Abstract
Background and objectives
Although anthropometric measures of body fat are associated with development of CKD, they may not be able to distinguish between various forms of fat and therefore may be less accurate than computed tomography (CT) measures. We compared the association of CT and anthropometric measures of obesity with kidney outcomes in the Health Aging and Body Composition Study.
Design, setting, participants, & measurements
Participants were recruited from March of 1997 through July of 1998. CT measures included visceral abdominal fat (VAT), subcutaneous adipose tissue (SAT), and intermuscular fat area (IMAT), whereas anthropometric measures included waist circumference (WC) and body mass index (BMI). Kidney outcomes included kidney function (KF) decline (30% decrease in eGFRcysC in follow-up at either year 3 or 10) or incident CKD (follow-up eGFRcysC≤60 ml/min per 1.73 m2 in individuals with baseline GFR>60 ml/min per 1.73 m2). Multivariable logistic regression models and Poisson regression models were used to evaluate the association with decline in KF and incident kidney disease, respectively. We also assessed for the independent associations among the exposure measures by including them in the same model.
Results
Two-thousand four-hundred and eighty-nine individuals were included. Mean age was 74±3 years, 49% were men, 39% were black, 59% were hypertensive, and 15% were diabetic. KF decline occurred in 17% of the population, whereas incident CKD also occurred in 17% of those at risk. In continuous models, SAT, VAT, IMAT, BMI, and WC (per SD increase) were all significantly associated with KF decline. There was a significant interaction between VAT and CKD with regard to KF decline (P=0.01). Only VAT, BMI, and WC were associated with incident CKD. Only VAT remained a significant risk factor for incident CKD when other exposure variables were included in the same model. There was no association between any measure of obesity and kidney outcomes when creatinine values at years 3 and 10 were used to estimate changes in eGFR.
Conclusions
Anthropometric measures of body fat appear to provide as consistent estimates of KF decline risk as CT measures in elders.
Keywords: chronic kidney disease; renal function decline; Aged; Body Composition; Body Mass Index; diabetes mellitus; Follow-Up Studies; Humans; Intra-Abdominal Fat; Logistic Models; Male; obesity; Renal Insufficiency, Chronic; risk factors; Subcutaneous Fat; Subcutaneous Fat, Abdominal; Tomography; Tomography, X-Ray Computed; Waist Circumference
Introduction
In the past two decades, there has been an increase in the prevalence of CKD (1,2) that has paralleled the increase in the prevalence of obesity. Although obesity is a major cause of diabetes and hypertension, the two primary causes of CKD (3,4), recent epidemiologic studies indicate that obesity is an independent risk factor for CKD (5–8). In cross-sectional studies there is a higher prevalence of CKD, defined by an eGFR<60 ml/min per 1.73 m2, with higher levels of body mass index (BMI), whereas in longitudinal studies higher levels of obesity have been associated with incident CKD and development of ESRD (8–10). Although higher BMI has been associated with development of CKD, it may not be the optimal measure of obesity. In fact, epidemiologic studies demonstrated that waist-to-hip ratio (WHR) was more closely associated with both cardiovascular events and progression of CKD in comparison with BMI in subjects with CKD (9,11). In CKD, muscle wasting is common (12) and lower BMI may reflect either decreased visceral fat or decreased muscle mass, the latter being a marker of both malnutrition and inflammation. Similar results have been found in older adults where WHR is more closely associated with all-cause mortality than BMI (13), and waist circumference (WC), but not BMI, was associated with kidney function (KF) decline (14). It has been hypothesized that WHR and WC may be better measures of risk as they reflect central obesity and visceral fat. Visceral fat is a key regulator of numerous adipokines and cytokines (15), and has also been associated with insulin resistance, metabolic syndrome, and diabetes (16,17), all pathophysiologic processes that are implicated in CKD. In addition, intermuscular adipose tissue (IMAT) is associated with both muscle function and mobility function in older adults and across a wide variety of comorbid conditions and is implicated in metabolic dysfunction such as insulin resistance. The gold standard and most accurate assessment of subcutaneous adipose tissue (SAT), visceral abdominal fat (VAT), and IMAT is computed tomography (CT) (18). We hypothesized that CT measures would confer the highest risk of kidney function decline in comparison with other measures. To our knowledge, no studies have evaluated whether adiposity assessed by CT scan is associated with KF decline and/or incident CKD and whether it provides a better measure of risk assessment than BMI and WC. The objective of this study was therefore to assess this question in the Health Aging and Body Composition (Health ABC) Study, a cohort composed of older adults where muscle wasting is prevalent and where direct measures of adiposity may be particularly important.
Materials and Methods
Subjects
Health ABC is a population-based, prospective study designed to evaluate the effects of weight and body composition on age-related physiologic and functional changes. Individuals aged 70–79 years were recruited from March of 1997 through July of 1998 at two field centers located in Pittsburgh, Pennsylvania and Memphis, Tennessee. The cohort consisted of 3075 men (48.4%) and women (51.6%), of whom 41.6% were black. All Health ABC participants with CT scan measurements at baseline and at least two measurements of cystatin C (the first at the time of abdominal CT) were included in the analysis.
Exposure Variables
VAT, SAT, and IMAT.
Abdominal fat was estimated with a 1-cm CT image obtained during suspended respiration between the fourth and fifth lumbar vertebrae. A GE 9800 Advantage was used in Pittsburgh, and a Siemens Somatom Plus and a Picker PQ2000S were used in Memphis. Central readings were performed at the University of Colorado Health Sciences Center. The adipose tissue density range was determined from a bimodal histogram of adipose and soft tissue intensities. Image pixels with intensity within this range were classified as adipose tissue. The fat area for the entire image was determined by multiplying the number of adipose tissue pixels by the area of a pixel. A region-of-interest line was drawn at the junction of the abdominal wall musculature and the visceral compartment, extending around the body to the back muscles. Adipose tissue within this circle was considered to be VAT. The difference in fat area between the entire image and the visceral fat is equal to the subcutaneous fat area (19). IMAT area and muscle attenuation (Hounsfield units) were recorded from thigh CT. The mean attenuation of thigh muscle was recorded. Lower attenuation indicates greater fat infiltration of muscle.
WC and BMI.
WC was measured using the smallest circumference between the lower ribs and iliac crests. WHR was not part of the baseline anthropometric measures performed at Health ABC because WC was not measured in a traditional way in HABC; instead, sagittal diameter was measured.
Outcomes.
KF was estimated using serum cystatin C using the formula: 133 × minutes (Scys/0.8, 1)−0.499×maximum (Scys/0.8, 1)−1.328×0.996age (×0.932 for women) (20). This formula was developed from the pooling of several cohorts with measured GFR. The years 3 and 10 cystatin C values were measured at the same time.
Decline in KF was defined as a 30% decrease in eGFRcysC in follow-up at either year 3 or 10. This definition for KF decline was on the basis of the recent Food and Drug Administration meeting as a recommended end point for clinical trials (21). Change in KF was defined by calculating the rates of change in eGFRcysC using two or three measurements of cystatin C.
Incident CKD was defined as a follow-up eGFRcysC<60 ml/min per 1.73 m2 in individuals with baseline GFR≥60 ml/min per 1.73 m2. To avoid those subjects with minor fluctuations in eGFRcysC that may be due to “noise,” the definition also included a 1 ml/min per 1.73 m2/yr decrease in eGFR.
Our primary analyses were on the basis of cystatin C for several reasons. First, compared with creatinine, cystatin C is less influenced by sex, race, and muscle mass and may therefore more accurately reflect KF in an elderly population (22). Second, cystatin C is more strongly associated with adverse outcomes in the elderly, appears more sensitive to changes in KF (23,24), and has been calibrated across the visits. All cystatin C measures were conducted at the University of Vermont and a series of internal controls were used to recalibrate the biased measures (years 3, 10) to the original standard. Third, we were unable to adjust for drift or calibration of creatinine given that years 3 and 10 creatinine values were standardized to isotope dilution mass spectrometry whereas baseline values were not. This led to year 3 creatinine eGFR being higher than the nonstandardized baseline value. In order to try to address this issue and perform analyses using serum creatinine, we repeated the analyses incorporating creatinine measures at years 3 and 10 and estimating eGFR on the basis of the Chronic Kidney Disease Epidemiology Collaboration equation using the same definition for KF decline and incident CKD.
