Abstract
Introduction
Pediatric delirium assessment is complicated by variations in baseline language and cognitive skills, regression of skills during illness, and absence of pediatric-specific modifiers within the Diagnostic and Statistical Manual of Mental Disorders (DSM) delirium criterion.
Objective
To develop a standardized approach to pediatric delirium assessment by psychiatrists.
Methods
A multidisciplinary group of clinicians used DSM criterion as the foundation for the Vanderbilt Assessment for Delirium in Infants and Children (VADIC). Pediatric-specific modifiers were integrated into the delirium criterion, including key developmental and assessment variations for children. The VADIC was used in clinical practice to prospectively assess critically ill infants and children. The VADIC was assessed for content validity by the American Academy of Child and Adolescent Psychiatry (AACAP) Delirium Special Interest Group (SIG).
Results
The AACAP-Delirium SIG determined that the VADIC demonstrated high content validity. The VADIC 1) preserved the core DSM delirium criterion; 2) appropriately paired interactive assessments with key criterion based on development, and 3) addressed confounders for delirium. A cohort of 300-patients with a median age of 20 months was assessed for delirium using the VADIC. Delirium prevalence was 47%.
Conclusion
The VADIC provides a comprehensive framework to standardize pediatric delirium assessment by psychiatrists. The need for consistency in both delirium education and diagnosis is highlighted given the high prevalence of pediatric delirium.
Keywords: Teaching methods, Delirium, Education, Psychiatry, Pediatric, Assessment
INTRODUCTION
Delirium assessment, management, and monitoring protocols are inconsistent among hospitalized pediatric patients including those in the ICU setting (1). With the advanced understanding of delirium in adults, there has been momentum to create and validate bedside tools for delirium screening and monitoring in pediatrics (2–10). Accurate delirium diagnosis is paramount and the Diagnostic and Statistical Manual (DSM) of Mental Disorders provides the framework for the psychiatrist’s core delirium assessment. For pediatric patients, however, the clinician must have the expertise to further incorporate learned variations in developmental stages of language and cognition (11) with the pathophysiology of illness given that pediatric-specific modifiers are not currently provided in the DSM.
Pediatric delirium is extremely common among critically ill infants and children (6–10). Acute brain dysfunction or delirium can occur during illness in the setting of hypoxia, hypo-perfusion, electrolyte abnormalities, or even iatrogenic factors such as excessive sedation, withdrawal, or sleep wake cycle disturbances. The associated behavioral dysregulation of delirium, especially with the hyperactive subtype, may be highly disruptive or dangerous to the patient or staff. Initial management choices by the medical team may include sedatives that while causing a patient to appear ‘sedate or calm’ temporarily, may actually exacerbate the acute brain dysfunction, creating a cyclic worsening and prolonged duration or severity of delirium. Child and Adolescent Psychiatry (CAP) Consultation Liaison (CL) services have the opportunity to promote delirium education for pediatricians, pediatric critical care teams, and psychiatry trainees while providing confirmatory delirium diagnosis (12, 13) including a differential for possible etiologies, treatment targets, and management strategies to modulate undesirable behavioral manifestations (14, 15).
The objective of this clinical project was to develop a reliable approach for qualitative delirium assessment in children by clinicians to promote consistencies in diagnosis and education.
METHODS
Development of the Vanderbilt Assessment for Delirium in Infants and Children
The DSM is a classification system that is based on both clinical expertise and available evidence based medicine to standardize criteria for the diagnosis of mental illness by health professionals. The most recent fifth edition, the DSM 5 (16), highlights both inattention and alteration in awareness as key diagnostic features, a commonly occurring fluctuating course of altered mental status, and an additional disturbance in cognition, for the diagnosis of delirium. There is significant variability for the diagnosis of pediatric delirium among clinicians.
