Abstract
Intracranial haemorrhages, including intracerebral haemorrhage (ICH), intraventricular haemorrhage (IVH) and subarachnoid haemorrhage (SAH), are leading causes of morbidity and mortality worldwide. In addition, haemorrhage contributes to tissue damage in traumatic brain injury (TBI). To date, efforts to treat the long-term consequences of cerebral haemorrhage have been unsatisfactory. Incident rates and mortality have not showed significant improvement in recent years. In terms of secondary damage following haemorrhage, it is becoming increasingly apparent that blood components are of integral importance, with haemoglobin-derived iron playing a major role. However, the damage caused by iron is complex and varied, and therefore, increased investigation into the mechanisms by which iron causes brain injury is required. As ICH, IVH, SAH and TBI are related, this review will discuss the role of iron in each, so that similarities in injury pathologies can be more easily identified. It summarises important components of normal brain iron homeostasis and analyses the existing evidence on iron-related brain injury mechanisms. It further discusses treatment options of particular promise.
Keywords: Brain, Hemorrhage, Subarachnoid
Introduction
Iron is a crucial nutrient for multiple biological functions, including, but not limited to, oxygen transport, electron transport, redox reactions, cell division, nucleotide synthesis and myelination.1 In the brain, iron homeostasis is of critical importance, and dysregulation can lead to serious neurodegenerative diseases such as Alzheimer's disease,2 Parkinson's disease3 and Hallerorden-Spatz syndrome.4 However, while much research has focused on understanding metal homeostasis in these diseases, the role of iron accumulation following intracranial haemorrhage (ICrH) and traumatic brain injury (TBI) has yet to be fully determined. ICrH is broadly defined as bleeding within the cranium, and has an incident rate of ∼40 per 100 000 people/year.5 ICrH can be subdivided into intracerebral haemorrhage (ICH), intraventricular haemorrhage (IVH) or subarachnoid haemorrhage (SAH). In addition, while TBI is not considered one of these subdivisions, it is often accompanied by ICrH. All forms of ICrH carry high mortality rates and poor prognosis. Injury following haemorrhage can be categorised into primary injury, sustained during the initial haemorrhage, and secondary injury, referring to subsequent and long-term damage due to other factors.
Over the past decade, interest in identifying the mechanisms of secondary injury after haemorrhage has spiked, and several specific blood components have been identified as being integral to this phase of damage.6 In particular, haemoglobin (Hb)-derived iron is thought to play an important role. Previous reviews have either generally discussed all blood components7 or specifically focused on one form of ICrH.8 This review focuses on the role iron accumulation plays in secondary damage following the entire spectrum of ICrH: ICH, SAH, IVH and TBI-induced haemorrhage, and assesses potential therapeutic options.
Iron homeostasis in normal brain
Because of its potential toxicity, iron content is tightly regulated in the brain. Little is found as the free ferric (Fe3+) or ferrous (Fe2+) ion. Some is bound to small organic molecules such as citrate, ATP or ascorbic acid.9 Iron is also an important component of many proteins.10 Thus, for example, it is an essential component of cytochromes a, b and c and cytochrome oxidase and other enzymes. There are also iron–sulphur clusters in Complex I and II of the electron transport chain. In some proteins, including neuroglobin and Hb, iron is bound in the form of haem. This section describes the regulation of these iron pools. Because of the importance of the latter in cerebral haemorrhage, regulation of haem iron will be reviewed separately.
Non-haem-bound iron
Brain iron homeostasis involves regulation of iron movement between blood and brain, between brain intracellular and extracellular spaces and between different iron pools within such spaces. The movement of iron across cell membranes requires specific transport systems. Under normal conditions, the most important uptake mechanism is the transferrin–transferrin receptor system (Tf–TfR). Transferrin (Tf) is an 80 kDa glycoprotein with high affinity for iron,11 with mRNA expression in oligodendrocytes, neurons and astrocytes. Once expressed, Tf scavenges free iron in the extracellular space. Tf binds to Fe3+ and, after binding to membrane TfR, undergoes endocytosis.12 The endosome is then acidified, releasing the Fe3+ and reducing it to the Fe2+ state.13 Once reduced, the iron is released from the endosome into the cytoplasm by Divalent Metal Transporter 1 (DMT1), a protein that is widely expressed and which is capable of transporting a broad range of divalent and trivalent ions, including iron, zinc, manganese, cobalt, cadmium, copper, nickel and lead.12 This cytosolic iron, also known as the labile iron pool, is largely contained within lysosomes and is in constant equilibrium with an iron-binding protein, ferritin (Ft).14 Ft is highly stable at a wide range of temperatures and acidities, and sequesters Fe2+ ions in ferroxidase centres of the Ft subunits. These ferroxidase centres have the important ability to consume all reagents of the radical Fenton reactions (see the Brain iron overload and toxicity section) and thereby inhibit iron-mediated oxidative stress.15 Ft is expressed in microglia and macrophages, but it is also found in some neurons.16 Should Ft levels become saturated, iron can be transported out into the cerebral interstitial fluid by ferroportin 1 (FP1). In conjunction with such transport, the toxic Fe2+ is oxidised to Fe3+ by the multicopper ferroxidase ceruloplasmin (CP) so that it can be bound more easily by transferrin once in the extracellular space. FP1 is stabilised by the amyloid precursor protein (APP), but the role of APP in iron transport is still a matter for debate.17 Duce et al18 suggested that neuronal APP possesses ferroxidase capabilities stronger than even Ft. However, this group recently demonstrated that APP lacks ferroxidase capabilities but remains essential for FP1 persistence on the neuronal surface, thereby supporting iron export from neurons.17 The precise mechanism by which it stabilises FP1, however, is undetermined.
Other iron transport systems
The systems described above are not the only iron transport systems present in the brain. Iron is also a substrate for some zinc transporters, such as the Zip8 and Zip14 pathways.19 Other iron transporters include the lactoferrin–lactoferrin receptor system in neurons20 and the melanotransferrin system, which is expressed in active microglia.21 However, these have not been the topic of much research in the realm of brain haemorrhage or TBI, with the exception of Terent et al.22
Regulation of iron homeostasis
The Tf–TfR import system, the Ft sequestering system and the FP1-CP exporter system are relatively ubiquitous throughout the brain. Regulation of these systems is predominantly controlled by iron regulatory proteins, IRP-1 and IRP-2. These proteins bind to an iron-responsive element, a relatively conserved specific hairpin loop in the 5′-UTR of the mRNA coding region of a number of iron-related proteins, including Ft, aconitase, APP, FP1, HIF2α and others.1 23 By binding to this hairpin loop, IRPs reduce mRNA expression.24 The IRPs are themselves inhibited by iron; as such, elevated intracellular iron results in elevated Ft and FP1 transcription, allowing greater sequestering and export of iron.25 Conversely, when iron levels are low, Ft and FP1 expression is inhibited, reducing the amount of energy wasted on unnecessary protein synthesis. In addition, IRPs bind to TfR and DMT1 mRNA, but in this case, they stabilise the mRNA and increase expression, thus allowing greater levels of iron influx during times of insufficient intracellular iron.1 26 The factors that play a role in this apparent dichotomy of IRP function have yet to be fully elucidated.
In addition to IRPs, the protein hepcidin is responsible for internalisation of FP1 and modulation of CP and DMT1 in the cerebral cortex and hippocampus.27 28 Therefore, it can cause iron accumulation within the cell when overexpressed.29 Hepcidin expression is increased in response to cellular iron overload and inflammation.30 It is therefore a potential therapeutic target in a variety of iron-related neurodegenerative disorders.
Haem-bound iron
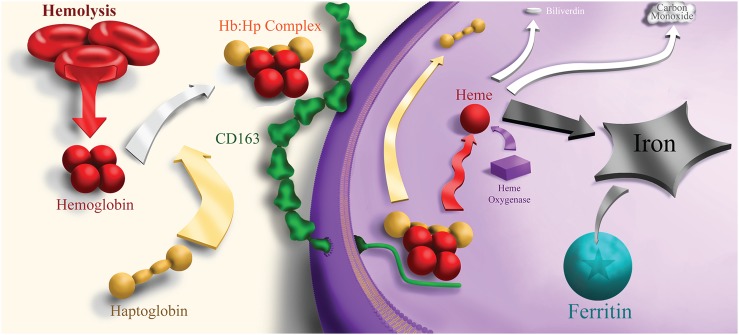
In order to understand the posthaemorrhagic effects of iron, it is important to understand the iron homeostasis in normal brain. Brain iron is present in one of the two forms: haem-bound or non-haem-bound. Haem is the core moiety of Hb and refers to a protoporphyrin IX scaffold supporting an Fe2+ central atom. Haem-bound iron is transported via a variety of transportation pathways. Predominant among them is the Hb-haptoglobin (Hp)-CD163 pathway (figure 1). Hb, the oxygen-carrying protein, contains about 70% of whole-body iron in its haem cores.31 It is not limited to erythroid cells, but rather it can be expressed in a wide range of glial cells, macrophages and neurons within the central nervous system.32–35 Within neurons, Hb may act as an oxygen reservoir and control mitochondrial function.36 While normally stored intracellularly, Hb is occasionally released from cells during haemolysis. This free extracellular Hb is subsequently scavenged by the protein Hp, an abundant plasma glycoprotein that binds to Hb with incredibly high affinity.37 Hp is a tetrameric, α2β2 serine protease, in which the α domain is responsible for dimer and multimer formations (Hp 1–1, 2–1 and 2–2 phenotypes), whereas the β subunit binds to Hb and Hp receptors after the Hb naturally dissociates into dimers.38 This newly formed complex is redox-inactive, with Hp assisting in diffusing any radical chemistry that may occur following H2O2 attack (see the Mitochondrial damage section).39
Figure 1.
Haemolysis and haemoglobin degradation after brain haemorrhages.
This complex has a high affinity for the membrane-bound receptor CD163, a 130 kDa transmembrane member of the scavenger receptor cysteine-rich domain-containing protein family. Binding of the Hb:Hp complex to CD163 results in endocytosis, preventing accumulation of Hb in the extracellular space.40 The regulatory mechanism of CD163 in the brain is not well understood, though it is apparent that it is upregulated following vascular compromise, inflammation and by the presence of Hp:Hb complexes.41 42 CD163 is shed from the cell membrane by ADAM17, a membrane-bound serine protease responsible for a variety of cell signalling, including TNF-α and Aβ formation in Alzheimer's disease.43–45 This ‘soluble’ CD163 is composed of 94% of the protein's ectodomain and is an inflammatory biomarker. CD163 has long been viewed as a monocyte/macrophage marker, expressed exclusively within that cell line. However, recent in vivo findings demonstrated that following IVH, hippocampal neurons express CD163.46 This finding has been corroborated and extended to cortical neurons by Chen-Roetling and Regan.47
Following endocytosis, the Hb:Hp complex dissociates, allowing Hb to be degraded to haem inside endosomes48 49 (figure 1). Inside the cell, haem can be bound by one of several haem-binding proteins,50 whose roles in ICrH have not yet been investigated, or it can be degraded by haem oxygenase (HO) proteins (the inducible HO-1 or the constitutively expressed HO-2). HO-1 mRNA expression is increased significantly by the presence of haem as well as a variety of other proinflammatory signal molecules.51 HO proteins degrade haem into carbon monoxide, biliverdin and Fe2+.52 The biliverdin is converted to bilirubin (an antioxidant known to be neurotoxic in preterm neonates) by biliverdin reductase,53 54 while the iron is bound by Ft and sequestered.
