Summary
Beta-cell replacement therapy is an effective means to restore glucose homeostasis in select humans with autoimmune diabetes. The scarcity of “healthy” human donor pancreata restricts the broader application of this effective curative therapy. “β-Like” cells derived from human embryonic stem cells (hESC), with the capacity to secrete insulin in a glucose-regulated manner, have been developed in vitro, with limitless capacity for expansion. Here we report long-term diabetes correction in mice transplanted with hESC-derived pancreatic endoderm cells (PECs) in a prevascularized subcutaneous site. This advancement mitigates chronic foreign-body response, utilizes a device- and growth factor-free approach, facilitates in vivo differentiation of PECs into glucose-responsive insulin-producing cells, and reliably restores glycemic control. Basal and stimulated human C-peptide secretion was detected throughout the study, which was abolished upon graft removal. Recipient mice demonstrated physiological clearance of glucose in response to metabolic challenge and safely retrieved grafts contained viable glucose regulatory cells.
Keywords: pancreatic endoderm cells, human pluripotent stem cells, diabetes, subcutaneous, prevascularized, cellular transplantation
Highlights
-
•
hESC-derived PECs in a prevascularized device-less site routinely reverse diabetes
-
•
Device-less PEC grafts functioned better than fat pad and subcutaneous PEC grafts
-
•
Human C-peptide secretion was glucose regulated in device-less PEC grafts
-
•
Safely retrieved grafts stained positive for insulin, glucagon, and somatostatin
Islet transplantation is limited to a small subset of patients due to the scarcity of human donors. Here, Shapiro and colleagues demonstrate that a potentially unlimited source of insulin-producing cells, hESC-pancreatic endoderm cells, can survive and differentiate into glucose-responsive insulin-producing cells which restore long-term glycemic control to diabetic mice upon transplantation into a safely retrievable subcutaneous (device-less) prevascularized site.
Introduction
The therapeutic use of insulin prevents an acute death sentence associated with untreated type 1 diabetes (T1D). While life sustaining, exogenous insulin replacement imprecisely mimics the dynamic oscillation in glycemic regulation achieved by native pancreatic islets of Langerhans (Bruin et al., 2015b). As such, patients are susceptible to long-term, debilitating vascular complications and, for some, are at an increased risk of life-threatening hypoglycemia (McCall, 2012).
Aside from pharmacological intervention, whole pancreas or islet cell transplantation represents an effective therapeutic strategy to restore physiologic glycemic control. Both modalities have become established as an efficacious means to achieve normoglycemia, prevent hypoglycemia, and potentially protect against vascular complications of T1D (Barton et al., 2012, Choudhary et al., 2015, Gruessner and Gruessner, 2013, Thompson et al., 2011). Despite marked progress in clinical islet transplantation with the achievement and maintenance of insulin independence in over half of recipients up to 5 years (Shapiro and Ricordi, 2014), transplant approaches are limited to those with life-threatening hypoglycemic unawareness or severe glucose lability (Shapiro et al., 2000). Furthermore, this approach remains restricted due to the scarcity of human pancreas donors. In light of recent progress in the field of stem cell biology with recapitulation of native pancreas embryonic development, the potential to expand new β cells has become a clinical reality, and the possibility of replacing human pancreatic islet donors with human embryonic stem cell (hESC)- or induced pluripotent stem cell (PSC)-derived insulin-producing products is within potential reach. Various degrees of pretransplant differentiation (Bruin et al., 2013, D'Amour et al., 2006, Kroon et al., 2008, Pagliuca et al., 2014, Rezania et al., 2012, Rezania et al., 2014) and diverse transplant modalities (Bruin et al., 2013, Kroon et al., 2008, Rezania et al., 2014, Vegas et al., 2016) are being explored in the laboratory. However, translation to clinical investigation, especially immune-isolating approaches, has been limited by host immune response to foreign materials (Tuch et al., 2009). Advancements in biomaterial chemistry have led to promising strategies to minimize the hosts' response to microencapsulation therapeutic cells in mice (Vegas et al., 2016).
Several approaches have been developed to differentiate hESCs into pancreatic progenitor cells (minimum of stage 4 [S4] of differentiation), which undertake the final stages of glucose-responsive β-cell differentiation in vivo (Bruin et al., 2013, D'Amour et al., 2006, Kelly et al., 2011, Kroon et al., 2008, Rezania et al., 2012, Schulz et al., 2012). Furthermore, advancements in the manufacture of pancreatic endoderm cells (PECs) for clinical trials (Schulz, 2015) and the generation of insulin-producing cells of increased maturity (>S5) derived from hESCs or induced PSCs in vitro, with capacity to restore normoglycemia rapidly compared with early progenitor cells, have been recently reported (Pagliuca et al., 2014, Rezania et al., 2014). As a means to minimize potential recipient risk in early clinical trials, the transplant site for hESC-derived cell-based therapies should ideally exploit an approach that is both retrievable but provides structural and vascular support (Stock and German, 2016).
In 2014, the US Food and Drug Administration and Health Canada granted ViaCyte Inc., a commercial leader in regenerative medicine technologies, permission to initiate the first-in-human pilot phase 1/2 clinical trial to test their VC-01 combination product in a small cohort of patients with T1D. This product combines CyT49 hESC-derived PECs (S4) contained within a macroencapsulated potentially immune protective device, transplanted subcutaneously (NCT02239354). It is hoped that early pilot results of this ongoing trial will help to direct future progression of the field. Ongoing development of extrahepatic sites for stem cell-derived product implantation will likely require further optimization to improve engraftment, oxygen delivery, and metabolic exchange.
In the present study we examined the potential of transplanting S4 CyT49 hESC-derived PECs within a prevascularized subcutaneous device-less (DL) site. In brief, this site transforms the inhospitable subcutaneous tissue into a viable and vascularized engraftment location through the temporary implantation of an angiocatheter. The foreign-body reaction to the in situ catheter culminates in a cloaking of the catheter in a vascularized collagen scaffold into which the cellular graft is infused, while the simultaneous catheter withdrawal extinguishes this reaction. We have previously demonstrated that this site is efficacious in reversing diabetes post transplant of both human and rodent islets, even in models of aggressive foreign-body reaction and alloimmunity (Pepper et al., 2015, Shapiro, 2016a, Shapiro, 2016b). Herein, we further evaluated the potential of hESC-derived PECs to differentiate in vivo and restore chemically induced diabetes following implant.
Results
Stage 4 Pancreatic Endoderm Cells Are Metabolically Naive Compared with Human Islets Prior to Transplant
Prior to transplantation into the DL site (Figure 1A), we sought to characterize the functional and physiological proficiency of the in vitro generated PECs, which express NKX6-1, PTF1A, NGN3, and NKX2-2 (Kroon et al., 2008; Figure 1B), relative to human islets. We assessed mitochondrial and respiratory capacity of both cell types by assessing their ability to consume oxygen, which has been previously shown to be an effective indicator of in vitro human islet function, as well as a predictive indicator of their subsequent post-transplant ability to reverse diabetes (Papas et al., 2007, Pepper et al., 2012). PECs demonstrated significantly lower oxygen consumption rates (OCR) compared with human islets (PECs: 129.1 ± 4.8 nmol/min mg DNA, n = 6, versus human islets: 226.3 ± 9.2 nmol/min mg DNA, n = 6, p < 0.001, unpaired two-tailed t test) (Figure 2A).
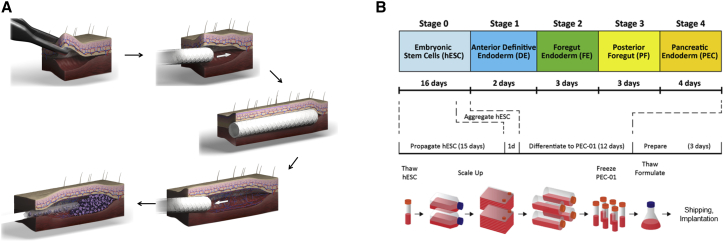
Figure 1.