The VADIC was developed by CAPs and pediatric professionals to standardize clinical psychiatrists in the assessment of delirium in sick infants and children in the preschool Confusion Assessment Method (psCAM) study (8). Specific challenges for delirium assessment in the hospitalized pediatric patient include: 1) baseline variations in language and cognitive development, 2) regression during illness of previously learned skills, 3) incapacity to speak due to presence of an endotracheal tube or mask, 4) differences in methods of communication due to affect or internal experience, and 5) expected age associated separation or stranger anxiety. The VADIC organizes the use of key tasks to assess for core DSM criteria such as attention, arousal, and cognition in pediatric patients of all ages. To facilitate delirium detection in hospitalized children, pediatric-specific behaviors demonstrating developmental and cognitive variations were integrated into the VADIC. The VADIC structures the assessment around patients demonstrating the lowest acceptable level of arousal, attention, and cognition which would determine the absence of delirium.
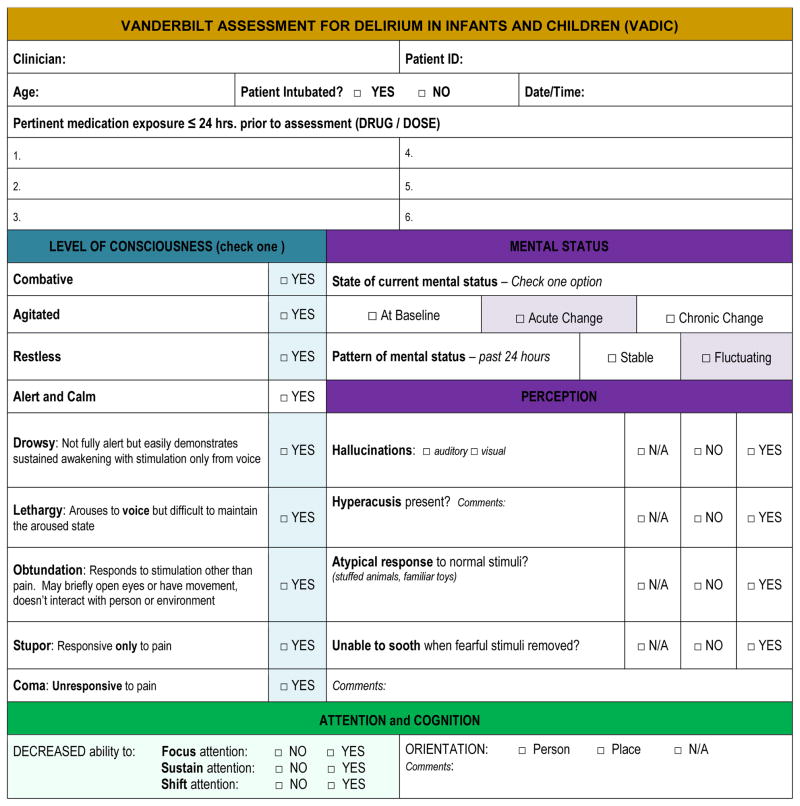
The Vanderbilt Assessment of Delirium in Infants and Children (VADIC) (Figure 1)
Figure 1.
Vanderbilt Assessment for Delirium in Infants and Children (VADIC) Form
OVERVIEW
The VADIC form guides the assessor to document direct observations and interactive assessments which highlight key delirium features such as inattention in pediatric patients. The form is separated into six (6) subdomains including: 1) level of consciousness, 2) mental status and perception, 3) attention and cognition, 4) sleep wake cycle, 5) affect, and 6) language and thought. The VADIC form organizes behavioral observations made both in the moment and over the past 24 hours within these domains anchored to DSM criterion. The assessor is also prompted by the VADIC form to document illness status such as acute hypoxia or respiratory distress, recent or significant amounts of sedation and/or analgesia, hypotension, recent fever, or other possible factors.
The approach to patient assessment using the VADIC recognizes the importance of family involvement and the need for reassurance that many pediatric patients require. The examiner is encouraged to utilize the bedside caregivers to engage with the child for required tasks through play, and compare the child’s reaction in the moment to the previously established baseline expectation. For example, the parent may be asked to present a favored toy to the patient to see if the child acts in a typical manner (e.g. reaching out for the toy, smiling with parent). The assessor may also engage in the same task and note for any signs of anxiety. If there is anxiety, the examiner notes how the parent comforts the child, how long it takes the child to soothe, and if this is congruent with baseline. Serial documentation of the pattern in patient responses to these objective assessments facilitates the tracking of the course of attention and cognition. Repetition of tasks guided by serial use of the VADIC provides a consistent approach to longitudinal data collection regarding the presence or absence of delirium.
