Abstract
Objective: The aims of this study were (1) to assess obsessive-compulsive symptoms (OCS) dimensionally in a school-aged community sample and to correlate them with clinical and demographical variables; (2) to determine a subgroup with significant OCS (“at-risk for OCD”) using the Child Behavior Checklist (CBCL-OCS) and (3) to compare it with the rest of the sample; (4) To review the CBCL-OCS subscale properties as a screening tool for pediatric OCD.
Methods: Data from the Brazilian High Risk Cohort were analyzed. The presence and severity of OCS were assessed through the CBCL-OCS subscale. DSM-IV psychiatric diagnoses were obtained by the Developmental and Well-Being Assessment. Behavioral problems were assessed using the Strengths and Difficulties Questionnaire, the Youth Strengths Inventory, and the CBCL internalizing and externalizing behavior subscales.
Results: A total of 2512 (mean age: 8.86 ± 1.84 years; 55.0% male) children were included. Moderate correlations were found between OCS severity and functional impairment (r = 0.36, p < 0.001). Children with higher levels of OCS had higher rates of psychiatric comorbidity and behavioral problems (p < 0.001). A score of 5 or higher in the CBCL-OCS scale determined an “at-risk for OCD” subgroup, comprising 9.7% of the sample (n = 244), with behavioral patterns and psychiatric comorbidities (e.g., tics [odds ratios, OR = 6.41, p < 0.001]), anxiety disorders grouped [OR = 3.68, p < 0.001] and depressive disorders [OR = 3.0, p < 0.001] very similar to those described in OCD. Sensitivity, specificity, positive predictive value, and negative predictive value of the CBCL-OCS for OCD diagnosis were, respectively, 48%, 91.5%; 15.1%, and 98.2%.
Conclusions: The dimensional approach suggests that the presence of OCS in children is associated with higher rates of comorbidity, behavioral problems, and impairment. The “at-risk for OCD” group defined by the CBCL revealed a group of patients phenotypically similar to full blown OCD.
Keywords: : child and adolescent psychiatry, epidemiology, dimensional obsessive-compulsive symptoms, school-aged children, child behavior checklist
Introduction
The lifetime prevalence of obsessive-compulsive disorder (OCD) is estimated as 2%–3% (Fontenelle et al. 2006; Ruscio et al. 2010), with most of the cases presenting their onset during childhood (Kessler et al. 2005; Alvarenga et al. 2012; de Mathis et al. 2013). The prevalence of OCD in childhood varies between 0.1% and 4% (Douglass et al. 1995; Fleitlich-Bilyk and Goodman 2004) and previous studies report that functional impairment (de Bruijn et al. 2010; Canals et al. 2012) and several psychiatric comorbidities are associated not only with full blown OCD, but also with subclinical OCD and obsessive-compulsive symptoms (OCS) as well (Flament et al. 1988; Zohar et al. 1992; Heyman et al. 2001; Shams et al. 2011; Alvarenga et al. 2015).
Moreover, longitudinal studies suggest that OCS can persist over time (Fullana et al. 2009) and increase the risk of developing OCD (Black and Gaffney 2008; Fullana et al. 2009), which supports a dimensional approach during evaluation.
Notwithstanding, only a small number of studies have assessed the presence of OCS in juvenile populations and the findings are not consistent across studies. For example, the reported prevalence rates of OCS range between 2% (Flament et al. 1988; Brynska and Wolanczyk 2005) and 19% (Valleni-Basile et al. 1994; Vivan Ade et al. 2014; Alvarenga et al. 2015), although most studies report a prevalence of ∼10% (Fullana et al. 2009; Mahfouz et al. 2009; Shams et al. 2011; Canals et al. 2012). Results on gender distribution are also inconclusive (Fontenelle and Hasler 2008). Most studies point out equal distribution between boys and girls (Zohar et al. 1992; Apter et al. 1996; Essau et al. 2000), but two studies reported OCS as more prevalent among girls (Brynska and Wolanczyk 2005; Vivan Ade et al. 2014) whereas two others found OCS being more common in boys (Canals et al. 2012; Jaisoorya et al. 2015). Regarding psychiatric comorbidity, the most frequently co-occurring conditions are major depression, anxiety disorders, tics, Tourette syndrome, and attention-deficit/hyperactivity disorder (ADHD) (Zohar et al. 1992; Heyman et al. 2001; Peterson et al. 2001; de Mathis et al. 2008; Shams et al. 2011; Canals et al. 2012; Lebowitz et al. 2012; Vivan Ade et al. 2014; Ortiz et al. 2015). The prevalence of overall comorbid conditions reported in juvenile OCS/OCD samples vary from 56% to 91% (Shams et al. 2011; Lebowitz et al. 2012; Vivan Ade et al. 2014). Concerning intelligence, one study showed no association between OCD and IQ levels (Douglass et al. 1995). In contrast, two other studies reported an association of OCS with lower IQs and lower global cognitive functioning (Zohar et al. 1992; Heyman et al. 2001) and another study did find that the OCD cases had a higher IQ (Peterson et al. 2001). In terms of the longitudinal course, most studies indicate that OCS increase with age (Apter et al. 1996; Heyman et al. 2001; Fullana et al. 2009).
Many of these inconsistencies are probably due to the diverse populations studied and to the different methodological approaches used to perform the diagnostic evaluation. Most of these studies consider OCS as a category (Apter et al. 1996; Mahfouz et al. 2009; Vivan Ade et al. 2014; Alvarenga et al. 2015), whereas a dimensional approach could be more informative, since obsessive-compulsive phenomena are expressed as a continuum from normal development to severe symptoms (Fontenelle and Hasler 2008).
