Abstract
Background
Asthma disproportionately affects minority populations and is associated with psychosocial stress such as racial/ethnic discrimination. We aimed to examine the association of perceived discrimination with asthma and poor asthma control in African American and Latino youth.
Methods
We included African American (n = 954), Mexican American (n = 1,086), other Latino (n = 522), and Puerto Rican Islander (n = 1,025) youth aged 8 to 21 years from the Genes-Environments and Admixture in Latino Americans study and the Study of African Americans, Asthma, Genes, and Environments. Asthma was defined by physician diagnosis, and asthma control was defined based on the National Heart, Lung, and Blood Institute guidelines. Perceived racial/ethnic discrimination was assessed by the Experiences of Discrimination questionnaire, with a focus on school, medical, and public settings. We examined the associations of perceived discrimination with each outcome and whether socioeconomic status (SES) and global African ancestry modified these associations.
Results
African American children reporting any discrimination had a 78% greater odds of experiencing asthma (OR, 1.78; 95% CI, 1.33-2.39) than did those not reporting discrimination. Similarly, African American children faced increased odds of poor asthma control with any experience of discrimination (OR, 1.97; 95% CI, 1.42-2.76) over their counterparts not reporting discrimination. These associations were not observed among Latino children. We observed heterogeneity of the association between reports of discrimination and asthma according to SES, with reports of discrimination increasing the odds of having asthma among low-SES Mexican American youth (interaction P = .01) and among high-SES other Latino youth (interaction P = .04).
Conclusions
Perceived discrimination is associated with increased odds of asthma and poorer control among African American youth. SES exacerbates the effect of perceived discrimination on having asthma among Mexican American and other Latino youth.
Key Words: children, health status disparity, psychosocial stress, race, socioeconomic status
Abbreviations: GALA II, Genes-Environments and Admixture in Latino Americans; NHLBI, National Heart, Lung, and Blood Institute; SES, socioeconomic status; SAGE II, Study of African Americans, Asthma, Genes, and Environments
Racial/ethnic discrimination, an interpersonal form of racism, is characterized as differential treatment or biased attitudes directed toward individuals on the sole basis of their race, color, national or ethnic origin, or immigrant status.1 These experiences are known to elicit emotional responses, ranging from anger and social rejection to chronic vigilance,2, 3, 4 resulting in a concern of constant harm5 and thus a source of psychosocial stress.6 Given the complex history of racial/ethnic relations in the United States,7 the prevalence and severity of discriminatory experiences varies across groups, with African Americans and Latinos being more affected.8, 9 Discrimination has been linked to poor mental health outcomes, including depression10 and substance abuse,11 in youth. Unlike the well-known association between perceived discrimination and physical health in adults,12, 13 this association is less known in children.14, 15
Asthma, a common childhood condition, varies across racial/ethnic groups, with African American and Puerto Rican children carrying the greatest burden.16, 17 Evidence suggests that psychosocial stress is an important contributor to asthma exacerbations.18 In fact, the Black Women’s Health Study demonstrated that women scoring in the highest quartile of perceived discrimination had an increased incidence of adult-onset asthma.19 However, the role of discrimination in childhood asthma has not been well established.
In addition to an individual’s race/ethnicity,9, 20 socioeconomic status (SES) may also impact the perception of discrimination in everyday experiences.21 SES may shape the exposure to racially biased treatment in receiving and accessing medical care22, 23 and to environmental risk factors.24, 25 Therefore, we expect that the relationship between perceived discrimination and asthma may vary with SES. Moreover, within a racial/ethnic group, the experiences of discrimination may vary widely based on an individual’s skin color. Therefore, African ancestry, a known contributor to skin color,26, 27 may affect the degree of discrimination an individual may encounter.28 African ancestry is also associated with asthma and worse pulmonary function in African Americans and Latinos.29, 30 Thus, it is possible that African ancestry may modify the role of experiences of discrimination on asthma-related outcomes.
Our study examined the association of perceived discrimination with asthma outcomes in a multicenter case-control study of African American and Latino youth in the mainland United States and Puerto Rico. Because asthma and discrimination vary with race/ethnicity, these associations are examined within each racial/ethnic group.14, 15, 16, 17 In addition, we aimed to study whether African ancestry and SES modified the associations between perceived discrimination and each asthma outcome examined (having asthma and poor asthma control).
Methods
Study Population
Participants are from the Genes-Environment and Admixture in Latino Americans (GALA II) study and the Study of African Americans, Asthma, Genes, and Environments (SAGE II). These are identical asthma case-control studies designed to examine complex genetic and socioenvironmental contributors to asthma prevalence and morbidity. The GALA II and SAGE II recruited Latino and African American youth, respectively, with and without asthma aged 8 to 21 years of age from the mainland United States (San Francisco Bay Area, Houston, Chicago, and New York) and Puerto Rico (San Juan, Puerto Rico) from 2006 to 2014. Survey respondents (participants < 16 years) or the participants (≥ 16 years) must have self-identified all four grandparents of the participant as Latino (GALA II) or African American (SAGE II) to be eligible for the study. Further details regarding eligibility criteria for the studies are described elsewhere.25 Written age-appropriate informed consent/assent was obtained from all participants and their legal guardians. The University of California, San Francisco (UCSF) and each study site's institutional review board (IRB) approved the SAGE II/GALA II protocol (SAGE II UCSF-IRB No. 10-02877, Reference No. 155745; GALA II UCSF-IRB No. 10-00889, Reference No.164561).
