Abstract
Background: Many advances in health care fail to reach patients. Implementation science is the study of novel approaches to mitigate this evidence-to-practice gap.
Methods: The American Thoracic Society (ATS) created a multidisciplinary ad hoc committee to develop a research statement on implementation science in pulmonary, critical care, and sleep medicine. The committee used an iterative consensus process to define implementation science and review the use of conceptual frameworks to guide implementation science for the pulmonary, critical care, and sleep community and to explore how professional medical societies such as the ATS can promote implementation science.
Results: The committee defined implementation science as the study of the mechanisms by which effective health care interventions are either adopted or not adopted in clinical and community settings. The committee also distinguished implementation science from the act of implementation. Ideally, implementation science should include early and continuous stakeholder involvement and the use of conceptual frameworks (i.e., models to systematize the conduct of studies and standardize the communication of findings). Multiple conceptual frameworks are available, and we suggest the selection of one or more frameworks on the basis of the specific research question and setting. Professional medical societies such as the ATS can have an important role in promoting implementation science. Recommendations for professional societies to consider include: unifying implementation science activities through a single organizational structure, linking front-line clinicians with implementation scientists, seeking collaborations to prioritize and conduct implementation science studies, supporting implementation science projects through funding opportunities, working with research funding bodies to set the research agenda in the field, collaborating with external bodies responsible for health care delivery, disseminating results of implementation science through scientific journals and conferences, and teaching the next generation about implementation science through courses and other media.
Conclusions: Implementation science plays an increasingly important role in health care. Through support of implementation science, the ATS and other professional medical societies can work with other stakeholders to lead this effort.
Keywords: implementation science, implementation research, knowledge translation, quality improvement, medical society
Contents
Overview
Introduction
Methods
Participants in the Ad Hoc Committee to Develop an ATS Research Statement
Literature Review and Discussion
Definition of Implementation Science
Implementation Science and Related Fields
Conceptual Frameworks
Stakeholder Involvement
Professional Medical Society Engagement in Implementation Science
Recommendations for Professional Medical Societies to Promote Implementation Science
Conclusions
Overview
Patients, clinicians, and health systems struggle with implementing evidence-based practices in pulmonary, critical care, and sleep medicine. Implementation science is a rigorous scientific discipline dedicated to the study of strategies to overcome the evidence-to-practice gap. This Research Statement summarizes the work of an ad hoc multi-stakeholder committee of the American Thoracic Society (ATS) to discuss implementation science and provide recommendations for how implementation science can be applied to pulmonary, critical care, and sleep medicine and the broader clinical and scientific community.
-
1.Definition of implementation science
-
•Implementation science is the study of the mechanisms by which health care interventions are adopted or not adopted in clinical and community settings.
-
•Implementation science is a theory-reliant field that emphasizes complex, multicomponent interventions that target multiple levels of a system and addresses adaptive challenges to behavior change.
-
•Implementation science encompasses the identification of facilitators and barriers (both individual and systemic) to adopting evidence-based care as well as the design and evaluation of interventions to improve implementation, thereby improving health in clinical and community settings.
-
•Implementation science is distinct from implementation itself. Implementation is the act of using systematic methods to adopt certain practices, whereas implementation science seeks to understand how and why adoption occurs or fails and to develop and test novel strategies for implementation.
-
•Implementation science is distinct from clinical effectiveness research, which emphasizes identifying and synthesizing best clinical practices.
-
•
-
2.Conceptual frameworks for implementation science apply to pulmonary, critical care, and sleep medicine
-
•Implementation science uses conceptual frameworks, which are models that allow researchers to systematically develop, coordinate, and evaluate interventions. Conceptual frameworks also facilitate the communication of findings from implementation science.
-
•Multiple valid conceptual frameworks are available. The selection of a conceptual framework depends on the specific research question and setting.
-
•
-
3.
Stakeholder engagement is critical to implementation science in that it provides essential context for identifying research questions, conducting studies, and promoting uptake of study results.
-
4.Professional medical societies can contribute substantially to the field of implementation science
-
•Professional medical societies could consider creating organizational homes that link stakeholders (researchers, front-line clinicians, funding agencies, health care delivery bodies) across diverse disciplines, thus fostering an environment supportive to both implementation and implementation science.
-
•Other important contributions could include developing clinical practice guidelines using rigorous methods and prioritizing targets for implementation that are strong recommendations based on high-quality evidence; collaborating on implementation science studies; and developing internal funding, conference programming, publication priorities, and education and training for implementation science.
-
•
Introduction
Despite advances in our understanding of diseases and how to treat them, health care innovations may be underused, overused, or misused, ultimately failing to benefit patients (1, 2). This problem is ubiquitous in all aspects of health care, including pulmonary, critical care, and sleep medicine. Patients, clinicians, and/or health systems frequently struggle with implementing effective practices in pulmonary, critical care, and sleep medicine, ranging from pulmonary nodule surveillance (3–5) to the adoption of lung-protective ventilation strategies (6), to the use of positive airway pressure for obstructive sleep apnea (7). Implementation science is intended to remedy this problem by developing and testing strategies that can help patients, clinicians, and health systems overcome this evidence-to-practice gap.
Translating new scientific discoveries into improved patient care is an active process; passive diffusion of evidence into practice is unreliable and inefficient. For more than a decade, the National Institutes of Health has promulgated research activities across a “translational spectrum” that includes biomedical discovery (understanding the biology of health and disease and identifying therapeutic targets), clinical efficacy research (assessing pharmaceutical or behavioral interventions delivered by research personnel in highly selected patient populations), clinical effectiveness research (evaluating the effects of interventions in practice or community settings, when delivered by clinical personnel), and implementation science (8–10).
For example, in the translational pathway of lung-protective ventilation for patients with acute respiratory distress syndrome (ARDS), biomedical discovery is represented by studies that demonstrated that higher tidal volumes and high airway pressures are injurious in animal models of lung injury and patients with ARDS (11–16); clinical efficacy research was conducted by experts in the ARDS Network and others on the effect of lung-protective ventilation on mortality in highly controlled research settings (17), and clinical effectiveness research could include studies of the benefits and harms of lung-protective ventilation compared with usual care or other treatment strategies in settings that are more representative of clinical practice (18, 19). In contrast, implementation science would seek to identify the facilitators and barriers of lung-protective ventilation use and use this knowledge to design strategies to improve its adoption and sustainability (6, 20–25).