The Child Behavior Checklist (CBCL) subscale for OCD (Nelson et al. 2001) is an internationally validated instrument that allows OCD and other pediatric psychiatric disorders to be dimensionally assessed. Huzdiak et al. (2006) had shown the CBCL to be a valid screening tool for OCD, with moderate sensitivity (75.3%–84.9%) and high specificity (82.2%–92.5%). Moreover, scores on the CBCL were found to have a positive predictive value (PPV) of OCD diagnosis based on Diagnostic and Statistical Manual of Mental Disorders, Third Edition Revised (DSM-IV) (American Psychiatric Association 1987) criteria (PPV) ranging between 70.5% and 83.3% and a negative predictive value (NPV), between 88.2% and 91.6%.
This study has four main objectives:
(1) To study the OCS distribution viewed from a dimensional perspective in a large community (nonclinical) pediatric sample using the CBCL;
(2) To assess the association of OCS with demographic (gender, age, and socioeconomic status) and clinical variables (IQ and other behavioral problems);
(3) To stratify our sample into at-risk for OCD based on the CBCL cutoff (Hudziak et al. 2006) and unaffected controls; to compare at-risk versus unaffected control groups regarding demographic (gender, age, and socioeconomic status) and clinical variables (psychiatric comorbidities, IQ, and other behavioral problems); and
(4) To reassess the psychometric properties of the CBCL-OCS as screening instrument for OCD, comparing with our previous sample of OCD defined by Developmental and Well-Being Assessment (DAWBA) with DSM-IV criteria.
Materials and Methods
Participants and data collection
Participants were 2512 school-aged children ranging from 6 to 12 years from a large community school-based cohort from the National Institute of Developmental Psychiatry (INPD) (inpd.org.br), the High Risk Cohort Study for Psychiatric Disorders. These students belong to 57 schools from two large cities in Brazil (22 in Porto Alegre and 35 in São Paulo) and the interviews were conducted by trained lay interviewers with the main caregivers (91.5% were mothers). The full methodology is described elsewere (Alvarenga et al. 2015; Salum et al. 2015).
Clinical assessment and instruments
Socioeconomic status
It was stratified into five classes from A (higher) to E (lower), according to a Brazilian classification system (Jannuzzi and Baeninger 1996).
Psychiatric diagnoses
They were obtained using the Brazilian Portuguese version of the DAWBA (Goodman et al. 2000), based on DSM-IV criteria. The DAWBA is validated in Brazil and can be administered by lay interviewers. Diagnoses were rated by two senior child psychiatrists. For OCD diagnosis we used the DAWBA and the DSM-IV criteria.
Global functioning
The Strengths and Difficulties Questionnaire (SDQ), Youth Strengths Inventory (YSI), and the Social Aptitude Scale (SAS) were used to evaluate, respectively, the functional impairment, positive attributes, and social abilities.
The SDQ is a 25-item questionnaire with five symptom subscales: Emotional, hyperactivity, conduct, social, and pro-social (Goodman 1999). The SDQ impact scores were used to evaluate functional impairment, burden, and social distress. The YSI is a 24-item scale designed to assess the child's positive attributes divided in two blocks of questions; the first block consists of characteristics of the child (e.g., “responsible, grateful”) while the second block accesses the child's attitudes that pleases the caregiver (e.g., “helps around at home,” “polite”) (Vidal-Ribas et al. 2015). The SAS is a 10-item scale designed to evaluate the individual's social abilities (Liddle et al. 2009).
Cognitive skills measurement
We assessed the estimated global IQ using the vocabulary and block design subtests of the Weschler Intelligence Scale for Children, 3rd edition–WISC-III (Wechsler 2002), the Tellegen and Briggs method (Tellegen and Briggs 1967), and Brazilian norms (Figueiredo 2001; do Nascimento 2002).
Behavioral problems
The CBCL (Achenbach 1991) is a dimensional instrument, one of the most widely used measures to evaluate behavioral problems. It has been validated in Brazil (Bordin et al. 2013) and includes a total score and several subscales. In this study we focused on the internalizing and externalizing behavior scores as well as the total score. OCS were quantified using the scale proposed by Nelson et al. (2001), which consists of eight items from the CBCL, with scores varying from 0 to 16. To define the at-risk for OCD group a cutoff point of 5 was used based on the work of Huzdiak et al. (2006).
Statistics
The correlations between OCS and the dimensional variables were estimated nonparametrically using the Spearman's test. To calculate the p-values of the quantitative variables, the Mann–Whitney's test was used. The Fisher's test was used to calculate the association between the categorical variables and the control or at-risk for OCD groups. To estimate the odds ratios (OR), we used a multiple logistic regression (LR) model. The variable selection was performed by the stepwise method with the Akaike's criterion. The normality of the data was verified by the Anderson–Darling test with a significance level of 0.05. All analyses were conducted in the R3.1.3 program.
Ethics
This study was approved by the Ethics Committee of the University of São Paulo School of Medicine and all parents provided their written consent.
Results
OCS distribution
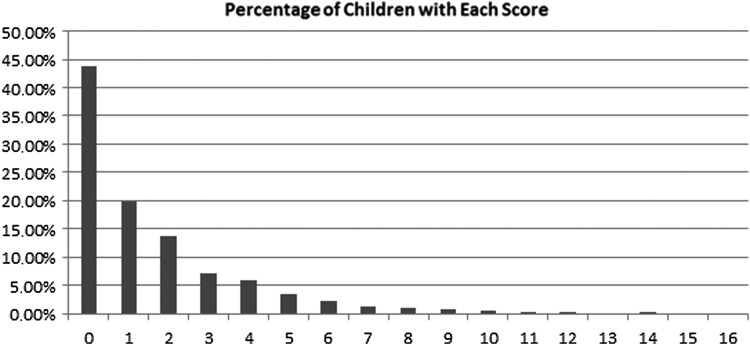
The OCS distribution among the 2512 children was calculated according to scores on the CBCL-OCS subscale varying from 0 to 16. The highest score in our study was 14. Frequencies of each score are shown in Figure 1.