Transplantation of hESC-Derived Pancreatic Endoderm Cells
(A) Summary and characteristics of the subcutaneous DL cellular transplant site.
(B) Overview of the four-stage in vitro differentiation protocol including key growth factors and small molecules that were supplemented at each stage.
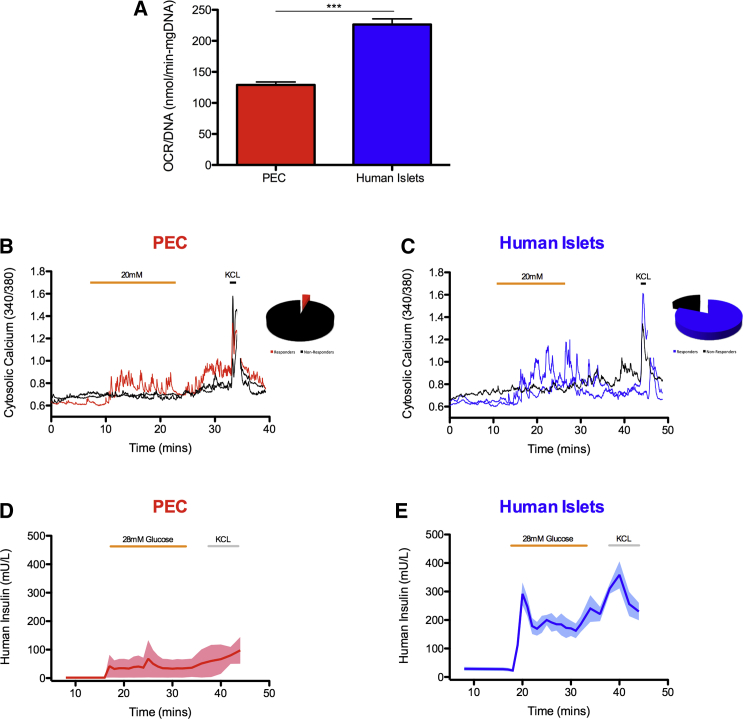
Figure 2.
Stage 4 Pancreatic Endoderm Cells Have Naive Functional Capacity Compared with Adult Human Islets
(A) Oxygen consumption rates of both PECs (n = 6 replicates, 10-μL cell samples per replicate) and human islets (n = 6 replicates, 500 islet samples per replicate) were assayed prior to transplantation. Data are presented as mean ± SEM. ∗∗∗p < 0.001, unpaired two-tailed t test.
(B and C) Representative examples of intracellular calcium signaling traces from (B) S4 PECs (red, left) and (C) human β cells (blue, right). Basal glucose was always 3 mM prior to and after exposure to 20 mM glucose. KCl (30 mM) was included at the end of each experiment. Inset depicts the proportion of responding (red for PECs and blue for human islets) and non-responding (black) cells. Black lines represent non-responsive PECs and human islets.
(D and E) In vitro secretion of human insulin from (D) S4 PECs (red, left; n = 6 replicates, 10-μL cell samples per replicate from two batches) and (E) human islets (blue, right; n = 6 replicates, 50 islets samples per replicate) during a glucose perifusion assay. The system exposes cell preparation to low glucose (2.8 mM), high glucose (28 mM), low glucose, and KCl (30 mM). Data are presented as mean ± SEM.
As such, prior to transplant we assayed the intracellular calcium concentration ([Ca2+]i) responses of S4 PECs to glucose. Despite the immature nature of these cell populations, a modest intracellular Ca2+ flux in response to high glucose (20 mM) and rapid direct depolarization with KCl (70 mM) was observed. However, this sensing was restricted to a small subset of the entire PEC population (4.5%: 2/44) (Figure 2B), mirroring the irregular profiles documented with more differentiated S7 human PSC (hPSC) progeny (Rezania et al., 2014). In contrast, nearly all primary human β cells (islets) (81.2%: 13/16) presented an intracellular Ca2+ flux in response to glucose (Figure 2C).
We sought to quantify the glucose-stimulated insulin-secreting capability of S4 PECs before transplantation through a dynamic perifusion assay. Emulating the Ca2+ flux data, S4 PECs displayed a modest response to an incremental increase in glucose perifusion (2.6–28 mM) compared with primary β cells (Figure 2D). Furthermore, exposure to KCl evoked a blunted insulin secretory response. In juxtaposition, human islets rapidly secreted insulin in response to high glucose exposure, while depolarization with KCl resulted in prompt insulin liberation as biologically expected (Figure 2E).
PECs Reverse Diabetes Post Transplant into the Subcutaneous DL Site
We examined the efficacy of PECs to differentiate in vivo and to subsequently restore glucose homeostasis post transplant into diabetic immunodeficient B6/Rag−/− mice. PECs were shipped overnight from ViaCyte and mice were randomly distributed into three different transplant groups: (1) epididymal fat pad (FP), (2) subcutaneous alone (SC), or (3) DL. Transplanted PECs were able to reverse diabetes in 33% (2/6) of the mice recipients in both FP and SC groups, with a mean time to euglycemia of 110.5 ± 10.5 and 116.0 ± 19.0 days post transplant, respectively (Figure 3A). In contrast, in the DL group, 100% of the mice (22/22) transplanted with PECs became normoglycemic within 99.8 ± 3.8 days, which translated a significantly higher rate in euglycemia compared with both FP and SC recipients (p < 0.01, p < 0.01 respectively, log rank) (Figure 3A).
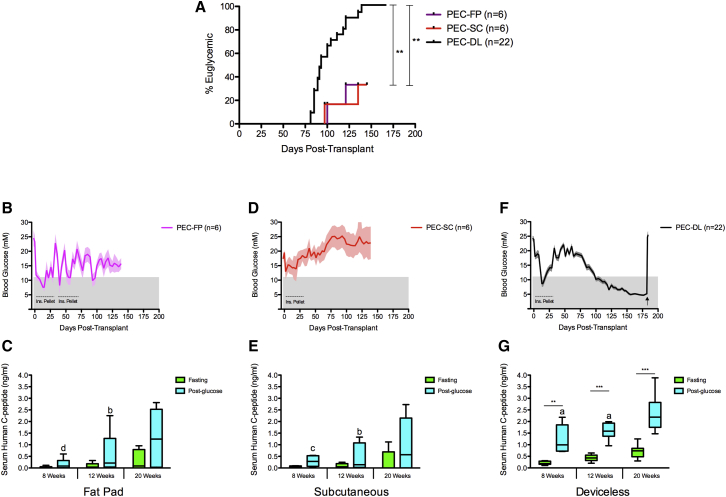
Figure 3.
Transplantation of Pancreatic Endoderm Cells Establishes and Maintains Normoglycemia in Diabetic B6/Rag−/− Mice
(A) The proportion of animals that achieved euglycemia was similar in fat pad recipients (FP, purple, n = 6 mice) and unmodified subcutaneous recipients (SQ, red, n = 6 mice) post transplant, whereas all device-less recipients (DL, black, n = 22 mice) reversed diabetes (∗∗p < 0.01, log rank, Mantel-Cox test).
(B, D, and F) Non-fasting blood glucose measurements showed that recipients of PECs transplanted into both FP (n = 4 of six mice) and SC space (n = 4 of six mice) failed to reverse diabetes, whereas all PEC-DL (n = 22 mice) recipients maintained normoglycemia post transplant until the grafts were retrieved (arrow), at which point they reverted to their pretransplant hyperglycemic state. Shaded area represents a non-fasting physiological range (<11.1 mM). Dashed lines represent time frame in which recipients were implanted with insulin (Ins.) pellets. Data points represent blood glucose mean ± SEM.
