SUMMARY
Extracorporeal membrane oxygenation (ECMO) is a lifesaving procedure used in neonates, children, and adults with severe, reversible, cardiopulmonary failure. On the basis of single-center studies, the incidence of AKI occurs in 70%–85% of ECMO patients. Those with AKI and those who require renal replacement therapy (RRT) are at high risk for mortality, independent of potentially confounding variables. Fluid overload is common in ECMO patients, and is one of the main indications for RRT. RRT to maintain fluid balance and metabolic control is common in some but not all centers. RRT on ECMO can be performed via an in-line hemofilter or by incorporating a standard continuous renal replacement machine into the ECMO circuit. Both of these methods require specific technical considerations to provide safe and effective RRT. This review summarizes available epidemiologic data and how they apply to our understanding of AKI pathophysiology during ECMO, identifies indications for RRT while on ECMO, reviews technical elements for RRT application in the setting of ECMO, and finally identifies specific research-focused questions that need to be addressed to improve outcomes in this at-risk population.
Introduction
Extracorporeal membrane oxygenation (ECMO) is a lifesaving procedure used in neonates, children, and adults with severe, reversible, cardiopulmonary failure. These patients are at high risk of developing AKI and fluid overload (FO). Renal replacement therapy (RRT) is commonly used to maintain fluid balance and metabolic control; however, the optimal timing, methodology, and prescriptions to support ECMO patients with renal dysfunction have not been extensively studied. This review summarizes AKI pathophysiology in ECMO patients, appraises epidemiology data, discusses indications for RRT, explains technical aspects of concomitant RRT and ECMO, and proposes future research to improve outcomes in this vulnerable population.
Epidemiology of AKI and RRT Use in ECMO
Until recently, one of the main problems with AKI epidemiology studies was the lack of consensus definitions. The RIFLE (1,2) (risk, injury, failure, loss, and end stage) and Acute Kidney Injury Network (3) classification definitions have stratified patients by AKI severity using absolute or percentage changes in serum creatinine. Single-center studies using the RIFLE definition in ECMO patients show the incidence of AKI as follows: 71% of neonates with congenital diaphragmatic hernia (4), 71% of children with a cardiac indication for ECMO (5), 78% of adults with respiratory failure (6), and 81% of adults post-cardiotomy (7). The incidence of AKI using contemporary categorical definitions in other neonatal and pediatric patients on ECMO has not been conducted, but a multicenter retrospective analysis is underway (8).
These single-center studies also suggest an association between AKI and poor outcomes. Adults with AKI had a 78% mortality compared with 20% in non-AKI patients (6). Congenital diaphragmatic hernia infants on ECMO who developed severe AKI were more likely to die, had increased time on mechanical ventilation, and increased ECMO duration than those without AKI (4). These small, single-center studies show the strong association between AKI and mortality. However, sample size limits the ability to determine if AKI is an independent risk factor for mortality in these studies.
In a single-center study of 121 children and adults, those with AKI (serum creatinine .1.5 mg/dl or dialysis) had higher independent odds of death after controlling for confounders, with an adult odds ratio of 12.1 (95% confidence interval, 2.5–59) and a pediatric odds ratio of 24.0 (95% confidence interval, 4.2–137)] (9). Although there seems to be a significant association between AKI and mortality in these groups, the small sample size provides for an imprecise estimate of the true odds of mortality in those with AKI. Larger cohorts are needed to better understand the true effect size.
Recent evaluation of the Extracorporeal Life Support Organization (ELSO) registry sheds light on the independent association between renal dysfunction and mortality. The ELSO registry captures data from 170 centers around the world and is divided into cardiac and non-cardiac indications. To determine the effect of AKI and RRT on mortality, Askenazi et al. (10) evaluated 7941 non-cardiac neonates (aged 30 days, at initiation) and 1962 non-cardiac children (aged 19 years) from the ELSO registry between 1998 and 2008. For this analysis, AKI was defined as an International Classification of Diseases (Ninth Revision) code for ARF or serum creatinine $1.5 mg/dl, and RRT was determined by Current Procedural Terminology codes. The incidence of AKI and/or RRT in neonates and children was 25% and 46%; respectively. Patients with AKI and those who received RRT had higher mortality than similar patients without AKI or RRT independent of potential confounders (demographics, ECMO characteristics, comorbidities, and physiologic parameters). Despite the po-tential limitations inherent to registry studies and the imprecise methods to define AKI in this population, these data suggest that therapies to prevent/ameliorate AKI and optimization of RRT could improve outcomes.
Pathophysiology of AKI in ECMO
Before patients are placed on ECMO, aggressive life-sustaining interventions have been implemented, yet the patient continues to have severe cardiopulmonary insufficiency. Indications for ECMO include reversible patient conditions with a high predicted mortality rate $80%. Before ECMO initiation, these critically ill patients are at high risk of AKI due to their condition (sepsis, ischemia, respiratory failure, cardiac failure, vasopressor requirements) and prevalent use of nephrotoxic medications.
In veno-arterial ECMO, cardiac output is a mixture of native cardiac (pulsatile) and ECMO pump flow (non-pulsatile). Although mechanical flow may be non-pulsatile, institution of venoarterial ECMO usually increases BP and flow to the vital organs including the kidneys. Veno-venous ECMO maintains native pulsatile cardiac output, and changes in renal perfusion are less than in veno-arterial ECMO. During initiation of ECMO, patient oxygenation improves, oxygen consumption is reduced, and hemodynamics improve in most patients. However, ECMO initiation with subsequent adjustments in vasopressors/ionotropes can cause rapid hemodynamic fluctuations that alter renal blood flow leading to ischemia/reperfusion-associated AKI (11).