The goals of this Official ATS Research Statement are to: (1) define implementation science and contrast it to related research activities; (2) discuss how existing conceptual frameworks for implementation science apply to pulmonary, critical care, and sleep medicine; (3) elucidate the essential role of stakeholders in implementation science; and (4) develop recommendations about how professional medical societies such as the ATS can more effectively support implementation science.
Methods
This project was developed in response to the ATS/NHLBI Implementation Research Workshop on May 17, 2014 (26), which called for an official ATS Research Statement to increase understanding within the clinical and scientific community about the role of implementation science in the context of broader efforts to close the evidence-to-practice gaps for pulmonary, critical care, and sleep disorders and to formulate recommendations about how the ATS could serve as an effective collaborator in such efforts.
Participants in the Ad Hoc Committee to Develop an ATS Research Statement
The ad hoc committee included ATS members with clinical expertise in pulmonary, critical care, and sleep medicine, as well as individuals with expertise in implementation science methodology, quality improvement, clinician and patient education, behavioral science, health economics, decision science, clinical trials, stakeholder engagement, health equity, health systems leadership, and a representative of the ATS Public Advisory Roundtable (see the online supplement). Potential conflicts of interest were disclosed and managed in accordance with the policies and procedures of the ATS.
Literature Review and Discussion
The committee participants were divided into three working groups, each focused on one of the following topics: (1) the definition of implementation science and its role within the translational research spectrum, (2) the use of conceptual frameworks to support implementation science, and (3) recommendations for the ATS and other professional medical societies about how they can engage in implementation science.
From February to May, 2015, the three co-chairs conducted a targeted literature search to facilitate discussions within the three working groups. Each working group was tasked with summarizing relevant literature identified during these searches and formulating provisional recommendations for further discussion at an in-person meeting on May 15, 2015, during the ATS International Conference in Denver, Colorado. During the course of these meetings, each working group independently identified the importance of involving stakeholders as a topic to include in this research statement.
A briefing book summarizing the work to date was distributed to participants in advance of the in-person meeting. The chairs led the discussion to further revise the recommendations for this Research Statement. Drafts of the Research Statement were circulated to all members of the committee to seek further feedback, and the revised draft was presented to the committee and a representative of the Executive Committee at the ATS Leadership Summit on September 17, 2015, in Orlando, Florida. The Research Statement was revised on the basis of this feedback and finalized with the input of all committee members.
Definition of Implementation Science
Implementation science is the scientific study of the mechanisms by which evidence-based health care interventions are adopted or not adopted in clinical and community settings.
These mechanisms may include process factors (e.g., patient or clinician behavior) and contextual factors (e.g., social support and other social determinants of health) that either mediate (i.e., factors that are in the causal pathway between implementation strategy and adoption of the intervention) or moderate (i.e., factors that strengthen or weaken the effects of the implementation strategy on the causal pathway) the delivery of care. Using the example of lung-protective ventilation in ARDS described above, if an implementation strategy includes a text reminder to the clinician’s mobile phone to lower a patient’s tidal volume, a mediating factor could be the extent to which the clinician reads his/her text messages. On the other hand, a moderating factor could be a clinician’s attitude toward lung-protective ventilation itself, which could modify the extent to which such text reminders lead to use of lower tidal volumes in individual patients. Implementation science also includes the development and evaluation of specific strategies that target these mediating and moderating mechanisms to accelerate improvement in health care delivery.
In addition, implementation science seeks to understand the core components (components of implementation strategies that are important to achieving adoption regardless of the context and setting) and adaptable components (components of implementation strategies that require tailoring to the patient, clinician, or health care system to achieve adoption) of the frequently multicomponent strategies used to facilitate adoption or de-adoption of clinical practices. Implementation science can also be used to study the mechanisms by which ineffective or harmful interventions are discarded.
Implementation Science and Related Fields
The importance of implementation science in the translational research spectrum can be understood best in the context of its historical development and its relationship with other fields.
Implementation is the act of translating evidence into practice. Systematic and intentional, it is concerned with improving care. Implementation science is the study of implementation (i.e., uncovering broadly applicable barriers to evidence adoption and developing and testing novel strategies to overcome those barriers).
Historically, several distinct intellectual traditions have developed that fall under the umbrella of implementation science, including quality improvement research and diffusion of innovations theory. Quality improvement research, with roots in industrial engineering and manufacturing, is focused on small, rapid-cycle tests of change (e.g., “plan-do-study-act” cycles), emphasizes local change, and addresses challenges of a more technical or logistical nature from an operational perspective (27–31).
In contrast, another implementation science tradition is rooted in the diffusion of innovations theory, which was developed in fields as diverse as sociology, anthropology, education, communication, economics, and management science. This tradition is focused on behavioral change. Early observations of individual behavior led to the development of the classic theory of the diffusion of innovations first proposed by Rogers (32), which has been expanded by Greenhalgh and others into many modern frameworks for implementation science (33–35).
An example of implementation is instructive. Consider a practice plan beginning to use a new bronchodilator inhaler for the management of chronic obstructive pulmonary disease on the basis of a new clinical practice guideline. Implementation in this area could consist of the practice plan developing a plan to increase inhaler use that targets anticipated logistical and process challenges, executing the plan, monitoring inhaler use to see if it increases, refining the intervention, and repeating the cycle until inhaler use is at target levels. In contrast, implementation science systematically identifies potential clinician-, patient-, and system-based facilitators of and barriers to adoption of the new bronchodilator inhaler and designs and evaluates a strategy that targets key facilitators and barriers (e.g., educational outreach to clinicians to overcome attitude or knowledge barriers, payment incentives to clinicians and patients to overcome payer barriers, electronic health record alerts to clinicians or a checklist or protocol to overcome systemic barriers in the recognition of eligible patients) to improve adoption of the inhaler. The characteristics of implementation science would lead to generalizable knowledge about barriers to implementation of the new inhaler and a suite of interventions that would provide a path to improved widespread adoption across practices. In summary, whereas existing strategies to translate evidence into practice either do not work, are only incrementally effective, or are too expensive (36, 37), implementation science strives to develop more effective, targeted strategies that are generalizable to other settings with similar barriers or likely to have similar barriers.