Outcome Assessments
Asthma
Asthma was defined by physician diagnosis and report of symptoms and medication use within the 2 years prior to recruitment. Within each catchment area, control subjects were frequency matched to case subjects by the hospital or community clinic site of recruitment. Eligible control subjects had no reported history of asthma, lung disease, or chronic illness and no reported symptoms of wheezing or shortness of breath (e-Table 1).
Asthma control
The National Heart, Lung, and Blood Institute (NHLBI) definition of asthma control is a composite score and the accepted standard to measure control.31 Asthma control was derived from information collected through a modified version of the 1978 American Thoracic Society–Division of Lung Diseases Epidemiology Questionnaire on symptoms, nighttime awakening, interference with normal activities, and rescue medication use during the week prior to participant recruitment and interview, as well as lung function measurements.32 Asthma control was defined for this analysis as controlled, partially controlled, or poorly controlled33 (e-Table 2).
Assessment of Perceived Discrimination
Perceived discrimination was ascertained using a modified version of the Experiences of Discrimination (EOD) questionnaire by asking selected questions directed to the participant, with the parent/caretaker’s permission and input.34 Consistent with previous studies,14, 35 we included questions pertinent to pediatric populations: “Have you ever experienced discrimination, been prevented from doing something, or been hassled or made to feel inferior, in any of the following situations because of your race, ethnicity, color, or language: (1) at school, (2) getting medical care, (3) getting services in a store or restaurant, and (4) on the street or in a public setting? The choice for each question was yes or no. Experiences of discrimination were defined as none or any (affirmative answer to at least one situation) and also categorized as never (negative answer to all four situations), rarely (affirmative answer to one or two situations), and often (affirmative answer to three or more situations).36
Covariates
Race/ethnicity was categorized as follows: African American, Mexican American, Puerto Rican, and other Latino (e-Appendix 1). For Latinos, the mother’s preferred spoken language was included as a confounder. In addition, for other Latino participants, a variable capturing the child’s Latino subgroup (ie, multiple Latino origin, Central American, South American, or Caribbean) was considered to account for variation within the category. Recruitment site was included as a covariate.
Informed by previous studies,33, 36 age, sex, current and in utero smoke exposure (ie, maternal smoking during pregnancy), history of breastfeeding, early-life daycare attendance, and reports of visible water damage or mold were considered confounders for the analyses. To capture SES, we used a composite index37, 38 composed of the following variables: maternal education, reported annual household income, and insurance status. Each participant’s ancestry was determined using the software program package ADMIXTURE and assuming three ancestral populations (African, Native American, and European). We focused on African ancestry and classified individuals as high/low ancestry using the population mean as a cut point for each racial/ethnic group (e-Appendix 1).
For participants with asthma, the brief medication questionnaire39 was used to ascertain reported controller medication use and included this variable as a covariate when examining asthma control. Controller medication use was defined as the report of inhaled corticosteroid, leukotriene inhibitor, or long-acting beta-agonist use in the 2 weeks prior to recruitment.
As of 2014, of the 1,370 and 4,236 eligible participants in SAGE II and GALA II, respectively, we excluded those with missing info on discrimination (n = 542), SES (n = 1,121), global African ancestry (n = 315), or other covariate (n = 41). These exclusions yielded final analytical sample sizes of 954 for SAGE II and 2,633 for GALA II. When compared with participants included in the analysis, excluded participants were more likely to be older (13.9 years vs 12.6 years; P < .001), to report current tobacco smoke exposure (26.0% vs 22.1%; P < .001), to be Puerto Rican Islander (38.5% vs 28.6%; P < .001), and to have asthma (39.6% vs 32.6%; P < .001).
Statistical Analysis
Descriptive statistics for case subjects and control subjects were examined according to race/ethnicity. Differences and associations were determined using the Student t test for continuous variables with a normal distribution, the Kruskal-Wallis test for continuous nonnormally distributed variables, and the χ2square test for categorical variables.
We used logistic regression models to quantify the association between the report of perceived discrimination (none/any) and asthma status (asthma yes/no) in each racial/ethnic group. This analysis was repeated with severity of discrimination (never, rarely, often) as an ordinal variable to examine for linear trend. Covariates significantly associated with asthma status (P < .2) were included in the final model. To determine whether the association between perceived discrimination (none vs any) and asthma varies with SES and proportion of African ancestry, interaction terms were tested in the final model for each racial/ethnic group.
After meeting the proportional assumption in each racial/ethnic group, ordinal logistic regression was used to estimate the association between perceived discrimination (none/any) with asthma control (controlled, partially controlled, and poorly controlled asthma) among participants with asthma (e-Appendix 1). This analysis was repeated with severity of discrimination (never, rarely, often) as an ordinal variable to examine for linear trend. Finally, interaction terms of perceived discrimination with SES and proportion of African ancestry were tested in the final model for each racial/ethnic group. Significance of main effects and interaction effects were determined at P = .05. All analyses were conducted with R, version 3.3.0.40
Results
Baseline Study Characteristics
Participants with asthma were younger and more likely to be male subjects compared with participants without asthma, regardless of racial/ethnic group (Table 1). African American participants with asthma were more likely to be from low-income households and have a low SES composite score, be under-insured and report greater discrimination than their counterparts without asthma (all P < .05). For Mexican Americans, those with asthma were more likely to be of high SES, have mothers with higher educational attainment and have better health insurance coverage (all P < .05) than those without asthma. No associations with SES composite index were observed in the other Latino or Puerto Rican groups. Reports of discrimination by situation and asthma status for each race/ethnic group are presented in e-Table 3.
