Abstract
The purpose of this study was to validate a commercially available IMU system against a standard lab-based motion capture system for the measurement of shoulder elevation, elbow flexion, trunk flexion/extension and neck flexion/extension kinematics. The validation analyses were applied to six surgical faculty members performing a standard, simulated surgical training task that mimics minimally invasive surgery. Three-dimensional joint kinematics were simultaneously recorded by an optical motion capture system and an IMU system with six sensors placed on the head, chest, and bilateral upper and lower arms. The sensor-to-segment axes alignment was accomplished manually. The IMU neck and trunk IMU flexion/extension angles were accurate to within 2.9±0.9 degrees and 1.6±1.1 degrees, respectively. The IMU shoulder elevation measure was accurate to within 6.8±2.7 degrees and the elbow flexion measure was accurate to within 8.2±2.8 degrees. In the Bland-Altman analyses, there were no significant systematic errors present; however, there was a significant inversely proportional error across all joints. As the gold standard measurement increased, the IMU underestimated the magnitude of the joint angle. This study reports acceptable accuracy of a commercially available IMU system; however, results should be interpreted as protocol specific.
Keywords: IMU, shoulder, biomechanics, ergonomics
Introduction
Upper body kinematic measures are widely used in ergonomics1–2 , orthopedics 3–4, and rehabilitation 5–7 to describe normal and pathological motion of the trunk, head, and arms. Traditional methods of motion capture utilize marker-based and electromagnetic laboratory-based systems to acquire highly accurate (within 1–3°) kinematic quantification6. While continued use of kinematic measurement within the laboratory is important and necessary, there is increased interest in the research and clinical practice communities to capture human motion outside of the laboratory setting8–10. Capturing kinematics during daily activities performed in their natural setting can advance our understanding of the cumulative biomechanical stress placed on joints that lead to musculoskeletal injury and disease11 that have been previously quantified with the use of 2D video analysis or subject observation12–13. Objective measurement of kinematics outside the laboratory requires wearable sensors that are easy to apply, unobtrusive, and reach a level of accuracy sufficient to answer the study question.
Inertial measurement units (IMUs) have grown in popularity for the measurement of joint motion outside of the laboratory. Current commercially available IMU sensors have a small form factor and easily attach to body segments with elastic straps. IMU sensors contain a gyroscope, magnetometer and accelerometer, and the fusion of this data provides the 3D rotations of each segment that can be applied directly in traditional kinematic calculation algorithms. However, prior to widespread application of IMUs in the real world, the sensors and collection protocols need to be validated. Validation studies of IMUs used to capture upper and lower body kinematics are increasing14–30.
To add to the body of literature documenting the accuracy of IMU systems for upper extremity kinematics, the purpose of this study was to validate a commercially available IMU system against a standard lab-based motion capture system for the measurement of shoulder elevation, elbow flexion, trunk flexion/extension and neck flexion/extension kinematics. For the future application of measuring the upper extremity biomechanics of surgeons during minimally invasive surgery, the validation analyses in this study were applied to participants performing a standard, simulated surgical training task that mimics minimally invasive surgery.
Methods
Participants
The Mayo Clinic Institutional Review Board approved the study and written informed consent was obtained from all research participants. Six surgical faculty members (3 male and 3 female) who perform minimally invasive surgery participated in this study. The mean±standard deviation age was 45±7 years, weight was 79.5±9.8 kg, and height was 176±9.8 cm. All six participants were right hand dominant.
