Abstract
Objective
To examine the relationship between plantar stress over a step, cumulative plantar stress over a day, and first metatarsophalangeal (MTP) joint pain among older adults.
Methods
Plantar stress and first MTP pain were assessed within the Multicenter Osteoarthritis Study. All included participants were asked if they had pain, aching, or stiffness at the first MTP joint on most days for the past 30 days. Pressure time integral (PTI) was quantified as participants walked on a pedobarograph, and mean steps per day were obtained using an accelerometer. Cumulative plantar stress was calculated as the product of regional PTI and mean steps per day. Quintiles of hallucal and second metatarsal PTI and cumulative plantar stress were generated. The relationship between predictors and the odds ratio of first MTP pain was assessed using a logistic regression model.
Results
Feet in the quintile with the lowest hallux PTI had 2.14 times increased odds of first MTP pain (95% confidence interval [95% CI] 1.42–3.25, P < 0.01). Feet in the quintile with the lowest second metatarsal PTI had 1.50 times increased odds of first MTP pain (95% CI 1.01–2.23, P = 0.042). Cumulative plantar stress was unassociated with first MTP pain.
Conclusion
Lower PTI was modestly associated with increased prevalence of frequent first MTP pain at both the hallux and second metatarsal. Lower plantar loading may indicate the presence of an antalgic gait strategy and may reflect an attempt at pain avoidance. The lack of association with cumulative plantar stress may suggest that patients do not limit their walking as a pain-avoidance mechanism.
INTRODUCTION
Pain at the first metatarsophalangeal (MTP) joint is one of the key symptoms of first MTP osteoarthritis (OA) (1). First MTP OA is the most common form of degenerative joint disease in the foot and affects 15–50% of adults over age 65 years (2). Individuals with first MTP OA have debilitating foot pain and reduction in motion, with consequent limitations in activities of daily living and quality of life (3). Foot pain has been linked to significant disability (4) and increased health care utilization (5).
The incidence and progression of OA have been linked to mechanical loading, sustained during weight-bearing activities of daily living (6). However, few studies have assessed mechanical loading in individuals with foot pain. Elevated mechanical loads, in terms of increased regional plantar pressure, may contribute to pain perception by stimulation of cutaneous nociceptors (7). Additionally, increased regional plantar pressure may influence net joint reaction forces and moments and lead to elevated articular joint stress (8). Consistent with this theory of mechanical overloading, recent reports have found increased regional plantar pressure accompanying foot pain in clinical populations (9,10). Compared to asymptomatic control subjects, patients with radiographic first MTP OA (hallux rigidus) or hallux limitus have demonstrated higher plantar loads under the great toe region (11,12). While previous studies have suggested that increased regional plantar loads may contribute to foot pain, objective evidence examining the relationship between hallucal pressure time integral (PTI) during walking and frequent first MTP joint pain in older adults is not available.
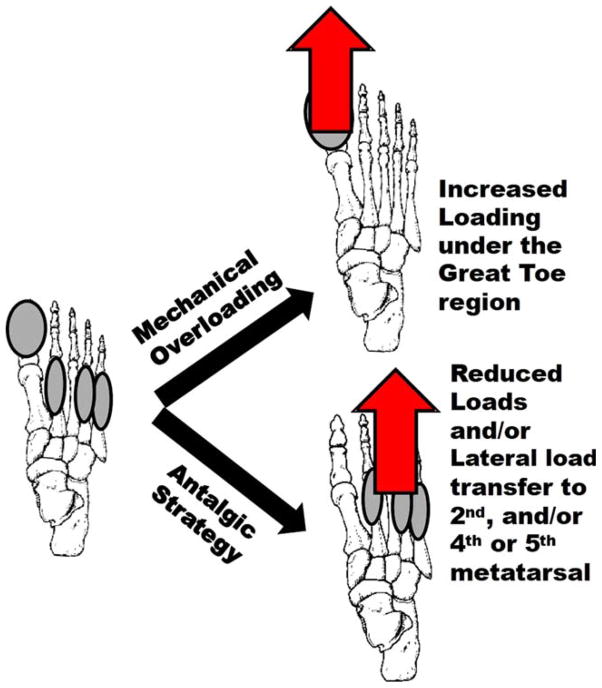
In contrast to the mechanical overloading hypothesis, some studies postulate that individuals experiencing foot pain adopt an antalgic strategy to avoid exacerbating their foot pain (Figure 1). An antalgic strategy is characterized by lower plantar loading and may reflect an attempt at pain avoidance. In agreement with the antalgic theory, individuals with first MTP OA have been reported to shift their weight laterally in an attempt to unload the painful first MTP region during walking (13,14). Similarly, lower forefoot loading has been reported in patients with rheumatoid arthritis (RA) and low Health Assessment Questionnaire (HAQ) score (more disability, more pain) compared to RA patients with high HAQ scores (15). These results may suggest that patients with pain (lower HAQ score, more disability) may adopt an antalgic loading strategy. However objective data quantifying the presence of either mechanical overloading (increased hallucal loading) or antalgic strategies (elevated second metatarsal loading) in individuals with frequent first MTP pain are lacking.