(C, E, and G) Serum human C-peptide levels were collected 8, 12, and 20 weeks post transplant after an overnight fasting period and post-60 min intraperitoneal glucose tolerance test. All recipients demonstrated detectable C peptide; however, only recipients of PECs transplanted into DL site showed significant glucose-responsive C-peptide secretion (∗∗p < 0.01, ∗∗∗p < 0.001, paired two-tailed t test). Different letters represent significant difference between transplant groups through 8–20 weeks post transplant (a, p<0.05; b, p<0.01; c, p<0.001; one-way ANOVA with Tukey test for multiple comparisons). Data points represent C-peptide mean ± SEM (FP, n = 6 mice; SC, n = 5 mice; DL, n = 9 mice; each sample assayed in triplicate) and represented as box-and-whisker plots.
Throughout the study, post-transplant non-fasting blood glucose profiles of the majority of mice in the FP group remained hyperglycemic, while exogenous insulin therapy had to be administered for 75 days post transplant to maintain an acceptable health status (Figure 3B). Despite marginal daily glycemic control, increasing stimulated serum human C peptide was detected between 8, 12, and 20 weeks post transplant; however, C-peptide concentrations detected post glucose challenge were not significantly greater than fasting levels, since recipients were hyperglycemic (p > 0.05, paired two-tailed t test, n = 6) (Figure 3C).
Similarly, the majority of mice in the SC group remained hyperglycemic post transplant; however, exogenous insulin therapy was only administered for 30 days post transplant to maintain an acceptable health status (Figure 3D). Comparable with the FP group, the SC transplant recipients demonstrated increased stimulated serum human C-peptide secretion between 8, 12, and 20 weeks post transplant, notwithstanding persistent hyperglycemia. Again, analogous to the FP group, the glucose-stimulated C-peptide concentrations were not significantly greater than fasting levels (p > 0.05, paired two-tailed t test, n = 5) (Figure 3E).
In contrast, all recipients of PECs transplanted using the DL technique (100%: 22/22) demonstrated physiological non-fasting blood glucose profiles and insulin independence approximately 100 days post transplant, which was maintained until the PEC-bearing DL grafts were harvested. Mice were maintained on exogenous insulin for 30 days post transplant with no mice receiving exogenous insulin thereafter prior to graft retrieval. After graft retrieval, all recipients reverted back to a pretransplant hyperglycemic state, indicative of graft-dependent euglycemia (Figure 3F). Furthermore, PEC-DL transplanted mice demonstrated consistent and rising glucose-responsive human C-peptide secretion between 8 and 20 weeks post transplant. This observation is highlighted by the significant increase in stimulated C peptide measured compared with fasting levels at 8 weeks (p < 0.01, paired two-tailed t test, n = 8), 12 weeks (p < 0.001, paired two-tailed t test, n = 8), and 20 weeks (p < 0.001, paired two-tailed t test, n = 9) post transplant (Figure 3G). Furthermore, the quantity of stimulated human C peptide secreted by the PEC-DL recipients was significantly greater than that of the PEC-FP and PEC-SC recipients at 8 weeks (p < 0.001 and p < 0.01, respectively, one-way ANOVA) and 12 weeks post transplant (p < 0.05 and p < 0.05, one-way ANOVA) (Figures 3C, 3E, and 3G).
Long-Term Durable Function of PEC Grafts Transplanted into DL Site
As a means to assess long-term function of euglycemic mice post transplant with PECs into the prevascularized DL site (n = 4), intraperitoneal glucose tolerance tests (IPGTTs) were conducted 24 weeks post transplant. Simultaneously, and as a measure of comparison, IPGTTs were also performed on euglycemic B6/Rag−/− mice 100 days post transplant of human islets engrafted under the kidney capsule (KC) (n = 6). In addition, naive non-diabetic, non-transplanted mice received IPGTTs, serving as a positive control (n = 6). PEC-DL recipients rapidly became normoglycemic following glucose challenge, demonstrating glucose clearance profiles similar to those of naive and human islet KC recipients (Figure 4A). Blood glucose area under the curves (AUCs) ± SEM for glucose clearance were similar between human islet KC recipients and PEC-DL mice (p > 0.05, two-tailed t test) (Figure 4B), demonstrating that the hESC-derived PECs transplanted in DL have the capacity to respond to a challenge of glucose to a mirrored degree as that of transplanted mature human β cells. Of interest, glucose profiles in the naive mice tested were significantly elevated compared with PEC-DL recipients (p < 0.05, two-tailed t test) (Figure 4B), which we postulate could be accounted for by the lower physiological glucose set point of human islets and their precursors compared with that of rodents.
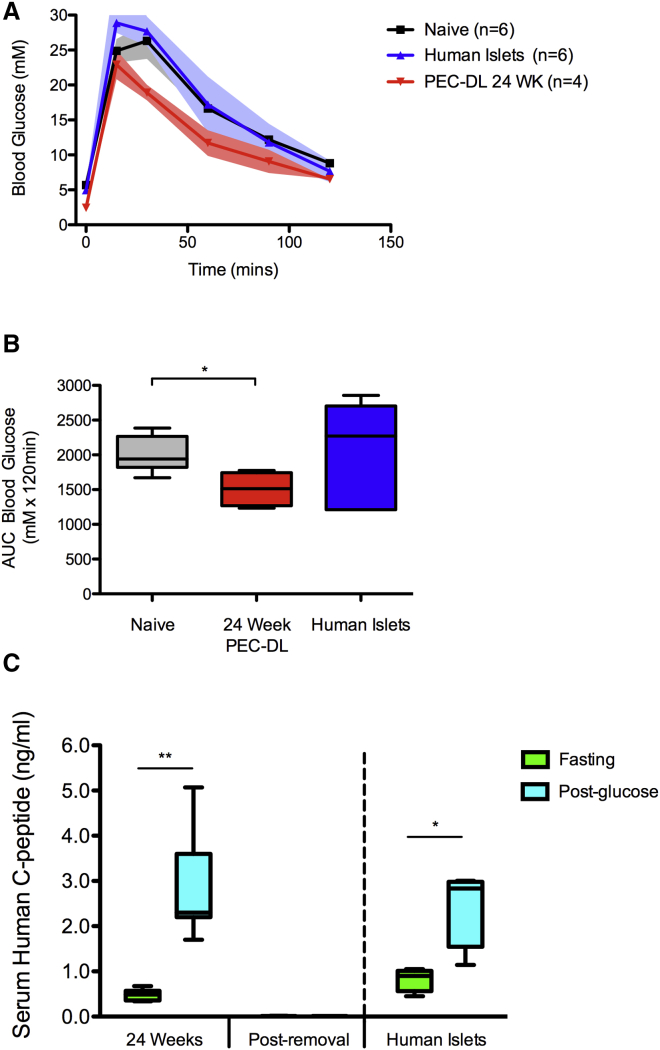
Figure 4.
Long-Term Function of Pancreatic Endoderm Cell Grafts Transplanted into the DL Space
Intraperitoneal glucose tolerance test of PEC-DL transplant recipients (blue, n = 4 mice), 24 weeks post transplant, in addition to naive non-diabetes mice (black/gray, n = 6 mice) and recipients of 1,000 human islet equivalents transplanted under kidney capsule (KC, red, n = 6 mice) post transplant.
(A and B) Blood glucose after dextrose bolus (B) AUC analysis did not differ between the naive and human islet KC recipients (p > 0.05, one-way ANOVA with Newman-Keuls post hoc testing for multiple comparison between transplant groups). PEC-DL recipients were more tolerant to the metabolic test than naive mice recipients (∗p > 0.05, one-way ANOVA with Newman-Keuls post hoc testing for multiple comparison to naive controls). Mice were administered 3 g/kg 50% dextrose intraperitoneally. Blood glucose measurements were monitored at 0, 15, 30, 60, 90 and 120 min. Data points represent blood glucose mean ± SEM.