FIG. 1.
Distribution of CBCL-OCS Scores among 2512 school-aged children. x-axis: Score on the CBCL-OCS; y-axis: Percentage of children (total = 2512) with each score. CBCL-OCS, Child Behavior Checklist–Obsessive-Compulsive Subscale.
Dimensional perspective: correlation of quantity of OCS with sociodemographic and clinical variables
The correlations of demographic and clinical variables with the OCS are presented in Table 1. There were no significant correlations between gender, socioeconomic status, or IQ with the quantity/severity of the OCS. On the other hand, the severity of OCS was slightly associated with age, and moderate to strong positive correlations were found between the severity of OCS and total, internalizing and externalizing behavior scores on the CBCL. Furthermore, moderate correlations between the SDQ impairment scores and the severity of OCS were found. In contrast, we found that OCS ratings were inversely correlated with the child's positive attributes as assessed by the YSI and their social aptitude (SAS).
Table 1.
Sociodemographic and Clinical Variables and Their Correlation with Obsessive-Compulsive Symptoms Ratings in the Entire Sample
| Correlation with higher score on CBCL-OCSa | ||
|---|---|---|
| n Total: 2512 | r | P |
| Age (higher) | 0.060 | 0.003 |
| Socioeconomic status | −0.040 | 0.055 |
| IQ | −0.030 | 0.186 |
| CBCL (total) | 0.650 | <0.0001 |
| Externalizing behavior | 0.530 | <0.0001 |
| Internalizing behavior | 0.690 | <0.0001 |
| Functional impairment (SDQ) | 0.360 | <0.0001 |
| Positive attributes (YSI) | −0.250 | <0.0001 |
| Social abilities (SAS) | −0.110 | <0.0001 |
CBCL-OCS criteria by Nelson et al. (2001): Score ranging from 0 to 14.
Socioeconomic status: Brazilian classification that categorizes families in five classes (A–E) according to educational level and income; CBCL: Child Behavior Checklist; CBCL total: Total score on CBCL; externalizing behavior: Score on CBCL externalizing behavior dimension; internalizing behavior: Score on CBCL internalizing behavior dimension; functional impairment: Scores on the SDQ impact session; positive attributes: Measured by scores on YSI; social abilities: Measured by scores on SAS.
OCS, obsessive-compulsive symptoms; SAS, Social Aptitude Scale; SDQ, Strengths and Difficulties Questionnaire; YSI, Youth Strengths Inventory.
Comparison of at-risk for OCD group versus unaffected controls
Two hundred forty-four children (9.7% of the total sample) scored 5 or more on the CBCL-OCS subscale and were identified as being at-risk for OCD. The remainder of the children (n = 2268) were considered unaffected controls. Table 2 shows the mean scores and standard deviations on different clinical sociodemographic and clinical variables for these two groups. There were significant differences in the CBCL total, internalizing and externalizing scores between the at-risk for OCD group and the unaffected controls, with the at-risk for OCD group presenting higher scores on all measures. On the measure of functional impairment, the SDQ impact score, there were also significant differences between groups, with the at-risk for OCD group also presenting a higher score. On the Social Aptitudes Scale and the YSI the at-risk for OCD group presented significantly lower scores as well. There were no significant differences between groups regarding gender, socioeconomic status, and age.
Table 2.
Sociodemographic Status and Clinical Variables of the At-Risk for Obsessive-Compulsive Disorder and Control Groups
| At-risk for OCD n = 244 (9.7%) | Unaffected controls n = 2268 (90.3%) | p | |
|---|---|---|---|
| Age | 9.05 (1.83) | 8.84 (1.85) | 0.078 |
| Gender (female) | 43.85 | 44.66 | 0. 839 |
| Socioeconomical status | 17.32 (4.19) | 17.43 (4.08) | 0.758 |
| IQ | 99.77 (17.22) | 101.79 (16.7) | 0.097 |
| CBCL total | 76.25 (30.54) | 25.38 (22.19) | <0.0001 |
| Internalizing | 23.8 (9.69) | 7.02(6.74) | <0.0001 |
| Externalizing | 19.8 (11.39) | 7.29 (7.93) | <0.0001 |
| Functional impairment (SDQ) | 2.48 (2.28) | 0.76 (1.36) | <0.0001 |
| Positive attributes (YSI) | 30.81 (9.04) | 35.86 (8.43) | <0.0001 |
| Social abilities (SAS) | 19.02 (6.47) | 20.37 (4.67) | <0.0001 |
Socioeconomic status: Brazilian classification that categorizes families in five classes (A–E) according to educational level and income; CBCL: Child Behavior Checklist; CBCL total: Total score on CBCL; externalizing behavior: Score on CBCL externalizing behavior dimension; internalizing behavior: Score on CBCL internalizing behavior dimension; functional impairment: Scores on the SDQ impact session; positive attributes: Measured by scores on YSI; social abilities: Measured by scores on SAS.
OCD, obsessive-compulsive disorder; SAS, Social Aptitude Scale; SDQ, Strengths and Difficulties Questionnaire; YSI, Youth Strengths Inventory.
The at-risk for OCD group had higher ORs for each of the assessed psychiatric conditions as compared to the unaffected control group (Table 3): Anxiety disorders as a group, separation anxiety, panic disorder and generalized anxiety, and major depression (ORs higher than nine times of being present in the at-risk for OCD group). Eating disorders, Tic disorders, conduct disorder and social phobia, oppositional defiant disorder, and ADHD were also more likely to occur in the at-risk for OCD group (Table 3).