Table 1.
Selected Characteristics of Participants From the SAGE II and GALA II According to Racial/Ethnic Group: 2006-2014
| Variable | African American |
Mexican American |
Other Latino |
Islander Puerto Rican |
||||
|---|---|---|---|---|---|---|---|---|
| Control Subject | Case Subject | Control Subject | Case Subject | Control Subject | Case Subject | Control Subject | Case Subject | |
| No. | 360 | 594 | 553 | 533 | 244 | 278 | 489 | 536 |
| Age, median (IQR), y | 15.7(5.85) | 13.5 (5.81) | 13.4 (6.45) | 12.3 (5.38) | 13.8 (4.98) | 11.7 (4.68) | 12.2 (3.71) | 11.2 (3.33) |
| Sex, male | 141 (39.2) | 310 (52.2) | 222 (40.1) | 300 (56.3) | 109 (44.7) | 156 (56.1) | 227 (46.4) | 315 (58.8) |
| Tobacco exposure | ||||||||
| Current | 123 (34.2) | 164 (27.6) | 122 (22.1) | 103 (19.3) | 40 (16.4) | 57 (20.5) | 85 (17.4) | 100 (18.7) |
| In utero | 48 (13.3) | 121 (20.4) | 12 (2.2) | 21 (3.9) | 7 (2.9) | 11 (4.0) | 22 (4.5) | 29 (5.4) |
| Preferred languagea | ||||||||
| Spanish | … | … | 478 (86.4) | 407 (76.4) | 191 (78.3) | 183 (65.8) | 481 (98.4) | 529 (98.7) |
| Income tertiles | ||||||||
| First | 94 (26.1) | 239 (40.2) | 265 (47.9) | 216 (40.5) | 115 (47.1) | 135 (48.6) | 197 (40.3) | 246 (45.9) |
| Second | 101 (28.1) | 187 (31.5) | 140 (25.3) | 170 (31.9) | 56 (23.0) | 72 (25.9) | 160 (32.7) | 158 (29.5) |
| Third | 165 (45.8) | 168 (28.3) | 148 (26.8) | 147 (27.6) | 73 (29.9) | 71 (25.5) | 132 (27.0) | 132 (24.6) |
| Insurance | ||||||||
| Uninsured | 12 (3.3) | 10 (1.7) | 74 (13.4) | 34 (6.4) | 21 (8.6) | 11 (4.0) | 12 (2.5) | 6 (1.1) |
| Government | 138 (38.3) | 294 (49.5) | 387 (70.0) | 375 (70.4) | 175 (71.7) | 221 (79.5) | 288 (58.9) | 316 (59.0) |
| Private | 210 (58.3) | 290 (48.8) | 92 (16.6) | 124 (23.3) | 48 (19.7) | 46 (16.5) | 189 (38.7) | 214 (39.9) |
| Education levela | ||||||||
| Some high school | 42 (11.7) | 89 (15.0) | 347 (62.7) | 278 (52.2) | 100 (41.0) | 115 (41.4) | 63 (12.9) | 78 (14.6) |
| High school graduate | 87 (24.2) | 147 (24.7) | 129 (23.3) | 133 (25.0) | 62 (25.4) | 73 (26.3) | 168 (34.4) | 171 (31.9) |
| Some college | 231 (64.2) | 358 (60.3) | 77 (13.9) | 122 (22.9) | 82 (33.6) | 90 (32.4) | 258 (52.8) | 287 (53.5) |
| SES statusb | ||||||||
| Low | 93 (25.6) | 240 (40.4) | 313 (56.6) | 230 (43.2) | 109 (44.7) | 126 (45.3) | 137 (28.0) | 170 (31.7) |
| Middle | 169 (46.9) | 248 (41.8) | 132 (23.9) | 149 (28.0) | 53 (21.7) | 60 (21.6) | 200 (40.9) | 194 (36.2) |
| High | 98 (27.2) | 106 (17.8) | 108 (19.5) | 154 (28.9) | 82 (33.6) | 92 (33.1) | 152 (31.1) | 172 (32.1) |
| Perceived discrimination, any | 152 (42.2) | 291 (49.0) | 161 (29.1) | 140 (26.3) | 66 (27.0) | 77 (27.7) | 33 (6.7) | 53 (9.9) |
| Severity of discriminationc | ||||||||
| Never | 208 (57.8) | 303 (51.0) | 392 (70.9) | 393 (73.7) | 178 (73.0) | 201 (72.3) | 456 (93.3) | 483 (90.1) |
| Rarely | 124 (34.4) | 229 (38.6) | 143 (25.9) | 126 (23.6) | 61 (25.0) | 71 (25.5) | 32 (6.5) | 49 (9.1) |
| Often | 28 (7.8) | 62 (10.4) | 18 (3.3) | 14 (2.6) | 5 (2.0) | 6 (2.2) | 1 (0.2) | 4 (0.7) |
| % African ancestry, mean (SD) | 77.6 (11.9) | 78.1 (12.0) | 4.3 (2.8) | 4.6 (3.1) | 16.1 (14.9) | 16.3 (15.5) | 21.4 (9.0) | 23.6 (11.9) |
| Asthma control | ||||||||
| Control | … | 165 (29.7) | … | 241 (48.1) | … | 86 (33.2) | … | 97 (18.8) |
| Partial | … | 168 (30.2) | … | 153 (30.5) | … | 91 (35.1) | … | 192 (37.2) |
| Poor | … | 223 (40.1) | … | 107 (21.4) | … | 82 (31.7) | … | 227 (44.0) |
Values are reported as No. (percentage) unless otherwise specified. Bold values are significant (P ≤ .05).
