Abstract
This study investigated racial differences in patient-physician communication around mental health versus biomedical issues. Data were collected from audiorecorded periodic health exams of adults with mental health needs in the Detroit area (2007--2009). Patients and their primary care physicians conversed for twice as long and physicians demonstrated greater empathy during mental health topics compared to biomedical topics. This increase varied by patient and physician race. Patient race predicted physician empathy, but physician race predicted talk time. Interventions to improve mental health communication could be matched to specific populations based on the separate contributions of patient and physician race.
Keywords: Mental health, Physician/patient communication, Primary Care, Health Disparities, Race & Ethnicity
1. Introduction
Patient-physician communication plays a central role in mental health diagnosis and treatment [1]. Variation in patient-physician communication around mental health is thought to contribute to racial and ethnic disparities in mental health care [1–2]. Whether racial differences in patient-physician communication are greater for mental health issues than for biomedical issues remains an important question for research and policy interventions that seek to improve mental health parity.
Previous studies have documented differences in the incidence, duration and quality of mental health communication by patient race/ethnicity in primary care settings. Physicians are less likely to address mental health issues with black or African-American patients compared to white patients [3–5]. When they do, the existing evidence shows that physicians spend less time discussing mental health issues with non-white patients than they do with white patients [3, 6], and expend less effort building rapport [3].
Interpreting the clinical significance of these differences requires accounting for the idiosyncrasies of each patient-physician relationship. Some relationships might be characterized by restrained emotional expression across all topics; others might display exuberant emotional expression across all topics. A subtle emotional expression would carry more weight in the former context than in the latter. Comparing the absolute amount of emotional expression across these two relationships devoid of context would miss this important distinction. The same concern arises when comparing the time spent discussing any particular topic. Indeed, prior research has shown significant variation across patient-physician encounters in the time spent on biomedical topics such as hypertension and nutrition counseling [7, 8].
In this paper, we study whether racial/ethnic differences in the duration and quality mental health communication found in prior studies [3–6] remain when we account for idiosyncratic variation in patient-physician communication. Specifically, we measure whether patient-physician dyads differ in how they choose to allocate time and patient engagement efforts across mental health and biomedical topics. By studying relative amounts of time and patient engagement efforts across topics in biomedical versus mental health categories (e.g., depression vs. hypertension), we are able to account for idiosyncratic variation in how each patient-physician dyad interacts. We furthermore separate out the relative contribution of patient and physician race to these differences. We hypothesize, based on prior literature demonstrating physicians’ racial/ethnic implicit biases [9–11], that patient race is the primary determinant of these differences.
We test three hypotheses in this paper: (1) the average physician spends more time and more patient engagement efforts on mental health topics compared to biomedical topics, (2) the average physician spends less time and fewer patient engagement efforts on mental health topics compared to biomedical topics with non-white patients than with white patients, and (3) physician race does not affect the amount of time or the degree of patient engagement allocated to mental health topics.
2. Methods
Data came from 22 outpatient clinics in an integrated delivery system in the Detroit, Michigan area. A convenience sample of subjects was enrolled in an observational study of preventive health discussions during periodic health exams (PHEs) between 2007–2009 [12]. Recruitment of subjects for the preventative health discussion study has been described elsewhere [12–13]. The participation rates were 47% for physicians and 50% for patients, resulting in a sample of 500 visits. A research assistant observed and recorded the visits with a digital audio recorder. Clinician-participants were practicing family or general internal medicine physicians.
The sample for the current analyses consisted of 322 office visits, representing 322 unique patients. Patients were included in the sample if they met any of the following criteria for mental health needs [14]: had a mental health diagnosis code in their electronic health record or visited a behavioral health center in the previous twelve months; filled a prescription for or were prescribed a mental health medication in the previous twelve months; a cumulative score of two or higher on the two-item Personal Health Questionnaire (PHQ2) that inquires about the frequency of depressed mood and anhedonia (inability to experience pleasure from usually enjoyable activities) over the past two weeks [15]; or any indication of a mental health discussion during the scheduled PHE as noted by the research assistant in attendance. We chose a threshold value of two on the PHQ2, rather than the clinically used depression screening threshold of three, to increase the sensitivity of our inclusion criteria [15]. Mental health diagnoses observed in the sample and used in the inclusion criteria included: mood disorders, anxiety disorders, schizophrenic disorders, and adjustment disorders. A flowchart illustrating the inclusion criteria for this study can be found in the supplementary appendix.
