Abstract
Background
Physical activity (PA) and its health benefits are a continuous point of discussion. Recommendations for children’s daily PA vary between guidelines. To better define the amount of PA necessary to prevent overweight and obesity in children, further research is needed. The present study investigates children’s compliance to physical activity guidelines (PAGs) and the association between objectively measured PA and body mass index (BMI).
Methods
Participating children were 11 years old (n = 419) and part of the European CHOP trial, which was conducted in Germany, Belgium, Poland, Spain, Italy. At least 2 days of PA measurements were collected from each child using a SenseWear™ armband. BMI was calculated from children’s height and weight. Thresholds of min·day−1 in PA needed to differentiate between normal and excess weight (overweight/obesity) were determined with Receiver Operator Characteristics (ROC) analysis. Additionally, adjusted linear and logistic regressions models were calculated for group differences and effects of a 5, 15 and 60 min·day−1 increases in PA on BMI.
Results
Median time spent in total PA was 462 min·day−1 (25th percentile; 75th percentile: 389; 534) and 75 min·day−1 (41; 115) in moderate to vigorous PA (MVPA). Girls spent 36 min·day−1 less in MVPA than boys and overweight/obese children 24 min·day−1 less than normal weight children (linear regression, p < 0.001). 63.2% of the children met PAGs of 60 min·day−1 in MVPA. The optimal threshold for min·day−1 in MVPA determined with ROC analysis was 46 min·day−1. Comparing 5, 15 and 60 min·day−1 increases in PA revealed that an additional 15 min·day−1 of vigorous PA had the same effect as 60 min·day−1 of MVPA. Sedentary time and light PA showed contrary associations to one another, with light PA being negatively and sedentary time being positively associated with excessive weight.
Conclusions
Current PAGs are met by 2/3 of children and seem appropriate to prevent excess weight in children. An official recommendation of daily 15–20 min of vigorous PA and further reduction of sedentary time could help to fight youth overweight and thus be of potential public health importance.
Trial registration
ClinicalTrials.gov Identifier: NCT00338689. Registered: June 19, 2006 (retrospectively registered).
Keywords: Physical activity guidelines, Obesity, Sensewear armband, Accelerometer
Background
Physical activity (PA), as stated by the World Health Organization (WHO) and confirmed by numerous studies, provides numerous health benefits [1], helps to prevent chronic diseases [2], balance daily energy expenditure (EE) and maintain a healthy body composition [3]. In 2008 the European Commission presented Physical Activity Guidelines (PAGs) for the European Union [4]. They cite the recommendations of the WHO: pre-school children should accumulate a minimum of 180 min·day−1of PA, children and adolescents (4–17 years) at least 60 min·day−1 in moderate- to vigorous-intensity PA (MVPA) and for adults a minimum of 30 min·day−1 in MVPA should be achieved [5]. While these recommendations specify the amount of MVPA for children, information about recommended daily time in other intensity levels of PA is lacking. The WHO recommends vigorous-intensity activities at least 3 times per week [5], but does not state an appropriate amount in min·day−1. Additionally, sedentary behaviour has changed dramatically in recent years [6] and is not specifically mentioned in current guidelines. Screen time of children and adolescents increased [7] and evidence of a causal relationship between sedentary behaviour and all-cause mortality continues to grow [8]. Large population data published in 2012 showed that, worryingly, 81% of the 13–15 year-old children worldwide are too inactive and do not meet current PAGs [9].
Overweight and obesity in children is still on the rise [10] and excessive weight in younger years negatively effects later health [11, 12]. Increasing PA, especially accompanied by healthy eating, can tackle this growing public health problem [13]. However, studies reported various results, when looking at activity and its effect on BMI. A review by Jansen and Leblanc [1] found only weak to modest relationships between PA and overweight/obesity in school-aged children. Mitchell et al. [14], confirmed these modest effects in normal weight children, but saw stronger associations in overweight children and demonstrated that PA is a valuable tool in fighting obesity.
With the rise and improvement of accelerometers in the last decade a re-evaluation of current PAGs is necessary. In light of this advancement, recent studies examined the association between LPA and weight in children, but found contrary results. For instance, studies by Kwon et al. [15] and Treuth et al. [16] found an negative correlation between LPA, body composition and BMI, whereas other studies reported no association between LPA and weight status [17, 18].
An ongoing examination of PA and sedentary time and its relation to BMI is essential to improve current PAGs [19] and help define the PA levels necessary to prevent adverse weight status in young people. The aim of this study is to examine objectively measured PA of children and their compliance to PAGs of 60 min·day−1 in MVPA per day and investigate whether these guidelines are adequate. Additionally, we analyse different intensities and durations of PA and sedentary time and how they are associated with BMI.
Methods
Study subjects and design
The underlying sample of children is part of the Childhood Obesity Project (CHOP) cohort. This European project was initiated in 2002 and recruited 1678 infants in Germany, Belgium, Italy, Spain and Poland during their first 8 weeks of life. The initial aim of the study was to investigate if different levels of dairy protein intake in early life influence BMI and body composition in later life [20]. Data for this analysis was collected during the 11 years follow up and represents a cross-sectional sample of 589 children, of which 445 had complete data on PA and anthropometry. Data collection was coordinated by 5 study teams in 8 urban and sub-urban areas: Germany (Nuremberg, Munich), Italy (Milano), Belgium (Brussels, Liege), Poland (Warsaw) and Spain (Reus, Tarragona). The trial was approved by ethics committees in each study centre and written informed consent was obtained from parents and children. All research was performed in accordance with the Declaration of Helsinki.
Activity assessment
Physical activity was measured using the SenseWear™ Armband 2 (SWA) (Body Media Inc., Pittsburgh, PA). The device is worn over the right triceps brachii muscle and incorporates five sensors: two-axis accelerometer (for movement patterns and step-count), galvanic skin response, skin temperature, near body temperature sensor and heat flux [21]. According to the study protocol, children were told to wear the SWA on 3 consecutive days for at least 20 h·day−1. This time frame was proposed by Trost et al. [22] for accelerometer studies and applied in other studies where SWA measurements were taken [23, 24]. Collected data was exported via the Professional InnerView Software 6.1 (Body Media Inc., Pittsburgh, PA). This software calculates the EE from the sensor parameters together with anthropometric data (gender, age, height, weight, BMI, handedness, smoking status). Physical activity intensity is classified by Metabolic Equivalents of Task (MET). METs are a practicable unit, defined by Jette et al. [25], which are commonly used to classify activities based on their EE. Studies have shown that the SWA is a valid tool for measuring EE and PA in children and adolescents [23, 24].