Delirium by its nature waxes and wanes over time; therefore the VADIC form supports documentation of both an “acute” and a “24-hour” assessment. The 24-hour determination documents delirium in the context of a fluctuating course. The clinician documents factors contributing to the diagnosis of delirium if the patient does not demonstrate key features of delirium “in the moment.”
DEVELOPMENTAL LEVEL
Psychiatric assessment for delirium in children requires determination of baseline development and mental status via a detailed history and physical. Psychiatrists must organize their clinical observations and patient interactions based on developmentally expected variability in communication, attention, and cognition, particularly in infants and preschool-aged children. The VADIC structures observation of sleep patterns, motor and speech capabilities, typical reactions to toys, and characteristic interactions during games such as peek-a-boo, in order to assess real-time variations from baseline.
LEVEL OF CONSCIOUSNESS and MENTAL STATUS
Alteration in awareness is a core feature for delirium diagnosis. Awareness is a function dependent on level of consciousness or arousal, on the ability to focus and sustain attention, and on the cognitive capacity to appreciate differences. It is valuable for a clinician to use an objective sedation scale when assessing the patient’s level of consciousness. The VADIC uses descriptions of various levels of consciousness similar to those used in the Richmond Agitation Sedation Scale (RASS) (17) and the State Behavioral Scale (18). The assessor first observes the patient for presence or absence of agitation without engaging. Then, if the eyes are closed, the assessor ‘talks’ to the patient to get a response, observing for various levels of eye contact or limb movement. Finally, the assessor provides physical stimuli for a patient response (i.e. stupor or coma).
The accurate and consistent assessment of arousal requires the consideration that a deeply asleep child may be confused with a child who truly has an altered level of consciousness. Therefore, the clinician must consider whether additional stimulation is needed during the arousal assessment to differentiate a patient with deep sleep versus decreased level of consciousness. If further physical stimulation (15 seconds) is deemed necessary in more sedate patients, the arousal state is then re-assessed following a non-stimulating period (15 seconds). For delirium to be present, an abrupt change or fluctuation from baseline mental status must be observed or documented. Patterns of fluctuation may be subtle and assumed to simply be part of the severe illness or medication administration. These fluctuations, regardless of etiology, are important to document on the VADIC form which may help differentiate the cause of delirium.
ATTENTION and COGNITION
Attentional disturbance is an essential feature for delirium diagnosis and can impact ways in which we can assess other components of cognition. Attention involves focusing and processing information from our surroundings. When a patient is unable to attend then the ability to comprehend, reason, respond, and form memory is negatively affected. Use of pediatric-specific tasks facilitates the examiner’s ability to assess both attention and cognition. One illustration of this would be having the parent walk from one side of the bed to the other and observe how the patient focuses and sustains attention with the parent through this movement and comparing reactions in that circumstance to the evaluator (relatively unknown to patient) performing the same task. The evaluator asks the parent if the reactions are baseline behavior or not in each interaction, and if not, the parent describes the differences observed. Another task may be presenting the child with a favored toy and then exchanging it for something less favored or removing it completely and noting the changes in behavior. In this way, one is noting the ability to focus and sustain attention on the toy and the cognitive task of recognizing the favored toy as demonstrated through the affective response. The clinician observes how the parent consoles the child to compare responses to comforting compared to baseline in terms of response and duration.
By making explicit the need to consider perception, language, sleep, and different characteristics of cognition, the assessor is required to consistently consider the developmental context. For example, a three-year-old child will demonstrate a different pattern of sleep and language at baseline compared to a six-month old child. A child who has been chronically ill may not develop along the typical neurologic or motor milestone trajectory. The minimum tasks necessary to establish the presence of basic attention and cognition can be done across developmental levels. For example, a non-delirious child should demonstrate the capacity to express preference for a game or toy regardless of age or developmental level even though the game or toy used by the examiner will vary with the age of the child. As a result, the VADIC form can assist the clinician to assess for the presence or absence of delirium in children with sufficient level of arousal even when medically fragile or with developmental delay.
