Key Points
Question
How is the 2013 American College of Cardiology/American Heart Association (ACC/AHA) Cholesterol Management Guideline related to lipid-lowering therapy use being adopted in cardiology practices in the United States?
Findings
In this study of 161 cardiology practices participating in the ACC Practice Innovation and Clinical Excellence Registry, there was minimal early adoption of the 2013 ACC/AHA Cholesterol Management Guideline.
Meaning
Aggressive efforts are needed for more effective guideline implementation to improve cardiovascular prevention.
Abstract
Importance
The 2013 American College of Cardiology/American Heart Association (ACC/AHA) Cholesterol Management Guideline recommends moderate-intensity to high-intensity statin therapy in eligible patients.
Objective
To examine adoption of the 2013 ACC/AHA guideline in US cardiology practices.
Design, Setting, and Participants
Among 161 cardiology practices, trends in the use of moderate-intensity to high-intensity statin and nonstatin lipid-lowering therapy (LLT) were analyzed before (September 1, 2012, to November 1, 2013) and after (February 1, 2014, to April 1, 2015) publication of the 2013 ACC/AHA guideline among 4 mutually exclusive risk groups within the ACC Practice Innovation and Clinical Excellence Registry. Interrupted time series analysis was used to evaluate for differences in trend in use of moderate-intensity to high-intensity statin and nonstatin LLT use in hierarchical logistic regression models. Participants were a population-based sample of 1 105 356 preguideline patients (2 431 192 patient encounters) and 1 116 472 postguideline patients (2 377 219 patient encounters). Approximately 97% of patients had atherosclerotic cardiovascular disease (ASCVD).
Exposures
Moderate-intensity to high-intensity statin and nonstatin LLT use before and after publication of the 2013 ACC/AHA guideline.
Main Outcomes and Measures
Time trend in the use of moderate-intensity to high-intensity statin and nonstatin LLT.
Results
In the study cohort, the mean (SD) age was 69.6 (12.1) years among 1 105 356 patients (40.2% female) before publication of the guideline and 70.0 (11.9) years among 1 116 472 patients (39.8% female) after publication of the guideline. Although there was a trend toward increasing use of moderate-intensity to high-intensity statins overall and in the ASCVD cohort, such a trend was already present before publication of the guideline. No significant difference in trend in the use of moderate-intensity to high-intensity statins was observed in other groups. The use of moderate-intensity to high-intensity statin therapy was 62.1% (before publication of the guideline) and 66.6% (after publication of the guideline) in the overall cohort, 62.7% (before publication) and 67.0% (after publication) in the ASCVD cohort, 50.6% (before publication) and 52.3% (after publication) in the cohort with elevated low-density lipoprotein cholesterol levels (ie, ≥190 mg/dL), 52.4% (before publication) and 55.2% (after publication) in the diabetes cohort, and 41.9% (before publication) and 46.9% (after publication) in the remaining group with 10-year ASCVD risk of 7.5% or higher. In hierarchical logistic regression models, there was a significant increase in the use of moderate-intensity to high-intensity statins in the overall cohort (4.8%) and in the ASCVD cohort (4.3%) (P < .01 for slope for both). There was no significant change for other risk cohorts. Nonstatin LLT use remained unchanged in the preguideline and postguideline periods in the hierarchical logistic regression models for all of the risk groups.
Conclusions and Relevance
Adoption of the 2013 ACC/AHA Cholesterol Management Guideline in cardiology practices was modest. Timely interventions are needed to improve guideline-concordant practice to reduce the burden of ASCVD.
This study examines trends in use of moderate-intensity and high-intensity statin in US cardiology practices before and after publication of the 2013 American College of Cardiology/American Heart Association Cholesterol Management Guideline.
Introduction
The 2013 American College of Cardiology/American Heart Association (ACC/AHA) Cholesterol Management Guideline recommended statin as the first-line lipid-lowering therapy (LLT) for primary and secondary prevention of atherosclerotic cardiovascular disease (ASCVD). The guideline emphasized using moderate-intensity to high-intensity statin therapy because clinical trials demonstrated greater benefit with more intensive statin therapy, without finding evidence to achieve a particular low-density lipoprotein cholesterol (LDL-C) target. The prior treatment approach from the Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel [ATP III]) guideline recommended achieving target LDL-C levels using any LLT. The 2013 ACC/AHA guideline recommendation represents a major shift.
Statin therapy was underused even in patients with established cardiovascular (CV) disease before publication of the 2013 ACC/AHA guideline. After simplification of the treatment strategy, cholesterol treatment was expected to be easier from the health care professional’s perspective, and moderate-intensity to high-intensity statin therapy use would be accelerated. One study estimated that 12.8 million additional adults would be eligible for statin therapy compared with the ATP III guideline, and this projection was echoed by several other studies. Therefore, understanding national trends in LLT use, particularly moderate-intensity to high-intensity statin and nonstatin LLT, is vital to understanding the potential effect of the 2013 ACC/AHA guideline. However, data related to guideline adoption are limited.