Other factors associated with ECMO initiation predispose patients to incident or exacerbation of AKI. Blood exposure to artificial surfaces causes systemic inflammation (12, 13), a hypercoagulable state (11,14,15), and hemolysis/hemoglobinuria, which may be exacerbated by air/fluid interface and the generation of excessive negative pressure (16–20).
Indications for RRT on ECMO
As for other critically ill patients, classic RRT indications in patients on ECMO include uremia, acidosis, electrolyte abnormalities, and FO. Center-specific staff availability, local expertise, and experience with RRT on ECMO currently drive decisions to initiate RRT. We conducted a survey of participating ELSO centers that revealed tremendous inter-center variation for initiating RRT. The most common reported RRT indications were FO (43%), FO prevention (16%), AKI (35%), and electrolyte disturbances (4%) (21). These data suggest that treatment/prevention of fluid accumulation plays a major role in decision making for RRT initiation.
Cumulative FO should be calculated and assessed daily in ECMO patients to determine if RRT could benefit the overall care. The following simple formula to measure cumulative FO has been evaluated in multiple studies: [Cumulative Fluid Intake since Intensive Care Unit (ICU) Admission (in liters) – Cumulative Fluid Output since ICU Admission (in liters)/ICU Admission Weight (in kilograms)] 3 100 (22–27). Using changes in daily weight to express fluid balance provides a similar estimate of FO (28).
Cumulative FO is independently associated with mortality, worse oxygenation, longer length of stay, and mechanical ventilation in critically ill patients receiving continuous RRT, as well as in those who do not receive RRT (25,29–35) (Table 1). Early studies investigating the development of FO using radio-labeled isotopes showed an elevation in both the total body water and extracellular fluid space in ECMO patients (36). Cumulative FO and failure to return to dry weight are associated with higher mortality (28,37) and prolonged ECMO duration (38). Moreover, improvement in FO or improving fluid balance is associated with improved lung function and time to weaning of ECMO (36,39). Neonates and children who receive concomitant RRT on ECMO compared with ECMO alone have decreased cumulative FO (37,40,41). On the basis of these studies, the international ELSO guidelines recommend to “return the extracellular fluid volume to normal (dry weight) and maintain it there” (42). These studies suggest that early RRT to prevent FO may improve out-comes and warrants further investigation.
TABLE 1.
Representative studies demonstrating negative effect of fluid overload in patients receiving ECMO, CRRT, and those who receive both ECMO and CRRT
| STUDY | N | Study Population details | Study Design | Method of FO Measurements | Main Outcomes | Main Findings |
|---|---|---|---|---|---|---|
| Heung et al., 2011 (35) | 170 | AKI attributed to ATN requiring RST, aged $18 yr, hospitalized | Retrospective, single center | FO% from baseline to RST initiationa | Renal recovery at 1 yr | Higher degree of fluid overload at RST initiation predicts worse renal recovery at 1 yr |
| Selewski et al., 2011 (28) | 113, 50 patients on ECMO | CRRT, 2006–2010, PICU, NICU, cardiac ICU | Retrospective, single center | FO% from ICU admission to CRRT initiationb,c | ICU mortality | Provides evidence for a weight-based definition of FO Higher FO% associated with increased mortality, independent of illness severity score and other clinical factors in patients on ECMO and general pediatric critical care |
| Sutherland et al., 2010 (25) | 297 | CRRT (all modalities), aged, 18 yr, all ICUs 2001–2005 | Retrospective, using prospectively collected multicenter registry data | FO% from ICU admission to CRRT initiationc | PICU mortality | HiHigher FO% (continuous) and FO% .20% associated with increased mortality, independent of illness severity and other clinical factors |
| Elbahlawan et al., 2010 (57) | 30 | CRRT with acute lung injury and ventilation in hematopoietic stem cell transplant, aged #19 yr, ICU, 1994–2006 | Retrospective, single center | FO% at 24 h before and 48 h after CRRT initiationc | PaO2/FiO2 ratio, ICU mortality | Both FO and PaO2/FiO2 ratio (oxygenation) improved from 24 h before to 48 h after CRRT initiation PaO2/FiO2 ratio and %FO were inversely associated |
| Fulop et al., 2010 (31) | 81 | CRRT (all modalities) with nephrology consultation, aged $18 yr, medical, cardiac, surgical ICUs, 2003–2004 | Retrospective, using prospectively collected single-center registry data | %Volume-related weight gain from baseline to RST initiationd | 30-d mortality | .10% weight gain associated with mortality, independent of other clinical factors |
| Hayes et al., 2009 (30) | 76 | CRRT (all modalities), aged, 18.9 yr, 2000–2005, PICU | Retrospective, single center | FO% from ICU admission to CRRT initiationc | Hospital mortality | FO% .20% associated with increased mortality, independent of illness severity and other clinical factors. FO% .20% also independently associated with prolonged hospitalization, duration of mechanical ventilation, and time to renal recovery |
| Bouchard et al., 2009 (58) | 353 | AKI/RST with nephrology consultation, aged $ 18 yr, ICU, 1999–2001e | Retrospective analysis of a prospective multicenter cohort study | FO% at AKI diagnosis, RST initiation, and RST cessationf | 30-d and hospital mortality | FO% at RST initiation was associated with mortality after adjustment for illness severity score RST patients with greater days of FO% .10% had increased mortality FO at RST cessation was associated with mortality, adjusted for illness severity score |
| Blijdorp et al., 2009 (38) | 61 | Pre-emptive CVVH during ECMO, aged, 28 d, NICU | Retrospective case-comparison study | Average daily fluid balance while on ECMO | Time on ECMO, time from decannulation to extubation | Adding CVVH pre-emptively improves outcomes by decreasing time on ECMO because of improved fluid management |
| Hoover et al., 2008 (40) | 52 | All patients receiving ECMO, aged 1 mo-18 yr, PICU, 1992–2006 | Retrospective case-matched study (patients receiving CVVH plus ECMO versus ECMO alone) | Fluid balance while on ECMOg | ECMO survival, fluid balance, caloric intake | Use of CVVH with ECMO wasassociated with improved fluid balance, improved caloric intake and decreased diuretic exposure |
| Gillespie et al., 2004 (27) | 88 | CVVH for AKI or volume overload, aged #20 yr, 1993–2002 | Retrospective, single center | FO% from ICU admission to CVVH initiationc | Mortality, from last known survival status | FO% .10% was associated with increased mortality independent of illness severity and other clinical factors |
| Foland et al., 2004 (59) | 113 | CVVH, aged, 18 yr, 1997–2003, PICU, NICU, cardiac ICU | Retrospective, single-center registry | FO% from up to 7 days before CVVH initiationh | PICU mortality | Higher FO% associated with increased mortality, independent of illness severity score and other clinical factors |
| Goldstein et al., 2001 (22) | 21 | CWH or CVVHD, aged #18 yr, PICU, 1996–1998 | Retrospective, single center | FO% from ICU admission to CVVH initiationc | PICU mortality | FO% at CVVH or CVVHD initiation was associated with increased mortality, independent of illness severity score |
ECMO, extracorporeal membrane oxygenation; CRRT, continuous renal replacement therapy; FO, fluid overload; ATN, acute tubular necrosis; RST, renal supportive therapy; PICU, pediatric intensive care unit; NICU, neonatal intensive care unit; ICU, intensive care unit; CVVH, continuous venovenous hemofiltration; CVVHD; continuous venovenous hemodialysis.