CONFOUNDERS FOR DELIRIUM ASSESSMENT
Pain, anxiety, and temperament may influence the expression of attention and cognition among infants and preschool-aged children (19). While sleep disturbance is not a criterion of delirium diagnosis, it is a factor that influences attention and other cognitive tasks. Observations and assessment of these factors are incorporated into the VADIC to ensure consideration as part of the delirium assessment. For example, temperament and anxiety can affect the willingness of a child to follow commands or engage in the tasks used to assess for inattention by an unknown examiner versus familiar caregivers. The assessor may conceal their presence while observing a child who has become fearful of providers entering the room but appears comfortable when there is only family, thereby factoring level of anxiety into mental status assessment of delirium.
Pain may also contribute to behavioral changes; the assessor should note on the VADIC form the recent administration of analgesia and the subsequent pharmacologic effects on affect and demeanor. The potential effects of both acute pain and recent analgesia influence the mental status particularly in pediatric patients. The examiner should document parental or familiar care-giver descriptions of “usual” sick behavior and caregiver observations about the ability to console the child when not delirious. This provides a baseline for assessment of response to pain in acute illness and emphasizes the critical importance of obtaining a history from parents and familiar hospital caregivers to understand the baseline capabilities versus the patient’s current level of functioning.
DELIRIUM DETERMINATION ON THE VADIC
As the clinician completes the form, the determination of delirium involves presence of an acute change in level of consciousness (box 1), with a fluctuating course (box 2) and inattention (box 3), which can be satisfied by any of the factors occurring (decreased focus, decreased sustaining of attention, or difficulty shifting attention). An additional disturbance of cognition (box 5) should be present as well as a change in affect (box 7) after excluding pain or anxiety as the contributor. Items that are supportive of delirium being present are inconsolability, perceptual disturbances, sleep/wake changes, and changes in language/thought. At least one of these factors (boxes 4, 6, or 8) must be present as well for the diagnosis of delirium. Subsyndromal delirium would be diagnosed if boxes 1 and 2 were present plus one of boxes 3 or 5 or 7.
RESULTS
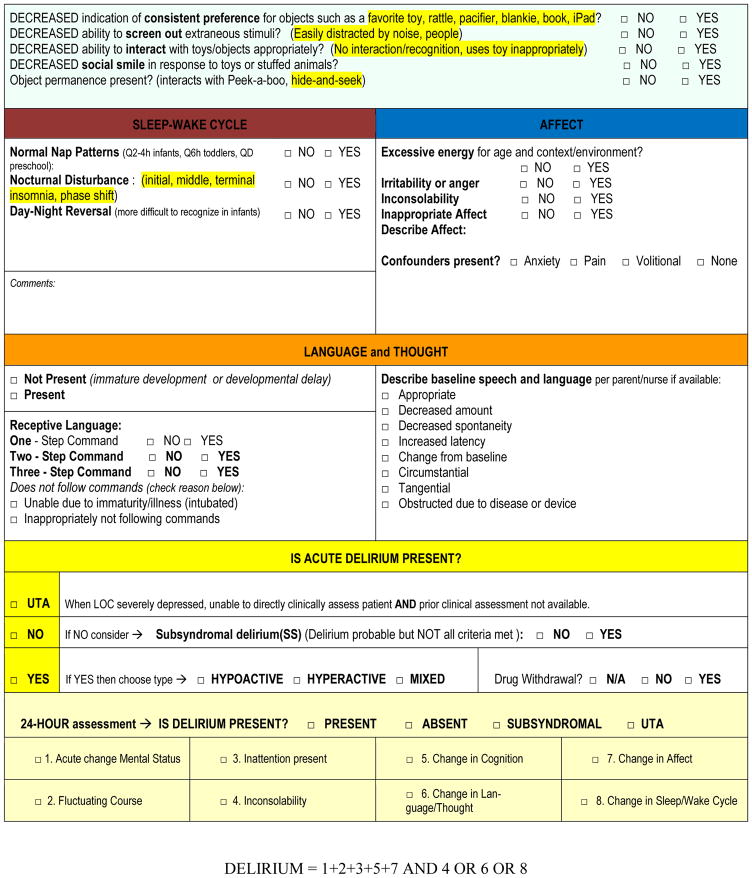
Members of the Physically Ill Child Committee Special Interest Group (SIG) of the American Academy of Child and Adolescent Psychiatry (AACAP) reviewed the VADIC form for content validity. This group is comprised of CAP CL psychiatrists from ten institutions who have expertise in delirium. Content validity is the estimate of how much a measure (the VADIC form) represents the trait it is measuring (in this case delirium). No attempt was made in determining construct or criterion validity. This form represents a qualitative way to operationalize the psychiatric assessment, utilizing the DSM 5 as the current diagnostic standard (13). There was agreement that the VADIC met content validity. The VADIC form was enhanced through expert feedback to include an index to help guide clinicians in the use of the form and to include a list of potential contributing factors for delirium that may impact normal behavior/development such as recent trauma, influence of anesthesia, pain, environmental factors, or a history of anxiety or depression. (Figure 2)
Figure 2.