Covariates.
These included socio-demographic factors (age, sex, race, clinical site, education level); lifestyle factors (current smoking [defined by current versus former or never], alcohol use [defined by >1 versus <1 drink/d]); and comorbid conditions (impaired fasting glucose [defined as fasting glucose from 100 to 125 mg/d], impaired glucose tolerance [IGT] [defined as a 2-hour glucose tolerance of 140–200 mg/dl], diabetes [defined by use of hypoglycemic agents, self-report, fasting plasma glucose ≥126 mg/dl, or an oral glucose tolerance test ≥200 mg/dl]; hypertension [defined by either self-report plus use of antihypertensive medications, or measured systolic BP >140 mmHg or diastolic BP >90 mmHg]; mean arterial pressure, heart failure, coronary heart disease [defined as myocardial infarction, angina, coronary artery bypass], total cholesterol, LDL cholesterol, HDL cholesterol, and urinary albumin-to-creatinine ratio [defined as milligrams of albumin/gram of creatinine]).
Statistical Analyses
We categorized participants by quartiles of VAT and SAT, and compared the distribution of demographics and covariates across quartiles using the chi-squared test for categoric variables and ANOVA or the Kruskal–Wallis test for continuous variables, as appropriate.
Spearman correlations were used to evaluate the correlations between VAT, SAT, and IMAT with BMI and WC. Unadjusted splines were performed to evaluate the relationship between SAT and VAT with KF decline (defined as eGFRcysC>30%) and incident CKD. Linear mixed models with random intercepts and slopes were used to estimate and compare linear trends in mean eGFR and were used to evaluate the association between VAT and SAT with KF decline (defined as eGFRcysC>30%). This approach took into account the correlation of observations within subjects. To evaluate the association of exposure variables and incident CKD, we used Poisson regression to calculate adjusted incident relative risks. Analyses were conducted with VAT and SAT as continuous variables (per SD increase) and then categorized as quartiles. Similar analyses were performed for BMI and WC.
Models were adjusted as follows: model 1 adjusted for demographics (age, sex, race, and site). Model 2 was adjusted as for model 1 plus systolic BP, mean arterial pressure, IGT, impaired fasting glucose, diabetes, albumin-to-creatinine ratio, and antihypertensive medications. Model 3 was adjusted as for model 2 variables plus smoking, LDL cholesterol, HDL cholesterol, hormone replacement therapy, prevalent coronary heart disease, and heart failure. For the incident CKD outcome, analyses were also adjusted for baseline eGFR. For the outcome of KF decline (defined as eGFRcysC>30%), interactions between SAT and VAT with baseline CKD (eGFR<60 ml/min per 1.73 m2) status were performed. Analyses were performed using S-Plus (release 8.0; Insightful Inc., Seattle, WA) and SPSS statistical software (release 16.0.1; SPSS Inc., Chicago, IL).
Sensitivity Analyses
Because assessment of eGFR incorporates body surface area, larger body size could be associated with lower eGFR in cross-sectional analyses. For this reason, the association between SAT and VAT with outcomes was repeated using decline in KF on a continuous scale. Given that body composition differs significantly by race and sex, interactions with these variables was evaluated for both kidney outcomes. Analyses were adjusted for BMI in order to assess if all of the exposure variables remained significant risk factors for kidney outcomes after adjusting for total adiposity. We also evaluated for independent associations among the exposure measures by including VAT, SAT, an IMAT in one model, and BMI and WC in another model. In addition, we evaluated if the results were consistent using a 40% decline in eGFRcysC (21). Finally, the BMI analyses were analyzed using World Health Organization (WHO) definitions for overweight and obesity.
Results
Of the 3075 Health ABC participants, 27 did not have baseline cys C measurements, 350 were missing follow-up cys C measurements, and 209 did not have CT performed, leaving 2489 subjects available for these analyses. The mean age was 74±3 years, 49% were men, 39% were black, 59% were hypertensive, and 15% were diabetic (Table 1). The mean eGFRcysC was 88 ml/min per 1.73 m2 and 8% had eGFR<60 ml/min per 1.73 m2. Higher quartiles of both SAT and VAT were associated with worse metabolic profiles (higher prevalence of diabetes, hypertension, cardiovascular disease, and worse lipid profile) and lower eGFRcysC (Table 1). The spearman correlations between SAT with VAT, BMI, and WC were 0.3, 0.8, and 0.6, respectively. The correlations between VAT with BMI and WC were 0.6 and 0.7, respectively. The correlations between SAT and VAT with IMAT were 0.6 and 0.5, respectively. Median length of follow-up was 8.9 years; the mean annual percent decline was 3.2±6.3.
Table 1.
Baseline participant characteristics by quartiles of visceral fat area
| Characteristic | Abdomen Visceral Fat (cm2) | All | |||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| <95 cm2 | 95–132 cm2 | 133–181 cm2 | >181 cm2 | ||
| N | 618 | 626 | 625 | 620 | 2489 |
| Age, yr | 74 (3) | 74 (3) | 74 (3) | 74 (3) | 74 (3) |
| Men, n (%) | 234 (38) | 284 (45) | 320 (51) | 369 (60) | 1207 (49) |
| Black, n (%) | 321 (52) | 248 (40) | 229 (37) | 175 (28) | 973 (39) |
| Site, n (%) | |||||
| Memphis | 268 (43) | 281 (45) | 322 (52) | 363 (59) | 1234 (50) |
| Pittsburgh | 350 (57) | 345 (55) | 303 (49) | 257 (42) | 1255 (50) |
| Diabetes, n (%) | 51 (8) | 73 (12) | 101 (16) | 135 (22) | 360 (15) |
| Hypertension, n (%) | 367 (59) | 363 (58) | 353 (57) | 385 (62) | 1468 (59) |
| SBP, mmHg | 135 (21) | 135 (20) | 135 (21) | 136 (21) | 135 (21) |
| DBP, mmHg | 71 (12) | 70 (12) | 72 (11) | 72 (11) | 71 (12) |
| Smoking, n (%) | |||||
| Never | 319 (52) | 279 (45) | 276 (44) | 231 (37) | 1105 (44) |
| Former | 207 (34) | 295 (47) | 291 (47) | 355 (57) | 1148 (46) |
| Current | 92 (15) | 50 (8) | 57 (9) | 34 (6) | 122 (9) |
| Alcohol, drinks/wk | |||||
| >1 | 163 (27) | 196 (31) | 199 (32) | 196 (32) | 754 (30) |
| HTN meds, n (%) | 278 (45) | 316 (51) | 340 (55) | 388 (63) | 1322 (53) |
| Oral estrogen, n (%) | 108 (18) | 84 (13) | 67 (11) | 45 (7) | 304 (12) |
| Prevalent CHD, n (%) | 103 (17) | 116 (19) | 132 (21) | 161 (26) | 512 (21) |
| Prevalent HF, n (%) | 9 (2) | 16 (3) | 19 (3) | 14 (2) | 58 (2) |
| Prevalent stroke, n (%) | 65 (11) | 52 (8) | 54 (9) | 54 (9) | 225 (9) |
| Cholesterol, mg/dl | 203 (36) | 203 (38) | 205 (39) | 200 (4) | 203 (38) |
| LDL cholesterol, mg/dl | 119 (33) | 123 (35) | 125 (34) | 120 (35) | 122 (34) |
| HDL cholesterol, mg/dl | 63 (18) | 55 (16) | 51 (16) | 47 (14) | 54 (17) |
| Triglycerides, mg/dla | 97 [75,124] | 114 [86,152] | 129 [98,179] | 146 [110,199] | 119 [88,165] |
| eGFR-cysC, ml/min per 1.73 m2 | 92 (17) | 90 (16) | 87 (18) | 84 (19) | 88 (18) |
| eGFR-cysC<60 ml/min per 1.73 m2 | 34 (6) | 35 (6) | 53 (9) | 72 (12) | 194 (8) |
| UACRa | 8 (5,17) | 7 (4,15) | 8 (4,18) | 9 (5,24) | 8 (5,19) |
| ACR>30 mg/g | 89 (15) | 84 (14) | 103 (17) | 137 (22) | 413 (17) |
| BMI | 24.1 (3.9) | 26.4 (3.7) | 28.0 (3.9) | 30.6 (4.2) | 27.3 (4.6) |
| Weight, kg | 65 (12) | 73 (11) | 78 (12) | 87 (14) | 76 (15) |
| Height, cm | 164 (9) | 166 (9) | 167 (9) | 168 (9) | 166 (9) |
| Waist circumference, cm | 89 (10) | 97 (10) | 102 (10) | 109 (10) | 99 (12) |
Data expressed as n and %, mean (SD). SBP, systolic BP; DPB, diastolic BP; HTN, hypertension; CHD, coronary heart disease; HF, heart failure; eGFR-cysC, eGFR-cystatin C; UACR, urinary albumin-to-creatinine ratio; ACR, albumin-to-creatinine ratio; BMI, body mass index.