Intracerebral haemorrhage
Introduction
ICH describes bleeding into the brain parenchyma due to the rupture of a cerebral blood vessel. Of the ICrH subtypes, ICH is the most common, accounting for ∼10–20% of all strokes.55 ICH can either be secondary or primary. Secondary ICH refers to bleeding caused by a pre-existing condition, such as a tumour, whereas primary ICH is a vessel rupture without an underlying lesion, with hypertension being a major cause. ICH incidence has not altered in the past three decades, being stable at ∼25 per 100 000 person-years.56 Of note, Asian populations are at significantly higher risk of ICH than non-Asian populations. Prognosis is very poor, with death occurring within 1 month in over 40% of cases.57 It is therefore of pressing concern to identify therapeutic targets for ICH. There is a substantial body of preclinical evidence that iron plays a role in ICH-induced injury8 and, in patients suffering from ICH, high-serum levels of Ft are independently associated with poor outcome.58
Iron transport into the cell
Haemoglobin
In ICH, erythrocytes are released into the brain parenchyma, where they lyse within hours/days, releasing their components, including Hb, into the extracellular space.59 This Hb may be scavenged by Hp and endocytosed by CD163 into macrophages and monocytes as described above. The Hp is produced locally in the brain by oligodendrocytes.60 However, recent findings suggest that Hp may also exacerbate neuronal vulnerability to Hb-mediated iron toxicity.47 That study suggests that Hp increases the ability for haem-bound iron to gain access to neurons via CD163, thereby increasing neurotoxicity. In contrast to glial cells, neurons have low Ft levels and thus lack sufficient iron buffering to handle the amount of Hb-derived iron.47 61 62
Haem
Hb that is not scavenged immediately degrades and releases haem.59 Haem can react with lipid peroxide-generated hydrogen peroxides according to the Fenton reactions, leading to the formation of reactive oxygen species (ROS).63 64 To prevent this, extracellular haem is bound by haemopexin,65 a 60 kDa glycoprotein that is normally not expressed in brain parenchyma,66 but which is induced after ICH.67 The resultant haem–haemopexin complex can be taken up into cells via CD91 (also known as low-density lipoprotein receptor-related protein, LRP1) and metabolised by HO proteins.68
CD91 is widely expressed in brain cell types, including in glial cells, macrophages and neurons.69 The haemopexin-CD91 pathway is, therefore, another potential mechanism by which iron can access neuronal cells. After endocytosis, haemopexin is degraded within the lysosome, and consequently, decreases in plasma haemopexin concentration occur in severe haemolysis seen during ICH.70 71 Normally, the iron released by this degradation is stored in Ft and inhibits IRPs, thus stimulating a variety of iron-related proteins, including APP.72 However, excessive levels of intracellular haem can result in overuse and quick degradation of Ft, resulting in the formation of haemosiderin, an intracellular insoluble iron storage complex.73 74 Haemosiderin is a major location of iron accumulation and is used as a marker for haemorrhagic injury.75 Haem–haemopexin complexes also increase the endogenous levels of holo-APP, as well as HO-1.76 Deletion of the haemopexin gene aggravates injury following ICH.77 78
Brain iron overload and toxicity
While the iron homeostatic mechanisms function well in normal physiological conditions, the amount of Hb released into the extracellular space following haemorrhage may overwhelm these iron-handling systems. Saturation of these systems, or iron overload, can result in the presence of iron in a form where it can participate in harmful reactions; for example, free radical production.
Mechanisms of iron toxicity
Iron toxicity is generally thought to result from the generation of free radicals via the Fenton reaction. In that reaction, ferrous iron reacts with hydrogen peroxide to form radical oxygen species according to the reaction below:
The resulting ferric iron can be reduced back to Fe2+ by a variety of reducing agents and thereby regenerate the starting reagents. In this way, the radical reaction cycle can begin again. Some cellular antioxidants like GSH and superoxide dismutase work to limit this damage, but these antioxidants have limited efficacy to combat the amount of oxidative stress during ICH.79 80
Mitochondrial damage
The oxidative damage resulting from such iron overload targets the mitochondrial inner membrane.81 82 Iron overload in HT-22 hippocampal neurons induces mitochondrial fragmentation that is dependent on dephosphorylation of dynamin-related protein 1 (Drp1), a mitochondrially localised GTPase, which controls mitochondrial fission.83 84 This mitochondrial fission is closely regulated by Calcineurin phosphatase signal pathways,85 86 which are also affected by iron overload.83
Oedema
Iron overload also induces significant perihaematomal oedema. Oedema has been repeatedly shown to be associated with poor outcome after ICH.87 88 In clinical studies, serum Ft is often used as an estimate of the body's iron load.89 90 Serum Ft levels are highly correlated to perihaematomal oedema volumes following ICH;91–94 while this is most likely because it reflects elevated iron levels, it has been proposed that serum Ft could play a role as an iron-independent proinflammatory signalling molecule in hepatic stellate cells.95 There has been no research to assess whether it could play an equivalent role in the brain. Nevertheless, iron overload has been shown to increase brain water content following ICH.96 Important to the formation of cerebral oedema is aquaporin 4 (AQP4), one of the most abundant water channel proteins in the brain.97–99 AQP4 is mostly expressed in astrocyte foot processes99 100 around blood vessels where it plays critical roles in brain water homeostasis. Increased expression of AQP4 is found in ICH,101 and there is a high correlation between iron accumulation and AQP4 expression.102 AQP4 is known to be regulated by metal ions such as mercury,103 but it is unknown whether iron has similar effects.
Cell death
The above-described damage culminates in widespread glial and neuronal cell death. This cell death is therefore intrinsically linked to its iron source. The form of cell death is not purely necrotic. Ferrous citrate infusion (designed to simulate post-ICH iron overload) results in increased LC3-II expression and autophagic cell death, as assessed by BECN1 staining.104 LC3-II is the activated conjugate of microtubule-associated protein 1A/1B light chain-3, and it is recruited to autophagosomal membranes, thereby being a key marker of autophagic cell death.105 Iron-induced autophagy following ICH has been documented previously,106 though the mechanism by which iron enhances autophagy is not fully understood. Autophagy is induced by oxidative stress, which has linked HO-1 (a marker for such stress) to this type of cell death following iron overload.107 During ICH, it is possible that HO-1 promotes the intracellular release and capture of redox-reactive iron, thereby promoting autophagy.108 Inhibition of autophagy leads to protection against iron-induced neurodegeneration.109–111
Apoptosis of neurons and astrocytes has also been identified after ICH.112 113 Haem alone can induce apoptotic cell death in neuronal cells (as identified by DNA fragmentation, caspase activation and mitochondrial membrane disruption).114 Such apoptosis is potentially related to a member of the high-temperature requirement (Htr) family, HtrA2, a mitochondrially located serine protease which, on release into the cytoplasm, contributes to apoptosis via caspase-dependent and caspase-independent pathways. Haem incubation of PC12 neuroblastoma cells resulted in HtrA2-mediated apoptosis.115 A variety of other apoptotic pathways have been proposed following ICH, including SSTR1, bcl-2, CHMP4B, ESCRT-III, VCAM1 and c-Fos,116–119 but their links (if any) to iron have not yet been identified.
Another form of regulated cell death of note is ferroptosis, an iron-dependent form of cell death distinct from autophagy, apoptosis, necrosis and other forms of cell death.120 On accumulation of lipid ROS, the RAS Selective Lethal proteins erastin and RSL3 mediate cell death that is critically dependent on iron (but not other divalent metals).121 However, research on ICH-induced ferroptosis has been significantly hindered by a lack of easily identifiable markers. Chang et al122 found that ICH increases ferroptosis-related gene expression (including IRP2), and that this expression could be ameliorated by treatment with (-)-epicatechin, a scavenger of free radicals and other pro-oxidants, that activates the Nrf2 signalling pathway, a master regulator of antioxidant defence mechanisms. However, besides that study, there has been a lack of successful studies investigating the ability of ICH-induced iron overload to activate ferroptotic pathways. Given the emphasis on the iron-dependent nature of ICH and ferroptosis, this may be a fertile field of inquiry.
Vicious cycle of iron accumulation
In haemorrhagic transformation after cerebral ischaemia, iron overload may engage in a vicious cycle. Cerebral ischaemia causes a shift to glycolytic from oxidative metabolism, lactic acid production and marked decreases in brain pH. Iron can be released from Ft following exposure to decreased pH, superoxide radicals and ascorbate123–126 and it may then damage mitochondria further inhibiting oxidative metabolism and result in the production of free radicals. In turn, this may cause further release of iron, a vicious cycle. The extent to which this occurs in ICH, SAH and IVH is uncertain and merits investigation.
Intraventricular haemorrhage
Introduction
IVH is defined by the presence of bleeding into the brain ventricular system. It is particularly common in preterm neonates (in such cases, the bleeding often originates from the germinal matrix and therefore, IVH is sometimes referred to as germinal matrix haemorrhage) and carries with it high morbidity and mortality. Over 12 000 premature infants develop IVH every year in the USA,127 and the incidence has increased over the last 20 years.7 IVH is also often a complication of other ICrH subtypes; 50% of patients with primary ICH and 45% of patients with SAH develop IVH.128 129 Despite this, IVH is probably the least studied and therefore least well-understood subtype of ICrH.
Iron in IVH
In IVH, blood can disperse within the ventricular system. Unlike in ICH, where iron has the greatest effects on perihaematomal tissue, in IVH blood-derived Hb and iron can have effects distant from the initial bleed. A significant proportion of the iron within the ventricular cerebrospinal fluid (CSF) following IVH is free or non-protein-bound,130 allowing it to engage in Fenton reactions. This iron eventually accumulates in the ependymal and subependymal regions as evidenced by the increase in Ft expression and iron deposition in those cells.131 132 In addition, after lysed red blood cell injection into the ventricles in a rat, periventricular HO-1 was upregulated, while iron injection resulted in ependymal cell injury with mitochondrial swelling and loss of cilia.132 The subventricular zone, a site of ongoing neuronal proliferation, became overloaded with iron following Hb injection in neonatal rats.133 IVH has been shown to cause substantial damage to the bordering hippocampus in an iron-dependent fashion.134 This damage has been identified as hydrocephalus-independent and possibly mediated by iron-activated c-Jun Kinase apoptotic pathways.46
Choroid plexus
One potentially important site of damage following IVH is the choroid plexus epithelium. The choroid plexuses are present in the lateral, third and fourth ventricles of the brain. They form a unique blood–CSF barrier and are the predominant CSF-generating tissue. TfR is present on choroid plexus epithelial cells and iron is localised to these cells in healthy brains.135 136 These cells are highly responsive to ischaemic insult, and subsequent choroid plexus cell death results in increased permeability of the blood–CSF barrier to a variety of proinflammatory cytokines and leucocytes,137 and decreased production of trophic factors.138 Choroid plexus cells express AQP1, which is involved in CSF production.139 However, following intraventricular injection of Hb to simulate IVH, AQP1 protein levels increased significantly and there was also an upregulation of AQP5, conveying a high degree of water permeability.140 In addition, Hb intraventricular injection resulted in ultrastructural damage to the choroid plexus that was accompanied by oxidative stress, cellular activation and an inflammatory response.141 This damage to the blood–CSF barrier, in addition to the increase in AQP expression, suggests that iron may cause increased CSF production by the choroid plexus.
Posthaemorrhagic hydrocephalus
Posthaemorrhagic hydrocephalus (PHH) is a common complication of IVH and the role of iron in PHH has been a topic of interest recently. It has been demonstrated repeatedly that iron is intimately involved in PHH.132 133 142 The mechanism underlying this action is not well understood. Potential mechanisms involve an increase in choroid plexus production of CSF and obstruction of CSF flow pathways. Meng et al143 have proposed that iron-mediated upregulation of the Wnt signalling pathway, which regulates fibrosis, is involved. However, this is clearly an area in which additional investigation would have significant impact into the development of treatments for PHH.
Subarachnoid haemorrhage
Introduction
SAH is defined by the presence of blood in the CSF in the subarachnoid space between the arachnoid membrane and the pia mater. It is most frequently occurs following the rupture of an intracranial aneurysm.144 Mortality rates are extremely high, estimated at between 40% and 50%,145 with incident rates of up between 2 and 32/100 000.146 SAH causes early and late brain injury, the latter being associated with delayed cerebral vasospasm.
