Abstract
Family meals have been associated with higher diet quality and reduced risk of obesity in children. Observational studies of the family meal have been employed with increasing frequency, yet there is currently no tool available for measuring the healthfulness of food served during the meal. Here we present the development and validation of the Healthy Meal Index (HMI), a novel tool for scoring the healthfulness of foods served to children during a meal, as well as sociodemographic predictors of meal scores. Parents of 233 children, aged 4–8 years, self-recorded three home dinners. A research assistant obtained a list of foods available during the meal (meal report) via phone call on the night of each video-recorded meal. This meal report was coded into component foods groups. Subsequently, meals were scored based on the availability of more healthy “Adequacy foods” and the absence of “Moderation foods”, (of which reduced consumption is recommended, according to pediatric dietary guidelines). Adjusted linear regression tested the association of sociodemographic characteristics with HMI scores. A validation study was conducted in a separate sample of 133 children with detailed meal data. In adjusted models, female children had higher HMI Moderation scores (p=0.02), but did not differ in HMI Adequacy or Total scores. Parents with more education served meals with higher HMI Adequacy (p=0.001) and Total scores (p=0.001), though no significant difference was seen in HMI Moderation score (p=0.21). The validation study demonstrated that the HMI was highly correlated with servings of foods and nutrients estimated from observations conducted by research staff. The HMI is a valuable tool for measuring the quality of meals served to children.
Keywords: Meal Observation, Meal Assessment, Family Meals, Pediatric Feeding, Dietary Quality
Introduction
Family meals have been associated with improved diet quality, including lower intake of sugar sweetened beverages and higher intake of fruits and vegetables, as well as decreased risk of obesity in children (Berge, et al., 2015; Cason, 2006; Fulkerson, Larson, Horning, & Neumark-Sztainer, 2014; Hammons & Fiese, 2011; Larson, Neumark-Sztainer, Hannan, & Story, 2007; Ogata & Hayes, 2014; Skafida, 2013; Videon & Manning, 2003; Welsh, French, & Wall, 2011). As a result, an increasing number of practice guidelines include family mealtimes as an obesity prevention strategy and promoting family mealtimes is being tested as an intervention strategy in a randomized controlled trial (Fruh, Fulkerson, Mulekar, Kendrick, & Clanton, 2011; Fulkerson et al., 2014; Gidding et al., 2006; Ogata & Hayes, 2014).
Hypothesized mechanisms through which the family meal improves diet and weight status include increased parent-child interaction due to eating together and that meals served in the context of family mealtimes are healthier and more consistent with dietary guidelines designed to prevent obesity (Berge et al., 2014; Fiese, Hammons, & Grigsby-Toussaint, 2012; Fruh et al., 2011; Fulkerson et al., 2014; Skafida, 2013; Welsh et al., 2011). A few prior studies have found that increased parental engagement and positive interaction during the meal are associated with healthy weight status and that reported family cohesion partially mediates the relationship between family meals and diet (Berge et al., 2014; Fiese et al., 2012; Welsh et al., 2011). One survey found that families who reported placing more emphasis on family meals also reported serving healthier foods more frequently (Neumark-Sztainer et al., 2014).
A growing number of studies have focused on indexing the contextual features of the family mealtime. In particular, there has been increased enthusiasm for employing videotaped or real time observation of family mealtimes (Berge et al., 2014; Bergmeier, Skouteris, & Hetherington, 2015; Fiese et al., 2012; Hughes et al., 2007; Hughes, Power, Orlet Fisher, Mueller, & Nicklas, 2005; Kong et al., 2013). Observed mealtime interactions provide unique information regarding the family feeding environment, particularly since behaviors observed during mealtimes have been reported to have low correlation with maternal self-report of feeding practices (Bergmeier et al., 2015). The creation of universal coding systems of feeding behaviors for observational meal studies has been identified as a priority for this field of research (Hughes et al., 2013).
While a number of methods have been employed to index maternal feeding behaviors and general family interaction patterns during observed family mealtimes (Bergmeier et al., 2015), we have been unable to identify any studies that have attempted to measure the healthfulness of foods served during those mealtimes. This methodological constraint has limited the ability to comprehensively characterize the family mealtime context. Existing healthfulness measures focus on children’s dietary intake, or foods actually consumed (Chiuve et al., 2012; George et al., 2014; Guenther et al., 2013; Guenther, Reedy, Krebs-smith, Reeve, & Basiotis, 2007; Marshall, Burrows, & Collins, 2014; Shanthy, Lino, Gerrior, & Peter, 1998). Characterization of the family mealtime, however, requires an index of the healthfulness of foods served during one meal. This is important, because food consumed is not always concordant with food served. Pediatric feeding guidelines recommend that caregivers serve a variety of healthful foods and allow children to decide what and how much to consume (Hetherington, Cecil, Jackson, & Schwartz, 2011; Hurley, Cross, & Hughes, 2011; Ogata & Hayes, 2014; Rhee, 2008; Vereecken, Haerens, De Bourdeaudhuij, & Maes, 2010). Thus, the key variable for measuring adherence to child feeding recommendations is the healthfulness of food served rather than that of food consumed.
This paper addresses three objectives. First, we describe the development of the Healthy Meal Index (HMI), a method to quantify the healthfulness of foods served during a meal. Secondly, we provide evidence to validate the HMI as an instrument. Lastly, we test the application of the HMI by examining the association of sociodemographic characteristics with HMI scores in a naturalistic setting.
Materials and Methods
Validation Sample Protocol
Participants and Recruitment
We validated the HMI utilizing meal data collected during home meal observations in a separate study that included 137 low-income children, aged 33 months (Mean(SD): 33.5(0.7)). This multi-component study, from which we utilized data for the HMI validation study, focused on child eating behavior. Children were recruited from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinics and Early Head Start programs (free, federally-subsidized early preschool) that serve low-income families. Inclusion criteria were that the caregiver had less than a four-year college degree and was fluent in English; and that the child was born at > 35 weeks gestation without significant complications, did not have food allergies, serious medical problems, or any form of disordered eating, and was not in foster care. None of the children enrolled in the primary research study, that is the focus of this report, were also enrolled in the validation study, though some were their siblings.
Home Mealtime Observation Protocol
The validation study utilized a home mealtime observation that required a trained research assistant (RA) to visit the home of participants to conduct behavioral assessments over 5 days. On the day of the final home visit, the parent (usually the mother) was asked to serve the child a typical meal and the research assistant recorded, in detail, the type and quantity of each food served to the child, including preparation methods and brands, based on visual observation. The RAs asked the parent preparing the meal for details on brand and/or preparation of any foods that were not apparent through visual observation of the meal preparation. In the validation study, food was served directly to the child by the parent, in contrast to other serving styles, such as family style or self-serve. Thus recorded quantities were specific to the individual child. The meal was scheduled and served at a time and place typical for the child. Meals were video-recorded and children were allowed to eat to satiety, as assessed by the parent. Each of the research assistants was trained the collection of dietary recalls using Nutrition Data System for Research (NDSR) and thus understood the level of detail required for accurate dietary assessment. Each research assistant was provided with resources to assist in visual portion size estimation. For the purpose of the validation study, the meal report was based on the list of foods recorded by the research assistant.