Figure 1.
Representation of mechanical overloading and antalgic patterns of load distribution. On the left, the grey ovals indicate the regions assessed: hallux, second, fourth, and fifth metatarsals. On the right, mechanical overloading (evidenced as increased loading on hallux) is depicted in the top image, and an antalgic strategy (evidenced as increased loading on second, fourth, or fifth metatarsal) is depicted in the bottom image. Color figure can be viewed in the online issue, which is available at http://onlinelibrary.wiley.com/journal/doi/10.1002/acr.22826/abstract.
Clinical and population-based studies indicate that individuals who report foot pain limit their physical activity to avoid exacerbating their pain (5,13). The combined effect of physical activity and plantar pressure has been proposed as a key mediator of tissue stress and the consequent evolution of symptoms (16). Cumulative regional plantar stress (the product of regional PTI and mean daily strides) has been used to evaluate the amount of mechanical trauma accumulated by plantar tissues in individuals with diabetes mellitus and neuropathy (17). While both limited physical activity and mechanical stress have been noted in individuals with foot pain, no studies have assessed the relationship between cumulative plantar stress and frequent first MTP joint pain.
The purpose of this study was to examine the relationship between plantar loading during walking and first MTP joint pain among older adults. We hypothesized that older adults reporting frequent first MTP pain will show elevated hallucal PTI during walking (reflective of mechanical overloading) and increased second metatarsal PTI (reflecting the use of an antalgic strategy). In addition, the study purpose was to evaluate the relationship between cumulative plantar stress for the hallux and second metatarsal regions and frequent first MTP joint pain in older adults. The findings of this study have direct relevance to patient care by informing practice. Walking has been ranked as the highest priority for improvement by patients seeking specialized care for foot and ankle disorders (18). By identifying key contributors to frequent first MTP pain, this study can motivate the design of targeted, effective intervention strategies.
SUBJECTS AND METHODS
Subjects
All procedures were approved by the Institutional Review Boards at the University of Iowa, University of Alabama, Birmingham, University of California, San Francisco, and Boston University School of Medicine. Participants were subjects in the Multicenter Osteoarthritis Study (MOST). The MOST comprises a community-based sample of men and women who either have, or are at risk for, knee OA. MOST participants were followed prospectively over 84 months. Details related to recruitment and study population have been described previously (19). The current study used data from the 60-month MOST clinic visit, when plantar load distribution and first MTP pain were assessed. The following exclusion criteria were used specific to the current study: legs with an open foot wound, lower extremity amputation, recent surgery, or a total knee replacement. Individuals unable to safely walk short distances without using an assistive device (such as a cane or walker or knee brace) were also excluded.
From the parent MOST study, 3,387 feet with plantar pressure data were available for analyses. After screening for exclusion criteria and missing data (no response to first MTP pain question), 2,589 legs were included (1,693 individuals, 58% women, mean ± SD age 61 ± 7 years, mean ± SD body mass index [BMI] 30.3 ± 5.8 kg/m2).
First MTP pain
The presence of frequent first MTP pain was assessed by asking participants if they experienced “pain, aching, or stiffness in the front of the foot on most days for the past 30 days,” and to identify the location of these symptoms on a foot diagram. For the current analysis, first MTP pain was defined as pain at the dorsal aspect of the great toe.
Plantar loading and cumulative plantar stress
Participants walked on a plantar pressure-measuring device (Emed, Novel Electronics) embedded in a walkway. Five trials per foot were acquired during self-selected speed walking. Walking speed was measured using an electronic walkway (GaitRite, CIR Systems). Starting position was standardized to avoid targeting and to ensure clean foot contact on the plantar pressure-measuring device. Using a second step protocol, a minimum of 3 and maximum of 5 steps were collected to ensure adequate reliability (20,21).
Novel Database software (Novel Electronics) was used to define regions of interest (hallux, second, fourth, and fifth metatarsal) (22). PTI defined as the area under the pressure-time curve throughout stance phase, expressed in Ns/cm2, was computed in the regions of interest. PTI represents the regional plantar load during each step and is highly relevant to physical stress theory (16). The definitions of independent variables used to characterize plantar loading are consistent with definitions used in previous studies (23–25).
Mean steps per day were obtained using accelerometer data (Stepwatch, Orthocare Innovations). Study participants wore this small device (75 × 50 × 20 mm, 1.5 ounces) at their ankle for 3–7 days. Reliability (26) and accuracy (27) of the accelerometer in quantifying physical activity have been established in previous studies. Accelerometer data were downloaded and analyzed (StepWatch Analysis Software, Orthocare Innovations) to quantify mean steps per 24 hours. Cumulative plantar stress was calculated as the product of regional PTI and mean steps per day (17,28).