Median (IQR).
Outcomes
KF Decline (Defined as eGFRcysC>30%).
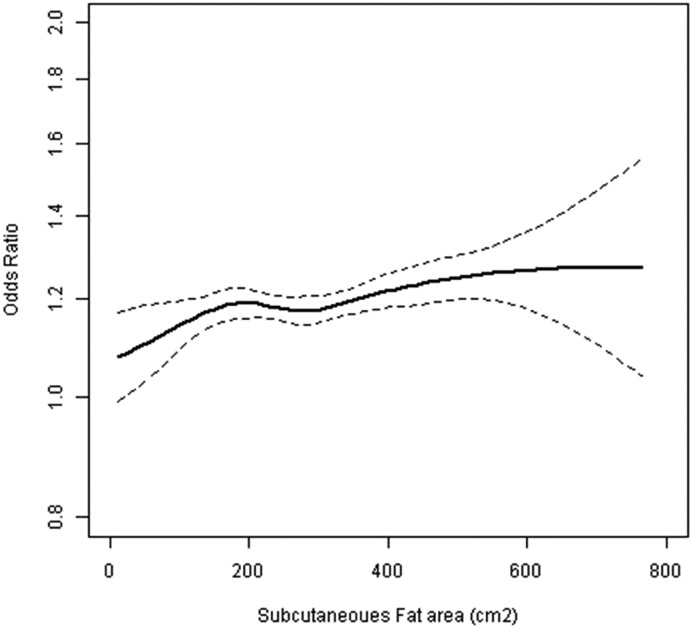
KF decline was present in 17% of the population. Figure 1 shows the splines relating VAT and SAT with KF decline, with VAT demonstrating a more linear relationship. In continuous models, each SD higher SAT was associated with higher odds of KF decline in univariate and fully adjusted models. SAT was not associated with KF decline when examined in quartiles (Table 2). In continuous models, each SD higher VAT was associated with significantly higher odds for KF decline in univariate and fully adjusted models. The highest quartile of VAT was associated with a significant risk for KF decline that was attenuated in the fully adjusted models (Table 2). In continuous models, each SD higher IMAT was associated with higher odds for KF decline in univariate and fully adjusted models. The highest quartile of IMAT was associated with a significant risk of KF decline in the fully adjusted models (Table 2). In continuous univariate and fully adjusted models, each SD higher BMI was associated with a significant risk for KF decline. WC was associated with a with higher risk increase for KF decline in univariate and fully adjusted models. In categoric analyses, the highest quartiles of both BMI and WC were significantly associated with KF decline (Table 2). The P value for the interaction between CKD and SAT was 0.6. There was, however, a significant interaction between VAT and CKD (P value=0.01). When the analyses were stratified by the presence or absence of CKD, VAT remained an independent risk factor for KF decline only in the population without CKD (Table 3). Analyses were repeated using creatinine eGFR at years 3 and 10. In unadjusted and partially adjusted models, SAT, VAT, IMAT, WC, and BMI were all associated with KF decline in unadjusted and partially adjusted continuous models, but no longer significant in the fully adjusted models. None of the exposure variables were associated with KF decline in continuous or categoric models. In categoric models, the highest quartile for all exposure variables was associated with KF decline in unadjusted and partially adjusted models, but the relationship was attenuated and no longer significant in the fully adjusted models (Supplemental Table 1, Table 4).
Figure 1.
Subcutaneous adipose tissue and kidney function decline. Spline analyses (unadjusted).
Table 2.
Association of measures of adiposity with kidney function decline
| Variable | N | ΔeGFR>30% | Unadjusted OR (95% CI) | Model 1a OR (95% CI) | Model 2b OR (95% CI) |
|---|---|---|---|---|---|
| Subcutaneous fat | |||||
| Continuous (per SD=121) | 2489 | 434 | 1.2 (1.0 to 1.3) | 1.3 (1.1 to 1.4) | 1.18 (1.04 to 1.33) |
| Quartiles | |||||
| <196 | 621 | 103 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 196–267 | 619 | 97 | 0.9 (0.7 to 1.3) | 1.0 (0.7 to 1.3) | 0.9 (0.7 to 1.3) |
| 268–357 | 633 | 108 | 1.0 (0.8 to 1.4) | 1.1 (0.8 to 1.6) | 1.0 (0.8 to 1.4) |
| >357 | 616 | 126 | 1.3 (1.0 to 1.7) | 1.6 (1.1 to 2.2) | 1.4 (1.0 to 1.9) |
| Visceral fat | |||||
| Continuous (per SD=67) | 2489 | 434 | 1.3 (1.2 to 1.4) | 1.3 (1.9 to 1.5) | 1.2 (1.0 to 1.3) |
| Quartiles | |||||
| <94 | 618 | 88 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 94–132 | 626 | 89 | 1.0 (0.7 to 1.3) | 1.0 (0.7 to 1.4) | 0.91 (0.7 to 1.3) |
| 133–181 | 625 | 115 | 1.4 (1.0 to 1.9) | 1.4 (1.0 to 1.9) | 1.2 (0.9 to 1.6) |
| >181 | 620 | 142 | 1.8 (1.4 to 2.4) | 1.9 (1.4 to 2.5) | 1.38 (1.0 to 1.9) |
| R thigh intermuscular fat area, cm2 | |||||
| Continuous (per SD=6.8) | 2481 | 430 | 1.2 (1.1 to 1.3) | 1.2 (1.1 to 1.3) | 1.1 (1.0 to 1.2) |
| Quartiles | |||||
| <6.15 | 631 | 83 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 6.15–9.01 | 641 | 104 | 1.3 (1.0 to 1.8) | 1.3 (1.0 to 1.8) | 1.3 (1.0 to 1.8) |
| 9.02–13.12 | 620 | 113 | 1.5 (1.1 to 2.1) | 1.5 (1.1 to 2.1) | 1.4 (1.0 to 1.9) |
| >13.12 | 589 | 130 | 1.9 (1.4 to 2.6) | 1.9 (1.4 to 2.6) | 1.5 (1.1 to 2.1) |
| Waist circumference | |||||
| Continuous (per SD=12.5) | 2488 | 434 | 1.3 (1.2 to 1.5) | 1.3 (1.2 to 1.5) | 1.2 (1.1 to 1.4) |
| Quartiles | |||||
| <91.7 | 616 | 81 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 91.7–99.2 | 645 | 98 | 1.2 (0.9 to 1.6) | 1.2 (0.8 to 1.6) | 1.2 (0.8 to 1.6) |
| 99.3–107.1 | 631 | 118 | 1.6 (1.2 to 2.1) | 1.5 (1.1 to 2.1) | 1.4 (1.0 to 2.0) |
| >107.1 | 596 | 137 | 2.0 (1.5 to 2.7) | 1.9 (1.4 to 2.6) | 1.6 (1.1 to 2.2) |
| BMI | |||||
| Continuous (per SD=4.6) | 2489 | 434 | 1.3 (1.2 to 1.4) | 1.3 (1.2 to 1.4) | 1.2 (1.0 to 1.3) |
| Quartiles | |||||
| <24.1 | 615 | 85 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 24.1–26.8 | 641 | 97 | 1.1 (0.8 to 1.5) | 1.1 (0.8 to 1.5) | 1.1 (0.8 to 1.5) |
| 26.9–30.0 | 638 | 119 | 1.5 (1.1 to 2.0) | 1.5 (1.1 to 2.0) | 1.3 (0.9 to 1.8) |
| >30.1 | 595 | 133 | 1.8 (1.3 to 2.4) | 1.8 (1.3 to 2.5) | 1.5 (1.1 to 2.1) |
OR, odds ratio; 95% CI, 95% confidence interval; ref, reference; R, right; BMI, body mass index.