Patient race/ethnicity was determined by self-report on a pre-visit survey [13] that included the investigator-defined categories: white or Caucasian; black or African-American; Asian, Native Hawaiian or other Pacific Islander; American Indian or Alaska Native; or “other.” Native Hawaiian or other Pacific Islander and American Indian or Alaska Native were combined with the “other” category due to the small number of subjects in each of these categories. Physician race/ethnicity was determined from medical group administrative records after completion of the initial data collection.
All recordings were transcribed and analyzed using a method described elsewhere [16]. Briefly, five trained research associates (“raters”) coded the audiotapes and transcripts for content, communication behaviors, and time spent on each topic. Scores from different coders were compared for all coded variables using intraclass correlations (ICC) for numerical variables and percentage agreement for categorical variables. Intraclass correlations and percentage agreement between raters and within the same rater ranged from 0.78 to 0.99.
Topics were coded according to the multidimensional interaction analysis (MDIA) system, modified for this study [17–18]. In particular, we coded an interaction from the audio-recording and its verbatim transcription based on topics sequentially introduced by the patient or physician [19]. A topic was defined as an issue that required a response from the other person and had at least two complete exchanges between patient and physician. Topics were grouped into seven major categories: biomedical, health behavior, mental health, psychosocial, patient-physician relationship, agenda setting, and other. Mental health topics included grief and mourning, depression, anxiety and general worries, and discussions of the patient’s own mortality. A topic could have multiple “instances” if the discussion on that topic occurred several times during the visit. The length of time spent on each topic was defined as the cumulative amount of time spent on all instances of the topic [16].
Within this MDIA framework, physician communication behaviors related to patient engagement were coded using two measures based on the Four Habits model. The Four Habits model outlines clusters of physician behaviors and skills associated with effective clinical practice and positive health outcomes [20]. Previously, Krupat et al had developed a coding scheme based on the Four Habits model that rated physician behaviors at the level of an entire visit [21]. Since we aimed to assess topic-level behaviors, we created our own, similar measures for each of the two Habits that could be measured at the topic-level: “Elicit the Patient’s Perspective” and “Demonstrate Empathy”. (The remaining two Habits were visit-level behaviors: “Invest in the Beginning” and “Invest in the End”.) We coded one variable for eliciting the patient’s perspective and one for demonstrating empathy. Values were coded only for topics where such physician behaviors would be expected; thus, the number of observations for each of these two variables was smaller than the total number of topics [22]. As described above, we found our two patient engagement measures to have high inter-rater reliability, similar to Krupat et al [21]. Descriptions and examples of these variables are found in Table 1.
Table 1.