GALA II = Genes-Environments and Admixture in Latino Americans; SAGE II = Study of African Americans, Asthma, Genes and Environment; SES = socioeconomic status.
Refers to the preferred language and education level of the participant’s mother.
SES status are tertiles of a composite index derived from reported income, mother’s education, and insurance status.
Discrimination score was categorized as never (negative answer to all four situations); rarely (affirmative answer to one situation), and often (affirmative answer to two or more situations).
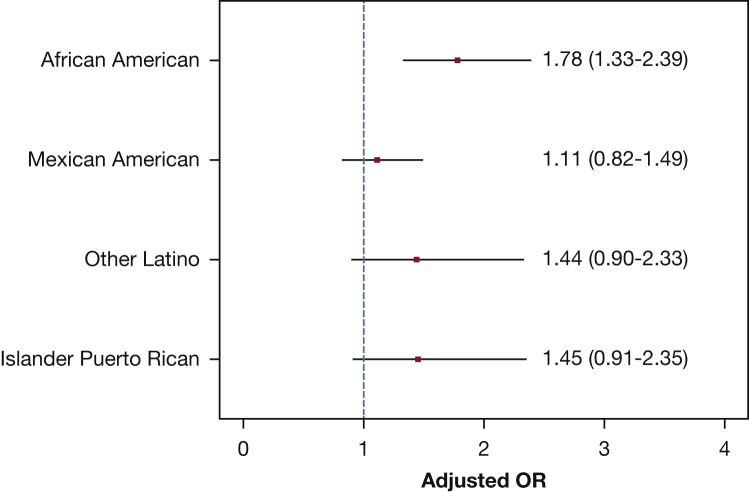
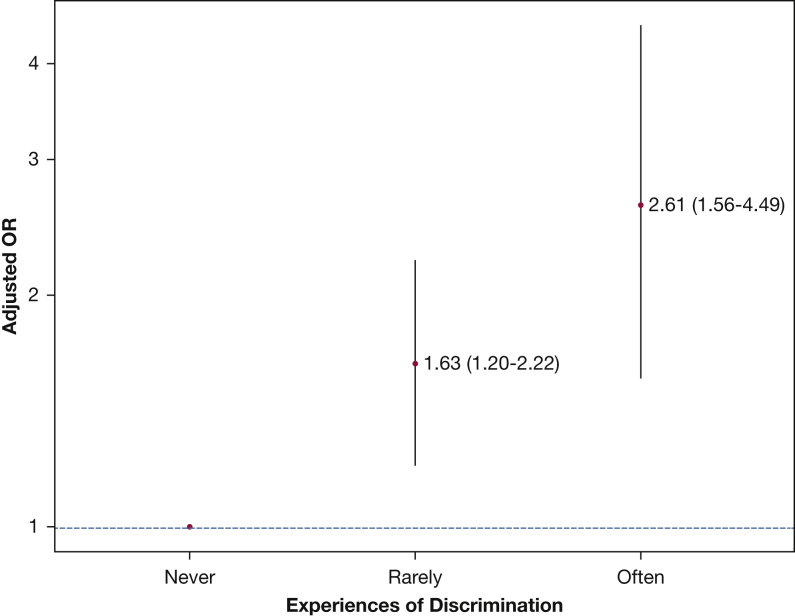
Asthma Probability
After adjusting for age, sex, current and in utero tobacco exposure, SES, global African ancestry, and study site, we found that African American children reporting any perceived discrimination had a 78% increased odds of having asthma (OR, 1.78; 95% CI, 1.33-2.39) compared with those denying discriminatory experiences (Fig 1). This association was not observed among the Latino subgroups. Only among African American children we observed increased odds of having asthma as reports of discrimination increased (P for trend, < .001) (Fig 2). For Latino subgroups, see e-Figures 1-3.
Figure 1.
Adjusted odds and corresponding 95% CIs of having asthma with report of perceived discrimination (any/none) according to racial/ethnic group for participants from the Study of African Americans, Asthma, Genes and Environment II (SAGE II) and Genes-Environments and Admixture in Latino Americans II (GALA II) 2006-2014. Models adjusted for age, sex, current and in utero tobacco exposure, socioeconomic status, study site, mother’s preferred language (Latino models), and child’s Latino subgroup (other Latino model).
Figure 2.
Adjusted odds and corresponding 95% CIs of having asthma by severity of reported perceived discrimination in African American children, Study of African Americans, Asthma, Genes and Environment II (SAGE II) 2006-2014. Models adjusted for age, sex, current and in utero tobacco exposure, socioeconomic status, and study site.
We examined whether the association between perceived discrimination and having asthma differed across the SES composite categories (low, middle, high) for each racial/ethnic group. Significant heterogeneity was observed among Mexican American and other Latino participants (P for interaction, .01 and .04, respectively) (Table 2). For Mexican Americans, we observed a 65% increased odds of asthma with perceived discrimination only among low-SES children (OR, 1.65; 95% CI, 1.09-2.50). Conversely, among other Latino children, perceived discrimination was associated with increased odds of asthma only among those with high SES (OR, 3.09; 95% CI, 1.03-10.1).