Adjusted for age, sex, race, and site.
Further adjusted for diabetes mellitus, systolic blood pressure, hypertension meds, albumin-to-creatinine ratio, smoking, LDL cholesterol, HDL cholesterol, oral estrogen, prevalent coronary heart disease, prevalent heart failure, and C-reactive protein. Kidney function decline was defined as eGFR-cystatin C decline >30%.
Table 3.
Association of visceral fat area with kidney function decline stratified by baseline CKD
| Variable | N | ΔeGFR>30% | Unadjusted OR (95% CI) | Model 1a OR (95% CI) | Model 2b OR (95% CI) | Model 3c OR (95% CI) |
|---|---|---|---|---|---|---|
| Visceral fat (eGFR≥60 ml/min per 1.73 m2) | ||||||
| Continuous (per SD=121) | 2295 | 387 | 1.4 (1.2 to 1.5) | 1.4 (1.2 to 1.5) | 1.3 (1.1 to 1.4) | 1.3 (1.1 to 1.4) |
| Quartiles | ||||||
| <196 | 584 | 79 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 196–267 | 591 | 78 | 0.9 (0.7 to 1.3) | 1.0 (0.7 to 1.3) | 0.9 (0.6 to 1.3) | 0.9 (0.6 to 1.2) |
| 268–357 | 572 | 102 | 1.4 (1.0 to 1.9) | 1.4 (1.0 to 1.9) | 1.2 (0.9 to 1.7) | 1.2 (0.9 to 1.7) |
| >357 | 548 | 128 | 2.0 (1.4 to 2.7) | 2.0 (1.5 to 2.8) | 1.6 (1.2 to 2.2) | 1.6 (1.1 to 2.3) |
| Visceral fat (eGFR<60 ml/min per 1.73 m2) | ||||||
| Continuous (per SD=67) | 194 | 47 | 0.8 (0.6 to 1.2) | 0.9 (0.6 to 1.2) | 0.8 (0.5 to 1.2) | 0.7 (0.5 to 1.1) |
| Quartiles | ||||||
| <94 | 34 | 9 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 94–132 | 35 | 11 | 1.4 (0.5 to 4.0) | 1.7 (0.6 to 5.3) | 1.0 (0.8 to 12.0) | 2.8 (0.7 to 11.8) |
| 133–181 | 53 | 13 | 1.0 (0.4 to 2.8) | 1.3 (0.4 to 3.8) | 1.2 (0.5 to 5.9) | 1.4 (0.4 to 5.8) |
| >181 | 72 | 14 | 0.7 (0.2 to 1.8) | 0.8 (0.3 to 2.5) | 1.4 (0.2 to 3.2) | 0.6 (0.1 to 2.6) |
Kidney function decline defined as eGFR-cystatin C decline >30%. OR, odds ratio; 95% CI, 95% confidence interval; ref, reference.
Adjusted for age, sex, race, and site.
Further adjusted for diabetes mellitus, systolic blood pressure, hypertension meds, albumin-to-creatinine ratio.
Further adjusted smoking, LDL cholesterol, HDL cholesterol, oral estrogen, prevalent coronary heart disease and prevalent heart failure.
Table 4.
Association of measures of adiposity with kidney function decline using eGFRcr
| Variable | N | ΔeGFR-Cr>30% | Unadjusted OR (95% CI) | Model 1a OR (95% CI) | Model 2b OR (95% CI) |
|---|---|---|---|---|---|
| Subcutaneous fat | |||||
| Continuous (per SD=121) | 1219 | 339 | 1.2 (1.1 to 1.4) | 1.2 (1.0 to 1.4) | 1.1 (0.9 to 1.3) |
| Quartiles | |||||
| <196 | 295 | 72 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 196–267 | 301 | 71 | 1.0 (0.7 to 1.4) | 1.0 (0.7 to 14) | 0.9 (0.6 to 1.3) |
| 268–357 | 322 | 92 | 1.2 (0.9 to 1.8) | 1.2 (0.8 to 1.7) | 1.0 (0.7 to 1.5) |
| >357 | 301 | 104 | 1.6 (1. 1 to 2.3) | 1.5 (1.0 to 2. 2) | 1.2 (0.8 to 1.9) |
| Visceral fat | |||||
| Continuous (per SD=67) | 1219 | 339 | 1.2 (1.0 to 1.3) | 1.2 (1.2 to 1.4) | 1.1 (0.9 to 1.3) |
| Quartiles | |||||
| <94 | 296 | 69 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 94–132 | 312 | 82 | 1.2 (0.9 to 1.8) | 1.3 (0.9 to 1.9) | 1.2 (0.8 to 1.8) |
| 133–181 | 315 | 96 | 1.6 (1.1 to 2.2) | 1.3 (1.2 to 2.4) | 1.4 (1.0 to 2.1) |
| >181 | 296 | 93 | 1.7 (1.2 to 2.5) | 1.8 (1.2 to 2.7) | 1.4 (0.9 to 2.1) |
| R thigh intermuscular fat area, cm2 | |||||
| Continuous (per SD=6.8) | 1215 | 337 | 1.2 (1.0 to 1.4) | 1.1 (1.0 to 1.3) | 1.0 (0.9 to 1.2) |
| Quartiles | |||||
| <6.15 | 329 | 84 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 6.15–9.01 | 332 | 81 | 0.9 (0.7 to 1.3) | 0.9 (0.6 to 1.3) | 0.8 (0.6 to 1.2) |
| 9.02–13.12 | 297 | 96 | 1.4 (1.0 to 2.0) | 1.3 (0.3 to 1.9) | 1.1 (0.8 to 1.6) |
| >13.12 | 257 | 76 | 1.2 (0.8 to 1.7) | 1.1 (0.7 to 1.6) | 0.8 (0.6 to 1.3) |
| Waist circumference | |||||
| Continuous (per SD=12.5) | 1219 | 339 | 1.2 (1.1 to 1.4) | 1.2 (1.1 to 1.4) | 1.1 (1.0 to 1.3) |
| Quartiles | |||||
| <91.7 | 306 | 77 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 91.7–99.2 | 328 | 77 | 0.9 (0.7 to 1.4) | 1.0 (0.7 to 1.4) | 0.9 (0.6 to 1.4) |
| 99.3–107.1 | 311 | 93 | 1.3 (0.9 to 1.8) | 1.3 (0.9 to 1.9) | 1.2 (0.8 to 1.8) |
| >107.1 | 274 | 92 | 1.5 (1.2 to 2. 2) | 1.5 (1.0 to 2.2) | 1.2 (0.8 to 1.8) |
| BMI | |||||
| Continuous (per SD=4.6) | 1219 | 339 | 1.2 (1.1 to 1.4) | 1.2 (1.1 to 1.4) | 1.1 (0.9 to 1.3) |
| Quartiles | |||||
| <24.1 | 292 | 68 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 24.1–26.8 | 329 | 78 | 1.1 (0.7 to 1.6) | 1.2 (0.8 to 1.7) | 1.1 (0.7 to 1.6) |
| 26.9–30.0 | 324 | 97 | 1.5 (1.0 to 2.2) | 1.6 (1.2 to 2.4) | 1.5 (1.0 to 2.2) |
| >30.1 | 274 | 96 | 1.8 (1.2 to 2.6) | 1.9 (1.3 to 2.8) | 1.5 (1.0 to 2.3) |
OR, odds ratio; 95% CI, 95% confidence interval; ref, reference; R, right; BMI, body mass index.