Description of variables used to measure physicians’ patient engagement
| Variable | Variable Description | Scoring rubric | Transcript example |
|---|---|---|---|
| Eliciting Patient Perspectives |
Physician asked the patient how psychosocial/medical disease/concerns affected the patient's life? |
5: Physician attempts to determine in detail/shows great interest in how the disease/concern is affecting the patient's lifestyle |
MD: …but one of the things I think it would be good for us to talk about, you know, down the line is how you’re dealing with the stress of your parents, because that can directly affect some of these other things you’re talking about. |
| 3: Physician attempts to determine briefly/shows only some interest in how the disease/concern is affecting the patient's lifestyle |
MD: Any pain in your joints or night cramps or anything? PT: Yeah, pain in the joints. Come on, doc. MD: [laughs] I got, I got that too. PT: Follow me one week when I’m running, yeah. |
||
| 1: Physician makes no attempt to determine/shows no interest in how the disease/concern is affecting the patient's lifestyle |
MD: I’m almost up to 40 [supplements]. What, what about if these interact in your body together to produce toxic effects? PT: That’s why I’ve got a list. MD: Honestly, I think you could stop them all. |
||
| Expressing Empathy |
Physician verbally expresses empathy or sympathy for any psychosocial concerns (distinct expressions such as "I'm so sorry to hear that"; "That must be hard") |
5: Physician makes comments clearly indicating acceptance/validation of patient's feelings (e.g., "I'd feel the same way‥", "I can see how that would worry you… ") |
PT: I’ve just had a full plate MD: Yeah. Absolutely PT: My mom couldn’t drive for a while and it’s just ohh, so, but now everything, and even with my arm I can’t deal with it, you know. Man, that’s a lot! MD: Yeah, that’s a lot. |
| 3: Physician briefly acknowledges patient's feelings but makes no effort to indicate acceptance/validation |
MD: How long has she been a diabetic? PT: Since she was eight. MD: Oh, okay. I’m sorry to hear that. |
||
| 1: Physician makes no attempt to respond to/validate the patient's feelings or possibly belittles or challenges them |
PT: The only thing is Alzheimer’s, which is my big concern. MD: She put that in there, who has that, or who had it? PT: My mother and, uh, three of her siblings out of nine. MD: Okay. So three aunts and, as you know, there’s not much we can do about that at this point. |
||
Source: Variables and scoring rubrics were adapted from Krupat et al [16].
The primary outcomes were patient and physician conversation time and the physician’s score on these two measures of patient engagement for mental health versus biomedical topics.
Multivariable models at the topic-level used generalized estimating equations, which accounted for clustering of topic-level outcomes within a visit. Specifically, an exchangeable correlation matrix was used, which allowed for a fixed correlation between topics in the same visit. Guided by previous literature [3, 6, 23], we established the following independent variables: patient race, physician race and their interactions with mental health topics. The estimated coefficients on our independent variables from our multivariate models measured whether the average mental health topic was associated with more time (or more patient engagement) compared to the average biomedical topic, accounting for the included covariates and the unobserved within-visit correlation.
Covariates included patient age, patient sex, Charlson Comorbidity Index, and physician gender and physician specialty as covariates. Several additional variables (physician age, whether the physician was an international medical graduate, patient mental health diagnoses or medications) were excluded from the main analysis because they did not affect the primary outcome of interest (data not shown). All statistical analyses were performed using Stata version 12.0 (StataCorp, College Station, Texas).
3. Results
The patient sample was composed of 322 adults with a mean age of 59, of whom 65% were female (n=210). The sample included 59 physicians, of whom 56% (n=33) were men and 71% (n=42) were in general internal medicine (versus family medicine). The physician sample was 47% white, 22% Asian American/Pacific Islander, 17% black/African-American and 14% “other” race. The patient sample was 65% white, 29% black/African-American, 4% Asian American/Pacific Islander and 2% “other” race (Table 2). Both white and black patients were significantly more likely to see a doctor of the same race than would be expected by chance (Supplementary Table 2; chi-squared test, p<.001). This was explained in part by the tendency for clinics to have higher proportions of patients and doctors of the same race (Pearson or Spearman correlation, p<.002) and in part by the disproportionate tendency of white patients to see white doctors given the racial composition of their clinic’s staff (Cochran-Mantel-Haenszl test: OR=2.9, p<.01 for whites; OR=1.6, non-significant for blacks). There were too few patients of other identified groups (Asian, “other”) to make useful inferences about their racial concordance.
Table 2.
Sample characteristics
| Variables | No. (%) |
|---|---|
| Patient characteristics (N=322) | |
| Age, mean | 59 |
| Male | 112 (35) |
| Race | |
| White or Caucasian | 210 (65) |
| Black or African-American | 93 (29) |
| Other | 19 (6) |
| Education | |
| Less than high school graduate or GED | 14 (4) |
| High school graduate or GED | 82 (25) |
| Some college | 131 (41) |
| 4-year college or more | 95 (30) |
| Charlson score ≥ 2 | 64 (20) |
| Physician characteristics (N=59) | |
| Age, mean | 50 |
| Male | 26 (44) |
| Race | |
| White or Caucasian | 28 (47) |
| Black or African-American | 10 (17) |
| Other | 21 (36) |
| Internal Medicine (vs. Family Medicine) | 42 (71) |
Mental health topics received more conversation time and higher patient engagement scores than biomedical topics. In multivariate analysis, the amount of time spent discussing a mental health topic was 0.97 minutes longer (p<.001) than the time spent discussing a biomedical topic in a single visit. This effect was driven largely by an increase in patient talk time (0.78 additional minutes, p<.001) during mental health topics compared to biomedical topics. Physicians spoke for an additional 0.18 minutes (10.8 seconds) during mental health topics, but this difference was not significant at the 5% level. Physicians scored 0.77 points higher (p<.001) in demonstrating empathy during mental health topics compared to biomedical topics, and they scored 0.38 points higher in eliciting the patient’s perspective (p=.01).