The boundary between implementation science and a number of other related research activities may not always be clear (Table 1). Clinical effectiveness research is focused on comparing health and economic outcomes of specific interventions in real-world clinical or community settings (38), whereas investigating the mechanisms by which the interventions are adopted in these real-world settings is a distinguishing feature of implementation science. Some studies use a hybrid effectiveness-implementation design (39); for example, a researcher may be testing the effects of an influenza vaccination campaign on work absenteeism during the fall and winter months (clinical effectiveness research) while also investigating whether a nurse-led communication strategy to promote vaccination overcomes known barriers to vaccination across different worksites (implementation science). Diffusion and dissemination focus on passive and active mechanisms, respectively, through which information reaches a target audience (40, 41). Implementation science overlaps significantly with diffusion and dissemination (41).
Table 1.
Terminology of Implementation Science and Other Related Fields
| Field | Definition | Examples |
|---|---|---|
| Clinical effectiveness research | Evaluating different approaches to diagnose, treat, or prevent disease in real-world clinical and community settings, using a range of health and economic outcomes as end points. | • Comparing effectiveness of peer coaching using outbound phone calls vs. a toll-free number that patients with chronic obstructive pulmonary disease can use to get answers to questions about use of supplemental oxygen |
| • Testing the use of step-up therapy with leukotriene modifiers vs. inhaled corticosteroids in children with uncontrolled asthma | ||
| Diffusion | Passive, untargeted, unplanned, and uncontrolled spread of innovations to end users (patients, caregivers, clinicians, and other health-related decision makers). Alternatively, the generic process through which an innovation is communicated via channels over time among members of a social system. | • Discussions among individuals in a group practice after a continuing medical education meeting |
| • Use of online chat rooms by people with specific health conditions after they learn about a new medical discovery from a newspaper article | ||
| Dissemination | Active approach of spreading an innovation to a target end user via determined channels using a planned strategy. Alternatively, what the source or sponsor does to reach and affect the decisions or behavior of potential end users. | • Use of peer-reviewed publications, conferences, and newsletters targeting members of a professional society |
| • “Grand rounds” at an academic health care center | ||
| Implementation science | Scientific study of the mechanisms by which effective health care interventions are adopted or discarded in clinical and community settings. Also includes the development and testing of specific strategies that target mediating or moderating mechanisms to accelerate the adoption or discontinuation of health care in clinical and community settings. | • Evaluation of strategies to promote use of directly observed tuberculosis therapy |
| • User-centered observations to understand how asthma action plans inform decisions made by caregivers of children with asthma |
Conceptual Frameworks
Conceptual frameworks are “strategic or action-planning models that provide a systematic way to develop, manage, and evaluate interventions” (41, 42). Due to their connection between observations and theory, conceptual frameworks serve multiple positive roles for the conduct of implementation science. First, conceptual frameworks provide definitions and terms that can be used broadly and consistently across multiple users and projects. Second, conceptual frameworks enhance the interpretability of individual research findings and allow them to be more easily tested by others. Third, conceptual frameworks can help researchers focus on the essential mechanisms of behavioral change by targeting relevant mediators and moderators. Failure to use a framework may make it less likely for implementation to succeed, because frameworks help to identify the factors that predict implementation success, enable the design of implementation strategies that target these factors, and facilitate measurement (41). For these reasons, funding agencies encourage the use of conceptual frameworks (26) to facilitate the review of proposed projects (43, 44).
More than 100 overlapping theories, conceptual models, and frameworks have been proposed to describe the process of implementation (42), classify various implementation strategies (45), and provide guidance when evaluating implementation efforts (46). A recent book describes several of these frameworks for implementation science and their implications for health care and public health (47).
We recommend the use of a conceptual framework in the planning and execution of studies using implementation science methods. However, there is no single “best” conceptual framework that will apply to all implementation gaps and across all clinical settings. Different conceptual frameworks can serve different purposes and are useful in different settings. When selecting a framework for implementation science, there are several characteristics that should be kept in mind. First, the framework or frameworks that are selected should be sufficiently comprehensive, such that all potentially critical factors that may affect implementation are considered (41). Second, the framework(s) should focus on the essential processes germane to the specific research question—for example, if the effect of an organizational change intervention on patient outcomes is being studied, frameworks that address organizational and systems barriers to implementation as well as outcome measurement are required.
In particular, frameworks should lead to an actionable plan and specific methods for one or more of the following: (1) identifying the facilitators and barriers to adoption of implementation-ready interventions, (2) designing implementation strategies or interventions that target barriers to adoption, and (3) testing these strategies in observational studies or clinical trials to evaluate whether they lead to initial and sustainable adoption. Table 2 lists several examples of frameworks that could be used to address research questions related to pulmonary, critical care, and sleep medicine that fall within these categories. The table is not intended to preclude consideration of other frameworks or to limit the application of a suggested framework to a particular category of questions. It is only meant to provide additional detail about some commonly used frameworks and provide insight into how they might be applied in an implementation science study.
Table 2.
Selecting a Conceptual Framework for Implementation Science
| Example of Specific Implementation Research Question | Family of Questions | Overall Goal | Theory or Conceptual Framework (Examples) |
|---|---|---|---|
| What are the barriers to and enablers of implementing asthma clinical pathways in community hospitals? | What are the behavioral and contextual barriers to and enablers of implementation? What component(s) should be included in the implementation strategy to overcome the barriers and enhance the enablers? | Develop an implementation strategy to translate research into practice | Behavior Change Wheel (59); PRECEDE (60) |
| What components should be included in a strategy to implement lung-protective ventilation in patients with ARDS? | |||
| What are the barriers to and enablers of implementing a behavioral weight loss program into a sleep apnea clinic? | |||
| Can best practices for asthma clinical pathway implementation be adapted to community hospitals? | What factors explain whether or not an implementation strategy is effective? Can a successful implementation strategy or health program be adapted to a different setting? | Understand what influences implementation outcomes | Consolidated Framework for Implementation Research (48); Theory of Diffusion (32) |
| What factors reduced the adoption of lung-protective ventilation in patients with ARDS by respiratory therapists? | |||
| Can a general behavioral weight loss program be adapted for use in a sleep apnea clinic? | |||
| Does a strategy to implement asthma clinical pathways improve asthma management in community hospitals? | Is an implementation strategy effective in translating research into practice? | Evaluate implementation strategy using process and clinical outcomes | RE-AIM (49); PRISM (61); Logic Model (62) |
| What is the effect of an implementation strategy to use lung-protective ventilation in patients with ARDS on mortality and ventilator duration? | |||
| Does adding a behavioral weight loss program into sleep apnea care reduce cardiovascular risk? |
Definition of abbreviations: ARDS = acute respiratory distress syndrome; PRECEDE = Predisposing, Reinforcing, and Enabling Causes in Education Diagnosis and Evaluation; PRISM = Practical, Robust Implementation and Sustainability Model; RE-AIM = Reach, Effectiveness, Adoption, Implementation, Maintenance.