We examined trends in the use of statin therapy (particularly moderate-intensity to high-intensity statins) and nonstatin LLT in patients from cardiology practices participating in the ACC National Cardiovascular Data Registry’s Practice Innovation and Clinical Excellence (PINNACLE) Registry before and after publication of the 2013 ACC/AHA guideline in 4 cohorts expected to benefit the most. We hypothesized that there would be an increasing trend for moderate-intensity to high-intensity statin therapy and a decreasing trend for nonstatin LLT use after publication of the 2013 ACC/AHA guideline in the guideline-specified groups.
Methods
Waiver of written informed consent and authorization for use of the PINNACLE Registry were obtained. Both were granted by Chesapeake Research Review Incorporated, Columbia, Maryland.
Study Populations
The PINNACLE Registry is the first national prospective outpatient CV registry, sponsored by the ACC to improve the quality of care in academic and private cardiology practices. Details of the registry have been previously described. Any patient visiting a cardiology practice participating in the PINNACLE Registry was considered in the present analysis. The 2013 ACC/AHA guideline was first published online on November 12, 2013. We considered the time between September 1, 2012, and November 1, 2013, as the preguideline period and the time between February 1, 2014, and April 1, 2015, as the postguideline period. We excluded data from the transition stage (November 1, 2013, to January 31, 2014). We also excluded 73 practices not participating in the PINNACLE Registry both before and after publication of the 2013 ACC/AHA guideline. We included 161 cardiology practices in our final analyses.
We identified 4 mutually exclusive patient groups who would benefit from LLT. These groups include individuals (1) aged at least 21 years with ASCVD (ASCVD cohort), (2) aged at least 21 years with LDL-C levels 190 mg/dL or higher (elevated LDL-C cohort), (3) aged 40 to 75 years with diabetes without ASCVD and with LDL-C levels 70 to 189 mg/dL (diabetes cohort), and (4) aged 40 to 75 years without ASCVD or diabetes with LDL-C levels 70 to 189 mg/dL and an estimated 10-year ASCVD risk of 7.5% or higher (to convert LDL-C level to millimoles per liter, multiply by 0.0259). Because the ATP III guideline used the Framingham Risk Score (FRS), we also used the FRS to determine LLT eligibility. This latter group included patients without ASCVD and diabetes and with a 10-year FRS of 10% or higher and LDL-C levels of 130 mg/dL or higher, or 10-year FRS less than 10% and LDL-C levels of 160 mg/dL or higher. The group eligible for LLT using the 2013 ACC/AHA guideline or the ATP III guideline is considered the primary prevention cohort for our analysis. Patients were hierarchically assigned to the highest-risk group even if they belonged to a lower-risk category. We considered ASCVD as the presence of any of the following: myocardial infarction, coronary artery disease, peripheral artery disease, stable or unstable angina, ischemic vascular disease, percutaneous transluminal coronary angioplasty, coronary artery bypass grafting, transient ischemic attack, ischemic stroke, or percutaneous coronary intervention with a bare metal stent, drug-eluting stent, or another (nonstent) intervention. After first recognizing patients with ASCVD, we then identified the elevated LDL-C cohort, followed by the diabetes cohort and the primary prevention cohort.
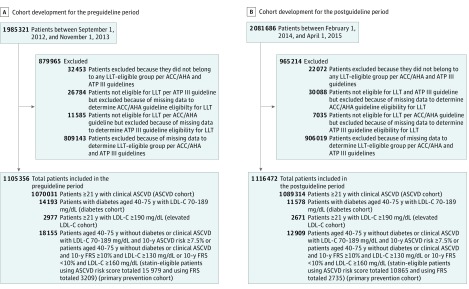
There were initially 1 985 321 patients during the preguideline period and 2 081 686 patients during the postguideline period (Figure 1). After exclusions (the primary reason was missing data to determine LLT eligibility in 42.7% before publication and 45.3% after publication of the 2013 ACC/AHA guideline), the final study populations included 1 105 356 preguideline period patients (2 431 192 patient encounters) and 1 116 472 postguideline period patients (2 377 219 patient encounters). Approximately 97% of patients during each guideline period had ASCVD.
Figure 1. Study Populations Before and After Publication of the 2013 American College of Cardiology/American Heart Association (ACC/AHA) Cholesterol Management Guideline.
A, There were 2 431 192 total patient encounters for patients included in the study in the preguideline period. B, There were 2 377 219 total patient encounters for patients included in the study in the postguideline period. ASCVD indicates atherosclerotic cardiovascular disease; ATP III, Adult Treatment Panel III; FRS, Framingham Risk Score; LDL-C, low-density lipoprotein cholesterol; and LLT, lipid-lowering therapy. To convert LDL-C level to millimoles per liter, multiply by 0.0259.
Study Variables
All variables used in this study were electronically abstracted. If there was more than 1 lipid panel available during each study period, the one with the highest LDL-C level was considered for analysis. Because it is often difficult to ascertain untreated cholesterol levels in contemporary referral-based practices, such as cardiology, we used cholesterol levels documented in electronic medical records to estimate risk irrespective of treatment with LLT.