Adjusted for age, sex, race, and site.
Further adjusted for diabetes mellitus, systolic blood pressure, hypertension meds, albumin-to-creatinine ratio, smoking, LDL cholesterol, HDL cholesterol, oral estrogen, prevalent coronary heart disease, prevalent heart failure, and C-reactive protein. Kidney function decline was defined as eGFR-Cr decline >30% (using creatinine at years 3 and 10).
Incident CKD.
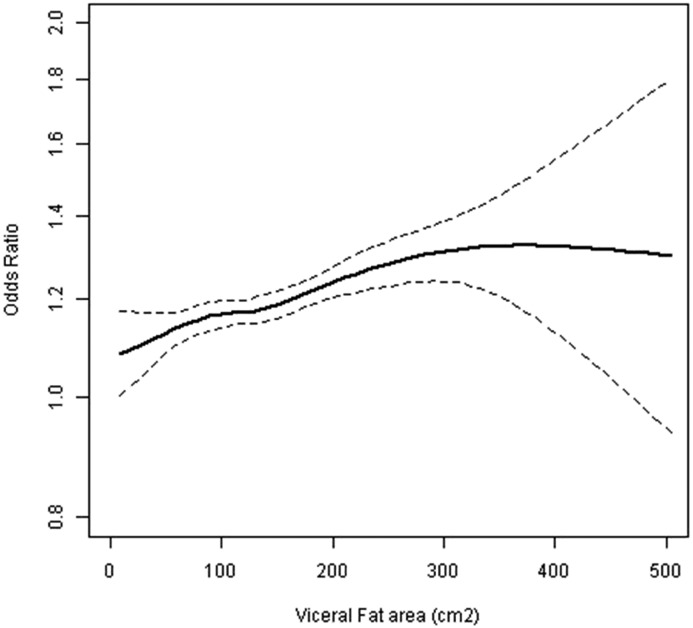
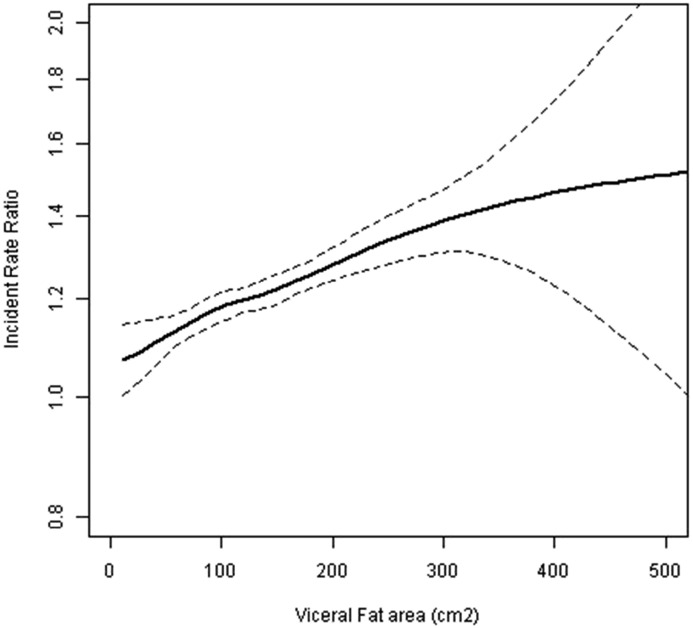
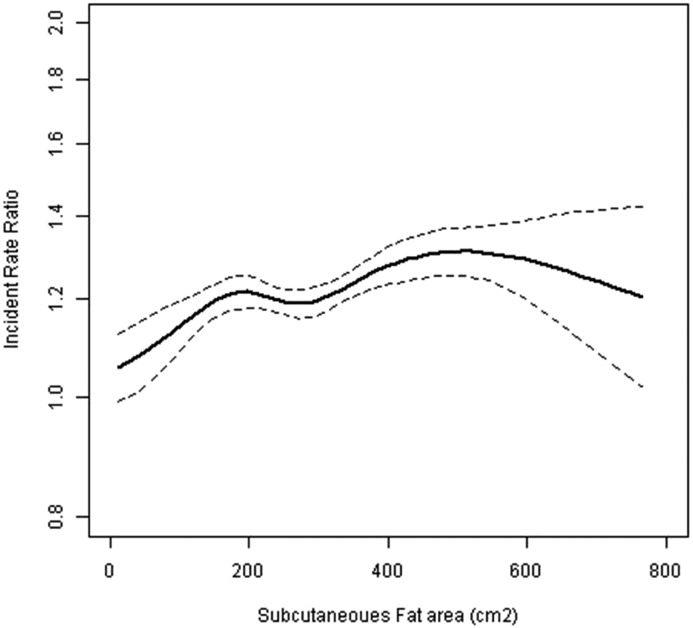
Incident CKD occurred in 17% of the population. Figures 2–4 show slope figures for VAT and SAT with incident CKD, demonstrating a more linear relationship between VAT and incident CKD. In continuous models, each SD higher SAT was associated with a significant risk for incident CKD, but this was no longer significant in the fully adjusted models. The highest quartile of SAT was associated with an increased risk for incident CKD that was also no longer significant in the fully adjusted models (Table 5). In continuous models, each SD higher VAT was associated with a significant risk for incident CKD in the univariate and fully adjusted models. The highest quartile of VAT was associated with a significant increased risk in the fully adjusted models (Table 5). In continuous models, each SD higher IMAT was associated with a significant risk for incident CKD in unadjusted models, but the association was no longer significant in the fully adjusted models. The highest quartile of IMAT was associated with a significant risk for incident CKD in the fully adjusted models (Table 5).
Figure 2.
Visceral adipose tissue and kidney function decline. Spline analyses (unadjusted).
Figure 4.
Visceral adipose tissue and incident kidney disease. Spline analyses (unadjusted).
Table 5.