PA was categorized into 4 groups based on recommendations by Trost et al. [26]: light PA (LPA; 1.5–3.9 METs) includes standing, light walking, stretching, washing dishes; moderate PA (MPA; 4–5.9 METs) includes brisk walking, stair-climbing, water aerobics, biking on level ground; vigorous PA (VPA; > = 6 METs) encompasses mostly exercise activities like jogging or soccer. Time spent in activity below 1.5 METs minus time spent lying and sleeping, as recorded by the SWA, was considered sedentary behaviour.
Anthropometric measurement
Anthropometric measurements were conducted during the 11 year follow-up visit at all study sites. Standard operation procedures relied on the WHO’s Growth Reference Study [27]. Study personnel at each site were trained and the same weight scale (SECA™ 702) and stadiometer (SECA™ 242) were used to measure weight and height at each site. Body mass index (BMI) was calculated (weight [kg]·height [m]−2) and transformed into BMI z-scores, adjusted for gender and age according to the WHO growth standards [27]. Cut-off values for weight status were as follows: normal weight BMI z-score > = −2 SD and <= +1SD, overweight BMI z-score > +1 SD and obese BMI z-score > +2 SD [27, 28]. Children with a BMI z-score < −2 SD were excluded as underweight children were not the focus of this analysis and could bias results.
Covariates
Study country, season of measurement and gender of child were regarded as fixed covariates for adjustment in regression models. Additional data from parents was collected during the initial CHOP study visit (within 8 weeks after child’s birth) and were also considered: educational status and nationality of parents (one or both parents not from study country), age of mother at birth and BMI of mother before pregnancy.
Data analyses
Data is reported as mean (μ) ± standard deviation (SD) for continuous variables and as number (n) and percentage (%) for factors. PA parameters were skewed and reported as median (25th percentile; 75th percentile). Student’s t-test and one-way ANOVA were used for group differences in parametric variables and Kruskal-Wallis one-way ANOVA was used for skewed variables. Linear regression models including covariates (as mentioned above) with PA, MVPA and sedentary time as dependent variables were calculated for adjusted group differences. Compliance to PAGs is reported as number (n) and percentage (%) of children meeting recommendations. Additionally, odds ratios (OR) for adherence to PAGs (yes/no) were calculated with adjusted logistic regression models.
To define amount of PA needed to prevent excess weight in children, Receiver Operating Characteristic (ROC) curve analysis was used. ROC analysis can provide optimal cut-off values for time spent in specific levels of PA to differentiate between being overweight/obese and normal weight. Sensitivity (correctly identify an overweight or obese child) and specificity (correctly identify a normal weight child) for every possible cut-off was calculated and optimal thresholds were determined with the Youden-index as the maximum value of [J]:
Area under the curve (AUC) ranges from 0.5 (test variable predicts outcome only by chance) and 1.0 (perfect prediction) and reflects the quality of the test variable in predicting the outcome.
The effects of an increase (5, 15 and 60 min) in different intensity levels of PA on weight status (normal or overweight/obese children; based on BMI z-score) were calculated, using logistic regression models adjusted for covariates. All regression models were controlled for normal distributed residuals. P-values ≤0.05 were seen as significant.
After export from the SWA, PA data was processed using R 3.3.0 (The R Foundation for Statistical Computing). All statistical analysis was performed using ‘IBM SPSS Statistics for Windows’ version 23 (IBM Corp., Armonk, N.Y., USA).
Results
Complete data about activity, anthropometry and covariates was collected from 445 children. Twenty-six children had to be excluded due to less than 2 days of recording data, underweight or technical reasons. There were no differences (p > 0.05) in PA or anthropometric variables between children with 2 days of recording and children with 3 or more days. For analysis children with 2 or more days and anthropometric data were included (n = 419).
Study characteristics are shown in Table 1. A total of 134 (32.0%) of the children were classified as overweight/obese. BMI at 11 years of age was significantly different between countries (BMI z-scores; p = 0.009), ranging from Germany with lowest mean BMI (μ: 17.89 ± SD: 3.07; BMI-z: 0.08 ± 1.15) to Italy with highest mean BMI (19.44 ± 3.27; BMI-z: 1.18 ± 0.69); no gender differences were seen. However, girls (148.6 cm ± 7.2) were significantly taller by 1.5 cm (p = 0.026) than boys (147.1 cm ± 6.5).
Table 1.
Anthropometric data/country of participating 11 year olds and numbers of physical activity measurements per season
| μ (SD) | |
| Weight (kg) | 41.5 (9.4) |
| Height (cm) | 147.9 (6.9) |
| BMI | 18.8 (3.3) |
| BMI z-score | 0.5 (1.2) |
| n (%) | |
| N Total | 419 (100%) |
| Gender | |
| Male | 190 (45.3%) |
| Female | 229 (54.7%) |
| BMI | |
| Normal | 285 (68.0%) |
| Overweight/Obese | 134 (32.0%) |
| Country | |
| Germany | 62 (14.8%) |
| Belgium | 60 (14.3%) |
| Italy | 103 (24.6%) |
| Poland | 62 (14.8%) |
| Spain | 132 (31.5%) |
| Season | |
| Winter | 137 (32.7%) |
| Spring | 105 (25.1%) |
| Summer | 65 (15.5%) |
| Autumn | 112 (26.7%) |
Adherence to guidelines and differences in PA
Table 2 displays the distribution of time spent in different levels of PA and sedentary behaviour. Differences in amount of min·day−1 in PA based on weight status (p < 0.001), country (p = 0.034) and season (p = 0.005) were observed. Children with excess weight spent more time in sedentary behaviour, Median = 433 min·day−1 (25th percentile; 75th percentile: 362; 504) and less time in physical activity, 426 min·day−1 (355; 496) than normal weight children (sedentary: 374 min·day−1 (330; 446), p < 0.001; PA: 478 min·day−1 (408; 541), p < 0.001). Gender difference were visible, with boys spending more time at higher intensities (MPA: p < 0.001, VPA: p < 0.001 and MVPA: p < 0.001) and girls more time at lower intensities (LPA: p < 0.001). PAGs of 60 min·day−1 were met by 63.2% of the children. Boys had a higher compliance (80.0%) than girls (50.0%).
