1 | Plain/clear language is used by my provider. | Mi proveedor usa un lenguaje claro/sencillo. |
| KAS-CM2 | I have a good rapport/relationship with my provider. | Yo tengo una buena relación con mi proveedor. |
| KAS-CM3 | I feel my provider criticizes me too much. | Yo siento que mi proveedor me critica mucho |
| KAS-CM4 | My provider spends lots of time educating me. | Mi proveedor emplea bastante tiempo en educarme. |
| KAS-CM5 | I can express negative feelings freely to my provider. | Yo puedo expresarle con libertad mis sentimientos negativos a mi proveedor. |
| KAS-CM6 | My provider listens to me without judgment. | Mi proveedor me escucha sin juzgarme. |
| KAS-CM7 | I feel my provider gives me enough information. | Yo siento que mi proveedor me da suficiente información. |
| KAS-CM8 | My provider does not allow me to state my opinion. | Mi proveedor no me permite expresar mi opinión. |
| KAS-CM9 | It is easy to understand my provider’s instructions. | Es fácil entender las instrucciones de mi proveedor. |
| KAS-CM10 | My provider gives me positive feedback. | Mi proveedor me hace observaciones positivas. |
| KAS-CM11 | I am able to talk to my provider about anything | Yo puedo hablar con mi proveedor de cualquier cosa. |
Note. This measure was introduced with the following verbal introduction (English version): “Now I am going to read to you some sentences that describe how you and your provider communicate with each other. Some questions will be about how your provider behaves with you. Again, please tell me how often this applies to you: Never, Rarely, Sometimes, or Always.”
Footnotes
As a sensitivity check of the effects of listwise deletion of missing data, we redid the analyses using MLR estimation in MPlus, which allows the partially incomplete observations to inform an EM algorithm estimate of the sample variance covariance. The conclusions about measurement invariance were identical to those presented in the body of the article.
To deal with these extreme distributions statistically, we recoded the KAS-CM to be binary (≤ 3 = 0, 4=1) and used statistical methods for binary responses in the factor analysis.
In the Strong Invariance model, the Spanish group had a significantly higher latent mean of communication than the English group (mean difference(se) = 1.13 (.44), Cohen’s d=1.13).
In practice, we conducted the tests of partial strong invariance systematically by first freeing the threshold for Item 4 (the item with the largest difference), then also freeing Item 1, then also freeing Item 8. The difference in Chi-square was significant for the first two models and not significant for the last one, in which the thresholds for Items 4, 1, and 8 were all free and the remaining item thresholds constrained to be equal.
Contributor Information
Kiara Alvarez, Disparities Research Unit, Department of Medicine, Massachusetts General Hospital and Harvard Medical School.
Ye Wang, Disparities Research Unit, Department of Medicine, Massachusetts General Hospital and Harvard Medical School.
Margarita Alegria, Disparities Research Unit, Department of Medicine, Massachusetts General Hospital and Harvard Medical School.
Andrea Ault-Brutus, Health Equity Research Lab, Cambridge Health Alliance and Harvard Medical School.
Natasha Ramanayake, Disparities Research Unit, Department of Medicine, Massachusetts General Hospital and Harvard Medical School.
Yi-Hui Yeh, Disparities Research Unit, Department of Medicine, Massachusetts General Hospital and Harvard Medical School.