[(Weight at RST Initiation – Baseline Weight)/Baseline Weight] 3 100%, with baseline weight based on prehospitalization data or hospital admission weight.
[(Weight at CRRT Initiation – ICU Admission Weight)/ICU Admission Weight] 3 100.
[(Total Fluid Intake – Total Fluid Output in liters, from ICU admission to CRRT)/ICU Admission Weight in kilograms] 3 100.
[(Weight at CRRT Initiation – First Available Hospital Weight)/Initial Weight) 3 100.
This study included adults who did and did not receive renal supportive therapy in the ICU. We report only on those who received RST.
[(Total Fluid Intake – Total Fluid Output in liters, from 3 d before nephrology consultation to RST or other relevant time point)/Hospital Admission Weight in kilograms) 3 100.
[(Total Fluid Intake – Total Fluid Output in liters, from ICU during ECMO)/Weight in kilograms per day on ECMO].
[(Total Fluid Intake – Total Fluid Output in liters, from 7 days before CVVH)/estimated dry weight in kilograms] 3 100.
The overall treatment goals, and whether RRT would help to achieve these goals, should factor into the decision to initiate RRT. Initiation of RRT may allow for the administration of adequate nutrition, medications, and blood products, while avoiding further fluid accumulation. Likewise, if high diuretic doses are being used to maintain urine output, the risk of long-term ototoxicity and lack of data that diuretics improve outcomes in critically ill patients (43,44) should be balanced with the potential benefits of managing fluids with RRT.
Finally, when deciding to initiate RRT and evaluating overall patient prognosis, one should be aware that the likelihood of long-term ESRD in ECMO survivors requiring RRT is extremely low. Two large ECMO center studies have independently reported their experience with concomitant RRT and ECMO over a combined 20-year period and showed no incidence of ESRD in the absence of primary renal disease (45,46).
Technical Aspects of RRT While on ECMO
In unstable patients with multiple organ failure, ECMO can improve hemodynamic stability by increasing cardiac output via an ECMO pump (in veno-arterial ECMO) or by increasing native cardiac output by improved myocardial oxygenation (47). The extracorporeal circuit can serve as a platform for additional organ support therapies, including RRT. Currently, the US Food and Drug Administration has not approved any RRT device for use in conjunction with ECMO and such use is off label. Several RRT techniques are available to support ECMO patients with AKI and/or FO. Because there are no comparison studies of these techniques, practice is based on expert opinion and local experience. We therefore do not recommend a particular method to provide RRT.
RRT options during ECMO include peritoneal dialysis, intermittent hemodialysis, and continuous RRT (CRRT). Each has its own advantages and disadvantages (48–50). Patient factors, treatment goals, and center experience play a role in the RRT selected. RRT on ECMO is usually provided as a continuous modality because of hemodynamic instability. Continuous peritoneal dialysis may achieve the desired fluid management goals but provide less efficient management of electrolyte imbalance and clearance. CRRT is the most common modality because it offers the ability of making rapid changes to targeted fluid balance and provides excellent solute clearance.
The two most common methods to provide CRRT are via the use of an in-line hemofilter or via a traditional CRRT device connected to the extracorporeal circuit. A recent international survey of 65 ECMO centers showed that 50.8% of centers exclusively use CRRT, 21.5% exclusively use an in-line hemofilter, and 23% use no RRT during ECMO (21).
RRT Using an In-Line Hemofilter
One method to provide CRRT is by incorporating an inline hemofilter into the ECMO circuit. The hemofilter is typically placed after the pump (to provide forward blood flow through the hemofilter) and before the oxygenator (to maintain the oxygenator’s use as a clot and air trap in case of complications) (Figure 1). After passing through the hemofilter, the blood is returned to the prepump limb of the circuit. In this configuration, the shunt creates a disparity between the pump measured flow and the flow being delivered to the patient. An ultrasonic flow probe on the arterial return line is needed to determine the actual flow delivered to the patient. The hemofilter blood flow rate can be derived by subtracting the flow delivered to the patient from the total ECMO blood flow rate. The hemofilter blood flow rate can be adjusted via the use of a stopcock or other flow-restricting device; however, the potential for hemolysis and thrombus formation due to turbulent flow limit this practice.
Figure 1.