High-intensity statin therapy corresponds to daily statin dosage that can reduce LDL-C levels by 50% or higher. Moderate-intensity statin therapy corresponds to daily statin dosage that can reduce LDL-C levels by 30% to less than 50%, and low-intensity statin therapy corresponds to statin dosage that can reduce LDL-C levels by less than 30%. Atorvastatin calcium (≥40 mg), rosuvastatin calcium (≥20 mg), and simvastatin (80 mg) were considered high-intensity statins; atorvastatin calcium (≥10 to <40 mg), rosuvastatin calcium (≥5 to <20 mg), simvastatin (≥20 to <80 mg), pravastatin sodium (≥40 mg), lovastatin (≥40 mg), fluvastatin sodium (≥80 mg), and pitavastatin (≥2 mg) were considered moderate-intensity statins; and the remaining statin dosages were considered low-intensity statins. This categorization included statin dosage alone or in combination with any other medication. For the purpose of this study, nonstatin LLT included ezetimibe, bile acid resin, and niacin. Fibrates and ω-3 fatty acids were not considered because of their minimal effect on LDL-C levels.
Prescription of an LLT at any time point during each study period was considered receiving LLT. For example, if nonstatin LLT was added to high-intensity statin therapy (or vice versa) at any time point during each study period, we considered it receipt of both nonstatin LLT and high-intensity statin therapy. If there was more than 1 statin dosage used during a study period, we considered the highest-intensity statin used in that period for our analysis. This approach would capture some information about statin intolerance because patients who were not receiving statin therapy (or were receiving lower-intensity statin therapy) later in the study could have received statin therapy (or higher-intensity statin therapy) earlier.
Statistical Analysis
We assessed baseline characteristics of the overall cohort before and after publication of the 2013 ACC/AHA guideline. We examined monthly trends in the use of moderate-intensity to high-intensity statin and nonstatin LLT using encounter-level data. Using patient-level data during each guideline period, we calculated the proportion of patients receiving low, moderate, high, and combined moderate-intensity to high-intensity statin therapy, as well as nonstatin LLT, and the proportion of patients not receiving any LLT. For a patient with multiple visits during a study period, we used the most recent visit to determine baseline characteristics. We used the t test for continuous variables and the χ2 test for categorical variables. As our primary outcome, we developed hierarchical logistic regression models using interrupted time series analysis to formally assess whether publication of the 2013 ACC/AHA guideline was associated with a differential trend in the use of moderate-intensity to high-intensity statin and nonstatin LLT. In each model, we allowed different slopes and intercepts during each period. The slope examines percentage LLT use over time, and the intercept assesses difference in LLT use at the starting point of the postguideline period . If the intercepts were statistically different, this result would imply an abrupt shift in LLT use at the beginning of the postguideline period. If the slopes were statistically different, this result would indicate an acceleration or deceleration in LLT use after publication of the 2013 ACC/AHA guideline. In that case, we quantified the absolute change in LLT use by estimating the predicted use of moderate-intensity to high-intensity statin and nonstatin LLT at the middle of the postguideline period using postguideline slope and intercept and compared it with the predicted use via preguideline slope and intercept. If neither the slope nor the intercept was significantly different, then this result would indicate no significantly different trend in LLT use between the 2 periods.
We found that most missing data were lacking LDL-C levels (93% of all excluded patients). To understand whether missing LDL-C levels were related primarily to patient-level factors or to cardiology practice, we calculated C statistics from 2 logistic models to predict the likelihood of missing LDL-C levels. One model included only patient-related factors as predictors (age, race, sex, health insurance status, body mass index, systolic and diastolic blood pressure, current smoking status, and hypertension), and the second model further included cardiology practice. In sensitivity analyses, we repeated the primary analyses using inverse probability weighting, which assigns higher weight to patients who were similar to those with missing LDL-C levels. Weights were calculated from a logistic regression model that included patient-level factors and cardiology practice, as described above. This analysis was performed in all groups except the ASCVD cohort because the presence of ASCVD qualifies for LLT regardless of LDL-C levels. Finally, the 2013 ACC/AHA guideline did not find sufficient information to base recommendations for or against statin therapy in patients with heart failure. Therefore, we examined statin use after excluding patients with heart failure from the ACC/AHA primary prevention cohort.
All analyses were evaluated at a 2-sided significance level of .05. Statistical analyses were performed using a software program (SAS, version 9.3; SAS Institute Inc).
Results
In the study cohort, the mean (SD) age was 69.6 (12.1) years before publication of the 2013 ACC/AHA guideline and 70.0 (11.9) years after publication of the 2013 ACC/AHA guideline (Table). The mean (SD) body mass index (calculated as weight in kilograms divided by height in meters squared) was 30.4 (8.8) in the preguideline period and 30.3 (8.3) in the postguideline period, with 86.7% having hypertension in the preguideline period and 86.8% having hypertension during the postguideline period. In the preguideline period, the mean (SD) number of LDL-C level assessments per patient was 0.5 (0.8) and in the postguideline period, the mean (SD) number of LDL-C level assessments per patient was 0.4 (0.7). LDL-C levels were missing in 64.7% of the preguideline period and 70.8% of the postguideline period. Most other variables were distributed similarly.