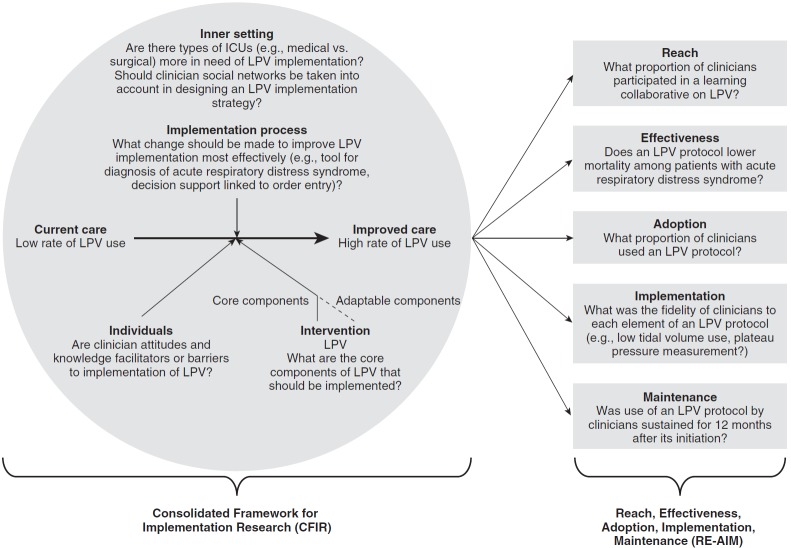
Figure 1 illustrates how two conceptual frameworks could be applied to a specific topic, in this case the implementation of lung-protective ventilation for ARDS. The Consolidated Framework for Implementation Research (CFIR) is a framework that synthesizes the concepts of many previous theories related to implementation science (48). CFIR comprises five domains:
-
•
Intervention: the characteristics of the evidence-based practice or innovation to be implemented, including its core and adaptable components
-
•
Outer setting: general context (social, political, economic) within which the organization undergoing implementation resides
-
•
Inner setting: specific context (structural, political, cultural) through which implementation will occur
-
•
Individuals: the people involved in the implementation process
-
•
Implementation process: the change process required to effect implementation
Figure 1.
An example of the application of conceptual frameworks to a specific intervention (lung-protective ventilation [LPV] for acute respiratory distress syndrome). ICU = intensive care unit.
The following are examples of studies that could use the CFIR framework in their design.
-
1.
A survey of critical care clinicians aiming to investigate facilitators and barriers to adoption of lung-protective ventilation could include topics that derive from several CFIR domains: an evaluation of the quality of evidence supporting lung-protective ventilation (Intervention); clinicians’ perceptions that lung-protective ventilation is being implemented at peer organizations (Outer Setting); clinicians’ perceptions of the climate at a clinician’s organization for lung-protective ventilation implementation or the social networks of clinicians within an organization (Inner Setting); clinicians’ attitudes toward lung-protective ventilation and any knowledge deficits (Individuals); clinician reporting of the extent to which their institution is planning, engaging in, or executing the necessary steps to implement lung-protective ventilation (Implementation Process).
-
2.
An electronic health record screening tool that aims to improve recognition of ARDS would need to take into account several aspects of Implementation Process: planning (e.g., designing the screening tool to take into account stakeholder needs and communication channels), engaging (e.g., identifying and enlisting opinion leaders to lead implementation efforts), executing the intervention, and evaluating its impact.
Reach, Effectiveness, Adoption, Implementation, Maintenance (RE-AIM) is an evaluation framework that is used to identify which aspects of implementation should be evaluated as outcomes (41, 49). For the ARDS screening tool described above, the RE-AIM framework would direct researchers to focus, for example, on measures of adoption of the screening tool (what proportion of clinicians use or respond to the prompt?) or maintenance of the tool (how well is the screening tool sustained over time?).
Stakeholder Involvement
The theme of early and continuous stakeholder engagement emerged from all three working groups as especially important to the success of both implementation and implementation science. Stakeholders can inform implementation science by engaging in the following activities: evidence prioritization (stakeholders participating in defining and prioritizing evidence gaps to guide the selection of the research question[s]), evidence generation (collaborating in the conduct of the study to fill evidence gaps), evidence dissemination (diffusion of new knowledge to end users, such as patients or clinicians), evidence integration (uptake and appropriate use of new knowledge by end users), and feedback (communicating to researchers the extent to which the new knowledge addressed the needs of end users). Which stakeholders are critical to implementation science depends on the research question and may include patients, their caregivers, and advocacy groups; community members; providers (e.g., clinicians across disciplines, care-delivery systems, professional societies representing clinicians); purchasers (e.g., governments, employers, self-insured consumers); payers (insurers, Centers for Medicare and Medicaid Services, individuals with deductibles); administrators (e.g., clinic director or chief executive officer of a health plan); policymakers (e.g., members of Congress); product makers (drug and device manufacturers); and researchers (50).
Professional Medical Society Engagement in Implementation Science
By virtue of their multidisciplinary nature and potential to provide a unifying forum for their field, professional medical societies are uniquely poised to develop clinical practice guidelines, to lead dissemination efforts, and to develop tools to facilitate the act of implementation (51, 52). However, how professional medical societies can participate in and facilitate implementation science remains largely unexplored. The traditional role of professional societies has been in the realm of evidence generation, by providing a vehicle for scientific collaboration, the sharing of content, and the production of clinical guidelines. Leadership in implementation science activities, including collaboration with crucial stakeholders, can potentially serve to improve the successful adoption of evidence known to improve patient outcomes.