(C) Serum human C-peptide levels were collected at 24 weeks post transplant after an overnight fasting period and post-60 min intraperitoneal glucose tolerance test. PECs transplanted into DL site (n = 4 mice) maintained significant glucose-responsive C-peptide secretion (∗∗p < 0.01, paired, two-tailed t test), similar to the glucose-responsive C-peptide secretion demonstrated by recipients of human islets (n = 6 mice) (∗p < 0.05, paired two-tailed t test). Following PEC graft retrieval, human C-peptide secretions were completely abolished (p > 0.05, paired, two-tailed t test). Data points represent C-peptide mean ± SEM (each sample assayed in triplicate).
Long-term, durable, glucose-regulated control exhibited by PEC-DL transplant recipients was exemplified by a significant increase in stimulated C peptide compared with fasting levels at 24 weeks (p < 0.01, paired two-tailed t test, n = 4 mice) (Figure 4C). The PEC-DL graft's ability to secrete human C peptide in a glucose-dependent manner emulates the intrinsic response of human islet grafts to a glucose challenge (p < 0.05, two-tailed t test, n = 6 mice) (Figure 4C). PEC-DL recipients' daily blood glucose homeostasis was completely abolished upon graft excision (Figure 3F), and also failed to secrete human C peptide at basal levels and post-glucose challenge (Figure 4C).
PEC-DL Grafts Possess Histological Similarities to Human Islets
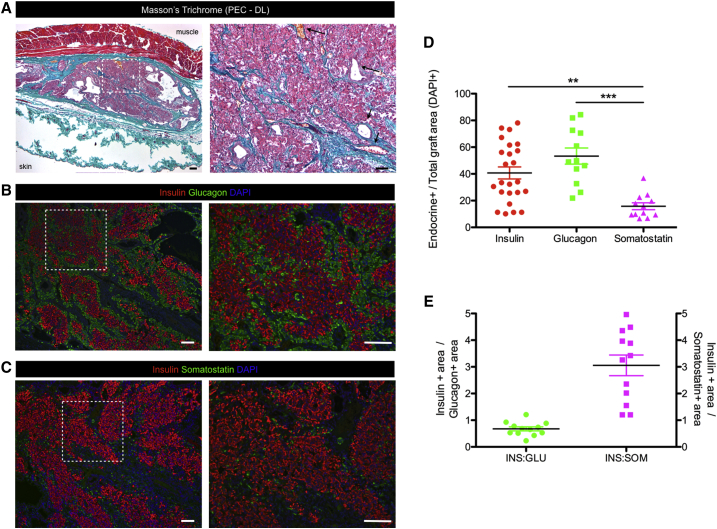
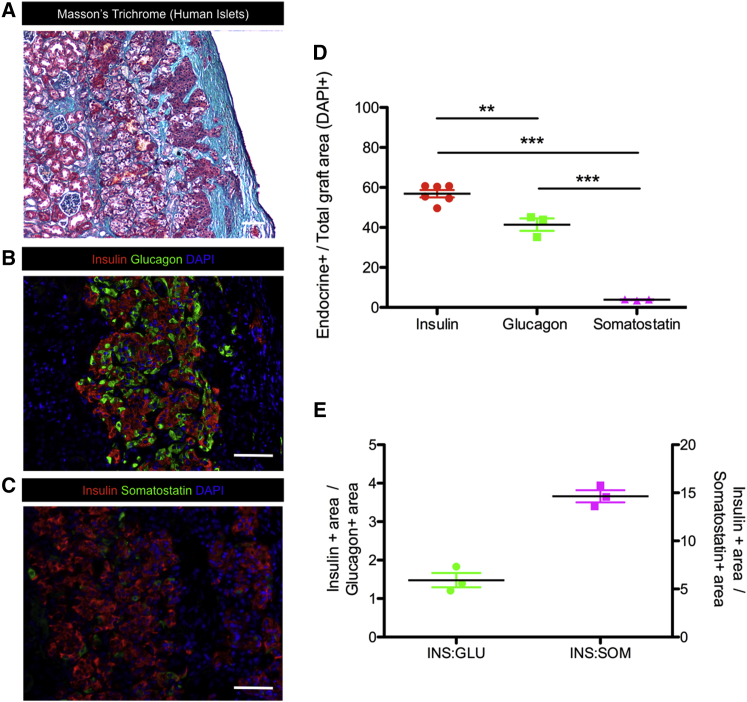
Histological examination of these retrieved PEC-DL grafts revealed cellular containment within the vascularized collagen scaffold evoked by the creation of the DL site (Figure 5A). The cellular composition of the hESC-derived PEC grafts consisted predominately of insulin-producing cells (40.7% ± 4.5% of total graft) and the counter-regulatory cells that secrete glucagon (53.3% ± 6.0% of total graft) (Figures 5B and 5D). Furthermore, the PEC grafts contained somatostatin-secreting cells (15.8% ± 4.5% of total graft), which accounted for the smallest endocrine cellular population compared with insulin and glucagon cells (p < 0.05 and p < 0.01, respectively, one-way ANOVA) (Figures 5C and 5D). Glucagon immunoreactivity was nearly twice as prevalent as insulin within the PEC grafts (0.67 ± 0.07 INS:GLU), whereas insulin immunoreactivity was approximately 3-fold greater relative to somatostatin immunoreactivity (3.1 ± 0.4 INS:SOM) (Figure 5E). These hESC-origin PEC grafts indeed resemble the native cytoarchitecture and composition of transplanted human pancreatic endocrine tissue (Figures 6A–6C). In fact the percentages of insulin+ and glucagon+ within the PE-DL grafts were similar to that of human islet grafts under the KC (insulin+ DL-PEC: 40.7% ± 4.5% versus human islet graft: 56.9% ± 4.5%, p > 0.05, two-tailed t test; glucagon+ DL-PEC: 53.3% ± 6.0% versus human islet graft: 41.4% ± 3.1%, p > 0.05, two-tailed t test) (Figures 6B and 6C). However, PE grafts in the DL site had significantly more somatostatin+ cells compared with human islet grafts (somatostatin+ DL-PEC: 15.8% ± 2.6% versus human islet graft: 3.8% ± 0.2%, p < 0.05, two-tailed t test) (Figures 6B and 6C). PEC grafts in the unmodified subcutaneous tissue also resembled DL graft with respect to endocrine cellular composition (p > 0.05, two-tailed t test) (Figure S1). In contrast to human islet grafts and PECs transplanted under the skin, PEC grafts implanted into the FP contained significantly less insulin+ and somatostatin+ cells (p < 0.01 and p < 0.05, respectively, two-tailed t test) (Figure S2).
Figure 5.
Long-Term hESC-Derived Pancreatic Endoderm Cell Grafts Transplanted into the DL Space Contain Glucose-Regulatory Cells
(A) Representative images of Masson's trichrome staining of a PEC graft cross-section in DL site >175 days post transplant, surrounded by collagen (blue) and smooth muscle and erythrocytes (red). Right panel: higher magnification of the inset. Arrows indicate blood vessels. Scale bars represent 100 μm.
(B and C) Representative immunofluorescent staining of PECs engrafted in the DL site harvested after >175 days. Grafts were stained with insulin (red), glucagon (green) (B), somatostatin (green) (C), and nuclear DAPI staining (blue). Right panel: higher magnification of the inset. Scale bars represent 100 μm.
(D) Area of insulin (INS), glucagon (GLU), and somatostatin (SOM) immunoreactivity relative to the total graft area (DAPI+).
(E) Areas of insulin+ relative to glucagon+ or somatostatin+ area for each graft.
∗∗p < 0.05, ∗∗∗p < 0.01, one-way ANOVA with Tukey test for multiple comparisons. All data are presented as mean ± SEM (n = 6 animals [grafts]/2–4 sections per graft).
Figure 6.
Immunohistochemistry of Representative Human Islet Graft Transplanted under the Kidney Capsule of an Immunodeficient Mouse
(A) Representative Masson's trichrome staining of human islet graft cross-section 100 days post transplant at 20×, surrounded by collagen (blue), and smooth muscle and erythrocytes (red). Scale bars represent 100 μm.