Vanderbilt Assessment for Delirium in Infants and Children (VADIC) Supplemental Notes
The VADIC form was used by the CAP CL service in the prospective assessment of 300 critically ill patients (8), structuring the clinical assessment by the CAP team as part of the validation of a screening tool for preschool aged delirium. The median age of the cohort was 20 months (range 11–37 months) with 43% requiring mechanical ventilation at least one day, and the most common admission diagnosis being acute respiratory distress syndrome. The VADIC form promoted a consistent, organized approach to delirium assessment by faculty and trainees. Completion of the VADIC form including assessment time and chart review could take up to 30 minutes, structuring the time needed for an initial assessment; use of the form streamlined follow up assessments to less than ten minutes by providing both the baseline information and organizing serial completion of consistent tasks and observations. Documentation of a patient consultation using the VADIC form permitted CL CAP faculty to assure an in-depth assessment by trainees, review the developmental considerations for conclusions of atypical versus expected behaviors, and consider the pattern of assessed features used to make a final determination of delirium presence or absence. The structure of the form encourages consistency among all disciplines assessing for delirium in the pediatric population. Delirium prevalence was 47% in this 300-patient cohort. The most common motoric subtype was hypoactive delirium (64%), followed by the mixed (29%), and hyperactive (7%) subtypes (8).
Trainees who have utilized the VADIC Form and have now progressed to a leadership role as teachers of assessment of pediatric delirium have shared their thoughts on the experience of this tool. The VADIC form encouraged them to organize their interview to capture the necessary pieces of information into a clear narrative. Trainees reported that by compartmentalizing the information and assessing the patient daily in each sphere on the VADIC form, they could more confidently document their pattern of observations of any disturbance, assess young children at a developmentally appropriate level, and then view the patient as a whole in determining the presence or absence of delirium.
In our individual services, we have utilized the VADIC form to educate our colleagues and trainees on pediatric delirium. As part of the education process, learners participate in simulations using the VADIC form to evaluate patients on video or in-person. Subsequent discussion and debriefings occur to enhance the level of understanding and skill of the clinician. This type of serial training exercise promotes consistency amongst assessors and the documentation of delirium symptoms.
DISCUSSION
The VADIC provides the framework for the CAP CL to use core DSM delirium criterion and integrate both behavioral observations and patient reactions to developmentally appropriate interactive tasks as part of their delirium assessment. The DSM-5 does not provide pediatric-specific parameters for delirium criterion to account for developmental variability; rather, it is left to the clinician to determine whether a patient’s response is appropriate given their current environment, the pharmacologic regimen, presenting developmental stage, and expected regression based on the illness. Delirium recognition and treatment requires collaboration among nurses, pediatricians, pediatric intensivists, child psychiatrists, and other pediatric mental health professionals. The neuropsychiatric assessment of patients who are critically ill, very young, or have developmental delays at baseline is challenging. Child and adolescent psychiatrists play a valuable role in identifying or confirming the presence of delirium, differentiating behaviors related to pain or anxiety, and effectively communicating findings with the medical group. The VADIC can be used for education, assessment, and communication; the use of the form will vary by clinical training and clinical role. The psychiatry team is in a position to educate a new generation of child psychiatrists to work with critical care and general medical teams in the assessment and management of delirium.