Table 3.
Distribution of Gender and Psychiatric Comorbidities with Odds Ratios in the At-Risk for Obsessive-Compulsive Disorder and Unaffected Control Groups
| Variables | At-risk for OCD (9.7%) n = 244 | Unaffected controls (90.3%) n = 2268 | OR | 95% CI | p |
|---|---|---|---|---|---|
| Psychiatric disorder (at least 1) | 61.07% | 22.18% | 5.50 | 4.14–7.33 | <0.0001 |
| Anxiety disorders | 30.33% | 6.83% | 5.93 | 4.25–8.24 | <0.0001 |
| Separation anxiety | 13.93% | 1.68% | 9.5 | 5.66–15.84 | <0.0001 |
| Specific phobia | 8.61% | 3% | 3.04 | 1.74–5.14 | <0.0001 |
| Social phobia | 2.87% | 0.84% | 3.5 | 1.23–8.79 | <0.0001 |
| GAD | 10.25% | 0.97% | 11.65 | 6.18–22.03 | <0.0001 |
| Mood disorders | 14.75% | 1.76% | 9.64 | 5.82–15.86 | <0.0001 |
| Major depression (MDD) | 14.75% | 1.63% | 10.44 | 6.25–17.36 | <0.0001 |
| ADHD | 22.95% | 9.61% | 2.80 | 1.97–3.93 | <0.0001 |
| Disruptive disorders | 15.57% | 5.86% | 2.96 | 1.95–4.41 | <0.0001 |
| ODD | 11.07% | 4.59% | 2.59 | 1.59–4.09 | <0.0001 |
| Conduct disorders | 5.33% | 1.19% | 4.67 | 2.18–9.51 | <0.0001 |
| Eating disorders | 1.64% | 0.26% | 6.28 | 1.29–26.67 | 0.011 |
| Tic disorder | 3.28% | 0.49% | 6.95 | 2.40–19.17 | <0.0001 |
| Others (grouped) | 3.69% | 0.44% | 8.65 | 3.07–23.89 | <0.0001 |
At-risk for OCD group: Determined by cutoff score 5 on OCS-CBCL; GAD: generalized anxiety disorder; MDD: major depressive disorder; ADHD: attention-deficit/hyperactivity disorder; ODD: Oppositional defiant disorder; others: Includes pervasive developmental disorder, stereotypic behavior, psychosis, and selective mutism grouped.
CI, confidence interval; OCD, obsessive-compulsive disorder; OR, odds ratios.
LR was modeled to discriminate which impact variables or comorbidities were more strongly associated with the at-risk for OCD group (Table 4). Tic disorder (OR: 6.41, 95% confidence interval [CI]: 2.12–19.38), anxiety disorders as a group (OR: 3.68, 95% CI: 2.51–5.41), major depressive disorder (OR: 3.00, 95% CI: 1.65–5.47), and disorders with lower prevalence such as psychotic disorders, autism, and selective mutism grouped (OR: 4.12, 95% CI: 1.32–12.85) were strongly associated with the at-risk for OCD group. There was also a small, but significant, association of SDQ scores and externalizing behavior measured by the CBCL externalizing behavior subscale score (without the diagnosis of ADHD or any disruptive behavior disorder) with the at-risk for OCD group.
Table 4.
Significant Variables Associated with the At-Risk for Obsessive-Compulsive Disorder Group After Logistic Regression
| Estimate | Standard errors | OR | 95% CI | p | |
|---|---|---|---|---|---|
| Tic disorder | 1.86 | 0.56 | 6.41 | 2.12–19.38 | 0.001 |
| Anxiety disorders | 1.30 | 0.20 | 3.68 | 2.51–5.41 | <0.001 |
| MDD | 1.10 | 0.31 | 3.00 | 1.65–5.47 | <0.001 |
| Other (grouped) | 1.42 | 0.58 | 4.12 | 1.32–12.85 | 0.015 |
| Functional impairment (SDQ) | 0.13 | 0.05 | 1.14 | 1.04–1.26 | 0.007 |
| CBCL ext | 0.14 | 0.01 | 1.15 | 1.12–1.17 | <0.001 |
Anxiety disorders: Includes separation anxiety, social and specific phobia, generalized anxiety and panic disorder and agoraphobia; MDD: Major depressive disorder; Other (grouped): Includes psychotic disorders, pervasive developmental disorder, selective mutism; functional impairment: Measured by SDQ impact session; CBCL ext: Child Behavior Checklist Externalizing Behavior Dimension.
CI, confidence interval; OR, odds ratios; SDQ, Strengths and Difficulties Questionnaire.