Table. Characteristics of Patients Before and After Publication of the 2013 American College of Cardiology/American Heart Association Cholesterol Management Guideline.
| Characteristic | Preguideline Period (n = 1 105 356) |
Postguideline Period (n = 1 116 472) |
|---|---|---|
| Age, mean (SD), y | 69.6 (12.1) | 70.0 (11.9) |
| White race, % | 91.2 | 92.1 |
| Women, % | 40.2 | 39.8 |
| No health insurance, % | 0.4 | 0.3 |
| BMI, mean (SD) | 30.4 (8.8) | 30.3 (8.3) |
| Blood pressure, mean (SD), mm Hg | ||
| Systolic | 128.3 (17.4) | 128.9 (17.4) |
| Diastolic | 73.6 (10.6) | 73.8 (10.6) |
| Current smoker, % | 16.5 | 16.5 |
| Hypertension, % | 86.7 | 86.8 |
| Cholesterol level, mean (SD), mg/dL | ||
| Total cholesterol | 163.3 (42.4) | 163.3 (42.7) |
| LDL-C | 89.0 (36.4) | 88.2 (36.8) |
| HDL-C | 48.2 (15.4) | 49.0 (15.9) |
| No. of LDL-C assessments per patient, mean (SD) | 0.5 (0.8) | 0.4 (0.7) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
SI conversion factor: To convert cholesterol levels to millimoles per liter, multiply by 0.0259.
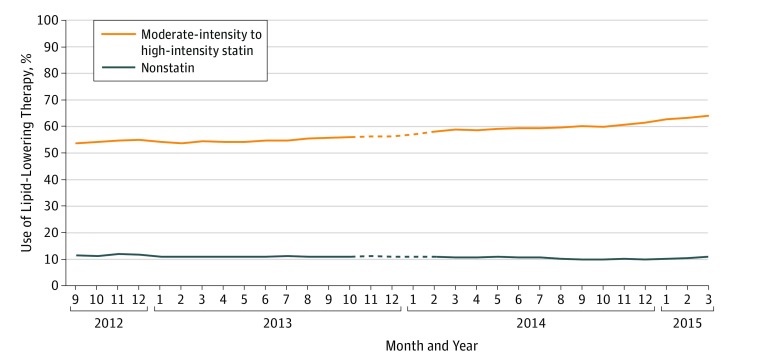
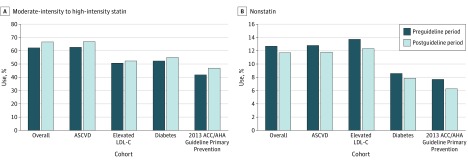
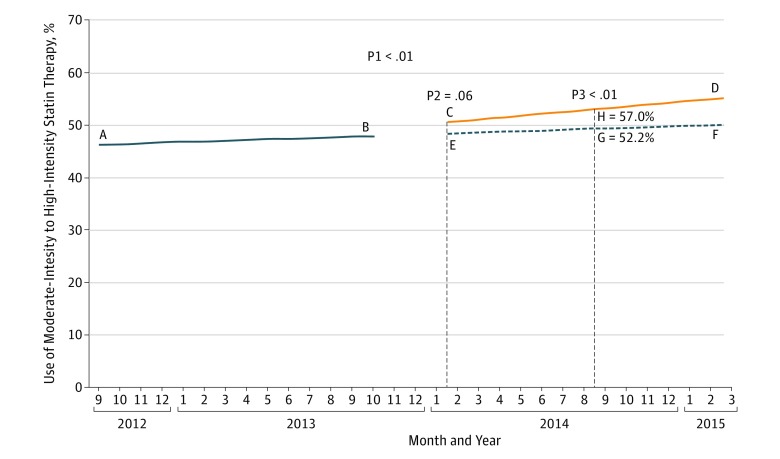
In the overall cohort, there was an increasing trend in moderate-intensity to high-intensity statin use after publication of the 2013 ACC/AHA guideline, but such a trend was already present before publication of the guideline (Figure 2). Before publication of the guideline, 62.1% of patients were receiving moderate-intensity to high-intensity statin therapy, which increased to 66.6% after publication of the guideline (Figure 3A). Further details by statin intensity are listed in the eTable in the Supplement. There was no discernible changing trend in nonstatin LLT use (Figure 2). Before publication of the guideline, 12.7% of the cohort were receiving nonstatin LLT, which decreased to 11.7% after publication of the guideline (Figure 3B). The proportion of patients not receiving any LLT was 29.1% before publication of the guideline and 24.1% after publication of the guideline (eFigure 1 in the Supplement). In hierarchical logistic regression models, there was a significant increase in moderate-intensity to high-intensity statin use in the postguideline period (ie, higher slope [P < .01]) (Figure 4). The predicted use of moderate-intensity to high-intensity statin therapy at the middle of the postguideline period using preguideline and postguideline models was 52.2% and 57.0%, respectively (difference of 4.8%, P < .01). There was no significant difference in the slope (P = .41) or intercept (P = .11) for nonstatin LLT, suggesting no significant difference in nonstatin LLT use.