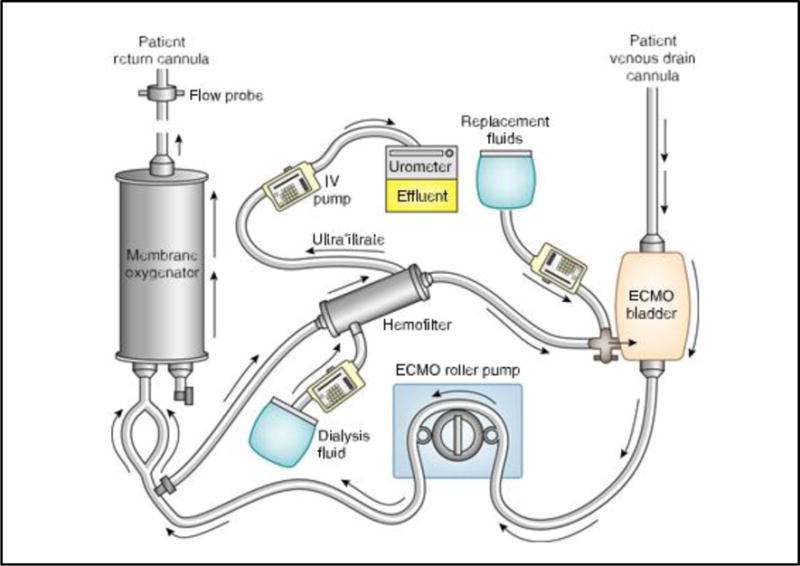
Renal replacement therapy using an in-line hemofilter during extracorporeal membrane oxygenation (ECMO). As blood comes from the patient via the venous drain cannula, it goes through the ECMO bladder to the ECMO pump, to the membrane oxygenator, and back to the patient via a return cannula. Blood is shunted from the circuit to the in-line hemofilter and returned to the ECMO pump. Fluid (ultrafiltrate) can be controlled using an intravenous (IV) pump. Replacement or dialysis fluid can be used for solute clearance and/or to achieve metabolic control.
Some centers use this technique to provide only slow continuous ultrafiltration. Other centers provide continuous convective clearance with replacement fluids delivered to the patient directly or through the ECMO circuit. Diffusive clearance can be achieved running countercurrent fluid using standard infusion pumps. Because these hemofilters are designed for use with high pressure systems, the fiber characteristics make diffusive clearance less effective than conventional membranes. In addition, the amount of ultra-filtration made is limited by the infusion pumps that maximize at approximately 1 L/h.
The hemofilter has the potential to generate large amounts of ultrafiltrate that can be regulated using a standard intravenous infusion device connected to the effluent port of the hemofilter. There are several methods to determine the amount of fluid being removed. The most precise method is to measure the actual volume of ultrafiltration removed using weight or a volumetric measuring device (such as a collection kit used when documenting urine output with a Foley catheter). The other method is to assume that the ultrafiltrate removed is equal to the rate programmed into the infusion device. This assumption may be inaccurate as these infusion devices (commonly referred to as “pumps”) are not really pumps but are flow restrictors. Individual infusion devices (tested under low pressures) report volume delivery accuracy of 62%–10%. Studies show higher inaccuracies when these devices infuse medication via central venous catheters in patients with elevated central venous pressure (51,52). The little data available on the accuracy of these intravenous devices to regulate ultrafiltration in an ECMO circuit suggest error rates as high as 12.5% (53). In laboratory experiments using pressure settings typical of ECMO, the differences between the prescribed and the actual ultrafiltration rate were as high as 34 ml/h (.800 ml/d) (54). Therefore, when using in-line hemofilters, it is imperative to precisely measure or closely monitor ultrafiltration volumes.
RRT Using a CRRT Machine
Alternatively, a commercially available CRRT machine can be connected in-line to the ECMO circuit (Figure 2). The CRRT machine is typically connected to the venous limb of the roller-head ECMO circuit before the pump. The blood is then returned from the CRRT machine to the ECMO circuit near the venous CRRT connection and before the ECMO pump (40,55). If a centrifugal ECMO pump is used, the CRRT machine should not be placed before the ECMO pump because there is a very risk of air entrainment. Instead, the CRRT machine should be placed after the pump.
Figure 2.
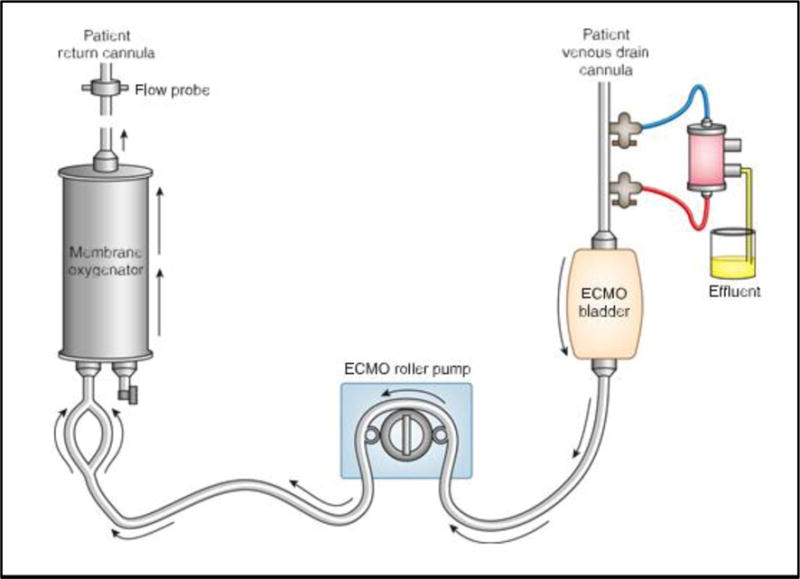
Renal replacement therapy (RRT) using RRT machine during extracorporeal membrane oxygenation (ECMO). If the ECMO circuit uses a roller pump, a proportion of the circuit blood comes from the patient via the venous drain cannula and enters the RRT machine where replacement, dialysis, and ultrafiltration occurs. Blood from the RRT machine then goes back to the ECMO bladder to the ECMO pump, the membrane oxygenator, and back to the patient via a return cannula. If a centrifugal pump is used, the RRT machine must be connected after the ECMO bladder to prevent air entrapment.