Primary Sample Protocol
Participants and Recruitment
The primary study population comprised 301 parent-child dyads who participated in a previous study investigating associations between stress and eating in children. In 2011–2013 approximately 2–4 years after the previous study (2009–2011), primary caregivers were invited to participate in this follow-up study, which was described as seeking to understand the different ways that mothers feed children. The study included a multi-method data collection to characterize maternal feeding. This report describes features of the observed family mealtime. Children enrolled in the previous study, recruited from Head Start programs (free, federally-subsidized preschool programs for low-income children) in Southeastern Michigan (Lumeng et al., 2014), were invited to participate. Inclusion criteria were the same as the validation study. Child sex, date of birth, parental race/ethnicity and parental education were collected at enrollment in the previous study.
Home Mealtime Observation Protocol
During recruitment by telephone, the primary caregiver was told, “Part of this research study is to better understand how families eat meals at home. We will loan you a video camera and ask you to tape your child’s dinnertime on 3 weeknights [defined as Monday, Tuesday, Wednesday, or Thursday]. You do not need to do anything special for these dinners. We just want to understand what a typical dinner is like in different families.” The parent was then asked to videotape dinners occurring in a context such that the primary caregiving parent was home and awake (as opposed to sleeping due to working an overnight shift), that the meal occurred at home (as opposed to somewhere else, like a relative’s house), and that the meal was prepared by the primary caregiving parent (even when preparation was defined as picking up “take out”). If a language besides English was spoken in the home, we requested that they speak only English during the videotaped meal. Following the dinnertime meal, on the same night, parents received a telephone call from a trained interviewer. The parent was asked to, “List all the foods that were available to the child at the meal. Please provide as much detail as possible and include condiments and drinks.” This list comprised the meal report. In order to reduce respondent burden and increase the likelihood of response, the interviewer did not ask for details about food preparation or ingredients. Participants were compensated $10 for each dinnertime meal recording they attempted. In order to roughly assess the validity of the meal reports, the list of foods in the meal report was compared to the foods available on the videotaped meal for 100 meals from 35 randomly chosen dyads (30 of which had provided 3 meals and 5 of which had provided 2 meals) in order to examine the completeness of the meal reports. The participants who had fewer than three videotaped meals were included in analyses comparing the meal reports to the foods visible on the videos, but were excluded from all other analyses.
Meal Report Coding
Each meal report from the primary study and the validation study was coded into food group categories by coders trained by a PhD level nutrition researcher. In the context of this paper, only the information provided in the meal report was utilized in meal coding and HMI scoring. Food categories (see Table 1) were determined by the food groupings on ChooseMyPlate.gov in accordance with the 2010 US Dietary Guidelines for Americans.” (U.S. Department of Agriculture & U.S. Department of Health and Human Services, 2010). The presence or absence of each food group, sweets and desserts, and beverages was recorded and subsequently, the details about the type of food, as shown in Table 1. A list of potential mixed dishes (e.g., tacos, burgers, spaghetti) based on the MyPlate Mixed Dish list, determined how each mixed dish was to be coded, unless otherwise specified in the meal report (United States Department of Agriculture, 2013). The MyPlate Mixed Dish list, published by the USDA, lists the food group servings available in common mixed dishes. When a unique mixed dish was encountered, research was conducted to determine the commonly used ingredients in the dish and it was then added to the Mixed Dish list to ensure reliable coding of all Mixed Dishes. Condiments and preparation methods were not uniformly available in the meal reports of the primary study participants; therefore, these details were not coded. The preparation method for potatoes and meats (i.e. deep frying vs. not) was identified by the food name (i.e. French fries, fish sticks, etc.) and coded accordingly.
Table 1.
Details coded for each Meal Report
| Fruits |
|
| Vegetables |
|
| Grains |
|
| Protein |
|
| Dairy (& alternatives) |
|
| Sweets and Desserts (Non-dairy) |
|
| Beverages (Non-dairy) |
|
| Other |
|
Reliability of Coded Meals
Thirty randomly chosen meals from each of the samples were coded by four experts with graduate training in nutrition to test and refine the coding system. Any discrepancies were discussed and adjustments to the coding system or clarification in the coding instructions were made until all expert coders agreed on the coding for these 30 meals. The relative scores of the 30 meals were assessed qualitatively by the nutrition experts in order to ensure that meals ranked appropriately in terms of healthfulness. These results were used as the standard against which subsequent coders’ reliability was assessed. Coders were required to achieve a Kappa of greater than 0.7 for each item (listed in Table 1) for all of the 30 meals prior to coding the remainder of the meals.
Meal Report Scoring--The Healthy Meal Index
We consulted current dietary guidelines and recommendations for children to construct the scoring criteria for the Healthy Meal Index (HMI), including MyPlate, the Dietary Guidelines for Americans, and the American Heart Association (AHA) Dietary Guidelines (Gidding et al., 2006; U.S. Department of Agriculture & U.S. Department of Health and Human Servies, 2010). These guidelines recommend increased consumption of fruits, vegetables, especially dark green, red, and orange vegetables and legumes, whole grains, lean protein, low-fat dairy (or increasing calcium consumption), and foods high in healthy fats, such as fish. In addition, guidelines recommend decreased consumption of saturated and trans fat, fried foods, added sugars, sodium, and sugar sweetened beverages. No guideline was used as the sole basis for our metric, because each had been developed for a different purpose, e.g., to assess healthfulness of the overall diet, of foods consumed and/or to assess diets of adults. We systemically adapted elements from those that were applicable to measuring the healthfulness of foods served to children during a single meal. Many of the key recommendations overlapped and we prioritized those in creating the HMI. The 2010 US Dietary Guidelines were used as the primary determinant of the food groups to be included and the points awarded, but we made several modifications to accommodate the application of the HMI to a specific meal. Based on current feeding recommendations, we made the decision to give a set number of points for the availability of different types of foods served, rather than to award points based on the quantities of foods available. Despite the recommendation to consume low-fat dairy foods, we were unable to distinguish the fat content of dairy products in the meal reports, and we, therefore, did not include this in the HMI scoring.
The Healthy Meal Index (HMI) scoring was adapted from the Healthy Eating Index and the Alternative Healthy Eating Index, in accordance with the current dietary recommendations for young children (Chiuve et al., 2012; Gidding et al., 2006; Guenther et al., 2014; Nicklas & Hayes, 2008; U.S. Department of Agriculture & U.S. Department of Health and Human Services, 2010). At the time the HMI was being developed, the HEI-2010, which measures adherence to the 2010 Dietary Guidelines, had not yet been released (Guenther et al., 2013). We therefore utilized other existing dietary healthfulness indices as a basis for the scoring system, mimicking their point structures, but made changes to conform to the current dietary guidelines. Similar to these existing dietary quality indices, the HMI has 2 components: the HMI Adequacy Score (based on the presence of foods that are recommended for a healthy diet) and the HMI Moderation score (based on the absence of foods recommended to be consumed in moderation), which are summed to obtain the HMI Total score (higher scores indicate healthier meals). The scale for scores for each item was chosen in order to maintain consistency with the scoring systems utilized in the HEI and AHEI. Scoring details are provided in Table 2. When the HEI-2010 was published, we reviewed the HMI to ensure that it was consistent with the HEI-2010. SAS Version 9.3 was used to score the meals, based on the foods that were coded in the verbal meal reports. An individual food could fall into more than one category and would receive the appropriate points for each of the relevant categories. For example, fast food fried chicken would be categorized as a protein, an added or saturated fat, and a convenience food. The HMI Adequacy score has a potential range of 0 to 65, the HMI Moderation score has a potential range of 0 to 40, and the HMI Total score has a potential range of 0 to 105. Higher scores indicate better dietary quality. For this analysis, we calculated the mean HMI Adequacy, HMI Moderation, and HMI Total scores across the 3 meals, which were used as the outcome variables of interest.