Statistical analysis
Quintiles of hallucal and second metatarsal plantar PTI were generated. The relationship between PTI and relative odds of first MTP joint pain was assessed using a logistic regression model with generalized estimating equations to account for the dependence between 2 feet of a single subject. Age, sex, BMI, knee OA status, and walking speed were included as covariates. A secondary analysis was also performed, similarly using PTI under the fourth and fifth metatarsals as exposure variables.
A similar analytic plan was followed to assess the relationship between cumulative plantar stress and odds ratio of the first MTP joint pain, adjusting for age, sex, BMI, knee OA status (at risk or with OA), and walking speed. A secondary analysis was performed by calculating cumulative stress using PTI under the fourth and fifth metatarsal. All statistical analysis was performed using SPSS software, version 22, at a significance level of α = 0.05.
RESULTS
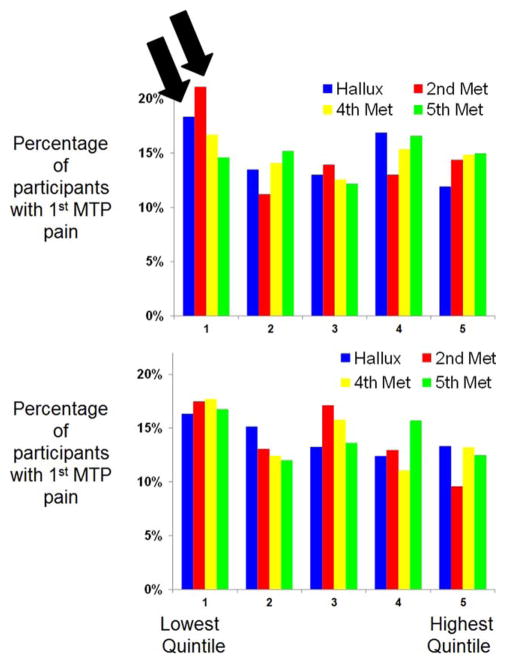
First MTP pain was reported in 14.7% of the legs tested (445 of 1,943 individuals, 22% of subjects). Mean ± SD steps per day was 8,765 ± 3,550 and 9,256 ± 3,725 in individuals with and without first MTP pain, respectively. Quintiles of PTI and cumulative stress were generated (Table 1), and percentage of participants reporting pain in each quintile is shown in Figure 2.
Table 1.
Summary of pressure time integral in kPa/s and cumulative stress in kPa/s × steps/day*
| Hallux | 2nd metatarsal | 4th metatarsal | 5th metatarsal | |
|---|---|---|---|---|
| Pressure time integral, kPa/s | ||||
| Q1 (lowest) | 2.99 ± 1.12 | 8.16 ± 1.42 | 5.96 ± 1.02 | 4.02 ± 0.88 |
| Q2 | 5.97 ± 0.77 | 11.15 ± 0.73 | 8.00 ± 0.47 | 6.22 ± 0.60 |
| Q3 | 8.85 ± 0.94 | 13.76 ± 0.86 | 9.63 ± 0.48 | 8.79 ± 0.93 |
| Q4 | 12.83 ± 1.50 | 17.31 ± 1.21 | 11.80 ± 0.85 | 13.14 ± 1.76 |
| Q5 (highest) | 23.16 ± 7.96 | 27.55 ± 7.76 | 18.98 ± 6.47 | 24.92 ± 8.27 |
| Cumulative stress, kPa/s × steps/day | ||||
| Q1 (lowest) | 49,839.23 ± 7,206.78 | 55,106.16 ± 16,029.58 | 38,384.22 ± 10,870.87 | 28,746.26 ± 9,186.37 |
| Q2 | 63,601.15 ± 12,029.58 | 92,900.55 ± 9,082.30 | 65,280.53 ± 6,088.35 | 53,429.51 ± 6,331.74 |
| Q3 | 77,363.06 ± 9,217.08 | 124,902.49 ± 9,440.27 | 88,114.47 ± 7,142.14 | 78,618.12 ± 8,796.11 |
| Q4 | 117,199.00 ± 13,844.22 | 164,343.29 ± 14,992.19 | 115,179.61 ± 9,817.14 | 119,600.55 ± 15,475.97 |
| Q5 (highest) | 214,699.35 ± 73,472.04 | 272,556.17 ± 77,980.78 | 195,872.52 ± 66,019.13 | 244,783.57 ± 96,723.42 |
Values are mean ± SD. Data for each quintile are organized by row, and the 4 regions of interest are presented in columns.
Figure 2.
Percentage of legs with first metatarsophalangeal (MTP) pain by quintile of pressure time integral (Top) and cumulative stress (Bottom). Quintiles are rank ordered such that 1 has the lowest mean and 5 has the highest mean. Each column represents a region of interest. Black arrows emphasize that the highest prevalence of first MTP pain was noted in the lowest quintile of the hallux and the second metatarsal pressure time integral. Met = metatarsophalangeal.
Feet in the quintile with the lowest hallux PTI had 2.14 times increased odds of first MTP pain (95% confidence interval [95% CI] 3.25–1.42, P < 0.01) (Table 2). Feet in the quintile with the lowest second metatarsal PTI had 1.50 times increased odds of first MTP pain (95% CI 1.01–2.23, P = 0.004). No significant relationships were found between cumulative plantar stress and odds of first MTP pain.