Iron in SAH
SAH-induced damage within the first 72 hours of ictus is classified as early brain injury and iron plays an integral role in such injury. Following SAH, erythrocytes lyse and release their components into the subarachnoid space, exposing the brain to high concentrations of Hb. The Hb is promptly broken down to haem extracellularly. The haem–haemopexin scavenging has been demonstrated to be active and potentially harmful following SAH. CD91, the receptor for haemopexin, is positively correlated with iron deposition in brain tissue, which in turn is negatively correlated with neurological outcome.68 This system may be responsible for intracellular accumulation of iron that results following SAH. Non-haem iron and Ft levels in the brain and CSF increase progressively for the first 72 hours.147 148 This increase is accompanied by a significant upregulation in HO-1 levels in microglia and neuronal death via oxidative DNA injury.149 A pilot study in human patients suggested a causal relationship between free iron in the CSF following SAH and brain injury.150 Indeed, suppression of hepcidin (and thus inhibition of FP1 internalisation) attenuated brain damage following experimental SAH, suggesting the importance of intracellular iron accumulation.29 This suggests that the initial inflammation caused by iron accumulation stimulates hepcidin expression, which in turn leads to a decreased efflux of iron from these cells. In this way, iron accumulation is a vicious cycle following SAH.
Additionally, a variety of other iron-handling proteins, such as Tf and TfR, are upregulated after SAH.151 Tf and TfR may also participate in intracellular iron accumulation. Once inside the cell, iron via the mitochondrial calcium uniporter can gain access to the mitochondrial matrix,152 153 where it can disrupt mitochondrial integrity, release caspase-3 and lead to neuronal degeneration. It is additionally possible that iron triggers apoptosis via cathepsins.154
Vasospasm
Endothelins (ET) are potent vasoconstrictors that have a major role in SAH-induced vasospasm. Following stimulation by angiotensin, thrombin, cytokines or ROS, ET-1 is upregulated,155 resulting in vasoconstriction. Such vasoconstriction is counteracted by nitric oxide (NO) that inhibits ET-1 release, resulting in vasodilation.156 Iron-containing haem has been shown to cause vasoconstriction.157 Indeed, reductions in free-iron levels ameliorate SAH-induced vasosconstriction.158 The iron within haem binds to the vasodilator NO,159 thereby reducing the ability of NO to inhibit ET-1 leading to vasoconstriction or vasospasm. Moreover, the formation of ROS by iron-mediated Fenton reactions is implicated in the generation of vasospasm, as the hydroxyl radicals also react with NO.160 161 Following vasospasm, ET also alters iron-regulatory proteins expression. Hepcidin is induced following ET-1 treatment/release, as is Ft and Tf/TfR.155 162 The increase in hepcidin expression may result in increased intracellular iron accumulation and, in turn, induce brain damage.
Traumatic brain injury
Introduction
TBI is the leading cause of death before the age of 40, with incident rates of ∼200 per 100 000 person-years.163 TBI accounts for about 40% of all deaths due to acute injury.164 TBI is often associated with a single or multiple ICrHs which may contribute to brain injury.165 As such, many of the findings specific to certain types of ICrH have significance to TBI. It is therefore important to include it in any discussion of ICrH-related research.
Iron accumulation in TBI
As in ICrH, damage from TBI is classified as primary or secondary, where primary injury refers to the immediate result of mechanical brain trauma, and secondary injury refers to the subsequent biomolecular and physiological responses to that injury. Iron has been frequently noted as a potential mediator for secondary injury following TBI due to its ability to form free radicals and induce oxidative stress.166 167 Iron levels in the brain are elevated following TBI.168–171 While haem-bound iron from erythrocyte lysis is a significant contributor to this, it appears that this iron is supplemented by a release of endogenous sources of iron, suggesting that, like in forms of haemorrhage, the secondary cell loss associated with TBI allows subsequent iron release and a vicious cycle is thus perpetrated.167 172 Repeated TBI results in chronically elevated iron levels, as is observed in chronic traumatic encephalopathy. Such iron deposition is positively correlated with cognitive impairment following TBI.173
Mechanism of iron-induced injury in TBI
In mice, decreasing CP and APP expression inhibits iron export from neurons. Knockout of these proteins increased brain injury and iron accumulation following TBI.174 However, the neuroprotective role of APP in TBI is not fully established. Aβ deposition is seen in some patients with repeated TBI, and iron has been shown to increase the toxicity of Aβ.167 175 176 Iron is associated with increased brain oedema formation and blood–brain barrier (BBB) disruption after TBI.177 Furthermore, there is evidence that iron can promote HO-1-mediated neurofibrillary tangle formation, which in turn results in tau phosphorylation as seen in Alzhemier's disease.178 HO-1 expression has been shown to be upregulated significantly in response to TBI.177 While it has been shown that iron further facilitates ROS-related damage to neuronal DNA,179 more research must be performed to assess the nature of this facilitation.
Treatments
Introduction
Preclinical evidence indicates that iron is a key player in brain injury after all forms of cerebral haemorrhage. To date, no existing neuroprotective therapy has been shown to improve morbidity or mortality following ICH in humans.180 However, using animal models, investigators have identified therapeutic treatments, including but not limited to deferoxamine (DFX) and minocycline, which target iron-mediated damage.
Deferoxamine
Attenuation of brain injury
DFX is a ferric ion chelator that is used clinically for systemic iron overload. The efficacy of DFX in treating haemorrhage-induced brain damage in preclinical models has been reviewed previously.181–183 Evidence of efficacy in TBI has also been demonstrated.184 A stratified meta-analysis showed DFX to be effective in experimental ICH, particularly when administered 2–4 hours after haemorrhage, and with a dosage of 10–50 mg/kg.181 DFX has been repeatedly demonstrated to ameliorate iron-induced oedema,185 neuronal death,186 hippocampal degeneration46 and inflammation.185 187–189 During SAH, DFX treatment chelates free iron before it can form ROS, thus ameliorating vasospasm.158
Attenuation of PHH
DFX significantly has been shown to reduce PHH.142 165 Gao et al132 showed that hydrocephalus developed after intraventricular injection of lysed but not packed erythrocytes into adult rats, and that DFX coinjection reduced ventricular enlargement by 27%. Strahle et al133 also demonstrated that iron injection alone could cause hydrocephalus in neonatal rats, and that DFX reduced ventricular enlargement by 57%. Intriguingly, iron was singled out as a key component inducing hydrocephalus due to a comparison between haem and protoporphyrin IX (the latter being the haem scaffold without the iron core) which demonstrated that protoporphyrin IX injection had no effect on ventricular volume compared with controls. Iron may induce PHH through free radical production and oxidative stress, but it is possible that it also activates the Wnt signalling pathway.143 The Wnt signalling pathway is involved in fibrosis in a variety of tissues and, therefore, it may play a role in obstructive non-communicating hydrocephalus formation following haemorrhage. DFX reduced Wnt1/Wnt3a upregulation following IVH most likely via iron chelation.143 These findings strongly implicated iron as a key player in PHH.
Clinical trials
In 2011, a Phase-I dose-finding study assessed DFX treatment in ICH and found it to be feasible and well tolerated.190 That led to a Phase-II trial of DFX in human ICH patients, the High Dose Deferoxamine in Intracerebral Hemorrhage (HI-DEF) trial.191 In that trial, there were some concerns over the occurrence of acute respiratory distress syndrome and currently, a lower dose of DFX is being tested in the Intracerebral Hemorrhage Deferoxamine Trial (iDEF; NCT02175225). In addition, a recent 42 patients study investigating DFX treatment for ICH concluded that DFX may slow haematoma absorption and inhibit oedema formation.192 Aside from these trials, there have been no other large-scale attempts to implement this treatment into human patients in ICrH. In addition, there has been a lack of DFX clinical trials that investigate any form of haemorrhage besides ICH. Given the preclinical effects of DFX and similarities in the role of iron in SAH and IVH to that ICH, advancement of DFX into large-scale clinical trials for IVH and SAH should be considered.
Minocycline
Effect on brain injury in animal models
Minocycline is another iron chelator. A tetracycline derivative, it has high lipophilicity allowing it to cross the BBB.193 It was originally investigated for its therapeutic potential as a macrophage/microglial inhibitor.194–196 It decreases post-ICrH damage mediated by thrombin-activated microglia197 by inhibiting matrix metalloproteinase and PARP-1 activation.198 199 However, more recently, minocycline has been investigated for its potential as an iron chelator. In vitro, it reduces iron-induced injury in cortical neuron with higher activity than DFX.200 In vivo, it reduces increases in serum iron levels, reduces iron overload and neuronal death and attenuates iron-induced brain oedema and BBB disruption following ICH.201 Coinjection of minocycline+FeCl2 compared with FeCl2 alone decreased Ft, CP, HO-1, Tf and TfR upregulation.202 Owing to its iron-chelating abilities, as well as its ability to inhibit harmful microglial activation, minocycline is a promising therapeutic option for ICrH.
Clinical trials
Minocycline currently used clinically as an antibiotic. There have, however, been few human pilot studies conducted that investigate the efficacy of minocycline treatment following haemorrhage or TBI. A study conducted with 152 patients saw a significant improvement in patient outcome with minocycline treatment compared with placebo.203 In the ongoing MINOS (Minocycline to Improve Neurologic Outcome in Stroke) trial, minocycline treatment has been shown to be safe in 10 mg/kg intravenous dosages.204 That trial has shown that minocycline decreases the expression of the potentially harmful matrix metalloproteinase-9 and the inflammatory cytokine IL-6 after stroke.205 206 However, it has yet to release results on the overall efficacy of minocycline. However, a pilot study conducted in 2013 involving 95 participants investigated the effects of minocycline in ischaemic and haemorrhagic stroke. It found that minocycline is safe, but not particularly efficacious.207 There is therefore significant controversy about the efficacy of minocycline in human trials. Given the concordance on the safety of the treatment, however, it seems sensible to move forward into a larger clinical trial.
Other iron chelators
Deferiprone
In addition to DFX and minocycline, there are several other iron-chelating drugs that have therapeutic potential with respect to ICrH and TBI. Deferiprone (DFP) is a bidentate chelator, requiring three molecules of DFP per iron cation chelated208 as opposed to the hexadentate DFX (1:1 ratio). DFP is effective at attenuating neurodegeneration induced by brain iron overload in Friedreich's ataxia.209 However, it has not been investigated as thoroughly as a treatment for ICrH damage. The few studies that have performed so have had mixed results; DFP administration at 8 hours post-SAH resulted in significantly decreased cerebral vasospasm in a rabbit model.210 However, in a rat ICH model, DFP failed to decrease ROS generation, oedema formation and morbidity, despite successfully reducing iron content.96 This latter study used a high dosage of DFP (125 mg/kg, which is above the 75–100 mg/kg typical dosage usually used to treat thalassaemia), and found that a dosage of 200 mg/kg was highly toxic to the rats in the study. It may therefore be of interest to reassess DFP's abilities as a treatment if used at a lower dose and possibly in conjunction with DFX administration (as is performed commonly in thalassaemia and other iron overload conditions).
Deferasirox
Deferasirox (DFS) is bidentate, requiring two equivalents of chelator for every one iron equivalent.208 It is delivered orally and is often used to treat anaemias or thalassaemia when DFX treatment is insufficient. It has only been cursorily investigated with respect to TBI. Systemic administration of DFS allows for mild improvements in hindlimb function following traumatic spinal cord injury at the T8 vertebra.211 The link between this improvement and any decrease in iron overload has not been investigated, however. Moreover, there have been no studies to the best of our knowledge investigating DFS following TBI or ICrH within the brain itself.
Clioquinol
The iron chelator Clioquinol (CQ) has attracted interest in the treatment of Alzheimer's and Parkinson's disease due to its ability to chelate a variety of metals, including copper, zinc and iron.212 213 Its hydrophobic nature allows it to pass through the BBB. In a rat model of ICH, CQ administration ameliorated motor dysfunction due to its ability to reduce ROS production in oligodendrocytes.214 In addition, CQ improved neurological outcome, reduced brain oedema and improved mortality rates in a different rat model while enhancing expression of the iron exporting protein FP1.96 These findings suggest CQ as a promising upcoming treatment option for ICH. However, its ability to treat other forms of ICrH has yet to be investigated, nor has it been clearly demonstrated that its effects are due to iron chelation.