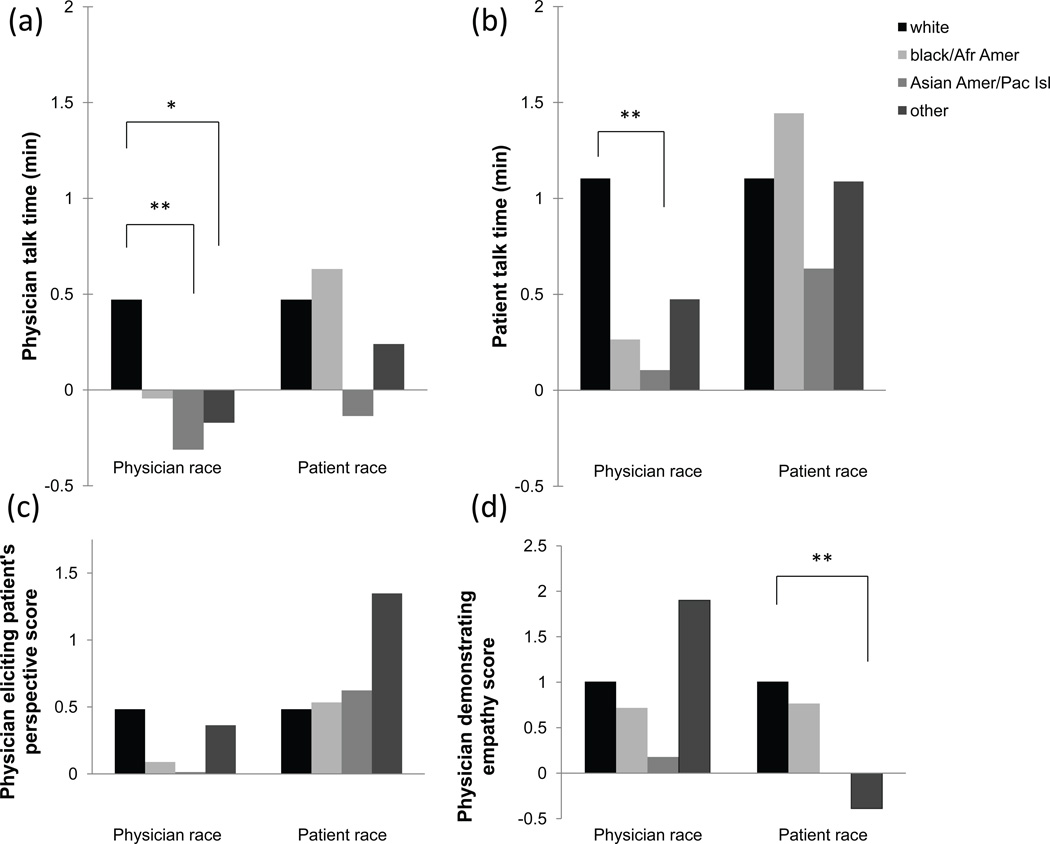
These increases in time and patient engagement measures were variably associated with patient and physician race. Figure 1 shows the results from a regression model that includes interactions between patient/physician race and topic content. The full set of regression results is available in the appendix. Each bar shows the difference in the outcome variable between mental health and biomedical topics by patient or physician race.
Figure 1. Association between race and amount of time and patient engagement allocated to mental health topics relative to biomedical topics.