Dialysis or replacement fluid (prefilter or postfilter) is used to efficiently clear solutes, and ultrafiltrate can be generated to remove the desired fluid.
Additional anticoagulation is not routinely used for the CRRT circuit, because heparinization of the ECMO circuit anticoagulates the entire circuit. Unusual situations in which bleeding on ECMO is excessive, activated clotting time goals are very low, or heparin has been temporarily discontinued require consideration of regional citrate anti-coagulation of the CRRT circuit. Use of the heater on the CRRT device is typically not needed, but may be used.
The access pressure alarms inherent to commercially available CRRT have set limits based on the individual CRRT device. The default access pressure alarms are typically negative. However, when these machines are operated in series with ECMO, the positive pressure at the entry point of the CRRT machine will create pressures close to zero or positive. These pressures can lie outside the default pressures of the machine and thus the alarm settings may have to changed when using RRT on ECMO. Some machines (including the Gambro Prismaflex and the Braun Diapact) give the clinician the ability to adjust alarm settings. Other machines (including the NxStage System One, the Fresenius 2008K, and the older Gambro Prisma) do not have these capabilities. If the machines are not able to change the default access pressure, flow restrictors placed on the outside of the tubing have been used to keep the pressures within the pressure alarm limits. These clamps are not recommended because they portend added risk of hemolysis and thrombosis.
There are advantages and disadvantages to using an inline hemofilter or a CRRT machine for RRT. In both of these techniques, the use of commercially prepared renal replacement fluid and limiting the use of ultrafiltration without replacement or dialysis fluids can reduce development of electrolyte abnormalities. With either type of circuit, return blood from the renal replacement machine should be connected before the oxygenator so that any air or clot will be trapped into the oxygenator and not sent to the patient. Careful attention to detail and development of protocols for RRT are critical to providing the best care and outcomes.
Future Research Needs
As outlined above, ECMO patients have a high incidence of AKI and RRT provision with associated poor outcomes. There is great opportunity to answer numerous questions to better understand the epidemiology of AKI. We must better understand how fluid provision and timing of RRT can affect patient outcomes. Evaluation of new AKI biomarkers and the application of a “renal angina” concept (56) to determine how a combination of clinical risk factors in conjunction with laboratory evidence may better identify those with AKI are greatly needed. A better understanding of the pathophysiology of AKI as related to ECMO initiation is needed to design preventative studies. Prospective evaluations of different techniques of RRT could help develop specific protocols describing optimal circuit integration parameters. A novel RRT device made specifically to interact with the ECMO circuit in a safe, accurate, effective, and simple manner could greatly improve RRT in these complex patients. The prescription of RRT (i.e., what fluids, what dose, and what method [dialysis versus replacement]) needs to be systematically explored. Answers to these and other important questions are likely to lead to improved outcomes in this vulnerable population.
The Kidney Interventions During Extracorporeal Membrane Oxygenation (KIDMO) group is an international, multidisciplinary collaboration composed of pediatric intensivists, cardiologists, ECMO experts, and nephrologists. Thus far, this group has coordinated a survey to better understand current clinical RRT practices and have altered the ELSO registry data collection forms to better document AKI and RRT. Starting in 2012, the ELSO registry is collecting more detailed serum creatinine and fluid intake/output data before, during, and after ECMO. This will allow for better data to understand the true incidence of AKI/FO and its effect on outcomes. In addition, a multicenter retrospective analysis of neonates and children on ECMO is underway to explore how AKI and FO affect clinical outcomes. Ultimately, prospective multicenter evaluations and intervention trials will be needed to prevent AKI, ameliorate the effects of AKI, and optimize RRT in ECMO patients.
AKI, FO, and RRT are common and are associated with poor outcomes in critically ill patients on ECMO. Cumulative FO should be used to help make decisions about RRT initiation. RRT on ECMO can be safely performed, but issues unique to ECMO must be carefully addressed. Centers providing ECMO should have a multidisciplinary team (involving nurses, ECMO specialists, nephrologists, surgeons, and intensivists) to devise center-specific protocols for RRT on ECMO.
Acknowledgments
We thank all of the nurses, perfusionists, and ECMO specialists at our institutions who provide an infrastructure and excellent care for these very vulnerable patients. G.M.F. received funding from the ELSO registry to study RRT use in ECMO patients.
Footnotes
Disclosures
D.J.A. is a consultant and is on the speaker’s bureau for Gambro. M.L.P. has several patents pending on a pediatric CRRT device that can be used with ECMO.