Figure 2. Observed Trends in the Use of Moderate-Intensity to High-Intensity Statin and Nonstatin Lipid-Lowering Therapy in the Overall Cohort.
The dashed line indicates the transition period. There were 2 431 192 total patient encounters before publication of the 2013 American College of Cardiology/American Heart Association Cholesterol Management Guideline. There were 2 377 219 total patient encounters after publication of the 2013 ACC/AHA Cholesterol Management Guideline.
Figure 3. Overall Use for the Preguideline and Postguideline Periods.
ACC/AHA indicates American College of Cardiology/American Heart Association; ASCVD, atherosclerotic cardiovascular disease; and LDL-C, low-density lipoprotein cholesterol.
Figure 4. Model Estimated Use of Moderate-Intensity to High-Intensity Statin Therapy in the Overall Cohort.
Line A to B, Moderate-intensity to high-intensity statin use for the preguideline period. Line C to D, Moderate-intensity to high-intensity statin use for the postguideline period. Line E to F, Projected moderate-intensity to high-intensity statin use for the postguideline period using preguideline data. G, Estimated moderate-intensity to high-intensity statin use at the middle of the postguideline period (ie, September 2014) using preguideline data. H, Estimated moderate-intensity to high-intensity statin use at the middle of the postguideline period (ie, September 2014) using postguideline data. P1 is the P value for difference in the rate of use of statin therapy between the preguideline and postguideline periods (ie, difference in slope). P2 is the P value for difference in the rate of use of statin therapy at the starting point of the postguideline period (ie, February 2014) (ie, difference in intercept). P3 is the P value for difference in the rate of use of statin therapy at the middle of the postguideline period (ie, September 2014) using preguideline vs postguideline data. Line E to F is dashed to show that it is based on projection of preguideline data. The first vertical dashed line indicates the beginning of the preguideline period, and the second vertical dashed line indicates the middle of the postguideline period.
There was an increasing trend in moderate-intensity to high-intensity statin use in the ASCVD cohort, but this trend was also present before publication of the 2013 ACC/AHA guideline (eFigure 2 in the Supplement). The proportion of patients receiving moderate-intensity to high-intensity statin therapy before publication of the guideline was 62.7% and the proportion of patients receiving moderate-intensity to high-intensity statin therapy after publication of the guideline was 67.0%. The proportion of patients receiving nonstatin LLT before publication of the ACC/AHA guideline was 12.8% and after publication of the ACC/AHA guideline was 11.8% (Figure 3). Treatment patterns by statin intensity are listed in the eTable in the Supplement. The proportion of patients not receiving any LLT was 22.0% before publication of the guideline and 19.3% after publication of the guideline (eFigure 1 in the Supplement). In hierarchical logistic regression models, there was a shift in moderate-intensity to high-intensity statin use at the beginning of the postguideline period using postguideline data compared with preguideline data (ie, P = .01 for intercept). Furthermore, there was a significant increase in moderate-intensity to high-intensity statin use in the postguideline period compared with the preguideline period (ie, higher slope [P < .01]). The estimated moderate-intensity to high-intensity statin use at the middle of the postguideline period using preguideline and postguideline models was 53.4% and 57.7%, respectively (difference of 4.3%, P < .01). There was no significant difference in nonstatin LLT use before and after publication of the guideline in the hierarchical logistic regression models (P > .05 for slope and intercept).
There was no observable changing trend in moderate-intensity to high-intensity statin or nonstatin LLT use in the elevated LDL-C cohort (eFigure 3 in the Supplement). The use of moderate-intensity to high-intensity statin and nonstatin LLT and the nonuse of LLT was similar during the preguideline and postguideline periods (Figure 3 and eTable and eFigure 1 in the Supplement). Hierarchical logistic regression models did not show significant differences in moderate-intensity to high-intensity statin or nonstatin LLT use (P > .05 for all). Results were similar for the diabetes cohort, 2013 ACC/AHA guideline primary prevention cohort, and the ATP III guideline primary prevention cohort (Figure 3 and eTable and eFigures 1, 4, 5, 6, and 7 in the Supplement).
In sensitivity analyses, C statistics were 0.56 for the model with only patient-level factors and 0.78 when the model further included cardiology practice, suggesting that cardiology practice was highly associated with missing LDL-C levels. Results from inverse probability weighting were similar to those of the main analyses. Among 14 087 patients without heart failure in the preguideline period, the use of any statin therapy was 50.8%. Among 9309 patients without heart failure in the postguideline period, the use of any statin therapy was 55.2% (eTable in the Supplement).