(B and C) Fluorescent image of human islet graft staining positive for insulin (red), glucagon (green) (B), somatostatin (green) (C), and nuclear DAPI staining (blue), Scale bars represent 100 μm.
(D) Area of insulin (INS), glucagon (GLU), and somatostatin (SOM) immunoreactivity relative to the total graft area (DAPI+).
(E) Areas of insulin+ relative to glucagon+ or somatostatin+ area for each graft.
∗∗p < 0.01, ∗∗∗p < 0.001; one-way ANOVA with Tukey test for multiple comparisons. All data are presented as mean ± SEM (n = 3 animals [grafts]/2–4 sections per graft).
Importantly, the presence of insulin+, glucagon+, and somatostatin+ cell types within the DL grafts, in addition to pancreatic polypeptide and ghrelin-secreting cells (Figure S3), are necessary for maintaining physiologically relevant glucose homeostasis.
Discussion
With the advent of the first-in-human pilot phase 1/2 clinical trial, jointly conducted in San Diego, USA and Edmonton, Canada, testing ViaCyte's VC-01 combination product in a small cohort of T1D patients, the clinical path for future stem cell-derived regenerative, reparative, and replacement therapies has been established.
However, further characterization of stem cell-derived insulin-producing cell therapies and optimization of suitable engraftment sites will prospectively be necessary to improve patient outcomes. As such, prior to transplantation we assessed the metabolic potency of the CyT49 PECs. The significantly lower OCR observed in the PECs suggests that they are metabolically quiescent compared with freshly isolated adult human islets at the time of transplantation. This quiescent mitochondrial potency of the PECs may, at least in part, be explained by the known metabolic plasticity associated with stem cell homeostasis and degree of differentiation (Ito and Suda, 2014); a reflection of the differentiation state of PECs and the immature status of their mitochondria. The dynamic interplay between the influence of microenvironments and energy balance on stem cell differentiation may indeed support the rationale for pursuing pancreatic progenitor-based therapy, compared with more in vitro differentiated insulin-secreting β cells (Schulz, 2015), as the former are equipped with the endogenous metabolic capacity to tolerate low oxygen tension niches (Ito and Suda, 2014). This becomes a critical cellular attribute upon transplantation, as all preclinical and clinical islet engraftment sites, including the subcutaneous tissue, to date have been demonstrated to be hypoxic compared with the native pancreas (Pepper et al., 2013).
hPSC-derived insulin-producing cells have previously been shown to exhibit various properties of mature β cells dependent upon the degree of in vitro differentiation (Bruin et al., 2013, D'Amour et al., 2006, Pagliuca et al., 2014, Rezania et al., 2012, Rezania et al., 2014). A unique characteristic of “β-like” cells is their inherent ability to respond to alterations in extracellular glucose levels through membrane depolarization leading to intracellular calcium [Ca2+]i elevations, culminating in insulin exocytosis (Mohammed et al., 2009). Both human PSC-derived S7 (Rezania et al., 2014) and stem cell-derived β-like cells (Pagliuca et al., 2014) have been demonstrated to have the capacity to rapidly increase [Ca2+]i in response to glucose, a characteristic of mature human β cells. However, Rezania et al. (2014) cautioned that only a small subset (5%–10%) of the S7 cell population actually possessed this physiological characteristic and exhibited reduced amplitude and dampened kinetics in Ca2+ flux, whereas Pagliuca et al. (2014) conclude that both the entire population and individual cells within their hPSC-derived SC-β-cell clusters fluxed calcium comparable with human islets. However, the authors failed to present the individual calcium traces of their hPSC-derived SC-β cell, making it unmerited to compare their “β-like” cells with those derived by Rezania et al. (2014) and mature human islets.
In comparison, little is known about the glucose-induced Ca2+ signaling ability of less mature pancreatic progenitors. One such study by Basford et al. (2012) demonstrated that >80% of insulin+ cells, derived from hESCs via a 22-day in vitro differentiation protocol (S5), increased intracellular Ca2+ during depolarization with KCl similar to human islets; however, they did not demonstrate glucose-stimulated insulin release. Notwithstanding the immature nature of S4 PECs, in the present study we observed a modest intracellular Ca2+ flux in the presence of high glucose and rapid direct depolarization with KCl, prior to transplantation, albeit this response was restricted to a small subset of PECs tested, mimicking the asymmetrical profiles exhibited by more differentiated hPSC progeny (Rezania et al., 2014). Alternatively, nearly all human β cells (islets) tested demonstrated an intracellular Ca2+ flux in response to glucose, again illustrating the undeveloped status of the PECs at the time of transplantation.
It has been established that hESC-derived insulin+ cells exhibit characteristics of human β cells, as they possess varying degrees of glucose sensitivity (Pagliuca et al., 2014, Rezania et al., 2014). Therefore, we examined the glucose-stimulated insulin-secreting capability of S4 PECs prior to transplant. Similar to the Ca2+ flux observations, PECs demonstrated a humble response to glucose perifusion compared with primary β cells. These findings echo the data described by Rezania et al. (2014) showing that both S6 and S7 hPSCs displayed abnormal and diminished in vitro insulin secretion in response to similar glucose stimuli. These data highlight the fact that prior to transplant, the S4 PECs are phenotypically and functionally infant compared with mature human β cells, as previously reported by D'Amour et al. (2006). Therefore, an obligate period of in vivo differentiation is required post transplant before glucose-dependent graft insulin secretion and glucose homeostasis becomes evident (Kroon et al., 2008, Schulz et al., 2012).
Subsequent to the transplantation of PECs into diabetic mice, regardless of engraftment site, an in vivo differentiation period of greater than 3 months was required prior to observing hyperglycemic correction. When transplanted into the FP of diabetic recipients, marginal glycemic control was observed. However, improved stimulated human C peptide was measured between 8 and 20 weeks post transplant, albeit not significantly different from basal levels. Significant basal and stimulated human C peptide at 8 weeks post transplant was reported by Kroon et al. (2008) when PECs where implanted into FP of non-diabetic recipients, utilizing the same hESC line and differentiation protocol, which may in part reflect the impact of recipient pretransplant hyperglycemia on the utility of the FP site.
In juxtaposition, when PECs were transplanted into the DL site, all recipients became euglycemic, which was preserved until grafts were successfully retrieved, whereas when PECs were transplanted into the unmodified SC site, the majority of the recipients remained hyperglycemic, highlighting the importance of prevascularizing the subcutaneous tissue to routinely achieve durable insulin independence after PEC transplant. This long-term glycemic correction and sustained normoglycemia mirrored our previous observations in DL transplants of both mouse and human islets (Pepper et al., 2015), as well as others when more mature insulin+ cells derived from hPSC were transplanted using encapsulated and KC transplant approaches (Pagliuca et al., 2014, Rezania et al., 2014, Vegas et al., 2016). The tightly regulated daily glycemic control within the PEC-DL cohort was superior to that observed in previous studies where S4 PECs were transplanted under the KC (Rezania et al., 2014), and similar to that reported when implanted into the FP (Kroon et al., 2008, Schulz et al., 2012); however the latter two FP studies did not evaluate their cells in mice with pre-existing diabetes. Perhaps a more appropriate comparison of glycemic control established in the present study and that of previous work is that by Rezania et al. (2012), where similar S4 PECs were transplanted into diabetic mice. The non-fasting glycemic control in our PEC-DL recipients resembles the fasting glycemic measurements of their KC recipients, albeit the C-peptide levels in the present study are higher at similar post-transplant weeks, using similar stimulation testing and assays (Rezania et al., 2012). Intriguingly, the non-fasting blood glucose values of long-term PEC-DL recipients were in the 3- to 5-mM range, reflecting a more human glycemic phenotype and set point than mouse (7–11 mmol). Of note, no hypoglycemic events occurred after transplantation, indicating that the PEC recipients acquire physiological glycemic compensatory regulation. Furthermore, PEC-DL transplanted recipients presented with increasing glucose-responsive human C-peptide secretion between 8 and 20 weeks post transplant, with stimulated concentrations exceeding that observed in FP and SC recipients. In contrast, previous studies which employed alternative S4 pancreatic progenitor cells that were transplanted either within an immunoisolating device or under the KC in mice did not demonstrate significant human C-peptide detection until 12 and 16 weeks, respectively (Bruin et al., 2013, Rezania et al., 2012).