Each subgraph represents the estimated time or patient engagement score for mental health topics relative to biomedical topics by patient or physician race, controlling for the other party’s race. The bars are linear combinations of coefficients from a multivariable generalized estimating equation for the relevant outcome and race (full results in appendix). Each bar represents the amount of time or the physician’s patient engagement score for mental health topics minus the same quantity for biomedical topics. Analysis of “physician demonstrating empathy score” does not include Asian American/Pacific Islander patients, since there were no observed mental health topics with an empathy measure among this group. P-values for each model (i.e. each graph) are corrected for multiple hypothesis testing using the Bonferroni-Holm method: *** p<0.01, ** p<0.05, * p<0.10.
Physician race was significantly associated with differences in both patient and physician talk time during mental health topics compared to biomedical topics (Figures 1a and 1b), but it was not associated with differences in patient engagement (Figures 1c and 1d). Specifically, seeing a white physician, but not an Asian American/Pacific Islander physician, was associated with an increase in the time spent talking during mental health topics compared to biomedical topics. The majority of the difference in mental health talk time by physician race was due to differences in patient talk time. Specifically, patients who saw Asian American/Pacific Islander physicians had less of an increase in time speaking (0.98 min shorter, p<0.05) during mental health versus biomedical topics, compared to patients who saw white physicians (Figure 1b). Asian American/Pacific Islander physicians also spent less time speaking during mental health topics than during biomedical topics compared to white physicians, although the difference was smaller than for patient talk time (0.78 min shorter, p<0.05, Figure 1a). We were unable to detect significant differences in patient or physician talk time during visits with black/African-American physicians compared to visits with white physicians.
In contrast, patient race was not associated with any increase in time spent discussing mental health topics (Figure 1a and 1b) but was associated with differences in physicians’ empathy scores. Of the two measures of patient engagement behavior--demonstrating empathy and eliciting a patient’s perspective, only physicians’ empathy scores varied significantly across our measures of patient and physician race (Figure 1c and 1d). White patients received a greater increase in physician empathy during mental health topics compared to biomedical topics than “other” minority race patients, controlling for physician race (Figure 1d). There were no significant differences in this score increase for black/African-American or Asian American/Pacific Islander patients compared to white patients.
We added race concordance to the above models and found no significant association between race concordance and any of the measures of allocation (see appendix). These results indicated that there was no additional association between race concordance and allocation decisions in our sample, once we had accounted for the association by patient and physician race.
4. Discussion and Conclusion
4.1 Discussion
This study measured whether patient-physician dyads differed in how they chose to allocate time and patient engagement efforts across mental health and biomedical topics according to patient race/ethnicity, physician race/ethnicity or racial/ethnic concordance. For both time and patient engagement measures, we studied relative amounts rather than absolute amounts used in previous studies [3, 6]. We were able to perform this analysis because our dataset uniquely measured our outcome variables at the level of individual topics within a visit.
We tested three hypotheses in our study. First, we found that the average physician in our sample spent more time and more patient engagement effort on mental health topics compared to biomedical topics, even when adjusting for idiosyncratic variation in the time spent on any particular topic. Second, we found that patient race and physician race both affected our outcome measures but along different dimensions. In particular, we found that physician race predicted differences in the time spent on mental health topics, whereas patient race predicted differences in physician-demonstrated empathy. Encounters with Asian American/Pacific Islander physicians had relatively less time devoted to mental health topics than to biomedical topics, compared to white physicians. This difference was largely due to patients, of all races, spending less time talking about their mental health concern with Asian American/Pacific Islander physicians compared to white physicians. In contrast, “other” race minority patients were less likely to receive the relative increase in physician empathy that white patients received around mental health topics. Unlike prior studies [3, 5], we were unable to detect significant differences in communication between white patients and physicians and black/African-American patients and physicians, although this may have been due to the relatively small number of black/African-American patients and physicians in our sample.
The idea that patient engagement may be affected by patient race/ethnicity is partially consistent with a previous study by Street et al [24]. Although their study found no difference in physicians’ use of patient-centered communication by patient race, they did find that physicians were more contentious with black/African-American patients and perceived black/African-American patients as less effective communicators. We found that physicians showed less of an increase in empathy during mental health topics among patients of “other” minority races. We were unable to comment on whether physicians’ perceptions of patient communication contributed to these observed differences in physician.