Table 2.
Adjusteda Odds of Having Asthma With Report of Perceived Discrimination (Any/None) According to Socioeconomic Statusb by Race/Ethnicity in GALA II and SAGE II Participants: 2006-2014
| Race/Ethnic Group | Low OR (95% CI) | Middle OR (95% CI) | High OR (95% CI) | P Value for Interaction |
|---|---|---|---|---|
| African American | 2.08 (1.21-3.63) | 1.51 (0.98-2.34) | 2.04 (1.09-3.91) | .57 |
| Mexican American | 1.65 (1.09-2.50) | 0.78 (0.42-1.46) | 0.65 (0.33-1.27) | .01 |
| Other Latino | 0.80 (0.40-1.59) | 1.91 (0.60-6.57) | 3.09 (1.03-10.1) | .04 |
| Islander Puerto Rican | 2.12 (0.81-6.28) | 1.42 (0.71-2.90) | 1.21 (0.50-3.02) | .43 |
See Table 1 legend for expansion of abbreviations.
Adjusted for age, sex, second-hand tobacco exposure, in utero tobacco exposure, global African ancestry, region, mother’s preferred language (Latino models), child’s Latino subgroup (other Latino model).
SES class is the tertiles of a composite SES index derived from reported income, mother’s education, and insurance status.
We observed no heterogeneity of the association between perceived discrimination and having asthma according to global African ancestry for any racial/ethnic group (high vs low; P for interaction ≥ .42) (e-Table 4). However, the association between perceived discrimination and asthma was observed only among African American children classified as having high global African ancestry (e-Table 4).
Asthma Control
African American participants with asthma were observed to have a 97% greater odds of poor asthma control associated with any report of perceived discrimination (OR, 1.97; 95% CI, 1.42-2.76) (Table 3) after controlling for age, sex, SES, second-hand tobacco smoke, in utero tobacco exposure, use of controller medication, and study site. Moreover, the strength of the association between poor asthma control and perceived discrimination increased with exposure to discrimination (P for trend, .006). These associations were not observed for Latino subgroups regardless of how discrimination was specified. No heterogeneity was noted in the association between asthma control and perceived discrimination according to SES and global African ancestry for any racial/ethnic group (P for interactions ≥ .22) (e-Tables 5, 6). Interestingly, perceived discrimination was associated with poor asthma control among African American children regardless of the proportion of their global African ancestry and among only those Mexican American children with a low African ancestry proportion (e-Table 6).
Table 3.
Adjusteda Odds of Poor Asthma Control With Report of Perceived Discrimination by Race/Ethnicity in GALA II and SAGE II Participants: 2006-2014
| Race/Ethnic Group | Any vs None OR (95% CI) |
Rarely vs None OR (95% CI) |
Often vs None OR (95% CI) |
|---|---|---|---|
| African American | 1.97 (1.42-2.76) | 1.93 (1.37-2.74) | 2.16 (1.25-3.75) |
| Mexican American | 1.38 (0.92-2.07) | 1.37 (0.91-2.07) | 1.52 (0.50-4.41) |
| Other Latino | 1.31 (0.77-2.22) | 1.31 (0.76-2.26) | 1.33 (0.29-6.31) |
| Islander Puerto Rican | 0.86 (0.50-1.51) | 0.86 (0.49-1.52) | 0.91 (0.14-7.71) |
Analysis limited to participants with asthma.
Adjusted for age, sex, SES, second-hand tobacco exposure, in utero tobacco exposure, study site, use of controller medication, mother’s preferred language (Latino models), and child’s Latino subgroup (other Latino model).
Discussion
We observed increased odds of asthma and poor asthma control with perceived racial/ethnic discrimination among African American youth. Additionally, the odds of asthma and poor control increase as the severity of perceived discrimination increased. For Mexican Americans and other Latinos, the association between perceived discrimination and asthma varied with SES, with increased odds observed for low-SES Mexican American children and other Latino children with high SES.
These findings contribute to the existing evidence implicating racial/ethnic discrimination as a predictor of negative health outcomes in children.10, 11, 14, 15 For asthma specifically, the findings are consistent with results correlating discriminatory experiences and subsequent asthma diagnosis in African-American adult women.19 To our knowledge, this study is the first to show an association between discrimination and an asthma diagnosis in African American and Latino children. We concur with findings that perceived discrimination is an important risk factor for poor asthma control among minority children41, 42 and emphasize the importance of considering psychosocial stress when assessing childhood asthma.1, 18, 42
Differential access to services and opportunities in society, resulting in reduced access to health-care services and medications, has been shown to affect asthma outcomes in minority populations.22, 23, 24, 25, 33 In addition, our findings suggest that perceived racial/ethnic discrimination is an independent risk factor for asthma in African Americans. Additionally, as evidenced by the Mexican American and other Latino participants, experiences of discrimination may work together with social status.43 Thus, perceived discrimination and SES, independently or jointly, may be relevant factors to consider for the health of minority children.