Table 2.
Relative odds of first metatarsophalangeal pain in quintiles of pressure time integral and cumulative plantar stress*
| Quintile 1 (lowest loads) | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 (highest loads) | P for trend | |
|---|---|---|---|---|---|---|
| Pressure time integral | ||||||
| Hallux | 2.1 (1.4–3.2)† | 1.2 (0.8–1.9) | 1.3 (0.9–2.0) | 1.6 (1.1–2.4) | 1.0 (ref) | 0.004 |
| Second metatarsal | 1.5 (2.2–1.0)† | 0.7 (0.5–1.1) | 0.9 (0.6–1.4) | 0.9 (0.6–1.4) | 1.0 (ref) | 0.004 |
| Fourth metatarsal | 1.1 (0.7–1.7) | 0.9 (0.6–1.4) | 0.8 (0.6–1.2) | 1.0 (0.7–1.5) | 1.0 (ref) | 0.66 |
| Fifth metatarsal | 1.0 (0.6–1.5) | 1.0 (0.7–1.5) | 0.8 (0.6–1.2) | 1.1 (0.8–1.6) | 1.0 (ref) | 0.89 |
| Cumulative stress | ||||||
| Hallux | 1.2 (0.8–1.8) | 1.1 (0.8–1.7) | 0.9 (0.6–1.4) | 0.9 (0.6–1.3) | 1.0 (ref) | 0.41 |
| Second metatarsal | 1.6 (1.1–2.5) | 1.3 (0.8–2.0) | 1.8 (1.2–2.8) | 1.4 (0.9–2.2) | 1.0 (ref) | 0.05 |
| Fourth metatarsal | 1.1 (0.8–1.7) | 0.8 (0.5–1.2) | 1.1 (0.7–1.7) | 0.8 (0.5–1.2) | 1.0 (ref) | 0.25 |
| Fifth metatarsal | 1.2 (0.8–1.8) | 0.8 (0.5–1.2) | 1.0 (0.7–1.5) | 1.2 (0.8–1.8) | 1.0 (ref) | 0.28 |
Values are adjusted odds ratio (95% confidence interval), unless indicated otherwise. Data are organized by region of interest in rows and quintiles in columns. ref = reference.
Significant.
DISCUSSION
The chief objective of this study was to examine the relationship between plantar loading during walking and first MTP joint pain among older adults. The key findings of our study indicate that lower PTI, at both the hallux (P < 0.01) and second metatarsal (P = 0.004), was modestly associated with increased prevalence of frequent first MTP pain. The reduction in plantar loading during walking may reflect an attempt at pain avoidance in individuals with frequent first MTP pain. These findings may suggest that individuals experiencing foot pain adopt an antalgic strategy to avoid exacerbating their foot pain. Our findings, demonstrating lower loading at the hallux and second metatarsal, are contrary to the mechanical overloading hypothesis that leads us to expect increased loading in individuals with musculoskeletal pain. Longitudinal studies are needed to examine the long-term consequences of persistent pain avoidance plantar loading patterns.
There are several unique aspects to this study. While a select handful of studies have examined foot pain in large cohorts of community-dwelling adults, this is the first study to simultaneously assess pain, plantar loading, and cumulative stress. Foot pain has emerged as an important public health concern due to its high prevalence and substantial negative impact on quality of life and physical mobility (29,30). In previous reports, the prevalence of foot pain has ranged from 12–37% in population-based cohorts (29,31–33). In the current study, we assessed first MTP pain, an anatomically specific subset of foot pain, and found a prevalence of 14.7%, which is consistent with previous findings (2,29,34). Similar to our study, 2 recent studies have assessed the prevalence of foot pain in community-dwelling adults with coexisting musculoskeletal symptoms (29,34). In the Johnston County Osteoarthritis Project (n = 2,572), Golightly et al (29) noted that foot symptoms were reported by 37.0% and knee symptoms were reported by 50.1% of participants. In the Progression Cohort of the Osteoarthritis Initiative (n = 1,389), Suri et al (34) found that 16.6%, 57.4%, and 87.9% of individuals reported foot, back, and knee pain, respectively. Taken together, these studies provide a context to facilitate generalizability of our findings and also underscore the presence of musculoskeletal pain comorbidity in community-dwelling adults.