References
- 1.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup Acute renal failure-definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–R212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007;71:1028–1035. doi: 10.1038/sj.ki.5002231. [DOI] [PubMed] [Google Scholar]
- 3.Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A, Acute Kidney Injury Network Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gadepalli SK, Selewski DT, Drongowski RA, Mychaliska GB. Acute kidney injury in congenital diaphragmatic hernia requiring extracorporeal life support: An insidious problem. J Pediatr Surg. 2011;46:630–635. doi: 10.1016/j.jpedsurg.2010.11.031. [DOI] [PubMed] [Google Scholar]
- 5.Smith AH, Hardison DC, Worden CR, Fleming GM, Taylor MB. Acute renal failure during extracorporeal support in the pediatric cardiac patient. ASAIO J. 2009;55:412–416. doi: 10.1097/MAT.0b013e31819ca3d0. [DOI] [PubMed] [Google Scholar]
- 6.Lin CY, Chen YC, Tsai FC, Tian YC, Jenq CC, Fang JT, Yang CW. RIFLE classification is predictive of short-term prognosis in critically ill patients with acute renal failure supported by extracorporeal membrane oxygenation. Nephrol Dial Transplant. 2006;21:2867–2873. doi: 10.1093/ndt/gfl326. [DOI] [PubMed] [Google Scholar]
- 7.Yan X, Jia S, Meng X, Dong P, Jia M, Wan J, Hou X. Acute kidney injury in adult postcardiotomy patients with extracorporeal membrane oxygenation: Evaluation of the RIFLE classification and the Acute Kidney Injury Network criteria. Eur J Cardiothorac Surg. 2010;37:334–338. doi: 10.1016/j.ejcts.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Selewski DT, Bridges BC, Cooper D, Paden ML, Zappitelli M, Fleming GM. Formation of the Kidney Intervention during Extracorporeal Membrane Oxygenation (KIDMO) pediatric study group [Abstract]; Presented at the 17th International Conference on Continuous Renal Replacement Therapies; San Diego, CA. February 14–17, 2012. [Google Scholar]
- 9.Hei F, Lou S, Li J, Yu K, Liu J, Feng Z, Zhao J, Hu S, Xu J, Chang Q, Liu Y, Wang X, Liu P, Long C. Five-year results of 121 consecutive patients treated with extracorporeal membrane oxygenation at Fu Wai Hospital. Artif Organs. 2011;35:572–578. doi: 10.1111/j.1525-1594.2010.01151.x. [DOI] [PubMed] [Google Scholar]
- 10.Askenazi DJ, Ambalavanan N, Hamilton K, Cutter G, Laney D, Kaslow R, Georgeson K, Barnhart DC, Dimmitt RA. Acute kidney injury and renal replacement therapy independently predict mortality in neonatal and pediatric noncardiac patients on extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2011;12:e1–e6. doi: 10.1097/PCC.0b013e3181d8e348. [DOI] [PubMed] [Google Scholar]
- 11.Keckler SJ, Laituri CA, Ostlie DJ, St Peter SD. A review of venovenous and venoarterial extracorporeal membrane oxygenation in neonates and children. Eur J Pediatr Surg. 2010;20:1–4. doi: 10.1055/s-0029-1231053. [DOI] [PubMed] [Google Scholar]
- 12.Mildner RJ, Taub N, Vyas JR, Killer HM, Firmin RK, Field DJ, Kotecha S. Cytokine imbalance in infants receiving extracorporeal membrane oxygenation for respiratory failure. Biol Neonate. 2005;88:321–327. doi: 10.1159/000087630. [DOI] [PubMed] [Google Scholar]
- 13.Kurundkar AR, Killingsworth CR, McIlwain RB, Timpa JG, Hartman YE, He D, Karnatak RK, Neel ML, Clancy JP, Anantharamaiah GM, Maheshwari A. Extracorporeal membrane oxygenation causes loss of intestinal epithelial barrier in the newborn piglet. Pediatr Res. 2010;68:128–133. doi: 10.1203/PDR.0b013e3181e4c9f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reed RC, Rutledge JC. Laboratory and clinical predictors of thrombosis and hemorrhage in 29 pediatric extracorporeal membrane oxygenation nonsurvivors. Pediatr Dev Pathol. 2010;13:385–392. doi: 10.2350/09-09-0704-OA.1. [DOI] [PubMed] [Google Scholar]
- 15.Urlesberger B, Zobel G, Zenz W, Kuttnig-Haim M, Maurer U, Reiterer F, Riccabona M, Dacar D, Gallisti S, Leschnik B, Muntean W. Activation of the clotting system during extracorporeal membrane oxygenation in term newborn infants. J Pediatr. 1996;129:264–268. doi: 10.1016/s0022-3476(96)70252-4. [DOI] [PubMed] [Google Scholar]
- 16.Betrus C, Remenapp R, Charpie J, Kudelka T, Brophy P, Smoyer WE, Lin JJ. Enhanced hemolysis in pediatric patients requiring extracorporeal membrane oxygenation and continuous renal replacement therapy. Ann Thorac Cardiovasc Surg. 2007;13:378–383. [PubMed] [Google Scholar]
- 17.Toomasian JM, Bartlett RH. Hemolysis and ECMO pumps in the 21st century. Perfusion. 2011;26:5–6. doi: 10.1177/0267659110396015. [DOI] [PubMed] [Google Scholar]
- 18.Pohlmann JR, Toomasian JM, Hampton CE, Cook KE, Annich GM, Bartlett RH. The relationships between air exposure, negative pressure, and hemolysis. ASAIO J. 2009;55:469–473. doi: 10.1097/MAT.0b013e3181b28a5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gbadegesin R, Zhao S, Charpie J, Brophy PD, Smoyer WE, Lin JJ. Significance of hemolysis on extracorporeal life support after cardiac surgery in children. Pediatr Nephrol. 2009;24:589–595. doi: 10.1007/s00467-008-1047-z. [DOI] [PubMed] [Google Scholar]
- 20.Bartlett RH. Invited commentary. Ann Thorac Surg. 1997;63:1339. [Google Scholar]
- 21.Fleming G, Askenazi DJ, Bridges BC, Cooper DS, Paden ML, Selewski DT. A multicenter international survey of renal supportive therapy during ECMO: The Kidney Intervention During Extracorporeal Membrane Oxygenation (KIDMO) Group. ASAIO; In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldstein SL, Currier H, Graf Cd, Cosio CC, Brewer ED, Sachdevaland R. Outcome in children receiving continuous venovenous hemofiltration. Pediatrics. 2001;107:1309–1312. doi: 10.1542/peds.107.6.1309. [DOI] [PubMed] [Google Scholar]