Table 2.
Scoring criteria for Healthy Meal Index
| HMI components | Awarded Score1 | Definition | ||
|---|---|---|---|---|
| 0 | 5 | 10 | ||
| Adequacy Score | ||||
| Fruit | N | Y | Fruit, excluding juice | |
| Vegetables | N | Y | Vegetables, excluding fried potatoes | |
| Vegetable Quality | N | Y | Dark Green/Red/Orange Vegetables & Legumes | |
| Vegetable Variety | N | Y | ≥2 types of vegetables | |
| Grains | N | Y | Any whole or refined grain, excludes fried/salty snacks | |
| Whole Grains | N | Y | Any whole grain, excludes fried/salty snacks | |
| Dairy | N | Y | Dairy or dairy substitutes | |
| Protein | N | Y | Meat, nuts, legumes, eggs, meat substitutes | |
| Healthy Fats | N | Y | Fish, nuts, avocados | |
| Moderation Score | ||||
| Convenience Foods | Y | N | Take-out, fast food, prepackaged, and processed | |
| SSB or Diet Drinks | Y | N | Drinks with added sugar, diet drinks, flavored milk | |
| Added & Saturated Fats | Y | N | Fried foods, beef, pork | |
| Desserts & Sweets | Y | N | Foods with high added sugar | |
Y indicates the score awarded if the food was available at the meal and N indicates the score awarded if the food was unavailable.
Data Analysis
Validation Study
We consulted the validation report, “Development and Evaluation of the Healthy Eating Index 2005: Technical Report” to guide development of the HMI validation methods (Guenther et al., 2007). For the validation study, a trained research assistant entered all food details and quantities into NDSR. NDSR provided overall food group and nutrient data for each meal. We limited the sample to the 133 children who had been served a full meal (either lunch or dinner), excluding 4 children who were served a snack, breakfast, or unknown meal.
We utilized several tests to examine construct validity of the HMI. We assessed the distribution and spread of the Adequacy, Moderation, and Total scores with univariate statistics, including measurement of skewness and kurtosis. We then compared the HMI component scores to the NDSR-calculated total quantity of each food group or nutrient that the score was designed to measure with Spearman correlations. We also compared each of the HMI component scores and to the total caloric content of the meal using Spearman correlations to determine whether the index measured diet quality independent of quantity. Finally, we conducted Principal Component Analysis (PCA) of the HMI component scores to determine whether the HMI captured a multi-dimensional construct of healthfulness or was driven by one underlying dimension. In addition to the measures of construct validity, we and obtained the Cronbach’s alpha for scored components of the Adequacy, Moderation, and Total Scores in order to measure the internal consistency of the scores. All of the statistical analyses for the validation study were conducted in SPSS (Version 22, IBM Corp.).
Primary Study
For the primary study, we limited the sample to only those participants who responded to all 3 telephone calls reporting what was served for dinner (n =233). The sample that provided all 3 meal reports (n = 233) differed from the sample that did not (n = 68) in regard to maternal race/ethnicity and age: those included in the sample were more likely to be White/non-Hispanic (72% versus 53% not included in the sample, p=0.004) and of older parental age (31.6 vs 28.9 years, p=0.001). There was no difference in regard to maternal education or child age.
We examined the associations between the HMI and sociodemographic characteristics in order to inform the application of the HMI. We performed unadjusted bivariate associations of demographic characteristics- child age, child gender, parental race, and parental education- with HMI Adequacy, HMI Moderation, and HMI Total Scores. We then conducted adjusted linear regression models including all covariates simultaneously (child age, child sex, parental race/ethnicity, and parental education) to test the association of these covariates with each of the 3 HMI scores. All analyses were conducted in SAS (Version 9.3, 2011, SAS Institute Inc.).
Results
Validation Study
In the validation study, the Adequacy, Moderation, and Total meal scores demonstrated normal distributions with the following characteristics (Mean(SD), skewness, kurtosis): Adequacy: 34.5(11.7), −0.17, −0.28; Moderation: 22.1(10.6), 0.07, −0.82; and Total: 56.6(17.0), 0.19, −0.42. Each of the HMI component scores was highly correlated with the total quantity of the food group or nutrient it represented; absolute values for correlation coefficients ranged from 0.433 to 0.909, as shown in Table 3. The negative correlations reported for the Moderation component scores were expected, as those scores are based on the absence of the respective foods. None of the HMI component scores were highly correlated with total caloric content of the meal measured by NDSR; absolute values for correlation coefficients ranged from 0.00 to 0.277, as shown in Table 3. The Principal Component Analysis revealed 5 distinct factors with eigenvalues greater than 1.0. The Cronbach’s alpha scores for the components that constructed each score were 0.395 for Adequacy, 0.402 for Moderation, and 0.364 for Total.
Table 3.
Correlations between the HMI component scores and the total measured servings of foods or nutrients in the validation sample
| HMI Component Score | Validation Quantity from NDSR | Correlation with Validation Quantity1 | Correlation with Total Kilocalories for Meal2 |
|---|---|---|---|
| Fruit | Total servings of whole fruit | .909** | −.173* |
| Vegetables | Total servings of vegetables (excludes fried potatoes) | .849** | −0.047 |
| Vegetable Quality | Total servings of dark green, red/orange vegetables, legumes | .866** | 0.00 |
| Vegetable Variety | Total servings of vegetables (excludes fried potatoes) | .600** | −0.066 |
| Grains | Total servings of grains | .460** | 0.16 |
| Whole Grains | Total servings of whole grains | .647** | −0.021 |
| Dairy | Total servings of dairy | .791** | .277** |
| Protein | Total servings of meats, eggs, nuts, seeds, meat alternatives | .643** | −0.021 |
| Healthy Fats | Total servings of eggs, fish, shellfish, nuts, seeds, avocado | .871** | −0.094 |
| Convenience Foods | Sodium content of meal | −.433** | −.171* |
| SSB or diet drinks | Total SSB and diet drinks servings | −.674** | −.223** |
| Added & Saturated Fats | Total servings of high fat and fried meats, fried grains | −.615** | −.174* |
| Desserts & Sweets | Total servings of candies and desserts | −.744** | −0.12 |
Spearman correlation coefficients for relationship between HMI component score and validation quantity from NDSR
Spearman correlation coefficients for relationship between HMI component score and total kilocalorie content of meal, as measured by NDSR
Correlation is significant at p < 0.01 level (2-tailed).
Correlation is significant at p < 0.05 level (2-tailed).