The relationship between SES and racial/ethnic discrimination is complex. In some cases, SES may lead to underreporting of discriminatory experiences among those with limited resources or better identification of racist attacks among those with fewer competing economic stressors.44 Additionally, historical experiences of discrimination in a particular racial/ethnic group may make such events more recognizable, regardless of SES. These varying accounts likely explain the different associations we observed between SES and discrimination among the population of African American and Latino participants. Additionally, unmeasured factors, related to both SES and discriminatory experiences, may account for some of the association seen with asthma and related outcomes. Communities that are affected by interpersonal discrimination to the greatest degree are also more likely to fall victim to incidences of structural racism, including living in areas exposed to higher levels of air pollution and substandard housing, as well as exposure to community violence.1, 7 The latter are factors that are also increased among those from socioeconomically disadvantaged backgrounds and have been independently shown to increase the risk of asthma and related outcomes.45
Although this study advances our understanding of race/ethnicity and health outcomes, there are important limitations that should be noted. Although we present evidence of a dose-response association between perceived discrimination and asthma in the African American participants, which provides strength to the observations presented, the use of a cross-sectional design limits our ability to make causal inference or establish a temporal relationship between asthma and perceived discrimination.
Although the Experiences of Discrimination questionnaire has been validated in US adult populations,34 we limited the questionnaire to items relevant to pediatric populations (school and medical settings, while receiving services, and in public). Despite this limitation, the questions we included overlap with those previously used in instruments validated for children.14, 15, 46 Unlike instruments specific for pediatric populations,35 we are missing items assessing experiences unique to pediatric populations, and as a result our instrument likely underestimates the true prevalence of discrimination and the magnitude of the association of interest in our study population. Moreover, by limiting our assessment to racial/ethnic discrimination, we may have missed important experiences of discrimination associated with sex, religion, language, and sexual orientation.47 In addition, our participants' distress may result from discriminatory events directed at other family members, including caregivers and siblings, which were not assessed. Finally, we excluded 2,019 participants due to missing data, mostly for discrimination and SES indicators. However, participants were selected based on disease status and not on perceived discrimination or SES (or both), and thus, it is unlikely that these exclusions biased our results.
The strength of this study lies in the availability of multiple variables and a large diverse sample size. Our design included more than 3,500 African American and Latino children from across the United States and Puerto Rico and supports the conclusion that discrimination operates independent of factors known to contribute to either asthma or discrimination itself. In addition, such a sample size allows the opportunity to examine heterogeneity within the study sample.
Future studies should aim to advance the quantification of discriminatory experience in pediatric populations and further establish the association of these experiences with physical health outcomes such as asthma. There is also a need for a clearer understanding of the mechanisms by which stress affects asthma, a condition particularly sensitive to psychosocial stress. Assessment of discrimination, as well as its forms (eg, sex, religion, language, sexual orientation, and physical ability) could help our understanding of the effect of perceived discrimination not only for a common disease such as asthma but also for other stress-related pediatric diseases.47
Conclusions
Consistent with prior studies in both adults13, 19 and children,11, 15 our findings suggest that racial/ethnic discrimination independently contributes to poor health outcomes. Thus, as experiences of discrimination contribute to asthma outcomes, one of the most common childhood conditions, these experiences may also contribute to health inequity in general among US children and adolescents throughout the life course.
Acknowledgments
Author contributions: N. T. and E. G. B. are responsible for the content of the manuscript, including the data and the analysis. N. T. developed the aims for the presented analyses, carried out the initial and final analyses with assistance from N. B. and S. S. and oversight from L. N. B. and S. S. N. T. N. B. drafted the initial manuscript. N. T., N. B., and S. S., revised the manuscript and approved the final manuscript as submitted. E. G. B. conceived the study. E. G. B., L. N. B., and S. S. designed the study. E. G. B., L. N. B., A. D., K. M., M. A. L., P. C. A., H. J. F., D. S., E. B-B., W. R-S., S. T., J. R. R-S., and K. B-D. planned and supervised the collection of data at specific clinical sites. C. E. supervised specimen processing and analysis. All authors participated in manuscript preparation and approved the final version of the manuscript.
Financial/nonfinancial disclosures: None declared.
Other contributions: The authors acknowledge the families and patients for their participation and thank the numerous health-care providers and community clinics for their support and participation in GALA II and SAGE II. In particular, the authors thank the study coordinator Sandra Salazar and the recruiters who obtained the data: Duanny Alva, MD, Gaby Ayala-Rodriguez, Ulysses Burley, MD, MPH Lisa Caine, RT, Elizabeth Castellanos, Jaime Colon, Denise DeJesus, Iliana Flexas, Blanca Lopez, Brenda Lopez, MD, Louis Martos, Vivian Medina, Juana Olivo, Mario Peralta, Esther Pomares, MD, Jihan Quraishi, RN, Johanna Rodriguez, Shahdad Saeedi, DPM, Dean Soto, Ana Taveras, and Emmanuel Viera.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Additional information: The e-Appendix, e-Figures, and e-Tables can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: This work was supported in part by the Sandler Family Foundation, the National Institutes of Health (R01-ES015794, U19-AI077439, R01-HL088133, R01-HL078885, R01-HL104608, R21ES24844-01, 1R01MD010443, and P60-MD006902), M01-RR00188 (to H. J. F.), the Flight Attendant Medical Research Institute (FAMRI), the RWJF Amos Medical Faculty Development Award (to E. G. B.), and the American Asthma Foundation (to E. G. B.). N. T. was supported by an institutional training grant from the NIGMS (T32-GM007546) and career development awards from the NHLBI (K12-HL119997 and K23-HL125551-01A1), Parker B. Francis Fellowship Program, and the American Thoracic Society. N. B. was supported by R25MD006832 from the NIMHD. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Drs Thakur and Barcelo contributed equally to this manuscript.