Table 3.
Cut-off points for min·day−1 in physical activitya/sedentary to differentiate between normal weight and overweight/obeseb children
| AUC (95%CI) | Youden index | Cut-off (min·day−1) | Sensitivity | Specificity | |
|---|---|---|---|---|---|
| Total | |||||
| Sedentary | 0.64 (0.58; 0.70) | .255 | 388 | 0.69 | 0.57 |
| LPA | 0.58 (0.52; 0.64) | .205 | 348 | 0.71 | 0.50 |
| MPA | 0.61 (0.55; 0.67) | .234 | 38 | 0.79 | 0.45 |
| VPA | 0.64 (0.58; 0.70) | .260 | 5 | 0.79 | 0.47 |
| MVPA | 0.62 (0.56; 0.68) | .230 | 46 | 0.78 | 0.45 |
| Male | |||||
| Sedentary | 0.63 (0.54; 0.72) | .249 | 382 | 0.77 | 0.48 |
| LPA | 0.60 (0.51; 0.68) | .286 | 344 | 0.64 | 0.65 |
| MPA | 0.63 (0.54; 0.72) | .239 | 69 | 0.62 | 0.62 |
| VPA | 0.67 (0.58; 0.75) | .290 | 20 | 0.55 | 0.74 |
| MVPA | 0.65 (0.56; 0.73) | .276 | 76 | 0.77 | 0.51 |
| Female | |||||
| Sedentary | 0.65 (0.57; 0.72) | .288 | 410 | 0.59 | 0.69 |
| LPA | 0.55 (0.47; 0.64) | .137 | 349 | 0.78 | 0.36 |
| MPA | 0.63 (0.55; 0.71) | .263 | 39 | 0.67 | 0.59 |
| VPA | 0.66 (0.58; 0.74) | .317 | 6 | 0.65 | 0.67 |
| MVPA | 0.64 (0.56; 0.72) | .271 | 46 | 0.66 | 0.61 |
P-values indicate AUC significantly > 0.50
aLPA: light physical activity (1.5–3.9 METs), MPA: moderate physical activity (MPA; 4–5.9 METs), VPA: vigorous physical (VPA; > = 6 METs)
MVPA: moderate to vigorous physical activity
bClassification through BMI z-scores, calculated according to WHO standards: normal weight > = − 2 SD and < = + 1SD, overweight/obese > +1 SD
Adjusted estimates of the linear regression model for time spent in PA revealed that overweight children spent 47 min·day−1 (95% CI: -69, −25; p < 0.001) less in PA than children of a normal weight; children in Italy (estimate: −36 min·day−1; 95% CI: -65, −8; p = 0.013) or Poland (estimate: −37 min·day−1, 95% CI: -69, −4; p = 0.028) spent less time daily in PA than children from Spain. Overall time in PA during winter was 39 min·day−1 (95%CI: -69, −9; p = 0.012) lower compared to summer. Analysis of results also showed that weight status and gender-based differences were observed for MVPA: girls spent 36 min·day−1 (95% CI: -46, −25; p < 0.001) less in MVPA than boys; overweight/obese 24 min·day−1 (95% CI: -36, −13; p < 0.001) less than normal weight children. Seasonal differences prevailed, with winter being associated with the lowest time spent on MVPA (estimate: −26 min·day−1; 95% CI: -42, −10; p = 0.001) compared to summer. No Interaction between season and country were seen.
Concerning adherence to PAGs, girls had 4.67 (95% CI: 2.87, 7.62; p < 0.001) times higher odds than boys to fall below current recommendations. Overweight and obese had more than twice the odds (OR 2.60; 95% CI: 1.55, 4.38; p < 0.001) than normal weight children.
Threshold determination
Results from the ROC analyses can be found in Table 3. The overall AUCs for PA variables and sedentary time were significantly (p < 0.05) greater than 0.5. With rising intensity levels of PA, the AUC increased and the threshold for min·day−1 in PA progressively decreased (from LPA cut-off: 348 min·day−1 to VPA cut-off: 5 min·day−1). For MVPA, the AUC was 0.62 (95%CI: 0.56, 0.68) and resulted in a threshold of 46 min·day−1. When stratifying for gender, girls’ thresholds were comparable with the overall sample results. Boys had higher cut-offs for minutes per day in MPA, VPA and MVPA needed differentiate the weight status.
Table 2.