- 23.Flores FX, Brophy PD, Symons JM, Fortenberry JD, Chua AN, Alexander SR, Mahan JD, Bunchman TE, Blowey D, Somers MJ, Baum M, Hackbarth R, Chand D, McBryde K, Benfield M, Goldstein SL. Continuous renal replacement therapy (CRRT) after stem cell transplantation. A report from the prospective pediatric CRRT Registry Group. Pediatr Nephrol. 2008;23:625–630. doi: 10.1007/s00467-007-0672-2. [DOI] [PubMed] [Google Scholar]
- 24.Michael M, Kuehnle I, Goldstein SL. Fluid overload and acute renal failure in pediatric stem cell transplant patients. Pediatr Nephrol. 2004;19:91–95. doi: 10.1007/s00467-003-1313-z. [DOI] [PubMed] [Google Scholar]
- 25.Sutherland SM, Zappitelli M, Alexander SR, Chua AN, Brophy PD, Bunchman TE, Hackbarth R, Somers MJ, Baum M, Symons JM, Flores FX, Benfield M, Askenazi D, Chand D, Fortenberry JD, Mahan JD, McBryde K, Blowey D, Goldstein SL. Fluid overload and mortality in children receiving continuous renal replacement therapy: The prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis. 2010;55:316–325. doi: 10.1053/j.ajkd.2009.10.048. [DOI] [PubMed] [Google Scholar]
- 26.Goldstein SL, Somers MJ, Baum MA, Symons JM, Brophy PD, Blowey D, Bunchman TE, Baker C, Mottes T, McAfee N, Barnett J, Morrison G, Rogers K, Fortenberry JD. Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int. 2005;67:653–658. doi: 10.1111/j.1523-1755.2005.67121.x. [DOI] [PubMed] [Google Scholar]
- 27.Gillespie RS, Seidel K, Symons JM. Effect of fluid overload and dose of replacement fluid on survival in hemofiltration. Pediatr Nephrol. 2004;19:1394–1399. doi: 10.1007/s00467-004-1655-1. [DOI] [PubMed] [Google Scholar]
- 28.Selewski DT, Cornell TT, Lombel RM, Blatt NB, Han YY, Mottes T, Kommareddi M, Kershaw DB, Shanley TP, Heung M. Weight-based determination of fluid overload status and mortality in pediatric intensive care unit patients requiring continuous renal replacement therapy. Intensive Care Med. 2011;37:1166–1173. doi: 10.1007/s00134-011-2231-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arikan AA, Zappitelli M, Goldstein SL, Naipaul A, Jefferson LS, Loftis LL. Fluid overload is associated with impaired oxygenation and morbidity in critically ill children [published online ahead of print July 14, 2011] Pediatr Crit Care Med. doi: 10.1097/PCC.0b013e31822882a3. [DOI] [PubMed] [Google Scholar]
- 30.Hayes LW, Oster RA, Tofil NM, Tolwani AJ. Outcomes of critically ill children requiring continuous renal replacement therapy. J Crit Care. 2009;24:394–400. doi: 10.1016/j.jcrc.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 31.Fu¨ lo¨ p T, Pathak MB, Schmidt DW, Lengva´rszky Z, Juncos JP, Lebrun CJ, Brar H, Juncos LA. Volume-related weight gain and subsequent mortality in acute renal failure patients treated with continuous renal replacement therapy. ASAIO J. 2010;56:333–337. doi: 10.1097/MAT.0b013e3181de35e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sakr Y, Vincent JL, Reinhart K, Groeneveld J, Michalopoulos A, Sprung CL, Artigas A, Ranieri VM, Sepsis Occurence in Acutely Ill Patients Investigators High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest. 2005;128:3098–3108. doi: 10.1378/chest.128.5.3098. [DOI] [PubMed] [Google Scholar]
- 33.Upadya A, Tilluckdharry L, Muralidharan V, Amoateng-Adjepong Y, Manthous CA. Fluid balance and weaning out-comes. Intensive Care Med. 2005;31:1643–1647. doi: 10.1007/s00134-005-2801-3. [DOI] [PubMed] [Google Scholar]
- 34.Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF, Jr, Hite RD, Harabin AL, National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- 35.Heung M, Wolfgram DF, Kommareddi M, Hu Y, Song PX, Ojo AO. Fluid overload at initiation of renal replacement therapy is associated with lack of renal recovery in patients with acute kidney injury. Nephrol Dial Transplant. 2012;27:956–961. doi: 10.1093/ndt/gfr470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Anderson HL, 3rd, Coran AG, Drongowski RA, Ha HJ, Bartlett RH. Extracellular fluid and total body water changes in neonates undergoing extracorporeal membrane oxygenation. J Pediatr Surg. 1992;27:1003–1007. doi: 10.1016/0022-3468(92)90547-k. discussion 1007–1008. [DOI] [PubMed] [Google Scholar]
- 37.Swaniker F, Kolla S, Moler F, Custer J, Grams R, Barlett R, Hirschl R. Extracorporeal life support outcome for 128 pediatric patients with respiratory failure. J Pediatr Surg. 2000;35:197–202. doi: 10.1016/s0022-3468(00)90009-5. [DOI] [PubMed] [Google Scholar]
- 38.Blijdorp K, Cransberg K, Wildschut ED, Gischler SJ, Jan Houmes R, Wolff ED, Tibboel D. Haemofiltration in newborns treated with extracorporeal membrane oxygenation: A case-comparison study. Crit Care. 2009;13:R48. doi: 10.1186/cc7771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kelly RE, Jr, Phillips JD, Foglia RP, Bjerke HS, Barcliff LT, Petrus L, Hall TR. Pulmonary edema and fluid mobilization as determinants of the duration of ECMO support. J Pediatr Surg. 1991;26:1016–1022. doi: 10.1016/0022-3468(91)90665-g. [DOI] [PubMed] [Google Scholar]
- 40.Hoover NG, Heard M, Reid C, Wagoner S, Rogers K, Foland J, Paden ML, Fortenberry JD. Enhanced fluid management with continuous venovenous hemofiltration in pediatric respiratory failure patients receiving extracorporeal membrane oxygenation support. Intensive Care Med. 2008;34:2241–2247. doi: 10.1007/s00134-008-1200-y. [DOI] [PubMed] [Google Scholar]
- 41.Cavagnaro F, Kattan J, Godoy L, Gonza´les A, Vogel A, Rodrıguez JI, Faunes M, Fajardo C, Becker P. Continuous renal replacement therapy in neonates and young infants during extracorporeal membrane oxygenation. Int J Artif Organs. 2007;30:220–226. doi: 10.1177/039139880703000307. [DOI] [PubMed] [Google Scholar]
- 42.Extracorporeal Life Support Organization. Guidelines. Available at: http://www.elso.med.umich.edu/Guidelines.html. Accessed March 8, 2012.