2,2′-Dipyridyl
Findings on 2,2′-dipyridyl (DP) have been mixed. A lipid-soluble ferrous chelator that acts intracellularly and can bypass the BBB, it showed promise in treating SAH-induced cerebral vasospasm, as it was shown to be effective in a primate model.215 In addition, DP has been shown to have greater cell membrane permeation and intracellular iron sequestering ability than DFX.61 However, to the best of our knowledge, there has been no subsequent research on its effectiveness in SAH since the turn of the century. In ICH, its effectiveness is controversial. Wu et al216 found that DP pretreatment decreased iron deposition and neurodegeneration following ICH, while additionally attenuating ROS production and microglial activation. Furthermore, this study found that DP post-treatment ameliorated neurobehavioral deficits and brain oedema formation while not affecting mortality rates. However, more recently, Caliaperumal et al217 performed a series of experiments assessing DP's effect following ICH and found that it failed to chelate non-haem iron levels following ICH, failed to reduce oedema in the ipsilateral cortex and failed to lessen tissue loss or decrease neurodegeneration. These somewhat contradictory findings could be partly explained by the difference in experimental setup (the first was more focused on a pretreatment vs post-treatment administration while the second was simply assessing post-treatment in a variety of circumstances), but they still warrant further investigation and clarification.
Future directions
Over the past few decades, there has been an absence of improvements to the therapeutic approaches available for ICrH. Mortality and incident rates have been remained largely unchanged. This review stresses the extent and severity of the roles that iron may play in all types of ICrH. It is therefore imperative that more investigation into all types of iron-related brain damage be conducted. Current upcoming treatment options such as DFX and minocycline are promising in animal models and preliminary human studies. Despite this, advancement into clinical trials for these drugs has been slow.
Additional therapeutic targets should be investigated as well. It may not be sufficient to simply chelate extracellular iron, as iron can act via the plethora of signalling pathways as discussed in this review. Therefore, investigation into additional iron-related pathways would be prudent. For example, there has been an absence of investigations finding ways to target specific iron-related proteins after injury. Targets such as hepcidin, IRP-1 and IRP-2, FP1 and Ft are well understood in terms of normal function, but methods to treat dysfunction following ICrH are lacking. Ferroptosis, the iron-dependent form of cell death, has yet to be investigated with respect to ICrH.
Additionally, the interplay between ICrH and neurodegenerative diseases merits continued investigation. While amyloid angiopathy is a major cause of ICH, proteins such as APP and phenomena such as neurofibrillary tangles suggest that there are further links between neurodegenerative diseases and haemorrhage/iron.
The recent identification of neuronal CD163 is a promising area of research. It provides a pathway by which Hb-bound iron may significantly enter neurons and thereby cause neuronal iron overload and death. Investigation into neuronal CD163 as a therapeutic target is currently being undertaken in this and other laboratories. Identification of ways to increase Hb reuptake by non-neuronal cells, decrease iron uptake by neurons and/or increase neuronal ability to sequester excess iron influx are important areas of study.
As with all neurological conditions, the delivery of therapeutics is a concern. Most therapeutics developed by the pharmaceutical industry do not cross the BBB. For example, DFX has limited BBB permeability. Strides are being made in delivery systems designed to deliver therapeutics to the brain and alternative routes of administration (eg, intranasal) are being investigated. Hopefully, those strides can be used to develop therapeutics for ICrH.
Conclusion
Iron has beneficial and detrimental actions. While it is essential to countless critical cellular functions, it can be harmful if concentrations overwhelm the defence mechanisms of the brain. Following haemorrhage, the brain is exposed to iron-rich Hb which can be disastrous should the existing homeostatic mechanisms be insufficient. Iron is a popular topic in a variety of neurodegenerative diseases, and indeed, it is gaining attention as a therapeutic target in ICrH and TBI, yet there are many iron-related therapies and experiments that have not yet been investigated. This review stresses the importance of iron in the secondary damage following ICrH. It is clear that the oxidative damage is a key factor in the poor prognosis associated with ICrH and TBI. Current treatment options have not seen a decrease in morbidity or mortality, and so it is of critical importance that we continue to seek out new therapies that are centred on the role of iron following ICH, IVH and SAH.
Footnotes
Funding: This study was supported by grants NS-073595, NS-079157, NS-084049, NS-091545 and NS-090925 from the National Institutes of Health (NIH) and the Joyce & Don Massey Family Foundation.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Kuhn LC. Iron regulatory proteins and their role in controlling iron metabolism. Metallomics 2015;7:232–43. doi:10.1039/c4mt00164h [DOI] [PubMed] [Google Scholar]
- 2.Quintana C, Bellefqih S, Laval JY, et al. . Study of the localization of iron, ferritin, and hemosiderin in alzheimer's disease hippocampus by analytical microscopy at the subcellular level. J Struct Biol 2006;153:42–54. doi:10.1016/j.jsb.2005.11.001 [DOI] [PubMed] [Google Scholar]
- 3.Berg D. In vivo detection of iron and neuromelanin by transcranial sonography—a new approach for early detection of substantia nigra damage. J Neural Transm (Vienna) 2006;113:775–80. doi:10.1007/s00702-005-0447-5 [DOI] [PubMed] [Google Scholar]
- 4.Swaiman KF. Hallervorden-Spatz syndrome and brain iron metabolism. Arch Neurol 1991;48:1285–93. doi:10.1001/archneur.1991.00530240091029 [DOI] [PubMed] [Google Scholar]
- 5.Nilsson OG, Lindgren A, Stahl N, et al. . Incidence of intracerebral and subarachnoid haemorrhage in southern Sweden. J Neurol Neurosurg Psychiatr 2000;69:601–7. doi:10.1136/jnnp.69.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keep RF, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol 2012;11:720–31. doi:10.1016/S1474-4422(12)70104-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garton T, Keep RF, Wilkinson DA, et al. . Intraventricular hemorrhage: the role of blood components in secondary injury and hydrocephalus. Transl Stroke Res 2016;7:447–51. doi:10.1007/s12975-016-0480-8 [DOI] [PubMed] [Google Scholar]
- 8.Xiong XY, Wang J, Qian ZM, et al. . Iron and intracerebral hemorrhage: from mechanism to translation. Transl Stroke Res 2014;5:429–41. doi:10.1007/s12975-013-0317-7 [DOI] [PubMed] [Google Scholar]
- 9.Bradbury MW. Transport of iron in the blood–brain–cerebrospinal fluid system. J Neurochem 1997;69:443–54. doi:10.1046/j.1471-4159.1997.69020443.x [DOI] [PubMed] [Google Scholar]
- 10.Connor JR, Menzies SL, Burdo JR, et al. . Iron and iron management proteins in neurobiology. Pediatr Neurol 2001;25:118–29. doi:10.1016/S0887-8994(01)00303-4 [DOI] [PubMed] [Google Scholar]
- 11.Aisen P, Leibman A, Zweier J. Stoichiometric and site characteristics of the binding of iron to human transferrin. J Biol Chem 1978;253:1930–7. [PubMed] [Google Scholar]
- 12.Ke Y, Qian ZM. Brain iron metabolism: neurobiology and neurochemistry. Prog Neurobiol 2007;83:149–73. doi:10.1016/j.pneurobio.2007.07.009 [DOI] [PubMed] [Google Scholar]
- 13.Qian ZM, Tang PL, Wang Q. Iron crosses the endosomal membrane by a carrier-mediated process. Prog Biophys Mol Biol 1997;67:1–15. doi:10.1016/S0079-6107(97)00009-6 [DOI] [PubMed] [Google Scholar]
- 14.Yu Z, Persson HL, Eaton JW, et al. . Intralysosomal iron: a major determinant of oxidant-induced cell death. Free Radic Biol Med 2003;34:1243–52. doi:10.1016/S0891-5849(03)00109-6 [DOI] [PubMed] [Google Scholar]
- 15.Arosio P, Carmona F, Gozzelino R, et al. . The importance of eukaryotic ferritins in iron handling and cytoprotection. Biochem J 2015;472:1–15. doi:10.1042/BJ20150787 [DOI] [PubMed] [Google Scholar]
- 16.Moos T, Rosengren Nielsen T, Skjorringe T, et al. . Iron trafficking inside the brain. J Neurochem 2007;103:1730–40. doi:10.1111/j.1471-4159.2007.04976.x [DOI] [PubMed] [Google Scholar]
- 17.Wong BX, Tsatsanis A, Lim LQ, et al. . Beta-amyloid precursor protein does not possess ferroxidase activity but does stabilize the cell surface ferrous iron exporter ferroportin. PLoS ONE 2014;9:e114174 doi:10.1371/journal.pone.0114174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duce JA, Tsatsanis A, Cater MA, et al. . Iron-export ferroxidase activity of beta-amyloid precursor protein is inhibited by zinc in alzheimer's disease. Cell 2010;142:857–67. doi:10.1016/j.cell.2010.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo S, Frazer DM, Anderson GJ. Iron homeostasis: transport, metabolism, and regulation. Curr Opin Clin Nutr Metab Care 2016;19:276–81. doi:10.1097/MCO.0000000000000285 [DOI] [PubMed] [Google Scholar]
- 20.Aisen P, Leibman A. Lactoferrin and transferrin: a comparative study. Biochim Biophys Acta 1972;257:314–23. doi:10.1016/0005-2795(72)90283-8 [DOI] [PubMed] [Google Scholar]
- 21.Qian ZM, Wang Q. Expression of iron transport proteins and excessive iron accumulation in the brain in neurodegenerative disorders. Brain Res Brain Res Rev 1998;27:257–67. doi:10.1016/S0165-0173(98)00012-5 [DOI] [PubMed] [Google Scholar]
- 22.Terent A, Hallgren R, Venge P, et al. . Lactoferrin, lysozyme, and beta 2-microglobulin in cerebrospinal fluid. Elevated levels in patients with acute cerebrovascular lesions as indices of inflammation. Stroke 1981;12:40–6. [DOI] [PubMed] [Google Scholar]
- 23.Rogers JT, Randall JD, Cahill CM, et al. . An iron-responsive element type II in the 5’-untranslated region of the alzheimer's amyloid precursor protein transcript. J Biol Chem 2002;277:45518–28. doi:10.1074/jbc.M207435200 [DOI] [PubMed] [Google Scholar]
- 24.Gray NK, Hentze MW. Iron regulatory protein prevents binding of the 43s translation pre-initiation complex to ferritin and ealas mrnas. EMBO J 1994;13:3882–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guo B, Yu Y, Leibold EA. Iron regulates cytoplasmic levels of a novel iron-responsive element-binding protein without aconitase activity. J Biol Chem 1994;269:24252–60. [PubMed] [Google Scholar]
- 26.Gunshin H, Allerson CR, Polycarpou-Schwarz M, et al. . Iron-dependent regulation of the divalent metal ion transporter. FEBS Lett 2001;509:309–16. doi:10.1016/S0014-5793(01)03189-1 [DOI] [PubMed] [Google Scholar]
- 27.Nemeth E, Tuttle MS, Powelson J, et al. . Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science 2004;306:2090–3. doi:10.1126/science.1104742 [DOI] [PubMed] [Google Scholar]