Minutes·day−1 spent physically activea/ inactive and number (%) of children who adhered to activity recommendations
| n | Sedentary | PA | LPA | MPA | VPA | MVPA | Adherence PAGsb | |
|---|---|---|---|---|---|---|---|---|
| Total | 419 | 391 (333; 473) | 462 (389; 534) | 379 (318; 429) | 60 (35; 93) | 11 (4; 24) | 75 (41; 115) | 265 (63.2%) |
| Gender | ||||||||
| Male | 190 | 404 (338; 480) | 458 (371; 530) | 353 (297; 396) | 71 (54; 107) | 19 (9; 33) | 95 (65; 139) | 152 (80.0%) |
| Female | 229 | 383 (330; 458) | 473 (395; 539) | 399 (346; 447) | 47 (27; 74) | 8 (3; 15) | 59 (33; 92) | 113 (49.3%) |
| BMI | ||||||||
| Normal | 285 | 374 (330; 446) | 478 (408; 541) | 384 (333; 431) | 65 (41; 95) | 13 (6; 26) | 82 (51; 126) | 198 (69.5%) |
| Overweight/Obese | 134 | 433 (362; 504) | 426 (355; 496) | 352 (288; 422) | 47 (27; 74) | 7 (2; 17) | 60 (30; 102) | 67 (50.0%) |
| Country | ||||||||
| Germany | 62 | 394 (333; 484) | 452 (390; 536) | 367 (317; 417) | 65 (39; 92) | 16 (8; 26) | 79 (50; 115) | 44 (71.0%) |
| Belgium | 60 | 373 (299; 423) | 451 (401; 537) | 387 (329; 453) | 55 (32; 84) | 12 (4; 22) | 69 (40; 106) | 36 (60.0%) |
| Italy | 103 | 428 (350; 503) | 452 (367; 524) | 381 (319; 422) | 50 (27; 84) | 9 (2; 20) | 59 (28; 100) | 51 (49.5%) |
| Poland | 62 | 426 (383; 511) | 452 (362; 518) | 353 (288; 398) | 68 (38; 107) | 10 (5; 21) | 78 (48; 128) | 43 (69.4%) |
| Spain | 132 | 365 (323; 440) | 491 (411; 540) | 391 (337; 437) | 67 (40; 95) | 12 (5; 28) | 82 (47; 125) | 91 (68.9%) |
| Season | ||||||||
| Winter | 137 | 409 (350; 492) | 439 (364; 515) | 369 (307; 418) | 55 (31; 80) | 10 (3; 20) | 65 (36; 106) | 79 (57.7%) |
| Spring | 105 | 407 (337; 488) | 461 (391; 540) | 374 (326; 422) | 61 (30; 92) | 13 (4; 25) | 77 (37; 113) | 64 (61.0%) |
| Summer | 65 | 360 (311; 415) | 496 (419; 555) | 381 (321; 427) | 77 (39; 117) | 14 (6; 25) | 92 (51; 143) | 47 (72.3%) |
| Autumn | 112 | 389 (320; 452) | 480 (414; 540) | 386 (338; 445) | 68 (39; 94) | 12 (6; 26) | 80 (49; 126) | 75 (67.0%) |
Values are Median (25th percentile; 75th percentile) unless otherwise stated
Bold: significant group differences (p < 0.05)
a PA: physical activity, LPA: light physical activity (1.5–3.9 METs), MPA: moderate physical activity (MPA; 4–5.9 METs), VPA: vigorous physical (VPA; > = 6 METs), MVPA: moderate and vigorous physical activity
b Adherence to physical activity guidelines (PAGs): Number of children adhering to current physical activity guidelines of 60 min·day −1 in MVPA (percentage of group in column)
Associations of different levels of PA with BMI
Figure 1 shows the odds ratios of being overweight/obese with an increase of 5, 15 and 60 min·day−1 in different PA intensities. 60 min·day−1 of LPA (OR: 0.79; 95% CI: 0.66, 0.95; p < 0.001) had about the same effect as 15 min·day−1 of MPA (OR: 0.83; 95% CI: 0.75, 0.96; p < 0.001) or MVPA (OR: 0.86; 95% CI: 0.79, 0.92; p < 0.001) and just 5 min·day−1 of VPA (OR: 0.87; 95% CI: 0.80, 0.95; p = 0.001). An increase of MVPA (OR: 0.53; 95% CI: 0.39, 0.73; p < 0.001) by an hour had the same effect as an hour of MPA (OR: 0.47; 95% CI: 0.32, 0.70; p < 0.001) or a 15 min·day−1 increase of VPA (OR: 0.66; 95% CI: 0.52, 0.84; p = 0.001. Testing for interaction between gender and levels of PA showed no effects.
Fig. 1.
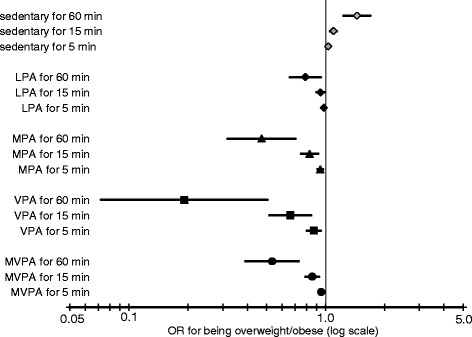
Odds Ratios (OR) and 95% confidence intervals of being overweight and/or obese for an increase in different intensities of physical activity, calculated with logistic regression models, adjusted for gender, country, season, education and nationality of parents, age and BMI of mother at birth. Note: ‘min’ stand for 5/15/60 min·day−1 increase in PA and sedentary time, with each line representing a separate model. LPA: light physical activity (1.5–3.9 METs), MPA: moderate physical activity (4–5.9 METs), VPA: vigorous physical (> = 6 METs), MVPA: moderate to vigorous physical activity
Analysis was repeated with children, who had at least 3 days of recording (n = 353), but showed no major differences. ROC analysis cut-offs remained similar, with two exceptions for the cut-off of boys’ sedentary time (471 min·day−1; difference: +89 min·day−1) and VPA time (5 min·day−1; difference: −15 min·day−1). Results of logistic regression models, examining the association between different duration and intensities of PA and sedentary time and weight status, were similar and remained significant.
Discussion
Results of this study suggest that PA is associated with BMI and current PAGs can be supported, as 60 min·day−1 of MVPA showed a meaningful risk reduction of excess weight gain. Approximately two thirds (63.2%) of the 11-year-old children in this study met WHO PAGs. Time spent in PA differed by gender (boys were more active than girls) and weight status (normal weight children were more active than overweight and obese children). Country differences were present, but showed no apparent regional patterns. An additional increase in time spent in higher intensity levels of PA seems to be beneficial for overweight prevention, as an additional 5 min·day−1 of VPA showed the same association with weight status, as an additional 15 min·day−1 of MPA. LPA was associated with a lower weight status, while sedentary behaviour was associated with excess weight.
Adherence to guidelines and differences in PA
Reported prevalence of children meeting the 60 min·day−1 of MVPA in previous studies ranges from 80% non-adherence [9] to 80% adherence [29]. These variations can be the result of a number of causes. As our and other studies have shown, is that PA and adherence to PAGs varies by country or region. For example, an observational study within the ENERGY-project examining PA of children from 5 different European countries, found rather large country differences [30]. One solution to tackle these differences could be the implementation of national or regional guidelines [5]. Recent review by Kahlmeier et al. [31] however, identified a lack of national PAGs in most European countries.