Another key feature of the current study is that we quantified plantar loading in one of the largest cohorts studied to date. The patterns and magnitude of plantar loading noted in the current study are consistent with recent reports quantifying plantar loading using similar technology, methods, and definitions of regions of interest (35). While a substantial body of literature supports the presence of mechanical overloading strategies in individuals with musculoskeletal pain, our study is the first that we are aware of to provide objective evidence supporting the presence of pain avoidance loading patterns. Evidence supporting the presence of mechanical overloading, reflected as increased plantar pressure, comes from recent studies in individuals with OA or RA. Zammitt et al (12) noted that individuals with radiographically defined first MTP joint OA demonstrated 23% increased peak pressure under the hallux compared to age- and sex-matched control subjects. Similarly, in individuals with midfoot OA, higher pressure was noted under the medial midfoot compared to age-, sex-, and BMI-matched control subjects (10,36). In individuals with RA, high forefoot pressure was associated with pain during barefoot walking (37). Taken together, these data support the mechanical overloading theory and indicate that regional plantar loading is directly related to patients’ symptoms. Consequently, current clinical decision-making and most of the existing literature support alleviating symptoms using strategies that decrease plantar loading (e.g., footwear or surgery).
In contrast, our results suggest that antalgic (pain avoidance) gait patterns may predominate in individuals with first MTP pain. Adjusting for age, sex, BMI, knee OA status, and walking speed, we found a modest and statistically significant relationship between regional (hallucal and second metatarsal) loading and odds of first MTP pain. Contrary to our hypothesis, we did not find evidence for lateral load transfer in our results. Evidence for lateral load transfer has been reported in small subgroups (25–30% of the study sample) in previous clinical studies assessing preoperative plantar load distribution patterns in individuals with first MTP OA (38,39). Recent evidence from a large population-based cohort showed that individuals with forefoot-only pain showed lower toe loads and higher midfoot and rear-foot loads (40). Taken together, these results may indicate that individuals with foot pain deploy multiple different load redistribution strategies. Some individuals may adopt a medial-lateral strategy while others may show an anterior-posterior redistribution. Future studies that are longitudinal in design and studies that stratify patients by the severity of their foot pain are essential to examine the development (or resolution) of plantar load redistribution strategies. Longitudinal studies are also indicated to examine the long-term consequences of pain avoidance strategies in individuals with foot pain. In contrast to mechanical overloading, the management of pain avoidance has received little attention in the literature. Based on physical stress theory, graduated reloading may be an especially relevant treatment goal in this population (16). Our findings, supporting pain avoidance, suggest that restoration of load distribution may be an important but frequently overlooked potential treatment goal in individuals with frequent first MTP disorders.
Cumulative stress is a measure of overall mechanical load sustained at the foot-floor interface, and may be relevant in individuals with musculoskeletal pain (41). Cumulative stress quantifies not only the magnitude of plantar pressure but also the number of steps taken over a day. This study is the first in the literature to present an estimate of cumulative stress in individuals with foot pain. However, in the current study, we did not find evidence supporting a cross-sectional relationship between cumulative plantar stress and first MTP pain, despite finding a relationship between PTI and first MTP pain. One possible reason for this finding may be that individuals experiencing first MTP pain reduce plantar load distribution by changing lower extremity biomechanics. This reduction in PTI may ameliorate symptoms and may not necessitate additional pain avoidance mechanisms, such as a systematic reduction in physical activity. Additionally, altering the number of steps taken per day may be influenced by a large number of social and environmental factors. Recent studies in individuals with musculoskeletal disorders show that while pain and health status can be barriers to physical activity, other factors such as support and access may facilitate physical activity (42). The lack of association with cumulative plantar stress in our study may suggest that subjects in our cohort did not limit their walking (steps/day) as a pain-avoidance mechanism. Longitudinal studies are needed to examine changes in the quantity of walking behavior in individuals with foot pain.
In summary, this is first study to simultaneously assess pain, plantar loading, and cumulative stress in a large, population-based cohort of older adults. Our results suggest that antalgic gait patterns may predominate in individuals with first MTP pain. The findings of our study must be interpreted in light of its limitations. The chief limitations are its cross-sectional design and the potential role of additional factors, such as joint deformity and foot posture, that may mediate the relationship between plantar loading and foot pain. A subset of the sample in our study may have had radiographic first MTP OA. Individuals in this subset (who have both first MTP pain and radiographic OA) could employ several possible modifications, depending on the underlying pathology. For instance, factors such as joint deformity (43) and external foot progression angle during walking (44) may influence the relationship between first MTP pain and plantar loads. Future studies examining plantar load and cumulative stress in the full spectrum of first MTP disorders are indicated to identify the discrete contributions of plantar load and radiographic changes to the prevalence of MTP pain.
In future studies, alternative biomechanical pathways that may mediate pain, such as joint range of motion (39), external foot progression angle (44), and foot posture, should be assessed. In healthy subjects, a recent simulation supports the contention that external foot progression angle may decrease medial and increase lateral loading (44). In individuals with first MTP OA, pronated foot posture has been hypothesized to contribute to increased symptom severity (45,46). However, objective evidence is mixed (47,48). Longitudinal studies are lacking and previous cross-sectional studies suggest that age and BMI play important roles in mediating first MTP symptoms (47,48).
Future studies should evaluate both the presence and severity of foot pain using robust outcome instruments. Most importantly, longitudinal studies are indicated to examine whether the incidence and progression of foot pain are related to the magnitude of plantar loading or cumulative plantar stress.
Significance & Innovations.