Surgical-task Protocol
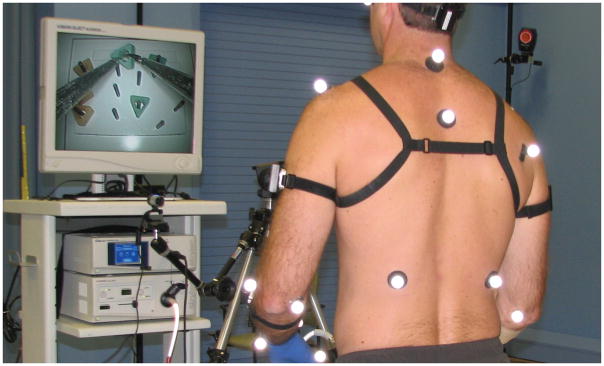
The IMUs were validated during the performance of a single task from The Fundamentals of Laparoscopic Surgery program (SAGES/ACS, FLS Program, Los Angeles, CA, USA), which includes a standard set of basic skills in minimally invasive laparoscopy31–32. Each surgeon performed the peg transfer task once using standard straight laparoscopic surgical instruments (Ethicon, 2015), with simultaneous measurement of joint motion captured with markers from the standard lab-based motion capture system and IMUs attached to the upper body segments (Figure 1). For the peg transfer task, the surgeon must grasp and transfer six small triangle shaped objects on a pegboard starting with the non-dominant hand and transferring midair to the dominant hand32–34. Once all six objects have been transferred to the opposite side of the pegboard, the procedure is reversed and each object is grasped with the dominant hand and transferred to the non-dominant hand and placed on the original side of the pegboard.
Figure 1.
Experimental setup. Participant is shown wearing reflective markers from the gold standard motion capture system and the IMUs are attached to the body with black Velcro straps. The peg transfer task is visible on the computer screen in front of the participant.
Standard Lab-based Kinematic Measurement
Three-dimensional marker trajectories of 12.5-mm reflective markers were placed on the surgeons’ head, trunk, upper arms and forearms and were recorded during the surgical task (80-Hz) using a 10 camera, Raptor 12 Digital RealTime Motion Capture System (Motion Analysis Corp., Santa Rosa, CA, USA). Local anatomic coordinate systems, following the right hand rule, were defined for each segment based on the upper extremity marker set (Table 1) as was described in full detail previously5. Static calibration (Arms down, thumbs forward) and dynamic movement trials of the surgeon were recorded for subsequent kinematic processing of the surgical task.
Table 1.
Coordinate System Definitions
| Segment | Markers | Coordinate System Origin | Coordinate System Sign Convention |
|---|---|---|---|
| Head | Anterior Left Right |
Geometric center between left and right | Anterior (+X), posterior (−X) Medial (+Z), lateral (−Z) Superior (+Y), inferior (−Y) |
| Trunk | Sternum Xiphoid C7 T10 |
Geometric Centerbetween Xiphoid and T10 | |
| Upper Arm | Acromion process Medial epicondyle Lateral epicondyle |
Shoulder center defined by regression equation5. | |
| Forearm | Medial epicondyle Lateral epicondyle Radial styloid Ulnar styloid |
Geometric center between epicondyle markers |
Inertial Measurement Unit Kinematic Measurement
Three-dimensional joint kinematics were simultaneously recorded (80 Hz) during the surgical task with an IMU system with six sensors (Opal™, APDM, Inc., Portland, OR USA) worn on the base of the back of the surgeon’s head, anterior sternum, and the lateral aspect of the bilateral upper-arms and forearms (Figure 1). All IMU sensors were similarly aligned with the positive y-axis pointing superiorly in the anatomical position. The static calibration pose for the IMUs was collected at the same time as the motion capture system static pose. For dynamic motion trials, data from the standard lab system and the IMU system were synchronized in time based on the upper arm elevation angles. The participants began each trial with their arms elevated above 45 degrees. When the trial began, the participants rapidly lowered their arms to neutral prior to picking up the surgical tools. The point of minimum elevation was identified in both the IMU and lab-based motion capture system signals for each joint for synchronization.
Data analyses
The standard lab-based kinematic data were filtered (6 Hz 4th order Butterworth filter) and processed with Visual3D software (CA-Motion, Inc., Germantown, MD) to produce three-dimensional marker trajectories. Euler joint angles5 were calculated for the peg transfer surgical task with reference to the static calibration pose. Shoulder elevation was defined as the upper arm motion relative to the trunk using the second rotation of the YXY rotation order (plane of elevation, elevation angle, and transverse plane)35. Elbow flexion was defined as the forearm relative to the upper arm, neck flexion/extension was defined as the head motion relative to the trunk, and trunk flexion/extension was defined as the trunk motion relative to the global coordinate system, all in the sagittal plane using a ZXY rotation order (sagittal, coronal, and transverse plane). To normalize the data with respect to time, the movement cycle was defined as the start of the task (i.e., initial grasp of the instrument) to the end of the task (i.e., release of grasp of the instrument). In addition to the time-series Euler angles for the joint motions described above, the maximum, minimum, mean, and range of motion of the Euler angles were determined for each joint for each participant.