- 28.Li L, Holscher C, Chen BB, et al. . Hepcidin treatment modulates the expression of divalent metal transporter-1, ceruloplasmin, and ferroportin-1 in the rat cerebral cortex and hippocampus. Biol Trace Elem Res 2011;143:1581–93. doi:10.1007/s12011-011-8967-3 [DOI] [PubMed] [Google Scholar]
- 29.Tan G, Liu L, He Z, et al. . Role of hepcidin and its downstream proteins in early brain injury after experimental subarachnoid hemorrhage in rats. Mol Cell Biochem 2016;418:31–8. doi:10.1007/s11010-016-2730-1 [DOI] [PubMed] [Google Scholar]
- 30.Rochette L, Gudjoncik A, Guenancia C, et al. . The iron-regulatory hormone hepcidin: a possible therapeutic target? Pharmacol Ther 2015;146:35–52. doi:10.1016/j.pharmthera.2014.09.004 [DOI] [PubMed] [Google Scholar]
- 31.Zhang AS, Enns CA. Iron homeostasis: recently identified proteins provide insight into novel control mechanisms. J Biol Chem 2009;284:711–15. doi:10.1074/jbc.R800017200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Biagioli M, Pinto M, Cesselli D, et al. . Unexpected expression of alpha- and beta-globin in mesencephalic dopaminergic neurons and glial cells. Proc Natl Acad Sci USA 2009;106:15454–9. doi:10.1073/pnas.0813216106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu L, Zeng M, Stamler JS. Hemoglobin induction in mouse macrophages. Proc Natl Acad Sci USA 1999;96:6643–7. doi:10.1073/pnas.96.12.6643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schelshorn DW, Schneider A, Kuschinsky W, et al. . Expression of hemoglobin in rodent neurons. J Cereb Blood Flow Metab 2009;29:585–95. doi:10.1038/jcbfm.2008.152 [DOI] [PubMed] [Google Scholar]
- 35.Richter F, Meurers BH, Zhu C, et al. . Neurons express hemoglobin alpha- and beta-chains in rat and human brains. J Comp Neurol 2009;515:538–47. doi:10.1002/cne.22062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saha D, Patgaonkar M, Shroff A, et al. . Hemoglobin expression in nonerythroid cells: novel or ubiquitous? Int J Inflam 2014;2014:803237 doi:10.1155/2014/803237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wicher KB, Fries E. Evolutionary aspects of hemoglobin scavengers. Antioxid Redox Signal 2010;12:249–59. doi:10.1089/ars.2009.2760 [DOI] [PubMed] [Google Scholar]
- 38.Thomsen JH, Etzerodt A, Svendsen P, et al. . The haptoglobin-cd163-heme oxygenase-1 pathway for hemoglobin scavenging. Oxid Med Cell Longev 2013;2013:523652 doi:10.1155/2013/523652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alayash AI. Haptoglobin: old protein with new functions. Clin Chim Acta 2011;412:493–8. doi:10.1016/j.cca.2010.12.011 [DOI] [PubMed] [Google Scholar]
- 40.Graversen JH, Madsen M, Moestrup SK. Cd163: a signal receptor scavenging haptoglobin–hemoglobin complexes from plasma. Int J Biochem Cell Biol 2002;34:309–14. doi:10.1016/S1357-2725(01)00144-3 [DOI] [PubMed] [Google Scholar]
- 41.Borda JT, Alvarez X, Mohan M, et al. . Cd163, a marker of perivascular macrophages, is up-regulated by microglia in simian immunodeficiency virus encephalitis after haptoglobin–hemoglobin complex stimulation and is suggestive of breakdown of the blood–brain barrier. Am J Pathol 2008;172:725–37. doi:10.2353/ajpath.2008.070848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Etzerodt A, Moestrup SK. Cd163 and inflammation: biological, diagnostic, and therapeutic aspects. Antioxid Redox Signal 2013;18:2352–63. doi:10.1089/ars.2012.4834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moller HJ. Soluble cd163. Scand J Clin Lab Invest 2012;72:1–13. doi:10.3109/00365513.2011.626868 [DOI] [PubMed] [Google Scholar]
- 44.Qian M, Shen X, Wang H. The distinct role of adam17 in app proteolysis and microglial activation related to alzheimer's disease. Cell Mol Neurobiol 2016;36:471–82. doi:10.1007/s10571-015-0232-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lisi S, D'Amore M, Sisto M. Adam17 at the interface between inflammation and autoimmunity. Immunol Lett 2014;162:159–69. doi:10.1016/j.imlet.2014.08.008 [DOI] [PubMed] [Google Scholar]
- 46.Garton TP, He Y, Garton HJ, et al. . Hemoglobin-induced neuronal degeneration in the hippocampus after neonatal intraventricular hemorrhage. Brain Res 2016;1635:86–94. doi:10.1016/j.brainres.2015.12.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen-Roetling J, Regan RF. Haptoglobin increases the vulnerability of cd163-expressing neurons to hemoglobin. J Neurochem 2016;139:586–95. doi:10.1111/jnc.13720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fruitier I, Garreau I, Lacroix A, et al. . Proteolytic degradation of hemoglobin by endogenous lysosomal proteases gives rise to bioactive peptides: hemorphins. FEBS Lett 1999;447:81–6. doi:10.1016/S0014-5793(99)00271-9 [DOI] [PubMed] [Google Scholar]
- 49.Schaer CA, Schoedon G, Imhof A, et al. . Constitutive endocytosis of cd163 mediates hemoglobin-heme uptake and determines the noninflammatory and protective transcriptional response of macrophages to hemoglobin. Circ Res 2006;99:943–50. doi:10.1161/01.RES.0000247067.34173.1b [DOI] [PubMed] [Google Scholar]
- 50.Kaliman PA, Barannik TB. [heme metabolism and oxidative stress]. Ukr Biokhim Zh (1999) 2001;73:5–15. [PubMed] [Google Scholar]
- 51.Tyrrell R. Redox regulation and oxidant activation of heme oxygenase-1. Free Radic Res 1999;31:335–40. doi:10.1080/10715769900300901 [DOI] [PubMed] [Google Scholar]
- 52.Unno M, Matsui T, Ikeda-Saito M. Crystallographic studies of heme oxygenase complexed with an unstable reaction intermediate, verdoheme. J Inorg Biochem 2012;113:102–9. doi:10.1016/j.jinorgbio.2012.04.012 [DOI] [PubMed] [Google Scholar]
- 53.Watchko JF. Bilirubin-induced neurotoxicity in the preterm neonate. Clin Perinatol 2016;43:297–311. doi:10.1016/j.clp.2016.01.007 [DOI] [PubMed] [Google Scholar]
- 54.O'Brien L, Hosick PA, John K, et al. . Biliverdin reductase isozymes in metabolism. Trends Endocrinol Metab 2015;26:212–20. doi:10.1016/j.tem.2015.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Feigin VL, Lawes CM, Bennett DA, et al. . Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet 2009;8:355–69. doi:10.1016/S1474-4422(09)70025-0 [DOI] [PubMed] [Google Scholar]
- 56.Ikram MA, Wieberdink RG, Koudstaal PJ. International epidemiology of intracerebral hemorrhage. Curr Atheroscler Rep 2012;14:300–6. doi:10.1007/s11883-012-0252-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.van Asch CJ, Luitse MJ, Rinkel GJ, et al. . Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet 2010;9:167–76. doi:10.1016/S1474-4422(09)70340-0 [DOI] [PubMed] [Google Scholar]
- 58.Perez de la Ossa N, Sobrino T, Silva Y, et al. . Iron-related brain damage in patients with intracerebral hemorrhage. Stroke 2010;41:810–3. doi:10.1161/STROKEAHA.109.570168 [DOI] [PubMed] [Google Scholar]
- 59.Wagner KR, Sharp FR, Ardizzone TD, et al. . Heme and iron metabolism: role in cerebral hemorrhage. J Cereb Blood Flow Metab 2003;23:629–52. doi:10.1097/01.WCB.0000073905.87928.6D [DOI] [PubMed] [Google Scholar]
- 60.Zhao X, Song S, Sun G, et al. . Neuroprotective role of haptoglobin after intracerebral hemorrhage. J Neurosci 2009;29:15819–27. doi:10.1523/JNEUROSCI.3776-09.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kress GJ, Dineley KE, Reynolds IJ. The relationship between intracellular free iron and cell injury in cultured neurons, astrocytes, and oligodendrocytes. J Neurosci 2002;22:5848–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Regan RF, Chen M, Li Z, et al. . Neurons lacking iron regulatory protein-2 are highly resistant to the toxicity of hemoglobin. Neurobiol Dis 2008;31:242–9. doi:10.1016/j.nbd.2008.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Musci G, Polticelli F, Bonaccorsi di Patti MC. Ceruloplasmin-ferroportin system of iron traffic in vertebrates. World J Biol Chem 2014;5:204–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Roeser HP, Lee GR, Nacht S, et al. . The role of ceruloplasmin in iron metabolism. J Clin Invest 1970;49:2408–17. doi:10.1172/JCI106460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tolosano E, Altruda F. Hemopexin: structure, function, and regulation. DNA Cell Biol 2002;21:297–306. doi:10.1089/104454902753759717 [DOI] [PubMed] [Google Scholar]
- 66.Camborieux L, Julia V, Pipy B, et al. . Respective roles of inflammation and axonal breakdown in the regulation of peripheral nerve hemopexin: an analysis in rats and in c57bl/wlds mice. J Neuroimmunol 2000;107:29–41. doi:10.1016/S0165-5728(00)00246-0 [DOI] [PubMed] [Google Scholar]
- 67.Wang G, Manaenko A, Shao A, et al. . Low-density lipoprotein receptor-related protein-1 facilitates heme scavenging after intracerebral hemorrhage in mice. J Cereb Blood Flow Metab Published Online First: 17 Jun 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Garland P, Durnford AJ, Okemefuna AI, et al. . Heme-hemopexin scavenging is active in the brain and associates with outcome after subarachnoid hemorrhage. Stroke 2016;47:872–6. [DOI] [PubMed] [Google Scholar]
- 69.Moestrup SK, Gliemann J, Pallesen G. Distribution of the alpha 2-macroglobulin receptor/low density lipoprotein receptor-related protein in human tissues. Cell Tissue Res 1992;269:375–82. doi:10.1007/BF00353892 [DOI] [PubMed] [Google Scholar]
- 70.Hvidberg V, Maniecki MB, Jacobsen C, et al. . Identification of the receptor scavenging hemopexin–heme complexes. Blood 2005;106:2572–9. doi:10.1182/blood-2005-03-1185 [DOI] [PubMed] [Google Scholar]
- 71.Nielsen MJ, Moller HJ, Moestrup SK. Hemoglobin and heme scavenger receptors. Antioxid Redox Signal 2010;12:261–73. doi:10.1089/ars.2009.2792 [DOI] [PubMed] [Google Scholar]
- 72.Cho HH, Cahill CM, Vanderburg CR, et al. . Selective translational control of the alzheimer amyloid precursor protein transcript by iron regulatory protein-1. J Biol Chem 2010;285:31217–32. doi:10.1074/jbc.M110.149161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schenck JF, Zimmerman EA. High-field magnetic resonance imaging of brain iron: birth of a biomarker? NMR Biomed 2004;17:433–45. doi:10.1002/nbm.922 [DOI] [PubMed] [Google Scholar]
- 74.Koeppen AH, Michael SC, Li D, et al. . The pathology of superficial siderosis of the central nervous system. Acta Neuropathol 2008;116:371–82. doi:10.1007/s00401-008-0421-z [DOI] [PubMed] [Google Scholar]
- 75.Greenberg SM, Vernooij MW, Cordonnier C, et al. . Cerebral microbleeds: a guide to detection and interpretation. Lancet 2009;8:165–74. doi:10.1016/S1474-4422(09)70013-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hahl P, Davis T, Washburn C, et al. . Mechanisms of neuroprotection by hemopexin: modeling the control of heme and iron homeostasis in brain neurons in inflammatory states. J Neurochem 2013;125:89–101. doi:10.1111/jnc.12165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ma B, Day JP, Phillips H, et al. . Deletion of the hemopexin or heme oxygenase-2 gene aggravates brain injury following stroma-free hemoglobin-induced intracerebral hemorrhage. J Neuroinflammation 2016;13:26 doi:10.1186/s12974-016-0490-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen L, Zhang X, Chen-Roetling J, et al. . Increased striatal injury and behavioral deficits after intracerebral hemorrhage in hemopexin knockout mice. J Neurosurg 2011;114:1159–67. doi:10.3171/2010.10.JNS10861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gaasch JA, Lockman PR, Geldenhuys WJ, et al. . Brain iron toxicity: differential responses of astrocytes, neurons, and endothelial cells. Neurochem Res 2007;32:1196–208. doi:10.1007/s11064-007-9290-4 [DOI] [PubMed] [Google Scholar]