In the absence of an understanding of normal variation in language and cognition among pediatric patients, (20–22) patient responses and behaviors can be misinterpreted as abnormal and lead to a delirium diagnosis when the abnormal patient response may be due to expected regression of skills during illness. Conversely, the expectation of skill regression may also skew interpretation of abnormal responses leading to under diagnosis of delirium. Both severity of illness and prolonged hospitalization may have complex consequences on development (23). Chronically ill children can demonstrate delays in speech and motor milestones and develop sensory or social dysfunction (24–28). Indeed, airway development, traumatic physical events, emotional dysregulation, and regression of skills may all impact individual language development and verbal expression (29). Hospitalized children commonly experience poor sleep hygiene, anxiety, fear, and pain, which influence the behaviors observed during delirium assessment. Additionally, sedation practices lead to abnormal arousal states, and may require that patients receive a higher level of stimulation prior to delirium assessment to enable more accurate patient observations. All of these factors in turn shape the pattern of expression of attention and cognition. The current lack of standardization in patient assessment confounds training regarding clinical assessment and biological understanding of pediatric delirium.
Understanding the development of acute changes in brain function and implementing both delirium monitoring and management protocols for children requires interdisciplinary contribution. Collaboration among nurses, intensivists, pediatricians, psychiatrists, and other child mental health professionals on the care of patients with delirium will promote a common understanding of delirium and language to accurately and consistently describe neuropsychiatric patient assessments. This collaboration will further the success of a cohesive strategy towards delirium management. The educational experience for trainees improves when they participate collaboratively in the assessment of pediatric delirium using a consistent approach that organizes the knowledge of child development and mental status assessment with the medical presentation of children with critical illness. The VADIC contributes to the educational experience by providing a structured and objective approach for delirium assessment and a consistent tool for communication with other disciplines leading to the possibility of improved care for critically ill children.
There is a limited number of child psychiatrists nationally and increasing awareness of the prevalence of delirium and its accompanying morbidity and mortality (4, 30, 31). The VADIC provides a conceptual structure for delirium among the various team members and facilitates a common language for all medical and mental health professionals to communicate clinical observations as the mental status evolves.
By improving the clinical skills of psychiatric and non-psychiatric providers in recognizing delirium in young children, we can improve clinical outcomes, reduce psychiatric morbidity, and implement preventative models to facilitate management algorithms. Effective teaching of CAP clinicians about pediatric delirium through the use of a structured assessment tool will position CAP as leaders in the teaching of all disciplines involved in critical care of children.
CONCLUSION
The VADIC provides a comprehensive framework to standardize pediatric delirium assessment by psychiatrists and trainees. Consistency for both delirium education and diagnosis is highlighted given the high prevalence of pediatric delirium.
Implications for Educators.
Identification of changes in attention and cognition are fundamental for diagnosis of pediatric delirium.
Assessment for pediatric delirium may be challenging in infants and younger children due to variations in language and cognitive development.
The observed clinical patterns and patient responses for the assessment of attention and cognition may be complicated by the critical care environment and necessary medical interventions.
The VADIC form provides a consistent and structured format for evaluating delirium and for teaching medical staff, medical and mental health practitioners, and trainees working with children how to conduct a pediatric delirium assessment.
Acknowledgments
Funding/Support: No external funding.
Footnotes
Potential Conflict of Interest: The authors have indicated they have no potential conflicts of interest to disclose.