This work was presented in abstract form at the annual meeting of the American Thoracic Society, May 16-21, 2014, San Diego, CA.
Supplementary Data
References
- 1.Williams D.R., Mohammed S.A. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mendes W.B., Major B., McCoy S., Blascovich J. How attributional ambiguity shapes physiological and emotional responses to social rejection and acceptance. J Pers Soc Psychol. 2008;94(2):278–291. doi: 10.1037/0022-3514.94.2.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pittman C.T. Getting mad but ending up sad: the mental health consequences for African American using anger to cope with racism. J Black Stud. 2011;42(7):1106–1124. doi: 10.1177/0021934711401737. [DOI] [PubMed] [Google Scholar]
- 4.Carter R.T. Racism and psychological and emotional injury: recognizing and assessing race-based traumatic stress. Couns Psychol. 2007;35(1):13–105. [Google Scholar]
- 5.Brondolo E., Thompson S., Brady N. The relationship of racism to appraisals and coping in a community sample. Ethn Dis. 2005;15:S5–S14. S5-S19. [PubMed] [Google Scholar]
- 6.Sanders-Phillips K. Racial discrimination: a continuum of violence exposure for children of color. Clin Child Fam Psychol Rev. 2009;12(2):174–195. doi: 10.1007/s10567-009-0053-4. [DOI] [PubMed] [Google Scholar]
- 7.Williams D.R., Mohammed S.A., Leavell J., Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roth W.D. “There is no racism here”: understanding latinos’ perception of color discrimination through sending-receiving society comparison. In: Hall R.E., editor. Racism in the 21st Century. Springer; New York, NY: 2008. pp. 205–234. [Google Scholar]
- 9.Torres-Harding S., Turner T. Assessing racial microaggression distress in a diverse sample. Eval Health Prof. 2014:1–27. doi: 10.1177/0163278714550860. [DOI] [PubMed] [Google Scholar]
- 10.Cheng E.R., Cohen A., Goodman E. The role of perceived discrimination during childhood and adolescence in understanding racial and socioeconomic influences on depression in young adulthood. J Pediatr. 2015;166(2):370–377.e1. doi: 10.1016/j.jpeds.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Basáñez T., Unger J.B., Soto D., Crano W., Baezconde-Garbanati L. Perceived discrimination as a risk factor for depressive symptoms and substance use among Hispanic adolescents in Los Angeles. Ethn Health. 2013;18(3):244–261. doi: 10.1080/13557858.2012.713093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen K.H., Subramanian S.V., Sorensen G., Tsang K., Wright R.J. Influence of experiences of racial discrimination and ethnic identity on prenatal smoking among urban black and Hispanic women. J Epidemiol Community Health. 2012;66(4):315–321. doi: 10.1136/jech.2009.107516. [DOI] [PubMed] [Google Scholar]
- 13.Borrell L.N., Kiefe C.I., Diez-Roux A.V., Williams D.R., Gordon-Larsen P. Racial discrimination, racial/ethnic segregation, and health behaviors in the CARDIA study. Ethn Health. 2013;18(3):227–243. doi: 10.1080/13557858.2012.713092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Priest N., Paradies Y., Trenerry B., Truong M., Karlsen S., Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med. 2013;95:115–127. doi: 10.1016/j.socscimed.2012.11.031. [DOI] [PubMed] [Google Scholar]
- 15.Pachter L.M., Coll C.G. Racism and child health: a review of the literature and future directions. J Dev Behav Pediatr. 2009;30(3):255–263. doi: 10.1097/DBP.0b013e3181a7ed5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akinbami L.J., Rhodes J.C., Lara M. Racial and ethnic differences in asthma diagnosis among children who wheeze. Pediatrics. 2005;115(5):1254–1260. doi: 10.1542/peds.2004-0897. [DOI] [PubMed] [Google Scholar]
- 17.Akinbami L.J., Moorman J.E., Simon A.E., Schoendorf K.C. Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001-2010. J Allergy Clin Immunol. 2014;134(3):547–555. doi: 10.1016/j.jaci.2014.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yonas M.A., Lange N.E., Celedon J.C. Psychosocial stress and asthma morbidity. Curr Opin Allergy Clin Immunol. 2012;12(2):202–210. doi: 10.1097/ACI.0b013e32835090c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coogan P.F., Yu J., O’Connor G.T. Experiences of racism and the incidence of adult-onset asthma in the Black Women’s Health Study. Chest. 2014;145(3):480–485. doi: 10.1378/chest.13-0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim G., Sellbom M., Ford K.-L. Race/ethnicity and measurement equivalence of the Everyday Discrimination Scale. Psychol Assess. 2014;26(3):892–900. doi: 10.1037/a0036431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hunt M.O., Wise L.A., Jipguep M., Cozier Y.C., Rosenberg L. Neighborhood racial composition and perceptions of racial discrimination: evidence from the Black Women’s Health Study. Soc Psychol Q. 2007;70(3):272–289. [Google Scholar]
- 22.Cabana M.D., Lara M., Shannon J. Racial and ethnic disparities in the quality of asthma care. Chest. 2007;132(5):810S–817S. doi: 10.1378/chest.07-1910. [DOI] [PubMed] [Google Scholar]
- 23.Federico S.G., Steiner J.F., Beaty B., Crane L., Kempe A. Disruptions in insurance coverage: patterns and relationship to health care access, unmet need, and utilization before enrollment in the State Children’s Health Insurance Program. Pediatrics. 2007;120(4):e1009–e1016. doi: 10.1542/peds.2006-3094. [DOI] [PubMed] [Google Scholar]