Furthermore, the physiological response to a glucose tolerance test demonstrated by the PEC-DL recipients is similar to that reported when the same PECs were transplanted into non-diabetic FP recipients (Kroon et al., 2008), and resembled the profile of mice transplanted with more mature S6 insulin-positive cells (Rezania et al., 2014). However, perhaps more importantly and relevant is the observation the PEC-DL recipients demonstrated glucose clearance similar to that of mice transplanted with human islets under the KC as well as non-diabetic mice. These observations further reflect the efficiency of PEC engraftment, their conserved human physiological phenotype, and their ability to restore carbohydrate control in a regulated biological manner.
Of importance, post-transplant euglycemia and human C-peptide secretion achieved by PEC-DL recipients was wholly halted upon graft excision. These observations validate graft-dependent euglycemia and illustrate the ability that when transplanted subcutaneously in the DL site, PEC grafts can be safely removed should the procedure be required. Histological analysis of the harvested PEC-DL grafts demonstrated cellular containment within a vascularized matrix. The composition of the PEC graft contained mainly insulin-producing cells along with cells staining positive for the glucose regulatory hormones of glucagon, somatostatin, ghrelin, and pancreatic polypeptide. The long-term euglycemia grafts resembled the composition described by others post transplant of hESC-derived insulin-producing cells transplanted in epididymal fat (Kelly et al., 2011, Kroon et al., 2008, Schulz et al., 2012) and under the KC in mice (Bruin et al., 2015a, Pagliuca et al., 2014, Rezania et al., 2014), as well as the cellular architecture of transplanted human pancreatic islets. It must be cautiously noted that the transplant microenvironment and the host recipient can critically influence the fate and composition of pancreatic progenitor cells post transplant (Bruin et al., 2015a, Motte et al., 2014). This phenomenon may too explain the differences in cellular composition of PEC grafts, in the present study, when transplanted under the skin compared with the FP. We demonstrated that PE grafts of the FP contained significantly fewer insulin+ cells, whereas PEC grafts under the skin resembled more human islet grafts transplanted under the renal capsule. Therefore, the extrapolation and comparison of PEC graft composition in rodents with clinical islet grafts should only be considered speculative, and can only be accurately evaluated following the completion of human clinical trials involving pancreatic progenitor cells.
Herein, we have shown that hESC-derived PECs can survive and differentiate into glucose-responsive insulin-producing cells while restoring long-term glycemic control to diabetic recipients upon transplantation into a safely retrievable subcutaneous prevascularized site. This transplant methodology facilitates graft-vascular ingrowth and biological nutrient exchange, which cannot be achieved through selectively impermeable encapsulation (Bruin et al., 2013, Vegas et al., 2016). Our approach provides a means to safely explant the cellular graft should unforeseen complications arise, meeting the proposed prerequisite for extrahepatic β-cell replacement strategies (Stock and German, 2016). Taken together, these results complement the current clinical investigation of ViaCyte's VC-01 combination product, and may indeed provide an appropriate surrogate niche for current and future stem cell-derived insulin-producing cell therapy. However, it remains to be seen whether the transplantation of pancreatic progenitors in an immune-isolating device will be preferential to transplanting these or more mature glucose-responsive insulin-secreting cells into a retrievable prevascularized subcutaneous site in the presence of standard clinical immunosuppressive therapy.
Experimental Procedures
ESC Culture Differentiation and Processing
CyT49 hESCs were cultured and differentiated to PECs as previously described (Schulz et al., 2012) with a modification of culture format during differentiation, which was carried out in roller bottles (Schulz, 2015; Figure 1B). Details regarding the differentiation procedure are outlined in Supplemental Experimental Procedures. Free aggregates were shipped at 18°–25°C to the University of Alberta for in vitro characterization and implantation.
Human Islets
Human islets were prepared by the Clinical Islet Laboratory at Alberta Health Services or IsletCore at Alberta Diabetes Institute. Deceased donor pancreata were processed for islet isolation with appropriate ethical approval and consent obtained from next-of-kin of the donor. Islets were isolated implementing a modified Ricordi technique (Kin, 2010). Permission for these studies was granted by the Health Research Ethics Board of the University of Alberta, Edmonton, Alberta Canada.
Oxygen Consumption Rates
Prior to transplantation, human islet and PEC fractional viability was assessed by OCR normalized to DNA quantity (OCR/DNA). Cell-preparation OCR was measured in triplicate (approximately 10 μL/replicate) using a fiber-optic sensor oxygen monitoring system (Instech Laboratories), as previously described (Papas et al., 2007, Pepper et al., 2012). OCR (nmol/min) was standardized to the amount of DNA (mg) in each chamber, quantified by a Quant-iT PicoGreen dsDNA kit (Molecular Probes).
Glucose-Stimulated Insulin Secretion
The glucose-responsive insulin secretory capacity of both human islets and PECs was assessed by dynamic perifusion, as described by Cabrera et al. (2008) and in Supplemental Experimental Procedures.
Measurements of [Ca2+]i
The PECs and human islets were hand-picked to assay calcium flux and dispersed by incubation in Ca2+-free buffer (Life Technologies) followed by trituration as previously described (Yan-Do et al., 2016). Details regarding cellular calcium flux assessment are provided in Supplemental Experimental Procedures. After the experiment, human pancreatic cell types (insulin, glucagon, and somatostatin+) were identified by immunocytochemistry as previously described (Yan-Do et al., 2016). Excitation ratios (340/380 nm) were subsequently calculated offline from captured images in regions of interest corresponding to identified insulin+ cell types, using ImageJ software (NIH).
Preparing a Prevascularized Subcutaneous Transplant Site
To house hESC-derived PECs, we utilized the foreign-body response elicited by medically approved vascular catheters to create a prevascularized subcutaneous DL transplant site as previously described for islet transplantation (Pepper et al., 2015). Details regarding mouse strain and DL procedure are outlined in Supplemental Experimental Procedures.
All animals within the study were housed under conventional conditions having access to food and water ad libitum. Mouse care was in accordance with the guidelines approved by the Canadian Council on Animal Care. Furthermore, all experimental protocols were reviewed and approved by the Research Ethics Board of the University of Alberta.
Diabetes Induction and Cell Transplantation
Three to five days before transplantation, normoglycemic (<11.1 mM) mice were rendered diabetic through administration of an intraperitoneal injection of streptozotocin (STZ) (Sigma-Aldrich Canada) at 180 mg/kg in acetate phosphate buffer (pH 4.5). Animals were considered diabetic when their non-fasting blood glucose levels exceeded a pre-established value of 15 mM (350 mg/dL) for two consecutive daily readings post STZ administration. Only animals meeting this inclusion criterion were selected for transplantation. At the time of transplantation, 10–20 μL (∼0.5–1.0 × 107 cells) of PECs (ViaCyte) or human islets of 1,000 equivalents (IEQ) were aspirated into polyethylene (PE-50) tubing using a microsyringe, and centrifuged into a pellet suitable for transplantation. PEC preparations were randomly transplanted to three recipient groups: DL, subcutaneous alone, or within the epididymal FPs. Human islets were transplanted under KC. PECs were transplanted into the DL site as previously described (Pepper et al., 2015, Pepper et al., 2016a, Pepper et al., 2016b), in addition to the native subcutaneous space by making a small (1 cm × 2 cm) subcutaneous pocket using blunt discretion in the left lower abdominal quadrant mimicking the graft location of the DL recipients. Furthermore, PECs were implanted into the epididymal FP as previously described (Kroon et al., 2008) and outlined in Supplemental Experimental Procedures.