Our findings on time allocation differ from two previous studies by Ghods et al [3] and Tai-Seale et al [25], both of which found that white patients received more direct communication from physicians on mental health concerns than non-white patients. Tai-Seale et al studied 385 primary care visits of white and non-white elderly adults and found that physicians spent on average 1.7 fewer minutes discussing mental health issues with their non-white patients compared to their white patients [25]. Their result did not account for physician race. Ghods et al adjusted for patient and physician characteristics in their study of 108 primary care visits of white or African-American patients with depressive symptoms [3]. They found that physicians made only one-third as many statements about depression in conversing with African-American patients as they did with white patients. In contrast, we found that physician race, not patient race, was associated with differences in the time allocated to mental health discussions.
This study has several limitations. First, we caveat that our finding around Asian American/Pacific Islander physicians may be confounded by the fact that nearly all Asian American/Pacific Islander physicians in our sample were also international medical graduates (IMGs). Although we would like to have separately identified the contributions of Asian American/Pacific Islander race and international medical graduate status, the two variables were too highly correlated to perform this analysis in our sample. Thus, our results on Asian American/Pacific Islander physicians may be picking up effects specific to IMGs. Prior studies have shown that IMGs may be less likely to identify symptoms of mental illness due to cultural differences in the manifestations and acceptance of mental illness [26].
Second, each patient-physician dyad chose whether or not to discuss a mental health topic. Although all of the patients in our sample met at least one criterion for having a potential need for mental health services, only 39% of visits contained a discussion of a mental health topic. As such, our results may not generalize to patient-physician dyads that chose not to discuss mental health topics. Third, our data are from a convenience sample and a single audiorecorded visit between patient-physician dyads. Fourth, we measured patient and physician race differently; we used self-reported race for patients and administrative records for physician race. We note that even if this measurement difference led to greater measurement error in one group versus the other (e.g. if administrative records had fewer racial/ethnic categories or did not reflect physicians’ self-reported race), this limitation would likely bias our study toward null results rather than any particular positive result. Finally, patients and physicians were non-randomly paired across race/ethnicity. This limitation also exists in other field-based studies of patient and physician race [3–6, 27].
4.2 Conclusion
The differences we found in the discussion of mental health topics compared to biomedical topics by patient and physician race/ethnicity are concerning in light of the continued disparities in mental health care quality and outcomes across race/ethnicity [1]. Based on previous literature showing a correlation between patient engagement and outcomes [28–30], we surmise that the racial differences that we detected may contribute to the documented racial/ethnic differences in the mental health treatment [31–34]. Our findings suggest that differences in office visit communication can appear in subtle ways, such as whether a physician demonstrates more empathy or allocates more time for patients to speak when the conversation changes, for example, from hypertension to depression. Further research is needed to determine the root causes of these subtle differences and whether these differences give rise to the documented racial/ethnic biases, perceptions and disparities in health outcomes [1, 10, 24].
4.3 Practice implications
Identifying the separate contributions of patient and physician race to observed communication differences can help to guide policy. Differences that vary primarily by patient race--in our case, expressing empathy--suggest that physicians of all racial/ethnic backgrounds could benefit from additional organizational support or education around this particular topic or skill [35–38]. This may include interventions to reverse the observed decline in physician empathy during the training process [39–41], or finding ways to ameliorate the emotional “cost” [42] of empathy in clinical work. On the other hand, differences that vary primarily by physician race suggest that targeted interventions toward specific physician populations or their patients would be more cost-effective for improving those particular disparities in patient-physician communication.
Supplementary Material
Acknowledgments
Source of Funding:
This study was funded by NIMH R01 MH081098 and NCI R01 CA112379 (MTS).