Accelerometer, gyroscope, and magnetometer data from the IMU sensor data were fused into quaternion rotation matrices in Motion Studio software (APDM, Inc., Portland, OR USA). The quaternion rotation matrices were transformed into joint-specific Euler angles as described in the standard lab-based kinematic data analysis description using custom scripts programmed in MATLAB® (R2015b, Mathworks Inc., Natick, MA USA). The data from all segments were low-pass filtered (6 Hz 4th order Butterworth filter).
Validation Analyses
Data from the neck, trunk and the dominant right shoulder and elbow were utilized from each participant for the validation. The sample-to-sample RMS error was calculated to quantify the accuracy of the time-series kinematic data from the IMU system relative to the gold standard for each participant. Absolute differences were calculated between the gold standard and IMU system for the maximum, minimum, mean and range of motion measures from each joint angle. Group averages and standard deviations are reported for all measures. Additionally, Bland-Altman and ICC(A,1) methods were utilized to compare joint angles between the gold standard and IMU system36. In the Bland-Altman plots, systematic error is present if the mean is greater than or less than zero.
Results
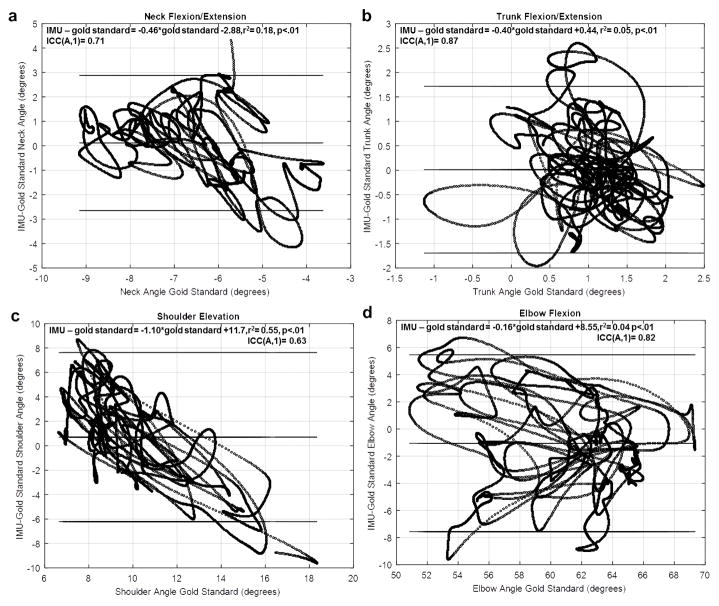
The IMU neck and trunk IMU flexion/extension angles were accurate to within 2.9±0.9 degrees (RMS error) and 1.6±1.1 degrees (RMS error), respectively (Table 2). The IMU shoulder elevation measure was accurate to within 6.8±2.7 degrees (RMS error) and the elbow flexion measure was accurate to within 8.2±2.8 degrees (RMS error) (Table 2). In the Bland-Altman analysis, there were no significant systematic errors present; however, there was a significant inversely proportional error across all joints (Figure 2). As the gold standard measurement increased, the IMU underestimated the magnitude of the joint angle. The associations (r2) of the proportional errors are below 0.2 except for the shoulder (r2=0.55).
Table 2.