Association of measures of adiposity with incident CKD
| Variable | N | Inc CKD | Rate (%/yr) | Unadjusted IRR (95% CI) | Model 1a IRR (95% CI) | Model 2b IRR (95% CI) |
|---|---|---|---|---|---|---|
| Subcutaneous fat | ||||||
| Continuous (per SD=121) | 2295 | 392 | 2.8 | 1.2 (1.1 to 1. 3) | 1.1 (1.0 to 1.3) | 1.1 (1.0 to 1.2) |
| Quartiles | ||||||
| <196 | 577 | 85 | 2.4 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 196–267 | 571 | 83 | 2.4 | 1.0 (0.7 to 1.3) | 0.9 (0.7 to 1.2) | 0.9 (0.7 to 1.2) |
| 268–357 | 593 | 107 | 2.9 | 1.2 (0.9 to 1.6) | 1.2 (0.9 to 1.6) | 1.1 (0.8 to 1.4) |
| >357 | 554 | 117 | 3.5 | 1.5 (1.1 to 1.9) | 1.3 (1.0 to 1.8) | 1.2 (0.9 to 1.6) |
| Visceral fat | ||||||
| Continuous (per SD=67) | 2295 | 392 | 2.8 | 1. 4 (1.3 to 1.5) | 1.2 (1.1 to 1.4) | 1.2 (1.1 to 1.3) |
| Quartiles | ||||||
| <94 | 584 | 65 | 1.8 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 94–132 | 591 | 89 | 2.3 | 1.3 (1.0 to 1.8) | 1.2 (0.8 to 1.5) | 1.1 (0.8 to 1.4) |
| 133–181 | 572 | 103 | 2.9 | 1.6 (1.2 to 2.2) | 1.2 (0.9 to 1.7) | 1.2 (0.9 to 1.5) |
| >181 | 548 | 135 | 4.2 | 2.3 (1.7 to 3.1) | 1.6 (1.1 to 2.2) | 1.5 (1.1 to 2.0) |
| R thigh intermuscular fat area, cm2 | ||||||
| Continuous (per SD=6.8) | 2288 | 388 | 2.8 | 1.2 (1.1 to 1.3) | 1.1 (1.1 to 1.3) | 1.1 (1.0 to 1.2) |
| Quartiles | ||||||
| <6.15 | 599 | 69 | 1.8 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 6.15–9.01 | 605 | 95 | 2.5 | 1.4 (1.0 to 1.9) | 1.2 (0.9 to 1.6) | 1.2 (0.9 to 1.6) |
| 9.02–13.12 | 567 | 117 | 3.4 | 1.9 (1.4 to 2.5) | 1.5 (1.1 to 1.9) | 1.4 (1.1 to 1.9) |
| >13.12 | 517 | 107 | 3.6 | 2.0 (1.5 to 2.7) | 1.5 (1.1 to 2.0) | 1.4 (1.1 to 1.9) |
| Waist circumference | ||||||
| Continuous (per SD=12.5) | 2294 | 392 | 2.8 | 1.3 (1.2 to 1.4) | 1.2 (1.1 to 1.3) | 1.2 (1.1 to 1.3) |
| Quartiles | ||||||
| <91.7 | 582 | 69 | 1.9 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 91.7–99.2 | 597 | 89 | 2.4 | 1.3 (0.9 to 1.7) | 1.2 (0.9 to 1.7) | 1.2 (0.9 to 1.6) |
| 99.3–107.1 | 586 | 110 | 3.1 | 1.6 (1.2 to 2.2) | 1.3 (1.0 to 1.7) | 1.2 (0.9 to 1.7) |
| >107.1 | 529 | 124 | 4.0 | 2.1 (1.6 to 2.8) | 1.6 (1.2 to 2.1) | 1.4 (1.1 to 1.9) |
| BMI | ||||||
| Continuous (per SD=4.6) | 2295 | 392 | 2.8 | 1.2 (1.2 to 1.4) | 1.2 (1.1 to 1.3) | 1.2 (1.0 to 1.3) |
| Quartiles | ||||||
| <24.1 | 575 | 71 | 2.0 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 24.1–26.8 | 607 | 91 | 2.4 | 1.2 (0.9 to 1.6) | 1.1 (0.8 to 1.5) | 1.1 (0.8 to 1.4) |
| 26.9–30.0 | 580 | 102 | 2.8 | 1.4 (1.1 to 1.9) | 1.1 (0.9 to 1.5) | 1.1 (0.8 to 1.5) |
| >30.1 | 533 | 128 | 4.1 | 2.0 (1.5 to 2.7) | 1.6 (1.2 to 2.1) | 1.4 (1.1 to 1.9) |
Incident CKD was defined as a follow-up eGFRcysC≤60 ml/min per 1.73 m2 in individuals with baseline GFR>60 ml/min per 1.73 m2. Inc, incident; IRR, incident rate ratio; 95% CI, 95% confidence interval; ref, reference; R, right; BMI, body mass index.
Adjusted for age, sex, race, site, and baseline eGFR.
Further adjusted for diabetes mellitus, systolic blood pressure, hypertension meds, albumin-to-creatinine ratio, smoking, LDL cholesterol, HDL cholesterol, oral estrogen, prevalent coronary heart disease, and prevalent heart failure.
Figure 3.
Subcutaneous adipose tissue and incident kidney disease. Spline analyses (unadjusted).
In continuous models, each SD higher BMI was associated with an increased risk for incident CKD in univariate and fully adjusted models. Likewise, in continuous models each SD higher WC was also associated with incident CKD in univariate and fully adjusted models. Higher quartiles of both BMI and WC were also associated with incident CKD (Table 5). Analyses were repeated using creatinine eGFR at years 3 and 10. None of the exposure variables were associated with incident CKD in the fully adjusted models (Table 6).
Table 6.
Association of measures of adiposity with incident CKD using eGFRcr
| Variable | N | Inc CKD | Rate (%/yr) | Unadjusted IRR (95% CI) | Model 1a IRR (95% CI) | Model 2b IRR (95% CI) |
|---|---|---|---|---|---|---|
| Subcutaneous fat | ||||||
| Continuous (per SD=121) | 1055 | 416 | 5.7 | 1.1 (1.0 to 1.1) | 1.0 (0.9 to 1.1) | 0.9 (0.9 to 1.0) |
| Quartiles | ||||||
| <196 | 260 | 101 | 5.6 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 196–267 | 259 | 90 | 5.0 | 0.9 (0.7 to 1.1) | 0.9 (0.7 to 1.1) | 0.8 (0.7 to 1.0) |
| 268–357 | 279 | 117 | 6.1 | 1.1 (0.9 to 1.3) | 1.0 (0.8 to 1.2) | 0.9 (0.8 to 1.2) |
| >357 | 257 | 108 | 6.1 | 1.1 (0.9 to 1.3) | 0.9 (0.7 to 1.2) | 0.9 (0.7 to 1.1) |
| Visceral fat | ||||||
| Continuous (per SD=67) | 1055 | 416 | 5.7 | 1.1 (1.0 to 1.2) | 1.0 (1.0 to 1.1) | 1.0 (0.9 to 1.1) |
| Quartiles | ||||||
| <94 | 270 | 90 | 4.8 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 94–132 | 275 | 113 | 5.9 | 1.2 (1.0 to 1.5) | 1.2 (1.0 to 1.5) | 1.2 (1.0 to 1.5) |
| 133–181 | 263 | 103 | 5.7 | 1.2 (0.9 to 1.5) | 1.1 (0.9 to 1.4) | 1.1 (0.9 to 1.3) |
| >181 | 247 | 110 | 6.4 | 1.3 (1.1 to 1.7) | 1.2 (0.9 to 1.5) | 1.1 (0.9 to 1.4) |
| R thigh intermuscular fat area (cm2) | ||||||
| Continuous (per SD=6.8) | 1052 | 415 | 5.7 | 1.1 (1.0 to 1.1) | 1.0 (0.9 to 1.1) | 1.0 (0.9 to 1.1) |
| Quartiles | ||||||
| <6.15 | 294 | 113 | 5.6 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 6.15–9.01 | 292 | 100 | 4.9 | 0.9 (0.7 to 1.1) | 0.9 (0.7 to 1.1) | 0.8 (0.7 to 1.0) |
| 9.02–13.12 | 245 | 116 | 6.8 | 1.2 (1.0 to 1.5) | 1.1 (0.9 to 1.3) | 1.1 (0.9 to 1.3) |
| >13.12 | 221 | 86 | 5.6 | 1.0 (0.8 to 13) | 0.9 (0.7 to 1.1) | 0.9 (0.7 to 1.1) |
| Waist circumference | ||||||
| Continuous (per SD=12.5) | 1055 | 416 | 5.7 | 1.0 (1.0 to 1.1) | 1.0 (0.9 to 1.1) | 1.0 (0.9 to 1.1) |
| Quartiles | ||||||
| <91.7 | 283 | 116 | 5.9 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 91.7–99.2 | 274 | 90 | 4.7 | 0.8 (0.6 to 1.0) | 0.8 (0.6 to 1.0) | 0.8 (0.6 to 1.0) |
| 99.3–107.1 | 263 | 108 | 5.9 | 1.0 (0.8 to 1.2) | 1.0 (0.8 to 1.2) | 0.9 (0.8 to 1.1) |
| >107.1 | 235 | 105 | 6.3 | 1.1 (0.9 to 1.3) | 0.9 (0.8 to 1.2) | 0.9 (0.7 to 1.1) |
| BMI | ||||||
| Continuous (per SD=4.6) | 1055 | 416 | 5.7 | 1.0 (1.0 to 1.1) | 1.0 (0.9 to 1.1) | 1.0 (0.9 to 1.1) |
| Quartiles | ||||||
| <24.1 | 269 | 93 | 5.0 | 1.0 (ref) | 1.0 (ref) | 1.0 (ref) |
| 24.1–26.8 | 281 | 114 | 5.8 | 1.2 (0.9 to 1.5) | 1.2 (1.0 to 1.5) | 1.2 (1.0 to 1.5) |
| 26.9–30.0 | 269 | 106 | 5.7 | 1.1 (0.9 to 1.4) | 1.1 (0.9 to 1.4) | 1.2 (0.9 to 1.4) |
| >30.1 | 236 | 103 | 6.3 | 1.3 (1.0 to 1.6) | 1.2 (1.0 to 1.5) | 1.2 (0.9 to 1.5) |
Incident CKD defined as eGFR-Cr<60 ml/min per 1.73 m2 at visit 10 and ΔeGFR-Cr>1ml/min per year among those with eGFR-Cr≥60 ml/min per 1.73 m2 at visit 3. Inc, incident; IRR, incident rate ratio; 95% CI, 95% confidence interval; ref, reference; R, right; BMI, body mass index.