In addition to regional differences, the differences in adherence and volume of PA by gender [30, 32, 33] and weight status [24, 34] can been seen in several international studies. Despite growing evidence of these discrepancies, PAGs fail to take these differences into account, as causal mechanisms are not completely understood. One explanation could be the influence of friendship and peers on physical activity. This was seen in a qualitative study by Carlin et al. [35], with male peer groups encouraging each other to be active, while in girls’ and overweight/obese groups, participation in sports had mostly negative connotations. Carlin et al. [35] emphasized that interventions and guidelines need to be tailored not just to gender, but also to groups with low PA levels, like overweight or obese children.
Another reason for the wide range of reported prevalence of children meeting PAGs, could be the lack of common cut-offs for MVPA. Current PAGs were established in the last decade and are mostly based on self-reported estimates of PA. However, subjective measurement tends to overestimate PA when compared to accelerometry [36]. The technological development in the last 10 years has led to better opportunities to objectively quantify PA in larger populations. However, with new technologies it is important to validate tools independently and find a clear definition for cut-offs between intensity levels of PA. The cut-offs in this study where based on EE and categories proposed by Trost et al. [26], to make results comparable to other samples. However, amount and intensity of PA can be measured in many different ways: e.g. steps [37], which are easy to understand and used in everyday life, or more complex definitions through fuzzy logic [38]. To date there is no consensus on what defines light, moderate or vigorous PA. Thus, 60 min·day−1 of MVPA recommended by PAGs, can be broadly interpreted.
Threshold determination
ROC analyses thresholds in the overall sample were comparable to current PAGs. Other multinational studies examining cut-offs for objectively measured PA found similar results, though thresholds tend to be higher. The worldwide sample of the ISCOLE study identified an optimal threshold of 55 min·day−1, with a higher cut-off for boys (65 min·day−1) than girls (49 min·day−1) [39]. These gender differences were also visible in the European HELENA study, where ROC analysis was conducted in 2094 adolescents (threshold MVPA overall: 71 min·day−1; boys: 56 min·day−1; girls: 51 min·day−1) [40]. Recent results reported by Laguna et al. [41], analysing recommended levels of PA in 439 Spanish children aged 8–10 years from the European Youth Heart Study, found thresholds of 79 min·day−1 of MVPA and 50 min·day−1 in VPA. Different thresholds can be mostly traced back to different measurement devices and methods, as well as different populations. A problem of our and similar studies is, that AUCs of the ROC analysis were close to 0.5 and the impact and precision of the test can be debated. Nevertheless, with rising intensity levels of PA (from light to vigorous) AUCs and the quality of the results increase. Time spent in VPA together with time spend in sedentary behaviour seem to be the best parameters, discriminating between normal and excess weight. These results are supported by the effects seen in our logistic regression analysis (Fig. 1).
Associations of different levels of PA with BMI
International PAGs state that in addition to 60 min·day−1 of MVPA, children and adolescents should engage in VPA at least 3 days per week, but no recommended duration is given. The importance of higher levels of PA has been seen in other cross-sectional or interventional studies about PA and obesity. For instance, Ness et al. [42] suggested, based on a cross-sectional analysis of 5500 12-year-old children as part of the Avon Longitudinal Study of Parents and Children (ALSPAC), that higher intensity PA may be more important than total activity. Laguna et al. [41] supported this statement and emphasized the importance of VPA in preventing overweight and obesity. An interventional study by de Araujo et al. [43] showed that high intensity training can be a proficient method for improving health parameters in obese children. In our study an increase of just 15–20 min·day−1 of VPA was comparable to an increase of 60 min·day−1 of MVPA in reducing the risk of excess weight. This indicates that an appropriate amount for a VPA recommendation could be 15–20 min·day−1, this however needs confirmation from other studies.
Recommendations based on the effectiveness of a certain amount of MVPA or VPA should be treated with caution. They may lead to the conclusion that when children spend 60 min·day−1 in MVPA or 20 min·day−1 in VPA, it does not matter how much time they spent in sedentary time for the rest of the day. Chastin et al. [44] showed that there are complex effects to be considered when trying to replace one behaviour by another (e.g. sedentary time with LPA). Additionally, it is not always feasible to convince children with an inactive lifestyle, to do VPA right away; to start at lower levels PA might be more efficient. The majority of current PAGs agree with the recommendation of 60 min·day−1 of MVPA for children. However, it remains unclear how to spend the other 23 h of the day. The Canadian 24-Hour Movement Guidelines were the first to offer an holistic approach to recommendations for sleeping time, PA and sedentary behaviour [45]. PA can be spilt into two parts: LPA and MVPA. LPA is seen as baseline activity according to United States Department of Health and Human Services [46] and MVPA as health-enhancing PA on top of that baseline. Together with sedentary time, LPA is the main component of activity during waking hours, but showed minimal effects on BMI in our study. Despite minor effects on BMI, Pate and al. [6] emphasized the importance to differentiate between LPA and sedentary time. Studies in adults and children have shown that LPA can be a good basis to reduce the negative health effects of sedentary behaviour [15, 47]. Results of our study confirm that LPA reduces the risk of being overweight, while sedentary time is more likely to increase the risk. Future interventions and guidelines should aim to keep sedentary time to a minimum and whenever possible promote LPA. Light intensity activities, like walking to school or playing active videogames can be a more feasible replacement for sedentary time, than MVPA or VPA, as hypothesized by Healy et al. [47].
Strengths and limitations
One strength of this study is PA measurement using the SWA, since unlike common used accelerometers, it is possible to include weight bearing activities into measurement. Furthermore, the multicentre design with children from 5 European countries and the complete standardisation of the study protocols and measurement tools for every site, gives a broad overview of the PA situation in Europe.
Due to the cross-sectional design of the study, statements about the cause and effect relationships and direction of the association are not possible. Measurement with the SWA has both benefits and downfalls. As with most accelerometers, it cannot be worn in water and cannot effectively measure activities like cycling. The sensewear algorithms seem to improve in measuring children’s EE [48], yet they are prone to under- and overestimate EE in the aforementioned situations. It is possible that more active kids took part in this study and were more likely to accept wearing the SWA, as accelerometer measurement was not mandatory during the CHOP trial. Furthermore, it is unknown, if wearing a sensor changes the PA behaviour of participants and increase their motivation to be more active than usual. Finally, it is only possible to measure PA with accelerometers for a short time frame (few days to week), due to memory and energy limitations of the sensor. Measurements in this study were conducted through the whole year and analysis was adjusted for season, keeping influence of time of measurement to a minimum.