Comparison of IMU derived joint angles to the standard lab-based motion capture system
| Joint Angle | Minimum Value Difference (deg) | Maximum Value Difference (deg) | Mean Value Difference (deg) | Range Difference (deg) | RMSE (deg) |
|---|---|---|---|---|---|
| Shoulder Elevation Mean | 5.9 | 4.7 | 3.0 | 8.1 | 6.8 |
| SD | 4.8 | 3.9 | 2.1 | 6.4 | 2.7 |
| Elbow Flexion Mean | 3.5 | 4.5 | 2.2 | 1.6 | 8.2 |
| SD | 2.7 | 3.0 | 1.6 | 8.8 | 2.8 |
| Neck Flexion Mean | 2.1 | 2.8 | 1.0 | 4.6 | 2.9 |
| SD | 2.8 | 2.6 | 0.6 | 5.0 | 0.9 |
| Trunk Flexion Mean | 1.4 | 1.9 | 0.5 | 1.7 | 1.6 |
| SD | 1.5 | 1.5 | 0.4 | 3.8 | 1.1 |
Figure 2.
Bland-Altman plots demonstrating the difference for joint angles when using IMU derived kinematics and standard lab-based motion capture system for (a) neck flexion/extension, (b) trunk flexion/extension, (c) shoulder elevation, and (d) elbow flexion. The dashed line represents the mean, while the solid lines represent the 95% limits of agreement (± 1.96 SD). ICC(A,1) values and linear regression equations are also presented.
Discussion
The purpose of this study was to determine the accuracy of a commercially available IMU system in measuring shoulder elevation and sagittal plane motion of the elbow, neck, and trunk relative to a standard lab-based marker-based motion capture system. Average IMU accuracy of the neck and trunk flexion/extension angles was within 3 degrees of the gold standard. Accuracy of IMU shoulder elevation was within 7 degrees of the gold standard and the elbow flexion measurement was within 9 degrees. Comparing the absolute range of motion measured by the two systems showed excellent range agreement for the neck, trunk, and elbow flexion/extension measures.
Previous studies that have tested the accuracy of the IMU system utilized in the present study reported RMSE errors up to 6.6 degrees for the trunk and up to 12.1 degrees for shoulder elevation over a multi-hour collection period14, 37. Our findings from short dynamic activity collections (<5 minutes) concur with the previous report and confirm that a range of accuracies can be expected across joints and data collection protocols. We noted differences up to 6 degrees in measuring the maximum angle and up to 5 degrees in the minimum angle. The differences in maximum and minimum values across joints are likely due to the specific IMU alignment on the segment. Aligning the IMU sensor with the anatomical reference of the segment is essential for achieving the best level of accuracy when the protocol does not utilize functional axes to transform the IMU axis to anatomical relevant axes17. To mimic the protocol utilized in the field based collections, functional axis setup was not implemented in the present study. Larger errors observed in the elbow would benefit from a functional motion axis setup. The forearm is a particularly challenging segment to properly place an IMU sensor due to the pronation/supination motion that can rotate the flexion/extension axis of the IMU such that it no longer aligns with the anatomical elbow flexion/extension axis. Larger errors in the forearm are likely due to placement and rotation challenges and likely not due to a sensor hardware or data fusion flaw.
Based on the Bland-Altman analyses, the IMU underestimates the gold standard at large joint angles and overestimates the joint angle at small angles. The largest error was observed in the shoulder elevation angle data. The correlations based on ICCs showed good to excellent agreement.
Interpreting kinematic outcomes in light of known system accuracy is essential to determine meaningful differences. For example, the IMU shoulder elevation accuracy was within 7 degrees, so this will require differences between groups or test-retest data sets utilizing the current protocol to be greater than 7 degrees to be a meaningful difference even if it reaches statistical significance. As 7 degrees of potential error may not be sufficient for some study questions, it is important to note that studies requiring high levels of kinematic accuracy will need to test additional protocols and may have to consider alternate measurement systems.
The limitations in this study include the small sample size and short collection time-frame. Additionally, as suggested earlier, improved results could have been achieved with additional post-processing; however, these results are typical and generalizable to an IMU collection protocol that would be utilized outside the laboratory setting. The validation comparison was performed against a standard lab-based motion capture system, which is also subject to errors. The measured resolution of the lab-based motion capture system is within 1 mm and 1° using a standard motion system accuracy device, and to within 3° of angular accuracy for human kinematics38.