Primary Study
In the primary sample of 233 parent-child dyads who self-recorded a home dinner, the number of families who served each of the components of the HMI out of the 3 recorded meals is shown in Table 4. The majority of meals contained a protein (76.4%), vegetable (56.2%), grain (54.5%) and/or a food high in added or saturated fats (52.4%). Fruits, whole grains, and foods high in healthy fats were rarely served; 64.4%, 86.3%, 82.0% of families did not serve them in any of the three meals, respectively. Most families served vegetables of higher quality (red/orange, dark green, or legumes), more than one vegetable, dairy, processed foods, SSB or diet drinks, and desserts or sweets in one or two, but not all three of the meals. Of the 100 meals utilized to test the accuracy of the meal report in comparison to the foods observed on the videotape, 77 meal reports of items served at the meal exactly matched the foods observed on the videotapes, excluding condiments. Of those that did not match exactly, 18 meal reports did not include items observed to be served on the video (omissions), while 3 included items not observed on the video (additions). In 2 of the videos the content of the meals could not be assessed due to poor framing of the video image. In families with 3 meal reports, the average change in mean Total HMI score across the three meals was 0.06 (SD: 1.67, range: −3.3, 3.3).
Table 4.
Frequency of families serving each food contributing to the HMI during the three recorded meals
| Number of Meals | ||||
|---|---|---|---|---|
| 0 % | 1 % | 2 % | 3 % | |
| Fruit | 64.4 | 20.2 | 11.2 | 4.3 |
| Vegetables | 2.2 | 9.9 | 31.8 | 56.2 |
| Vegetable Quality | 13.3 | 36.5 | 33.5 | 16.7 |
| Vegetable Variety | 23.6 | 34.3 | 27.9 | 14.2 |
| Grains | 0.4 | 12.0 | 33.1 | 54.5 |
| Whole Grains | 86.3 | 11.6 | 2.2 | 0.0 |
| Dairy | 7.7 | 19.7 | 37.3 | 35.2 |
| Protein | 0.9 | 4.7 | 18.0 | 76.4 |
| Healthy Fats | 82.0 | 13.3 | 3.4 | 1.3 |
| Processed Foods | 23.6 | 34.3 | 32.6 | 9.4 |
| SSB or Diet Drinks | 30.0 | 25.3 | 25.3 | 19.3 |
| Added and Saturated Fats | 3.4 | 11.6 | 32.6 | 52.4 |
| Desserts and Sweets | 0.0 | 79.8 | 17.2 | 3.0 |
The sample demographics and unadjusted bivariate associations with mean HMI scores are shown in Table 5. The mean HMI Adequacy score was 35.0 (SD: 7.5; range 13.3 to 58.3); mean HMI Moderation score was 22.7 (SD: 6.2; range 6.7 to 40.0); and the mean HMI Total score was 57.8 (SD: 10.1; range 30.0 to 86.7). Meals served to female children had higher HMI Moderation scores (p = .03). There were no significant associations of child age or parental race/ethnicity with any of the 3 HMI scores. Higher parental education was associated with higher HMI Adequacy (p=0.0005) and HMI Total (p=0.0009) scores.
Table 5.
Unadjusted bivariate associations with HMI scores
| N (%) | Adequacy Score | Moderation Score | Total Score | ||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | p | Mean (SD) | p | Mean (SD) | p | ||
| Child Age | 0.9 | 0.2 | 0.3 | ||||
| 4–5 years | 121 (51.9) | 35.0 (7.8) | 22.2 (5.8) | 57.1 (9.9) | |||
| 6–8 years | 112 (48.1) | 35.1 (7.3) | 23.3 (6.7) | 58.4 (10.3) | |||
| Child Sex | 0.6 | 0.03 | 0.08 | ||||
| Female | 114 (48.9) | 35.3 (7.9) | 23.6 (6.1) | 58.9 (9.8) | |||
| Male | 119 (51.1) | 34.8 (7.2) | 21.9 (6.3) | 56.6 (10.3) | |||
| Parental Race/Ethnicity | 0.3 | 0.9 | 0.4 | ||||
| Non-Hispanic white | 167 (71.7) | 35.4 (7.6) | 22.7 (6.1) | 58.1 (10.3) | |||
| Hispanic or non-white | 66 (28.3) | 34.2 (7.5) | 22.6 (6.6) | 56.8 (9.8) | |||
| Parental Education | <0.001 | 0.2 | <0.001 | ||||
| < High school | 107 (45.9) | 33.2 (7.1) | 22.2 (6.1) | 55.4 (9.0) | |||
| > High school | 126 (54.1) | 36.6 (7.6) | 23.2 (6.4) | 59.8 (10.6) | |||
The three adjusted linear regression models, including all covariates simultaneously, are shown in Table 6. In adjusted models, we found no difference in HMI scores by age or parental race/ethnicity. Female children had higher HMI Moderation scores (β(SE)=1.84 (0.82); p=0.02) and Total scores (β(SE)=2.5(1.3); p=0.05), but did not differ in HMI Adequacy scores. Parents with some education past high school served meals with higher mean HMI Adequacy scores (β(SE)=3.42 (0.97); p=0.001) and Total scores (β(SE)=4.43 (1.30); p=0.001), though no significant difference was seen in Moderation scores (β(SE)=1.02 (0.82); p=0.21).
Table 6.
Multiple linear regression models predicting HMI Adequacy, Moderation, and Total scores
| Adequacy | Moderation | Total | ||||
|---|---|---|---|---|---|---|
| β (SD) | p | β (SD) | p | β (SD) | p | |
| Child Age (mo) | 0.02 (0.06) | 0.76 | 0.04 (0.05) | 0.45 | 0.05 (0.1) | 0.48 |
| Child Sex | ||||||
| Female (vs. Male) | 0.7 (1.0) | 0.49 | 1.8 (0.8) | 0.02 | 2.5 (1.3) | 0.05 |
| Parental Race/Ethnicity | ||||||
| Non-Hispanic white (vs. not) | 1.1 (1.1) | 0.33 | −0.03 (0.9) | 0.97 | 1.0 (1.4) | 0.48 |
| Parental Education: | ||||||
| > High school (vs. < High school) | 3.4 (1.0) | <0.001 | 1.0 (0.8) | 0.21 | 4.4 (1.3) | <0.001 |
Discussion
This study presents the Healthy Meal Index, a tool for measuring the healthfulness of meals served at family mealtimes. The HMI is based on existing evidence and guidelines for defining a healthy diet in children. In addition, the HMI coding was easily applied with reliability following limited training and was shown to be a valid measure of meal healthfulness. We found that families served certain food groups more often than others, with higher reports of proteins, vegetables, and grains, and lower reports of fruits, whole grains, and foods high in healthy fats. Next, we examined how the measures of healthfulness derived using this tool are linked with demographic characteristics. We found that higher maternal education was associated with healthier meals served in terms of Adequacy, but not Moderation scores and that female children were served meals with higher Moderation scores.