Conclusions
Results of this study have shown that two thirds of the children met current PAGs and recommendations of 60 min·day−1 of MVPA can help prevent excess body weight in children. Despite the fact that children appear to meet current PAGs, overweight and obesity are still on the rise and continue to be a major public health problem. One solution to this could be an additional recommendation of daily 15 min to 20 min in VPA, as this timeframe seem to provide meaningful risk reduction of overweight and obesity. Additional focus should be placed on reducing sedentary time and replacing it with light activity, like walking to school or activity programmes during recess. PA and its promotion can be valuable tools for controlling the body weight of children and subsequently improve their long-term health. Ongoing research in the field of PA is needed to react to changes in lifestyle and monitor activity levels during the early years.
Acknowledgments
We thank the participating families and all project partners for their enthusiastic support of the project.
The European Childhood Obesity Trial Study Group: Philippe Goyens, Clotilde Carlier, Joana Hoyos, Pascale Poncelet, Elena Dain (Université Libre de Bruxelles –Brusselles, Belgium); Françoise Martin, Annick Xhonneux, Jean-Paul Langhendries, Jean-Noel Van Hees † (CHC St Vincent –Liège-Rocourt, Belgium); Ricardo Closa-Monasterolo, Joaquin Escribano, Veronica Luque, Natalia Ferre, Marta Zaragoza-Jordana, Mariona Gispert-Llauradó, Carem Rubio-Torrents (Universitat Rovira i Virgili, IISPV, Taragona, Spain); Marcello Giovannini, Enrica Riva, Carlo Agostoni, Silvia Scaglioni, Elvira Verduci, Fiammetta Vecchi, Alice Re Dionigi (University of Milano, Milano, Italy); Jerzy Socha, Piotr Socha (Children’s Memorial Health Institute, Department of Gastroenterology, Hepatology and Immunology, Warsaw, Poland); Anna Dobrzańska, Dariusz Gruszfeld (Children’s Memorial Health Institute, Neonatal Intensive Care Unit, Warsaw, Poland); Anna Stolarczyk, Agnieszka Kowalik (Children’s Memorial Health Institute, Department of Pediatrics, Warsaw, Poland); Roman Janas, Ewa Pietraszek (Children’s Memorial Health Institute, Diagnostic Laboratory, Warsaw, Poland); Emmanuel Perrin (Danone Research Centre for Specialized Nutrition, Schiphol, The Netherlands); Rüdiger von Kries (Division of Pediatric Epidemiology, Institute of Social Pediatrics and Adolescent Medicine, Ludwig Maximilians University of Munich, Munich, Germany); Helfried Groebe, Anna Reith, Renate Hofmann (Klinikum Nurnberg Sued, Nurnberg, Germany); Berthold Koletzko, Veit Grote, Martina Weber, Peter Rzehak, Sonia Schiess, Jeannette Beyer, Michaela Fritsch, Uschi Handel, Ingrid Pawellek, Sabine Verwied-Jorky, Iris Hannibal, Hans Demmelmair, Gudrun Haile, Melissa Theurich, Phillipp Schwarzfischer (Division of Nutritional Medicine and Metabolism, Dr. von Hauner Childrens Hospital, University of Munich Medical Centre, Munich, Germany)
Funding
The studies reported herein have been carried out with partial financial support from the Commission of the European Community, specific RTD Programme "Quality of Life and Management of Living Resources", within the European Union’s Seventh Framework Programme (FP7/2007–2013), project EarlyNutrition under grant agreement no. 289346, the EU H2020 project PHC-2014-DynaHealth under grant no. 633595. This manuscript does not necessarily reflect the views of the Commission and in no way anticipates the future policy in this area. The funding body had no influence on the design of the study and collection, analysis, and interpretation of data and on writing this manuscript.
Availability of data and materials
The CHOP cohorts’ data are available only to the collaborating scientists from the respective CHOP participating centres. The data may be available upon request for some of the participating centres but not for all due to relevant data protection laws.
Authors’ contributions
PS: analysis of the data, drafted and finalized the manuscript; MW: participated in the data analysis and critical reading of manuscript; DG, PS, VL, JE, AX, EV, BM: conduct of study, data entry at study sites and critical reading of manuscript; BK: designed the research and critical reading of manuscript; VG: participated in the data analysis and critical reading of manuscript. All authors have read and approved the final version of this manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Belgium: Comitè d’Ethique Medicale de Centre Hospitalier Chretien Liege; No. OM87
Germany: Bayerische Landesärztekammer Ethik-Kommission, No. 02070
Italy: Azienda Ospedaliera San Paolo Comitato Etico, No 14/2002
Poland: Instytut Pomnik-Centrum Zdrowia Dziecka Komitet Etyczny, No 243/KE/2001
Spain: Comité ético de investigación clínica del Hospital Universitario de Tarragona Joan XXIII, Comité ético de investigación clínica del Hospital Universitario Sant Joan de Reus
Written informed consent has been obtained from all participants included in the analysed study and the study is being conducted in accordance with the declaration of Helsinki.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- ANOVA
Analysis of Variance
- AUC
Area under the Curve
- BMI
Body mass index
- CHOP
Childhood obesity project
- CI
Confidence Interval
- EE
Energy expenditure
- LPA
light physical activity
- MET
Metabolic Equivalents of Task
- min
minutes
- MPA
Moderate physical activity
- MVPA
Moderate to vigorous physical activity
- OR
Odds ratio
- PA
Physical activity
- PAGs
Physical activity guidelines
- SWA
Sensewear armband
- VPA
Vigorous physical activity
- WHO
World health organisation
Contributor Information
Phillipp Schwarzfischer, Email: Phillipp.Schwarzfischer@med.uni-muenchen.de.
Martina Weber, Email: Martina.Weber@med.uni-muenchen.de.