Footnotes
Authorship: All authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Contributors: The authors gratefully acknowledge Ashley L. Stone, MPH; Caroline Wilson, MSc; and Cheryl Stults, PhD for invaluable contributions in constructing the dataset
Prior presentations: None
Conflicts of Interest
None of the authors have any conflicts of interest
References
- 1.McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Aff (Millwood) 2008;27:393–403. doi: 10.1377/hlthaff.27.2.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smedley BD, Stith AY, Nelson AR. Unequal Treatment:Confronting Racial and Ethnic Disparities in Health Care. The National Academies Press; 2003. pp. 69–71. [PubMed] [Google Scholar]
- 3.Ghods BK, Roter DL, Ford DE, Larson S, Arbelaez JJ, Cooper LA. Patient-physician communication in the primary care visits of African Americans and whites with depression. J Gen Intern Med. 2008;23:600–606. doi: 10.1007/s11606-008-0539-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tai-Seale M, Bramson R, Drukker D, et al. Understanding primary care physicians' propensity to assess elderly patients for depression using interaction and survey data. Med Care. 2005;43:1217–1224. doi: 10.1097/01.mlr.0000185734.00564.c1. [DOI] [PubMed] [Google Scholar]
- 5.Roter DL, Stewart M, Putnam SM, Lipkin M, Jr, Stiles W, Inui TS. Communication patterns of primary care physicians. J Amer Med Assoc. 1997;277:350–356. [PubMed] [Google Scholar]
- 6.Tai-Seale M, McGuire T, Colenda C, Rosen D, Cook MA. Two-minute mental health care for elderly patients: inside primary care visits. J Am Geriatr Soc. 2007;55:1903–1911. doi: 10.1111/j.1532-5415.2007.01467.x. [DOI] [PubMed] [Google Scholar]
- 7.Eaton CB, Goodwin MA, Stange KC. Direct observation of nutrition counseling in community family practice. Am Journal Prev Med. 2002;23:174–179. doi: 10.1016/s0749-3797(02)00494-4. [DOI] [PubMed] [Google Scholar]
- 8.Milder IE, Blokstra A, de Groot J, van Dulmen S, Bemelmans WJ. Lifestyle counseling in hypertension-related visits-analysis of video-taped practice visits. BMC Fam Prac. 2008;9:1–8. doi: 10.1186/1471-2296-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, Dubé R, Taleghani CK, Burke JE, Williams S, Eisenberg JM, Ayers W, Escarce JJ. The Effect of Race and Sex on Physicians' Recommendations for Cardiac Catheterization. N Engl J Med. 1999;340:618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 10.Van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians' perceptions of patients. Social Science & Medicine. 2000;50:813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 11.Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. Implicit Bias among Physicians and its Prediction of Thrombolysis Decisions for Black and White Patients. J Gen Intern Med. 2007;22:1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wunderlich T, Cooper G, Divine G, et al. Inconsistencies in patient perceptions and observer ratings of shared decision making: the case of colorectal cancer screening. Patient Educ Couns. 2010;80:358–363. doi: 10.1016/j.pec.2010.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shires DA, Stange KC, Divine G, et al. Prioritization of evidence-based preventive health services during periodic health examinations. Am Journal Prev Med. 2012;42:164–173. doi: 10.1016/j.amepre.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vera M, Alegria M, Freeman DH, Jr, Robles R, Pescosolido B, Pena M. Help seeking for mental health care among poor Puerto Ricans: problem recognition, service use, and type of provider. Med Care. 1998;36:1047–1056. doi: 10.1097/00005650-199807000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 16.Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42:1871–1894. doi: 10.1111/j.1475-6773.2006.00689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greene MG, Adelman RD, Friedmann E, Charon R. Older patient satisfaction with communication during an initial medical encounter. Soc Sci Med. 1994;38:1279–1288. doi: 10.1016/0277-9536(94)90191-0. [DOI] [PubMed] [Google Scholar]
- 18.Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42:1871–1894. doi: 10.1111/j.1475-6773.2006.00689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charon R, Greene MG, Adelman RD. Multi-dimensional interaction analysis: a collaborative approach to the study of medical discourse. Soc Sci Med. 1994;39:955–965. doi: 10.1016/0277-9536(94)90207-0. [DOI] [PubMed] [Google Scholar]