In conclusion, this study reports acceptable accuracy of a commercially available IMU system for measuring upper body kinematics compared to a standard lab-based motion capture system. The results of this study are protocol specific as is the case in any accuracy study. Different sensor placement and different analysis methods will result in disparate outcomes. IMU kinematic data should be interpreted with the inversely proportional error in mind. IMU measurements are overestimated at small joint angles and underestimated at large joint angles.
Acknowledgments
This publication was made possible by funding from the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery and by the National Institutes of Health (R01 HD84423-01).
Footnotes
Conflict of Interest Disclosure: None of the authors has a conflict of interest to declare, and all authors were involved in the study design, data collection and interpretation, and contributed to the writing of the manuscript. This manuscript is not currently being considered for publication by another journal.
References
- 1.Yu D, Lowndes B, Morrow M, Kaufman K, Bingener J, Hallbeck S. Impact of novel shift handle laparoscopic tool on wrist ergonomics and task performance. Surg Endosc. 2015 doi: 10.1007/s00464-015-4634-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gadotti IC, Elbaum L, Jung Y, Garbalosa V, Kornbluth S, Da Costa B, Maitra K, Brunt D. Evaluation of eye, head and trunk coordination during target tracking tasks. Ergonomics. 2016:1–8. doi: 10.1080/00140139.2016.1146345. [DOI] [PubMed] [Google Scholar]
- 3.Rainbow MJ, Wolff AL, Crisco JJ, Wolfe SW. Functional kinematics of the wrist. J Hand Surg Eur Vol. 2016;41(1):7–21. doi: 10.1177/1753193415616939. [DOI] [PubMed] [Google Scholar]
- 4.Jun BJ, Lee TQ, McGarry MH, Quigley RJ, Shin SJ, Iannotti JP. The effects of prosthetic humeral head shape on glenohumeral joint kinematics during humeral axial rotation in total shoulder arthroplasty. J Shoulder Elbow Surg. 2016 doi: 10.1016/j.jse.2015.11.058. [DOI] [PubMed] [Google Scholar]
- 5.Morrow MM, Hurd WJ, Kaufman KR, An KN. Shoulder demands in manual wheelchair users across a spectrum of activities. J Electromyogr Kinesiol. 2010;20(1):61–7. doi: 10.1016/j.jelekin.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao KD, Van Straaten MG, Cloud BA, Morrow MM, An KN, Ludewig PM. Scapulothoracic and Glenohumeral Kinematics During Daily Tasks in Users of Manual Wheelchairs. Front Bioeng Biotechnol. 2015;3:183. doi: 10.3389/fbioe.2015.00183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin YL, Karduna A. A four-week exercise program does not change rotator cuff muscle activation and scapular kinematics in healthy subjects. J Orthop Res. 2016 doi: 10.1002/jor.23234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fantozzi S, Giovanardi A, Magalhaes FA, Di Michele R, Cortesi M, Gatta G. Assessment of three-dimensional joint kinematics of the upper limb during simulated swimming using wearable inertial-magnetic measurement units. J Sports Sci. 2016;34(11):1073–80. doi: 10.1080/02640414.2015.1088659. [DOI] [PubMed] [Google Scholar]
- 9.Pellegrini A, Tonino P, Paladini P, Cutti A, Ceccarelli F, Porcellini G. Motion analysis assessment of alterations in the scapulo-humeral rhythm after throwing in baseball pitchers. Musculoskelet Surg. 2013;97(Suppl 1):9–13. doi: 10.1007/s12306-013-0253-4. [DOI] [PubMed] [Google Scholar]
- 10.Tranquilli C, Bernetti A, Picerno P. Ambulatory joint mobility and muscle strength assessment during rehabilitation using a single wearable inertial sensor. Med Sport. 2013;66(4):583–597. [Google Scholar]