- 43.Bagshaw SM, Delaney A, Haase M, Ghali WA, Bellomo R. Loop diuretics in the management of acute renal failure: A systematic review and meta-analysis. Crit Care Resusc. 2007;9:60–68. [PubMed] [Google Scholar]
- 44.Ho KM, Sheridan DJ. Meta-analysis of frusemide to prevent or treat acute renal failure. BMJ. 2006;333:420. doi: 10.1136/bmj.38902.605347.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Meyer RJ, Brophy PD, Bunchman TE, Annich GM, Maxvold NJ, Mottes TA, Custer JR. Survival and renal function in pediatric patients following extracorporeal life support with hemofiltration. Pediatr Crit Care Med. 2001;2:238–242. doi: 10.1097/00130478-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 46.Paden ML, Warshaw BL, Heard ML, Fortenberry JD. Recovery of renal function and survival after continuous renal replacement therapy during extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2011;12:153–158. doi: 10.1097/PCC.0b013e3181e2a596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ingyinn M, Rais-Bahrami K, Evangelista R, Hogan I, Rivera O, Mikesell GT, Short BL. Comparison of the effect of venovenous versus venoarterial extracorporeal membrane oxygenation on renal blood flow in newborn lambs. Perfusion. 2004;19:163–170. doi: 10.1191/0267659104pf736oa. [DOI] [PubMed] [Google Scholar]
- 48.Goldstein SL. Overview of pediatric renal replacement therapy in acute renal failure. Artif Organs. 2003;27:781–785. doi: 10.1046/j.1525-1594.2003.07281.x. [DOI] [PubMed] [Google Scholar]
- 49.Ronco C, Bellomo R, Ricci Z. Continuous renal replacement therapy in critically ill patients. Nephrol Dial Transplant. 2001;16(Suppl 5):67–72. doi: 10.1093/ndt/16.suppl_5.67. [DOI] [PubMed] [Google Scholar]
- 50.Maxvold NJ, Bunchman TE. Renal failure and renal replacement therapy. Crit Care Clin. 2003;19:563–575. doi: 10.1016/s0749-0704(03)00010-1. [DOI] [PubMed] [Google Scholar]
- 51.Murphy RS, Wilcox SJ. High risk infusions—accuracy compromised by changes in patient venous pressure. J Med Eng Technol. 2009;33:470–474. doi: 10.1080/03091900902952659. [DOI] [PubMed] [Google Scholar]
- 52.Murphy RS, Wilcox SJ. The link between intravenous multiple pump flow errors and infusion system mechanical compliance. Anesth Analg. 2010;110:1297–1302. doi: 10.1213/ANE.0b013e3181d56758. [DOI] [PubMed] [Google Scholar]
- 53.Jenkins R, Chen B, Funk JE. Maximum ultrafiltration rate in continuous arteriovenous hemofiltration does not occur at the lowest level of the ultrafiltrate collection chamber. ASAIO J. 1993;39:M618–M620. [PubMed] [Google Scholar]
- 54.Sucosky P, Dasi LP, Paden ML, Fortenberry JD, Yoganathan AP. Assessment of current continuous hemofiltration systems and development of a novel accurate fluid management system for use in extracorporeal membrane oxygenation. J Med Devices. 2008;2:035002. [Google Scholar]
- 55.Santiago MJ, Sa´ nchez A, Lo´ pez-Herce J, Pe´rez R, del Castillo J, Urbano J, Carrillo A. The use of continuous renal replacement therapy in series with extracorporeal membrane oxygenation. Kidney Int. 2009;76:1289–1292. doi: 10.1038/ki.2009.383. [DOI] [PubMed] [Google Scholar]
- 56.Goldstein SL, Chawla LS. Renal angina. Clin J Am Soc Nephrol. 2010;5:943–949. doi: 10.2215/CJN.07201009. [DOI] [PubMed] [Google Scholar]
- 57.Elbahlawan L, West NK, Avent Y, Cheng C, Liu W, Barfield RC, Jones DP, Rajasekaran S, Morrison RR. Impact of continuous renal replacement therapy on oxygenation in children with acute lung injury after allogeneic hematopoietic stem cell transplantation. Pediatr Blood Cancer. 2010;55:540–545. doi: 10.1002/pbc.22561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL, Program to Improve Care in Acute Renal Disease (PICARD) Study Group Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76:422–427. doi: 10.1038/ki.2009.159. [DOI] [PubMed] [Google Scholar]
- 59.Foland JA, Fortenberry JD, Warshaw BL, Pettignano R, Merritt RK, Heard ML, Rogers K, Reid C, Tanner AJ, Easley KA. Fluid overload before continuous hemofiltration and survival in critically ill children: a retrospective analysis. Crit Care Med. 2004;32:1771–1776. doi: 10.1097/01.ccm.0000132897.52737.49. [DOI] [PubMed] [Google Scholar]