Discussion
Within the PINNACLE Registry, a large national cardiology outpatient registry, we found a modest increase in moderate-intensity to high-intensity statin prescription after publication of the 2013 ACC/AHA guideline in the ASCVD cohort but not in other guideline-recommended groups. Nonstatin LLT prescription did not change. One-third of patients with ASCVD and almost one-half without ASCVD were not receiving guideline-recommended moderate-intensity to high-intensity statin therapy after the publication of the 2013 ACC/AHA guideline.
A recent study evaluating patients enrolled in a single health plan did not show an appreciable change in statin use after publication of the 2013 ACC/AHA guideline in patients with ASCVD (net 1.4% increase) or in patients with diabetes (net 2.4% increase). In a study from the Department of Veterans Affairs, high-intensity statin use in patients with ASCVD increased by 6% after publication of the 2013 ACC/AHA guideline. The duration for both of these studies was limited to 6 months before and after publication of the 2013 ACC/AHA guideline, and LLT use was not examined in all 4 patient groups. Another study showed that publication of the 2013 ACC/AHA guideline was not associated with increased statin use. We examined time trends, statin intensities, and nonstatin LLT use 14 months before and after publication of the 2013 ACC/AHA guideline in all 4 cohorts. While it can take up to 17 years for evidence to be fully implemented in clinical practice, our study shows the minimal effect associated with the publication of the 2013 ACC/AHA guideline on cardiology practice.
The expected trend in nonstatin LLT use was not clear in patients with LDL-C levels 190 mg/dL or higher because these patients may require nonstatin LLT after maximal statin therapy. We found no significant change in trend in nonstatin LLT use or moderate-intensity to high-intensity statin use in this group.
Simplification of statin-based treatment approaches by the 2013 ACC/AHA guideline was expected to make cholesterol treatment straightforward and to increase evidence-based statin use. Using data from the National Health and Nutrition Examination Surveys, the number of individuals eligible for statin therapy after publication of the 2013 ACC/AHA guideline was estimated to increase by 2.4 million in patients with ASCVD, by 2.2 million in patients with diabetes, and by 8.2 million in patients in whom statins would be used for primary prevention. We found that, despite a modest effect of the guideline in patients with ASCVD, the change in statin use was less than the eligibility estimates, suggesting incomplete adoption of the 2013 ACC/AHA guideline. While the largest increase in statin eligibility was predicted for patients without ASCVD, our analyses did not show such an increase in statin use.
Full application of the 2013 ACC/AHA guideline was expected to decrease the number of new ASCVD events by 450 000 during 10 years. Although eligible for statin therapy, 258 721 patients with ASCVD and 9742 patients without ASCVD in our analysis were not receiving statin therapy during the postguideline period. In addition, 20% to 40% of patients in the postguideline period were not receiving any LLT. Assuming that statin therapy reduces the relative risk for CV events during 5 years by 30% in patients with clinical ASCVD and by 25% in patients without ASCVD, guideline-concordant statin therapy could potentially prevent 77 616 additional CV events in those with ASCVD and 2435 additional CV events in those without ASCVD among patients included in the present analysis alone. This benefit highlights the importance of timely interventions in guideline dissemination.
Compared with the ATP III guideline, the 2013 ACC/AHA guideline represented a paradigm shift by recommending an approach based on statin dosage rather than on LDL-C target and has been the subject of controversy. However, it is possible that health care professionals were already using an approach based on statin intensity before publication of the 2013 ACC/AHA guideline, which could explain our findings. However, previous analyses have shown that undertreatment was common in real-world practice before publication of the 2013 ACC/AHA guideline, and we found that it has improved minimally under the new guideline. In a separate study, our group found significant gaps among clinicians in their understanding of the 2013 ACC/AHA guideline, such that only 48% of practicing health care professionals had read the 2013 ACC/AHA guideline, 50% knew the 4 patient groups who would benefit from statin use, and 29% knew the definitions of statin intensity. It is unclear how much of the current trend in LLT use and LDL-C level assessments is a result of lack of understanding or a disagreement with the 2013 ACC/AHA guideline. Future research should focus on barriers to adoption of the cholesterol guideline and mitigation of such barriers. Using a case-based educational intervention to target gaps at the clinician level, our group found remarkable improvement in the knowledge of health care professionals regarding the new guideline, suggesting a role of such activities for guideline dissemination.
Limitations
Our study has several limitations. The 2013 ACC/AHA guideline highlighted the importance of shared decision making, recommending a clinician-patient discussion regarding patient preference and the benefits and potential harms of LLT. It is possible that after their risk-benefit discussion some patients may have opted not to receive LLT, particularly statins. Although this issue is important, our analyses could not account for it. Lower statin use could be partly related to statin intolerance, for which data were not collected. However, we believe that our approach of considering the highest statin dosage prescribed should account for some statin intolerance. In routine practice, statin intolerance can range from 10% to 15%; therefore, statin intolerance alone may not fully explain the large gap in recommended vs actual statin use. Most of our missing data were lacking LDL-C levels. In sensitivity analyses, we found that missing LDL-C levels were mostly explained by cardiology practice rather than patient-related factors, which could be due to incomplete mapping of referral records for decision making that is not reflected in electronic health records. However, results from sensitivity analyses were similar. We used cholesterol levels from electronic medical records irrespective of treatment, which should not affect results for the ASCVD cohort but could have underestimated statin eligibility in other cohorts (eg, if a patient at baseline was prescribed statin therapy but he or she no longer appeared to be eligible for statin therapy when we assessed the patient because of lower cholesterol levels). Although representing an appropriate treatment, such a patient would be dropped from the denominator, resulting in underestimation of the percentage appropriately treated. Because our study was based on a cardiology practice registry, most patients were receiving LLT for ASCVD. Therefore, despite a sizable number of patients in each of the 4 cohorts, better assessment for adoption of the 2013 ACC/AHA guideline in patients without ASCVD would require a database in which these groups were more completely represented.