- 24.Holt E.W., Theall K.P., Rabito F.A. Individual, housing, and neighborhood correlates of asthma among young urban children. J Urban Heal. 2012;90(1):116–129. doi: 10.1007/s11524-012-9709-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nishimura K.K., Galanter J.M., Roth L.A. Early-life air pollution and asthma risk in minority children. The GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013;188(3):309–318. doi: 10.1164/rccm.201302-0264OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parra E.J., Kittles R.A., Shriver M.D. Implications of correlations between skin color and genetic ancestry for biomedical research. Nat Genet. 2004;36(11 Suppl):S54–S60. doi: 10.1038/ng1440. [DOI] [PubMed] [Google Scholar]
- 27.Leite T.K.M., Fonseca R.M.C., de França N.M., Parra E.J., Pereira R.W. Genomic ancestry, self-reported “color” and quantitative measures of skin pigmentation in Brazilian admixed siblings. PLoS One. 2011;6(11):e27162. doi: 10.1371/journal.pone.0027162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hochschild J.L., Weaver V. The skin color paradox and the American racial order. Soc Forces. 2007;86(2):643–670. [Google Scholar]
- 29.Flores C., Ma S.F., Pino-Yanes M. African ancestry is associated with asthma risk in African Americans. PLoS One. 2012;7:1. doi: 10.1371/journal.pone.0026807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pino-Yanes M., Thakur N., Gignoux C.R. Genetic ancestry influences asthma susceptibility and lung function among Latinos. J Allergy Clin Immunol. 2015;135(1):228–235. doi: 10.1016/j.jaci.2014.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Heart, Lung and Blood Institute. Guidelines for the Diagnosis and Management of Asthma (EPR-3), 2007; https://www.nhlbi.nih.gov/health-pro/guidelines/current/asthma-guidelines. Accessed July 1, 2013.
- 32.Ferris B. Epidemiology standardization project (American Thoracic Society) Am Rev Respir Dis. 1978;118(6 Part 2):1–120. [PubMed] [Google Scholar]
- 33.Oh S.S., Tcheurekdjian H., Roth L.A. Effect of secondhand smoke on asthma control among black and Latino children. J Allergy Clin Immunol. 2012;129(6):1478–1483.e7. doi: 10.1016/j.jaci.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krieger N., Smith K., Naishadham D., Hartman C., Barbeau E.M. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 35.Pachter L.M., Bernstein B.A., Szalacha L.A., Coll C.G. Perceived racism and discrimination in children and youths: an exploratory study. Health Soc Work. 2010;35(1):61–69. doi: 10.1093/hsw/35.1.61. [DOI] [PubMed] [Google Scholar]
- 36.Almqvist C., Worm M., Leynaert B. Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy. 2008;63(1):47–57. doi: 10.1111/j.1398-9995.2007.01524.x. [DOI] [PubMed] [Google Scholar]
- 37.Thakur N., Oh S.S., Nguyen E.A. Socioeconomic status and childhood asthma in urban minority youths. The GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013;188(10):1202–1209. doi: 10.1164/rccm.201306-1016OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thakur N., Martin M., Castellanos E. Socioeconomic status and asthma control in African American youth in SAGE II. J Asthma. 2014;51(7):720–728. doi: 10.3109/02770903.2014.905593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Svarstad B.L., Chewning B.A., Sleath B.L., Claesson C. The Brief Medication Questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Educ Couns. 1999;37(2):113–124. doi: 10.1016/s0738-3991(98)00107-4. [DOI] [PubMed] [Google Scholar]
- 40.R Core Team. R: A language and environment for statistical computing. 2016. https://www.r-project.org/. Accessed May 3, 2016.
- 41.Coutinho M.T., McQuaid E.L., Koinis-Mitchell D. Contextual and cultural risks and their association with family asthma management in urban children. J Child Health Care. 2013;17(2):138–152. doi: 10.1177/1367493512456109. [DOI] [PubMed] [Google Scholar]
- 42.Koinis-Mitchell D., McQuaid E.L., Seifer R. Multiple urban and asthma-related risks and their association with asthma morbidity in children. J Pediatr Psychol. 2007;32(5):582–595. doi: 10.1093/jpepsy/jsl050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Drake K.A., Galanter J.M., Burchard E.G. Race, ethnicity and social class and the complex etiologies of asthma. Pharmacogenomics. 2008;9(4):453–462. doi: 10.2217/14622416.9.4.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karlsen S., Nazroo J.Y. Relation between racial discrimination, social class, and health among ethnic minority groups. Am J Public Health. 2002;92(4):624–631. doi: 10.2105/ajph.92.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williams D.R., Sternthal M., Wright R.J. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123(suppl):S174–S184. doi: 10.1542/peds.2008-2233H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Coker T.R., Elliott M.N., Kanouse D.E. Perceived racial/ethnic discrimination among fifth-grade students and its association with mental health. Am J Public Health. 2009;99(5):878–884. doi: 10.2105/AJPH.2008.144329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Grollman E.A. Multiple forms of perceived discrimination and health among adolescents and young adults. J Health Soc Behav. 2012;53(2):199–214. doi: 10.1177/0022146512444289. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.