All recipient mice were maintained under anesthesia with inhalant isoflurane, and placed in a supine position. Prior to recovery, recipients received a 0.1-mg/kg subcutaneous bolus of buprenorphine.
Evaluation of Graft Function
Graft function was assessed through non-fasting blood glucose measurements, using a portable glucometer (OneTouch Ultra 2; LifeScan) three times per week following islet transplantation, in all groups transplanted. Reversal of diabetes was defined as two consecutive readings <11.1 mM and maintained until study completion. Exogenous insulin therapy (LinBit pellet; LinShin) was administered subcutaneously peri-transplant and subsequently thereafter based on the recipients’ body weight, activity, and physical appearance to maintain an acceptable health status. Details regarding metabolic assessment, human C-peptide secretion, and glucose tolerance testing are provided in Supplemental Experimental Procedures.
Cellular Graft Retrieval
For confirmation of graft-dependent euglycemia, animals with functional grafts had their PEC transplants explanted by subcutaneous graft excision. The subcutaneous grafts within the DL transplanted animals were excised with a margin of surrounding abdominal skin containing the graft. Excised grafts were preserved for immunohistochemistry in 10% formalin. Following PEC-graft removal, non-fasting blood glucose measurements were monitored for the subsequent 7 days to observe a return to hyperglycemia (pretransplant), confirming post-transplant graft function.
Histological Assessment
Immunofluorescence with anti-insulin, anti-glucagon, anti-somatostatin, anti-ghrelin, and anti-pancreatic polypeptide antibodies was used to identify the presence of pancreatic β cells, α cells, δ cells, ɛ cells, and PP cells, respectively. Details regarding tissue preparation and antibodies are provided in Supplemental Experimental Procedures. Using a fluorescent microscope, the resulting microphotographs were taken using the appropriate filter with AxioVision imaging software. Graft cellular composition was analyzed using ImageJ software (NIH). Representative sections were stained with Masson's trichrome to identify collagen.
Statistical Analysis
Non-fasting blood glucose and human C-peptide data are presented as the mean ± SEM. Human C-peptide analysis was conducted through paired two-tailed t test. Blood glucose AUC analysis for glucose tolerance test and histological analysis was conducted through parametric one-way ANOVA using GraphPad Prism (GraphPad Software). Newman-Keuls and Tukey post hoc tests were used following the analyses of variance for multiple comparisons between study groups. Kaplan-Meier survival function curves were compared using the log-rank statistical method. p < 0.05 was considered significant.
Author Contributions
A.R.P. and A.M.J.S. initiated and designed the experiments. A.R.P., R.P., A.B., J.W., Y.R., R.Y.-D., B.G.-L., and D.O. performed the experiments. T.K. isolated and provided human islets. A.R.P., P.E.M., and A.M.J.S. analyzed the data. All authors provided input in manuscript writing and discussion.
Acknowledgments
We thank the Clinical Islet Laboratory and Alberta Health Services for providing human islet research preparations. This work was supported in part by the Diabetes Research Institute Foundation of Canada (DRIFCan), Collaborative Research & Innovation Opportunities – Alberta Innovates Healthcare Solutions (AIHS) & Canadian Institutes of Health Research – Proof of Principle. All authors are members of the Alberta Diabetes Institute and of the Canadian National Transplant Research Program (CNTRP). A.M.J.S. is supported through a Canada Research Chair (CRC) in Transplantation Surgery and Regenerative Medicine, and through a Senior Clinical Scholarship from AIHS. A.R.P. is supported by an AIHS Postdoctoral fellowship. A.B. is supported by scholarships from the University of Alberta and the Alberta Diabetes Institute. P.E.M. holds a Killam Annual Professorship. We also thank ViaCyte, Inc. for kindly providing the PECs. A.M.J.S. serves as an advisor to ViaCyte Inc. with respect to design and testing on ongoing clinical and experimental trials of stem cell products. The Governors of The University of Alberta have filed patent applications with the Canadian Intellectual Property Office (CA.2865122) and the United States Patent and Trademark Office (US 14/863541) pertaining to the DL transplant technology.
Published: June 6, 2017
Footnotes
Supplemental Information includes Supplemental Experimental Procedures and three figures and can be found with this article online at http://dx.doi.org/10.1016/j.stemcr.2017.05.004.
Supplemental Information
References
- Barton F.B., Rickels M.R., Alejandro R., Hering B.J., Wease S., Naziruddin B., Oberholzer J., Odorico J.S., Garfinkel M.R., Levy M. Improvement in outcomes of clinical islet transplantation: 1999-2010. Diabetes Care. 2012;35:1436–1445. doi: 10.2337/dc12-0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basford C.L., Prentice K.J., Hardy A.B., Sarangi F., Micallef S.J., Li X., Guo Q., Elefanty A.G., Stanley E.G., Keller G. The functional and molecular characterisation of human embryonic stem cell-derived insulin-positive cells compared with adult pancreatic beta cells. Diabetologia. 2012;55:358–371. doi: 10.1007/s00125-011-2335-x. [DOI] [PubMed] [Google Scholar]
- Bruin J.E., Asadi A., Fox J.K., Erener S., Rezania A., Kieffer T.J. Accelerated maturation of human stem cell-derived pancreatic progenitor cells into insulin-secreting cells in immunodeficient rats relative to mice. Stem Cell Reports. 2015;5:1081–1096. doi: 10.1016/j.stemcr.2015.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruin J.E., Rezania A., Kieffer T.J. Replacing and safeguarding pancreatic beta cells for diabetes. Sci. Transl. Med. 2015;7:316ps323. doi: 10.1126/scitranslmed.aaa9359. [DOI] [PubMed] [Google Scholar]
- Bruin J.E., Rezania A., Xu J., Narayan K., Fox J.K., O'Neil J.J., Kieffer T.J. Maturation and function of human embryonic stem cell-derived pancreatic progenitors in macroencapsulation devices following transplant into mice. Diabetologia. 2013;56:1987–1998. doi: 10.1007/s00125-013-2955-4. [DOI] [PubMed] [Google Scholar]
- Cabrera O., Jacques-Silva M.C., Berman D.M., Fachado A., Echeverri F., Poo R., Khan A., Kenyon N.S., Ricordi C., Berggren P.O. Automated, high-throughput assays for evaluation of human pancreatic islet function. Cell Transpl. 2008;16:1039–1048. [PMC free article] [PubMed] [Google Scholar]
- Choudhary P., Rickels M.R., Senior P.A., Vantyghem M.C., Maffi P., Kay T.W., Keymeulen B., Inagaki N., Saudek F., Lehmann R. Evidence-informed clinical practice recommendations for treatment of type 1 diabetes complicated by problematic hypoglycemia. Diabetes Care. 2015;38:1016–1029. doi: 10.2337/dc15-0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Amour K.A., Bang A.G., Eliazer S., Kelly O.G., Agulnick A.D., Smart N.G., Moorman M.A., Kroon E., Carpenter M.K., Baetge E.E. Production of pancreatic hormone-expressing endocrine cells from human embryonic stem cells. Nat. Biotechnol. 2006;24:1392–1401. doi: 10.1038/nbt1259. [DOI] [PubMed] [Google Scholar]
- Gruessner R.W., Gruessner A.C. The current state of pancreas transplantation. Nat. Rev. Endocrinol. 2013;9:555–562. doi: 10.1038/nrendo.2013.138. [DOI] [PubMed] [Google Scholar]