To date, professional medical societies, including the ATS, have largely created tools for local implementation (e.g., clinical practice guidelines, quality measures, continuing medical education) without significantly focusing on promoting the implementation science that would make these tools more effective (Table 3) (53–57). Several other professional societies are engaged in quality improvement, dissemination, and the act of implementation (e.g., clinical practice guidelines, the American Heart Association’s Get With the Guidelines, educational initiatives such as maintenance of certification and performance improvement modules, and registries) (58). A systematic review of how other professional societies are supporting implementation science and the effectiveness of such support is outside the scope of work for this statement but could be the basis of future work in this area. Whether these efforts have translated to improvements in care or outcomes is unclear. These strategies do not usually anticipate or address the barriers health care clinicians, patients, and systems encounter in translating evidence into practice, the importance of behavioral change, or the potential benefits of multicomponent interventions targeting multiple levels of a system. Implementation science is focused on these critical issues.
Table 3.
Examples of Current American Thoracic Society Efforts in Implementation Science and Related Fields
| Dissemination | International Conference programming |
| Development of clinical practice guidelines | |
| International Guidelines Center resources | |
| National Guideline Clearinghouse | |
| Patient information materials | |
| Maintenance of certification questions | |
| Performance measures—development or maintenance | Evaluation of COPD using spirometry (NQF #0091/PQRS #051) (63, 64) |
| Bronchodilator therapy for COPD (NQF #0102/PQRS #052) (63, 64) | |
| Quality improvement | Quality Improvement and Implementation Committee |
| International Conference programming | |
| Develop MOC performance improvement products | |
| Publication in ATS journals | |
| Implementation science | Revising the scope of the Quality Improvement Committee to become the Quality Improvement and Implementation Committee |
| International Conference programming (2015 postgraduate course on implementation science) | |
| Documents Development and Implementation Committee web-based toolkit | |
| • Clinical practice guideline summary for clinicians | |
| • Summary of implementation barriers and approaches | |
| • Podcasts | |
| • Slide sets | |
| • List of expert contacts for outreach | |
| • Links to clinical practice guidelines, International Guidelines Center resources, and patient information materials |
Definition of abbreviations: ATS = American Thoracic Society; COPD = chronic obstructive pulmonary disease; MOC = maintenance of certification; NQF = National Quality Forum; PQRS = Physician Quality Reporting System.
There are barriers within professional medical societies to supporting implementation science. Inadequate understanding about the differences between implementation science and the act of implementation, quality improvement, and dissemination is an important barrier and one that this research statement is designed to address. In addition, implementation science experts may be located in different parts of the society, with no clearly defined “home” and little mechanism for coordination or communication. Indeed, the historical fracturing of implementation science within a professional medical society is at odds with the synergy inherent in successful implementation science.
Recommendations for Professional Medical Societies to Promote Implementation Science
Professional medical societies can overcome the above barriers—and become leaders in implementation science—by building on their legacy in discovery, efficacy, and effectiveness science; dissemination; and quality improvement (26). Because of the potentially significant financial investment, professional societies should carefully consider whether the involvement in implementation science fits with their overall mission and vision. First and foremost, societies could consider creating or empowering an existing structure to specifically address implementation science as a distinct discipline. The society could consider providing financial and staffing resources for this structure to specifically support implementation science. Such a structure would bridge communication gaps within an inherently multihome organization and create a unified vision for how implementation science can be further advanced, including through advocacy efforts involving Congress, the National Institutes of Health, and other groups. There is a danger that creating a new structure within a society could merely lead to yet another silo, removing implementation science experts from other areas where they may have closer contact with “on-the-ground” practitioners and other scientists. This problem can be mitigated by ensuring regular, direct communication between the new implementation science home and other areas of the medical society and by implementation science experts not discontinuing their existing affiliation with other key committees and groups throughout the organization; other recommendations that would mitigate this potential problem are discussed below.
The ATS has expanded the Quality Improvement and Implementation Committee (QIIC) to include content and scientific experts from implementation science, quality improvement, health services, education, and ATS leadership. Now that the ATS has taken this step to build an implementation science home, the charge of the QIIC could be expanded to include specific implementation science benchmarks. The QIIC would promote communication, collaboration, and strategic development of implementation science agendas across the existing assemblies and committees of the ATS. It would also allow a well-coordinated approach to fostering society interactions with key stakeholders in funding, policy, patient advocacy, and health care bodies.
Once an implementation science home is created and financial and staffing resources are provided, the professional society and its members (e.g., ATS members) would have a multidisciplinary collaborative team to go to for their implementation science needs. Table 4 lists some activities that professional societies may consider.
Table 4.
Recommendations for Professional Medical Societies to Consider for Supporting Implementation Science
| Create an organizational home for implementation science and provide financial and staffing support |
| Link front-line clinicians with implementation scientists to rigorously study innovations in care delivery, and use existing quality improvement programs as laboratories to study novel implementation approaches |
| Prioritize the use of rigorous methods to develop clinical practice guidelines that explicitly rate the quality of evidence and the strength of recommendations, and prioritize targets for implementation that are strong recommendations based on high-quality evidence (low risk of bias) (65) |
| Seek opportunities to be active collaborators in the conduct of implementation science studies (e.g., society-driven comparative implementation studies, convening stakeholders to prioritize evidence, and identify opportunities to disseminate study results) |
| Advocate with funding agencies to set the research agenda for implementation science in their field |
| Assist individual implementation researchers in obtaining grants, and form a consortium for investigators to share strategies and methods |
| Assist external stakeholders in collaborating on the planning and conduct of implementation science studies |
| Collaborate with fiscal bodies that are responsible for health care delivery, seeking opportunities to link science with care improvement |
| Consider implementation science studies when making internal funding decisions |
| Create implementation science programming at professional society conferences (e.g., scientific symposia and postgraduate courses) |
| Promote implementation science through scientific journals (e.g., American Journal of Respiratory and Critical Care Medicine and Annals of the American Thoracic Society), and encourage journal editors to explicitly seek articles in implementation science |
| Link successful implementation strategies with toolkits that promote local adoption (e.g., websites, protocols, order sets, and videos) |
| Teach the next generation about implementation science through continuing medical education, workshops, and other media, and support their research through internal funding mechanisms |
Conclusions
Implementation science is the part of the translational research spectrum that focuses on understanding the mechanisms by which health care interventions are adopted or not adopted in clinical and community settings. There are multiple opportunities for professional medical societies such as the ATS to more fully leverage the expertise of their members to support implementation science. By leading the effort to support implementation science, the ATS can help to narrow the evidence-to-practice gap and potentially improve care.