Adjusted for age, sex, race, site and baseline eGFR.
Further adjusted for diabetes mellitus, systolic blood pressure, hypertension meds, albumin-to-creatinine ratio, smoking, LDL cholesterol, HDL cholesterol, oral estrogen, prevalent coronary heart disease, and prevalent heart failure.
Sensitivity Analyses.
There was no association between SAT and VAT with KF decline when eGFR was modeled as a continuous variable. In addition, there was no interaction between any measures of obesity with sex and race (Supplemental Table 1). When analyses were adjusted for BMI, only VAT (per SD) remained a significant risk factor for incident CKD in continuous models (incident rate ratio, 1.9; 95% confidence interval, 1.0 to 1.3). None of the other exposure variables were associated with incident CKD or KF decline (defined as eGFRcysC>30%) after adjustment for BMI. In addition, we assessed for independent associations among the exposure measures by including them in the same model. For the outcome of KF decline, none of the variables in the combined models were associated with outcomes. For the outcome of incident CKD, only VAT remained an independent risk factor for incident CKD (Supplemental Tables 2 and 3). When defining KF decline as eGFRcysC>40% decline, neither SAT nor VAT were associated with KF decline in continuous or categoric models (Supplemental Table 4). Obesity, defined by the WHO as ≥30 kg/m2, was associated with KF decline and incident CKD (Supplemental Tables 5 and 6).
Discussion
In Health ABC, a cohort of initially well functioning older persons with predominantly normal baseline KF, VAT, WC, IMAT, and BMI were all associated with incident CKD and KF decline when eGFR was defined as eGFRcysC>30%. SAT was associated with KF decline only in continuous models, but was not associated with incident CKD. None of the measures of adiposity were associated with kidney outcomes when eGFR was estimated using creatinine. Our results are consistent with observational studies that have demonstrated that central obesity, assessed by WC or WHR, is associated with incident CKD (9,25,26). However, we also observed that anthropometric measures of general adiposity such as BMI provide a similar risk assessment compared with direct measures. In addition, IMAT, an ectopic fat depot within leg muscles (27), was also associated with kidney outcomes.
The potential mechanisms as to why VAT and IMAT confer a higher risk for incident CKD than SAT may relate to their anatomic location. Adipose tissue stored in ectopic locations outside of the subcutaneous tissue such as in the muscle, liver, and abdominal cavity is linked with chronic inflammation, IGT, increased total cholesterol, and decreased strength and mobility in older adults (27). VAT is associated with release of proinflammatory markers (28) and insulin resistance has been associated with structural changes in the kidney such as mesangial expansion and increased renal fibrosis (29,30). In addition, VAT may confer hemodynamic effects on the kidney such as higher filtration fraction and as a result increased glomerular capillary pressure (31). Likewise, IMAT is associated with negative outcomes in the older population (27). In addition to the negative metabolic effects, IMAT is also associated with muscle weakness and decreased mobility function, also prevalent in patients with CKD. WC reflects VAT and therefore we hypothesized that VAT would provide at least an equal measure of risk compared with WC for kidney outcomes, and a better measure of risk assessment than SAT and BMI. In our study, BMI, however, had similar risk associations to VAT. This may be due to the fact that BMI combines measures of SAT and VAT and the VAT component may be predominant. The analyses demonstrating an association of VAT with incident CKD independent of BMI were consistent with this hypothesis. Our results demonstrated that CT measures of visceral adiposity do not appear superior to the conventional anthropometric measures of visceral adiposity such as WC for kidney prognosis assessment. Our findings are reassuring that, at least for kidney prognosis, direct measures of visceral fat are not warranted.
We also noted that visceral adiposity was a risk factor for KF decline only in those subjects without baseline CKD. These results are in agreement with others where, in those subjects with CKD, obesity is no longer a risk factor for CKD progression (25,32,33). These findings may be the consequence of the presence of other powerful competing risk factors for CKD progression such as hypertension, diabetes, and proteinuria in those with CKD.
Our study has several strengths. This is the only study of which we are aware to assess the risk of kidney outcomes with direct measures of adiposity. This is especially important in the older population where muscle wasting is prevalent and where anthropometric measures may not be as good as direct measures of adiposity. In addition, Health ABC has detailed assessments of risk factors and outcomes, long-term follow-up, and a large sample of older adults that are at higher risk for kidney outcomes. Our study also has some limitations. First, we were not able to asses WHR because direct hip measurements were not performed in Health ABC. Second, albuminuria, an important marker of kidney disease, was not measured during follow-up in Health ABC and we cannot determine whether measures of fat are associated with change in albumin excretion. Third, our primary results are on the basis of cystatin C because baseline creatinine has not been isotope dilution mass spectrometry-calibrated in Health ABC. We attempted to address this by repeating the creatinine analyses using only the years 3 and 10 data. We believe the differences in results on the basis of eGFRcysC versus eGFRcr may be due to the fact that the exposure variable was not assessed at the same time as the baseline creatinine, and creatinine was assessed at only two time points with the eGFRcr analyses. We acknowledge, however, that we cannot rule out the possibility that factors other than eGFR, such as inflammation and obesity, may affect cystatin C levels and the eGFRcr data are more accurate (34). In addition, when defining KF decline as eGFRcysC>40% decline, neither SAT nor VAT were associated with KF decline in either continuous or categoric models. Although this may be related to fewer events, it is also possible that there is no true association with the >40% decline. Finally, our results may not be generalizable to younger populations.
In conclusion, we found that VAT, IMAT, BMI, and WC are all associated with incident CKD and KF decline when using eGFRcysC>30%. SAT, however, was not associated with incident CKD. Anthropometric measures of body fat appear to provide as consistent estimates of KF decline risk as CT measures in elders.
Disclosures
None.
Supplementary Material
Acknowledgments
This research was supported in part by the Intramural Research Program of the National Institutes of Health and the National Institute on Aging (NIA) Contracts N01-AG-6-2101, N01-AG-6-2103, N01-AG-6-2106, NIA grant R01-AG028050, and National Institute of Nursing Research grant R01-NR012459, and has been approved for submission by the NIA. M. Shlipak, M. Sarnak, J.I., and R.K. were supported by NIA grant 5R01AG027002-07. M.M. was supported by CONACYT grant SS113960. The study sponsors had no role in study design; collection, analysis, and interpretation of the data; writing the report; and the decision to submit the report for publication.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.07010716/-/DCSupplemental.