- Ito K., Suda T. Metabolic requirements for the maintenance of self-renewing stem cells. Nat. Rev. Mol. Cell Biol. 2014;15:243–256. doi: 10.1038/nrm3772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly O.G., Chan M.Y., Martinson L.A., Kadoya K., Ostertag T.M., Ross K.G., Richardson M., Carpenter M.K., D'Amour K.A., Kroon E. Cell-surface markers for the isolation of pancreatic cell types derived from human embryonic stem cells. Nat. Biotechnol. 2011;29:750–756. doi: 10.1038/nbt.1931. [DOI] [PubMed] [Google Scholar]
- Kin T. Islet isolation for clinical transplantation. Adv. Exp. Med. Biol. 2010;654:683–710. doi: 10.1007/978-90-481-3271-3_30. [DOI] [PubMed] [Google Scholar]
- Kroon E., Martinson L.A., Kadoya K., Bang A.G., Kelly O.G., Eliazer S., Young H., Richardson M., Smart N.G., Cunningham J. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat. Biotechnol. 2008;26:443–452. doi: 10.1038/nbt1393. [DOI] [PubMed] [Google Scholar]
- McCall A.L. Insulin therapy and hypoglycemia. Endocrinol. Metab. Clin. North Am. 2012;41:57–87. doi: 10.1016/j.ecl.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammed J.S., Wang Y., Harvat T.A., Oberholzer J., Eddington D.T. Microfluidic device for multimodal characterization of pancreatic islets. Lab Chip. 2009;9:97–106. doi: 10.1039/b809590f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motte E., Szepessy E., Suenens K., Stange G., Bomans M., Jacobs-Tulleneers-Thevissen D., Ling Z., Kroon E., Pipeleers D., Beta Cell Therapy Consortium EU-FP7 Composition and function of macroencapsulated human embryonic stem cell-derived implants: comparison with clinical human islet cell grafts. Am. J. Physiol. Endocrinol. Metab. 2014;307:E838–E846. doi: 10.1152/ajpendo.00219.2014. [DOI] [PubMed] [Google Scholar]
- Pagliuca F.W., Millman J.R., Gurtler M., Segel M., Van Dervort A., Ryu J.H., Peterson Q.P., Greiner D., Melton D.A. Generation of functional human pancreatic beta cells in vitro. Cell. 2014;159:428–439. doi: 10.1016/j.cell.2014.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papas K.K., Pisania A., Wu H., Weir G.C., Colton C.K. A stirred microchamber for oxygen consumption rate measurements with pancreatic islets. Biotechnol. Bioeng. 2007;98:1071–1082. doi: 10.1002/bit.21486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper A.R., Hasilo C.P., Melling C.W., Mazzuca D.M., Vilk G., Zou G., White D.J. The islet size to oxygen consumption ratio reliably predicts reversal of diabetes posttransplant. Cell Transpl. 2012;21:2797–2804. doi: 10.3727/096368912X653273. [DOI] [PubMed] [Google Scholar]
- Pepper A.R., Gala-Lopez B., Ziff O., Shapiro A.M. Revascularization of transplanted pancreatic islets and role of the transplantation site. Clin. Dev. Immunol. 2013;2013:352315. doi: 10.1155/2013/352315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper A.R., Gala-Lopez B., Pawlick R., Merani S., Kin T., Shapiro A.M. A prevascularized subcutaneous device-less site for islet and cellular transplantation. Nat. Biotechnol. 2015;33:518–523. doi: 10.1038/nbt.3211. [DOI] [PubMed] [Google Scholar]
- Pepper A.R., Bruni A., Pawlick R.L., Gala-Lopez B., Rafiei Y., Wink J., Kin T., Shapiro A.M. Long-term function and optimization of mouse and human islet transplantation in the subcutaneous device-less site. Islets. 2016;8:186–194. doi: 10.1080/19382014.2016.1253652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper A.R., Pawlick R., Bruni A., Gala-Lopez B., Wink J., Rafiei Y., Bral M., Abualhassan N., Shapiro A.M. Harnessing the foreign body reaction in marginal mass device-less subcutaneous islet transplantation in mice. Transplantation. 2016;100:1474–1479. doi: 10.1097/TP.0000000000001162. [DOI] [PubMed] [Google Scholar]
- Rezania A., Bruin J.E., Riedel M.J., Mojibian M., Asadi A., Xu J., Gauvin R., Narayan K., Karanu F., O'Neil J.J. Maturation of human embryonic stem cell-derived pancreatic progenitors into functional islets capable of treating pre-existing diabetes in mice. Diabetes. 2012;61:2016–2029. doi: 10.2337/db11-1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezania A., Bruin J.E., Arora P., Rubin A., Batushansky I., Asadi A., O'Dwyer S., Quiskamp N., Mojibian M., Albrecht T. Reversal of diabetes with insulin-producing cells derived in vitro from human pluripotent stem cells. Nat. Biotechnol. 2014;32:1121–1133. doi: 10.1038/nbt.3033. [DOI] [PubMed] [Google Scholar]
- Schulz T.C. Concise review: manufacturing of pancreatic endoderm cells for clinical trials in type 1 diabetes. Stem Cells Transl. Med. 2015;4:927–931. doi: 10.5966/sctm.2015-0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz T.C., Young H.Y., Agulnick A.D., Babin M.J., Baetge E.E., Bang A.G., Bhoumik A., Cepa I., Cesario R.M., Haakmeester C. A scalable system for production of functional pancreatic progenitors from human embryonic stem cells. PLoS One. 2012;7:e37004. doi: 10.1371/journal.pone.0037004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro, A.M. (2016a). Cellular transplant site. Canadian patent CA 2865122, filed September 24, 2014, and published March 24, 2016.
- Shapiro, A.M. (2016b). Cellular transplant site. US patent US20160082158A1, filed September 24, 2014, and published March 24, 2016.
- Shapiro A.M., Ricordi C. Islet cell transplantation—indications, risks and long-term outcomes. In: Kirk A.D., Knechtle S.J., Larsen C.P., Madsen J.C., Pearson T.C., Webber S.A., editors. Textbook of Organ Transplantation. Wiley-Blackwell; 2014. pp. 1314–1333. [Google Scholar]
- Shapiro A.M., Lakey J.R., Ryan E.A., Korbutt G.S., Toth E., Warnock G.L., Kneteman N.M., Rajotte R.V. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N. Engl. J. Med. 2000;343:230–238. doi: 10.1056/NEJM200007273430401. [DOI] [PubMed] [Google Scholar]
- Stock P.G., German M.S. A path to insulin independence: “The end of the beginning”. Cell Stem Cell. 2016;18:431–433. doi: 10.1016/j.stem.2016.03.010. [DOI] [PubMed] [Google Scholar]
- Thompson D.M., Meloche M., Ao Z., Paty B., Keown P., Shapiro R.J., Ho S., Worsley D., Fung M., Meneilly G. Reduced progression of diabetic microvascular complications with islet cell transplantation compared with intensive medical therapy. Transplantation. 2011;91:373–378. doi: 10.1097/TP.0b013e31820437f3. [DOI] [PubMed] [Google Scholar]
- Tuch B.E., Keogh G.W., Williams L.J., Wu W., Foster J.L., Vaithilingam V., Philips R. Safety and viability of microencapsulated human islets transplanted into diabetic humans. Diabetes Care. 2009;32:1887–1889. doi: 10.2337/dc09-0744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vegas A.J., Veiseh O., Gurtler M., Millman J.R., Pagliuca F.W., Bader A.R., Doloff J.C., Li J., Chen M., Olejnik K. Long-term glycemic control using polymer-encapsulated human stem cell-derived beta cells in immune-competent mice. Nat. Med. 2016;22:306–311. doi: 10.1038/nm.4030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan-Do R., Duong E., Manning Fox J.E., Dai X., Suzuki K., Khan S., Bautista A., Ferdaoussi M., Lyon J., Wu X. A glycine-insulin autocrine feedback loop enhances insulin secretion from human beta-cells and is impaired in type 2 diabetes. Diabetes. 2016;65:2311–2321. doi: 10.2337/db15-1272. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.