Julia R. Jeffries, Icahn School of Medicine at Mount Sinai, Mount Sinai Hospital
Patrick E. Shrout, Department of Psychology, New York University
References
- Alegría M, Polo A, Gao S, Santana L, Rothstein D, Jimenez A, … Normand SL. Evaluation of a patient activation and empowerment intervention in mental health care. Medical care. 2008;46(3):247. doi: 10.1097/MLR.0b013e318158af52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Roter DL, Valentine A, Chen C-n, Li X, Lin J, … Larson S. Patient–clinician ethnic concordance and communication in mental health intake visits. Patient education and counseling. 2013;93(2):188–196. doi: 10.1016/j.pec.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Sribney W, Perez D, Laderman M, Keefe K. The role of patient activation on patient–provider communication and quality of care for US and foreign born Latino patients. Journal of general internal medicine. 2009;24(3):534–541. doi: 10.1007/s11606-009-1074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, D.C: National Academies Press; 2001. [PubMed] [Google Scholar]
- Balsa AI, McGuire TG. Prejudice, clinical uncertainty and stereotyping as sources of health disparities. Journal of health economics. 2003;22(1):89–116. doi: 10.1016/s0167-6296(02)00098-x. [DOI] [PubMed] [Google Scholar]
- Barry MJ, Edgman-Levitan S. Shared decision making—the pinnacle of patient-centered care. New England Journal of Medicine. 2012;366(9):780–781. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- Beisecker AE, Beisecker TD. Patient information-seeking behaviors when communicating with doctors. Medical care. 1990;28(1):19–28. doi: 10.1097/00005650-199001000-00004. [DOI] [PubMed] [Google Scholar]
- Clever SL, Jin L, Levinson W, Meltzer DO. Does doctor–patient communication affect patient satisfaction with hospital care? Results of an analysis with a novel instrumental variable. Health services research. 2008;43(5p1):1505–1519. doi: 10.1111/j.1475-6773.2008.00849.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, Inui TS. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American journal of public health. 2012;102(5):979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of internal medicine. 2003;139(11):907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- Cortes DE, Mulvaney-Day N, Fortuna L, Reinfeld S, Alegría M. Patient–provider communication: Understanding the role of patient activation for Latinos in mental health treatment. Health Education & Behavior. 2008 doi: 10.1177/1090198108314618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Las Cuevas C, Perestelo-Perez L, Rivero-Santana A, Cebolla-Martí A, Scholl I, Härter M. Validation of the Spanish version of the 9-item Shared Decision-Making Questionnaire. Health expectations: an international journal of public participation in health care and health policy. 2014 doi: 10.1111/hex.12183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Las Cuevas C, Rivero-Santana A, Perestelo-Pérez L, Pérez-Ramos J, Serrano-Aguilar P. Attitudes toward concordance in psychiatry: a comparative, cross-sectional study of psychiatric patients and mental health professionals. BMC psychiatry. 2012;12(1):53. doi: 10.1186/1471-244X-12-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuBard CA, Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among US Hispanics. American journal of public health. 2008;98(11):2021–2028. doi: 10.2105/AJPH.2007.119008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan E, Best C, Hagen S. Shared decision making interventions for people with mental health conditions. The Cochrane Library. 2010 doi: 10.1002/14651858.CD007297.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliacin J, Salyers MP, Kukla M, Matthias MS. Patients’ Understanding of Shared Decision Making in a Mental Health Setting. Qualitative health research. 2015;25(5):668–678. doi: 10.1177/1049732314551060. [DOI] [PubMed] [Google Scholar]
- Gilmer TP, Kronick RG. Hard Times And Health Insurance: How Many Americans Will Be Uninsured By 2010? Health Affairs. 2009;28(4):w573–w577. doi: 10.1377/hlthaff.28.4.w573. [DOI] [PubMed] [Google Scholar]