We utilized several methods in order to test the validity and reliability of the HMI. First, in the construction of the HMI, we consulted several pediatric dietary guidelines and current dietary healthfulness indices, to ensure the content validity of the HMI as a measure (Chiuve et al., 2012; Gidding et al., 2006; Guenther et al., 2014; Nicklas & Hayes, 2008; U.S. Department of Agriculture & U.S. Department of Health and Human Services, 2010). Additionally, this was confirmed by measuring the Spearman correlation coefficients between the HMI component scores and total quantity of relevant foods and nutrients as measured by NDSR in the validation study. While the majority of components had very high correlations with measured servings, relatively low correlations were found for Total Grains and Convenience Foods. We did not have an equivalent measure of Convenience Foods available from NDSR and thus chose sodium as the best proxy measure. It was chosen due to the high sodium content of convenience foods; however, there are other contributors to the sodium content of meals than those foods classified into Convenience Foods. The low correlation found for Total Grains is likely due to the high variation in total grain quantity among meals that contained grains. The correlations between each component score and the total caloric content of the meal were low, demonstrating that the HMI is able to measure quality of meals, independent of quantity, which is desirable, as the HMI is intended to be measure of quality, not quantity. There were 5 factors identified by the PCA, demonstrating that the HMI measures more than one construct. While the Cronbach’s alpha scores were low for each of the component scores, the different components were intended to measure different constructs of the meal; this result was expected. Nutrition experts coded and scored 30 meals, which were used to qualitatively assess the construct validity of the HMI as a method for ranking meals in terms of healthfulness and also as a method for ensuring inter-rater reliability of the coders. Finally, we tested the validity of the meal reports by comparing the content of the meal reports to the content of 100 videotapes and found the content to match exactly in 77% of the meals. We surmise that in some of the videos with food omissions, those foods were not made available to the children during that meal.
A useful element of the HMI is that it differentiates between Adequacy and Moderation foods. We found different associations between demographic variables and food type that would not have been observed by characterizing only the overall meal healthfulness. This demonstrates that parental decision-making about providing Adequacy and Moderation foods may differ and that different factors may play a role in predicting each. Furthermore, when examining each component of the HMI, we found that certain healthful foods, such as proteins, vegetables, and grains were served with higher frequency. However, within each of these food groups, families were more likely to serve less healthy options; families served added and saturated fats at the majority of meals, yet rarely served healthy fats and almost never served whole grains. While families may be meeting basic guidelines about overall food groups, they also serve moderation foods frequently and miss opportunities to serve healthier varieties of foods.
In contrast to diet assessment using NDSR, which is an excellent choice for characterizing dietary intake in certain research studies, the HMI does not account for quantity of foods, only the availability of foods served to a child at a meal. There are several reasons why we chose not to include quantity of foods served in the HMI. First, assessing quantity served to a particular child is often difficult to do consistently across a wide variety of meal structures. For example, in a family-style meal, a large quantity of food is made available to all family members to share. In other meals, a child may or may not ask for additional servings of a food and that request may or may not be granted by a parent. These variations make standard measurement of quantity served difficult. Second, the HMI was developed primarily for use in scoring parents’ telephone reports of the foods served to a child; research staff were not present to observe and quantify foods. We minimized response burden for the parents by limiting the phone call length to 5 minutes. We had the opportunity to validate the HMI using data that had been collected in a different study during meals observed by a research assistant, but this was not true of the primary study. Finally, we sought to develop a tool which could be applied pragmatically to a variety of settings. NDSR indeed could be used by researchers to assess foods served at a meal, but is a labor-intensive, expensive program that requires personnel with advanced training and access to an NDSR license to complete. In contrast, use of the HMI does not require advanced training or purchase and maintenance of a license.
Previous research has found differences in diet quality by sociodemographic characteristics. By measuring the association of the HMI with these variables, we were able to assess whether or not our results were consistent with earlier reports. The observation that greater parental education was associated with higher HMI scores is consistent with prior literature, which has consistently found parental education to be associated with higher diet quality (Crawford et al., 1995; Rasmussen et al., 2006; Xie, Gilliland, Li, & Rockett, 2003). Another study using parental-reported survey data on foods usually served during meals also found higher education to be associated with healthier meals, including more vegetables and fewer servings of SSB and fast food (Neumark-Sztainer et al., 2014). The association between parental education and HMI scores should be further investigated in other studies; the healthfulness of meals served may be an important mediator of the association between lower parental education and lower quality dietary intake among their children.
The observation that parents serve healthier meals to girls is notable, and may reflect greater restriction of highly palatable foods among daughters compared to sons. Previous research has found that girls have higher diet quality than boys (Lorson, Melgar-Quinonez, & Taylor, 2009; Rasmussen et al., 2006; Torres, Santos, Orraca, Elias, & Palacios, 2014; Xie et al., 2003) and that they have a greater preference for healthier foods (Granner et al., 2004; Robinson & Thomas, 2004). Child gender has also been previously shown to be associated with parental feeding behavior (Fisher & Birch, 1999). In one experimental study overweight mothers served meals to boys that contained a higher content of food characterized as ‘unhealthy’ than in meals served to girls (Bouhlal, McBride, Ward, & Persky, 2015). Although we only saw differences in HMI Moderation Scores and not in Adequacy Scores, it is possible that the drivers of Adequacy scores may differ by child sex.
While we did not find any associations of race/ethnicity with HMI scores, previous literature on associations between race and diet quality in children has been mixed (Crawford et al., 1995; de Hoog et al., 2014; Erinosho et al., 2012; Kamphuis et al., 2006; Xie et al., 2003). This may indicate that differences in diet quality by race/ethnicity are driven by factors other than the healthfulness of meals served in the home. Another study of parental-reported survey data on usual meal content found that non-Hispanic white families served healthier meals than black families, but the difference between other racial/ethnic groups was not statistically different (Neumark-Sztainer et al., 2014). Furthermore, our study population was restricted to low income families attending Head Start programs; it is possible that some previous studies had unmeasured confounding by income (Kamphuis et al., 2006) or that we could not observe differences due to grouping all minorities into one category for statistical efficiency.
We did not find any association of child age with HMI scores; however, the child age range in this study was narrow. Previous studies of US children have shown that consumption of milk, fruits, and vegetables decreases with age (Kamphuis et al., 2006; Lytle, Seifert, Greenstein, & McGovern, 2000). It is possible that the overall dietary changes that occur throughout childhood are driven by changes in the school food environment and exposure to more foods outside the home as children age. In addition, the HMI measures whether or not specific foods are available to children, not quantities or consumption, therefore the differences others have observed in consumption may not be represented in differences in foods served by parents.
Strengths and Limitations
Characterization of the family meal has been previously limited due to the lack of a tool to measure the healthfulness of the foods served to children during meals. Although measures of dietary quality exist, these are primarily designed to measure intake and are not adequate for measuring the quality of foods served in all settings, such as those in which detailed meal data is not available. Recent research on child feeding suggests that controlling the quantity of foods served may constrain a child’s ability to self-regulate food intake. Therefore, we developed a tool that emphasizes, as do the current child feeding recommendations, the overall healthfulness of foods served.
The HMI provides an easy to use tool for assessing the dietary quality of meals served to young children and has potential for adaptation to a wide variety of settings. We have shown the HMI to be a reliable and valid measure to code a list of foods available at a meal by trained staff without use of specialized software. The HMI has the potential to be utilized for other applications, such as menus, where detailed information on preparation or ingredients may not be available. The HMI would need to be adapted for use in other studies that did not obtain a phone recall after the meal. Yet, if the food on the videotape is visible and identifiable, there is potential for use of the HMI. We found the 5-minute phone call easily added to our protocol, suggesting future observational studies could also incorporate the meal report in order to use the HMI.