- 80.Welch KD, Davis TZ, Van Eden ME, et al. . Deleterious iron-mediated oxidation of biomolecules. Free Radic Biol Med 2002;32:577–83. doi:10.1016/S0891-5849(02)00760-8 [DOI] [PubMed] [Google Scholar]
- 81.Calabrese V, Lodi R, Tonon C, et al. . Oxidative stress, mitochondrial dysfunction and cellular stress response in Friedreich's ataxia. J Neurol Sci 2005;233:145–62. doi:10.1016/j.jns.2005.03.012 [DOI] [PubMed] [Google Scholar]
- 82.Shamoto-Nagai M, Maruyama W, Yi H, et al. . Neuromelanin induces oxidative stress in mitochondria through release of iron: mechanism behind the inhibition of 26s proteasome. J Neural Transm (Vienna) 2006;113:633–44. doi:10.1007/s00702-005-0410-5 [DOI] [PubMed] [Google Scholar]
- 83.Park J, Lee DG, Kim B, et al. . Iron overload triggers mitochondrial fragmentation via calcineurin-sensitive signals in HT-22 hippocampal neuron cells. Toxicology 2015;337:39–46. doi:10.1016/j.tox.2015.08.009 [DOI] [PubMed] [Google Scholar]
- 84.Cho B, Choi SY, Cho HM, et al. . Physiological and pathological significance of dynamin-related protein 1 (Drp1)-dependent mitochondrial fission in the nervous system. Exp Neurobiol 2013;22:149–57. doi:10.5607/en.2013.22.3.149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Slupe AM, Merrill RA, Flippo KH, et al. . A calcineurin docking motif (LXVP) in dynamin-related protein 1 contributes to mitochondrial fragmentation and ischemic neuronal injury. J Biol Chem 2013;288:12353–65. doi:10.1074/jbc.M113.459677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cereghetti GM, Stangherlin A, Martins de Brito O, et al. . Dephosphorylation by calcineurin regulates translocation of Drp1 to mitochondria. Proc Natl Acad Sci USA 2008;105:15803–8. doi:10.1073/pnas.0808249105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xi G, Keep RF, Hoff JT. Mechanisms of brain injury after intracerebral haemorrhage. Lancet 2006;5:53–63. doi:10.1016/S1474-4422(05)70283-0 [DOI] [PubMed] [Google Scholar]
- 88.Zazulia AR, Diringer MN, Derdeyn CP, et al. . Progression of mass effect after intracerebral hemorrhage. Stroke 1999;30:1167–73. doi:10.1161/01.STR.30.6.1167 [DOI] [PubMed] [Google Scholar]
- 89.Cook JD. Defining optimal body iron. Proc Nutr Soc 1999;58:489–95. doi:10.1017/S0029665199000634 [DOI] [PubMed] [Google Scholar]
- 90.Wang W, Knovich MA, Coffman LG, et al. . Serum ferritin: past, present and future. Biochim Biophys Acta 2010;1800:760–9. doi:10.1016/j.bbagen.2010.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mehdiratta M, Kumar S, Hackney D, et al. . Association between serum ferritin level and perihematoma edema volume in patients with spontaneous intracerebral hemorrhage. Stroke 2008;39:1165–70. doi:10.1161/STROKEAHA.107.501213 [DOI] [PubMed] [Google Scholar]
- 92.Bakhshayesh B, Hosseininezhad M, Saadat SN, et al. . Iron overload is associated with perihematoma edema growth following intracerebral hemorrhage that may contribute to in-hospital mortality and long-term functional outcome. Curr Neurovasc Res 2014;11:248–53. doi:10.2174/1567202611666140530124855 [DOI] [PubMed] [Google Scholar]
- 93.Hua Y, Keep RF, Hoff JT, et al. . Thrombin preconditioning attenuates brain edema induced by erythrocytes and iron. J Cereb Blood Flow Metab 2003;23:1448–54. doi:10.1097/01.WCB.0000090621.86921.D5 [DOI] [PubMed] [Google Scholar]
- 94.Yang G, Hu R, Zhang C, et al. . A combination of serum iron, ferritin and transferrin predicts outcome in patients with intracerebral hemorrhage. Sci Rep 2016;6:21970 doi:10.1038/srep21970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ruddell RG, Hoang-Le D, Barwood JM, et al. . Ferritin functions as a proinflammatory cytokine via iron-independent protein kinase c zeta/nuclear factor kappab-regulated signaling in rat hepatic stellate cells. Hepatology 2009;49:887–900. doi:10.1002/hep.22716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wang G, Hu W, Tang Q, et al. . Effect comparison of both iron chelators on outcomes, iron deposit, and iron transporters after intracerebral hemorrhage in rats. Mol Neurobiol 2016;53:3576–85. doi:10.1007/s12035-015-9302-3 [DOI] [PubMed] [Google Scholar]
- 97.Taniguchi M, Yamashita T, Kumura E, et al. . Induction of aquaporin-4 water channel mRNA after focal cerebral ischemia in rat. Brain Res Mol Brain Res 2000;78:131–7. doi:10.1016/S0169-328X(00)00084-X [DOI] [PubMed] [Google Scholar]
- 98.Mao J, Yu JL, Fu XM, et al. . [Changes on the expression of aquaporin-4 is associated with edema of brain in neonatal rats subjected to hypoxic ischemic brain damage]. Sichuan Da Xue Xue Bao Yi Xue Ban 2014;45:386–9, 409. [PubMed] [Google Scholar]
- 99.Nagelhus EA, Ottersen OP. Physiological roles of aquaporin-4 in brain. Physiol Rev 2013;93:1543–62. doi:10.1152/physrev.00011.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Saadoun S, Papadopoulos MC, Davies DC, et al. . Aquaporin-4 expression is increased in oedematous human brain tumours. J Neurol Neurosurg Psychiatry 2002;72:262–5. doi:10.1136/jnnp.72.2.262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tang Y, Wu P, Su J, et al. . Effects of aquaporin-4 on edema formation following intracerebral hemorrhage. Exp Neurol 2010;223:485–95. doi:10.1016/j.expneurol.2010.01.015 [DOI] [PubMed] [Google Scholar]
- 102.Qing WG, Dong YQ, Ping TQ, et al. . Brain edema after intracerebral hemorrhage in rats: the role of iron overload and aquaporin 4. J Neurosurg 2009;110:462–8. doi:10.3171/2008.4.JNS17512 [DOI] [PubMed] [Google Scholar]
- 103.Ximenes-da-Silva A. Metal ion toxins and brain aquaporin-4 expression: an overview. Front Neurosci 2016;10:233 doi:10.3389/fnins.2016.00233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wang LF, Yokoyama KK, Chen TY, et al. . Male-specific alleviation of iron-induced striatal injury by inhibition of autophagy. PLoS ONE 2015;10:e0131224 doi:10.1371/journal.pone.0131224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tanida I, Ueno T, Kominami E. Lc3 and autophagy. Methods Mol Biol 2008;445:77–88. doi:10.1007/978-1-59745-157-4_4 [DOI] [PubMed] [Google Scholar]
- 106.He Y, Wan S, Hua Y, et al. . Autophagy after experimental intracerebral hemorrhage. J Cereb Blood Flow Metab 2008;28:897–905. doi:10.1038/sj.jcbfm.9600578 [DOI] [PubMed] [Google Scholar]
- 107.Wang LF, Yokoyama KK, Lin CL, et al. . Knockout of ho-1 protects the striatum from ferrous iron-induced injury in a male-specific manner in mice. Sci Rep 2016;6:26358 doi:10.1038/srep26358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zukor H, Song W, Liberman A, et al. . Ho-1-mediated macroautophagy: a mechanism for unregulated iron deposition in aging and degenerating neural tissues. J Neurochem 2009;109:776–91. doi:10.1111/j.1471-4159.2009.06007.x [DOI] [PubMed] [Google Scholar]
- 109.Zhang Z, Miah M, Culbreth M, et al. . Autophagy in neurodegenerative diseases and metal neurotoxicity. Neurochem Res 2016;41:409–22. doi:10.1007/s11064-016-1844-x [DOI] [PubMed] [Google Scholar]
- 110.Chew KC, Ang ET, Tai YK, et al. . Enhanced autophagy from chronic toxicity of iron and mutant A53T alpha-synuclein: implications for neuronal cell death in Parkinson disease. J Biol Chem 2011;286:33380–9. doi:10.1074/jbc.M111.268409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kamalinia G, Khodagholi F, Atyabi F, et al. . Enhanced brain delivery of deferasirox-lactoferrin conjugates for iron chelation therapy in neurodegenerative disorders: in vitro and in vivo studies. Mol Pharm 2013;10:4418–31. doi:10.1021/mp4002014 [DOI] [PubMed] [Google Scholar]
- 112.Matsushita K, Meng W, Wang X, et al. . Evidence for apoptosis after intercerebral hemorrhage in rat striatum. J Cereb Blood Flow Metab 2000;20:396–404. doi:10.1097/00004647-200002000-00022 [DOI] [PubMed] [Google Scholar]
- 113.Karwacki Z, Kowianski P, Dziewatkowski J, et al. . Apoptosis in the course of experimetal intracerebral haemorrhage in the rat. Folia Morphol (Warsz) 2005;64:248–52. [PubMed] [Google Scholar]
- 114.Levy YS, Streifler JY, Panet H, et al. . Hemin-induced apoptosis in PC12 and neuroblastoma cells: implications for local neuronal death associated with intracerebral hemorrhage. Neurotox Res 2002;4:609–16. doi:10.1080/1029842021000045624 [DOI] [PubMed] [Google Scholar]
- 115.Sun H, Li L, Zhou F, et al. . The member of high temperature requirement family HtrA2 participates in neuronal apoptosis after intracerebral hemorrhage in adult rats. J Mol Histol 2013;44:369–79. doi:10.1007/s10735-013-9489-4 [DOI] [PubMed] [Google Scholar]
- 116.Yuan D, Shen J, Yan Y, et al. . Upregulated expression of sstr1 is involved in. neuronal apoptosis and is coupled to the reduction of bcl-2 following intracerebral hemorrhage in adult rats. Cell Mol Neurobiol 2014;34:951–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Shen J, Liu Y, Song Y, et al. . CHMP4b, ESCRT-III associating protein, associated with neuronal apoptosis following intracerebral hemorrhage. Brain Res 2015;1597:1–13. doi:10.1016/j.brainres.2014.11.043 [DOI] [PubMed] [Google Scholar]
- 118.Zhang D, Yuan D, Shen J, et al. . Up-regulation of VCAM1 relates to neuronal apoptosis after intracerebral hemorrhage in adult rats. Neurochem Res 2015;40:1042–52. doi:10.1007/s11064-015-1561-x [DOI] [PubMed] [Google Scholar]
- 119.Chen X, Shen J, Wang Y, et al. . Up-regulation of c-Fos associated with neuronal apoptosis following intracerebral hemorrhage. Cell Mol Neurobiol 2015;35:363–76. doi:10.1007/s10571-014-0132-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Dixon SJ, Lemberg KM, Lamprecht MR, et al. . Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 2012;149:1060–72. doi:10.1016/j.cell.2012.03.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cao JY, Dixon SJ. Mechanisms of ferroptosis. Cell Mol Life Sci 2016;73:2195–209. doi:10.1007/s00018-016-2194-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chang CF, Cho S, Wang J. (-)-Epicatechin protects hemorrhagic brain via synergistic Nrf2 pathways. Ann Clin Transl Neurol 2014;1:258–71. doi:10.1002/acn3.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ying W, Han SK, Miller JW, et al. . Acidosis potentiates oxidative neuronal death by multiple mechanisms. J Neurochem 1999;73:1549–56. doi:10.1046/j.1471-4159.1999.0731549.x [DOI] [PubMed] [Google Scholar]
- 124.Bishop GM, Robinson SR. Quantitative analysis of cell death and ferritin expression in response to cortical iron: implications for hypoxia–ischemia and stroke. Brain Res 2001;907:175–87. doi:10.1016/S0006-8993(01)02303-4 [DOI] [PubMed] [Google Scholar]