- Glass KE, Wills CE, Holloman C, Olson J, Hechmer C, Miller CK, Duchemin AM. Shared decision making and other variables as correlates of satisfaction with health care decisions in a United States national survey. Patient education and counseling. 2012;88(1):100–105. doi: 10.1016/j.pec.2012.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregorich SE. Do self-report instruments allow meaningful comparisons across diverse population groups? Testing measurement invariance using the confirmatory factor analysis framework. Medical care. 2006;44(11 Suppl 3):S78. doi: 10.1097/01.mlr.0000245454.12228.8f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamann J, Kohl S, McCabe R, Bühner M, Mendel R, Albus M, Bernd J. What can patients do to facilitate shared decision making? A qualitative study of patients with depression or schizophrenia and psychiatrists. Social psychiatry and psychiatric epidemiology. 2015:1–9. doi: 10.1007/s00127-015-1089-z. [DOI] [PubMed] [Google Scholar]
- Hamann J, Leucht S, Kissling W. Shared decision making in psychiatry. Acta Psychiatrica Scandinavica. 2003;107(6):403–409. doi: 10.1034/j.1600-0447.2003.00130.x. [DOI] [PubMed] [Google Scholar]
- Hamann J, Mendel R, Cohen R, Heres S, Ziegler M, Bühner M, Kissling W. Psychiatrists’ use of shared decision making in the treatment of schizophrenia: patient characteristics and decision topics. Psychiatric Services. 2009;60(8):1107–1112. doi: 10.1176/ps.2009.60.8.1107. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal. 1999;6(1):1–55. [Google Scholar]
- Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. American journal of public health. 2004;94(12):2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SC, Boren D, Solem SL. The Kim Alliance Scale: development and preliminary testing. Clinical Nursing Research. 2001;10(3):314–331. doi: 10.1177/c10n3r7. [DOI] [PubMed] [Google Scholar]
- Kim SC, Kim S, Boren D. The Quality of Therapeutic Alliance between Patient and Provide Predicts General Satisfaction. Military medicine. 2008;173(1):85–90. doi: 10.7205/milmed.173.1.85. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ, Groleau D, Guzder J, Blake C, Jarvis E. Cultural Consultation: A Model of Mental Health Service for Multicultural Societies. Focus. 2014 doi: 10.1177/070674370304800302. [DOI] [PubMed] [Google Scholar]
- Korsch BM, Gozzi EK, Francis V. Gaps in doctor-patient communication I. Doctor-patient interaction and patient satisfaction. Pediatrics. 1968;42(5):855–871. [PubMed] [Google Scholar]
- Kriston L, Scholl I, Hölzel L, Simon D, Loh A, Härter M. The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient education and counseling. 2010;80(1):94–99. doi: 10.1016/j.pec.2009.09.034. [DOI] [PubMed] [Google Scholar]
- Levinson W, Stiles WB, Inui TS, Engle R. Physician frustration in communicating with patients. Medical care. 1993;31(4):285–295. doi: 10.1097/00005650-199304000-00001. [DOI] [PubMed] [Google Scholar]
- Little P, Everitt H, Williamson I, Warner G, Moore M, Gould C, … Payne S. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. Bmj. 2001;323(7318):908–911. doi: 10.1136/bmj.323.7318.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh HW, Hau KT, Wen Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural equation modeling. 2004;11(3):320–341. [Google Scholar]
- Matías-Carrelo LE, Chávez LM, Negrón G, Canino G, Aguilar-Gaxiola S, Hoppe S. The Spanish translation and cultural adaptation of five mental health outcome measures. Culture, medicine and psychiatry. 2003;27(3):291–313. doi: 10.1023/a:1025399115023. [DOI] [PubMed] [Google Scholar]
- Mead N, Bower P. Measuring patient-centredness: a comparison of three observation-based instruments. Patient education and counseling. 2000;39(1):71–80. doi: 10.1016/s0738-3991(99)00092-0. [DOI] [PubMed] [Google Scholar]
- Mulvaney-Day NE, Earl TR, Diaz-Linhart Y, Alegría M. Preferences for relational style with mental health clinicians: A qualitative comparison of African American, Latino and Non-Latino White patients. Journal of clinical psychology. 2011;67(1):31–44. doi: 10.1002/jclp.20739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 1998–2015. [Google Scholar]