References
- 1.Levey AS, Atkins R, Coresh J, Cohen EP, Collins AJ, Eckardt KU, Nahas ME, Jaber BL, Jadoul M, Levin A, Powe NR, Rossert J, Wheeler DC, Lameire N, Eknoyan G: Chronic kidney disease as a global public health problem: Approaches and initiatives - a position statement from Kidney Disease Improving Global Outcomes. Kidney Int 72: 247–259, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Kramer H, Cao G, Dugas L, Luke A, Cooper R, Durazo-Arvizu R: Increasing BMI and waist circumference and prevalence of obesity among adults with type 2 diabetes: The National Health and Nutrition Examination Surveys. J Diabetes Complications 24: 368–374, 2010 [DOI] [PubMed] [Google Scholar]
- 3.Hall JE, Kuo JJ, da Silva AA, de Paula RB, Liu J, Tallam L: Obesity-associated hypertension and kidney disease. Curr Opin Nephrol Hypertens 12: 195–200, 2003 [DOI] [PubMed] [Google Scholar]
- 4.Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC: Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care 17: 961–969, 1994 [DOI] [PubMed] [Google Scholar]
- 5.Kramer H: Obesity and chronic kidney disease. Contrib Nephrol 151: 1–18, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Kramer HJ, Saranathan A, Luke A, Durazo-Arvizu RA, Guichan C, Hou S, Cooper R: Increasing body mass index and obesity in the incident ESRD population. J Am Soc Nephrol 17: 1453–1459, 2006 [DOI] [PubMed] [Google Scholar]
- 7.Iseki K, Ikemiya Y, Kinjo K, Inoue T, Iseki C, Takishita S: Body mass index and the risk of development of end-stage renal disease in a screened cohort. Kidney Int 65: 1870–1876, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Vivante A, Golan E, Tzur D, Leiba A, Tirosh A, Skorecki K, Calderon-Margalit R: Body mass index in 1.2 million adolescents and risk for end-stage renal disease. Arch Intern Med 172: 1644–1650, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elsayed EF, Sarnak MJ, Tighiouart H, Griffith JL, Kurth T, Salem DN, Levey AS, Weiner DE: Waist-to-hip ratio, body mass index, and subsequent kidney disease and death. Am J Kidney Dis 52: 29–38, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsu CY, McCulloch CE, Iribarren C, Darbinian J, Go AS: Body mass index and risk for end-stage renal disease. Ann Intern Med 144: 21–28, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Elsayed EF, Tighiouart H, Weiner DE, Griffith J, Salem D, Levey AS, Sarnak MJ: Waist-to-hip ratio and body mass index as risk factors for cardiovascular events in CKD. Am J Kidney Dis 52: 49–57, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mak RH, Ikizler AT, Kovesdy CP, Raj DS, Stenvinkel P, Kalantar-Zadeh K: Wasting in chronic kidney disease. J Cachexia Sarcopenia Muscle 2: 9–25, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Srikanthan P, Seeman TE, Karlamangla AS: Waist-hip-ratio as a predictor of all-cause mortality in high-functioning older adults. Ann Epidemiol 19: 724–731, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oh H, Quan SA, Jeong JY, Jang SN, Lee JE, Kim DH: Waist circumference, not body mass index, is associated with renal function decline in korean population: Hallym aging study. PLoS One 8: e59071, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wajchenberg BL: Subcutaneous and visceral adipose tissue: Their relation to the metabolic syndrome. Endocr Rev 21: 697–738, 2000 [DOI] [PubMed] [Google Scholar]
- 16.Goodpaster BH, Krishnaswami S, Harris TB, Katsiaras A, Kritchevsky SB, Simonsick EM, Nevitt M, Holvoet P, Newman AB: Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch Intern Med 165: 777–783, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Vega GL, Adams-Huet B, Peshock R, Willett D, Shah B, Grundy SM: Influence of body fat content and distribution on variation in metabolic risk. J Clin Endocrinol Metab 91: 4459–4466, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Jensen MD, Kanaley JA, Reed JE, Sheedy PF: Measurement of abdominal and visceral fat with computed tomography and dual-energy x-ray absorptiometry. Am J Clin Nutr 61: 274–278, 1995 [DOI] [PubMed] [Google Scholar]
- 19.Sutton-Tyrrell K, Newman A, Simonsick EM, Havlik R, Pahor M, Lakatta E, Spurgeon H, Vaitkevicius P: Aortic stiffness is associated with visceral adiposity in older adults enrolled in the study of health, aging, and body composition. Hypertension 38: 429–433, 2001 [DOI] [PubMed] [Google Scholar]
- 20.Inker LA, Schmid CH, Tighiouart H, Eckfeldt JH, Feldman HI, Greene T, Kusek JW, Manzi J, Van Lente F, Zhang YL, Coresh J, Levey AS; CKD-EPI Investigators : Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med 367: 20–29, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levey AS, Inker LA, Matsushita K, Greene T, Willis K, Lewis E, de Zeeuw D, Cheung AK, Coresh J: GFR decline as an end point for clinical trials in CKD: A scientific workshop sponsored by the National Kidney Foundation and the US Food and Drug Administration. Am J Kidney Dis 64: 821–835, 2014 [DOI] [PubMed] [Google Scholar]
- 22.Finney H, Newman DJ, Price CP: Adult reference ranges for serum cystatin C, creatinine and predicted creatinine clearance. Ann Clin Biochem 37: 49–59, 2000 [DOI] [PubMed] [Google Scholar]
- 23.Sarnak MJ, Katz R, Stehman-Breen CO, Fried LF, Jenny NS, Psaty BM, Newman AB, Siscovick D, Shlipak MG; Cardiovascular Health Study : Cystatin C concentration as a risk factor for heart failure in older adults. Ann Intern Med 142: 497–505, 2005 [DOI] [PubMed] [Google Scholar]
- 24.Shlipak MG, Katz R, Fried LF, Jenny NS, Stehman-Breen CO, Newman AB, Siscovick D, Psaty BM, Sarnak MJ: Cystatin-C and mortality in elderly persons with heart failure. J Am Coll Cardiol 45: 268–271, 2005 [DOI] [PubMed] [Google Scholar]
- 25.Franceschini N, Gouskova NA, Reiner AP, Bostom A, Howard BV, Pettinger M, Umans JG, Brookhart MA, Winkelmayer WC, Eaton CB, Heiss G, Fine JP: Adiposity patterns and the risk for ESRD in postmenopausal women. Clin J Am Soc Nephrol 10: 241–250, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Noori N, Hosseinpanah F, Nasiri AA, Azizi F: Comparison of overall obesity and abdominal adiposity in predicting chronic kidney disease incidence among adults. J Ren Nutr 19(3): 228–237, 2009 [DOI] [PubMed] [Google Scholar]
- 27.Addison O, Marcus RL, Lastayo PC, Ryan AS: Intermuscular fat: A review of the consequences and causes. Int J Endocrinol 2014: 309570, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grundy SM: Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab 89: 2595–2600, 2004 [DOI] [PubMed] [Google Scholar]
- 29.Bagby SP: Obesity-initiated metabolic syndrome and the kidney: A recipe for chronic kidney disease? J Am Soc Nephrol 15: 2775–2791, 2004 [DOI] [PubMed] [Google Scholar]
- 30.Anderson PW, Zhang XY, Tian J, Correale JD, Xi XP, Yang D, Graf K, Law RE, Hsueh WA: Insulin and angiotensin II are additive in stimulating TGF-beta 1 and matrix mRNAs in mesangial cells. Kidney Int 50: 745–753, 1996 [DOI] [PubMed] [Google Scholar]
- 31.Ribstein J, du Cailar G, Mimran A: Combined renal effects of overweight and hypertension. Hypertension 26: 610–615, 1995 [DOI] [PubMed] [Google Scholar]
- 32.Brown RN, Mohsen A, Green D, Hoefield RA, Summers LK, Middleton RJ, O’Donoghue DJ, Kalra PA, New DI: Body mass index has no effect on rate of progression of chronic kidney disease in non-diabetic subjects. Nephrol Dial Transplant 27: 2776–2780, 2012 [DOI] [PubMed] [Google Scholar]
- 33.Muntner P, Judd SE, Gao L, Gutiérrez OM, Rizk DV, McClellan W, Cushman M, Warnock DG: Cardiovascular risk factors in CKD associate with both ESRD and mortality. J Am Soc Nephrol 24: 1159–1165, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Knight EL, Verhave JC, Spiegelman D, Hillege HL, de Zeeuw D, Curhan GC, de Jong PE: Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement. Kidney Int 65: 1416–1421, 2004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.