Foot pain results in significant disability and increased health care utilization. Mechanical loads, quantified terms of plantar stress over a step, and cumulative plantar stress over a day, have been postulated to contribute to foot pain.
In contrast to this mechanical overloading hypothesis, some studies suggest that individuals experiencing foot pain adopt an antalgic strategy to avoid exacerbating their foot pain. An antalgic strategy is characterized by lower plantar loading, and may reflect an attempt at pain avoidance. Objective data quantifying the presence of either loading strategy are not available. These data are the necessary precursors to motivate the design of targeted, effective intervention strategies.
To address this critical gap in the literature, we examined the relationship between plantar loading during walking and first metatarsophalangeal (MTP) joint pain among older adults.
Our findings uncovered the presence of an antalgic gait strategy. Lower pressure time integral was modestly associated with increased prevalence of frequent first MTP pain at both the hallux and second metatarsal. The lack of association with cumulative plantar stress may suggest that the individuals with first MTP pain in this cohort did not limit their walking as a pain-avoidance mechanism.
Acknowledgments
Dr. Rao’s work was supported by the Rheumatology Research Foundation Scientist Development Award. The work of Drs. Nevitt, Lewis, Torner, and Felson was supported by the National Institute on Aging (grants AG-19069, AG-18947, AG-18832, and AG-18820, respectively).
Footnotes
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Dr. Rao had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design. Rao, Gross, Nevitt, Torner, Hillstrom.
Acquisition of data. Gross, Nevitt, Lewis, Torner, Hietpas, Hillstrom.
Analysis and interpretation of data. Rao, Niu, Torner, Felson, Hillstrom.
References
- 1.Zammit GV, Munteanu SE, Menz HB. Development of a diagnostic rule for identifying radiographic osteoarthritis in people with first metatarsophalangeal joint pain. Osteoarthritis Cartilage. 2011;19:939–45. doi: 10.1016/j.joca.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 2.Thomas MJ, Roddy E, Zhang W, Menz HB, Hannan MT, Peat GM. The population prevalence of foot and ankle pain in middle and old age: a systematic review. Pain. 2011;152:2870–80. doi: 10.1016/j.pain.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 3.Gilheany MF, Landorf KB, Robinson P. Hallux valgus and hallux rigidus: a comparison of impact on health-related quality of life in patients presenting to foot surgeons in Australia. J Foot Ankle Res. 2008;1:14. doi: 10.1186/1757-1146-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keysor JJ, Dunn JE, Link CL, Badlissi F, Felson DT. Are foot disorders associated with functional limitation and disability among community-dwelling older adults? J Aging Health. 2005;17:734–52. doi: 10.1177/0898264305280998. [DOI] [PubMed] [Google Scholar]
- 5.Gorter K, Kuyvenhoven M, de Melker R. Health care utilisation by older people with non-traumatic foot complaints. What makes the difference? Scand J Prim Health Care. 2001;19:191–3. doi: 10.1080/028134301316982450. [DOI] [PubMed] [Google Scholar]
- 6.Andriacchi TP, Mundermann A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr Opin Rheumatol. 2006;18:514–8. doi: 10.1097/01.bor.0000240365.16842.4e. [DOI] [PubMed] [Google Scholar]
- 7.Hunter DJ, McDougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Rheum Dis Clin North Am. 2008;34:623–43. doi: 10.1016/j.rdc.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu J, Cheung JT, Fan Y, Zhang Y, Leung AK, Zhang M. Development of a finite element model of female foot for high-heeled shoe design. Clin Biomech (Bristol, Avon) 2008;23(Suppl 1):S31–8. doi: 10.1016/j.clinbiomech.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Ellis SJ, Yu JC, Johnson AH, Elliott A, O’Malley M, Deland J. Plantar pressures in patients with and without lateral foot pain after lateral column lengthening. J Bone Joint Surg Am. 2010;92:81–91. doi: 10.2106/JBJS.H.01057. [DOI] [PubMed] [Google Scholar]
- 10.Rao S, Baumhauer JF, Nawoczenski DA. Is barefoot regional plantar loading related to self-reported foot pain in patients with midfoot osteoarthritis? Osteoarthritis Cartilage. 2011;19:1019–25. doi: 10.1016/j.joca.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Van Gheluwe B, Dananberg HJ, Hagman F, Vanstaen K. Effects of hallux limitus on plantar foot pressure and foot kinematics during walking. J Am Podiatr Med Assoc. 2006;96:428–36. doi: 10.7547/0960428. [DOI] [PubMed] [Google Scholar]