The use of videotaped meals and meal reports to measure mealtime interactions in the home may provide a more accurate representation of behavior than parent self-reported feeding behavior, laboratory observations, or in-person home observations. Additionally, we prioritized reduction of respondent burden during the meal report and creation of a simple to use measure that could be widely applicable across settings where detailed meal data is not available. However, there is still the potential that parents may have adjusted the foods served to children or their behavior due to the knowledge of being observed. The nature of using self-reported data on the foods served at meals carries the limitation of recall or reporting bias by the parents. In this research context, parents may have been influenced by social desirability bias when choosing foods to serve or report. Parents’ interpretation of the question about which foods were available to the child during the meal may have varied, contributing to random error. Parental report also may have differed by ways meals were served to the child, such as pre-plated or family style.
Several assumptions were required in the coding and scoring of the meal reports. In general, all foods needed to be classified into groups for coding, so the variation within the groups was not accounted for in the scoring. Portion sizes were not assessed, although these have been shown to affect total intake in children by age five (Rolls, Engell, & Birch, 2000). The lack of preparation, condiment, and ingredient information may have limited our ability to measure all aspects of meal healthfulness; however we did capture the major components of the US Dietary Guidelines.
The validation of the HMI was an additional strength of this study. The validation study utilized NDSR, a widely accepted and utilized software program for nutrient analysis in research settings. However, because it accounts for ingredient choices, brands, and preparation methods, NDSR requires detailed food data which were not available in the self-recorded home meal observations; therefore, we utilized meal data from another meal observation study in which a research assistant was present to record all details about the foods available. To conduct the validation study, we utilized meal data collected in a sample of preschool children that was similar in terms of sociodemographic characteristics. We utilized an observation protocol in which trained research staff were present at the meal and recorded quantities, ingredients, and brand names of all of the foods served. This level of detail was not possible to collect during the parent-recorded home dinners, but appropriate to assess construct validity of the HMI. One limitation of the validation study protocol was that trained staff quantified foods visually, which is not as accurate as direct measurement by weight. Additionally, given the different study population and meal observation methods, there may be different correlations between HMI scores and the quantity of relevant foods and nutrients in the primary study, which we were unable to measure. Finally, we were unable to directly validate convenience foods, due to the lack of comparable variable(s) in NDSR. We chose to include convenience foods in the HMI Moderation score, as these are likely to contain higher levels of added sodium (Institute of Medicine, 2010). Other studies have found ‘fast foods’ to be associated with decreased diet quality and risk of obesity in children (Bowman, Gortmaker, Ebbeling, Pereira, & Ludwig, 2004; Paeratakul, Ferdinand, Champagne, Ryan, & Bray, 2003; Spence, Cutumisu, Edwards, Raine, & Smoyer-Tomic, 2009). Given the ubiquity of convenience products available in the grocery store (such as frozen pizzas, macaroni and cheese, fried chicken), which have comparable nutritional value to fast foods, we expanded this category to include all such foods. Correlations were lower than for other food groups, but within ranges generally regarded as adequate to demonstrate construct validity of self-report dietary measures in comparison with more objective measures (Willett, 2012).
Conclusions
We have provided a novel tool for child feeding research to measure meal healthfulness in a natural setting. Future research should examine the effects of the healthfulness of meals served during family mealtimes on children’s dietary quality and risk of obesity in longitudinal studies.
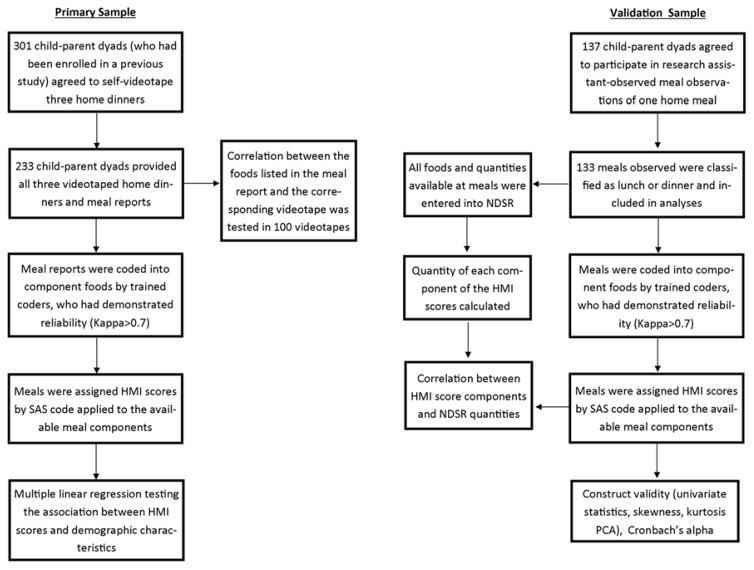
Figure 1.
Overview of Study Methods Conducted on the Primary and Validation Samples
Acknowledgments
This research was supported by grant numbers 5R01HD061356 and 1R01HD069179 of the National Institutes of Health. N. Kasper and S. Ball were supported in part by the University of Michigan Momentum Center: Driving Discovery to End Child Obesity.
References
- Berge JM, Rowley S, Trofholz A, Hanson C, Rueter M, MacLehose RF, Neumark-Sztainer D. Childhood Obesity and Interpersonal Dynamics During Family Meals. Pediatrics. 2014;134(5):923–932. doi: 10.1542/peds.2014-1936. http://doi.org/10.1542/peds.2014-1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Wall M, Hsueh T, Fulkerson JA, Larson N, Neumark-Sztainer D. The Protective Role of Family Meals for Youth Obesity: 10-Year Longitudinal Associations. The Journal of Pediatrics. 2015;166(2):296–301. doi: 10.1016/j.jpeds.2014.08.030. http://doi.org/10.1016/j.jpeds.2014.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmeier H, Skouteris H, Hetherington M. Systematic research review of observational approaches used to evaluate mother-child mealtime interactions during preschool years. The American Journal of Clinical Nutrition. 2015;101(1):7–15. doi: 10.3945/ajcn.114.092114. http://doi.org/10.3945/ajcn.114.092114. [DOI] [PubMed] [Google Scholar]
- Bouhlal S, McBride CM, Ward DS, Persky S. Drivers of overweight mothers’ food choice behaviors depend on child gender. Appetite. 2015;84:154–160. doi: 10.1016/j.appet.2014.09.024. http://doi.org/10.1016/j.appet.2014.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowman SA, Gortmaker SL, Ebbeling CB, Pereira MA, Ludwig DS. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics. 2004;113(1):112–118. doi: 10.1542/peds.113.1.112. http://doi.org/10.1542/peds.113.1.112. [DOI] [PubMed] [Google Scholar]
- Cason KL. Family mealtimes: more than just eating together. Journal of the American Dietetic Association. 2006;106(4):532–3. doi: 10.1016/j.jada.2006.01.012. http://doi.org/10.1016/j.jada.2006.01.012. [DOI] [PubMed] [Google Scholar]
- Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, … Willett WC. Alternative dietary indices both strongly predict risk of chronic disease. The Journal of Nutrition. 2012;142(6):1009–18. doi: 10.3945/jn.111.157222. http://doi.org/10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford PB, Obarzanek E, Schreiber GB, Barrier P, Goldman S, Frederick MM, Sabry ZI. The effects of race, household income, and parental education on nutrient intakes of 9- and 10-year-old girls NHLBI growth and health study. Annals of Epidemiology. 1995;5(5):360–368. doi: 10.1016/1047-2797(95)00033-4. Retrieved from http://www.sciencedirect.com/science/article/pii/1047279795000334. [DOI] [PubMed] [Google Scholar]
- de Hoog MLA, Kleinman KP, Gillman MW, Vrijkotte TGM, van Eijsden M, Taveras EM. Racial/ethnic and immigrant differences in early childhood diet quality. Public Health Nutrition. 2014;17(6):1308–17. doi: 10.1017/S1368980013001183. http://doi.org/10.1017/S1368980013001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erinosho TO, Berrigan D, Thompson FE, Moser RP, Nebeling LC, Yaroch AL. Dietary intakes of preschool-aged children in relation to caregivers’ race/ethnicity, acculturation, and demographic characteristics: Results from the 2007 California Health Interview Survey. Maternal and Child Health Journal. 2012;16(9):1844–1853. doi: 10.1007/s10995-011-0931-5. http://doi.org/10.1007/s10995-011-0931-5. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Hammons A, Grigsby-Toussaint D. Family mealtimes: A contextual approach to understanding childhood obesity. Economics and Human Biology. 2012;10(4):365–374. doi: 10.1016/j.ehb.2012.04.004. http://doi.org/10.1016/j.ehb.2012.04.004. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Restricting access to foods and children’s eating. Appetite. 1999;32(3):405–419. doi: 10.1006/appe.1999.0231. http://doi.org/10.1006/appe.1999.0231. [DOI] [PubMed] [Google Scholar]
- Fruh SM, Fulkerson JA, Mulekar MS, Kendrick LAJ, Clanton C. The Surprising Benefits of the Family Meal. Journal for Nurse Practitioners. 2011;7(1):18–22. http://doi.org/10.1016/j.nurpra.2010.04.017. [Google Scholar]
- Fulkerson JA, Larson N, Horning M, Neumark-Sztainer D. A review of associations between family or shared meal frequency and dietary and weight status outcomes across the lifespan. Journal of Nutrition Education and Behavior. 2014;46(1):2–19. doi: 10.1016/j.jneb.2013.07.012. http://doi.org/10.1016/j.jneb.2013.07.012. [DOI] [PubMed] [Google Scholar]
- Fulkerson JA, Neumark-Sztainer D, Story M, Gurvich O, Kubik MY, Garwick A, Dudovitz B. The Healthy Home Offerings via the Mealtime Environment (HOME) Plus study: Design and methods. Contemp Clin Trials. 2014;38(1):59–68. doi: 10.1016/j.cct.2014.01.006. http://doi.org/10.1016/j.biotechadv.2011.08.021.Secreted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George SM, Ballard-Barbash R, Manson JE, Reedy J, Shikany JM, Subar AF, … Neuhouser ML. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: evidence to inform national dietary guidance. American Journal of Epidemiology. 2014;180(6):616–25. doi: 10.1093/aje/kwu173. http://doi.org/10.1093/aje/kwu173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gidding SS, Dennison BA, Birch LL, Daniels SR, Gillman MW, Gilman MW, … Van Horn L. Dietary recommendations for children and adolescents: a guide for practitioners. Pediatrics. 2006;117(2):544–59. doi: 10.1542/peds.2005-2374. http://doi.org/10.1542/peds.2005-2374. [DOI] [PubMed] [Google Scholar]
- Granner ML, Sargent RG, Calderon KS, Hussey JR, Evans AE, Watkins KW. Factors of Fruit and Vegetable Intake by Race, Gender, and Age among Young Adolescents. Journal of Nutrition Education and Behavior. 2004;36(4):173–180. doi: 10.1016/s1499-4046(06)60231-5. http://doi.org/10.1016/S1499-4046(06)60231-5. [DOI] [PubMed] [Google Scholar]
- Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HAB, Kuczynski KJ, … Krebs-Smith SM. Update of the Healthy Eating Index: HEI-2010. Journal of the Academy of Nutrition and Dietetics. 2013;113:569–580. doi: 10.1016/j.jand.2012.12.016. http://doi.org/10.1016/j.jand.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guenther PM, Kirkpatrick SI, Reedy J, Krebs-Smith SM, Buckman DW, Dodd KW, … Carroll RJ. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. The Journal of Nutrition. 2014;144(3):399–407. doi: 10.3945/jn.113.183079. http://doi.org/10.3945/jn.113.183079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guenther PM, Reedy J, Krebs-smith SM, Reeve BB, Basiotis PP. Development and Evaluation of the Healthy Eating Index-2005 Technical Report Acknowledgments. 2007;2600 [Google Scholar]
- Hammons AJ, Fiese BH. Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics. 2011;127(6):e1565–e1574. doi: 10.1542/peds.2010-1440. http://doi.org/10.1542/peds.2010-1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetherington MM, Cecil JE, Jackson DM, Schwartz C. Feeding infants and young children. From guidelines to practice. Appetite. 2011;57:791–795. doi: 10.1016/j.appet.2011.07.005. http://doi.org/10.1016/j.appet.2011.07.005. [DOI] [PubMed] [Google Scholar]
- Hughes SO, Frankel LA, Beltran A, Hodges E, Hoerr S, Lumeng J, … Kremers S. Food parenting measurement issues: working group consensus report. Childhood Obesity (Print) 2013 Aug;(9 Suppl):S95–102. doi: 10.1089/chi.2013.0032. http://doi.org/10.1089/chi.2013.0032. [DOI] [PMC free article] [PubMed]
- Hughes SO, Patrick H, Power TG, Fisher JO, Anderson CB, Nicklas TA. The impact of child care providers’ feeding on children’s food consumption. Journal of Developmental and Behavioral Pediatrics: JDBP. 2007;28(2):100–7. doi: 10.1097/01.DBP.0000267561.34199.a9. http://doi.org/10.1097/01.DBP.0000267561.34199.a9. [DOI] [PubMed] [Google Scholar]
- Hughes SO, Power TG, Orlet Fisher J, Mueller S, Nicklas TA. Revisiting a neglected construct: parenting styles in a child-feeding context. Appetite. 2005;44(1):83–92. doi: 10.1016/j.appet.2004.08.007. http://doi.org/10.1016/j.appet.2004.08.007. [DOI] [PubMed] [Google Scholar]
- Hurley KM, Cross MB, Hughes SO. A Systematic Review of Responsive Feeding and Child Obesity in High-Income Countries. The Journal of Nutrition. 2011;141:495–501. doi: 10.3945/jn.110.130047. http://doi.org/10.3945/jn.110.130047.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Strategies to Reduce Sodium Intake in the United States. Washington DC: National Academies Press; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamphuis CBM, Giskes K, De Bruijn G, Wendel-vos W, Brug J, Van Lenthe FJ. Systematic Review Environmental determinants of fruit and vegetable consumption among adults: a systematic review. British Journal of Nutrition. 2006:620–635. http://doi.org/10.1079/BJN20061896. [PubMed]