- 11.Keyserling WM. Workplace risk factors and occupational musculoskeletal disorders, Part 2: A review of biomechanical and psychophysical research on risk factors associated with upper extremity disorders. Aihaj. 2000;61(2):231–43. doi: 10.1080/15298660008984532. [DOI] [PubMed] [Google Scholar]
- 12.Aitchison LP, Cui CK, Arnold A, Nesbitt-Hawes E, Abbott J. The ergonomics of laparoscopic surgery: a quantitative study of the time and motion of laparoscopic surgeons in live surgical environments. Surg Endosc. 2016 doi: 10.1007/s00464-016-4855-4. [DOI] [PubMed] [Google Scholar]
- 13.Douoguih WA, Dolce DL, Lincoln AE. Early Cocking Phase Mechanics and Upper Extremity Surgery Risk in Starting Professional Baseball Pitchers. Orthop J Sports Med. 2015;3(4) doi: 10.1177/2325967115581594. 2325967115581594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schall MC, Jr, Fethke NB, Chen H, Oyama S, Douphrate DI. Accuracy and repeatability of an inertial measurement unit system for field-based occupational studies. Ergonomics. 2015:1–23. doi: 10.1080/00140139.2015.1079335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGinnis RS, Cain SM, Tao S, Whiteside D, Goulet GC, Gardner EC, Bedi A, Perkins NC. Accuracy of Femur Angles Estimated by IMUs During Clinical Procedures Used to Diagnose Femoroacetabular Impingement. IEEE transactions on bio-medical engineering. 2015;62(6):1503–13. doi: 10.1109/TBME.2015.2392758. [DOI] [PubMed] [Google Scholar]
- 16.Leardini A, Lullini G, Giannini S, Berti L, Ortolani M, Caravaggi P. Validation of the angular measurements of a new inertial-measurement-unit based rehabilitation system: comparison with state-of-the-art gait analysis. J Neuroeng Rehabil. 2014;11:136. doi: 10.1186/1743-0003-11-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouvier B, Duprey S, Claudon L, Dumas R, Savescu A. Upper Limb Kinematics Using Inertial and Magnetic Sensors: Comparison of Sensor-to-Segment Calibrations. Sensors (Basel) 2015;15(8):18813–33. doi: 10.3390/s150818813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cutti AG, Ferrari A, Garofalo P, Raggi M, Cappello A, Ferrari A. 'Outwalk': a protocol for clinical gait analysis based on inertial and magnetic sensors. Med Biol Eng Comput. 2010;48(1):17–25. doi: 10.1007/s11517-009-0545-x. [DOI] [PubMed] [Google Scholar]
- 19.Cutti AG, Giovanardi A, Rocchi L, Davalli A, Sacchetti R. Ambulatory measurement of shoulder and elbow kinematics through inertial and magnetic sensors. Med Biol Eng Comput. 2008;46(2):169–78. doi: 10.1007/s11517-007-0296-5. [DOI] [PubMed] [Google Scholar]
- 20.El-Gohary M, McNames J. Shoulder and elbow joint angle tracking with inertial sensors. IEEE Trans Biomed Eng. 2012;59(9):2635–41. doi: 10.1109/TBME.2012.2208750. [DOI] [PubMed] [Google Scholar]
- 21.Faber GS, Kingma I, Bruijn SM, van Dieen JH. Optimal inertial sensor location for ambulatory measurement of trunk inclination. J Biomech. 2009;42(14):2406–9. doi: 10.1016/j.jbiomech.2009.06.024. [DOI] [PubMed] [Google Scholar]
- 22.Favre J, Aissaoui R, Jolles BM, de Guise JA, Aminian K. Functional calibration procedure for 3D knee joint angle description using inertial sensors. J Biomech. 2009;42(14):2330–5. doi: 10.1016/j.jbiomech.2009.06.025. [DOI] [PubMed] [Google Scholar]
- 23.Ha TH, Saber-Sheikh K, Moore AP, Jones MP. Measurement of lumbar spine range of movement and coupled motion using inertial sensors - a protocol validity study. Man Ther. 2013;18(1):87–91. doi: 10.1016/j.math.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 24.Hyde RA, Ketteringham LP, Neild SA, Jones RS. Estimation of upper-limb orientation based on accelerometer and gyroscope measurements. IEEE Trans Biomed Eng. 2008;55(2 Pt 1):746–54. doi: 10.1109/TBME.2007.912647. [DOI] [PubMed] [Google Scholar]