- 20.Frankel RM, Stein T. Getting the Most out of the Clinical Encounter: The Four Habits Model. The Permanente Journal. 1999;3:79–88. [PubMed] [Google Scholar]
- 21.Krupat E, Frankel R, Stein T, Irish J. The Four Habits Coding Scheme: validation of an instrument to assess clinicians' communication behavior. Patient Educ Couns. 2006;62:38–45. doi: 10.1016/j.pec.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 22.Stone AL, Tai-Seale M, Stults CD, Luiz JM, Frankel RM. Three types of ambiguity in coding empathic interactions in primary care visits: Implications for research and practice. Patient Educ Couns. 2012;89:63–68. doi: 10.1016/j.pec.2012.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. J Amer Med Assoc. 1999;282:583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 24.Street RL, Jr, Gordon H, Haidet P. Physicians' communication and perceptions of patients: is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007;65:586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tai-Seale M, McGuire T, Colenda C, Rosen D, Cook MA. Two-Minute Mental Health Care for Elderly Patients: Inside Primary Care Visits. J Am Geriatr Soc. 2007;55:1903–1911. doi: 10.1111/j.1532-5415.2007.01467.x. [DOI] [PubMed] [Google Scholar]
- 26.Kales HC, DiNardo AR, Blow FC, McCarthy JF, Ignacio RV, Riba MB. International medical graduates and the diagnosis and treatment of late-life depression. Acad Med. 2006;81:171–175. doi: 10.1097/00001888-200602000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 28.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians' empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359–364. doi: 10.1097/ACM.0b013e3182086fe1. [DOI] [PubMed] [Google Scholar]
- 29.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 30.Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roy-Byrne PP, Perera P, Pitts CD, Christi JA. Paroxetine response and tolerability among ethnic minority patients with mood or anxiety disorders: a pooled analysis. J Clin Psychiatry. 2005;66:1228–1233. doi: 10.4088/jcp.v66n1004. [DOI] [PubMed] [Google Scholar]
- 32.Leo RJ, Sherry C, Jones AW. Referral patterns and recognition of depression among African-American and Caucasian patients. Gen Hosp Psychiatry. 1998;20:175–182. doi: 10.1016/s0163-8343(98)00019-x. [DOI] [PubMed] [Google Scholar]
- 33.Skaer TL, Sclar DA, Robison LM, Galin RS. Trends in the rate of depressive illness and use of antidepressant pharmacotherapy by ethnicity/race: an assessment of office-based visits in the United States, 1992–1997. Clin Ther. 2000;22:1575–1589. doi: 10.1016/s0149-2918(00)83055-6. [DOI] [PubMed] [Google Scholar]
- 34.Harman JS, Edlund MJ, Fortney JC. Disparities in the adequacy of depression treatment in the United States. Psychiatr Serv. 2004;55:1379–1385. doi: 10.1176/appi.ps.55.12.1379. [DOI] [PubMed] [Google Scholar]
- 35.Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27:1280–1286. doi: 10.1007/s11606-012-2063-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stepien KA, Baernstein A. Educating for empathy. A review. J Gen Intern Med. 2006;21:524–530. doi: 10.1111/j.1525-1497.2006.00443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bonvicini KA, Perlin MJ, Bylund CL, Carroll G, Rouse RA, Goldstein MG. Impact of communication training on physician expression of empathy in patient encounters. Patient Educ Couns. 2009;75:3–10. doi: 10.1016/j.pec.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 38.Spiro H. What is empathy and can it be taught? Ann Intern Med. 1992;116:843–846. doi: 10.7326/0003-4819-116-10-843. [DOI] [PubMed] [Google Scholar]
- 39.Bellini LM, Shea JA. Mood change and empathy decline persist during three years of internal medicine training. Acad Med. 2005;80:164–167. doi: 10.1097/00001888-200502000-00013. [DOI] [PubMed] [Google Scholar]
- 40.Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84:1182–1191. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 41.Neumann M, Edelhauser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86:996–1009. doi: 10.1097/ACM.0b013e318221e615. [DOI] [PubMed] [Google Scholar]
- 42.Larson EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. J Amer Med Assoc. 2005;293:1100–1106. doi: 10.1001/jama.293.9.1100. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.