Dariusz Gruszfeld, Email: D.Gruszfeld@IPCZD.PL.
Piotr Socha, Email: p.socha@czd.pl.
Veronica Luque, Email: veronica.luque@urv.cat.
Joaquin Escribano, Email: joaquin.escribano@urv.cat.
Annick Xhonneux, Email: ANNICK.XHONNEUX@CHC.BE.
Elvira Verduci, Email: elvira.verduci@unimi.it.
Benedetta Mariani, Email: bma.mariani@gmail.com.
Berthold Koletzko, Email: office.koletzko@med.lmu.de.
Veit Grote, Phone: +49 (0)89 44005-2826, Email: veit.grote@med.uni-muenchen.de.
References
- 1.Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity--a systematic review of longitudinal studies. BMC Public Health. 2013;13:813. doi: 10.1186/1471-2458-13-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Regional Office for Europe. EUR/RC65/9: Physical activity strategy for the WHO European Region 2016–2025. http://www.euro.who.int/__data/assets/pdf_file/0010/282961/65wd09e_PhysicalActivityStrategy_150474.pdf?ua=1. Accessed 11 Aug 2016.
- 4.European Commission. EU Physical Activity Guidelines: Recommended Policy Actions in Support of Health-Enhancing Physical Activity. http://ec.europa.eu/sport/library/policy_documents/eu-physical-activity-guidelines-2008_en.pdf. Accessed 11 Aug 2016.
- 5.World Health Organization. Global recommendations on physical activity for health. http://www.who.int/dietphysicalactivity/publications/9789241599979/en/. Accessed 11 Aug 2016.
- 6.Pate RR, O'Neill JR, Lobelo F. The evolving definition of "sedentary". Exerc Sport Sci Rev. 2008;36(4):173–178. doi: 10.1097/JES.0b013e3181877d1a. [DOI] [PubMed] [Google Scholar]
- 7.Hinkley T, Salmon J, Okely AD, Crawford D, Hesketh K. Preschoolers' physical activity, screen time, and compliance with recommendations. Med Sci Sports Exerc. 2012;44(3):458–465. doi: 10.1249/MSS.0b013e318233763b. [DOI] [PubMed] [Google Scholar]
- 8.Biddle SJ, Bennie JA, Bauman AE, Chau JY, Dunstan D, Owen N, et al. Too much sitting and all-cause mortality: is there a causal link? BMC Public Health. 2016;16(1):635. doi: 10.1186/s12889-016-3307-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 10.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global burden of disease study 2013. Lancet. 2014;384(9945):766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guo SS, Chumlea WC. Tracking of body mass index in children in relation to overweight in adulthood. Am J Clin Nutr. 1999;70(1):145S–148S. doi: 10.1093/ajcn/70.1.145s. [DOI] [PubMed] [Google Scholar]
- 12.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa heart study. Pediatrics. 2001;108(3):712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 13.Sothern MS. Obesity prevention in children: physical activity and nutrition. Nutrition (Burbank, Los Angeles County, Calif). 2004; 20(7–8):704–708. doi:10.1016/j.nut.2004.04.007. [DOI] [PubMed]
- 14.Mitchell JA, Pate RR, Espana-Romero V, O'Neill JR, Dowda M, Nader PR. Moderate-to-vigorous physical activity is associated with decreases in body mass index from ages 9 to 15 years. Obesity (Silver Spring) 2013;21(3):E280–E293. doi: 10.1002/oby.20118. [DOI] [PubMed] [Google Scholar]
- 15.Kwon S, Janz KF, Burns TL, Levy SM. Association between light-intensity physical activity and adiposity in childhood. Pediatr Exerc Sci. 2011;23(2):218. doi: 10.1123/pes.23.2.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Treuth MS, Hou N, Young DR, Maynard LM. Accelerometry-measured activity or sedentary time and overweight in rural boys and girls. Obes Res. 2005;13(9):1606–1614. doi: 10.1038/oby.2005.197. [DOI] [PubMed] [Google Scholar]
- 17.Thompson AM, Campagna PD, Durant M, Murphy RJ, Rehman LA, Wadsworth LA. Are overweight students in grades 3, 7, and 11 less physically active than their healthy weight counterparts? Int J Pediatr Obes. 2009;4(1):28–35. doi: 10.1080/17477160802170050. [DOI] [PubMed] [Google Scholar]
- 18.Hughes AR, Henderson A, Ortiz-Rodriguez V, Artinou ML, Reilly JJ. Habitual physical activity and sedentary behaviour in a clinical sample of obese children. Int J Obes. 2006;30(10):1494–1500. doi: 10.1038/sj.ijo.0803334. [DOI] [PubMed] [Google Scholar]
- 19.Oja P, Bull FC, Fogelholm M, Martin BW. Physical activity recommendations for health: what should Europe do? BMC Public Health. 2010;10:10. doi: 10.1186/1471-2458-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koletzko B, von Kries R, Closa R, Escribano J, Scaglioni S, Giovannini M, et al. Lower protein in infant formula is associated with lower weight up to age 2 y: a randomized clinical trial. Am J Clin Nutr. 2009;89(6):1836–1845. doi: 10.3945/ajcn.2008.27091. [DOI] [PubMed] [Google Scholar]
- 21.Andre D, Pelletier R, Farringdon J, Safier S, Talbott W, Stone R, et al. The development of the SenseWear® armband, a revolutionary energy assessment device to assess physical activity and lifestyle. BodyMedia Inc. 2006;
- 22.Trost SG, Pate RR, Freedson PS, Sallis JF, Taylor WC. Using objective physical activity measures with youth: how many days of monitoring are needed? Med Sci Sports Exerc. 2000;32(2):426–431. doi: 10.1097/00005768-200002000-00025. [DOI] [PubMed] [Google Scholar]
- 23.Soric M, Starc G, Borer KT, Jurak G, Kovac M, Strel J, et al. Associations of objectively assessed sleep and physical activity in 11-year old children. Ann Hum Biol. 2015;42(1):31–37. doi: 10.3109/03014460.2014.928367. [DOI] [PubMed] [Google Scholar]
- 24.Soric M, Misigoj-Durakovic M. Physical activity levels and estimated energy expenditure in overweight and normal-weight 11-year-old children. Acta Paediatr. 2010;99(2):244–250. doi: 10.1111/j.1651-2227.2009.01553.x. [DOI] [PubMed] [Google Scholar]
- 25.Jette M, Sidney K, Blumchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol. 1990;13(8):555–565. doi: 10.1002/clc.4960130809. [DOI] [PubMed] [Google Scholar]
- 26.Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43(7):1360–1368. doi: 10.1249/MSS.0b013e318206476e. [DOI] [PubMed] [Google Scholar]