Acknowledgments
This official research statement was prepared by an ad hoc committee of the Assembly on Behavioral Science and Health Services Research.
Members of the committee are as follows:
Curtis H. Weiss, M.D., M.S. (Co-Chair)
Jerry A. Krishnan, M.D., Ph.D. (Co-Chair)
Carey C. Thomson, M.D., M.P.H. (Co-Chair)
David H. Au, M.D., M.S.
Bruce G. Bender, Ph.D.
Shannon S. Carson, M.D.
Adithya Cattamanchi, M.D.
Michelle M. Cloutier, M.D.
Colin R. Cooke, M.D.
Karen Erickson, B.S.
Maureen George, Ph.D., R.N.
Joe K. Gerald, M.D., Ph.D.
Lynn B. Gerald, Ph.D., M.S.P.H.
Christopher H. Goss, M.D., M.Sc.
Michael K. Gould, M.D., M.S.
Robert Hyzy, M.D.
Jeremy M. Kahn, M.D., M.Sc.
Brian S. Mittman, Ph.D.
Erika M. Mosesón, M.D., M.A.
Richard A. Mularski, M.D.
Sairam Parthasarathy, M.D.
Sanjay R. Patel, M.D.
Cynthia S. Rand, Ph.D.
Nancy S. Redeker, Ph.D., R.N.
Theodore F. Reiss, M.D., M.B.E.
Kristin A. Riekert, Ph.D.
Gordon D. Rubenfeld, M.D., M.Sc.
Judith A. Tate, Ph.D., R.N.
Kevin C. Wilson, M.D.
Footnotes
This Official Research Statement of the American Thoracic Society (ATS) was approved by the ATS Board of Directors, July 2016
Author Disclosures: S.S.C. receives research support from United Pharmaceuticals and Triangle Pharmaceuticals. C.H.G. received research support from Vertex Pharmaceuticals and Transave; reviews grants for Gilead Sciences; and served on an advisory committee of KaloBios Pharmaceuticals and as a speaker for F. Hoffmann-La Roche Ltd. and MedScape. J.M.K. received research support from Cerner Corporation and had an uncompensated informal research collaboration with Phillips VISICU. S.P. holds a patent for a home breathing device, patent number: WO2015048766 A1. S.R.P. served as a consultant for Apnicure and on a data and safety monitoring board of Philips Respironics. T.F.R. is an employee of Celgene Corporation. K.A.R. serves as a speaker and consultant for Gilead Sciences Inc., a book editor for Springer Publishing, and a speaker for Vertex Pharmaceuticals Incorporated. C.H.W., J.A.K., D.H.A., B.G.B., A.C., M.M.C., C.R.C., K.E., M.G., J.K.G., L.B.G., M.K.G., R.H., B.S.M., E.M.M., R.A.M., C.S.R., N.S.R., G.D.R., J.A.T., K.C.W., and C.C.T. reported no relationships with relevant commercial interests.
References
- 1.Balas E, Boren S.Yearbook of medical informatics: managing clinical knowledge for health care improvementStutthart, Germany: Schattauer Verlagsgesellschaft mbH; 2000 [PubMed]
- 2.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 3.MacMahon H. Compliance with Fleischner Society guidelines for management of lung nodules: lessons and opportunities. Radiology. 2010;255:14–15. doi: 10.1148/radiol.10092382. [DOI] [PubMed] [Google Scholar]
- 4.Eisenberg RL, Bankier AA, Boiselle PM. Compliance with Fleischner Society guidelines for management of small lung nodules: a survey of 834 radiologists. Radiology. 2010;255:218–224. doi: 10.1148/radiol.09091556. [DOI] [PubMed] [Google Scholar]
- 5.Wiener RS, Gould MK, Slatore CG, Fincke BG, Schwartz LM, Woloshin S. Resource use and guideline concordance in evaluation of pulmonary nodules for cancer: too much and too little care. JAMA Intern Med. 2014;174:871–880. doi: 10.1001/jamainternmed.2014.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalhan R, Mikkelsen M, Dedhiya P, Christie J, Gaughan C, Lanken PN, Finkel B, Gallop R, Fuchs BD. Underuse of lung protective ventilation: analysis of potential factors to explain physician behavior. Crit Care Med. 2006;34:300–306. doi: 10.1097/01.ccm.0000198328.83571.4a. [DOI] [PubMed] [Google Scholar]
- 7.Parthasarathy S, Subramanian S, Quan SF. A multicenter prospective comparative effectiveness study of the effect of physician certification and center accreditation on patient-centered outcomes in obstructive sleep apnea. J Clin Sleep Med. 2014;10:243–249. doi: 10.5664/jcsm.3518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zerhouni E. Medicine: the NIH Roadmap. Science. 2003;302:63–72. doi: 10.1126/science.1091867. [DOI] [PubMed] [Google Scholar]
- 9.Zerhouni EA. Translational and clinical science–time for a new vision. N Engl J Med. 2005;353:1621–1623. doi: 10.1056/NEJMsb053723. [DOI] [PubMed] [Google Scholar]
- 10.Mensah GA, Engelgau M, Stoney C, Mishoe H, Kaufmann P, Freemer M, Fine L Trans-NHLBI T4 Translation Research Work Groups. News from NIH: a center for translation research and implementation science. Transl Behav Med. 2015;5:127–130. doi: 10.1007/s13142-015-0310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsuno K, Miura K, Takeya M, Kolobow T, Morioka T. Histopathologic pulmonary changes from mechanical ventilation at high peak airway pressures. Am Rev Respir Dis. 1991;143:1115–1120. doi: 10.1164/ajrccm/143.5_Pt_1.1115. [DOI] [PubMed] [Google Scholar]
- 12.Tremblay L, Valenza F, Ribeiro SP, Li J, Slutsky AS. Injurious ventilatory strategies increase cytokines and c-fos m-RNA expression in an isolated rat lung model. J Clin Invest. 1997;99:944–952. doi: 10.1172/JCI119259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parker JC, Hernandez LA, Peevy KJ. Mechanisms of ventilator-induced lung injury. Crit Care Med. 1993;21:131–143. doi: 10.1097/00003246-199301000-00024. [DOI] [PubMed] [Google Scholar]
- 14.Dreyfuss D, Basset G, Soler P, Saumon G. Intermittent positive-pressure hyperventilation with high inflation pressures produces pulmonary microvascular injury in rats. Am Rev Respir Dis. 1985;132:880–884. doi: 10.1164/arrd.1985.132.4.880. [DOI] [PubMed] [Google Scholar]
- 15.Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures: protection by positive end-expiratory pressure. Am Rev Respir Dis. 1974;110:556–565. doi: 10.1164/arrd.1974.110.5.556. [DOI] [PubMed] [Google Scholar]