Conclusions
Despite the anticipated increase in statin-eligible patients after publication of the 2013 ACC/AHA Cholesterol Management Guideline, the use of moderate-intensity to high-intensity statin therapy in cardiology practices has increased only modestly in patients with ASCVD, with no significant change in other risk groups. Nonstatin LLT use remained unchanged. One-third to one-half of eligible patients were not receiving evidence-based moderate-intensity to high-intensity statin therapy after publication of the 2013 ACC/AHA guideline. More aggressive interventions are needed to improve guideline-directed statin prescribing.
eTable. Overall Use of Statin and Its Dose Intensity During Each Guideline Period
eFigure 1. Eligible Patients Not on Any Lipid-Lowering Therapy During Each Guideline Period
eFigure 2. Trends in the Use of Moderate-High Intensity Statin and Non-statin LLT in Patients ≥21 Years With ASCVD
eFigure 3. Trends in the Use of Moderate-High Intensity Statin and Non-statin LLT in Patients ≥21 Years With LDL-C≥190 mg/dL
eFigure 4. Trends in the Use of Moderate-High Intensity Statin and Non-statin LLT in 40-75 Years Old Diabetic Patients With LDL-C 70-189 mg/dL and Without ASCVD
eFigure 5. Trends in the Use of Moderate-High Intensity Statin and Non-statin LLT in 40-75 Years Old Primary Prevention Cohort With 10 Year ASCVD Risk ≥7.5% and LDL-C 70-189 mg/dL, and Without Diabetes
eFigure 6. Trends in the Use of Moderate-High Intensity Statin and Non-statin LLT in 40-75 Years Old Primary Prevention Cohort With 10 Year FRS≥10% and LDL-C≥130 mg/dL or 10 Year FRS<10% and LDL-C≥160 mg/dL
eFigure 7. Overall Use of LLT During Each Guideline Period in the ATP III Primary Prevention Cohort
References
- 1.Stone NJ, Robinson JG, Lichtenstein AH, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25, PtB):2889-2934. [DOI] [PubMed] [Google Scholar]
- 2.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486-2497. [DOI] [PubMed] [Google Scholar]
- 3.Arnold SV, Spertus JA, Tang F, et al. Statin use in outpatients with obstructive coronary artery disease. Circulation. 2011;124(22):2405-2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ioannidis JP. More than a billion people taking statins? potential implications of the new cardiovascular guidelines. JAMA. 2014;311(5):463-464. [DOI] [PubMed] [Google Scholar]
- 5.Pencina MJ, Navar-Boggan AM, D’Agostino RB Sr, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370(15):1422-1431. [DOI] [PubMed] [Google Scholar]
- 6.Schoen MW, Salas J, Scherrer JF, Buckhold FR. Cholesterol treatment and changes in guidelines in an academic medical practice. Am J Med. 2015;128(4):403-409. [DOI] [PubMed] [Google Scholar]
- 7.Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382(9907):1762-1765. [DOI] [PubMed] [Google Scholar]
- 8.Yeboah J, Sillau S, Delaney JC, et al. Implications of the new American College of Cardiology/American Heart Association cholesterol guidelines for primary atherosclerotic cardiovascular disease event prevention in a multi ethnic cohort: Multi-Ethnic Study of Atherosclerosis (MESA). Am Heart J. 2015;169(3):387-395.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan PS, Oetgen WJ, Buchanan D, et al. Cardiac performance measure compliance in outpatients: the American College of Cardiology and National Cardiovascular Data Registry’s PINNACLE (Practice Innovation and Clinical Excellence) program. J Am Coll Cardiol. 2010;56(1):8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Virani SS, Woodard LD, Ramsey DJ, et al. Gender disparities in evidence-based statin therapy in patients with cardiovascular disease. Am J Cardiol. 2015;115(1):21-26. [DOI] [PubMed] [Google Scholar]
- 11.Virani SS, Woodard LD, Akeroyd JM, Ramsey DJ, Ballantyne CM, Petersen LA. Is high-intensity statin therapy associated with lower statin adherence compared with low- to moderate-intensity statin therapy? implications of the 2013 American College of Cardiology/American Heart Association Cholesterol Management Guidelines. Clin Cardiol. 2014;37(11):653-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenson RS, Kent ST, Brown TM, et al. Underutilization of high-intensity statin therapy after hospitalization for coronary heart disease. J Am Coll Cardiol. 2015;65(3):270-277. [DOI] [PubMed] [Google Scholar]
- 13.Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13(6)(suppl):S38-S44. [DOI] [PubMed] [Google Scholar]