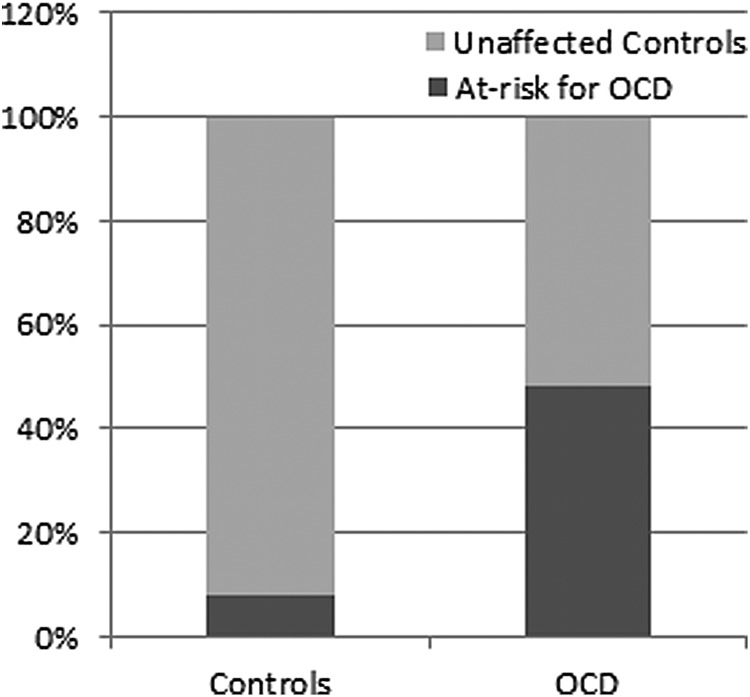
Comparison of OCS-CBCL scores and DAWBA OCD section scores
Finally, we compared the at-risk for OCD group according to the CBCL (scores equal and above cutoff of 5) with the OCD and control groups defined in our previous work using the DSM-IV criteria and the DAWBA (Alvarenga et al. 2015) (Fig. 2). In this analysis, of the 2512 children, we obtained 77 children diagnosed with OCD. Sensitivity, specificity, PPV, and NPV of the CBCL-OCS with the cutoff of 5 were calculated. Results were as follows: sensitivity: 48%, specificity: 91.5% PPV: 15.1%, and NPV: 98.2%.
FIG. 2.
Percentage of at-risk for OCD using the CBCL in the OCD and control groups according to DSM-IV criteria using the DAWBA. x-axis: Control and OCD according to DSM-IV criteria using the DAWBA. y-axis: Percentage of at-risk for OCD according to the CBCL in each group. CBCL, Child Behavior Checklist; DAWBA, Developmental and Well-Being Assessment; OCD, obsessive-compulsive disorder.
Discussion
To our knowledge, this is the first study to address the OCS in youth population using a dimensional approach. The OCS distribution among the studied population follows a convex downward curve, as expected. Our results indicated that the severity of OCS did not differ between genders and it is (slightly) associated with increasing age. This is in agreement with most of the previous studies (Zohar et al. 1992; Valleni-Basile et al. 1994; Essau et al. 2000; Heyman et al. 2001; Shams et al. 2011; Canals et al. 2012), but in contrast to others that reported a discrete higher prevalence of OCS in boys (Flament et al. 1988; Alvarenga et al. 2015) and to other studies that suggested higher rates of OCS in girls (Brynska and Wolanczyk 2005; Vivan Ade et al. 2014).
There were nonsignificant correlations between OCS and socioeconomic status. This finding is consistent with most epidemiological studies of OCS in pediatric populations (Flament et al. 1988; Douglass et al. 1995; Brynska and Wolanczyk 2005; Shams et al. 2011; Jaisoorya et al. 2015), although there are studies that associate OCS with lower socioeconomic status (Heyman et al. 2001; Voltas et al. 2014). Likewise, we found no correlation between global IQ and OCS. These data are in line with findings from studies by Douglass et al. (1995), but not others (Zohar et al. 1992; Heyman et al. 2001; Peterson et al. 2001; Grisham et al. 2011). The dimensional approach allows the conclusion that IQ is not related to the severity of OCS, which may explain some of the inconsistencies in the previous literature data.
On the other hand, OCS severity was moderately correlated to functional impairment, as well as to internalizing and externalizing behaviors. This was an expected result that supports the idea of a continuum between mild OC symptoms and low impairment in contrast to severe OC symptoms and high functional impairment (Apter et al. 1996; Fontenelle and Hasler 2008). The analysis of positive attributes and social aptitudes showed negative correlations, also expected, but surprisingly, mild correlations. These results is in accordance to Grisham et al. (2011) who reported that social isolation and internalizing and conduct problems in childhood predicted later OCD.
The prevalence of children with significant OCS or at-risk for OCD was 9.7% using the criteria of the CBCL-OCD subscale (5 or more OCS) (Nelson et al. 2001; Hudziak et al. 2006). These data are in accordance with prevalence rates reported in four different studies (Apter et al. 1996; Fullana et al. 2009; Shams et al. 2011; Canals et al. 2012) but differed from others (Flament et al. 1988; Zohar et al. 1992; Valleni-Basile et al. 1994; Mahfouz et al. 2009; Vivan Ade et al. 2014). The differences in OCS prevalence rates may have been due to different methodological approaches.
The at-risk for OCD group had several internalizing, externalizing, and social behavior problems compared to the unaffected control group. This finding meets with studies on the most recent literature that emphasize the pathological and maladaptive features of OCS, instead of the normal or adaptive aspects of OCS (Fullana et al. 2009; Canals et al. 2012; Alvarenga et al. 2015). The at-risk group was also at increased risk for generalized anxiety, major depression, separation anxiety, and tic disorder.
The more robust analysis (LR model) indicated that tic disorder, anxiety disorders grouped, and depression were strongly associated with the presence of OCS. These comorbidities resemble the pattern reported in full-blown pediatric OCD (Flament et al. 1988; Zohar et al. 1992; Heyman et al. 2001; de Mathis et al. 2008; 2013; Shams et al. 2011; Canals et al. 2012; Vivan Ade et al. 2014; Voltas et al. 2014; Ortiz et al. 2015). OCS were significantly associated with functional impairment even when controlled by the pattern of comorbidities When considering the positive attributes and social aptitude, no associations were found. This is probably because the presence of psychiatric comorbidity has a synergistic action worsening the functional impairment already caused by the OCS. This information is relevant, since not only full blown OCD, but “just OCS” (Pauls et al. 1995) are commonly associated with other psychiatric disorders in children. In the present report, 61% of the at-risk for OCD group showed, at least, one psychiatric comorbidity, which is in accordance with earlier studies (Heyman et al. 2001; Shams et al. 2011; Canals et al. 2012; Vivan Ade et al. 2014). Interestingly, not only internalizing behavior, but also externalizing behavior was associated with OCS. The role of externalizing behaviors in OCS has been recently emphasized in the literature (Grisham et al. 2011; Lebowitz et al. 2011; Alvarenga et al. 2015). Coercive behavior was positively correlated to OCS severity, as it is used to impose family accommodation (Geller et al. 1996; Peris et al. 2008; Lebowitz et al. 2011).