- 16.Kolobow T, Moretti MP, Fumagalli R, Mascheroni D, Prato P, Chen V, Joris M. Severe impairment in lung function induced by high peak airway pressure during mechanical ventilation: an experimental study. Am Rev Respir Dis. 1987;135:312–315. doi: 10.1164/arrd.1987.135.2.312. [DOI] [PubMed] [Google Scholar]
- 17.Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 18.Needham DM, Colantuoni E, Mendez-Tellez PA, Dinglas VD, Sevransky JE, Dennison Himmelfarb CR, Desai SV, Shanholtz C, Brower RG, Pronovost PJ. Lung protective mechanical ventilation and two year survival in patients with acute lung injury: prospective cohort study. BMJ. 2012;344:e2124. doi: 10.1136/bmj.e2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Needham DM, Yang T, Dinglas VD, Mendez-Tellez PA, Shanholtz C, Sevransky JE, Brower RG, Pronovost PJ, Colantuoni E. Timing of low tidal volume ventilation and intensive care unit mortality in acute respiratory distress syndrome: a prospective cohort study. Am J Respir Crit Care Med. 2015;191:177–185. doi: 10.1164/rccm.201409-1598OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rubenfeld GD, Cooper C, Carter G, Thompson BT, Hudson LD. Barriers to providing lung-protective ventilation to patients with acute lung injury. Crit Care Med. 2004;32:1289–1293. doi: 10.1097/01.ccm.0000127266.39560.96. [DOI] [PubMed] [Google Scholar]
- 21.Dennison CR, Mendez-Tellez PA, Wang W, Pronovost PJ, Needham DM. Barriers to low tidal volume ventilation in acute respiratory distress syndrome: survey development, validation, and results. Crit Care Med. 2007;35:2747–2754. doi: 10.1097/01.CCM.0000287591.09487.70. [DOI] [PubMed] [Google Scholar]
- 22.Umoh NJ, Fan E, Mendez-Tellez PA, Sevransky JE, Dennison CR, Shanholtz C, Pronovost PJ, Needham DM. Patient and intensive care unit organizational factors associated with low tidal volume ventilation in acute lung injury. Crit Care Med. 2008;36:1463–1468. doi: 10.1097/CCM.0b013e31816fc3d0. [DOI] [PubMed] [Google Scholar]
- 23.Walkey AJ, Wiener RS. Risk factors for underuse of lung-protective ventilation in acute lung injury. J Crit Care. 2012;27:323.e1–323.e9. doi: 10.1016/j.jcrc.2011.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Belda TE, Gajic O, Rabatin JT, Harrison BA. Practice variability in management of acute respiratory distress syndrome: bringing evidence and clinician education to the bedside using a web-based teaching tool. Respir Care. 2004;49:1015–1021. [PubMed] [Google Scholar]
- 25.Wolthuis EK, Korevaar JC, Spronk P, Kuiper MA, Dzoljic M, Vroom MB, Schultz MJ. Feedback and education improve physician compliance in use of lung-protective mechanical ventilation. Intensive Care Med. 2005;31:540–546. doi: 10.1007/s00134-005-2581-9. [DOI] [PubMed] [Google Scholar]
- 26.Bender BG, Krishnan JA, Chambers DA, Cloutier MM, Riekert KA, Rand CS, Schatz M, Thomson CC, Wilson SR, Apter A, et al. American Thoracic Society and National Heart, Lung, and Blood Institute Implementation Research Workshop Report. Ann Am Thorac Soc. 2015;12:S213–S221. doi: 10.1513/AnnalsATS.201506-367OT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The W. Edwards Deming InstituteThe PDSA cycle [accessed 2016 Sep 13]. Available from: https://www.deming.org/theman/theories/pdsacycle
- 28.Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, Sexton B, Hyzy R, Welsh R, Roth G, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355:2725–2732. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- 29.Weiss CH, Moazed F, McEvoy CA, Singer BD, Szleifer I, Amaral LA, Kwasny M, Watts CM, Persell SD, Baker DW, et al. Prompting physicians to address a daily checklist and process of care and clinical outcomes: a single-site study. Am J Respir Crit Care Med. 2011;184:680–686. doi: 10.1164/rccm.201101-0037OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Donabedian A. The quality of care: how can it be assessed? JAMA. 1988;260:1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- 31.George ML. Lean six sigma: combining six sigma quality with lean production speed. New York, NY: McGraw-Hill; 2002. [Google Scholar]
- 32.Rogers EM. Diffusion of innovations. New York, NY: Free Press; 2003. [Google Scholar]
- 33.Ryan B, Gross N. The diffusion of hybrid seed corn in two Iowa communities. Rural Sociol. 1943;8:15–24. [Google Scholar]
- 34.Coleman J, Katz E, Menzel H. The diffusion of an innovation among physicians. Sociometry. 1957;20:253–270. [Google Scholar]
- 35.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sinuff T, Muscedere J, Adhikari NK, Stelfox HT, Dodek P, Heyland DK, Rubenfeld GD, Cook DJ, Pinto R, Manoharan V, et al. KRITICAL Working Group, the Canadian Critical Care Trials Group, and the Canadian Critical Care Society. Knowledge translation interventions for critically ill patients: a systematic review. Crit Care Med. 2013;41:2627–2640. doi: 10.1097/CCM.0b013e3182982b03. [DOI] [PubMed] [Google Scholar]
- 37.Lagu T. Translating knowledge into practice in critical care settings. Crit Care Med. 2013;41:2659–2660. doi: 10.1097/CCM.0b013e31829e4cab. [DOI] [PubMed] [Google Scholar]