Financial Disclosure: Dr. Smith was supported by the Foundation for Anesthesia Education and Research (FAER) and supported in part by the Vanderbilt CTSA grant UL1 TR000445 from NCRR/NIH.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Brummel NE, Vasilevskis EE, Han JH, Boehm L, Pun BT, Ely EW. Implementing delirium screening in the ICU: secrets to success. Crit Care Med. 2013;41(9):2196–2208. doi: 10.1097/CCM.0b013e31829a6f1e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blankespoor RJ, Janssen NJ, Wolters AM, Van Os J, Schieveld JN. Post-hoc revision of the pediatric anesthesia emergence delirium rating scale: clinical improvement of a bedside-tool? Minerva Anestesiol. 2012 Aug;78(8):896–900. [PubMed] [Google Scholar]
- 3.Janssen NJ, Tan EY, Staal M, et al. On the utility of diagnostic instruments for pediatric delirium in critical illness: an evaluation of the Pediatric Anesthesia Emergence Delirium Scale, the Delirium Rating Scale 88, and the Delirium Rating Scale-Revised R-98. Intensive Care Med. 2011 Aug;37(8):1331–7. doi: 10.1007/s00134-011-2244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schieveld JN, Leroy PL, van Os J, Nicolai J, Vos GD, Leentjens AF. Pediatric delirium in critical illness: phenomenology, clinical correlates and treatment response in 40 cases in the pediatric intensive care unit. Intensive Care Med. 2007 Jun;33(6):1033–40. doi: 10.1007/s00134-007-0637-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004 May;100(5):1138–1145. doi: 10.1097/00000542-200405000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Silver G, Traube C, Kearney J, et al. Detecting pediatric delirium: development of a rapid observational assessment tool. Intensive Care Med. 2012 Jun;38(6):1025–31. doi: 10.1007/s00134-012-2518-z. [DOI] [PubMed] [Google Scholar]
- 7.Smith HA, Boyd J, Fuchs DC, et al. Diagnosing delirium in critically ill children: Validity and reliability of the Pediatric Confusion Assessment Method for the Intensive Care Unit. Crit Care Med. 2011 Jan;39(1):150–7. doi: 10.1097/CCM.0b013e3181feb489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith HA, Gangopadhyay M, Goben CM, et al. The Preschool Confusion Assessment Method for the ICU: Valid and Reliable Delirium Monitoring for Critically Ill Infants and Children. Crit Care Med. 2016 Mar;44(3):592–600. doi: 10.1097/CCM.0000000000001428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Traube C, Silver G, Kearney J, Patel A, et al. Cornell Assessment of Pediatric Delirium: a valid, rapid, observational tool for screening delirium in the PICU*. Crit Care Med. 2014 Mar;42(3):656–63. doi: 10.1097/CCM.0b013e3182a66b76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Dijk M, Knoester H, van Beusekom BS, Ista E. Screening pediatric delirium with an adapted version of the Sophia Observation withdrawal Symptoms scale (SOS) Intensive Care Med. 2012 Mar;38(3):531–2. doi: 10.1007/s00134-011-2434-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silver G, Kearney J, Traube C, Hertzig M. Delirum screening anchored in child development: the Cornell assessment for pediatric delirium. Palliat Support Care. 2015 Aug;13(4):1005–11. doi: 10.1017/S1478951514000947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schieveld JN, van der Valk JA, Smeets I, et al. Diagnostic considerations regarding pediatric delirium: a review and a proposal for an algorithm for pediatric intensive care units. Intensive Care Med. 2009 Nov;35(11):1843–9. doi: 10.1007/s00134-009-1652-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silver G, Kearney J, Traube C, Atkinson TM, Wyka KE, Walkup J. Pediatric delirium: evaluating the gold standard. Palliat Support Care. 2015 Jun;13(3):513–6. doi: 10.1017/S1478951514000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith HA, Fuchs DC, Pandharipande PP, Barr FE, Ely EW. Delirium: an emerging frontier in the management of critically ill children. Crit Care Clin. 2009 Jul;25(3):593–614. x. doi: 10.1016/j.ccc.