Finally, the proposed model of screening using CBCL-OCS criteria in our sample resulted in excellent specificity and NPV, however, with low sensitivity and PPV, which undermines its use as a single screening tool for clinical OCD. On the other hand, it is plausible that the at-risk group for OCD by the CBCL criterion determines a subgroup with a high index of psychopathology and pattern of comorbidity that resembles the full-blow OCD, which makes us question the validity of the DSM-IV categorical model for pediatric OCD.
This study has several limitations. It is a cross-sectional study, susceptible to recall bias. Correlations of the severity of OCS with clinical and sociodemographic variables would be better examined in a longitudinal design. All diagnoses were established by proxy (mothers in 91.5% of cases). Furthermore, questionnaires were applied by a lay interviewer despite checked by senior psychiatrists.
Conclusions
A dimensional approach associates the severity of OCS with increasing psychopathology (behavioral and social problems, psychiatric comorbidity). Clinically significant OCS are a prevalent phenomenon in children (prevalence around 10%) and are associated with older age, higher frequency of behavioral problems, functional impairment, and psychiatric comorbidities. The pattern of psychiatric comorbidities found in the “OCS” group resembles that found in full-blown OCD. The cutoff point of 5 or higher in the CBCL proposed in the literature determined an at-risk for OCD group very similar phenotypically to OCD, but its use as a single screening tool may be questioned. On the other hand, our results question the validity of the use of a categorical diagnosis for pediatric OCD.
Clinical Significance
The dimensional approach of the psychopathological phenomena, as an alternative to the categorical method, is one of the targets of current nosology in psychiatry. This study provides new evidence for the existence of a positive association between OCS severity and functional impairment in youth, which supports the notion of a continuum between OCS and OCD. From a clinical perspective, these data suggest that early intervention, directed at children with subclinical symptoms detected by mean of a screening tool like the CBCL-OCD, appears relevant to prevent the development of more severe psychopathology and greater functional impairment.
Acknowledgments
The authors of this article would like to acknowledge the professors Giovanni Salum, Guilherme Polanczyk, Jair Mari, Luis Rohde, and Rodrigo Bressan for the work involved in carrying out this cohort.
Disclosures
Laura O. Saad and Raony C. Cesar: No disclosure; Maria C. do Rosário: Acted as a speaker for Shire and Novartis in the last 5 years; Marcelo C. Bastituzzo, Marcelo Q. Hoexter, and Gisele G. Manfro: No disclosure to report; James F. Leckman: Received support from the National Institutes of Health (salary and research funding), Tourette Association of America (formerly the Tourette Syndrome Association), Grifols (formerly Talecris), UBS Optimus Foundation, the Open Road Alliance, John Wiley & Sons (book royalties), McGraw-Hill (book royalties), and Oxford University Press (book royalties). He also serves on the scientific advisory boards of National Organization for Rare Disorders (NORD) and the Brain and Behavior Research Foundation (formerly NARSAD). Roseli G. Shavitt: Travel grant from Lundbeck to attend the 23rd Annual International OCF M; Eurípedes C. Miguel and Pedro G. Alvarenga: No disclosure to report.
References
- Achenbach TM: Integrative Guide to the 1991 CBCL/4-18, YSR, and TRF Profiles (1st ed.). Burlington (Vermont), University of Vermont, 1991 [Google Scholar]
- Alvarenga PG, do Rosario MC, Cesar RC, Manfro GG, Moriyama TS, Bloch MH, Shavitt RG, Hoexter MQ, Coughlin CG, Leckman JF, Miguel EC: Obsessive-compulsive symptoms are associated with psychiatric comorbidities, behavioral and clinical problems: A population-based study of Brazilian school children. Eur Child Adolesc Psychiatry 25:175–182, 2016 [DOI] [PubMed] [Google Scholar]
- Alvarenga PG, Mastrorosa RS, Rosário MC: Obsessive compulsive disorder in children and adolescents. In: The IACAPAP Textbook of Child and adolescent Mental Health (1st ed.). Edited by Rey JM. Paris: IACAPAP; pp 1–17, 2012 [Google Scholar]
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- Apter A., Fallon TJ, Jr., King RA, Ratzoni G, Zohar AH, Binder M, Weizman A, Leckman JF, Pauls DL, Kron S, Cohen DJ: Obsessive-compulsive characteristics: From symptoms to syndrome. J Am Acad Child Adolesc Psychiatry 35:907–912, 1996 [DOI] [PubMed] [Google Scholar]
- Black DW, Gaffney GR: Subclinical obsessive-compulsive disorder in children and adolescents: Additional results from a “high-risk” study. CNS Spectr 13(9 Suppl 14):54–61, 2008 [DOI] [PubMed] [Google Scholar]