- 38.Carson SS, Goss CH, Patel SR, Anzueto A, Au DH, Elborn S, Gerald JK, Gerald LB, Kahn JM, Malhotra A, et al. American Thoracic Society Comparative Effectiveness Research Working Group. An official American Thoracic Society research statement: comparative effectiveness research in pulmonary, critical care, and sleep medicine. Am J Respir Crit Care Med. 2013;188:1253–1261. doi: 10.1164/rccm.201310-1790ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50:217–226. doi: 10.1097/MLR.0b013e3182408812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weiss CH, Poncela-Casasnovas J, Glaser JI, Pah AR, Persell SD, Baker DW, Wunderink RG, Nunes Amaral LA. Adoption of a high-impact innovation in a homogeneous population. Phys Rev X. 2014;4:041008. doi: 10.1103/PhysRevX.4.041008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10:53. doi: 10.1186/s13012-015-0242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. 2012;43:337–350. doi: 10.1016/j.amepre.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gross PA, Greenfield S, Cretin S, Ferguson J, Grimshaw J, Grol R, Klazinga N, Lorenz W, Meyer GS, Riccobono C, et al. Optimal methods for guideline implementation: conclusions from Leeds Castle meeting. Med Care. 2001;39:II85–II92. [PubMed] [Google Scholar]
- 44.Perkins MB, Jensen PS, Jaccard J, Gollwitzer P, Oettingen G, Pappadopulos E, Hoagwood KE. Applying theory-driven approaches to understanding and modifying clinicians’ behavior: what do we know? Psychiatr Serv. 2007;58:342–348. doi: 10.1176/ps.2007.58.3.342. [DOI] [PubMed] [Google Scholar]
- 45.Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, Glass JE, York JL. A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev. 2012;69:123–157. doi: 10.1177/1077558711430690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Proctor EK, Landsverk J, Aarons G, Chambers D, Glisson C, Mittman B. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Adm Policy Ment Health. 2009;36:24–34. doi: 10.1007/s10488-008-0197-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and implementation research in health: translating science to practice. Oxford, UK: Oxford University Press; 2012. [Google Scholar]
- 48.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Concannon TW, Meissner P, Grunbaum JA, McElwee N, Guise JM, Santa J, Conway PH, Daudelin D, Morrato EH, Leslie LK. A new taxonomy for stakeholder engagement in patient-centered outcomes research. J Gen Intern Med. 2012;27:985–991. doi: 10.1007/s11606-012-2037-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.American Thoracic SocietyStatements, guidelines, and reports [accessed 2016 Sep 13]. https://www.thoracic.org/statements/index.php
- 52.Classen DC, Mermel LA. Specialty society clinical practice guidelines: time for evolution or revolution? JAMA. 2015;314:871–872. doi: 10.1001/jama.2015.7462. [DOI] [PubMed] [Google Scholar]
- 53.American Thoracic SocietyDocuments development and implementation committee [accessed 2016 Sep 13]. Available from: http://www.thoracic.org/members/committees/committeeDetail.php?id=a0I40000001BLJoEAO
- 54.American Thoracic SocietyQuality improvement and implementation committee [accessed 2016 Sep 13]. Available from: http://www.thoracic.org/members/committees/committeeDetail.php?id=a0I40000001BLK5EAO
- 55.Thomson CC, Welsh CH, Carno MA, Wenzel SE, Chung F, Brozek JL, Wilson KC ATS/ERS Task Force on Severe Asthma and the American Thoracic Society Implementation Task Force. Severe asthma. Ann Am Thorac Soc. 2014;11:996–997. doi: 10.1513/AnnalsATS.201405-199CME. [DOI] [PubMed] [Google Scholar]
- 56.Raghu G, Rochwerg B, Zhang Y, Garcia CA, Azuma A, Behr J, Brozek JL, Collard HR, Cunningham W, Homma S, et al. American Thoracic Society; European Respiratory society; Japanese Respiratory Society; Latin American Thoracic Association. An Official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis. An update of the 2011 clinical practice guideline. Am J Respir Crit Care Med. 2015;192:e3–e19. doi: 10.1164/rccm.201506-1063ST. [DOI] [PubMed] [Google Scholar]
- 57.Kahn JM, Gould MK, Krishnan JA, Wilson KC, Au DH, Cooke CR, Douglas IS, Feemster LC, Mularski RA, Slatore CG, et al. ATS Ad Hoc Committee on the Development of Performance Measures from ATS Guidelines. An official American thoracic society workshop report: developing performance measures from clinical practice guidelines. Ann Am Thorac Soc. 2014;11:S186–S195. doi: 10.1513/AnnalsATS.201403-106ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.American Heart Association[accessed 2016 Sep 13]. Available from: http://www.heart.org/HEARTORG/Professional/GetWithTheGuidelines/Get-With-The-Guidelines—HFStroke_UCM_001099_SubHomePage.jsp
- 59.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Green LW. Health education planning: a diagnostic approach. Palo Alto, CA: Mayfield Publishing Company; 1980. [Google Scholar]
- 61.Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf. 2008;34:228–243. doi: 10.1016/s1553-7250(08)34030-6. [DOI] [PubMed] [Google Scholar]
- 62.Stone VI, Lane JP. Modeling technology innovation: how science, engineering, and industry methods can combine to generate beneficial socioeconomic impacts. Implement Sci. 2012;7:44. doi: 10.1186/1748-5908-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.National Quality Forum[accessed 2016 Sep 13]. Available from: http://www.qualityforum.org/QPS/QPSTool.aspx
- 64.Centers for Medicare and Medicaid ServicesMeasures codes [accessed 2016 Sep 13]. Available from: https://www.cms.gov/apps/ama/license.asp?file=/PQRS/downloads/PQRS_2016_Measure_List_01072016.xlsx
- 65.Schünemann HJ, Jaeschke R, Cook DJ, Bria WF, El-Solh AA, Ernst A, Fahy BF, Gould MK, Horan KL, Krishnan JA, et al. ATS Documents Development and Implementation Committee. An official ATS statement: grading the quality of evidence and strength of recommendations in ATS guidelines and recommendations. Am J Respir Crit Care Med. 2006;174:605–614. doi: 10.1164/rccm.200602-197ST. [DOI] [PubMed] [Google Scholar]