- 14.Tran JN, Kao TC, Caglar T, et al. Impact of the 2013 cholesterol guideline on patterns of lipid-lowering treatment in patients with atherosclerotic cardiovascular disease or diabetes after 1 year. J Manag Care Spec Pharm. 2016;22(8):901-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodriguez F, Lin S, Maron DJ, Knowles JW, Virani SS, Heidenreich PA. Use of high-intensity statins for patients with atherosclerotic cardiovascular disease in the Veterans Affairs Health System: Practice impact of the new cholesterol guidelines. Am Heart J. 2016;182:97-102. [DOI] [PubMed] [Google Scholar]
- 16.Gaskin FS, Iyengar R, Eatherly M, et al. Impact of new ACC/AHA cholesterol treatment guidelines on statin utilization patterns in the United States. J Am Coll Cardiol. 2016;67(13)(suppl):1962. Abstract 1191-388. [Google Scholar]
- 17.Committee on Quality of Health Care in America, Institute of Medicine Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 18.Miedema MD, Lopez FL, Blaha MJ, et al. Eligibility for statin therapy according to new cholesterol guidelines and prevalent use of medication to lower lipid levels in an older US cohort: the Atherosclerosis Risk in Communities Study Cohort. JAMA Intern Med. 2015;175(1):138-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeFilippis AP, Young R, Carrubba CJ, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;162(4):266-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association Cholesterol Management Guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2015;66(15):1657-1668. [DOI] [PubMed] [Google Scholar]
- 21.Pursnani A, Massaro JM, D’Agostino RB Sr, O’Donnell CJ, Hoffmann U. Guideline-based statin eligibility, coronary artery calcification, and cardiovascular events. JAMA. 2015;314(2):134-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naci H, Brugts JJ, Fleurence R, Tsoi B, Toor H, Ades AE. Comparative benefits of statins in the primary and secondary prevention of major coronary events and all-cause mortality: a network meta-analysis of placebo-controlled and active-comparator trials. Eur J Prev Cardiol. 2013;20(4):641-657. [DOI] [PubMed] [Google Scholar]
- 23.Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;1(1):CD004816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amin NP, Martin SS, Blaha MJ, Nasir K, Blumenthal RS, Michos ED. Headed in the right direction but at risk for miscalculation: a critical appraisal of the 2013 ACC/AHA risk assessment guidelines. J Am Coll Cardiol. 2014;63(25, pt A):2789-2794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ray KK, Kastelein JJ, Boekholdt SM, et al. The ACC/AHA 2013 guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: the good the bad and the uncertain: a comparison with ESC/EAS guidelines for the management of dyslipidaemias 2011. Eur Heart J. 2014;35(15):960-968. [DOI] [PubMed] [Google Scholar]
- 26.Virani SS, Pokharel Y, Steinberg L, et al. Provider understanding of the 2013 ACC/AHA cholesterol guideline. J Clin Lipidol. 2016;10(3):497-504.e4. doi:10.1016/j.jacl.2015.11.002 [DOI] [PubMed] [Google Scholar]
- 27.Pokharel Y, Steinberg L, Chan W, et al. Case-based educational intervention to assess change in providers’ knowledge and attitudes towards the 2013 American College of Cardiology/American Heart Association cholesterol management guideline. Atherosclerosis. 2016;246:115-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Banach M, Rizzo M, Toth PP, et al. Statin intolerance: an attempt at a unified definition: position paper from an international lipid expert panel. Arch Med Sci. 2015;11(1):1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Overall Use of Statin and Its Dose Intensity During Each Guideline Period
eFigure 1. Eligible Patients Not on Any Lipid-Lowering Therapy During Each Guideline Period
eFigure 2. Trends in the Use of Moderate-High Intensity Statin and Non-statin LLT in Patients ≥21 Years With ASCVD
eFigure 3. Trends in the Use of Moderate-High Intensity Statin and Non-statin LLT in Patients ≥21 Years With LDL-C≥190 mg/dL
eFigure 4. Trends in the Use of Moderate-High Intensity Statin and Non-statin LLT in 40-75 Years Old Diabetic Patients With LDL-C 70-189 mg/dL and Without ASCVD
eFigure 5. Trends in the Use of Moderate-High Intensity Statin and Non-statin LLT in 40-75 Years Old Primary Prevention Cohort With 10 Year ASCVD Risk ≥7.5% and LDL-C 70-189 mg/dL, and Without Diabetes
eFigure 6. Trends in the Use of Moderate-High Intensity Statin and Non-statin LLT in 40-75 Years Old Primary Prevention Cohort With 10 Year FRS≥10% and LDL-C≥130 mg/dL or 10 Year FRS<10% and LDL-C≥160 mg/dL
eFigure 7. Overall Use of LLT During Each Guideline Period in the ATP III Primary Prevention Cohort