- Bordin IA, Rocha MM, Paula CS, Teixeira MC, Achenbach TM, Rescorla LA, Silvares EF: Child Behavior Checklist (CBCL),Youth Self-Report (YSR) and Teacher's Report Form(TRF): An overview of the development of the original and Brazilian versions. Cad Saude Publica 29:13–28, 2013 [DOI] [PubMed] [Google Scholar]
- Brynska A, Wolanczyk T: Epidemiology and phenomenology of obsessive-compulsive disorder in non-referred young adolescents: A Polish perspective. Eur Child Adolesc Psychiatry 14:319–327, 2005 [DOI] [PubMed] [Google Scholar]
- Canals J, Hernandez-Martinez C, Cosi S, Voltas N: The epidemiology of obsessive—compulsive disorder in Spanish school children. J Anxiety Disord 26:746–752, 2012 [DOI] [PubMed] [Google Scholar]
- de Bruijn C, Beun S, de Graaf R, ten Have M, Denys D: Subthreshold symptoms and obsessive-compulsive disorder: Evaluating the diagnostic threshold. Psychol Med 40:989–997, 2010 [DOI] [PubMed] [Google Scholar]
- de Mathis MA, Diniz JB, Hounie AG, Shavitt RG, Fossaluza V, Ferrao Y, Leckman JF, de Braganca Pereira C, do Rosario MC, Miguel EC: Trajectory in obsessive-compulsive disorder comorbidities. Eur Neuropsychopharmacol 23:594–601, 2013 [DOI] [PubMed] [Google Scholar]
- de Mathis MA, do Rosario MC, Diniz JB, Torres AR, Shavitt RG, Ferrao YA, Fossaluza V, de Braganca Pereira CA, Miguel EC: Obsessive-compulsive disorder: Influence of age at onset on comorbidity patterns. Eur Psychiatry 23:187–194, 2008 [DOI] [PubMed] [Google Scholar]
- do Nascimento E, de Figueiredo VLM: WISC-III and WAIS-III: Alterations in the current American original versions of the adaptations for use in Brazil. Psicol Reflex Crit 15:603–612, 2002 [Google Scholar]
- Douglass HM, Moffitt TE, Dar R, McGee R, Silva P: Obsessive-compulsive disorder in a birth cohort of 18-year-olds: Prevalence and predictors. J Am Acad Child Adolesc Psychiatry 34:1424–1431, 1995 [DOI] [PubMed] [Google Scholar]
- Essau CA, Conradt J, Petermann F: Frequency, comorbidity, and psychosocial impairment of anxiety disorders in German adolescents. J Anxiety Disord 14:263–279, 2000 [DOI] [PubMed] [Google Scholar]
- Figueiredo VLM, Pinheiro S, do Nascimento E: Uma adaptação brasileira do teste de inteligencia WISC-III. Curso de Pos-Graduação em Psicologia [An adaptation of the brazilian intelligence test WISC-III],2:101–107, 2001 [Google Scholar]
- Flament MF, Whitaker A, Rapoport JL, Davies M, Berg CZ, Kalikow K, Sceery W, Shaffer D: Obsessive compulsive disorder in adolescence: An epidemiological study. J Am Acad Child Adolesc Psychiatry 27:764–771, 1988 [DOI] [PubMed] [Google Scholar]
- Fleitlich-Bilyk B, Goodman R: Prevalence of child and adolescent psychiatric disorders in southeast Brazil. J Am Acad Child Adolesc Psychiatry 43:727–734, 2004 [DOI] [PubMed] [Google Scholar]
- Fontenelle LF, Hasler G: The analytical epidemiology of obsessive-compulsive disorder: Risk factors and correlates. Prog Neuropsychopharmacol Biol Psychiatry 32:1–15, 2008 [DOI] [PubMed] [Google Scholar]
- Fontenelle LF, Mendlowicz MV, Versiani M: The descriptive epidemiology of obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry 30:327–337, 2006 [DOI] [PubMed] [Google Scholar]
- Fullana MA, Mataix-Cols D, Caspi A, Harrington H, Grisham JR, Moffitt TE, Poulton R: Obsessions and compulsions in the community: Prevalence, interference, help-seeking, developmental stability, and co-occurring psychiatric conditions. Am J Psychiatry 166:329–336, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller DA, Biederman J, Griffin S, Jones J, Lefkowitz TR: Comorbidity of juvenile obsessive-compulsive disorder with disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry 35:1637–1646, 1996 [DOI] [PubMed] [Google Scholar]
- Goodman R: The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry 40:791–799, 1999 [PubMed] [Google Scholar]
- Goodman R, Ford T, Richards H, Gatward R, Meltzer H: The Development and Well-Being Assessment: Description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry 41:645–655, 2000 [PubMed] [Google Scholar]
- Grisham JR, Fullana MA, Mataix-Cols D, Moffitt TE, Caspi A, Poulton R: Risk factors prospectively associated with adult obsessive-compulsive symptom dimensions and obsessive-compulsive disorder. Psychol Med 41:2495–2506, 2011 [DOI] [PubMed] [Google Scholar]
- Heyman I, Fombonne E, Simmons H, Ford T, Meltzer H, Goodman R: Prevalence of obsessive-compulsive disorder in the British nationwide survey of child mental health. Br J Psychiatry 179:324–329, 2001 [DOI] [PubMed] [Google Scholar]
- Hudziak JJ, Althoff RR, Stanger C, van Beijsterveldt CE, Nelson EC, Hanna GL, Boomsma DI, Todd RD: The Obsessive Compulsive Scale of the Child Behavior Checklist predicts obsessive-compulsive disorder: A receiver operating characteristic curve analysis. J Child Psychol Psychiatry 47:160–166, 2006 [DOI] [PubMed] [Google Scholar]
- Jaisoorya TS, Janardhan Reddy YC, Thennarasu K, Beena KV, Beena M, Jose DC: An epidemological study of obsessive compulsive disorder in adolescents from India. Compr Psychiatry 61:106–114, 2015 [DOI] [PubMed] [Google Scholar]