- Oates J, Weston WW, Jordan J. The impact of patient-centered care on outcomes. Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- Patel SR, Bakken S, Ruland C. Recent advances in shared decision making for mental health. Current opinion in psychiatry. 2008;21(6):606. doi: 10.1097/YCO.0b013e32830eb6b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peek ME, Wilson SC, Gorawara-Bhat R, Odoms-Young A, Quinn MT, Chin MH. Barriers and facilitators to shared decision-making among African-Americans with diabetes. Journal of general internal medicine. 2009;24(10):1135–1139. doi: 10.1007/s11606-009-1047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pippins JR, Alegría M, Haas JS. Association between language proficiency and the quality of primary care among a national sample of insured Latinos. Medical care. 2007;45(11):1020. doi: 10.1097/MLR.0b013e31814847be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polo AJ, Alegría M, Sirkin JT. Increasing the engagement of Latinos in services through community-derived programs: The Right Question Project–Mental Health. Professional Psychology: Research and Practice. 2012;43(3):208. [Google Scholar]
- Quirk A, Chaplin R, Lelliott P, Seale C. How pressure is applied in shared decisions about antipsychotic medication: a conversation analytic study of psychiatric outpatient consultations. Sociology of health & illness. 2012;34(1):95–113. doi: 10.1111/j.1467-9566.2011.01363.x. [DOI] [PubMed] [Google Scholar]
- Rodenburg-Vandenbussche S, Pieterse AH, Kroonenberg PM, Scholl I, van der Weijden T, Luyten GP, … van Vliet IM. Dutch Translation and Psychometric Testing of the 9-Item Shared Decision Making Questionnaire (SDM-Q-9) and Shared Decision Making Questionnaire-Physician Version (SDM-Q-Doc) in Primary and Secondary Care. PloS one. 2015;10(7) doi: 10.1371/journal.pone.0132158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooks RN, Wiltshire JC, Elder K, BeLue R, Gary LC. Health information seeking and use outside of the medical encounter: Is it associated with race and ethnicity? Social Science & Medicine. 2012;74(2):176–184. doi: 10.1016/j.socscimed.2011.09.040. [DOI] [PubMed] [Google Scholar]
- Roter DL, Stewart M, Putnam SM, Lipkin M, Stiles W, Inui TS. Communication patterns of primary care physicians. Jama. 1997;277(4):350–356. [PubMed] [Google Scholar]
- Schillinger D, Bindman A, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician–patient communication among diabetes patients. Patient education and counseling. 2004;52(3):315–323. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- Scholl I, Kriston L, Dirmaier J, Buchholz A, Härter M. Development and psychometric properties of the Shared Decision Making Questionnaire–physician version (SDM-Q-Doc) Patient education and counseling. 2012;88(2):284–290. doi: 10.1016/j.pec.2012.03.005. [DOI] [PubMed] [Google Scholar]
- Simon D, Schorr G, Wirtz M, Vodermaier A, Caspari C, Neuner B, … Edwards A. Development and first validation of the shared decision-making questionnaire (SDM-Q) Patient education and counseling. 2006;63(3):319–327. doi: 10.1016/j.pec.2006.04.012. [DOI] [PubMed] [Google Scholar]
- Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ: Canadian Medical Association Journal. 1995;152(9):1423. [PMC free article] [PubMed] [Google Scholar]
- Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient education and counseling. 2009;74(3):295–301. doi: 10.1016/j.pec.2008.11.015. [DOI] [PubMed] [Google Scholar]
- Swanson KA, Bastani R, Rubenstein LV, Meredith LS, Ford DE. Effect of mental health care and shared decision making on patient satisfaction in a community sample of patients with depression. Medical Care Research and Review. 2007;64(4):416–430. doi: 10.1177/1077558707299479. [DOI] [PubMed] [Google Scholar]
- Wills CE, Holmes-Rovner M. Integrating decision making and mental health interventions research: research directions. Clinical Psychology: Science and Practice. 2006;13(1):9–25. doi: 10.1111/j.1468-2850.2006.00002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zolnierek KBH, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Medical care. 2009;47(8):826. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]