- Kong A, Jones BL, Fiese BH, Schiffer LA, Odoms-Young A, Kim Y, … Fitzgibbon ML. Parent-child mealtime interactions in racially/ethnically diverse families with preschool-age children. Eating Behaviors. 2013;14(4):451–455. doi: 10.1016/j.eatbeh.2013.08.005. http://doi.org/10.1016/j.eatbeh.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson NI, Neumark-Sztainer D, Hannan PJ, Story M. Family meals during adolescence are associated with higher diet quality and healthful meal patterns during young adulthood. Journal of the American Dietetic Association. 2007;107(9):1502–10. doi: 10.1016/j.jada.2007.06.012. http://doi.org/10.1016/j.jada.2007.06.012. [DOI] [PubMed] [Google Scholar]
- Lorson BA, Melgar-Quinonez HR, Taylor Ca. Correlates of Fruit and Vegetable Intakes in US Children. Journal of the American Dietetic Association. 2009;109(3):474–478. doi: 10.1016/j.jada.2008.11.022. http://doi.org/10.1016/j.jada.2008.11.022. [DOI] [PubMed] [Google Scholar]
- Lumeng JC, Miller AL, Peterson KE, Kaciroti N, Sturza J, Rosenblum K, Vazquez DM. Diurnal Cortisol Pattern, Eating Behaviors and Overweight in Low-Income Preschool-Aged Children. Appetite. 2014;73:65–72. doi: 10.1016/j.appet.2013.10.016. http://doi.org/10.4049/jimmunol.0800997.Chronic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle LA, Seifert S, Greenstein J, McGovern P. How Do Children’s Eating Patterns and Food Choices Change Over Time? Results from a Cohort Study. American Journal of Health Promotion. 2000;14(4):222–228. doi: 10.4278/0890-1171-14.4.222. http://doi.org/10.4278/0890-1171-14.4.222. [DOI] [PubMed] [Google Scholar]
- Marshall S, Burrows T, Collins CE. Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. J Hum Nutr Diet. 2014:1–22. doi: 10.1111/jhn.12208. http://doi.org/10.1111/jhn.12208. [DOI] [PubMed]
- Neumark-Sztainer D, MacLehose R, Loth K, Fulkerson JA, Eisenberg ME, Berge J. What’s for dinner? Types of food served at family dinner differ across parent and family characteristics. Public Health Nutrition. 2014;17(1):145–155. doi: 10.1017/S1368980012004594. http://doi.org//S13689800124594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicklas TA, Hayes D. Position of the American Dietetic Association: Nutrition Guidance for Healthy Children Ages 2 to 11 Years. Journal of the American Dietetic Association. 2008;108(6):1038–1047. doi: 10.1016/j.jada.2008.04.005. http://doi.org/10.1016/j.jada.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Ogata BN, Hayes D. Position of the academy of nutrition and dietetics: Nutrition guidance for healthy children ages 2 to 11 years. Journal of the Academy of Nutrition and Dietetics. 2014;114:1257–1276. doi: 10.1016/j.jand.2014.06.001. http://doi.org/10.1016/j.jand.2014.06.001. [DOI] [PubMed] [Google Scholar]
- Paeratakul S, Ferdinand DP, Champagne CM, Ryan DH, Bray Ga. Fast-food consumption among US adults and children: Dietary and nutrient intake profile. Journal of the American Dietetic Association. 2003;103(10):1332–1338. doi: 10.1016/s0002-8223(03)01086-1. http://doi.org/10.1016/S0002-8223(03)01086-1. [DOI] [PubMed] [Google Scholar]
- Rasmussen M, Krølner R, Klepp KI, Lytle L, Brug J, Bere E, Due P. Determinants of fruit and vegetable consumption among children and adolescents: a review of the literature. Part I: Quantitative studies. The International Journal of Behavioral Nutrition and Physical Activity. 2006;3(22):1–19. doi: 10.1186/1479-5868-3-22. http://doi.org/10.1186/1479-5868-3-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee K. Childhood Overweight and the Relationship between Parent Behaviors, Parenting Style, and Family Functioning. The ANNALS of the American Academy of Political and Social Science. 2008;615(1):11–37. http://doi.org/10.1177/0002716207308400. [Google Scholar]
- Robinson CH, Thomas SP. The Interaction Model of Client Health Behavior as a Conceptual Guide in the Explanation of Children’s Health Behaviors. Public Health Nursing. 2004;21(1):73–84. doi: 10.1111/j.1525-1446.2004.21110.x. http://doi.org/10.1111/j.1525-1446.2004.21110.x. [DOI] [PubMed] [Google Scholar]
- Rolls BJ, Engell D, Birch LL. Serving portion size influences 5-year-old but not 3-year-old children’s food intakes. Journal of the American Dietetic Association. 2000;100(2):232–4. doi: 10.1016/S0002-8223(00)00070-5. http://doi.org/10.1016/S0002-8223(00)00070-5. [DOI] [PubMed] [Google Scholar]
- Shanthy A, Lino M, Gerrior SA, Peter P. The Healthy Eating Index, 1994–96 1998 [Google Scholar]
- Skafida V. The family meal panacea: exploring how different aspects of family meal occurrence, meal habits and meal enjoyment relate to young children’s diets. Sociology of Health & Illness. 2013;35(6):906–23. doi: 10.1111/1467-9566.12007. http://doi.org/10.1111/1467-9566.12007. [DOI] [PubMed] [Google Scholar]
- Spence JC, Cutumisu N, Edwards J, Raine KD, Smoyer-Tomic K. Relation between local food environments and obesity among adults. BMC Public Health. 2009;9:192. doi: 10.1186/1471-2458-9-192. http://doi.org/10.1186/1471-2458-9-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres R, Santos E, Orraca L, Elias A, Palacios C. Diet quality, social determinants, and weight status in Puerto Rican children aged 12 years. Journal of the Academy of Nutrition and Dietetics. 2014;114(8):1230–5. doi: 10.1016/j.jand.2014.01.011. http://doi.org/http://dx.doi.org/10.1016/j.jand.2014.01.011 show. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture, & U.S. Department of Health and Human Services. Dietary Guidelines for Americans. 2010. [Google Scholar]
- United States Department of Agriculture. 2013 ChooseMyPlate.gov.
- Vereecken C, Haerens L, De Bourdeaudhuij I, Maes L. The relationship between children’s home food environment and dietary patterns in childhood and adolescence. Public Health Nutrition. 2010;13(10A):1729–35. doi: 10.1017/S1368980010002296. http://doi.org/10.1017/S1368980010002296. [DOI] [PubMed] [Google Scholar]
- Videon TM, Manning CK. Influences on adolescent eating patterns: the importance of family meals. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2003;32(5):365–73. doi: 10.1016/s1054-139x(02)00711-5. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12729986. [DOI] [PubMed] [Google Scholar]
- Welsh EM, French Sa, Wall M. Examining the Relationship Between Family Meal Frequency and Individual Dietary Intake: Does Family Cohesion Play a Role? Journal of Nutrition Education and Behavior. 2011;43(4):229–235. doi: 10.1016/j.jneb.2010.03.009. http://doi.org/10.1016/j.jneb.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett W. Nutritional Epidemiology. 3. Oxford Univ Press; 2012. [Google Scholar]
- Xie B, Gilliland FD, Li YF, Rockett HR. Effects of Ethnicity, Family Income, and Education on Dietary Intake among Adolescents. Preventive Medicine. 2003;36(1):30–40. doi: 10.1006/pmed.2002.1131. http://doi.org/10.1006/pmed.2002.1131. [DOI] [PubMed] [Google Scholar]