- Jannuzzi PM, Baeninger R: Qualificação socioeconômica e demográfica das classes da escala Abipeme. Rev Adm São Paulo 31:82–90, 1996. [Socialeconomic and demographic qualification of the classes of the Abipeme scale] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE: Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:593–602, 2005 [DOI] [PubMed] [Google Scholar]
- Lebowitz ER, Motlagh MG, Katsovich L, King RA, Lombroso PJ, Grantz H, Lin H, Bentley MJ, Gilbert DL, Singer HS, Coffey BJ, Kurlan RM, Leckman JF: Tourette syndrome in youth with and without obsessive compulsive disorder and attention deficit hyperactivity disorder. Eur Child Adolesc Psychiatry 21:451–457, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz ER, Omer H, Leckman JF: Coercive and disruptive behaviors in pediatric obsessive-compulsive disorder. Depress Anxiety 28:899–905, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddle EB, Batty MJ, Goodman R: The Social Aptitudes Scale: An initial validation. Soc Psychiatry Psychiatr Epidemiol 44:508–513, 2009 [DOI] [PubMed] [Google Scholar]
- Mahfouz AA, Al-Gelban KS, Al Amri H, Khan MY, Abdelmoneim I, Daffalla AA, Shaban H, Mohammed AA: Adolescents' mental health in Abha city, southwestern Saudi Arabia. Int J Psychiatry Med 39:169–177, 2009 [DOI] [PubMed] [Google Scholar]
- Nelson EC, Hanna GL, Hudziak JJ, Botteron KN, Heath AC, Todd RD: Obsessive-compulsive scale of the child behavior checklist: Specificity, sensitivity, and predictive power. Pediatrics 108:E14, 2001 [DOI] [PubMed] [Google Scholar]
- Ortiz AE, Morer A, Moreno E, Plana MT, Cordovilla C, Lazaro L: Clinical significance of psychiatric comorbidity in children and adolescents with obsessive-compulsive disorder: Subtyping a complex disorder. Eur Arch Psychiatry Clin Neurosci 266:199–208, 2015 [DOI] [PubMed] [Google Scholar]
- Pauls DL, Alsobrook JP, 2nd, Goodman W, Rasmussen S, Leckman JF: A family study of obsessive-compulsive disorder. Am J Psychiatry 152:76–84, 1995 [DOI] [PubMed] [Google Scholar]
- Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J: Correlates of accommodation of pediatric obsessive-compulsive disorder: Parent, child, and family characteristics. J Am Acad Child Adolesc Psychiatry 47:1173–1181, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson BS, Pine DS, Cohen P, Brook JS: Prospective, longitudinal study of tic, obsessive-compulsive, and attention-deficit/hyperactivity disorders in an epidemiological sample. J Am Acad Child Adolesc Psychiatry 40:685–695, 2001 [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Stein DJ, Chiu WT, Kessler RC: The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry 15:53–63, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salum GA, Gadelha A, Pan PM, Moriyama TS, Graeff-Martins AS, Tamanaha AC, Alvarenga P, Valle Krieger F, Fleitlich-Bilyk B, Jackowski A, Sato JR, Brietzke E, Polanczyk GV, Brentani H, de Jesus Mari J, Do Rosario MC, Manfro GG, Bressan RA, Mercadante MT, Miguel EC, Rohde LA: High risk cohort study for psychiatric disorders in childhood: Rationale, design, methods and preliminary results. Int J Methods Psychiatr Res 24:58–73, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shams G, Foroughi E, Esmaili Y, Amini H, Ebrahimkhani N: Prevalence rates of obsessive-compulsive symptoms and psychiatric comorbidity among adolescents in Iran. Acta Med Iran 49:680–687, 2011 [PubMed] [Google Scholar]
- Tellegen A, Briggs PF: Old wine in new skins: Grouping Wechsler subtests into new scales. J Consult Psychol 31:499–506, 1967 [DOI] [PubMed] [Google Scholar]
- Valleni-Basile LA, Garrison CZ, Jackson KL, Waller JL, McKeown RE, Addy CL, Cuffe SP: Frequency of obsessive-compulsive disorder in a community sample of young adolescents. J Am Acad Child Adolesc Psychiatry 33:782–791, 1994 [DOI] [PubMed] [Google Scholar]
- Vidal-Ribas P, Goodman R, Stringaris A: Positive attributes in children and reduced risk of future psychopathology. Br J Psychiatry 206:17–25, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vivan Ade S, Rodrigues L, Wendt G, Bicca MG, Braga DT, Cordioli AV: Obsessive-compulsive symptoms and obsessive-compulsive disorder in adolescents: A population-based study. Rev Bras Psiquiatr 36:111–118, 2014 [DOI] [PubMed] [Google Scholar]
- Voltas N, Hernandez-Martinez C, Arija V, Aparicio E, Canals J: A prospective study of paediatric obsessive-compulsive symptomatology in a Spanish community sample. Child Psychiatry Hum Dev 45:377–387, 2014 [DOI] [PubMed] [Google Scholar]
- Wechsler D. (ed): WISC-III: Escala de Inteligência Wechsler Para Crianças. São Paulo, Casa do Psicólogo; [WISC-III: Wechsler intelligence scale for children], 2002 [Google Scholar]
- Zohar AH, Ratzoni G, Pauls DL, Apter A, Bleich A, Kron S, Rappaport M, Weizman A, Cohen DJ: An epidemiological study of obsessive-compulsive disorder and related disorders in Israeli adolescents. J Am Acad Child Adolesc Psychiatry 31:1057–1061, 1992 [DOI] [PubMed] [Google Scholar]