- 125.Siesjo BK, Agardh CD, Bengtsson F. Free radicals and brain damage. Cerebrovasc Brain Metab Rev 1989;1:165–211. [PubMed] [Google Scholar]
- 126.Baader SL, Bruchelt G, Carmine TC, et al. . Ascorbic-acid-mediated iron release from cellular ferritin and its relation to the formation of DNA strand breaks in neuroblastoma cells. J Cancer Res Clin Oncol 1994;120:415–21. doi:10.1007/BF01240141 [DOI] [PubMed] [Google Scholar]
- 127.Ballabh P. Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res 2010;67:1–8. doi:10.1203/PDR.0b013e3181c1b176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bhattathiri PS, Gregson B, Prasad KS, et al. . Intraventricular hemorrhage and hydrocephalus after spontaneous intracerebral hemorrhage: results from the STICH trial. Acta Neurochir Suppl 2006;96:65–8. doi:10.1007/3-211-30714-1_16 [DOI] [PubMed] [Google Scholar]
- 129.Rosen DS, Macdonald RL, Huo D, et al. . Intraventricular hemorrhage from ruptured aneurysm: clinical characteristics, complications, and outcomes in a large, prospective, multicenter study population. J Neurosurg 2007;107:261–5. doi:10.3171/JNS-07/08/0261 [DOI] [PubMed] [Google Scholar]
- 130.Savman K, Nilsson UA, Blennow M, et al. . Non-protein-bound iron is elevated in cerebrospinal fluid from preterm infants with posthemorrhagic ventricular dilatation. Pediatr Res 2001;49:208–12. doi:10.1203/00006450-200102000-00013 [DOI] [PubMed] [Google Scholar]
- 131.Fukumizu M, Takashima S, Becker LE. Glial reaction in periventricular areas of the brainstem in fetal and neonatal posthemorrhagic hydrocephalus and congenital hydrocephalus. Brain Dev 1996;18:40–5. doi:10.1016/0387-7604(95)00103-4 [DOI] [PubMed] [Google Scholar]
- 132.Gao C, Du H, Hua Y, et al. . Role of red blood cell lysis and iron in hydrocephalus after intraventricular hemorrhage. J Cereb Blood Flow Metab 2014;34:1070–5. doi:10.1038/jcbfm.2014.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Strahle JM, Garton T, Bazzi AA, et al. . Role of hemoglobin and iron in hydrocephalus after neonatal intraventricular hemorrhage. Neurosurgery 2014;75:696–705; discussion 706 doi:10.1227/NEU.0000000000000524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Chen Z, Gao C, Hua Y, et al. . Role of iron in brain injury after intraventricular hemorrhage. Stroke 2011;42:465–70. doi:10.1161/STROKEAHA.110.602755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Giometto B, Bozza F, Argentiero V, et al. . Transferrin receptors in rat central nervous system. An immunocytochemical study. J Neurol Sci 1990;98:81–90. doi:10.1016/0022-510X(90)90183-N [DOI] [PubMed] [Google Scholar]
- 136.Lu J, Kaur C, Ling EA. Expression and upregulation of transferrin receptors and iron uptake in the epiplexus cells of different aged rats injected with lipopolysaccharide and interferon-gamma. J Anat 1995;187:603–11. [PMC free article] [PubMed] [Google Scholar]
- 137.Kaur C, Rathnasamy G, Ling EA. The choroid plexus in healthy and diseased brain. J Neuropathol Exp Neurol 2016;75:198–213. doi:10.1093/jnen/nlv030 [DOI] [PubMed] [Google Scholar]
- 138.Chodobski A, Szmydynger-Chodobska J. Choroid plexus: target for polypeptides and site of their synthesis. Microsc Res Tech 2001;52:65–82. doi:10.1002/1097-0029(20010101)52:1<65::AID-JEMT9>3.0.CO;2-4 [DOI] [PubMed] [Google Scholar]
- 139.Boassa D, Yool AJ. Physiological roles of aquaporins in the choroid plexus. Curr Top Dev Biol 2005;67:181–206. doi:10.1016/S0070-2153(05)67005-6 [DOI] [PubMed] [Google Scholar]
- 140.Sveinsdottir S, Gram M, Cinthio M, et al. . Altered expression of aquaporin 1 and 5 in the choroid plexus following preterm intraventricular hemorrhage. Dev Neurosci 2014;36:542–51. doi:10.1159/000366058 [DOI] [PubMed] [Google Scholar]
- 141.Gram M, Sveinsdottir S, Cinthio M, et al. . Extracellular hemoglobin—mediator of inflammation and cell death in the choroid plexus following preterm intraventricular hemorrhage. J Neuroinflammation 2014;11:200 doi:10.1186/s12974-014-0200-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Chen Q, Tang J, Tan L, et al. . Intracerebral hematoma contributes to hydrocephalus after intraventricular hemorrhage via aggravating iron accumulation. Stroke 2015;46:2902–8. doi:10.1161/STROKEAHA.115.009713 [DOI] [PubMed] [Google Scholar]
- 143.Meng H, Li F, Hu R, et al. . Deferoxamine alleviates chronic hydrocephalus after intraventricular hemorrhage through iron chelation and wnt1/wnt3a inhibition. Brain Res 2015;1602:44–52. doi:10.1016/j.brainres.2014.08.039 [DOI] [PubMed] [Google Scholar]
- 144.Wirth FP. Surgical treatment of incidental intracranial aneurysms. Clin Neurosurg 1986;33:125–35. [PubMed] [Google Scholar]
- 145.Naggara O, Nataf F. [subarachnoid hemorrhage in young patients]. Rev Prat 2013;63:951–9. [PubMed] [Google Scholar]
- 146.Kotlega D, Golab-Janowska M, Masztalewicz M, et al. . Potential role of statins in the intracerebral hemorrhage and subarachnoid hemorrhage. Neurol Neurochir Pol 2015;49:322–8. [DOI] [PubMed] [Google Scholar]
- 147.Lee JY, Keep RF, Hua Y, et al. . Deferoxamine reduces early brain injury following subarachnoid hemorrhage. Acta Neurochir Suppl 2011;112:101–6. doi:10.1007/978-3-7091-0661-7_18 [DOI] [PubMed] [Google Scholar]
- 148.Suzuki H, Muramatsu M, Tanaka K, et al. . Cerebrospinal fluid ferritin in chronic hydrocephalus after aneurysmal subarachnoid hemorrhage. J Neurol. 2006;253:1170–6. doi:10.1007/s00415-006-0184-1 [DOI] [PubMed] [Google Scholar]
- 149.Ono S, Zhang ZD, Marton LS, et al. . Heme oxygenase-1 and ferritin are increased in cerebral arteries after subarachnoid hemorrhage in monkeys. J Cereb Blood Flow Metab 2000;20:1066–76. doi:10.1097/00004647-200007000-00006 [DOI] [PubMed] [Google Scholar]
- 150.Gomes JA, Selim M, Cotleur A, et al. . Brain iron metabolism and brain injury following subarachnoid hemorrhage: icefish-pilot (csf iron in sah). Neurocrit Care 2014;21:285–93. doi:10.1007/s12028-014-9977-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lee JY, Keep RF, He Y, et al. . Hemoglobin and iron handling in brain after subarachnoid hemorrhage and the effect of deferoxamine on early brain injury. J Cereb Blood Flow Metab 2010;30:1793–803. doi:10.1038/jcbfm.2010.137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Sripetchwandee J, Sanit J, Chattipakorn N, et al. . Mitochondrial calcium uniporter blocker effectively prevents brain mitochondrial dysfunction caused by iron overload. Life Sci 2013;92:298–304. doi:10.1016/j.lfs.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 153.Yan H, Hao S, Sun X, et al. . Blockage of mitochondrial calcium uniporter prevents iron accumulation in a model of experimental subarachnoid hemorrhage. Biochem Biophys Res Commun 2015;456:835–40. doi:10.1016/j.bbrc.2014.12.073 [DOI] [PubMed] [Google Scholar]
- 154.Wang Y, Gao A, Xu X, et al. . The neuroprotection of lysosomotropic agents in experimental subarachnoid hemorrhage probably involving the apoptosis pathway triggering by cathepsins via chelating intralysosomal iron. Mol Neurobiol 2015;52:64–77. doi:10.1007/s12035-014-8846-y [DOI] [PubMed] [Google Scholar]
- 155.Bickford JS, Ali NF, Nick JA, et al. . Endothelin-1-mediated vasoconstriction alters cerebral gene expression in iron homeostasis and eicosanoid metabolism. Brain Res 2014;1588:25–36. doi:10.1016/j.brainres.2014.09.022 [DOI] [PubMed] [Google Scholar]
- 156.Stow LR, Jacobs ME, Wingo CS, et al. . Endothelin-1 gene regulation. FASEB J 2011;25:16–28. doi:10.1096/fj.10-161612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Joerk A, Seidel RA, Walter SG, et al. . Impact of heme and heme degradation products on vascular diameter in mouse visual cortex. J Am Heart Assoc 2014;3:e001220 doi:10.1161/JAHA.114.001220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Vollmer DG, Hongo K, Ogawa H, et al. . A study of the effectiveness of the iron-chelating agent deferoxamine as vasospasm prophylaxis in a rabbit model of subarachnoid hemorrhage. Neurosurgery 1991;28:27–32. doi:10.1227/00006123-199101000-00005 [DOI] [PubMed] [Google Scholar]
- 159.Pluta RM, Oldfield EH. Analysis of nitric oxide (NO) in cerebral vasospasm after aneursymal bleeding. Rev Recent Clin Trials 2007;2:59–67. doi:10.2174/157488707779318062 [DOI] [PubMed] [Google Scholar]
- 160.Ayer RE, Zhang JH. Oxidative stress in subarachnoid haemorrhage: significance in acute brain injury and vasospasm. Acta Neurochir Suppl 2008;104:33–41. doi:10.1007/978-3-211-75718-5_7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Yu Y, Lin Z, Yin Y, et al. . The ferric iron chelator 2,2’-dipyridyl attenuates basilar artery vasospasm and improves neurological function after subarachnoid hemorrhage in rabbits. Neurol Sci 2014;35:1413–19. doi:10.1007/s10072-014-1730-8 [DOI] [PubMed] [Google Scholar]
- 162.Corradini E, Rozier M, Meynard D, et al. . Iron regulation of hepcidin despite attenuated smad1,5,8 signaling in mice without transferrin receptor 2 or Hfe. Gastroenterology 2011;141:1907–14. doi:10.1053/j.gastro.2011.06.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Bruns J Jr, Hauser WA. The epidemiology of traumatic brain injury: a review. Epilepsia 2003;44(Suppl 10):2–10. doi:10.1046/j.1528-1157.44.s10.3.x [DOI] [PubMed] [Google Scholar]
- 164.Popescu C, Anghelescu A, Daia C, et al. . Actual data on epidemiological evolution and prevention endeavours regarding traumatic brain injury. J Med Life 2015;8:272–7. [PMC free article] [PubMed] [Google Scholar]
- 165.Zhao J, Chen Z, Xi G, et al. . Deferoxamine attenuates acute hydrocephalus after traumatic brain injury in rats. Transl Stroke Res 2014;5:586–94. doi:10.1007/s12975-014-0353-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Petronilho F, Feier G, de Souza B, et al. . Oxidative stress in brain according to traumatic brain injury intensity. J Surg Res 2010;164:316–20. doi:10.1016/j.jss.2009.04.031 [DOI] [PubMed] [Google Scholar]
- 167.Nisenbaum EJ, Novikov DS, Lui YW. The presence and role of iron in mild traumatic brain injury: an imaging perspective. J Neurotrauma 2014;31:301–7. doi:10.1089/neu.2013.3102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Millerot-Serrurot E, Bertrand N, Mossiat C, et al. . Temporal changes in free iron levels after brain ischemia relevance to the timing of iron chelation therapy in stroke. Neurochem Int 2008;52:1442–8. doi:10.1016/j.neuint.2008.04.002 [DOI] [PubMed] [Google Scholar]
- 169.Justicia C, Ramos-Cabrer P, Hoehn M. MRI detection of secondary damage after stroke: chronic iron accumulation in the thalamus of the rat brain. Stroke 2008;39:1541–7. doi:10.1161/STROKEAHA.107.503565 [DOI] [PubMed] [Google Scholar]
- 170.Raz E, Jensen JH, Ge Y, et al. . Brain iron quantification in mild traumatic brain injury: a magnetic field correlation study. AJNR Am J Neuroradiol 2011;32:1851–6. doi:10.3174/ajnr.A2637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Liu HD, Li W, Chen ZR, et al. . Increased expression of ferritin in cerebral cortex after human traumatic brain injury. Neurol Sci 2013;34:1173–80. doi:10.1007/s10072-012-1214-7 [DOI] [PubMed] [Google Scholar]