- 25.Luinge HJ, Veltink PH, Baten CT. Ambulatory measurement of arm orientation. J Biomech. 2007;40(1):78–85. doi: 10.1016/j.jbiomech.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 26.O'Donovan KJ, Kamnik R, O'Keeffe DT, Lyons GM. An inertial and magnetic sensor based technique for joint angle measurement. J Biomech. 2007;40(12):2604–11. doi: 10.1016/j.jbiomech.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 27.Perez R, Costa U, Torrent M, Solana J, Opisso E, Caceres C, Tormos JM, Medina J, Gomez EJ. Upper limb portable motion analysis system based on inertial technology for neurorehabilitation purposes. Sensors (Basel) 2010;10(12):10733–51. doi: 10.3390/s101210733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Picerno P, Cereatti A, Cappozzo A. Joint kinematics estimate using wearable inertial and magnetic sensing modules. Gait Posture. 2008;28(4):588–95. doi: 10.1016/j.gaitpost.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 29.Theobald PS, Jones MD, Williams JM. Do inertial sensors represent a viable method to reliably measure cervical spine range of motion? Man Ther. 2012;17(1):92–6. doi: 10.1016/j.math.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 30.Zhou H, Stone T, Hu H, Harris N. Use of multiple wearable inertial sensors in upper limb motion tracking. Medical Engineering & Physics. 2008;30(1):123–133. doi: 10.1016/j.medengphy.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 31.Brown-Clerk B, de Laveaga AE, LaGrange CA, Wirth LM, Lowndes BR, Hallbeck MS. Laparoendoscopic single-site (LESS) surgery versus conventional laparoscopic surgery: comparison of surgical port performance in a surgical simulator with novices. Surg Endosc. 2011;25(7):2210–8. doi: 10.1007/s00464-010-1524-x. [DOI] [PubMed] [Google Scholar]
- 32.Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, Hoffman K. Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery. 2004;135(1):21–7. doi: 10.1016/s0039-6060(03)00156-9. [DOI] [PubMed] [Google Scholar]
- 33.Derossis AM, Fried GM, Abrahamowicz M, Sigman HH, Barkun JS, Meakins JL. Development of a model for training and evaluation of laparoscopic skills. Am J Surg. 1998;175(6):482–7. doi: 10.1016/s0002-9610(98)00080-4. [DOI] [PubMed] [Google Scholar]
- 34.Keyser EJ, Derossis AM, Antoniuk M, Sigman HH, Fried GM. A simplified simulator for the training and evaluation of laparoscopic skills. Surg Endosc. 2000;14(2):149–53. doi: 10.1007/s004649900088. [DOI] [PubMed] [Google Scholar]
- 35.Wu G, van der Helm FC, Veeger HE, Makhsous M, Van Roy P, Anglin C, Nagels J, Karduna AR, McQuade K, Wang X, Werner FW, Buchholz B. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion--Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38(5):981–992. doi: 10.1016/j.jbiomech.2004.05.042. [DOI] [PubMed] [Google Scholar]
- 36.Fortune E, Lugade VA, Amin S, Kaufman KR. Step detection using multi-versus single tri-axial accelerometer-based systems. Physiol Meas. 2015;36(12):2519–35. doi: 10.1088/0967-3334/36/12/2519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Vries WH, Veeger HE, Cutti AG, Baten C, van der Helm FC. Functionally interpretable local coordinate systems for the upper extremity using inertial & magnetic measurement systems. Journal of biomechanics. 2010;43(10):1983–8. doi: 10.1016/j.jbiomech.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 38.Morrow MM, Kaufman KR, An KN. Scapula kinematics and associated impingement risk in manual wheelchair users during propulsion and a weight relief lift. Clinical biomechanics. 2011;26(4):352–7. doi: 10.1016/j.clinbiomech.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]