- 12.Zammit GV, Menz HB, Munteanu SE, Landorf KB. Plantar pressure distribution in older people with osteoarthritis of the first metatarsophalangeal joint (hallux limitus/rigidus) J Orthop Res. 2008;26:1665–9. doi: 10.1002/jor.20700. [DOI] [PubMed] [Google Scholar]
- 13.Nawoczenski DA. Nonoperative and operative intervention for hallux rigidus. J Orthop Sports Phys Ther. 1999;29:727–35. doi: 10.2519/jospt.1999.29.12.727. [DOI] [PubMed] [Google Scholar]
- 14.Shereff MJ, Baumhauer JF. Hallux rigidus and osteoarthrosis of the first metatarsophalangeal joint. J Bone Joint Surg Am. 1998;80:898–908. doi: 10.2106/00004623-199806000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Schmiegel A, Rosenbaum D, Schorat A, Hilker A, Gaubitz M. Assessment of foot impairment in rheumatoid arthritis patients by dynamic pedobarography. Gait Posture. 2008;27:110–4. doi: 10.1016/j.gaitpost.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Mueller MJ, Maluf KS. Tissue adaptation to physical stress: a proposed “Physical Stress Theory” to guide physical therapist practice, education, and research. Phys Ther. 2002;82:383–403. [PubMed] [Google Scholar]
- 17.Maluf KS, Mueller MJ. Comparison of physical activity and cumulative plantar tissue stress among subjects with and without diabetes mellitus and a history of recurrent plantar ulcers. Clin Biomech (Bristol, Avon) 2003;18:567–75. doi: 10.1016/s0268-0033(03)00118-9. [DOI] [PubMed] [Google Scholar]
- 18.Sangeorzan BJ, Beskin JL, Britt SM, Brage M, Holt S, Kadel NJ. Issues of importance to patients seeking care from members of the AOFAS: a preliminary report of the outcomes committee of the AOFAS. Foot Ankle Int. 2005;26:638–44. doi: 10.1177/107110070502600811. [DOI] [PubMed] [Google Scholar]
- 19.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56:2986–92. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 20.McPoil TG, Cornwall MW, Dupuis L, Cornwall M. Variability of plantar pressure data: a comparison of the two-step and midgait methods. J Am Podiatr Med Assoc. 1999;89:495–501. doi: 10.7547/87507315-89-10-495. [DOI] [PubMed] [Google Scholar]
- 21.Meyers-Rice B, Sugars L, McPoil T, Cornwall MW. Comparison of three methods for obtaining plantar pressures in nonpathologic subjects. J Am Podiatr Med Assoc. 1994;84:499–504. doi: 10.7547/87507315-84-10-499. [DOI] [PubMed] [Google Scholar]
- 22.Ellis SJ, Stoecklein H, Yu JC, Syrkin G, Hillstrom H, Deland JT. The accuracy of an automasking algorithm in plantar pressure measurements. HSS J. 2011;7:57–63. doi: 10.1007/s11420-010-9185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burns J, Crosbie J, Hunt A, Ouvrier R. The effect of pes cavus on foot pain and plantar pressure. Clin Biomech (Bristol, Avon) 2005;20:877–82. doi: 10.1016/j.clinbiomech.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 24.Schmiegel A, Vieth V, Gaubitz M, Rosenbaum D. Pedography and radiographic imaging for the detection of foot deformities in rheumatoid arthritis. Clin Biomech (Bristol, Avon) 2008;23:648–52. doi: 10.1016/j.clinbiomech.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 25.Gurney JK, Kersting UG, Rosenbaum D. Between-day reliability of repeated plantar pressure distribution measurements in a normal population. Gait Posture. 2008;27:706–9. doi: 10.1016/j.gaitpost.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 26.Menz HB, Zammit GV, Munteanu SE. Plantar pressures are higher under callused regions of the foot in older people. Clin Exp Dermatol. 2007;32:375–80. doi: 10.1111/j.1365-2230.2007.02421.x. [DOI] [PubMed] [Google Scholar]
- 27.Shepherd EF, Toloza E, McClung CD, Schmalzried TP. Step activity monitor: increased accuracy in quantifying ambulatory activity. J Orthop Res. 1999;17:703–8. doi: 10.1002/jor.1100170512. [DOI] [PubMed] [Google Scholar]
- 28.Lott DJ, Maluf KS, Sinacore DR, Mueller MJ. Relationship between changes in activity and plantar ulcer recurrence in a patient with diabetes mellitus. Phys Ther. 2005;85:579–88. [PubMed] [Google Scholar]
- 29.Golightly YM, Hannan MT, Shi XA, Helmick CG, Renner JB, Jordan JM. Association of foot symptoms with self-reported and performance-based measures of physical function: the Johnston County osteoarthritis project. Arthritis Care Res (Hoboken) 2011;63:654–9. doi: 10.1002/acr.20432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Menz HB, Dufour AB, Casey VA, Riskowski JL, McLean RR, Katz P, et al. Foot pain and mobility limitations in older adults: the Framingham Foot Study. J Gerontol A Biol Sci Med Sci. 2013;68:1281–5. doi: 10.1093/gerona/glt048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomas E, Peat G, Croft P. Defining and mapping the person with osteoarthritis for population studies and public health. Rheumatology (Oxford) 2014;53:338–45. doi: 10.1093/rheumatology/ket346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Badlissi F, Dunn JE, Link CL, Keysor JJ, McKinlay JB, Felson DT. Foot musculoskeletal disorders, pain, and foot-related functional limitation in older persons. J Am Geriatr Soc. 2005;53:1029–33. doi: 10.1111/j.1532-5415.2005.53315.x. [DOI] [PubMed] [Google Scholar]