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith HA, Brink E, Fuchs DC, Ely EW, Pandharipande PP. Pediatric delirium: monitoring and management in the pediatric intensive care unit. Pediatr Clin North Am. 2013 Jun;60(3):741–60. doi: 10.1016/j.pcl.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Diagnostic and statistical manual of mental health disorders, Fifth Edition, (DSM-5) Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 17.Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation–Sedation Scale. Am J Respir Crit Care Med. 2001 Nov 15;166(10):1338–1344. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 18.Curley MA, Harris SK, Fraser KA, et al. State behavioral scale: a sedation assessment instrument for infants and young children supported on mechanical ventilation. Pediatr Crit Care Med. 2006 Mar;7(2):107–14. doi: 10.1097/01.PCC.0000200955.40962.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Compas BE, Connor-Smith J, Jaser SS. Temperament, Stress Reactivity, and Coping: Implications for Depression in Childhood and Adolescence. J Clin Child Adolesc Psychol. 2004 Mar;33(1):21–31. doi: 10.1207/S15374424JCCP3301_3. [DOI] [PubMed] [Google Scholar]
- 20.Schieveld JN, Staal M, Voogd L, Fincken J, Vos G, van Os J. Refractory agitation as a marker for pediatric delirium in very young infants at a pediatric intensive care unit. Intensive Care Med. 2010 Nov;36(11):1982–3. doi: 10.1007/s00134-010-1989-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silver GH1, Kearney JA, Kutko MC, Bartell AS. Infant delirium in pediatric critical care settings. Am J Psychiatry. 2010 Oct;167(10):1172–7. doi: 10.1176/appi.ajp.2010.09111606. [DOI] [PubMed] [Google Scholar]
- 22.Turkel SB, Jacobson JR, Tavare CJ. The diagnosis and management of delirium in infancy. Journal of Child and Adolescent Psychopharmacology. 2013 Jun;23(5):352–356. doi: 10.1089/cap.2013.0001. [DOI] [PubMed] [Google Scholar]
- 23.Mrazek DA. Continuities and Discontinuities in Development. New York, NY: Plenum Publishing Corp; 1984. Effects of Hospitalization on Early Child Development; pp. 211–225. [Google Scholar]
- 24.Colville G, Kerry S, Pierce C. Children’s factual and delusional memories of intensive care. Am J Respir Crit Care Med. 2008 May;177(9):976–982. doi: 10.1164/rccm.200706-857OC. [DOI] [PubMed] [Google Scholar]
- 25.Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. 1992 Jul;121(1):68–74. doi: 10.1016/s0022-3476(05)82544-2. [DOI] [PubMed] [Google Scholar]
- 26.Larsen GY, Donaldson AE, Parker HB, Grant MJ. Preventable harm occurring to critically ill children. Pediatr Crit Care Med. 2007 Jul;8(4):331–6. doi: 10.1097/01.PCC.0000263042.73539.99. [DOI] [PubMed] [Google Scholar]
- 27.Rees G, Gledhill J, Garralda ME, Nadel S. Psychiatric outcome following paediatric intensive care unit (PICU) admission: A cohort study. Intensive Care Med. 2004 Aug;30(8):1607–14. doi: 10.1007/s00134-004-2310-9. [DOI] [PubMed] [Google Scholar]
- 28.Smith HAB, Doran S, Sopfe J, et al. Executive dysfunction and post-traumatic stress disorders after critical illness in children. Crit Care Med. 2013 Dec;41(12) abstract 653. [Google Scholar]
- 29.Davydow DS, Richardson LP, Zatzick DF, Katon WJ. Psychiatric morbidity in pediatric critical illness survivors: a comprehensive review of the literature. Arch Pediatr Adolesc Med. 2010 Apr;164(4):377–385. doi: 10.1001/archpediatrics.2010.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schieveld JN, Leentjens AF, Jellinck MS. Delirium in Severely Ill Young Children in the Pediatric Intensive Care Unit (PICU) J Am Acad Child Adol Psychiat. 2005 Apr;44(4):392–4. doi: 10.1097/01.chi.0000153231.64968.1a. discussion 395. [DOI] [PubMed] [Google Scholar]
- 31.Turkel SB, Tavare CJ. Delirium in children and adolescents. J Neuropsychiatry Clin Neuro-sci. 2003 Fall;15(4):431–435. doi: 10.1176/jnp.15.4.431. [DOI] [PubMed] [Google Scholar]