- 27.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Onis M. WHO child growth standards based on length/height, weight and age. Acta Paediatr. 2006;95(S450):76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 29.Pujadas Botey A, Bayrampour H, Carson V, Vinturache A, Tough S. Adherence to Canadian physical activity and sedentary behaviour guidelines among children 2 to 13 years of age. Prev Med Rep. 2016;3:14–20. doi: 10.1016/j.pmedr.2015.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Verloigne M, Van Lippevelde W, Maes L, Yıldırım M, Chinapaw M, Manios Y, et al. Levels of physical activity and sedentary time among 10-to 12-year-old boys and girls across 5 European countries using accelerometers: an observational study within the ENERGY-project. Int J Behav Nutr Phys Act. 2012;9(1):1. doi: 10.1186/1479-5868-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kahlmeier S, Wijnhoven TM, Alpiger P, Schweizer C, Breda J, Martin BW. National physical activity recommendations: systematic overview and analysis of the situation in European countries. BMC Public Health. 2015;15:133. doi: 10.1186/s12889-015-1412-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Belcher BR, Berrigan D, Dodd KW, Emken BA, Chou CP, Spruijt-Metz D. Physical activity in US youth: effect of race/ethnicity, age, gender, and weight status. Med Sci Sports Exerc. 2010;42(12):2211–2221. doi: 10.1249/MSS.0b013e3181e1fba9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Riddoch CJ, Bo Andersen L, Wedderkopp N, Harro M, Klasson-Heggebo L, Sardinha LB, et al. Physical activity levels and patterns of 9- and 15-yr-old European children. Med Sci Sports Exerc. 2004;36(1):86–92. doi: 10.1249/01.MSS.0000106174.43932.92. [DOI] [PubMed] [Google Scholar]
- 34.Kreuser F, Kromeyer-Hauschild K, Gollhofer A, Korsten-Reck U, Rottger K. "obese equals lazy?" analysis of the association between weight status and physical activity in children. J Obes. 2013;2013:437017. doi: 10.1155/2013/437017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carlin A, Murphy MH, Gallagher AM. Current influences and approaches to promote future physical activity in 11-13 year olds: a focus group study. BMC Public Health. 2015;15(1):1270. doi: 10.1186/s12889-015-2601-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adamo KB, Prince SA, Tricco AC, Connor-Gorber S, Tremblay M. A comparison of indirect versus direct measures for assessing physical activity in the pediatric population: a systematic review. Int J Pediatr Obes. 2009;4(1):2–27. doi: 10.1080/17477160802315010. [DOI] [PubMed] [Google Scholar]
- 37.Vale S, Trost SG, Duncan MJ, Mota J. Step based physical activity guidelines for preschool-aged children. Prev Med. 2015;70:78–82. doi: 10.1016/j.ypmed.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 38.Zitouni D, Guinhouya BC. Fuzzy logic for characterizing the moderate intensity of physical activity in children. J Sci Med Sport. 2016;19(2):142–148. doi: 10.1016/j.jsams.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 39.Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput JP, Fogelholm M, et al. Physical activity, sedentary time, and obesity in an international sample of children. Med Sci Sports Exerc. 2015;47(10):2062–2069. doi: 10.1249/MSS.0000000000000649. [DOI] [PubMed] [Google Scholar]
- 40.Martinez-Gomez D, Ruiz JR, Ortega FB, Veiga OL, Moliner-Urdiales D, Mauro B, et al. Recommended levels of physical activity to avoid an excess of body fat in European adolescents: the HELENA study. Am J Prev Med. 2010;39(3):203–211. doi: 10.1016/j.amepre.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 41.Laguna M, Ruiz JR, Lara MT, Aznar S. Recommended levels of physical activity to avoid adiposity in Spanish children. Pediatr Obes. 2013;8(1):62–69. doi: 10.1111/j.2047-6310.2012.00086.x. [DOI] [PubMed] [Google Scholar]
- 42.Ness AR, Leary SD, Mattocks C, Blair SN, Reilly JJ, Wells J, et al. Objectively measured physical activity and fat mass in a large cohort of children. PLoS Med. 2007;4(3) doi: 10.1371/journal.pmed.0040097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.De Araujo ACC, Roschel H, Picanço AR, do Prado DML, Villares SMF, de Sa pinto AL et al. Similar health benefits of endurance and high-intensity interval training in obese children. PloS one. 2012; 7(8):e42747. [DOI] [PMC free article] [PubMed]
- 44.Chastin SF, Palarea-Albaladejo J, Dontje ML, Skelton DA. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-Metabolic health markers: a novel compositional data analysis approach. PLoS One. 2015;10(10) doi: 10.1371/journal.pone.0139984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tremblay MS, Carson V, Chaput JP. Introduction to the Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. 2016; 41(6 Suppl 3):iii-iv. doi:10.1139/apnm-2016-0203. [DOI] [PubMed]
- 46.United States . Department of Health and Human Services.: 2008 physical activity guidelines for Americans : be active, healthy, and happy! Washington. U.S. Dept. of Health and Human Services: DC; 2008. [Google Scholar]
- 47.Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, et al. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007;30(6):1384–1389. doi: 10.2337/dc07-0114. [DOI] [PubMed] [Google Scholar]
- 48.Calabro MA, Welk GJ, Eisenmann JC. Validation of the SenseWear pro armband algorithms in children. Med Sci Sports Exerc. 2009;41(9):1714–1720. doi: 10.1249/MSS.0b013e3181a071cf. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The CHOP cohorts’ data are available only to the collaborating scientists from the respective CHOP participating centres. The data may be available upon request for some of the participating centres but not for all due to relevant data protection laws.