- 172.Onyszchuk G, LeVine SM, Brooks WM, et al. . Post-acute pathological changes in the thalamus and internal capsule in aged mice following controlled cortical impact injury: a magnetic resonance imaging, iron histochemical, and glial immunohistochemical study. Neurosci Lett 2009;452:204–8. doi:10.1016/j.neulet.2009.01.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lu L, Cao H, Wei X, et al. . Iron deposition is positively related to cognitive impairment in patients with chronic mild traumatic brain injury: assessment with susceptibility weighted imaging. Biomed Res Int 2015;2015:470676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ayton S, Zhang M, Roberts BR, et al. . Ceruloplasmin and beta-amyloid precursor protein confer neuroprotection in traumatic brain injury and lower neuronal iron. Free Radic Biol Med 2014;69:331–7. doi:10.1016/j.freeradbiomed.2014.01.041 [DOI] [PubMed] [Google Scholar]
- 175.McKee AC, Cantu RC, Nowinski CJ, et al. . Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol 2009;68:709–35. doi:10.1097/NEN.0b013e3181a9d503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wang L, Xi G, Keep RF, et al. . Iron enhances the neurotoxicity of amyloid beta. Transl Stroke Res 2012;3:107–13. doi:10.1007/s12975-011-0099-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Okubo S, Xi G, Keep RF, et al. . Cerebral hemorrhage, brain edema, and heme oxygenase-1 expression after experimental traumatic brain injury. Acta Neurochir Suppl 2013;118:83–7. [DOI] [PubMed] [Google Scholar]
- 178.Hui Y, Wang D, Li W, et al. . Long-term overexpression of heme oxygenase 1 promotes tau aggregation in mouse brain by inducing tau phosphorylation. J Alzheimers Dis 2011;26:299–313. [DOI] [PubMed] [Google Scholar]
- 179.Li H, Swiercz R, Englander EW. Elevated metals compromise repair of oxidative DNA damage via the base excision repair pathway: implications of pathologic iron overload in the brain on integrity of neuronal DNA. J Neurochem 2009;110:1774–83. doi:10.1111/j.1471-4159.2009.06271.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Gomes JA, Manno E. New developments in the treatment of intracerebral hemorrhage. Neurol Clin 2013;31:721–35. doi:10.1016/j.ncl.2013.03.002 [DOI] [PubMed] [Google Scholar]
- 181.Cui HJ, He HY, Yang AL, et al. . Efficacy of deferoxamine in animal models of intracerebral hemorrhage: a systematic review and stratified meta-analysis. PLoS ONE 2015;10:e0127256 doi:10.1371/journal.pone.0127256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Hua Y, Keep RF, Hoff JT, et al. . Deferoxamine therapy for intracerebral hemorrhage. Acta Neurochir Suppl 2008;105:3–6. doi:10.1007/978-3-211-09469-3_1 [DOI] [PubMed] [Google Scholar]
- 183.Selim M. Deferoxamine mesylate: a new hope for intracerebral hemorrhage: from bench to clinical trials. Stroke 2009;40:S90–1. doi:10.1161/STROKEAHA.108.533125 [DOI] [PubMed] [Google Scholar]
- 184.Zhang L, Hu R, Li M, et al. . Deferoxamine attenuates iron-induced long-term neurotoxicity in rats with traumatic brain injury. Neurol Sci 2013;34:639–45. doi:10.1007/s10072-012-1090-1 [DOI] [PubMed] [Google Scholar]
- 185.Xie Q, Gu Y, Hua Y, et al. . Deferoxamine attenuates white matter injury in a piglet intracerebral hemorrhage model. Stroke 2014;45:290–2. doi:10.1161/STROKEAHA.113.003033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Hatakeyama T, Okauchi M, Hua Y, et al. . Deferoxamine reduces neuronal death and hematoma lysis after intracerebral hemorrhage in aged rats. Transl Stroke Res 2013;4:546–53. doi:10.1007/s12975-013-0270-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Zhou X, Xie Q, Xi G, et al. . Brain CD47 expression in a swine model of intracerebral hemorrhage. Brain Res 2014;1574:70–6. doi:10.1016/j.brainres.2014.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Chun HJ, Kim DW, Yi HJ, et al. . Effects of statin and deferoxamine administration on neurological outcomes in a rat model of intracerebral hemorrhage. Neurol Sci 2012;33:289–96. doi:10.1007/s10072-011-0733-y [DOI] [PubMed] [Google Scholar]
- 189.Wu H, Wu T, Xu X, et al. . Iron toxicity in mice with collagenase-induced intracerebral hemorrhage. J Cereb Blood Flow Metab 2011;31:1243–50. doi:10.1038/jcbfm.2010.209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Selim M, Yeatts S, Goldstein JN, et al. . Safety and tolerability of deferoxamine mesylate in patients with acute intracerebral hemorrhage. Stroke 2011;42:3067–74. doi:10.1161/STROKEAHA.111.617589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Yeatts SD, Palesch YY, Moy CS, et al. . High dose deferoxamine in intracerebral hemorrhage (HI-DEF) trial: rationale, design, and methods. Neurocrit Care 2013;19:257–66. doi:10.1007/s12028-013-9861-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Yu Y, Zhao W, Zhu C, et al. . The clinical effect of deferoxamine mesylate on edema after intracerebral hemorrhage. PLoS ONE 2015;10:e0122371 doi:10.1371/journal.pone.0122371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Klein NC, Cunha BA. Tetracyclines. Med Clin North Am 1995;79:789–801. doi:10.1016/S0025-7125(16)30039-6 [DOI] [PubMed] [Google Scholar]
- 194.Tikka TM, Koistinaho JE. Minocycline provides neuroprotection against N-methyl-D-aspartate neurotoxicity by inhibiting microglia. J Immunol 2001;166:7527–33. doi:10.4049/jimmunol.166.12.7527 [DOI] [PubMed] [Google Scholar]
- 195.Tikka T, Fiebich BL, Goldsteins G, et al. . Minocycline, a tetracycline derivative, is neuroprotective against excitotoxicity by inhibiting activation and proliferation of microglia. J Neurosci 2001;21:2580–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Wasserman JK, Schlichter LC. Neuron death and inflammation in a rat model of intracerebral hemorrhage: effects of delayed minocycline treatment. Brain Res 2007;1136:208–18. doi:10.1016/j.brainres.2006.12.035 [DOI] [PubMed] [Google Scholar]
- 197.Wu J, Yang S, Xi G, et al. . Minocycline reduces intracerebral hemorrhage-induced brain injury. Neurol Res 2009;31:183–8. doi:10.1179/174313209X385680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Murata Y, Rosell A, Scannevin RH, et al. . Extension of the thrombolytic time window with minocycline in experimental stroke. Stroke 2008;39:3372–7. doi:10.1161/STROKEAHA.108.514026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Alano CC, Kauppinen TM, Valls AV, et al. . Minocycline inhibits poly(adp-ribose) polymerase-1 at nanomolar concentrations. Proc Natl Acad Sci USA 2006;103:9685–90. doi:10.1073/pnas.0600554103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Chen-Roetling J, Chen L, Regan RF. Minocycline attenuates iron neurotoxicity in cortical cell cultures. Biochem Biophys Res Commun 2009;386:322–6. doi:10.1016/j.bbrc.2009.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Zhao F, Hua Y, He Y, et al. . Minocycline-induced attenuation of iron overload and brain injury after experimental intracerebral hemorrhage. Stroke 2011;42:3587–93. doi:10.1161/STROKEAHA.111.623926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Zhao F, Xi G, Liu W, et al. . Minocycline attenuates iron-induced brain injury. Acta Neurochir Suppl 2016;121:361–5. [DOI] [PubMed] [Google Scholar]
- 203.Lampl Y, Boaz M, Gilad R, et al. . Minocycline treatment in acute stroke: an open-label, evaluator-blinded study. Neurology 2007;69:1404–10. doi:10.1212/01.wnl.0000277487.04281.db [DOI] [PubMed] [Google Scholar]
- 204.Fagan SC, Waller JL, Nichols FT, et al. . Minocycline to improve neurologic outcome in stroke (MINOS): a dose-finding study. Stroke 2010;41:2283–7. doi:10.1161/STROKEAHA.110.582601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Switzer JA, Hess DC, Ergul A, et al. . Matrix metalloproteinase-9 in an exploratory trial of intravenous minocycline for acute ischemic stroke. Stroke 2011;42:2633–5. doi:10.1161/STROKEAHA.111.618215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Switzer JA, Sikora A, Ergul A, et al. . Minocycline prevents Il-6 increase after acute ischemic stroke. Transl Stroke Res 2012;3:363–8. doi:10.1007/s12975-012-0150-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Kohler E, Prentice DA, Bates TR, et al. . Intravenous minocycline in acute stroke: a randomized, controlled pilot study and meta-analysis. Stroke 2013;44:2493–9. doi:10.1161/STROKEAHA.113.000780 [DOI] [PubMed] [Google Scholar]
- 208.Poggiali E, Cassinerio E, Zanaboni L, et al. . An update on iron chelation therapy. Blood Transfus 2012;10:411–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Abbruzzese G, Cossu G, Balocco M, et al. . A pilot trial of deferiprone for neurodegeneration with brain iron accumulation. Haematologica 2011;96:1708–11. doi:10.3324/haematol.2011.043018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Arthur AS, Fergus AH, Lanzino G, et al. . Systemic administration of the iron chelator deferiprone attenuates subarachnoid hemorrhage-induced cerebral vasospasm in the rabbit. Neurosurgery 1997;41:1385–91; discussion 1391–1382 doi:10.1097/00006123-199712000-00028 [DOI] [PubMed] [Google Scholar]
- 211.Sauerbeck A, Schonberg DL, Laws JL, et al. . Systemic iron chelation results in limited functional and histological recovery after traumatic spinal cord injury in rats. Exp Neurol 2013;248:53–61. doi:10.1016/j.expneurol.2013.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Cherny RA, Atwood CS, Xilinas ME, et al. . Treatment with a copper-zinc chelator markedly and rapidly inhibits beta-amyloid accumulation in alzheimer's disease transgenic mice. Neuron 2001;30:665–76. doi:10.1016/S0896-6273(01)00317-8 [DOI] [PubMed] [Google Scholar]
- 213.Kaur D, Yantiri F, Rajagopalan S, et al. . Genetic or pharmacological iron chelation prevents MPTP-induced neurotoxicity in vivo: a novel therapy for Parkinson's disease. Neuron 2003;37:899–909. doi:10.1016/S0896-6273(03)00126-0 [DOI] [PubMed] [Google Scholar]
- 214.Masuda T, Hida H, Kanda Y, et al. . Oral administration of metal chelator ameliorates motor dysfunction after a small hemorrhage near the internal capsule in rat. J Neurosci Res 2007;85:213–22. doi:10.1002/jnr.21089 [DOI] [PubMed] [Google Scholar]
- 215.Horky LL, Pluta RM, Boock RJ, et al. . Role of ferrous iron chelator 2,2’-dipyridyl in preventing delayed vasospasm in a primate model of subarachnoid hemorrhage. J Neurosurg 1998;88:298–303. doi:10.3171/jns.1998.88.2.0298 [DOI] [PubMed] [Google Scholar]
- 216.Wu H, Wu T, Li M, et al. . Efficacy of the lipid-soluble iron chelator 2,2’-dipyridyl against hemorrhagic brain injury. Neurobiol Dis 2012;45:388–94. doi:10.1016/j.nbd.2011.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Caliaperumal J, Wowk S, Jones S, et al. . Bipyridine, an iron chelator, does not lessen intracerebral iron-induced damage or improve outcome after intracerebral hemorrhagic stroke in rats. Transl Stroke Res 2013;4:719–28. doi:10.1007/s12975-013-0272-3 [DOI] [PubMed] [Google Scholar]