- 33.Benvenuti F, Ferrucci L, Guralnik JM, Gangemi S, Baroni A. Foot pain and disability in older persons: an epidemiologic survey. J Am Geriatr Soc. 1995;43:479–84. doi: 10.1111/j.1532-5415.1995.tb06092.x. [DOI] [PubMed] [Google Scholar]
- 34.Suri P, Morgenroth DC, Kwoh CK, Bean JF, Kalichman L, Hunter DJ. Low back pain and other musculoskeletal pain comorbidities in individuals with symptomatic osteoarthritis of the knee: data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken) 2010;62:1715–23. doi: 10.1002/acr.20324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bryant AR, Tinley P, Singer KP. Normal values of plantar pressure measurements determined using the EMED-SF system. J Am Podiatr Med Assoc. 2000;90:295–9. doi: 10.7547/87507315-90-6-295. [DOI] [PubMed] [Google Scholar]
- 36.Menz HB, Munteanu SE, Zammit GV, Landorf KB. Foot structure and function in older people with radiographic osteoarthritis of the medial midfoot. Osteoarthritis Cartilage. 2010;18:317–22. doi: 10.1016/j.joca.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 37.Van der Leeden M, Steultjens M, Dekker JH, Prins AP, Dekker J. Forefoot joint damage, pain and disability in rheumatoid arthritis patients with foot complaints: the role of plantar pressure and gait characteristics. Rheumatology (Oxford) 2006;45:465–9. doi: 10.1093/rheumatology/kei186. [DOI] [PubMed] [Google Scholar]
- 38.Mulier T, Steenwerckx A, Thienpont E, Sioen W, Hoore KD, Peeraer L, et al. Results after cheilectomy in athletes with hallux rigidus. Foot Ankle Int. 1999;20:232–7. doi: 10.1177/107110079902000405. [DOI] [PubMed] [Google Scholar]
- 39.Nawoczenski DA, Ketz J, Baumhauer JF. Dynamic kinematic and plantar pressure changes following cheilectomy for hallux rigidus: a mid-term followup. Foot Ankle Int. 2008;29:265–72. doi: 10.3113/FAI.2008.0265. [DOI] [PubMed] [Google Scholar]
- 40.Riskowski JL, Hagedorn TJ, Dufour AB, Hannan MT. Associations of region-specific foot pain and foot biomechanics: the Framingham Foot Study. J Gerontol A Biol Sci Med Sci. 2015;70:1281–8. doi: 10.1093/gerona/glv067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maly MR, Robbins SM, Stratford PW, Birmingham TB, Callaghan JP. Cumulative knee adductor load distinguishes between healthy and osteoarthritic knees: a proof of principle study. Gait Posture. 2013;37:397–401. doi: 10.1016/j.gaitpost.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 42.McPhail SM, Schippers M, Marshall AL, Waite M, Kuipers P. Perceived barriers and facilitators to increasing physical activity among people with musculoskeletal disorders: a qualitative investigation to inform intervention development. Clin Interv Aging. 2014;9:2113–22. doi: 10.2147/CIA.S72731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Keiserman LS, Sammarco VJ, Sammarco GJ. Surgical treatment of the hallux rigidus. Foot Ankle Clin. 2005;10:75–96. doi: 10.1016/j.fcl.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 44.Rosenbaum D. Foot loading patterns can be changed by deliberately walking with in-toeing or out-toeing gait modifications. Gait Posture. 2013;38:1067–9. doi: 10.1016/j.gaitpost.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 45.Mahiquez MY, Wilder FV, Stephens HM. Positive hindfoot valgus and osteoarthritis of the first metatarsophalangeal joint. Foot Ankle Int. 2006;27:1055–9. doi: 10.1177/107110070602701210. [DOI] [PubMed] [Google Scholar]
- 46.Zammit GV, Menz HB, Munteanu SE. Structural factors associated with hallux limitus/rigidus: a systematic review of case control studies. J Orthop Sports Phys Ther. 2009;39:733–42. doi: 10.2519/jospt.2009.3003. [DOI] [PubMed] [Google Scholar]
- 47.Munteanu SE, Zammit GV, Menz HB. Factors associated with foot pain severity and foot-related disability in individuals with first metatarsophalangeal joint OA. Rheumatology (Oxford) 2012;51:176–83. doi: 10.1093/rheumatology/ker344. [DOI] [PubMed] [Google Scholar]
- 48.Menz HB, Roddy E, Marshall M, Thomas MJ, Rathod T, Myers H, et al. Demographic and clinical factors associated with radiographic severity of first metatarsophalangeal joint osteoarthritis: cross-sectional findings from the Clinical Assessment Study of the Foot. Osteoarthritis Cartilage. 2015;23:77–82. doi: 10.1016/j.joca.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]